First trimester screening E Keshavarz MD Langdon Down
- Slides: 36
First trimester screening E. Keshavarz MD
�Langdon Down (London 1866) �Subgroup of idiots…. Down syndrome(mongolian people) �Down’s theory: retrogression of ethnic type �(Darwin’s contemporary scientific reasoning for evolution) �Theory was not true but 100 years later: �Skin: dirty yellowish tinge skin and is deficient in elasticity, giving the appearance of being too large for the body
� 1866: congenital, dating from intrauterine life � 1909: association with maternal age � 1914: no increased within families � 1914: syphilis, TB, epilepsy, alcholism, insanity, nervous e instability , endocrine abnormalities(thyroid , adrenal , pitiutary , thymus) � 1932: diz. t: un. equally monoz. t: equally transmission from mother to the baby *** 1934: unequal migration of chromosomes during cell division…trisomy
� 1960: familial Down syndrome translocation(15: 21), no trisomy 1961: mosaism type of Down syndrome mosaism of normal and trisomic cells 1966: karyotyping of cultured amniotic fluid cells
�Whole or a segment of long arm of ch 21 is in three copies: 1 -non dysjunction(95%) 2 -translocation 3 -mosaicism � 1991: 95% of non dysjunction: maternal origin
Only amniocentesis ! � 1 -private health care system: >35 y was 5% now 10% and more! 2 - NHS: 5% pregnant mothers…>37 -40 y only 30% of trisomy 21 babies !
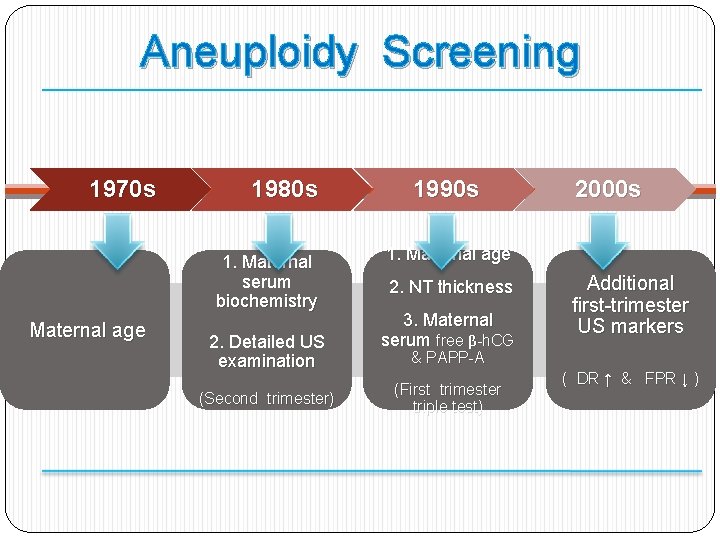
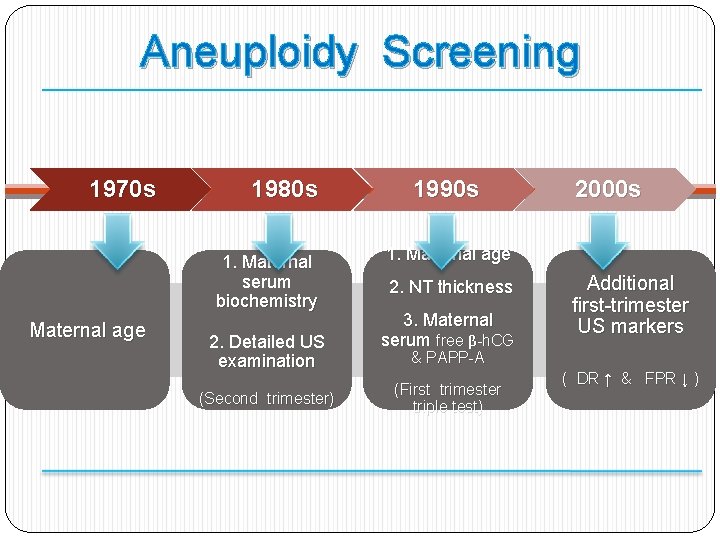
Aneuploidy Screening 1970 s 1980 s 1. Maternal serum biochemistry Maternal age 2. Detailed US examination (Second trimester) 1990 s 2000 s 1. Maternal age 2. NT thickness 3. Maternal serum free β-h. CG Additional first-trimester US markers & PAPP-A (First trimester triple test) ( DR ↑ & FPR ↓ )
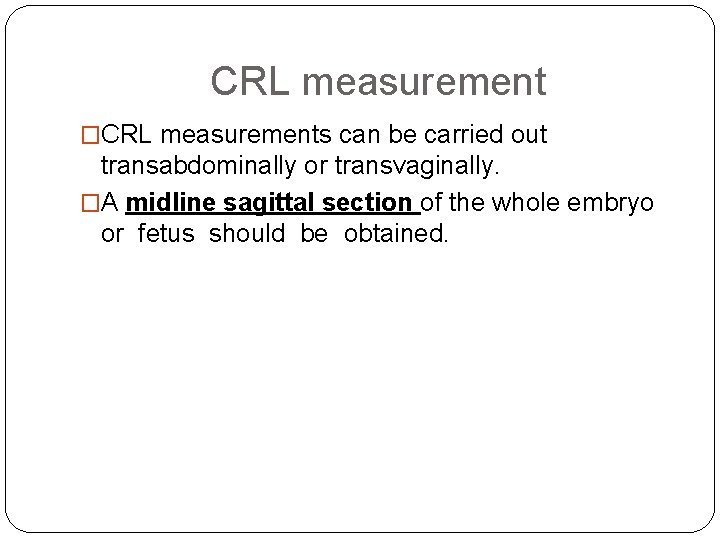
CRL measurement �CRL measurements can be carried out transabdominally or transvaginally. �A midline sagittal section of the whole embryo or fetus should be obtained.
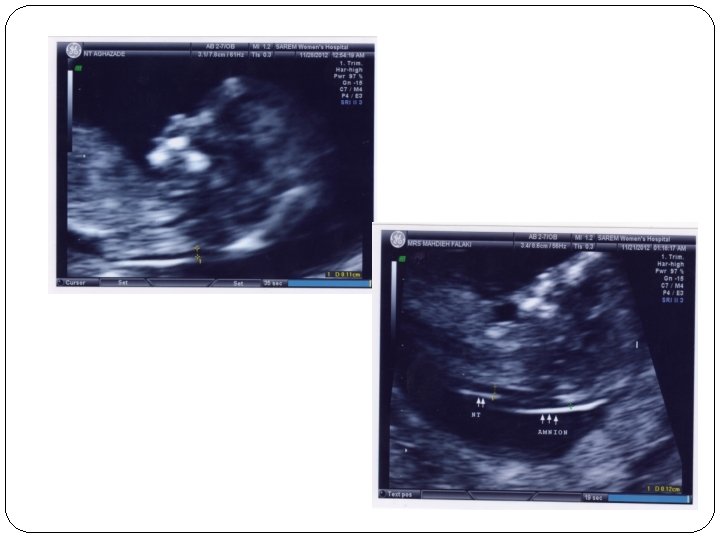
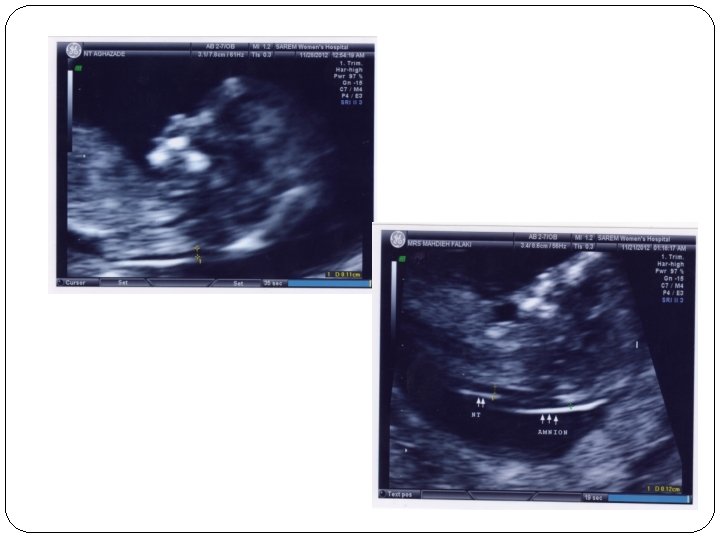
NT measurement - CRL: 45 -84 mm (11 w-13 w 6 d) - TAS(95% success)=TVS(other 5%) - Waiting for spontaneous fetal movement, asking the mother to cough, tapping the maternal abdomen(amnion membrane!)
NT measurement - Good work after 80 -100 sonography and at least 10 min - Study on 100, 000 cases: normal: 1. 2 (11 w) to 1. 9(13 w 6 d) abnormal: above the 95 th centile(>=3 mm)
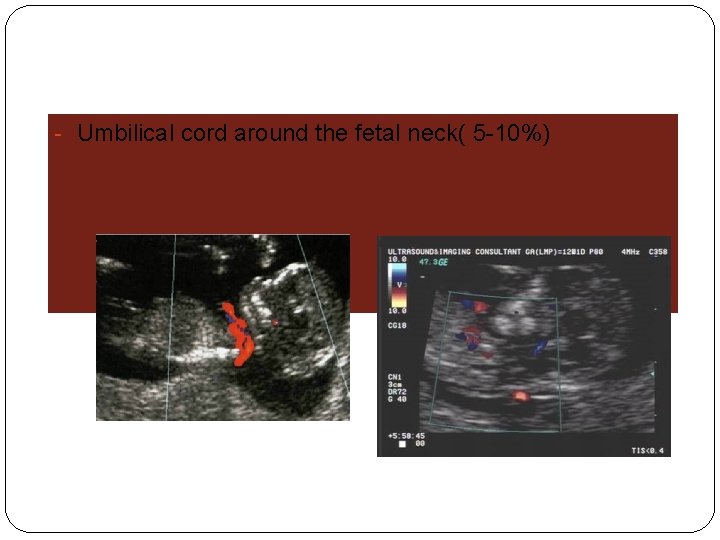
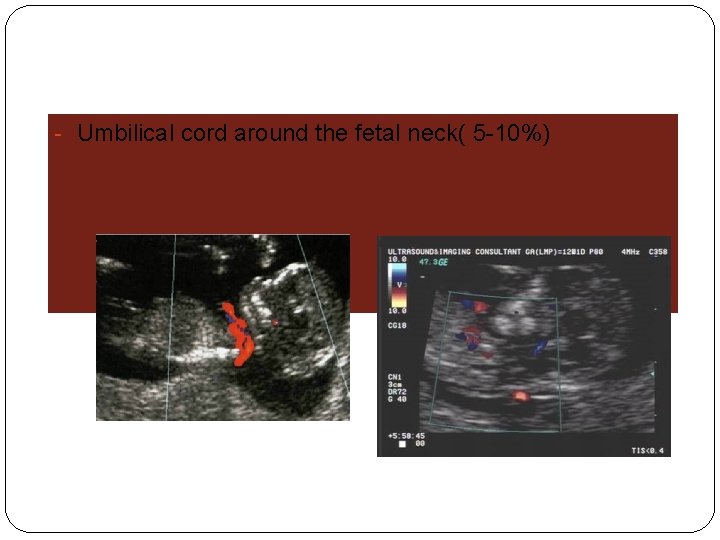
- Umbilical cord around the fetal neck( 5 -10%)
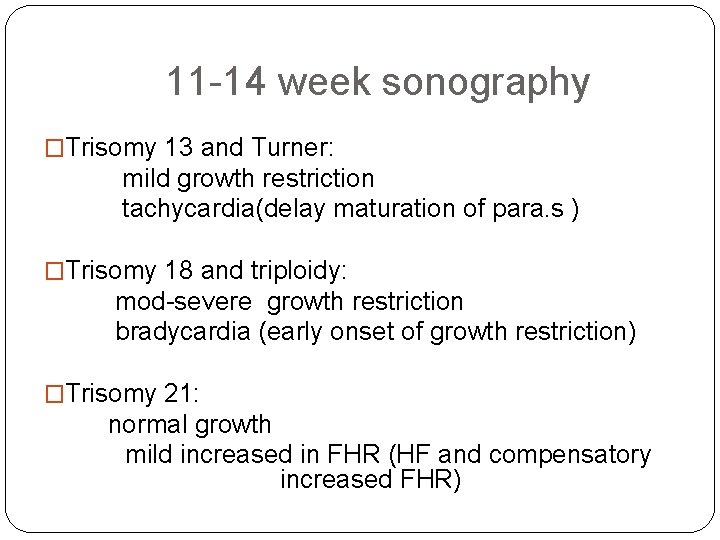
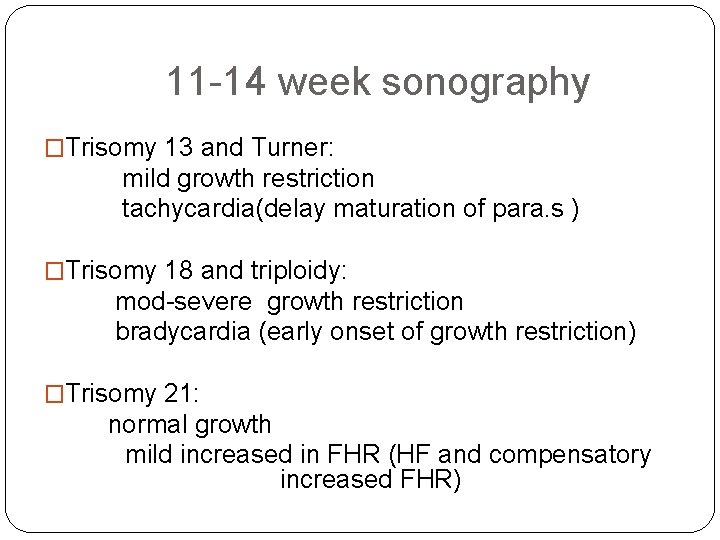
11 -14 week sonography �Trisomy 13 and Turner: mild growth restriction tachycardia(delay maturation of para. s ) �Trisomy 18 and triploidy: mod-severe growth restriction bradycardia (early onset of growth restriction) �Trisomy 21: normal growth mild increased in FHR (HF and compensatory increased FHR)
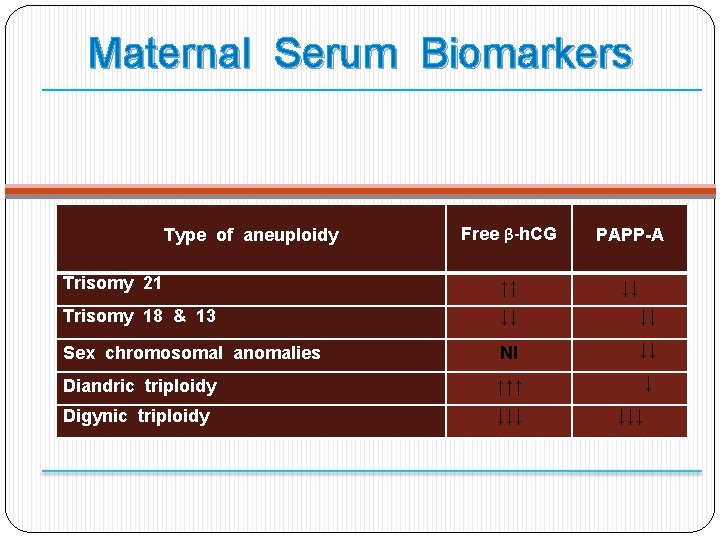
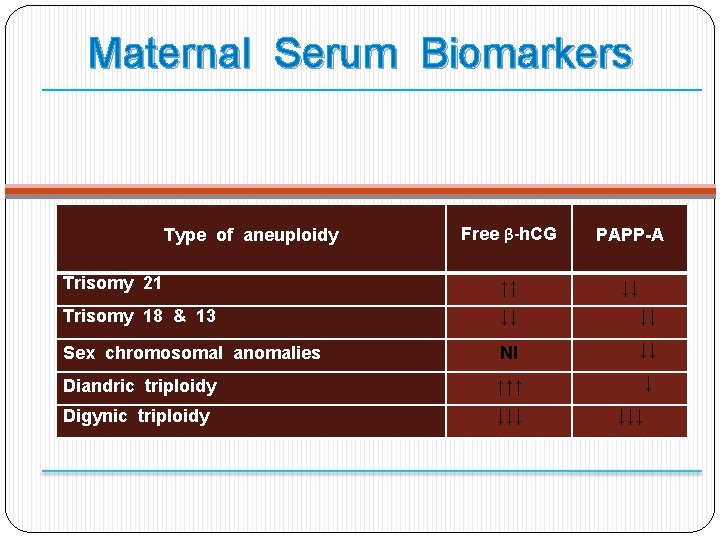
Maternal Serum Biomarkers Free β-h. CG PAPP-A Trisomy 21 ↑↑ ↓↓ Trisomy 18 & 13 ↓↓ ↓↓ Sex chromosomal anomalies Nl ↓↓ Diandric triploidy ↑↑↑ ↓ Digynic triploidy ↓↓↓ Type of aneuploidy ↓↓↓
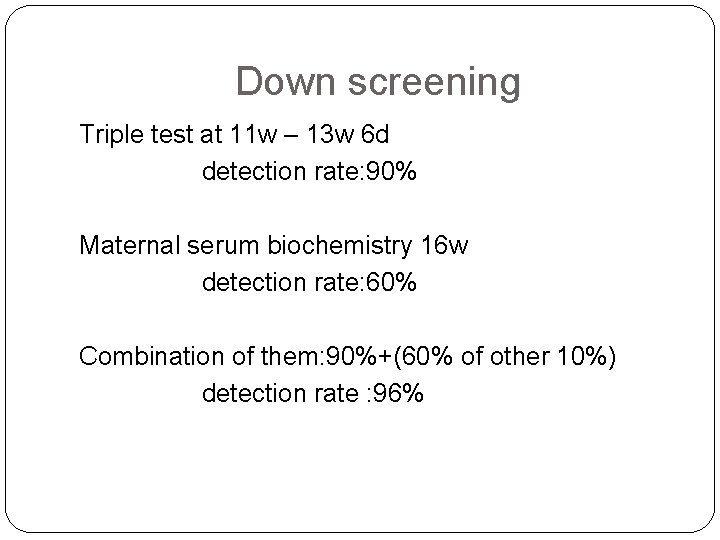
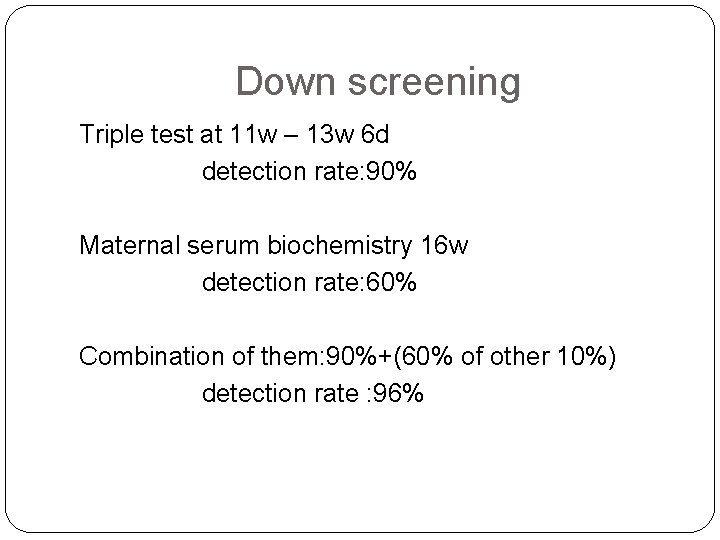
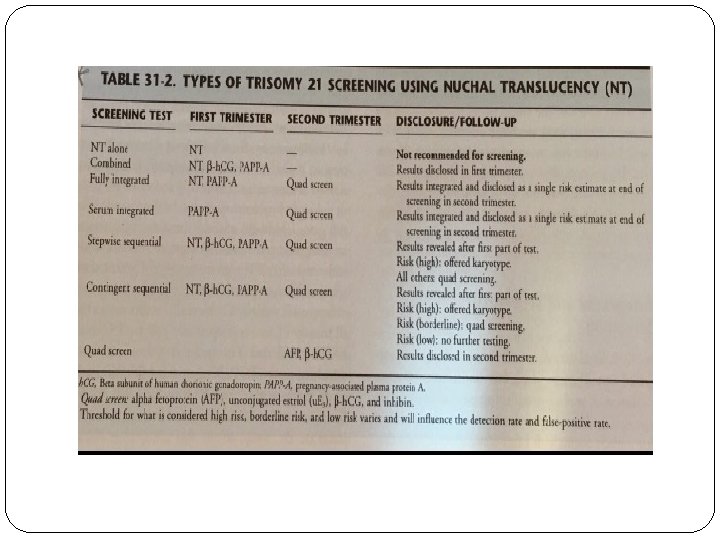
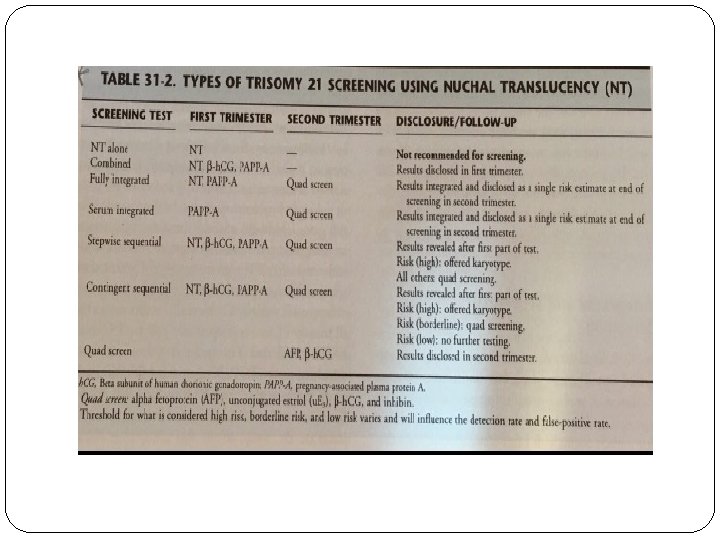
Down screening Triple test at 11 w – 13 w 6 d detection rate: 90% Maternal serum biochemistry 16 w detection rate: 60% Combination of them: 90%+(60% of other 10%) detection rate : 96%
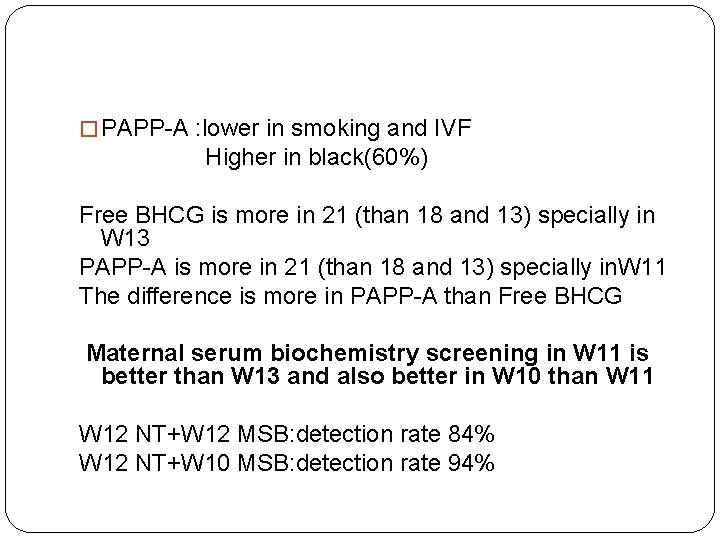
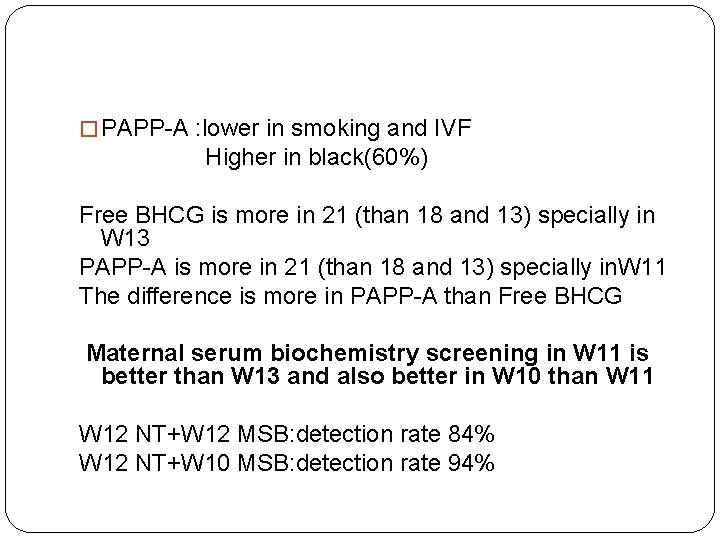
� PAPP-A : lower in smoking and IVF Higher in black(60%) Free BHCG is more in 21 (than 18 and 13) specially in W 13 PAPP-A is more in 21 (than 18 and 13) specially in. W 11 The difference is more in PAPP-A than Free BHCG Maternal serum biochemistry screening in W 11 is better than W 13 and also better in W 10 than W 11 W 12 NT+W 12 MSB: detection rate 84% W 12 NT+W 10 MSB: detection rate 94%
OSCAR �New methods of biochemical testing within 30 min(time-resolved-amplified-cryptateemission)+ NT at the same time: �One Step Clinics for Assessment of Risk
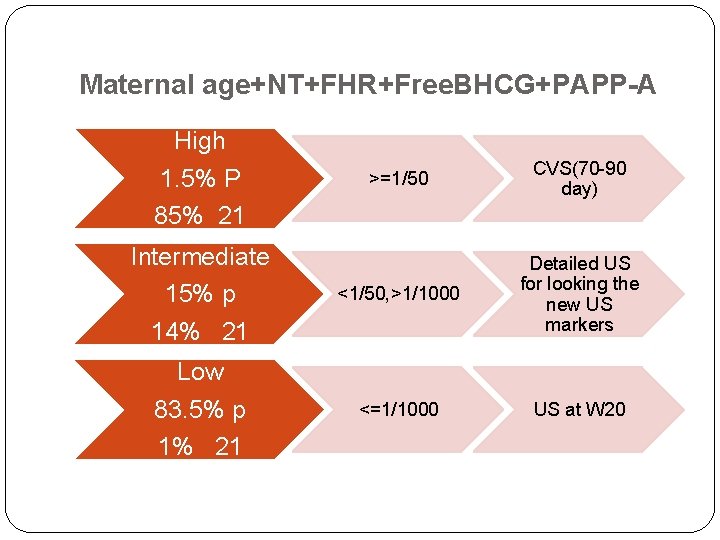
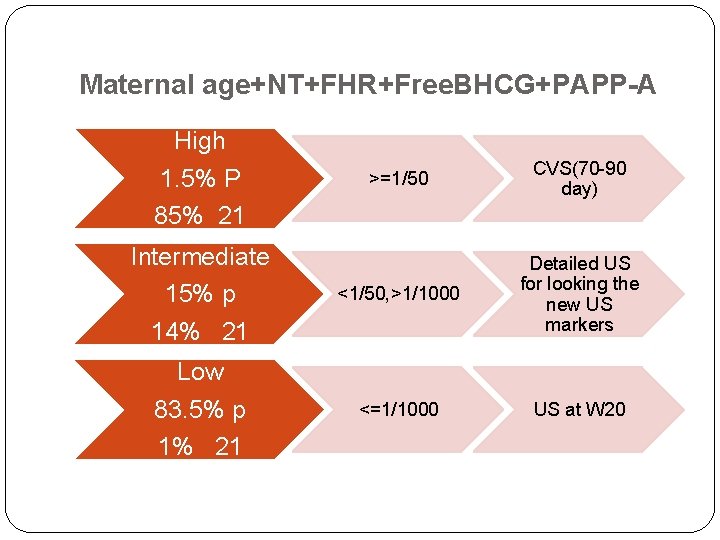
Maternal age+NT+FHR+Free. BHCG+PAPP-A High 1. 5% P 85% 21 >=1/50 CVS(70 -90 day) Intermediate 15% p 14% 21 <1/50, >1/1000 Detailed US for looking the new US markers Low 83. 5% p 1% 21 <=1/1000 US at W 20
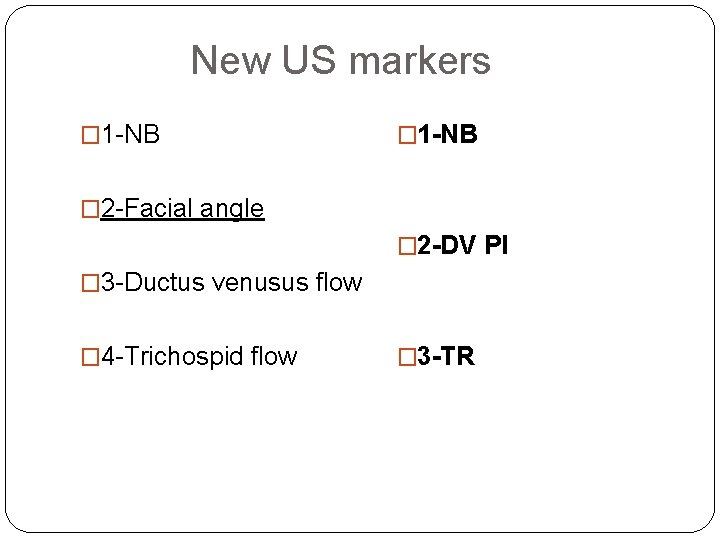
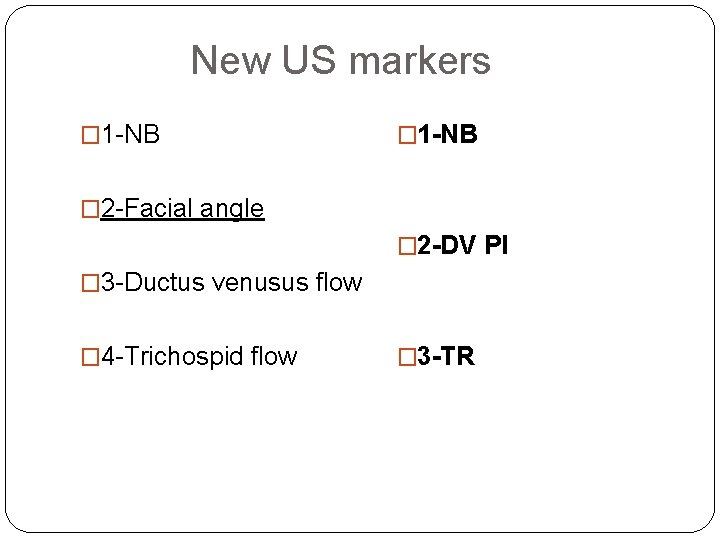
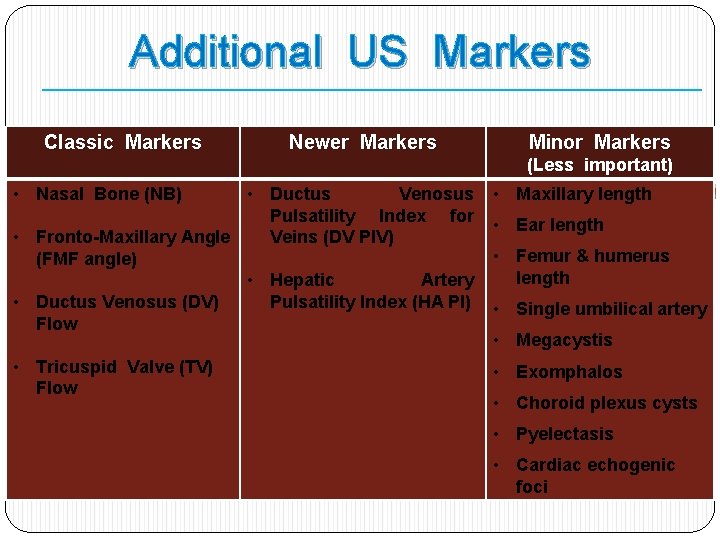
New US markers � 1 -NB � 2 -Facial angle � 2 -DV PI � 3 -Ductus venusus flow � 4 -Trichospid flow � 3 -TR
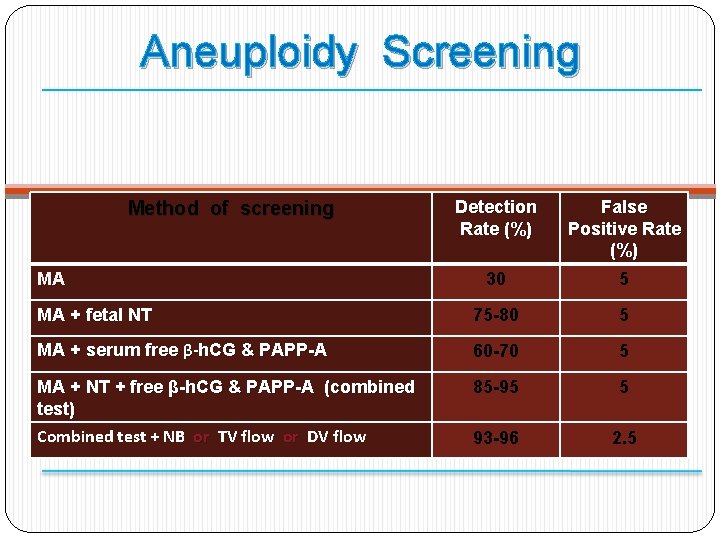
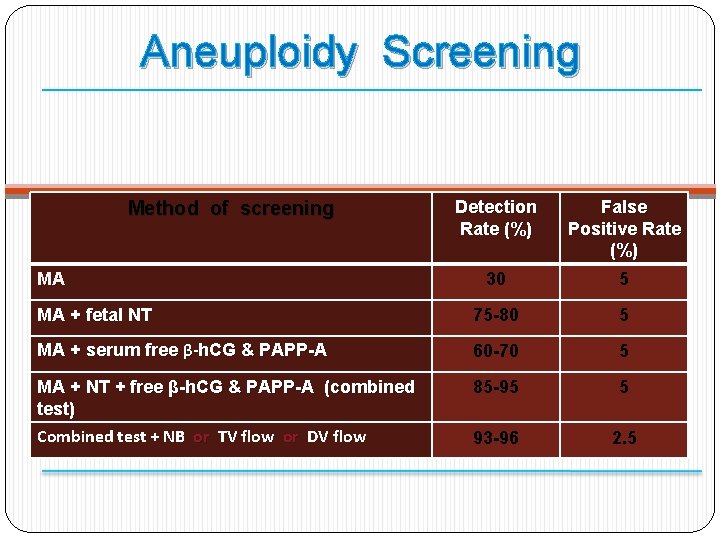
Aneuploidy Screening Detection Rate (%) False Positive Rate (%) 30 5 MA + fetal NT 75 -80 5 MA + serum free β-h. CG & PAPP-A 60 -70 5 MA + NT + free β-h. CG & PAPP-A (combined test) Combined test + NB or TV flow or DV flow 85 -95 5 93 -96 2. 5 Method of screening MA
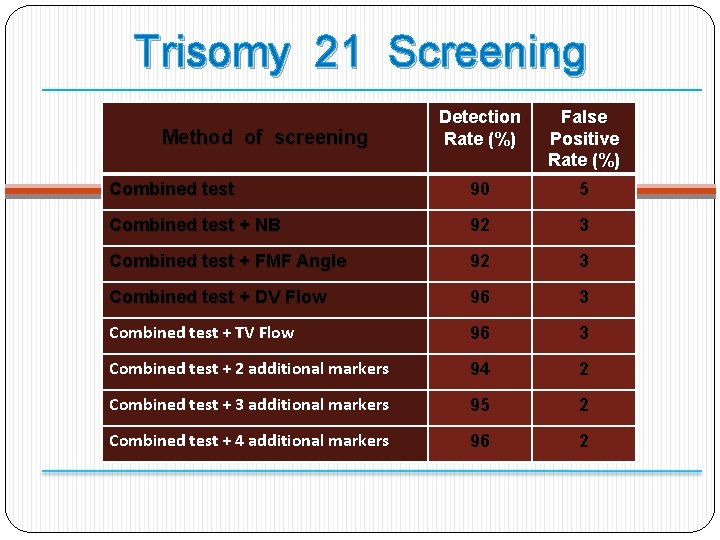
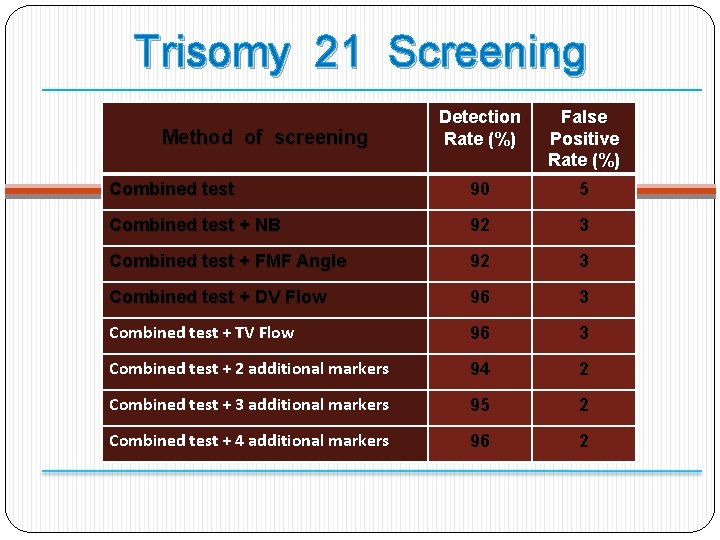
Trisomy 21 Screening Detection Rate (%) False Positive Rate (%) Combined test 90 5 Combined test + NB 92 3 Combined test + FMF Angle 92 3 Combined test + DV Flow 96 3 Combined test + TV Flow 96 3 Combined test + 2 additional markers 94 2 Combined test + 3 additional markers 95 2 Combined test + 4 additional markers 96 2 Method of screening
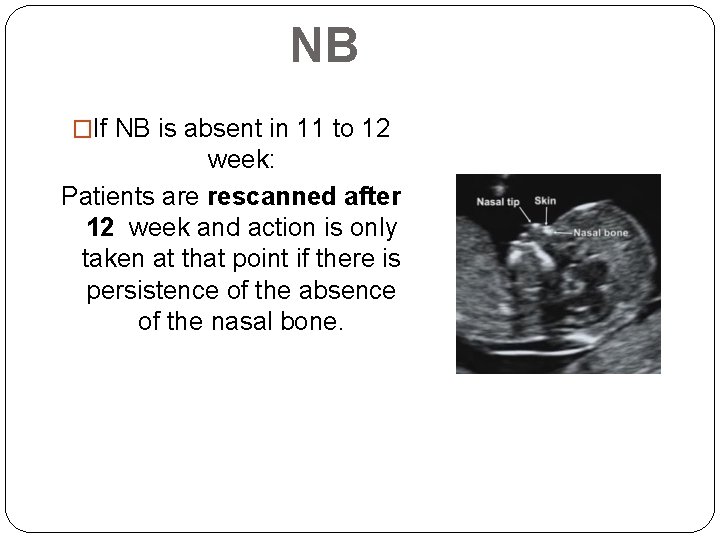
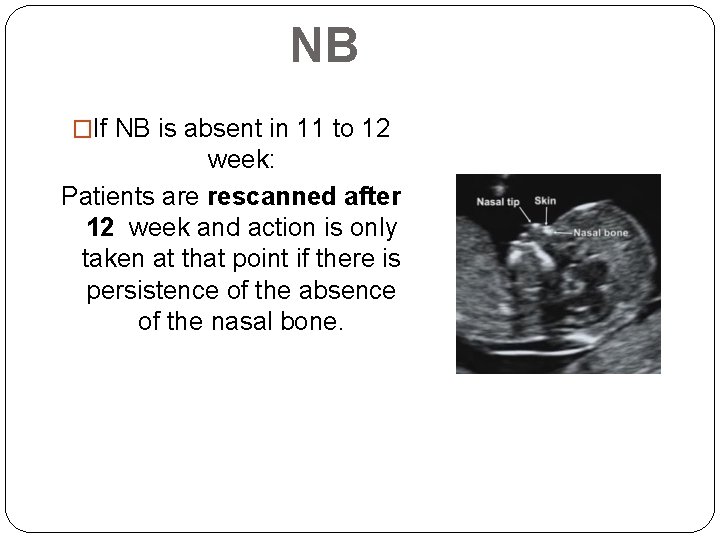
NB �If NB is absent in 11 to 12 week: Patients are rescanned after 12 week and action is only taken at that point if there is persistence of the absence of the nasal bone.
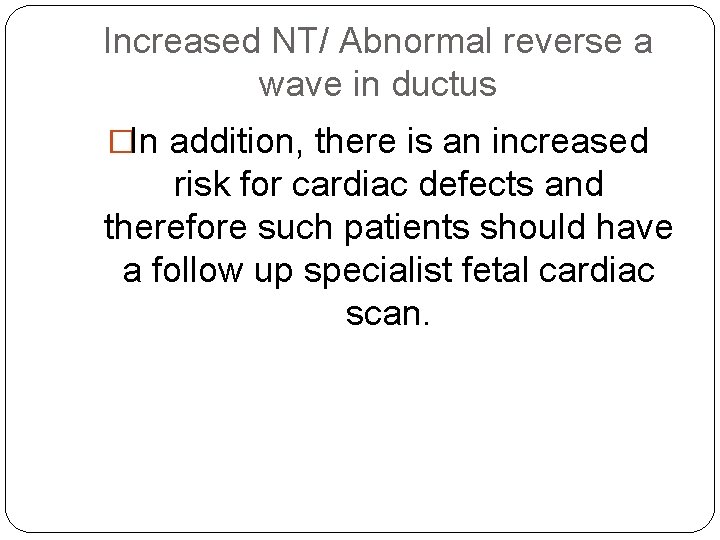
Increased NT/ Abnormal reverse a wave in ductus �In addition, there is an increased risk for cardiac defects and therefore such patients should have a follow up specialist fetal cardiac scan.
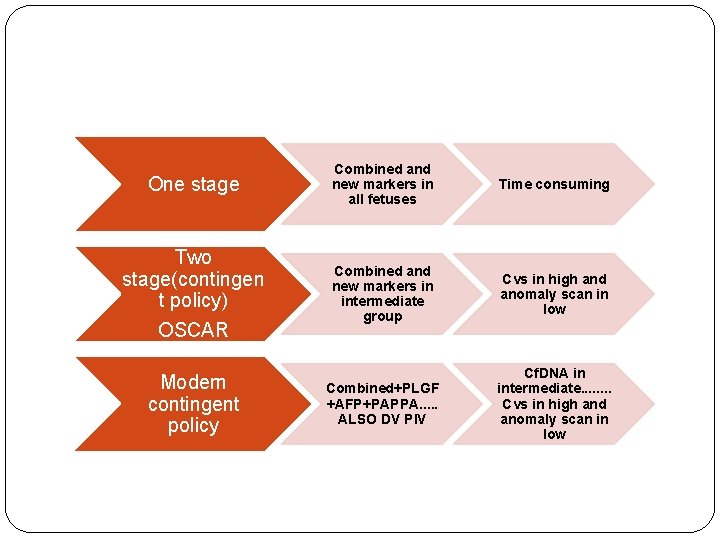
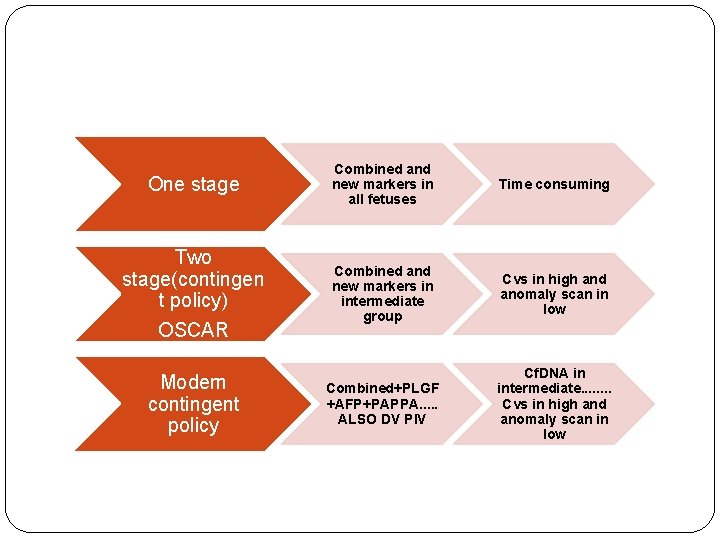
One stage Two stage(contingen t policy) OSCAR Modern contingent policy Combined and new markers in all fetuses Time consuming Combined and new markers in intermediate group Cvs in high and anomaly scan in low Combined+PLGF +AFP+PAPPA. . . ALSO DV PIV Cf. DNA in intermediate. . . . Cvs in high and anomaly scan in low
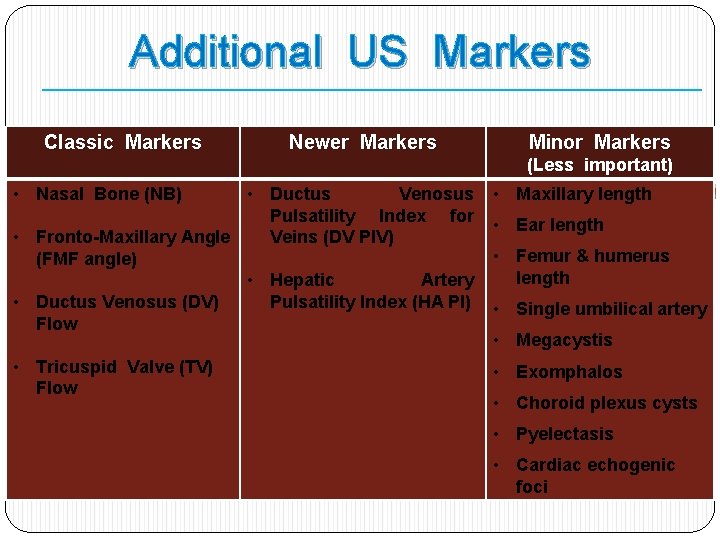
Additional US Markers Classic Markers Newer Markers Minor Markers (Less important) • Nasal Bone (NB) • Ductus Venosus Pulsatility Index for Veins (DV PIV) • Fronto-Maxillary Angle (FMF angle) • Hepatic Artery Pulsatility Index (HA PI) • Ductus Venosus (DV) Flow • Maxillary length • Tricuspid Valve (TV) Flow • Exomphalos • Ear length • Femur & humerus length • Single umbilical artery • Megacystis • Choroid plexus cysts • Pyelectasis • Cardiac echogenic foci
Preeclampsia
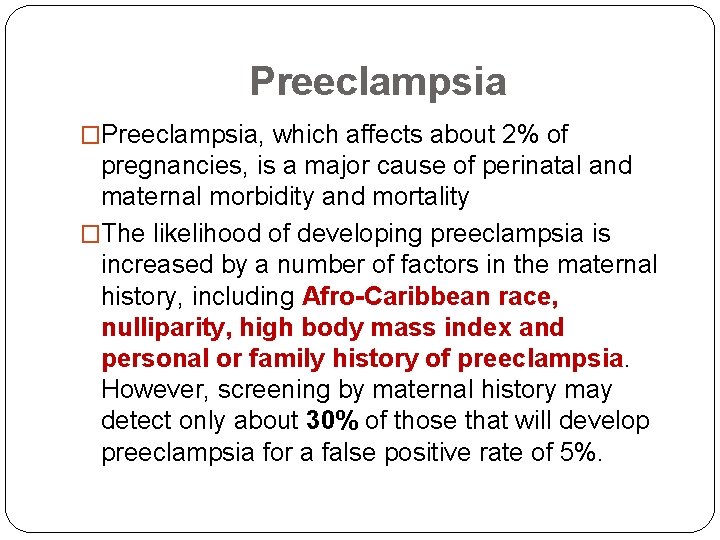
Preeclampsia �Preeclampsia, which affects about 2% of pregnancies, is a major cause of perinatal and maternal morbidity and mortality �The likelihood of developing preeclampsia is increased by a number of factors in the maternal history, including Afro-Caribbean race, nulliparity, high body mass index and personal or family history of preeclampsia. However, screening by maternal history may detect only about 30% of those that will develop preeclampsia for a false positive rate of 5%.
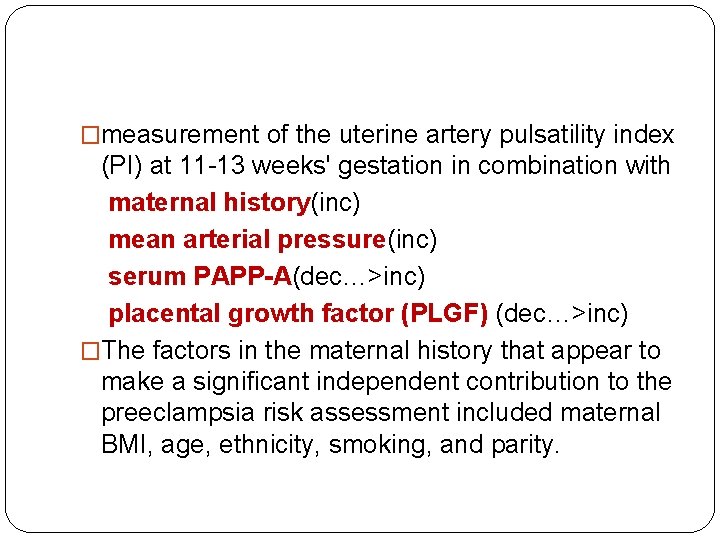
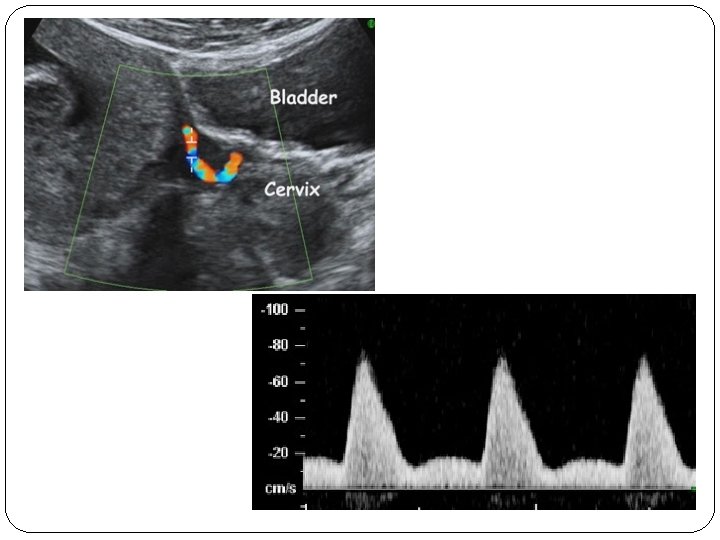
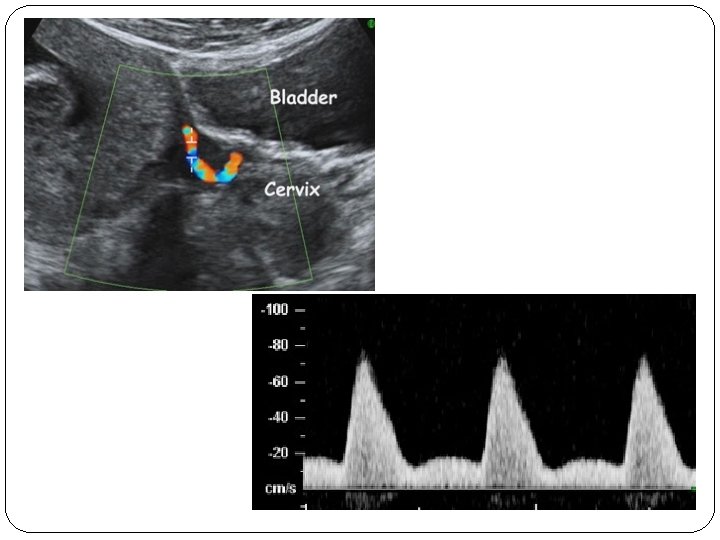
�measurement of the uterine artery pulsatility index (PI) at 11 -13 weeks' gestation in combination with maternal history(inc) mean arterial pressure(inc) serum PAPP-A(dec…>inc) placental growth factor (PLGF) (dec…>inc) �The factors in the maternal history that appear to make a significant independent contribution to the preeclampsia risk assessment included maternal BMI, age, ethnicity, smoking, and parity.
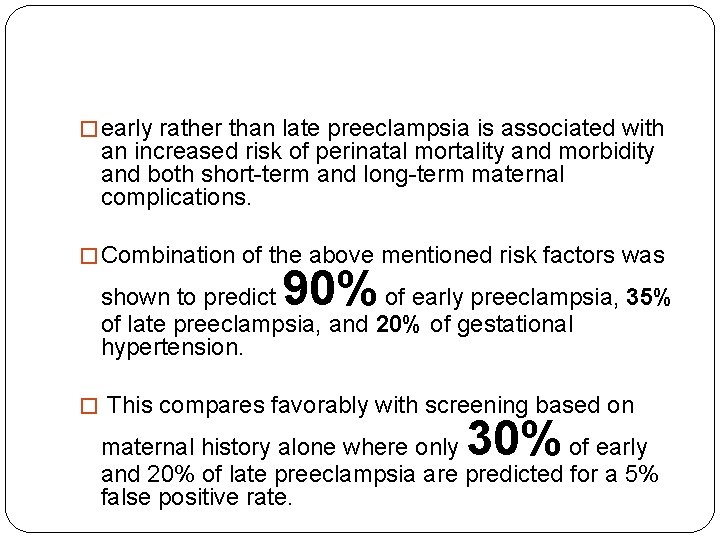
� early rather than late preeclampsia is associated with an increased risk of perinatal mortality and morbidity and both short-term and long-term maternal complications. � Combination of the above mentioned risk factors was 90% shown to predict of early preeclampsia, 35% of late preeclampsia, and 20% of gestational hypertension. � This compares favorably with screening based on 30% maternal history alone where only of early and 20% of late preeclampsia are predicted for a 5% false positive rate.
Gender Determination
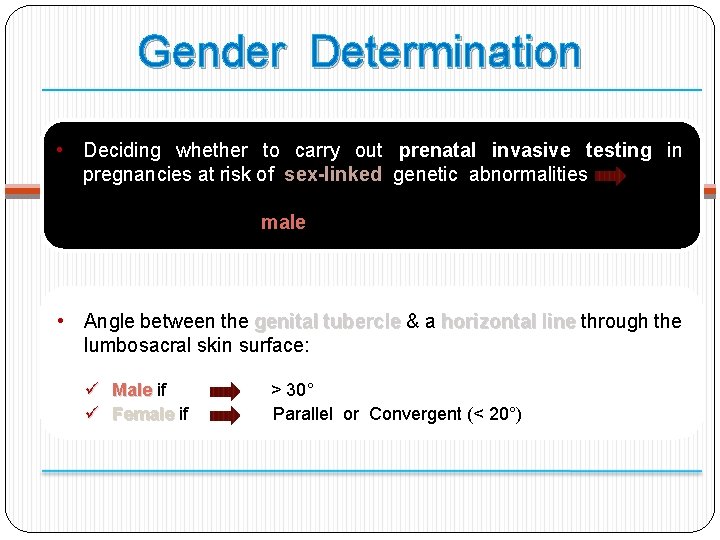
Gender Determination • Deciding whether to carry out prenatal invasive testing in pregnancies at risk of sex-linked genetic abnormalities Just necessary in male fetuses • Angle between the genital tubercle & a horizontal line through the lumbosacral skin surface: ü ü Male if Female if > 30° Parallel or Convergent (< 20°)
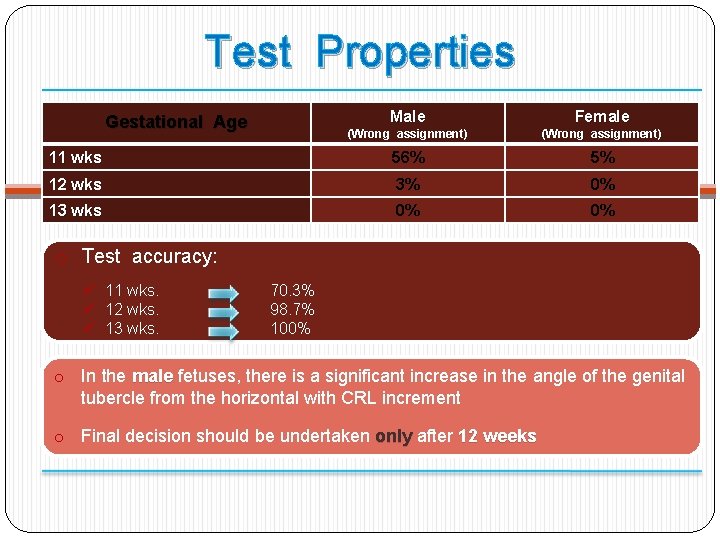
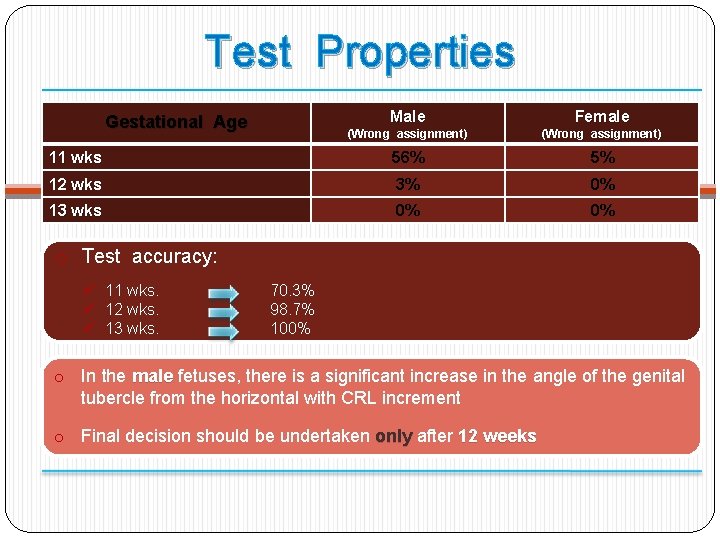
Test Properties Male Female (Wrong assignment) 11 wks 56% 5% 12 wks 3% 0% 13 wks 0% 0% Gestational Age o Test accuracy: ü 11 wks. ü 12 wks. ü 13 wks. 70. 3% 98. 7% 100% o In the male fetuses, there is a significant increase in the angle of the genital tubercle from the horizontal with CRL increment o Final decision should be undertaken only after 12 weeks
Thank you