Second trimester miscrriage A late or second trimester
- Slides: 7
Second trimester miscrriage A late or second trimester miscarriage occures between 12 -24 weeks gestation. After 24 weeks gestation the baby is potentially viable and birth is refered to as pre term delivery.
Aetiology : The likely aetiology behind second trimester losses varies with gestation. At 12 -15 weeks , the predominant causes are those of first trimester miscarriage - fetal chromosomal and structural anomalies and possibly endocrine causes. At the latter part of the second trimester , between 19 and 23 weeks , the commonest factors underlying the miscarriages wil be those of very pre term births , these include ascending genital tract infection , intrauterine bleeding and cervical weakness. The weakness may be congenital or acquired through procedures such as cone biopsy or repeated cervical dilatation. Epidemiological risk factors for second trimester miscarriage include poor socioeconomic status , smoking , genital tract infections , previous miscarriage or premature birth and increasing maternal age. Amniosetesis a procedure performed at 16 -18 weeks gestation is associate with o. 5 % of subsequent pregnancy loss
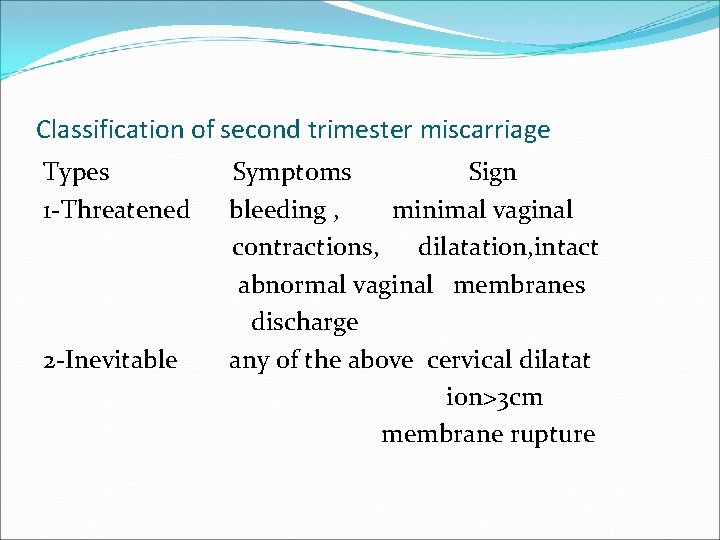
Classification of second trimester miscarriage Types 1 -Threatened 2 -Inevitable Symptoms Sign bleeding , minimal vaginal contractions, dilatation, intact abnormal vaginal membranes discharge any of the above cervical dilatat ion>3 cm membrane rupture
3 -Missed 4 -Septic usually none fetal death on US above and malaise fever, tachycardia hypotention, uterine tenderness Investigations : 1 -urine sample for infection 2 -cevical swabs for infection 3 - full blood count for anemia , leukocytosis 4 - blood group Rh if –ve give ante D
Trans abdominal ultrasound to confirm gestation and viability , and assess amniotic fluid volume. Transvaginal ultrasound for cervical length measurement. Differential diagnosis : 1 -Bowel disorders: conctipation , colitis , gastrointeritis. 2 -Urinary disorders : infection , renal stone disease. 3 -cervical disorders: ectropion , leucorrhoea. neoplasia. 4 - uterine disorders: red degeneration of fibroids , round ligaments stretching.
Treatment Support this include sympathy , explanations , pain relieve and reassurance. If the pre viable membrane rupture precise diagnosis should be confirmed by speculum examination and follow up ultrasound scan if no contraction and no sign of infection no urgency to interfere but severe oligohydramnia carry risk of fetal lung hypo plasia. Carful observation of body temperature , and changing vaginal discharge or lower uterine tenderness are recommended. Established chorioamnitis needs delivery. Antibiotics should be given during follow up of the patient during expectant management.
Tocolytics : There is currently no place for tocolysis in the prevention of mid trimester pregnancy loss , tocolytics only used for short term i. e. 48 hours prolongation of pregnancy. Emergency cervical circulage when the cervical canal is opened and the membrane is bulging it is suitable to insert suture around the cervix to close it after reducing the membrane. Bleeding , infection and contractions are contraindications. Delivery : adequate pain relief should offered , these deliveries are usually vaginal and quick.