Drugs interactions and precautions Alex Moores MRPharm S


- Slides: 70
Drugs, interactions and precautions Alex Moores MRPharm. S Pg. Dip. Clin. Pharm Independent Pharmacist Prescriber
Clinical Pharmacist Prescriber in primary care • • Long-term condition clinics Lead for medicines management Medication reviews Point of call for clinical team • • Drug interactions Medication queries Best practice advice Polypharmacy
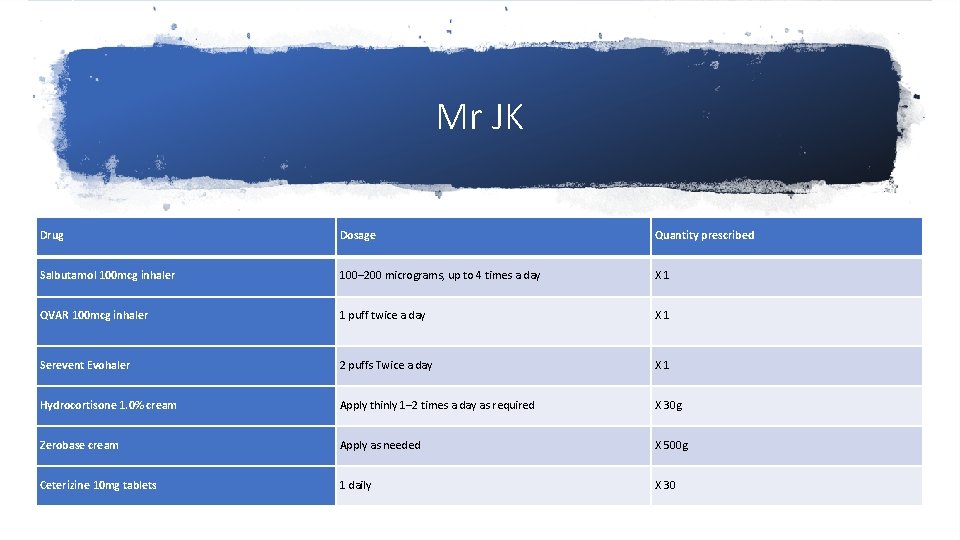
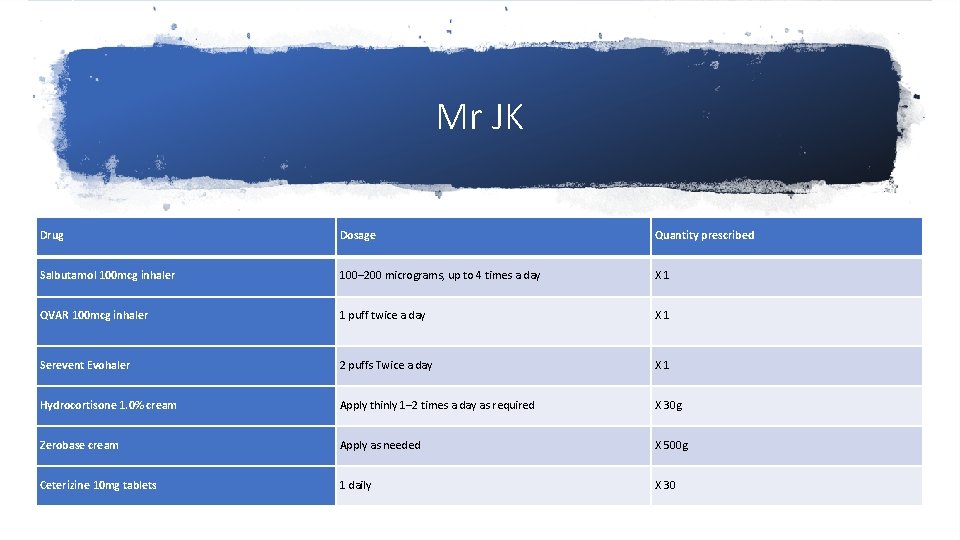
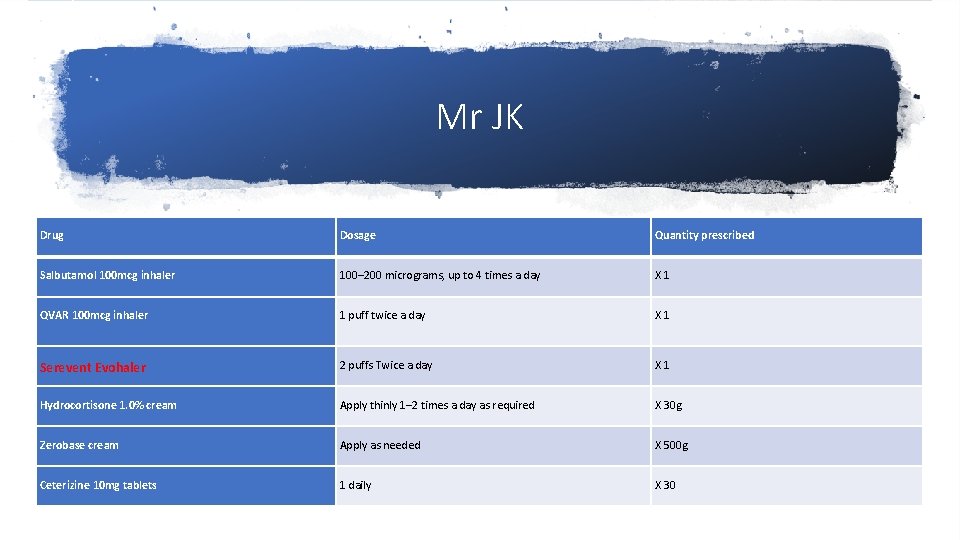
Mr JK Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day X 1 QVAR 100 mcg inhaler 1 puff twice a day X 1 Serevent Evohaler 2 puffs Twice a day X 1 Hydrocortisone 1. 0% cream Apply thinly 1– 2 times a day as required X 30 g Zerobase cream Apply as needed X 500 g Ceterizine 10 mg tablets 1 daily X 30
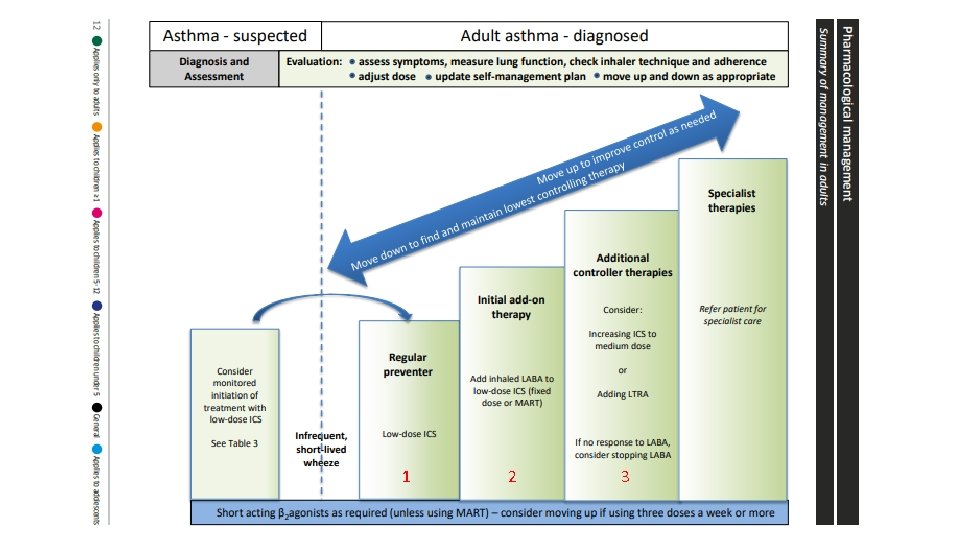
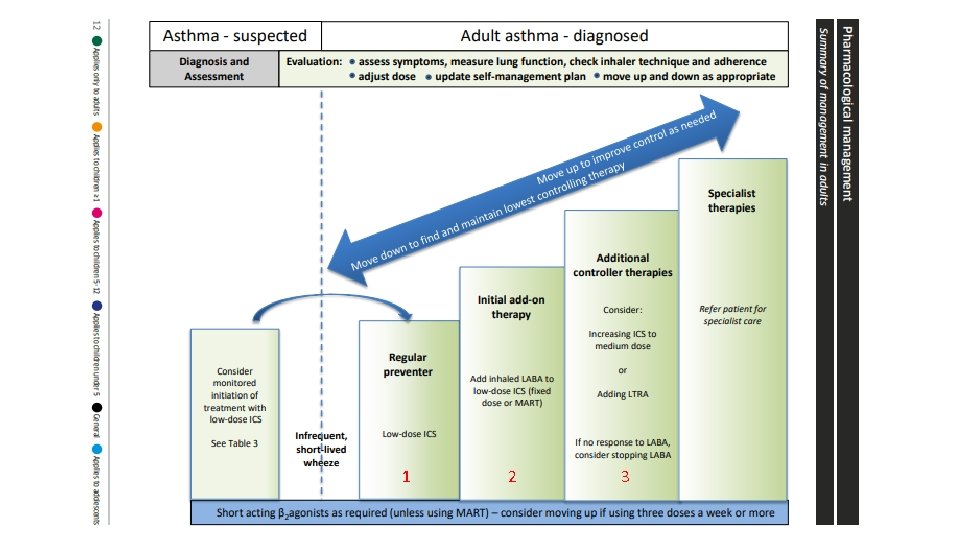
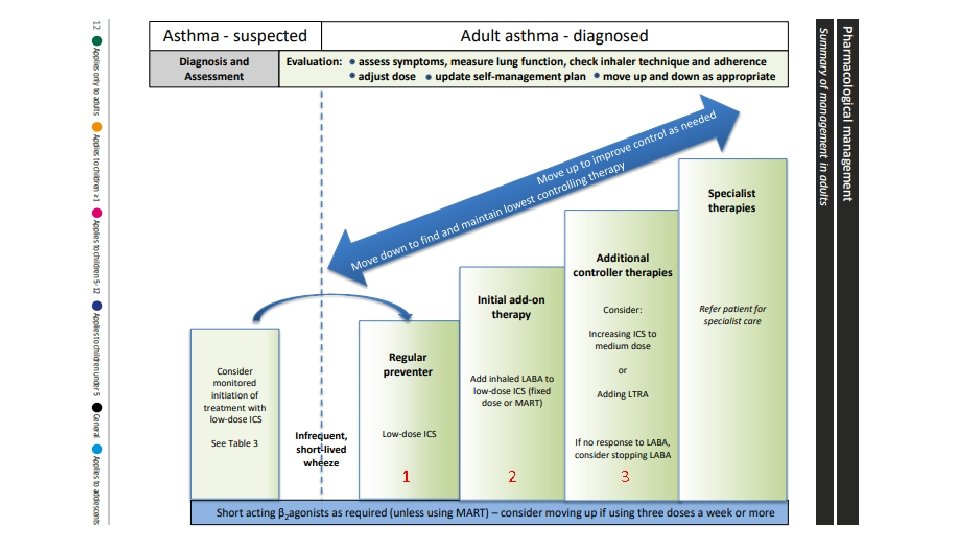
1 2 3
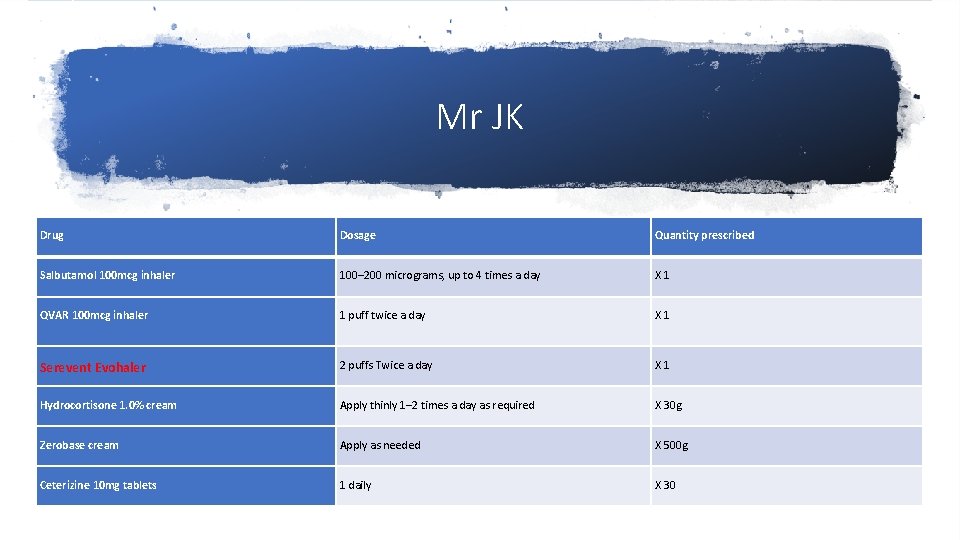
Mr JK Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day X 1 QVAR 100 mcg inhaler 1 puff twice a day X 1 Serevent Evohaler 2 puffs Twice a day X 1 Hydrocortisone 1. 0% cream Apply thinly 1– 2 times a day as required X 30 g Zerobase cream Apply as needed X 500 g Ceterizine 10 mg tablets 1 daily X 30
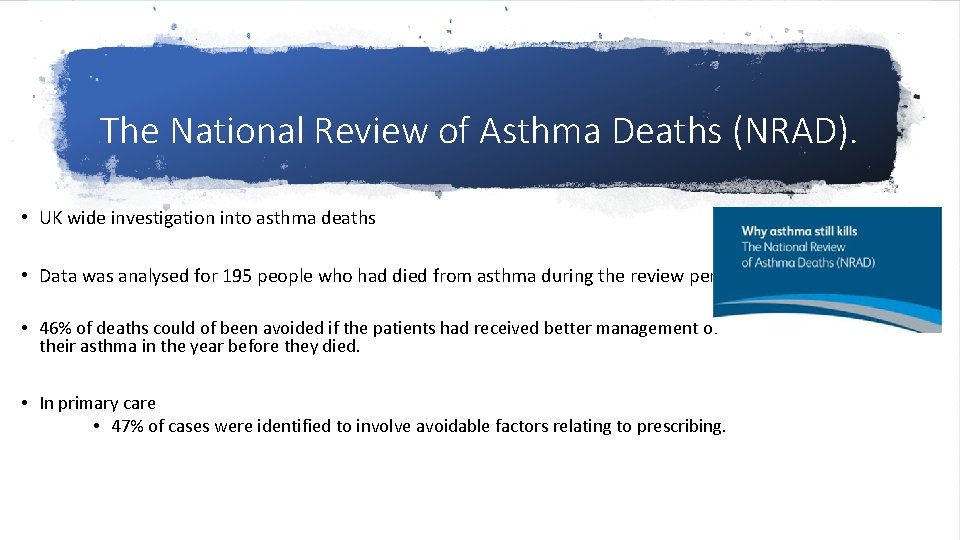
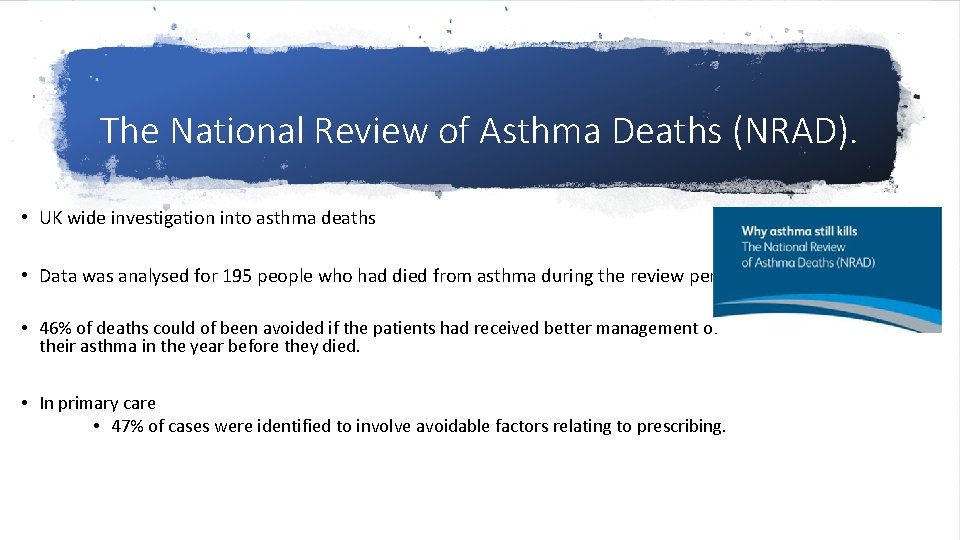
The National Review of Asthma Deaths (NRAD). • UK wide investigation into asthma deaths • Data was analysed for 195 people who had died from asthma during the review period. • 46% of deaths could of been avoided if the patients had received better management of their asthma in the year before they died. • In primary care • 47% of cases were identified to involve avoidable factors relating to prescribing.

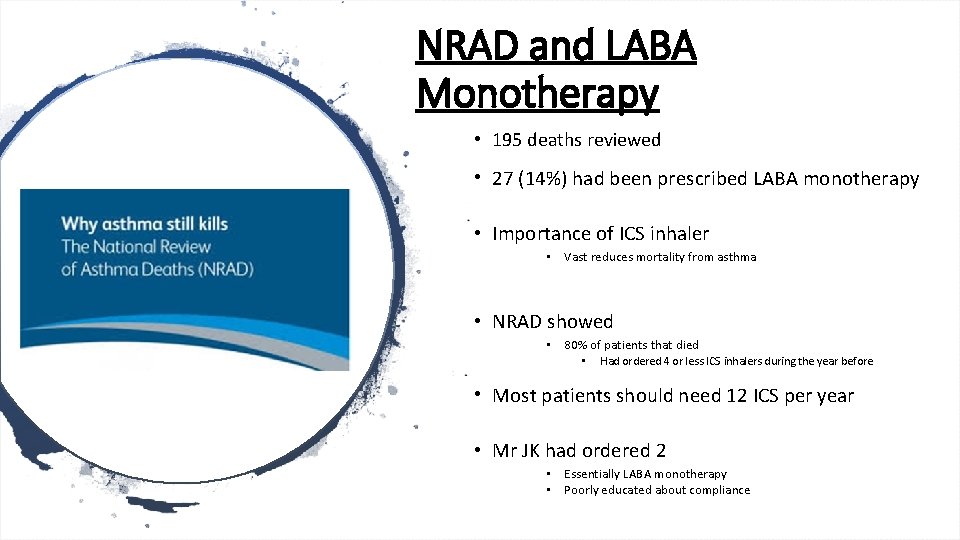
• Major concern LABA Monotherapy • Prescribing LABA inhalers without an ICS • Associated with increased mortality • Unlicensed
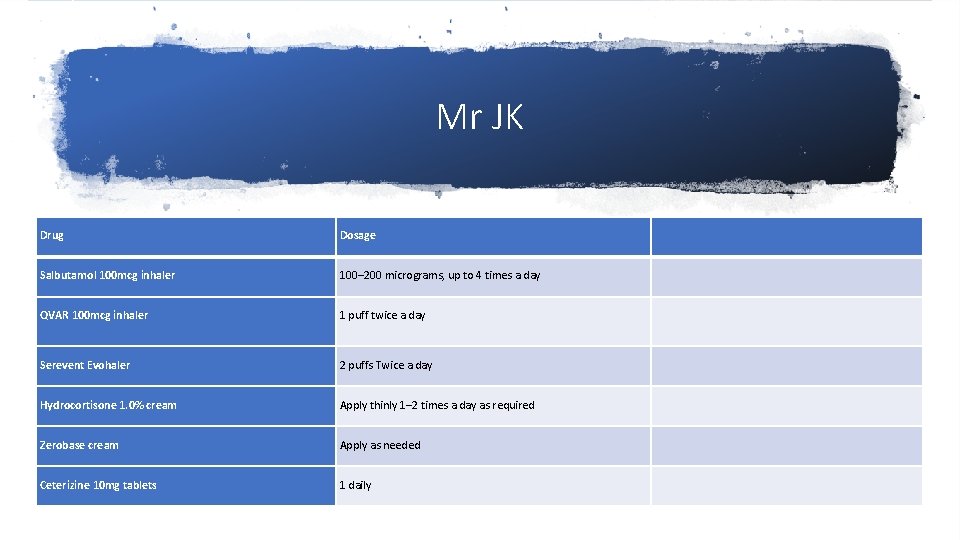
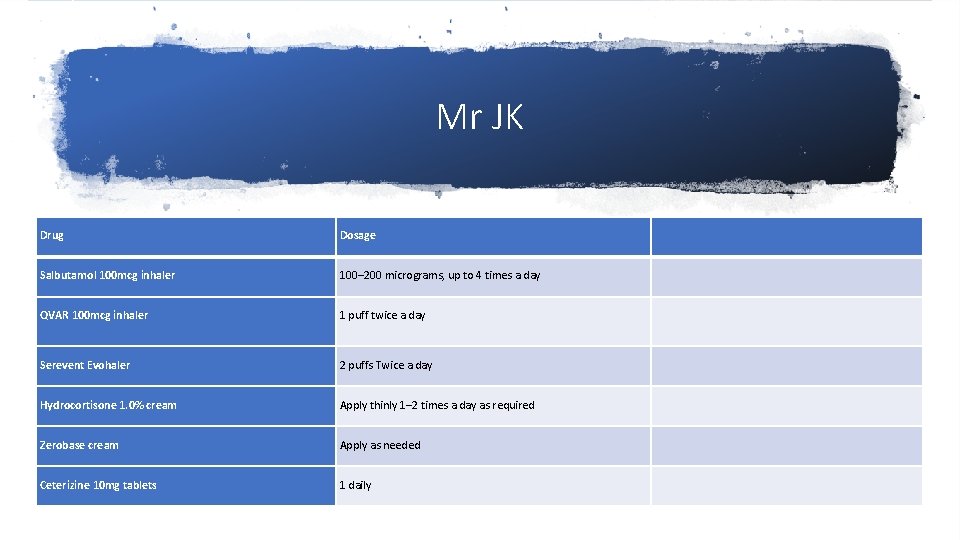
Mr JK Drug Dosage Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day QVAR 100 mcg inhaler 1 puff twice a day Serevent Evohaler 2 puffs Twice a day Hydrocortisone 1. 0% cream Apply thinly 1– 2 times a day as required Zerobase cream Apply as needed Ceterizine 10 mg tablets 1 daily
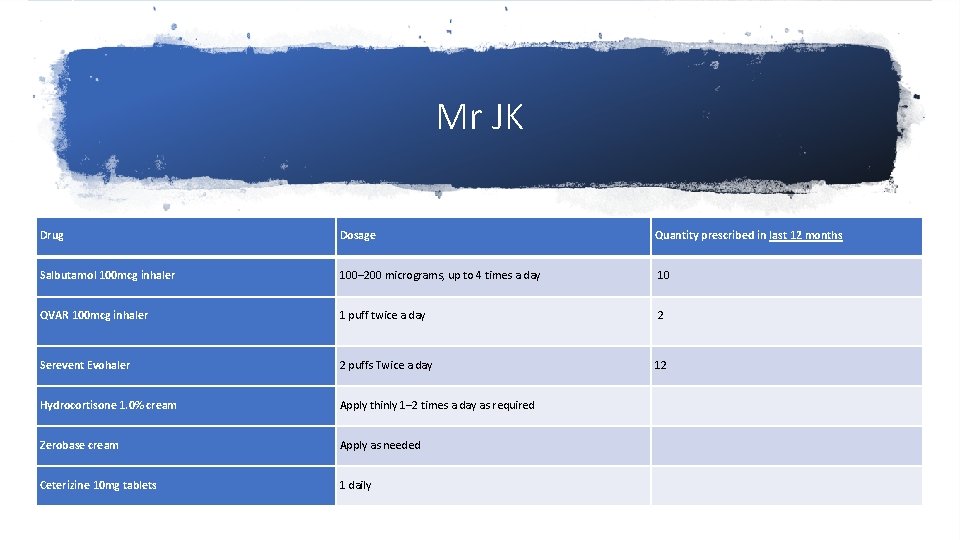
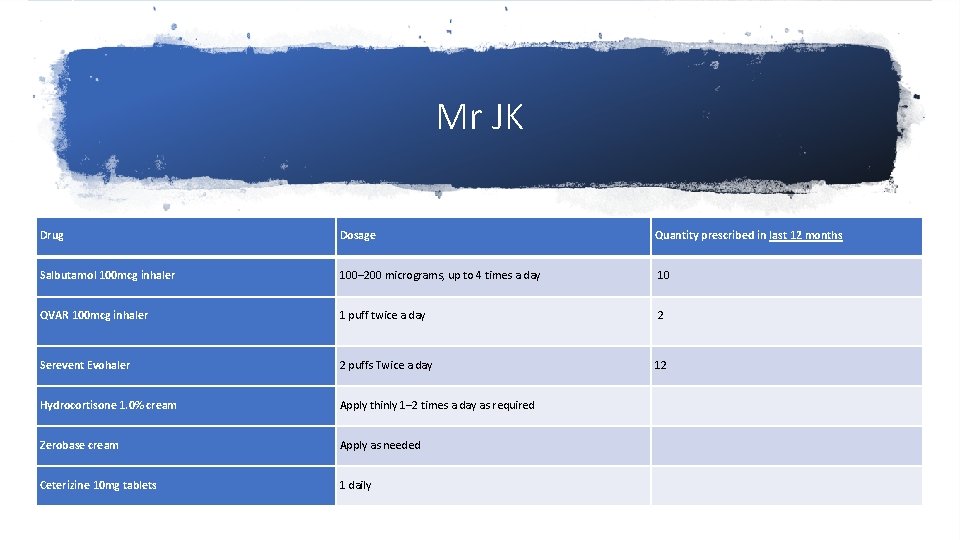
Mr JK Drug Dosage Quantity prescribed in last 12 months Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 10 QVAR 100 mcg inhaler 1 puff twice a day 2 Serevent Evohaler 2 puffs Twice a day 12 Hydrocortisone 1. 0% cream Apply thinly 1– 2 times a day as required Zerobase cream Apply as needed Ceterizine 10 mg tablets 1 daily
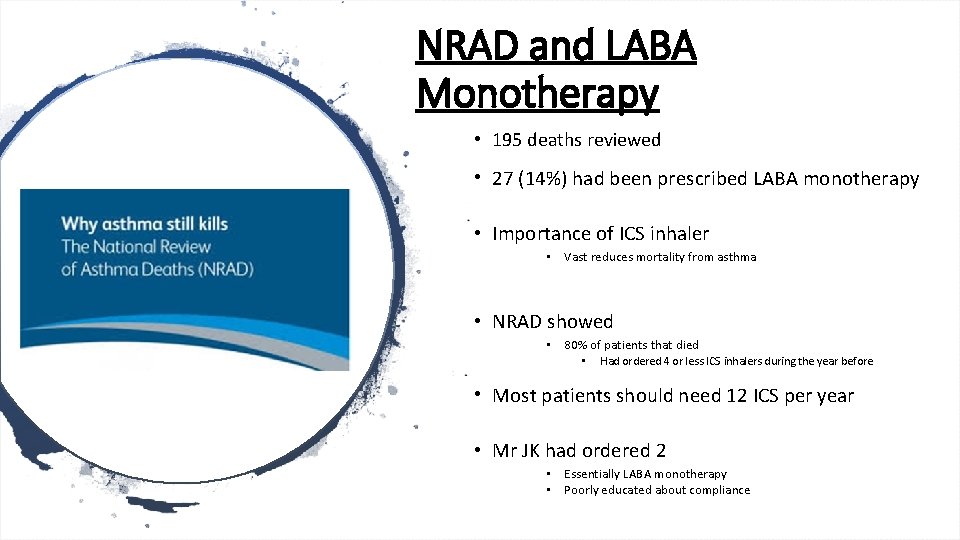
NRAD and LABA Monotherapy • 195 deaths reviewed • 27 (14%) had been prescribed LABA monotherapy • Importance of ICS inhaler • Vast reduces mortality from asthma • NRAD showed • 80% of patients that died • Had ordered 4 or less ICS inhalers during the year before • Most patients should need 12 ICS per year • Mr JK had ordered 2 • Essentially LABA monotherapy • Poorly educated about compliance
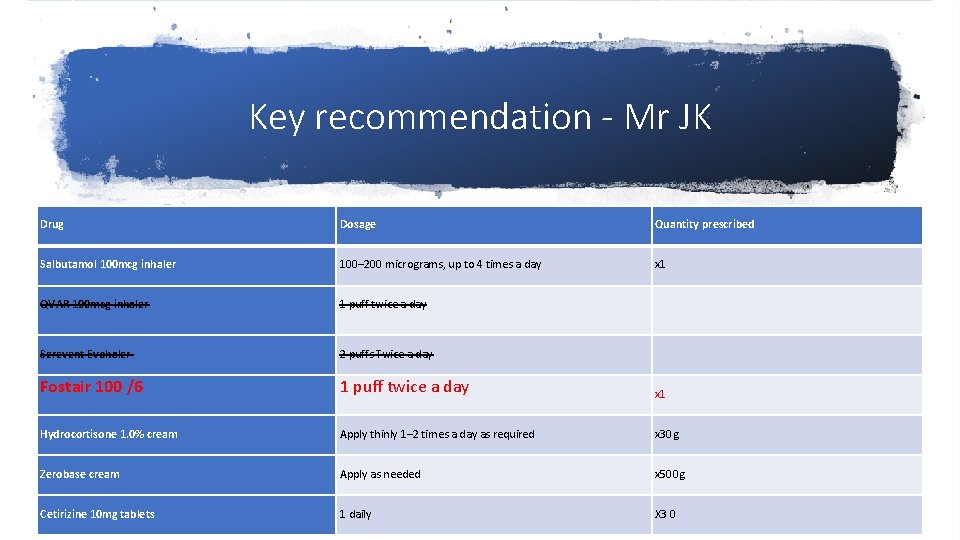
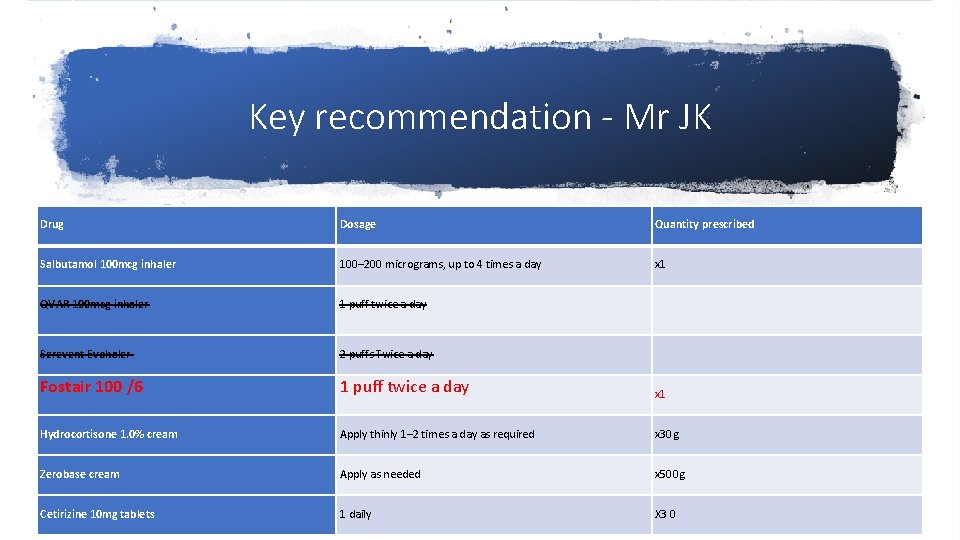
Key recommendation - Mr JK Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day x 1 QVAR 100 mcg inhaler 1 puff twice a day Serevent Evohaler 2 puffs Twice a day Fostair 100 /6 1 puff twice a day x 1 Hydrocortisone 1. 0% cream Apply thinly 1– 2 times a day as required x 30 g Zerobase cream Apply as needed x 500 g Cetirizine 10 mg tablets 1 daily X 3 0
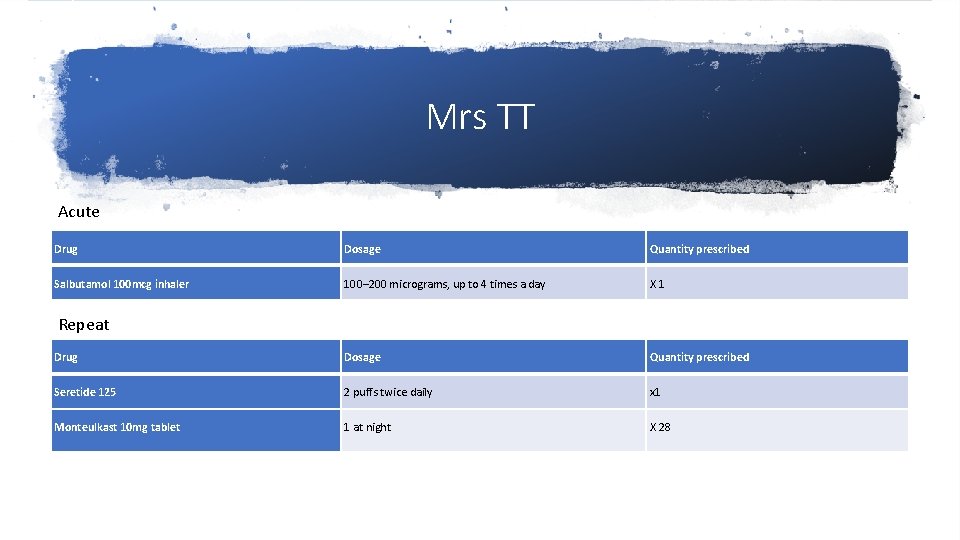
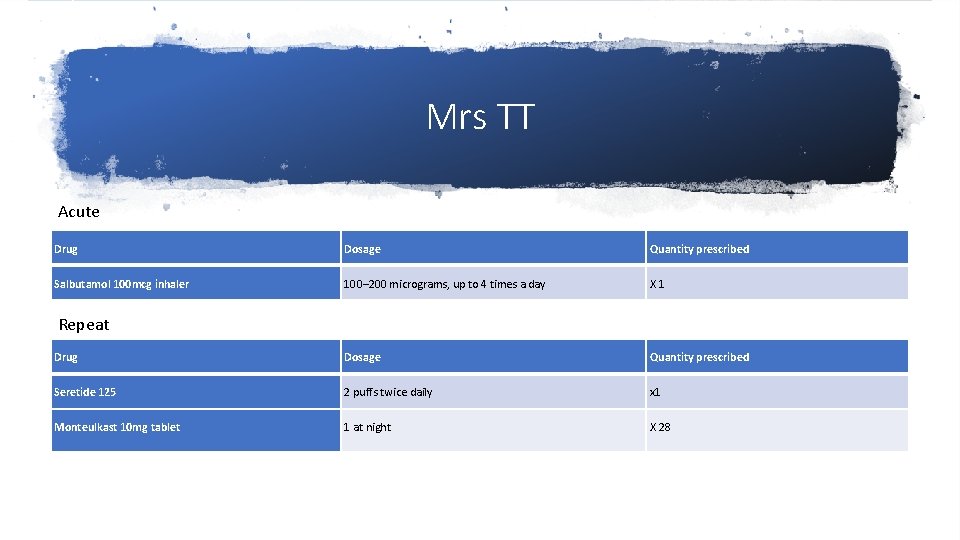
Mrs TT Acute Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day X 1 Drug Dosage Quantity prescribed Seretide 125 2 puffs twice daily x 1 Monteulkast 10 mg tablet 1 at night X 28 Repeat
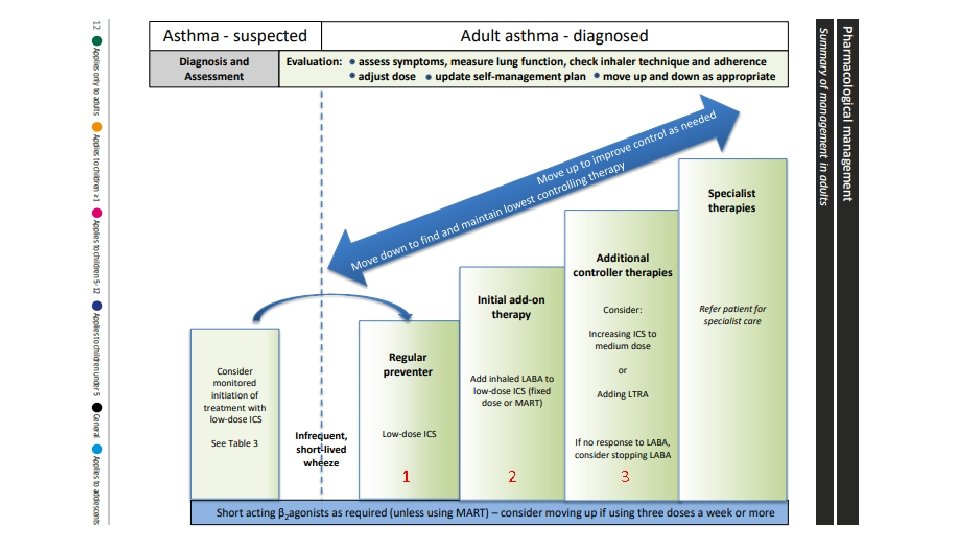
1 2 3
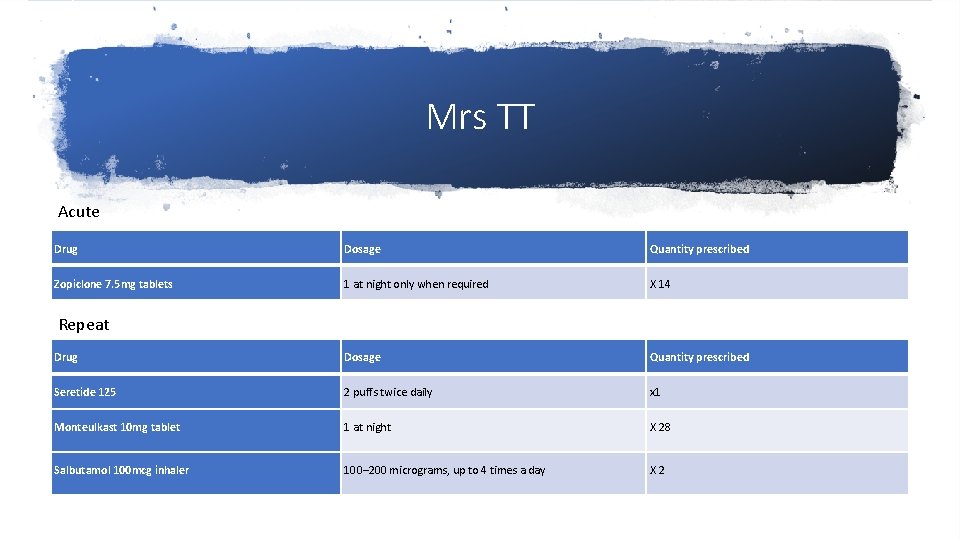
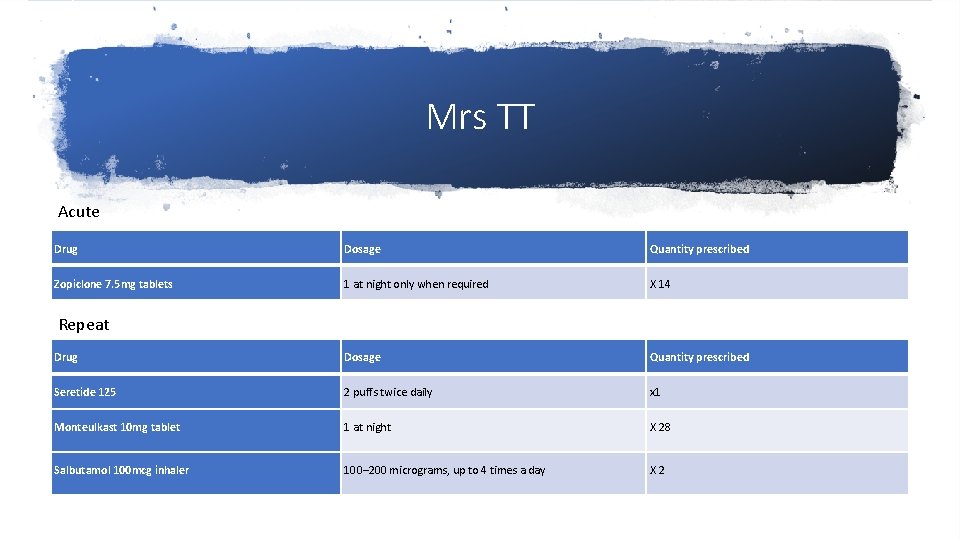
Mrs TT Acute Drug Dosage Quantity prescribed Zopiclone 7. 5 mg tablets 1 at night only when required X 14 Drug Dosage Quantity prescribed Seretide 125 2 puffs twice daily x 1 Monteulkast 10 mg tablet 1 at night X 28 Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day X 2 Repeat
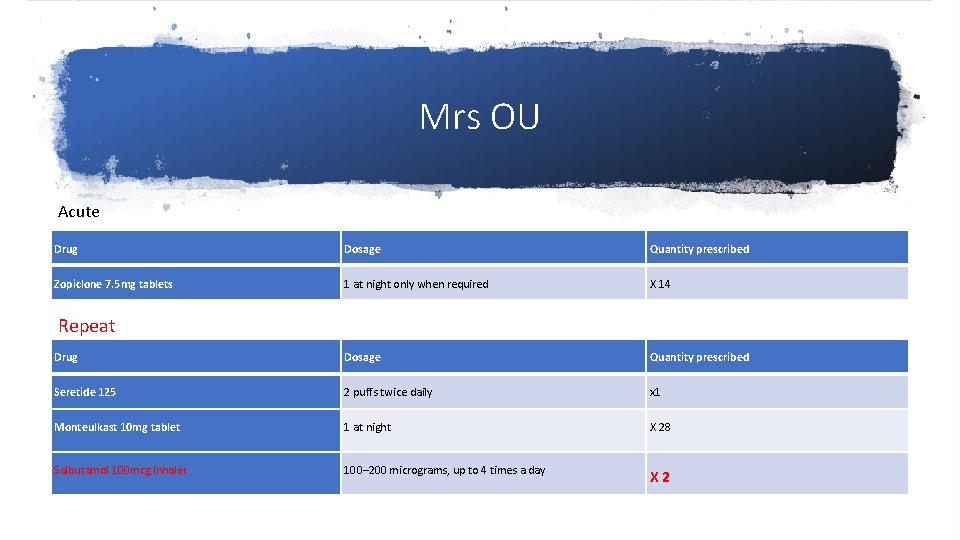
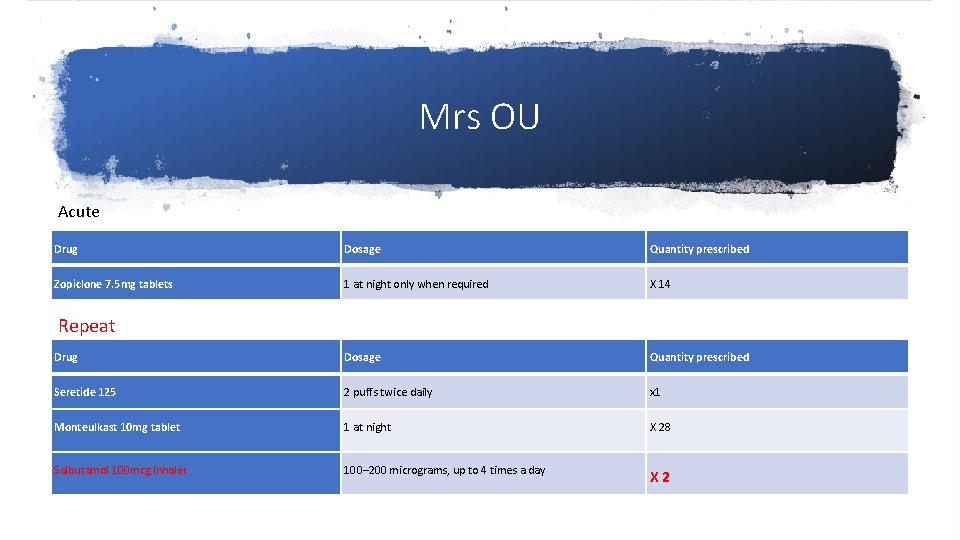
Mrs OU Acute Drug Dosage Quantity prescribed Zopiclone 7. 5 mg tablets 1 at night only when required X 14 Drug Dosage Quantity prescribed Seretide 125 2 puffs twice daily x 1 Monteulkast 10 mg tablet 1 at night X 28 Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day X 2 Repeat
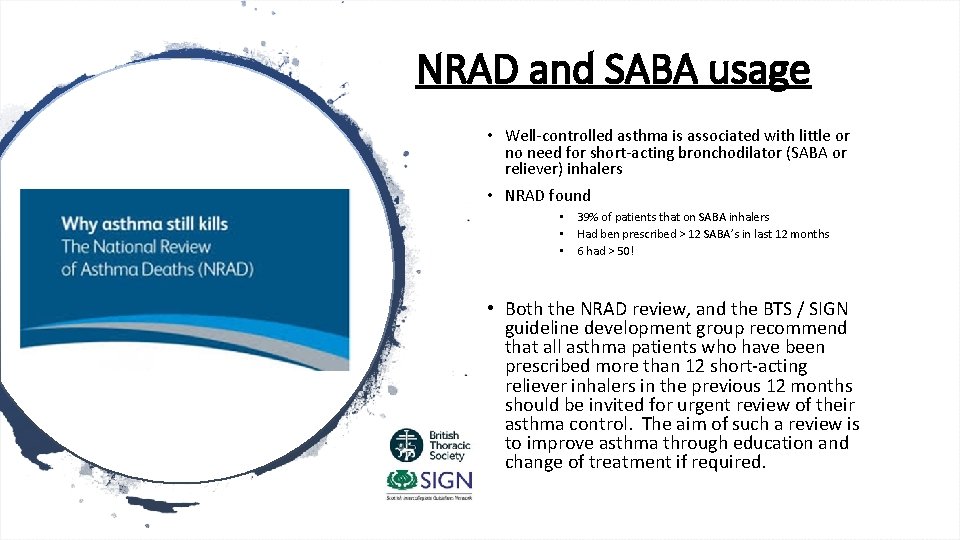
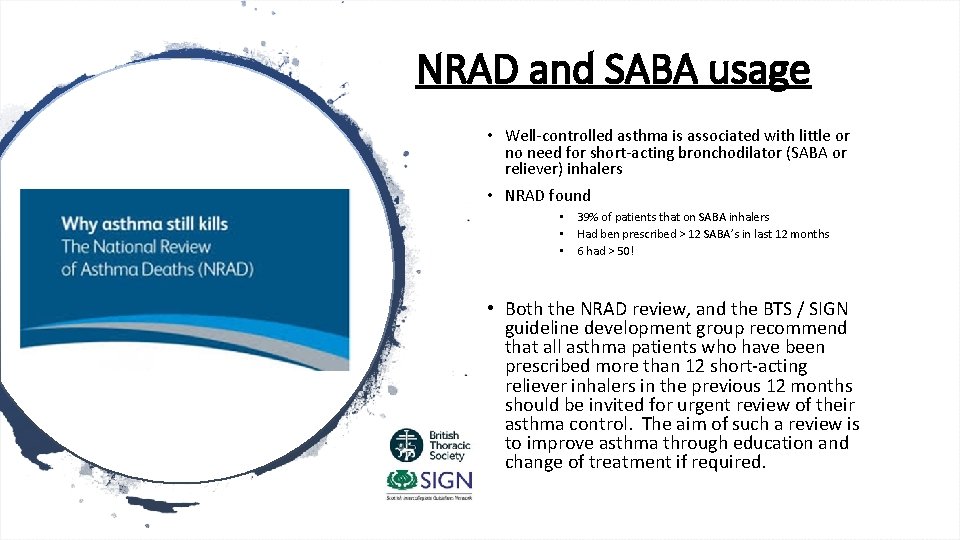
NRAD and SABA usage • Well-controlled asthma is associated with little or no need for short-acting bronchodilator (SABA or reliever) inhalers • NRAD found • • • 39% of patients that on SABA inhalers Had ben prescribed > 12 SABA’s in last 12 months 6 had > 50! • Both the NRAD review, and the BTS / SIGN guideline development group recommend that all asthma patients who have been prescribed more than 12 short-acting reliever inhalers in the previous 12 months should be invited for urgent review of their asthma control. The aim of such a review is to improve asthma through education and change of treatment if required.
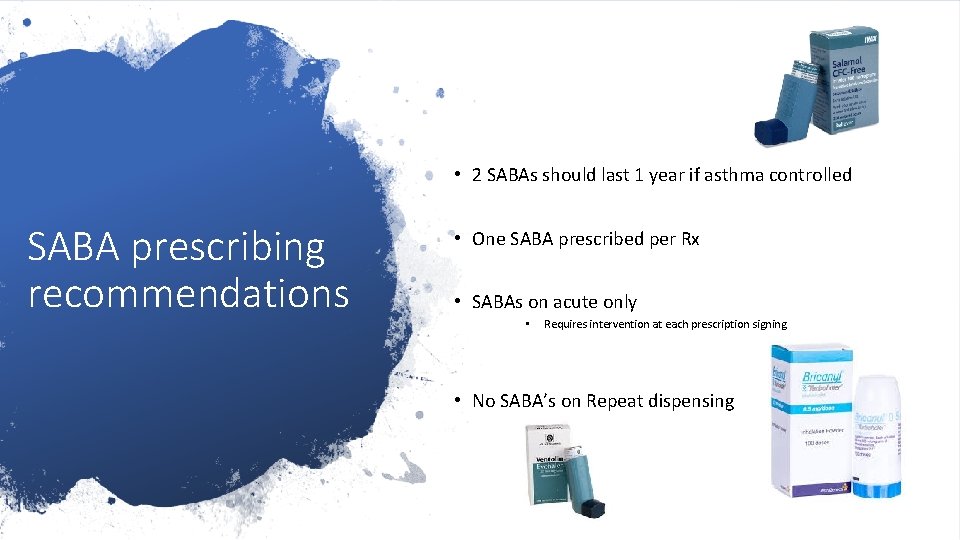
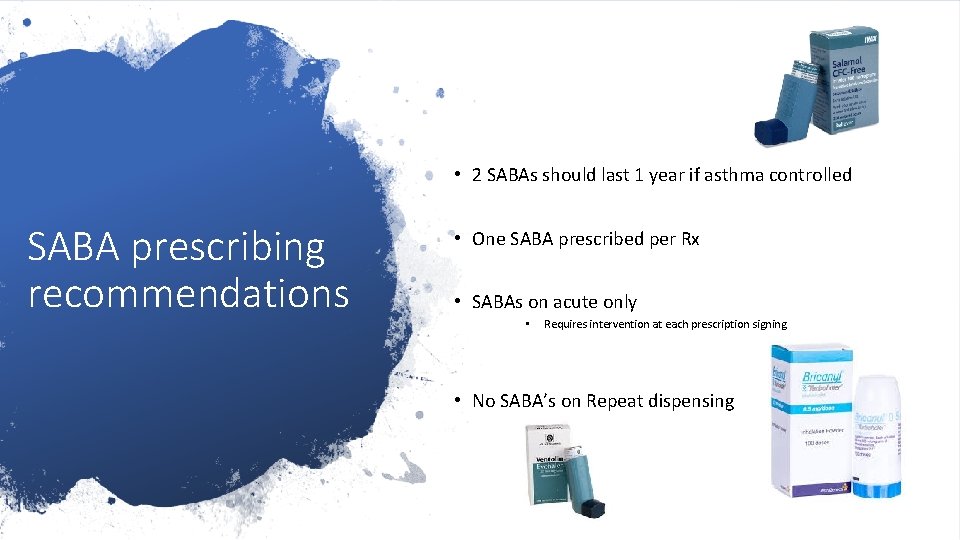
• 2 SABAs should last 1 year if asthma controlled SABA prescribing recommendations • One SABA prescribed per Rx • SABAs on acute only • Requires intervention at each prescription signing. • No SABA’s on Repeat dispensing
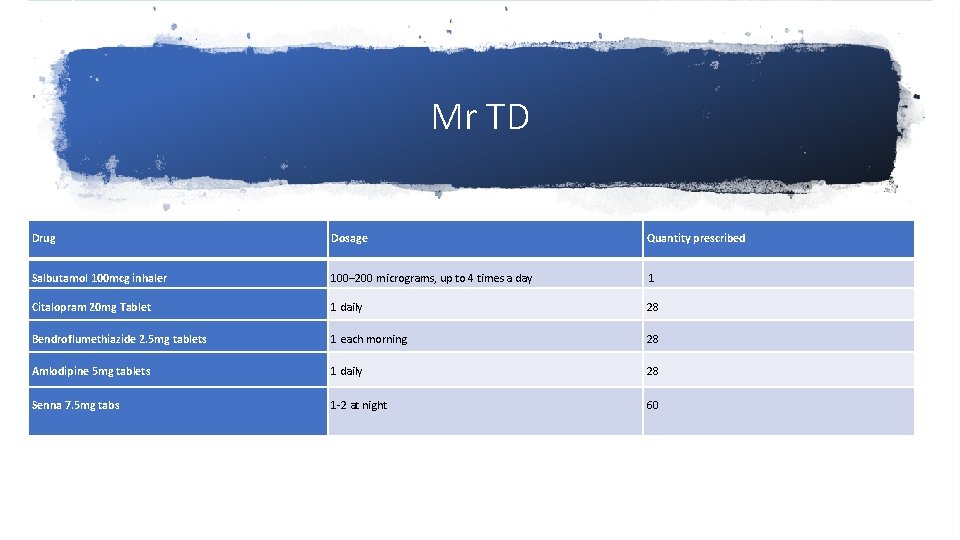
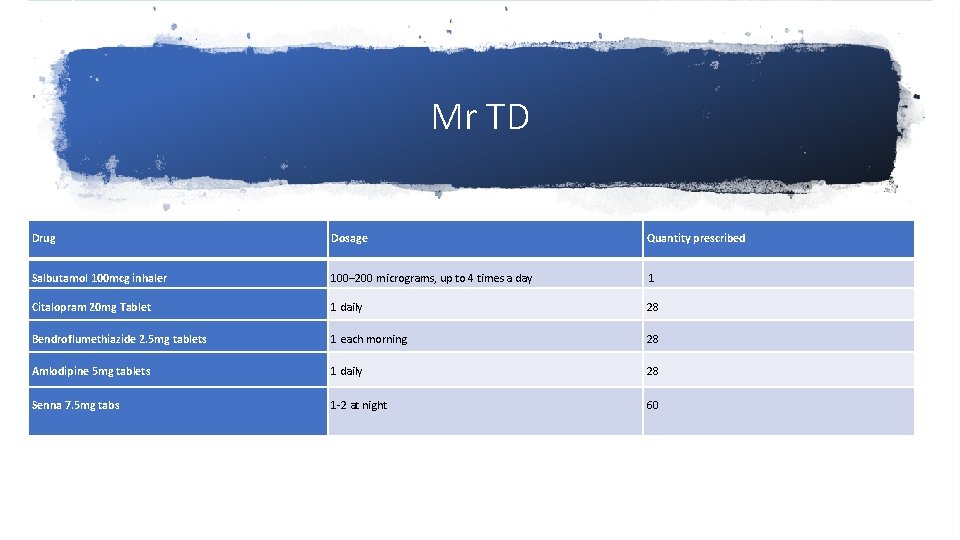
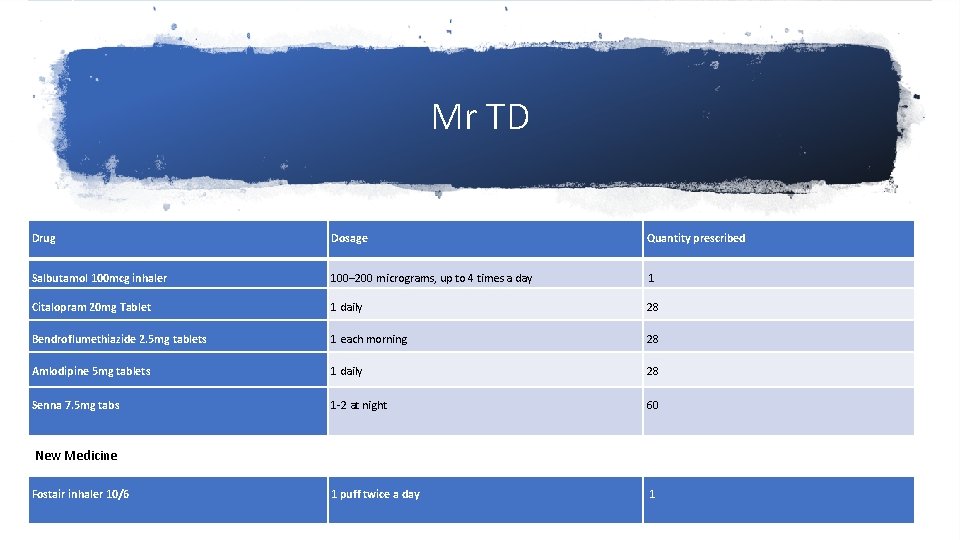
Mr TD Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg Tablet 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60
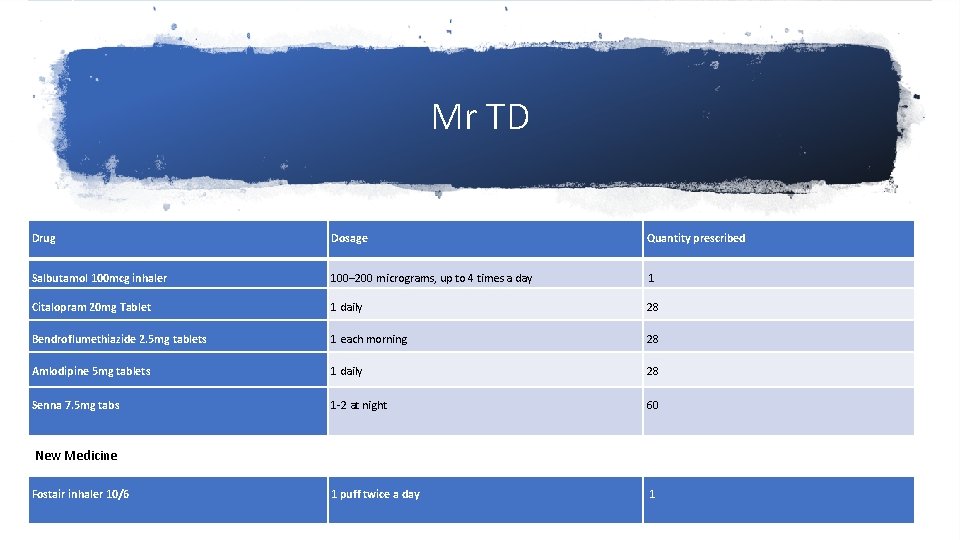
Mr TD Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg Tablet 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6

“high risk alert – risk of torsade de pointes”
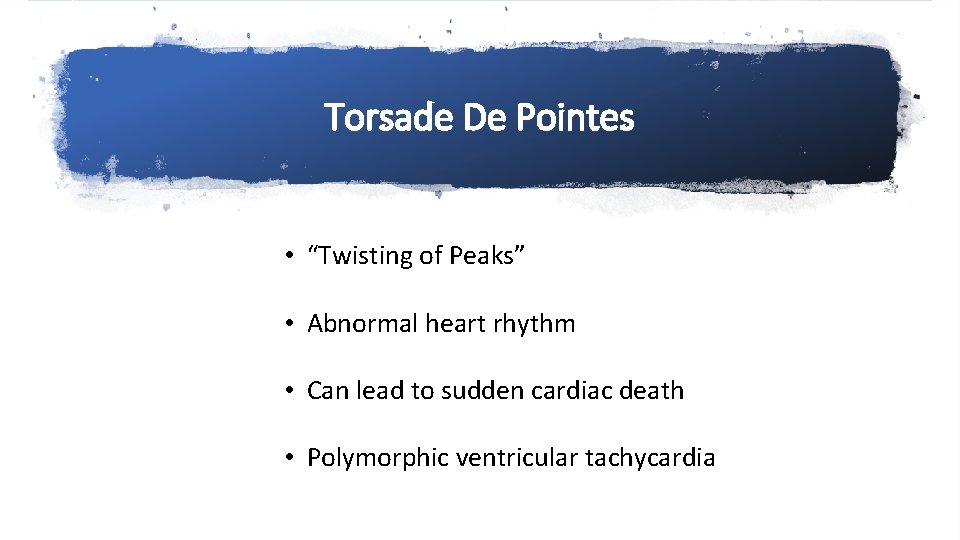
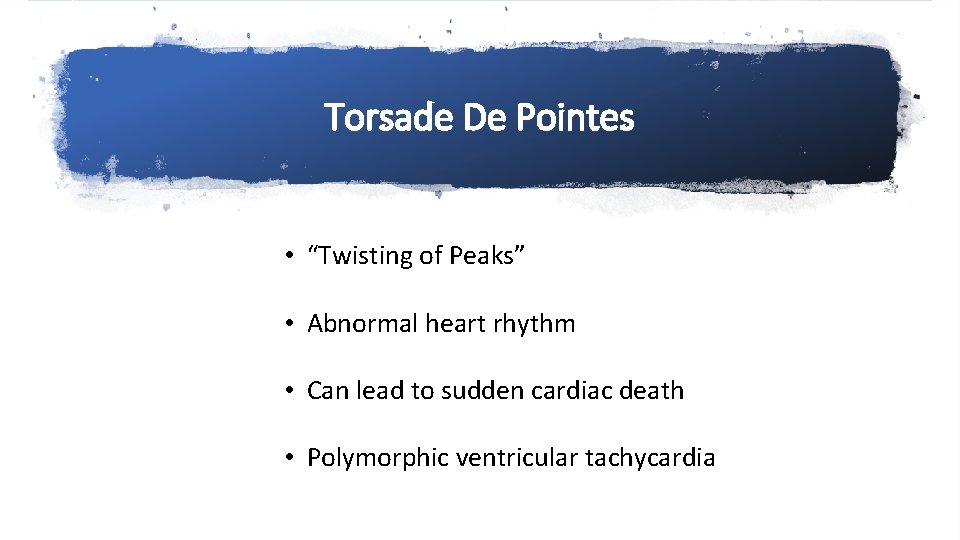
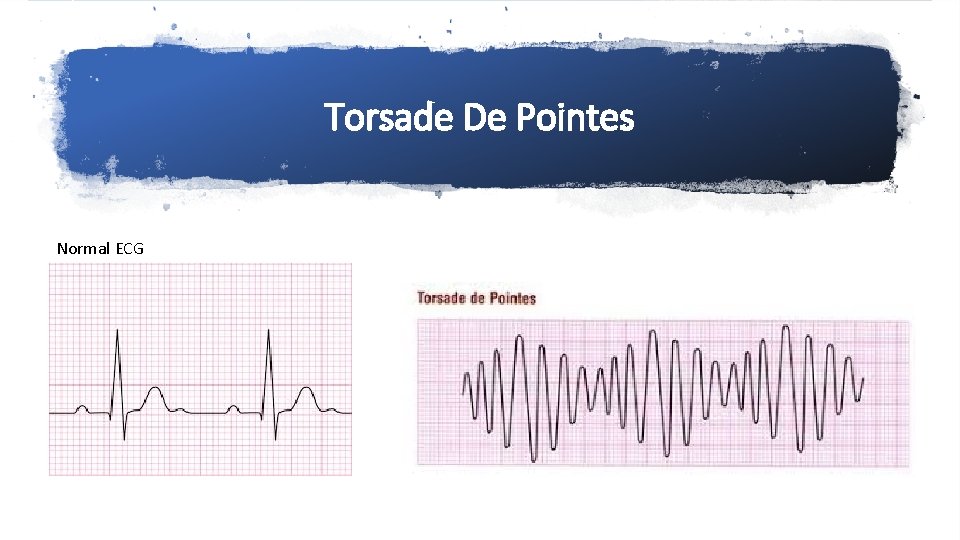
Torsade De Pointes • “Twisting of Peaks” • Abnormal heart rhythm • Can lead to sudden cardiac death • Polymorphic ventricular tachycardia
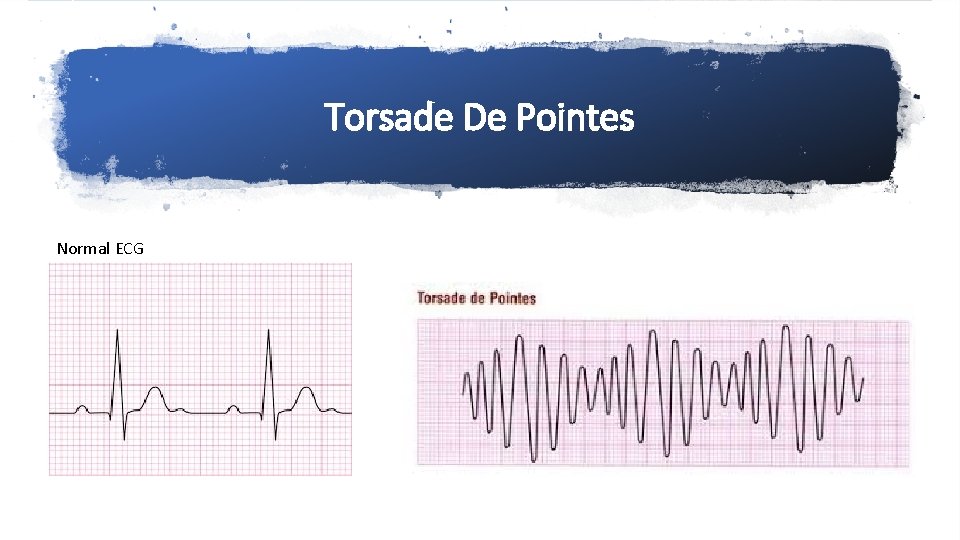
Torsade De Pointes Normal ECG
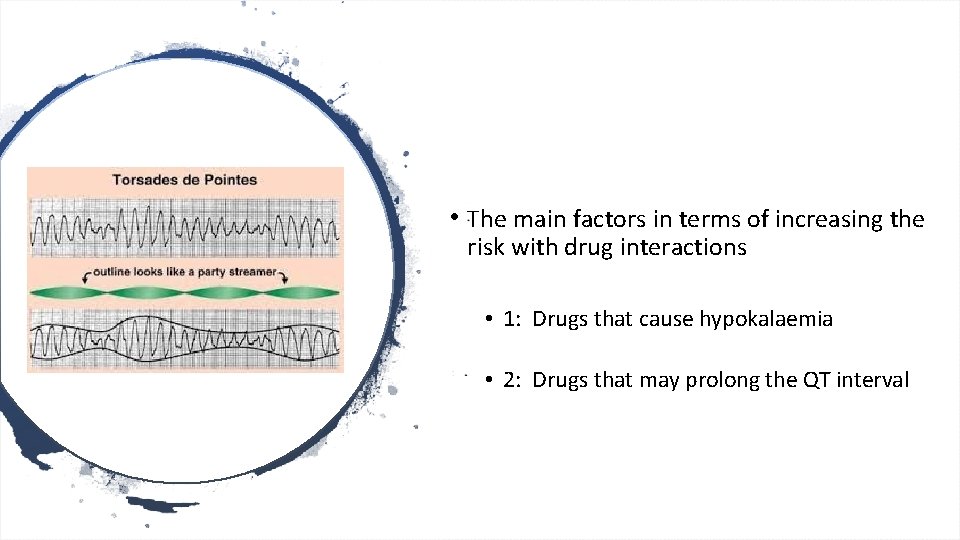
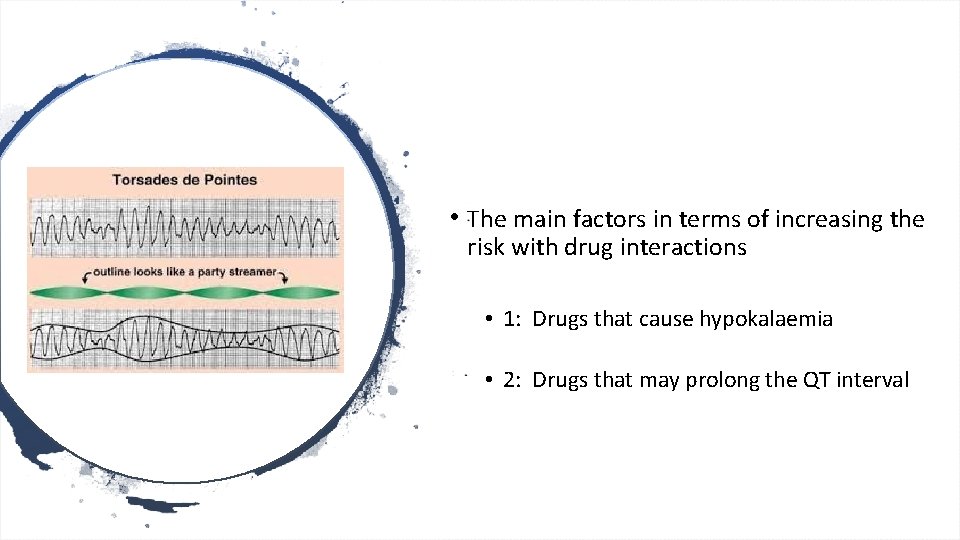
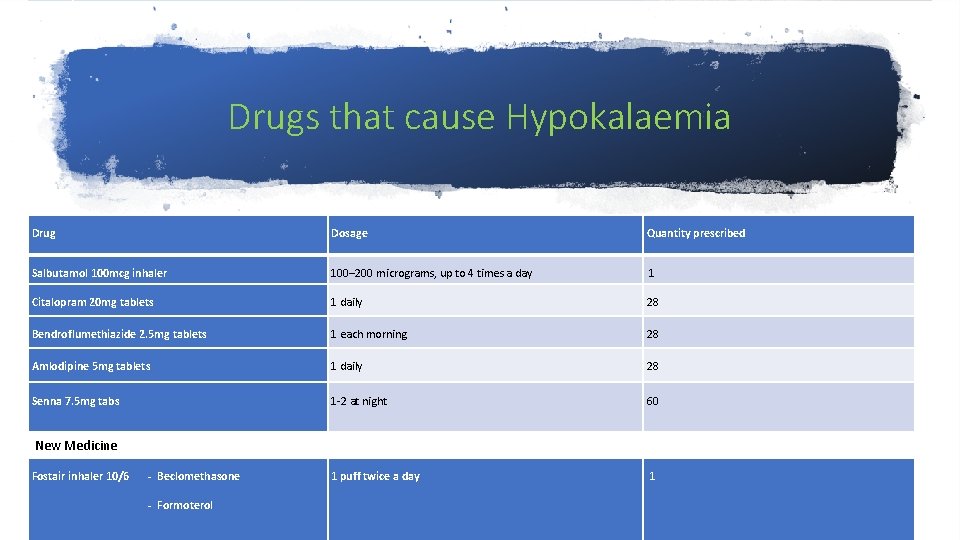
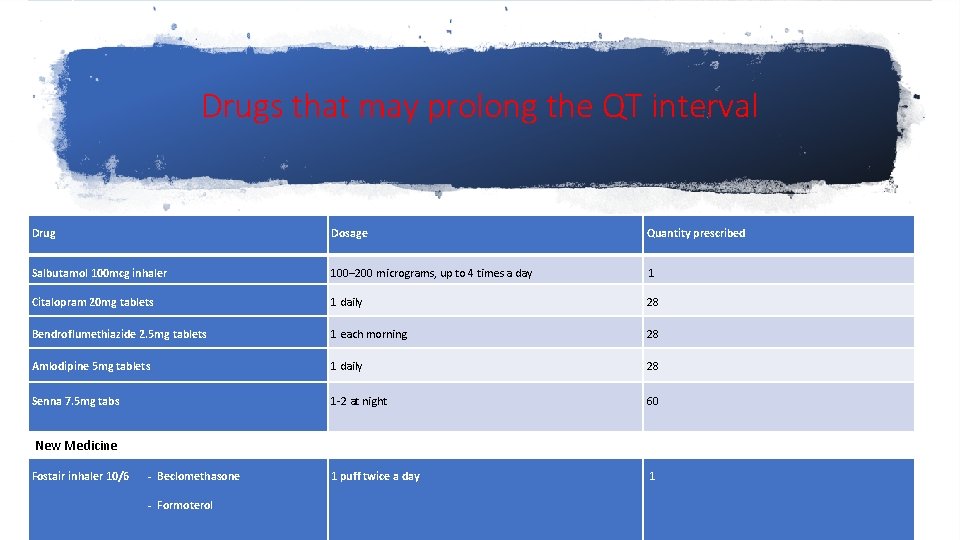
• The main factors in terms of increasing the risk with drug interactions • 1: Drugs that cause hypokalaemia • 2: Drugs that may prolong the QT interval
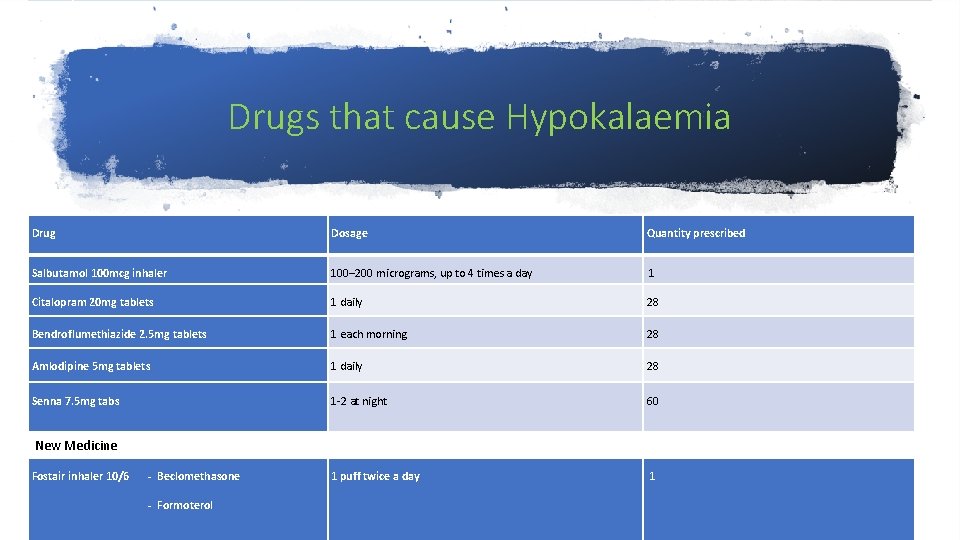
Drugs that cause Hypokalaemia Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
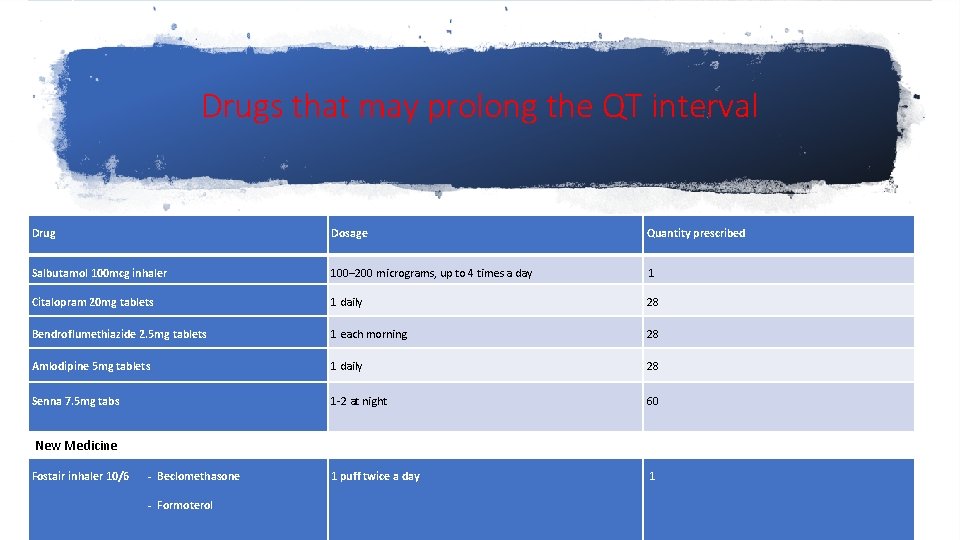
Drugs that may prolong the QT interval Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
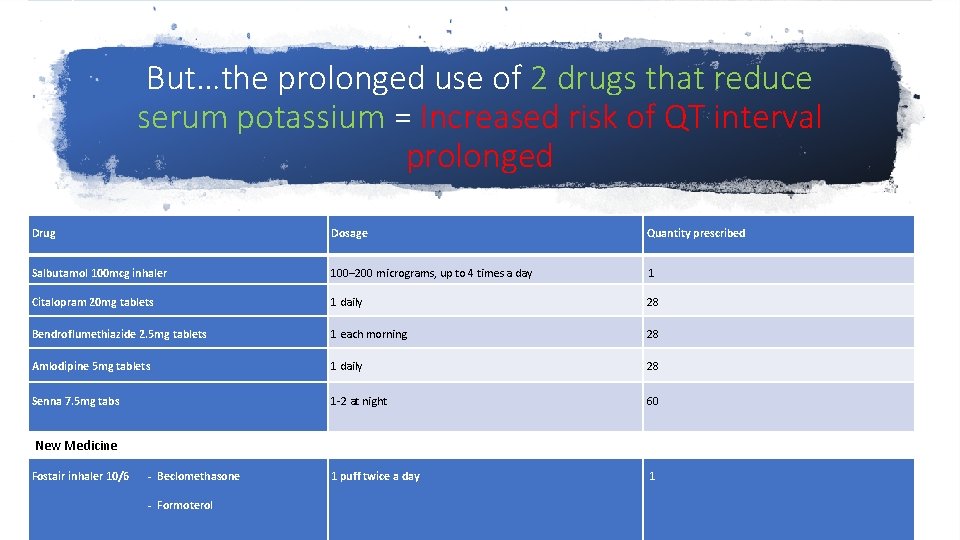
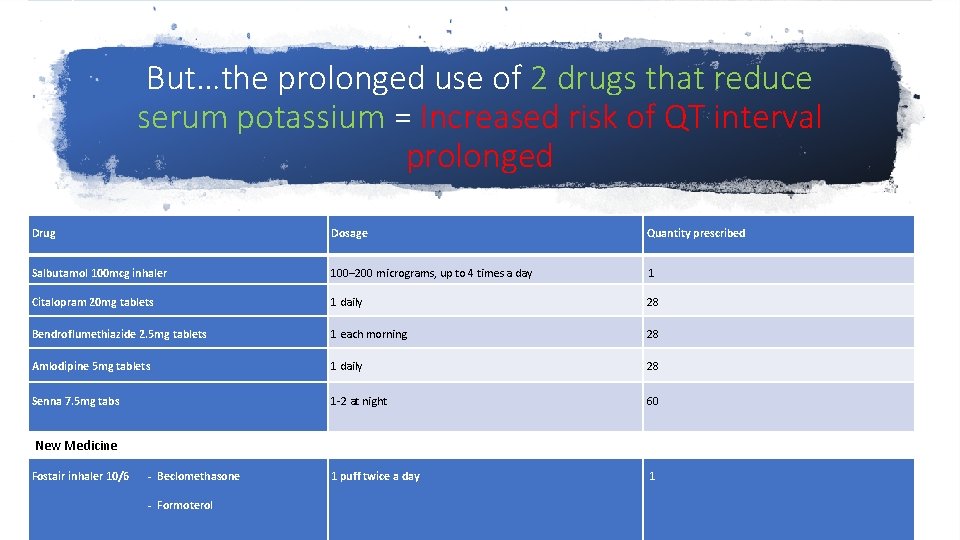
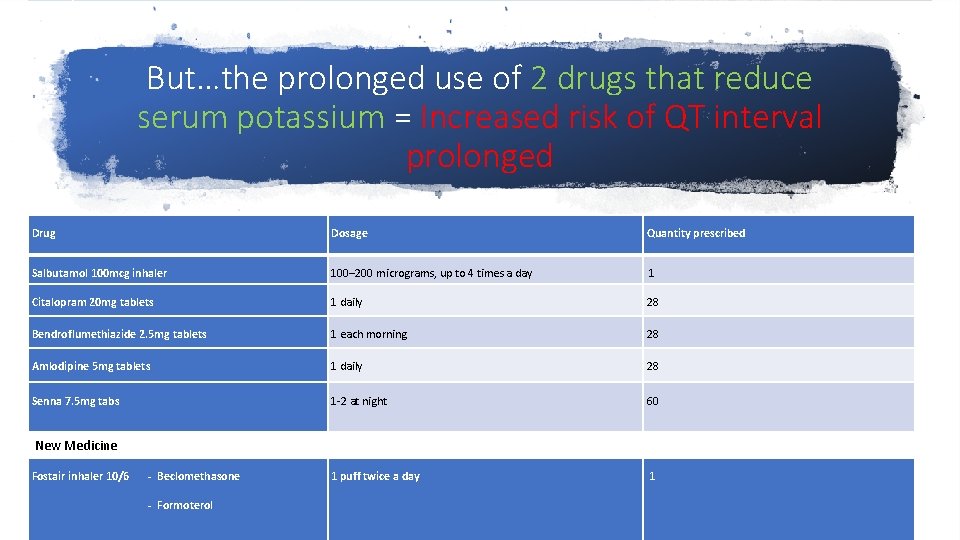
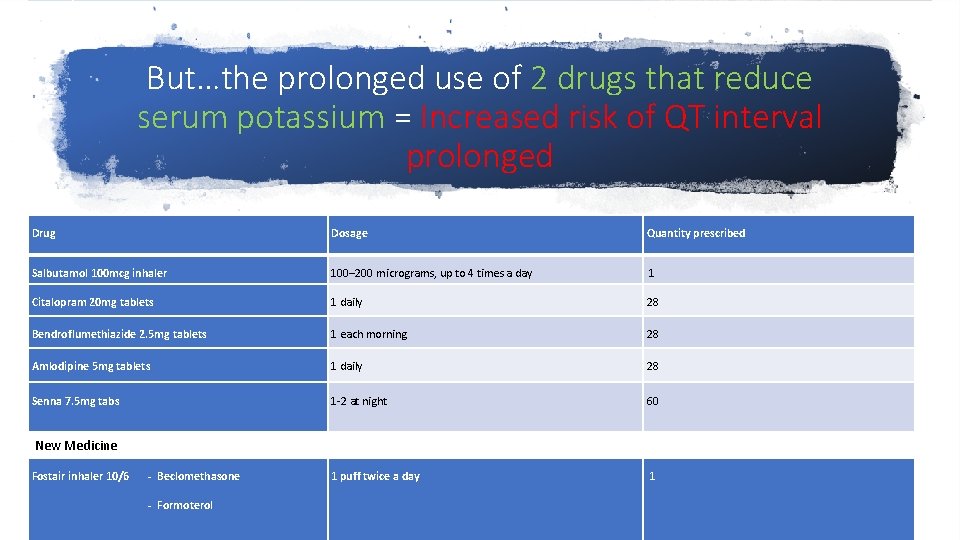
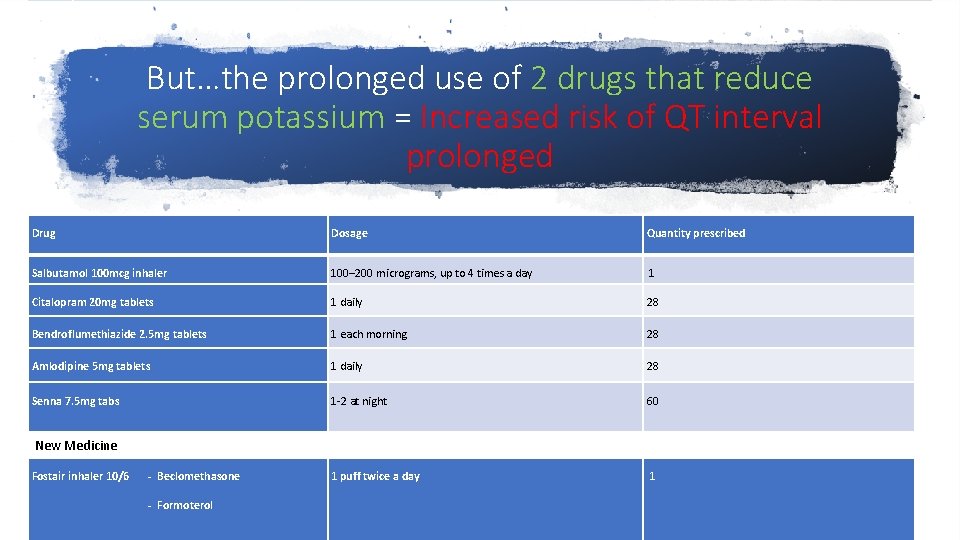
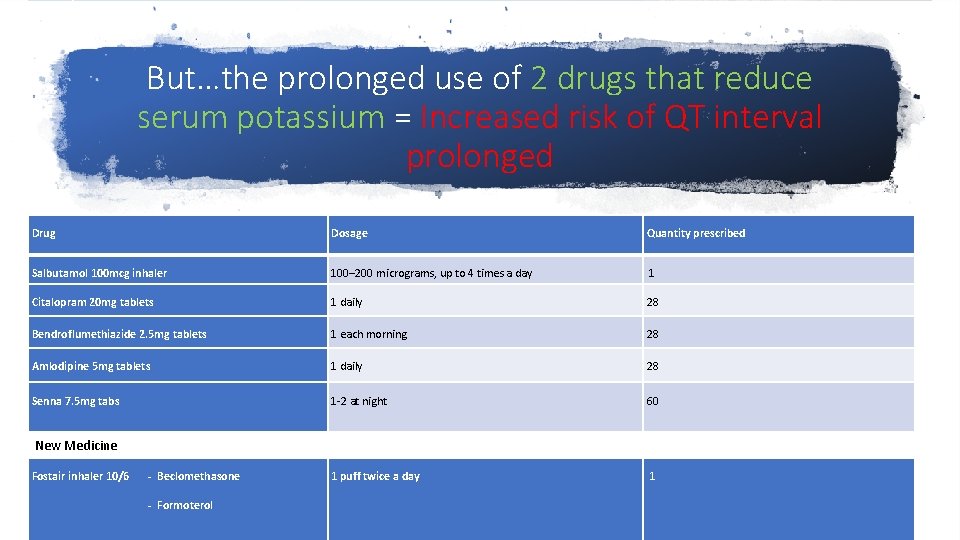
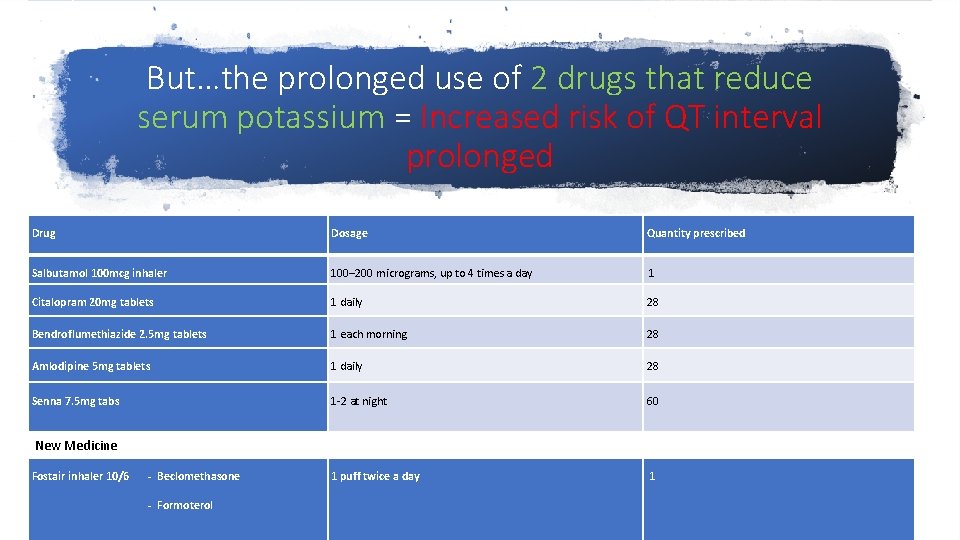
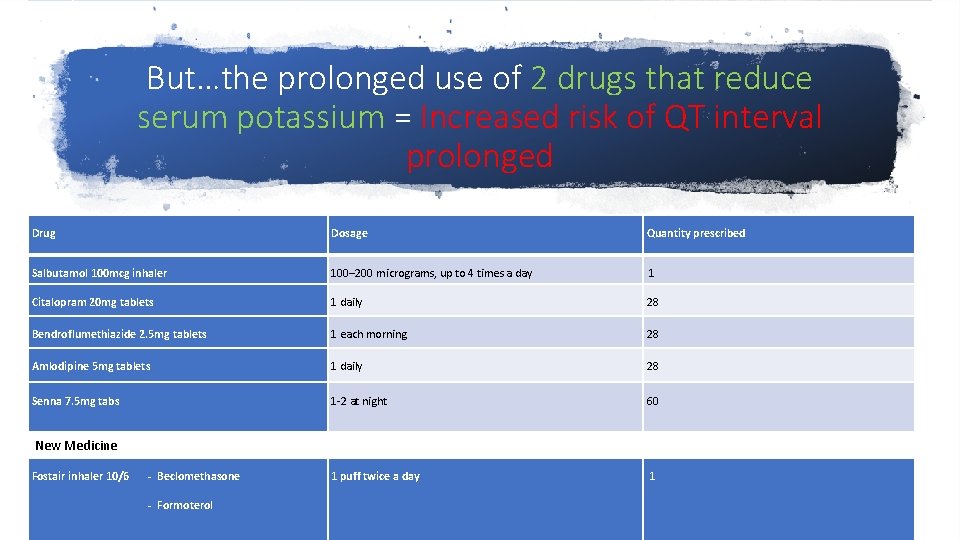
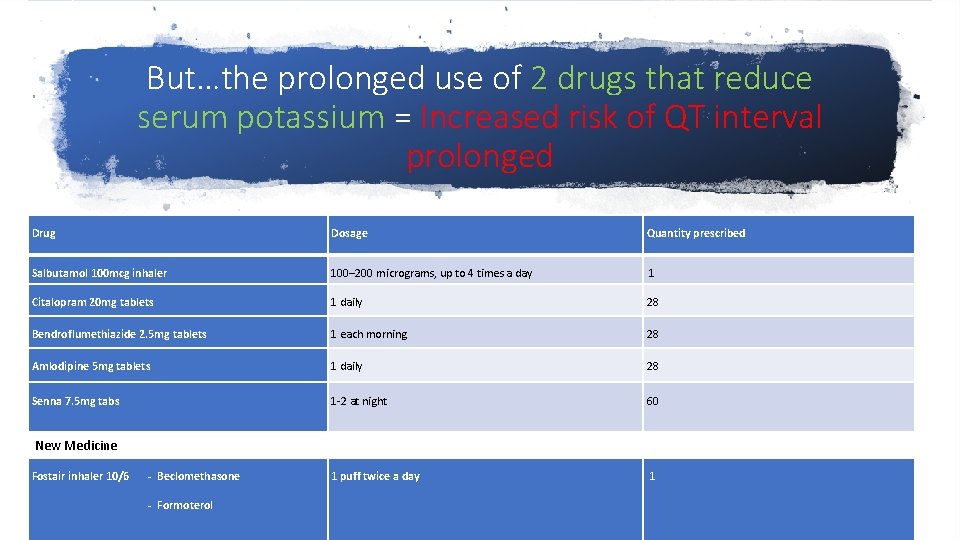
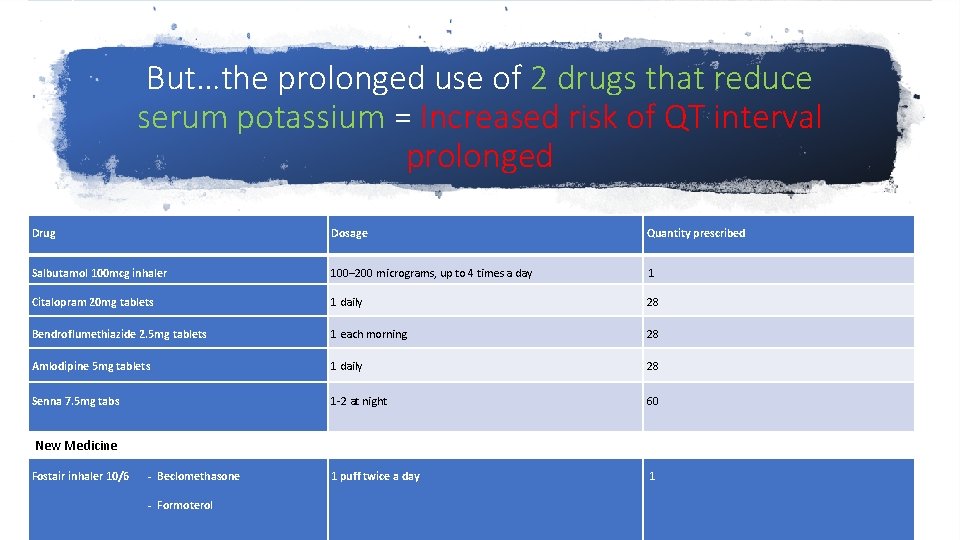
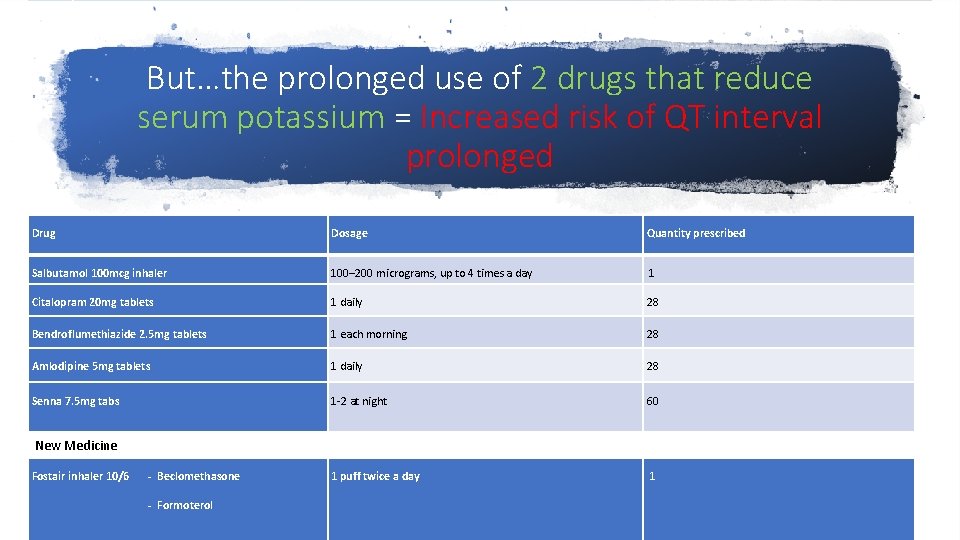
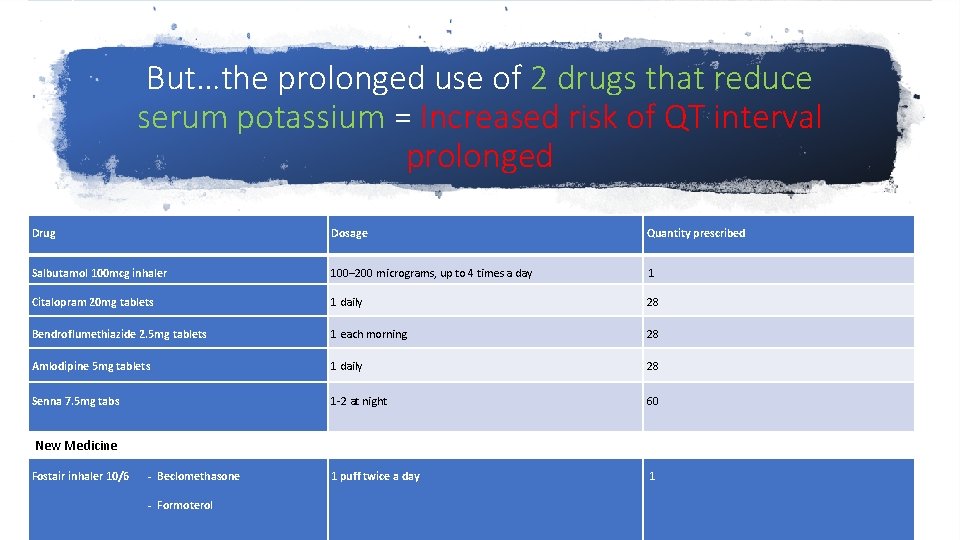
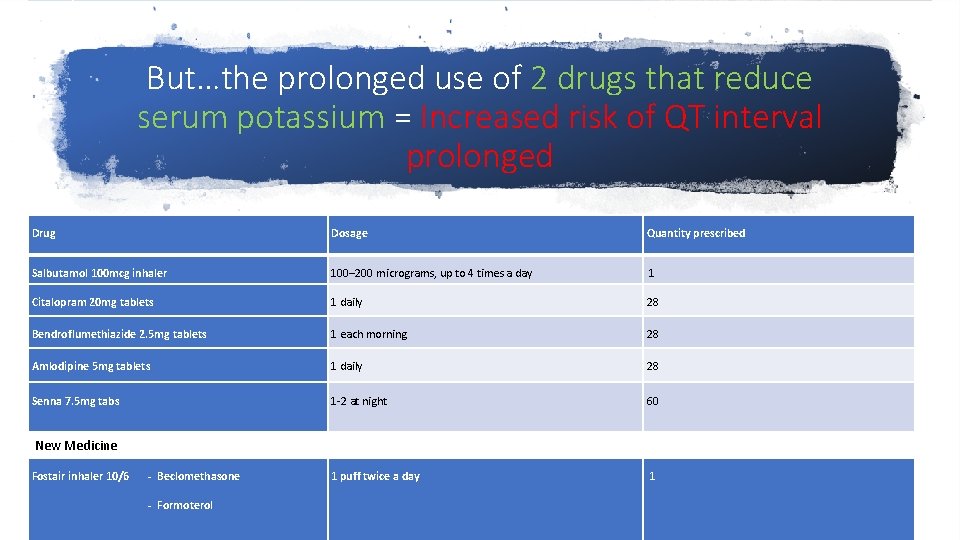
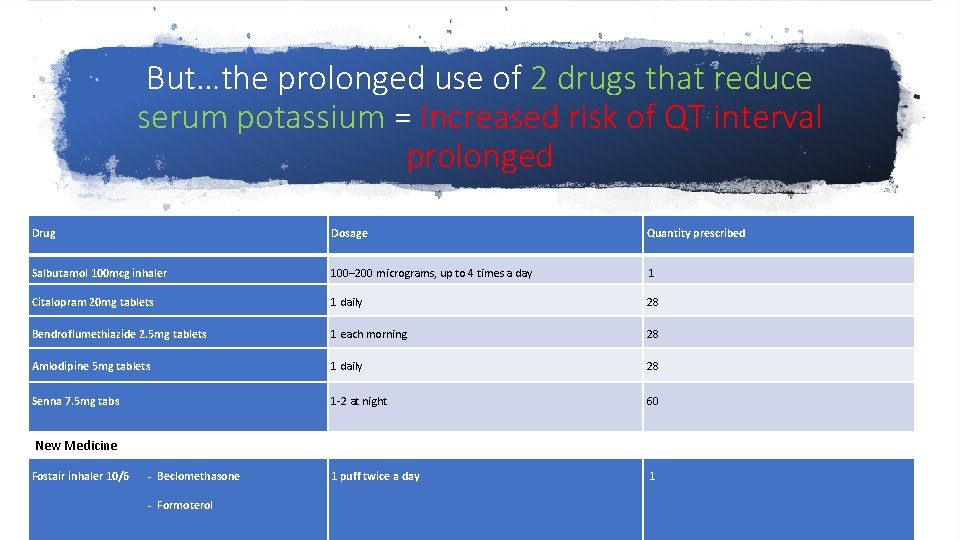
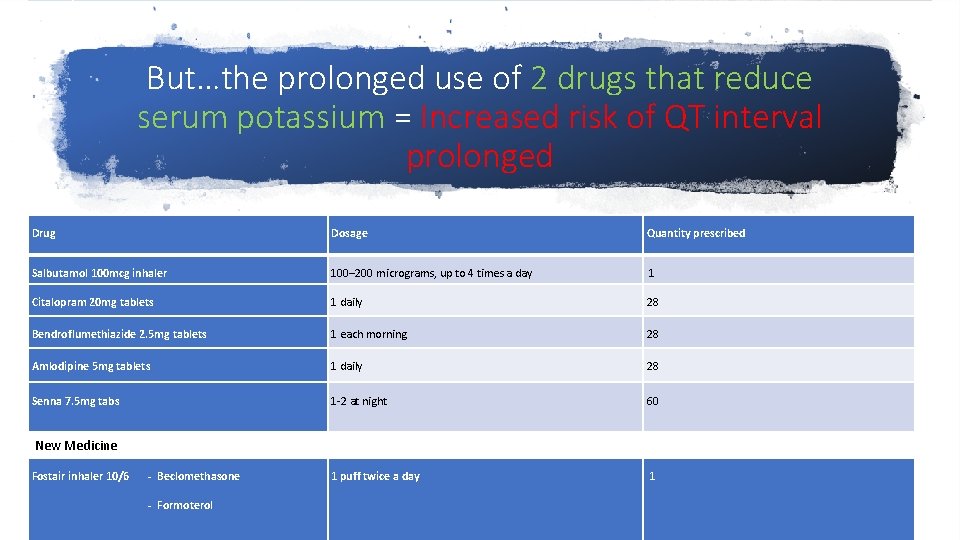
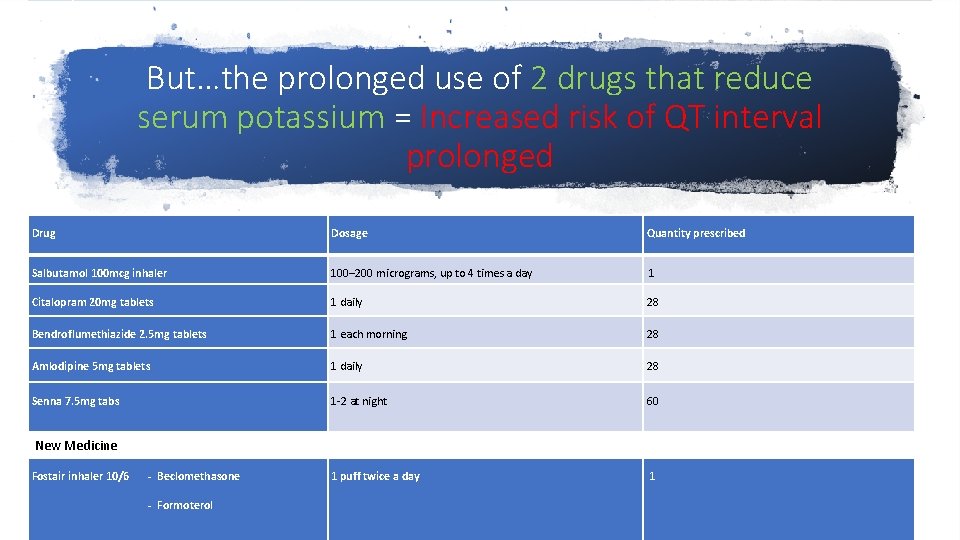
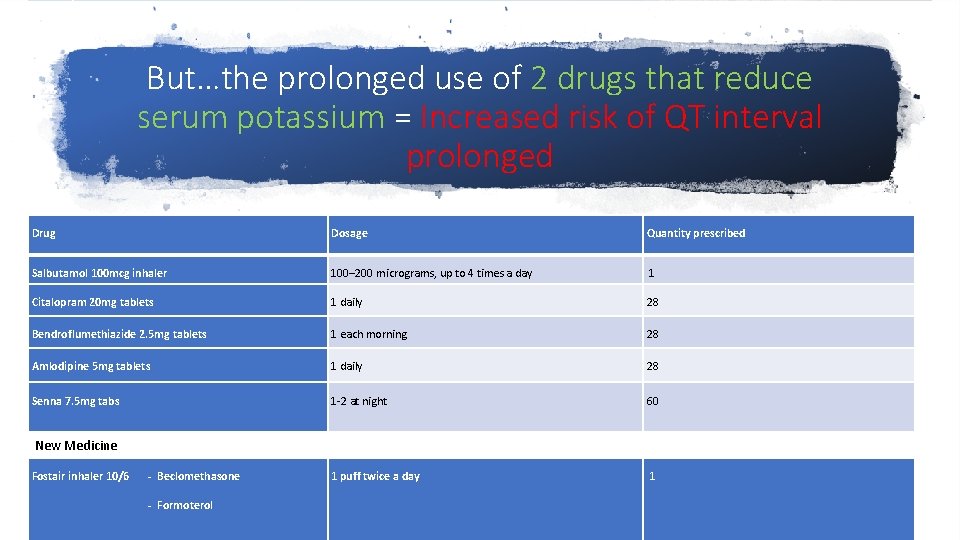
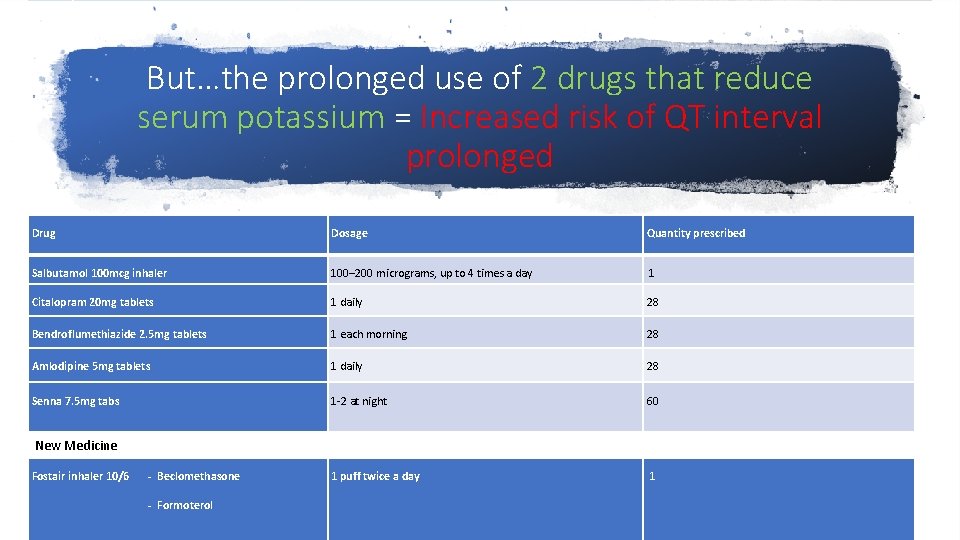
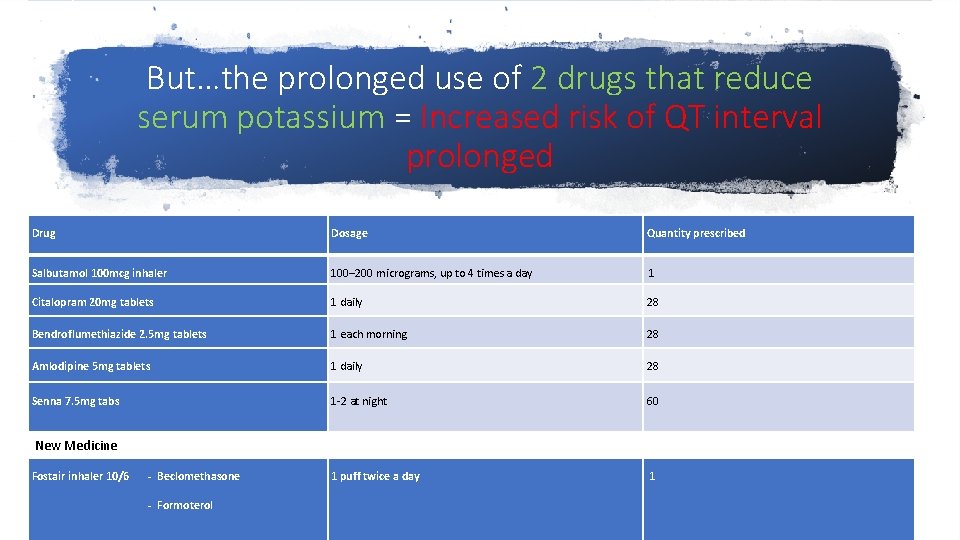
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
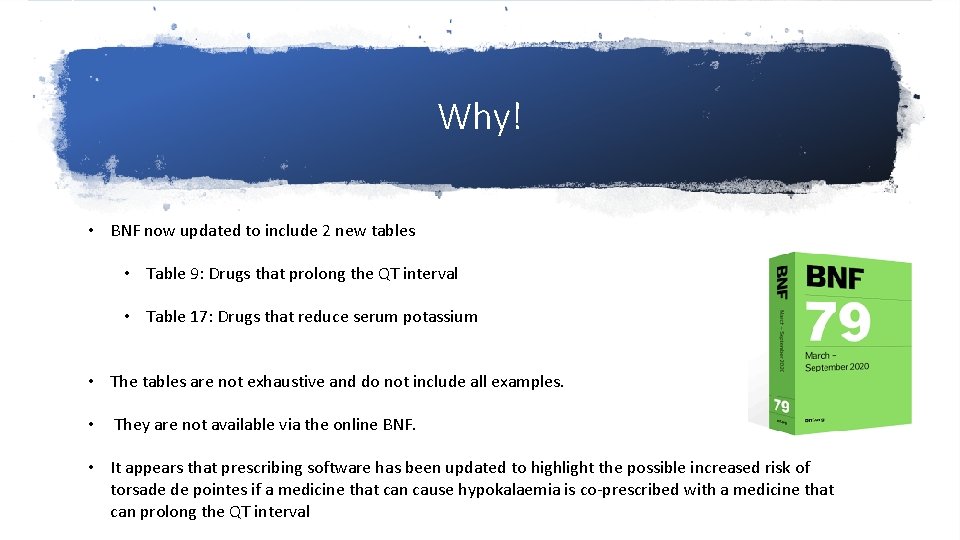
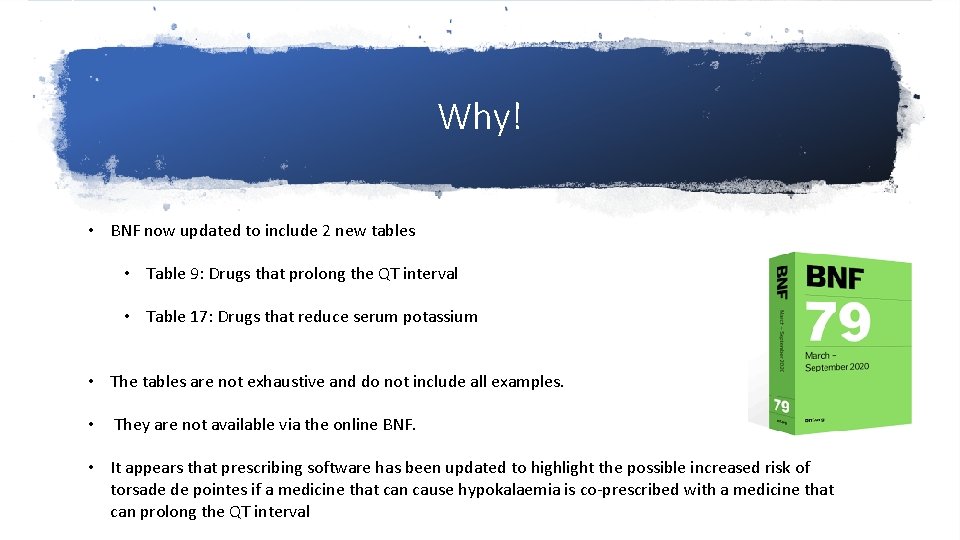
Why! • BNF now updated to include 2 new tables • Table 9: Drugs that prolong the QT interval • Table 17: Drugs that reduce serum potassium • The tables are not exhaustive and do not include all examples. • They are not available via the online BNF. • It appears that prescribing software has been updated to highlight the possible increased risk of torsade de pointes if a medicine that can cause hypokalaemia is co-prescribed with a medicine that can prolong the QT interval
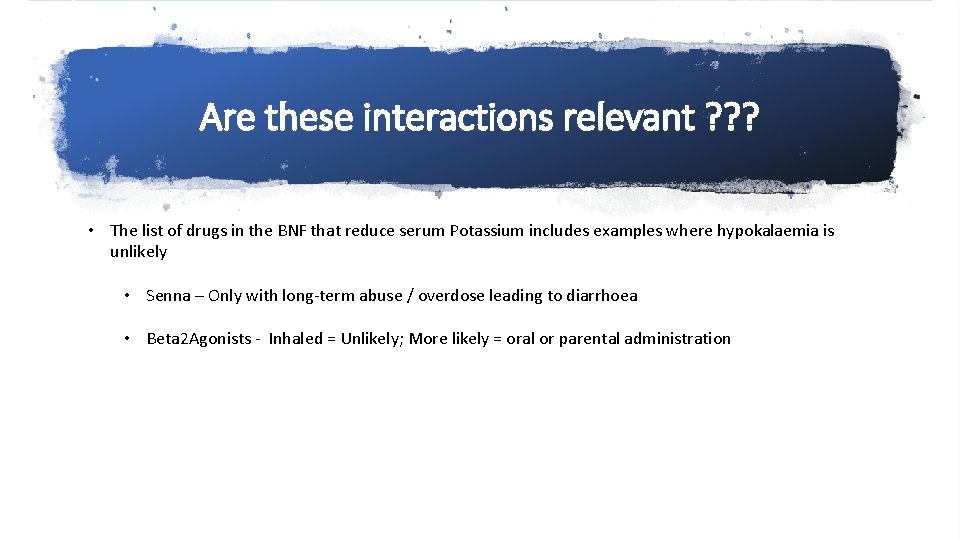
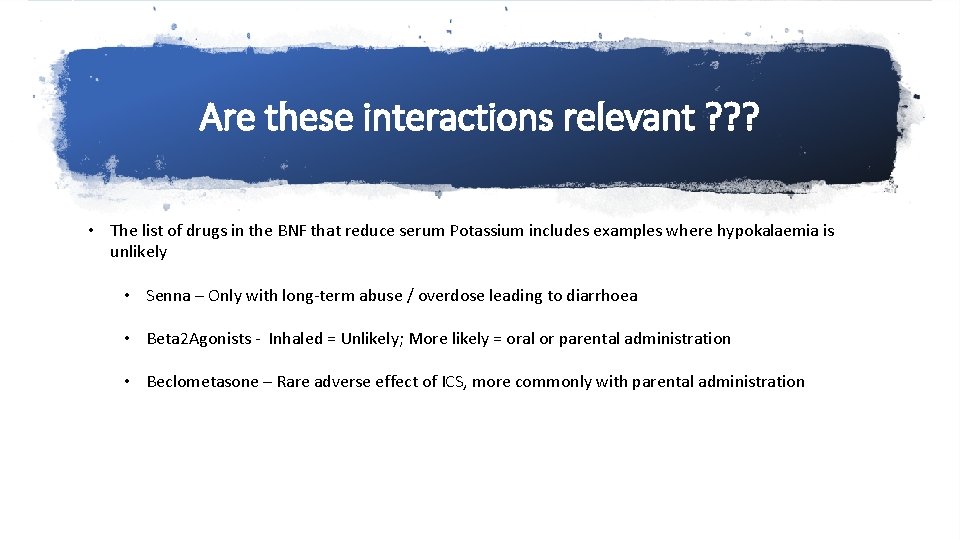
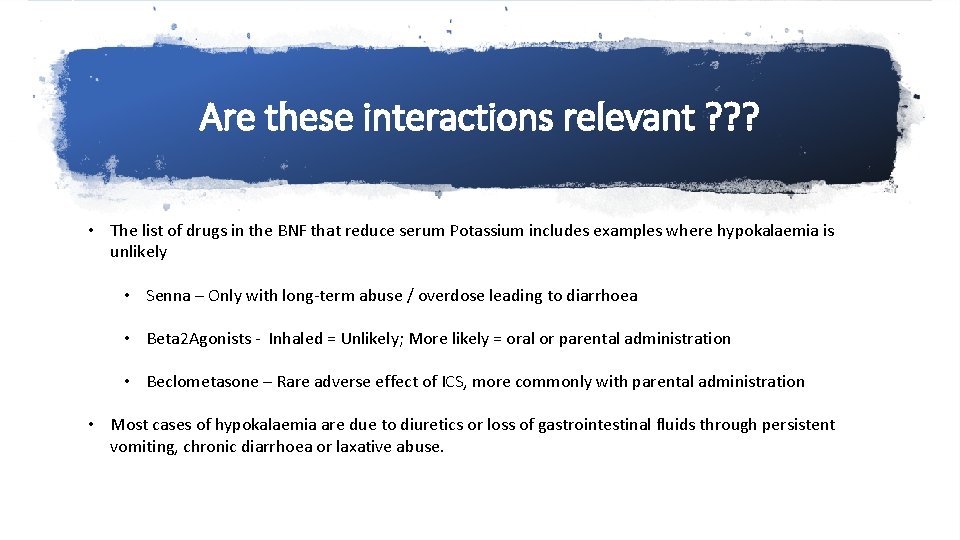
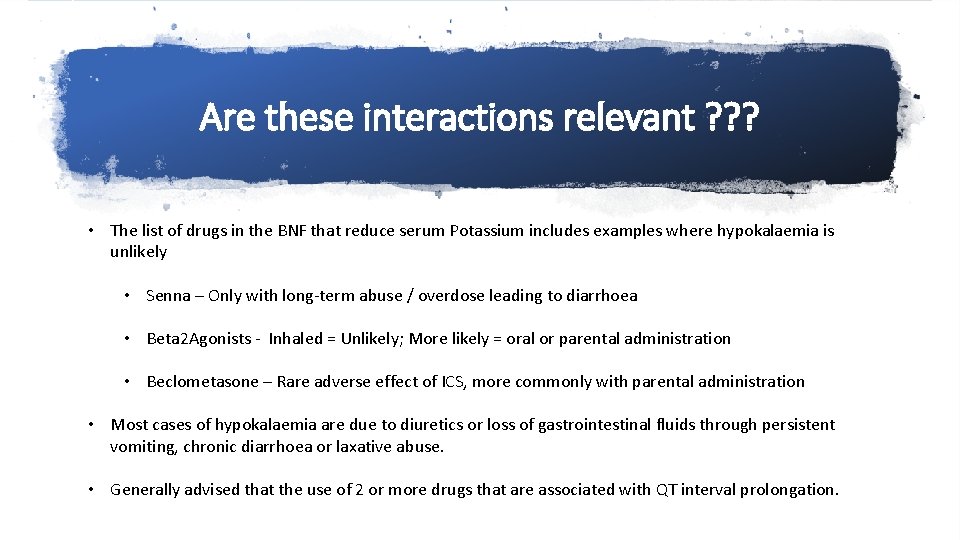
Are these interactions relevant ? ? ? • The list of drugs in the BNF that reduce serum Potassium includes examples where hypokalaemia is unlikely • Senna – Only with long-term abuse / overdose leading to diarrhoea
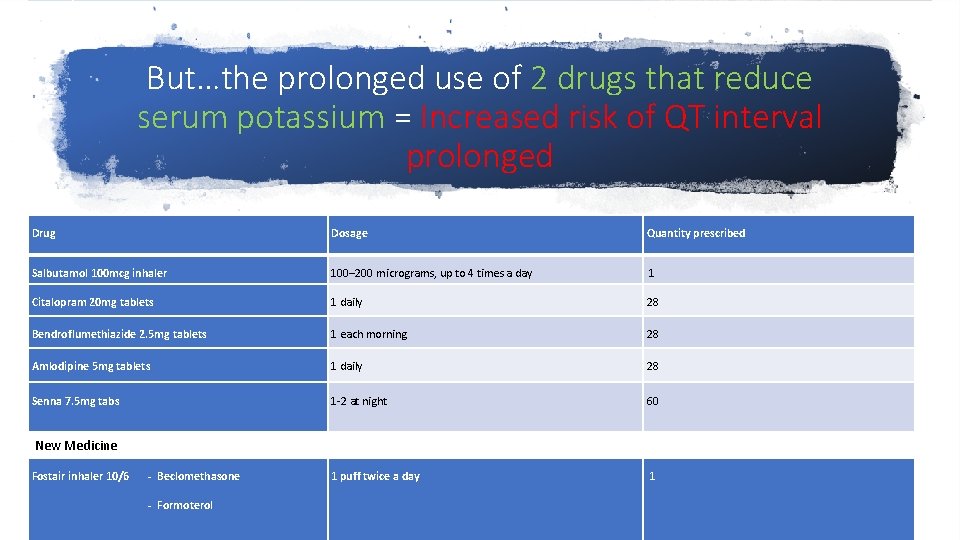
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
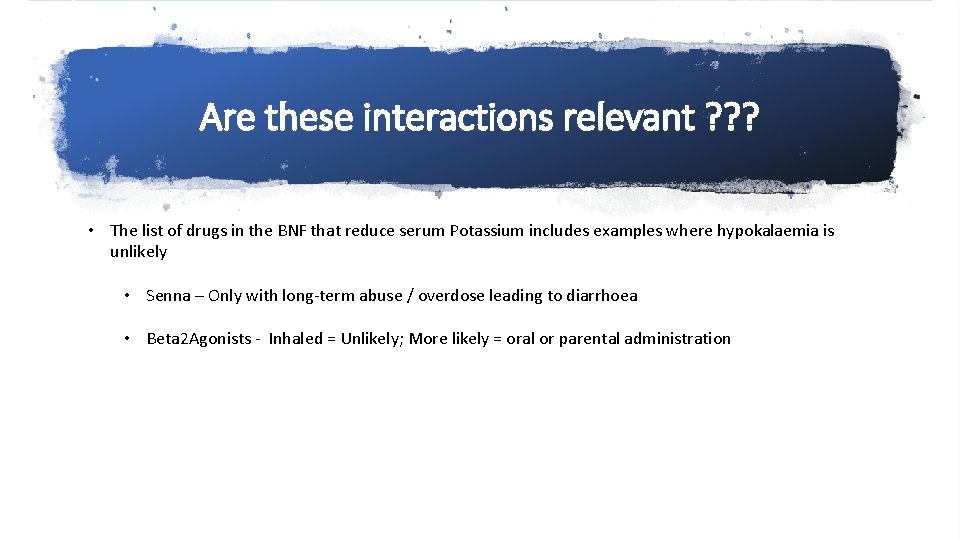
Are these interactions relevant ? ? ? • The list of drugs in the BNF that reduce serum Potassium includes examples where hypokalaemia is unlikely • Senna – Only with long-term abuse / overdose leading to diarrhoea • Beta 2 Agonists - Inhaled = Unlikely; More likely = oral or parental administration
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
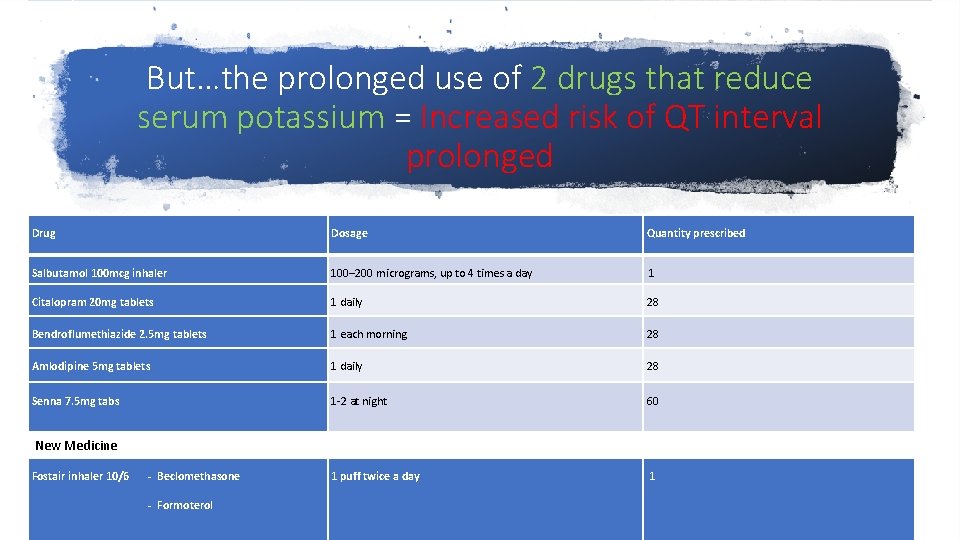
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
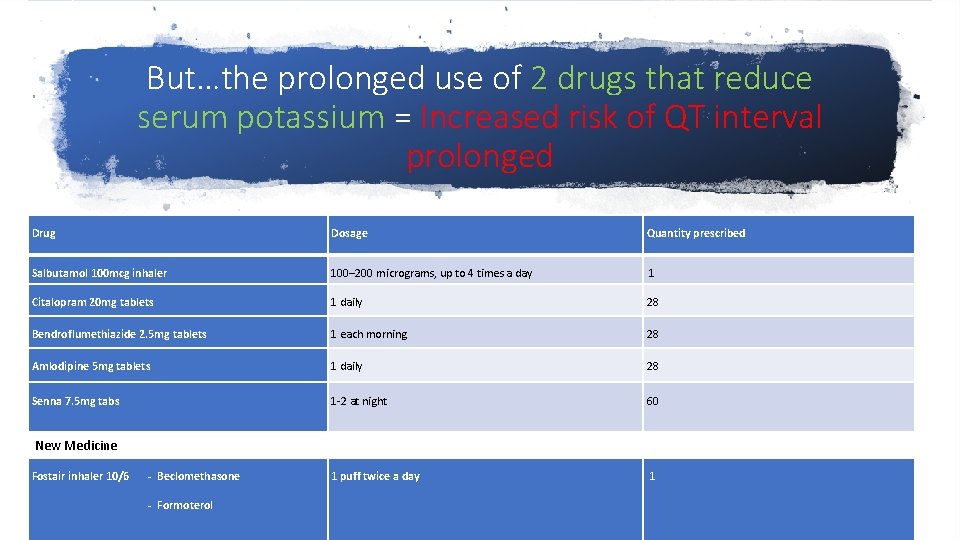
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
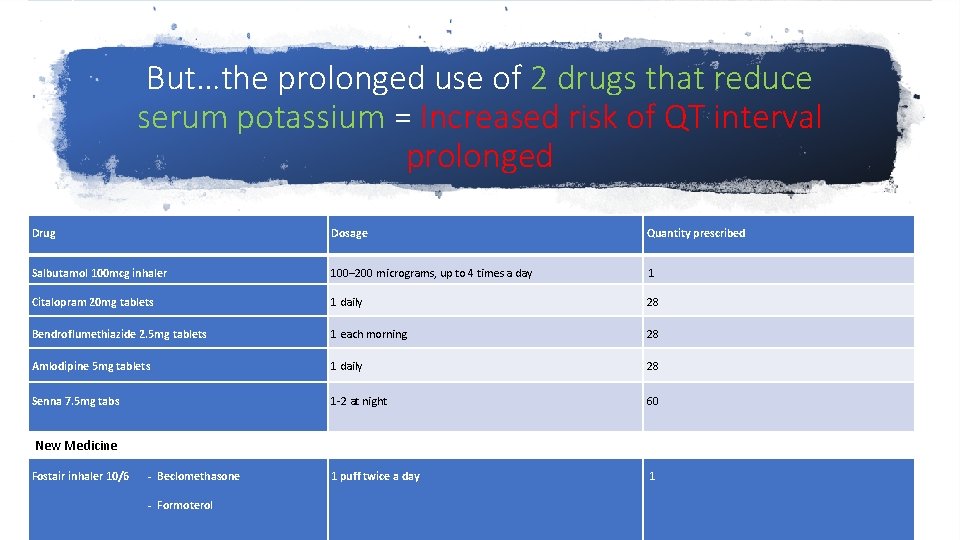
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
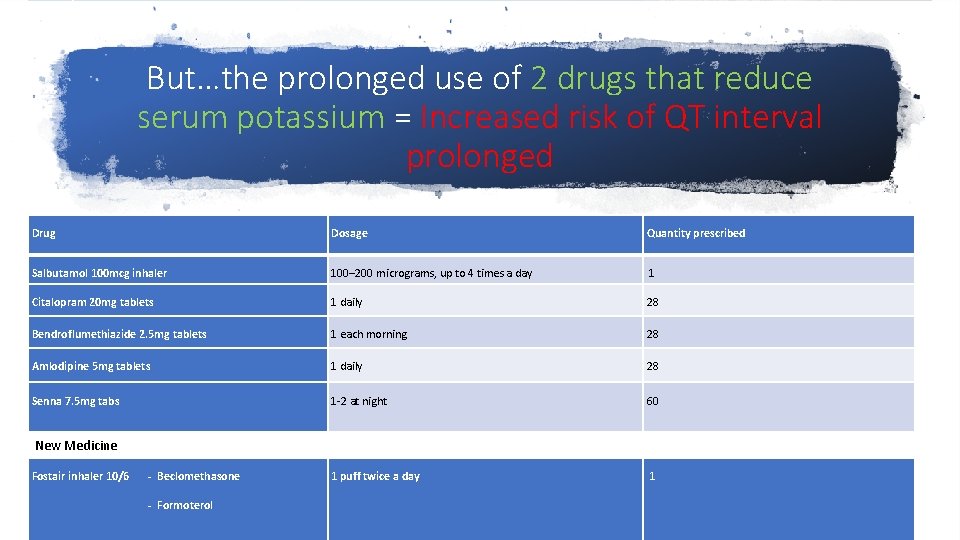
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
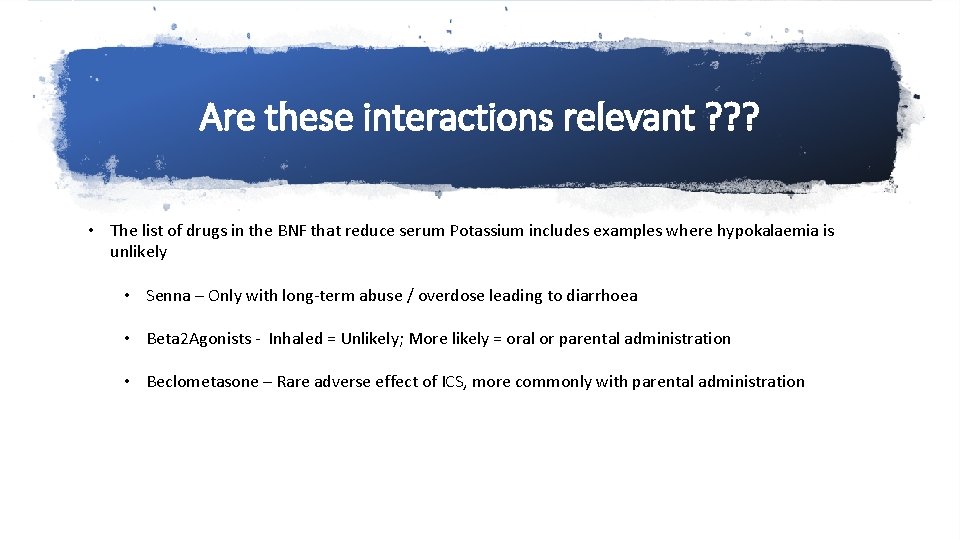
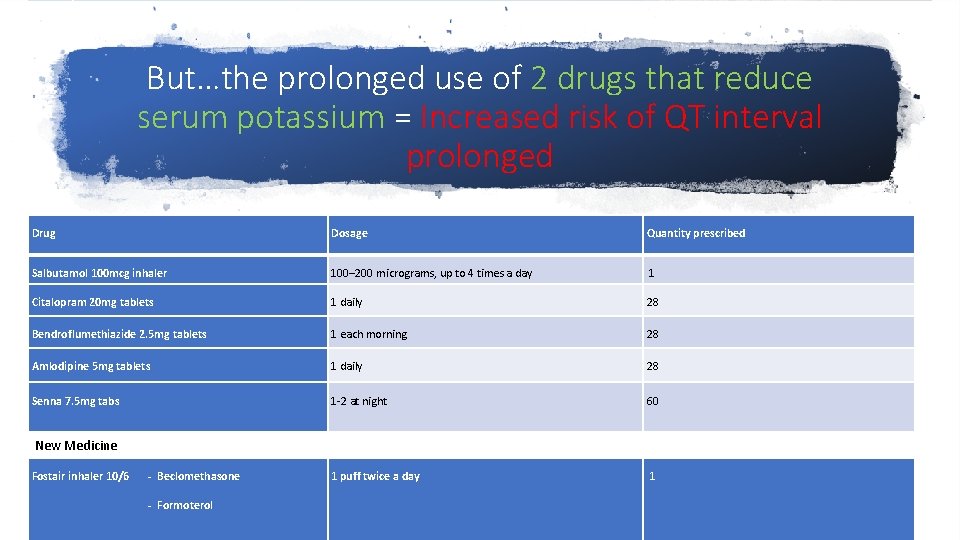
Are these interactions relevant ? ? ? • The list of drugs in the BNF that reduce serum Potassium includes examples where hypokalaemia is unlikely • Senna – Only with long-term abuse / overdose leading to diarrhoea • Beta 2 Agonists - Inhaled = Unlikely; More likely = oral or parental administration • Beclometasone – Rare adverse effect of ICS, more commonly with parental administration
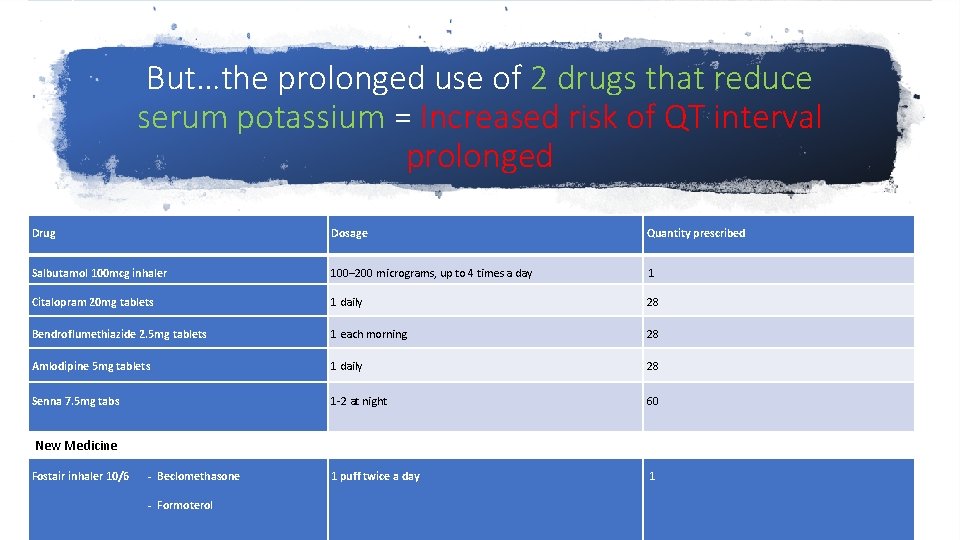
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
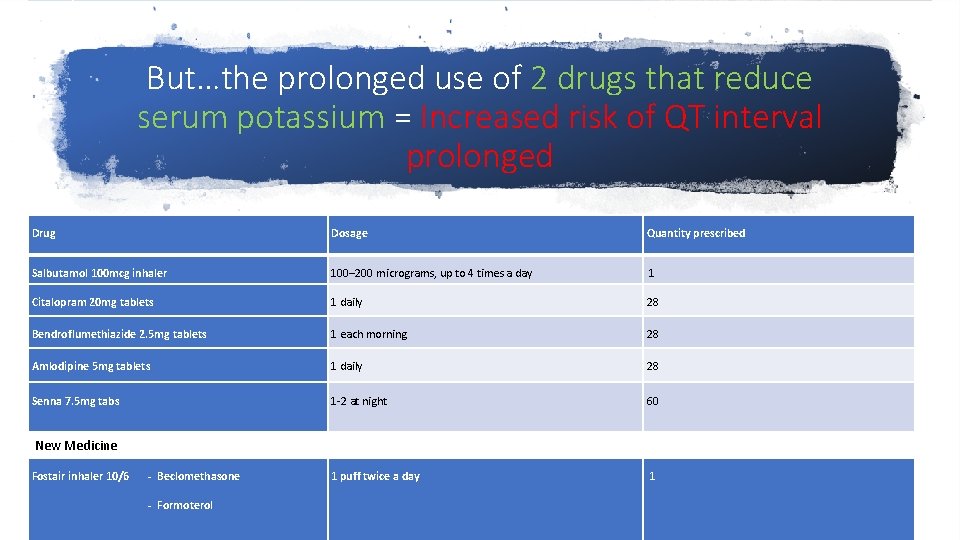
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
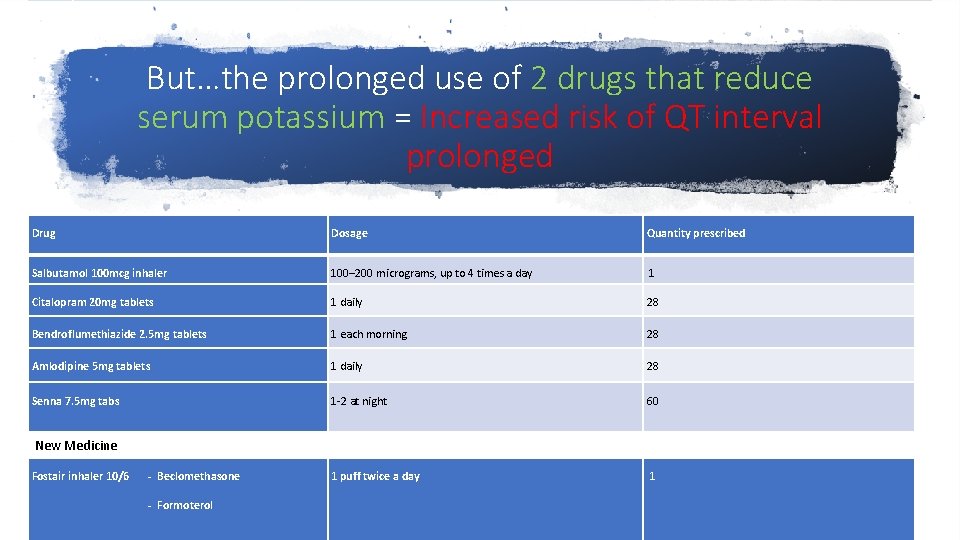
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
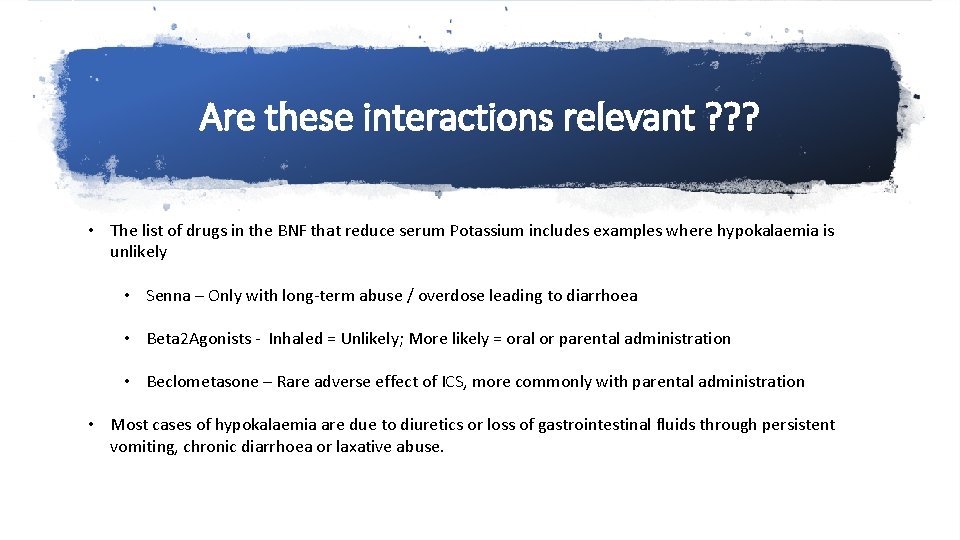
Are these interactions relevant ? ? ? • The list of drugs in the BNF that reduce serum Potassium includes examples where hypokalaemia is unlikely • Senna – Only with long-term abuse / overdose leading to diarrhoea • Beta 2 Agonists - Inhaled = Unlikely; More likely = oral or parental administration • Beclometasone – Rare adverse effect of ICS, more commonly with parental administration • Most cases of hypokalaemia are due to diuretics or loss of gastrointestinal fluids through persistent vomiting, chronic diarrhoea or laxative abuse.
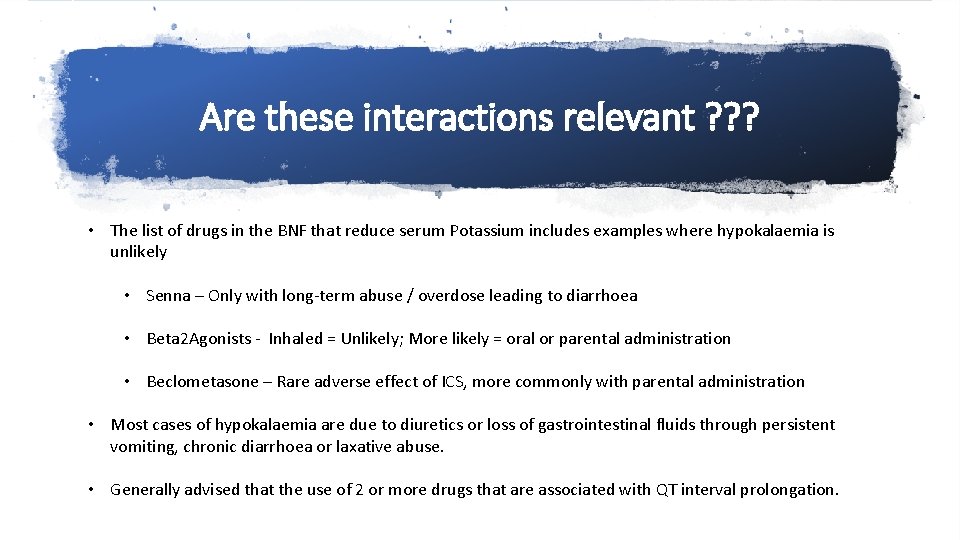
Are these interactions relevant ? ? ? • The list of drugs in the BNF that reduce serum Potassium includes examples where hypokalaemia is unlikely • Senna – Only with long-term abuse / overdose leading to diarrhoea • Beta 2 Agonists - Inhaled = Unlikely; More likely = oral or parental administration • Beclometasone – Rare adverse effect of ICS, more commonly with parental administration • Most cases of hypokalaemia are due to diuretics or loss of gastrointestinal fluids through persistent vomiting, chronic diarrhoea or laxative abuse. • Generally advised that the use of 2 or more drugs that are associated with QT interval prolongation.
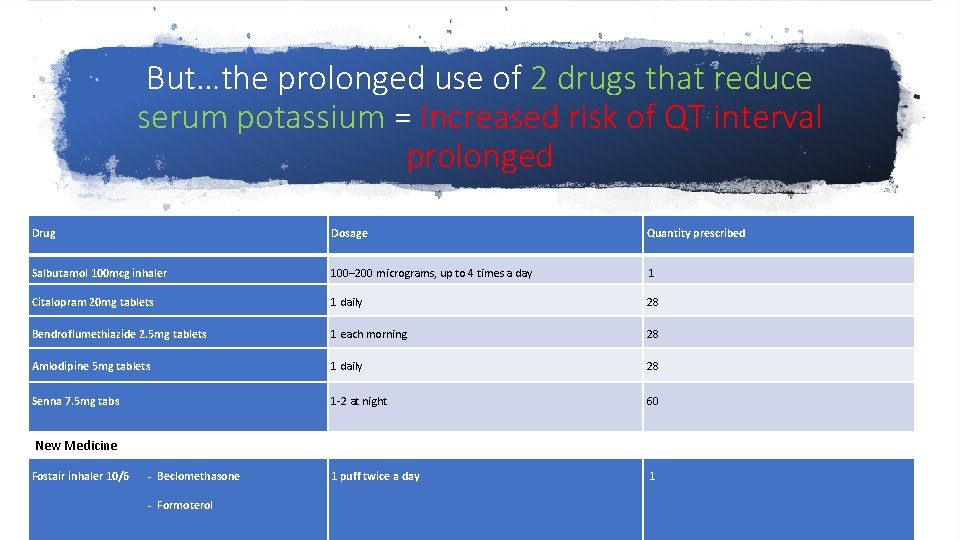
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
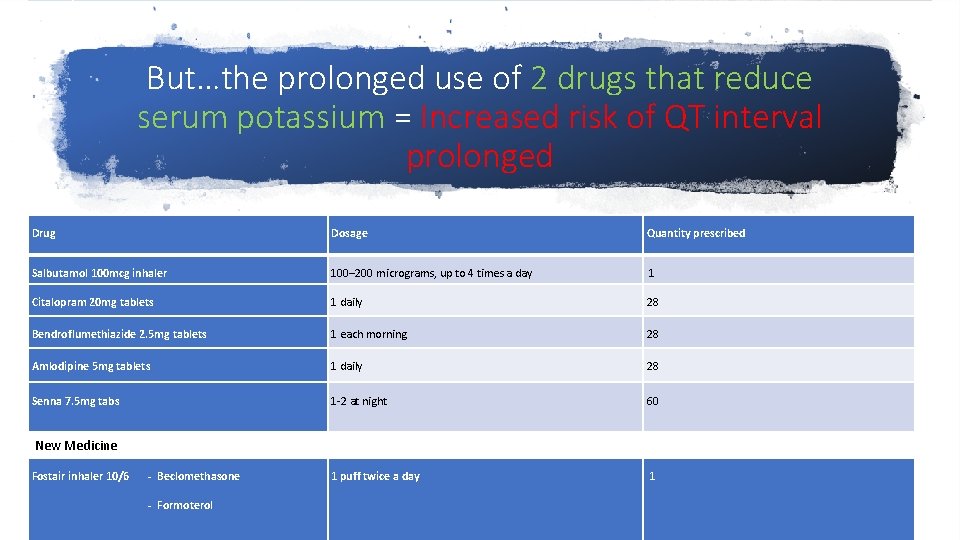
But…the prolonged use of 2 drugs that reduce serum potassium = Increased risk of QT interval prolonged Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Citalopram 20 mg tablets 1 daily 28 Bendroflumethiazide 2. 5 mg tablets 1 each morning 28 Amlodipine 5 mg tablets 1 daily 28 Senna 7. 5 mg tabs 1 -2 at night 60 1 puff twice a day 1 New Medicine Fostair inhaler 10/6 - Beclomethasone - Formoterol
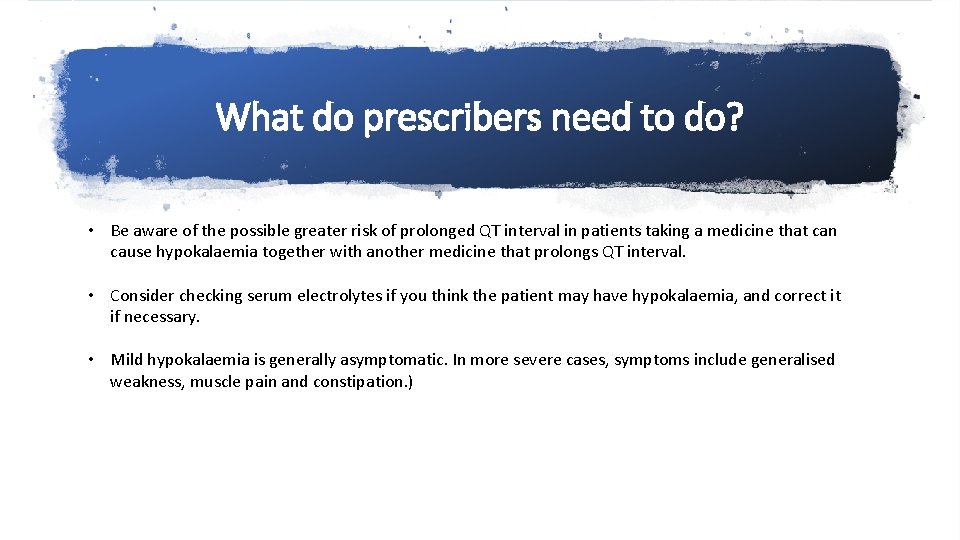
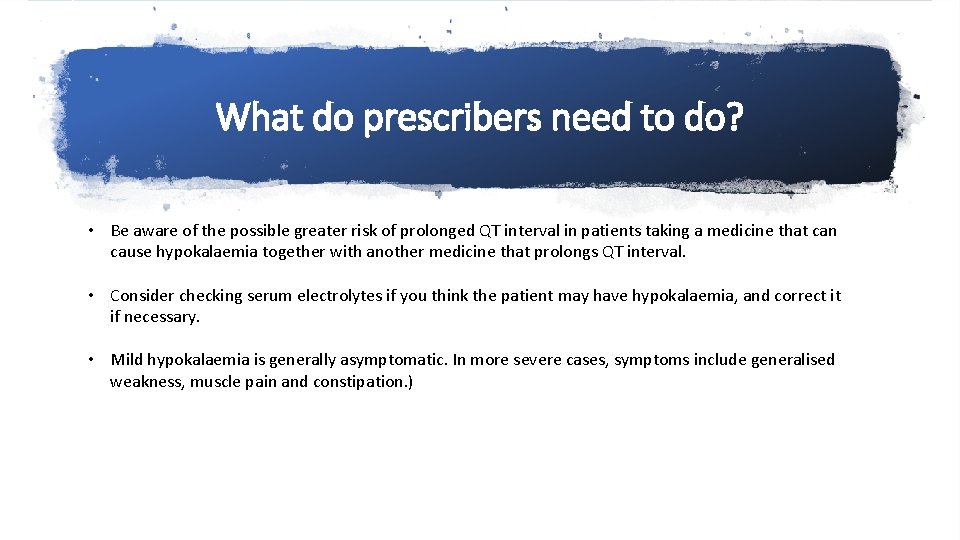
What do prescribers need to do? • Be aware of the possible greater risk of prolonged QT interval in patients taking a medicine that can cause hypokalaemia together with another medicine that prolongs QT interval. • Consider checking serum electrolytes if you think the patient may have hypokalaemia, and correct it if necessary. • Mild hypokalaemia is generally asymptomatic. In more severe cases, symptoms include generalised weakness, muscle pain and constipation. )
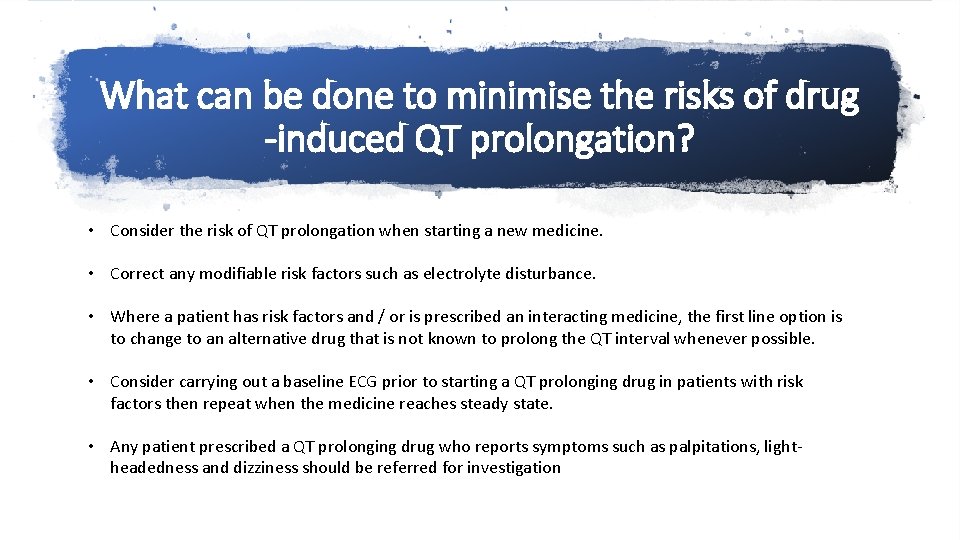
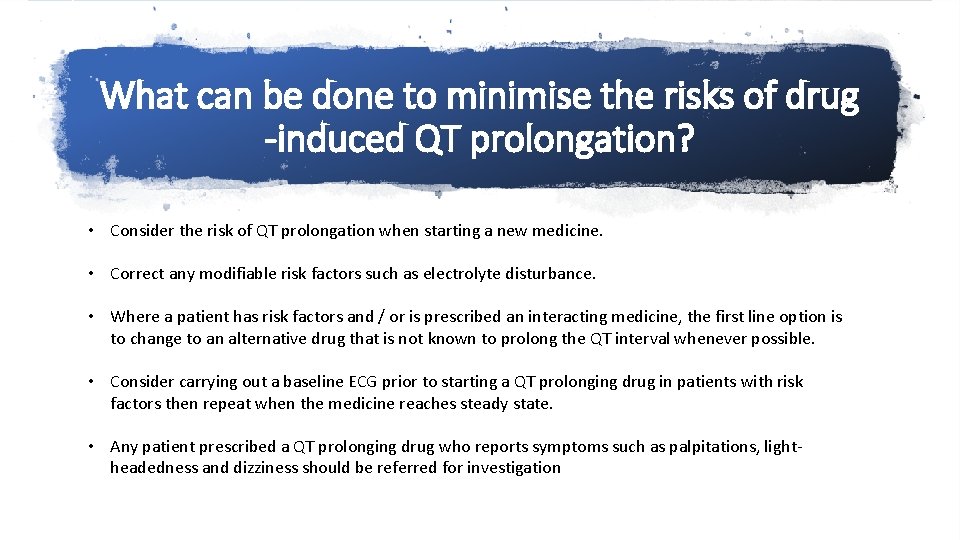
What can be done to minimise the risks of drug -induced QT prolongation? • Consider the risk of QT prolongation when starting a new medicine. • Correct any modifiable risk factors such as electrolyte disturbance. • Where a patient has risk factors and / or is prescribed an interacting medicine, the first line option is to change to an alternative drug that is not known to prolong the QT interval whenever possible. • Consider carrying out a baseline ECG prior to starting a QT prolonging drug in patients with risk factors then repeat when the medicine reaches steady state. • Any patient prescribed a QT prolonging drug who reports symptoms such as palpitations, lightheadedness and dizziness should be referred for investigation
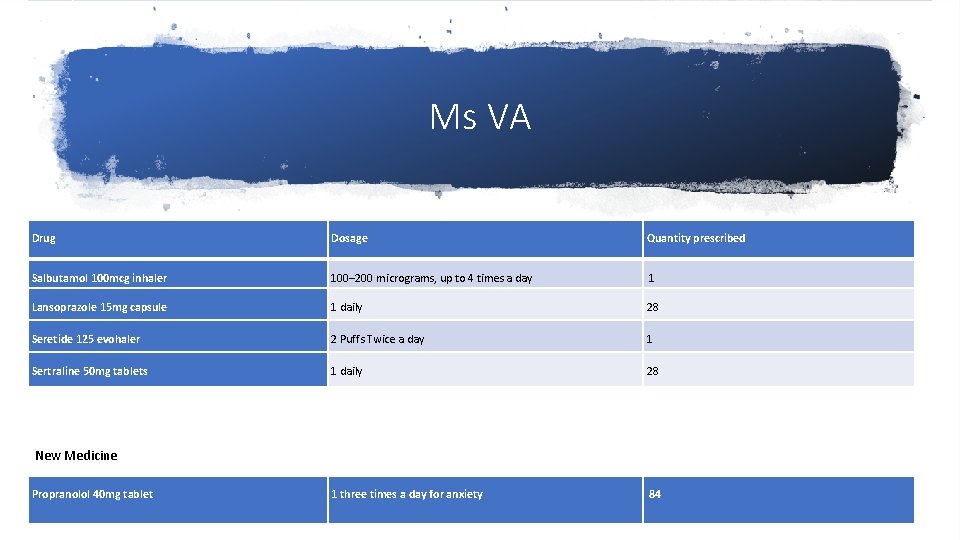
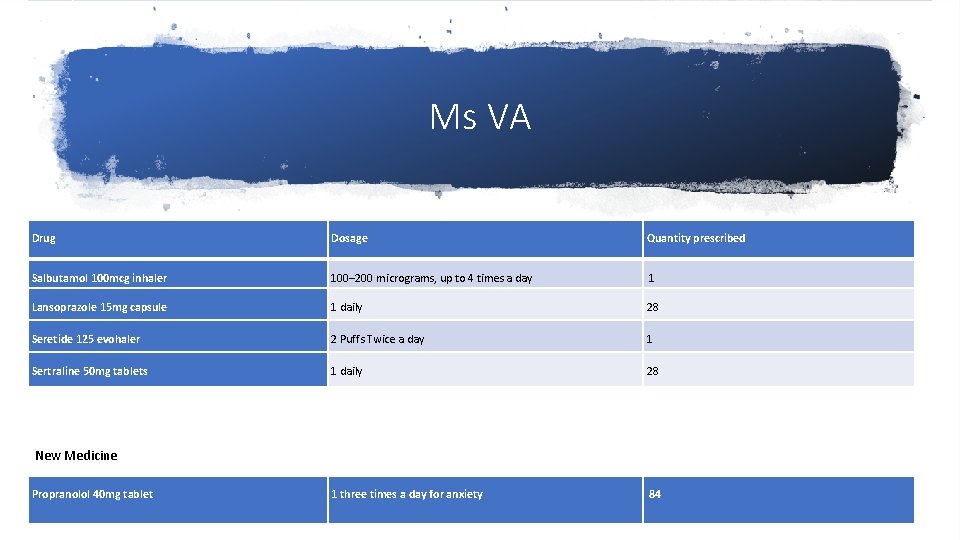
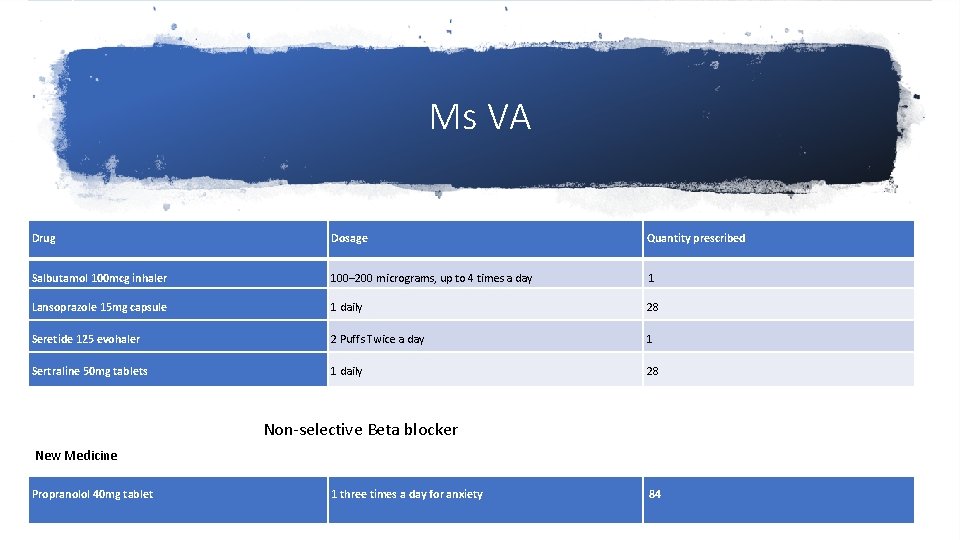
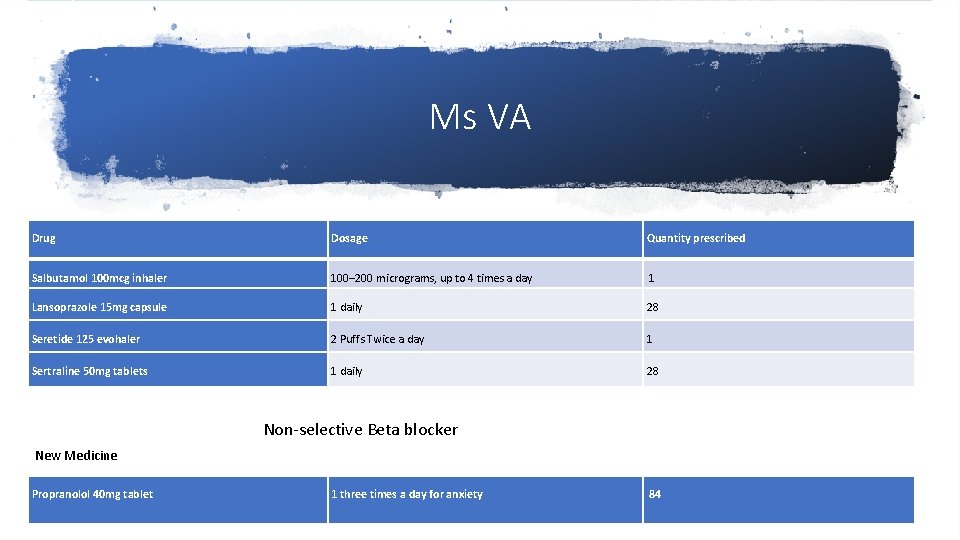
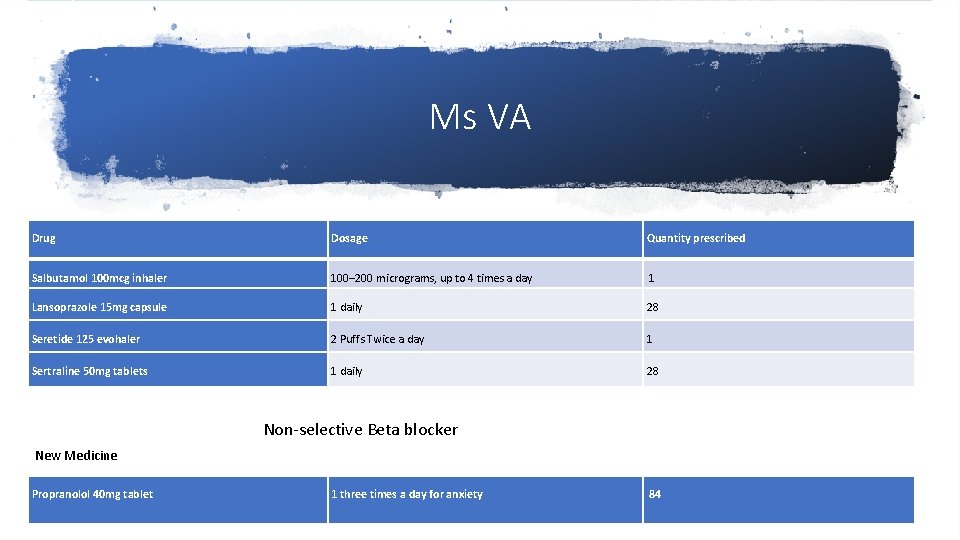
Ms VA Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Lansoprazole 15 mg capsule 1 daily 28 Seretide 125 evohaler 2 Puffs Twice a day 1 Sertraline 50 mg tablets 1 daily 28 1 three times a day for anxiety 84 New Medicine Propranolol 40 mg tablet
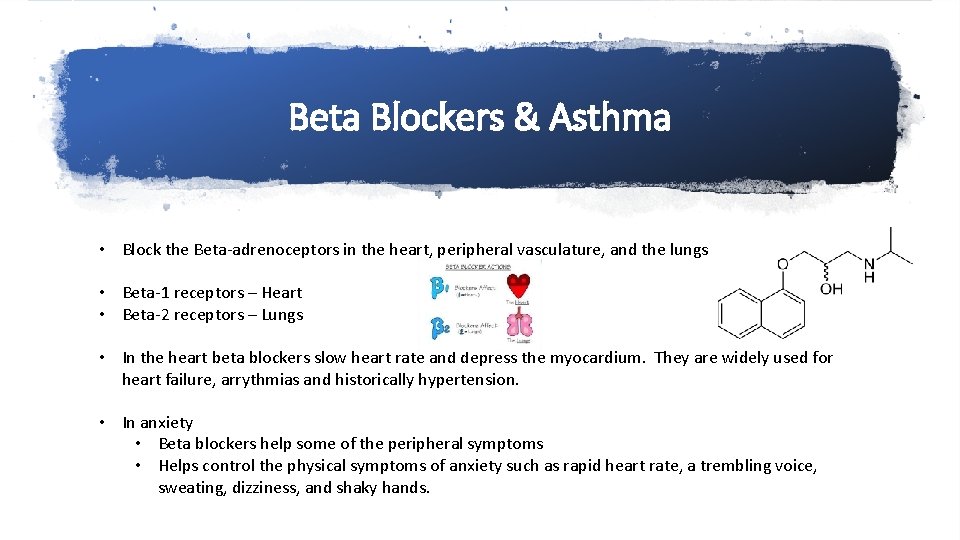
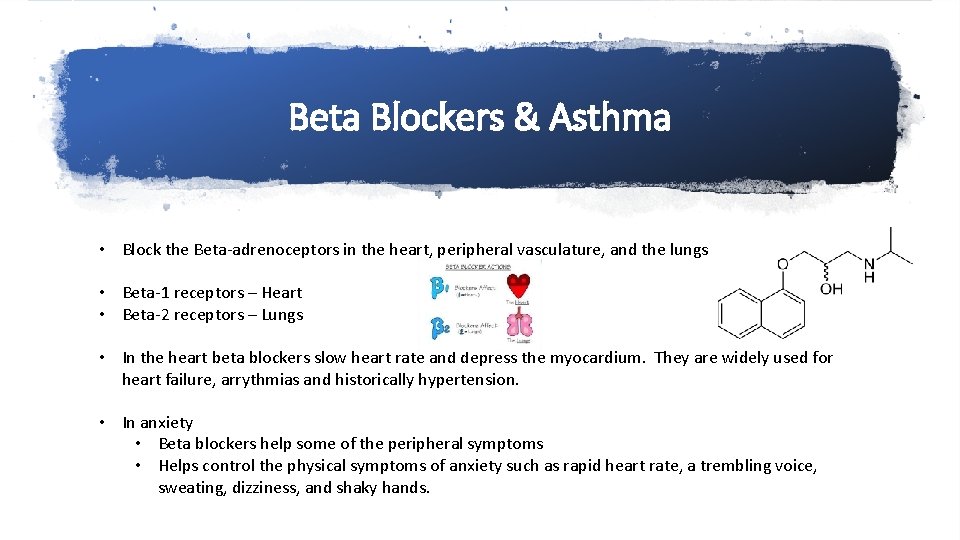
Beta Blockers & Asthma • Block the Beta-adrenoceptors in the heart, peripheral vasculature, and the lungs • Beta-1 receptors – Heart • Beta-2 receptors – Lungs • In the heart beta blockers slow heart rate and depress the myocardium. They are widely used for heart failure, arrythmias and historically hypertension. • In anxiety • Beta blockers help some of the peripheral symptoms • Helps control the physical symptoms of anxiety such as rapid heart rate, a trembling voice, sweating, dizziness, and shaky hands.
Beta Blockers & Asthma • In the Airways • Beta blockers can precipitate bronchospasm • Should be avoided in patients with a history of asthma
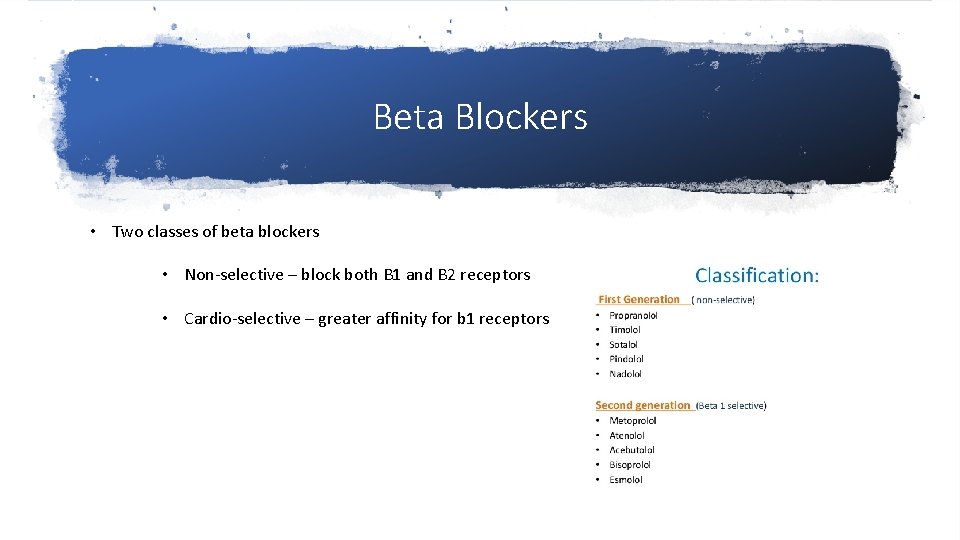
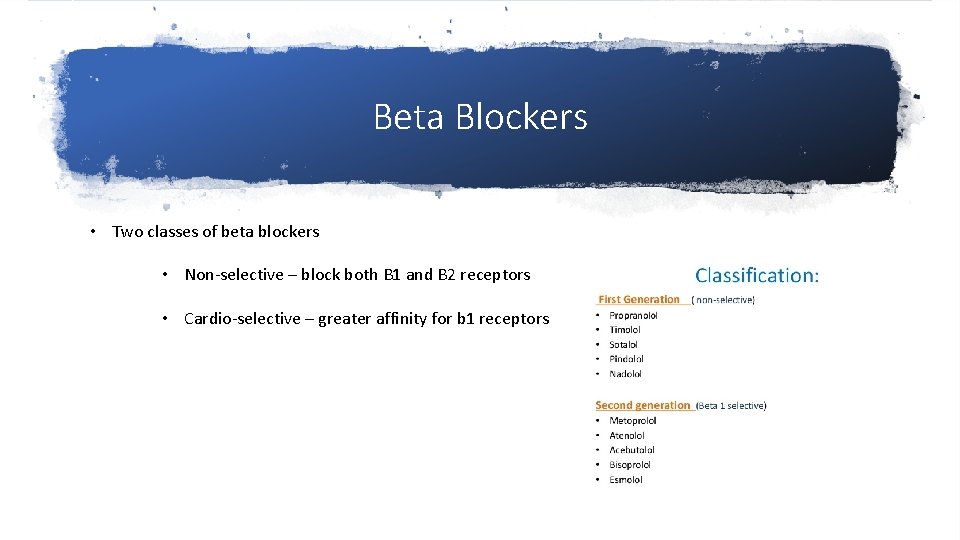
Beta Blockers • Two classes of beta blockers • Non-selective – block both B 1 and B 2 receptors • Cardio-selective – greater affinity for b 1 receptors
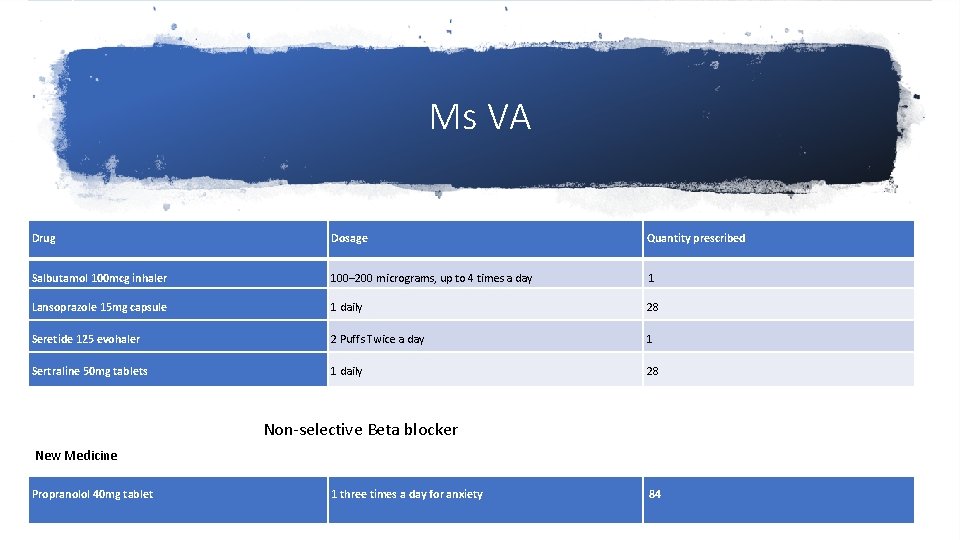
Ms VA Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Lansoprazole 15 mg capsule 1 daily 28 Seretide 125 evohaler 2 Puffs Twice a day 1 Sertraline 50 mg tablets 1 daily 28 Non-selective Beta blocker New Medicine Propranolol 40 mg tablet 1 three times a day for anxiety 84
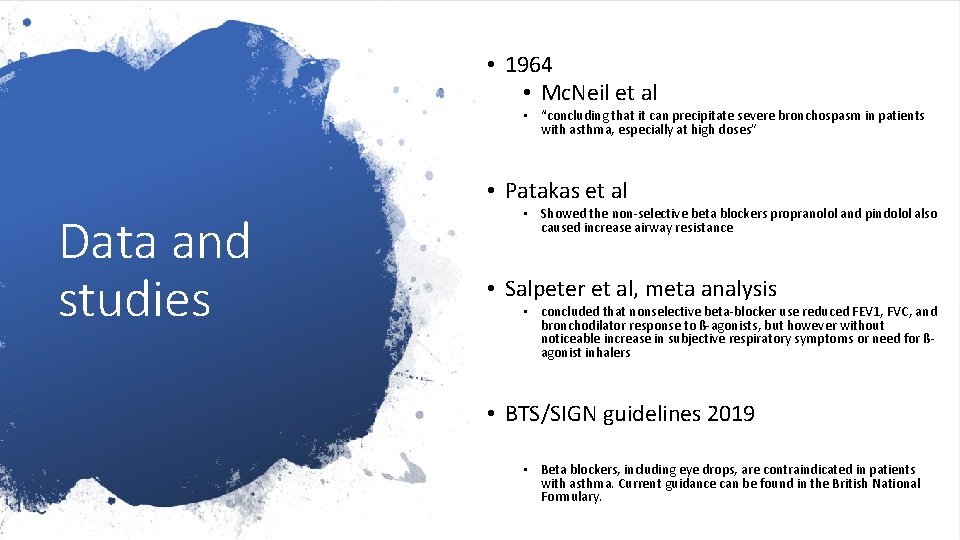
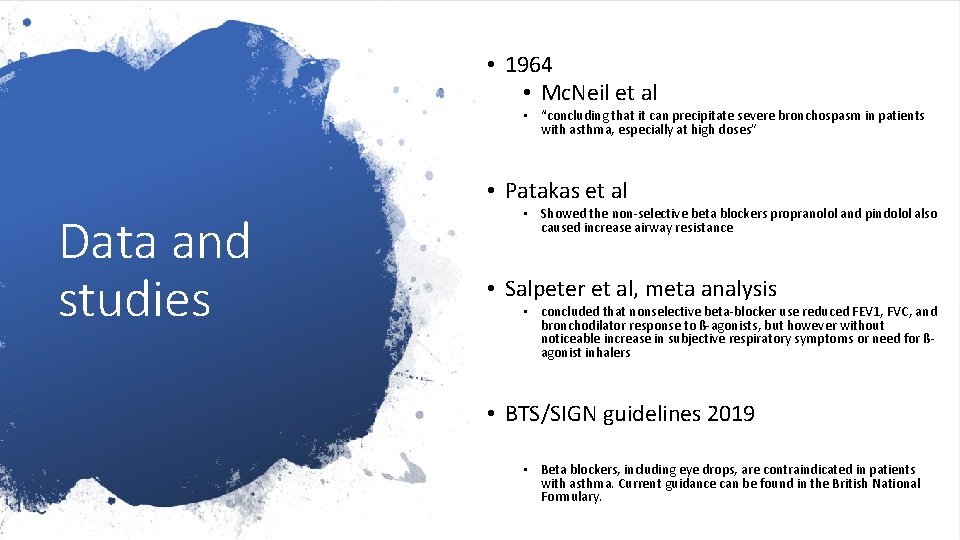
• 1964 • Mc. Neil et al • “concluding that it can precipitate severe bronchospasm in patients with asthma, especially at high doses” • Patakas et al Data and studies • Showed the non-selective beta blockers propranolol and pindolol also caused increase airway resistance • Salpeter et al, meta analysis • concluded that nonselective beta-blocker use reduced FEV 1, FVC, and bronchodilator response to ß-agonists, but however without noticeable increase in subjective respiratory symptoms or need for ßagonist inhalers • BTS/SIGN guidelines 2019 • Beta blockers, including eye drops, are contraindicated in patients with asthma. Current guidance can be found in the British National Formulary.
Ms VA Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Lansoprazole 15 mg capsule 1 daily 28 Seretide 125 evohaler 2 Puffs Twice a day 1 Sertraline 50 mg tablets 1 daily 28 Non-selective Beta blocker New Medicine Propranolol 40 mg tablet 1 three times a day for anxiety 84
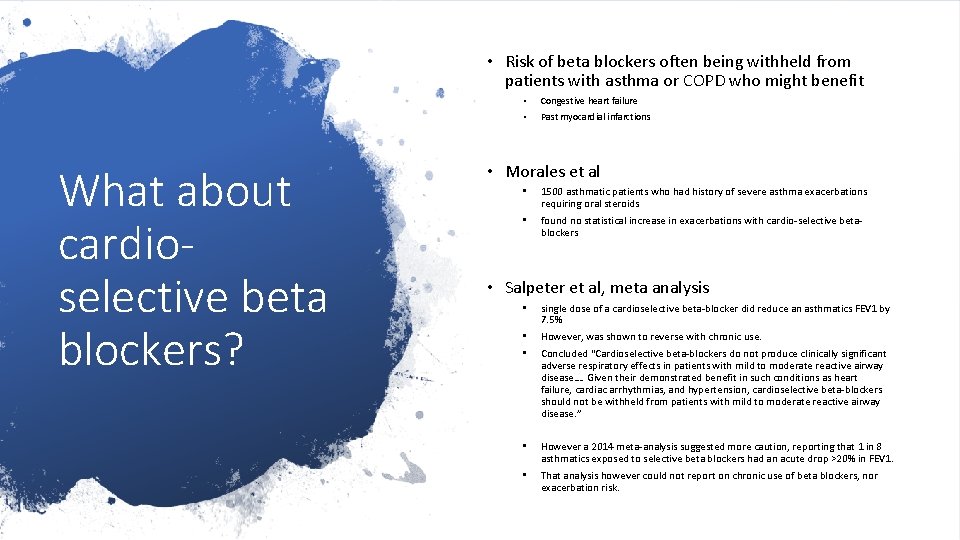
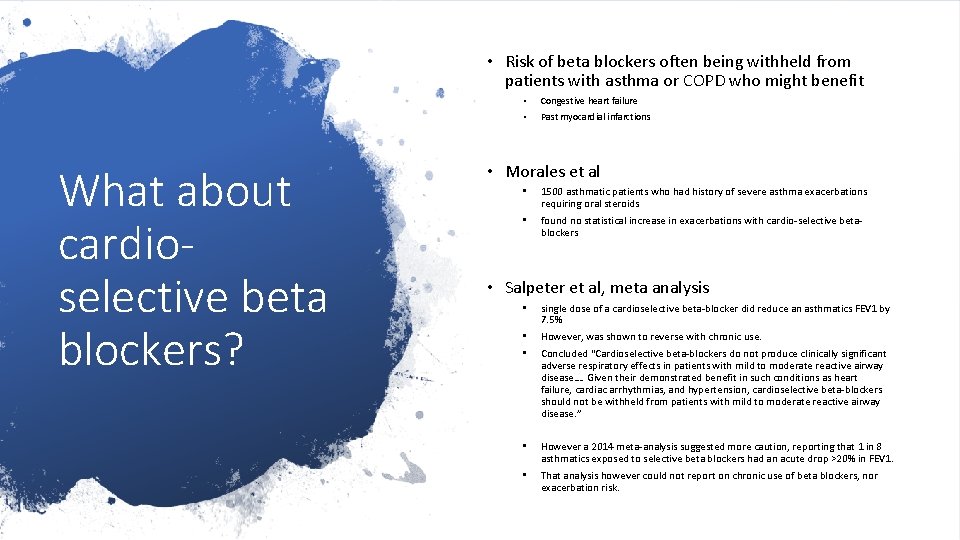
• Risk of beta blockers often being withheld from patients with asthma or COPD who might benefit What about cardioselective beta blockers? • Congestive heart failure • Past myocardial infarctions • Morales et al • 1500 asthmatic patients who had history of severe asthma exacerbations requiring oral steroids • found no statistical increase in exacerbations with cardio-selective betablockers • Salpeter et al, meta analysis • single dose of a cardioselective beta-blocker did reduce an asthmatics FEV 1 by 7. 5% • • However, was shown to reverse with chronic use. • However a 2014 meta-analysis suggested more caution, reporting that 1 in 8 asthmatics exposed to selective beta blockers had an acute drop >20% in FEV 1. • That analysis however could not report on chronic use of beta blockers, nor exacerbation risk. Concluded “Cardioselective beta-blockers do not produce clinically significant adverse respiratory effects in patients with mild to moderate reactive airway disease…. Given their demonstrated benefit in such conditions as heart failure, cardiac arrhythmias, and hypertension, cardioselective beta-blockers should not be withheld from patients with mild to moderate reactive airway disease. ”
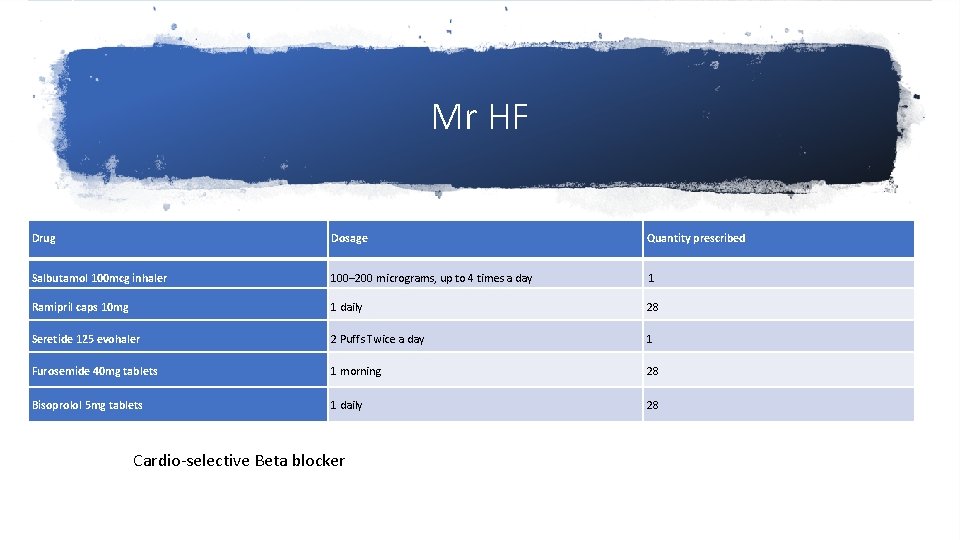
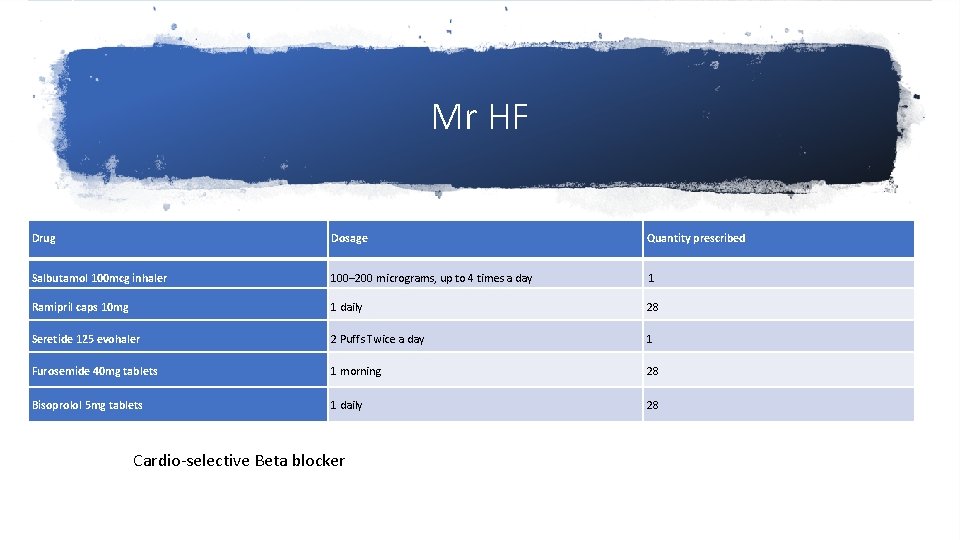
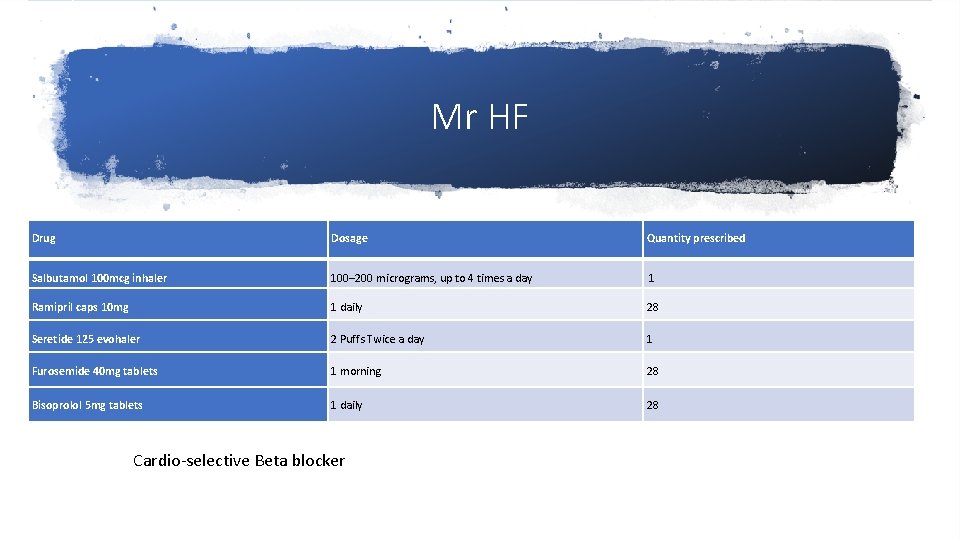
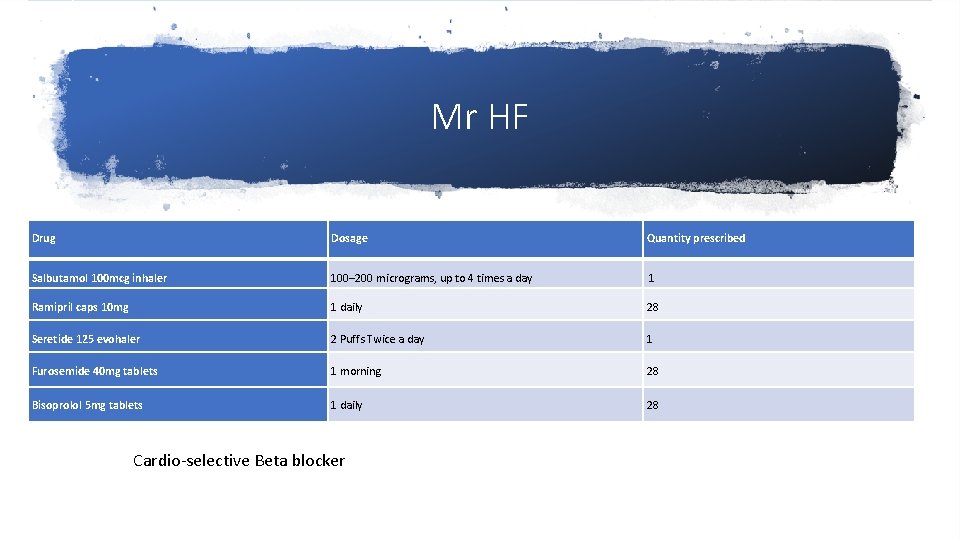
Mr HF Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Ramipril caps 10 mg 1 daily 28 Seretide 125 evohaler 2 Puffs Twice a day 1 Furosemide 40 mg tablets 1 morning 28 Bisoprolol 5 mg tablets 1 daily 28 Cardio-selective Beta blocker
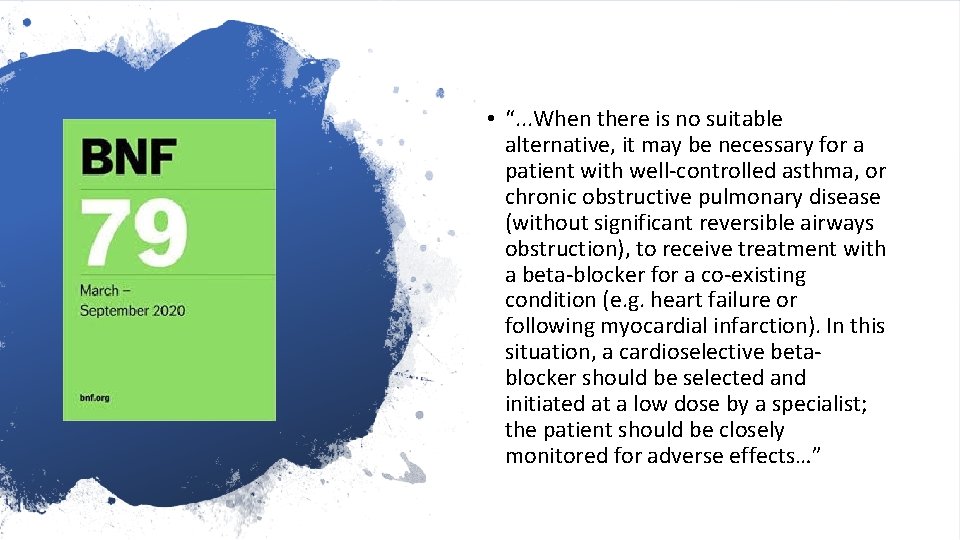
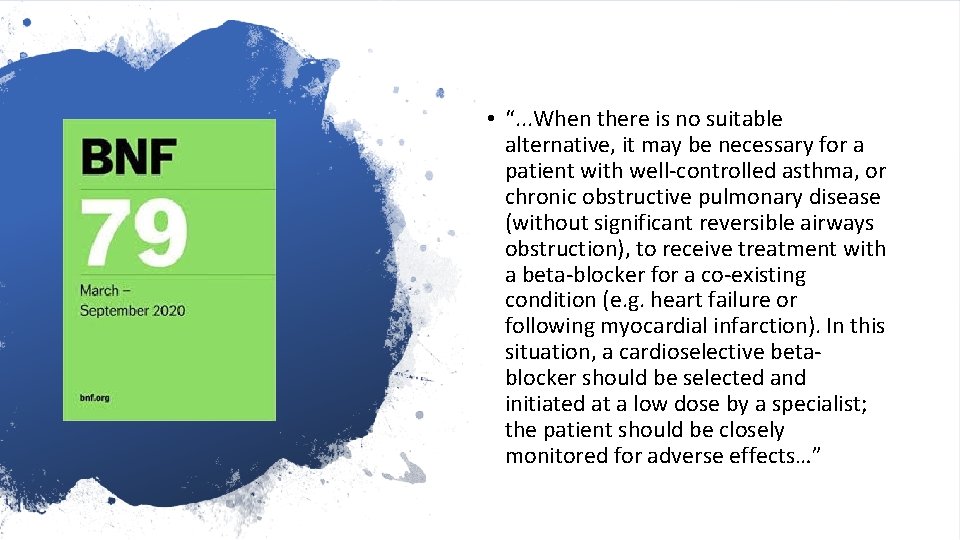
• “. . . When there is no suitable alternative, it may be necessary for a patient with well-controlled asthma, or chronic obstructive pulmonary disease (without significant reversible airways obstruction), to receive treatment with a beta-blocker for a co-existing condition (e. g. heart failure or following myocardial infarction). In this situation, a cardioselective betablocker should be selected and initiated at a low dose by a specialist; the patient should be closely monitored for adverse effects…”
Mr HF Drug Dosage Quantity prescribed Salbutamol 100 mcg inhaler 100– 200 micrograms, up to 4 times a day 1 Ramipril caps 10 mg 1 daily 28 Seretide 125 evohaler 2 Puffs Twice a day 1 Furosemide 40 mg tablets 1 morning 28 Bisoprolol 5 mg tablets 1 daily 28 Cardio-selective Beta blocker
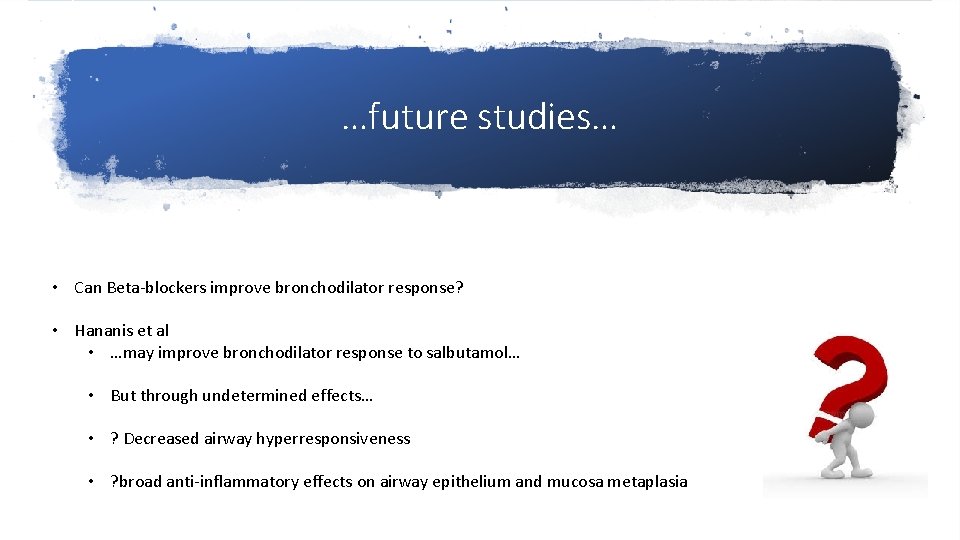
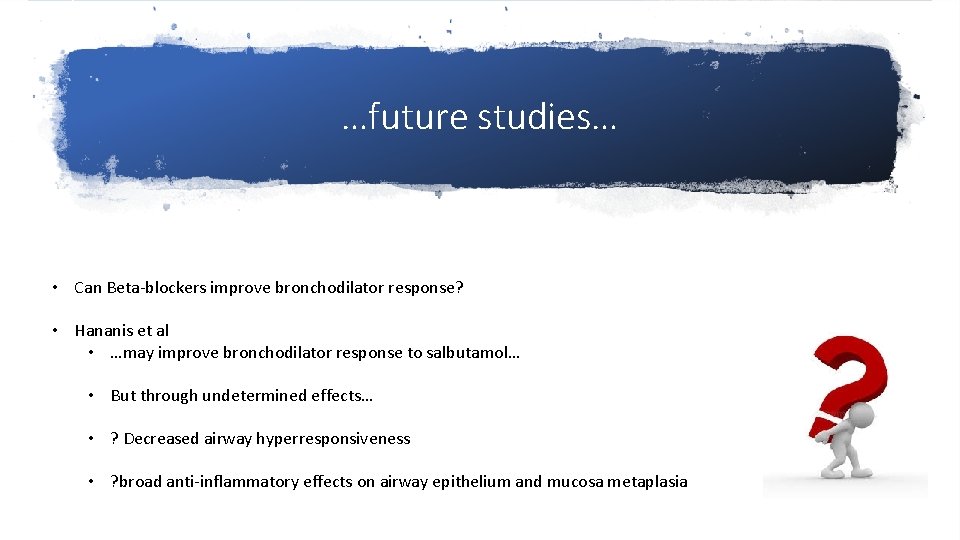
…future studies… • Can Beta-blockers improve bronchodilator response? • Hananis et al • …may improve bronchodilator response to salbutamol… • But through undetermined effects… • ? Decreased airway hyperresponsiveness • ? broad anti-inflammatory effects on airway epithelium and mucosa metaplasia
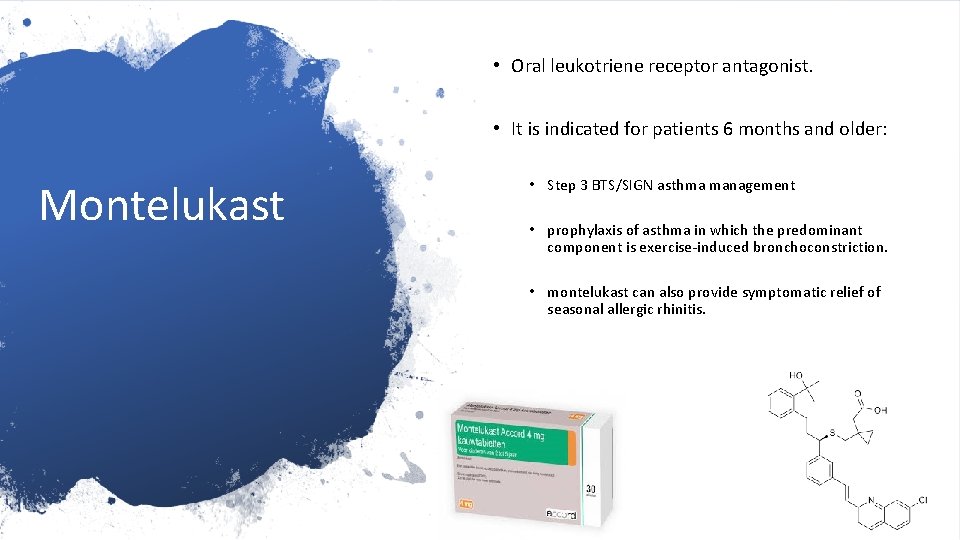
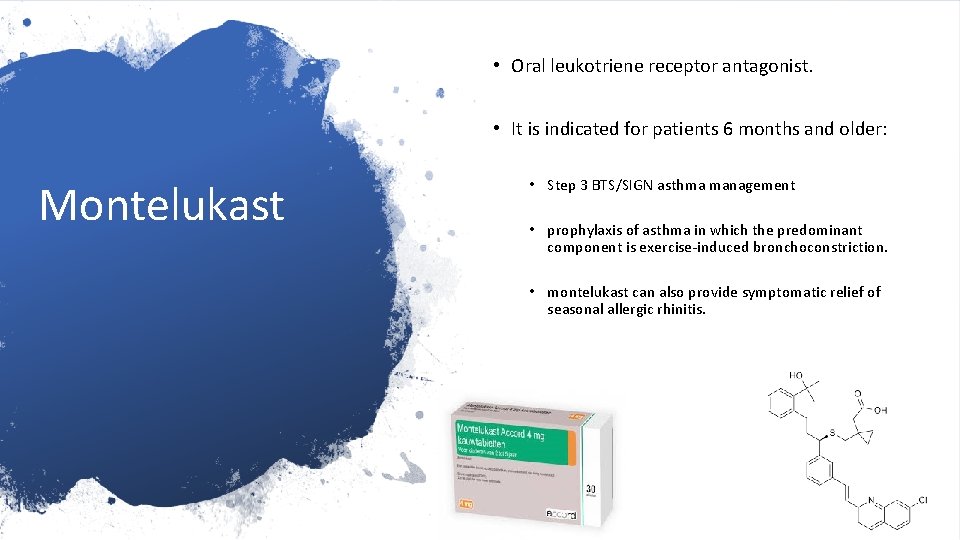
• Oral leukotriene receptor antagonist. • It is indicated for patients 6 months and older: Montelukast • Step 3 BTS/SIGN asthma management • prophylaxis of asthma in which the predominant component is exercise-induced bronchoconstriction. • montelukast can also provide symptomatic relief of seasonal allergic rhinitis.
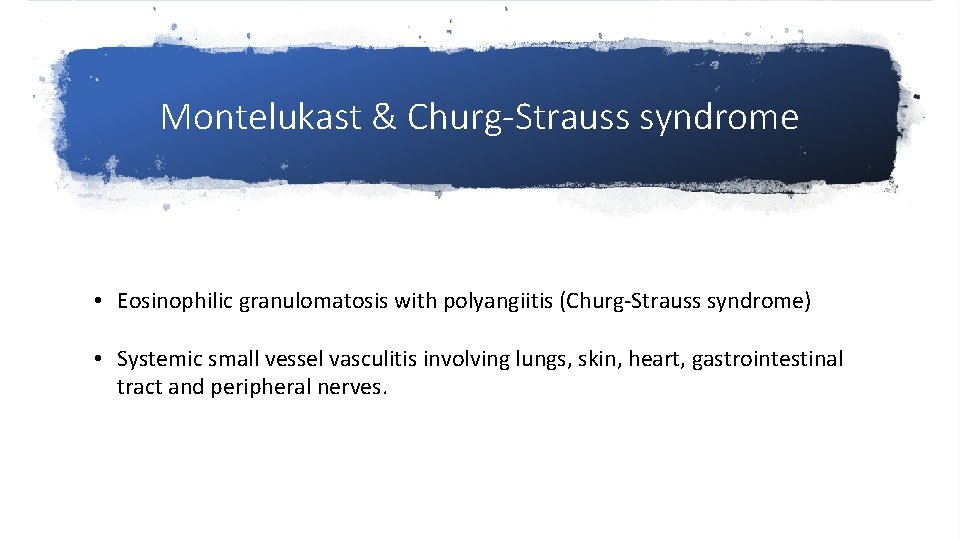
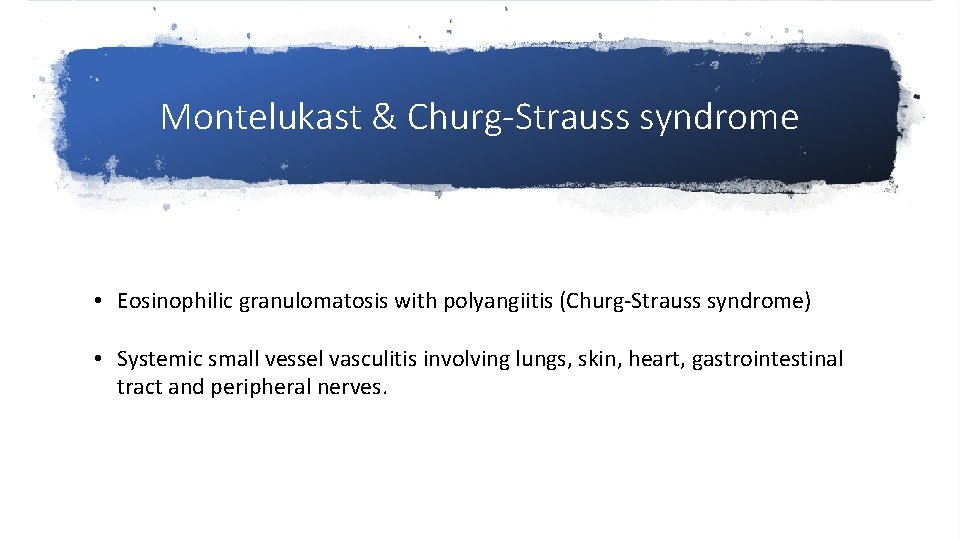
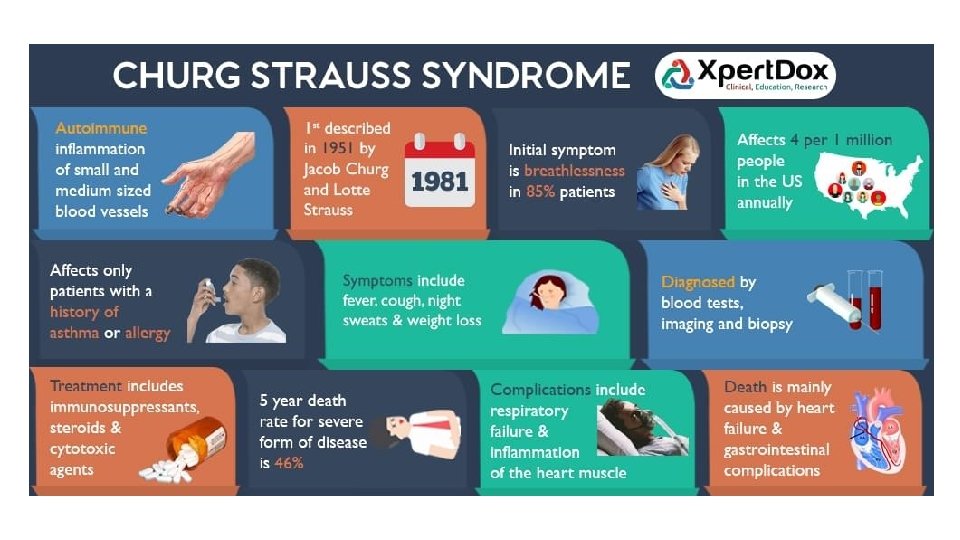
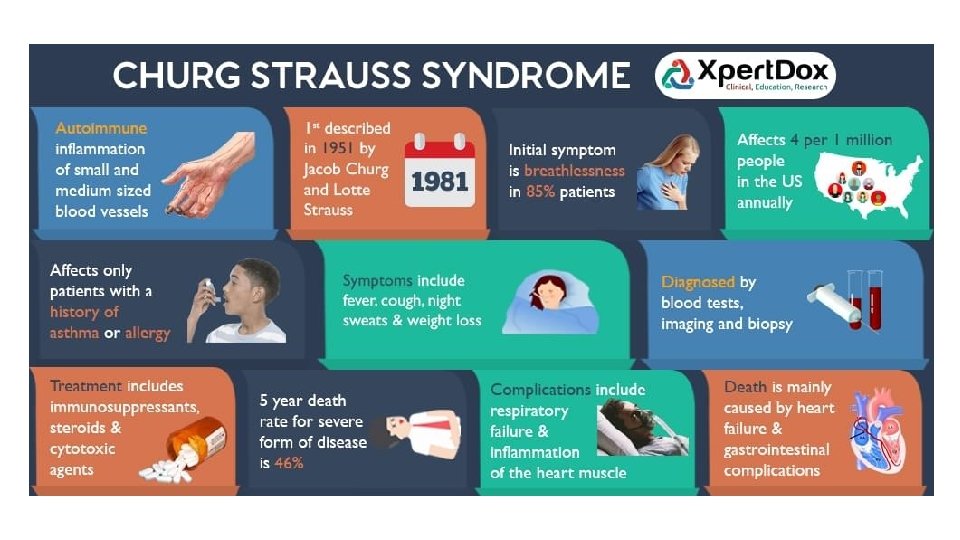
Montelukast & Churg-Strauss syndrome • Eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome) • Systemic small vessel vasculitis involving lungs, skin, heart, gastrointestinal tract and peripheral nerves.
• From BNF… • “Prescribers should be alert to the development of eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, or peripheral neuropathy. ”
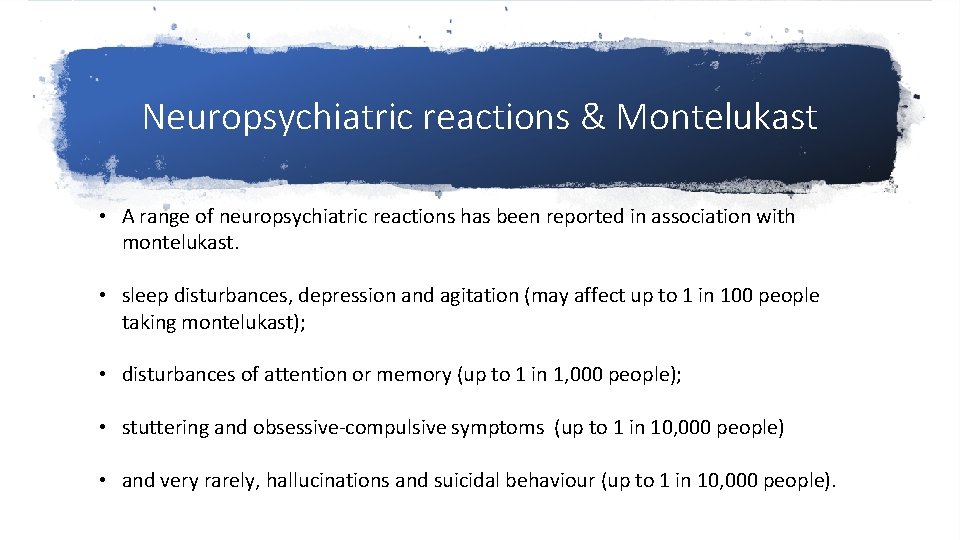
Neuropsychiatric reactions & Montelukast • A range of neuropsychiatric reactions has been reported in association with montelukast. • sleep disturbances, depression and agitation (may affect up to 1 in 100 people taking montelukast); • disturbances of attention or memory (up to 1 in 1, 000 people); • stuttering and obsessive-compulsive symptoms (up to 1 in 10, 000 people) • and very rarely, hallucinations and suicidal behaviour (up to 1 in 10, 000 people).
Neuropsychiatric reactions • The EU review also evaluated very rare reports of cases of speech impairment (dysphemia), described as ‘stuttering’. Most of the cases were reported in children younger than 5 years, occurred shortly after montelukast was started (median time to onset 8 days) and sometimes occurred in conjunction with other suspected neuropsychiatric events. Where information was provided, in most cases the events resolved on stopping treatment.
Advice for healthcare professionals • Be alert for neuropsychiatric reactions in patients taking montelukast; events have been reported in adults, adolescents, and children (see list of reported events below) • Advise patients and their caregivers to read carefully the list of neuropsychiatric reactions in the patient information leaflet and seek medical advice immediately should they occur • Evaluate carefully the risks and benefits of continuing treatment if neuropsychiatric reactions occur • Be aware of newly recognised neuropsychiatric reactions of speech impairment (stuttering) and obsessive–compulsive symptoms • Report suspected adverse drug reactions associated with montelukast to the Yellow Card Scheme
Polypharmacy
• Discuss relationship between depression / anxiety and SABA over use. • From nrad…Psychosocial factors contributing to the risk of asthma death and its perception were identified by panels in 51 (26%) of those who died, and included depression and mental health issues in 32 (16%) and substance misuse in 12 (6%).
 Alex moores
Alex moores Barrier technique in burns
Barrier technique in burns Darroch moores
Darroch moores Moores law graph
Moores law graph Moores head
Moores head Madisonmoores nudes
Madisonmoores nudes Moores ssm
Moores ssm Andrew moores
Andrew moores Eldridge moores cause of death
Eldridge moores cause of death Interactions between ais and internal and external parties
Interactions between ais and internal and external parties Qualities behaviors and complexities
Qualities behaviors and complexities Graphing monetary and fiscal policy interactions
Graphing monetary and fiscal policy interactions The properties and interactions of magnets
The properties and interactions of magnets Sphere interactions
Sphere interactions 6.1 habitats niches and species interactions
6.1 habitats niches and species interactions Integral product architecture
Integral product architecture Factors that influences communication
Factors that influences communication Symbiosis and species interactions keystone webquest
Symbiosis and species interactions keystone webquest Naive bayes pays attention to complex interactions and
Naive bayes pays attention to complex interactions and Product architectures
Product architectures Niches and community interactions
Niches and community interactions Regional and transregional interactions
Regional and transregional interactions Fundamental particles and interactions
Fundamental particles and interactions Regional and transregional interactions
Regional and transregional interactions Health and safety using ict
Health and safety using ict Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Chapter 16 infection control and standard precautions
Chapter 16 infection control and standard precautions Sports medicine taping techniques
Sports medicine taping techniques Noncovalent interactions
Noncovalent interactions Congress formal and informal powers
Congress formal and informal powers Species interaction
Species interaction Wikimedia commons
Wikimedia commons Sertraline interactions
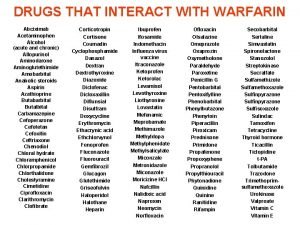
Sertraline interactions Grapefruit-drug interactions chart
Grapefruit-drug interactions chart Interactions in the environment grade 7
Interactions in the environment grade 7 What are abiotic factors
What are abiotic factors Section 20-1 review species interactions
Section 20-1 review species interactions Plant system interactions worksheet answers
Plant system interactions worksheet answers Moa of h2 antagonist
Moa of h2 antagonist Types of interactions
Types of interactions Circulatory system interactions with other systems
Circulatory system interactions with other systems Diaxial interactions
Diaxial interactions Diazepam cyp450
Diazepam cyp450 Pathway that food takes through the digestive system
Pathway that food takes through the digestive system Chapter 22 reaching out cross-cultural interactions
Chapter 22 reaching out cross-cultural interactions Vitamin e main function
Vitamin e main function Special interactions
Special interactions Cholinomimetic
Cholinomimetic Chapter 22 reaching out cross-cultural interactions
Chapter 22 reaching out cross-cultural interactions Chapter 22 reaching out cross-cultural interactions
Chapter 22 reaching out cross-cultural interactions Which of the following tells you population density
Which of the following tells you population density Heterotrophs
Heterotrophs Protein binding interactions
Protein binding interactions Nutrient interactions
Nutrient interactions Foss chemical interactions
Foss chemical interactions Interactions
Interactions Dicloxaxillin
Dicloxaxillin Chapter 5 evolution and community ecology
Chapter 5 evolution and community ecology Molecular biology
Molecular biology Protein binding interactions
Protein binding interactions Intramolecular interactions
Intramolecular interactions Protein binding interactions
Protein binding interactions Wave interactions
Wave interactions The maximum distance a wave varies from its rest position
The maximum distance a wave varies from its rest position Insight therapies involve verbal interactions
Insight therapies involve verbal interactions Integumentary interactions with other systems
Integumentary interactions with other systems Cape buffalo and cattle egrets relationship
Cape buffalo and cattle egrets relationship Skeletal interactions with other systems
Skeletal interactions with other systems Dna-protein interactions
Dna-protein interactions Light interactions
Light interactions Interaction planning process
Interaction planning process