STANDARD PRECAUTIONS ISOLATION PRACTICES STERILE TECHNIQUE STANDARD PRECAUTIONS

- Slides: 28
STANDARD PRECAUTIONS ISOLATION PRACTICES STERILE TECHNIQUE
STANDARD PRECAUTIONS 1996, CDC developed a system of isolation to provide guidelines on how to prevent spread of infection (updated 2007) ………. practices are referred to as Standard Precautions (a 2 Tiered system).
Standard Precautions include wearing protective barriers when risk of contact with any body excretions, secretions, and moist membranes and tissues. Acknowledges that all are potentially infectious.
FIRST TIER Precautions designed for care of all clients regardless of their diagnosis or presumed infection status. Standard Precautions apply to: 1) Blood 2) All body fluids, secretions, and excretions 3) Non-intact skin 4) Mucous Membranes
SECOND TIER It alerts the nurse to take additional precautions to interrupt the transmission of a specified infection or organism. These Transmission-Based Precautions are for patients known, or suspected of being infected by a particular pathogen transmission: (a) airborne precautions (b) droplet precautions (c) contact precautions
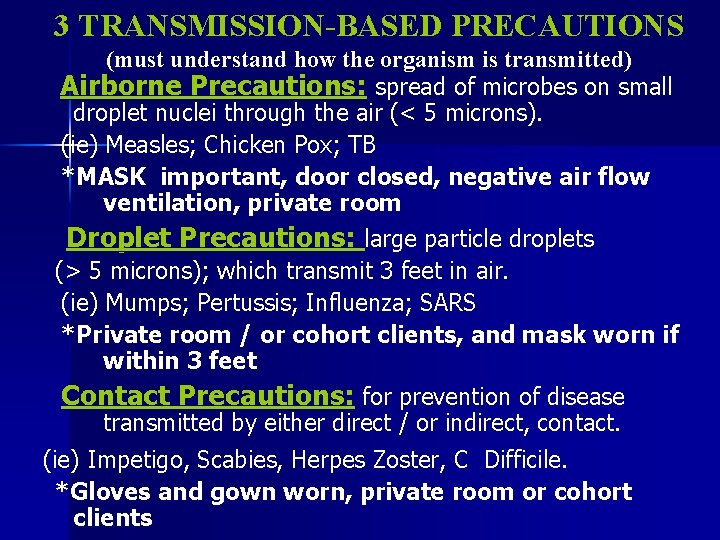
3 TRANSMISSION-BASED PRECAUTIONS (must understand how the organism is transmitted) Airborne Precautions: spread of microbes on small droplet nuclei through the air (< 5 microns). (ie) Measles; Chicken Pox; TB *MASK important, door closed, negative air flow ventilation, private room Droplet Precautions: large particle droplets (> 5 microns); which transmit 3 feet in air. (ie) Mumps; Pertussis; Influenza; SARS *Private room / or cohort clients, and mask worn if within 3 feet Contact Precautions: for prevention of disease transmitted by either direct / or indirect, contact. (ie) Impetigo, Scabies, Herpes Zoster, C Difficile. *Gloves and gown worn, private room or cohort clients
BUGS ARE GETTING SMARTER THAN THE DRUGS!! Some microorganisms that are particularly difficult to destroy. Some prevalent ones are: ~ Methicillin-Resistant Staphylococcus Aureus (MRSA) ~ Vancomycin-Resistant Enterococcus (VRE)
n Skills Text p. 197 – Box 8 -1 & Table 8 -2 – Guidelines for Standard Precautions (2 tiered system) published by the CDC in 1996 Standard Precautions Fundamentals text, p. 807 – READ *****
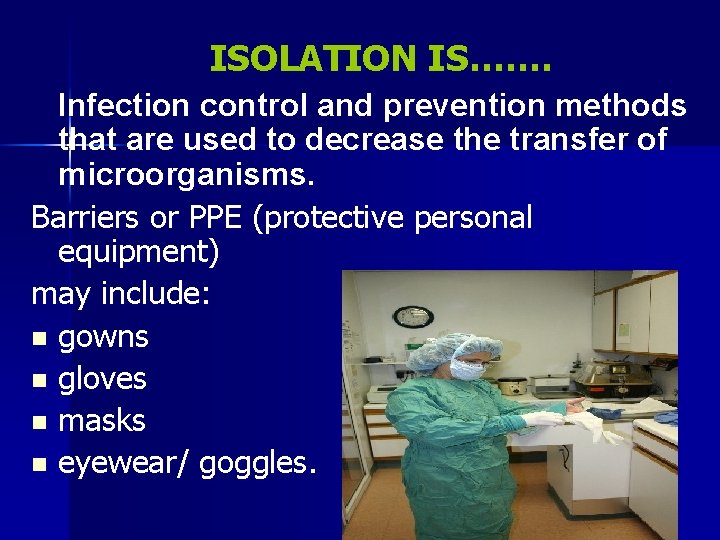
ISOLATION IS……. Infection control and prevention methods that are used to decrease the transfer of microorganisms. Barriers or PPE (protective personal equipment) may include: n gowns n gloves n masks n eyewear/ goggles.
“PROTECTIVE ISOLATION” aka “REVERSE ISOLATION” Protects the client with a compromised or suppressed immune system; who is highly susceptible to contracting an infection.
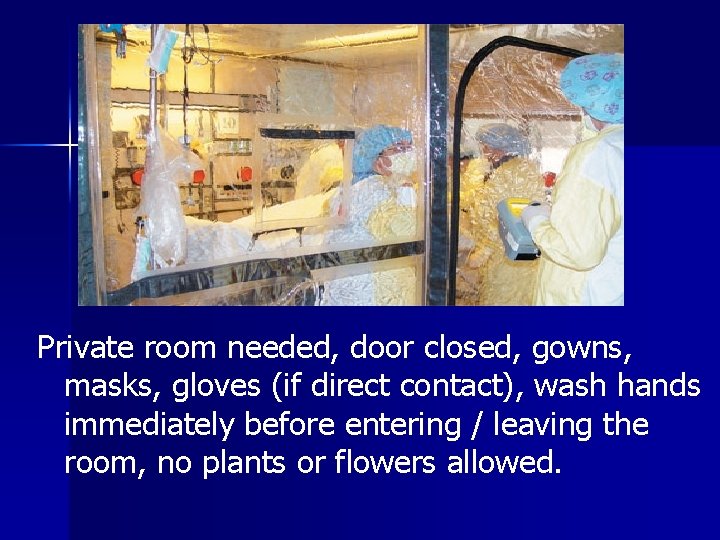
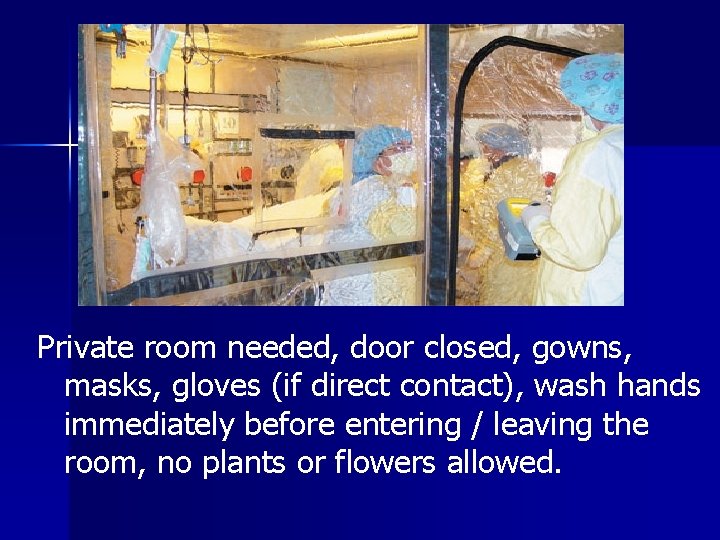
Private room needed, door closed, gowns, masks, gloves (if direct contact), wash hands immediately before entering / leaving the room, no plants or flowers allowed.
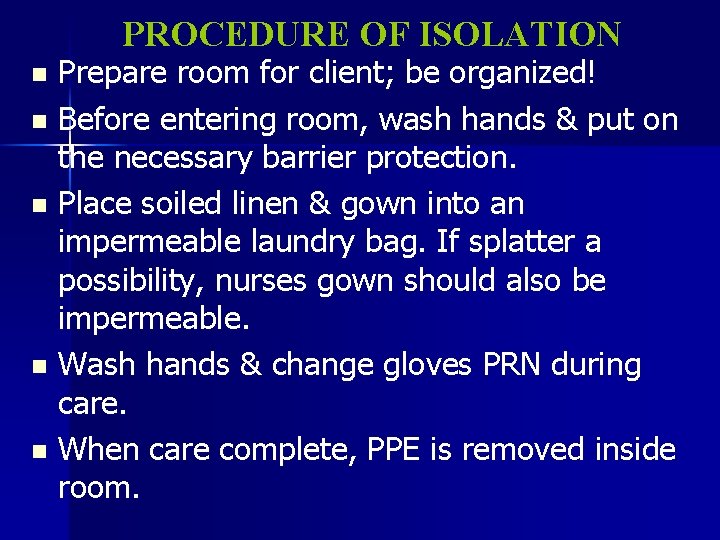
PROCEDURE OF ISOLATION Prepare room for client; be organized! n Before entering room, wash hands & put on the necessary barrier protection. n Place soiled linen & gown into an impermeable laundry bag. If splatter a possibility, nurses gown should also be impermeable. n Wash hands & change gloves PRN during care. n When care complete, PPE is removed inside room. n
In what order do you dress/undress PPE? Must think critically, esp upon leaving isolation…. . may depend upon the area in which you are working. As a general rule: ~ gloves are last put on & 1 st taken off ~ if airborne precautions, mask stays on until out of room. Consider your gloves, outside of your goggles, front of your mask, sleeves & front of your gown all to be contaminated. Remember to wash hands once all PPE removed.
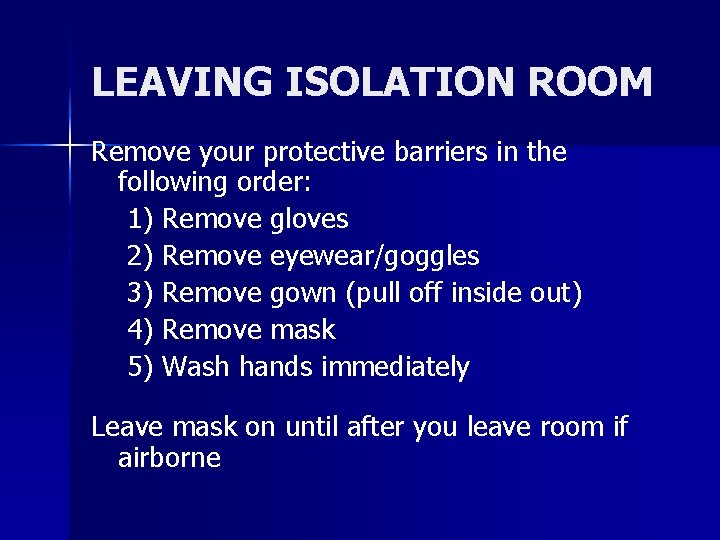
LEAVING ISOLATION ROOM Remove your protective barriers in the following order: 1) Remove gloves 2) Remove eyewear/goggles 3) Remove gown (pull off inside out) 4) Remove mask 5) Wash hands immediately Leave mask on until after you leave room if airborne
CLIENT CONCERNS RELATED TO ISOLATION Explain purpose of isolation & the necessary precautions. Sensory deprivation may be evident by signs of loneliness or boredom. S & S of depression - decreased motivation, anger, lack of appetite, or difficulty sleeping. What interventions can you plan, while working with a client in isolation?
“STERILE TECHNIQUE” aka “SURGICAL ASEPSIS”
What is the purpose of STERILE TECHNIQUE ?
PURPOSE OF STERILE TECHNIQUE To ELIMINATE all microorganisms from objects that come into contact with the tissues of the body that are normally sterile.
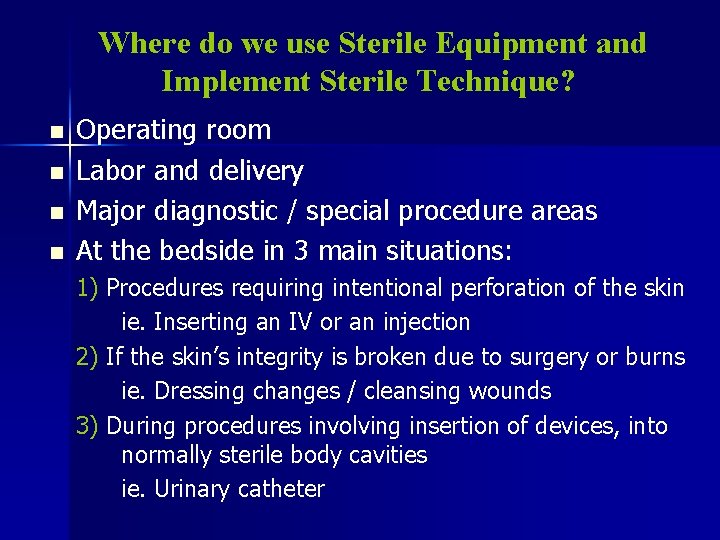
Where do we use Sterile Equipment and Implement Sterile Technique? n n Operating room Labor and delivery Major diagnostic / special procedure areas At the bedside in 3 main situations: 1) Procedures requiring intentional perforation of the skin ie. Inserting an IV or an injection 2) If the skin’s integrity is broken due to surgery or burns ie. Dressing changes / cleansing wounds 3) During procedures involving insertion of devices, into normally sterile body cavities ie. Urinary catheter
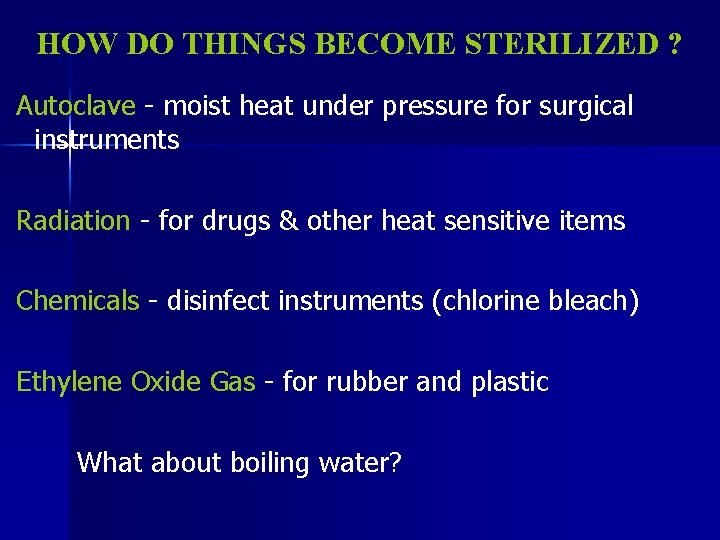
HOW DO THINGS BECOME STERILIZED ? Autoclave - moist heat under pressure for surgical instruments Radiation - for drugs & other heat sensitive items Chemicals - disinfect instruments (chlorine bleach) Ethylene Oxide Gas - for rubber and plastic What about boiling water?
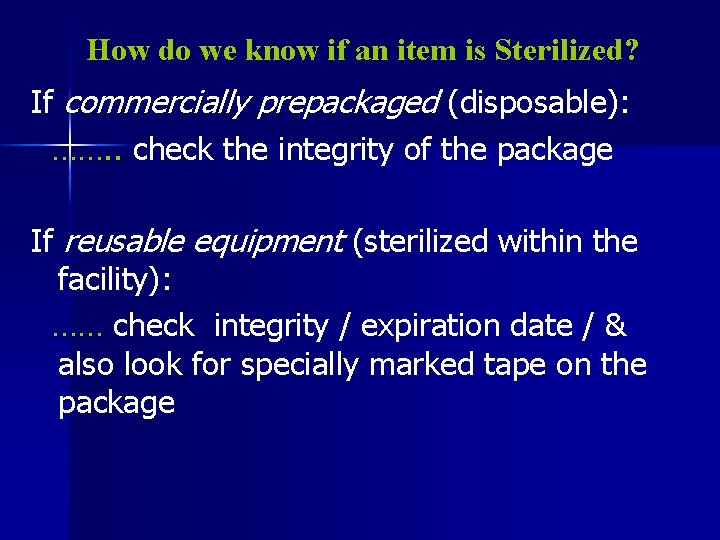
How do we know if an item is Sterilized? If commercially prepackaged (disposable): ……. . check the integrity of the package If reusable equipment (sterilized within the facility): …… check integrity / expiration date / & also look for specially marked tape on the package
AREAS WHERE STERILE EQUIPMENT IS USED AND STERILE TECHNIQUE IS NECESSARY n Operating room Labor and Delivery Major diagnostic areas n At the bedside in 3 main situations— n n – – – intentional perforation of skin (IV/injection) when skin integrity is broken (dsg change) inserting device into sterile body cavity (catheter)
Principles of Surgical Asepsis p 814 - 815 Fundamentals text A sterile object remains sterile only when touched by another sterile object. n Only sterile objects may be placed on a sterile field. n A sterile object/ or field out of the range of vision, or an object held below waist level, is considered contaminated. n A sterile object/or field, becomes contaminated by prolonged exposure to air. n
…. . Surgical Aseptic Principles continued…. If in contact with a wet contaminated surface, the sterile object/ or field becomes contaminated by capillary action. n Microbes move in the direction of gravity. n Edges of a sterile field are considered contaminated…. a 2. 5 cm border. n If ever in doubt - consider it unsterile! n

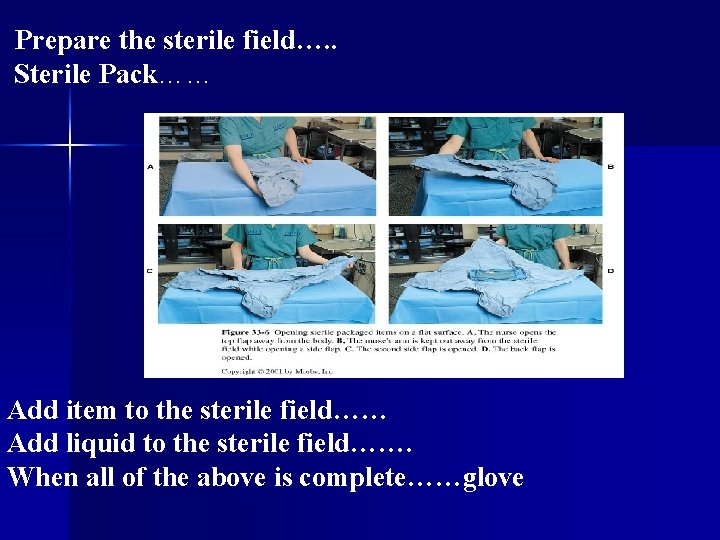
Preparing a a Sterile Dressing Tray
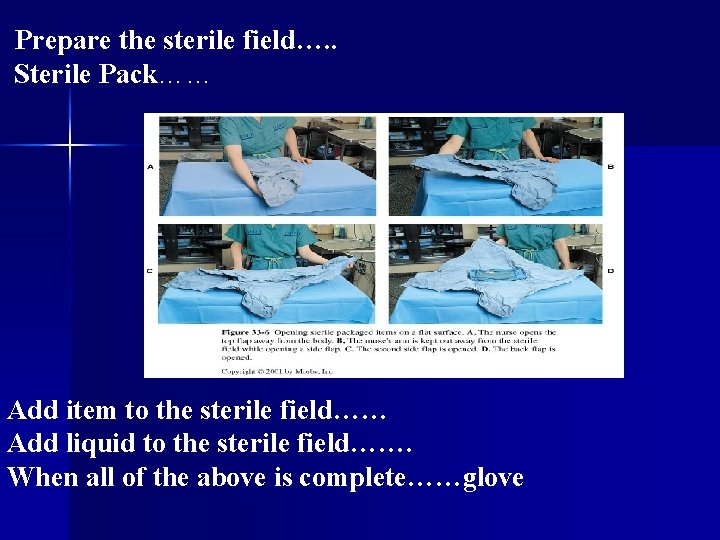
Prepare the sterile field…. . Sterile Pack…… Add item to the sterile field…… Add liquid to the sterile field……. When all of the above is complete……glove
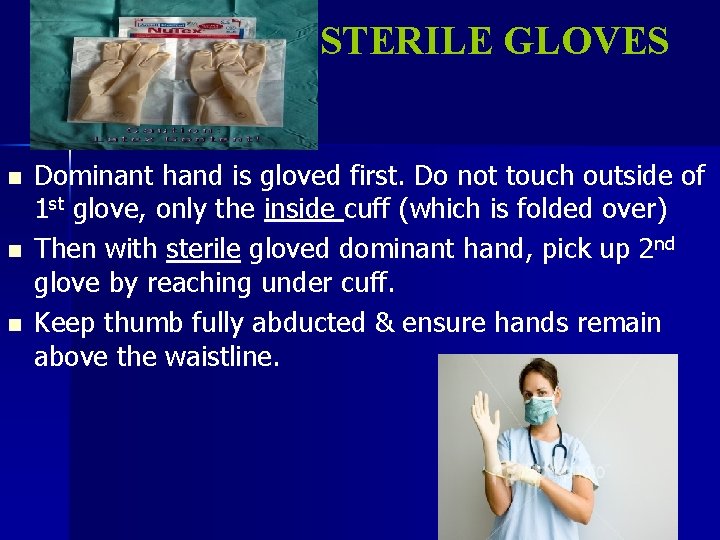
STERILE GLOVES n n n Dominant hand is gloved first. Do not touch outside of 1 st glove, only the inside cuff (which is folded over) Then with sterile gloved dominant hand, pick up 2 nd glove by reaching under cuff. Keep thumb fully abducted & ensure hands remain above the waistline.
Please refer to Skills testing schedule N 125 Exam December 16, 2008 (0900 h) @ Oland’s Center Gymnasium GOOD LUCK !