DM 2 Outpatient Glycemic Control DM Inpatient Glycemic

















































- Slides: 89

DM 2 Outpatient Glycemic Control
DM Inpatient Glycemic control
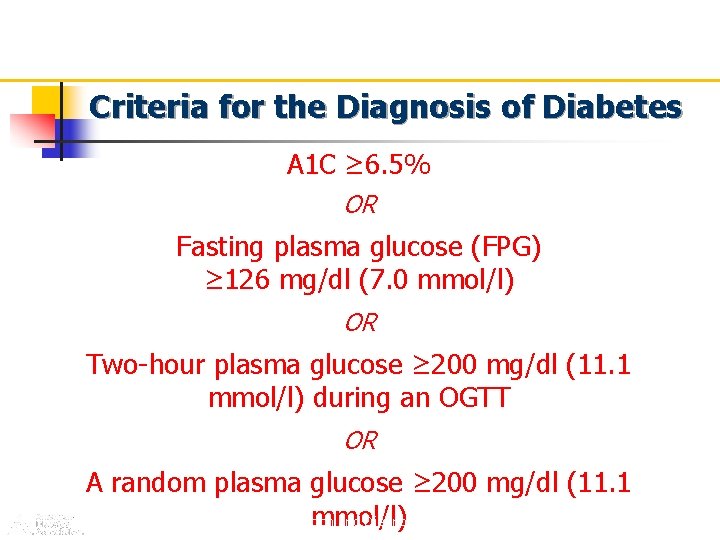
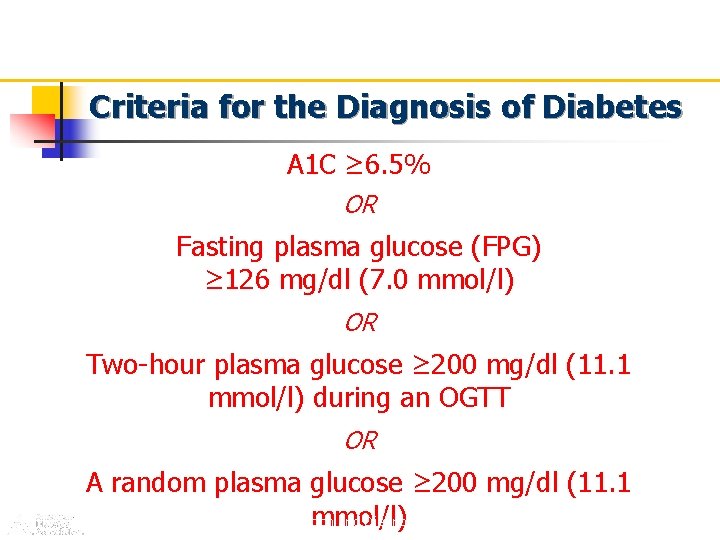
Criteria for the Diagnosis of Diabetes A 1 C ≥ 6. 5% OR Fasting plasma glucose (FPG) ≥ 126 mg/dl (7. 0 mmol/l) OR Two-hour plasma glucose ≥ 200 mg/dl (11. 1 mmol/l) during an OGTT OR A random plasma glucose ≥ 200 mg/dl (11. 1 ADA. I. Classification and Diagnosis. Diabetes Care 2011; 34(suppl 1): S 13. Table 2. mmol/l)





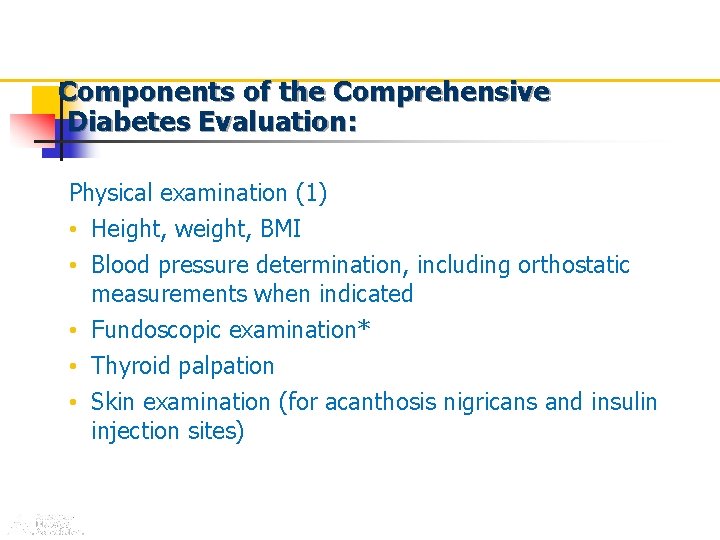
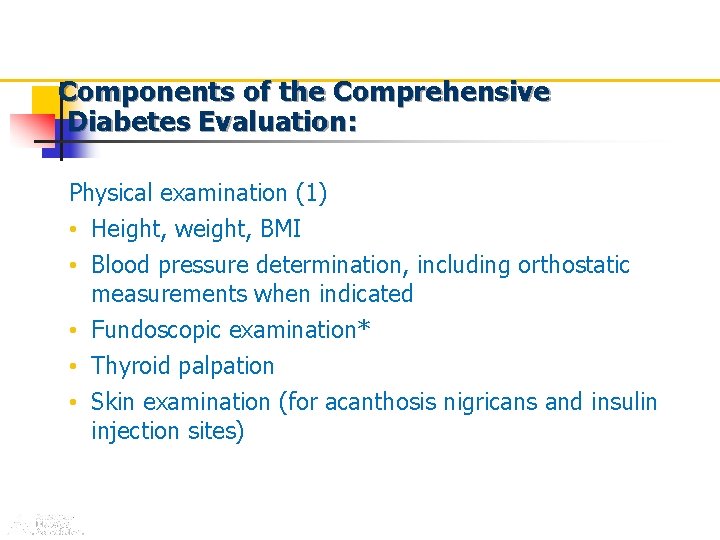
Components of the Comprehensive Diabetes Evaluation: Physical examination (1) • Height, weight, BMI • Blood pressure determination, including orthostatic measurements when indicated • Fundoscopic examination* • Thyroid palpation • Skin examination (for acanthosis nigricans and insulin injection sites) *See appropriate referrals for these categories. ADA. V. Diabetes Care 2011; 34(suppl 1): S 17. Table 8.
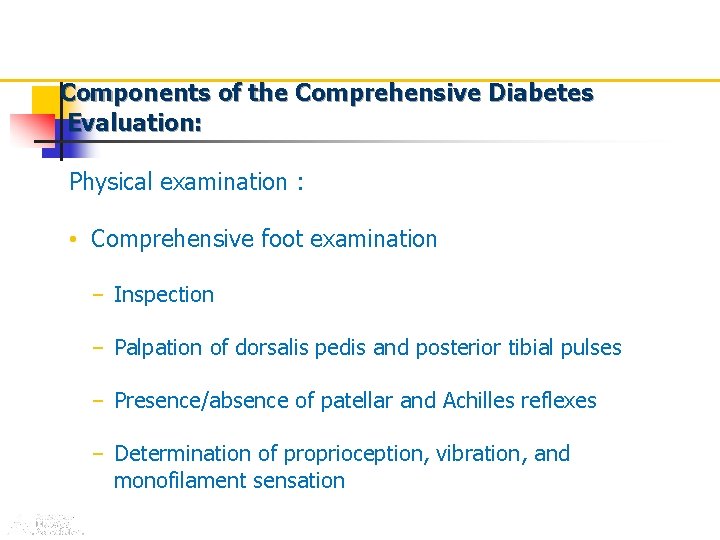
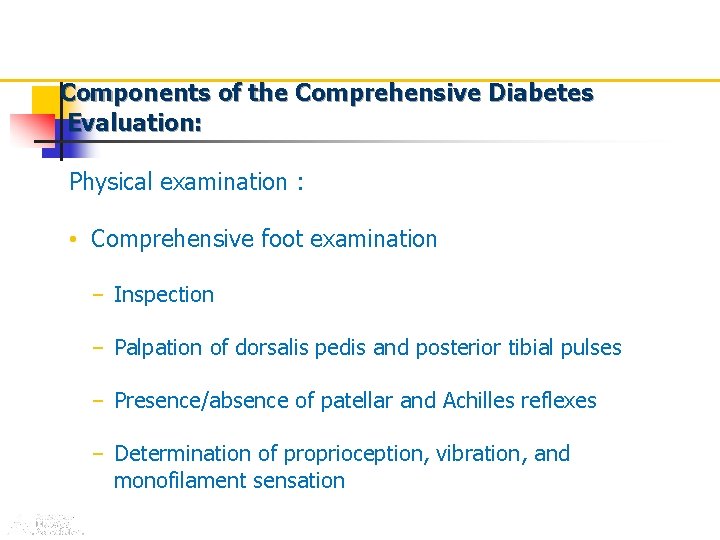
Components of the Comprehensive Diabetes Evaluation: Physical examination : • Comprehensive foot examination – Inspection – Palpation of dorsalis pedis and posterior tibial pulses – Presence/absence of patellar and Achilles reflexes – Determination of proprioception, vibration, and monofilament sensation *See appropriate referrals for these categories. ADA. V. Diabetes Care 2011; 34(suppl 1): S 17. Table 8.
Initial Metabolic Evaluation Referrales
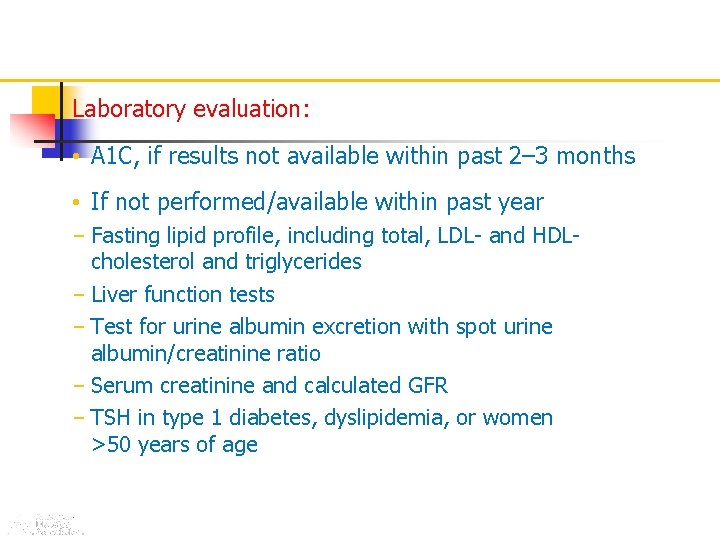
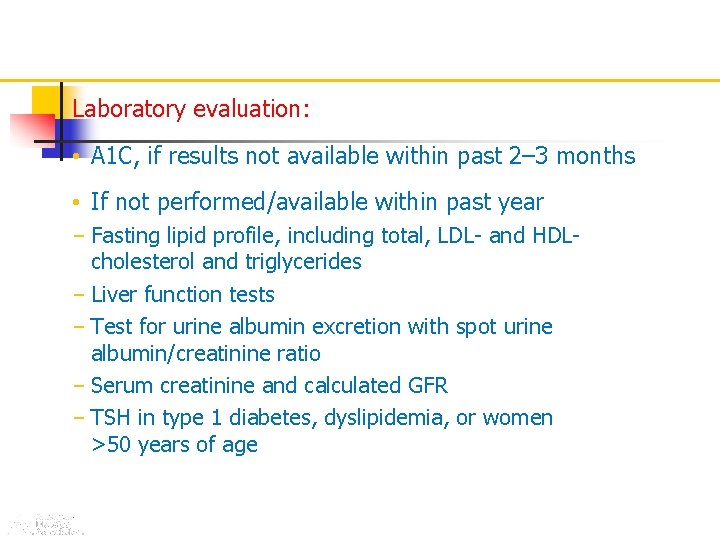
Laboratory evaluation: • A 1 C, if results not available within past 2– 3 months • If not performed/available within past year – Fasting lipid profile, including total, LDL- and HDLcholesterol and triglycerides – Liver function tests – Test for urine albumin excretion with spot urine albumin/creatinine ratio – Serum creatinine and calculated GFR – TSH in type 1 diabetes, dyslipidemia, or women >50 years of age ADA. V. Diabetes Care 2011; 34(suppl 1): S 17. Table 8.
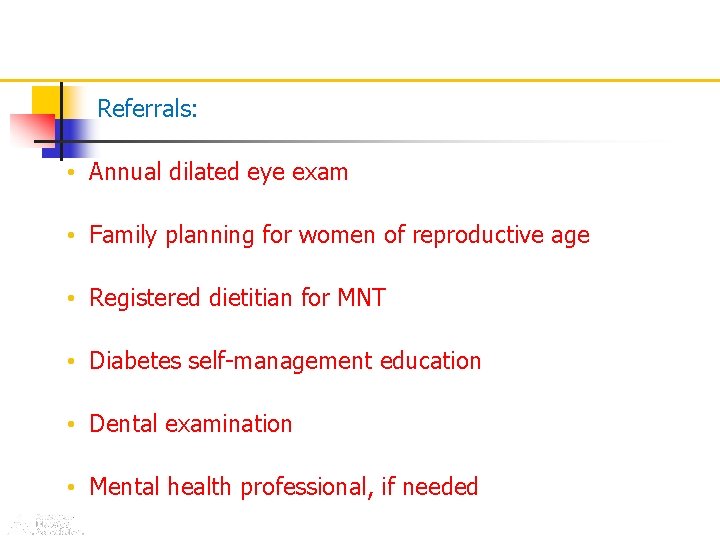
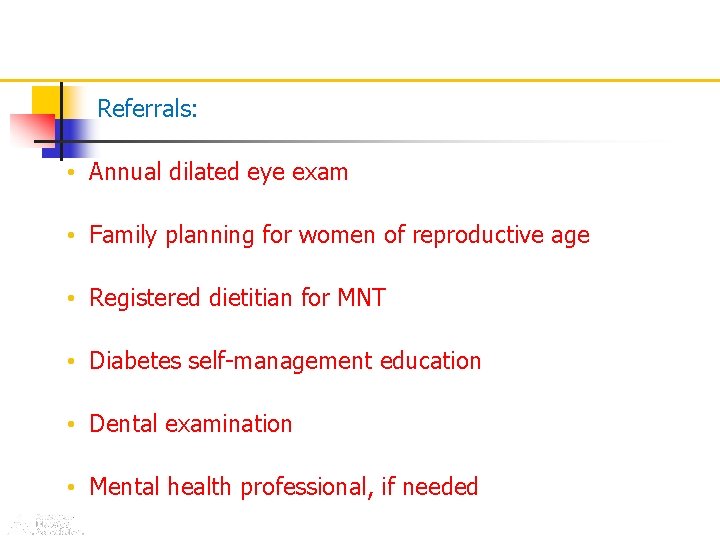
Referrals: • Annual dilated eye exam • Family planning for women of reproductive age • Registered dietitian for MNT • Diabetes self-management education • Dental examination • Mental health professional, if needed ADA. V. Diabetes Care 2011; 34(suppl 1): S 17. Table 8.
Target Hb. A 1 C A -B -C –D- E


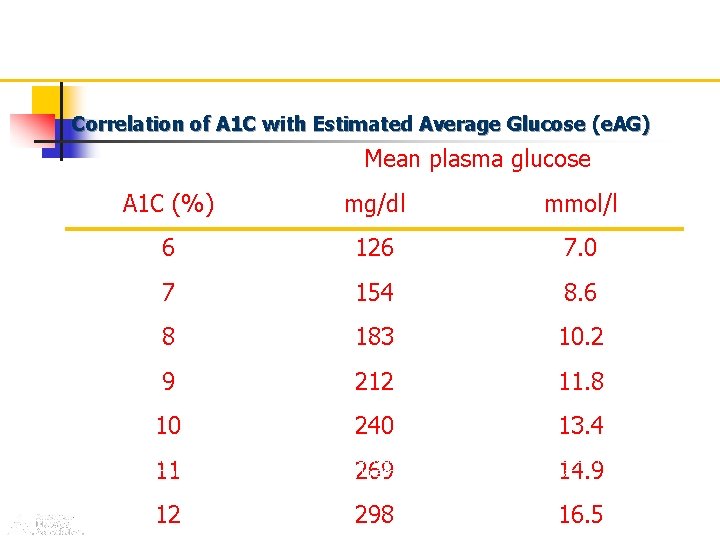
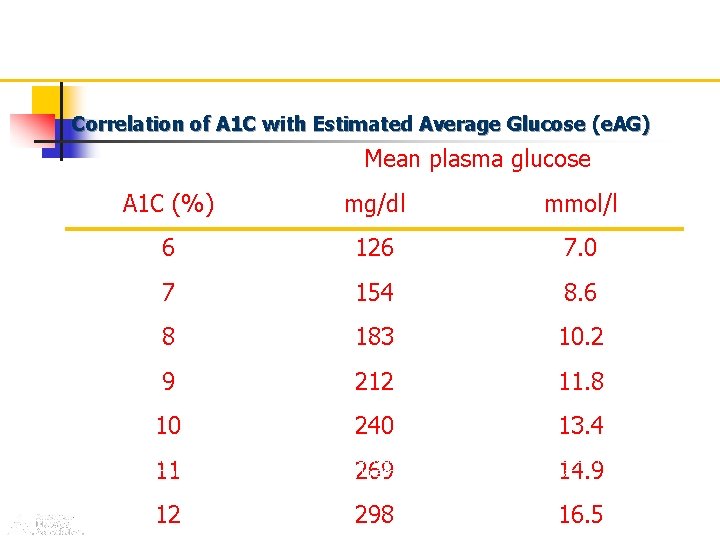
Correlation of A 1 C with Estimated Average Glucose (e. AG) Mean plasma glucose A 1 C (%) mg/dl mmol/l 6 126 7. 0 7 154 8. 6 8 183 10. 2 9 212 11. 8 10 240 13. 4 11 269 14. 9 12 298 16. 5 These estimates are based on ADAG data of ~2, 700 glucose measurements over 3 months per A 1 C measurement in 507 adults with type 1, type 2, and no diabetes. The correlation between A 1 C and average glucose was 0. 92. A calculator for converting A 1 C results into estimated average glucose (e. AG), in either mg/dl or mmol/l, is available at http: //professional. diabetes. org/Glucose. Calculator. aspx.


Considering: Age Body weight GFR
Outpatient Management: Bp control Lipid management Cigar discontinuous Glycemic control

















Early and aggressive insulin therapy: Reduces long-term vascular risk and potentially may prolong B-cell lifespan and Function.
initiating combination therapy or insulin immediately for all patients with A 1 C ; ≥ 9% at diagnosis. n
Recent clinical treatment guidelines, suggest that these agents may be less effective as add-on therapy for patients with an A 1 C ≥ 9. 5% and therefore recommend the initiation of insulin in all patients with an A 1 C > 10%.
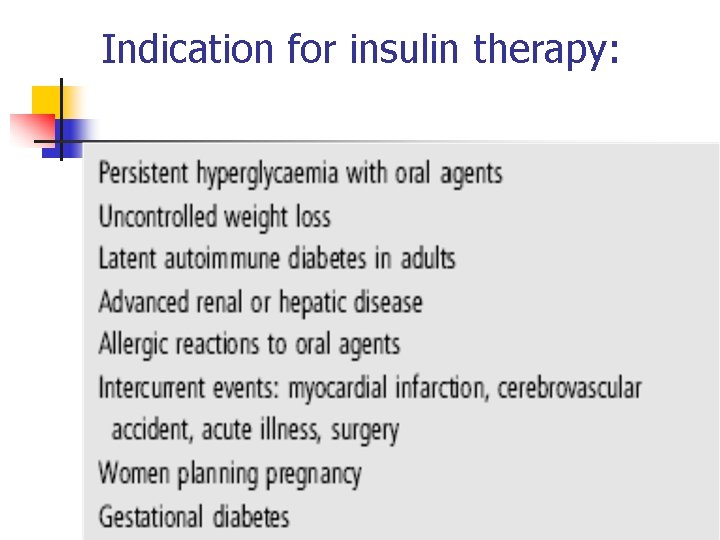
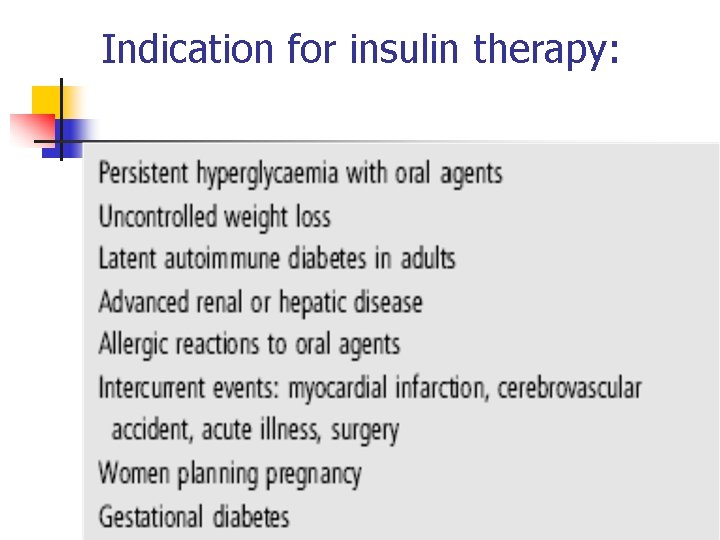
Indication for insulin therapy:
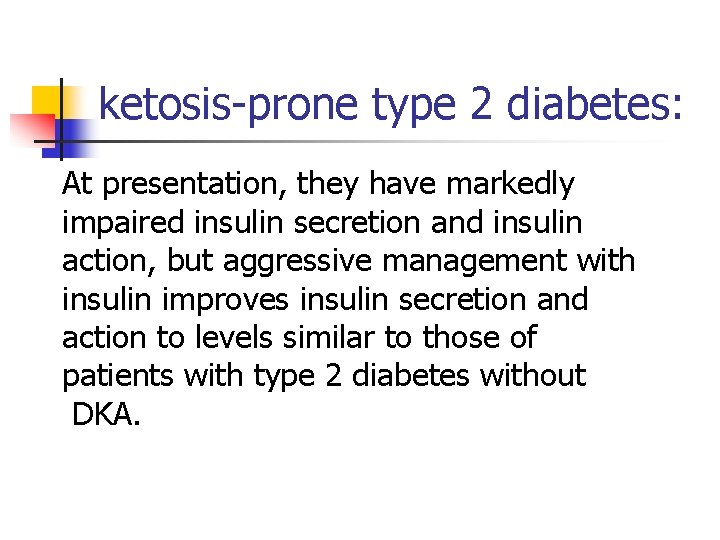
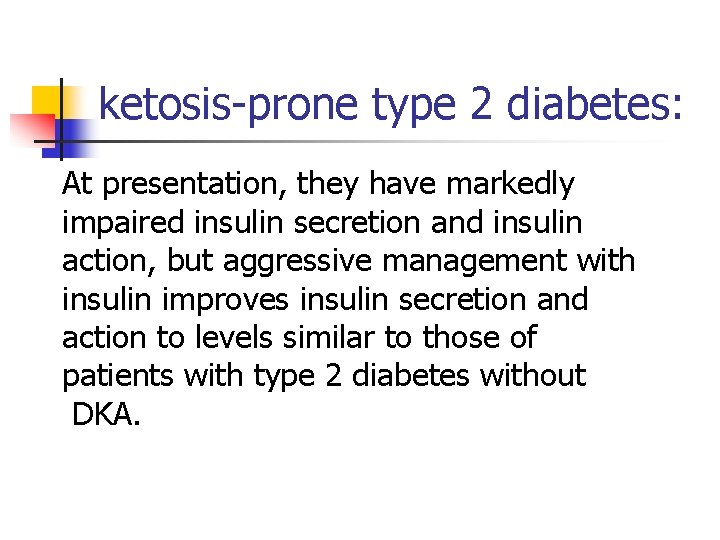
ketosis-prone type 2 diabetes: At presentation, they have markedly impaired insulin secretion and insulin action, but aggressive management with insulin improves insulin secretion and action to levels similar to those of patients with type 2 diabetes without DKA.
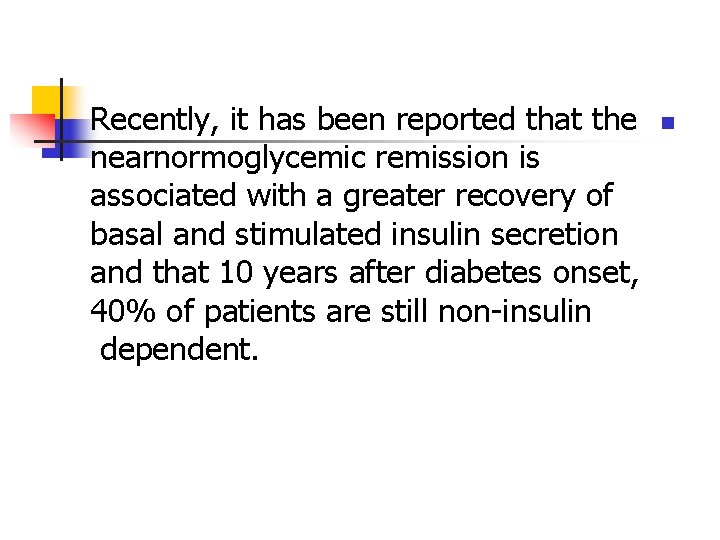
Recently, it has been reported that the nearnormoglycemic remission is associated with a greater recovery of basal and stimulated insulin secretion and that 10 years after diabetes onset, 40% of patients are still non-insulin dependent. n
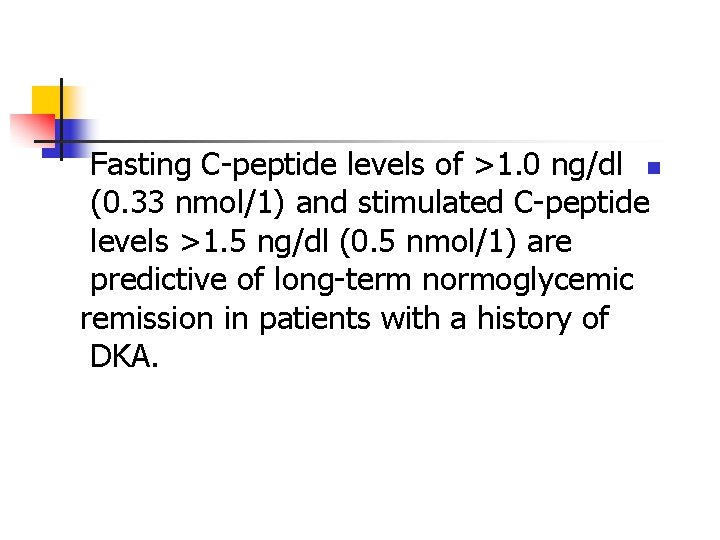
Fasting C-peptide levels of >1. 0 ng/dl n (0. 33 nmol/1) and stimulated C-peptide levels >1. 5 ng/dl (0. 5 nmol/1) are predictive of long-term normoglycemic remission in patients with a history of DKA.
Barriers to insulin initiation and intensification: The steps involved in insulin therapy: Initiation n Optimisation n Intensification n n
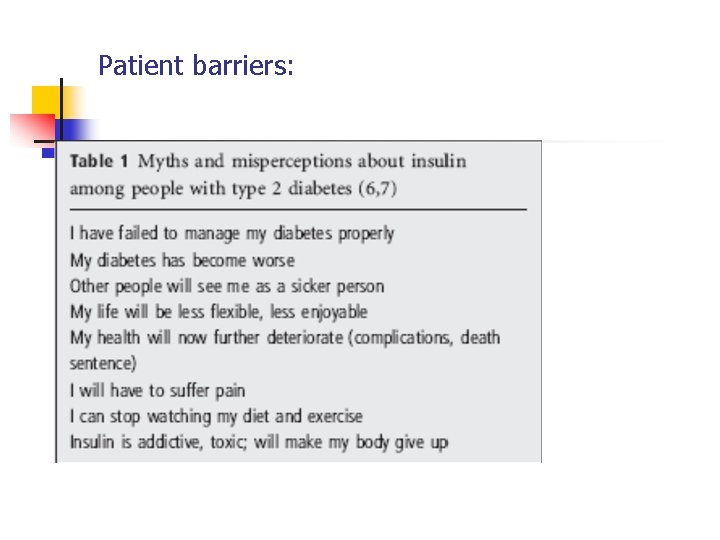
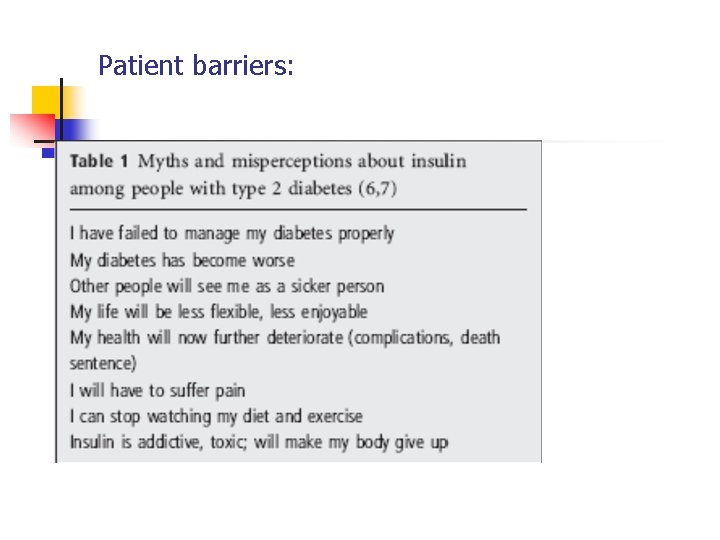
Patient barriers:
Physician barriers: Low motivation n Education barriers n

Insulin initiation strategies: In general, patients are initiated on n relatively less intensive insulin regimens to ease them into an appropriate routine. The insulin regimen can then be intensified as needed to meet glycemic. goals. n
Basal insulins: NPH n Glargin n Detemir n


Treat-to-Target trial: Glargine or NPH? n A 1 c reduction of: 1. 6% n Nocturnal hypoglycemia? Variablity in duration? n n

Long-acting analogs may also possess n added benefit when compared to NPH insulin in regard to rates of hypoglycemia and, in the case of insulin detemir, . decreased weight gain.


Titration:
Starting with a basal insulin analogue: The OADs, n including metformin and a secretagogue, are usually retained. n
For patients who experience dose waning toward the end of the dosing interval, twice-daily dosing may be considered or the administration time for single-dose regimens can be moved to earlier in the day during the period the patient will be using prandial coverage or periods of. greater physical activity


Premixed insulin: initiating a once-daily regimen in patients n for whom hyperglycemia is not severe and a twice-daily regimen in patients with an. Al. C > 8. 5%



Rapid-acting products: Ideally, these agents should be n administered with a lag time before eating that is proportional to the preprandial glucose level. The higher the glucose level, the greater amount of time before the meal the insulin should be administered to allow for onset of effect and a downward trend of premeal. hyperglycemia before eating.
Rapid-acting products: rapid-acting insulin should be n administered earlier (e. g. , 10 -15 minutes before the meal) for meals that contain primarily rapidly absorbed carbohydrates to ensure onset during carbohydrate absorption. Conversely, this insulin could be administered later (e. g. , at the first bite or 15 minutes after the meal) for meals with high fat content, which may. slow carbohydrate absorption.
Most patients start a once-daily n regimen before dinner, while maintaining sensitisers and discontinuing evening secretagogues, and should use 12 U initially. n n n
A recent study shows 41% of patients with type 2 diabetes attained an A 1 C less than 7% on a once-daily regimen of BIAsp 30 and OADs. n n
the addition of oncedaily biphasic insulin n aspart 70/30 before the evening meal in patients failing to meet glycemic goals on metformin resulted in A 1 C reductions of 1. 1 -1. 3%.
it is important to note that when A 1 C levels are 8. 5% or above, initiating insulin therapy with a twice-daily premixed insulin analogue is more effective at achieving glycaemic control than basal insulin.



Lingvay et al, recently demonstrated a n 100% success rate in achieving a goal Al. C of < 7. 0% in patients with newly diagnosed type 2 diabetes by initiating twice-daily biphasic insulin aspart 70/30. insulin in combination with metformin.
Patients usually remain on sensitisers whereas secretagogues are generally discontinued if using two or more injections. n n







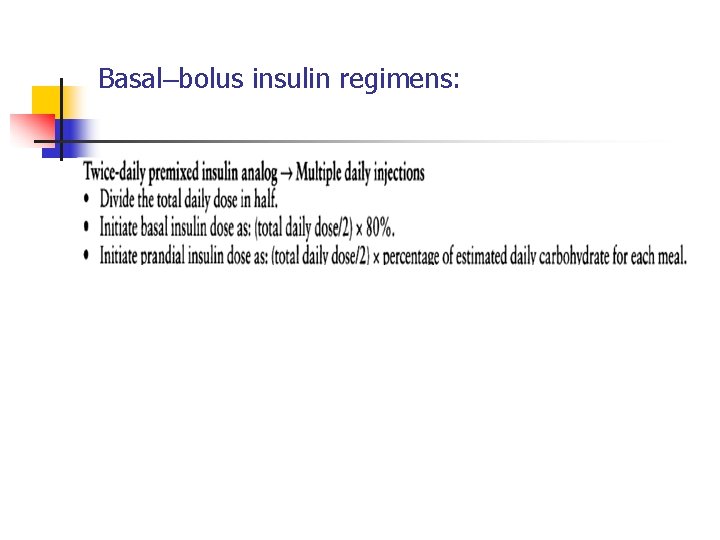
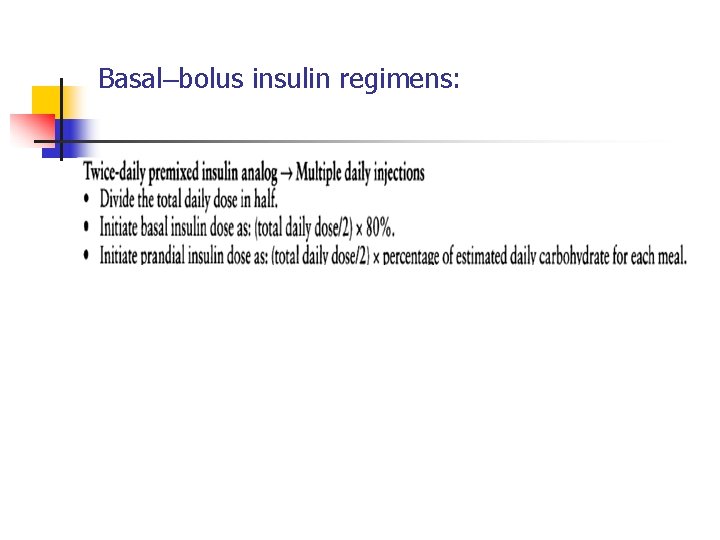
Basal–bolus insulin regimens:
Use of insulin glargine and cancer incidence in Scotland: a study from the Scottish Diabetes Research Network Epidemiology Group-Diabetologia(2009) Overall, insulin glargine use n was not associated with an increased risk of all cancers over a 4 year time frame. In the subgroup of insulin glargine only users to more likely reflect allocation bias rather n than an effect of insulin glargine itself. n n

 Miracles wichita ks
Miracles wichita ks Inpatient in nh
Inpatient in nh Thcic inpatient data
Thcic inpatient data Poa indicators are assigned in the inpatient setting for
Poa indicators are assigned in the inpatient setting for Inpatient pharmacy workflow
Inpatient pharmacy workflow Glycemic control algorithm
Glycemic control algorithm Outpatient clinical documentation improvement
Outpatient clinical documentation improvement Bulk ward stock
Bulk ward stock Outpatient medical center leesville la
Outpatient medical center leesville la Outpatient cdi
Outpatient cdi Outpatient parenteral antimicrobial therapy (opat)
Outpatient parenteral antimicrobial therapy (opat) Torrance memorial human resources
Torrance memorial human resources Monterey county behavioral health salinas
Monterey county behavioral health salinas Northshore outpatient pharmacy
Northshore outpatient pharmacy Stephanie dougherty singer
Stephanie dougherty singer Oatmeal glycemic index
Oatmeal glycemic index Glycemic index of tofu
Glycemic index of tofu What is the glycemic index of cocoyam
What is the glycemic index of cocoyam Mappillai samba rice glycemic index
Mappillai samba rice glycemic index Kefir glycemic index
Kefir glycemic index Lactose glycemic index
Lactose glycemic index Oreo glycemic index
Oreo glycemic index Can dogs eat gushers
Can dogs eat gushers Low gi indian foods
Low gi indian foods Translational research institute on pain in later life
Translational research institute on pain in later life Product and process control
Product and process control Control volume vs control surface
Control volume vs control surface Stock control e flow control
Stock control e flow control Control volume vs control surface
Control volume vs control surface Difference between positive and negative control
Difference between positive and negative control What is negative control
What is negative control Jelaskan tentang error control pada data link control?
Jelaskan tentang error control pada data link control? Control de errores
Control de errores Negative control vs positive control examples
Negative control vs positive control examples Control flow errors
Control flow errors Scalar control vs vector control
Scalar control vs vector control Komponen ltspice
Komponen ltspice What is xfinity home automation
What is xfinity home automation Spider control teton county
Spider control teton county Sphere of control and influence
Sphere of control and influence Mouse control whitehouse
Mouse control whitehouse Evaluate the effectiveness of social control inside prisons
Evaluate the effectiveness of social control inside prisons Glasser 5 basic needs
Glasser 5 basic needs Sensotronic brake control
Sensotronic brake control Top down control
Top down control Welding incomplete penetration
Welding incomplete penetration Traffic control austin
Traffic control austin System control
System control Hardware and control structures
Hardware and control structures Military power and control wheel
Military power and control wheel Version control systems industry
Version control systems industry Independent variable temperature
Independent variable temperature Intervenierende variable
Intervenierende variable Shoulder taper length
Shoulder taper length Poison control utah
Poison control utah Bank control account
Bank control account Mémoire inspe
Mémoire inspe Lead free control plan
Lead free control plan Planeación organización dirección y control de bimbo
Planeación organización dirección y control de bimbo Wilkes microprogrammed control unit
Wilkes microprogrammed control unit Srmvcas
Srmvcas Radar control service
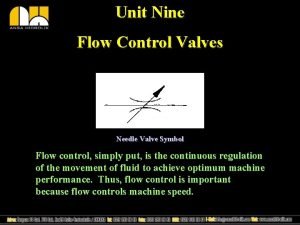
Radar control service Flow control valve symbol
Flow control valve symbol Feed-forward control physiology
Feed-forward control physiology Wheel network
Wheel network How to control for confounding variables in regression
How to control for confounding variables in regression Thermodynamic vs kinetic control
Thermodynamic vs kinetic control Inflation
Inflation Unit 13 biological cultural and chemical control of pests
Unit 13 biological cultural and chemical control of pests Unified access control
Unified access control Ad as unemployment
Ad as unemployment Underwater optical control
Underwater optical control Skinny protocol
Skinny protocol Preference for specific design control for procedural bias
Preference for specific design control for procedural bias Trimble compaction control
Trimble compaction control Flow control udp
Flow control udp Control de concurrencia
Control de concurrencia Tower enroute control routes
Tower enroute control routes Tqm tqc
Tqm tqc Manual gsk 980 tdc en español
Manual gsk 980 tdc en español Social cognitive personality
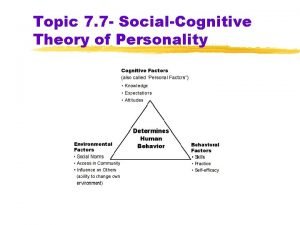
Social cognitive personality Oem grid control
Oem grid control Aviation tool control
Aviation tool control Acceptance sampling procedure
Acceptance sampling procedure Timing and control in computer architecture
Timing and control in computer architecture Steady state error in control system
Steady state error in control system Premise control
Premise control Damodaran control premium
Damodaran control premium Formal agents of social control
Formal agents of social control Negative vs positive control
Negative vs positive control