Jean Jurek Stacey Mosay Daphne Neris Lecture Notes
- Slides: 32
Jean Jurek Stacey Mosay Daphne Neris Lecture Notes to Accompany ICD-10 -CM Guidelines Chapter 4 Part 2
Outline Selection of the Principal Diagnosis and Additional Diagnoses for the Inpatient Setting Present on Admission (POA) Guidelines Copyright © F. A. Davis 2018 2
Learning Outcomes After studying this chapter, you should be able to: 1. Discuss the importance of the UHDDS and its relationship to diagnostic coding. 2. Describe the patient care flow and associated documentation in the inpatient setting. 3. Define the term principal diagnosis as it relates to the inpatient setting. 4. Describe the specific sequencing rule that is followed when multiple diagnoses are documented. 5. Apply diagnostic coding sequencing rules to these coding situations: (a) two or more principal diagnoses (b) treatment plan not carried out (c) complications (d) uncertain diagnoses 6. Describe the guidelines for selecting the principal diagnosis following admission from an observation unit or from an outpatient surgery. 7. Discuss the criteria for reporting additional diagnoses. 8. Define POA and describe how it is assigned. 9. Based on diagnostic statements, correctly assign diagnosis codes for the inpatient setting. Copyright © F. A. Davis 2018 3
Learning Outcomes (cont. ) After this presentation, you should be able to: 2 a. Describe the patient care flow and associated documentation in the inpatient setting. 2 b. Discuss the importance of the UHDDS and its relationship to diagnostic coding. 2 c. Define the term principal diagnosis as it relates to the inpatient setting. 2 d. Describe the specific sequencing rule that is followed when multiple diagnoses are documented. Copyright © F. A. Davis 2018 2 e. Apply diagnostic coding sequencing rules to these coding situations: (a) Two or more principal diagnoses (b) Treatment plan not carried out (c) Complications (d) Uncertain diagnoses 2 f. Describe the guidelines for selecting the principal diagnosis following admission from an observation unit and outpatient surgery. 2 g. Discuss the criteria for reporting additional diagnoses. 2 h. Define POA and describe how it is assigned. 2 i. Based on diagnostic statements, correctly assign diagnosis codes for the inpatient setting. 4
Selection of the Principal Diagnosis and Additional Diagnoses for the Inpatient Setting Copyright © F. A. Davis 2018 5
The Uniform Hospital Discharge Data Set (UHDDS)—Guidance Applied to inpatient and non-outpatient settings The goal is to obtain uniform comparable discharge data on all inpatients pertaining to: Patient identification Provider information Clinical information of the patient episode of care Financial information Copyright © F. A. Davis 2018 6
Documentation in the Inpatient Setting The content and flow of documentation assists the coder in selecting the principal and secondary diagnoses that should be reported in the inpatient setting. Copyright © F. A. Davis 2018 7
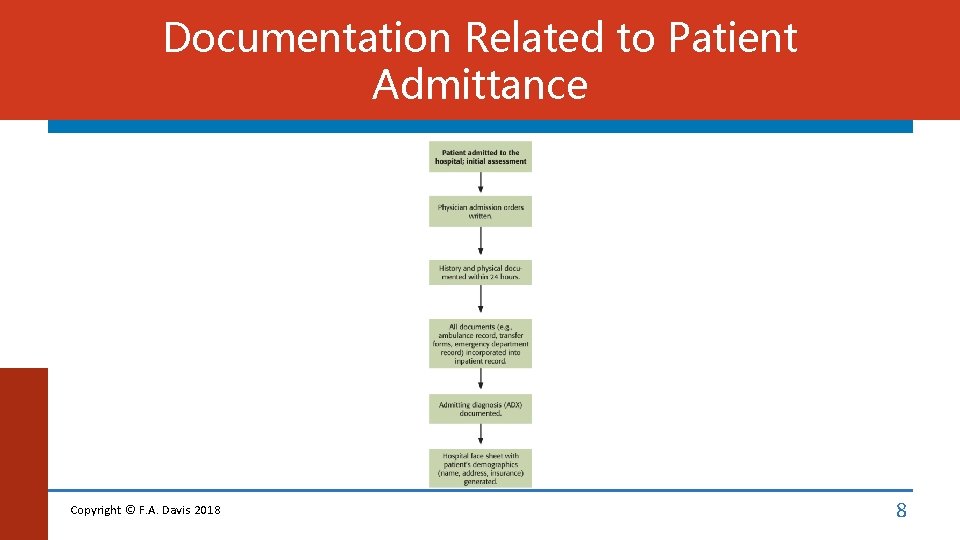
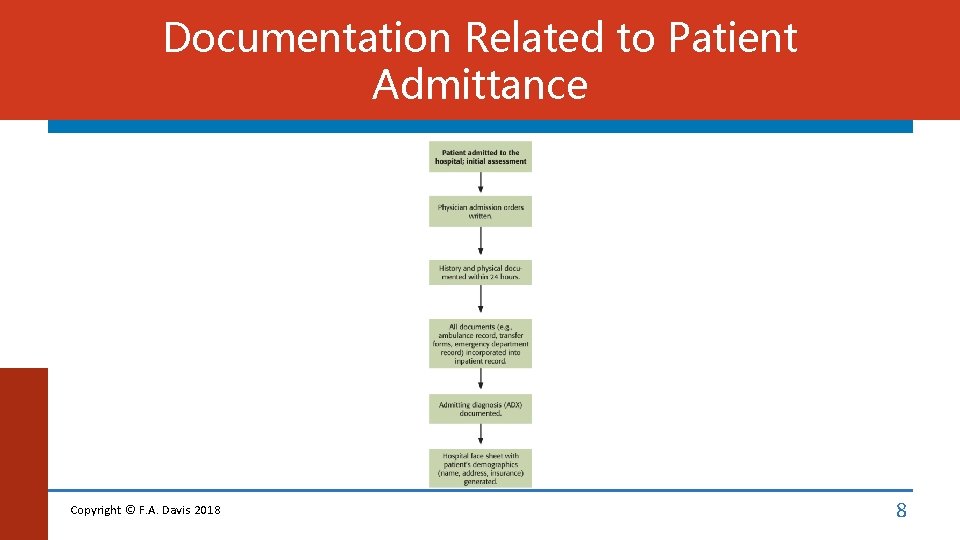
Documentation Related to Patient Admittance Copyright © F. A. Davis 2018 8
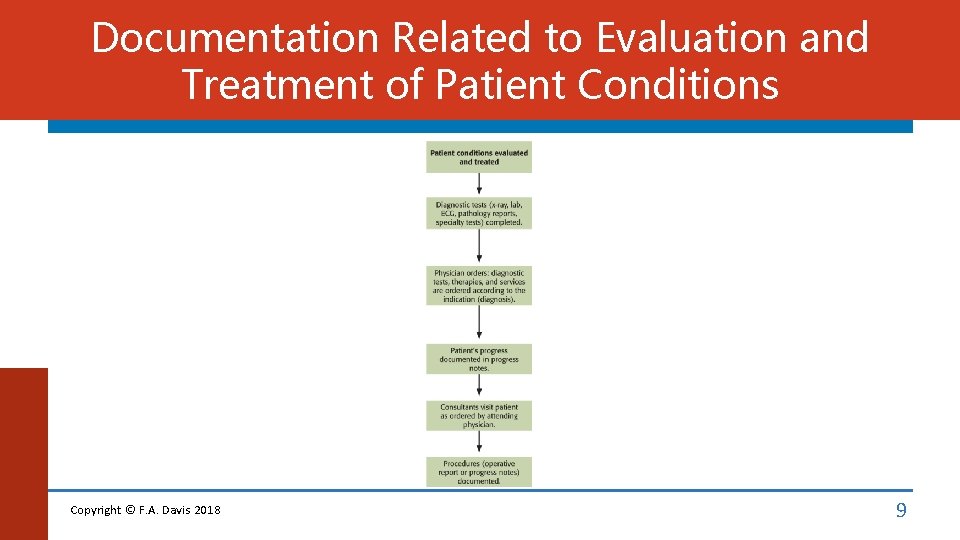
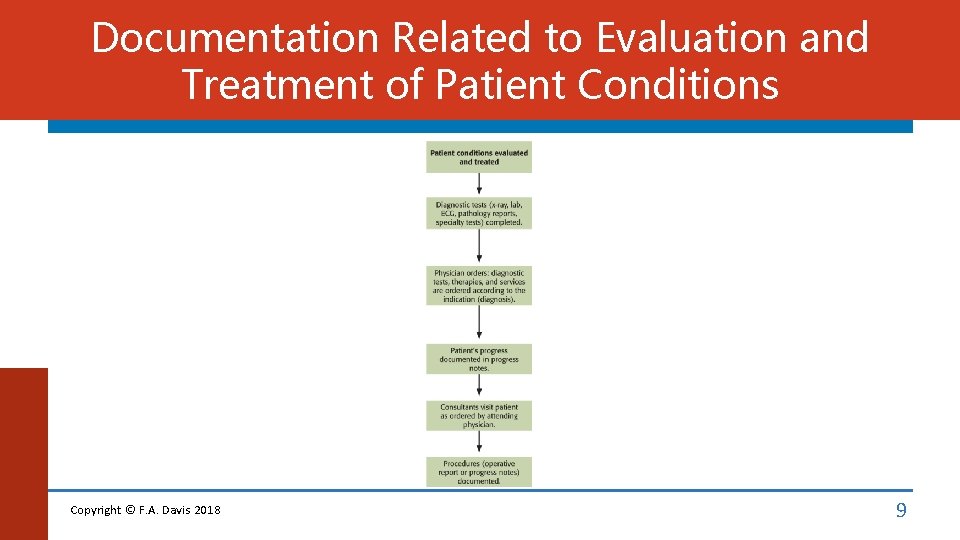
Documentation Related to Evaluation and Treatment of Patient Conditions Copyright © F. A. Davis 2018 9
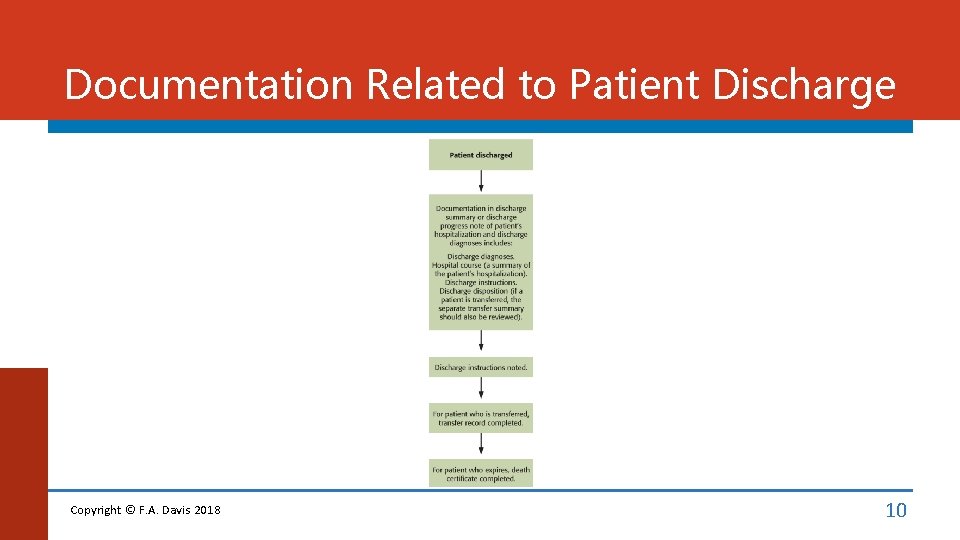
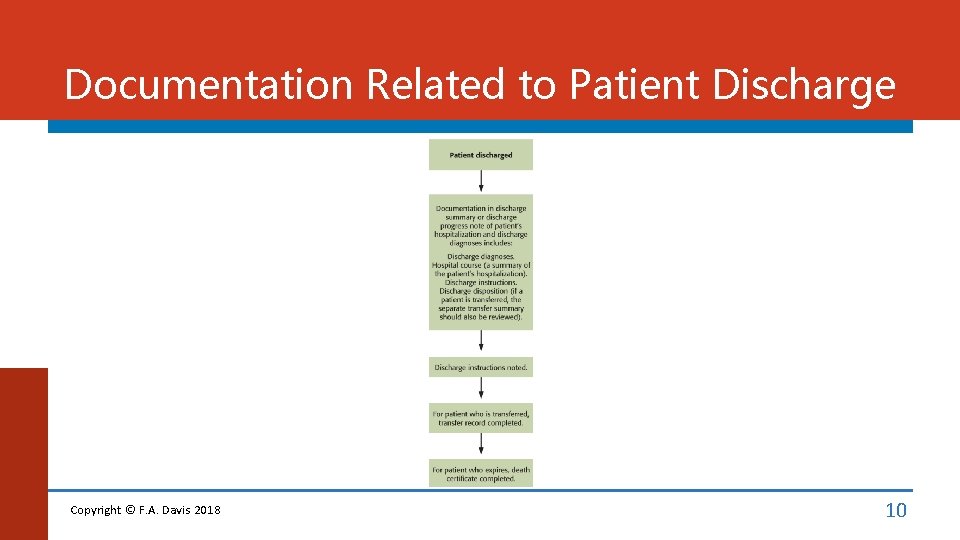
Documentation Related to Patient Discharge Copyright © F. A. Davis 2018 10
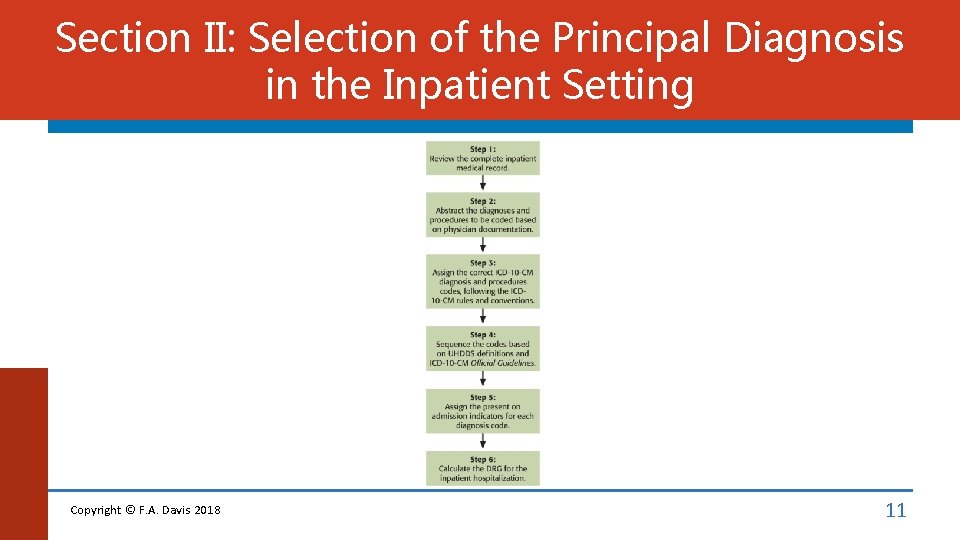
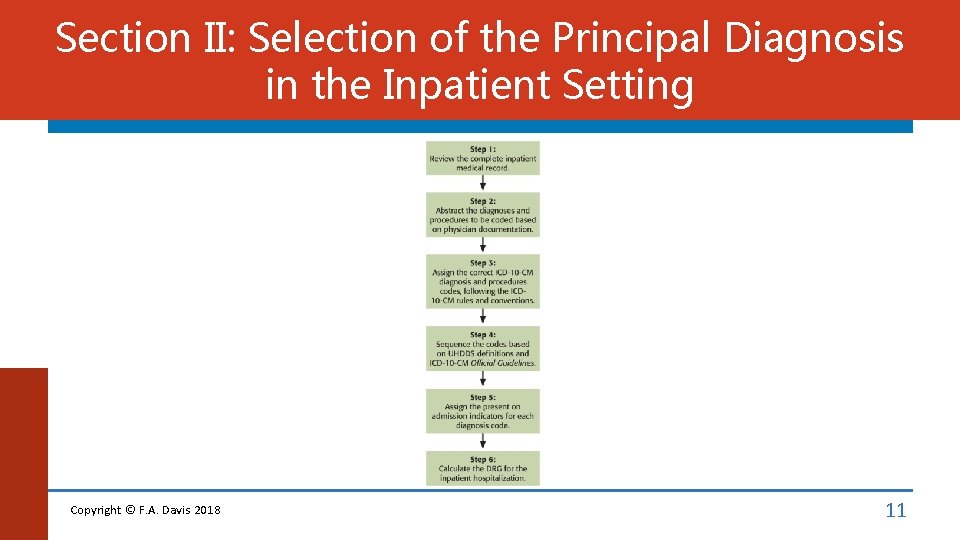
Section II: Selection of the Principal Diagnosis in the Inpatient Setting Copyright © F. A. Davis 2018 11
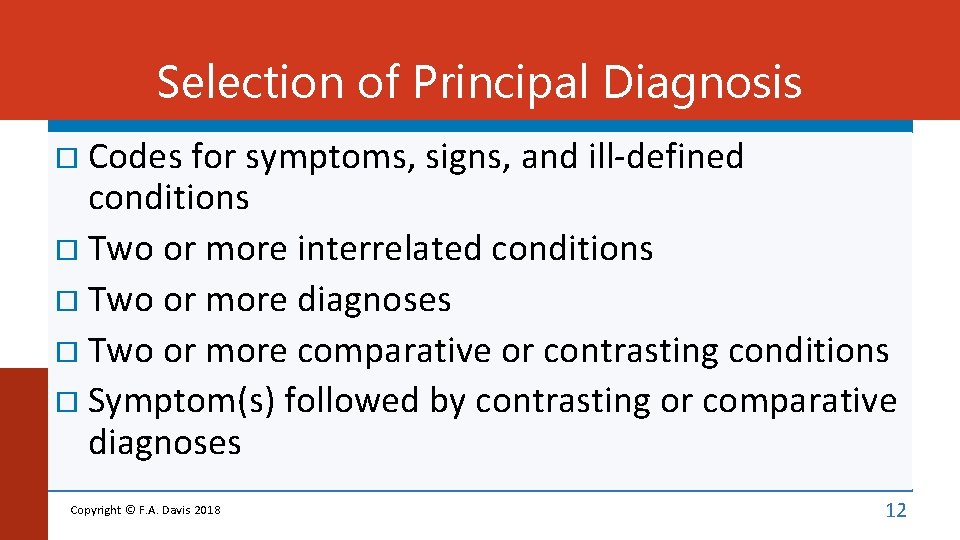
Selection of Principal Diagnosis Codes for symptoms, signs, and ill-defined conditions Two or more interrelated conditions Two or more diagnoses Two or more comparative or contrasting conditions Symptom(s) followed by contrasting or comparative diagnoses Copyright © F. A. Davis 2018 12
Selection of Principal Diagnosis (cont. ) Original treatment plan not carried out Complications Uncertain diagnosis Admission from observation unit Following medical observation Following postoperative observation Admission Copyright © F. A. Davis 2018 from outpatient surgery 13
Jin presents with painful urination and becomes dehydrated. After study, the attending physician determines that the pain is caused by acute tubulo-interstitial nephritis caused by E coli bacteria. What is the principal diagnosis? A. Acute tubulo-interstitial nephritis B. Dehydration C. E coli bacteria infection D. Painful urination
Section III: Reporting Additional Diagnoses The Official Guidelines also indicate which conditions should be reported as secondary diagnoses, meaning other diagnoses. Other diagnoses are defined by UHDDS as: A comorbidity that represents conditions that coexist at the time of admission, or a complication that is a condition that develops subsequently, or that affects the treatment received or the length of stay. Diagnoses that relate to an earlier episode that have no bearing on the current hospital stay are to be excluded. Copyright © F. A. Davis 2018 15
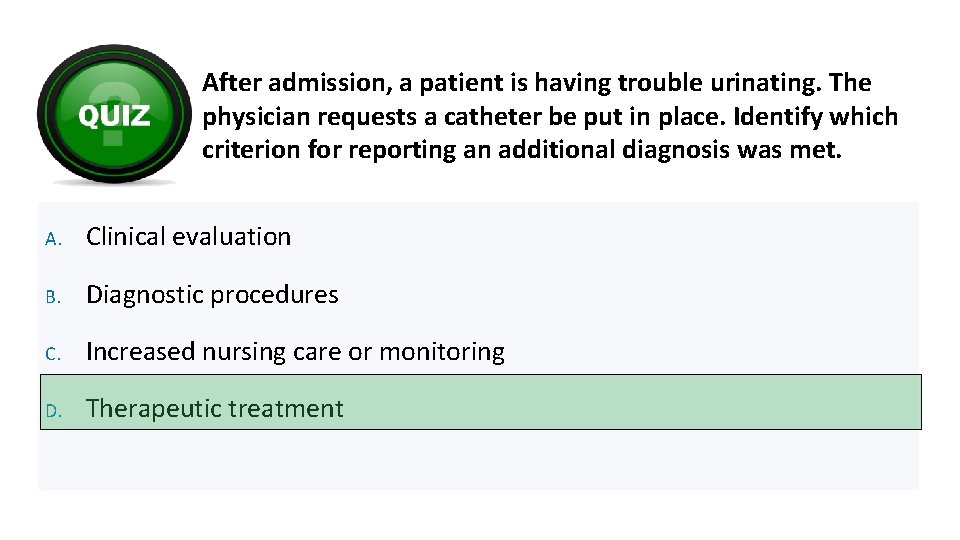
Reporting Additional Diagnoses General Rules If the patient requires at least one of the following conditions, an additional diagnosis of condition must be reported: Clinical evaluation Therapeutic treatment Diagnostic procedures Extended length of hospital stay Increased nursing care or monitoring Copyright © F. A. Davis 2018 16
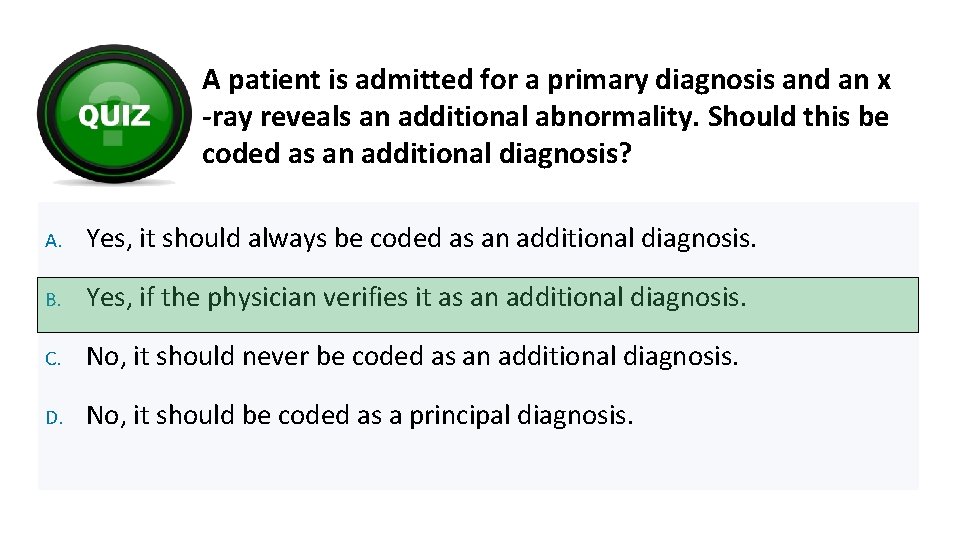
Reporting Additional Diagnoses Further Guidelines Previous conditions Abnormal findings Uncertain diagnosis Copyright © F. A. Davis 2018 17
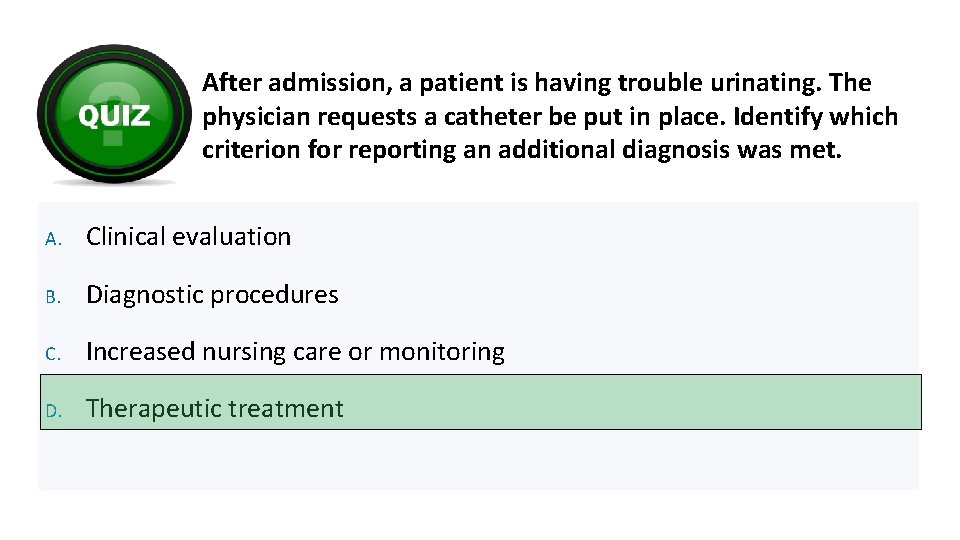
After admission, a patient is having trouble urinating. The physician requests a catheter be put in place. Identify which criterion for reporting an additional diagnosis was met. A. Clinical evaluation B. Diagnostic procedures C. Increased nursing care or monitoring D. Therapeutic treatment
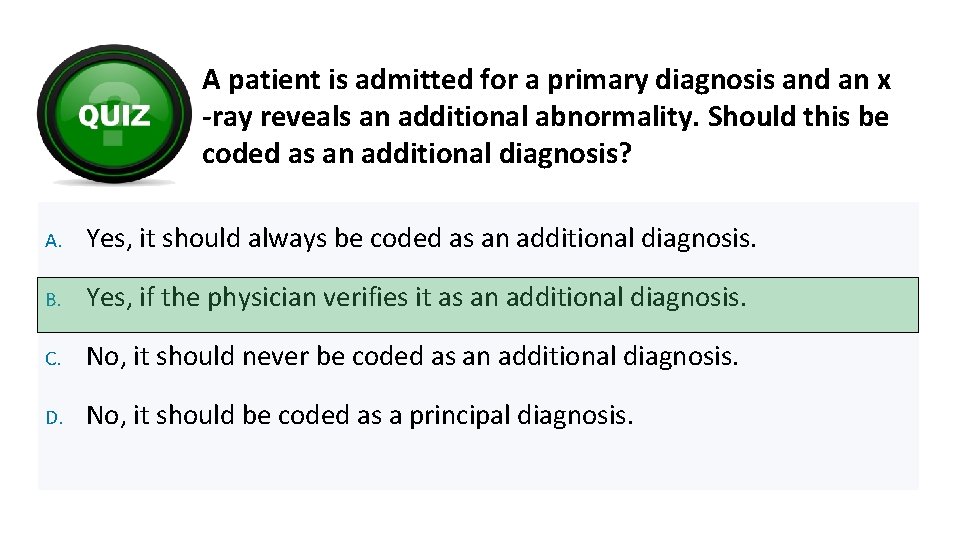
A patient is admitted for a primary diagnosis and an x -ray reveals an additional abnormality. Should this be coded as an additional diagnosis? A. Yes, it should always be coded as an additional diagnosis. B. Yes, if the physician verifies it as an additional diagnosis. C. No, it should never be coded as an additional diagnosis. D. No, it should be coded as a principal diagnosis.
Present on Admission (POA) Guidelines Copyright © F. A. Davis 2018 20
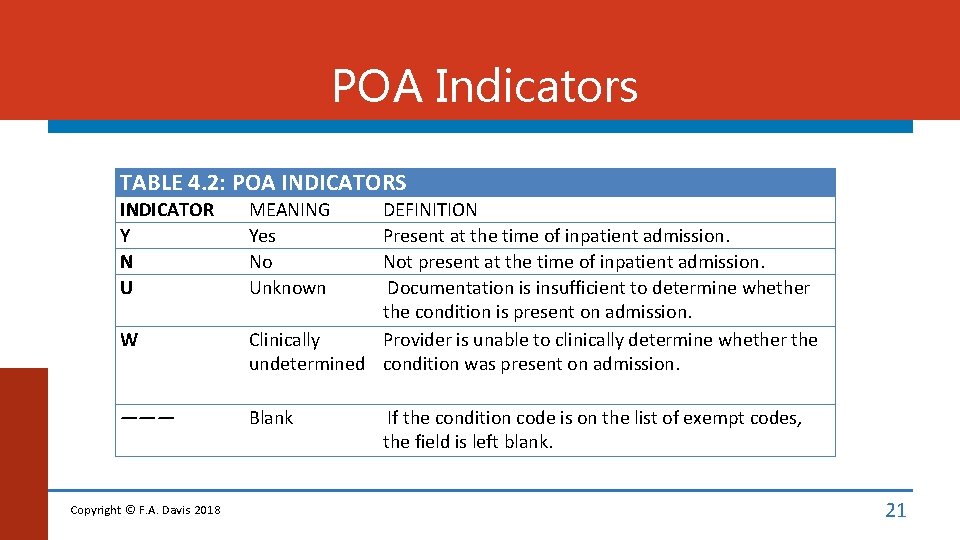
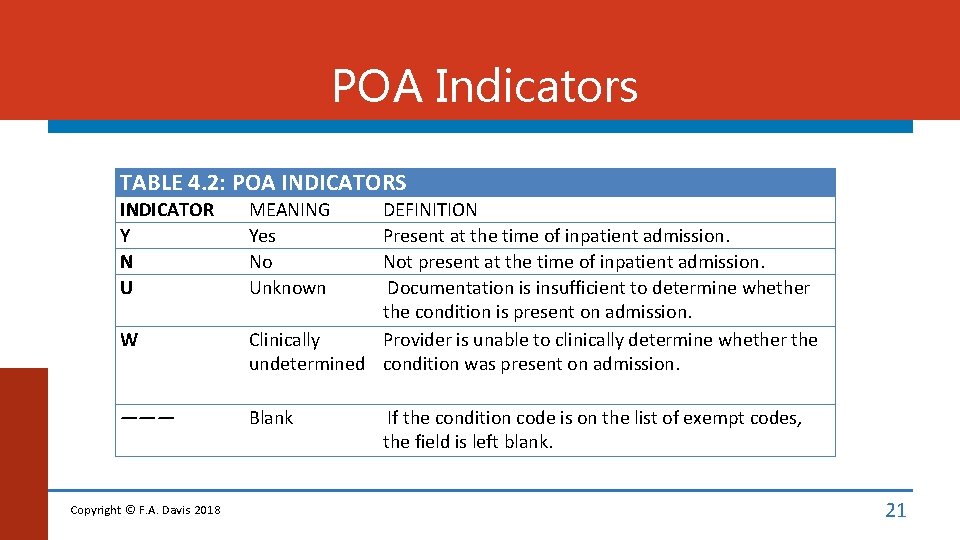
POA Indicators TABLE 4. 2: POA INDICATORS INDICATOR Y N U W ——— Copyright © F. A. Davis 2018 MEANING Yes No Unknown DEFINITION Present at the time of inpatient admission. Not present at the time of inpatient admission. Documentation is insufficient to determine whether the condition is present on admission. Clinically Provider is unable to clinically determine whether the undetermined condition was present on admission. Blank If the condition code is on the list of exempt codes, the field is left blank. 21
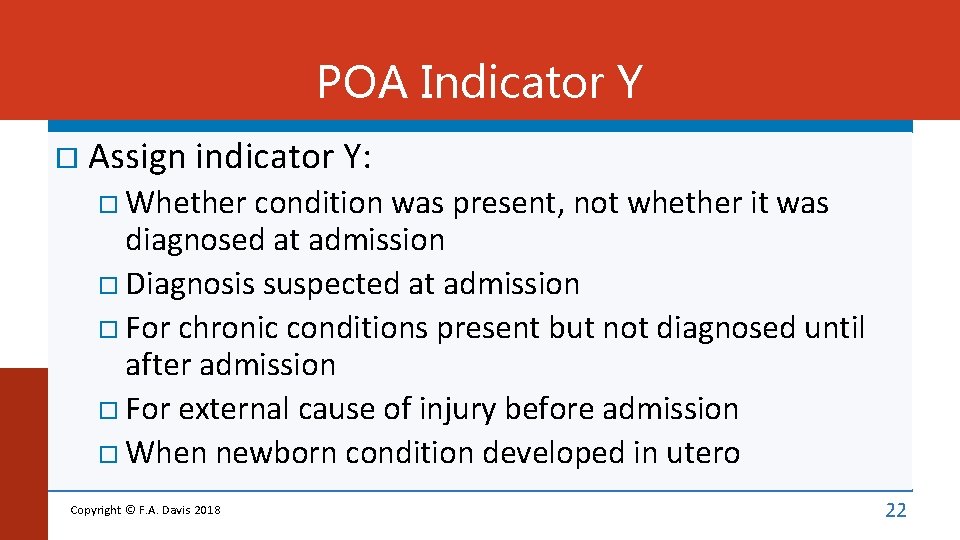
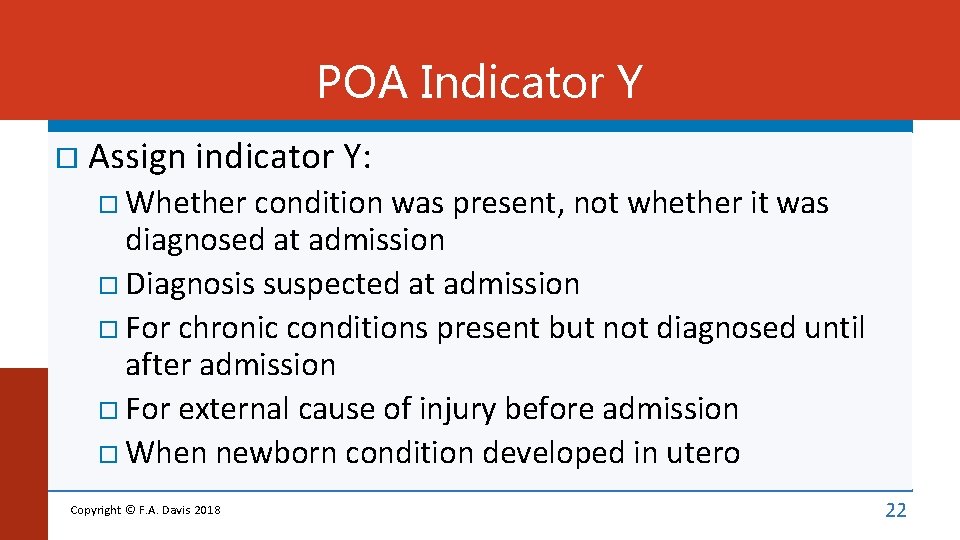
POA Indicator Y Assign indicator Y: Whether condition was present, not whether it was diagnosed at admission Diagnosis suspected at admission For chronic conditions present but not diagnosed until after admission For external cause of injury before admission When newborn condition developed in utero Copyright © F. A. Davis 2018 22
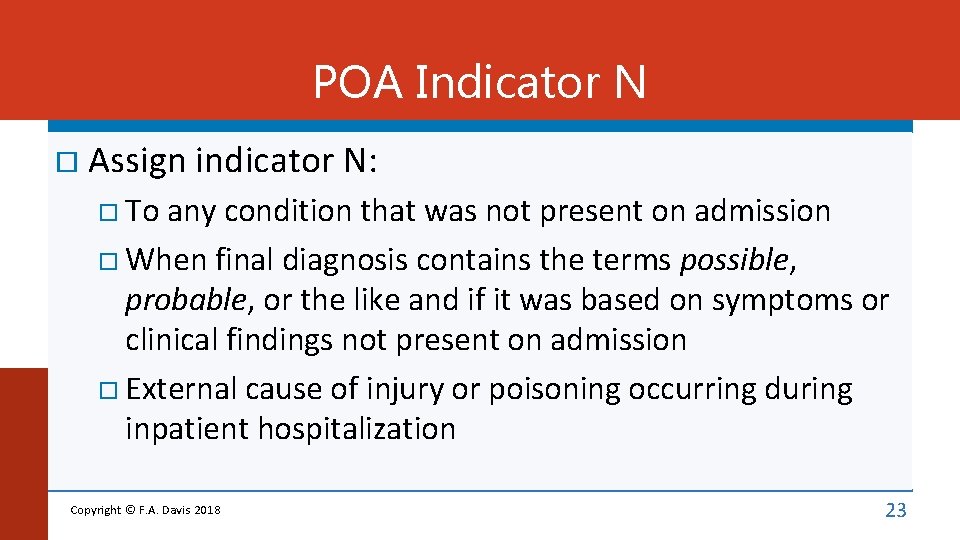
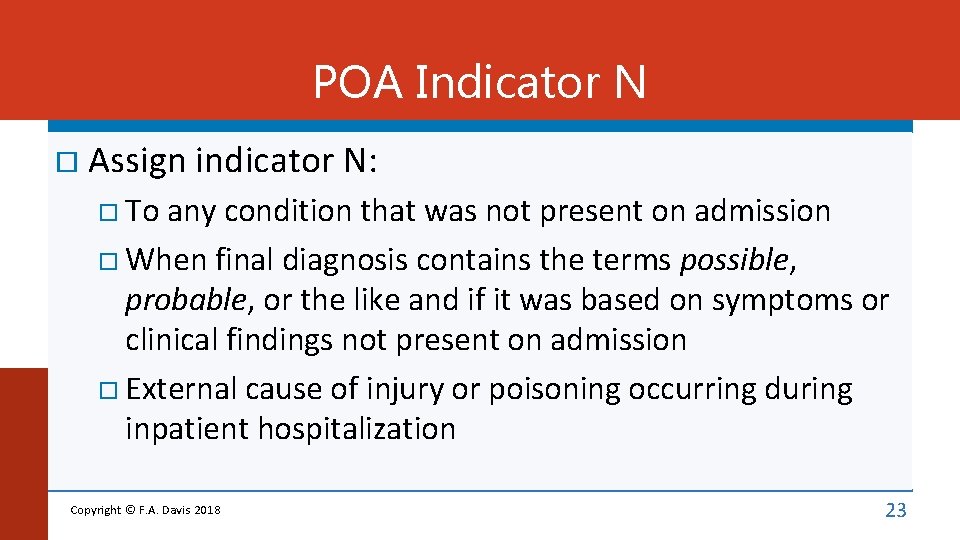
POA Indicator N Assign indicator N: To any condition that was not present on admission When final diagnosis contains the terms possible, probable, or the like and if it was based on symptoms or clinical findings not present on admission External cause of injury or poisoning occurring during inpatient hospitalization Copyright © F. A. Davis 2018 23
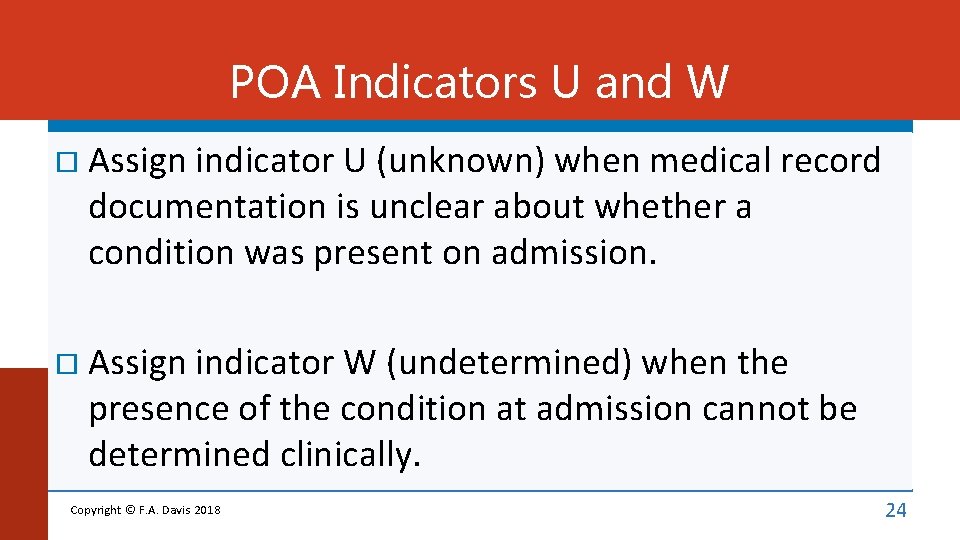
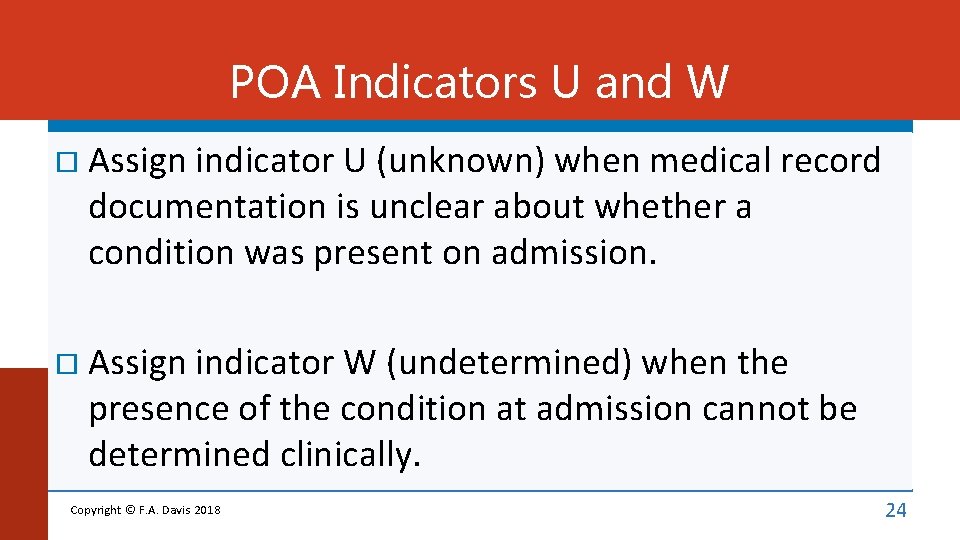
POA Indicators U and W Assign indicator U (unknown) when medical record documentation is unclear about whether a condition was present on admission. Assign indicator W (undetermined) when the presence of the condition at admission cannot be determined clinically. Copyright © F. A. Davis 2018 24
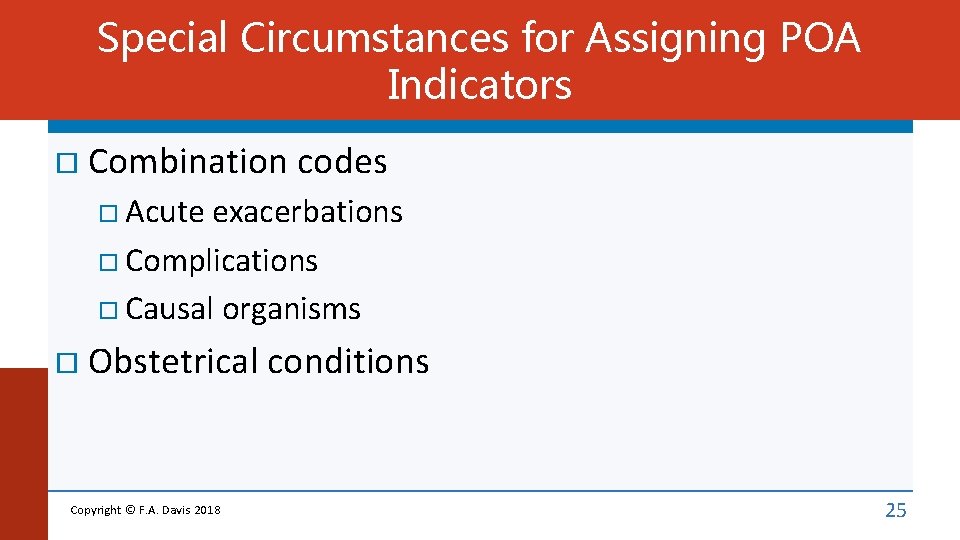
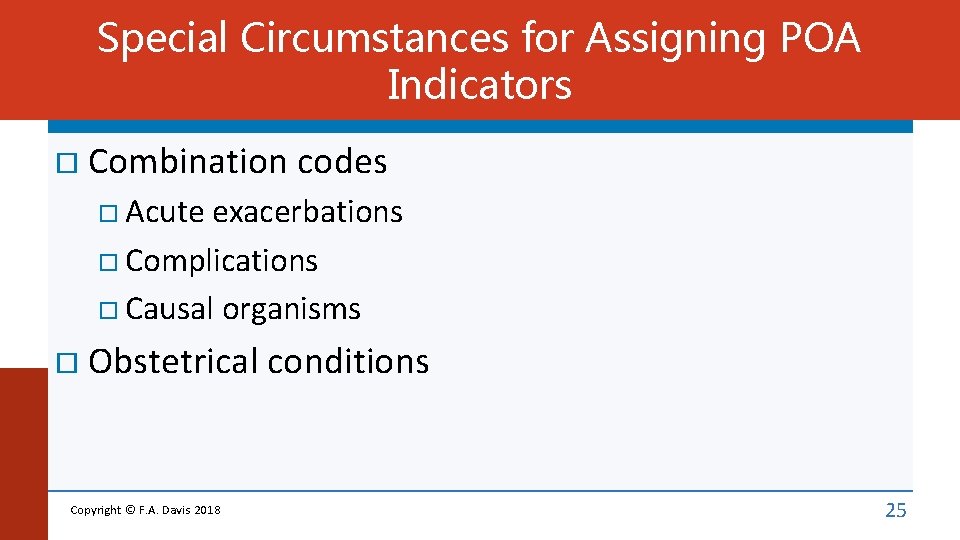
Special Circumstances for Assigning POA Indicators Combination codes Acute exacerbations Complications Causal organisms Obstetrical Copyright © F. A. Davis 2018 conditions 25
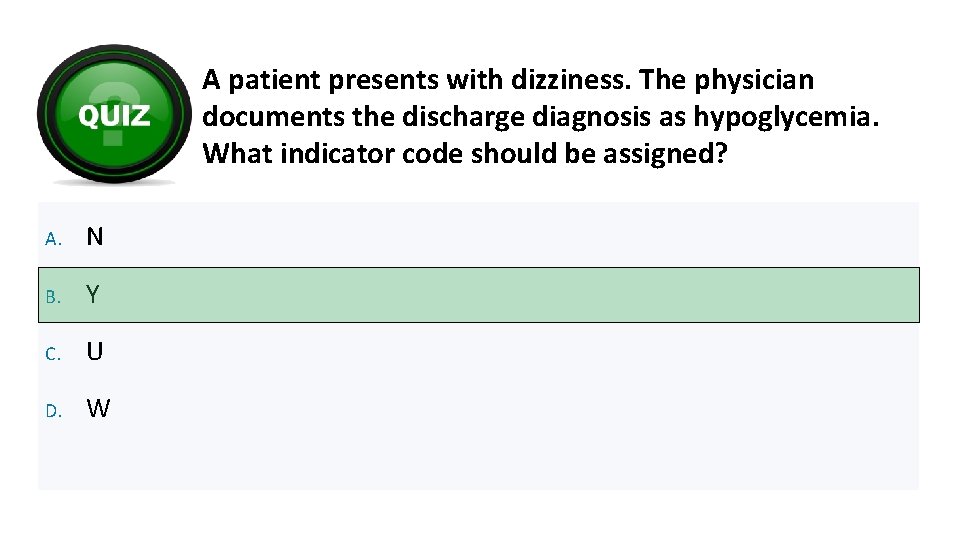
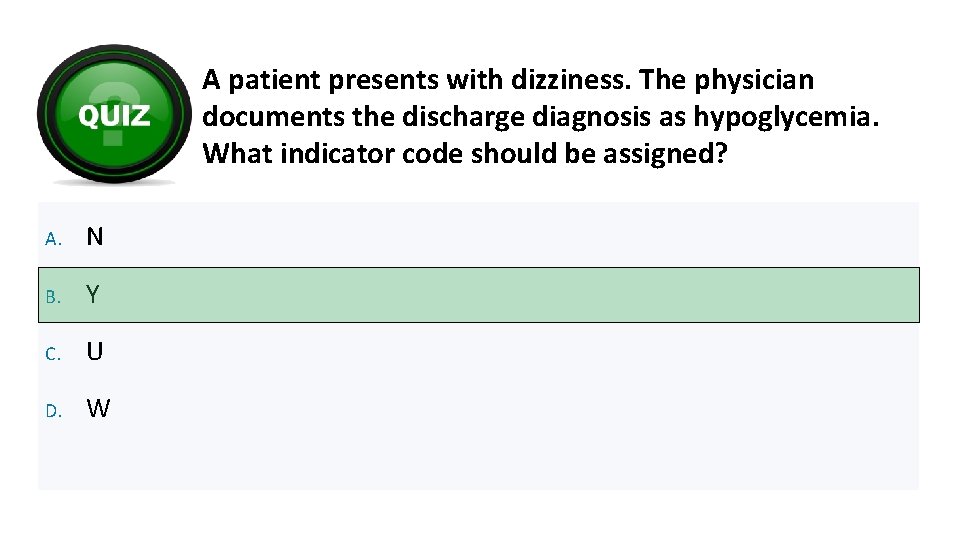
A patient presents with dizziness. The physician documents the discharge diagnosis as hypoglycemia. What indicator code should be assigned? A. N B. Y C. U D. W
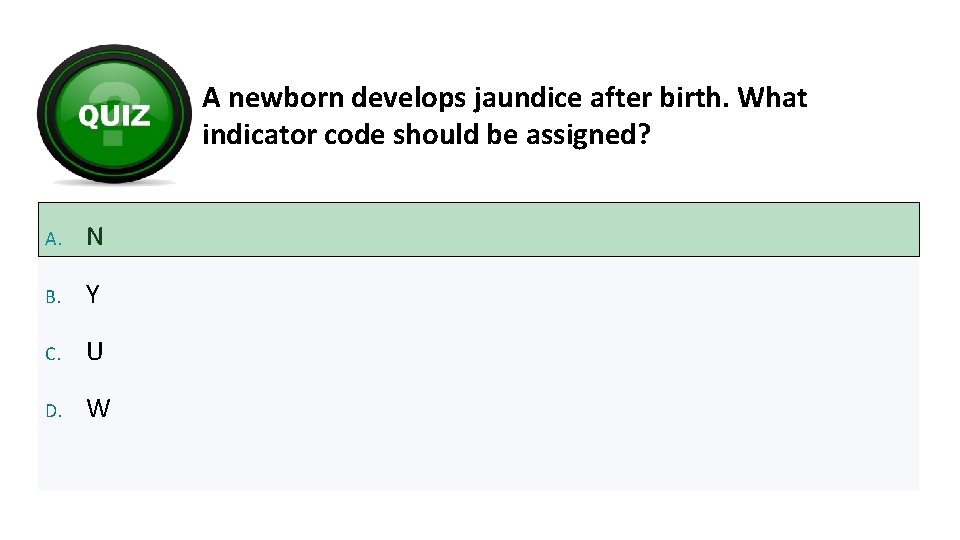
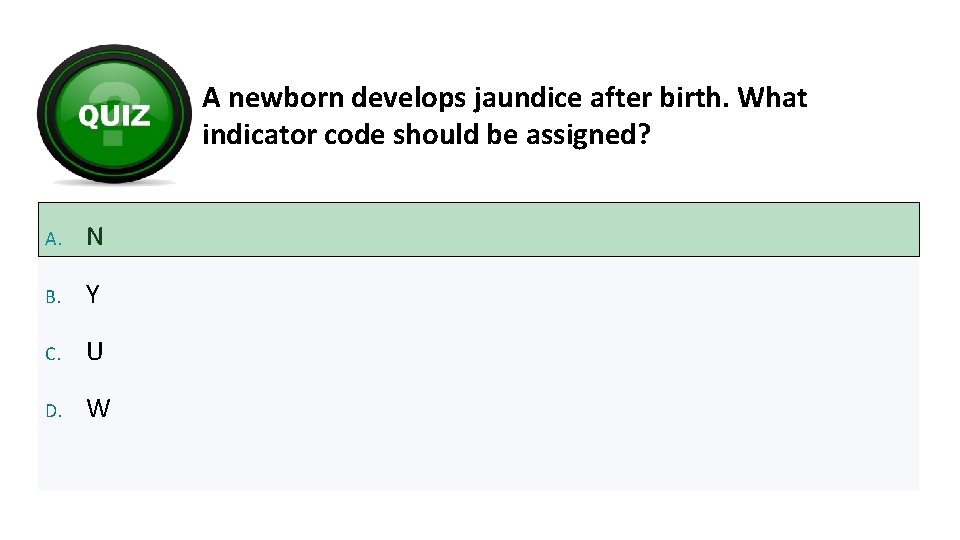
A newborn develops jaundice after birth. What indicator code should be assigned? A. N B. Y C. U D. W
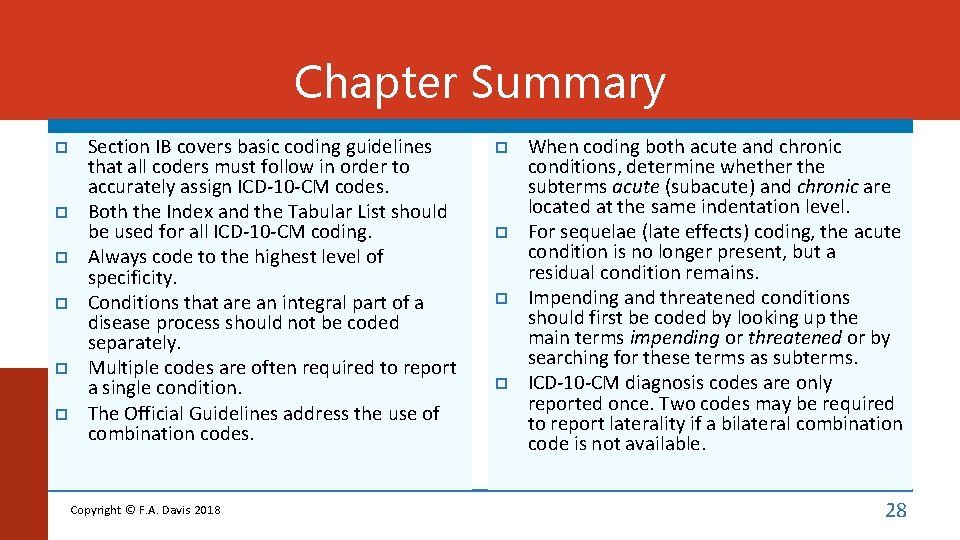
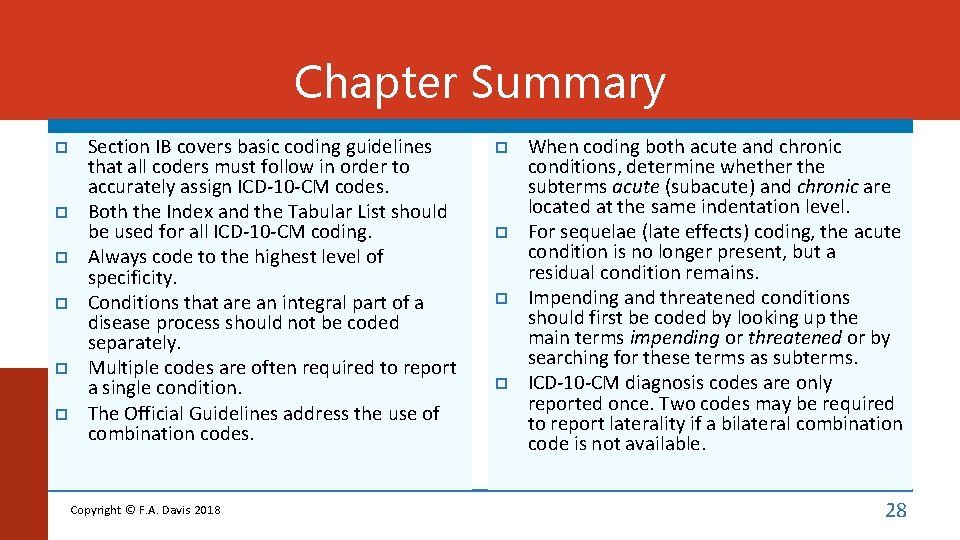
Chapter Summary Section IB covers basic coding guidelines that all coders must follow in order to accurately assign ICD-10 -CM codes. Both the Index and the Tabular List should be used for all ICD-10 -CM coding. Always code to the highest level of specificity. Conditions that are an integral part of a disease process should not be coded separately. Multiple codes are often required to report a single condition. The Official Guidelines address the use of combination codes. Copyright © F. A. Davis 2018 When coding both acute and chronic conditions, determine whether the subterms acute (subacute) and chronic are located at the same indentation level. For sequelae (late effects) coding, the acute condition is no longer present, but a residual condition remains. Impending and threatened conditions should first be coded by looking up the main terms impending or threatened or by searching for these terms as subterms. ICD-10 -CM diagnosis codes are only reported once. Two codes may be required to report laterality if a bilateral combination code is not available. 28
Chapter Summary (cont. ) Documentation used to report body mass index (BMI) and the stage of pressure ulcers can be obtained from clinicians who are not the patient’s provider. A cause-and-effect relationship must be documented in order to assign a code for a complication of care or a complication of a procedure. The Uniform Hospital Discharge Data Set (UHDDS) definitions apply to all nonoutpatient settings. The definition of principal diagnosis, which is based on the UHDDS definitions, is “that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care. The main rule regarding sequencing of the principal diagnosis codes is that codes for signs and symptoms should not be sequenced first when the underlying condition has been established. Copyright © F. A. Davis 2018 However, if a sign or symptom is followed by comparative or contrasting conditions, the symptom code is sequenced first. When each of two or more interrelated conditions potentially meets the definition of principal diagnosis, either condition can be first listed. If the original treatment plan was not carried out, the definition of principal diagnosis still applies, so the diagnosis after study is first. If the reason for admission is as a complication of medical care, the complication code is sequenced first. If a documented diagnosis at discharge is uncertain, probable, suspected, likely, questionable, possible, or still to be ruled out, the condition is coded as if it existed or was established. 29
Chapter Summary (cont. ) External cause codes are assigned as appropriate in the inpatient setting. For admission following medical observation, the principal diagnosis is the medical condition that leads to the hospital admission; for admission following postoperative observation, the principal diagnosis is that determined after study; and for admission after outpatient surgery, the admission circumstances determine the principal diagnosis. Copyright © F. A. Davis 2018 Codes for additional diagnoses, other diagnoses, and secondary diagnoses are not sequenced first. Once ICD-10 -CM codes have been assigned and sequenced, each code must be assigned an indicator that identifies whether the condition was present on admission. The entire inpatient coding process requires review of complete documentation and abstraction of diagnoses and procedures from the patient record. 30
Copyright © 2018 by F. A. Davis Company. All rights reserved. This product is protected by copyright. No part of it may be reproduced, stored in a retrieval system, or transmitted in any form or by any means—electronic, mechanical, photocopying, recording, or otherwise—without written permission from the publisher.
Credits Editor-in-Chief: Margaret Biblis Senior Acquisitions Editor: Quincy Mc. Donald Developmental Editor: Amelia L. Blevins Production Manager: Bob Butler Director, Digital Solutions: Kirk Pedrick Developed by Cognition catalysts, helping customers enhance content and empower learners The publisher is not responsible for errors of omission or for consequences from application of information in this presentation, and makes no warranty, expressed or implied, in regard to its content. Any practice described in this presentation should be applied by the reader in accordance with professional standards of care used with regard to the unique circumstances that may apply in each situation. Copyright © F. A. Davis 2018 32