CHF and COPD stream tools and outcome measures














- Slides: 63
CHF and COPD stream tools and outcome measures
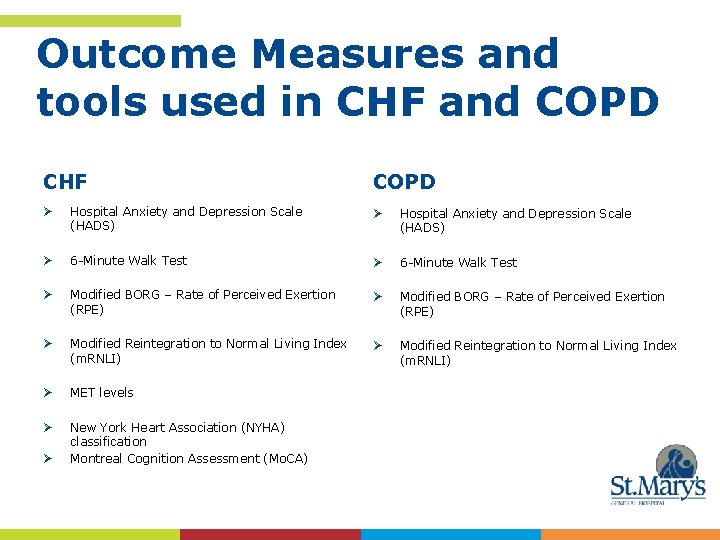
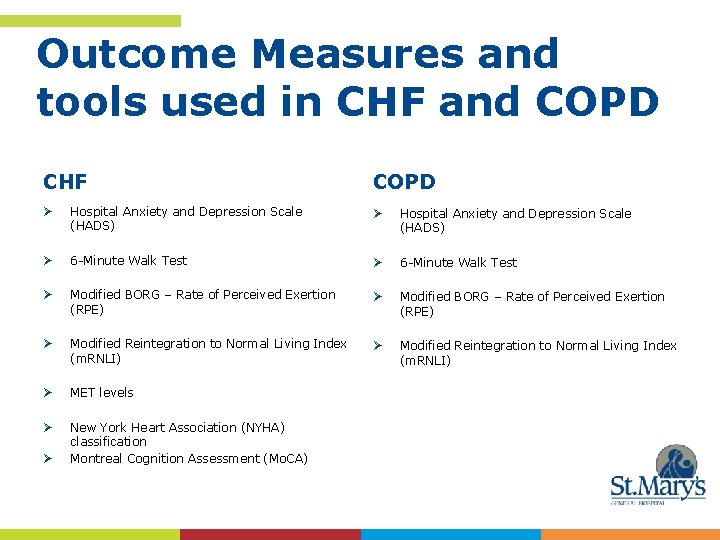
Outcome Measures and tools used in CHF and COPD CHF COPD Ø Hospital Anxiety and Depression Scale (HADS) Ø 6 -Minute Walk Test Ø Modified BORG – Rate of Perceived Exertion (RPE) Ø Modified Reintegration to Normal Living Index (m. RNLI) Ø MET levels Ø New York Heart Association (NYHA) classification Montreal Cognition Assessment (Mo. CA) Ø
Hospital Anxiety and Depression Scale (HADS)
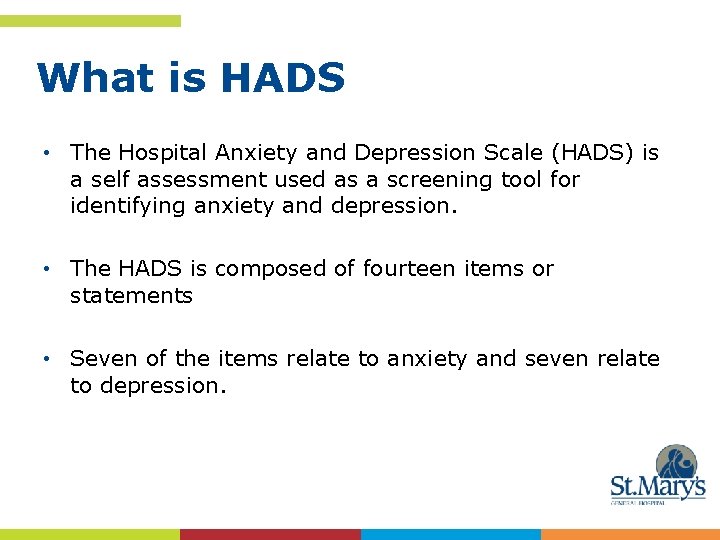
What is HADS • The Hospital Anxiety and Depression Scale (HADS) is a self assessment used as a screening tool for identifying anxiety and depression. • The HADS is composed of fourteen items or statements • Seven of the items relate to anxiety and seven relate to depression.
How do I perform the HADS? • Instruct the patient to read each statement with the four responses. • The patient should choose one response from the four given which currently describes their feelings over the past week as it relates to the statement. • Dissuade the patient from thinking too long about their answers, they should go with their first response.

Scoring the HADS • The questions relating to anxiety are marked "A", and to depression "D". • Each response has a score ranging from 0 -3 • The responses are summed to provide a separate score for anxiety and depression.
Interpretation of the HADS • A higher score (usually >8) indicates a likelihood of depression or anxiety.
Pros of using HADS as an outcome measure • The questionnaire is completed by the patient and only takes 2 -5 minutes for the clinician to interpret • Although originally designed to be used with hospital populations it has been found to perform well with non -hospital groups – therefore a good tool to compare across the continuum of care. • No training required to administer tool • The HADS is a validated tool.
Cons of HADS as an outcome measure
References • http: //www. rehabmeasures. org/default. aspx • http: //en. wikipedia. org/wiki/Hospital_Anxiety_and_De pression_Scale
References The tool can be obtained through the National Foundation for Education Research http: //www. nfernelson. co. uk or email: information@nfer-nelson. co. uk. They will supply the scale, the chart for recording the scores and a manual with instructions and interpretations.

6 Minute Walk Test
What is the 6 minute walk test? • The 6 Minute Walk Test is a test of aerobic capacity/endurance. • It assesses the distance walked over a 6 minute period. • It is a self-paced test and assesses the patient’s sub maximal level of functional capacity. Most ADL are performed at sub maximal levels of exertion; the 6 minute walk test can therefore be considered a fair reflection on a patient’s functional exercise level for daily physical activities.
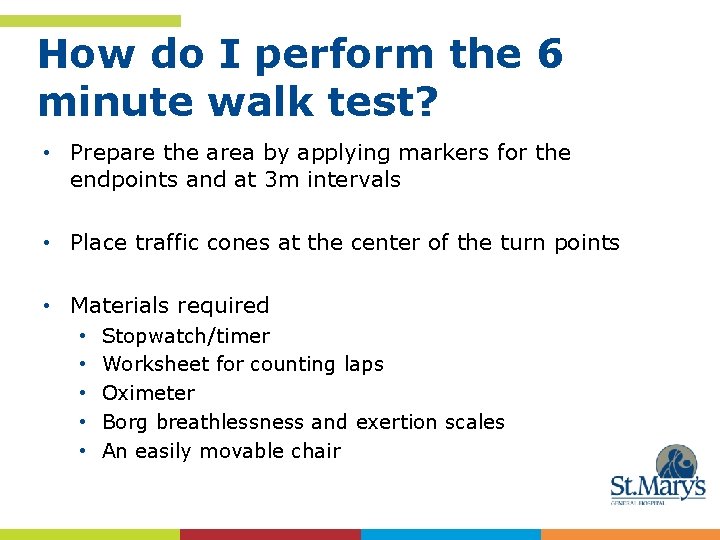
How do I perform the 6 minute walk test? • Prepare the area by applying markers for the endpoints and at 3 m intervals • Place traffic cones at the center of the turn points • Materials required • • • Stopwatch/timer Worksheet for counting laps Oximeter Borg breathlessness and exertion scales An easily movable chair
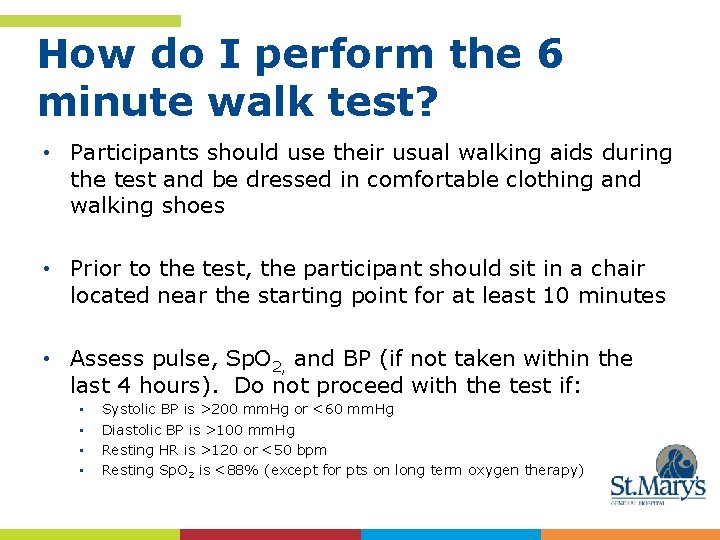
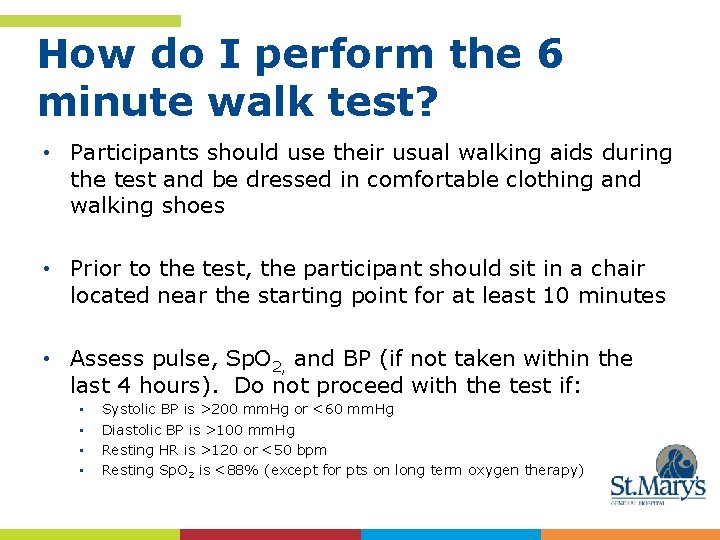
How do I perform the 6 minute walk test? • Participants should use their usual walking aids during the test and be dressed in comfortable clothing and walking shoes • Prior to the test, the participant should sit in a chair located near the starting point for at least 10 minutes • Assess pulse, Sp. O 2, and BP (if not taken within the last 4 hours). Do not proceed with the test if: • • Systolic BP is >200 mm. Hg or <60 mm. Hg Diastolic BP is >100 mm. Hg Resting HR is >120 or <50 bpm Resting Sp. O 2 is <88% (except for pts on long term oxygen therapy)
How do I perform the 6 minute walk test? • Explain the use of the modified BORG for assessing breathlessness. • Explain the use of the modified BORG rating for perceived exertion

How do I perform the 6 minute walk test? • Read the following instructions to the patient: “The object of the test is to walk as far as possible for 6 minutes. You will walk back and forth in this hallway. Six minutes is a long time to walk, so you will be exerting yourself. You will probably get out of breath or become exhausted. You are permitted to slow down, to stop, and to rest as necessary. You may lean against the wall while resting, but resume walking as soon as you are able. You will be walking back and forth around the cones. You should pivot briskly around the cones and continue back the other way without hesitation. Now I’m going to show you. ” • Demonstrate by walking one lap yourself. • To begin the test say to the patient: “Are you ready to do that? I am going to use this counter to keep track of the number of laps you complete. I will click it each time you turn around at this starting line. Remember that the object is to walk AS FAR AS POSSIBLE for 6 minutes, but don’t run or jog. Start now, or whenever you are ready. ”
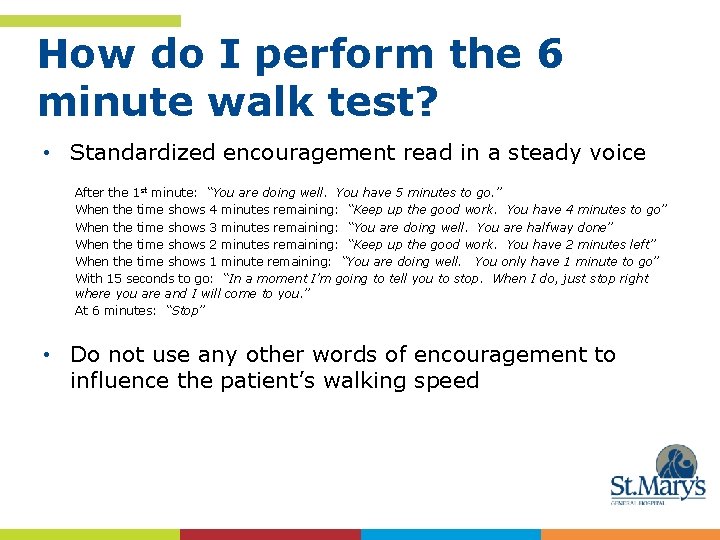
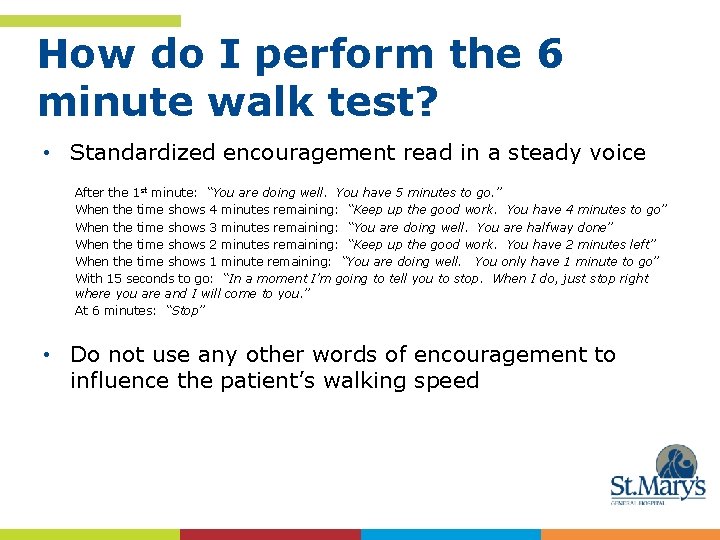
How do I perform the 6 minute walk test? • Standardized encouragement read in a steady voice After the 1 st minute: “You are doing well. You have 5 minutes to go. ” When the time shows 4 minutes remaining: “Keep up the good work. You have 4 minutes to go” When the time shows 3 minutes remaining: “You are doing well. You are halfway done” When the time shows 2 minutes remaining: “Keep up the good work. You have 2 minutes left” When the time shows 1 minute remaining: “You are doing well. You only have 1 minute to go” With 15 seconds to go: “In a moment I’m going to tell you to stop. When I do, just stop right where you are and I will come to you. ” At 6 minutes: “Stop” • Do not use any other words of encouragement to influence the patient’s walking speed
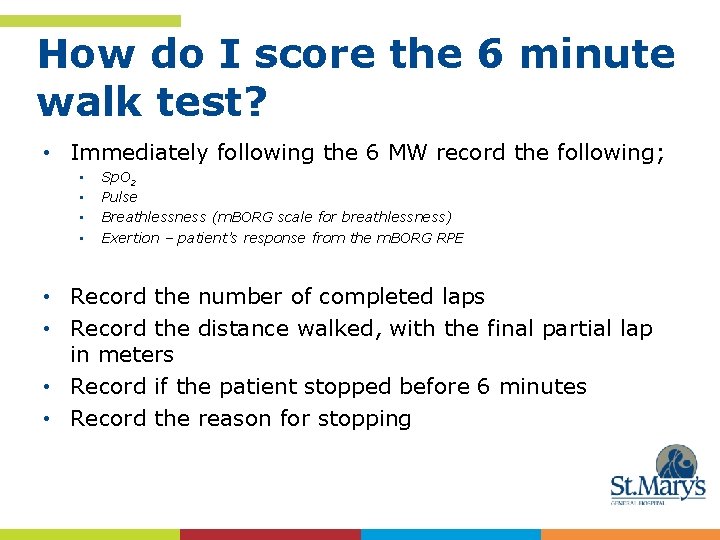
How do I score the 6 minute walk test? • Immediately following the 6 MW record the following; • • Sp. O 2 Pulse Breathlessness (m. BORG scale for breathlessness) Exertion – patient’s response from the m. BORG RPE • Record the number of completed laps • Record the distance walked, with the final partial lap in meters • Record if the patient stopped before 6 minutes • Record the reason for stopping
How do I interpret the 6 minute walk test? • The higher the distance the patient can achieve the more fit they are, and consequently the more functional or independent may be! • As an outcome draw comparisons for the distance walk, the RPE for breathlessness and the RPE for exertion.
Pros for using the 6 Minute Walk Test • It takes approximately 6 to 30 minutes to administer • It is a simple test that requires a 100 ft long hallway, no exercise equipment or advanced training for the technicians • It is self-paced and assesses the sub maximal level of functional capacity. Patient’s choose their own intensity of exercise and are allowed to stop and rest during the test.

Cons of 6 Minute Walk Test • Space limitations to set up the test walking track

References http: //en. wikipedia. org/wiki/Metabolic_equivalent Accessed May 14, 2013 Clin. Cardiol. 13, 555 -565 (1990). Metabolic Equivalents (METS) in Exercise Testing, Exercise Prescription, and Evaluation of Functional Capacity. M. JETTE.

Modified BORG (m. BORG)
What is the Modified BORG scale (m. BORG)? • The Borg Rating of Perceived Exertion (RPE) Scale and Borg Rating of Breathlessness are used as indicators to monitor and guide exercise or activity intensity. • The original scale introduced by Gunnar Borg rated exertion on a scale of 6 -20. More commonly used today is the revised modified scale from 0 -10.
How do I perform the m. BORG? • It is easy to use, however clinicians must take time to educate the patient and ensure appropriate understanding prior to use.
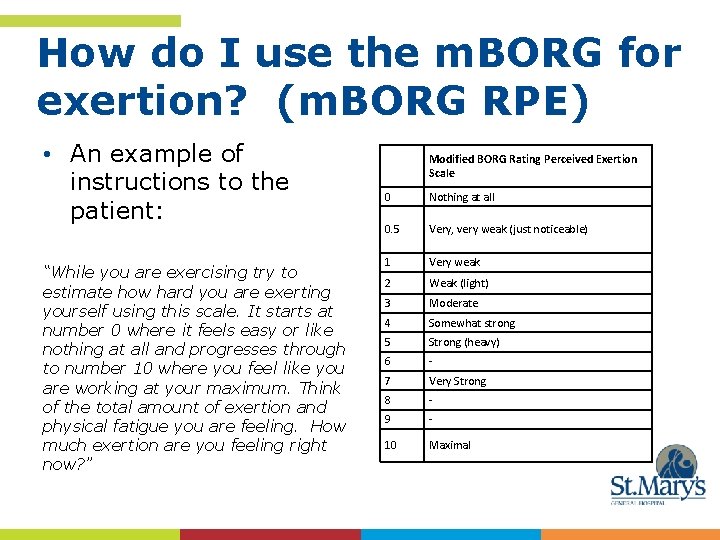
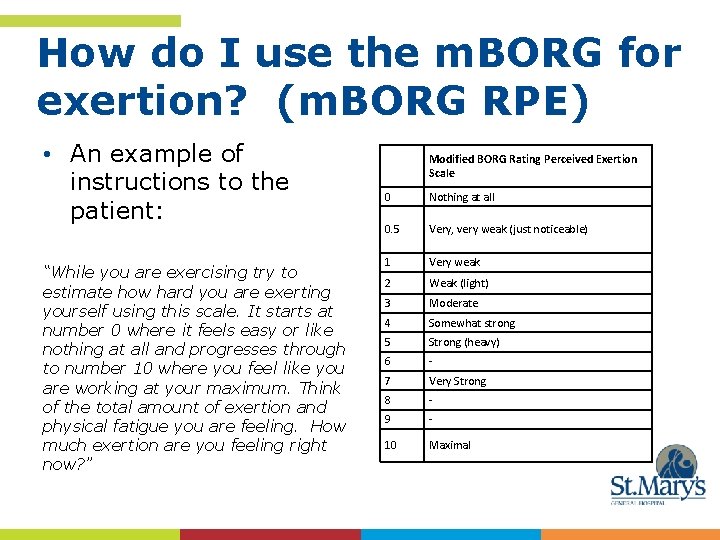
How do I use the m. BORG for exertion? (m. BORG RPE) • An example of instructions to the patient: “While you are exercising try to estimate how hard you are exerting yourself using this scale. It starts at number 0 where it feels easy or like nothing at all and progresses through to number 10 where you feel like you are working at your maximum. Think of the total amount of exertion and physical fatigue you are feeling. How much exertion are you feeling right now? ” Modified BORG Rating Perceived Exertion Scale 0 Nothing at all 0. 5 Very, very weak (just noticeable) 1 Very weak 2 Weak (light) 3 Moderate 4 Somewhat strong 5 Strong (heavy) 6 - 7 Very Strong 8 - 9 - 10 Maximal
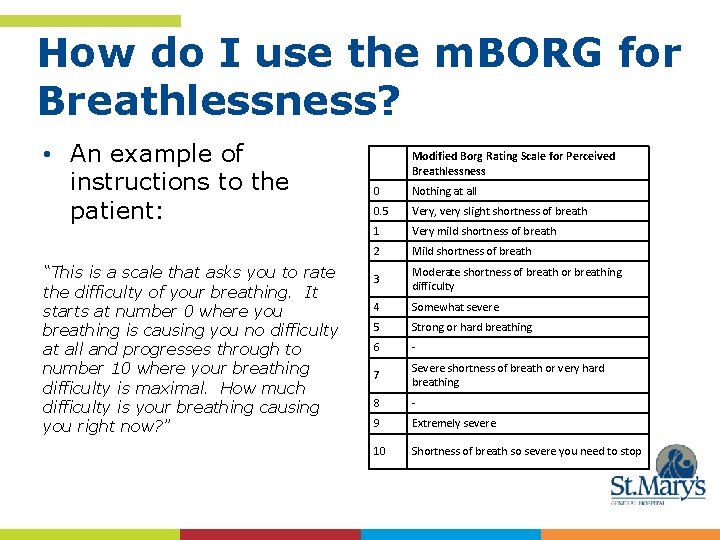
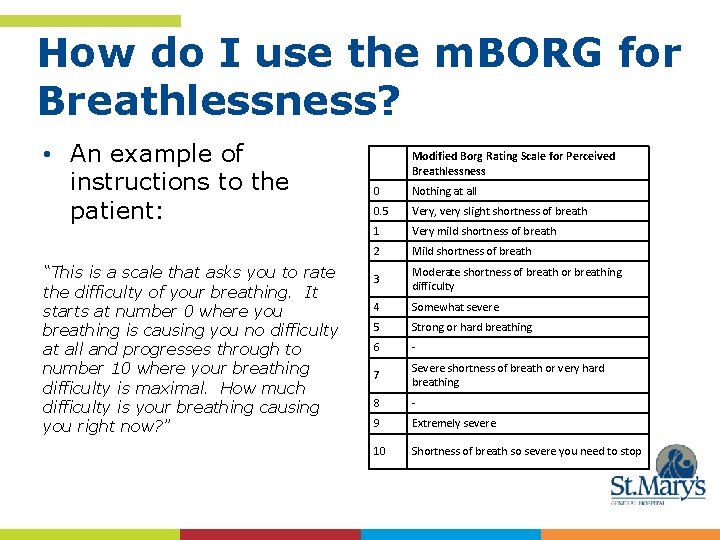
How do I use the m. BORG for Breathlessness? • An example of instructions to the patient: “This is a scale that asks you to rate the difficulty of your breathing. It starts at number 0 where you breathing is causing you no difficulty at all and progresses through to number 10 where your breathing difficulty is maximal. How much difficulty is your breathing causing you right now? ” Modified Borg Rating Scale for Perceived Breathlessness 0 Nothing at all 0. 5 Very, very slight shortness of breath 1 Very mild shortness of breath 2 Mild shortness of breath 3 Moderate shortness of breath or breathing difficulty 4 Somewhat severe 5 Strong or hard breathing 6 - 7 Severe shortness of breath or very hard breathing 8 - 9 Extremely severe 10 Shortness of breath so severe you need to stop
Scoring and Interpretation of the m. BORG • The score is the rate the patient assigns for a given activity in relation to the activity outcomes. • When interpreting the scores, the practitioner takes into consideration the activity. The score is the patient’s subjective response to that activity. IE: a patient may have the same m. RPE score pre and post treatment, yet achieve a greater distance on the 6 minute walk test with less breathlessness and less exertion.
Pros of using the m. BORG • Using the BORG scale does not require any special skills or equipment • It is motivational demonstrating improvement in ability with certain activities over time. • The RPE can be used as a guide for exercise intensity. Exercising at moderate levels will help increase endurance and improve lung function. Knowing what “zone” they should exercise in, will help the patient recognize when they are exerting themselves to a level where they may be putting themselves at risk.
Cons of using the m. BORG • It is a subjective measure rating the patient’s level of exertion or breathlessness
References • www. acsm. org/docs/currentcomments/perceivedexertion. pdf • http: //en. wikipedia. org/wiki/Borg_scale • www. ncbi. nlm. nih. gov/pmc/articles/PMC 2941353/
Modified Reintegration to Normal Living Index (m. RNLI)
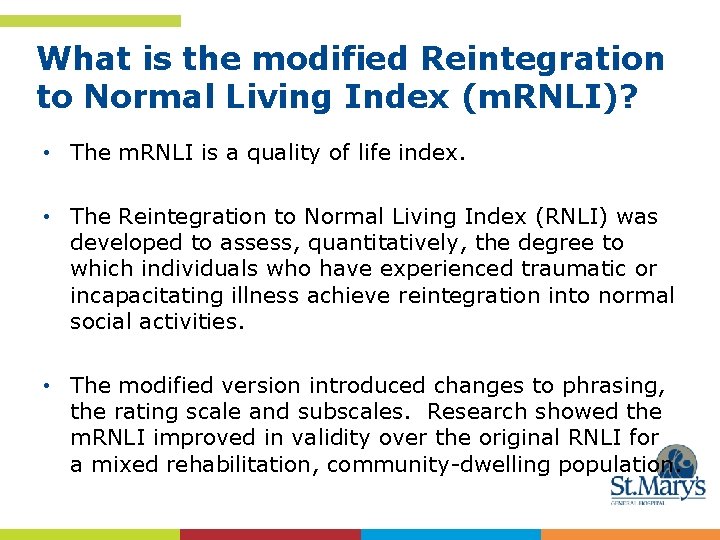
What is the modified Reintegration to Normal Living Index (m. RNLI)? • The m. RNLI is a quality of life index. • The Reintegration to Normal Living Index (RNLI) was developed to assess, quantitatively, the degree to which individuals who have experienced traumatic or incapacitating illness achieve reintegration into normal social activities. • The modified version introduced changes to phrasing, the rating scale and subscales. Research showed the m. RNLI improved in validity over the original RNLI for a mixed rehabilitation, community-dwelling population.

How do I use the m. RNLI? 1. I move around my house as I need to 2. I move around my community as I need to. 3. I am able to make longer trips as I need to. 4. I am comfortable with how my self-care needs are met (dressing, feeding toileting bathing). 5. I spend most of my days occupied in work activity that is necessary or important to me (such as paid or voluntary work, housework, or studying etc. ). 6. I am able to participate in recreational activities as I want to (hobbies, crafts, sports, reading, television, games, computers etc. ). 7. I socialize with friends, family and/or business acquaintances as I want to or is necessary. 8. I have a role in my family which meets my needs and those of my family members. (Family means people with whom you live and/or relatives with whom you don’t live but see on a regular basis. ) 9. In general, I am comfortable with my personal relationships. 10. In general, I am comfortable with myself when I am in the company of others. 11. I feel that I can deal with life events as they happen. Does not describe me or my situation Sometimes Mostly describes me or my situation Fully describes me or my situation • Instructions to the patient: “For each of the following statements, please indicate how well each statement describes you and/or your situation by placing a mark in a box. Please mark only one box per question. ”
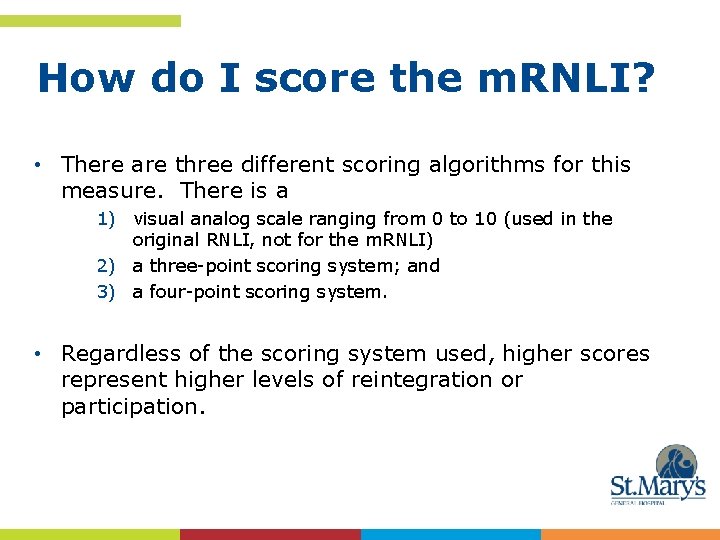
How do I score the m. RNLI? • There are three different scoring algorithms for this measure. There is a 1) visual analog scale ranging from 0 to 10 (used in the original RNLI, not for the m. RNLI) 2) a three-point scoring system; and 3) a four-point scoring system. • Regardless of the scoring system used, higher scores represent higher levels of reintegration or participation.
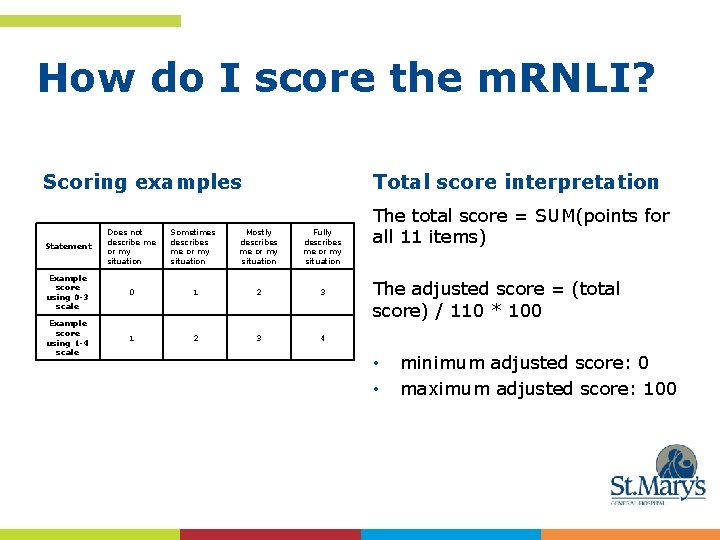
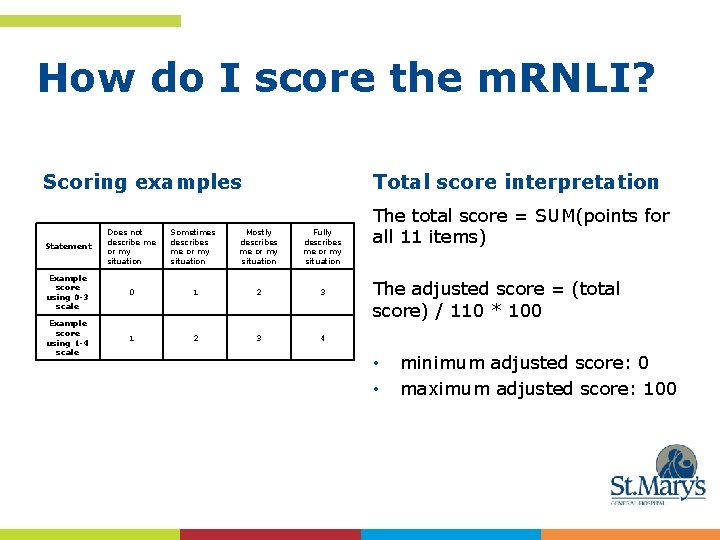
How do I score the m. RNLI? Scoring examples Total score interpretation Statement Does not describe me or my situation Sometimes describes me or my situation Mostly describes me or my situation Fully describes me or my situation Example score using 0 -3 scale 0 1 2 3 Example score using 1 -4 scale 1 2 3 4 The total score = SUM(points for all 11 items) The adjusted score = (total score) / 110 * 100 • • minimum adjusted score: 0 maximum adjusted score: 100
m. RNLI interpretation • The higher the score the better the patient’s perceived reintegration.
Pros of the m. RNLI • Self administered • Ease of scoring and interpretation • Can be used in conjunction with goal setting, encouraging the patient to consider how their current state impacts their life, and what goals they would like to work towards to achieve improved quality of life

Cons of the m. RNLI • Patients sometimes have difficulty relating to the statements
References http: //www. parqol. com/page. cfm? id=114 http: //strokengine. ca/assess/pdf/RNLI. pdf http: //www. rehabmeasures. org http: //link. springer. com/referenceworkentry/10. 1007%2 F 978 -0 -387 -79948 -3_1962
Understanding MET levels

What is a MET level • METs are a way of expressing rate of oxygen utilization. One MET is the rate of oxygen utilization at rest (when your body is sitting quietly) and is equivalent to 3. 5 ml oxygen/kg body weight/min. An activity that uses oxygen at twice the resting rate is equal to a 2 MET level. • MET levels are based on the intensity of the work, not the length of time that someone performs the work • METs describe the functional capacity or exercise tolerance of an individual.
Why you may want to know about METs? • Certain activities may be too intense for some people. All activities have an energy requirement or a “metabolic cost”. This is expressed as a metabolic equivalent or METs. • Sometimes physicians refer to METs during patient assessments. It can be seen as an indicator of how “functional” a patient is. • Knowing someone’s MET level or range may provide you with some insight as to their current level of activity or level of independence.

Examples of MET level requirements Physical activity Light intensity activities MET <3 Activities of Daily Living MET Light activities sleeping 0. 9 Bathing in tub/eating 1 -2 watching television 1. 0 writing, desk work, typing 1. 8 walking, 1. 7 mph (2. 7 km/h), level ground, strolling, very slow 2. 3 Light housework walking, 2. 5 mph (4 km/h) 2. 9 Moderate intensity activities 3 to 6 2 Warm shower - sitting 2 -3 Fixing meals 2. 5 Moderate activities bicycling, stationary, 50 watts, very light effort 3. 0 Washing floors 3. 3 walking 3. 0 mph (4. 8 km/h) 3. 3 Warm shower standing 3 -4 calisthenics, home exercise, light or moderate effort, general 3. 5 Grocery shopping/vaccuming 3 -4 walking 3. 4 mph (5. 5 km/h) 3. 6 Mowing lawn - riding 3 -4 bicycling, <10 mph (16 km/h), leisure, to work or for pleasure 4. 0 Gardening – weeding and raking 3. 5 Gardening - digging 4. 4 bicycling, stationary, 100 watts, light effort 5. 5 Snow shoveling 5. 1 Vigorous intensity activities >6 jogging, general 7. 0 calisthenics (e. g. pushups, sit-ups, pullups, jumping jacks), heavy, vigorous effort 8. 0 running jogging, in place 8. 0 rope jumping 10. 0 Vigorous intensity activities Mowing lawn - walking 7. 0 Chopping wood 8. 0 Carpentry work 5 -7
How do I use MET levels in practice? • METS can be used as an intensity guide for patients when they exercise • As a general rule, 4– 6 METs is considered moderate intensity. When exercising patients should strive for at least 30– 45 minutes of moderately intense activity on most days of the week. • Knowing the range of METs at which they should be exercising makes it easier to choose appropriate activities.
What do MET levels mean as an outcome? • The higher the MET level the patient can achieve the more fit they are, and consequently the more functional or independent they are! • Physical conditioning lowers a persons RPE for a given MET level, (more about RPE to come!)
Pros of using MET levels as an outcome measure • When used in conjunction with RPE it provides feedback to patients re progress • Accuracy when obtained via exercise stress treadmill test
Cons of MET levels as an outcome measure • Requires patients to participate in an exercise stress test • Defining an exercise prescription through use of MET levels requires specialized training

References http: //en. wikipedia. org/wiki/Metabolic_equivalent Accessed May 14, 2013 Clin. Cardiol. 13, 555 -565 (1990). Metabolic Equivalents (METS) in Exercise Testing, Exercise Prescription, and Evaluation of Functional Capacity. M. JETTE.
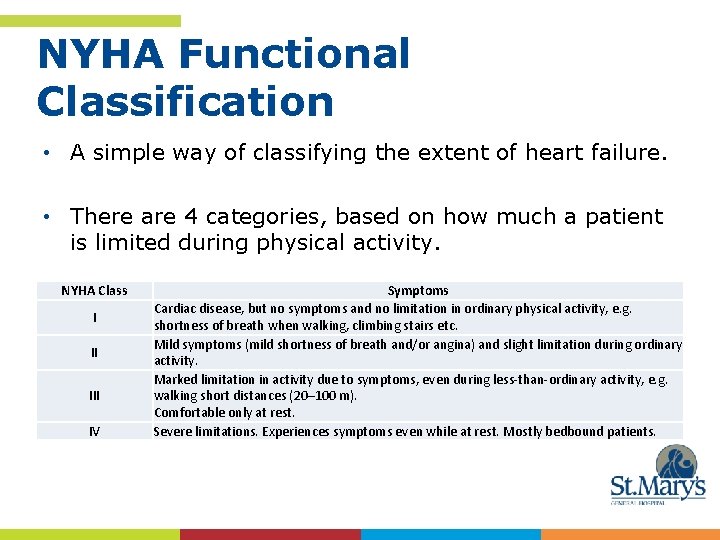
Understanding NYHA classification
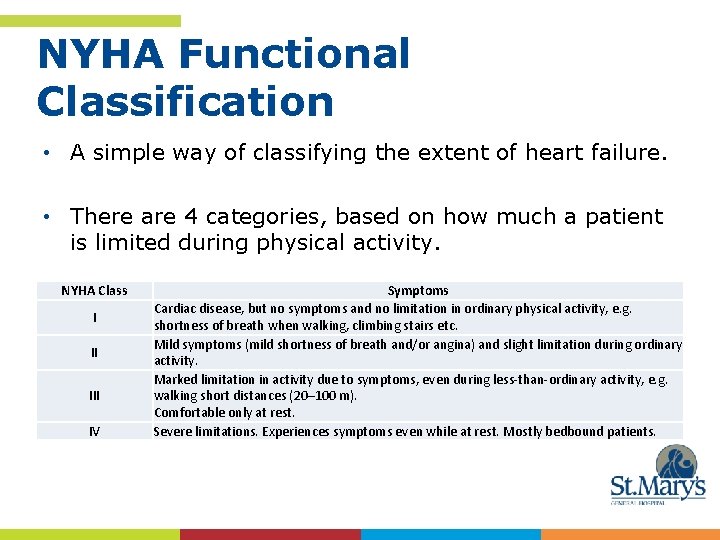
NYHA Functional Classification • A simple way of classifying the extent of heart failure. • There are 4 categories, based on how much a patient is limited during physical activity. NYHA Class I II IV Symptoms Cardiac disease, but no symptoms and no limitation in ordinary physical activity, e. g. shortness of breath when walking, climbing stairs etc. Mild symptoms (mild shortness of breath and/or angina) and slight limitation during ordinary activity. Marked limitation in activity due to symptoms, even during less-than-ordinary activity, e. g. walking short distances (20– 100 m). Comfortable only at rest. Severe limitations. Experiences symptoms even while at rest. Mostly bedbound patients.
Why you may want to know about NYHA • Doctors usually classify patients' heart failure according to the severity of their symptoms. • It may help you define your plan of care and determine your exercise prescription
References http: //en. wikipedia. org/wiki/New_York_Heart_Association_Fu nctional_Classification http: //www. heart. org/HEARTORG/Conditions/Heart. Failure/Abo ut. Heart. Failure/Classes-of-Heart. Failure_UCM_306328_Article. jsp#

Montreal Cognition Assessment (Mo. CA)

What is the Mo. CA? • The Montreal cognitive Assessment (Mo. CA) was designed as a rapid screening tool for mild cognitive dysfunction. • It assesses: • • Attention and concentration Executive functions Memory Language Visuoconstructional skills Conceptual thinking Calculations orientation
How do I perform the Mo. CA? • The test may be administered by anyone who understands and follows the instructions • Test instructions are specific and may be repeated once with the exception of items tested on the list of words, list of digits, list of letters, subtraction answers and phrases to repeat, these may not be repeated. • For complete instructions and scoring access the website www. mocatest. org. There are detailed instructions which should be followed
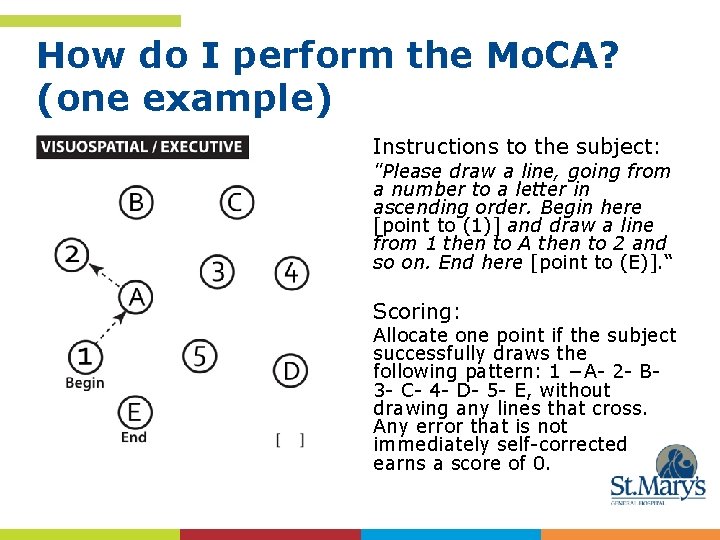
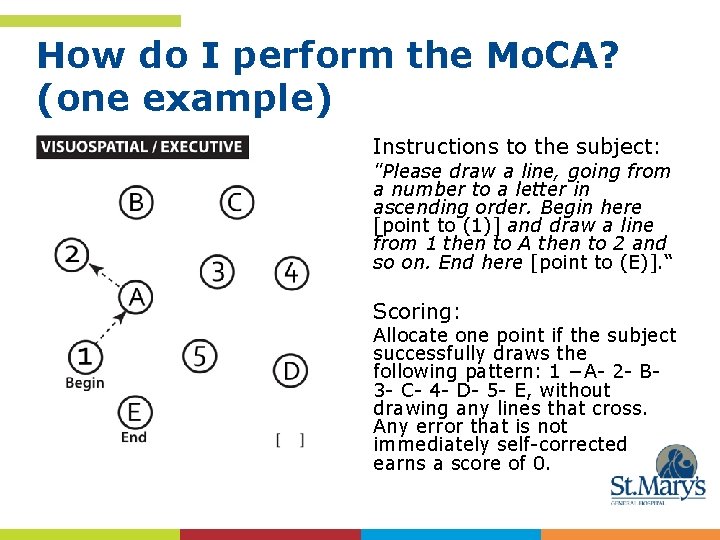
How do I perform the Mo. CA? (one example) Instructions to the subject: "Please draw a line, going from a number to a letter in ascending order. Begin here [point to (1)] and draw a line from 1 then to A then to 2 and so on. End here [point to (E)]. “ Scoring: Allocate one point if the subject successfully draws the following pattern: 1 −A- 2 - B- 3 - C- 4 - D- 5 - E, without drawing any lines that cross. Any error that is not immediately self-corrected earns a score of 0.
Mo. CA interpretation? • The score is a summation of the 11 tests. The total possible score is 30 points; a score of 26 or above is considered normal. • 18 -26 = mild cognitive impairment, • 10 -17= moderate cognitive impairment • less than 10= severe cognitive impairment • Only a health professional with expertise in the cognitive field may interpret the results.
Pros of using the Mo. CA • At this time no special training is required to administer the test.
Cons of using the Mo. CA • The test administrator must follow the written script in providing the patient instructions for the test • Interpretation of the results should be completed by health care providers who are experts in cognition

References http: //www. mocatest. org
Thank you to the following organizations for their collaborative efforts which led to the development of the COPD and CHF care paths, patient education material and Care-giver resources. Cambridge Cardiac Care Cambridge Memorial Hospital Grand River Hospital Groves Memorial Hospital Guelph General Hospital Mount Forest Family Health Team St. Joseph’s Health Care, Guelph St. Mary’s General Hospital Upper Grand Family Health Team Waterloo Wellington Community Care Access Center The Cardiopulmonary Rehab Stream of Care