APPROACH TO THE PATENTS WTH CHRONIC ARTHRITIS Dr





















- Slides: 67
APPROACH TO THE PATİENTS WİTH CHRONIC ARTHRITIS Dr. MÜGE BIÇAKÇIGİL KALAYCI
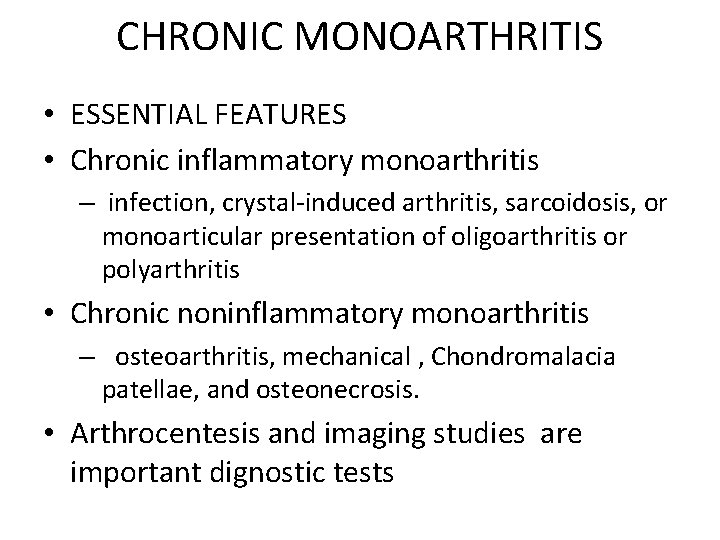
CHRONIC MONOARTHRITIS • ESSENTIAL FEATURES • Chronic inflammatory monoarthritis – infection, crystal-induced arthritis, sarcoidosis, or monoarticular presentation of oligoarthritis or polyarthritis • Chronic noninflammatory monoarthritis – osteoarthritis, mechanical , Chondromalacia patellae, and osteonecrosis. • Arthrocentesis and imaging studies are important dignostic tests
CHRONIC MONOARTHRITIS • INITIAL CLINICAL EVALUATION • Infections, particularly indolent infections, are a concern with inflammatory monoarthritis that lasts from weeks to months. • The particular joint involved influences the differential diagnosis.
CHRONIC MONOARTHRITIS • LABORATORY EVALUATION • A critical step is to determine whether the monoarthritis is inflammatory, preferably by analyzing synovial fluid. • Synovial fluid should be sent for culture (bacterial, mycobacterial, and fungal), WBC count, and gram stain and examined for crystals by polarized light microscopy.
CHRONIC MONOARTHRITIS • Routine laboratory studies (eg, complate blood cell count, creatinine, and urine analysis) and determination of the ESR or CRP and uric acid level can provide helpful information. • Patients with inflammatory monoarthritis and negative bacterial cultures shoud be tested for reactivity to purified protein derivative (PPD)
CHRONIC MONOARTHRITIS • IMAGING STUDIES • Unlike in acute monoarthritis , radiographs can be helpful in evaluating chronic monoarthritis and can point to correct diagnosis in cases of infection, osteoarthritis, and osteonecrosis.
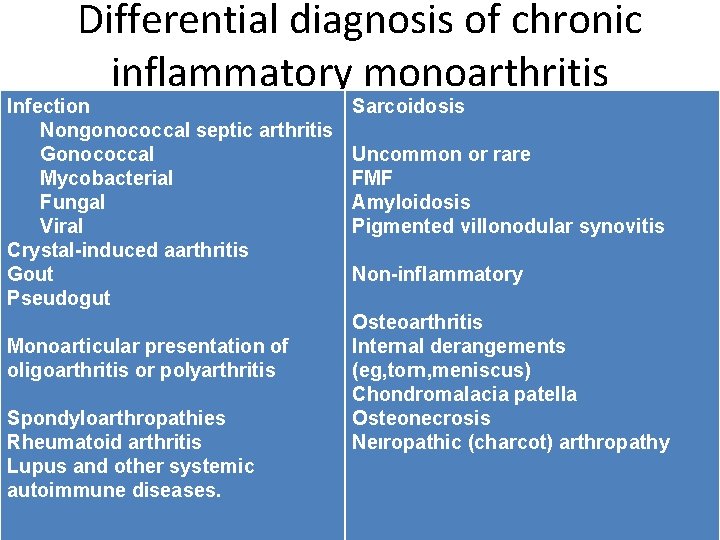
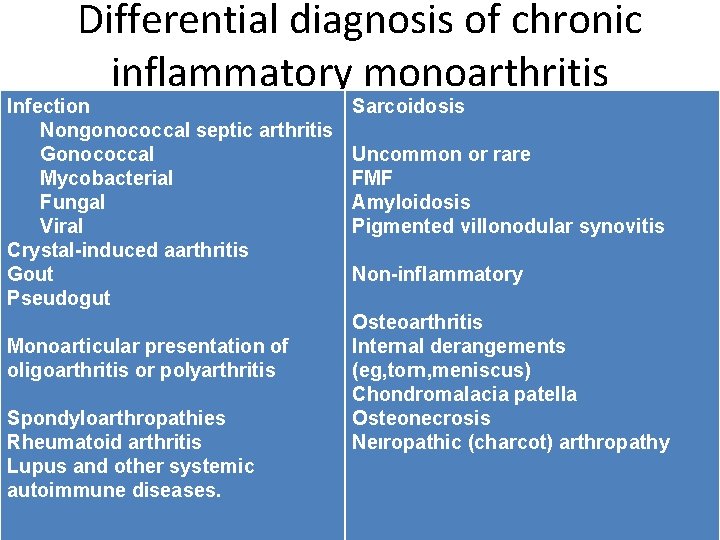
Differential diagnosis of chronic inflammatory monoarthritis Infection Nongonococcal septic arthritis Gonococcal Mycobacterial Fungal Viral Crystal-induced aarthritis Gout Pseudogut Monoarticular presentation of oligoarthritis or polyarthritis Spondyloarthropathies Rheumatoid arthritis Lupus and other systemic autoimmune diseases. Sarcoidosis Uncommon or rare FMF Amyloidosis Pigmented villonodular synovitis Non-inflammatory Osteoarthritis Internal derangements (eg, torn, meniscus) Chondromalacia patella Osteonecrosis Neıropathic (charcot) arthropathy
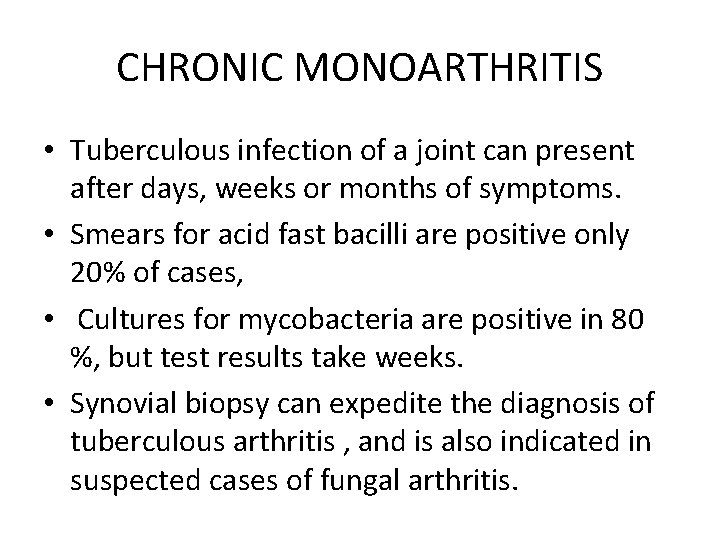
CHRONIC MONOARTHRITIS • Tuberculous infection of a joint can present after days, weeks or months of symptoms. • Smears for acid fast bacilli are positive only 20% of cases, • Cultures for mycobacteria are positive in 80 %, but test results take weeks. • Synovial biopsy can expedite the diagnosis of tuberculous arthritis , and is also indicated in suspected cases of fungal arthritis.
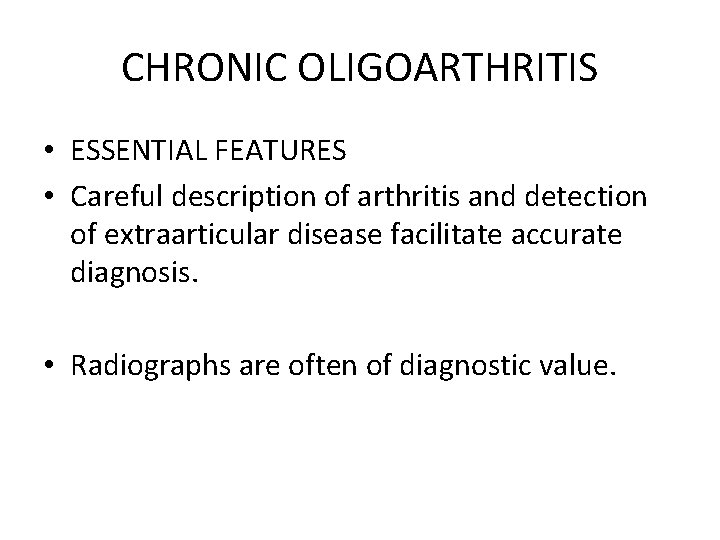
CHRONIC OLIGOARTHRITIS • ESSENTIAL FEATURES • Careful description of arthritis and detection of extraarticular disease facilitate accurate diagnosis. • Radiographs are often of diagnostic value.
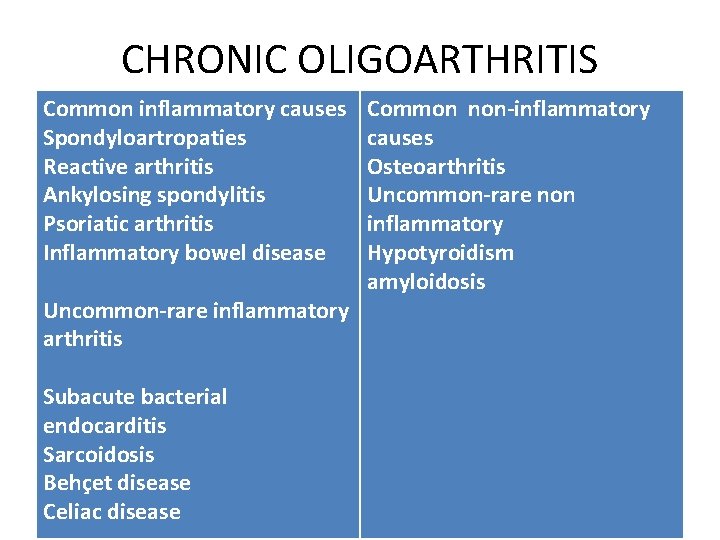
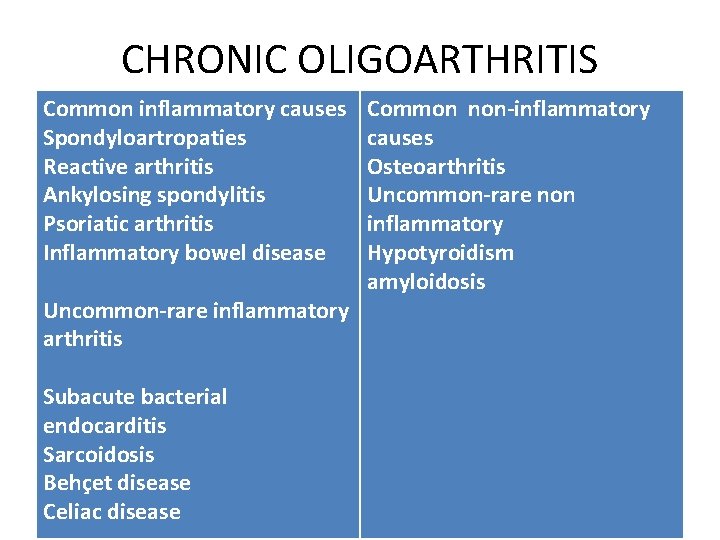
CHRONIC OLIGOARTHRITIS Common inflammatory causes Spondyloartropaties Reactive arthritis Ankylosing spondylitis Psoriatic arthritis Inflammatory bowel disease Uncommon-rare inflammatory arthritis Subacute bacterial endocarditis Sarcoidosis Behçet disease Celiac disease Common non-inflammatory causes Osteoarthritis Uncommon-rare non inflammatory Hypotyroidism amyloidosis
CHRONIC OLIGOARTHRITIS • Spondyloartropathies are the most common cause of chr. Oligoarthritis • Early onset rheumatoid arthritis must be distinquished. • Osteoarthritis presents as oligoarthritis of the hips or knees
CHRONIC OLIGOARTHRITIS • Laboratory evaluation • Synovial fluid analysis- culture- crystals • RF-dd(x) of RA • HLA B 27 - limited value
CHRONIC OLIGOARTHRITIS • Radiographs and Imaging studies-considerable value • Evidence of sacroitis indicates a spondyloarthropaty and narrow dd(x) • Erosions of RA and Gout
CHRONIC OLIGOARTHRITIS • Spondyloartropaties- asymmetric oligoarthritis • RA- symmetric poliarthritis • İn early RA- oligoartitis • Stiffness and pain in low back- Spa • RA- only cervical spine
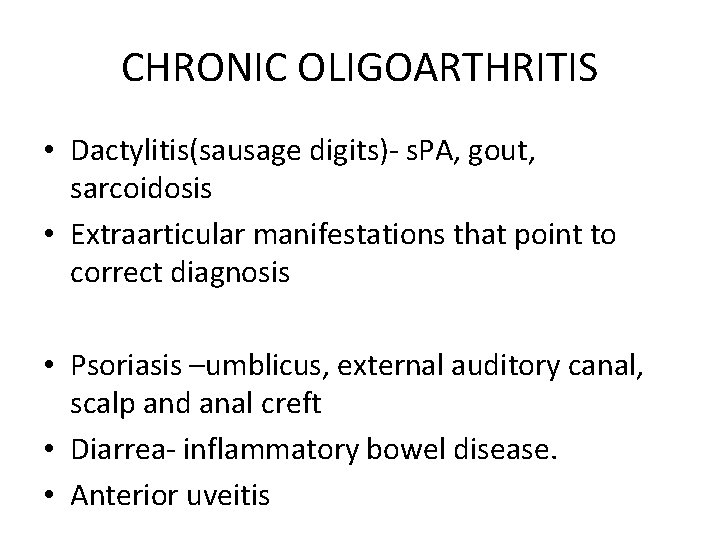
CHRONIC OLIGOARTHRITIS • Dactylitis(sausage digits)- s. PA, gout, sarcoidosis • Extraarticular manifestations that point to correct diagnosis • Psoriasis –umblicus, external auditory canal, scalp and anal creft • Diarrea- inflammatory bowel disease. • Anterior uveitis
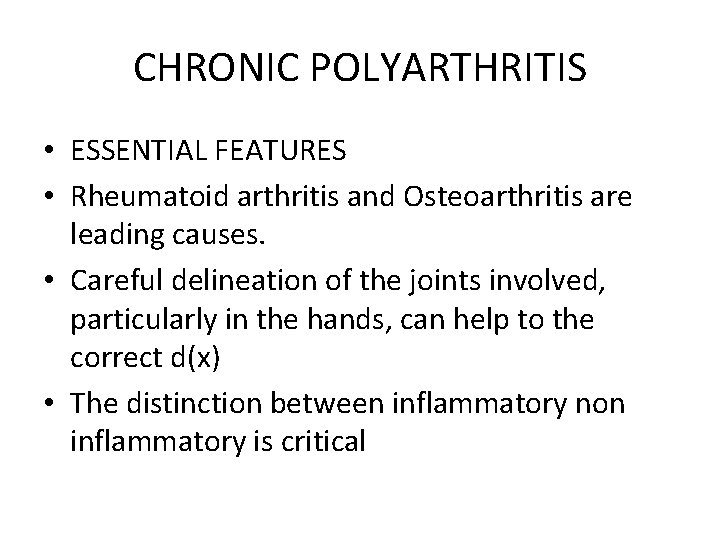
CHRONIC POLYARTHRITIS • ESSENTIAL FEATURES • Rheumatoid arthritis and Osteoarthritis are leading causes. • Careful delineation of the joints involved, particularly in the hands, can help to the correct d(x) • The distinction between inflammatory non inflammatory is critical
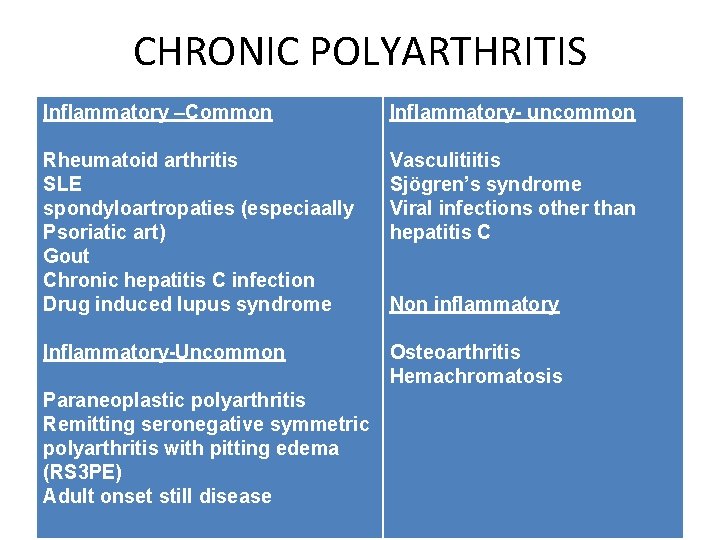
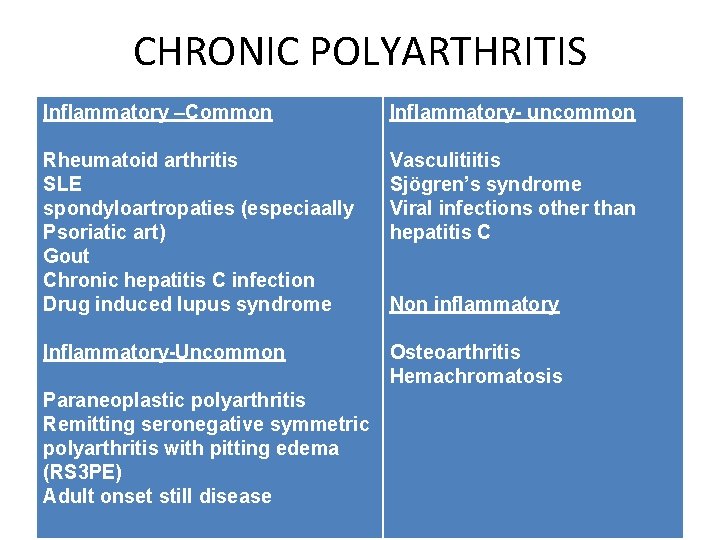
CHRONIC POLYARTHRITIS Inflammatory –Common Inflammatory- uncommon Rheumatoid arthritis SLE spondyloartropaties (especiaally Psoriatic art) Gout Chronic hepatitis C infection Drug induced lupus syndrome Vasculitiitis Sjögren’s syndrome Viral infections other than hepatitis C Inflammatory-Uncommon Osteoarthritis Hemachromatosis Paraneoplastic polyarthritis Remitting seronegative symmetric polyarthritis with pitting edema (RS 3 PE) Adult onset still disease Non inflammatory
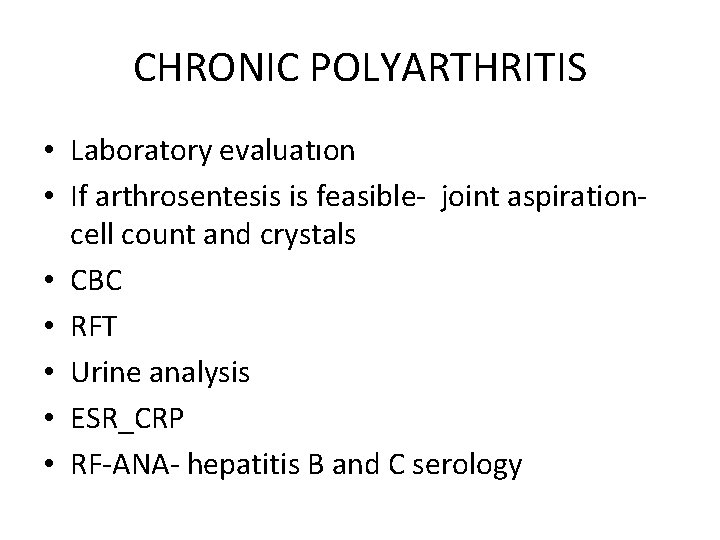
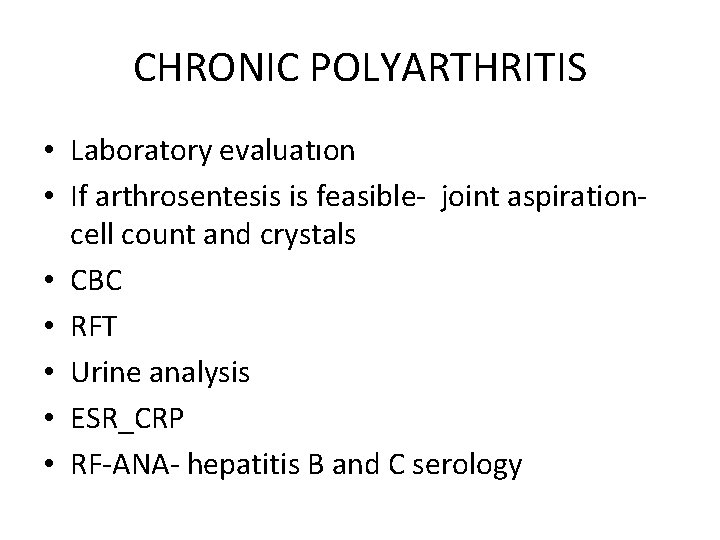
CHRONIC POLYARTHRITIS • Laboratory evaluatıon • If arthrosentesis is feasible- joint aspiration- cell count and crystals • CBC • RFT • Urine analysis • ESR_CRP • RF-ANA- hepatitis B and C serology
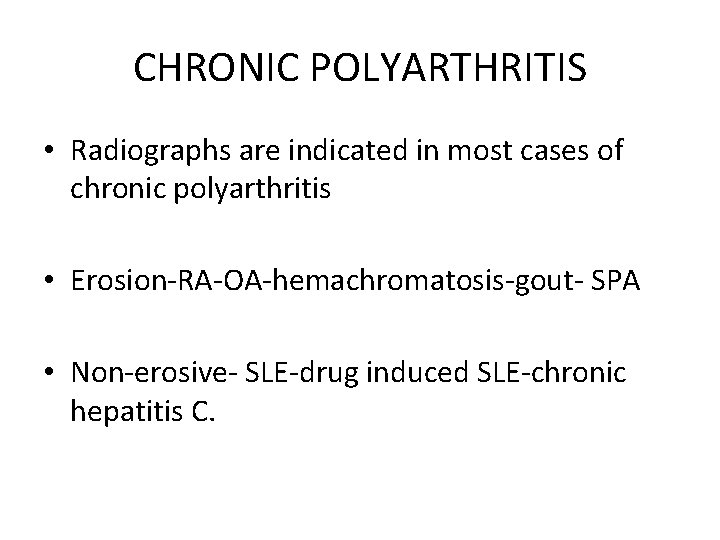
CHRONIC POLYARTHRITIS • Radiographs are indicated in most cases of chronic polyarthritis • Erosion-RA-OA-hemachromatosis-gout- SPA • Non-erosive- SLE-drug induced SLE-chronic hepatitis C.
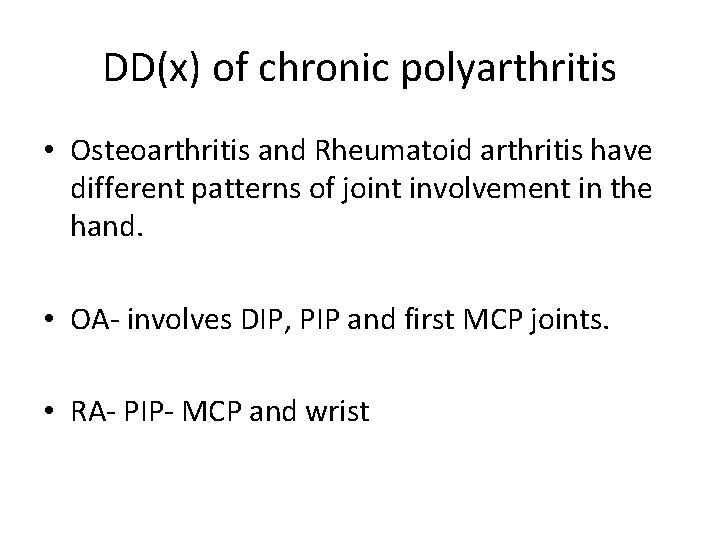
DD(x) of chronic polyarthritis • Osteoarthritis and Rheumatoid arthritis have different patterns of joint involvement in the hand. • OA- involves DIP, PIP and first MCP joints. • RA- PIP- MCP and wrist
• Osteoarthritis and Rheumatoid arthritis spare certain joints • OA- does not involve MCP, wrist, elbow, ankles • • RA- spare DIP, thoracic and lumbosacral spine and sacroiic joints • Psoriatic arthritis- DIP joints
ASSOCIATED HISTORY • • • Predisposing factors • Medication • Bowels • Urinary • Rashes • Eyes • Raynaud’s • Sicca • Family History

EXAMINATION • Multi-system • Disability • Range of movement • Signs of inflammation

INVESTIGATIONS • • • FBE/E/LFT • ESR/CRP • Iron studies • Uric Acid • Auto antibodies • HLA-B 27 • Viral serology • Joint fluid • Imaging
Skin and nail findings and arthritis
Skin rashes • Diffuse eruption with fever and systemic findings • Generally viral or due to primary immunological disease • Must be differentiated from bacterial diseases • SLE, DM • Rheumatic fever • Still disease • Kawasaki disease

Adult still disease
Papulosquamaus lesions • Psoriatic arthritis • Reiter Syndrome • SLE


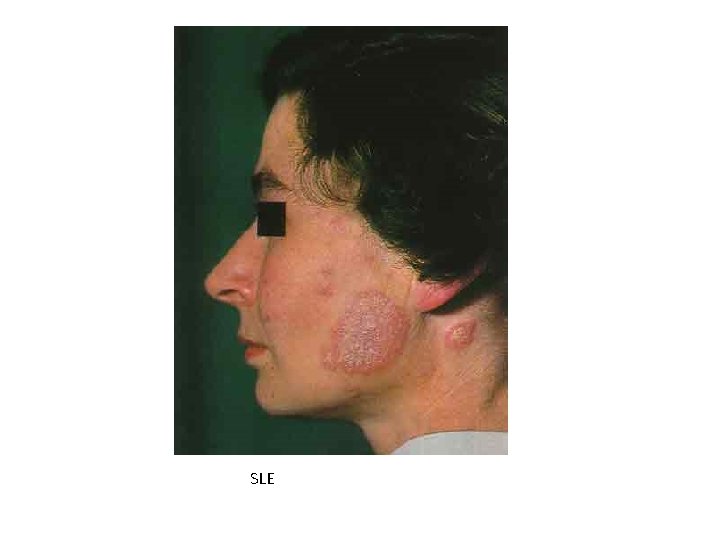
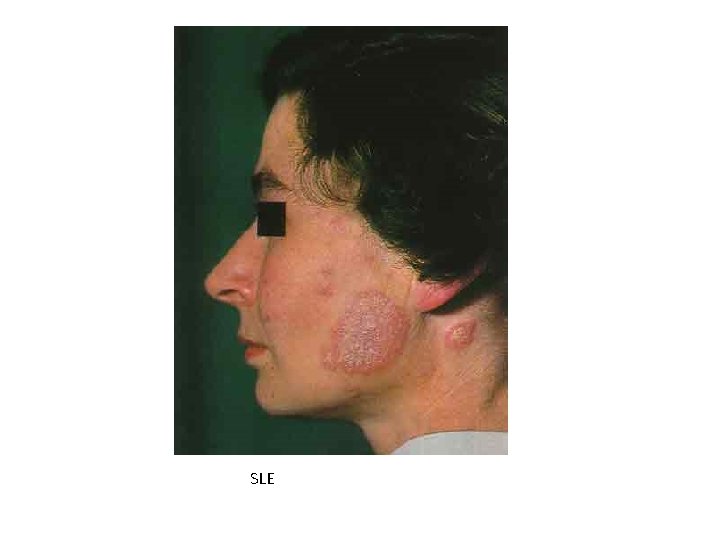
SLE
Annular lesions • Rheumatic fever • Subcutaneous Lupus

Facial lesions • Malar and discoid rash • Lupus pernio: Sarcoidosis • Dermatomyositis-gottron papules-heliotrope rash • Lupus vulgaris: cutanous tuberculosis




Nodular lesions • RA, ARA, crystal artropathies • Erythema nodosum: Behçet’s disease, Sarcoidosis, spondyloartropathies, tbc


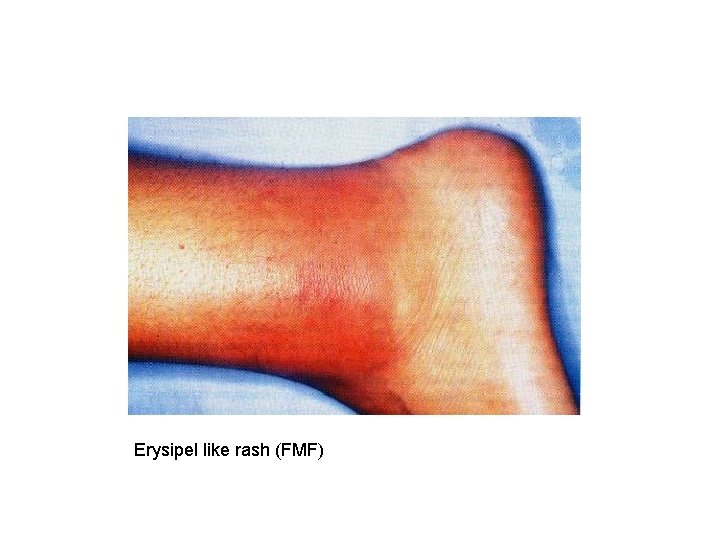
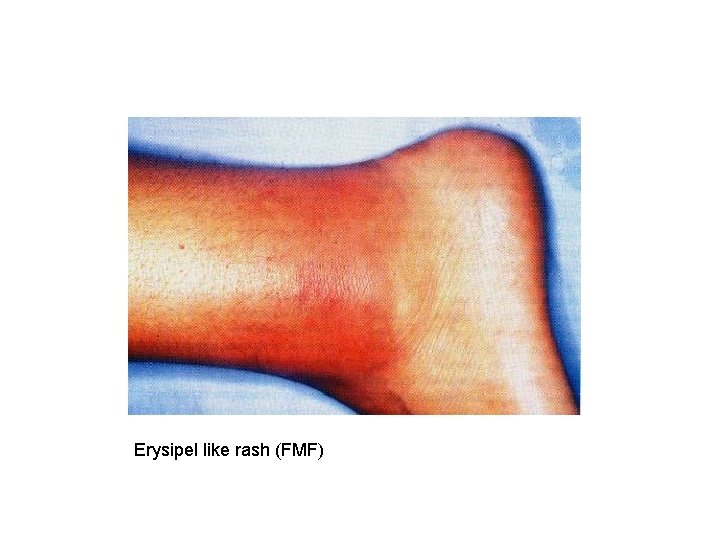
Erysipel like rash (FMF)

Acneiform lesions( behçet’s disease)
Purpura • purpura: vasculitis


Skin thickening • Scleroderma • Eosinophilic fasitis and eosinophilic myalgia syndrome.


Photosensitive skin eruption • Connective tissue diseases, SLE, DM. . . • Phototoxic drug allergies (sulfa, thiazid. . )
Oral ulcers • Behçet ‘s disase • Crohn disease • Spondyloarthropathies • SLE Genital ulcers n Behçets disease n Reactive arthritis


Sousage digits/Enthesopathy • Reactive arthritis • Psoriatic arthritis

Sousoge digits
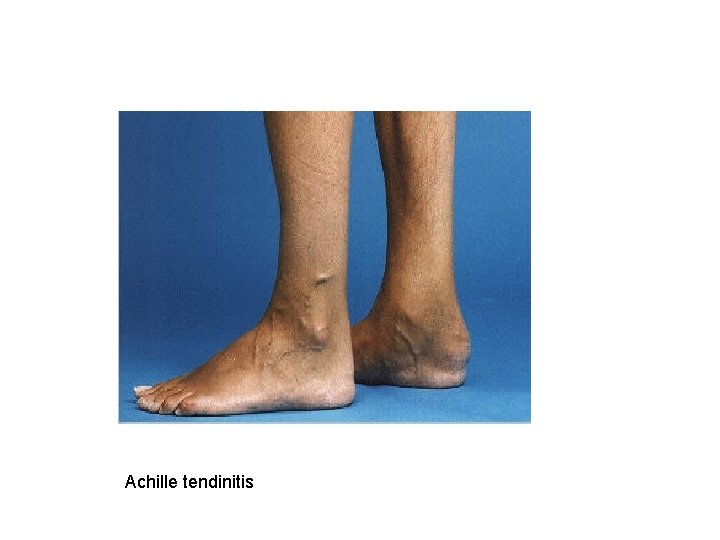
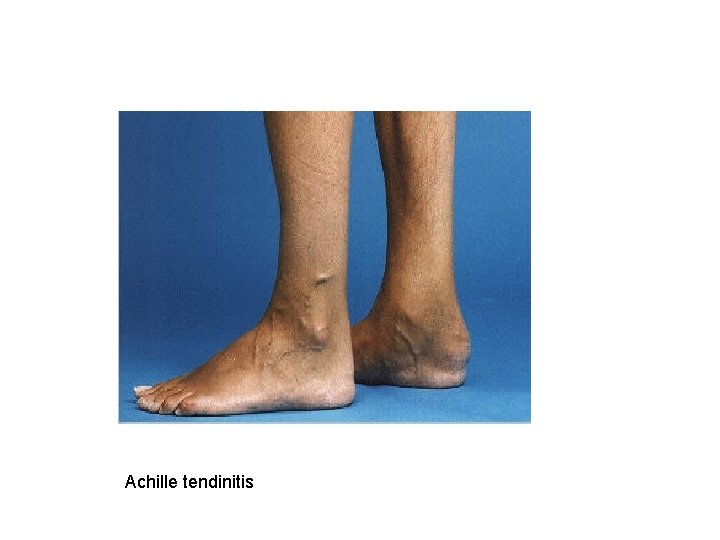
Achille tendinitis
Raynaud • Primary or secondary • Primary- female- %5 -8 • Secondary – connective tissue disorders • Scleroderma, SLE, SS, RA, DM/PM. . .

Fever, weight loss, malaise and arthritis
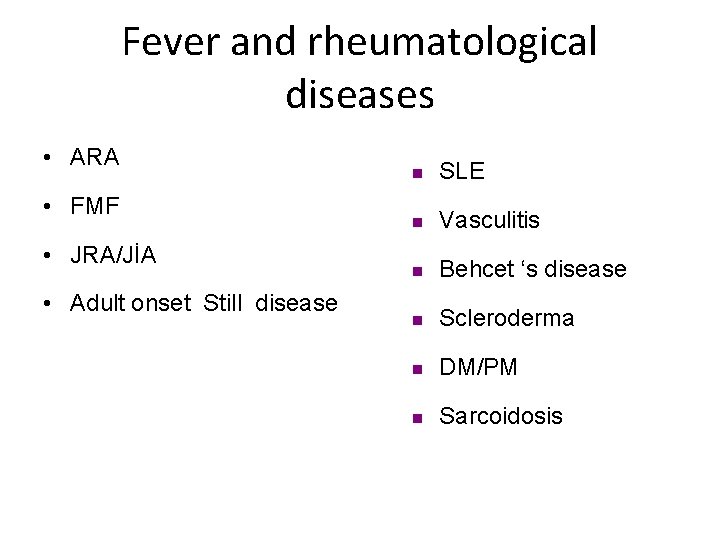
Fever and rheumatological diseases • ARA • FMF • JRA/JİA • Adult onset Still disease n SLE n Vasculitis n Behcet ‘s disease n Scleroderma n DM/PM n Sarcoidosis
Eye and arthritis
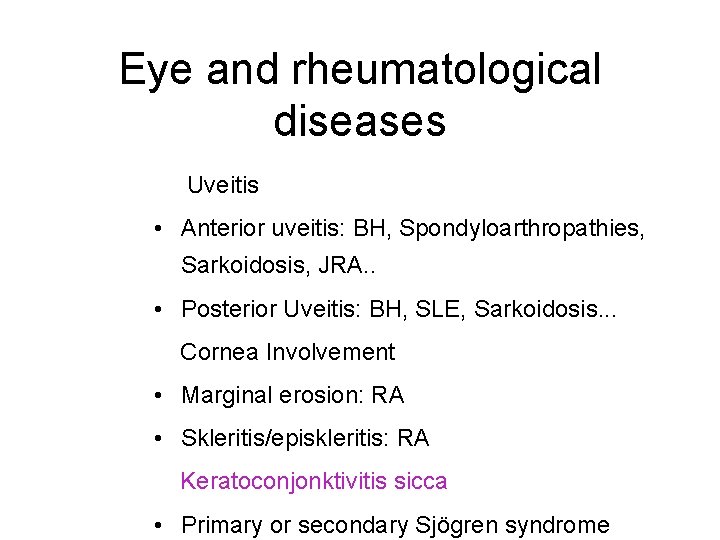
Eye and rheumatological diseases Uveitis • Anterior uveitis: BH, Spondyloarthropathies, Sarkoidosis, JRA. . • Posterior Uveitis: BH, SLE, Sarkoidosis. . . Cornea Involvement • Marginal erosion: RA • Skleritis/episkleritis: RA Keratoconjonktivitis sicca • Primary or secondary Sjögren syndrome
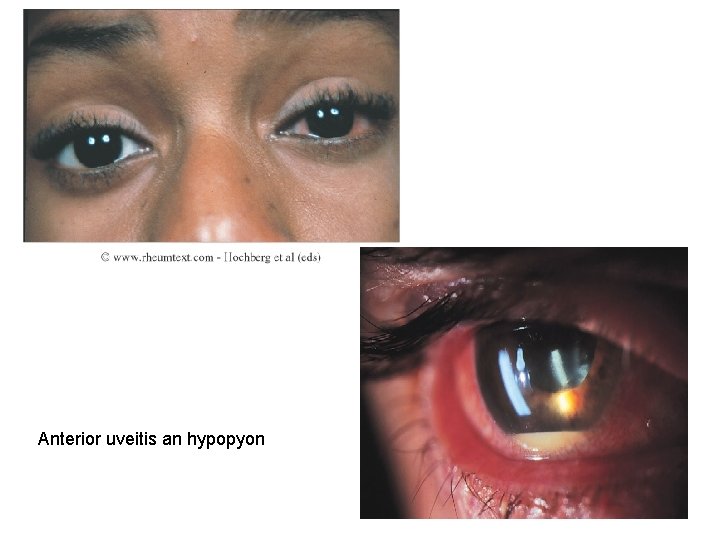
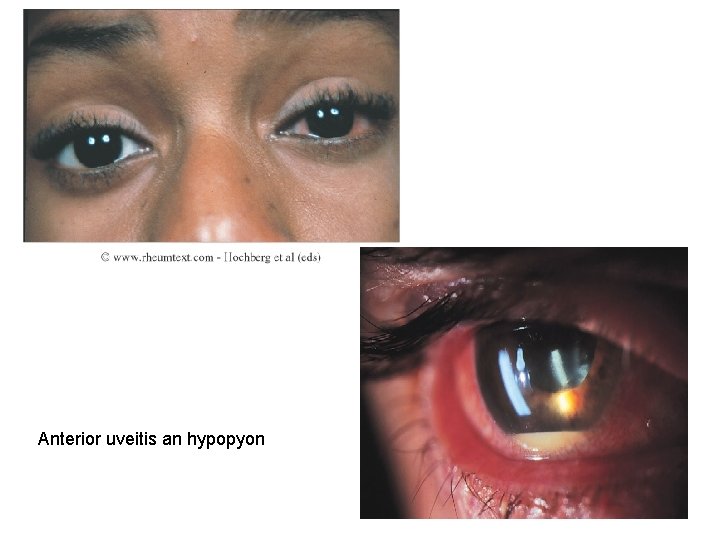
Anterior uveitis an hypopyon
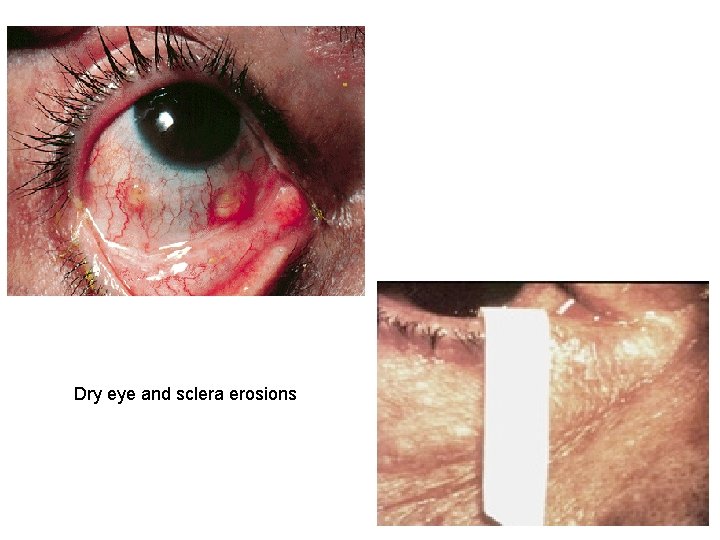
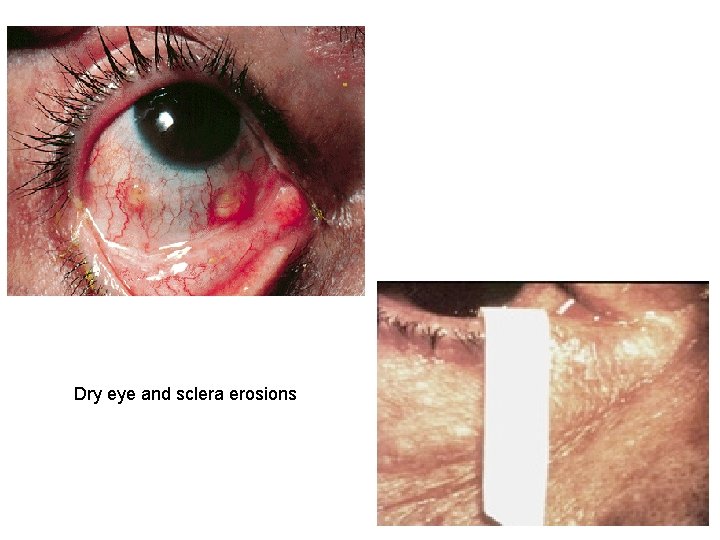
Dry eye and sclera erosions
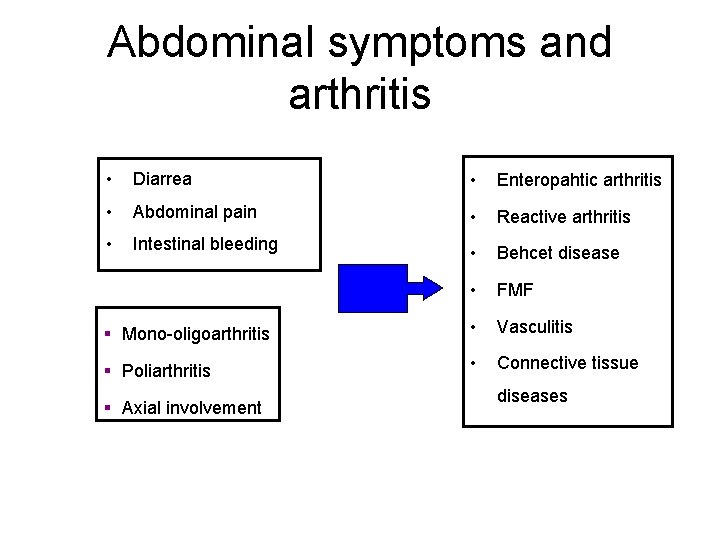
Abdominal symptoms and arthritis
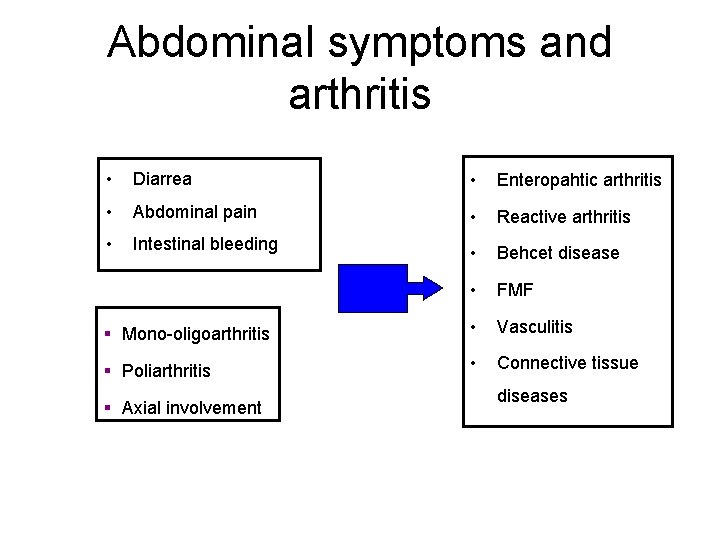
Abdominal symptoms and arthritis • Diarrea • Enteropahtic arthritis • Abdominal pain • Reactive arthritis • Intestinal bleeding • Behcet disease • FMF § Mono-oligoarthritis • Vasculitis § Poliarthritis • Connective tissue § Axial involvement diseases
 Design and patents act 1988
Design and patents act 1988 Insecticide act
Insecticide act Patrick j kelly free energy
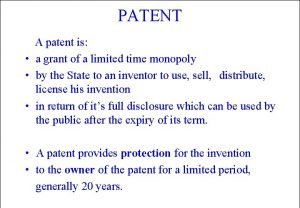
Patrick j kelly free energy Types of patents
Types of patents Patents
Patents Simproved harry potter world
Simproved harry potter world Advantages and disadvantages of patents
Advantages and disadvantages of patents What is the copyright designs and patents act 1988
What is the copyright designs and patents act 1988 Types of patent
Types of patent Barik meaning
Barik meaning Osteoarthritis morning stiffness
Osteoarthritis morning stiffness Nursing diagnosis for gouty arthritis
Nursing diagnosis for gouty arthritis Septic arthritis complications
Septic arthritis complications Gonorrhea
Gonorrhea Left knee arthritis
Left knee arthritis Arthritis treatment
Arthritis treatment Boutonniere and swan neck deformity
Boutonniere and swan neck deformity Eular recommendations psoriatic arthritis
Eular recommendations psoriatic arthritis Food allergies and arthritis
Food allergies and arthritis Extra articular manifestations of rheumatoid arthritis
Extra articular manifestations of rheumatoid arthritis Rheumatoid arthritis
Rheumatoid arthritis Soft tissue rheumatoid arthritis
Soft tissue rheumatoid arthritis Gardening with arthritis
Gardening with arthritis Sacroilitis
Sacroilitis Steinbrocker stage
Steinbrocker stage Zveren
Zveren Caprine arthritis encefalitis
Caprine arthritis encefalitis Anatomi fisiologi asam urat
Anatomi fisiologi asam urat Infusion therapy for arthritis
Infusion therapy for arthritis Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Peripheral arthritis
Peripheral arthritis Reiter's syndrome
Reiter's syndrome Bakgil
Bakgil Rheumatoid arthritis side effects
Rheumatoid arthritis side effects Septic arthritis antibiotics
Septic arthritis antibiotics Nongonococcal septic arthritis
Nongonococcal septic arthritis Arthritis in shoulder nhs
Arthritis in shoulder nhs Septic workup
Septic workup Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Rheumatoid arthritis nursing management
Rheumatoid arthritis nursing management Kode icd 10 dystonia
Kode icd 10 dystonia Septic arthritis complications
Septic arthritis complications Rehaklinik psoriasis arthritis
Rehaklinik psoriasis arthritis B t cells
B t cells Gout treatment
Gout treatment Eular criteria for ra
Eular criteria for ra Poststreptococcal reactive arthritis
Poststreptococcal reactive arthritis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Arthritis foundation indiana
Arthritis foundation indiana Arthritis and food allergies
Arthritis and food allergies Psoriasis arthritis nhs
Psoriasis arthritis nhs Z line deformity
Z line deformity Viral arthritis
Viral arthritis Pauciarticular juvenile rheumatoid arthritis
Pauciarticular juvenile rheumatoid arthritis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis What is subluxation
What is subluxation Narbentypen
Narbentypen Septic arthritis antibiotics
Septic arthritis antibiotics Kode icd 10 fraktur vertebra thorakal
Kode icd 10 fraktur vertebra thorakal Seronegative arthritis
Seronegative arthritis Multiple conflict
Multiple conflict Tony wagner's seven survival skills
Tony wagner's seven survival skills Comparison between virtual circuit and datagram network
Comparison between virtual circuit and datagram network Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Research approaches definition
Research approaches definition Waterfall vs shower approach
Waterfall vs shower approach Diagram for traditional approach
Diagram for traditional approach