Anatomy Physiology Lesson 12 THE MALE REPRODUCTIVE SYSTEM
- Slides: 64
Anatomy & Physiology Lesson 12
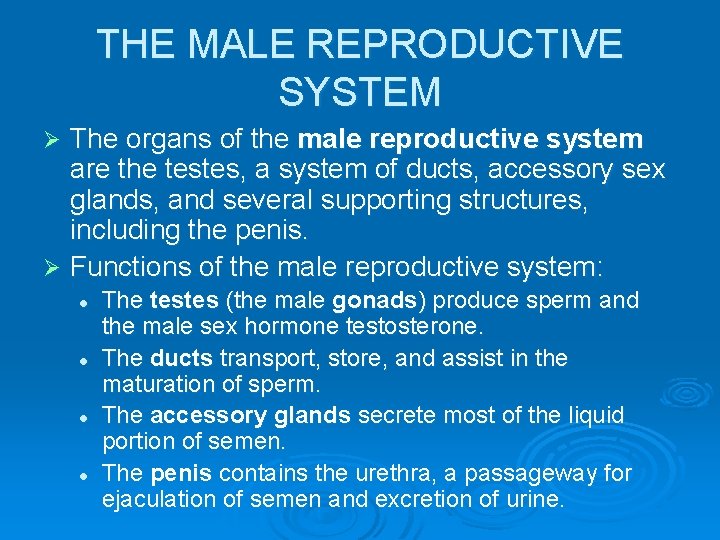
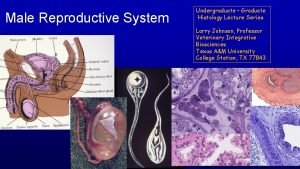
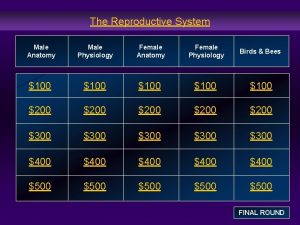
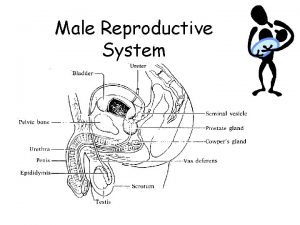
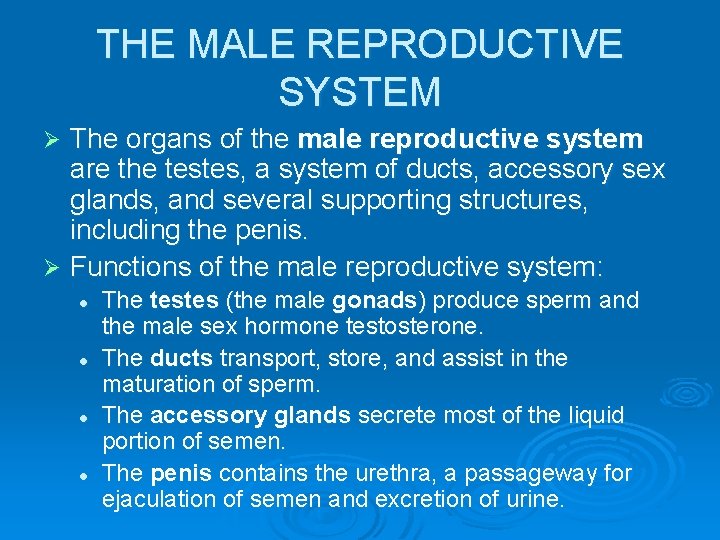
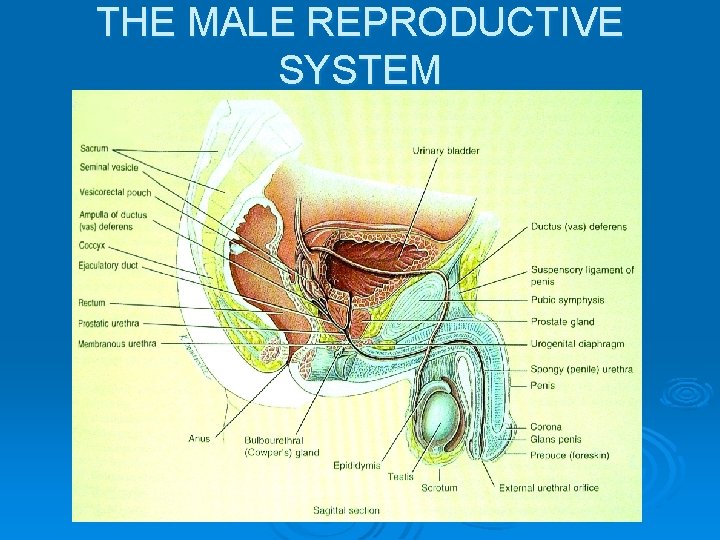
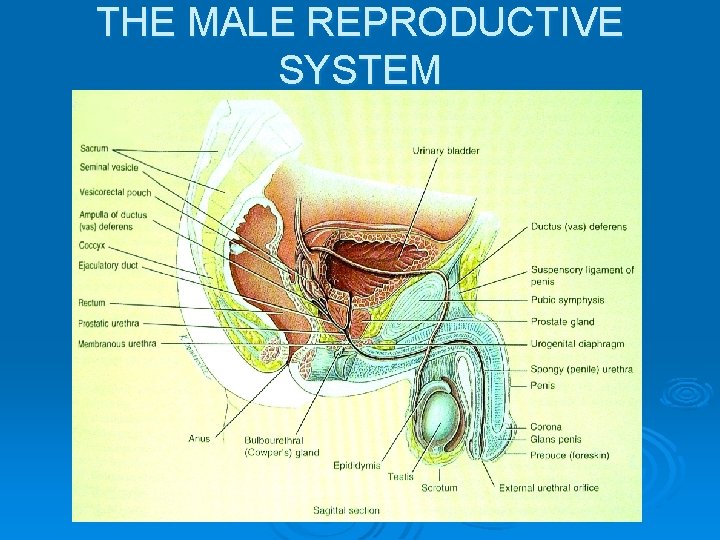
THE MALE REPRODUCTIVE SYSTEM The organs of the male reproductive system are the testes, a system of ducts, accessory sex glands, and several supporting structures, including the penis. Ø Functions of the male reproductive system: Ø l l The testes (the male gonads) produce sperm and the male sex hormone testosterone. The ducts transport, store, and assist in the maturation of sperm. The accessory glands secrete most of the liquid portion of semen. The penis contains the urethra, a passageway for ejaculation of semen and excretion of urine.
THE MALE REPRODUCTIVE SYSTEM
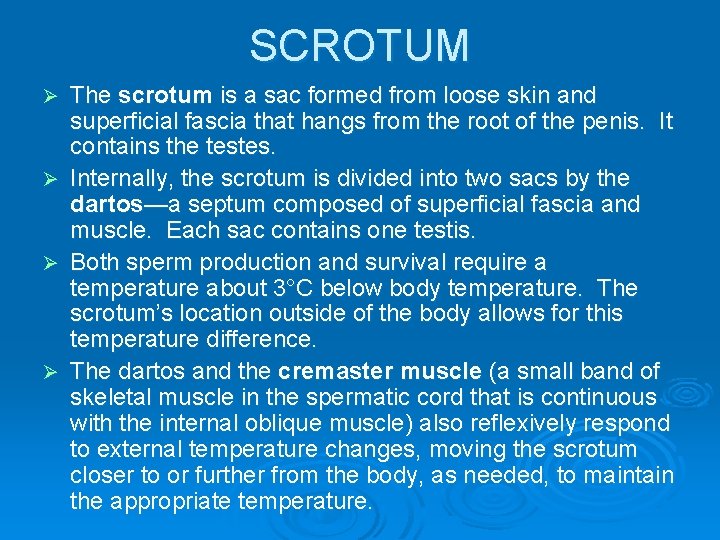
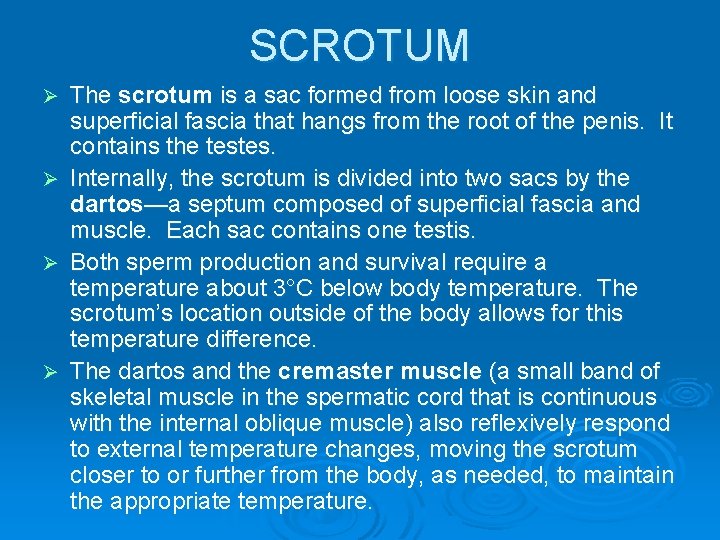
SCROTUM The scrotum is a sac formed from loose skin and superficial fascia that hangs from the root of the penis. It contains the testes. Ø Internally, the scrotum is divided into two sacs by the dartos—a septum composed of superficial fascia and muscle. Each sac contains one testis. Ø Both sperm production and survival require a temperature about 3°C below body temperature. The scrotum’s location outside of the body allows for this temperature difference. Ø The dartos and the cremaster muscle (a small band of skeletal muscle in the spermatic cord that is continuous with the internal oblique muscle) also reflexively respond to external temperature changes, moving the scrotum closer to or further from the body, as needed, to maintain the appropriate temperature. Ø
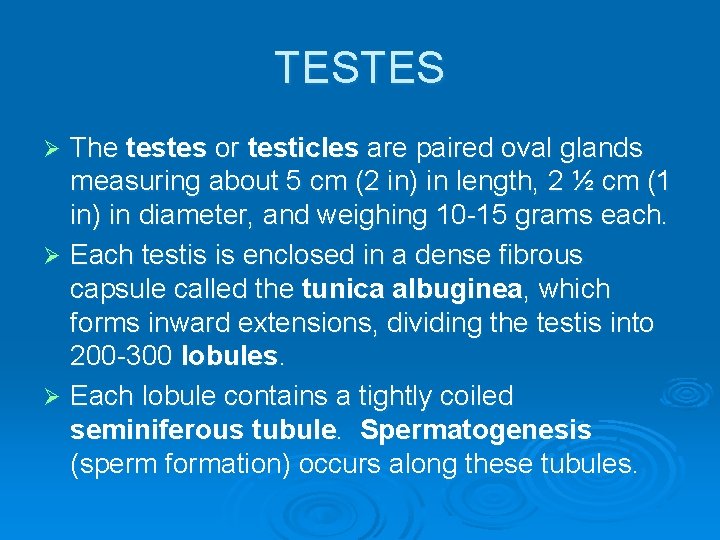
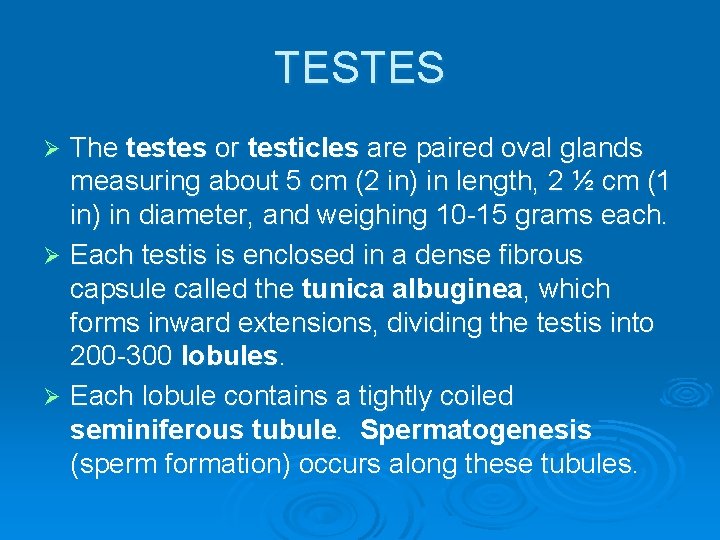
TESTES The testes or testicles are paired oval glands measuring about 5 cm (2 in) in length, 2 ½ cm (1 in) in diameter, and weighing 10 -15 grams each. Ø Each testis is enclosed in a dense fibrous capsule called the tunica albuginea, which forms inward extensions, dividing the testis into 200 -300 lobules. Ø Each lobule contains a tightly coiled seminiferous tubule. Spermatogenesis (sperm formation) occurs along these tubules. Ø
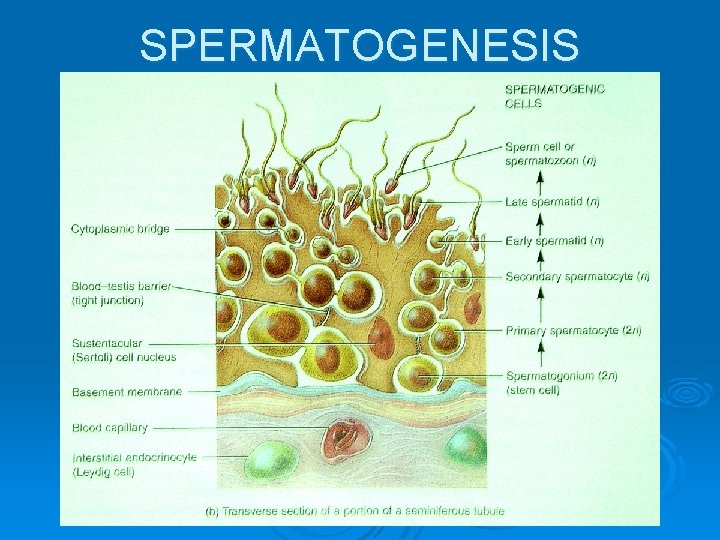
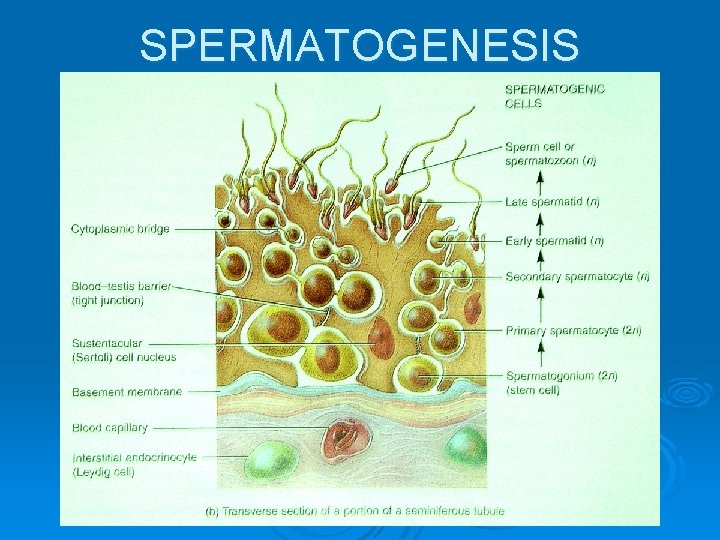
SPERTMATOGENIC CELLS Sperm-forming spermatogenic cells, together with supporting cells, line the seminiferous tubules. Ø The most immature spermatogenic cells are called spermatogonia. They lie next to the basement membrane. Ø Toward the lumen of the tubule are progressively more mature cells (primary spermatocytes, secondary spermatocytes, spermatids, and sperm). Ø Nearly mature sperm cells or spermatozoa are released into the lumen of the seminiferous tubule. Ø
SUPPORTING CELLS Embedded among the spermatogenic cells are sustentacular cells (Sertoli cells). These cells form tight junctions around the spermatogenic cells, forming the blood-testis barrier. To reach the developing gametes, substances must first pass through the sustentacular cells, which is vitally important, since the spermatogenic cells have surface antigens which would otherwise be recognized as foreign and destroyed by the immune system. Ø Sustentacular cells support, protect, and nourish developing sperm cells. They also help to oversee many aspects of the spermatogenic process. Ø In the spaces between adjacent seminiferous tubules are clusters of interstitial endocrinocytes or Leydig cells, which secrete testosterone, the most important androgen (male sex hormone). Ø
SPERMATOGENESIS Spermatogenesis takes about 74 days. Ø Spermatogonia are diploid stem cells that undergo mitosis. Some of the daughter cells remain near the basement membrane to later undergo mitosis and sperm production. Ø Other daughter cells move away from the basement membrane of the seminiferous tubule, undergo differentiation, and become primary spermatocytes, which are still diploid cells. Ø
SPERMATOGENESIS In reduction division (meiosis I), each primary spermatocyte divides to become two haploid secondary spermatocytes. Each chromosome within a secondary spermatocyte, however, is still composed of two chromatids (copies of the DNA). This is the phase when crossing-over and recombination occurs to create genetically unique daughter cells. Ø The second nuclear division is equatorial division (meiosis II), during which each secondary spermocyte again divides to produce two spermatids, each of which is haploid and possesses only one DNA copy. During spermatogenesis, the four daughter cells do not undergo complete cytoplasmic separation—they remain in constant contact with each other via cytplasmic bridges. Ø The final stage of spermatogenesis is spermiogenesis, during which the spermatids separate from each other and develop into mature sperm cells (spermatozoa). The release of a sperm cell from its contact with a sustentacular cell into the lumen of the seminiferous tubule is known as spermiation. Ø
SPERMATOGENESIS
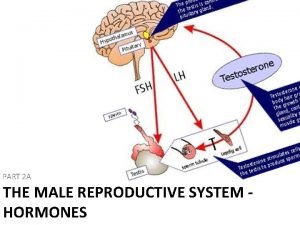
HORMONAL CONTROL OF SPERMATOGENESIS At puberty the hypothalamus releases gonadotropin releasing hormone (Gn. RH). Ø This stimulates the anterior pituitary gland to increase secretion of luteinizing hormone (LH) and follicle-stimulation hormone (FSH). Ø LH stimulates the interstitial endocrinocytes (Leydig cells) to secrete testosterone. The enzyme 5 alpha-reductase in some target cells converts testosterone into an even stronger androgen called dihydrotestosterone (DHT). Ø
HORMONAL CONTROL OF SPERMATOGENESIS FSH acts synergistically with testosterone on the sustentacular cells to produce a protein called androgen-binding protein (ABP), which binds with testosterone, maintaining high levels of testosterone in the seminiferous tubules, so spermatogenesis can reach completion. Ø The sustentacular cells secrete inhibin which acts on the anterior pituitary to inhibit FSH stimulation. The release of inhibin regulates the rate of spermatogenesis. Ø
EFFECTS OF ANDROGENS Ø Both androgens (testosterone and DHT) bind to the same receptors in the nuclei of target cells. The resulting hormone-receptor complex acts to turn on the transcription of some genes and turn of the transcription of others. Effects of these changes in gene activity include: l l Development—Testosterone stimulates development of the male reproductive system and is converted in the brain to estrogens, which may play a masculinizing role in the development of certain regions of the male brain. DHT stimulates development of the external genitalia. Sexual characteristics—Testosterone and DHT cause development and enlargement of the male sex organs and the development of masculine secondary sexual characteristics. Sexual functions—Androgens contribute to male sexual behavior, spermatogenesis, and sex drive (in both males and females). Metabolism—Androgens are anabolic hormones that stimulate protein synthesis, resulting in heavier muscle and bone mass in most men. They also stimulate closure of the epiphyseal plates.
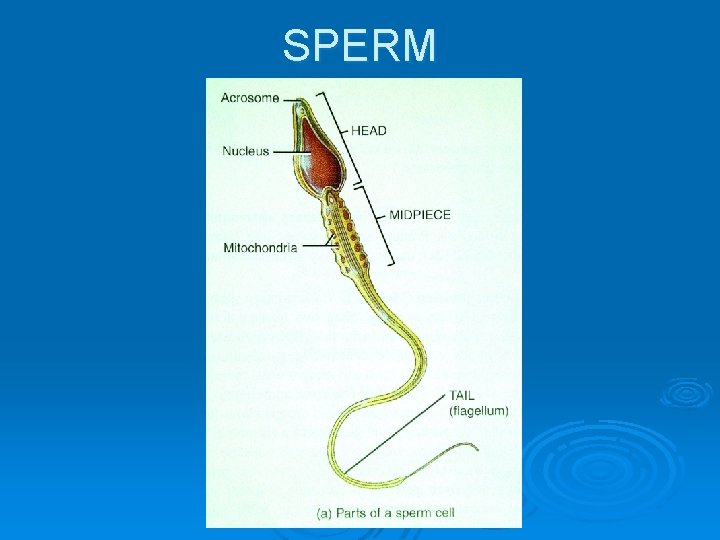
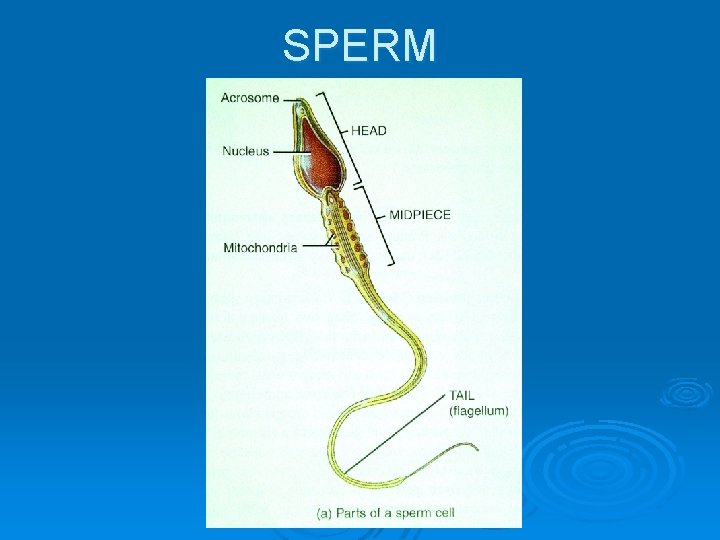
SPERM About 300 million sperm reach maturity each day. Ø They usually survive no more than 48 hours in the female reproductive tract. Ø Each sperm cell is composed of: Ø l l l A head—contains the nuclear material (DNA) and a lysosome-like structure called an acrosome, which contains enzymes that allow to the sperm cell to penetrate a secondary oocyte (ovum). A midpiece—contains many mitochondria, which carry on metabolism and provide ATP for locomotion. A tail—a flagellum which propels the sperm cell.
SPERM
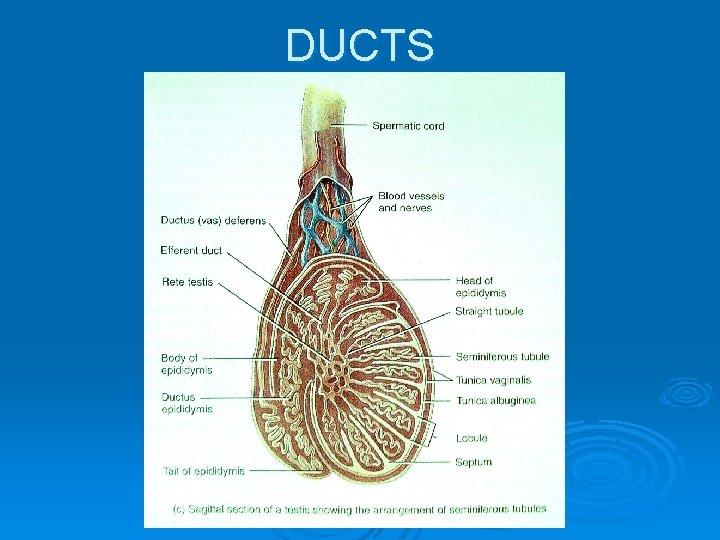
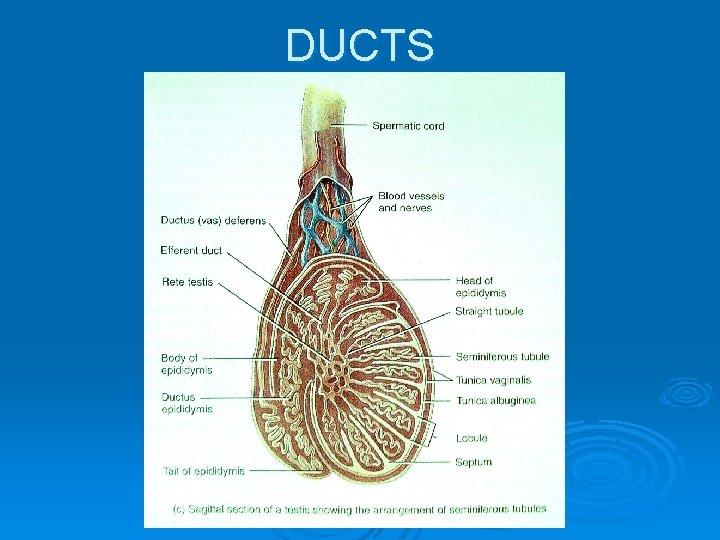
DUCTS Following their release into the lumen, sperm and fluid flow through the seminiferous tubules to the straight tubules. The sperm are propelled forward by pressure from newly forming fluid and sperm behind them. The fluid is produced by sustentacular cells. Ø The straight tubules lead to a testicular network of ducts called the rete testis which lead toward the epididymis. Ø In the epididymis the sperm move through a series of efferent ducts and eventually empty into a single tube called the ductus epididymis. Sperm maturation occurs over a 10 -14 day period in the ductus epididymous and may be stored here for a month or more. Peristaltic contraction of the ductus epididymis helps propel sperm into the ductus (vas) deferens. Ø
DUCTS The ductus (vas) deferens is about 45 cm (18 in) long. It ascends along the posterior border of the epididymis, passes through the inguinal canal, enters the pelvic cavity, loops over the ureter, and travels down the posterior surface of the urinary bladder. The dilated terminal portion of the vas deferens is called the ampulla. Ø The ductus deferens stores sperm for up to several months. Peristaltic contractions of its muscular coat helps to propel sperm toward the urethra. Ø
DUCTS The ejaculatory duct is located posterior to the bladder where the seminal vesicle and the ampulla of the ductus deferens join. It ejects sperm and secretions of the seminal vesicle into the urethra just prior to ejaculation. Ø The male urethra is the shared terminal duct of the reproductive and urinary systems. It serves as a passageway for both semen (a mixture of sperm and various fluids) and urine. It passes through the prostate gland, the urogenital diaphragm, and the penis and is subdivided into the prostatic urethra, the membranous urethra, and the spongy (penile) urethra. It terminates at the external urethral orifice. Ø
DUCTS
ACCESSORY SEX GLANDS Ø The accessory sex glands secrete most of the liquid portion of semen. These include: l The paired seminal vesicles, convoluted pouch-like structures that lie at the base of the urinary bladder and rectum. They secrete an alkaline, viscous fluid that contains fructose (used for ATP production by sperm), prostaglandins (contribute to sperm motility and viability), and semenogelin (a protein that causes coagulation of semen after ejaculation). This fluid helps to neutralize the acidic environment in the female reproductive tract and constitutes about 60% of the volume of semen.
ACCESSORY SEX GLANDS l l The single, doughnut-shaped prostate gland is found inferior to the urinary bladder and surrounds the prostatic urethra. It secretes a milky, slightly acidic fluid into the urethra through many prostatic ducts. Prostatic fluid contains citrate (used by sperm for ATP production), acid phosphatase (function unknown), and several proteolytic enzymes (liquify coagulated semen). Secretions of the prostate gland compose about 25% of semen volume and contribute to sperm motility and viability. The paired bulbourethral or Cowper’s glands are each about the size of a pea, lie inferior to the prostate gland, and have ducts that open into the spongy urethra. During sexual arousal, the bulbourethral glands prepare the way for the safe passage of sperm by secreting an alkaline substance that neutralizes acids in the urethra and mucus that lubricates the end of the penis.
SEMEN Ø Ø Ø Semen is a mixture of sperm and seminal fluid. The average volume of semen in an ejaculation is 2 ½-5 ml, with a sperm count of 50 -150 million sperm/ml. (A sperm count below 20 million/ml indicates probably infertility. ) Semen is slightly alkaline, has a milky appearance, and a sticky consistency. It provides sperm with a transportation medium and nutrients, and neutralizes the hostile acidic environment of the male urethra and female vagina. Semen contains an antibiotic called seminoplasmin that can destroy certain bacteria. Once ejaculated, liquid semen coagulates within 5 minutes, then reliquifies within 10 -20 minutes. Abnormal or delayed reliquification may cause complete or partial immobilization of sperm.
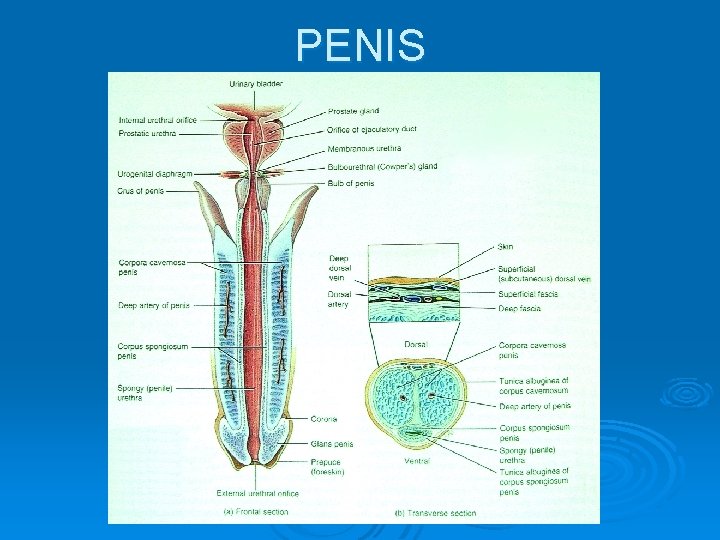
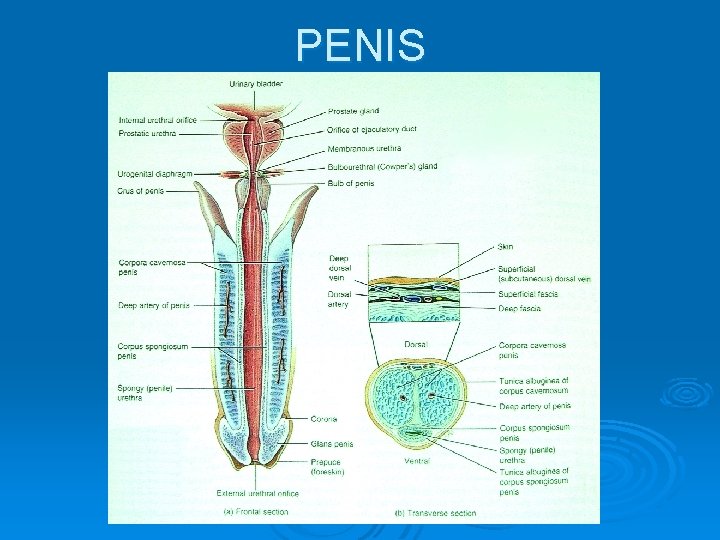
PENIS The penis contains the urethra, is cylindrical in shape, and consists of a body, root, and glans penis. Ø The body is composed of three cylindrical masses of tissue, each surrounded by fibrous tissue called the tunica albuginea. Ø l l The paired dorsolateral masses are called the corpora cavernosa penis. The smaller midventral mass, the corpus spongiosum penis, contains the spongy urethra and keeps the spongy urethra open during ejaculation. All three masses consist of erectile tissue permeated by blood sinuses and enclosed by fascia and skin. Ø With sexual stimulation, the arteries supplying the penis dilate and large amounts of blood fill the sinuses, compressing the veins that drain the penis. These vascular changes result in an erection, a parasympathetic reflex. Ø
PENIS Ejaculation is a sympathetic reflex. As part of this reflex, the smooth muscle sphincter at the base of the urinary bladder closes, preventing urine from being expelled during ejaculation or sperm from entering the bladder. Ø Even before ejaculation occurs, peristaltic contractions of the ampulla, seminal vesicles, ejaculatory ducts, and prostate gland propel semen into the spongy urethra, which usually leads to the discharge of a small amount of semen prior to ejaculation. This is called emission. Ø
PENIS Ø The root of the penis is the proximal, attached portion. It consists of: l l The bulb of the penis—the expanded portion at the base of the corpus spongiosum penis. The crura of the penis—the two separated and tapered portions of the corpora cavernosa penis. The bulb is attached to the inferior surface of the urogenital diaphragm and enclosed by the bulbospongiosus muscle. Ø Each crus is attached to the ischial and inferior rami and surrounded by the ischiocavernosus muscle. Contraction of these muscles aids in ejaculation. Ø
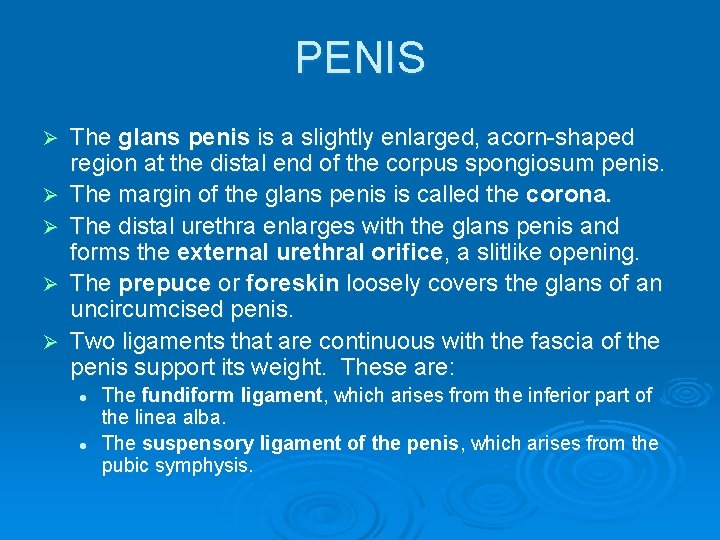
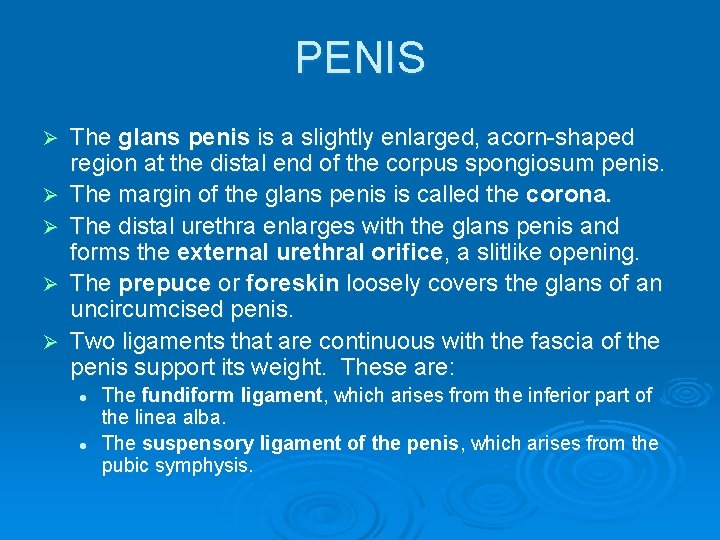
PENIS Ø Ø Ø The glans penis is a slightly enlarged, acorn-shaped region at the distal end of the corpus spongiosum penis. The margin of the glans penis is called the corona. The distal urethra enlarges with the glans penis and forms the external urethral orifice, a slitlike opening. The prepuce or foreskin loosely covers the glans of an uncircumcised penis. Two ligaments that are continuous with the fascia of the penis support its weight. These are: l l The fundiform ligament, which arises from the inferior part of the linea alba. The suspensory ligament of the penis, which arises from the pubic symphysis.
PENIS
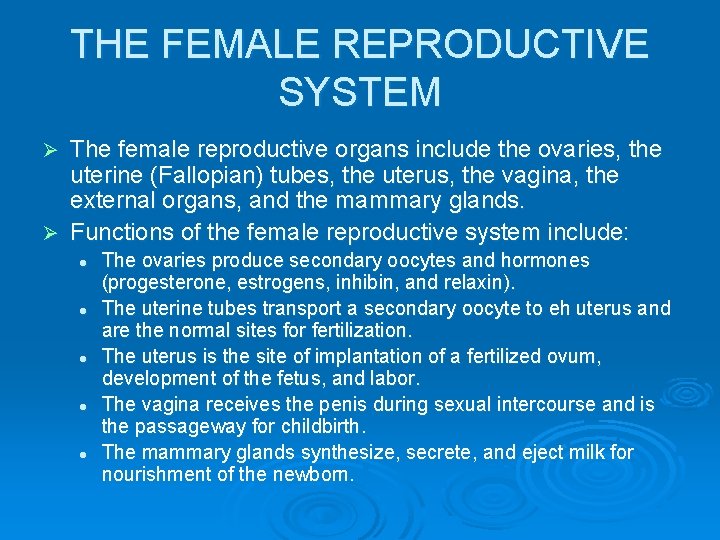
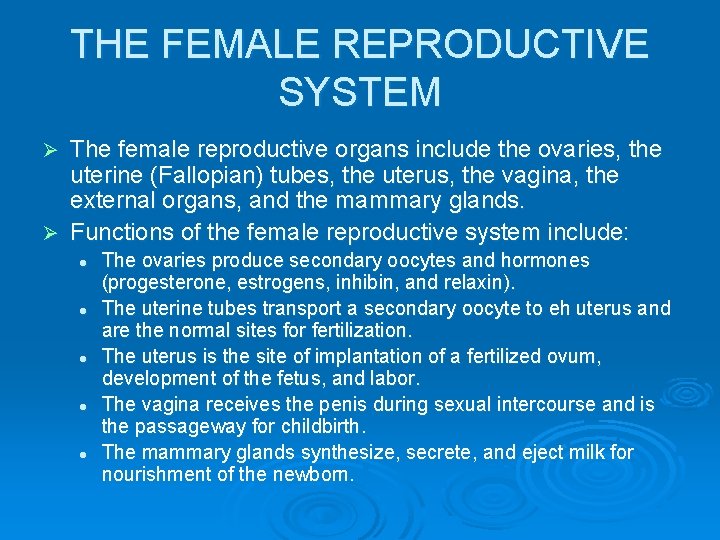
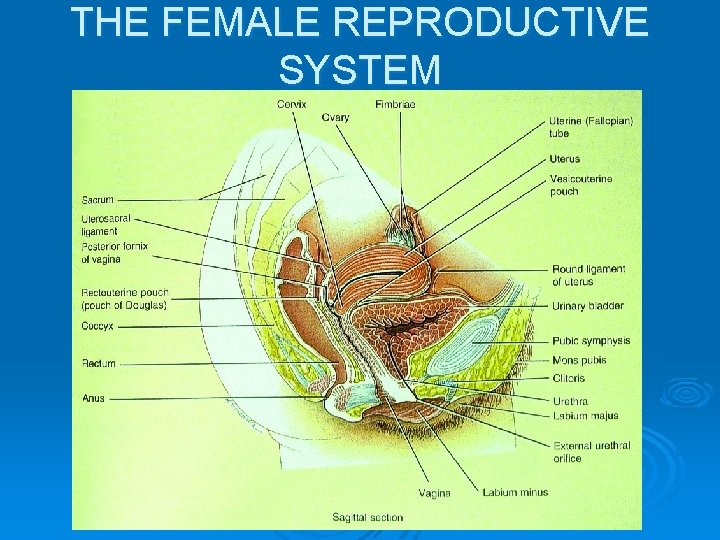
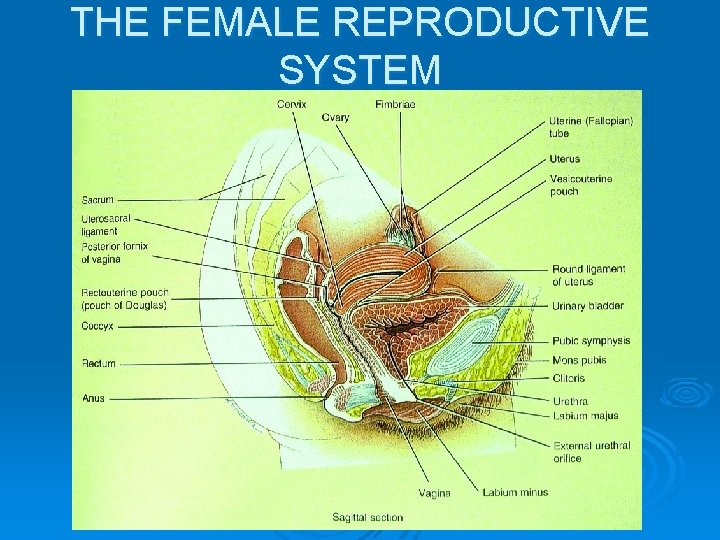
THE FEMALE REPRODUCTIVE SYSTEM The female reproductive organs include the ovaries, the uterine (Fallopian) tubes, the uterus, the vagina, the external organs, and the mammary glands. Ø Functions of the female reproductive system include: Ø l l l The ovaries produce secondary oocytes and hormones (progesterone, estrogens, inhibin, and relaxin). The uterine tubes transport a secondary oocyte to eh uterus and are the normal sites for fertilization. The uterus is the site of implantation of a fertilized ovum, development of the fetus, and labor. The vagina receives the penis during sexual intercourse and is the passageway for childbirth. The mammary glands synthesize, secrete, and eject milk for nourishment of the newborn.
THE FEMALE REPRODUCTIVE SYSTEM
OVARIES The ovaries or female gonads are paired glands that resemble unshelled almonds in shape and size. Ø They lie in the superior portion of the pelvic cavity, one on either side of the uterus. Ø A series of ligaments (the broad ligament, the ovarian ligament, and the suspensory ligament) hold the ovaries in position. Ø Each ovary contains a hilus, where blood vessels and nerves enter and exit the ovary and the mesovarium (a double-layered fold of peritoneum) is attached. Ø
OVARIES Ø Each ovary is composed of the following parts: l l l The germinal epithelium is a layer of simple epithelium that covers the surface of the ovary and is continuous with the mesothelium that covers the mesovarium. The tunica albuginea is a capsule of whitish, dense, irregular CT immediately deep to the germinal epithelium. The stroma is a region of CT deep to the tunica albuginea and composed of a superficial, dense layer called the cortex and a deep, loose layer called the medulla.
OVARIES l l l The ovarian follicles lie in the cortex and consist of oocytes in various stages of development, with their surrounding cells, which nourish a developing oocyte and begin to secrete estrogens as the follicle grows larger. When the surrounding cells form a single layer they are called follicular cells, but later in development, when they form several layers, they are termed granulosa cells. A mature (Graafian) follicle is a large, fluid-filled follicle that will soon rupture and expel a secondary oocyte in the process called ovulation. A corpus luteum contains the remnants of an ovulated mature follicle and produces progesterone, estrogens, relaxin, and inhibin until it degenerates into fibrous tissue, at which time it is called a corpus albicans.
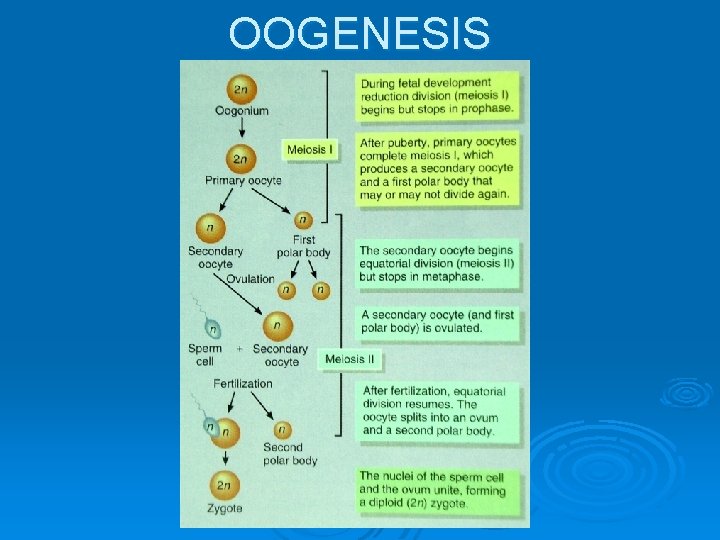
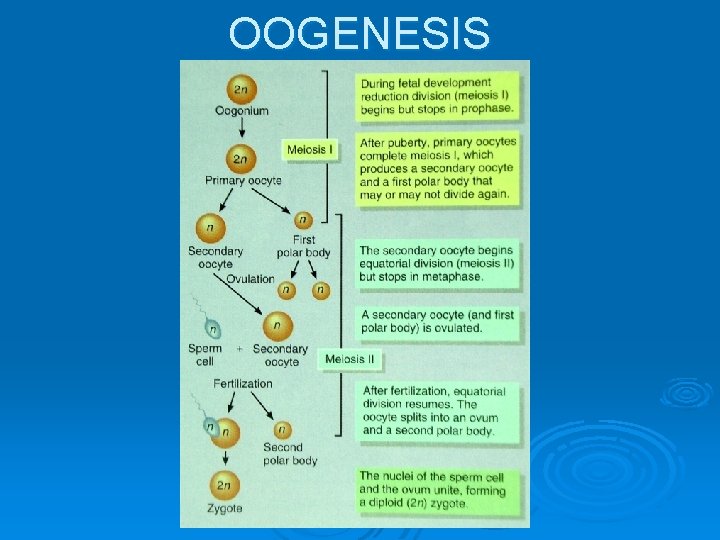
OOGENESIS Ø The formation of haploid secondary oocytes (gametes) in the ovaries is called oogenesis. l Reduction division (meiosis I)—During early fetal development germ cells within the ovaries differentiate into oogonia—diploid cells that divide mitotically to produce millions of germ cells. A few of these germ cells develop into larger cells called primary oocytes that enter the prophase of reduction division, but do not complete it until after puberty. After puberty, under the influence of the gonadotropin hormones secreted by the anterior pituitary gland each month, one primary oocyte completes reduction division, resulting in two haploid cells of unequal size, each with 23 chromosomes of two chromatids each. The larger cell, called the secondary oocyte receives most of the cytoplasm while the smaller cell, mostly consisting of discarded nuclear material, is called the first polar body. The secondary oocyte proceeds to the metaphase of equatorial division (meiosis II), then stops. The mature (Graafian) follicle in which these events are taking place will soon rupture and release its secondary oocyte.
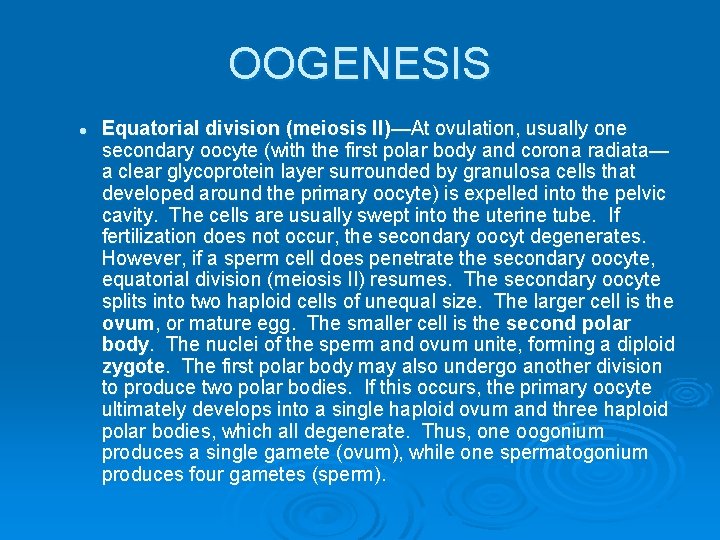
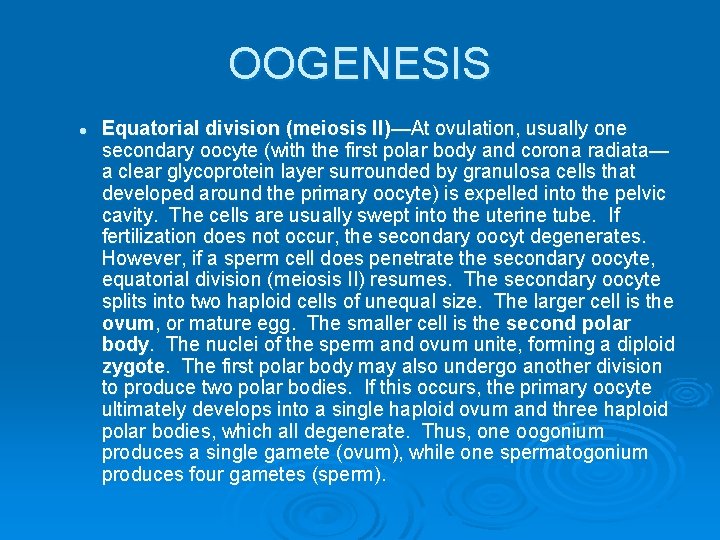
OOGENESIS l Equatorial division (meiosis II)—At ovulation, usually one secondary oocyte (with the first polar body and corona radiata— a clear glycoprotein layer surrounded by granulosa cells that developed around the primary oocyte) is expelled into the pelvic cavity. The cells are usually swept into the uterine tube. If fertilization does not occur, the secondary oocyt degenerates. However, if a sperm cell does penetrate the secondary oocyte, equatorial division (meiosis II) resumes. The secondary oocyte splits into two haploid cells of unequal size. The larger cell is the ovum, or mature egg. The smaller cell is the second polar body. The nuclei of the sperm and ovum unite, forming a diploid zygote. The first polar body may also undergo another division to produce two polar bodies. If this occurs, the primary oocyte ultimately develops into a single haploid ovum and three haploid polar bodies, which all degenerate. Thus, one oogonium produces a single gamete (ovum), while one spermatogonium produces four gametes (sperm).
OOGENESIS
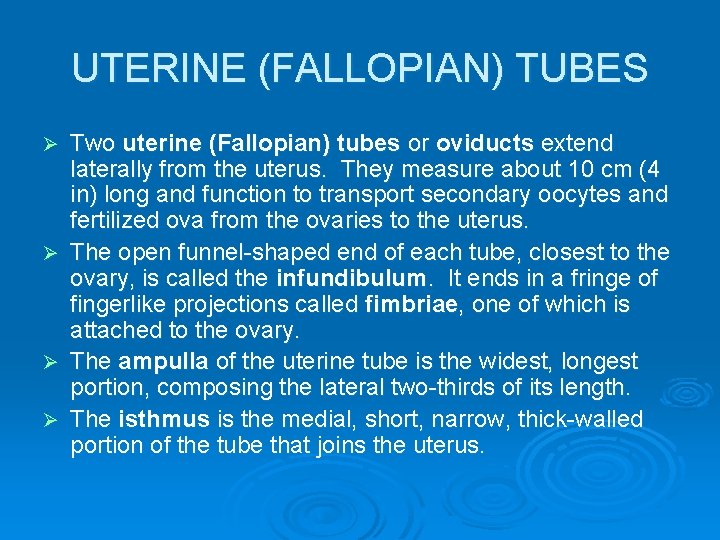
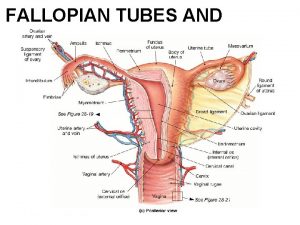
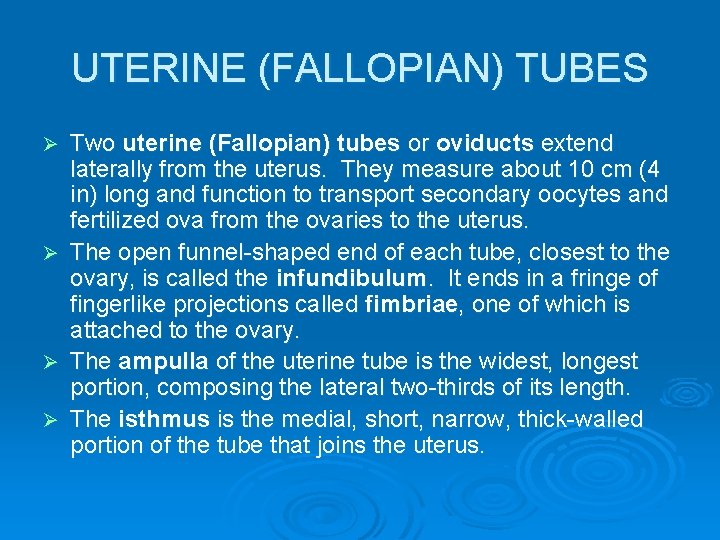
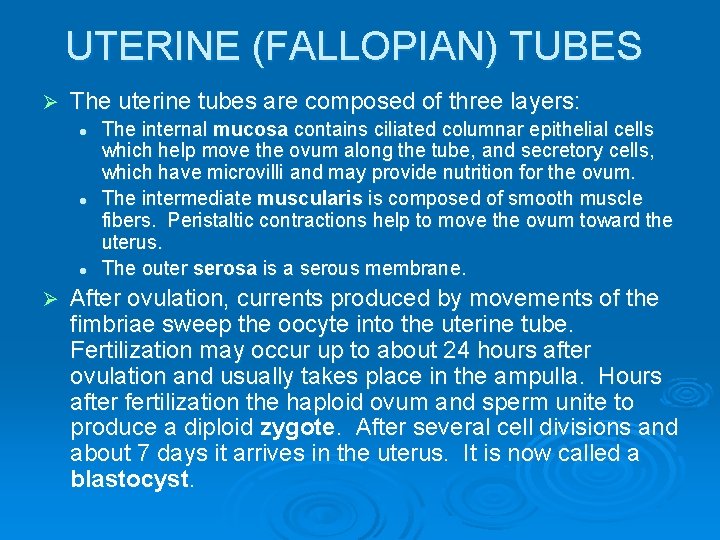
UTERINE (FALLOPIAN) TUBES Two uterine (Fallopian) tubes or oviducts extend laterally from the uterus. They measure about 10 cm (4 in) long and function to transport secondary oocytes and fertilized ova from the ovaries to the uterus. Ø The open funnel-shaped end of each tube, closest to the ovary, is called the infundibulum. It ends in a fringe of fingerlike projections called fimbriae, one of which is attached to the ovary. Ø The ampulla of the uterine tube is the widest, longest portion, composing the lateral two-thirds of its length. Ø The isthmus is the medial, short, narrow, thick-walled portion of the tube that joins the uterus. Ø
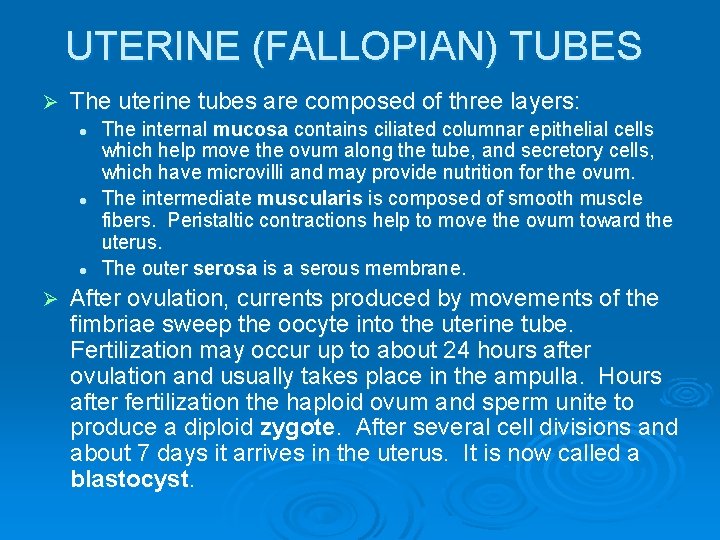
UTERINE (FALLOPIAN) TUBES Ø The uterine tubes are composed of three layers: l l l Ø The internal mucosa contains ciliated columnar epithelial cells which help move the ovum along the tube, and secretory cells, which have microvilli and may provide nutrition for the ovum. The intermediate muscularis is composed of smooth muscle fibers. Peristaltic contractions help to move the ovum toward the uterus. The outer serosa is a serous membrane. After ovulation, currents produced by movements of the fimbriae sweep the oocyte into the uterine tube. Fertilization may occur up to about 24 hours after ovulation and usually takes place in the ampulla. Hours after fertilization the haploid ovum and sperm unite to produce a diploid zygote. After several cell divisions and about 7 days it arrives in the uterus. It is now called a blastocyst.
UTERUS The uterus forms part of the pathway for sperm to reach the uterine tubes, and is the site of menstruation, fetal development, and labor. Ø It is located between the urinary bladder and the rectum and is about the size and shape of an inverted pear. Ø It measures about 7 ½ cm (3 in) long, 5 cm (2 in) wide, and 2 ½ cm (1 in) thick in a woman who has never been pregnant. It is larger in a woman has recently been pregnant and smaller (atrophied) in a woman whose female sex hormone levels are low (as when taking BCP or after menopause). Ø
UTERUS Ø Anatomically, the uterus is divided into: l l l The fundus—dome-shaped superior to the uterine tubes. The body—major tapering central portion of the uterus. The cervix—the inferior narrow portion opening into the vagina. The secretory cells of the cervical mucosa produce cervical mucus, a mixture of water, glycoprotein, serumtype proteins, lipids, enzymes, and inorganic salts. At or near the time of ovulation cervical mucus becomes thinner, more alkaline, and more receptive to sperm. At other times, it forms a plug that impedes the penetration of sperm into the cervix. Ø Both the cervix and mucus serve as a reservoir for sperm, protect sperm from the hostile vaginal environment, and protect sperm from phagocytes. Ø
UTERUS The constricted isthmus is located between the cervis and the body of the uterus. Ø The interior of the body of the uterus is called the uterine cavity. Ø The interior of the cervix is called the cervical canal, which opens into the uterine cavity at the internal os and int the vagina at the external os. Ø Normally, the uterus bends anteriorly over the urinary bladder at the junction between the cervix and the body. This is called anteflexion. Ø The uterus is held in position, with some room for movement, by the paired broad ligaments, uterosacral ligaments, cardinal (lateral cervical) ligaments, and round ligaments. Ø
UTERUS Ø The uterus consists of three layers: l l l The outer perimetrium or serosa is part of the visceral peritoneum. The middle myometrium consists of three layers of smooth muscle fibers and forms the bulk of the uterine wall, which is thickest in the fundus and thinnest in the cervix. The inner endometrium is highly vascularized and divided into two layers: • The stratum functionalis, the layer closer to the uterine cavity, is shed during menstruation. • The stratum basalis, the deeper layer, is permanent and gives rise to a new stratum functionalis after each menstruation.
VAGINA The vagina serves as a passageway for menstrual flow and childbirth and receives semen from the penis during sexual intercourse. Ø It is a tubular, fibromuscular organ lined with mucous membrane and measuring about 10 cm (4 in) in length. Ø It is situated between the urinary bladder and the rectum, is directed superiorly and posteriorly, and attaches to the uterus. Ø A recess called the fornix surrounds the attachment to the cervix. Ø
VAGINA Ø Ø Ø The mucosa of the vagina is continuous with that of the uterus. It consists of nonkeratinized stratified squamous epithelium and areolar CT that lies in a series of transverse folds called rugae. The vaginal mucosa contains large stores of glycogen, which decompose to produce organic acids. The resulting low p. H environment retards microbial growth, but is also hostile to sperm. The muscularis is very stretchy to receive the penis during sexual intercourse and allow for childbirth. The adventitia is composed of areolar CT and anchors the vagina to adjacent organs. Near the vaginal orifice (the opening to the exterior) may be a thin fold of vascularized mucous membrane called the hymen, which may form a partial border around the orifice.
VULVA Ø The term vulva or pudendum refers to the external genitalia of the female. Its components are: l l Mons pubis—An elevation of adipose tissue located anterior to vaginal and urethral openings. It is covered by skin and pubic hair and cushions the pubic symphysis. Labia majora—Two longitudinal folds of skin extend inferiorly and posteriorly from the mons pubis. They are covered with pubic hair and contain an abundance of adipose tissue, sebaceous glands, and apocrine glands.
VULVA l l Labia minora—Two smaller folds of skin lie medial to the labia majora. The labia minora do not have pubic hair or fat and have very few sudoriferous glands. They do contain many sebaceous glands, however. Clitoris—A small, cylindrical mass of erectile tissue and nerves located at the anterior junction of the labia minora. A layer of skin called the prepuce is formed where the labia minora meet and covers the body of the clitoris. The glans is the exposed portion of the clitoris. The clitoris is capable of enlargement upon tactile stimulation and plays a role in sexual excitement in the female.
VULVA l Vestibule—The region between the labia minora, containing the hymen (if present), vaginal orifice, external urethral orifice, and the openings of several ducts. The bulb of the vestibule consists of two masses of erectile tissue just deep to the labia on either side of the vaginal orifice. The bulb becomes engorged with blood during sexual arousal, narrowing the vaginal orifice and placing pressure on the penis. Between the vaginal orifice and the clitoris is the external urethral orifice, the opening to the urethra. On either side of the external urethral orifice are the duct openings of the paraurethral (Skene’s) glands, which are embedded in the wall of the urethra and secrete mucus. On either side of the vaginal orifice are the greater vestibular (Barholin’s) glands. These glands open by ducts into grooves between the hymen and labia minora and produce a small amount of mucus during sexual arousal and intercourse. Several lesser vestibular glands also open into the vestibule.
PERINEUM The perineum is the diamond-shaped area medial to the thighs and buttocks of both males and females. It contains the external genitalia and anus. Ø It is bounded anteriorly by the pubic symphysis, laterally by the ischial tuberosities, and posteriorly by the coccyx. Ø A transverse line between the ischial tuberosities divides the perineum into an anterior urogenital triangle (containing the external genitalia) and a posterior anal triangle (containing the anus). Ø
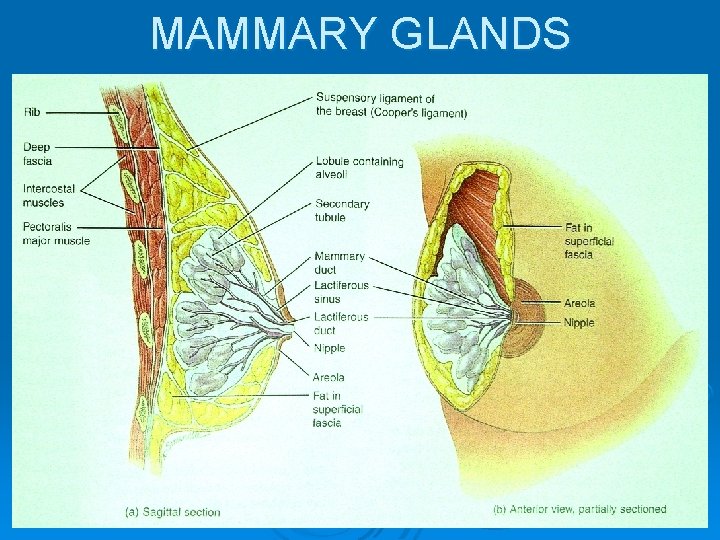
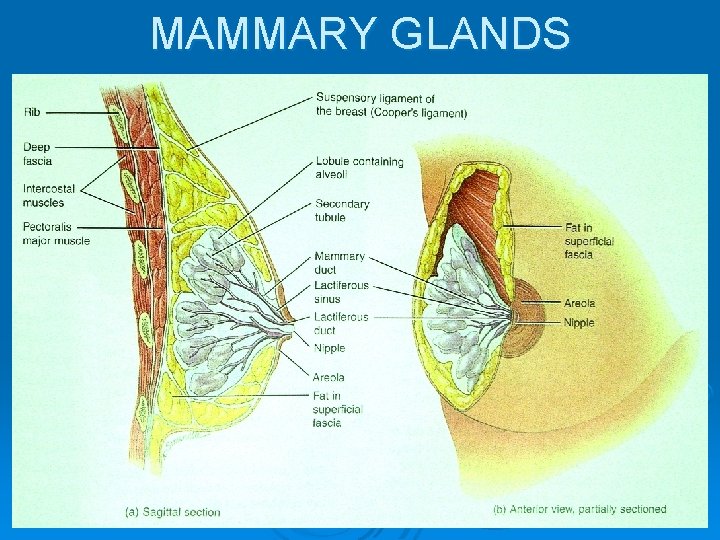
MAMMARY GLANDS Ø Ø Ø The two mammary glands are modified sudoriferous (sweat) glands that produce milk. They lie over the pectoralis major and serratus anterior muscles and are attached to them by a deep fascia layer of dense irregular CT. Each breast has one pigmented nipple which has a series of closely spaced openings—the external openings of lactiferous ducts, where milk emerges. The circular pigmented skin around the nipple is the areola, which appears rough because it contains modified sebaceous (oil) glands. Strands of CT called the suspensory ligaments of the breast (Cooper’s ligaments) run between the skin and deep fascia and support the breast.
MAMMARY GLANDS Ø Ø Within each breast, the mammary gland consists of 1520 lobes separated by adipose tissue. Each lobe consists of several smaller lobules, composed of milk-secreting glands called alveoli embedded in CT. Surrounding the alveoli are spindle-shaped cells called myoepithelial cells which contract to help propel milk toward the nipples. During milk production, it passes from the alveoli into secondary tubules, then into the mammary ducts. Near the nipple the mammary ducts expand to form lactiferous sinuses, where some milk may be stored before drainage into a lactiferous duct. Each lactiferous duct carries milk from one of the lobes to the exterior.
MAMMARY GLANDS The primary functions of the mammary glands are synthesis, secretion, and ejection of milk. Together these functions are called lactation. Ø Milk production is stimulated primarily by the hormone prolactin, with contributions from progesterone and estrogens. Ø Milk ejection occurs in the presence of oxytocin, which is released by the posterior pituitary gland in response to stimulation of the nipple by an infant’s suckling. Ø
MAMMARY GLANDS
THE FEMALE REPRODUCTIVE CYCLE Ø Ø Ø During their reproductive years, females normally experience a cyclical sequence of changes in the ovaries and uterus that involve both oogenesis and preparation of the uterus to receive a fertilized ovum. Each cycle typically takes about a month. Hormones secreted by the hypothalamus, anterior pituitary gland, and ovaries control the principal events. The series of events associated with maturation of an oocyte is called the ovarian cycle. The uterine (menstrual) cycle is the series of changes in the endometrium of the uterus that prepares it for the arrival of a fertilized ovum. The term female reproductive cycle encompasses the ovarian cycle, the uterine cycle, the hormonal changes that regulate them, and the cyclical changes that occur in the breasts and cervix.
HORMONAL REGULATION Ø Ø Ø Gonadotropin releasing hormone (Gn. RH) from the hypothalamus controls the uterine and ovarian cycles. Gn. RH stimulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland. FSH stimulates the initial release of estrogens by growing follicles. LH stimulates continued development of follicles and their full secretion of estrogen, brings about ovulation, promotes formation of the corpus luteum, and stimulates the production of estrogens, progesterone, relaxin, and inhibin by the corpus luteum At least six different estrogens have been isolated from female plasma, but only three are present in significant quantities: beta (β)-estradiol, estrone, and estriol. βestradiol is the primary estrogen in nonpregnant women and is synthesized in the ovaries.
HORMONAL REGULATION Ø Estrogens, secreted by follicular cells, have four important functions: l l l Promote development and maintenance of female reproductive structures, secondary sex characteristics, and breasts. Help control fluid and electrolyte balance. Increase protein anabolism (work synergistically with human growth hormone in this purpose). Lower blood cholesterol level. Moderate levels inhibit release of Gn. RH, FSH, and LH.
HORMONAL REGULATION Progesterone, from the corpus luteum, acts synergistically with estrogens to prepare the endometrium for implantation of a fertilized ovum and the mammary glands for milk production. High levels of progesterone also inhibit secretion of Gn. RH and LH. Ø Relaxin, from the corpus luteum, relaxes uterine muscles to aid in implantation of a fertilized ovum. (During pregnancy the placenta produces higher levels of relaxin, which continues to relax uterine muscle, relaxes the symphysis pubis, and helps dilate the cervix. ) Ø Inhibin, secreted by the granulosa cells of the growing follicle and the corpus luteum, inhibits the secretion of FSH and, to a lesser degree, LH. Ø
MENSTRUAL PHASE Ø The menstrual phase or menstruation or menses last approximately the first 5 days of the cycle. l Ovaries—About 20 secondary (antral) follicles, some in each ovary, begin to enlarge. Follicular fluid secreted by the granulosa cells and blood capillaries accumulates in the enlarging antrum while the oocyte remains near the edge of the follicles.
MENSTRUAL PHASE l Uterus—Menstrual flow consists of 50 -150 ml of blood, tissue fluid, mucus, and epithelial cells from the endometrium. This discharge occurs because reduces estrogen and progesterone levels cause the uterine spiral arteries to constrict, cutting off the blood supply to the stratum functionalis, which eventually sloughs off. At this time the endometrium is very thin because only the stratum basalis remains.
PREOVULATORY PHASE Ø The preovulatory phase is the time between menstruation and ovulation. It is more variable in length than the other phases and usually lasts about 6 -13 days (in a 28 -day cycle).
PREOVULATORY PHASE l Ovaries—Under the influence of FSH, the secondary follicles continue to grow and begin to secrete estrogen and inhibin. By about day 6 one follicle has surpassed the others, so becomes the dominant follicle. Estrogen and inhibin secreted by the dominant follicle decrease FSH secretion, which causes the other follicles to stop growing and undergo atresia. The dominant follicle becomes the mature (Graafian) follicle, continues to enlarge until it is more than 20 mm in diameter, and forms a blisterlike bulge on the surface of the ovary. Under the influence of LH, the follicle continues to increase its estrogen production. It also produces a small amount of progesterone a day or two before ovulation. The menstrual phase and preovulatory phase together are termed the follicular phase because the ovarian follicles are growing and developing.
PREOVULATORY PHASE l Uterus—Estrogens released into the blood by ovarian follicles stimulate repair of the endometrium. Cells of the stratum basalis undergo mitosis and produce a new stratum functionalis, the endometrium thickens, endometrial glands develop, and blood supply to the stratum functionalis is reestablished. The preovulatory phase is also called the proliferative phase because the endometrium is proliferating.
OVULATION Ovulation, which usually occurs around day 14, is the rupture of the mature follicle, which releases the secondary oocyte into the pelvic cavity. During ovulation, the secondary oocyte remains surrounded by its zona pelucida and corona radiata. Ø The high levels of estrogens during the late preovulatory phase exert a positive feedback effect on both LH and Gn. RH, causing ovulation: Ø l l l Ø High estrogen levels stimulate the hypothalamus to produce more Gn. RH and the anterior pituitary to produce more LH. Gn. RH promotes the release of FSH and more LH by the anterior pituitary. The LH surge brings about rupture of the mature follicle and expulsion of a secondary oocyte. The ovulated oocyte and its corona radiata are usually swept into the ovarian tube, but some are lost into the pelvic cavity and disintegrate. After ovulation the mature follicle collapses and blood within it forms a clot to become the corpus hemorrhagicum. The clot is absorbed by the remaining follicular cells, which enlarge, change character, and form the corpus luteum under the influence of LH. The corpus luteum responds to LH by secreting progesterone, estrogen, relaxin, and inhibin.
POSTOVULATORY PHASE The postovulatory phase is the most consistent in length, lasting 14 days, the time between ovulation and the onset of the next menses. Ø After ovulation, LH secretion stimulates the mature follicle to develop into the corpus luteum. During its 2 -week lifespan the corpus luteum secretes increasing amounts of progesterone and some estrogen. Ø
POSTOVULATORY PHASE l Ovary—If the secondary oocyte is fertilized and begins to divide, the corpus luteum persists past its normal lifespan, maintained by human chorionic gonadotropin (h. CG), a hormone produced by the embryo as soon as 8 -12 days following fertilization. The chorion eventually develops into the placenta. The presence h. CG in maternal blood or urine is an indication of pregnancy. As the pregnancy progresses, the placenta begins to secrete estrogens (support pregnancy) and progesterone (supports pregnancy and breast development), so the role of the corpus luteum becomes insignificant. This phase is also called the luteal phase. If h. CG does not prolong the life of the corpus luteum, its secretions decline after 2 weeks and it degenerates into a scar called the corpus albicans. The resulting lack of estrogens and progesterone cause menstruation. Also, decreased levels of estrogens, progesterone, and inhibin promote the release of Gn. RH, FSH, and LH, which stimulate follicular growth and the start of a new ovarian cycle.
POSTOVULATORY PHASE l Uterus—Progesterone and estrogens produced by the corpus luteum promote growth and coiling of the endometrial glands (which begin to secrete glycogen), vascularization of the superficial endometrium, thickening of the endometrium, and increased tissue fluid. These preparatory changes peak about one week after ovulation, corresponding to the expected time of arrival of a fertilized ovum. This phase is also called the secretory phase.
 Lesson 20.2 the male reproductive system
Lesson 20.2 the male reproductive system Chapter 16 lesson 3 the female reproductive system
Chapter 16 lesson 3 the female reproductive system Lesson 2: the male reproductive system
Lesson 2: the male reproductive system Chapter 2 human reproductive anatomy and physiology
Chapter 2 human reproductive anatomy and physiology Prostate diagram
Prostate diagram Function of vagina
Function of vagina Male reproductive system and its function
Male reproductive system and its function Frog testis labeled
Frog testis labeled Anatomy of the reproductive system exercise 42
Anatomy of the reproductive system exercise 42 Oogenesis process
Oogenesis process Diagram of male reproductive organ
Diagram of male reproductive organ Parts of male and female reproductive system
Parts of male and female reproductive system The reproductive system chapter 16
The reproductive system chapter 16 Luteinizing hormone in male reproductive system
Luteinizing hormone in male reproductive system Human reproductive system
Human reproductive system Art-labeling activity: the male reproductive system, part 1
Art-labeling activity: the male reproductive system, part 1 Male reproductive system information
Male reproductive system information Where is sperm located
Where is sperm located Bull reproductive system parts and functions
Bull reproductive system parts and functions Asexual reproduction
Asexual reproduction Function of male reproductive system
Function of male reproductive system Anatomy of fish reproductive system
Anatomy of fish reproductive system Reporoductive system
Reporoductive system Male fetal pig reproductive system labeled
Male fetal pig reproductive system labeled Male plant reproductive system
Male plant reproductive system Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Base of prostate gland
Base of prostate gland Cow reproductive system female
Cow reproductive system female Pearson
Pearson Colon function in male reproductive system
Colon function in male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Similarities between male and female reproductive system
Similarities between male and female reproductive system Male reproductive system labeled
Male reproductive system labeled Pathway of sperm in male reproductive system
Pathway of sperm in male reproductive system Drawing of the male and female reproductive system
Drawing of the male and female reproductive system Plants reproductive system
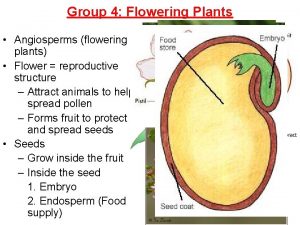
Plants reproductive system Summary of the reproductive system
Summary of the reproductive system What is fgm
What is fgm V
V What does sperm contain
What does sperm contain Uterian tube
Uterian tube Male reproductive system
Male reproductive system Similarity between male and female reproductive system
Similarity between male and female reproductive system Male reproductive system of mammals
Male reproductive system of mammals Figure 16-1 is a sagittal view of the male reproductive
Figure 16-1 is a sagittal view of the male reproductive Male reproductive system side view
Male reproductive system side view Function of fallopian tube
Function of fallopian tube Figure 28-1 the male reproductive system
Figure 28-1 the male reproductive system Figure 16-1 male reproductive system
Figure 16-1 male reproductive system Folliculogenesis
Folliculogenesis What are primary sexual characteristics
What are primary sexual characteristics Spermatogonia histology
Spermatogonia histology Epididymiis
Epididymiis Male reproductive system of birds
Male reproductive system of birds Colliculus seminalis
Colliculus seminalis Male reproductive system
Male reproductive system Male reproductive system
Male reproductive system Anatomy and physiology unit 7 cardiovascular system
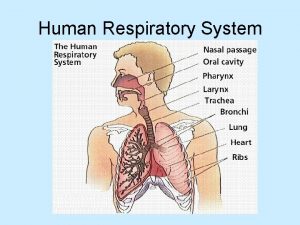
Anatomy and physiology unit 7 cardiovascular system Picture of human respiratory system
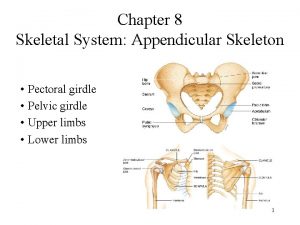
Picture of human respiratory system Pectoral girdle acetabulum
Pectoral girdle acetabulum Falopian tube parts
Falopian tube parts Perinetrium
Perinetrium Male reproductive organ
Male reproductive organ What produces pollen grains
What produces pollen grains Lesson 3 the female reproductive system
Lesson 3 the female reproductive system