UNDERSTANDING OF PAIN Nociceptive Neuropathic Mixed Pain Nur





- Slides: 70
UNDERSTANDING OF PAIN “ Nociceptive, Neuropathic & Mixed Pain ” Nur Surya Wirawan Department of Anesthesiology, Intensive Care and Pain Management Faculty of Medicine University of Hasanuddin Makassar
Objective After this lecture, participants are able to understand : 1. 2. 3. 4. 5. 6. 7. Definition of Pain Mechanism of Pain perception Nociceptive Pain Neuropathic Pain Mixed Pain Chronic Pain Take Home Messange
Before Eve was created from Adam's Rib, Adam was put into sleep
Descartes (17 th Century) First ideas…. Pain was faithfully transmitted from periphery to brain A pure stimulus response relationship
Progress in understanding pain MELZACK and WALL ‘Gate Control Theory’ 1965 -

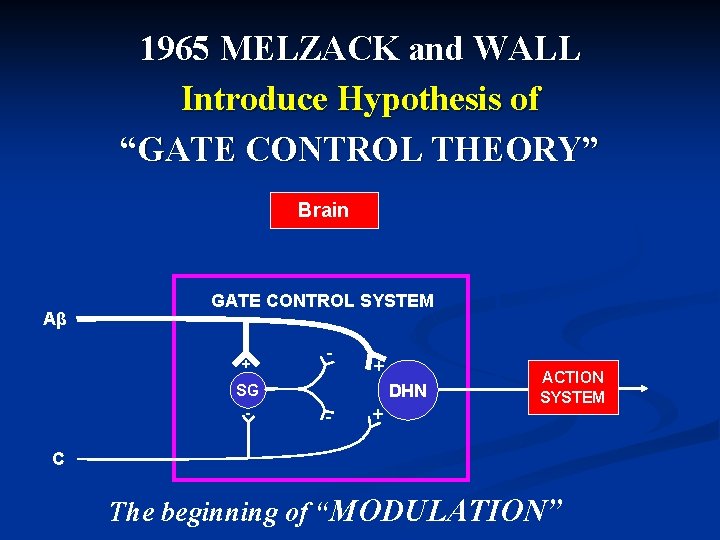
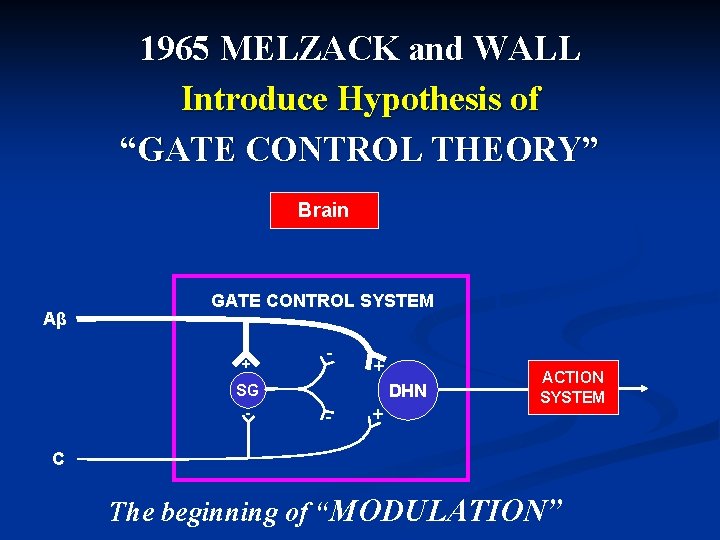
1965 MELZACK and WALL Introduce Hypothesis of “GATE CONTROL THEORY” Brain Aβ GATE CONTROL SYSTEM + SG - - + DHN - + ACTION SYSTEM C The beginning of “MODULATION”

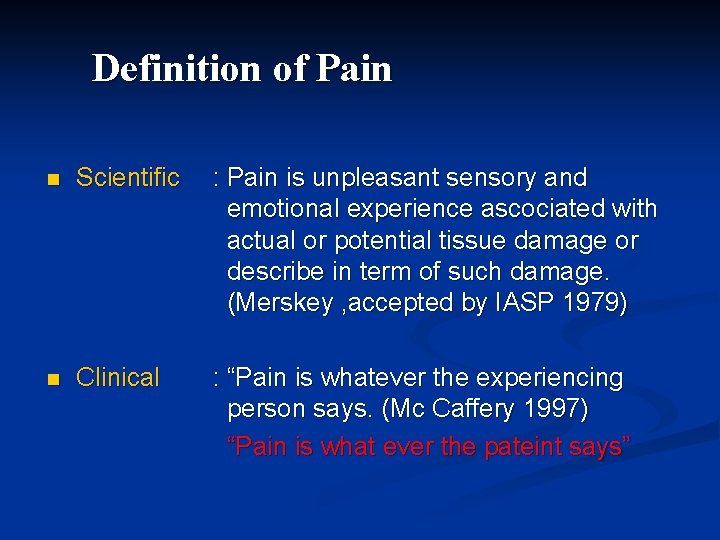
Definition of Pain n Scientific : Pain is unpleasant sensory and emotional experience ascociated with actual or potential tissue damage or describe in term of such damage. (Merskey , accepted by IASP 1979) n Clinical : “Pain is whatever the experiencing person says. (Mc Caffery 1997) “Pain is what ever the pateint says”
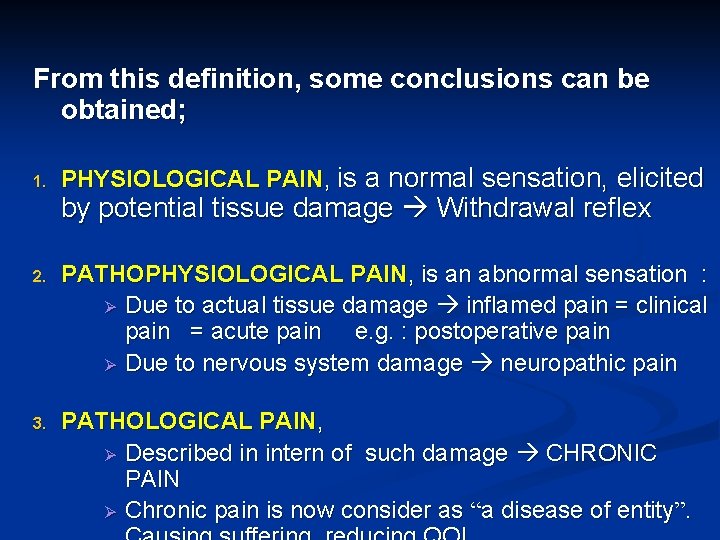
From this definition, some conclusions can be obtained; 1. PHYSIOLOGICAL PAIN, is a normal sensation, elicited by potential tissue damage Withdrawal reflex 2. PATHOPHYSIOLOGICAL PAIN, is an abnormal sensation : Ø Due to actual tissue damage inflamed pain = clinical pain = acute pain e. g. : postoperative pain Ø Due to nervous system damage neuropathic pain 3. PATHOLOGICAL PAIN, Ø Described in intern of such damage CHRONIC PAIN Ø Chronic pain is now consider as “a disease of entity”.

KLASIFIKASI NYERI Menurut waktu Nyeri akut & kronik NYERI Menurut patofisiologinya : Ø Nyeri fisiologik Ø Nyeri klinis ( nyeri patofisiologik) 1. Nyeri nosiseptif 2. Nyeri neuropatik • Perifer • Sentral 3. Nyeri psikogenik / idiopatik
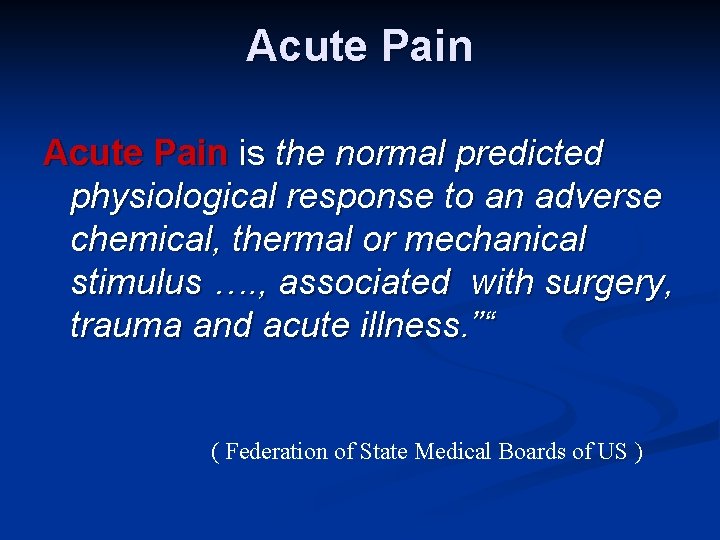
Acute Pain is the normal predicted physiological response to an adverse chemical, thermal or mechanical stimulus …. , associated with surgery, trauma and acute illness. ”“ ( Federation of State Medical Boards of US )
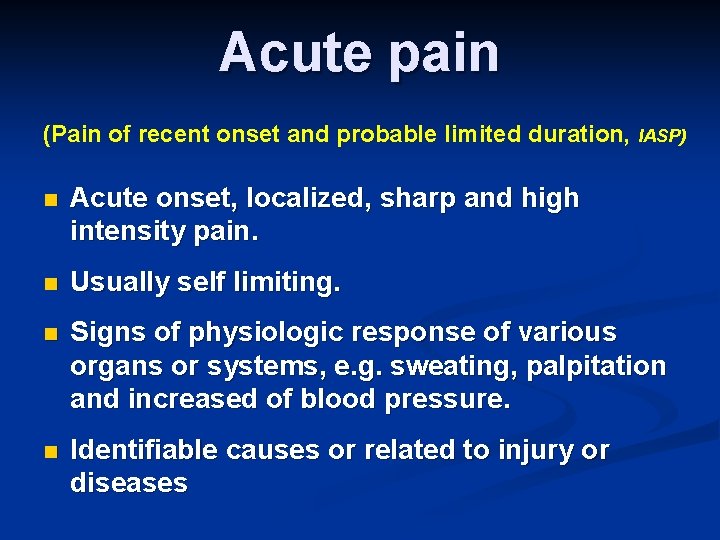
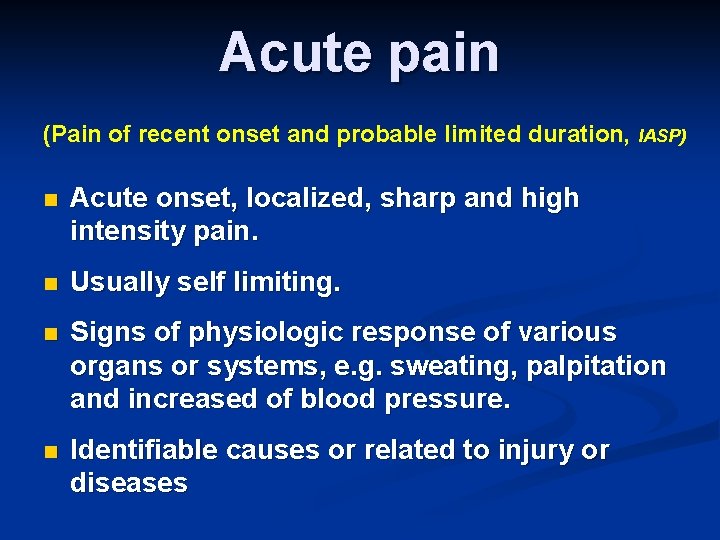
Acute pain (Pain of recent onset and probable limited duration, IASP) n Acute onset, localized, sharp and high intensity pain. n Usually self limiting. n Signs of physiologic response of various organs or systems, e. g. sweating, palpitation and increased of blood pressure. n Identifiable causes or related to injury or diseases
Causes of acute pain q Trauma q Surgery q Delivery q Invasive medical procedures q Acute illness.
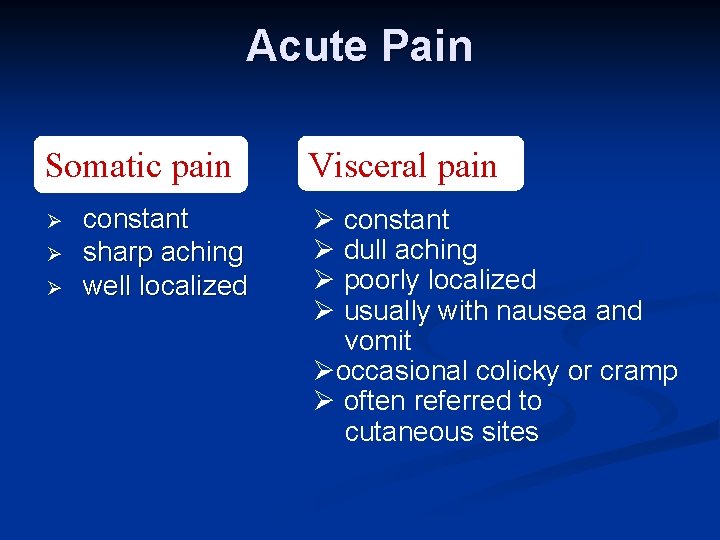
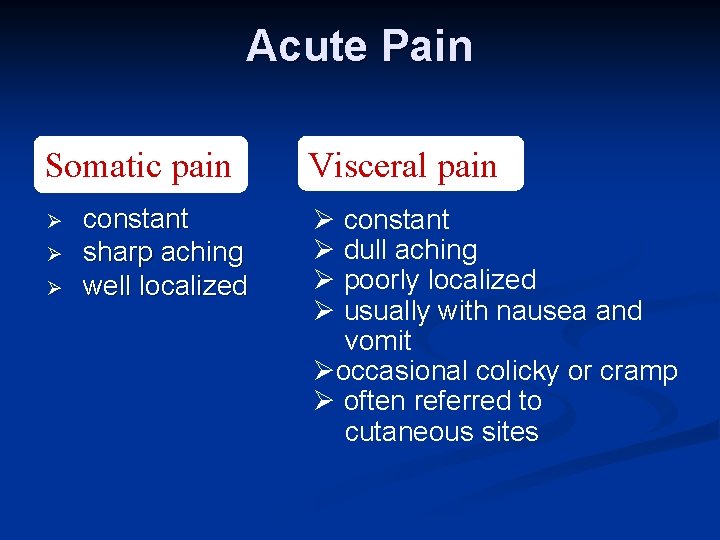
Acute Pain Somatic pain Ø Ø Ø constant sharp aching well localized Visceral pain Ø constant Ø dull aching Ø poorly localized Ø usually with nausea and vomit Øoccasional colicky or cramp Ø often referred to cutaneous sites
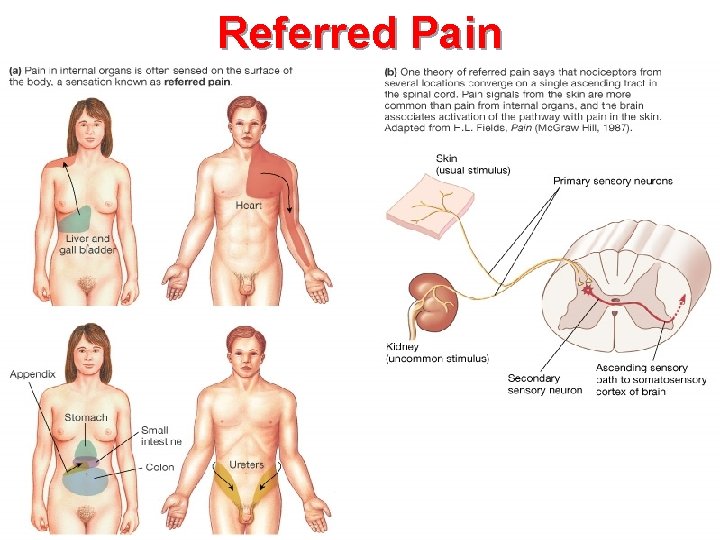
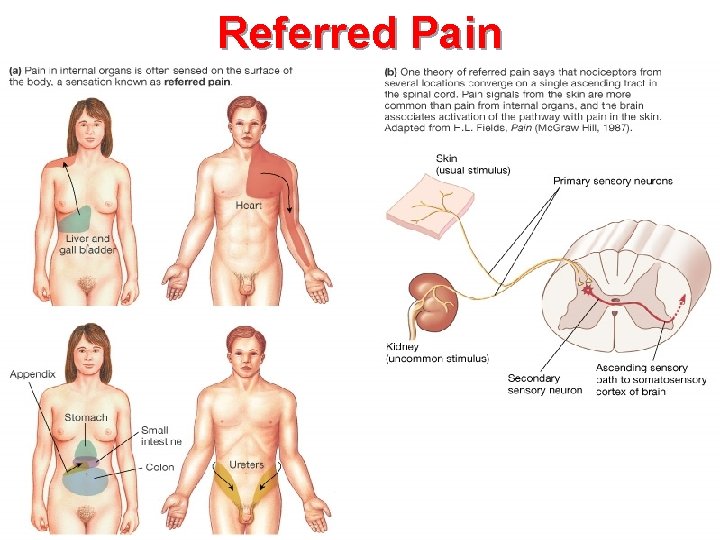
Referred Pain Figure 10 -13: Referred pain
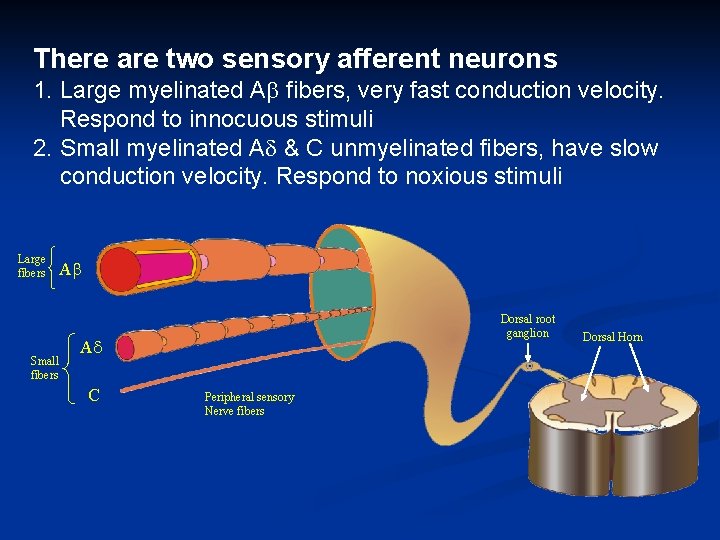
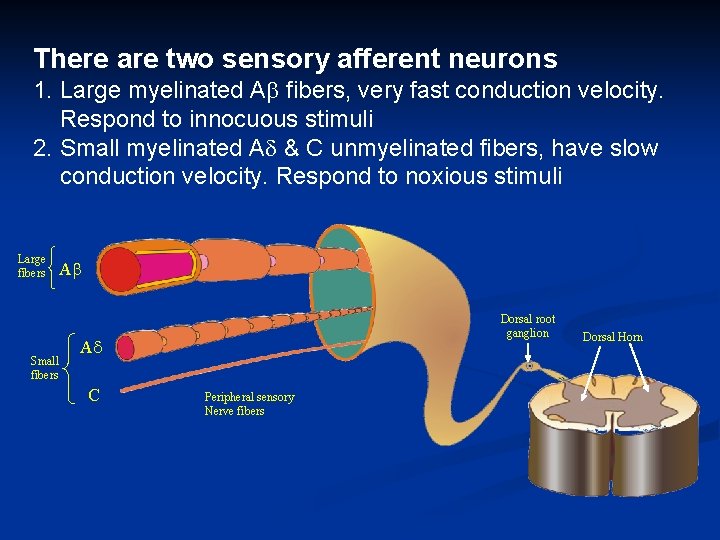
There are two sensory afferent neurons 1. Large myelinated A fibers, very fast conduction velocity. Respond to innocuous stimuli 2. Small myelinated A & C unmyelinated fibers, have slow conduction velocity. Respond to noxious stimuli Large fibers Small fibers A Dorsal root ganglion A C Peripheral sensory Nerve fibers Dorsal Horn
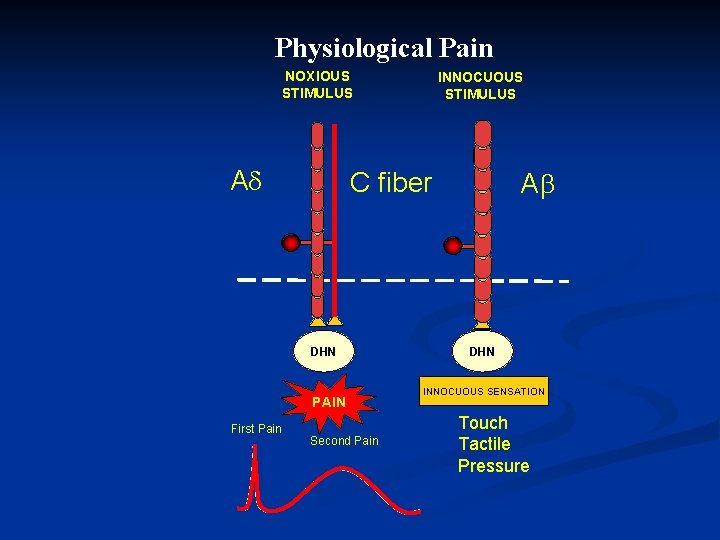
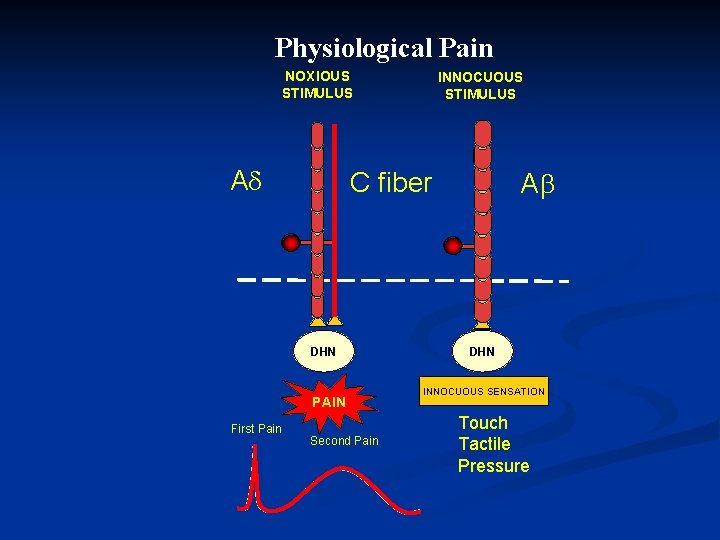
Physiological Pain NOXIOUS STIMULUS A C fiber DHN PAIN First Pain INNOCUOUS STIMULUS Second Pain A DHN INNOCUOUS SENSATION Touch Tactile Pressure
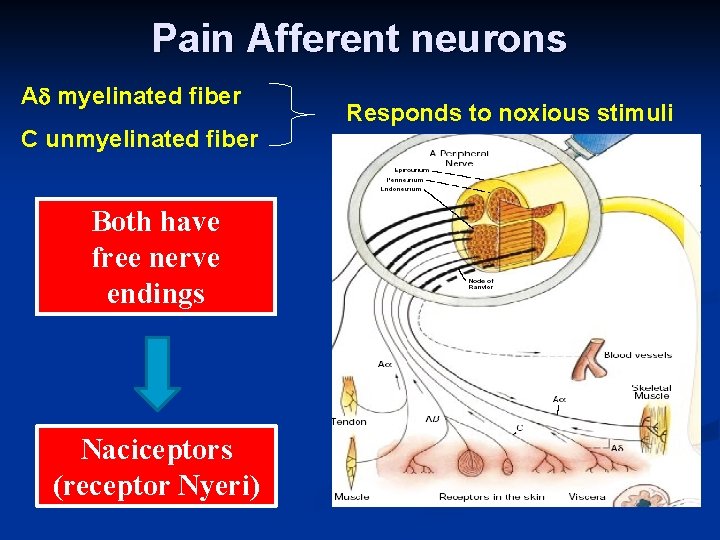
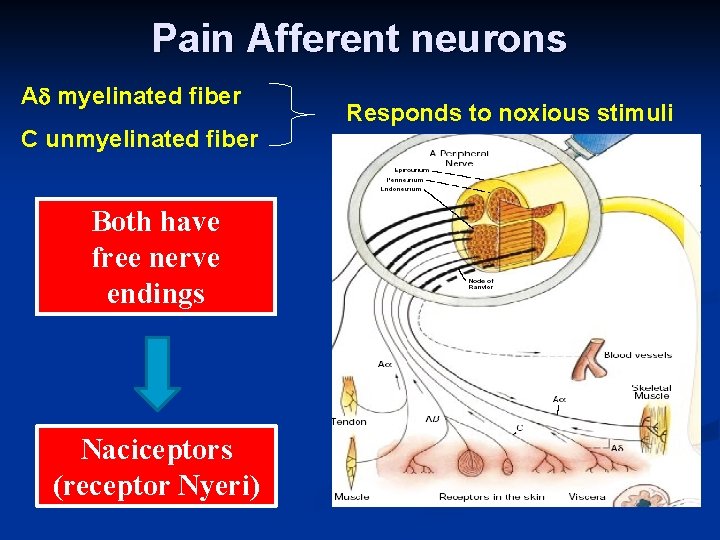
Pain Afferent neurons A myelinated fiber C unmyelinated fiber Both have free nerve endings Naciceptors (receptor Nyeri) Responds to noxious stimuli
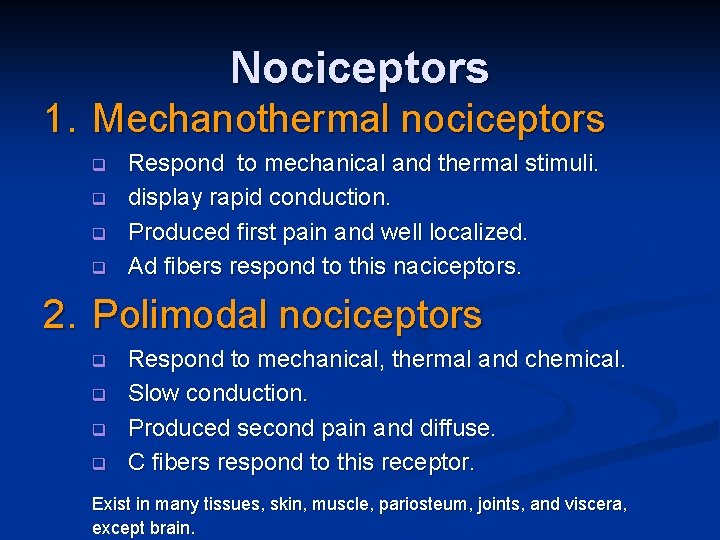
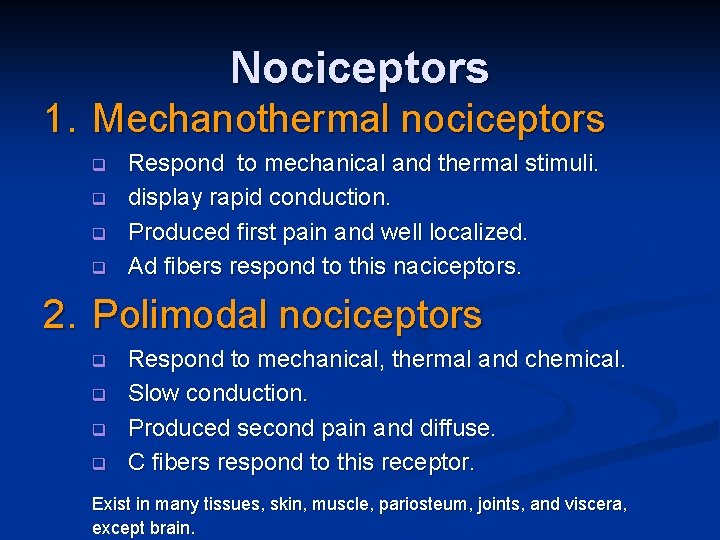
Nociceptors 1. Mechanothermal nociceptors q q Respond to mechanical and thermal stimuli. display rapid conduction. Produced first pain and well localized. Ad fibers respond to this naciceptors. 2. Polimodal nociceptors q q Respond to mechanical, thermal and chemical. Slow conduction. Produced second pain and diffuse. C fibers respond to this receptor. Exist in many tissues, skin, muscle, pariosteum, joints, and viscera, except brain.
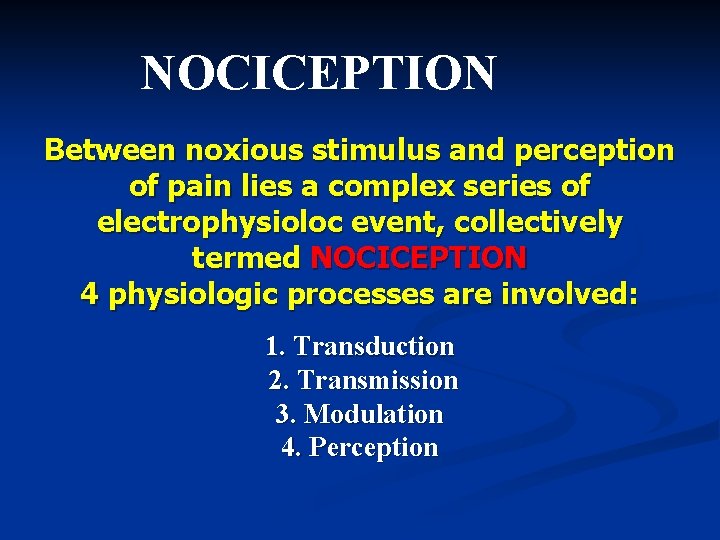
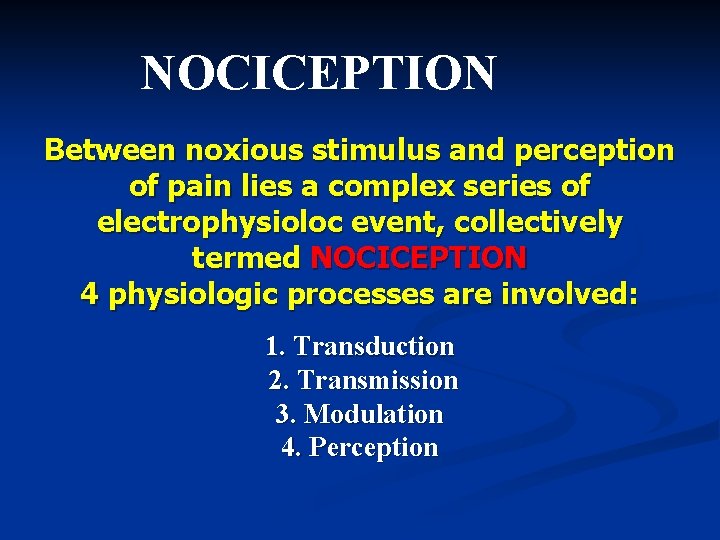
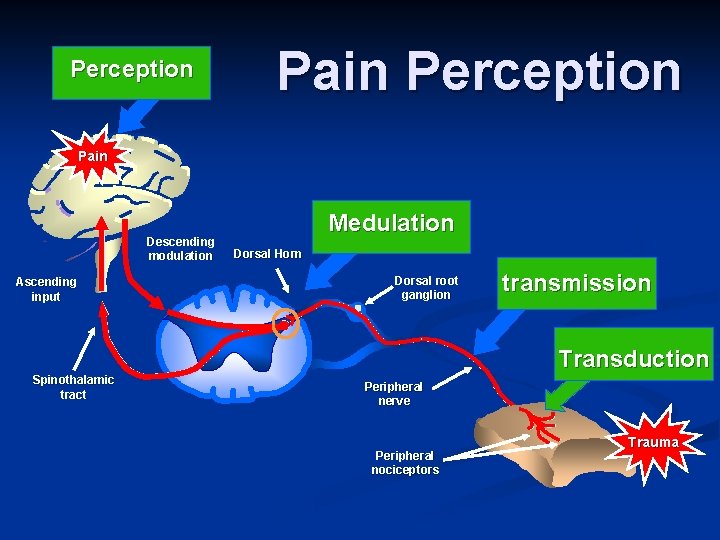
NOCICEPTION Between noxious stimulus and perception of pain lies a complex series of electrophysioloc event, collectively termed NOCICEPTION 4 physiologic processes are involved: 1. Transduction 2. Transmission 3. Modulation 4. Perception
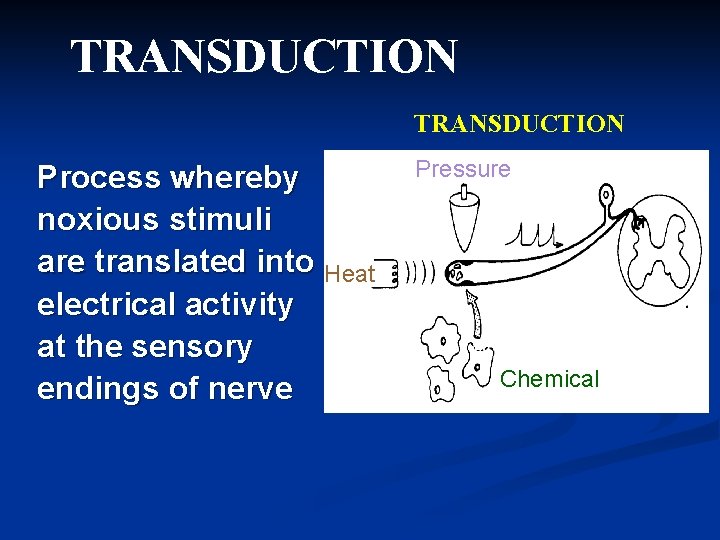
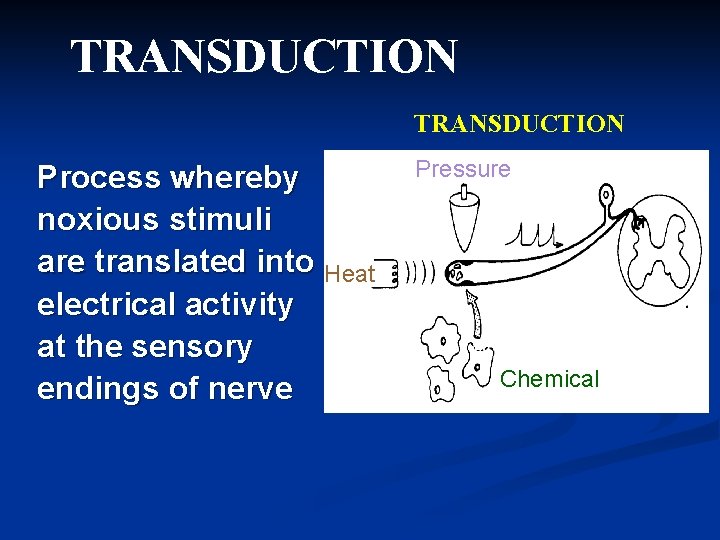
TRANSDUCTION Process whereby noxious stimuli are translated into Heat electrical activity at the sensory endings of nerve Pressure Chemical
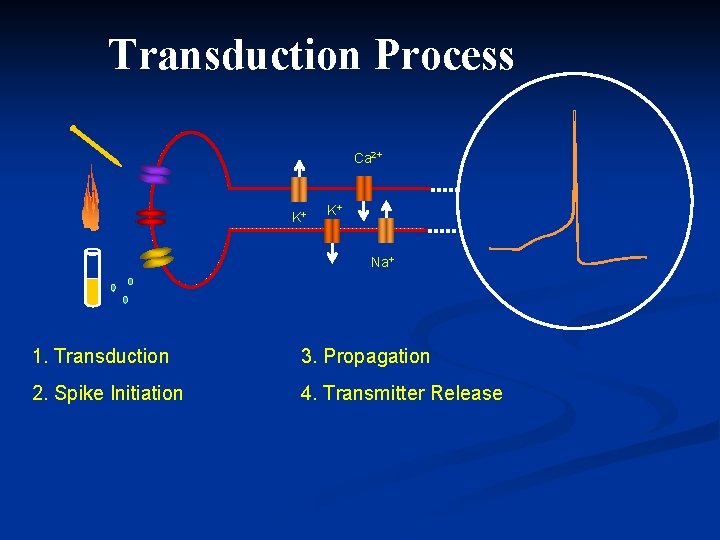
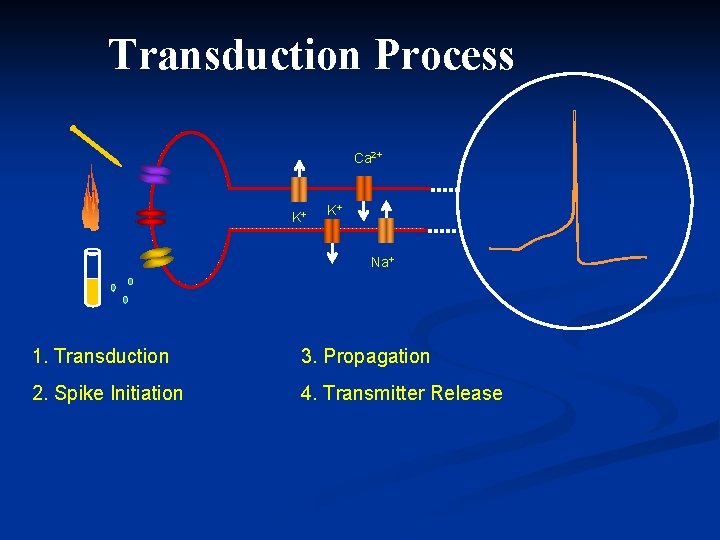
Transduction Process Ca 2+ K+ K+ Na+ 1. Transduction 3. Propagation 2. Spike Initiation 4. Transmitter Release Modified Meliala, 2006
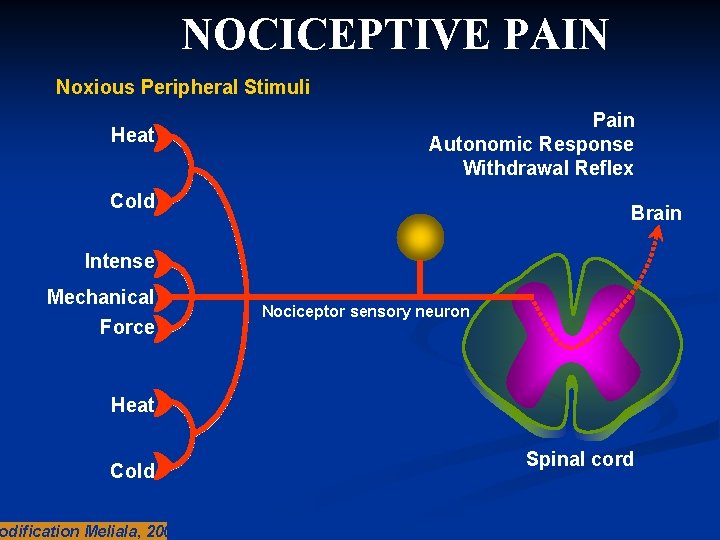
NOCICEPTIVE PAIN Noxious Peripheral Stimuli Heat Pain Autonomic Response Withdrawal Reflex Cold Brain Intense Mechanical Force Nociceptor sensory neuron Heat Cold odification Meliala, 2005 Spinal cord
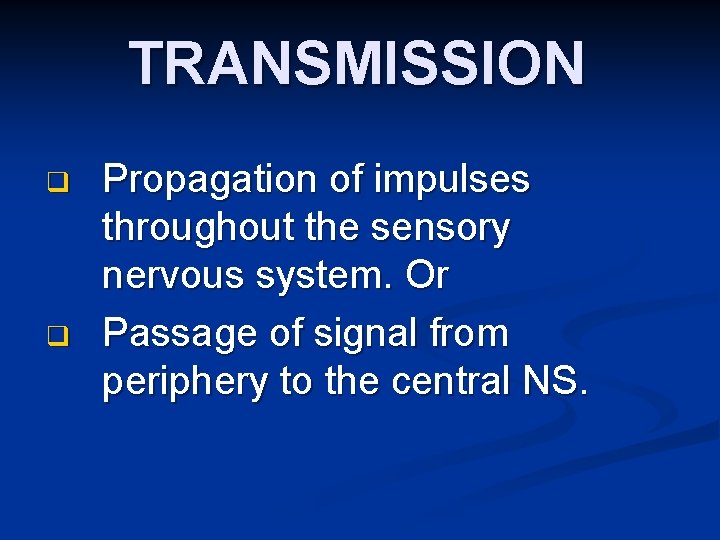
TRANSMISSION q q Propagation of impulses throughout the sensory nervous system. Or Passage of signal from periphery to the central NS.
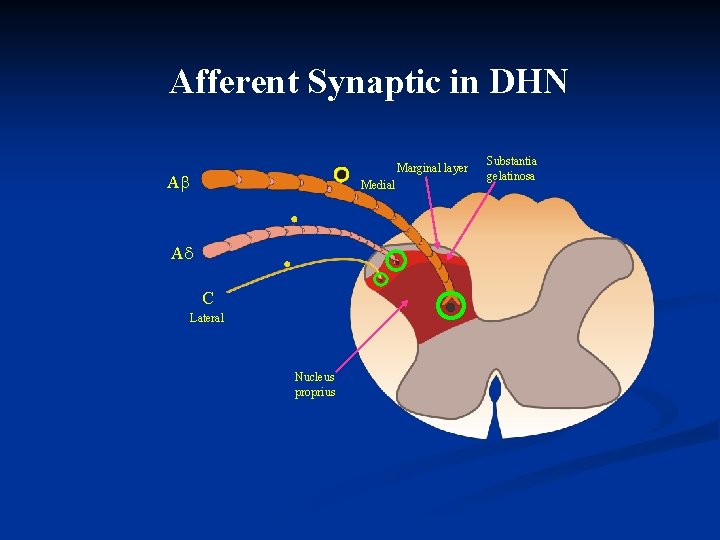
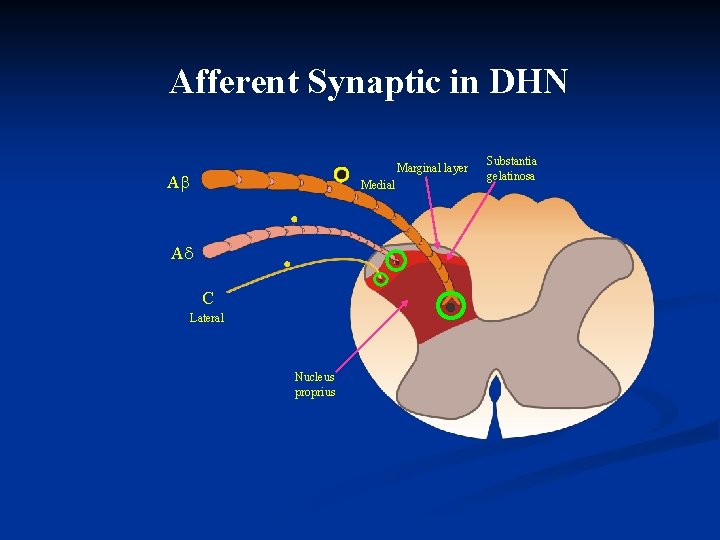
Afferent Synaptic in DHN Marginal layer A Medial A C Lateral Nucleus proprius Substantia gelatinosa
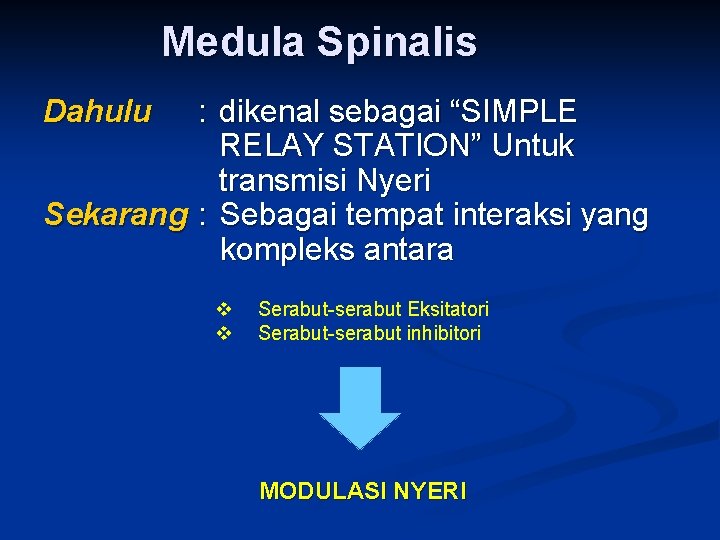
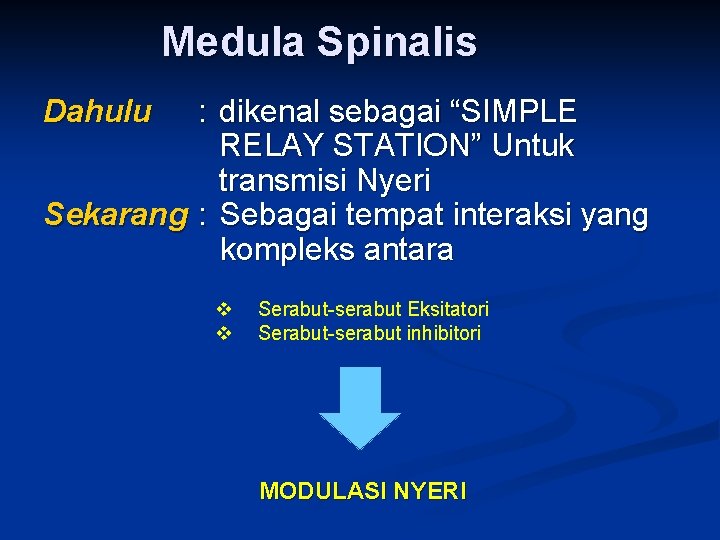
Medula Spinalis Dahulu : dikenal sebagai “SIMPLE RELAY STATION” Untuk transmisi Nyeri Sekarang : Sebagai tempat interaksi yang kompleks antara v v Serabut-serabut Eksitatori Serabut-serabut inhibitori MODULASI NYERI
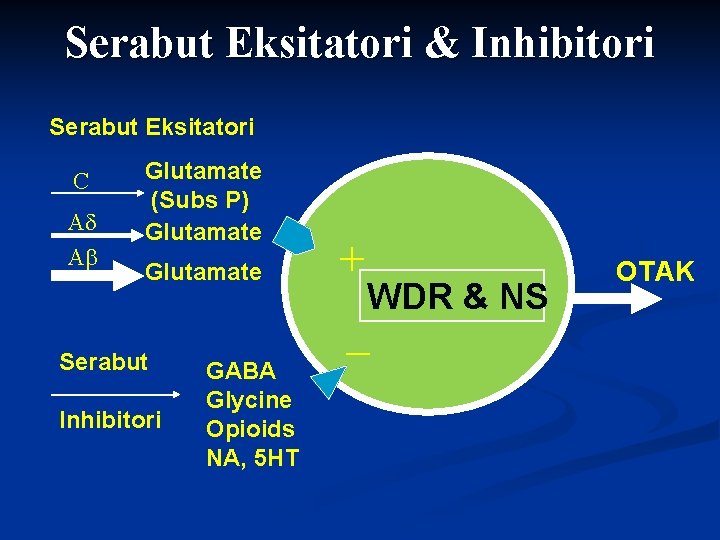
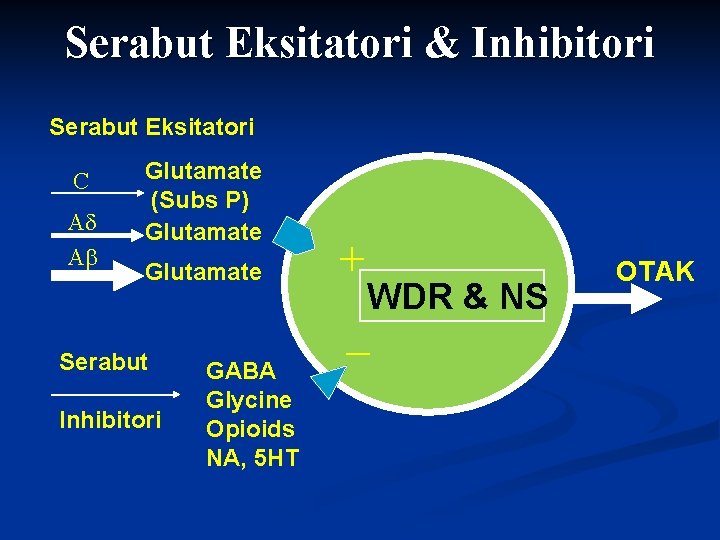
Serabut Eksitatori & Inhibitori Serabut Eksitatori C A A Glutamate (Subs P) Glutamate Serabut Inhibitori GABA Glycine Opioids NA, 5 HT + WDR & NS - OTAK
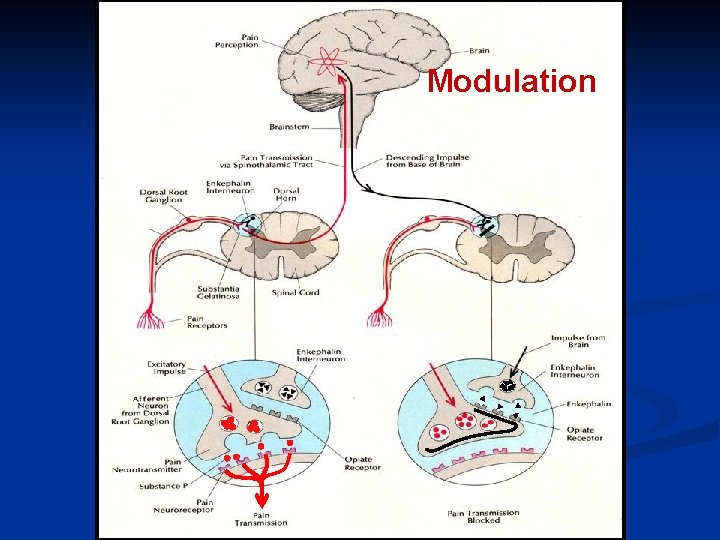
MODULATION n The process whereby endogenous analgesic system (opioid, serotonergic, and noradrenergic) can modify nociceptive transmission
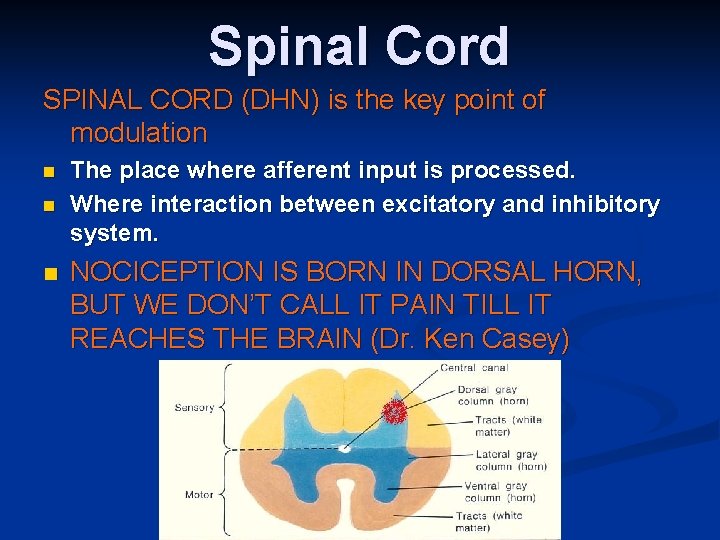
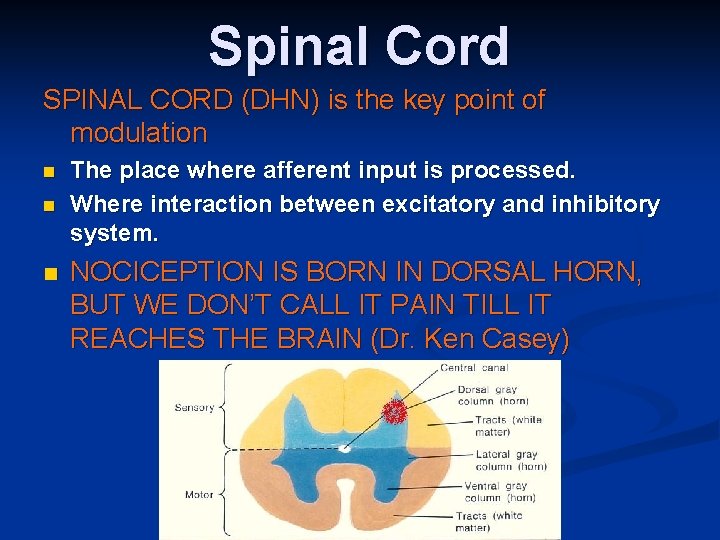
Spinal Cord SPINAL CORD (DHN) is the key point of modulation n The place where afferent input is processed. Where interaction between excitatory and inhibitory system. NOCICEPTION IS BORN IN DORSAL HORN, BUT WE DON’T CALL IT PAIN TILL IT REACHES THE BRAIN (Dr. Ken Casey)
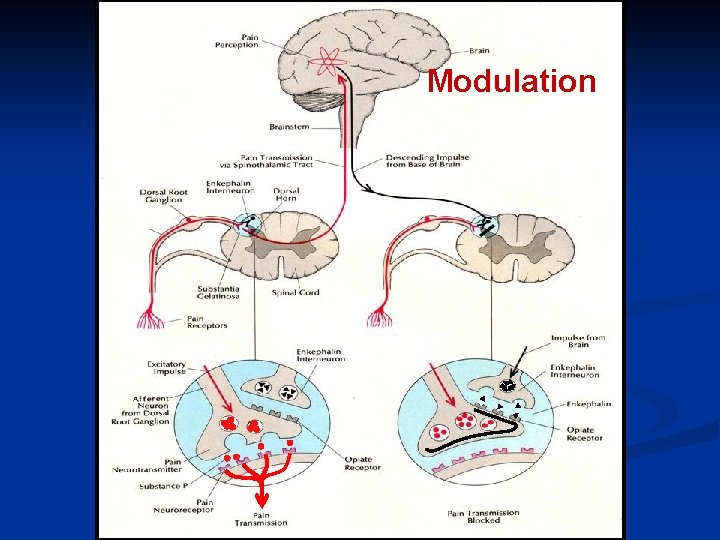
Modulation
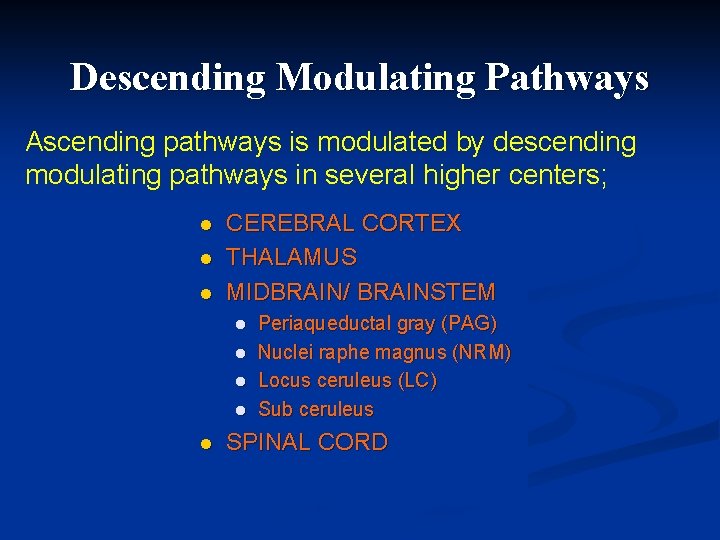
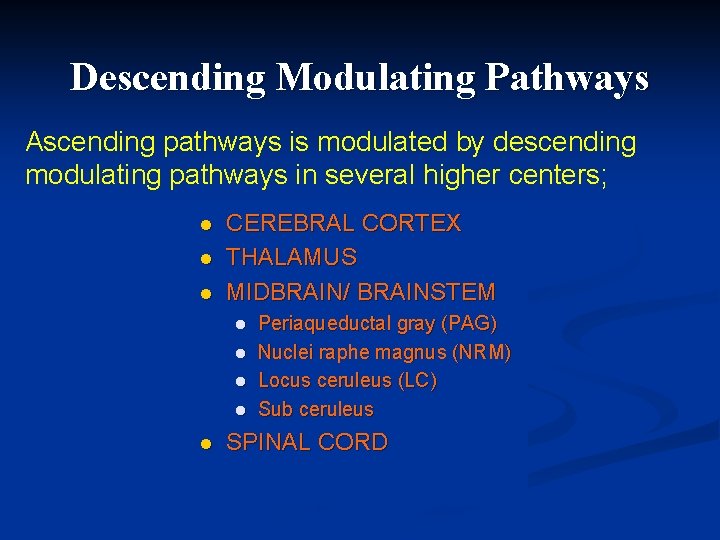
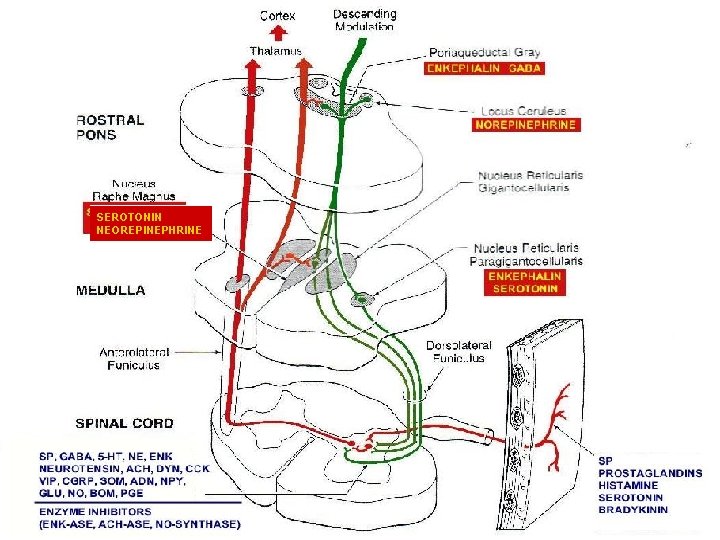
Descending Modulating Pathways Ascending pathways is modulated by descending modulating pathways in several higher centers; l l l CEREBRAL CORTEX THALAMUS MIDBRAIN/ BRAINSTEM l l l Periaqueductal gray (PAG) Nuclei raphe magnus (NRM) Locus ceruleus (LC) Sub ceruleus SPINAL CORD
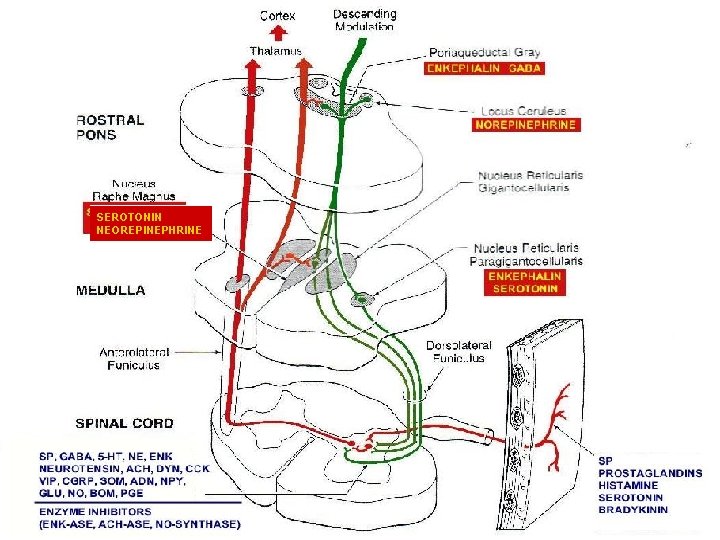
SEROTONIN NEOREPINEPHRINE
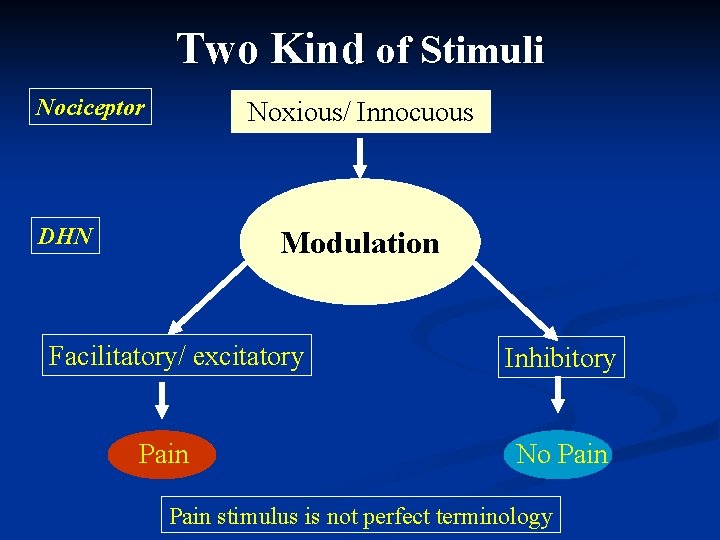
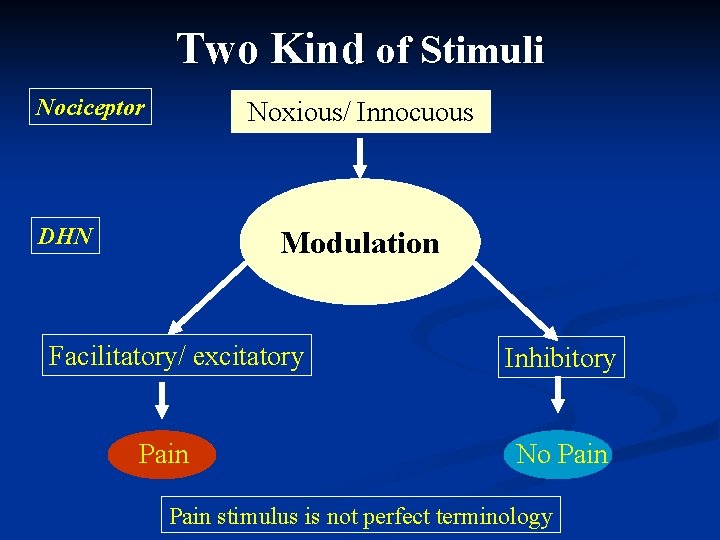
Two Kind of Stimuli Nociceptor Noxious/ Innocuous DHN Modulation Facilitatory/ excitatory Pain Inhibitory No Pain stimulus is not perfect terminology
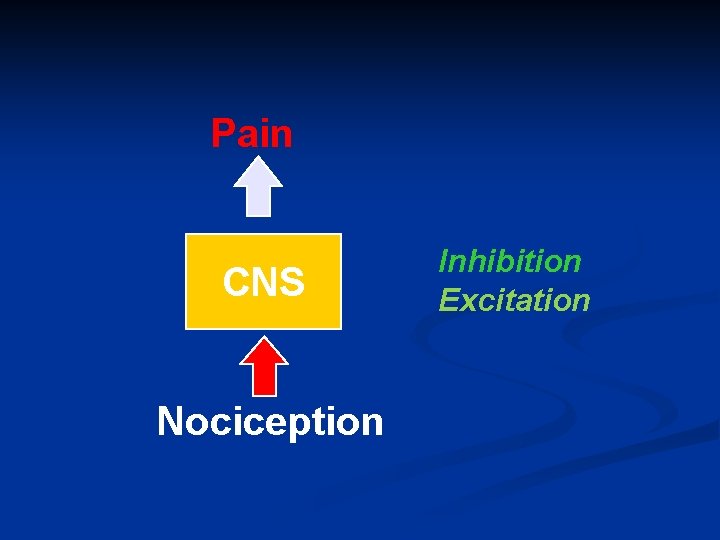
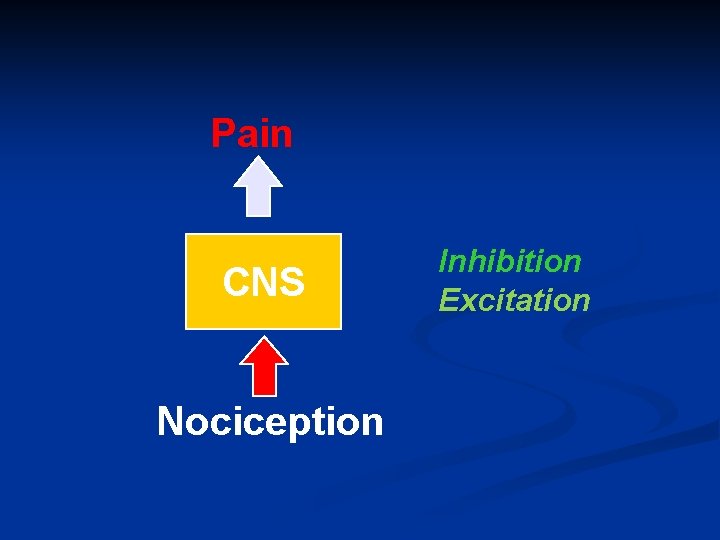
Pain CNS Nociception Inhibition Excitation
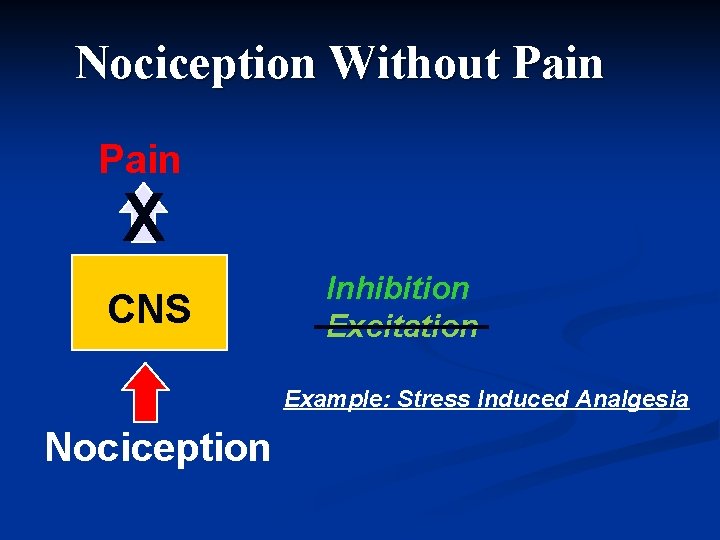
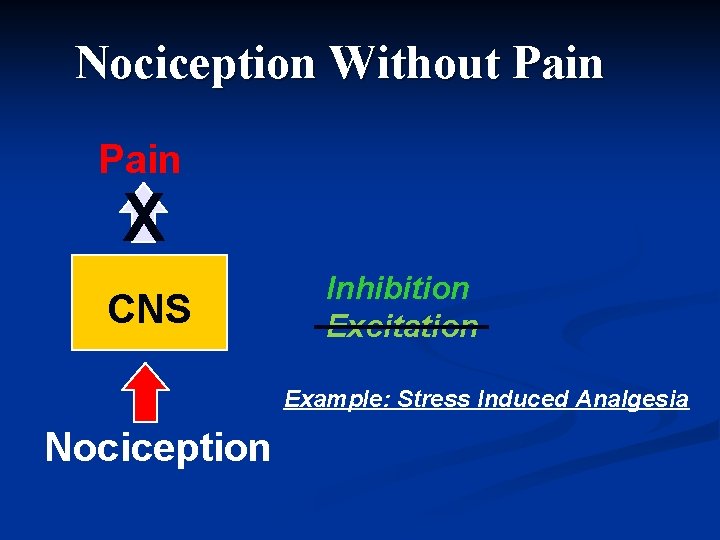
Nociception Without Pain X CNS Inhibition Excitation Example: Stress Induced Analgesia Nociception
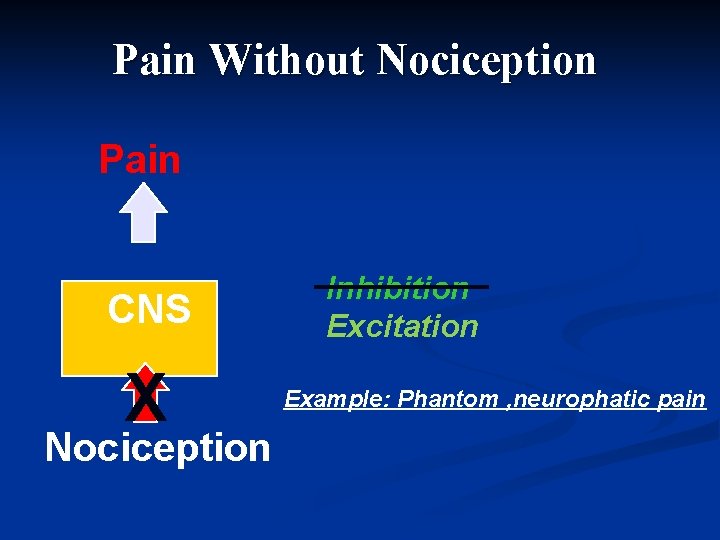
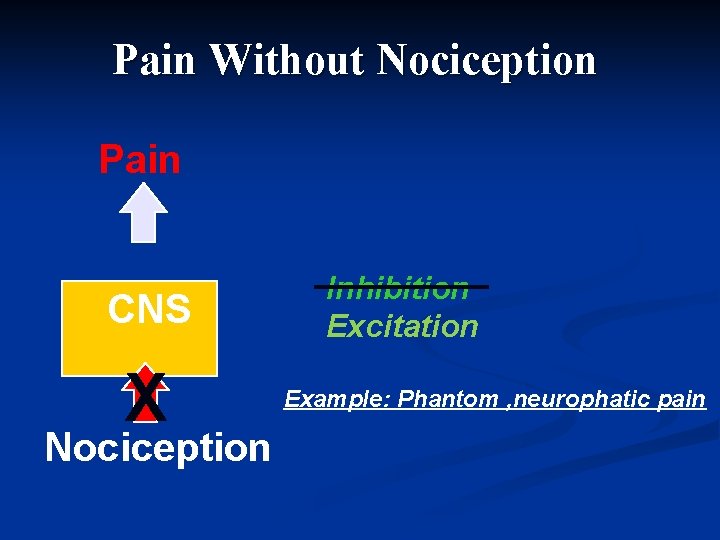
Pain Without Nociception Pain CNS X Nociception Inhibition Excitation Example: Phantom , neurophatic pain
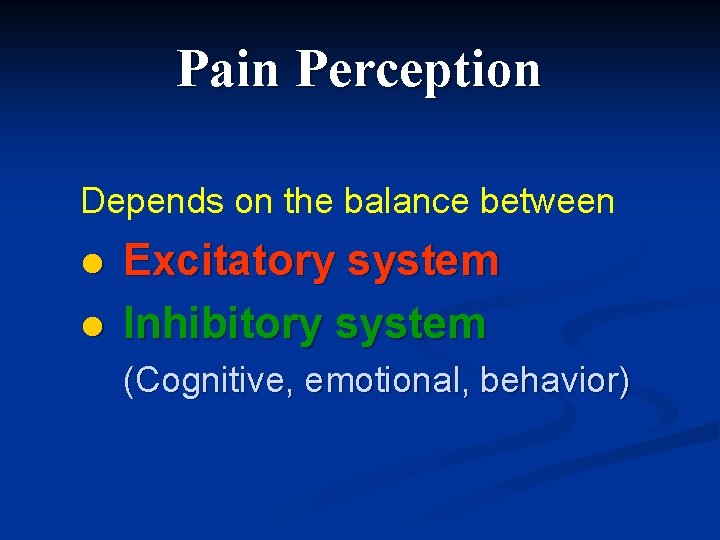
Pain Perception Depends on the balance between: l l Excitatory system Inhibitory system (Cognitive, emotional, behavior)


Beecher Pain perception depend on the meaning of i
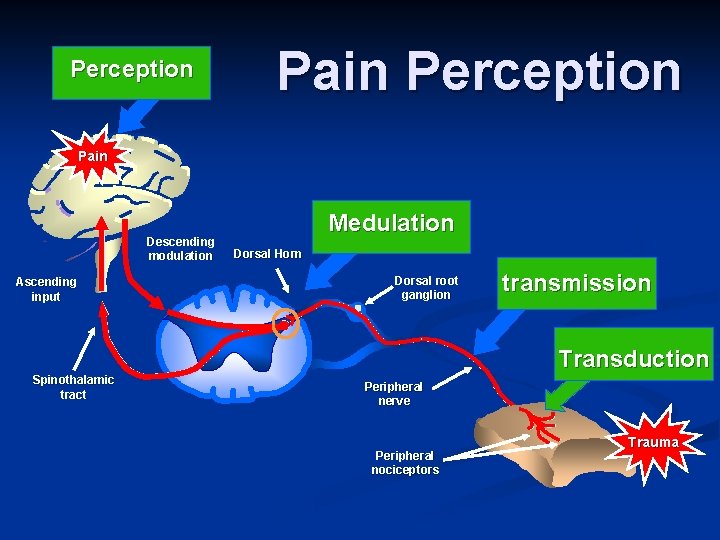
Perception Pain Descending modulation Ascending input Medulation Dorsal Horn Dorsal root ganglion transmission Transduction Spinothalamic tract Peripheral nerve Peripheral nociceptors Adapted from Gottschalk A et al. Am Fam Physician. 2001; 63: 1981, and Kehlet H et al. Anesth Analg. 1993; 77: 1049. Trauma
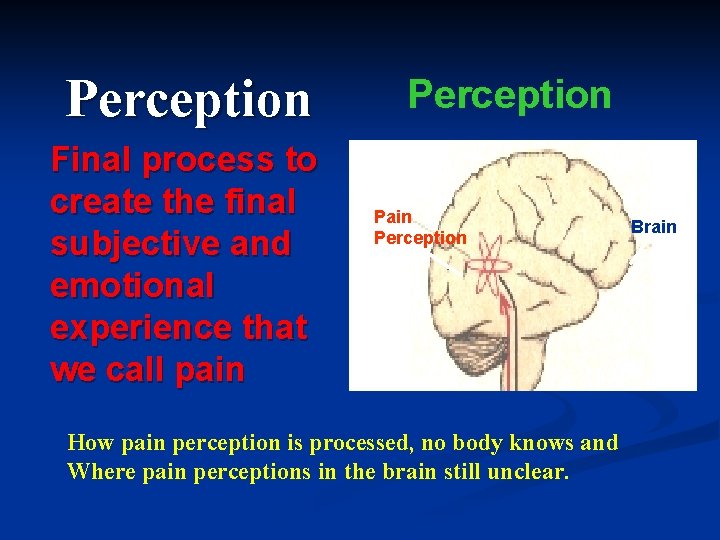
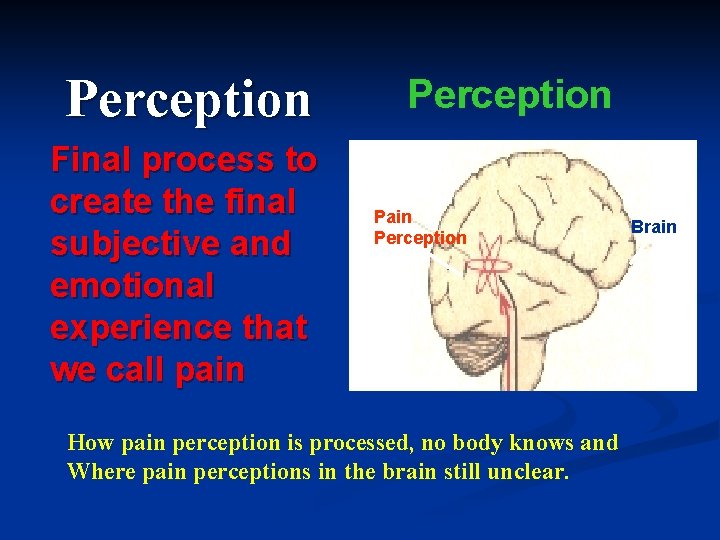
Perception Final process to create the final subjective and emotional experience that we call pain Perception Pain Perception How pain perception is processed, no body knows and Where pain perceptions in the brain still unclear. Brain
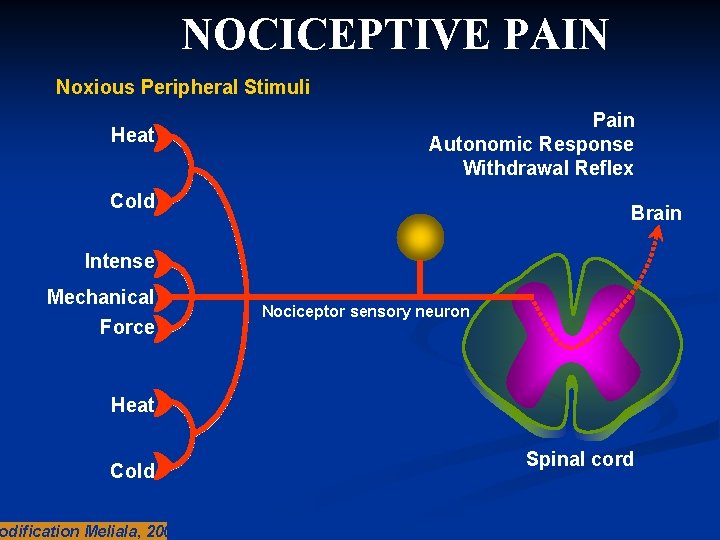
What is nociceptive pain? q A sensory experience that occurs when specific peripheral sensory neurons (nociceptors) respond to noxious stimuli q Painful region is typically localized at the site of injury – often described as throbbing, aching or stiffness q Usually time-limited and resolves when damaged tissue heals (e. g. bone fractures, burns and bruises) q Can also be chronic (e. g. osteoarthritis) q Responds to conventional analgesics
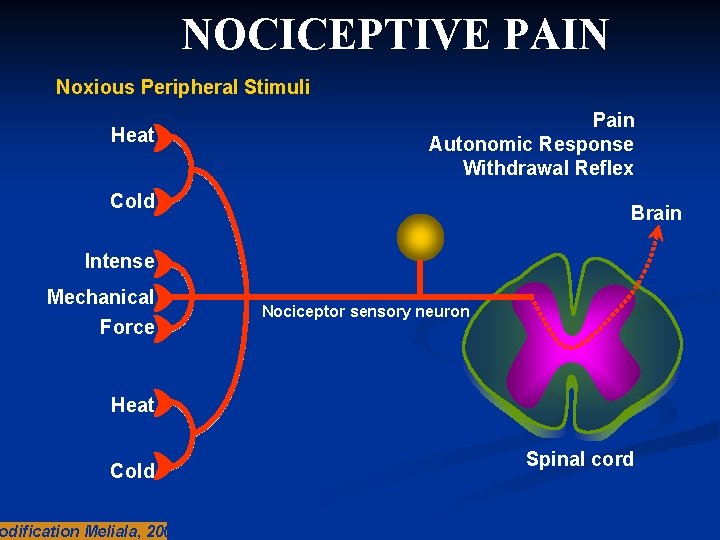
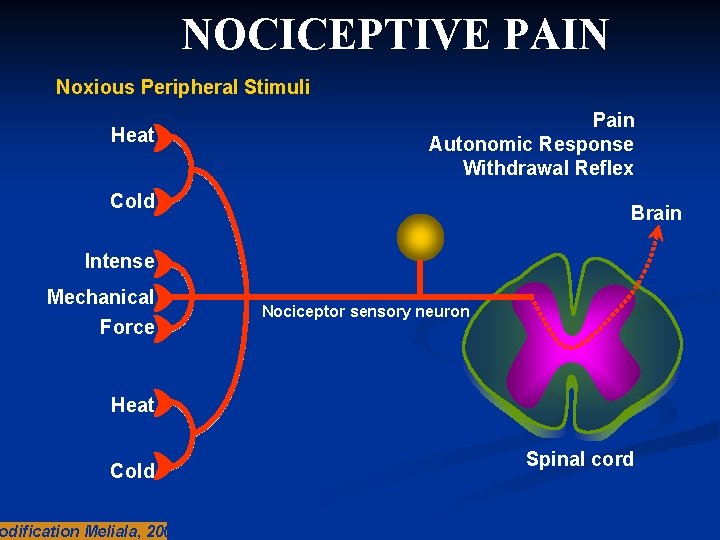
NOCICEPTIVE PAIN Noxious Peripheral Stimuli Heat Pain Autonomic Response Withdrawal Reflex Cold Brain Intense Mechanical Force Nociceptor sensory neuron Heat Cold odification Meliala, 2005 Spinal cord
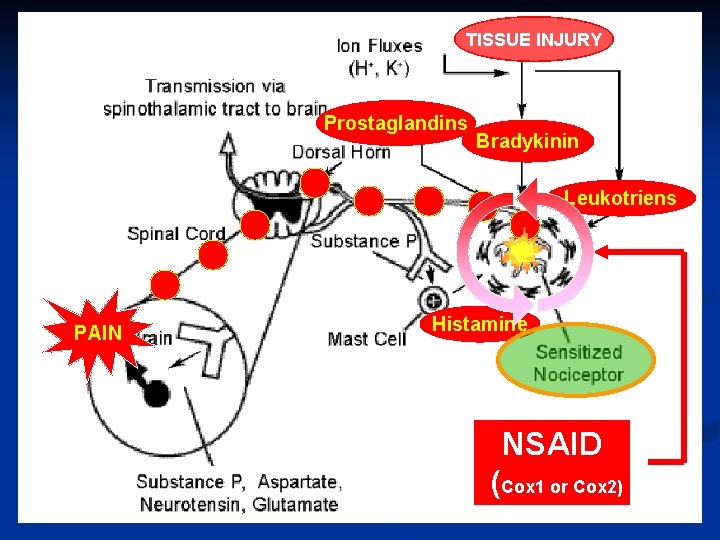
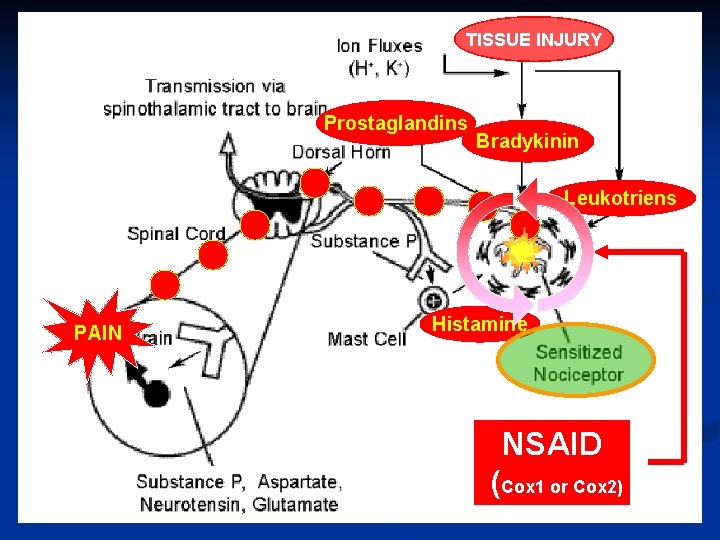
TISSUE INJURY Prostaglandins Bradykinin Leukotriens PAIN Histamine NSAID (Cox 1 or Cox 2)
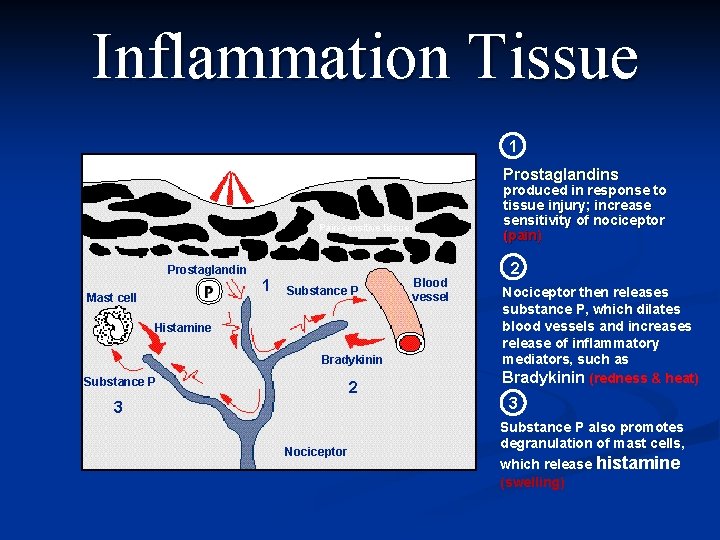
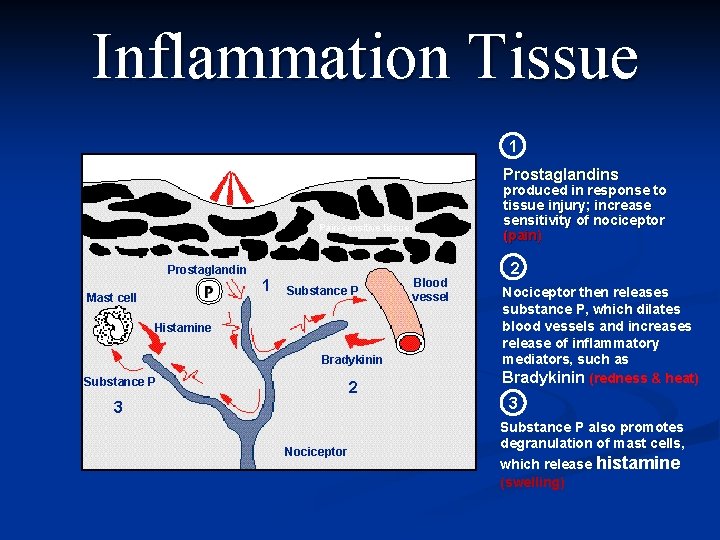
Inflammation Tissue 1 Painful stimulus Prostaglandins produced in response to tissue injury; increase sensitivity of nociceptor (pain) Pain-sensitive tissue Prostaglandin 1 Mast cell Substance P Histamine Bradykinin Substance P 2 3 Nociceptor Blood vessel 2 Nociceptor then releases substance P, which dilates blood vessels and increases release of inflammatory mediators, such as Bradykinin (redness & heat) 3 Substance P also promotes degranulation of mast cells, which release histamine (swelling)
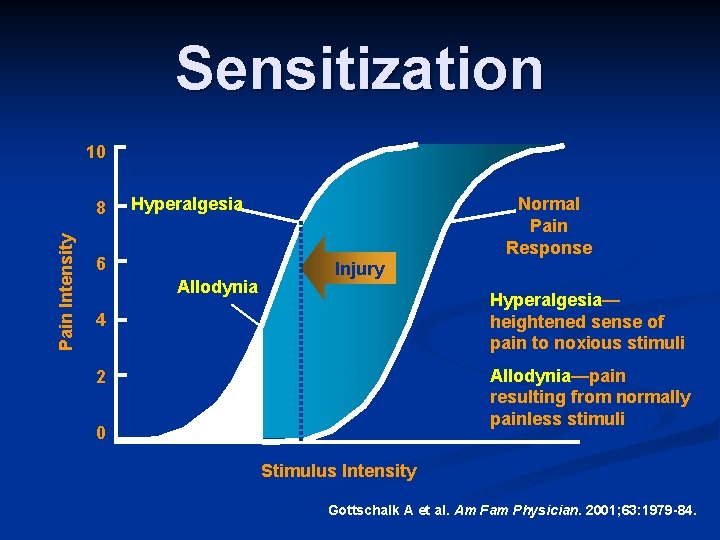
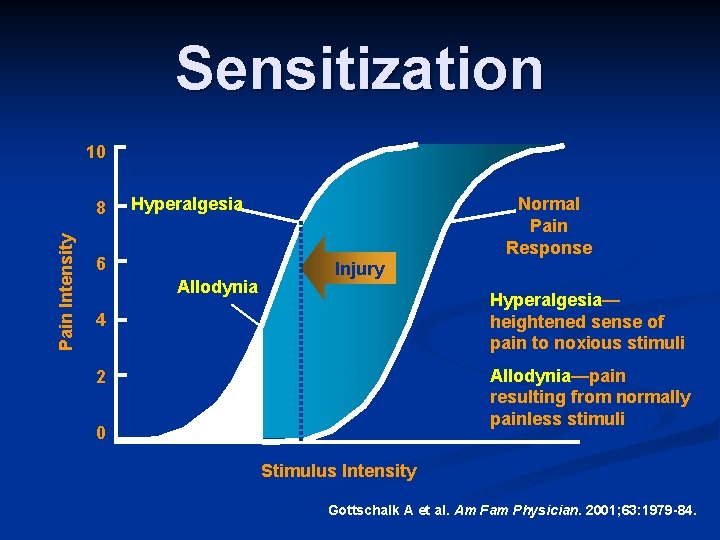
Sensitization 10 Pain Intensity 8 Hyperalgesia 6 Allodynia Normal Pain Response Injury Hyperalgesia— heightened sense of pain to noxious stimuli 4 Allodynia—pain resulting from normally painless stimuli 2 0 Stimulus Intensity Gottschalk A et al. Am Fam Physician. 2001; 63: 1979 -84.
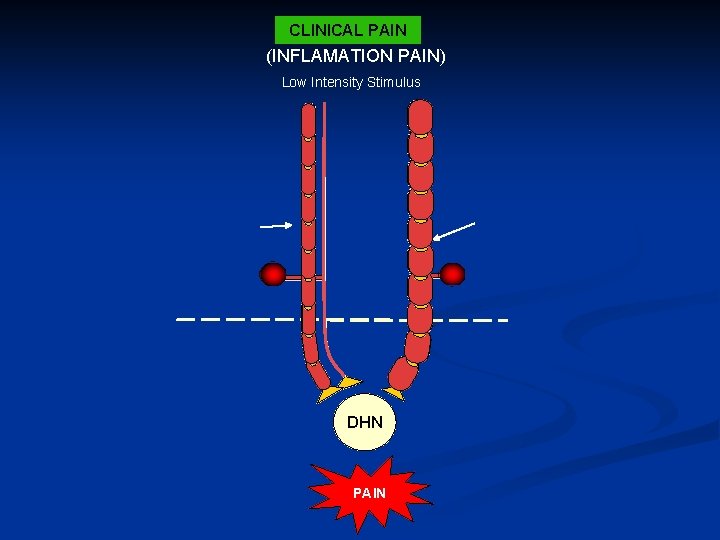
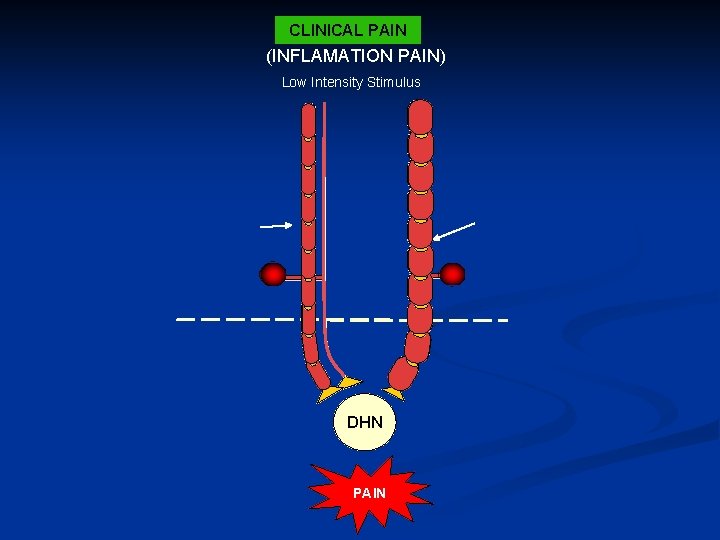
CLINICAL PAIN (INFLAMATION PAIN) Low Intensity Stimulus Ab Fiber Ad Fiber PNS CNS DHN PAIN Hyperexitable DHN
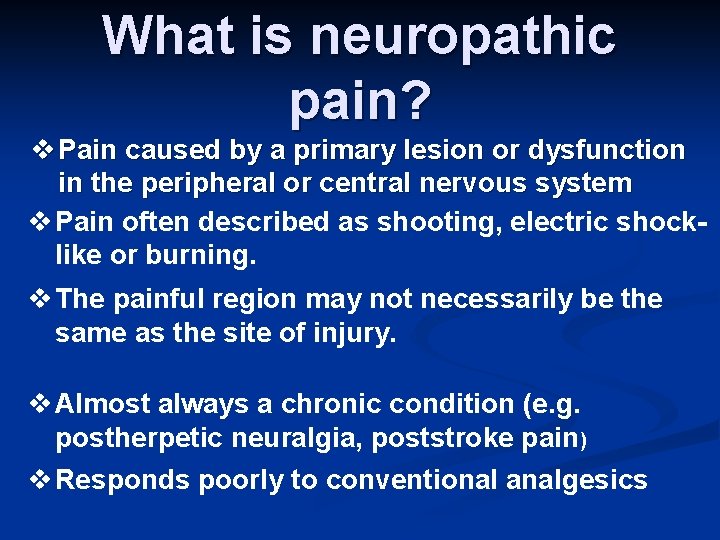
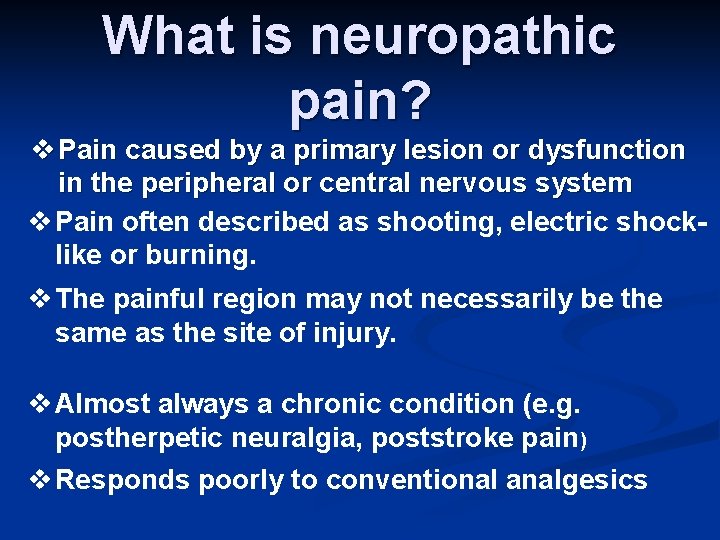
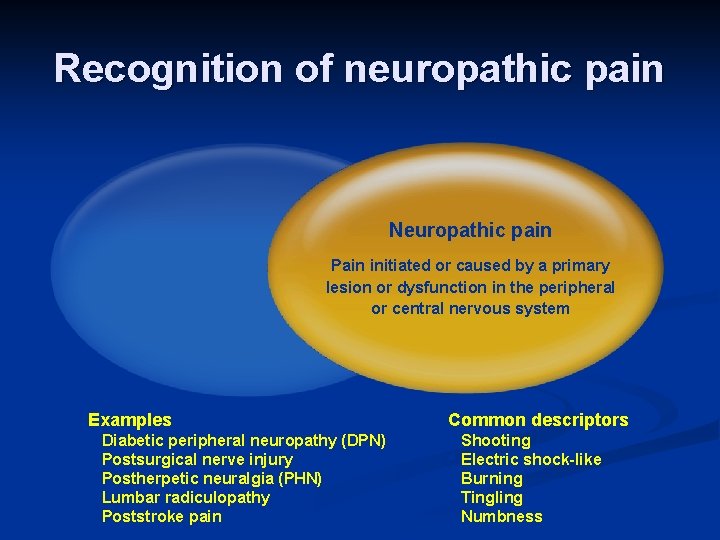
What is neuropathic pain? v Pain caused by a primary lesion or dysfunction in the peripheral or central nervous system v Pain often described as shooting, electric shocklike or burning. v The painful region may not necessarily be the same as the site of injury. v Almost always a chronic condition (e. g. postherpetic neuralgia, poststroke pain) v Responds poorly to conventional analgesics
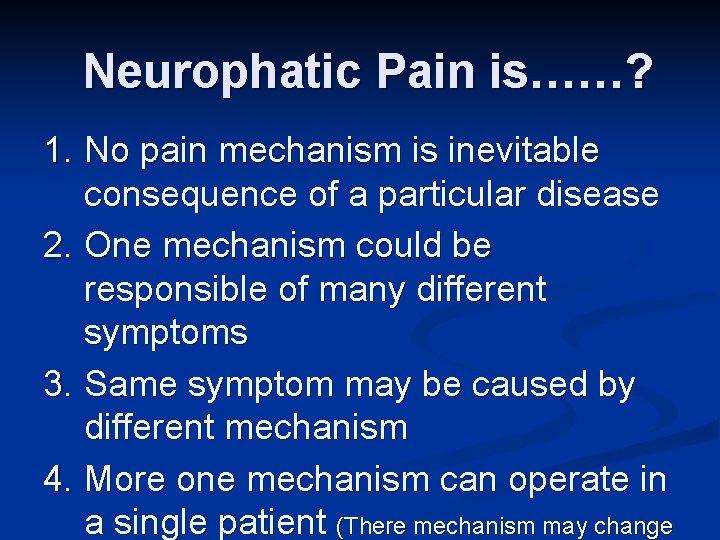
Neurophatic Pain is……? 1. No pain mechanism is inevitable consequence of a particular disease 2. One mechanism could be responsible of many different symptoms 3. Same symptom may be caused by different mechanism 4. More one mechanism can operate in a single patient (There mechanism may change
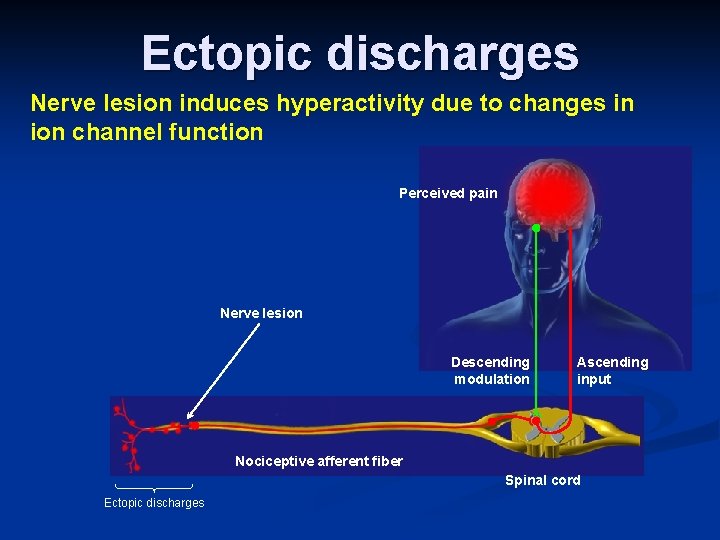
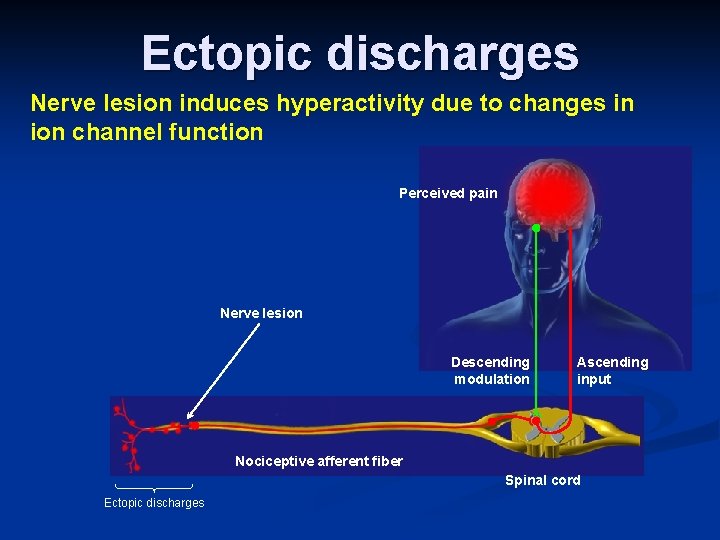
Ectopic discharges Nerve lesion induces hyperactivity due to changes in ion channel function Perceived pain Nerve lesion Descending modulation Ascending input Nociceptive afferent fiber Spinal cord Ectopic discharges
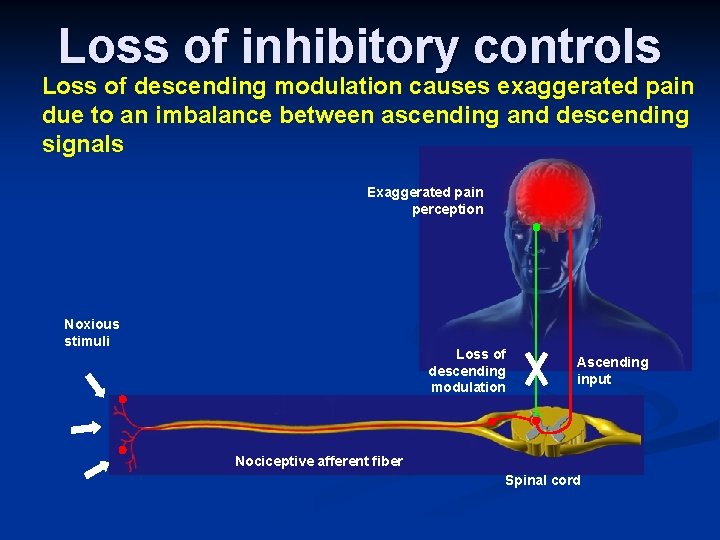
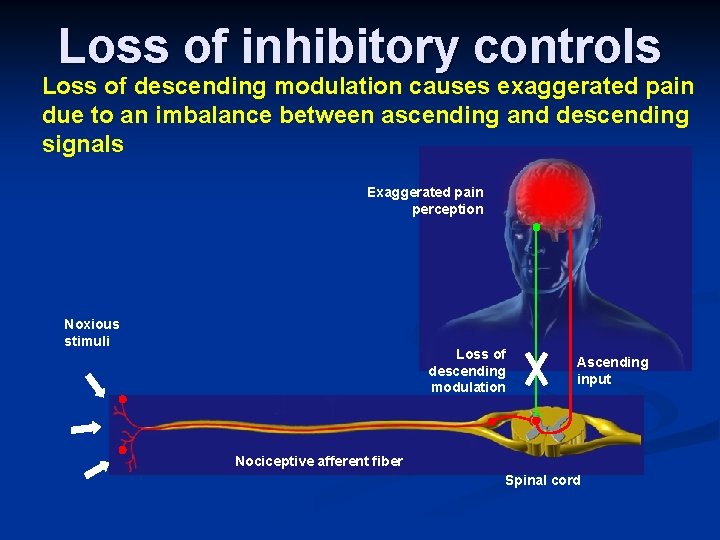
Loss of inhibitory controls Loss of descending modulation causes exaggerated pain due to an imbalance between ascending and descending signals Exaggerated pain perception Noxious stimuli Loss of descending modulation Ascending input Nociceptive afferent fiber Spinal cord
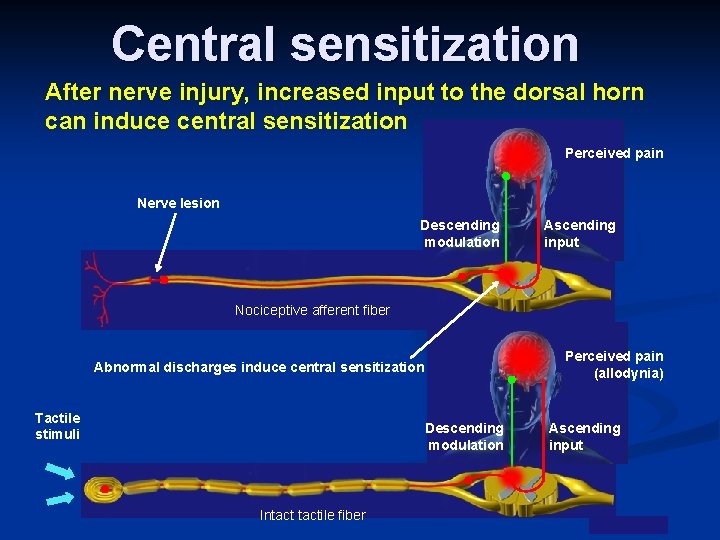
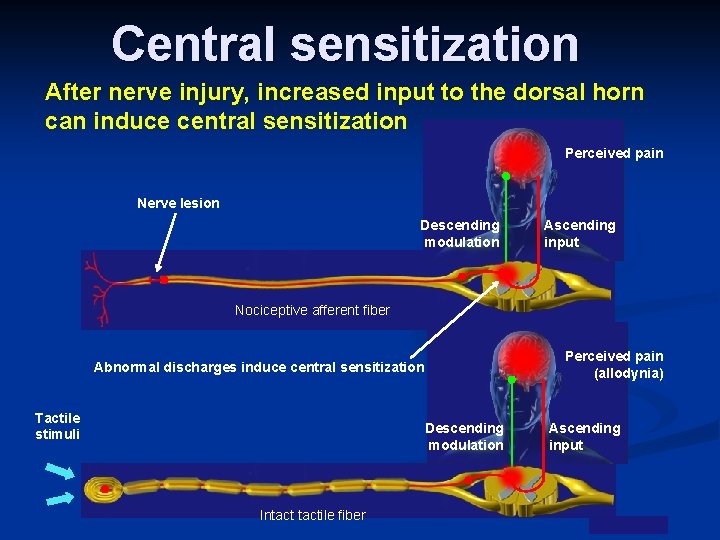
Central sensitization After nerve injury, increased input to the dorsal horn can induce central sensitization Perceived pain Nerve lesion Descending modulation Ascending input Nociceptive afferent fiber Perceived pain (allodynia) Abnormal discharges induce central sensitization Tactile stimuli Descending modulation Intactile fiber Ascending input
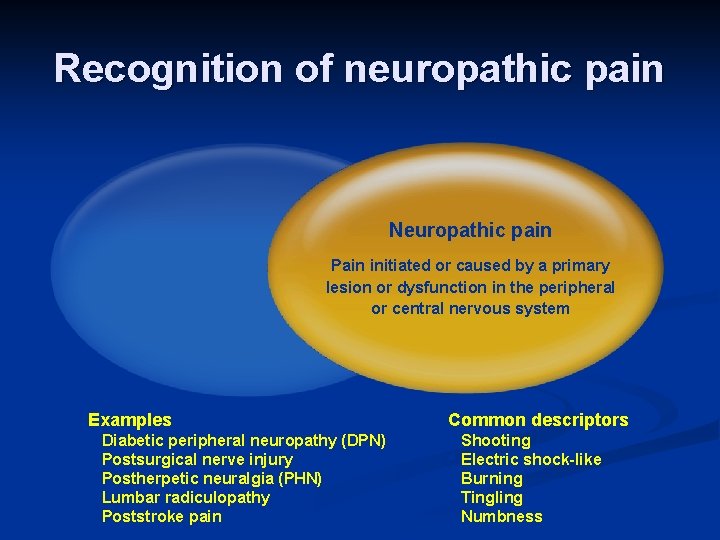
Recognition of neuropathic pain Neuropathic pain Pain initiated or caused by a primary lesion or dysfunction in the peripheral or central nervous system Examples • • • Diabetic peripheral neuropathy (DPN) Postsurgical nerve injury Postherpetic neuralgia (PHN) Lumbar radiculopathy Poststroke pain Common descriptors • • • Shooting Electric shock-like Burning Tingling Numbness
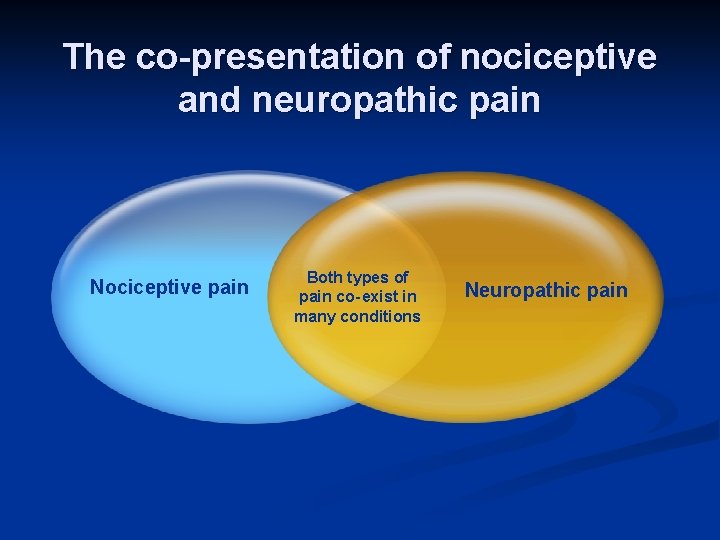
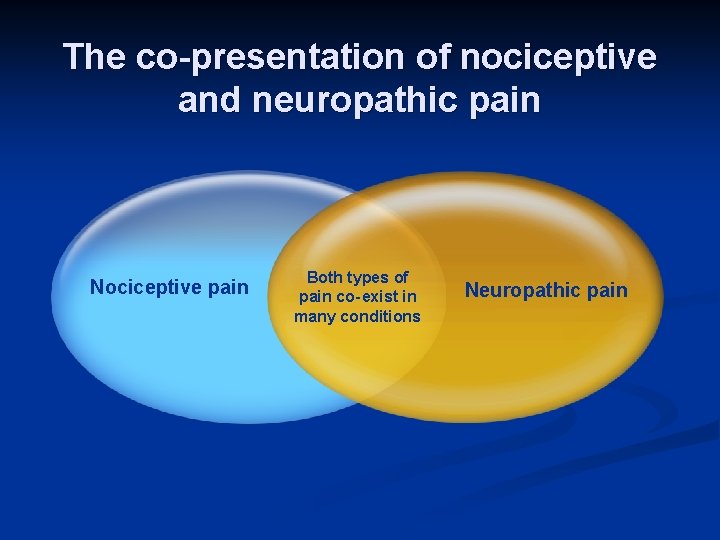
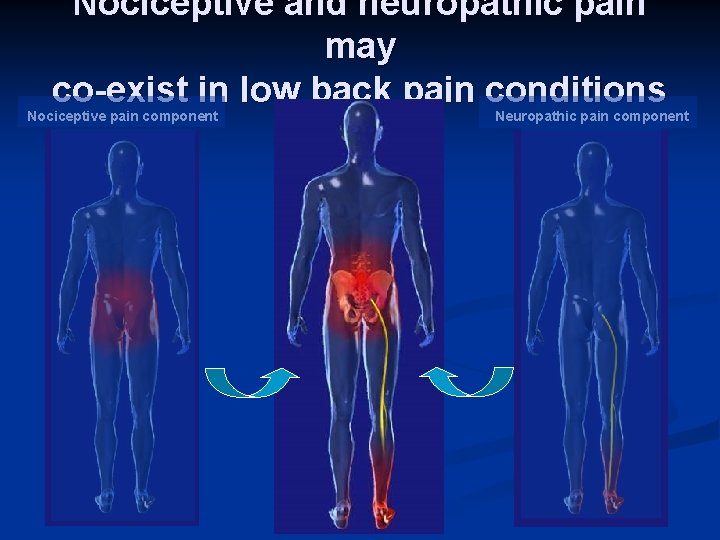
The co-presentation of nociceptive and neuropathic pain Nociceptive pain Both types of pain co- exist in many conditions Neuropathic pain
Co-existence of nociceptive and neuropathic pain • Co-existence of pain types has been referred to as either a “mixed” or “combined” pain state • Examples include low back pain associated with radiculopathy, cancer pain and carpal tunnel syndrome • Effective management requires a broader therapeutic approach to relieve both the nociceptive and neuropathic pain components
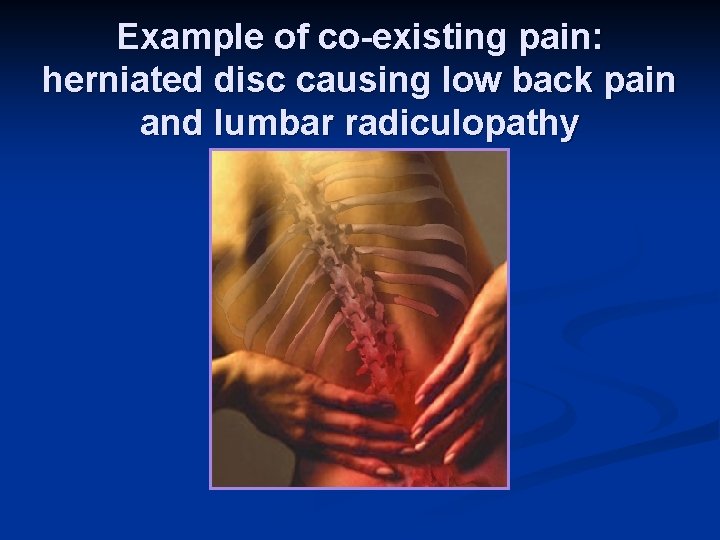
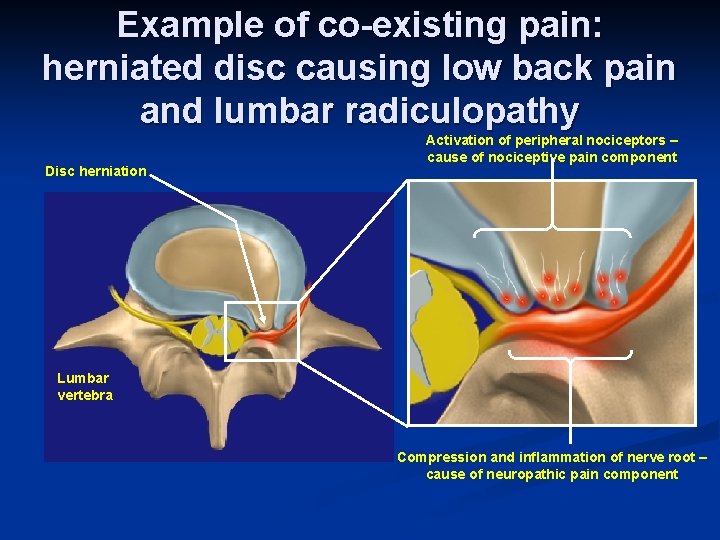
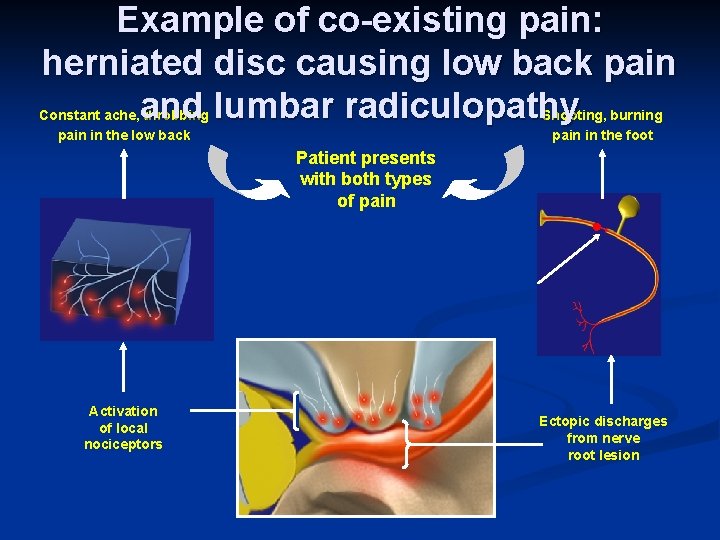
Example of co-existing pain: herniated disc causing low back pain and lumbar radiculopathy
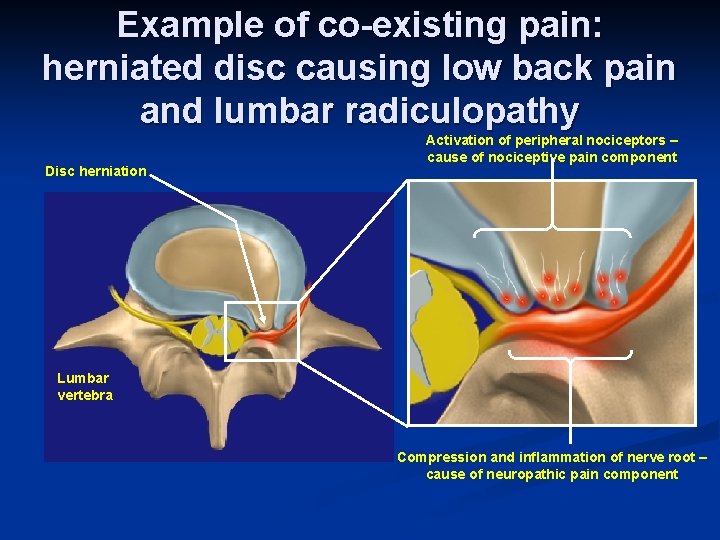
Example of co-existing pain: herniated disc causing low back pain and lumbar radiculopathy Disc herniation Activation of peripheral nociceptors – cause of nociceptive pain component Lumbar vertebra Compression and inflammation of nerve root – cause of neuropathic pain component
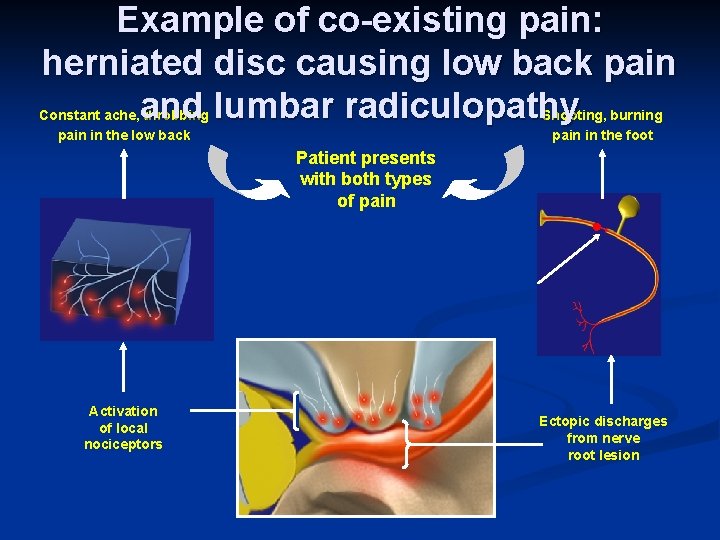
Example of co-existing pain: herniated disc causing low back pain and lumbar radiculopathy Constant ache, throbbing pain in the low back Shooting, burning pain in the foot Patient presents with both types of pain Lesion Activation of local nociceptors Ectopic discharges from nerve root lesion
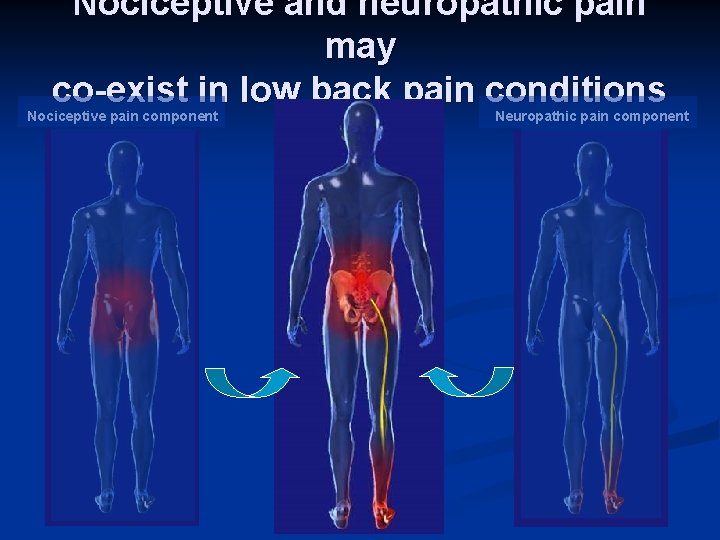
Nociceptive and neuropathic pain may co-exist in low back pain conditions Nociceptive pain component Neuropathic pain component
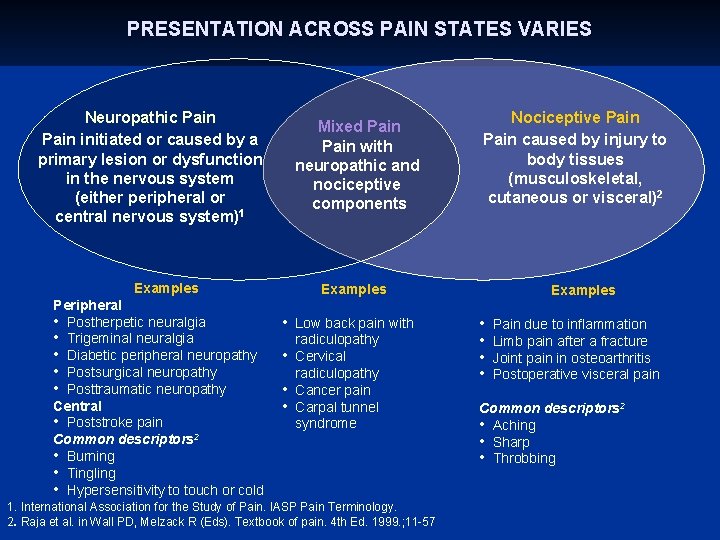
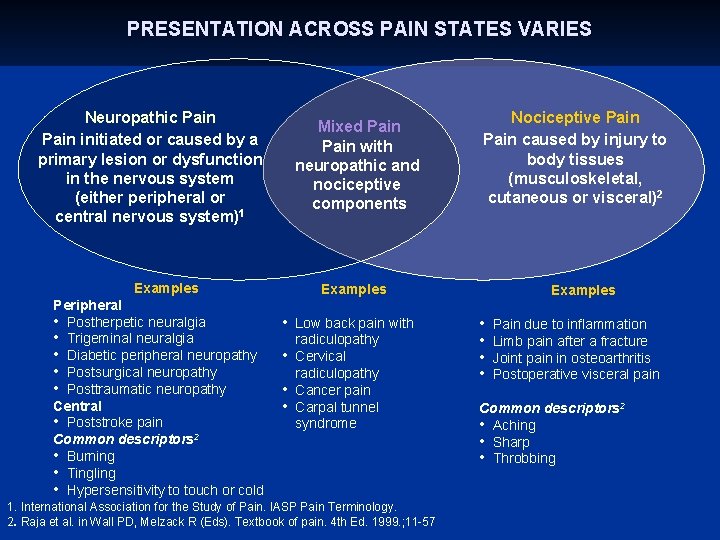
PRESENTATION ACROSS PAIN STATES VARIES Neuropathic Pain initiated or caused by a primary lesion or dysfunction in the nervous system (either peripheral or central nervous system)1 Mixed Pain with neuropathic and nociceptive components Examples Peripheral • Postherpetic neuralgia • Trigeminal neuralgia • Diabetic peripheral neuropathy • Postsurgical neuropathy • Posttraumatic neuropathy Central • Poststroke pain Common descriptors 2 • Burning • Tingling • Hypersensitivity to touch or cold Nociceptive Pain caused by injury to body tissues (musculoskeletal, cutaneous or visceral)2 Examples • Low back pain with • • • radiculopathy Cervical radiculopathy Cancer pain Carpal tunnel syndrome 1. International Association for the Study of Pain. IASP Pain Terminology. 2. Raja et al. in Wall PD, Melzack R (Eds). Textbook of pain. 4 th Ed. 1999. ; 11 -57 Examples • • Pain due to inflammation Limb pain after a fracture Joint pain in osteoarthritis Postoperative visceral pain Common descriptors 2 • Aching • Sharp • Throbbing
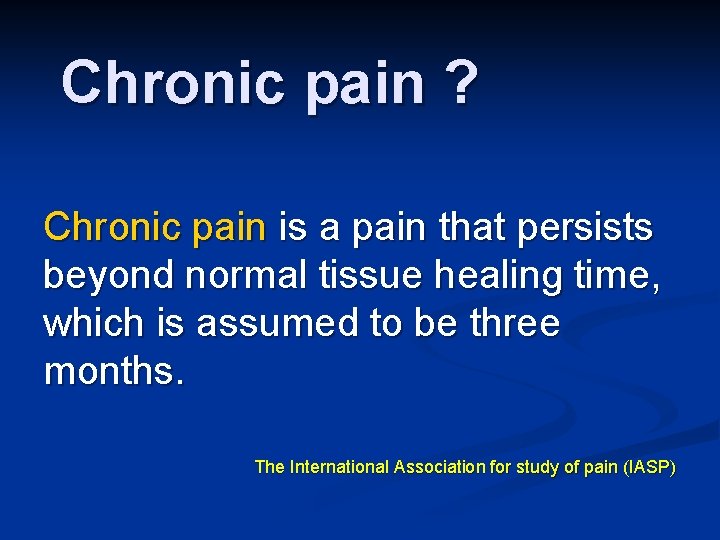
Chronic pain ? Chronic pain is a pain that persists beyond normal tissue healing time, which is assumed to be three months. The International Association for study of pain (IASP)
panthom pain
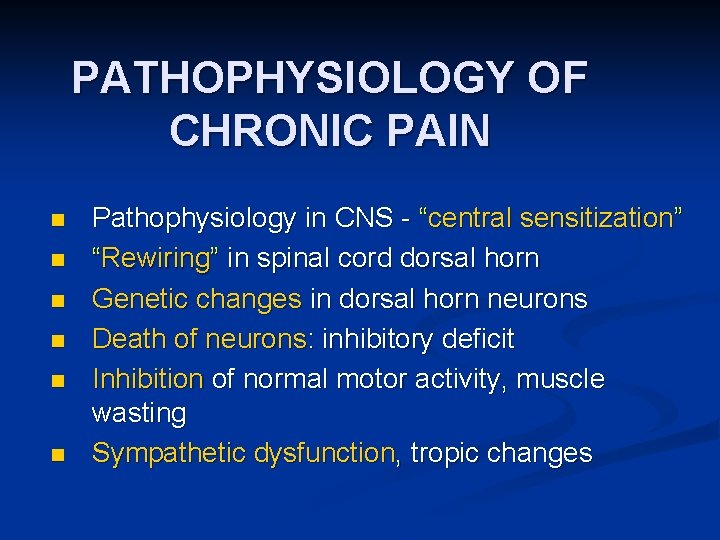
PATHOPHYSIOLOGY OF CHRONIC PAIN n n n Pathophysiology in CNS - “central sensitization” “Rewiring” in spinal cord dorsal horn Genetic changes in dorsal horn neurons Death of neurons: inhibitory deficit Inhibition of normal motor activity, muscle wasting Sympathetic dysfunction, tropic changes
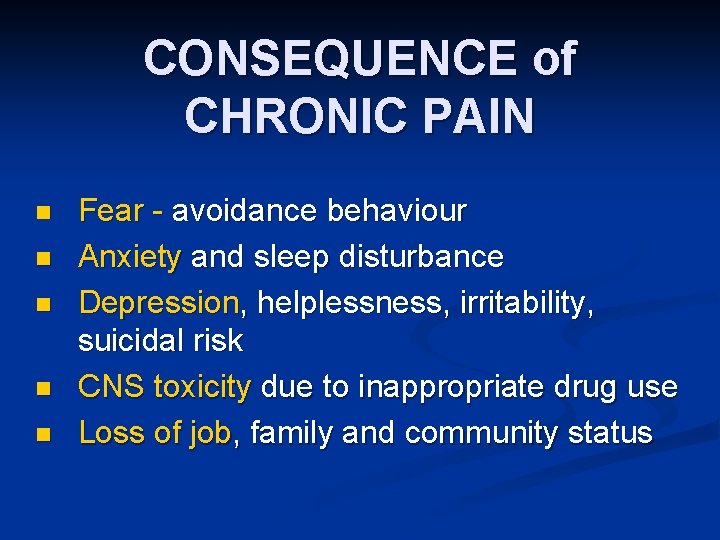
CONSEQUENCE of CHRONIC PAIN n n n Fear - avoidance behaviour Anxiety and sleep disturbance Depression, helplessness, irritability, suicidal risk CNS toxicity due to inappropriate drug use Loss of job, family and community status
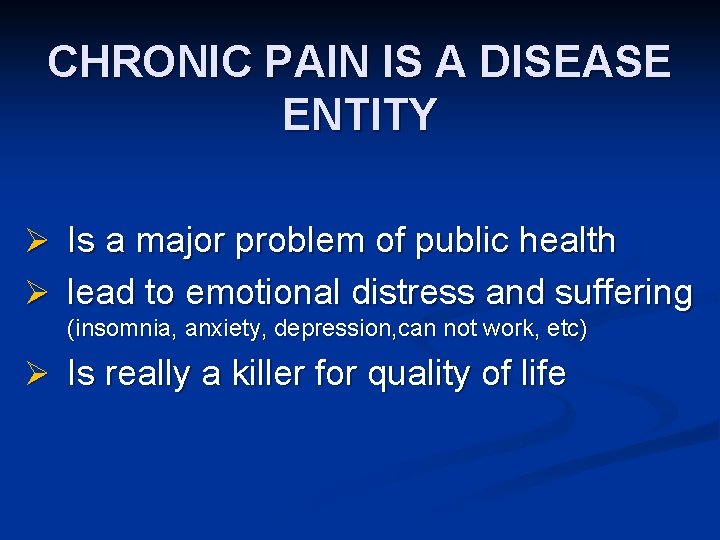
CHRONIC PAIN IS A DISEASE ENTITY Ø Is a major problem of public health Ø lead to emotional distress and suffering (insomnia, anxiety, depression, can not work, etc) Ø Is really a killer for quality of life
Conclution 1. -Pain is a very subjective feeling -Pain is what ever the patient says 2. -Only nociceptive pain is respond to NSAID (cox 1 or cox 2) 3. -Neurophatic pain do not respond to NSAID but it may respond to antidepressants or anticonvulsants may be opioid. 4. - Chronic pain, is pain beyond naciceptive, occur after healing process, difficult to treat and reduced quality of life.
Take Home Message It’s important to more understanding PAIN, type and characteristic of pain. . Because… In many parts of Indonesia : Many people may die in pain, but Many more people dying with pain, Even many more people living in pain This is our task to help them as a Doctor
The task of a doctor: n n n TO CURE IS SOMETIMES TO TREAT IS OFTEN TO COMFORT IS ALWAYS A. Pare (1598)
 Fentanyl buccal
Fentanyl buccal Neuropathic pain
Neuropathic pain Neuropathic pain
Neuropathic pain Non nsaid
Non nsaid Neuropathic pain
Neuropathic pain Painful neuropathy
Painful neuropathy Nociceptive pain
Nociceptive pain Nociceptive pain
Nociceptive pain Nociceptive pain
Nociceptive pain Nociceptive pain
Nociceptive pain Pain ascending pathway
Pain ascending pathway Epicritic pain
Epicritic pain Nociceptor stimulus
Nociceptor stimulus Crude touch
Crude touch Nociceptive
Nociceptive Pain
Pain David lewis mad pain and martian pain
David lewis mad pain and martian pain Are sore breasts and cramps a sign of pregnancy
Are sore breasts and cramps a sign of pregnancy Signs of period vs pregnancy
Signs of period vs pregnancy Logo nur ihsan
Logo nur ihsan Nur adnan
Nur adnan Obat meroyan
Obat meroyan Nur hidayat
Nur hidayat Dr nur syahid
Dr nur syahid Nur ahmad husin
Nur ahmad husin Je desto beispiel
Je desto beispiel Niken satuti nur handayani
Niken satuti nur handayani Nur 102
Nur 102 Aber slovosled
Aber slovosled Parts of debate
Parts of debate Frösche lustig
Frösche lustig Andini nur nabila
Andini nur nabila Crisostomo ibarra lines in noli me tangere tagalog
Crisostomo ibarra lines in noli me tangere tagalog Nur alam shah
Nur alam shah Nur 102
Nur 102 Dr nur ahmad tabri
Dr nur ahmad tabri Nur
Nur Astria nur irfansyah
Astria nur irfansyah Definisi kartografi
Definisi kartografi Der jürgen klinsmann und ich wir sind ein gutes trio
Der jürgen klinsmann und ich wir sind ein gutes trio Nur akar
Nur akar Nur 102
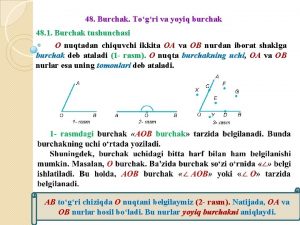
Nur 102 Yoyiq burchak necha gradusga teng
Yoyiq burchak necha gradusga teng Nur ahmad husin
Nur ahmad husin Gedichte 6. klasse
Gedichte 6. klasse Dr nur rofiah
Dr nur rofiah Iswari nur hidayati
Iswari nur hidayati Nur 680
Nur 680 Letak nur muhammad dalam tubuh manusia
Letak nur muhammad dalam tubuh manusia Hanif nur widhiyanti
Hanif nur widhiyanti Hanif nur widhiyanti
Hanif nur widhiyanti Nur azizah umy
Nur azizah umy Nur alia file upload
Nur alia file upload Ich liege nur noch rum
Ich liege nur noch rum In den kopf schauen
In den kopf schauen Nur endah januarti
Nur endah januarti Iim ibrahim nur
Iim ibrahim nur Nur endah januarti
Nur endah januarti Nur dağı hira mağarası nerede
Nur dağı hira mağarası nerede Nur muhammad taraki
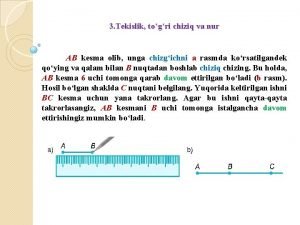
Nur muhammad taraki Kesma va nur
Kesma va nur Dr nur mohammad hadi zahalan
Dr nur mohammad hadi zahalan Nur verrückte habens eilig
Nur verrückte habens eilig Die gazelle rilke
Die gazelle rilke Struktur mikrokontroler
Struktur mikrokontroler Levy olivia nur
Levy olivia nur Nur aras
Nur aras Nur 211 final exam
Nur 211 final exam Penyelesaian dari persamaan 16m=64 adalah
Penyelesaian dari persamaan 16m=64 adalah Meral güneş ergin
Meral güneş ergin Salma nur azizah
Salma nur azizah