Pain Classification Nociceptive Neuropathic Central and Mixed Rachael
- Slides: 13
Pain Classification: Nociceptive, Neuropathic, Central and Mixed Rachael Rzasa Lynn, MD Chronic Pain Zoom Webinar 2 December 2015
Definitions • Most basic = neurophysiologic classification – based on presumed mechanism of pain. • Simplified, there are 2 types of pain: – nociceptive pain – non-nociceptive pain • Neuropathic pain • Idiopathic pain – ≠psychogenic pain!
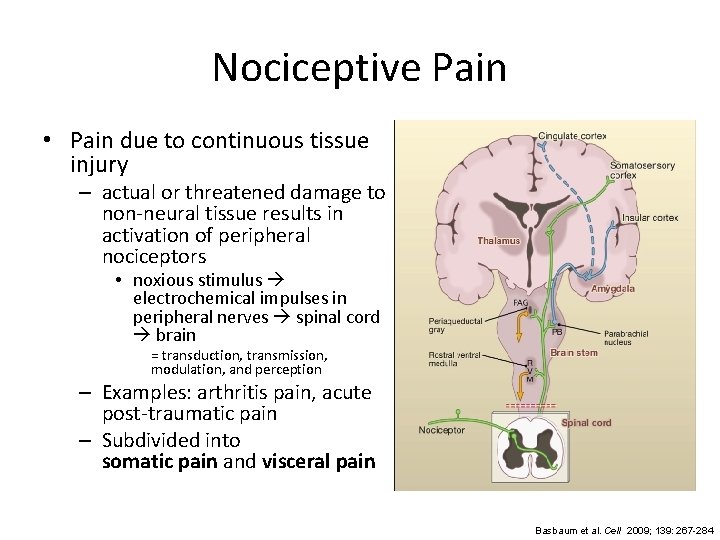
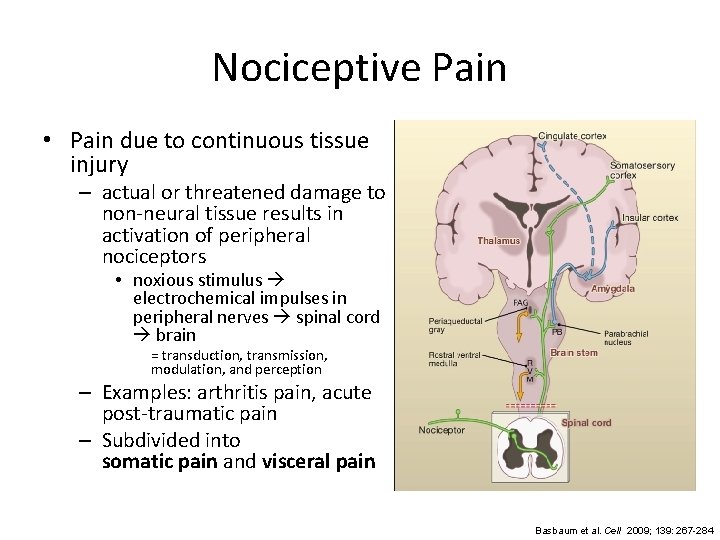
Nociceptive Pain • Pain due to continuous tissue injury – actual or threatened damage to non-neural tissue results in activation of peripheral nociceptors • noxious stimulus electrochemical impulses in peripheral nerves spinal cord brain = transduction, transmission, modulation, and perception – Examples: arthritis pain, acute post-traumatic pain – Subdivided into somatic pain and visceral pain Basbaum et al. Cell 2009; 139: 267 -284
Nociceptive Pain • Somatic pain – excitation and/or sensitization of nociceptors in tissues such as bone, periarticular soft tissue, joints, and muscles • Well localized • Intermittent or constant • “aching, ” “stabbing, ” “gnawing, ” “throbbing”
Nociceptive Pain • Visceral pain – Not produced by all visceral organs • Liver, kidney, most solid viscera, and lung parenchyma are not sensitive to pain. – Not always created by visceral injury – Cutting intestine causes no pain, stretching of the bladder is painful – Diffuse and poorly localized • No separate visceral sensory pathway and low proportion of afferent nerve fibers from viscera • Intermittent or constant • “dull, ” “colicky, ” “squeezing” – Referrs to other locations. – Accompanied by motor and autonomic reflexes • Eg, nausea, vomiting, muscle tension, etc.
Neuropathic Pain • “Pain arising as a direct consequence of a lesion or disease affecting the somatosensory system. ” – at any point(s) within the somatosensory pathways – Pain from lesion/disease sustained by aberrant processing in the peripheral and/or central nervous system – typically described as “sharp” or “burning” • This is a clinical description (NOT a diagnosis) – According to IASP, • “this requires a demonstrable lesion or a disease that satisfies established neurological diagnostic criteria. ” • “The presence of symptoms or signs (e. g. , touch-evoked pain) alone does not justify the use of the term neuropathic. ” • “It is common…that diagnostic testing may yield inconclusive or even inconsistent data. In such instances, clinical judgment is required to reduce the totality of findings in a patient into one putative diagnosis or concise group of diagnoses. ”
Neuropathic Pain • Subsets – Peripherally generated pain: • involves such cervical or lumbar radiculopathy, spinal nerve lesions, and brachial or lumbosacral plexopathies – Centrally generated pain: • involves injury to the central nervous system at the level of the spinal cord or above. – Sympathetically maintained pain: • may be generated peripherally or centrally • characterized by localized autonomic dysregulation – vasomotor or sudomotor changes, edema, sweating, trophic changes including atrophy – Complex Regional Pain Syndrome
Central Pain States • Central pain: Pain initiated or caused by a primary lesion or dysfunction in the central nervous system. – Can be produced by an type of vascular, demyelinating, infectious, inflammatory, or traumatic lesion in the brain or spinal cord • Eg, post-stroke pain • Central sensitization: Increase in the excitability of neurons in the spinal cord. – Increased responsiveness of nociceptive neurons in the central nervous system • Increased response to input to which they normally respond • Activation in response to subthreshold input
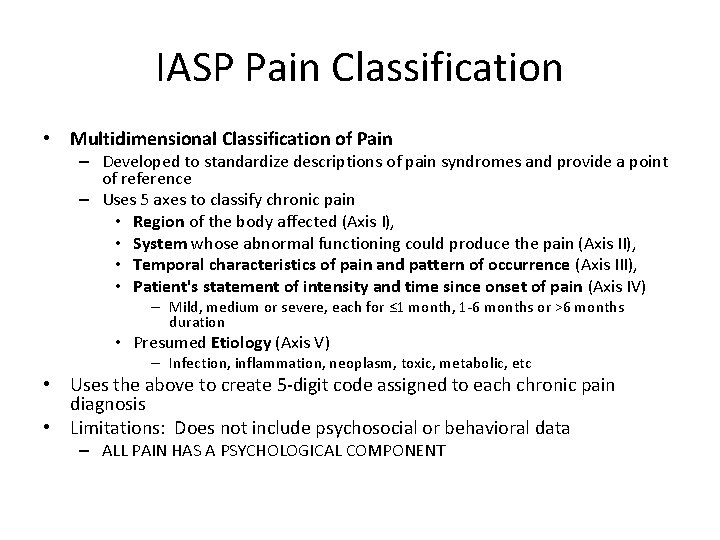
IASP Pain Classification • Multidimensional Classification of Pain – Developed to standardize descriptions of pain syndromes and provide a point of reference – Uses 5 axes to classify chronic pain • Region of the body affected (Axis I), • System whose abnormal functioning could produce the pain (Axis II), • Temporal characteristics of pain and pattern of occurrence (Axis III), • Patient's statement of intensity and time since onset of pain (Axis IV) – Mild, medium or severe, each for ≤ 1 month, 1 -6 months or >6 months duration • Presumed Etiology (Axis V) – Infection, inflammation, neoplasm, toxic, metabolic, etc • Uses the above to create 5 -digit code assigned to each chronic pain diagnosis • Limitations: Does not include psychosocial or behavioral data – ALL PAIN HAS A PSYCHOLOGICAL COMPONENT
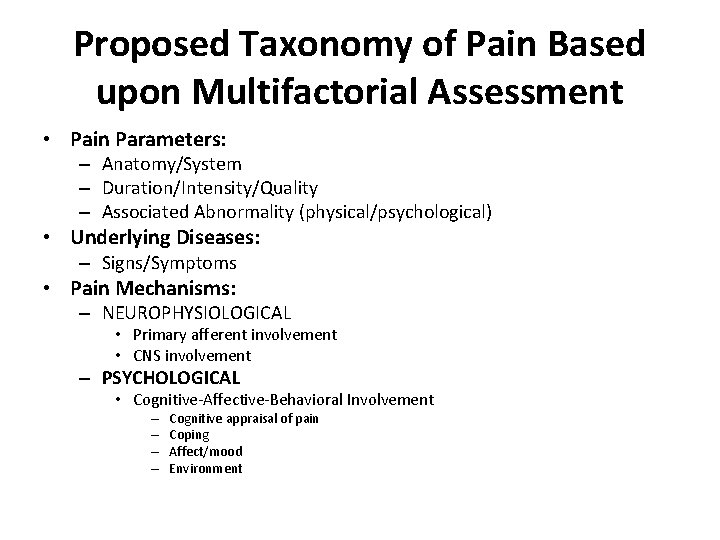
Proposed Taxonomy of Pain Based upon Multifactorial Assessment • Pain Parameters: – Anatomy/System – Duration/Intensity/Quality – Associated Abnormality (physical/psychological) • Underlying Diseases: – Signs/Symptoms • Pain Mechanisms: – NEUROPHYSIOLOGICAL • Primary afferent involvement • CNS involvement – PSYCHOLOGICAL • Cognitive-Affective-Behavioral Involvement – – Cognitive appraisal of pain Coping Affect/mood Environment
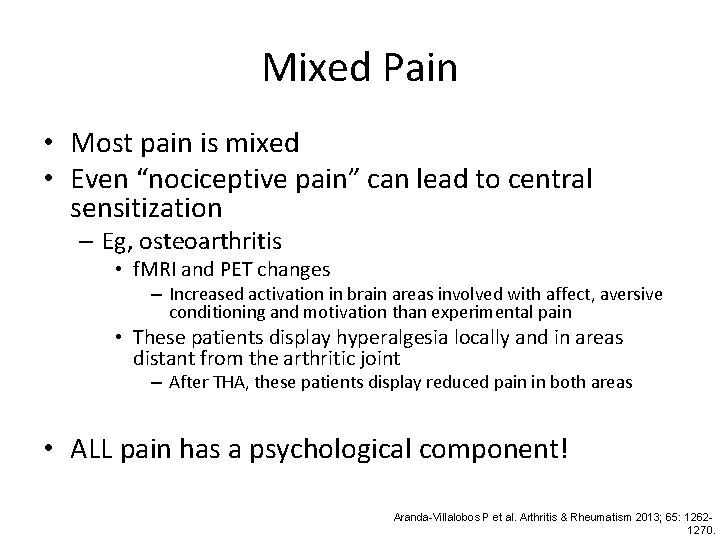
Mixed Pain • Most pain is mixed • Even “nociceptive pain” can lead to central sensitization – Eg, osteoarthritis • f. MRI and PET changes – Increased activation in brain areas involved with affect, aversive conditioning and motivation than experimental pain • These patients display hyperalgesia locally and in areas distant from the arthritic joint – After THA, these patients display reduced pain in both areas • ALL pain has a psychological component! Aranda-Villalobos P et al. Arthritis & Rheumatism 2013; 65: 12621270.
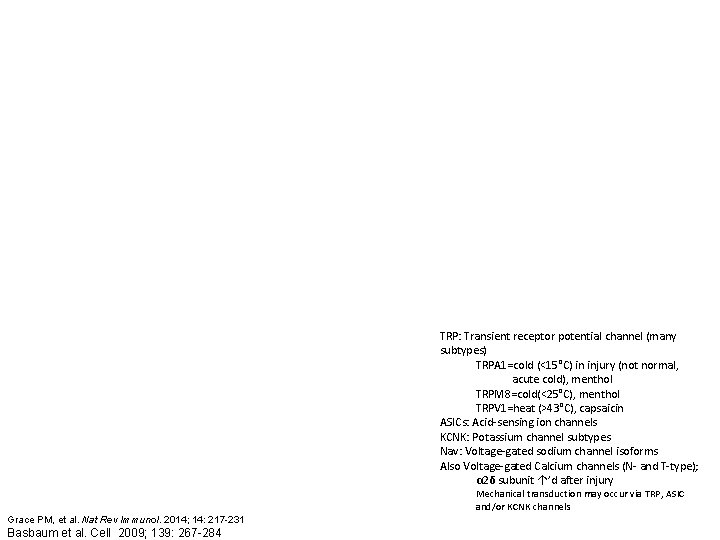
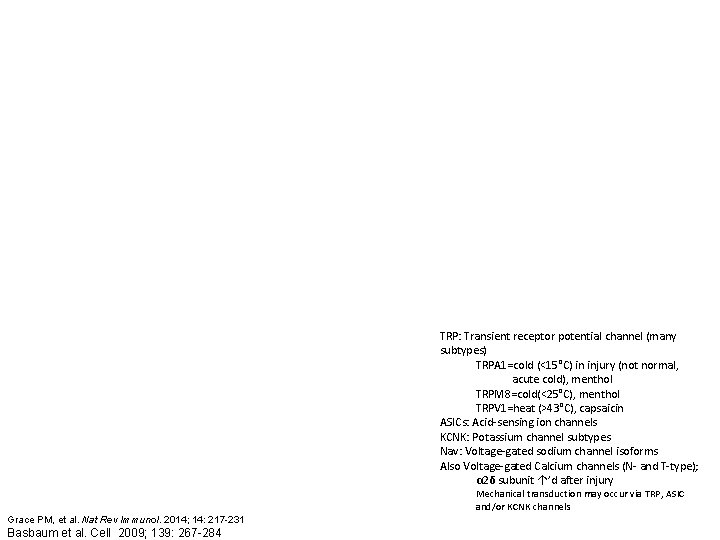
TRP: Transient receptor potential channel (many subtypes) TRPA 1=cold (<15°C) in injury (not normal, acute cold), menthol TRPM 8=cold(<25°C), menthol TRPV 1=heat (>43°C), capsaicin ASICs: Acid-sensing ion channels KCNK: Potassium channel subtypes Nav: Voltage-gated sodium channel isoforms Also Voltage-gated Calcium channels (N- and T-type); α 2δ subunit ↑’d after injury Mechanical transduction may occur via TRP, ASIC and/or KCNK channels Grace PM, et al. Nat Rev Immunol. 2014; 14: 217 -231 Basbaum et al. Cell 2009; 139: 267 -284
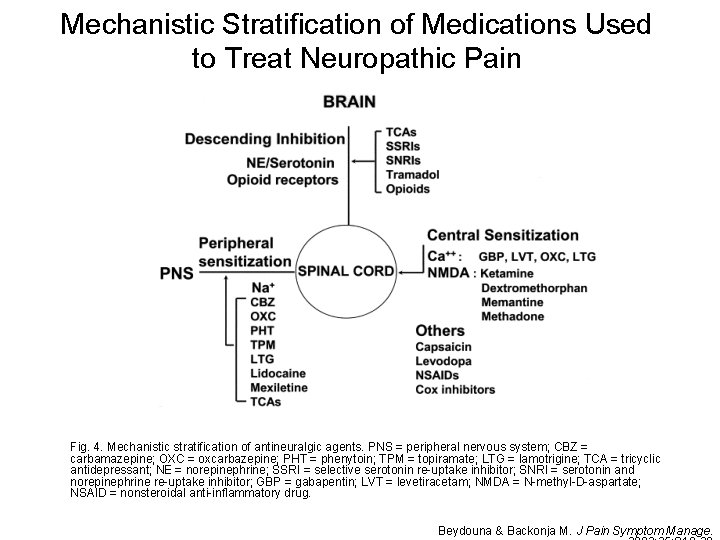
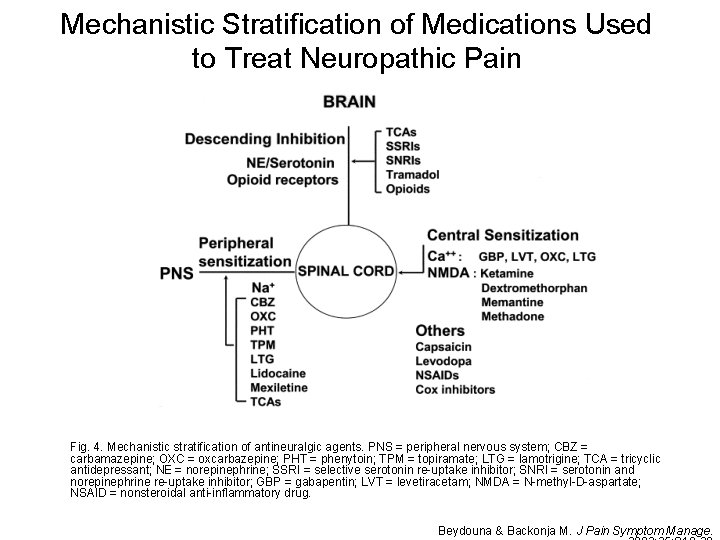
Mechanistic Stratification of Medications Used to Treat Neuropathic Pain Fig. 4. Mechanistic stratification of antineuralgic agents. PNS = peripheral nervous system; CBZ = carbamazepine; OXC = oxcarbazepine; PHT = phenytoin; TPM = topiramate; LTG = lamotrigine; TCA = tricyclic antidepressant; NE = norepinephrine; SSRI = selective serotonin re-uptake inhibitor; SNRI = serotonin and norepinephrine re-uptake inhibitor; GBP = gabapentin; LVT = levetiracetam; NMDA = N-methyl-D-aspartate; NSAID = nonsteroidal anti-inflammatory drug. Beydouna & Backonja M. J Pain Symptom Manage.