Treatment of neuropathic pain Low technology treatment methods

- Slides: 30

Treatment of neuropathic pain “Low technology treatment methods”
I General aspect of management of neuropathic pain
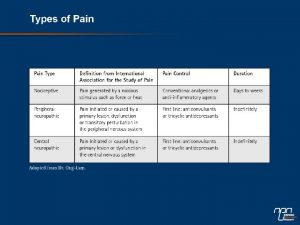
IASP definition of neuropathic pain Neuropathic pain is a pain caused by a lesion or disease of the somatosensory system. www. iasp-pain. org/resources/pain. Definition
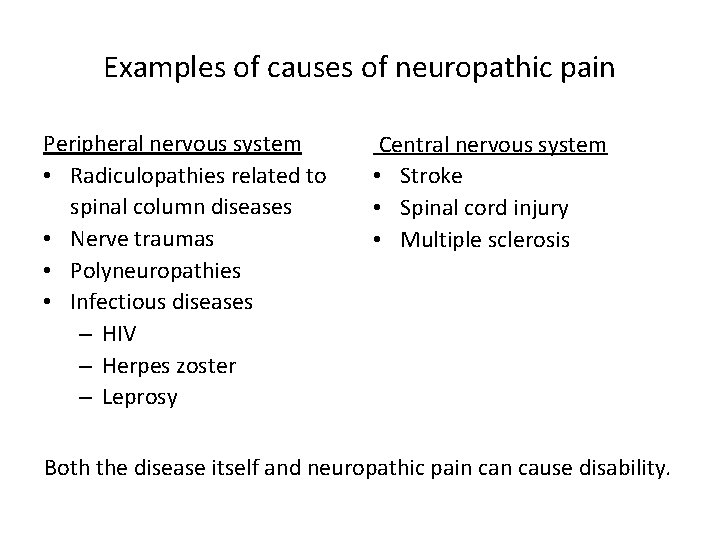
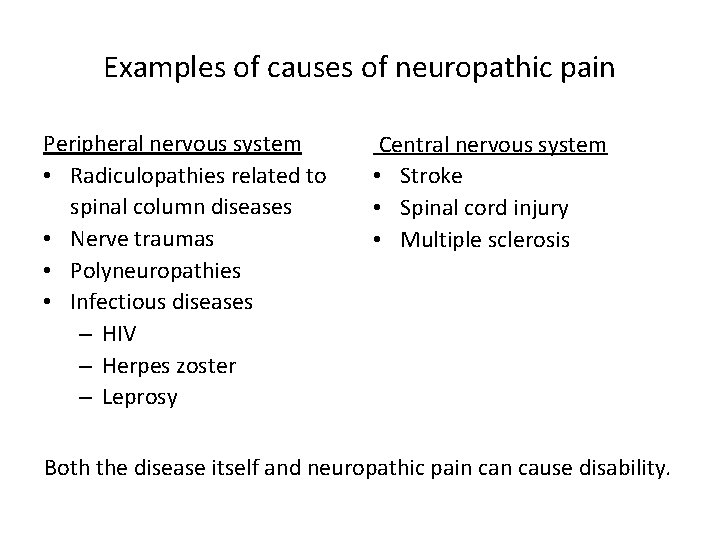
Examples of causes of neuropathic pain Peripheral nervous system • Radiculopathies related to spinal column diseases • Nerve traumas • Polyneuropathies • Infectious diseases – HIV – Herpes zoster – Leprosy Central nervous system • Stroke • Spinal cord injury • Multiple sclerosis Both the disease itself and neuropathic pain cause disability.
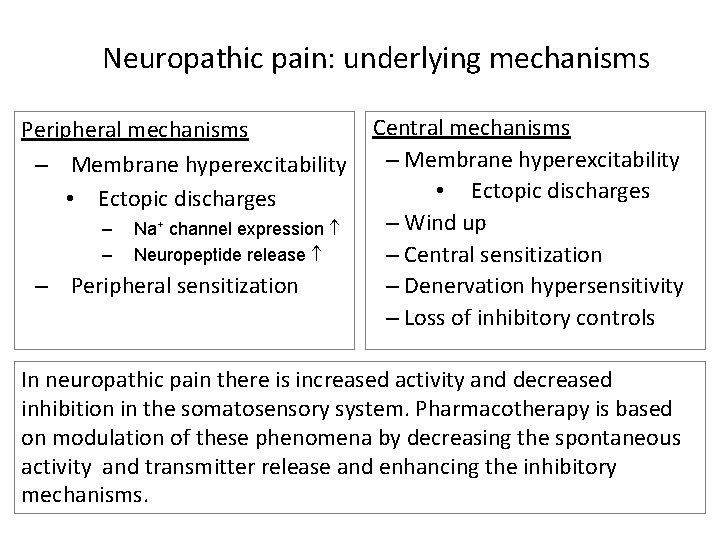
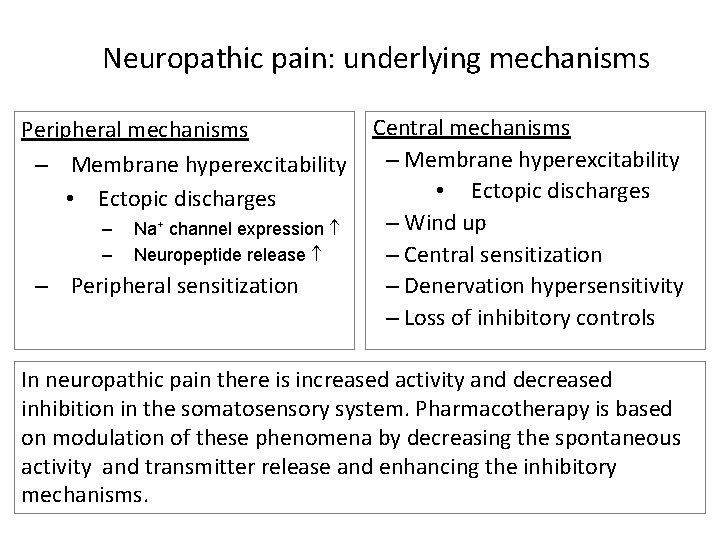
Neuropathic pain: underlying mechanisms Peripheral mechanisms – Membrane hyperexcitability • Ectopic discharges – – Na+ channel expression Neuropeptide release – Peripheral sensitization Central mechanisms – Membrane hyperexcitability • Ectopic discharges – Wind up – Central sensitization – Denervation hypersensitivity – Loss of inhibitory controls In neuropathic pain there is increased activity and decreased inhibition in the somatosensory system. Pharmacotherapy is based on modulation of these phenomena by decreasing the spontaneous activity and transmitter release and enhancing the inhibitory mechanisms.
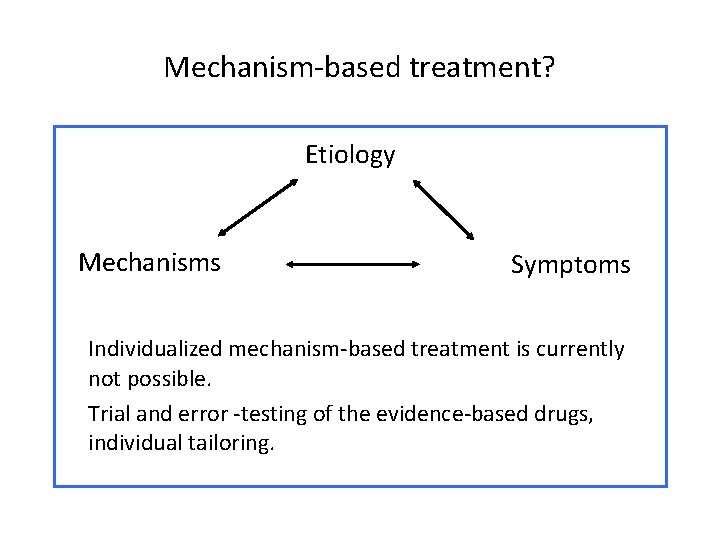
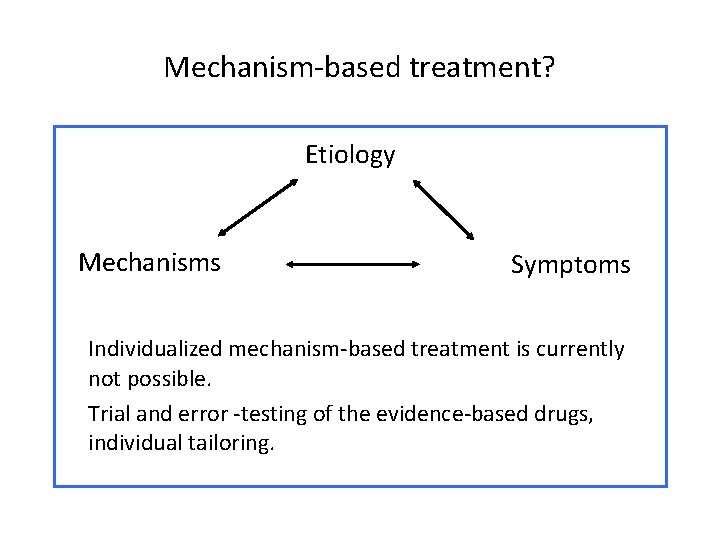
Mechanism-based treatment? Etiology Mechanisms Symptoms Individualized mechanism-based treatment is currently not possible. Trial and error -testing of the evidence-based drugs, individual tailoring.
What is expected from a doctor? • To know the concept of neuropathic pain • To be able to recognize neuropathic pain • To be able to diagnose the causative disease and to treat it, if possible (e. g. , diabetes) • To be able to start the first line medication to relieve neuropathic pain • To be able to refer the patient to a specialist, if needed (for diagnostic procedures or treatment)
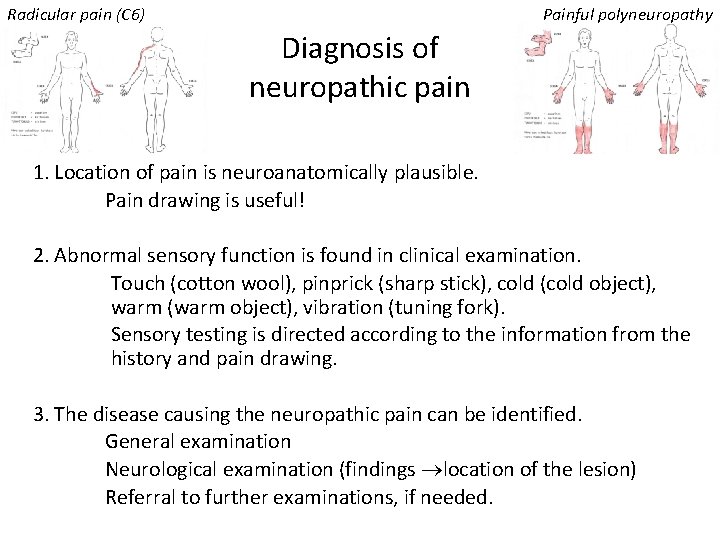
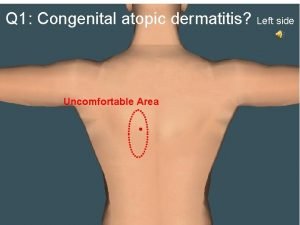
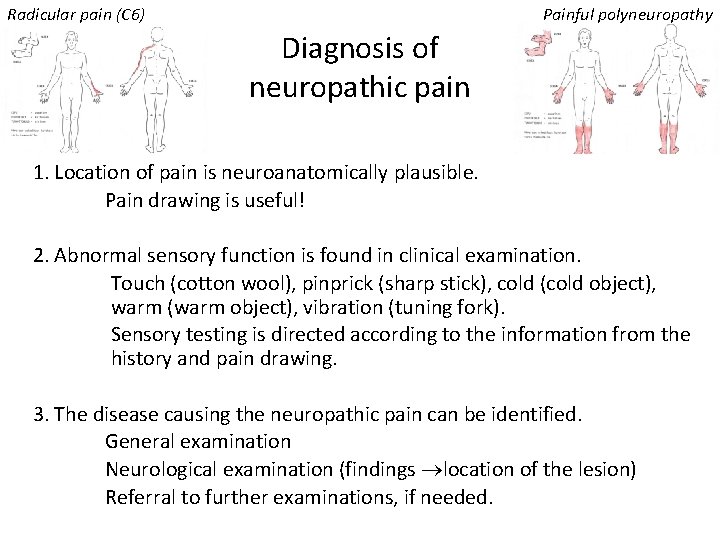
Radicular pain (C 6) Painful polyneuropathy Diagnosis of neuropathic pain 1. Location of pain is neuroanatomically plausible. Pain drawing is useful! 2. Abnormal sensory function is found in clinical examination. Touch (cotton wool), pinprick (sharp stick), cold (cold object), warm (warm object), vibration (tuning fork). Sensory testing is directed according to the information from the history and pain drawing. 3. The disease causing the neuropathic pain can be identified. General examination Neurological examination (findings location of the lesion) Referral to further examinations, if needed.
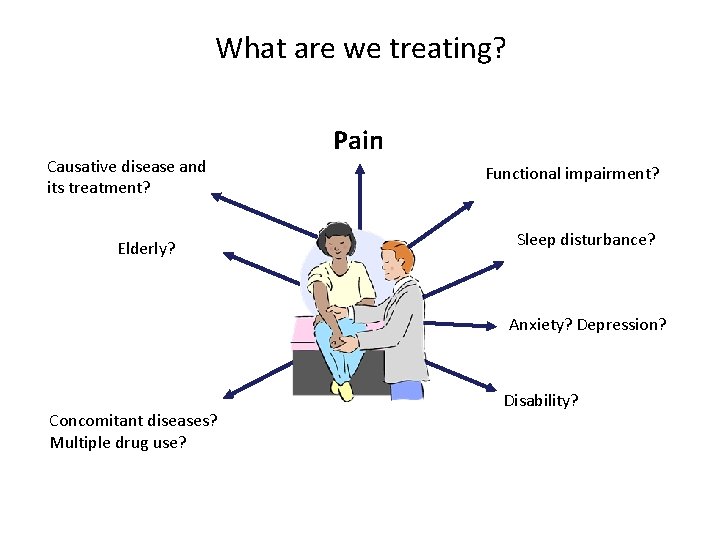
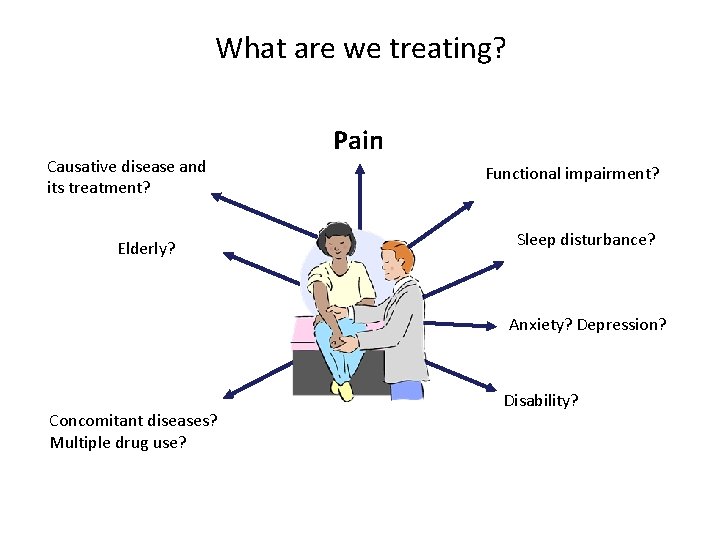
What are we treating? Causative disease and its treatment? Elderly? Pain Functional impairment? Sleep disturbance? Anxiety? Depression? Concomitant diseases? Multiple drug use? Disability?
Information, follow-up, case managment • The patient needs information of the character of the pain and of the causative disease and its treatment • Follow-up and a possibility of the patient to contact the doctor or nurse (the “case-manager”) is important to ensure compliance and safe treatment • Support of the patient is an essential part of the management • Team work is recommended
Pharmacotherapy of neuropathic pain • Pharmacotherapy is the most important treatment for those with moderate or severe pain • Goals: – (partial) pain relief (>50%, >30%) Complete pain relief is exceptional; hence some pain relief is a realistic goal, which needs to be explained to the patient. – functional improvement and better quality of life – better sleep and mood, relief of anxiety • Many patients have some, moderate or intolerable side effects • There are many refractory patients
Principles of pharmacotherapy of neuropathic pain 1) Individual drug selection – Cause of neuropathic pain • Most evidence comes from studies of painful polyneuropathies and postherpetic neuralgia, but in less studied conditions, the drugs with evidence from the best studied conditions are tested – Other medical problems and their medication • Be careful with the contraindications and precautions – cardiac conduction disturbances: don’t select TCAs – urinary retention: don’t select TCAs – uncontrolled blood pressure: don’t select venlafaxine – Previous drug trials • If some drug has been adequately tested previously with poor result, repetition of trial with the same drug is not rational
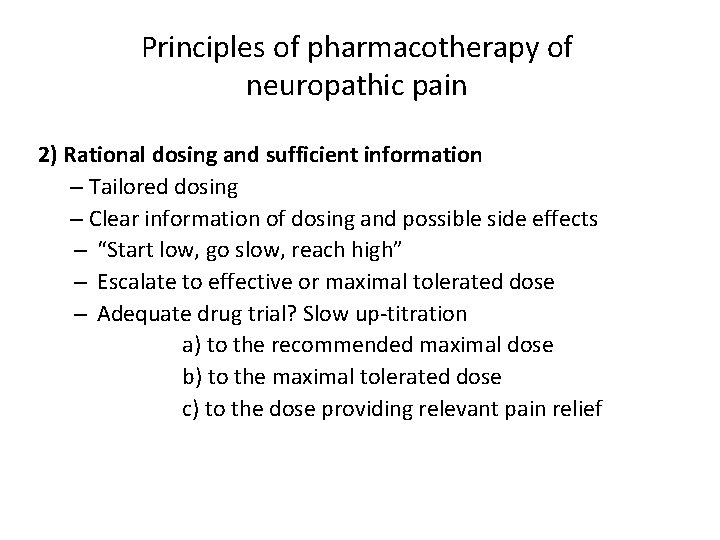
Principles of pharmacotherapy of neuropathic pain 2) Rational dosing and sufficient information – Tailored dosing – Clear information of dosing and possible side effects – “Start low, go slow, reach high” – Escalate to effective or maximal tolerated dose – Adequate drug trial? Slow up-titration a) to the recommended maximal dose b) to the maximal tolerated dose c) to the dose providing relevant pain relief
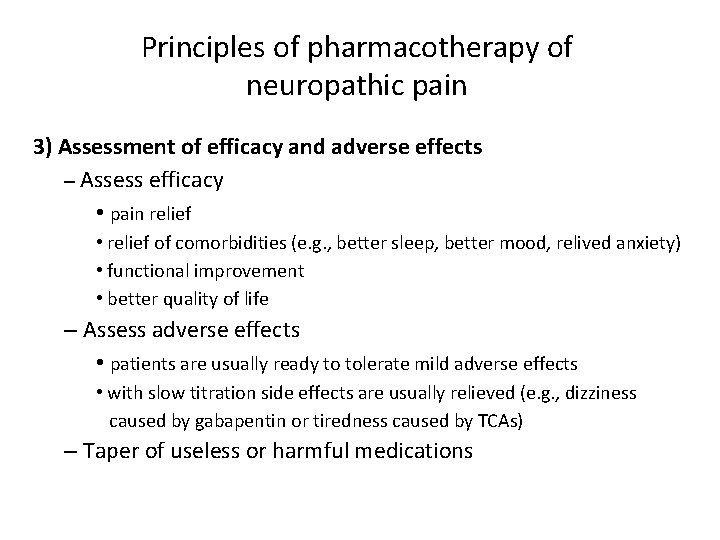
Principles of pharmacotherapy of neuropathic pain 3) Assessment of efficacy and adverse effects – Assess efficacy • pain relief • relief of comorbidities (e. g. , better sleep, better mood, relived anxiety) • functional improvement • better quality of life – Assess adverse effects • patients are usually ready to tolerate mild adverse effects • with slow titration side effects are usually relieved (e. g. , dizziness caused by gabapentin or tiredness caused by TCAs) – Taper of useless or harmful medications
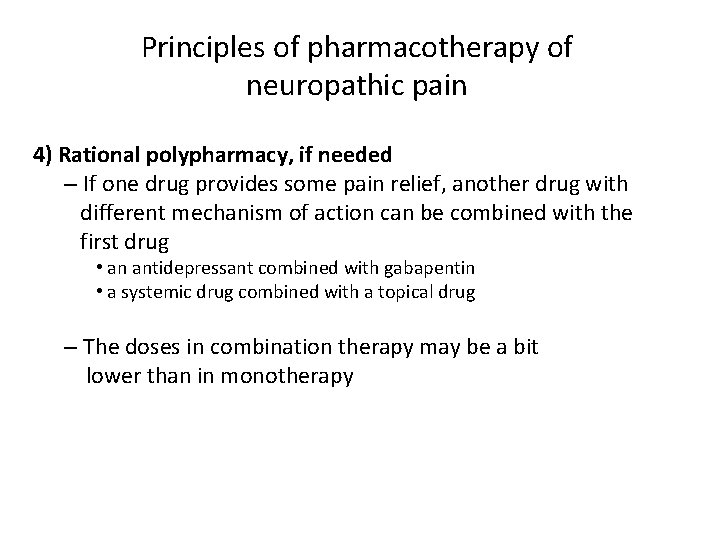
Principles of pharmacotherapy of neuropathic pain 4) Rational polypharmacy, if needed – If one drug provides some pain relief, another drug with different mechanism of action can be combined with the first drug • an antidepressant combined with gabapentin • a systemic drug combined with a topical drug – The doses in combination therapy may be a bit lower than in monotherapy
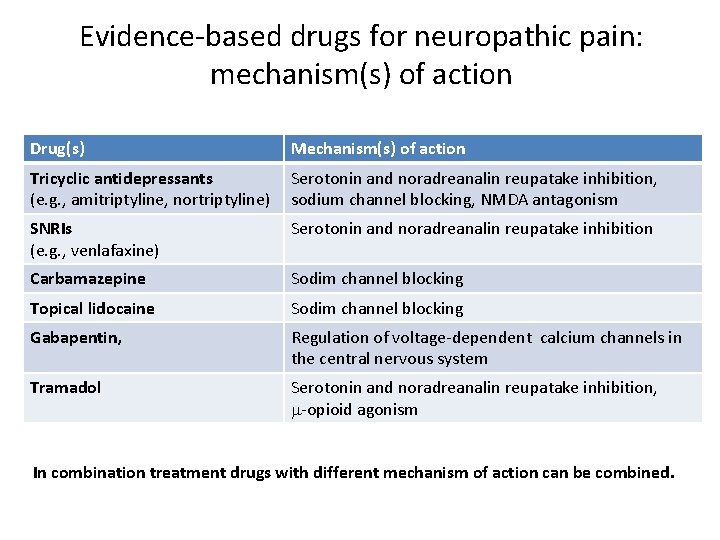
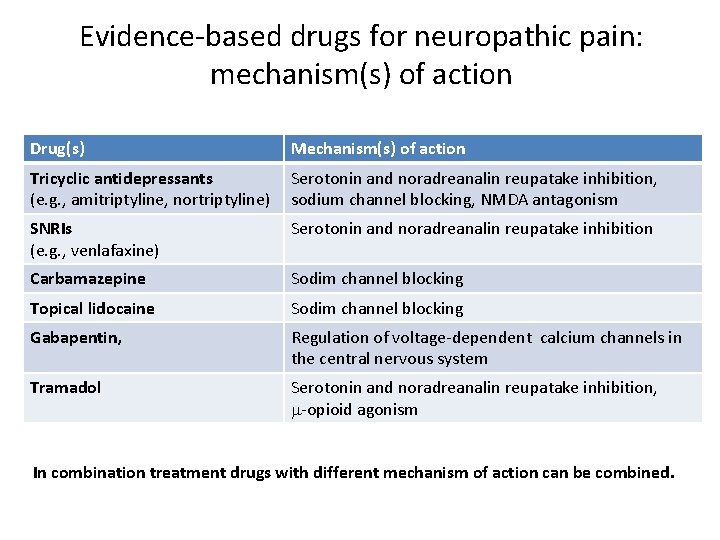
Evidence-based drugs for neuropathic pain: mechanism(s) of action Drug(s) Mechanism(s) of action Tricyclic antidepressants (e. g. , amitriptyline, nortriptyline) Serotonin and noradreanalin reupatake inhibition, sodium channel blocking, NMDA antagonism SNRIs (e. g. , venlafaxine) Serotonin and noradreanalin reupatake inhibition Carbamazepine Sodim channel blocking Topical lidocaine Sodim channel blocking Gabapentin, Regulation of voltage-dependent calcium channels in the central nervous system Tramadol Serotonin and noradreanalin reupatake inhibition, m-opioid agonism In combination treatment drugs with different mechanism of action can be combined.
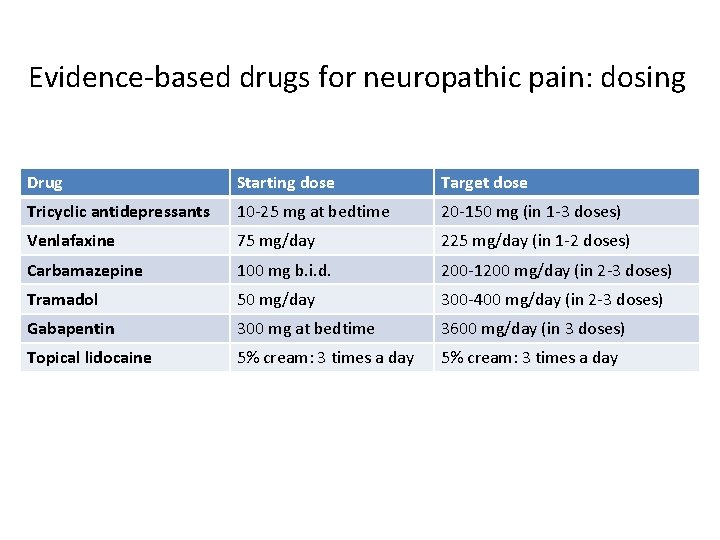
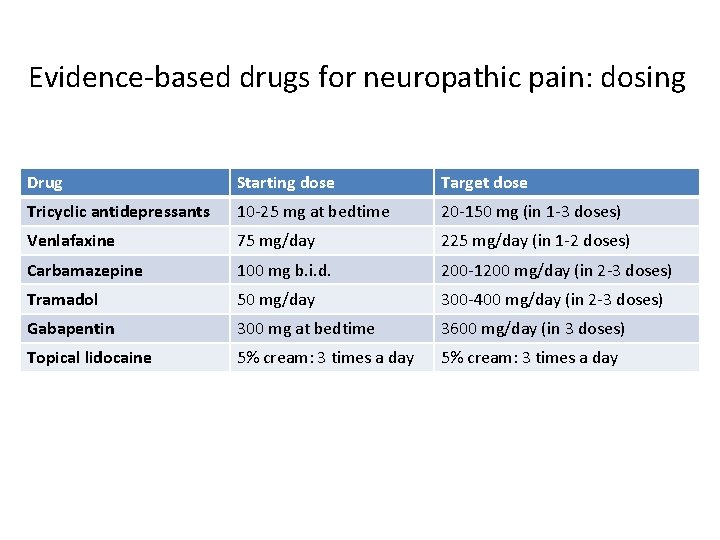
Evidence-based drugs for neuropathic pain: dosing Drug Starting dose Target dose Tricyclic antidepressants 10 -25 mg at bedtime 20 -150 mg (in 1 -3 doses) Venlafaxine 75 mg/day 225 mg/day (in 1 -2 doses) Carbamazepine 100 mg b. i. d. 200 -1200 mg/day (in 2 -3 doses) Tramadol 50 mg/day 300 -400 mg/day (in 2 -3 doses) Gabapentin 300 mg at bedtime 3600 mg/day (in 3 doses) Topical lidocaine 5% cream: 3 times a day
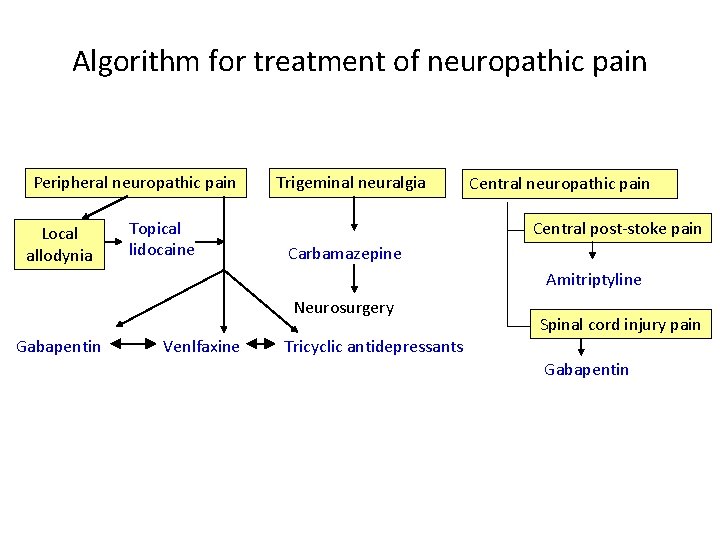
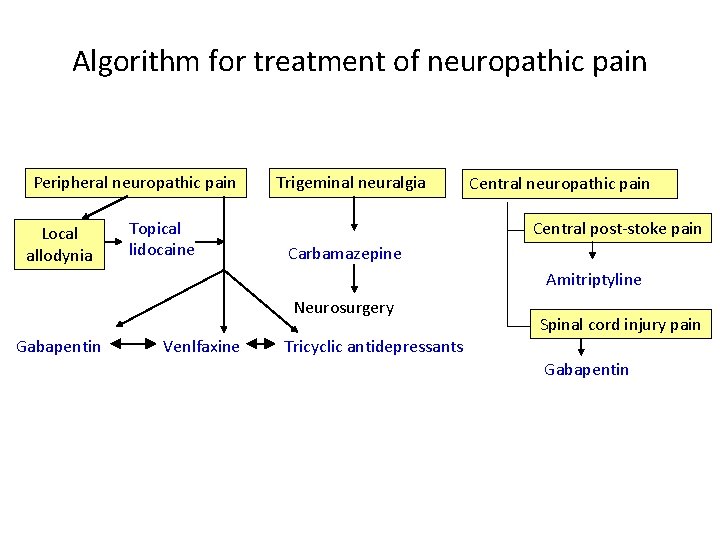
Algorithm for treatment of neuropathic pain Peripheral neuropathic pain Local allodynia Topical lidocaine Trigeminal neuralgia Central neuropathic pain Central post-stoke pain Carbamazepine Amitriptyline Neurosurgery Gabapentin Venlfaxine Tricyclic antidepressants Spinal cord injury pain Gabapentin
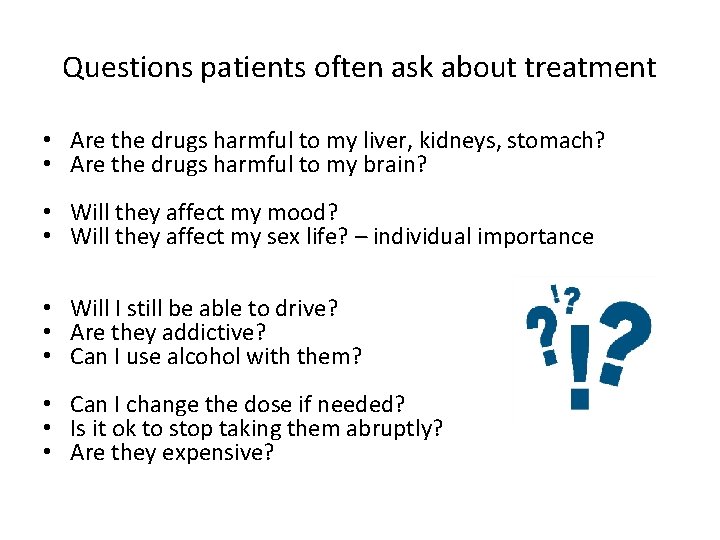
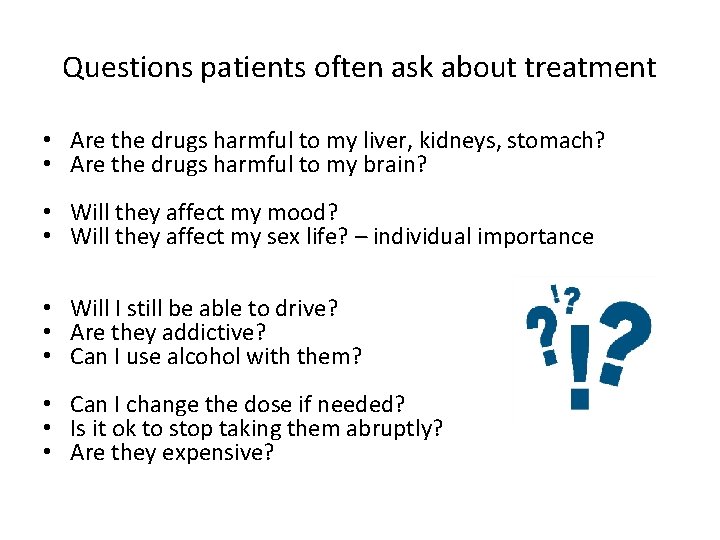
Questions patients often ask about treatment • Are the drugs harmful to my liver, kidneys, stomach? • Are the drugs harmful to my brain? • Will they affect my mood? • Will they affect my sex life? – individual importance • Will I still be able to drive? • Are they addictive? • Can I use alcohol with them? • Can I change the dose if needed? • Is it ok to stop taking them abruptly? • Are they expensive?
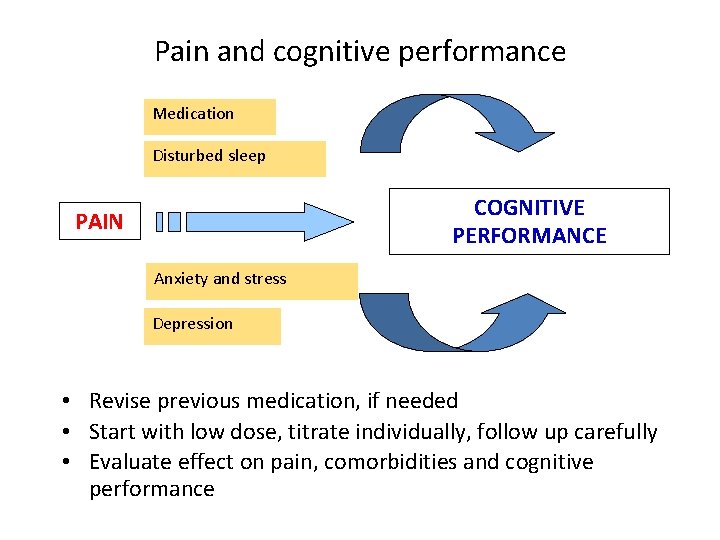
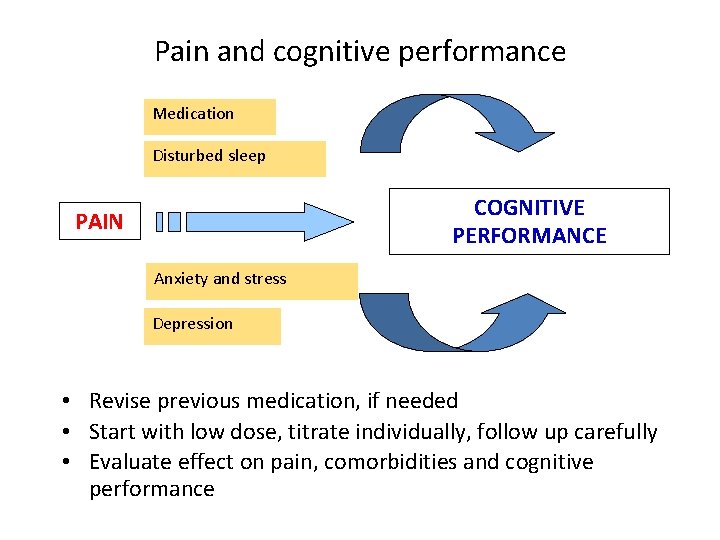
Pain and cognitive performance Medication Disturbed sleep COGNITIVE PERFORMANCE PAIN Anxiety and stress Depression • Revise previous medication, if needed • Start with low dose, titrate individually, follow up carefully • Evaluate effect on pain, comorbidities and cognitive performance
II Detailed information of the drugs for neuropathic pain
Tricyclic antidepressants (TCAs): efficacy, dosing • Efficacy: – The efficacy of TCAs has been established in peripheral neuropathic pain (pain diabetic neuropathy, postherpetic neuralgia) and in central post stroke pain • The pain relieving effect of TCAs in independent of their antidepressant effect (comes quicker and with lower dose) • Dosing: – Starting: 10– 25 mg in a single dose at bedtime – Effective dosages vary from 25– 150 mg from case to case – The average dosage for amitriptyline is 75 mg/day – Monitoring of serum drug concentrations may be helpful
Contraindications and precautions of TCAs • TCAs cannot be used in recovery phase of myocardial infarction or in patients with cardiac conduction disturbances. • TCAs should be used with caution in patients with history of seizures, prostatic hypertrophy, urinary retention, chronic constipation, narrow-angle glaucoma, increased intraocular pressure, suicidal ideations and in patients receiving concomitant SSRI, SNRI or tramadol treatment.
Adverse effects of TCAs • Anticholinergic adverse effects are common • Dry mouth drink water, salivation-producing resoriblets • Constipation bulk laxatives • Blurred vision or urinary retention taper TCA off • Cardiovascular adverse effects: • Orthostatic hypotension monitor blood pressure (supine and standing) • Prolongation of PR and QTc intervals ECG screening • Increased heart rate taper TCA off • Sedation, confusion and sweating can also occur • Imipramine and nortriptyline cause fewer anticholinergic effects and less sedation
Venlafaxine • Efficacy of venlafaxine has been shown in painful polyneuropathy • Dosing: start with 75 mg once daily, and escalate the dose with 75 mg at 2 weeks interval. Effective dosage is 150 -225 mg/day. • Venlafaxine is contraindicated in patients with uncontrolled hypertension, and blood pressure monitoring is recommended during the treatment • Venlafaxine should be used with caution in patients with history of mania, seizures and bleeding tendency • Adverse effects: nausea, dry mouth, headache and sweating, abnormal dreams, decreased libido, dizziness, insomnia, nervousness, sedation, tremor, visual disturbance, hypertension, palpitations, anorexia and urination hesitancy
Carbamazepine (slow release) • Is a drug of choice for primary trigeminal neuralgia • Dosing: slowly raise the initial dosage of 100 mg twice daily until freedom from pain is achieved (often 600 -800 mg daily, even 1200 mg daily) • Adverse effects: Sedation, dizziness, gait abnormalities, liver and blood changes, hyponatraemia, enzyme induction • Blood count, liver enzyme and plasma sodium monitoring is recommend • Carbamazepine has lots of interactions with other drugs (e. g. , oral contraceptives) – Check the possible interactions before prescribing carbamazepine – Check serum drug concentration in suspected enzyme induction • Once the neuralgia is in remission, try to decrease the dose slowly
Tramadol • Tramadol itself has serotoninergic and noradrenergic effect, and its active metabolite (after metabolism by CYP 2 D 6 enxyme) is opioid agonist • Dosing: testi with a 50 mg capsule, and if it is well tolerated, escalate the dose gradually up to 300 -400 mg/day • Depot and short-acting capsules can be combined • Adverse effects: nausea, sedation, excessive sweating, dizziness, constipation, headache • Use with caution in patients with epilepsy or SSRI or SNRI medication
Gabapentin • The efficacy of gabapentin has been established in painful diabetic neuropathy and postherpetic neuralgia • Dosing: start with 300 mg at bedtime, and escalate with 300 mg/day or more slowly until sufficient pain relief • Effective dose: 900 -3600 mg/day (divided in 3 doses) • Adverse effects: dizziness, somnolence, peripheral oedema, weight gain, asthenia, headache, dry mouth and blurred vision • If renal function impaired, reduce the dose • No pharmacokinetic interactions
III Patient cases
Summary • Tailored medication – Choice of the drug(s) – Careful dose escalation • • Sufficient information for the patient Realistic goal-setting Close follow-up Psychosocial support, non-pharmacological methods
 Rachel beaty
Rachel beaty Neuropathic pain
Neuropathic pain Neuropathic pain
Neuropathic pain Description of pain
Description of pain Neuropathic pain
Neuropathic pain Neuropathic pain
Neuropathic pain Martian pain
Martian pain Pms vs pregnancy
Pms vs pregnancy Pms or pregnancy
Pms or pregnancy Anterolisthesis cervical icd 10
Anterolisthesis cervical icd 10 Low back pain definition
Low back pain definition Laporan kasus low back pain
Laporan kasus low back pain Right side headache
Right side headache Rontgen vls adalah
Rontgen vls adalah Mid low high
Mid low high Communication style bias
Communication style bias Significant figures
Significant figures Low voltage hazards
Low voltage hazards Pain treatment satisfaction scale
Pain treatment satisfaction scale Wax pattern fabrication
Wax pattern fabrication High tech assistive technology
High tech assistive technology Assistive technology for low incidence disabilities
Assistive technology for low incidence disabilities Vena jugularis superficialis
Vena jugularis superficialis Anna neary
Anna neary Referred pain definition
Referred pain definition Par ton corps tu nous donnes la vie
Par ton corps tu nous donnes la vie Societal impact of pain
Societal impact of pain Modified bassini repair
Modified bassini repair University hospital of pisa
University hospital of pisa Pain management okc soonercare
Pain management okc soonercare Remains poem simon armitage
Remains poem simon armitage