Salivary Glands Dr Mohammad nofal Anatomy Paired Major













- Slides: 48
Salivary Glands Dr. Mohammad nofal
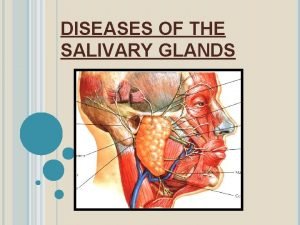
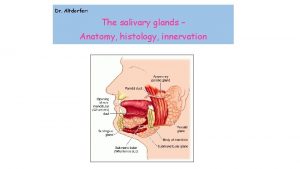
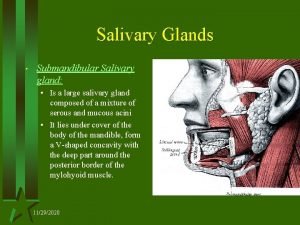
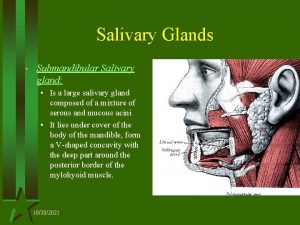
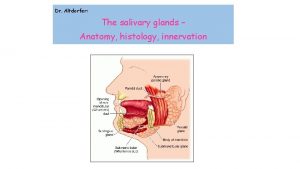
Anatomy Paired Major Salivary glands l Parotid: Stenson duct 2° molar tooth. l Submandibular: Warton duct lateral to frenulum. l Sublingual: in Warton duct.
Anatomy Minor Salivary Glands l In Soft palate, Hard palate , gingiva, lips. l In all oral mucosa except the upper surface of the tongue.

Saliva: 1000 – 1500 ml/day
Sialadenitis l Acute l Chronic
Acute l - Viral: Mumps Self limited viral infection. Common in children. Diffuse inflammation of one or both parotid glands. May be associated with pancreatitis, orchitis in adults, oophritis is rare.
l - Acute Bacterial: Dryness of mouth. Ascending infection. Cause Staphylococcus aureus. Seen in elderly post. op and common in Parotid gland.
Chronic Autoimmune (sjogren syndrome) - Inflammation causes destruction of major and minor salivary glands) - 90 % women 35 - 45 years of age. - 60% associated with SLE, Rheumatoid arthritis or scleroderma. l
Sialolithiasis Most common in the duct of submandibular salivary glands. - Intermittent obstruction chronic sialadenitis dilatation of the ducts and atrophy of acinar cells superimposed infection and microabscesses. l
SALIVARY NEOPLASMS
l 70 -80% of Salivary tumors Parotids. l 70 -80% of Parotid tumors benign. l 80% of benign tumors pleomorphic adenoma.
Pleomorphic adenoma l l l Most common. Peak age: 5° decade. Proliferation of: - epith. - myoepith. - stroma tissue resemble cartilage and bone.
presentaion l Solitary Painless mass in Parotid area, firm, slowly growing, mobile. l Intraoral pharyngeal mass extending from parapharynx (deep lobe) l 2 -10% may turn into malignant (usually adenocarcinoma)



l Gross appearance: irregular round to ovoid mass, well defined borders, white to tan cut surface. l Sometimes have haemorhage and infarcted areas.

Papillary Cystadenoma Lymphomatosum(Warthin) l l l Occurs only in Parotid. 10% bilat. More in males(90%) More in smokers. Cystic mass(may be fluctuant) Doesnot change into malignancy.
l Gross appearance: ovoid to spherical mass with variable no. Of cysts that excude a clear fluid.

Rare Benign Types l Oxyphilic adenoma, oncocytic adenoma, basal cell adenoma, sebaceous adenoma, canalicular adenoma.
Benign non epithelial tumors l l l Haemangioma: most common in children, comressible mass, ttt include steroids , angiogram & surgery, spontaneous regession may occure. Lipoma Lymphangioma(cystic hygroma): 50% manifest at birth, 80% by 2 years.
Malignant Tumors l l l l 96% discrete mass. 4% diffuse enlargement. 12 -24% painful. 17% fixed to masseter. 8 -26% fascial nerve dysfunction. 9% skin ulceration. Formication: parasthesia described as feeling of ants crawling on skin.

l LN metastases increase with high grade mucoepidermoid and squamous cell ca. l Less with adenoid cystic acinic cell ca.
Risk of malignancy: 20% in Parotids. 40% in submandibular. 60% in minor salivary glands
Malignant Tumors l Mucoepidermoid: -most common. -usually in parotid, 2° site is palate. -peak age 5° decade. -high or low grade. -
Malignant Tumors l l Adenoid cystic : 2° most common, but is the most common in other glands than parotid. Usually well defined but not encapsulated. Rarely involves lymphnodes, may have perineural invasion , may reach base of skull. Has a tendency for distant mets. specially lung.
Malignant Tumors l Acinic cell Ca. : 2° most common parotid and paediatric ca. Has a good prog. : 5 years-------85% 10 years------68% 25 years------50% l
Malignant Tumors - Adenocarcinoma and Squamous Cell Carcinoma are rare and aggressive types.
Evaluation l A complete hx. Including onset(first time the mass was noticed, uni or bilat. , progression, hx. Of pain, hx. Of trauma, contact hx. . . . etc)
Evaluation l P/E. Should include in addition to the mass : -The rest of salivary glands. -Fascial Nerve examination with all its branches. -Oral examination for pharyngial bulge, and orifices of salivary ducts. -Cervical lymphnodes.
Evaluation l In Diffuse Swelling: to role out sialadenitis - Antibiotic trial for 10 days. - Sialogram.
Radiological Evaluation l CT Scan and MRI: To determine the extension of the disease.






Fine Needle Aspiration l The accuracy, sensitivity and specificity reported in the literature vary from 84 -97%, 54 -95% and 86 -100% respectively. l Some surgeons argue its importance: - ttt always surgery. - tumor implantation.
Treatment l l l Problem: fascial nerve passes through the Parotid. Benign: superfiscial parotidectomy with nerve preservation. Malignant: total parotidectomy with nerve preservation. if one branch is involvod excision of that branch.
Neck Dissection l If positive LNs Neck Dissection. l No consensus on neg LNs. -in high grade mucoepidermoid, squamous or adenocrcinoma prophylactic neck dissection may be justified.
l Chemotherapy: not effective. l External beam radiotherapy: effective.
Submandibular l l Total excision of the mass with preservation of marginal mandibular, hypoglossal, lingual nerves if possible. If involved should be sacrified, sometimes with platysma and skin.
Minor Salivary Glands l Excised sometimes with adjacent bone as hard palate. l Necrotizing sialometaplesia: a self limiting disease betweenhard and soft palate that may ulcerate and mimic malignancy.
 Submandibular gland excision
Submandibular gland excision Dysphagia terminology
Dysphagia terminology Saliva formation
Saliva formation Sialography
Sialography Minor salivary glands
Minor salivary glands Incision for parotid abscess
Incision for parotid abscess Webers glands
Webers glands Minor salivary glands
Minor salivary glands Minor salivary glands
Minor salivary glands Nie wiem association
Nie wiem association Striated duct
Striated duct Pancreas organ
Pancreas organ Intestinal structure
Intestinal structure Merocrine gland
Merocrine gland Major endocrine glands male and female
Major endocrine glands male and female Chapter 16 matching questions 6-10
Chapter 16 matching questions 6-10 Cylindroma slideshare
Cylindroma slideshare Lactobacillus colony count test
Lactobacillus colony count test Pathogenesis of pleomorphic adenoma
Pathogenesis of pleomorphic adenoma Nasal concha cadaver
Nasal concha cadaver Oncocytoma salivary gland
Oncocytoma salivary gland Salivary gland tumor
Salivary gland tumor Snyder test for dental caries
Snyder test for dental caries Oncocytoma salivary gland
Oncocytoma salivary gland Party wall appearance seen in
Party wall appearance seen in Salivary amylase digestion of starch
Salivary amylase digestion of starch Glandular epithelial cell
Glandular epithelial cell Salivary gland disorders classification
Salivary gland disorders classification Pleomorphic adenoma
Pleomorphic adenoma Mucous acini diagram
Mucous acini diagram Role of bile juice in digestion
Role of bile juice in digestion Pleomorphic adenomas
Pleomorphic adenomas Pearo-nn
Pearo-nn Mohammad irfan bowdoin
Mohammad irfan bowdoin Mohammad davidson
Mohammad davidson Mohammad sharifkhani
Mohammad sharifkhani My.edu.sharif
My.edu.sharif Laila hammoud
Laila hammoud Dr. mohammad diab
Dr. mohammad diab Vlsi
Vlsi Dr mohammad khan
Dr mohammad khan Sumbangan mohammad eunos abdullah
Sumbangan mohammad eunos abdullah Mohammad sadegh rasooli
Mohammad sadegh rasooli Mohammad sharifkhani
Mohammad sharifkhani Mohammad ali javidian
Mohammad ali javidian Mohammad alomar
Mohammad alomar Mohammad arjomand
Mohammad arjomand Dr mohammad aman
Dr mohammad aman Mohammad alipour
Mohammad alipour