Anatomy and Physiology of the Salivary Glands 3


- Slides: 23
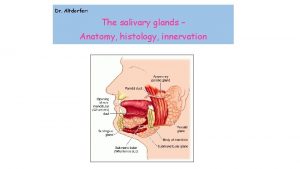
Anatomy and Physiology of the Salivary Glands
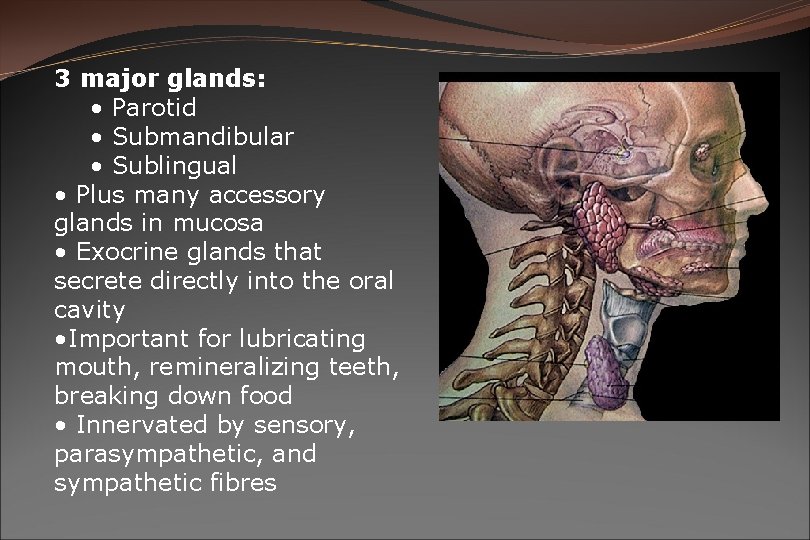
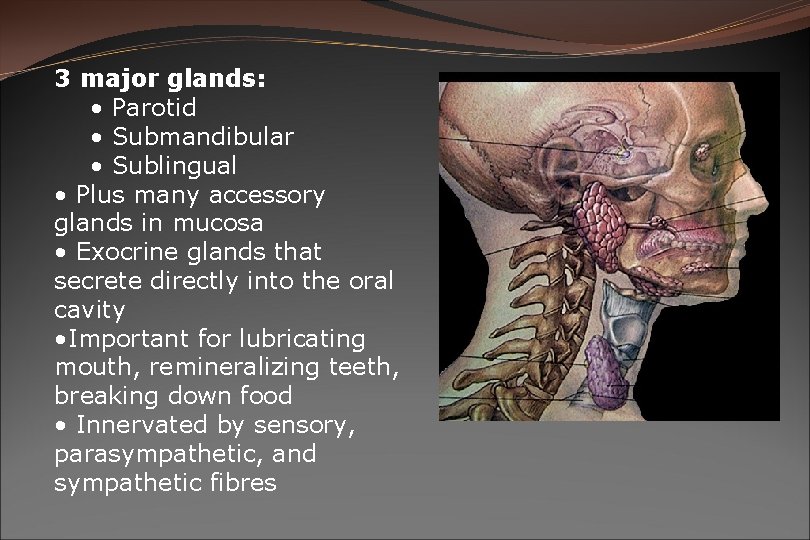
3 major glands: • Parotid • Submandibular • Sublingual • Plus many accessory glands in mucosa • Exocrine glands that secrete directly into the oral cavity • Important for lubricating mouth, remineralizing teeth, breaking down food • Innervated by sensory, parasympathetic, and sympathetic fibres
Embryology � 6 th to 8 th week of gestation �Begin as oral ectodermal outpouchings into mesenchyma – point of origin is duct orifice �Parotid – first to develop & last to become encapsulated
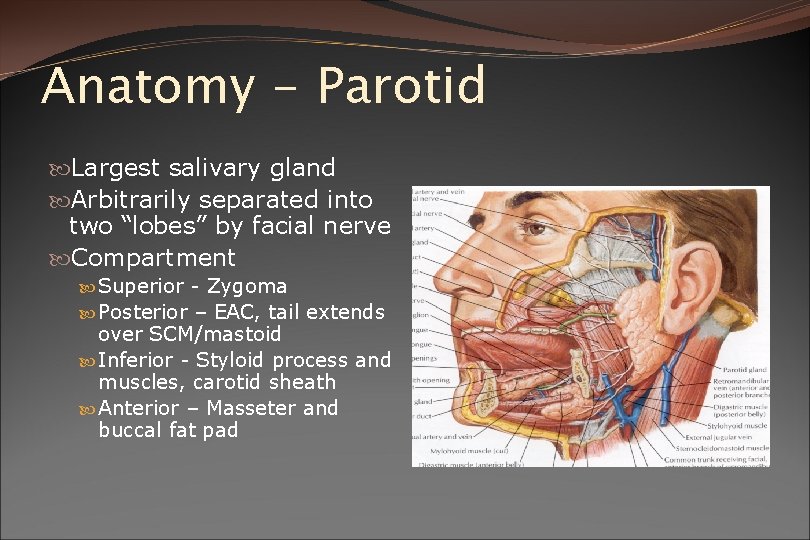
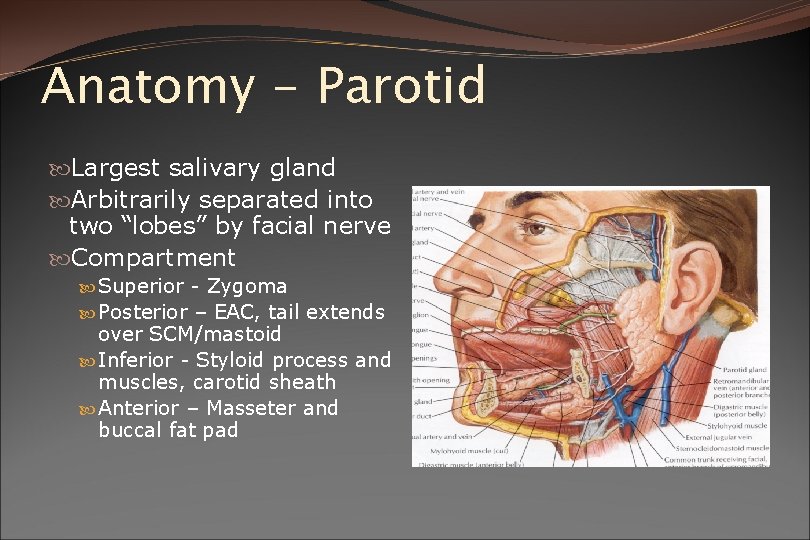
Anatomy - Parotid Largest salivary gland Arbitrarily separated into two “lobes” by facial nerve Compartment Superior - Zygoma Posterior – EAC, tail extends over SCM/mastoid Inferior - Styloid process and muscles, carotid sheath Anterior – Masseter and buccal fat pad
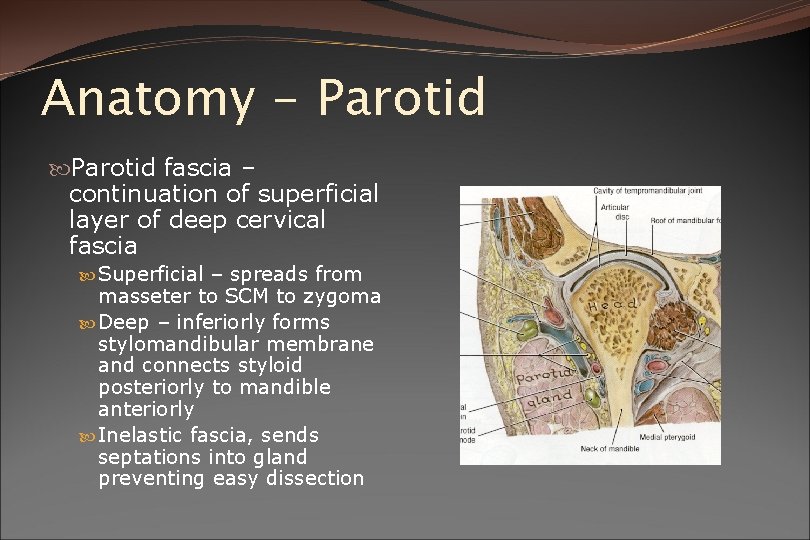
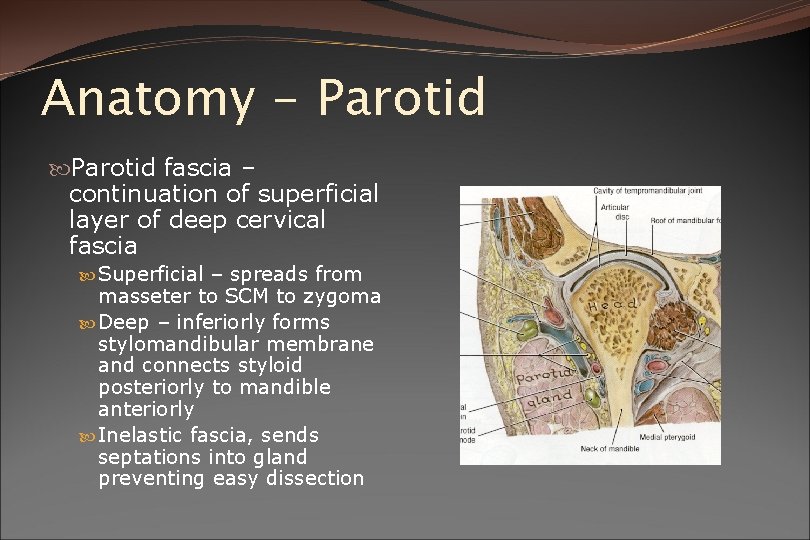
Anatomy - Parotid fascia – continuation of superficial layer of deep cervical fascia Superficial – spreads from masseter to SCM to zygoma Deep – inferiorly forms stylomandibular membrane and connects styloid posteriorly to mandible anteriorly Inelastic fascia, sends septations into gland preventing easy dissection
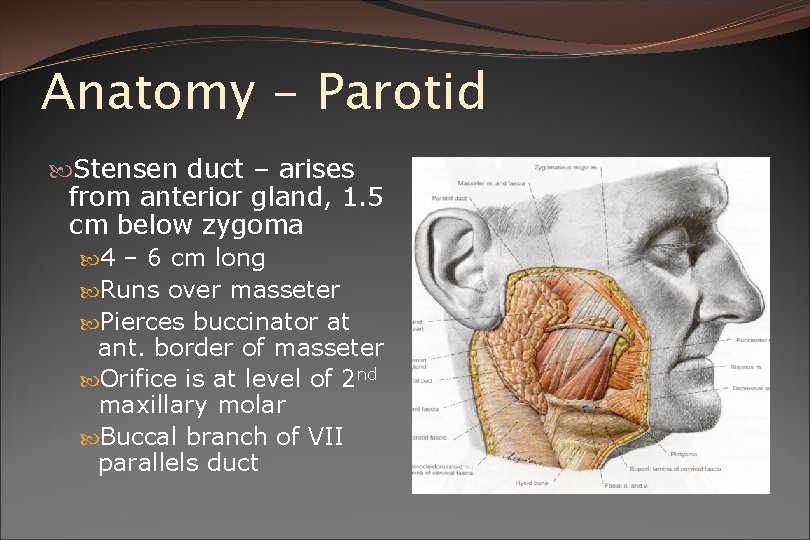
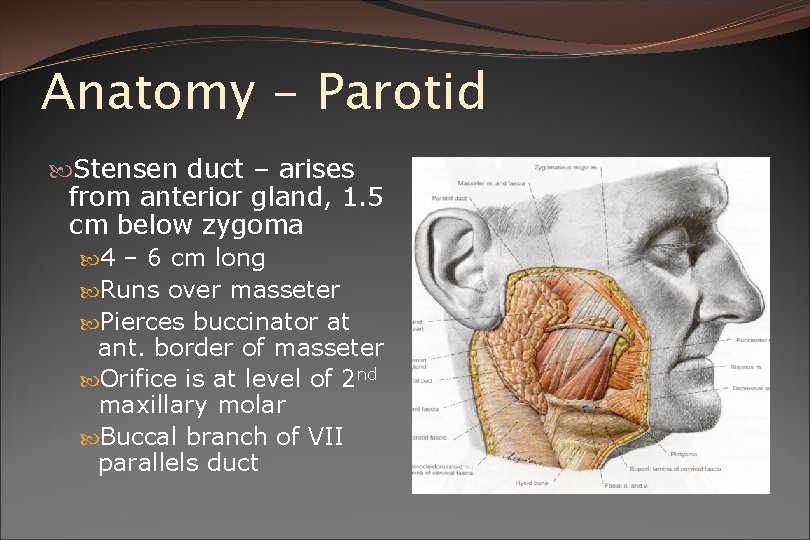
Anatomy - Parotid Stensen duct – arises from anterior gland, 1. 5 cm below zygoma 4 – 6 cm long Runs over masseter Pierces buccinator at ant. border of masseter Orifice is at level of 2 nd maxillary molar Buccal branch of VII parallels duct
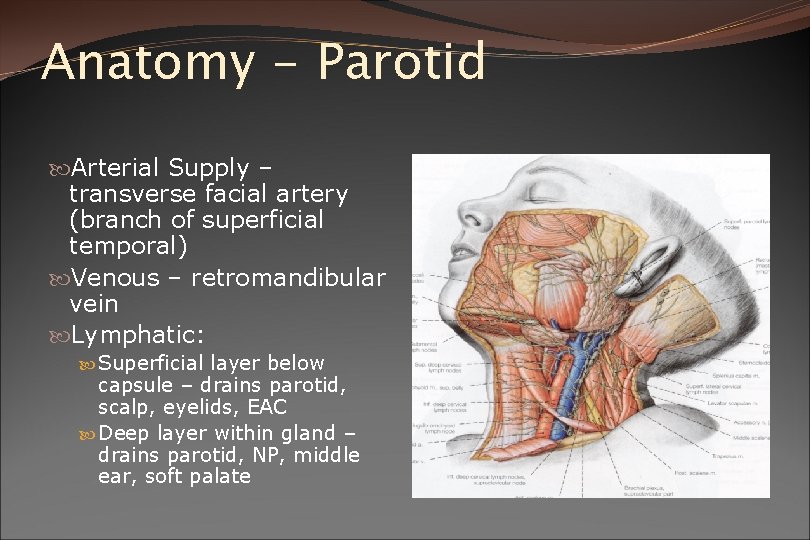
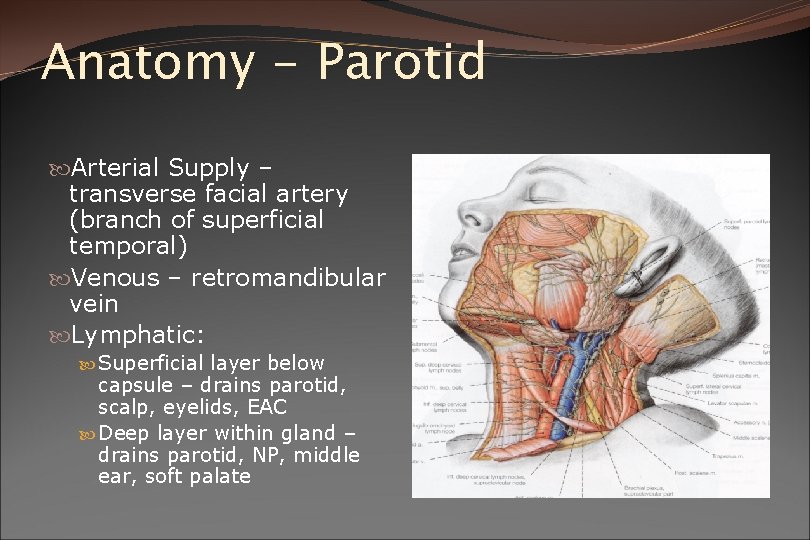
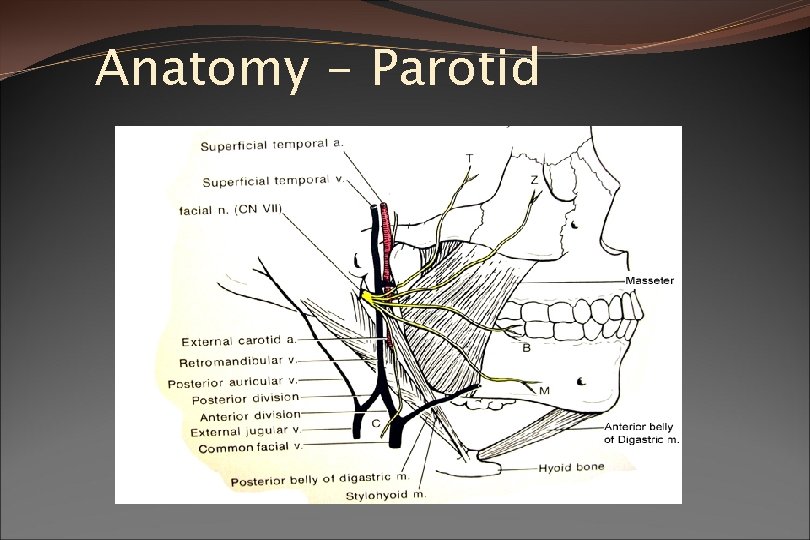
Anatomy - Parotid Arterial Supply – transverse facial artery (branch of superficial temporal) Venous – retromandibular vein Lymphatic: Superficial layer below capsule – drains parotid, scalp, eyelids, EAC Deep layer within gland – drains parotid, NP, middle ear, soft palate
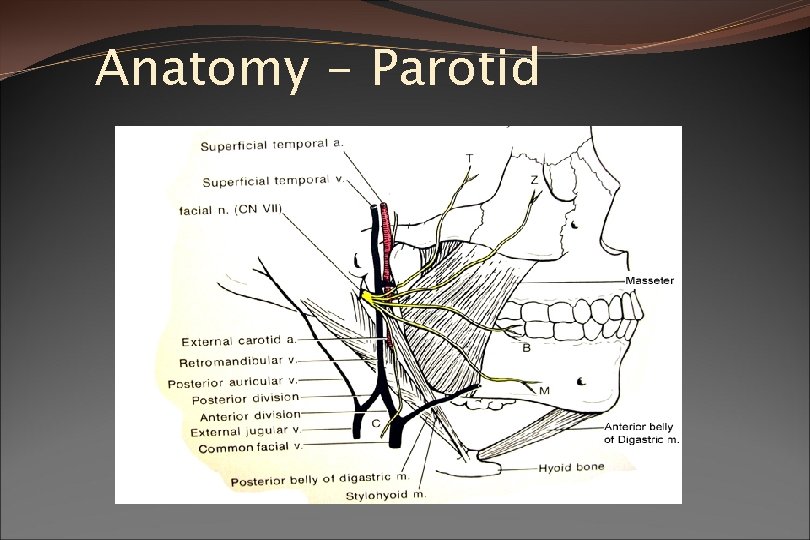
Anatomy - Parotid
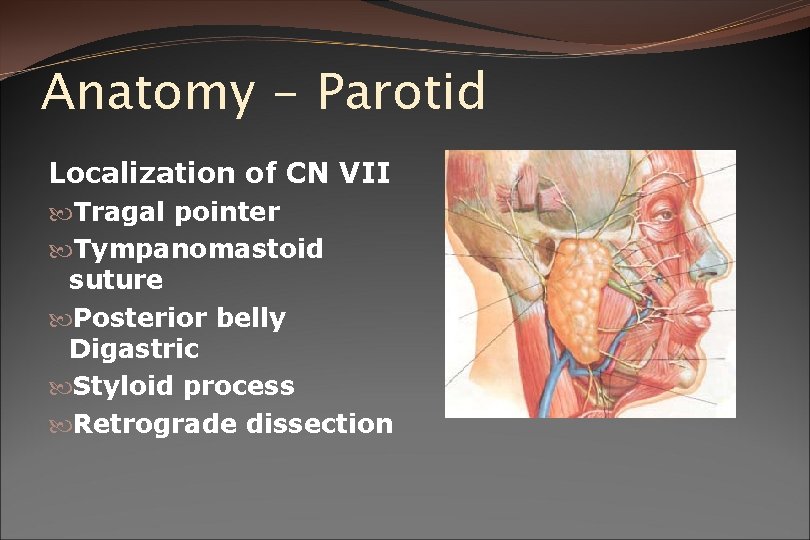
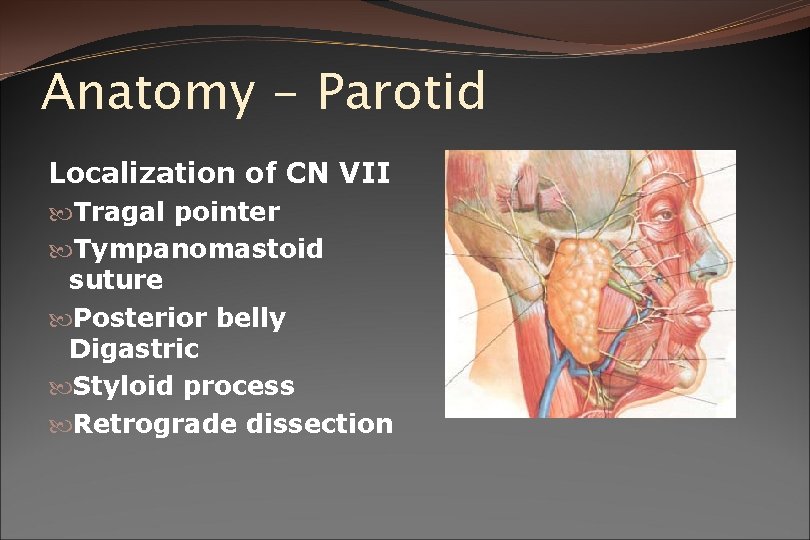
Anatomy - Parotid Localization of CN VII Tragal pointer Tympanomastoid suture Posterior belly Digastric Styloid process Retrograde dissection
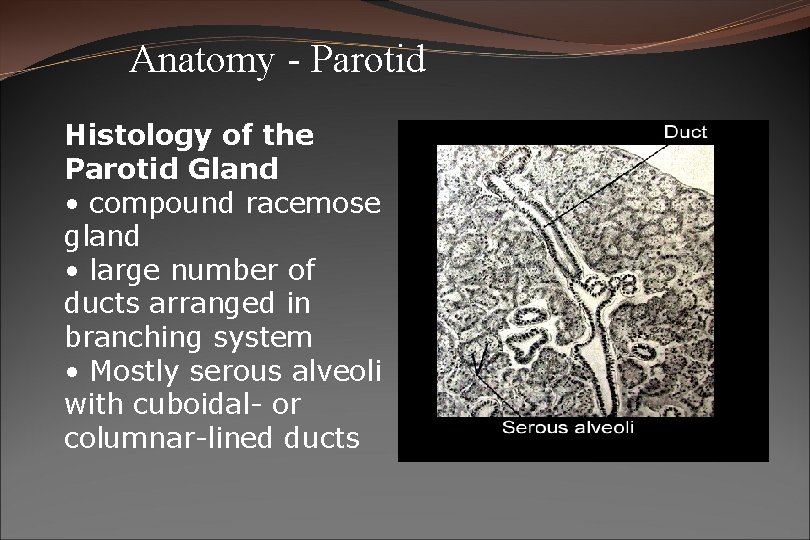
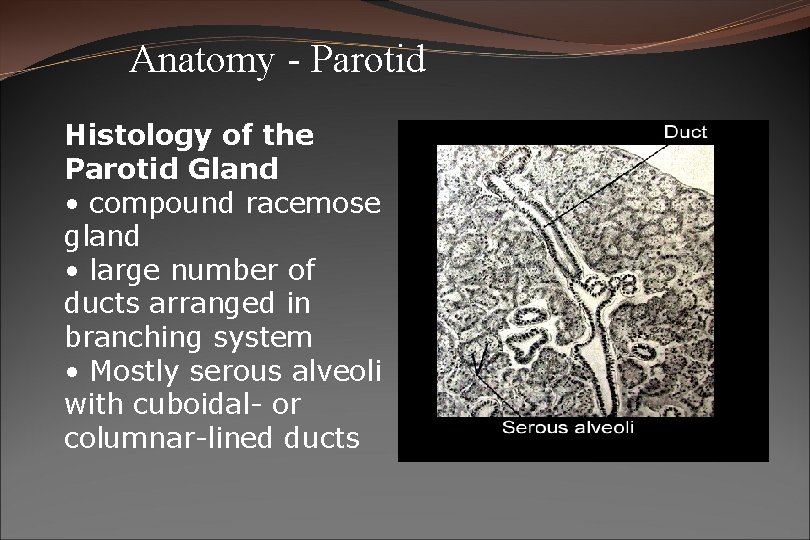
Anatomy - Parotid Histology of the Parotid Gland • compound racemose gland • large number of ducts arranged in branching system • Mostly serous alveoli with cuboidal- or columnar-lined ducts
Important Points about the Parotid �Largest of the salivary glands �Mostly watery serous secretion �Closely associated with facial nerve and vasculature of the face �Parotid duct opens through cheek above upper second molar �Produces most stimulated saliva
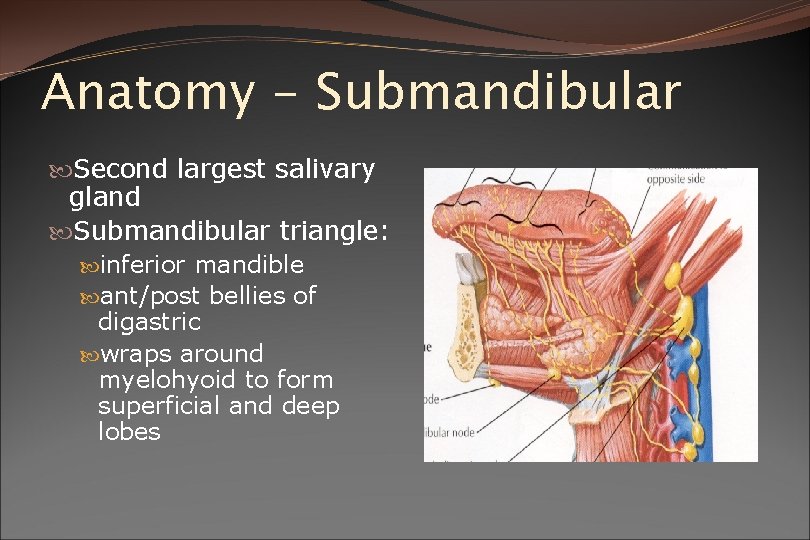
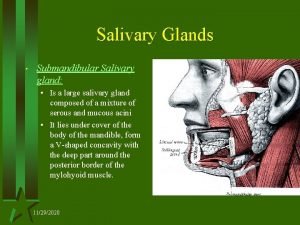
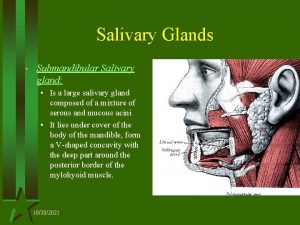
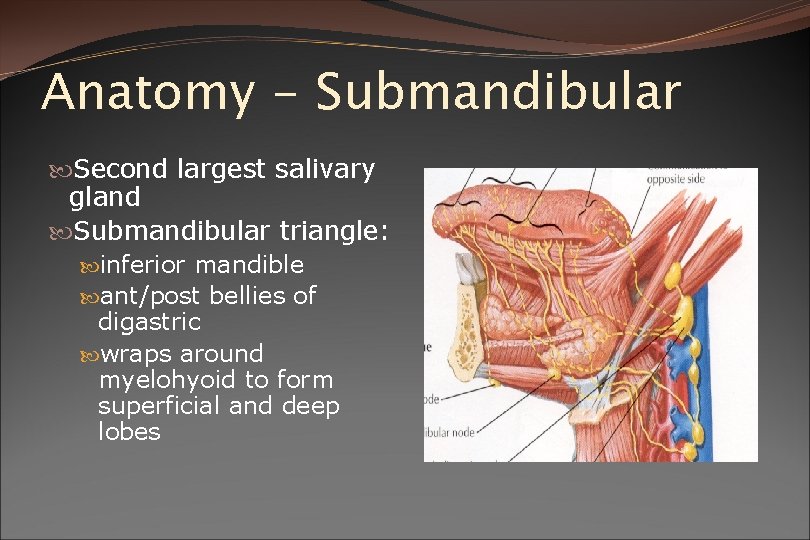
Anatomy - Submandibular Second largest salivary gland Submandibular triangle: inferior mandible ant/post bellies of digastric wraps around myelohyoid to form superficial and deep lobes
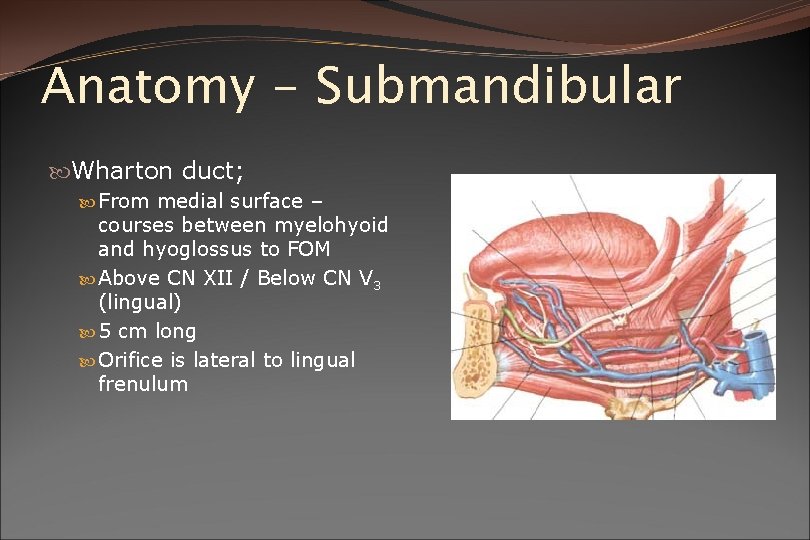
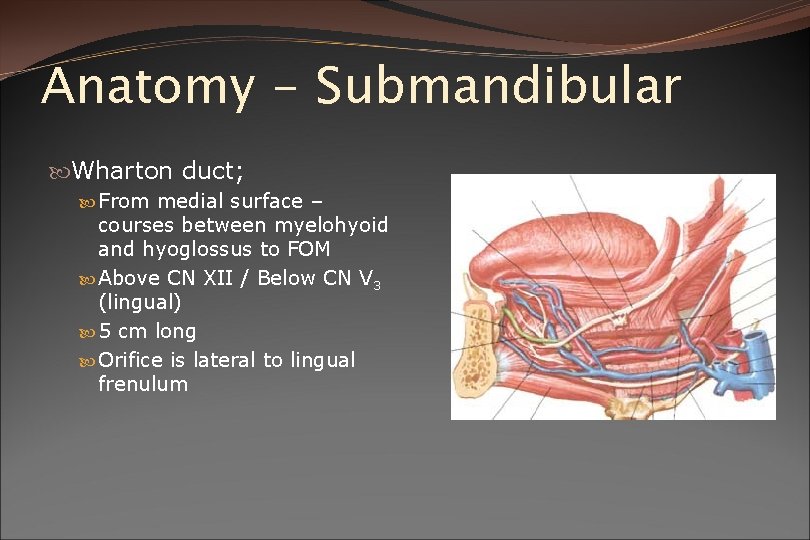
Anatomy - Submandibular Wharton duct; From medial surface – courses between myelohyoid and hyoglossus to FOM Above CN XII / Below CN V 3 (lingual) 5 cm long Orifice is lateral to lingual frenulum

Anatomy - Submandibular Arterial Supply – Facial artery Venous Drainage – Anterior facial vein Lymphatics: around gland in fascia drain to deep cervical chain
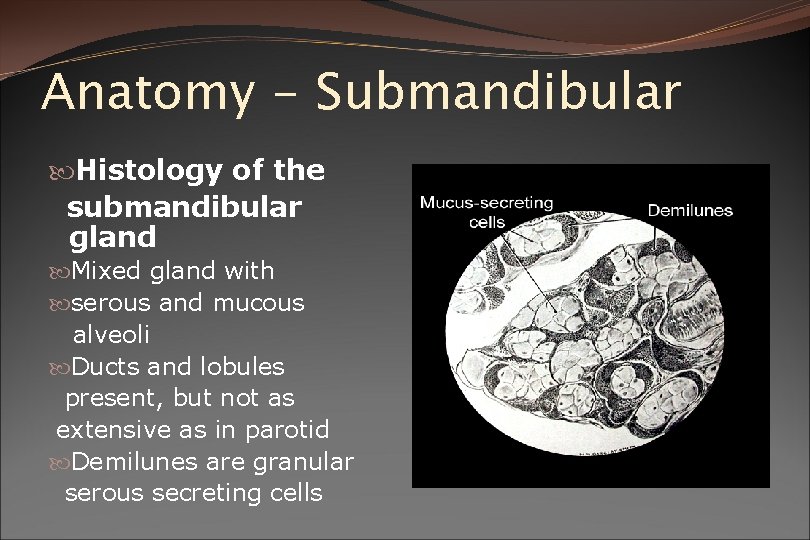
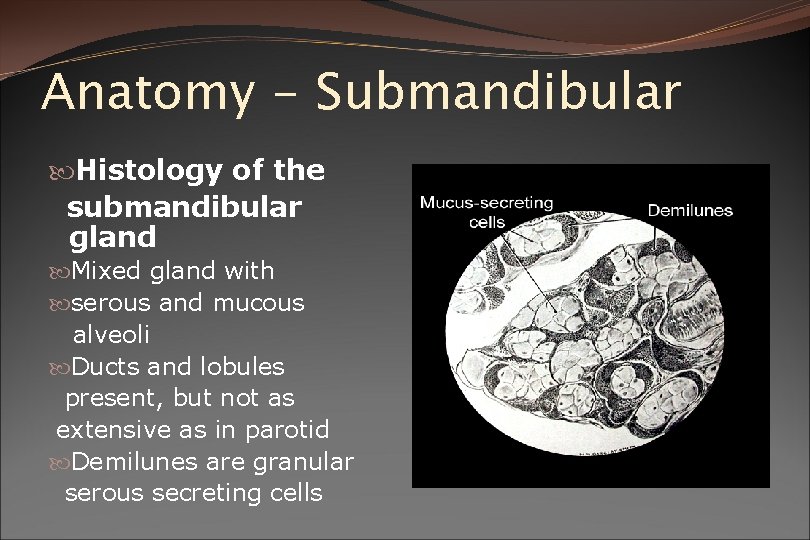
Anatomy - Submandibular Histology of the submandibular gland Mixed gland with serous and mucous alveoli Ducts and lobules present, but not as extensive as in parotid Demilunes are granular serous secreting cells
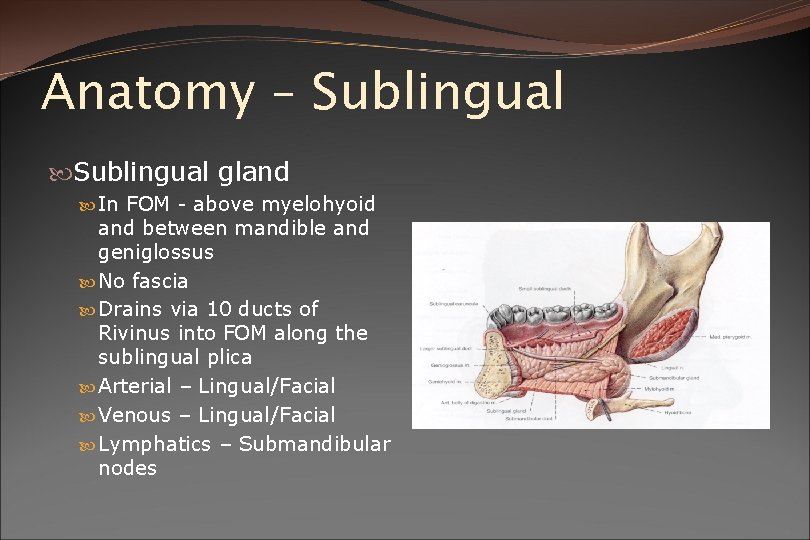
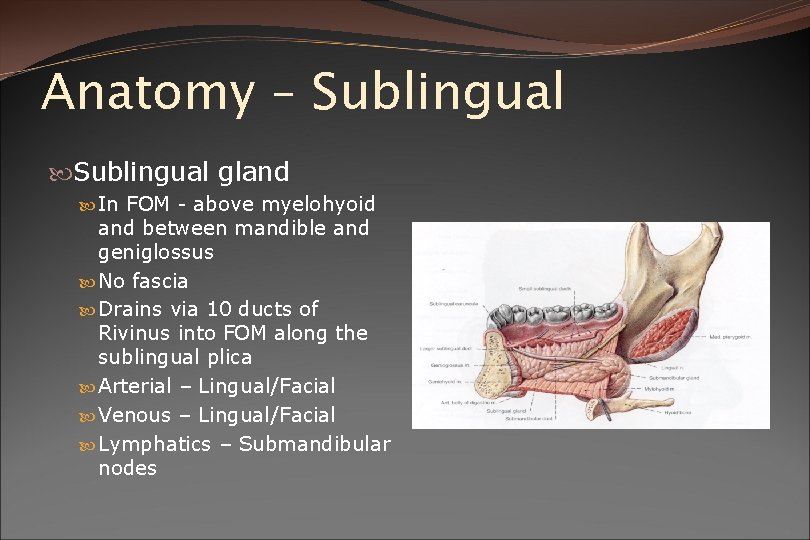
Anatomy – Sublingual gland In FOM - above myelohyoid and between mandible and geniglossus No fascia Drains via 10 ducts of Rivinus into FOM along the sublingual plica Arterial – Lingual/Facial Venous – Lingual/Facial Lymphatics – Submandibular nodes
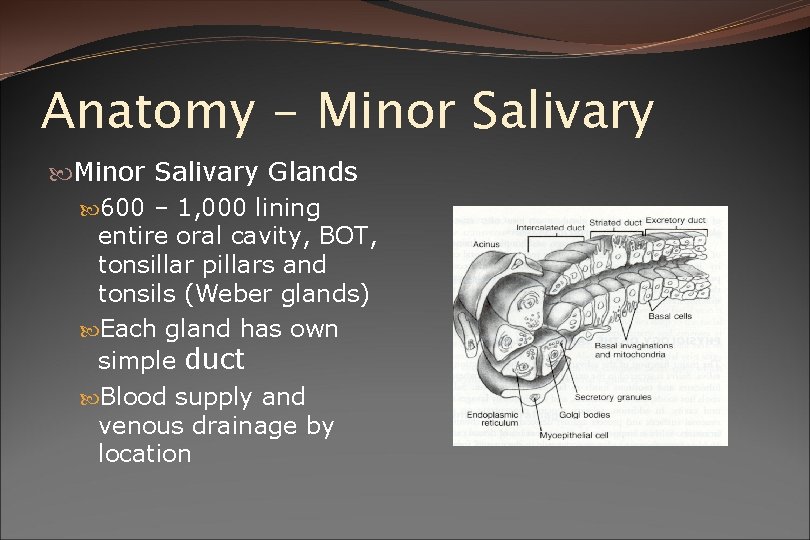
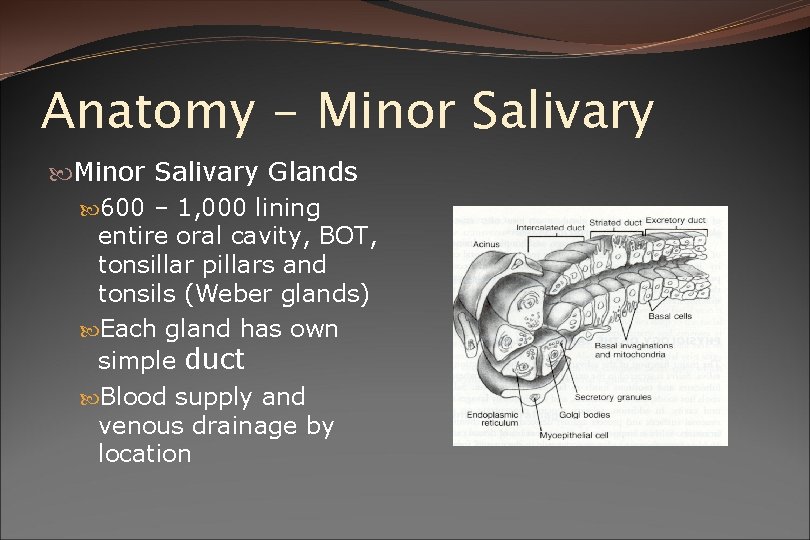
Anatomy - Minor Salivary Glands 600 – 1, 000 lining entire oral cavity, BOT, tonsillar pillars and tonsils (Weber glands) Each gland has own simple duct Blood supply and venous drainage by location
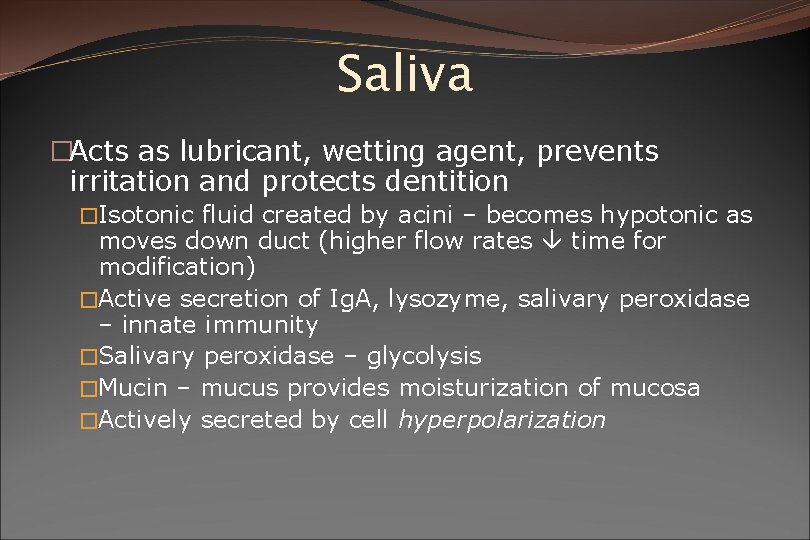
Saliva �Acts as lubricant, wetting agent, prevents irritation and protects dentition �Isotonic fluid created by acini – becomes hypotonic as moves down duct (higher flow rates time for modification) �Active secretion of Ig. A, lysozyme, salivary peroxidase – innate immunity �Salivary peroxidase – glycolysis �Mucin – mucus provides moisturization of mucosa �Actively secreted by cell hyperpolarization
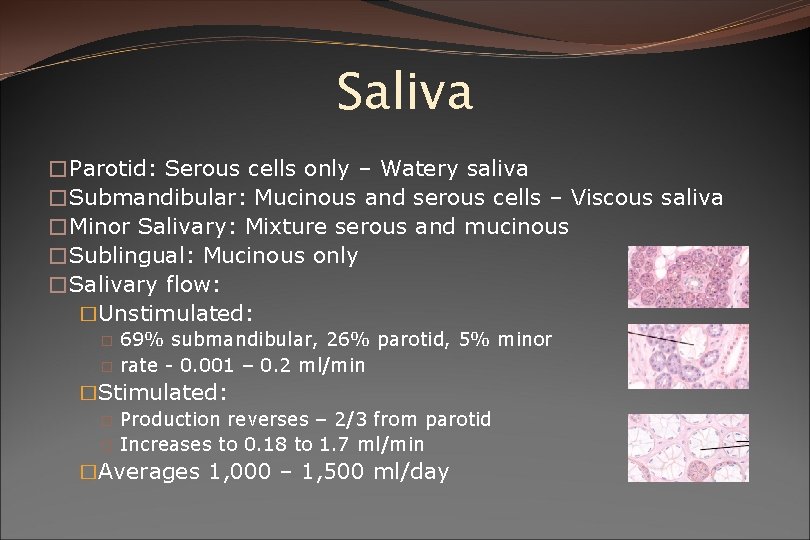
Saliva �Parotid: Serous cells only – Watery saliva �Submandibular: Mucinous and serous cells – Viscous saliva �Minor Salivary: Mixture serous and mucinous �Sublingual: Mucinous only �Salivary flow: �Unstimulated: 69% submandibular, 26% parotid, 5% minor � rate - 0. 001 – 0. 2 ml/min � �Stimulated: � Production reverses – 2/3 from parotid � Increases to 0. 18 to 1. 7 ml/min �Averages 1, 000 – 1, 500 ml/day
Function of Saliva Moistens oral mucosa Moistens & cools food Medium for dissolved food Buffer (HCO 3) Salivary peroxidase Glycolysis Digestion (Amylase, Lipase) Antibacterial lysozyme, Ig. A, Peroxidase, FLOW) Mineralization Protective for dentition
Innervation of the Salivary Glands Main control by parasympathetic system: Submandibular and sublingual: Via chordatympani of facial nerve through submandibular ganglion Parotid: Glossopharyngeal nerve via otic ganglion Sympathetic fibres through cervical ganglion then follow blood vessels to glands

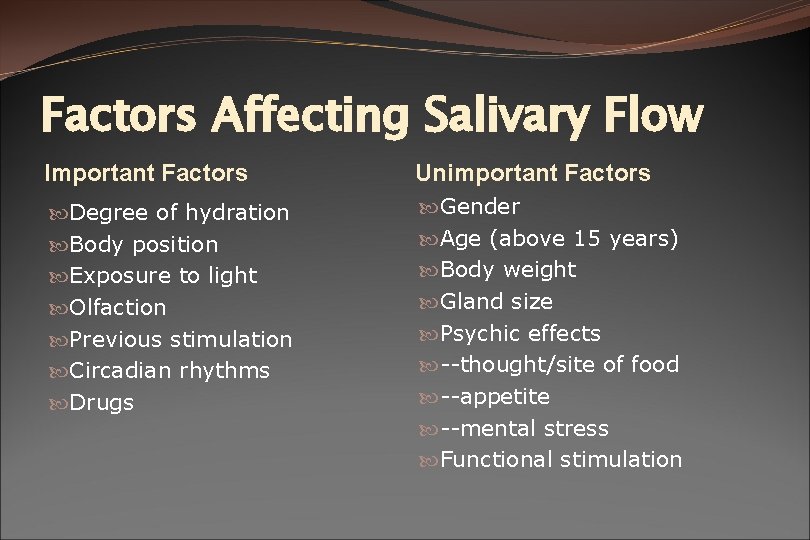
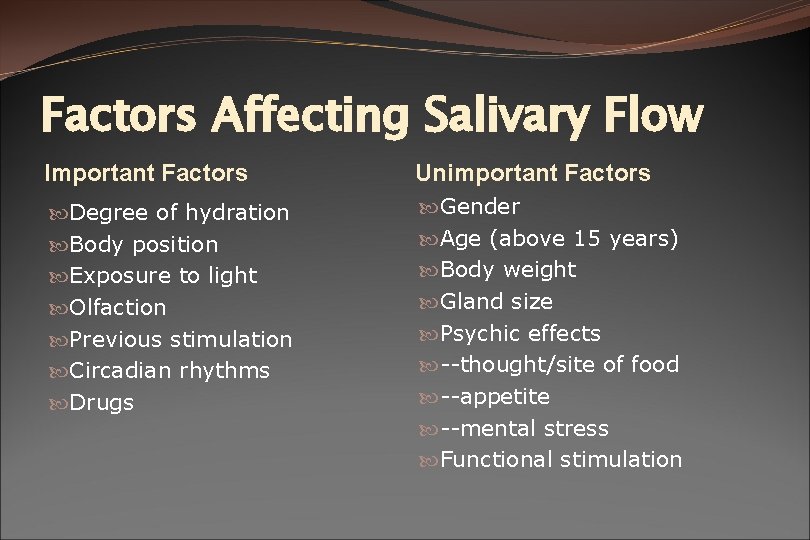
Factors Affecting Salivary Flow Important Factors Unimportant Factors Degree of hydration Body position Exposure to light Olfaction Previous stimulation Circadian rhythms Drugs Gender Age (above 15 years) Body weight Gland size Psychic effects --thought/site of food --appetite --mental stress Functional stimulation
 Submandibular gland excision
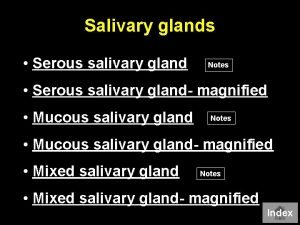
Submandibular gland excision Types of salivary glands
Types of salivary glands Types of salivary glands
Types of salivary glands Git organs
Git organs Anatom
Anatom Colon
Colon Submandibular gland histology
Submandibular gland histology Minor salivary glands
Minor salivary glands Minor salivary glands
Minor salivary glands Minor salivary glands
Minor salivary glands Sublingual gland pig
Sublingual gland pig Saliva formation
Saliva formation Submandibular gland
Submandibular gland Holocrine
Holocrine Upper airway anatomy
Upper airway anatomy Tattoo anatomy and physiology
Tattoo anatomy and physiology Anatomy science olympiad
Anatomy science olympiad Imperfect flowers examples
Imperfect flowers examples Anatomy and physiology bones
Anatomy and physiology bones Ulcer definition anatomy
Ulcer definition anatomy Sheep liver lobes
Sheep liver lobes Podbřišek
Podbřišek Difference between anatomy and physiology
Difference between anatomy and physiology Anatomy and physiology of blood
Anatomy and physiology of blood