Respiratory Infections of Interest for the Respiratory Therapist





- Slides: 48
Respiratory Infections of Interest for the Respiratory Therapist Emilio V. Perez-Jorge, MD, FACP Infectious Diseases Lexington Medical Center

�evperezjorge@lexhealth. org
Disclosures and Conflicts of Interests
Objectives: What could be interesting for RTs? � Some new bugs, same old syndromes ◦ Strep and non-streptococcal Pharyngitis ◦ Upper respiratory infections and airway compromise � � � Infection control issues and prevention of transmission of respiratory infections Review new concepts and terminology of Hospital Acquired Pneumonia (VAP, VAE) New diagnostic techniques: Respiratory PCR, MALDI TOF and other rapid tests Antibiotic resistance and stewardship Updates on chronic infections: MAC and other atypical mycobacteria, Bronchiectasis
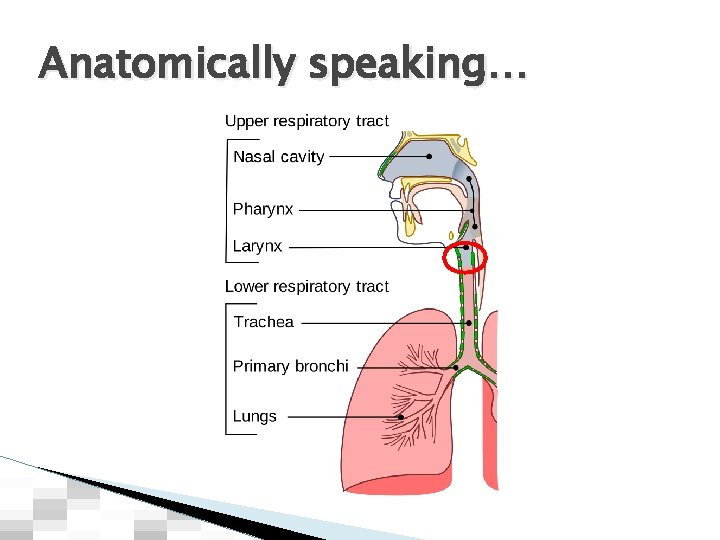
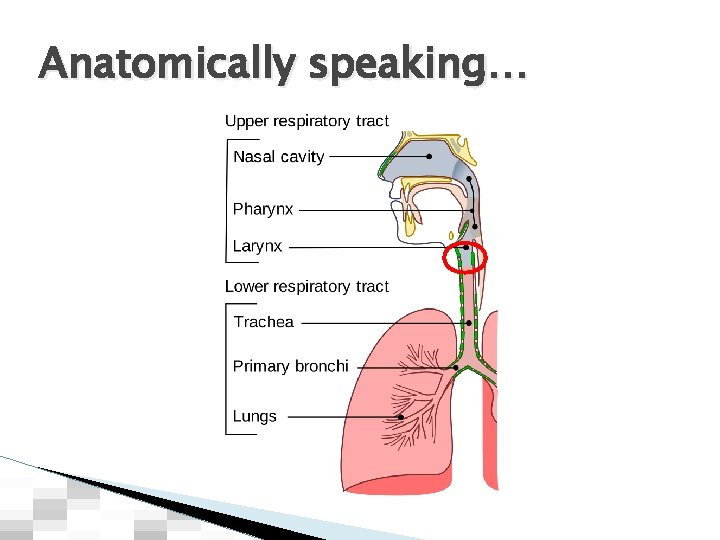
Anatomically speaking…
Think like a Realtor LOCATION, LOCATION 6
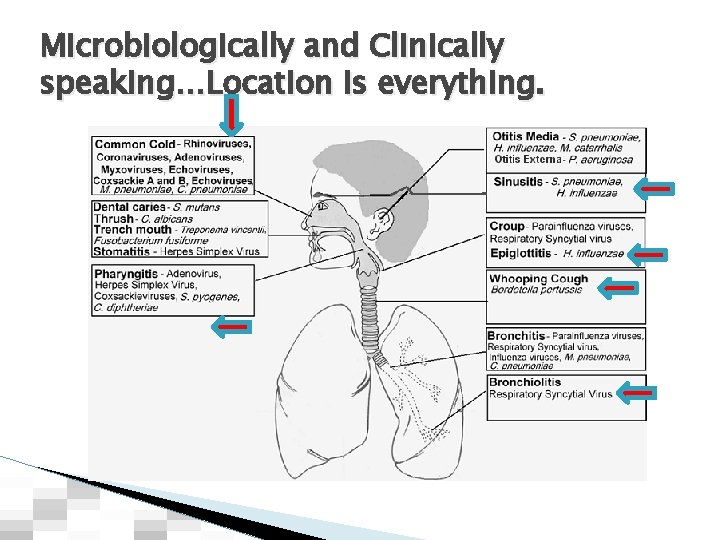
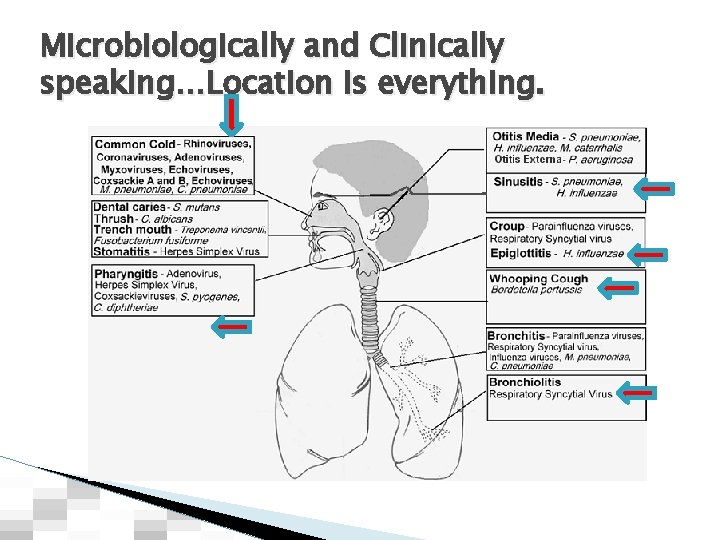
Microbiologically and Clinically speaking…Location is everything.
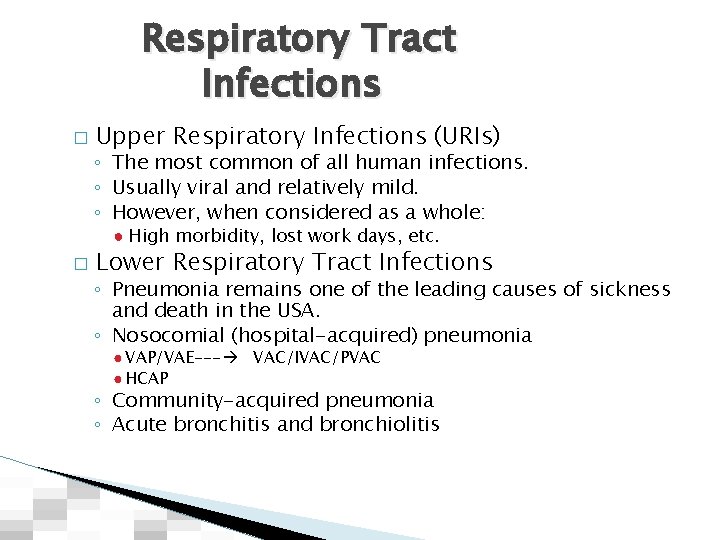
Respiratory Tract Infections � Upper Respiratory Infections (URIs) ◦ The most common of all human infections. ◦ Usually viral and relatively mild. ◦ However, when considered as a whole: ● High morbidity, lost work days, etc. � Lower Respiratory Tract Infections ◦ Pneumonia remains one of the leading causes of sickness and death in the USA. ◦ Nosocomial (hospital-acquired) pneumonia ● VAP/VAE--- VAC/IVAC/PVAC ● HCAP ◦ Community-acquired pneumonia ◦ Acute bronchitis and bronchiolitis
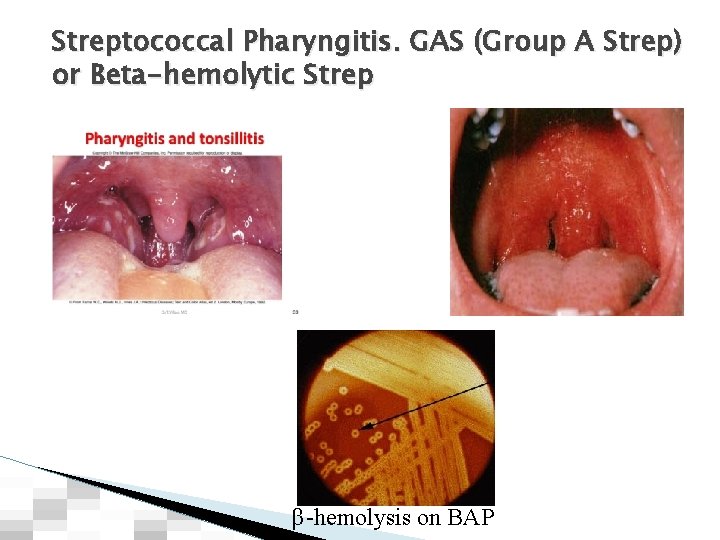
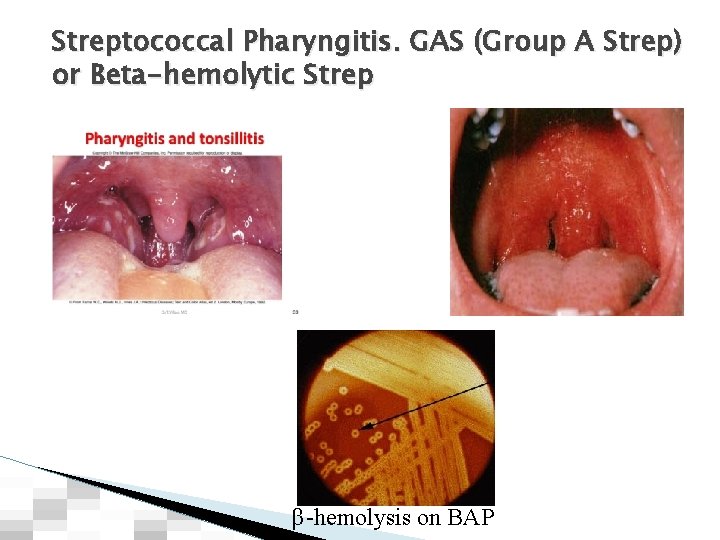
Streptococcal Pharyngitis. GAS (Group A Strep) or Beta-hemolytic Strep β-hemolysis on BAP
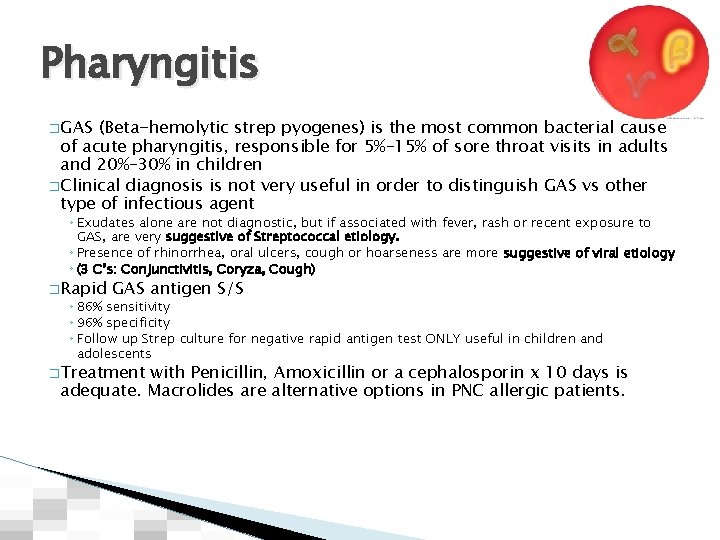
Pharyngitis � GAS (Beta-hemolytic strep pyogenes) is the most common bacterial cause of acute pharyngitis, responsible for 5%– 15% of sore throat visits in adults and 20%– 30% in children � Clinical diagnosis is not very useful in order to distinguish GAS vs other type of infectious agent ◦ Exudates alone are not diagnostic, but if associated with fever, rash or recent exposure to GAS, are very suggestive of Streptococcal etiology. ◦ Presence of rhinorrhea, oral ulcers, cough or hoarseness are more suggestive of viral etiology ◦ (3 C’s: Conjunctivitis, Coryza, Cough) � Rapid GAS antigen S/S ◦ 86% sensitivity ◦ 96% specificity ◦ Follow up Strep culture for negative rapid antigen test ONLY useful in children and adolescents � Treatment with Penicillin, Amoxicillin or a cephalosporin x 10 days is adequate. Macrolides are alternative options in PNC allergic patients.
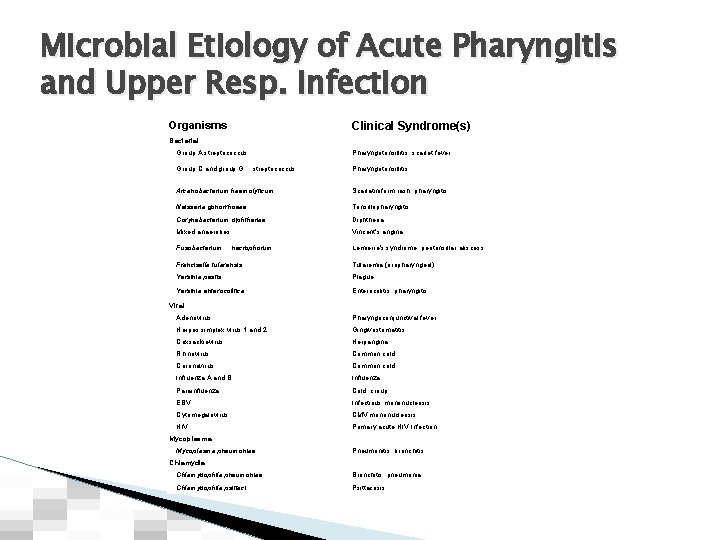
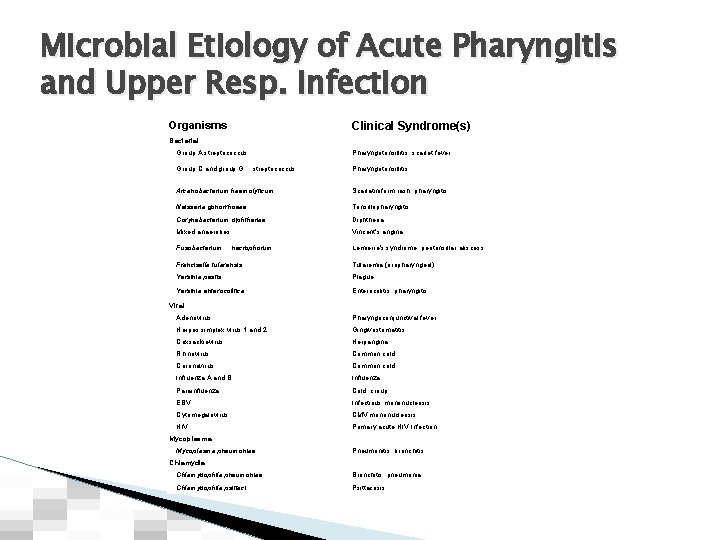
Microbial Etiology of Acute Pharyngitis and Upper Resp. infection Clinical Syndrome(s) Organisms Bacterial Group A streptococcus Group C and group G Pharyngotonsillitis, scarlet fever streptococcus Pharyngotonsillitis Arcanobacterium haemolyticum Scarlatiniform rash, pharyngitis Neisseria gonorrhoeae Tonsillopharyngitis Corynebacterium diphtheriae Diphtheria Mixed anaerobes Vincent's angina Fusobacterium necrophorum Lemierre's syndrome, peritonsillar abscess Francisella tularensis Tularemia (oropharyngeal) Yersinia pestis Plague Yersinia enterocolitica Enterocolitis, pharyngitis Viral Adenovirus Pharyngoconjunctival fever Herpes simplex virus 1 and 2 Gingivostomatitis Coxsackievirus Herpangina Rhinovirus Common cold Coronavirus Common cold Influenza A and B Influenza Parainfluenza Cold, croup EBV Infectious mononucleosis Cytomegalovirus CMV mononucleosis HIV Primary acute HIV Infection Mycoplasma pneumoniae Pneumonitis, bronchitis Chlamydia Chlamydophila pneumoniae Bronchitis, pneumonia Chlamydophila psittaci Psittacosis
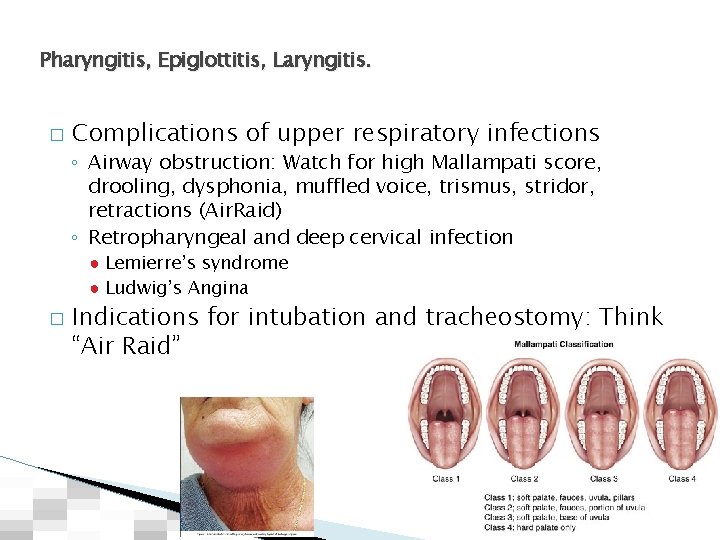
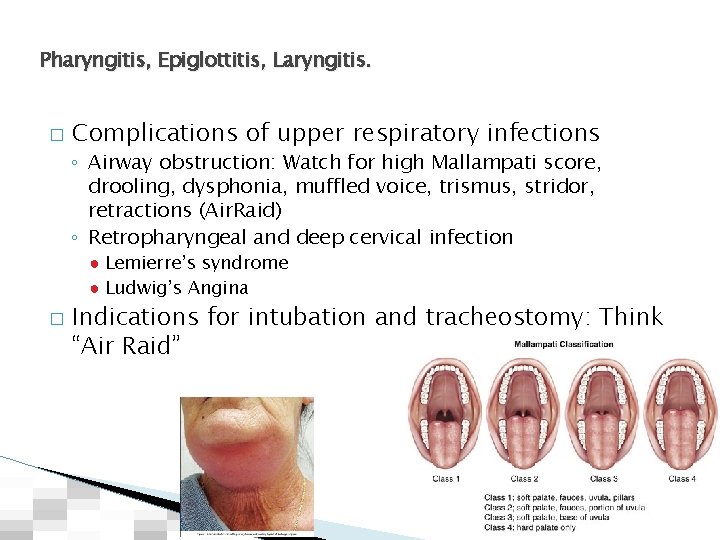
Pharyngitis, Epiglottitis, Laryngitis. � Complications of upper respiratory infections ◦ Airway obstruction: Watch for high Mallampati score, drooling, dysphonia, muffled voice, trismus, stridor, retractions (Air. Raid) ◦ Retropharyngeal and deep cervical infection ● Lemierre’s syndrome ● Ludwig’s Angina � Indications for intubation and tracheostomy: Think “Air Raid”
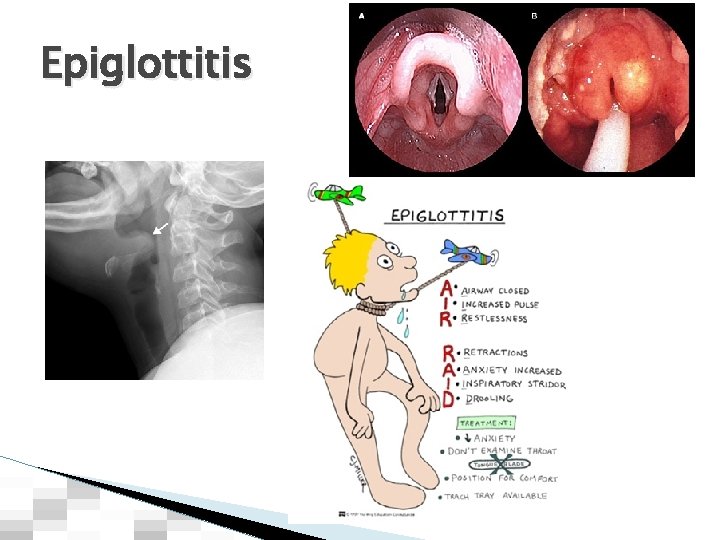
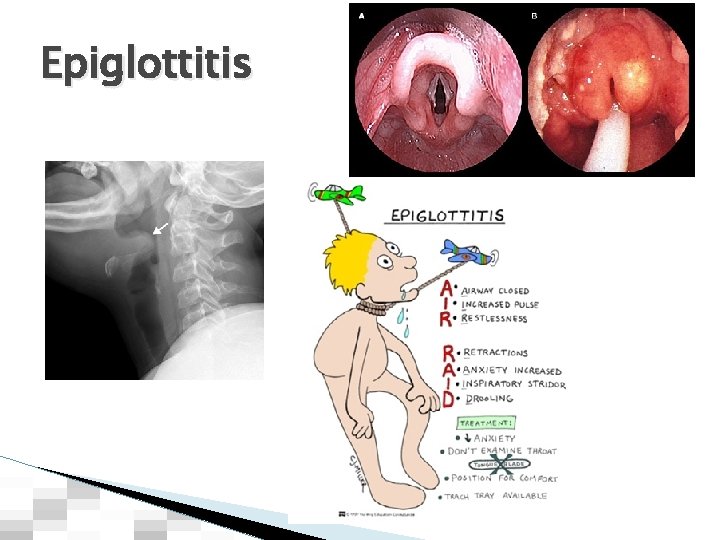
Epiglottitis
Transmission of Respiratory Pathogens � 3 types of transmission ◦ Droplets ◦ Airborne ◦ Contact
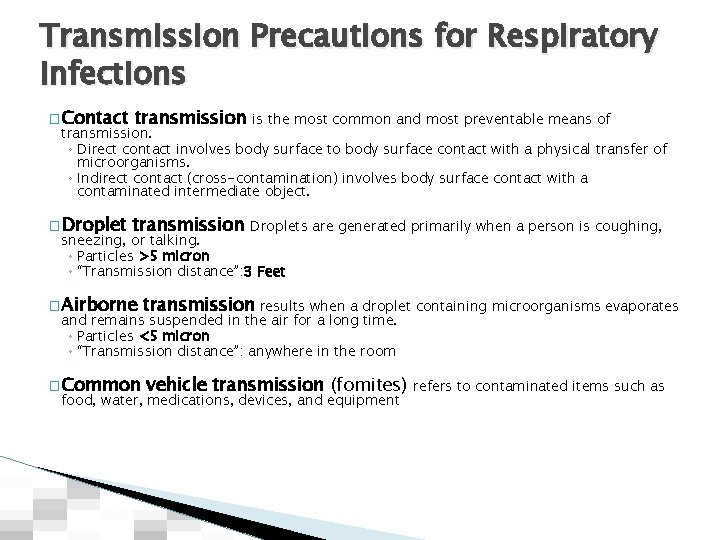
Transmission Precautions for Respiratory Infections � Contact transmission is the most common and most preventable means of � Droplet transmission Droplets are generated primarily when a person is coughing, transmission. ◦ Direct contact involves body surface to body surface contact with a physical transfer of microorganisms. ◦ Indirect contact (cross-contamination) involves body surface contact with a contaminated intermediate object. sneezing, or talking. ◦ Particles >5 micron ◦ “Transmission distance”: 3 Feet � Airborne transmission results when a droplet containing microorganisms evaporates � Common vehicle transmission (fomites) and remains suspended in the air for a long time. ◦ Particles <5 micron ◦ “Transmission distance”: anywhere in the room food, water, medications, devices, and equipment refers to contaminated items such as
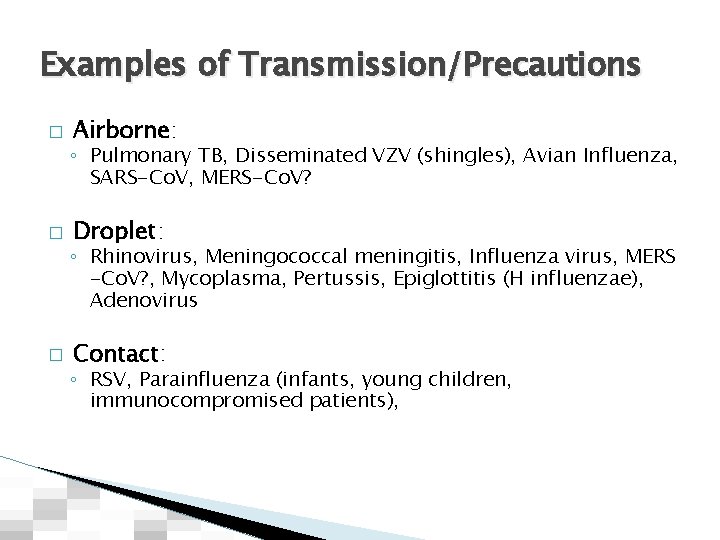
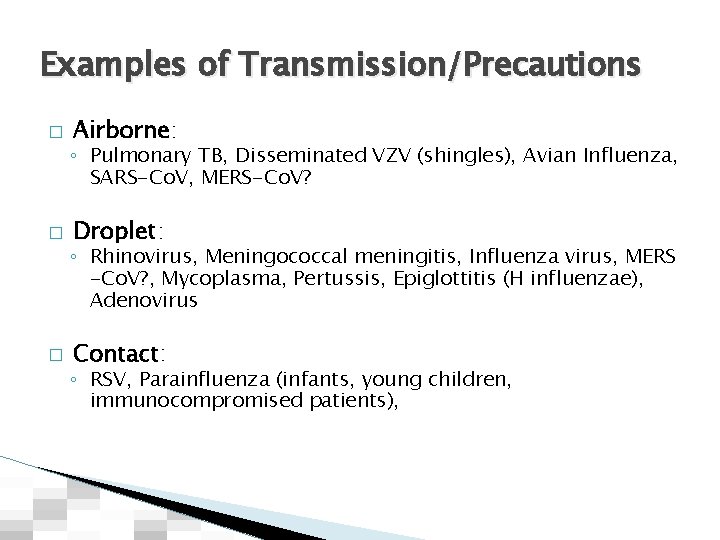
Examples of Transmission/Precautions � Airborne: ◦ Pulmonary TB, Disseminated VZV (shingles), Avian Influenza, SARS-Co. V, MERS-Co. V? � Droplet: ◦ Rhinovirus, Meningococcal meningitis, Influenza virus, MERS -Co. V? , Mycoplasma, Pertussis, Epiglottitis (H influenzae), Adenovirus � Contact: ◦ RSV, Parainfluenza (infants, young children, immunocompromised patients),
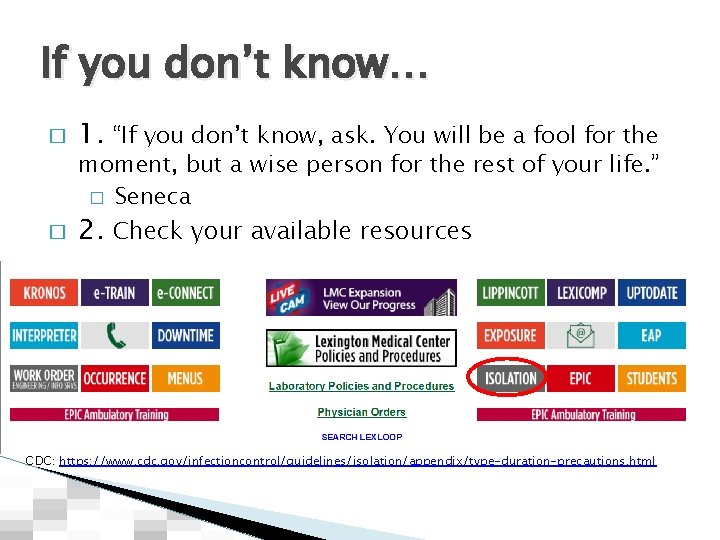
If you don’t know… � 1. “If you don’t know, ask. You will be a fool for the moment, but a wise person for the rest of your life. ” � Seneca � 2. Check your available resources CDC: https: //www. cdc. gov/infectioncontrol/guidelines/isolation/appendix/type-duration-precautions. html
Pneumonia in the ICU/intubated patient: VAP or VAE? � � � Different terminology Standardizes the clinical and diagnostic criteria (clinical vs surveillance definition) Physicians (and Radiologists) overestimate the incidence of PNA Not every CXRay abnormality indicates PNA The terminology can be confusing, even for ID docs, infection control practitioners, etc

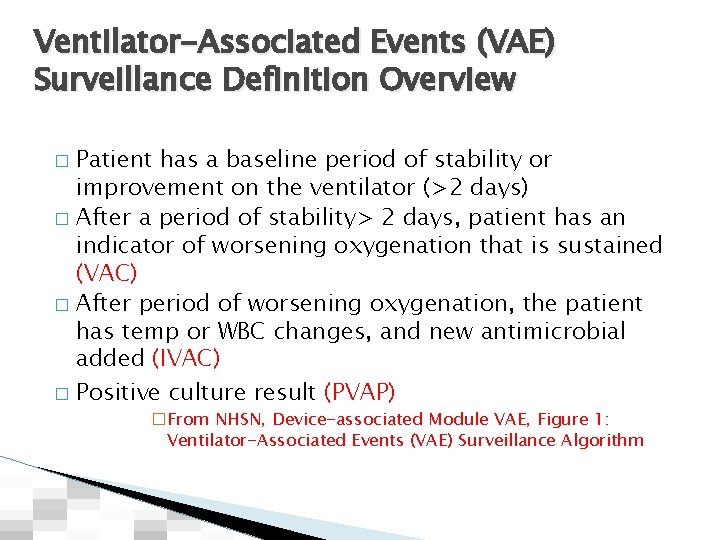
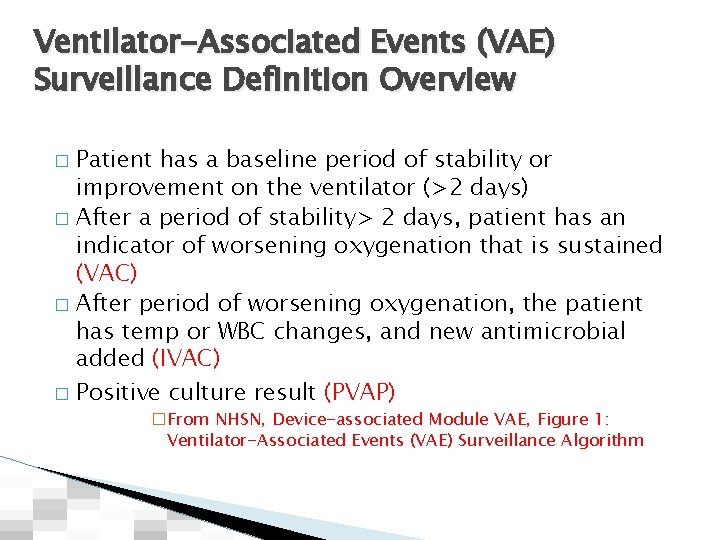
Ventilator-Associated Events (VAE) Surveillance Definition Overview Patient has a baseline period of stability or improvement on the ventilator (>2 days) � After a period of stability> 2 days, patient has an indicator of worsening oxygenation that is sustained (VAC) � After period of worsening oxygenation, the patient has temp or WBC changes, and new antimicrobial added (IVAC) � Positive culture result (PVAP) � �From NHSN, Device-associated Module VAE, Figure 1: Ventilator-Associated Events (VAE) Surveillance Algorithm

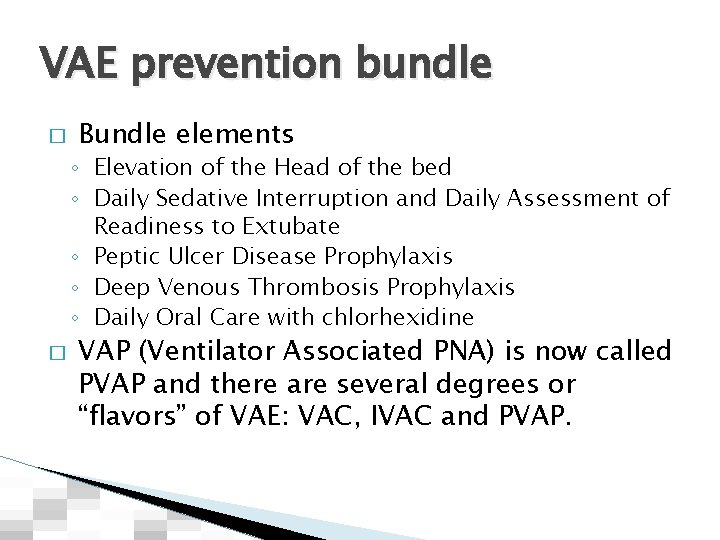
VAE prevention bundle � Bundle elements ◦ Elevation of the Head of the bed ◦ Daily Sedative Interruption and Daily Assessment of Readiness to Extubate ◦ Peptic Ulcer Disease Prophylaxis ◦ Deep Venous Thrombosis Prophylaxis ◦ Daily Oral Care with chlorhexidine � VAP (Ventilator Associated PNA) is now called PVAP and there are several degrees or “flavors” of VAE: VAC, IVAC and PVAP.
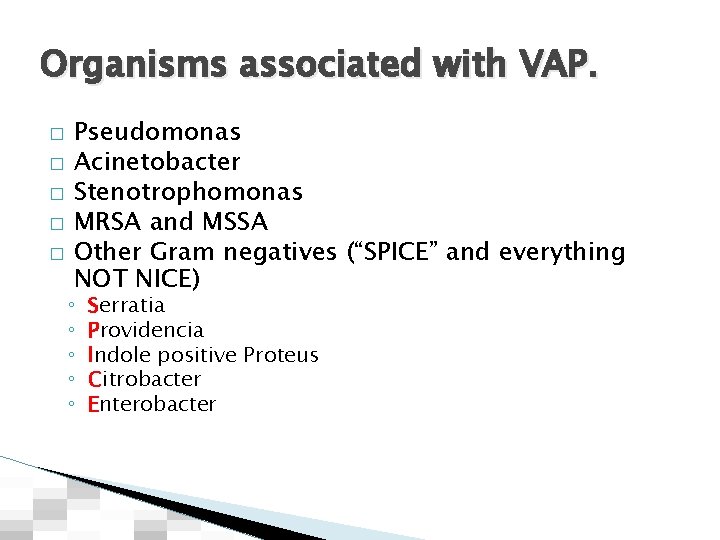
Organisms associated with VAP. � � � Pseudomonas Acinetobacter Stenotrophomonas MRSA and MSSA Other Gram negatives (“SPICE” and everything NOT NICE) ◦ ◦ ◦ Serratia Providencia Indole positive Proteus Citrobacter Enterobacter
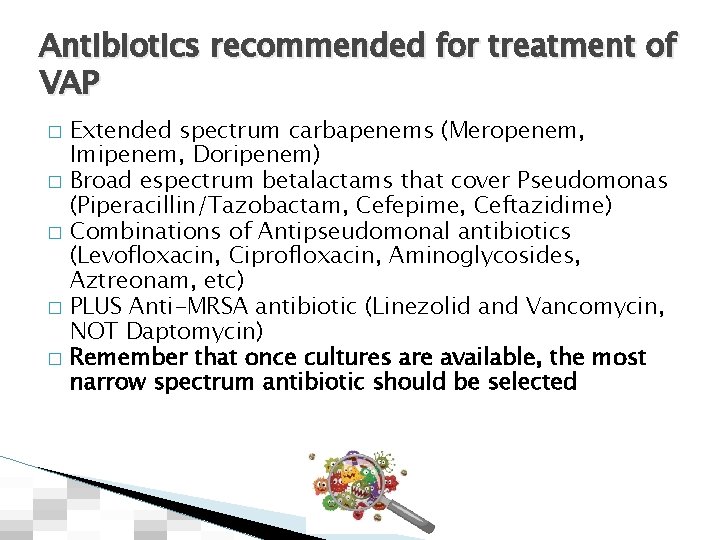
Antibiotics recommended for treatment of VAP � � � Extended spectrum carbapenems (Meropenem, Imipenem, Doripenem) Broad espectrum betalactams that cover Pseudomonas (Piperacillin/Tazobactam, Cefepime, Ceftazidime) Combinations of Antipseudomonal antibiotics (Levofloxacin, Ciprofloxacin, Aminoglycosides, Aztreonam, etc) PLUS Anti-MRSA antibiotic (Linezolid and Vancomycin, NOT Daptomycin) Remember that once cultures are available, the most narrow spectrum antibiotic should be selected
New diagnostic techniques for respiratory infections � Multiplex PCR/Film array panels: ◦ e. g. Respiratory Biofire Panel ◦ Tests for multiple bacterial and viral pathogens � � Rapid bacterial identification by Maldi-TOF Special tests on the BAL ◦ Galactomannan � 16 s Ribosomal RNA sequencing
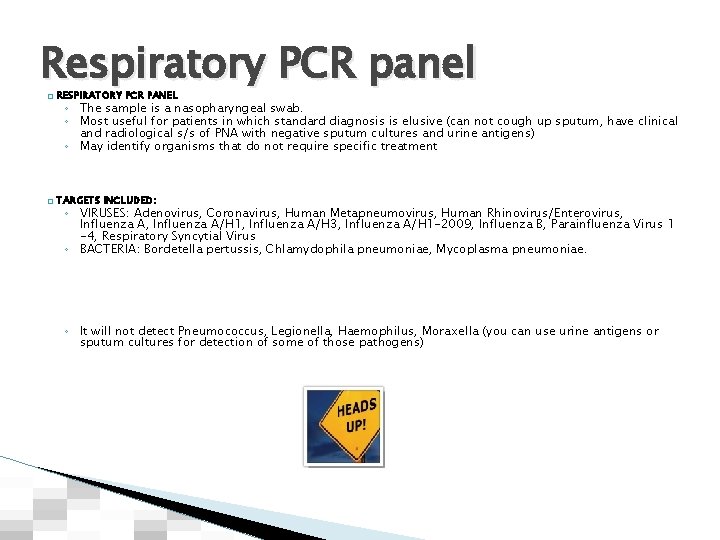
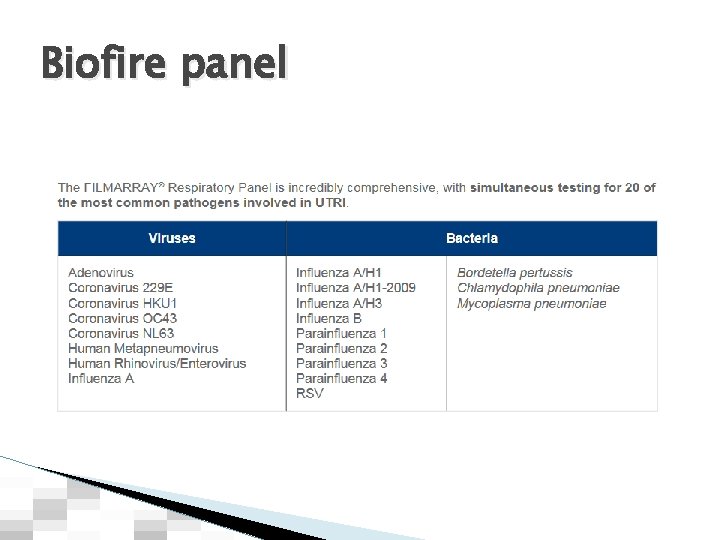
Respiratory PCR panel � RESPIRATORY PCR PANEL � TARGETS INCLUDED: ◦ The sample is a nasopharyngeal swab. ◦ Most useful for patients in which standard diagnosis is elusive (can not cough up sputum, have clinical and radiological s/s of PNA with negative sputum cultures and urine antigens) ◦ May identify organisms that do not require specific treatment ◦ VIRUSES: Adenovirus, Coronavirus, Human Metapneumovirus, Human Rhinovirus/Enterovirus, Influenza A/H 1, Influenza A/H 3, Influenza A/H 1 -2009, Influenza B, Parainfluenza Virus 1 -4, Respiratory Syncytial Virus ◦ BACTERIA: Bordetella pertussis, Chlamydophila pneumoniae, Mycoplasma pneumoniae. ◦ It will not detect Pneumococcus, Legionella, Haemophilus, Moraxella (you can use urine antigens or sputum cultures for detection of some of those pathogens)
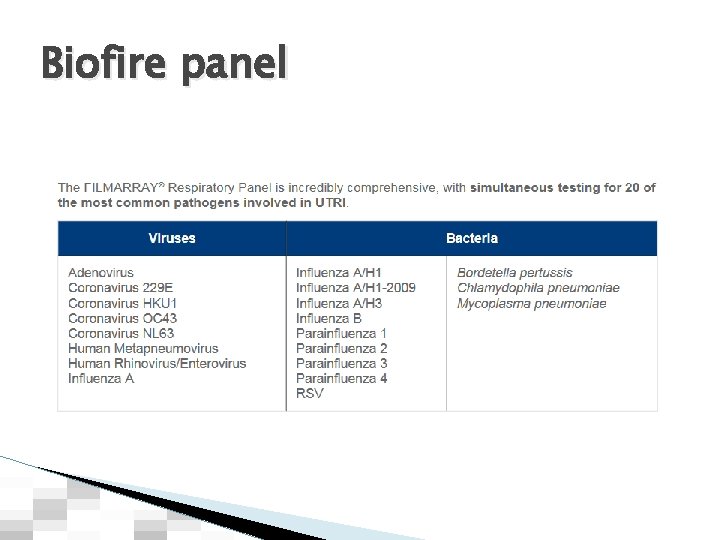
Biofire panel
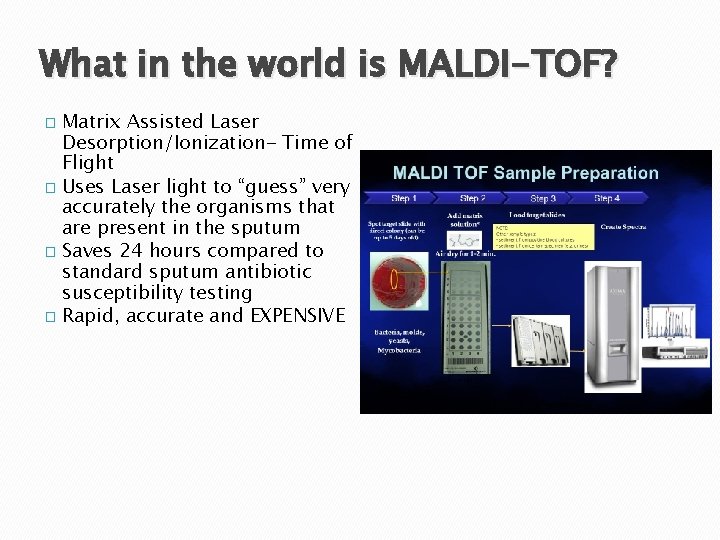
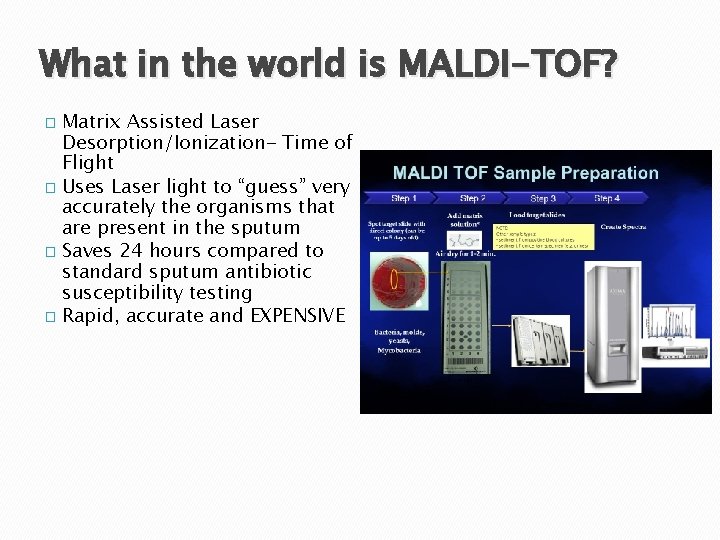
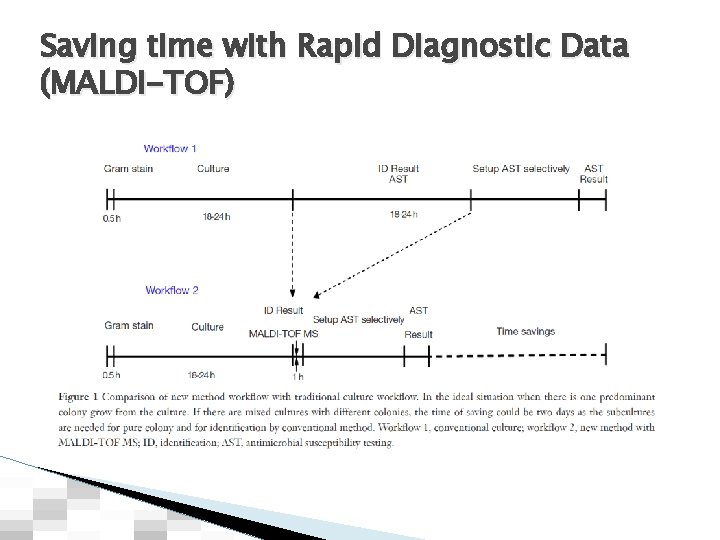
What in the world is MALDI-TOF? � Matrix Assisted Laser Desorption/Ionization- Time of Flight � Uses Laser light to “guess” very accurately the organisms that are present in the sputum � Saves 24 hours compared to standard sputum antibiotic susceptibility testing � Rapid, accurate and EXPENSIVE
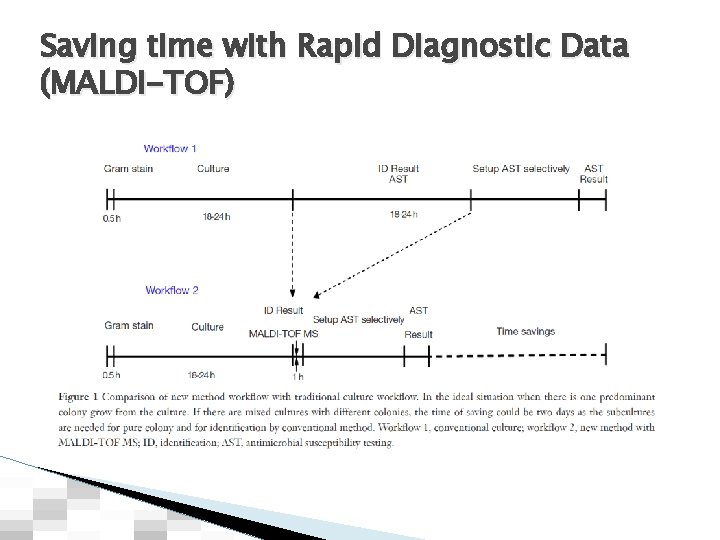
Saving time with Rapid Diagnostic Data (MALDI-TOF)
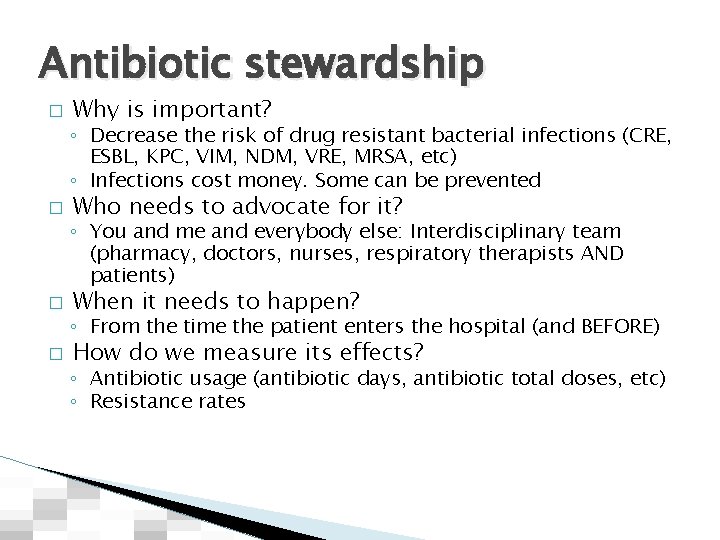
Antibiotic stewardship � Why is important? ◦ Decrease the risk of drug resistant bacterial infections (CRE, ESBL, KPC, VIM, NDM, VRE, MRSA, etc) ◦ Infections cost money. Some can be prevented � Who needs to advocate for it? ◦ You and me and everybody else: Interdisciplinary team (pharmacy, doctors, nurses, respiratory therapists AND patients) � When it needs to happen? ◦ From the time the patient enters the hospital (and BEFORE) � How do we measure its effects? ◦ Antibiotic usage (antibiotic days, antibiotic total doses, etc) ◦ Resistance rates
Drugs of abuse? : Think Antibiotics
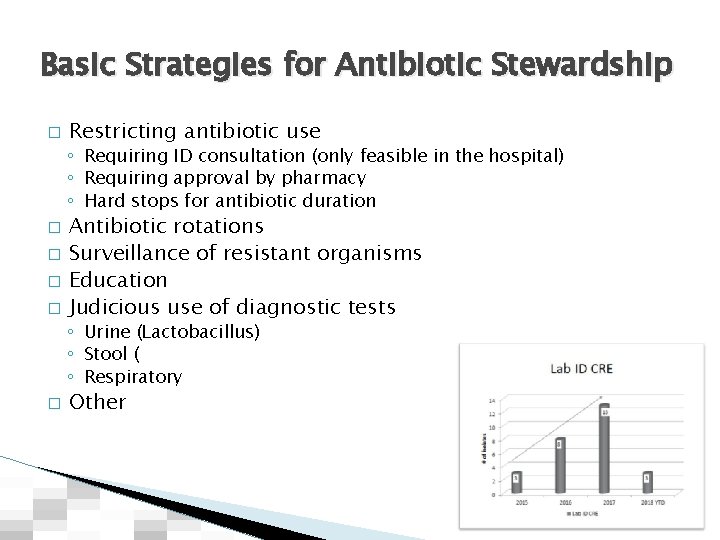
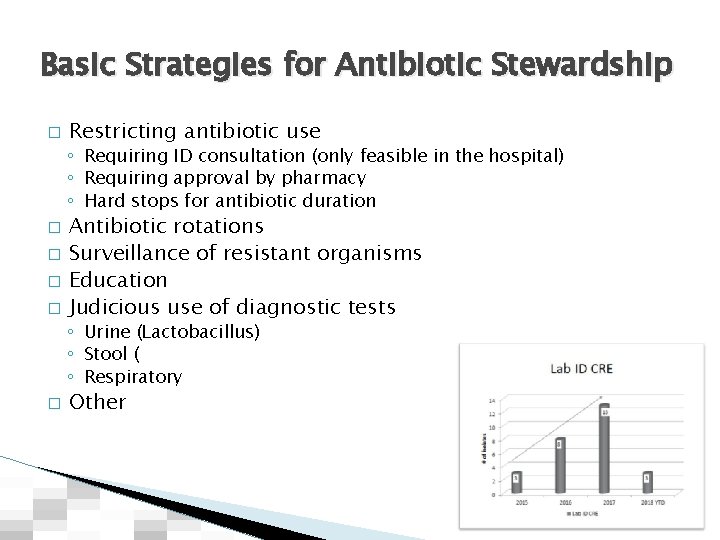
Basic Strategies for Antibiotic Stewardship � Restricting antibiotic use ◦ Requiring ID consultation (only feasible in the hospital) ◦ Requiring approval by pharmacy ◦ Hard stops for antibiotic duration � � Antibiotic rotations Surveillance of resistant organisms Education Judicious use of diagnostic tests ◦ Urine (Lactobacillus) ◦ Stool ( ◦ Respiratory � Other
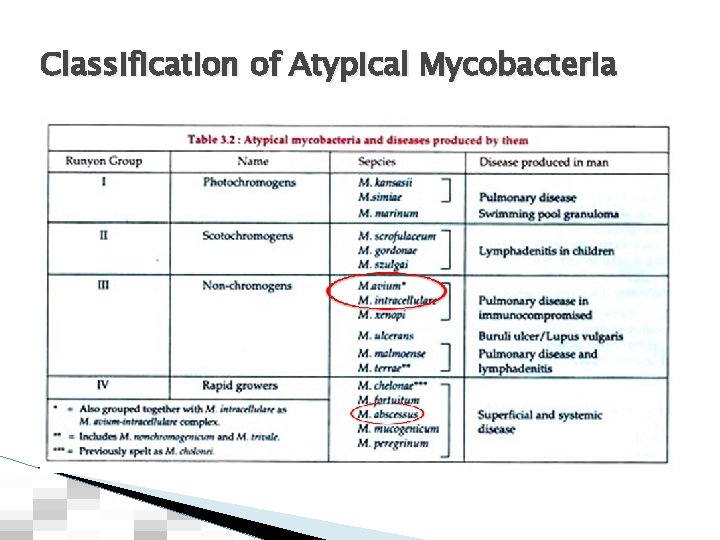
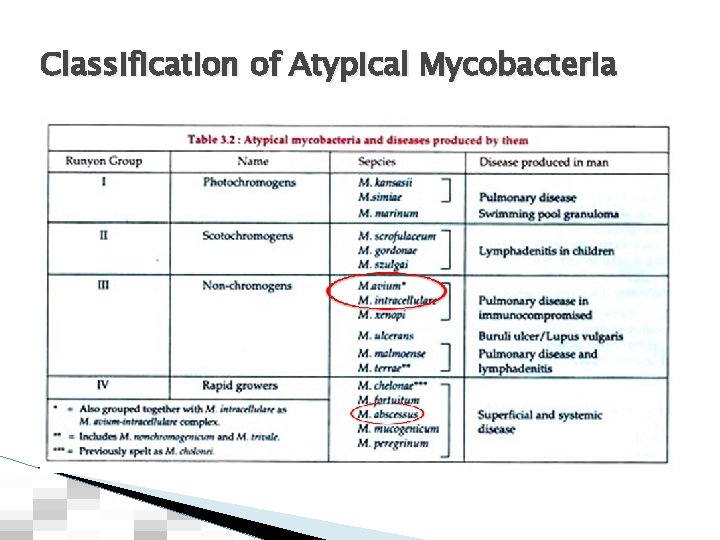
Classification of Atypical Mycobacteria
Mycobacterium Avium Complex (MAC) and other NTM � � � Very common infection in the Southeastern US Increasing incidence Widespread environmental pathogen (usually water born) No human transmission Diagnostic criteria for infection are strict Treatment is: ◦ Long and cumbersome ◦ Frequently associated with side effects ◦ Not very effective
The alphabet soup of NTMB (Atypical mycobacteria) � � NTBM/NTM: Non tuberculous mycobacteria MOTT: Mycobacterium other than tuberculosis AFB: Acid Fast Bacilli MAC/MAI: Mycobacterium avium complex/intracellulare
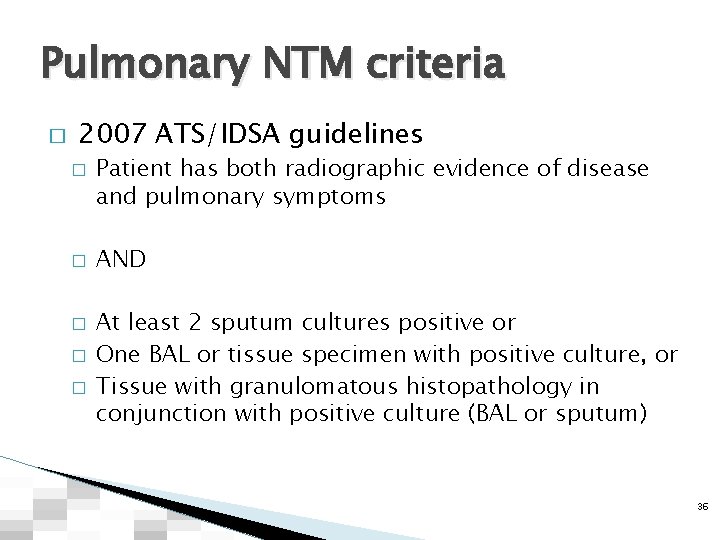
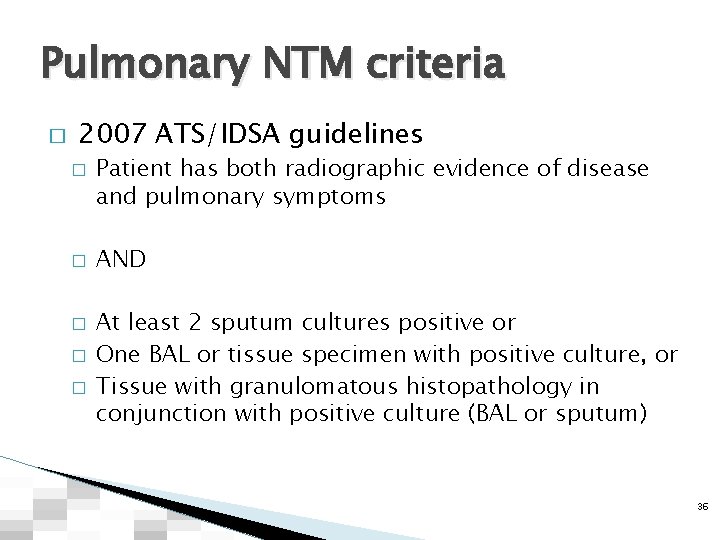
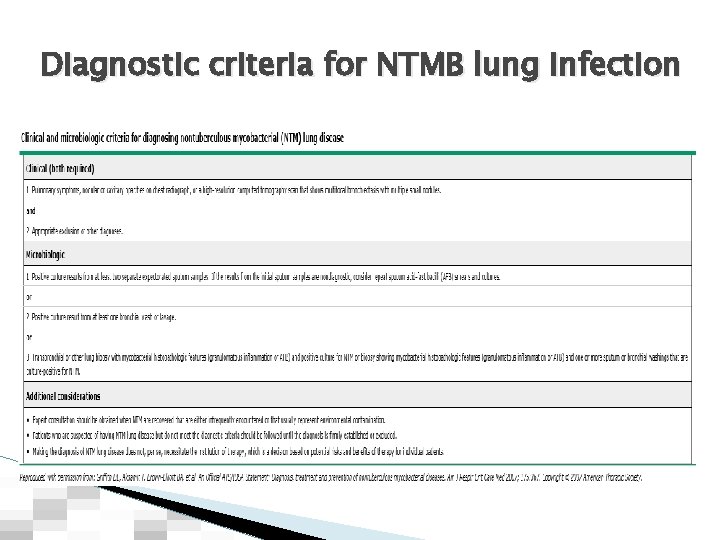
Pulmonary NTM criteria � 2007 ATS/IDSA guidelines � � � Patient has both radiographic evidence of disease and pulmonary symptoms AND At least 2 sputum cultures positive or One BAL or tissue specimen with positive culture, or Tissue with granulomatous histopathology in conjunction with positive culture (BAL or sputum) 36

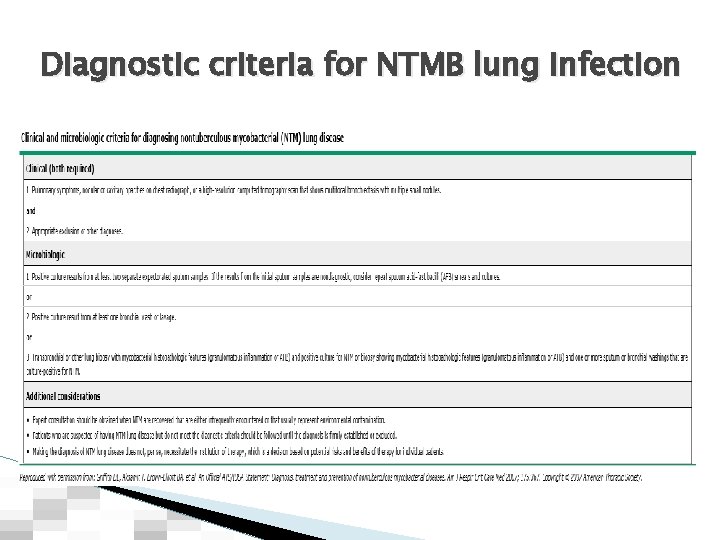
Diagnostic criteria for NTMB lung infection
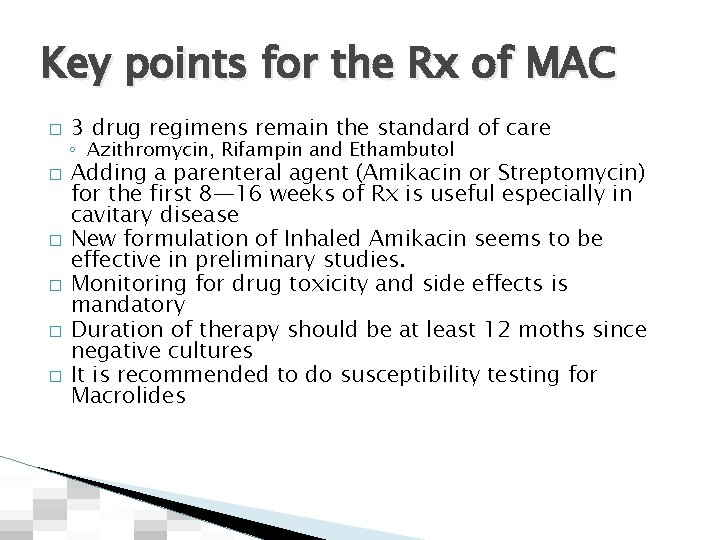
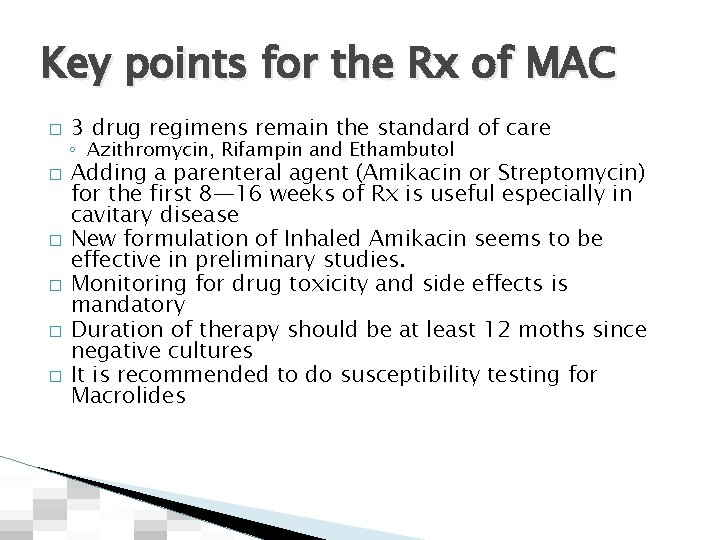
Key points for the Rx of MAC � � � 3 drug regimens remain the standard of care ◦ Azithromycin, Rifampin and Ethambutol Adding a parenteral agent (Amikacin or Streptomycin) for the first 8— 16 weeks of Rx is useful especially in cavitary disease New formulation of Inhaled Amikacin seems to be effective in preliminary studies. Monitoring for drug toxicity and side effects is mandatory Duration of therapy should be at least 12 moths since negative cultures It is recommended to do susceptibility testing for Macrolides
What do you see?
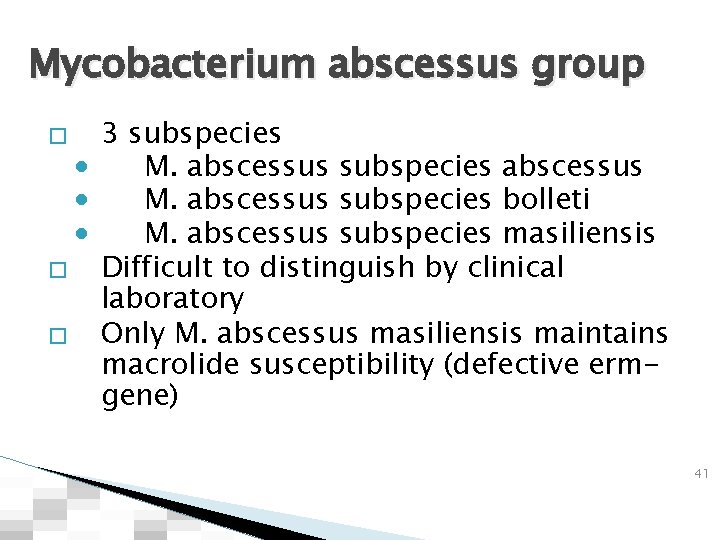
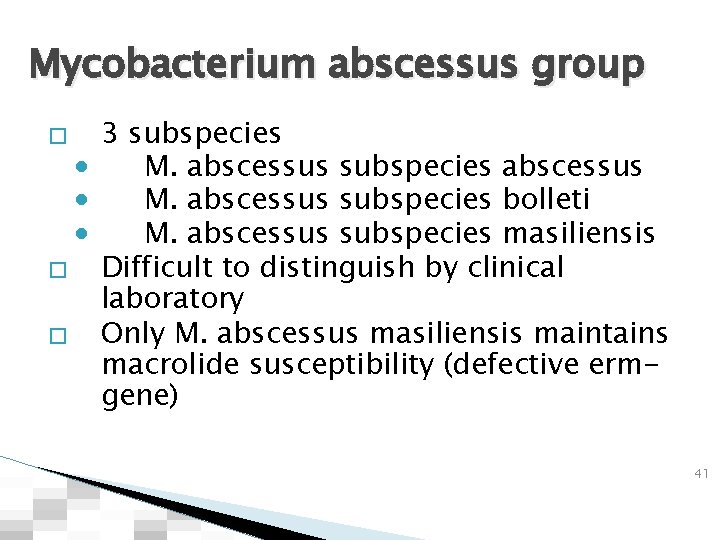
Mycobacterium abscessus group 3 subspecies • M. abscessus subspecies abscessus • M. abscessus subspecies bolleti • M. abscessus subspecies masiliensis � Difficult to distinguish by clinical laboratory � Only M. abscessus masiliensis maintains macrolide susceptibility (defective ermgene) � 41
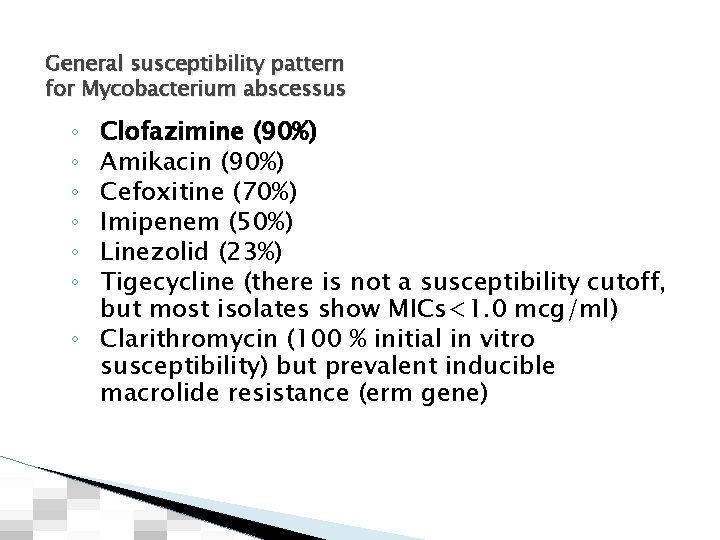
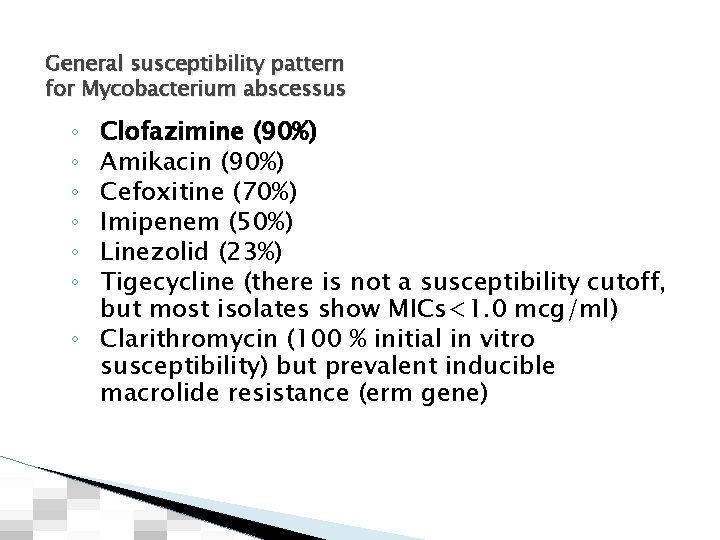
General susceptibility pattern for Mycobacterium abscessus Clofazimine (90%) Amikacin (90%) Cefoxitine (70%) Imipenem (50%) Linezolid (23%) Tigecycline (there is not a susceptibility cutoff, but most isolates show MICs<1. 0 mcg/ml) ◦ Clarithromycin (100 % initial in vitro susceptibility) but prevalent inducible macrolide resistance (erm gene) ◦ ◦ ◦
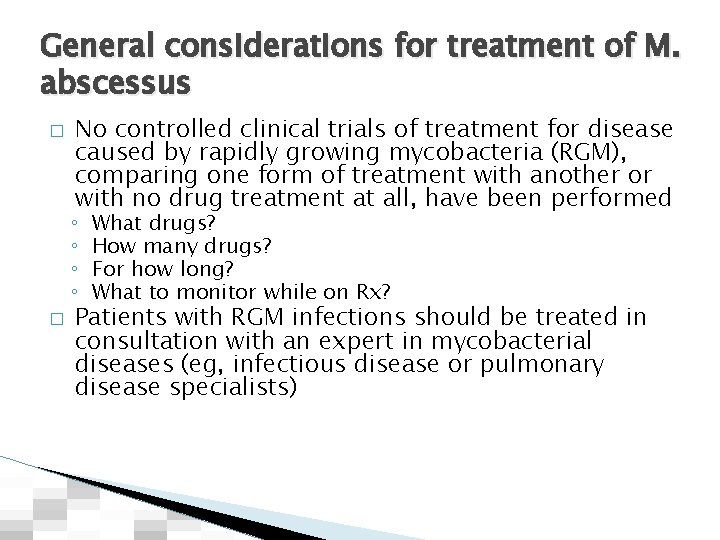
General considerations for treatment of M. abscessus � No controlled clinical trials of treatment for disease caused by rapidly growing mycobacteria (RGM), comparing one form of treatment with another or with no drug treatment at all, have been performed ◦ ◦ � What drugs? How many drugs? For how long? What to monitor while on Rx? Patients with RGM infections should be treated in consultation with an expert in mycobacterial diseases (eg, infectious disease or pulmonary disease specialists)
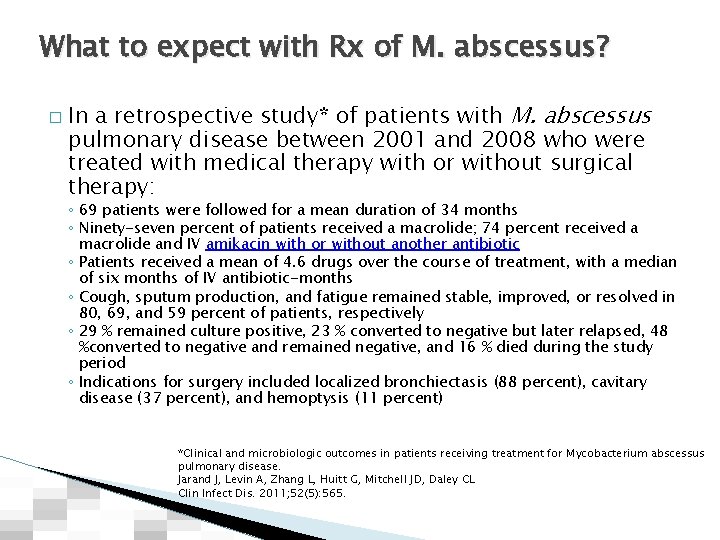
What to expect with Rx of M. abscessus? � In a retrospective study* of patients with M. abscessus pulmonary disease between 2001 and 2008 who were treated with medical therapy with or without surgical therapy: ◦ 69 patients were followed for a mean duration of 34 months ◦ Ninety-seven percent of patients received a macrolide; 74 percent received a macrolide and IV amikacin with or without another antibiotic ◦ Patients received a mean of 4. 6 drugs over the course of treatment, with a median of six months of IV antibiotic-months ◦ Cough, sputum production, and fatigue remained stable, improved, or resolved in 80, 69, and 59 percent of patients, respectively ◦ 29 % remained culture positive, 23 % converted to negative but later relapsed, 48 %converted to negative and remained negative, and 16 % died during the study period ◦ Indications for surgery included localized bronchiectasis (88 percent), cavitary disease (37 percent), and hemoptysis (11 percent) *Clinical and microbiologic outcomes in patients receiving treatment for Mycobacterium abscessus pulmonary disease. Jarand J, Levin A, Zhang L, Huitt G, Mitchell JD, Daley CL Clin Infect Dis. 2011; 52(5): 565.
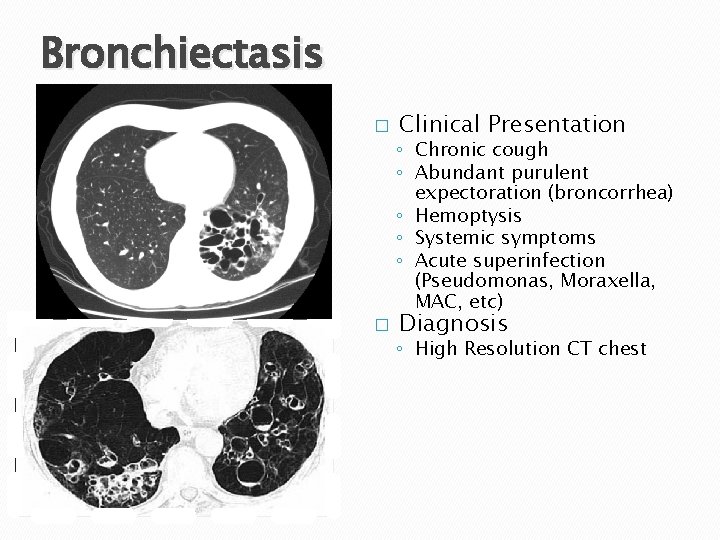
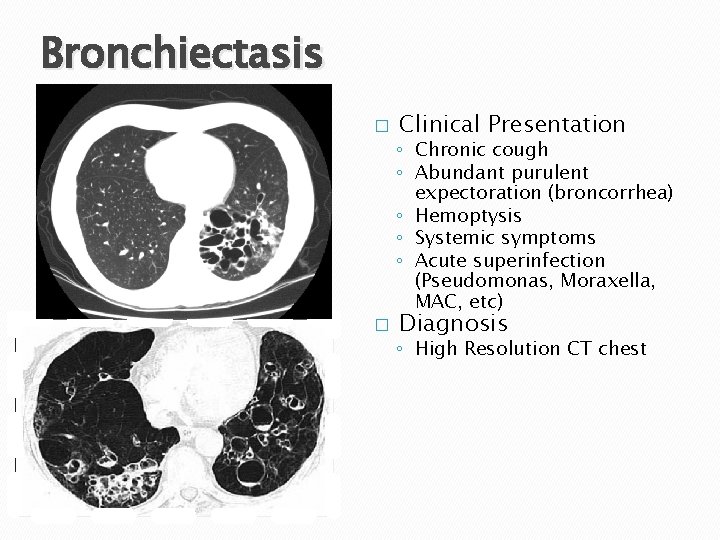
Bronchiectasis � Clinical Presentation ◦ Chronic cough ◦ Abundant purulent expectoration (broncorrhea) ◦ Hemoptysis ◦ Systemic symptoms ◦ Acute superinfection (Pseudomonas, Moraxella, MAC, etc) � Diagnosis ◦ High Resolution CT chest
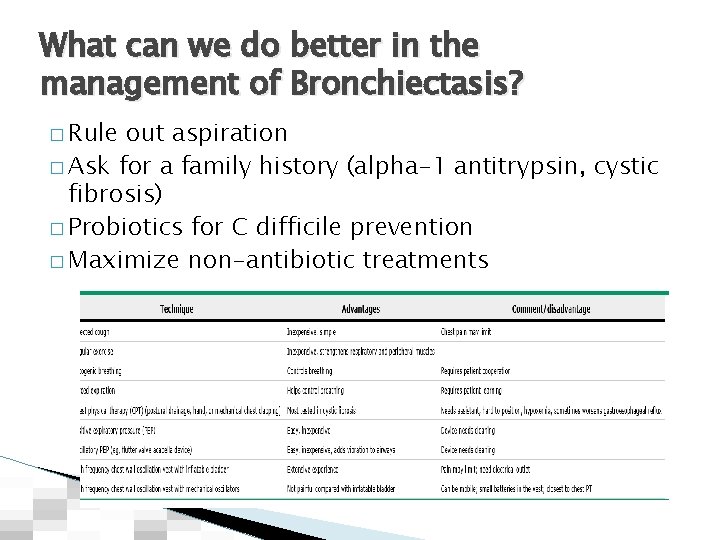
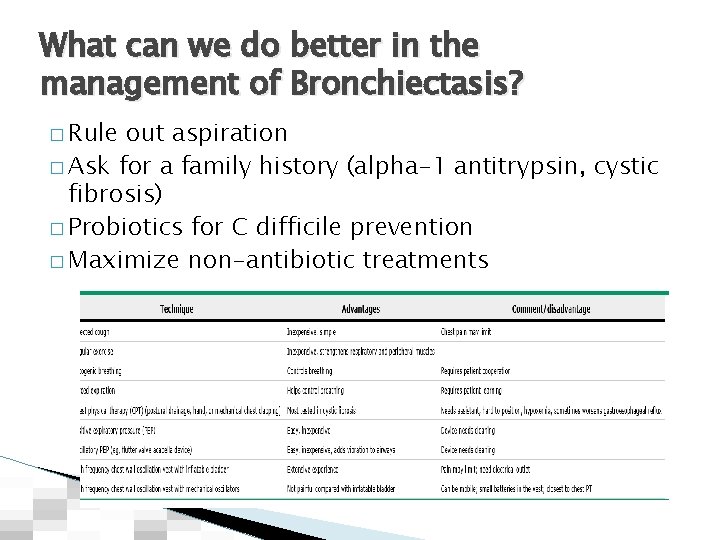
What can we do better in the management of Bronchiectasis? � Rule out aspiration � Ask for a family history (alpha-1 antitrypsin, cystic fibrosis) � Probiotics for C difficile prevention � Maximize non-antibiotic treatments
Treatment for Bronchiectasis � Oral agents have variable penetration in the lung and alveolar tissue. Quinolones and macrolides are usually the best option � IV antibiotics reserve for severe exacerbations � Aerosolized agents are very effective for short term treatment. Be aware of bronchospasm. ◦ Tobramycin and Gentamicin (Amikacin? ) ◦ Aztreonam ◦ Colistin � Development of antimicrobial resistance is a concern � Don’t forget the basics: Mucolytic agents, hydration, bronchodilation, bronchial hygiene, etc.

evperezjorge@lexhealth. org
 Cell lysis complement system
Cell lysis complement system Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Johnson and johnson botnet infections
Johnson and johnson botnet infections Infections opportunistes digestives
Infections opportunistes digestives Methotrexate and yeast infections
Methotrexate and yeast infections Genital infections
Genital infections Storch infections
Storch infections Bacterial vaginosis
Bacterial vaginosis Opportunistic infections
Opportunistic infections Amber blumling
Amber blumling Storch infections
Storch infections Postpartum infections
Postpartum infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Classification of acute gingival infections
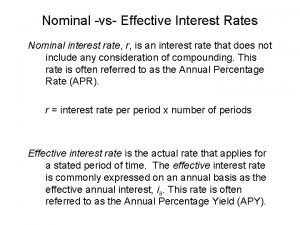
Classification of acute gingival infections What is real interest rate and nominal interest rate
What is real interest rate and nominal interest rate Effective interest rate formula
Effective interest rate formula Simple interest
Simple interest Conducting zone and respiratory zone
Conducting zone and respiratory zone Therapist driven protocols
Therapist driven protocols Massage therapist
Massage therapist Therapist responsibilities
Therapist responsibilities Yvonne jackson therapist
Yvonne jackson therapist Robyn smith therapist
Robyn smith therapist Senior occupational therapist
Senior occupational therapist Difference between oedipus complex and electra complex
Difference between oedipus complex and electra complex Orthoptist music therapist
Orthoptist music therapist Raul and sophia were having a picnic
Raul and sophia were having a picnic Gillian hazell speech language therapist
Gillian hazell speech language therapist Randall woodfield
Randall woodfield Dental health aide therapist
Dental health aide therapist Annie o'connor physical therapist
Annie o'connor physical therapist Wont bouncer therapist referee have advice
Wont bouncer therapist referee have advice Observed experiential integration
Observed experiential integration Eclectic psychology
Eclectic psychology Fspos vägledning för kontinuitetshantering
Fspos vägledning för kontinuitetshantering Orubbliga rättigheter
Orubbliga rättigheter Steg för steg rita
Steg för steg rita Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Kanaans land
Kanaans land Bästa kameran för astrofoto
Bästa kameran för astrofoto Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Ro i rom pax
Ro i rom pax Dikt fri form
Dikt fri form Datumr
Datumr Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? Matematisk modellering eksempel
Matematisk modellering eksempel