Residual Ridge Resorption Introduction E The most striking



- Slides: 38

Residual Ridge Resorption
Introduction E The most striking feature of the extraction wound healing is that even after the healing of wounds E The size of the residual ridge is reduced most rapidly in the first six months, but the bone resorption activity of the residual ridge continues throughout life at a slower rate, resulting in removal of a large amount of jaw structure. E This unique phenomenon has been described as residual ridge reduction.

Pathology of RRR
Gross Pathology: • A frequent lay expression for RRR is “My gums have shrunk”. • Actually the basic change in RRR is a reduction in the size of the bony ridge under the mucoperiosteum. • It is primarily a localized of bone structure. Sometimes it may leave the overlying mucoperiosteum excessive and redundant • Lamie has stated: “One factor in RRR may be a cicatrizing mucoperiosterm that is a seeking a reduced area, resulting in pressure resoption of the underlying bone”.
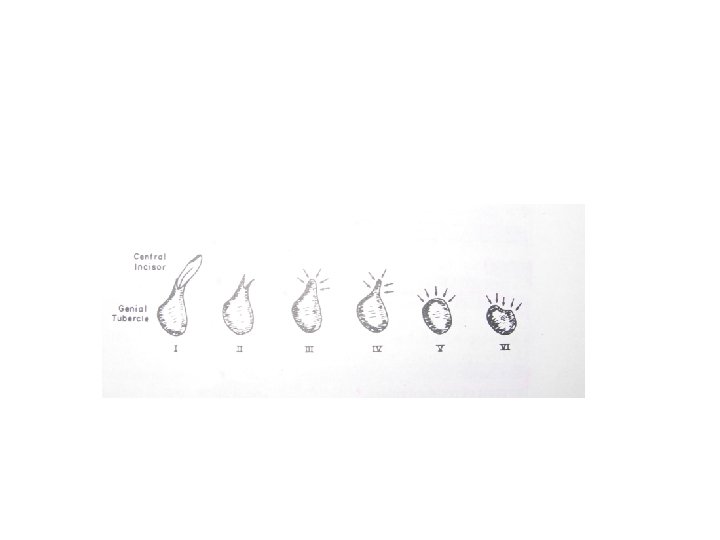
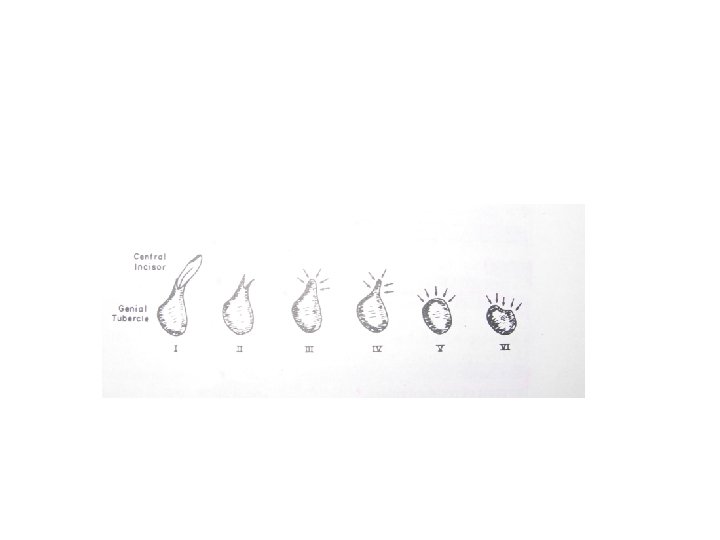
Atwood s classification • There exists a wide variety of shapes and sizes of residual ridges. They are categorized into common residual ridge configuration in a system of six orders given by Atwood. C Order I - Pre-extraction. C Order II - Post-extraction. C Order III - High, well rounded. C Order IV - Knife-edge. C Order V - low, well-rounded. C Order VI - depressed.
Microscopic Pathology • Microscopic studies have revealed osteoclastic activity on the external surface of the crest of residual ridges. • The scalloped margins of Howship’s lacunae sometimes contain visible osteoclasts which cause bone resorption. • Frequently, the scalloped external surface is inactive without visible bone resorbing cells and is covered by fibrous non-osteogenic periosteum.
Microscopic Pathology • There exists a wide variation in the configuration, density and porosity of the residual ridges, sometimes even with evidence of osteoporosis. Smooth, periosteal lamellar bone is present on the lingual, inferior and labial surfaces of the mandibles, but is totally absent on the crest of the ridge. • Studies have shown the presence of new bone and reversal lines inside the residual ridge and minute areas of bony repair on the periosteal side in some specimens. • The mucoperiosteum shows varying degrees of keratinization, acanthosis, edema and architectural pattern of mucosal epithelium in the same mouth and between subjects
PATHOPHYSIOLOGY OF RRR • Except during growth when bone formation exceeds bone resorption, bone resorption and bone formation are normally in equilibrium. • Osteoporosis is a generalized disease of bone in which bone is in negative balance, because bone resorption exceeds bone formation. • In periodontal disease, there is a localized destruction of the bone around teeth, perhaps due to certain local pathologic processes. • In both generalized osteoporosis and localized periodontal disease, when bone matrix is lost it does not ordinarily return.
• To date the process of RRR has not been reversed such that the residual ridge has increased in size. • Yet the physiologic process of internal bone remodeling goes on even in the presence of this pathologic external osteoclastic activity that is responsible for the loss of so much bone substance. • It is clear that a great deal residual ridge may be removed in toto, and yet there is often a cortical layer of bone over the crest of the ridge • Enlow’s work, which has clearly illustrated the normal growth pattern of long bones.
Pathogenesis of RRR • Annual increments of bone loss have a cumulative effect, leaving less and less residual ridge. • A number of cephalometric studies of RRR have been carried out in a number of different countries • RRR is chronic, progressive, irreversible and cumulative. Usually, RRR proceeds slowly over a long period of time, flowing from one stage imperceptibly to the next. Autonomous regrowth has not been reported
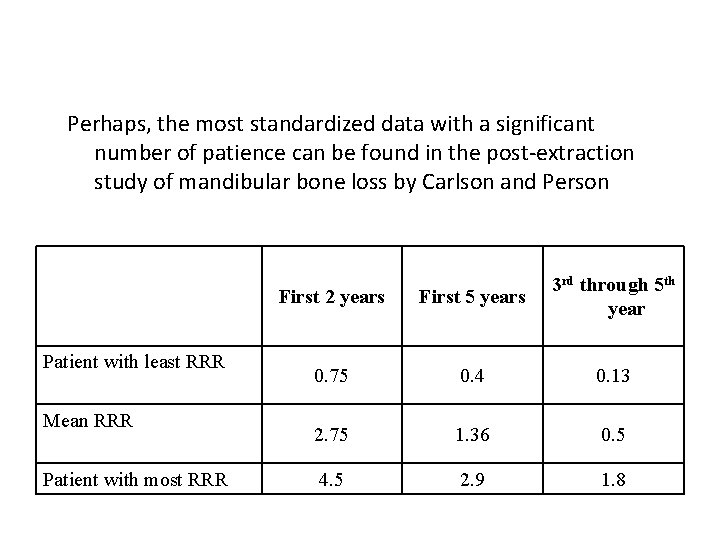
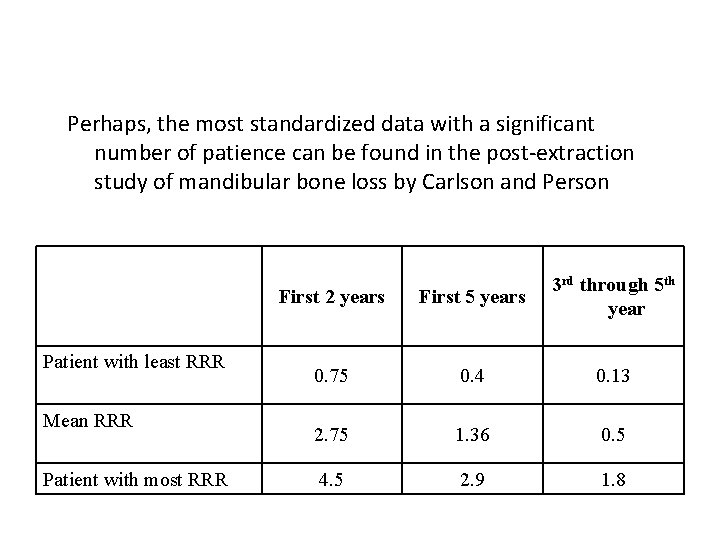
Perhaps, the most standardized data with a significant number of patience can be found in the post-extraction study of mandibular bone loss by Carlson and Person Patient with least RRR Mean RRR Patient with most RRR First 2 years First 5 years 3 rd through 5 th year 0. 75 0. 4 0. 13 2. 75 1. 36 0. 5 4. 5 2. 9 1. 8
• Tallgren has presented an interesting graph of mean rates of RRR of patients who were studied at various post-extraction time periods over a 25 year period. • In separate studies in different parts of the world, Tallgren, Atwood and Coy found that the mean ratio of anterior maxillary RRR to anterior mandibular RRR was 1: 4.
Etiology of RRR: • RRR is a multi-factorial, biomechanical disease that results from a combination of anatomic, metabolic and mechanical determinants. • Since all of these factors vary from one patient to the next, these different co-factors may combine in infinite variety of ways, thus explaining the variations in RRR between patients
Anatomic Factors RRR Anatomic factors • The more the bone there is, the more RRR there will ultimately be • The amount of bone is not a prognosticator of the rate of RRR, for sometimes large ridges resorb rapidly and some knifeedges ridges may remain with little or no change for a long period of time. • Rather, we should try to evaluate the present status of the residual ridge to determine what has gone on before
Introduction • The most striking feature of the extraction wound healing is that even after the healing of wounds • The size of the residual ridge is reduced most rapidly in the first six months, but the bone resorption activity of the residual ridge continues throughout life at a slower rate, resulting in removal of a large amount of jaw structure. • This unique phenomenon has been described as residual ridge reduction. Your subtopic goes here
Quality of bone Intra-oral roentgenograms are made to check the density of residual ridges. • On theoretic grounds, with everything else equal, the denser the bone, the slower the rate of resorption, merely because there is more bone to be resorbed per unit of time. Every patient is however is different. • Any anatomic advantages may be completely offset by certain metabolic disadvantages. • * Osteoporosic patients decreased density of bone Increased RRR
Metabolic factors: RRR Bone resorption factors Bone formation factors
The four main levels of bone activity are: C 1) equilibrium C 2) growth C 3) atrophy, resulting from downward osteoblastic activity as in osteoporosis and in disuse atrophy, and C 4) resorption, caused by upward osteoclastic activity as in hyperparathyroidism and in pressure resorption.
Functional Factors: Functional factors include the frequency, intensity, duration and direction of forces applied to bone which are translated into cellular activity, resulting in either bone formation or bone resorption, depending upon on the patient’s individual resistance to these forces. RRR Force Damping Effect
• Basset, has suggested that the mechanism by which fore is translated into bone remodeling (Wolff’s law) may be through the bioelectric properties of bone. • In considering force, one must concern oneself not only with the amount of force, but also with the frequency of force, duration, direction of force, the area over which the force is distributed (force per unit area) and the damping effect of the underlying tissue.
• RRR Force • The amount of force applied to the bone may be affected inversely by the “damping effect” • RRR 1 Damping effect
• The importance of time in extraction to the bone loss curves, should be emphasized by adding an inverse relation RRR 1 Time
Prosthetic Factors
• The prosthetic factors are extremely difficult to evaluate because of tremendous number of variables, including anatomic, metabolic and functional factors. • The traditional design of dentures includes many features whose goal is to reduce the amount of force to the ridge and to thereby reduce RRR.
• These prosthetic factors include broad-area coverage (to reduce the force per unit area) • decreased number of dental units, decreased buccolingual width of teeth, and improved tooth form (to decrease the amount of force required to penetrate a bolus of food); avoidance of inclined planes (to minimize dislodgement of dentures and shear forces) • centralization of occlusal contacts (to increase stability of dentures and to maximize compressive forces); provision of adequate tongue room (to increase stability of denture in speech and mastication)
• Adequate interocclusal distance during rest jaw relation (to decrease the frequency and duration of tooth contacts) etc. • Various clinical studies have attempted to correlate one or more of these factors with the rate of RRR.
Mechanical Stress by prostheses affecting bone resorption A prospective clinical study addressing the mechanical factors on RRR was conducted by Carlson et al in which partially edentulous patients (Kennedy Class I) were divided into three experimental groups wearing 1) no mandibular dentures, 2) partial denture with bilateral free-end denture bases and 3) partial denture with anterior alveolar bar.
• The longitudinal observation of the edentulous ridge of these patients revealed the increased rate of RRR in the groups of wearing dentures. • Bone that receives constant mechanical stimuli maintains a coupled cellular activity between osteoclasts and osteoblasts. When the bone tissue is placed in a state of immobilization or a weightless environment, it bears less mechanical stress and cannot sustain the normal coupled remodeling process and results in loss of calcified bone mass described as disuse atrophy. • Conversely, applied mechanical force can stimulate bone opposition.
• Yeh and Rodan reported that repetitive mechanical stresses applied to osteoblastic cells in vitro significantly increased prostaglandin E 2 Synthesis. • The direct relationship between mechanical and residual ridge and prostaglandin mediated bone resorption causing severe form of RRR has not yet been fully elucidated. • The hypothesis presented is that RRR is a multifactorial disease in which different variables in an infinite variety of combinations may combine to cause the disease in a given patient. For ease, only the major categories of co-factor are included.
Kenneth E Wical and Charles 1974 used Panoramic radiographs for evaluation and classification of mandibular resorption. By using this method edentulous patients could be classified according to their severity of the bone disease as : Class I : upto one third of the original vertical height lost. Class II: from one third to two thirds of the vertical height lost. Class III: two thirds or more of the mandibular height lost.
TREATMENT AND PREVENTION OF RRR
/////// • The best way to manage the problem of residual ridge reorption is by using every means to prevent it. • The introduction of dental implants has revoluitionized clinical practice. • Use of implants for providing implant supported or implant assisted prosthesis also helps avert continuing residual ridge resorption • Clinicians must try to retain residual roots whenever feasible • Overdentures help minimize ridge resorption and contribute to enhanced retention stability , support of prosthesis along with preservation of proprrioception.
• Mc Cord et al reviewed treatments for the edentulous mandible, in an attempt to present overview of prosthodontic options for patients. • These authors stressed the need for thorough diagnosis prior to the prescription of replacement dentures. • Many techniques or treatment strategies have been suggested in an attempt to provide functionally acceptable replacement prosthesis. • One such philosophy is the copy or template denture technique which duplicates the polished surface of the previous denture and thus facilitates patient’s neuromuscular adaptation to dentures
BASIS OF THE CLINICAL PROBLEM Clinical experience would indicate that the nature of the mucosa overlying the atrophic mandibular has a significant influence on the patient’s ability to withstand functional loading. In function the lower denture is forced through a bolus of food; this means that, in effect, the mucosa is ultimately sandwiched between the denture base and the mandibular bone. Overloading therefore results in discomfort and/or pain. Classically easing follows easing and a vicious cycle is established by relining the denture. The problem facing the prosthodontist in such cases is whether it is preferable to improve a current denture or to prescribe a new replacement denture
References: • Atwood D. A. Reduction of residual ridges: A major oral disease entity. J Prosthet Dent 1971; 26: 266 -279. • Atwood D. A. Some clinical factors related to resorption of residual ridge. J Prosthet Dent 1962; 12: 441 -450. • Jahangiri L. Current prospective in residual ridge remodelling and its clinical implications: A review. J Prosthet Dent 1998; 80: 224 -237. • Tallgren A. A continuing reduction of the residual alveolar ridges in complete denture wearer: A mixed-longitudinal study covering 25 years. J Prosthet Dent 1972; 27: 120 -132. • Winkler: Essentials of complete denture prosthodontics IInd edition. • Wyatt C. C. L. Effects of prosthodontic treatment on alveolar bone loss: A review of literature. J. Prosthet Dent. 1998; 80: 362 -366.
References: • Atwood D. A. Reduction of residual ridges: A major oral disease entity. J Prosthet • Mc Cord JF, Tysown KW. A conservative prosthodontic option for the treatment of edentulous patients with atrophic (flat)mandibular ridges. Brit Dent J 1997 ; 186(12): 469 -72 • Mc Cord JF, Tyson KW. Chairside Options for the treatment of complete denture problems associated with the atrophic mandibular ridge. Brit Dent J 2000; 188(1): 10 -14

Thankyou