RenalGU ITE Review Michelle Slezak Henry Ford Hospital










- Slides: 43

Renal/GU ITE Review Michelle Slezak Henry Ford Hospital Department of Emergency Medicine
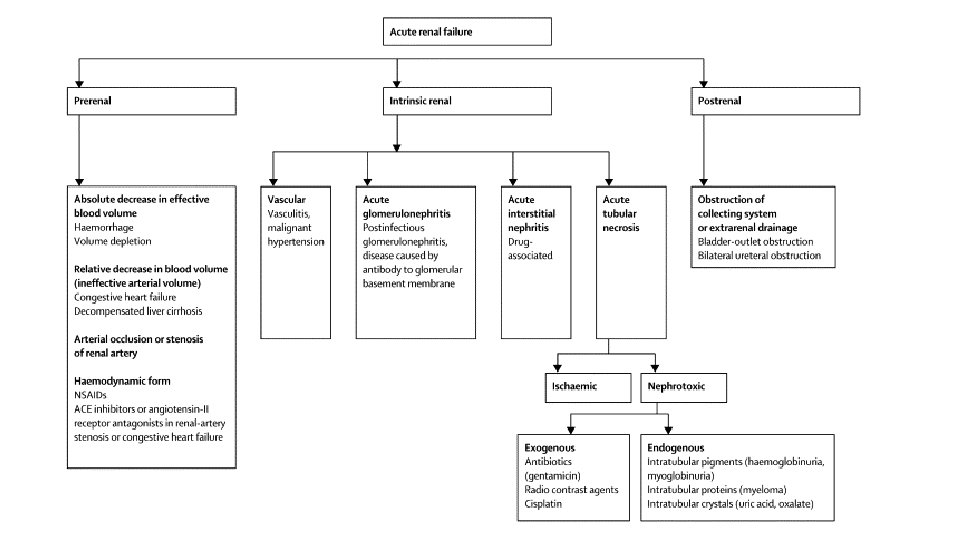
Renal Failure
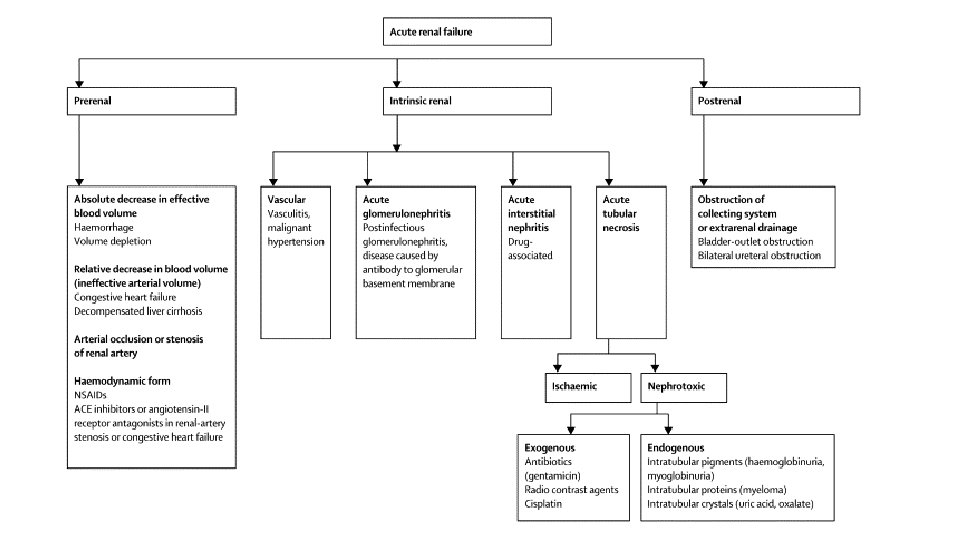


Prerenal azotemia • 60% of AKI • Patients are oliguric • Kidney retains resorptive function and ability to conserve sodium • Urine studies • • • Concentrated (SG >1. 020) Osmolality >500 FENa <1% Urine Na <20 m. Eq/L UA normal or occasional hyaline cast • BUN/Cr >20 • Causes • Hypovolemia (V/D, blood loss, diuretics, skin losses) • Decreased effective blood volume (sepsis, anaphylaxis, third spacing, hypoalbuminemic states, decreased cardiac output) • Treatment- correct hypoperfusion
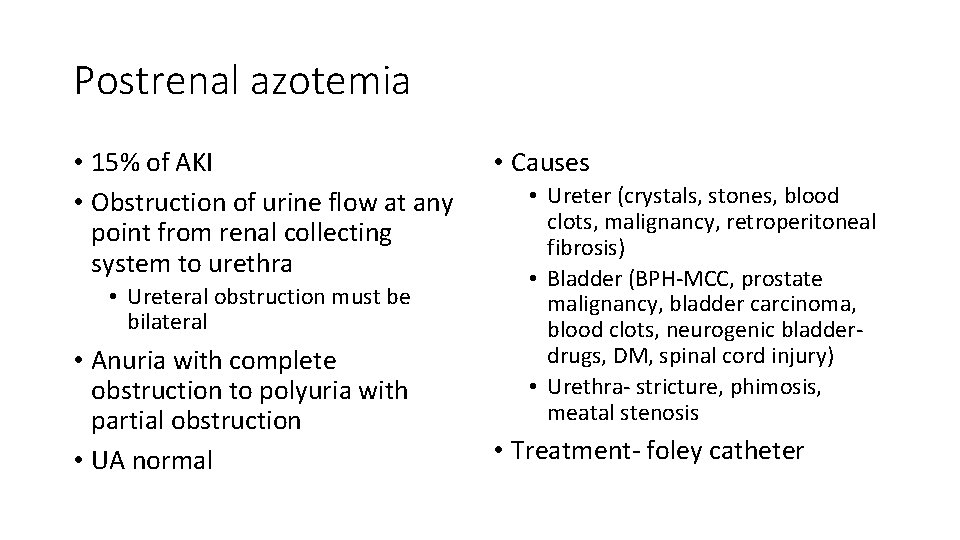
Postrenal azotemia • 15% of AKI • Obstruction of urine flow at any point from renal collecting system to urethra • Ureteral obstruction must be bilateral • Anuria with complete obstruction to polyuria with partial obstruction • UA normal • Causes • Ureter (crystals, stones, blood clots, malignancy, retroperitoneal fibrosis) • Bladder (BPH-MCC, prostate malignancy, bladder carcinoma, blood clots, neurogenic bladderdrugs, DM, spinal cord injury) • Urethra- stricture, phimosis, meatal stenosis • Treatment- foley catheter
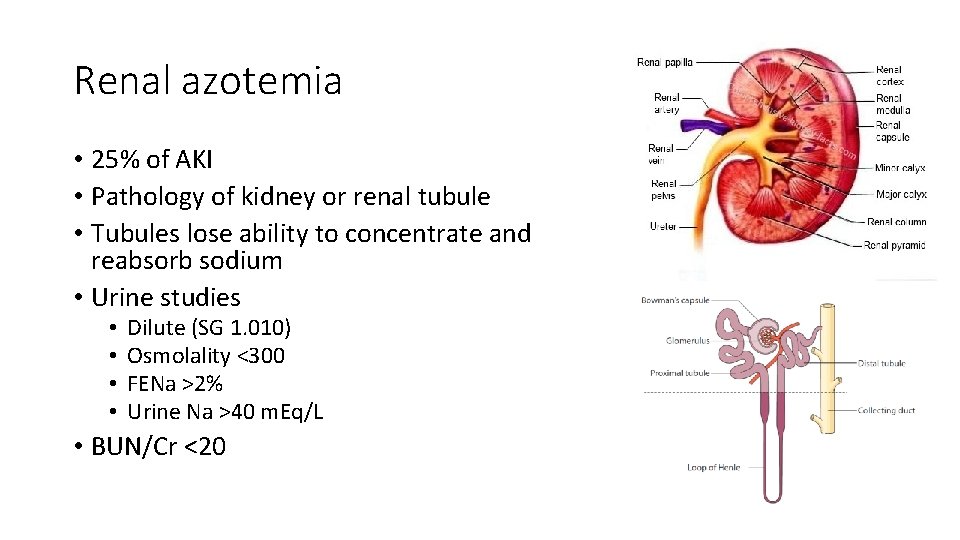
Renal azotemia • 25% of AKI • Pathology of kidney or renal tubule • Tubules lose ability to concentrate and reabsorb sodium • Urine studies • • Dilute (SG 1. 010) Osmolality <300 FENa >2% Urine Na >40 m. Eq/L • BUN/Cr <20
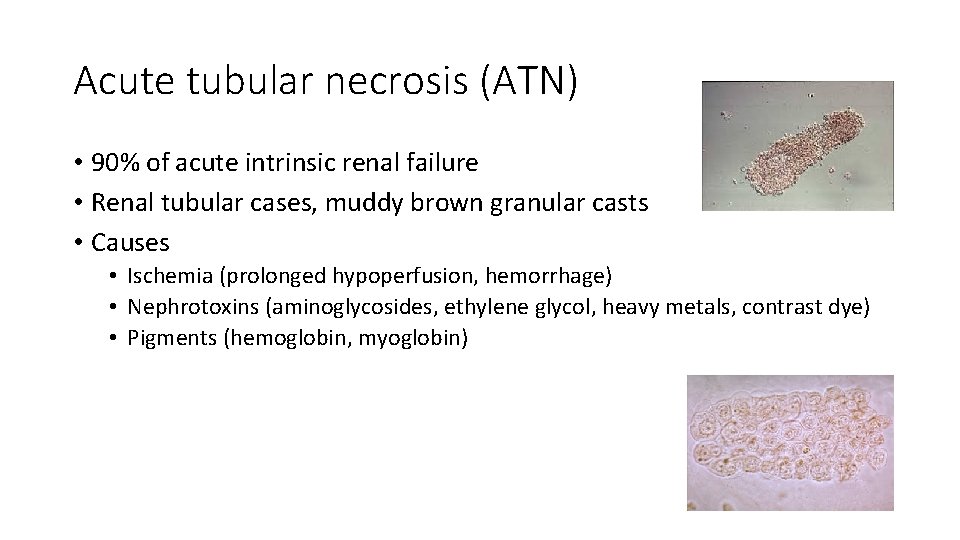
Acute tubular necrosis (ATN) • 90% of acute intrinsic renal failure • Renal tubular cases, muddy brown granular casts • Causes • Ischemia (prolonged hypoperfusion, hemorrhage) • Nephrotoxins (aminoglycosides, ethylene glycol, heavy metals, contrast dye) • Pigments (hemoglobin, myoglobin)
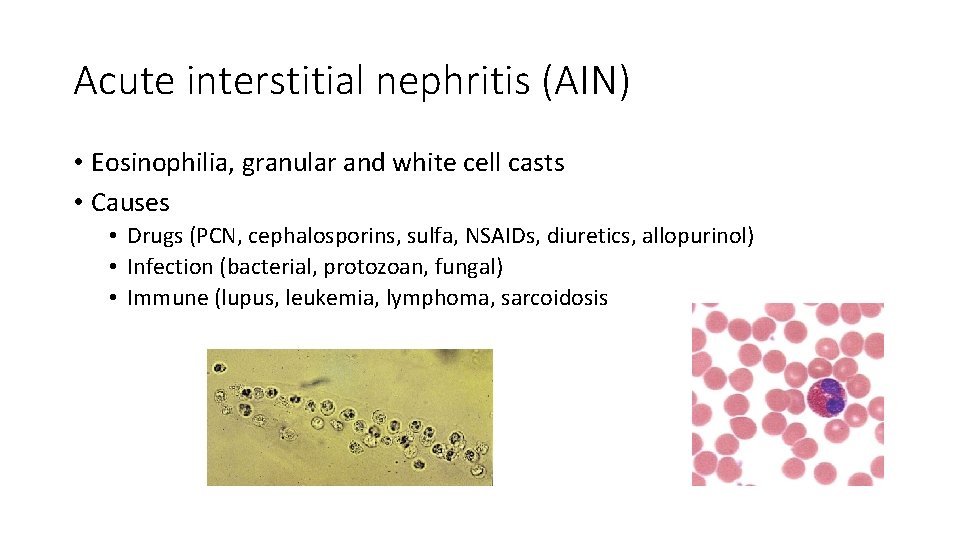
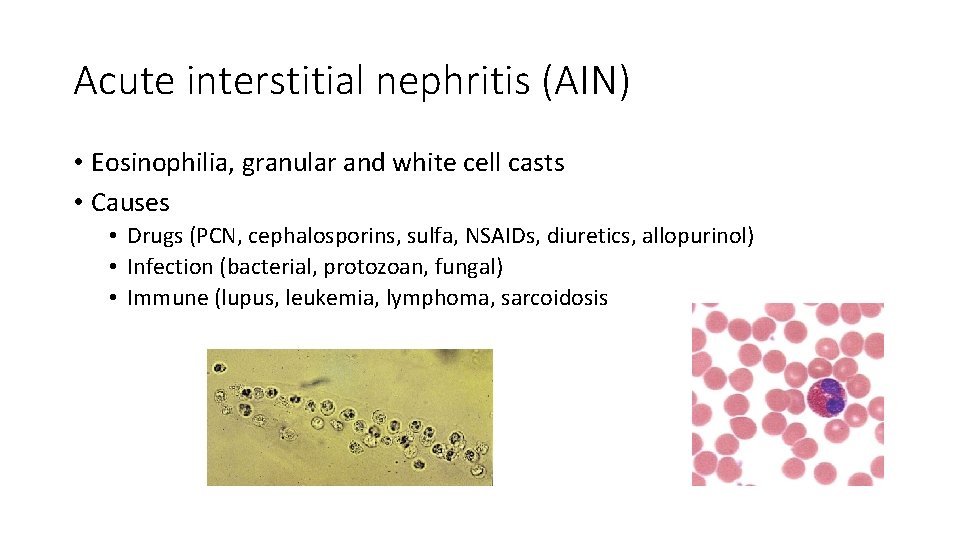
Acute interstitial nephritis (AIN) • Eosinophilia, granular and white cell casts • Causes • Drugs (PCN, cephalosporins, sulfa, NSAIDs, diuretics, allopurinol) • Infection (bacterial, protozoan, fungal) • Immune (lupus, leukemia, lymphoma, sarcoidosis
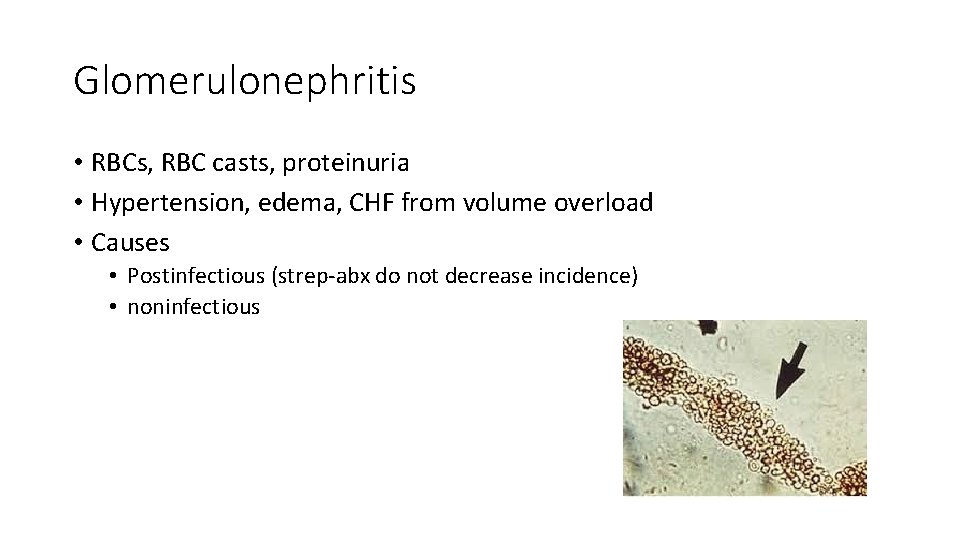
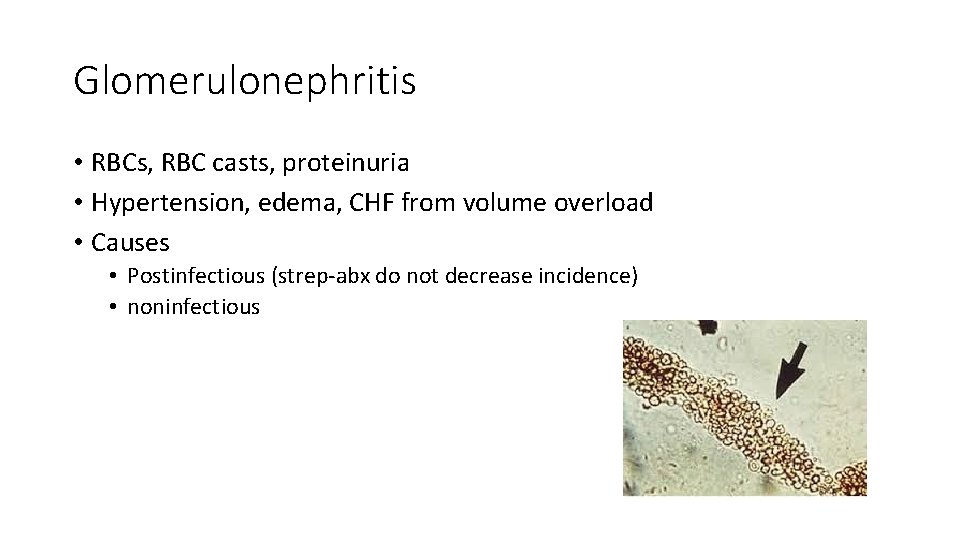
Glomerulonephritis • RBCs, RBC casts, proteinuria • Hypertension, edema, CHF from volume overload • Causes • Postinfectious (strep-abx do not decrease incidence) • noninfectious
Other intrinsic AKI • Vascular • Vasoconstrictive disease (malignant hypertension, TTP) • Vasculitis • Thrombosis • Renal artery/renal vein • Treatment for all renal AKI • Remove offending agent • Treat any underlying cause
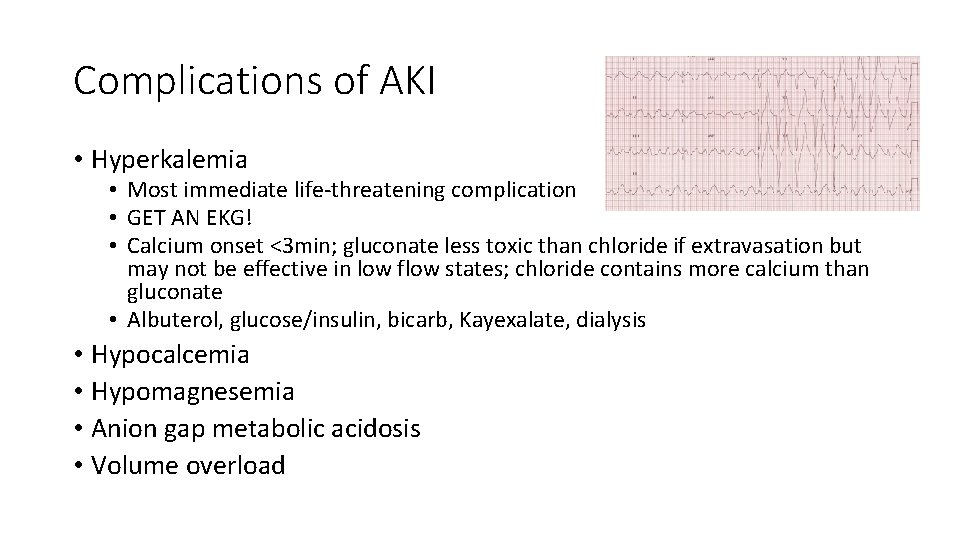
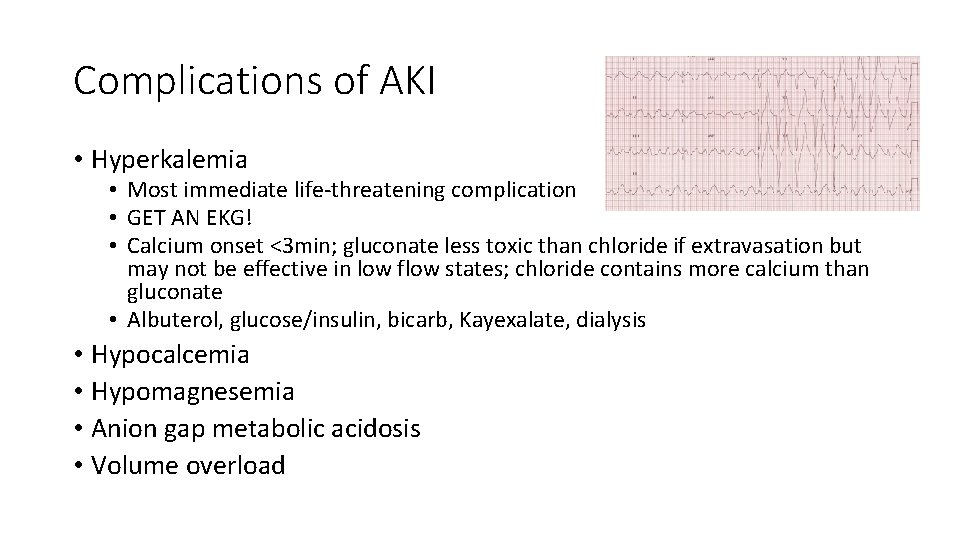
Complications of AKI • Hyperkalemia • Most immediate life-threatening complication • GET AN EKG! • Calcium onset <3 min; gluconate less toxic than chloride if extravasation but may not be effective in low flow states; chloride contains more calcium than gluconate • Albuterol, glucose/insulin, bicarb, Kayexalate, dialysis • Hypocalcemia • Hypomagnesemia • Anion gap metabolic acidosis • Volume overload
Indications for dialysis (AEIOU) • A: acidosis • E: electrolyte abnormalities (resistant hyper. K) • I: ingestion of toxic dialyzable substance (lithium, methanol, ethylene glycol) • O: overload of fluid • U: uremia (pericarditis, encephalopathy, bleeding)
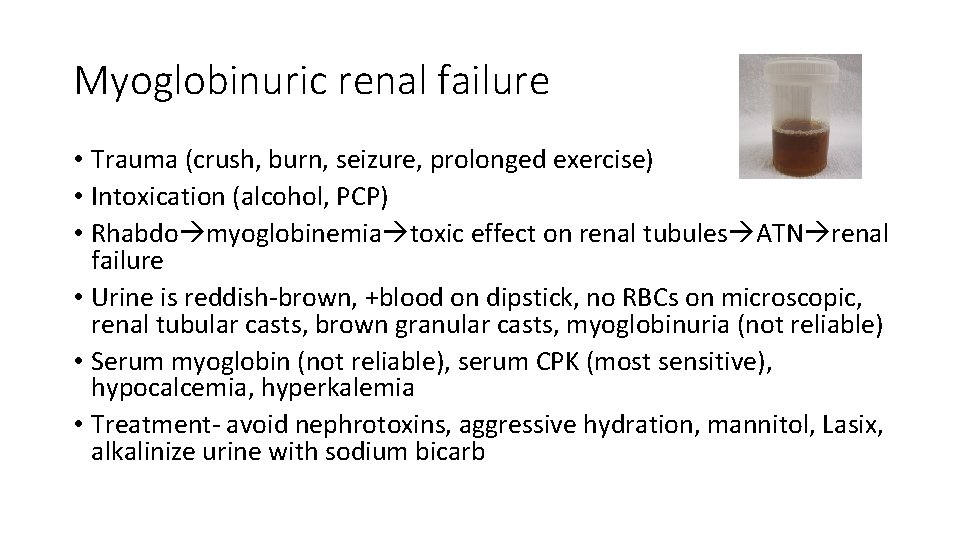
Myoglobinuric renal failure • Trauma (crush, burn, seizure, prolonged exercise) • Intoxication (alcohol, PCP) • Rhabdo myoglobinemia toxic effect on renal tubules ATN renal failure • Urine is reddish-brown, +blood on dipstick, no RBCs on microscopic, renal tubular casts, brown granular casts, myoglobinuria (not reliable) • Serum myoglobin (not reliable), serum CPK (most sensitive), hypocalcemia, hyperkalemia • Treatment- avoid nephrotoxins, aggressive hydration, mannitol, Lasix, alkalinize urine with sodium bicarb
Other renal failure • Nephrotic syndrome • High urine protein excretion, peripheral edema, metabolic abnormalities (hypoalbuminemia, hypercholesterolemia) • Minimal change disease • Kids; may be preceded by URI or immunization; responds to steroids • Focal segmental glomerulosclerosis (FSGS) • African Americans, sickle cell, IVDU, htn, DM; higher frequency of renal failure • Tx- steroids, immunosuppressants • Membranous nephropathy • • Caucasians (30 -50%); HBV, HCV, syphilia, malaria, gold, penicillamind 24% assoc w/ neoplasm Proteinuria, occasional microhematuria, hypercoagulopathy (renal vein thrombosis) Spontaneous remission in 25%

Other renal failure • Membranoproliferative glomerulonephritis (MPGN) • Can present with nephrotic or nephritic features • Assoc w/ infection, autoimmune disease, HCV, cryoglobulins, low C 3 • 50% mortality or progression to ESRD w/in 5 yrs of diagnosis • Diabetic nephropathy • Leading cause of ESRD in US • Onset 5 -10 yrs after onset of type I DM • Tx- TGCP, ACEI • Others • Malignancy (lymphoma, myeloma) • Infection (HIV, HBV, HCV, syphilis, leprosy, malaria) • SLE, amyloidosis, sickle cell, preeclampsia
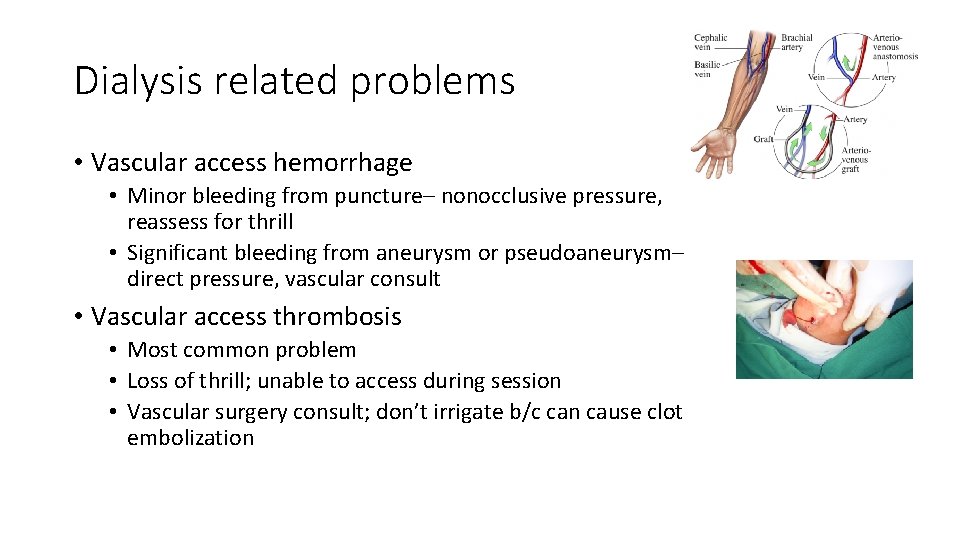
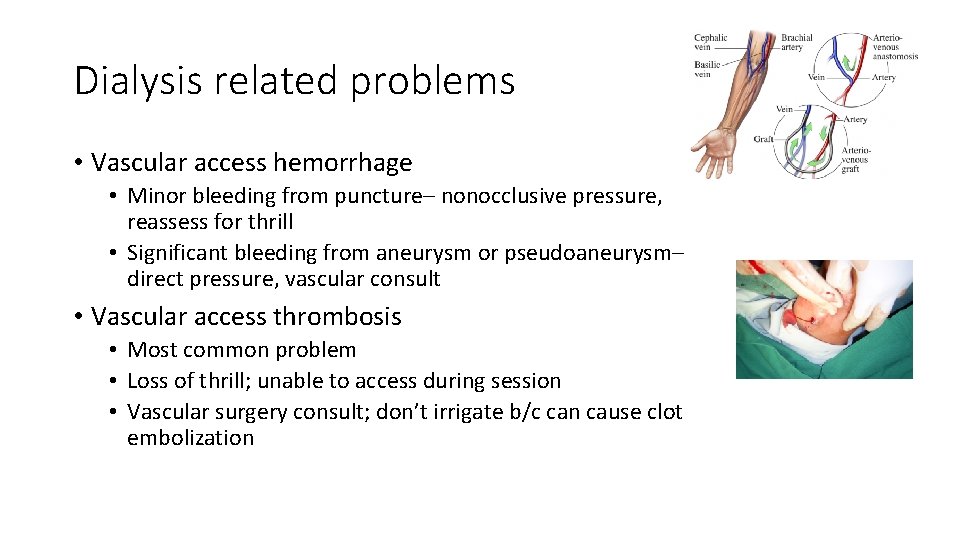
Dialysis related problems • Vascular access hemorrhage • Minor bleeding from puncture– nonocclusive pressure, reassess for thrill • Significant bleeding from aneurysm or pseudoaneurysm– direct pressure, vascular consult • Vascular access thrombosis • Most common problem • Loss of thrill; unable to access during session • Vascular surgery consult; don’t irrigate b/c can cause clot embolization
Dialysis related problems • Vascular access infection • Often staph; more common in artificial than native grafts • Signs of infection (redness, warmth, induration) may be absent; may only have fever • Treatment– blood cultures, antibiotics (Vanco); may not require device removal • Peritoneal dialysis • Peritonitis– cloudy dialysate effluent • Abdominal pain, fever • Fluid WBC >100 with >50% PMNs or positive Gram stain

Dialysis related problems • Disequilibrium syndrome • • Rapid solute shifts during hemodialysis Most often during first session Headache, nausea, malaise, disorientation, confusion, seizure, coma, death Treatment is supportive; r/o other causes of AMS • Cardiac arrest • Beware of hyperkalemia and acute pericardial tamponade
Urinary Tract Problems
Urinary tract infections • Cystitis • Dysuria, urgency, frequency, hematuria, suprapubic discomfort, significant bacteriuria • Causes– SEEK PP • Staph saprophyticus (2 nd), E coli (1 st), Enterobacter, Klebsiella, Proteus, Pseudomonas • Uncomplicated UTI • Most UTIs; nonpregnant, healthy women with no neurologic or structural dysfunction • Treatment– 3 -6 days (Bactrim, quinolone, nitrofurantoin)
Urinary tract infections • Complicated UTI • Associated with any neurologic, structural, or comorbid condition that increases risk for acquiring infection and reduced efficacy of standard tx regimens • Predispose • Structural (calculi, catheters, stents, prostatic infection, urinary diversion procedures) • Metabolic or hormonal (diabetes, pregnancy) • Vesicoureteral reflux, immunocompromised, recent urinary tract instrumentation, male gender, extremes of age, unusual pathogens, recent antibiotic use of failed treatment for UTI, symptoms longer than 7 days • Treatment– 7 -10 days
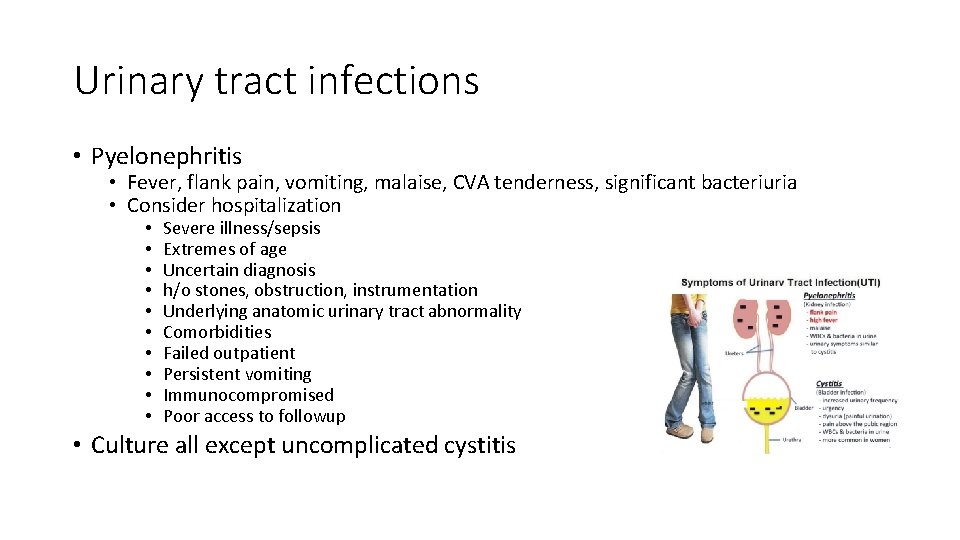
Urinary tract infections • Pyelonephritis • Fever, flank pain, vomiting, malaise, CVA tenderness, significant bacteriuria • Consider hospitalization • • • Severe illness/sepsis Extremes of age Uncertain diagnosis h/o stones, obstruction, instrumentation Underlying anatomic urinary tract abnormality Comorbidities Failed outpatient Persistent vomiting Immunocompromised Poor access to followup • Culture all except uncomplicated cystitis

Nephrolithiasis • Composition • 80% contain calcium (2/3 calcium oxalate, 1/3 calcium phosphate) • Dehydration, hyperoxaluria, hypercalciuria (hyperthyroidism, hyperparathyroidism, neoplasm, sarcoidosis, multiple myeloma, distal RTA), PUD (ingest large amts of calcium) • 15% struvite (magnesium-ammonium-phosphate) • Caused by chronic UTI from urea-splitting organisms (Proteus) • 6 -10% uric acid • Gout, myeloproliferative disease, leukemia, high protein diet • 1 -3% cysteine • familial
Nephrolithiasis • Presentation • • • Unilateral colicky pain in flank, back, lower quadrant Radiation to groin, labia, testicles Dysuria, frequency, hematuria Nausea, vomiting Severe discomfort, diaphoresis, restlessness • Beware of AAA, iliac aneurysms, renal vein thrombosis • Diagnosis • • • Only 80% have hematuria 90% seen on KUB; can be used to follow progression/passage CT is test of choice IVP can show delayed nephrogram, hydronephrosis, hydroureter, extravasation US in pregnant and kids Image– first episode, unclear diagnosis, coexistent UTI, elderly
Nephrolithiasis • Most common sites of stone impaction • ureteropelvic junction, pelvic brim (where ureter crosses iliac vessels), ureterovesical junction (most narrow point in ureter) • Likelihood of spontaneous passage • <5 mm pass 90%; 5 -8 mm pass 15%; >8 mm pass 5% • Coexistent UTI is an emergency!! • NSAIDs and narcotics act synergistically • Admit • High-grade obstruction, intractable pain/vomiting, associated UTI, solitary or transplanted kidney, unclear diagnosis, extravasation of dye, renal failure, stone >5 mm (relative)

Bladder calculi • Elderly men • Complication of other urologic disease • Urinary stasis • Infection of residual bladder urine with urea-splitting organisms • Pain on voiding, hematuria, sudden interruption of urinary stream
Hematuria • • • Trauma: bladder injury, ureter injury, retroperitoneal injury Anemia, thrombocytopenia, renal insufficiency: HUS Flank pain: nephrolithiasis Urine + for heme and – for RBCs: rhabdomyolysis Dysuria, frequency: UTI Hearing loss: Alport syndrome Hemoptysis: Goodpasture syndrome Immigrant: Schistosomiasis Nephrotic syndrome, flank pain: renal vein thrombosis Proteinuria, RBC casts: glomerulonephritis Recent URI: glomerulonephritis, Ig. A nephropathy Gross hematuria: imaging is recommended for age >40
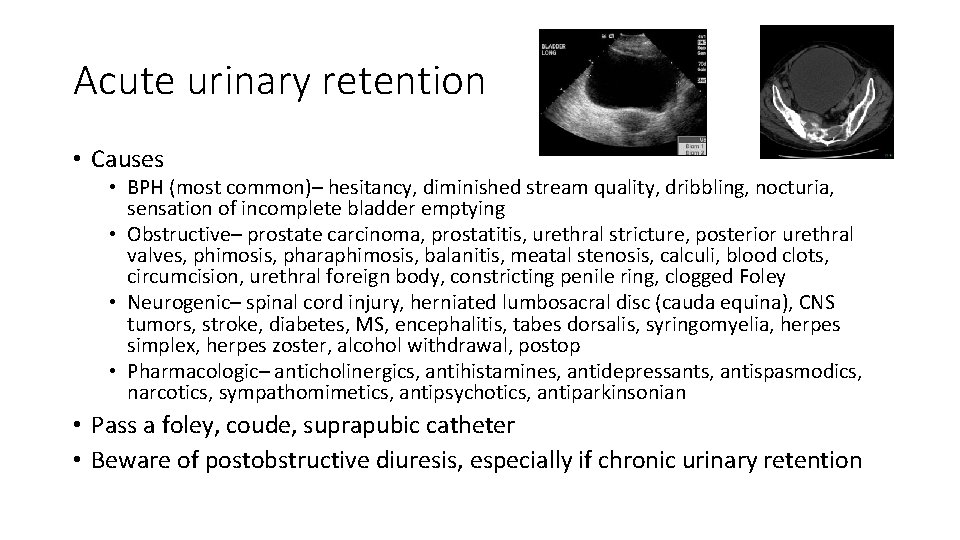
Acute urinary retention • Causes • BPH (most common)– hesitancy, diminished stream quality, dribbling, nocturia, sensation of incomplete bladder emptying • Obstructive– prostate carcinoma, prostatitis, urethral stricture, posterior urethral valves, phimosis, pharaphimosis, balanitis, meatal stenosis, calculi, blood clots, circumcision, urethral foreign body, constricting penile ring, clogged Foley • Neurogenic– spinal cord injury, herniated lumbosacral disc (cauda equina), CNS tumors, stroke, diabetes, MS, encephalitis, tabes dorsalis, syringomyelia, herpes simplex, herpes zoster, alcohol withdrawal, postop • Pharmacologic– anticholinergics, antihistamines, antidepressants, antispasmodics, narcotics, sympathomimetics, antipsychotics, antiparkinsonian • Pass a foley, coude, suprapubic catheter • Beware of postobstructive diuresis, especially if chronic urinary retention
Male GU Disorders

Orchitis • Usually direct extension of epididymitis • Viral orchitis caused by mumps • Symptoms evolve several days after onset of parotitis • Testicular pain and swelling
Acute bacterial prostatitis • Frequency, urgency, dysuria, obstructive voiding sx, perineal discomfort, fever, myalgias, malaise, low back or rectal pain • Usually Gram negatives (80% E coli) • Tender, swollen prostate is warm and firm • Do not massage the prostate b/c can precipitate bacteremia • Treatment with quinolone or Bactrim for 30 days • If urinary drainage needed, suprapubic catheter (not foley)
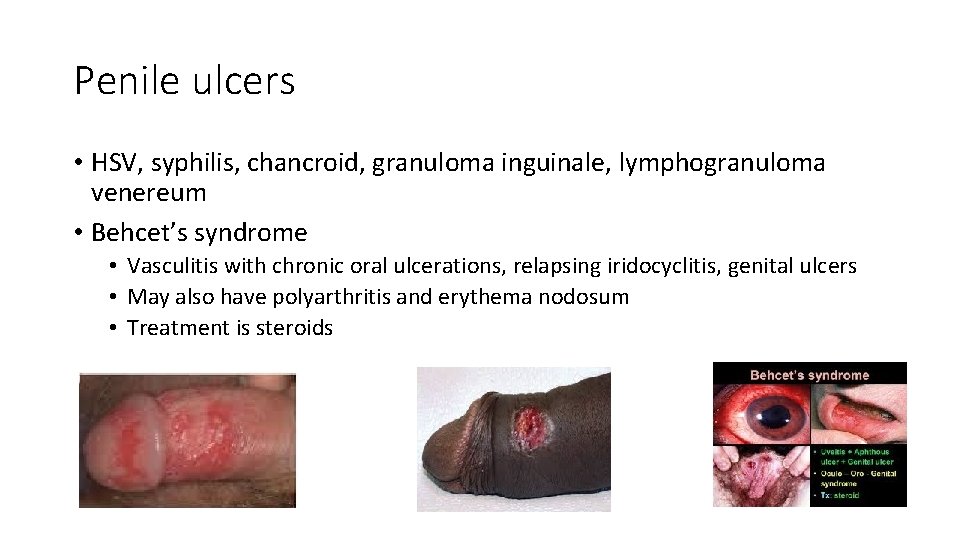
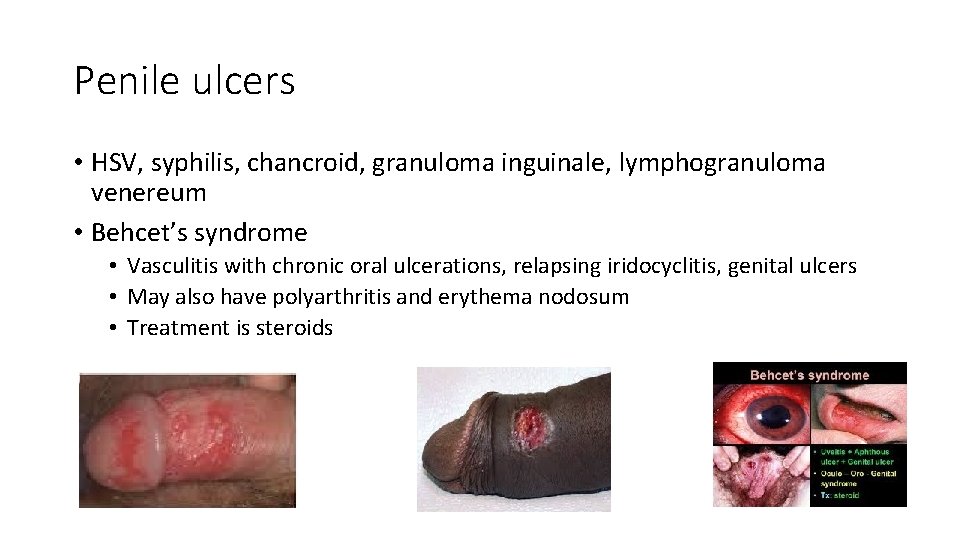
Penile ulcers • HSV, syphilis, chancroid, granuloma inguinale, lymphogranuloma venereum • Behcet’s syndrome • Vasculitis with chronic oral ulcerations, relapsing iridocyclitis, genital ulcers • May also have polyarthritis and erythema nodosum • Treatment is steroids

Fournier’s gangrene • Necrotizing infection of subq tissue of perineum • Bacteroides fragilis, E coli • Acute onset, toxic • Painful, erythematous, edematous scrotum, +/crepitus/gangrene • Risk– diabetes, chronic steroids, alcoholic, local trauma • Treatment– Abx, urology consult, debridement, hyperbaric oxygen
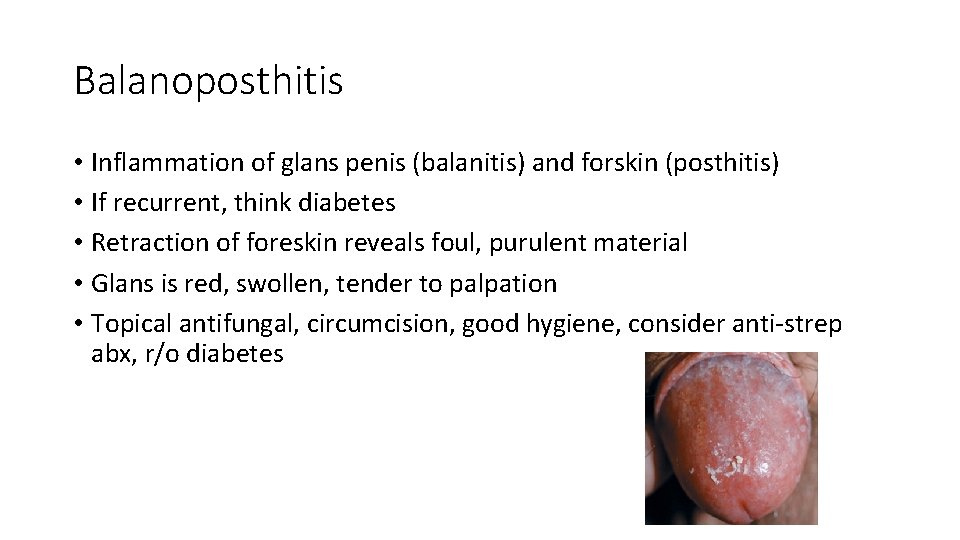
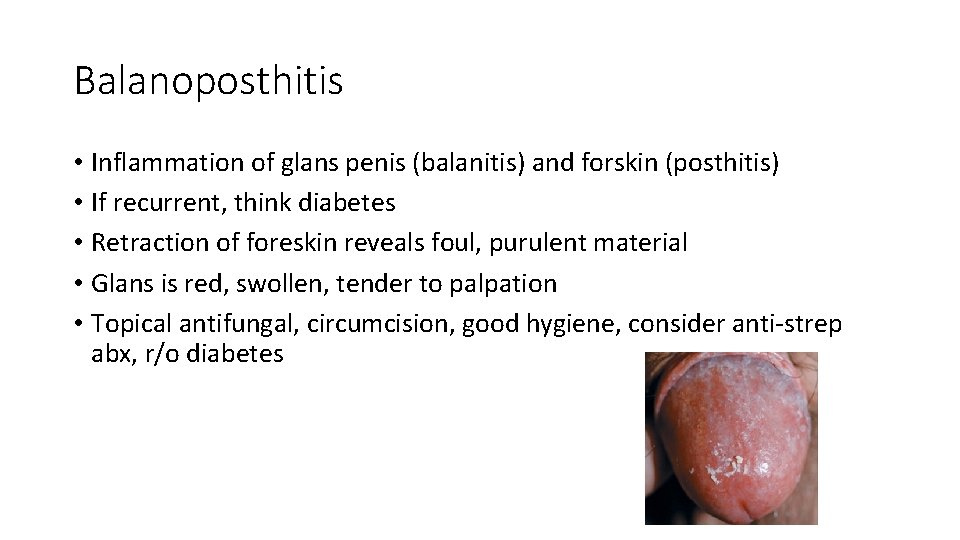
Balanoposthitis • Inflammation of glans penis (balanitis) and forskin (posthitis) • If recurrent, think diabetes • Retraction of foreskin reveals foul, purulent material • Glans is red, swollen, tender to palpation • Topical antifungal, circumcision, good hygiene, consider anti-strep abx, r/o diabetes
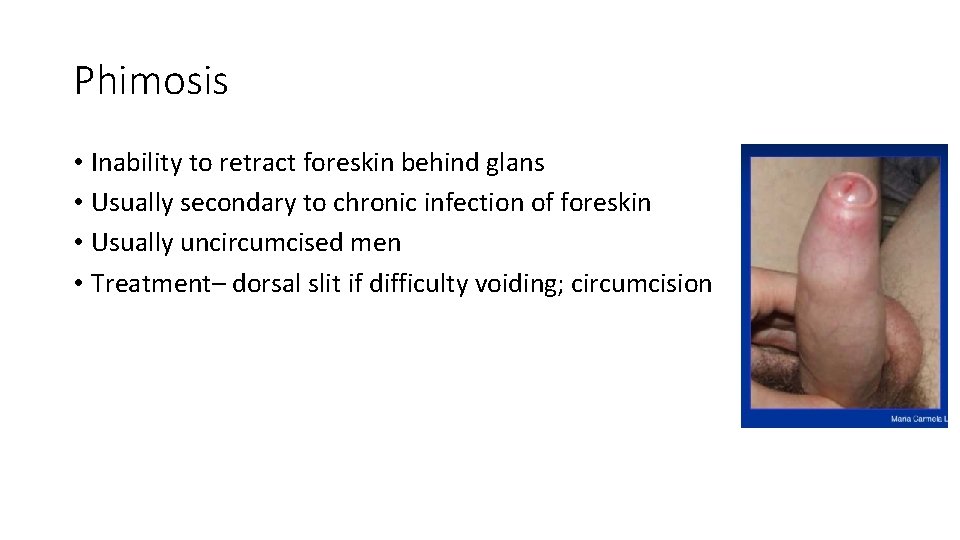
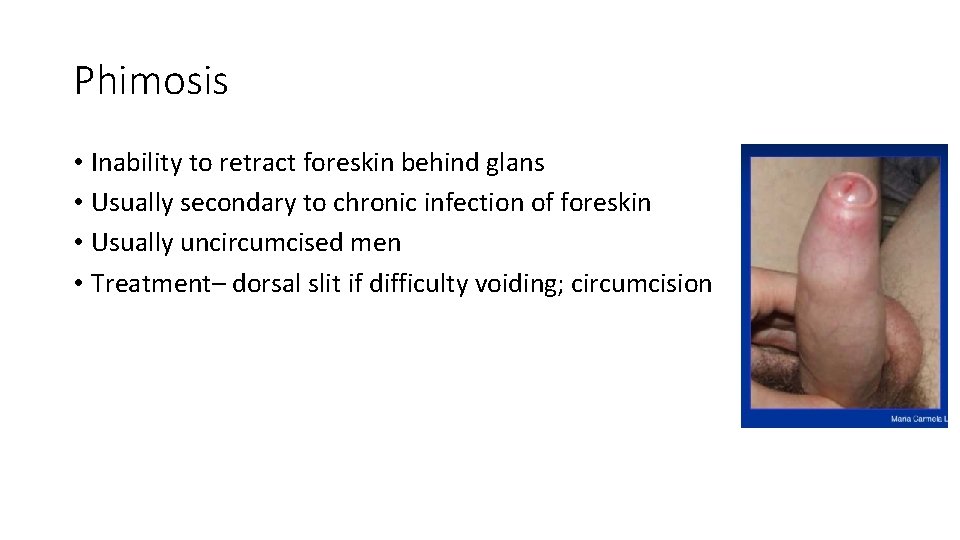
Phimosis • Inability to retract foreskin behind glans • Usually secondary to chronic infection of foreskin • Usually uncircumcised men • Treatment– dorsal slit if difficulty voiding; circumcision
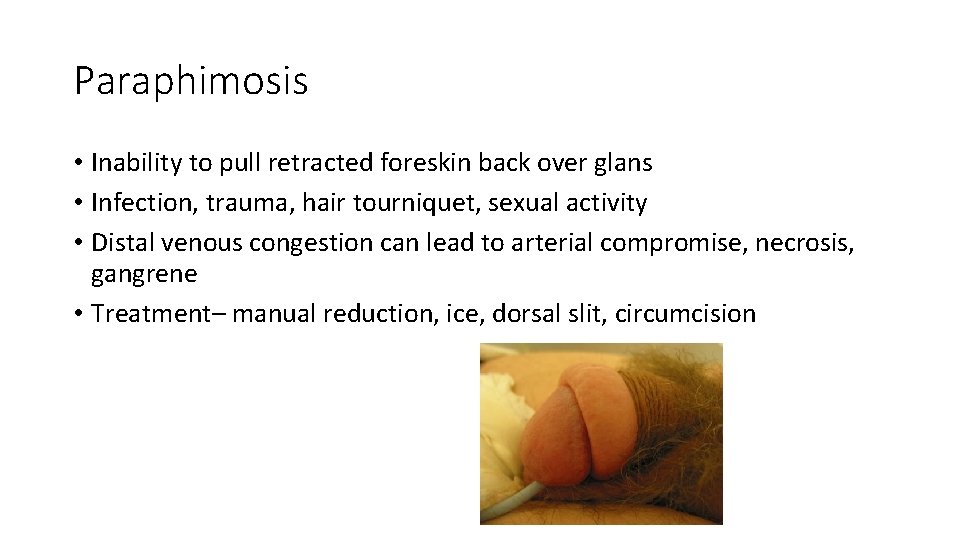
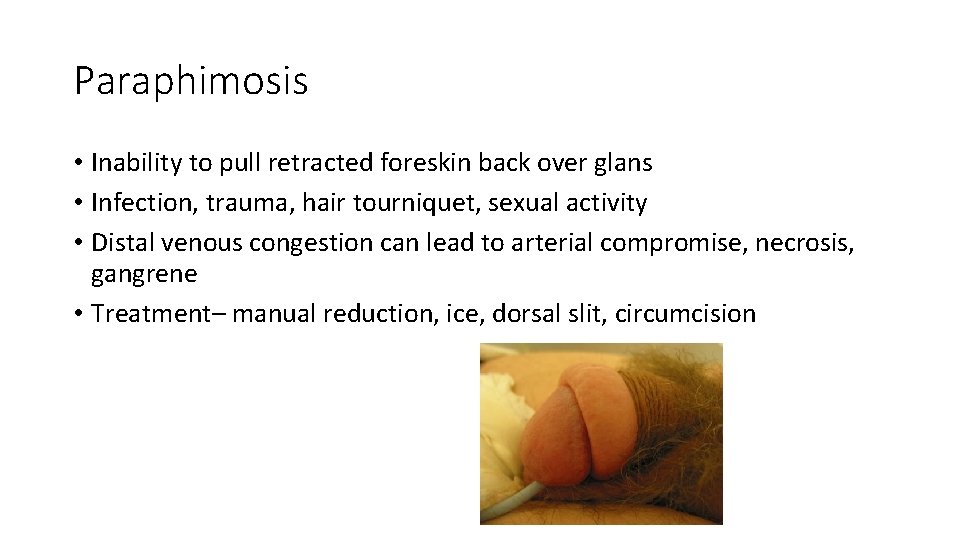
Paraphimosis • Inability to pull retracted foreskin back over glans • Infection, trauma, hair tourniquet, sexual activity • Distal venous congestion can lead to arterial compromise, necrosis, gangrene • Treatment– manual reduction, ice, dorsal slit, circumcision

Penile fracture • Tear of tunica albuginea (usually during erection) • Retrograde urethrogram to r/o urethral injury
Priapism • Low-flow • Decreased venous outflow venous stasis, ischemia of corpus cavernosae but spares glans and corpus spongiosum rigid, painful penile shaft and soft glans • Causes– sickles cell, leukemia, intracavernosal injections of ED, trazodone, marijuana, idiopathic • High-flow • Rare; not a true emergency • Increased arterial blood flow to corpus cavernosae increased venous blood flow partially rigid, painless penile shaft and hard glans • Causes– groin/straddle injury (arterial-cavernosal shunt), high spinal cord injury/lesion • Terbutaline subq, analgesia, pseudoephedrine injection, corporeal aspiration, shunt surgery
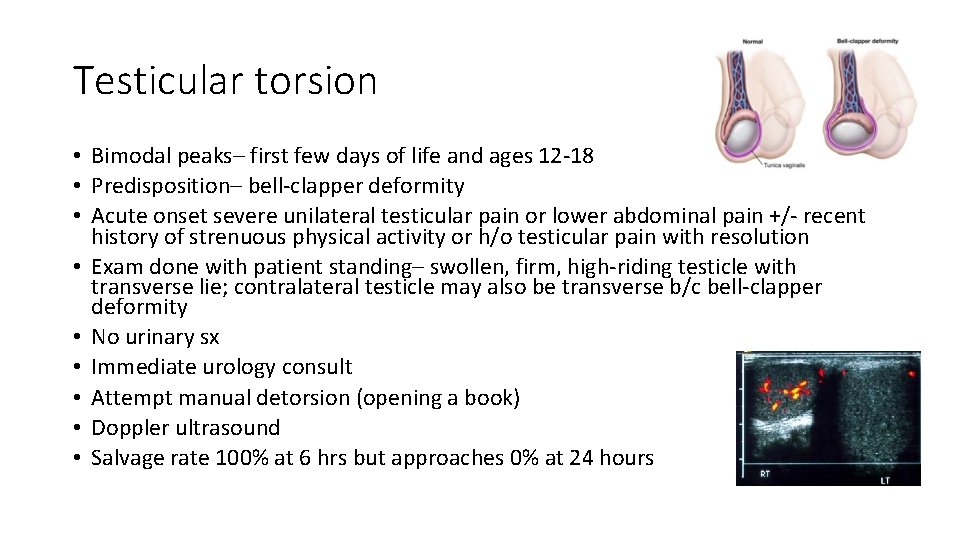
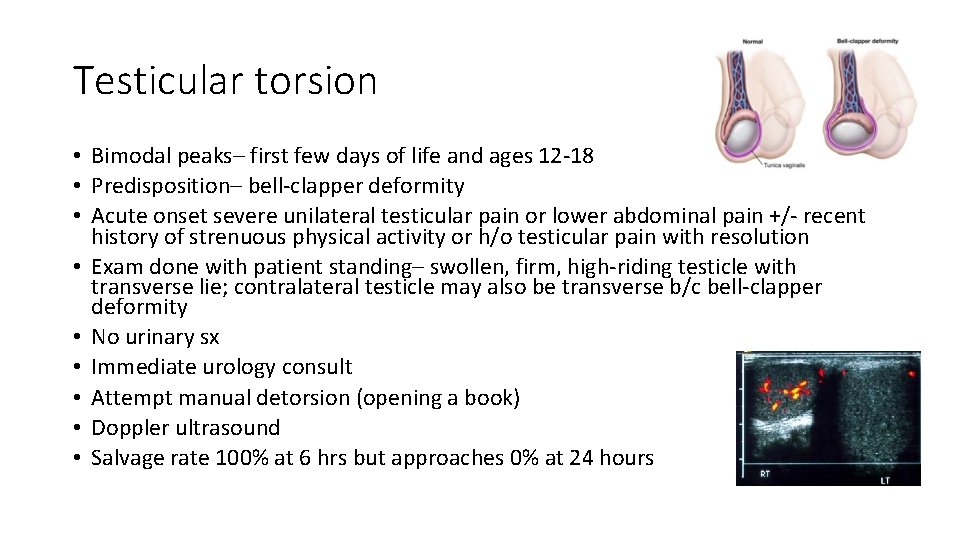
Testicular torsion • Bimodal peaks– first few days of life and ages 12 -18 • Predisposition– bell-clapper deformity • Acute onset severe unilateral testicular pain or lower abdominal pain +/- recent history of strenuous physical activity or h/o testicular pain with resolution • Exam done with patient standing– swollen, firm, high-riding testicle with transverse lie; contralateral testicle may also be transverse b/c bell-clapper deformity • No urinary sx • Immediate urology consult • Attempt manual detorsion (opening a book) • Doppler ultrasound • Salvage rate 100% at 6 hrs but approaches 0% at 24 hours
Torsion of appendices epididymis and testis • Unilateral pain, more gradual in onset, not as severe, localized to involved appendix early; late, generalized scrotal swelling and tenderness • Blue dot sign– visualization of necrotic appendix testis through scrotal wall on superior aspect of testicle on transillumination • Self-resolving, benign process • Rest, scrotal elevation, analgesia
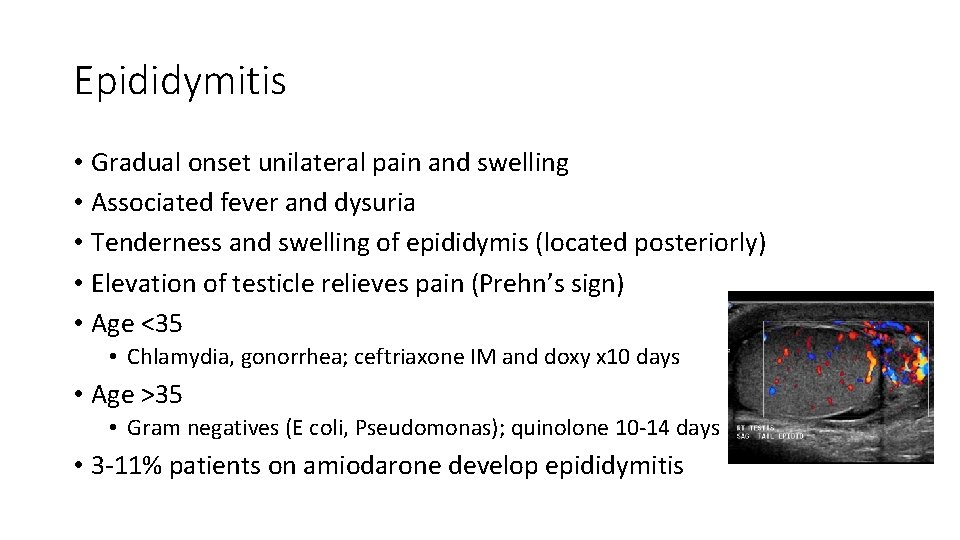
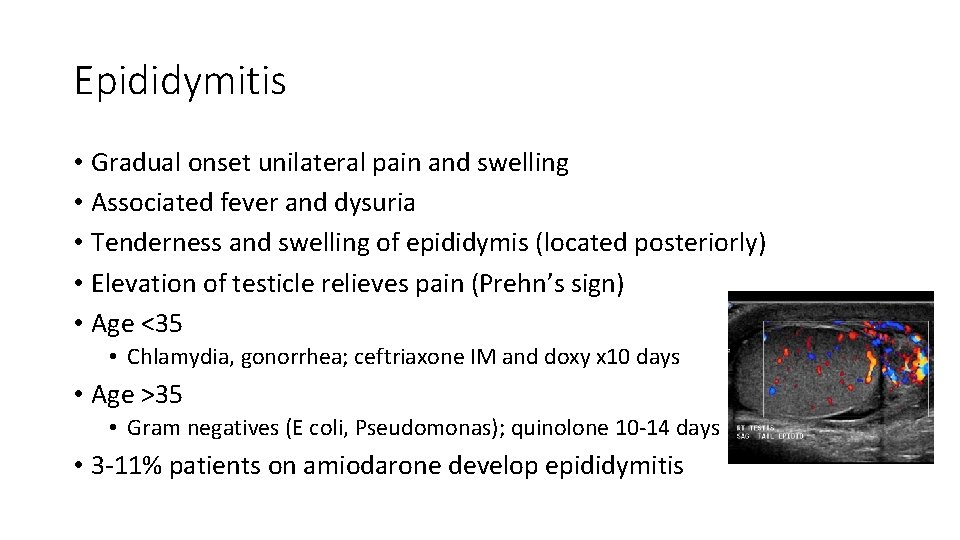
Epididymitis • Gradual onset unilateral pain and swelling • Associated fever and dysuria • Tenderness and swelling of epididymis (located posteriorly) • Elevation of testicle relieves pain (Prehn’s sign) • Age <35 • Chlamydia, gonorrhea; ceftriaxone IM and doxy x 10 days • Age >35 • Gram negatives (E coli, Pseudomonas); quinolone 10 -14 days • 3 -11% patients on amiodarone develop epididymitis
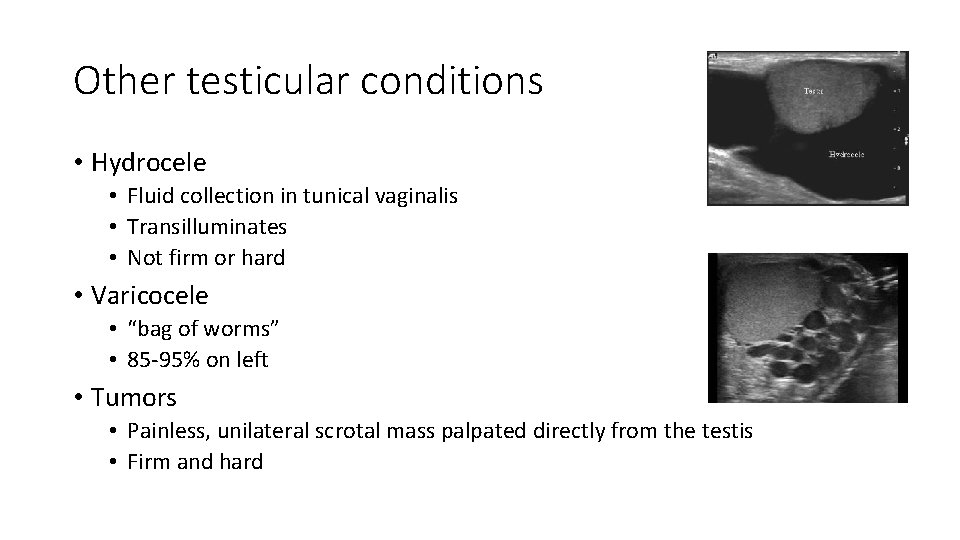
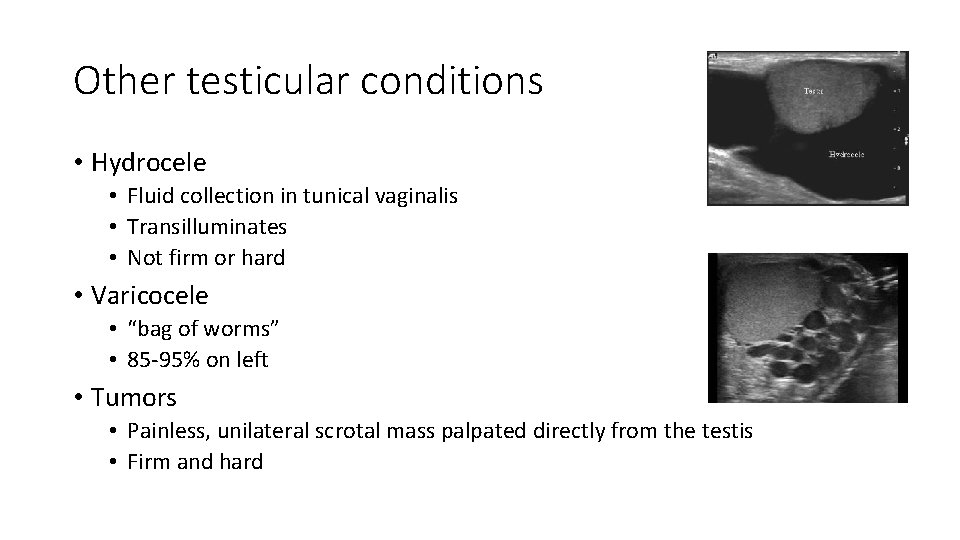
Other testicular conditions • Hydrocele • Fluid collection in tunical vaginalis • Transilluminates • Not firm or hard • Varicocele • “bag of worms” • 85 -95% on left • Tumors • Painless, unilateral scrotal mass palpated directly from the testis • Firm and hard
 Aeiou dialisis
Aeiou dialisis Mendez rojas class chart
Mendez rojas class chart Henry ford 14 principles of management
Henry ford 14 principles of management Henry ford paternalistic leadership
Henry ford paternalistic leadership Henry ford famous inventions
Henry ford famous inventions Henry fords life
Henry fords life How did henry ford treat his workers
How did henry ford treat his workers Missed call from nnn
Missed call from nnn Henry ford teoria
Henry ford teoria Henry ford family guy
Henry ford family guy Henry ford early college application
Henry ford early college application Batova sustava riadenia
Batova sustava riadenia Henry ford last words
Henry ford last words Henry ford linha de montagem
Henry ford linha de montagem Which innovation helped henry ford realize his vision?
Which innovation helped henry ford realize his vision? Praise points ite
Praise points ite Iron 11 phosphate formula
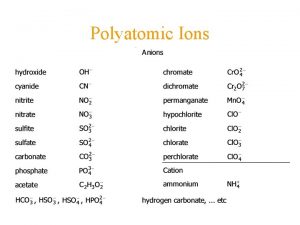
Iron 11 phosphate formula Ate ite ide chart
Ate ite ide chart Dr janalynn beste
Dr janalynn beste It essentials chapter 14
It essentials chapter 14 Ate ite ide chart
Ate ite ide chart Ite programme
Ite programme Ite osi
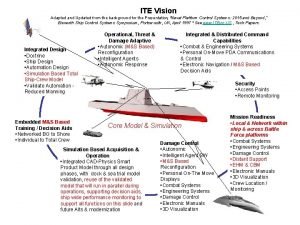
Ite osi Ite vision
Ite vision Ite bully
Ite bully Ite ceccano
Ite ceccano Types of network communication
Types of network communication 100 bedded hospital staff requirements
100 bedded hospital staff requirements Chapter review motion part a vocabulary review answer key
Chapter review motion part a vocabulary review answer key Ap gov review final exam review
Ap gov review final exam review Narrative review vs systematic review
Narrative review vs systematic review Traditional and systematic review venn diagram
Traditional and systematic review venn diagram Narrative review vs systematic review
Narrative review vs systematic review Double interview social thinking
Double interview social thinking Apologive
Apologive Michelle rohl
Michelle rohl Michelle taylor xxx
Michelle taylor xxx Michelle keiper
Michelle keiper Dr michelle reid husband
Dr michelle reid husband Tom tassie car dealership ohio
Tom tassie car dealership ohio Michelle wilkins dr phil
Michelle wilkins dr phil Michelle de abreu
Michelle de abreu Chop onboarding portal
Chop onboarding portal Zev sunleaf
Zev sunleaf