PERIODONTAL MEDICINE Oral Disease and Systemic Disorders Infectious





- Slides: 54
PERIODONTAL MEDICINE
Oral Disease and Systemic Disorders Infectious diseases can cause inflammatory changes at distance body sites. Hippocrates “Focal Infection Theory” in the 1920’s 1940’s.
Oral Disease and Systemic Disorders (contd, ) • The oral cavity is a portal of entry as well as the site of disease for microbial infections that affect general health status. Surgeon General’s Report on Oral Health in America, 2000 • The mouth can become a source of disease or pathological processes affecting other parts of the body…… Surgeon General’s Call to Action to Promote Oral Health, 2003
Initiation and Progression of Periodontitis is a gum infection, initiated by specific bacteria that activate a series of inflammatory and immunologic changes leading to destruction of connective tissue and bone, and possible loss of . teeth
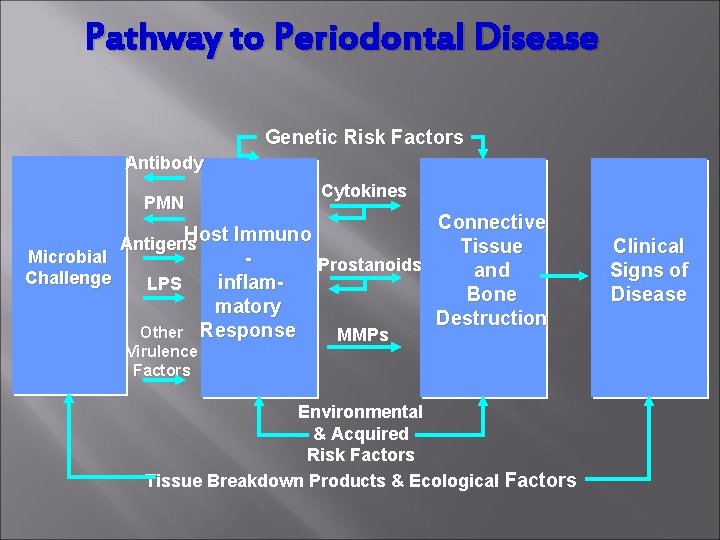
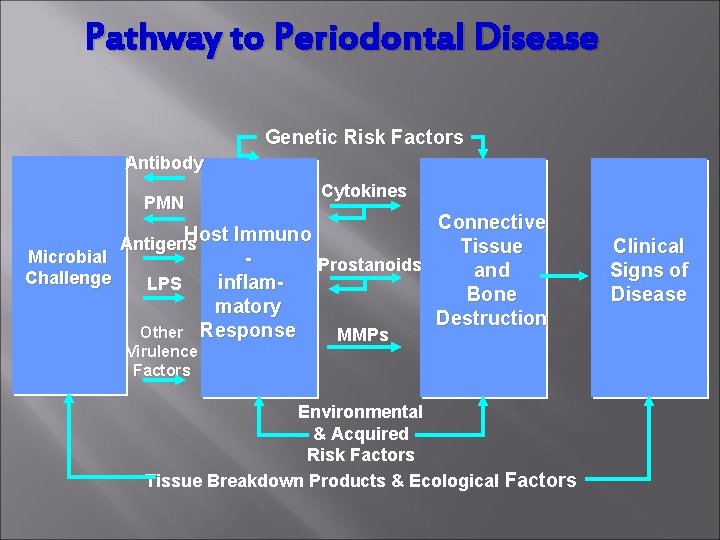
Pathway to Periodontal Disease Genetic Risk Factors Antibody PMN Cytokines Connective Host Immuno Antigens Tissue Microbial Prostanoids and Challenge inflam. LPS Bone matory Destruction Other Response MMPs Virulence Factors Environmental & Acquired Risk Factors Tissue Breakdown Products & Ecological Factors Clinical Signs of Disease

Progression of Periodontal Disease Risk Factors Rate of Progression Severity of Disease

Moderate to severe Periodontitis

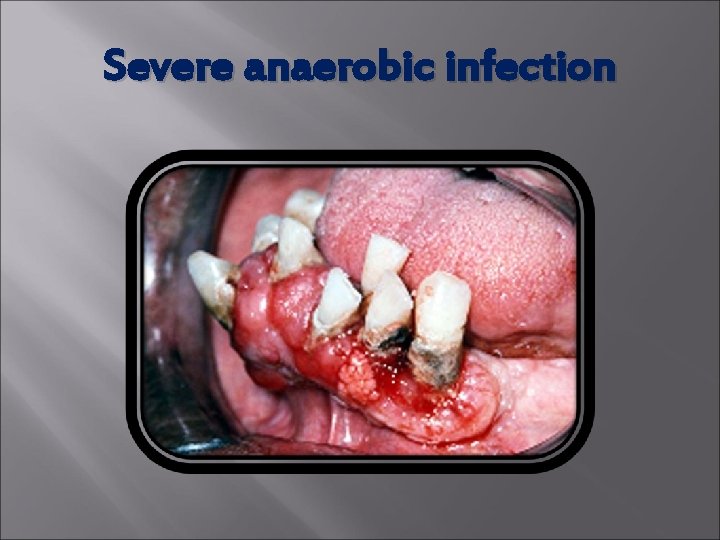
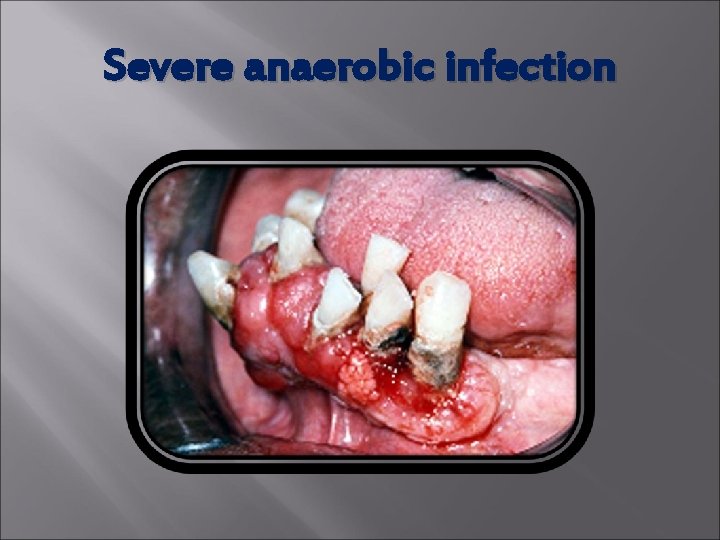
Severe anaerobic infection
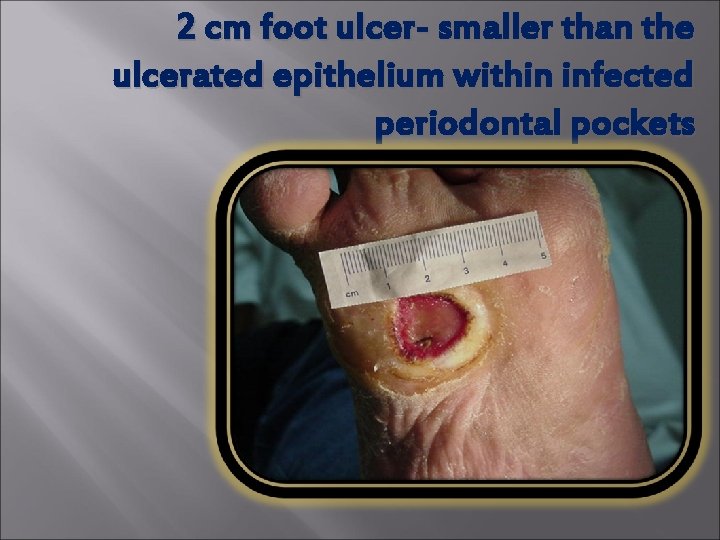
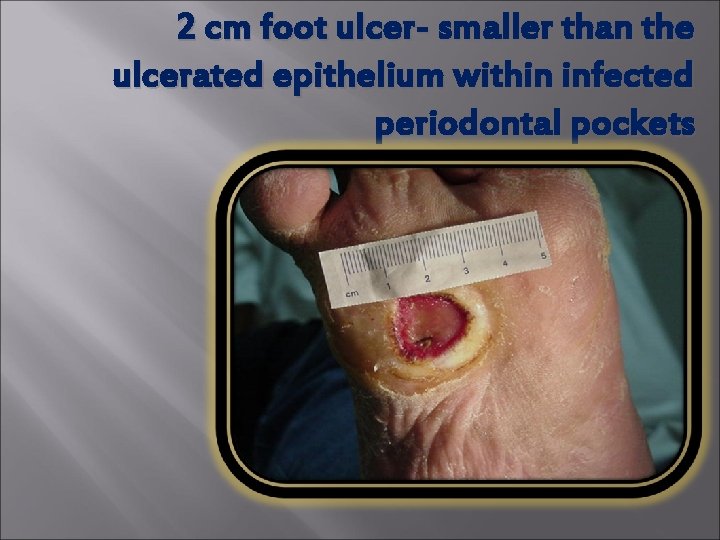
2 cm foot ulcer- smaller than the ulcerated epithelium within infected periodontal pockets
Oral Disease and Systemic Disorders Periodontal disease needs to be viewed more broadly in terms of systemic inflammation, either as a consequence of an underlying hyperinflammatory trait or as a factor contributing to systemic inflammation. Slade, Offenbacker, Beck et al J. Dent Res 2000
Periodontitis has an association with: q Diabetes q Infective Endocarditis q Cardiovascular Disease q Pre-Term, Low Birth Weight Infants q Pulmonary Disease
Pro-inflammatory cytokines (IL-1, IL-6, TNFA) and prostaglandins (Pg. E 2) accumulate in the gum tissues in active periodontitis at extraordinary circulation. levels and can enter the Salvi et al, Annals of Perio 97
Periodontitis is an anaerobic infection flooding the blood stream 24 hours a day with endotoxins and inflammatory mediators. Offenbacher, 1998
Periodontitis and Surgical Complications “The bacteria from periodontitis can enter the blood stream and cause systemic complications … and compromise recovery from any surgery, particularly patients receiving implants, transplants, or replacements of body parts since it may cause these procedures to fail. ”
Oral Disease and Systemic Disorders Periodontitis has an association with: q Diabetes q Infective Endocarditis q Cardiovascular Disease q Pre-Term, Low Birth Weight Infants q Pulmonary Disease
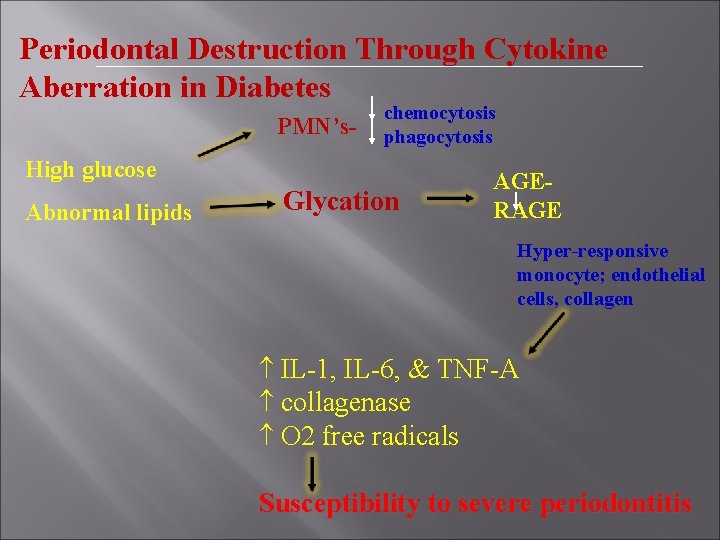
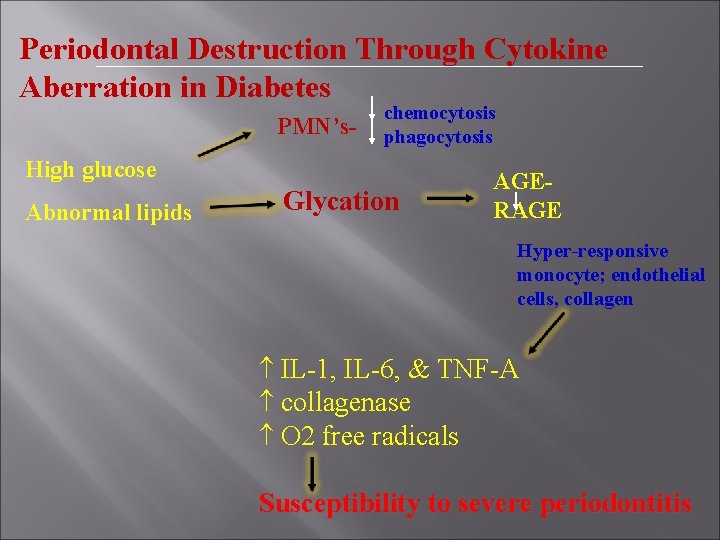
Periodontal Destruction Through Cytokine Aberration in Diabetes PMN’s- chemocytosis phagocytosis High glucose Abnormal lipids Glycation AGERAGE Hyper-responsive monocyte; endothelial cells, collagen IL-1, IL-6, & TNF-A collagenase O 2 free radicals Susceptibility to severe periodontitis
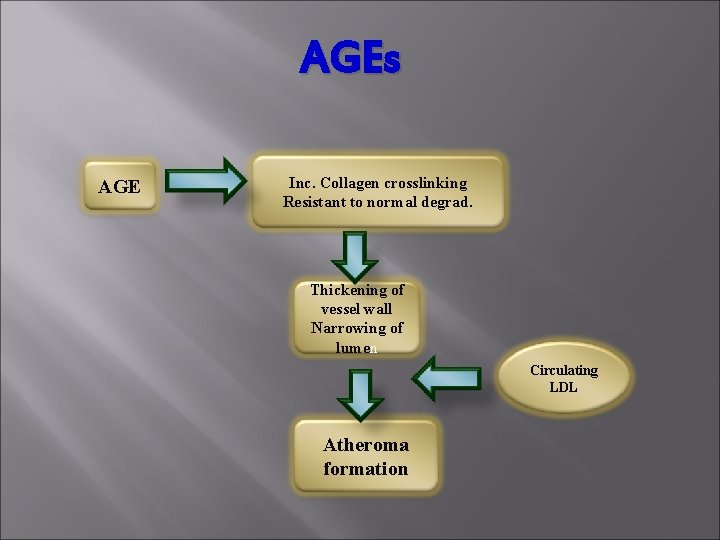
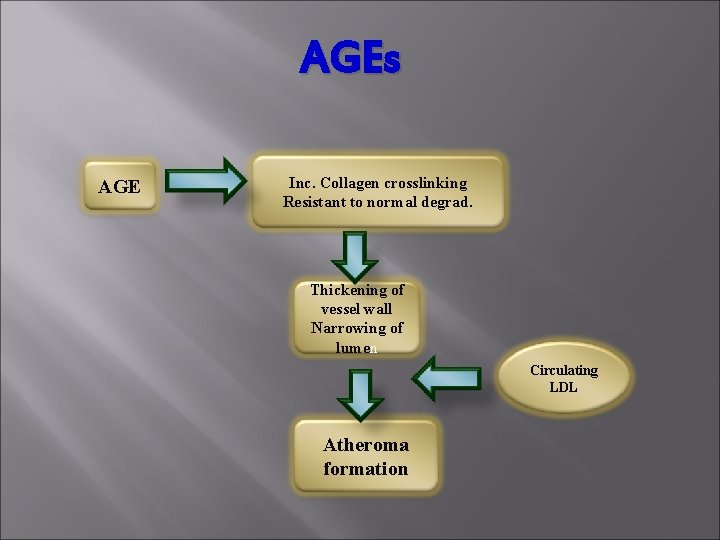
AGEs AGE Inc. Collagen crosslinking Resistant to normal degrad. Thickening of vessel wall Narrowing of lumen Circulating LDL Atheroma formation
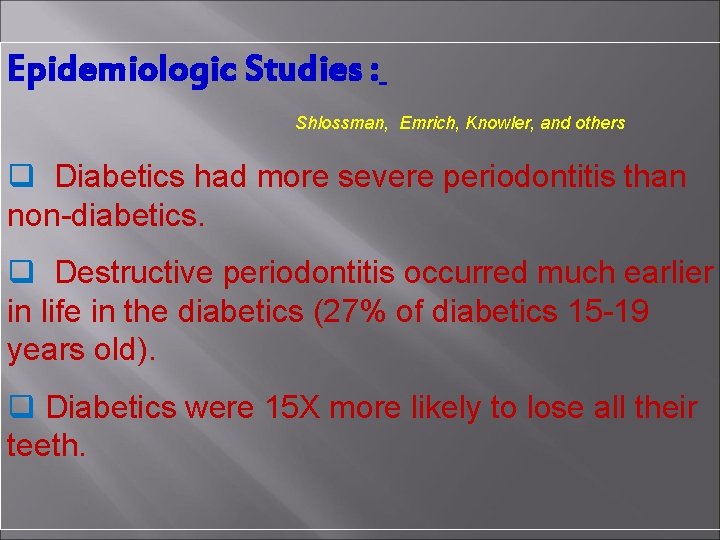
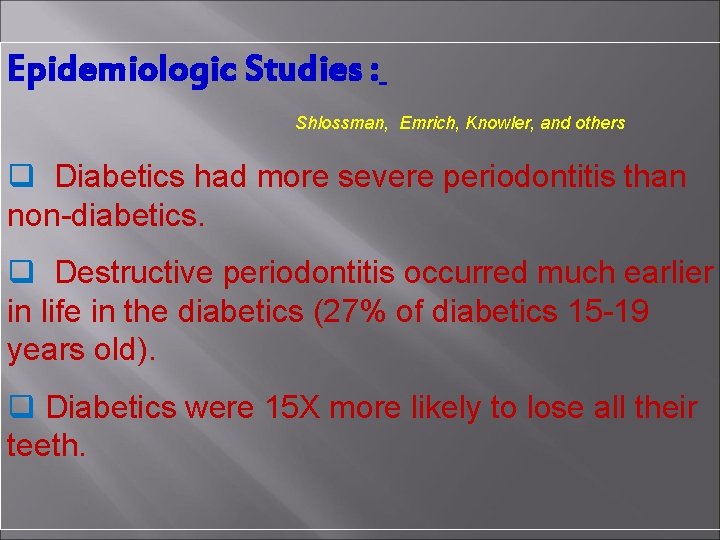
Epidemiologic Studies : Shlossman, Emrich, Knowler, and others q Diabetics had more severe periodontitis than non-diabetics. q Destructive periodontitis occurred much earlier in life in the diabetics (27% of diabetics 15 -19 years old). q Diabetics were 15 X more likely to lose all their teeth.
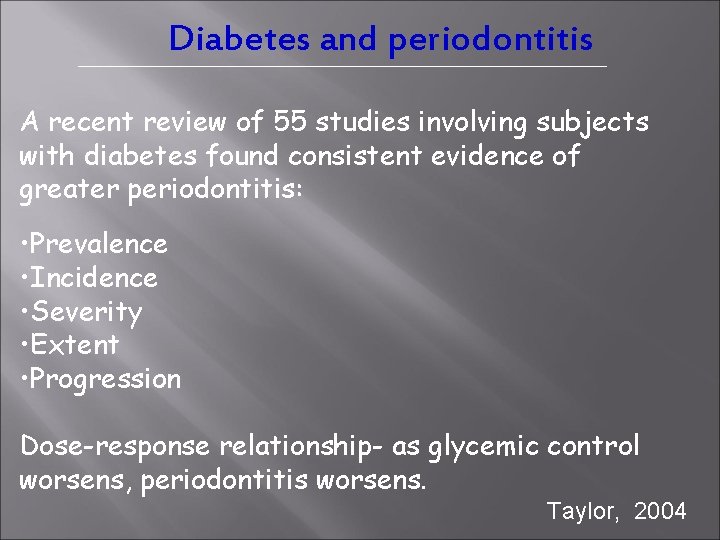
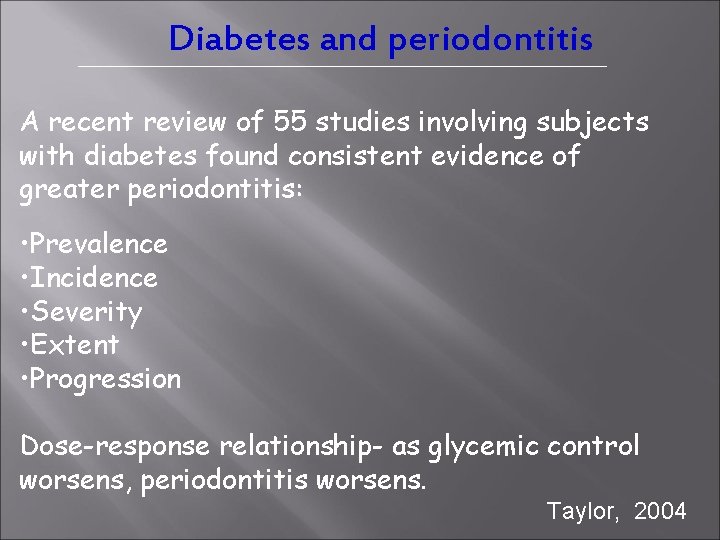
Diabetes and periodontitis A recent review of 55 studies involving subjects with diabetes found consistent evidence of greater periodontitis: • Prevalence • Incidence • Severity • Extent • Progression Dose-response relationship- as glycemic control worsens, periodontitis worsens. Taylor, 2004
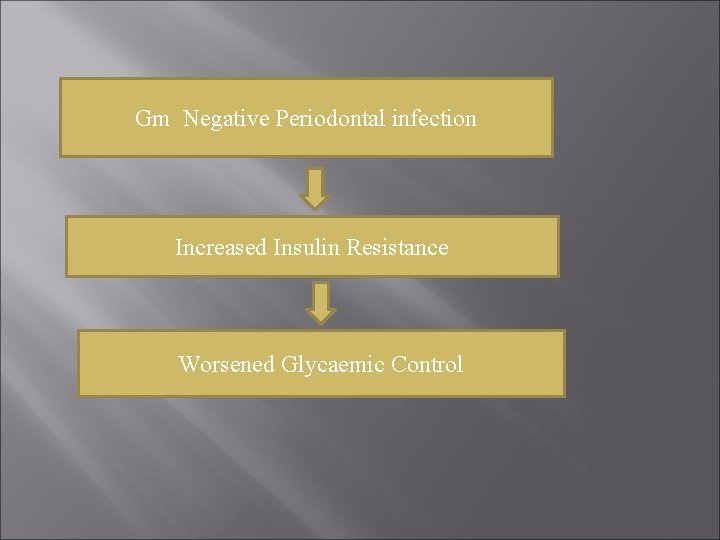
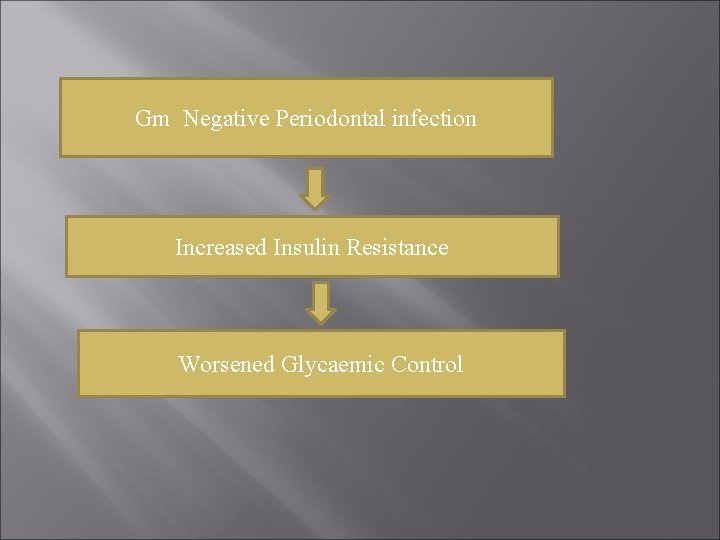
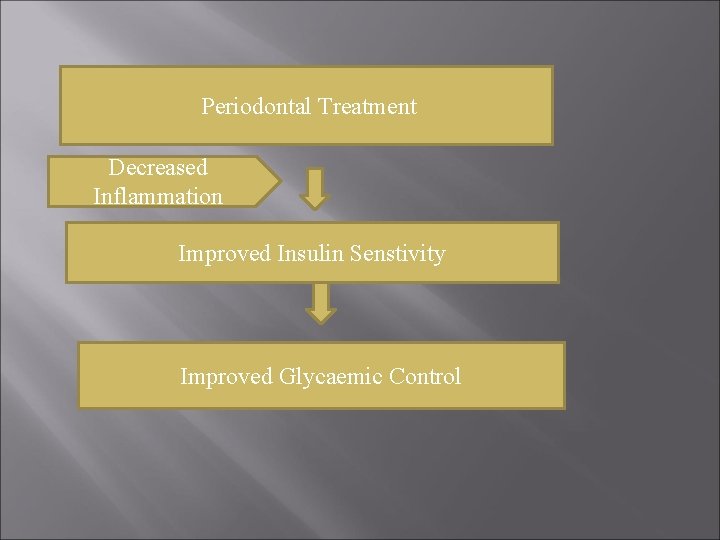
Gm Negative Periodontal infection Increased Insulin Resistance Worsened Glycaemic Control
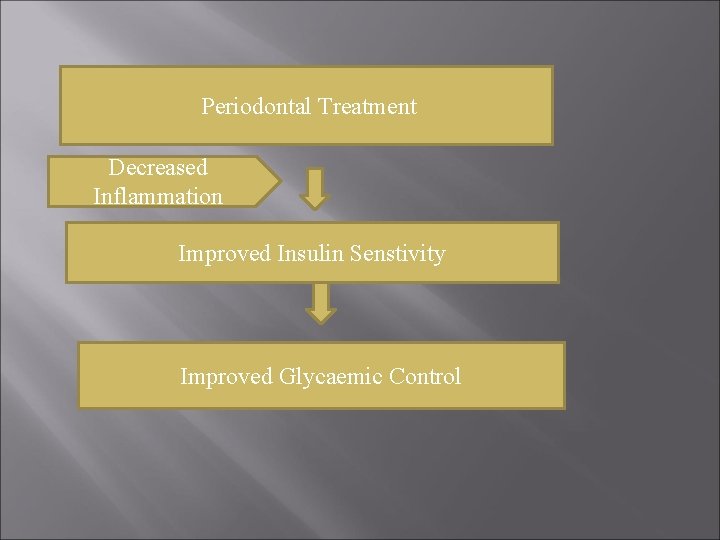
Periodontal Treatment Decreased Inflammation Improved Insulin Senstivity Improved Glycaemic Control
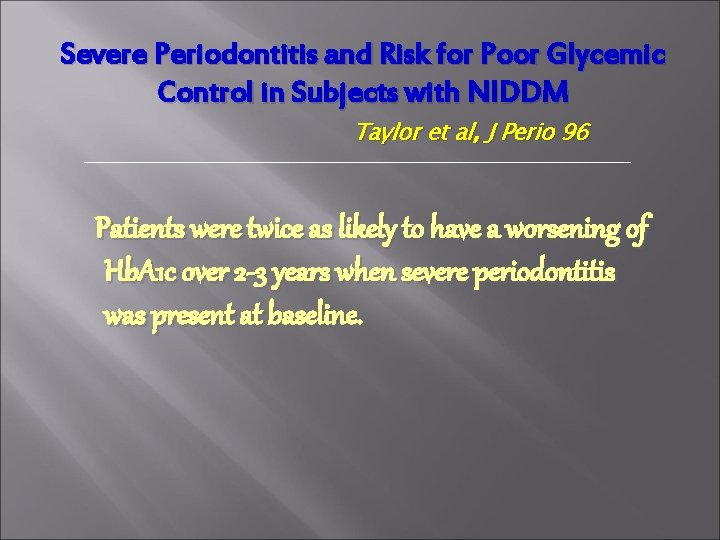
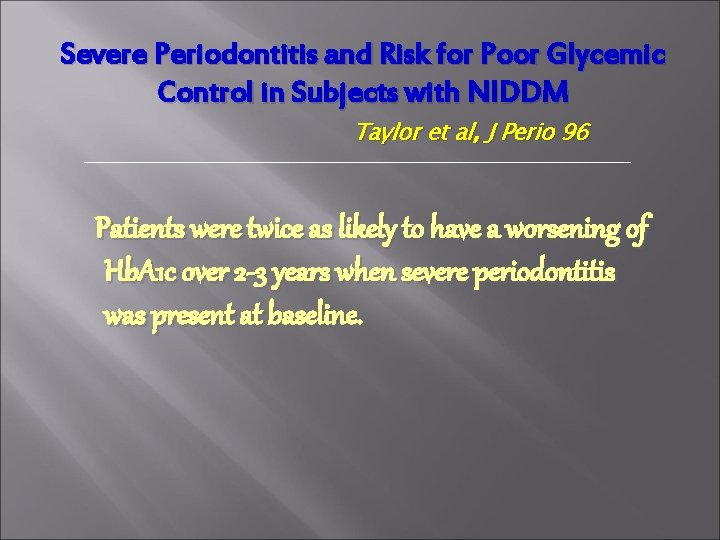
Severe Periodontitis and Risk for Poor Glycemic Control in Subjects with NIDDM Taylor et al, J Perio 96 Patients were twice as likely to have a worsening of Hb. A 1 c over 2 -3 years when severe periodontitis was present at baseline.

DM and Periodontitis- The 2 Way Relationship DM serum lipids blood glucose AGE binding/accumulation Inflammatory State Destructive Environment Further aggravated lipid metabolism & insulin resistance Periodontitis, with additional Pg. E 2 & cytokines IL- 1ß, IL-6, & TNF- A Periodontal Pathogens Increased Periodontal Destruction
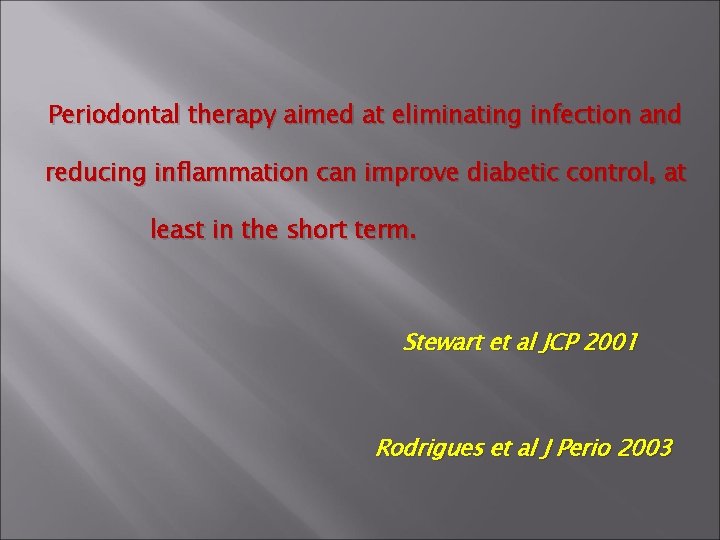
Periodontal therapy aimed at eliminating infection and reducing inflammation can improve diabetic control, at least in the short term. Stewart et al JCP 2001 Rodrigues et al J Perio 2003
Oral Disease and Systemic Disorders Periodontitis has an association with: • Diabetes • Cardiovascular Disease • Pre-Term, Low Birth Weight Infants • Pulmonary Disease
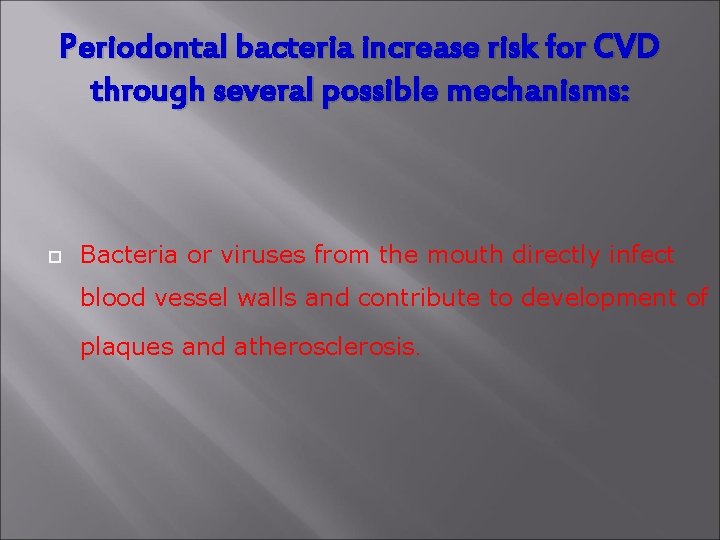
Periodontal bacteria increase risk for CVD through several possible mechanisms: Bacteria or viruses from the mouth directly infect blood vessel walls and contribute to development of plaques and atherosclerosis.
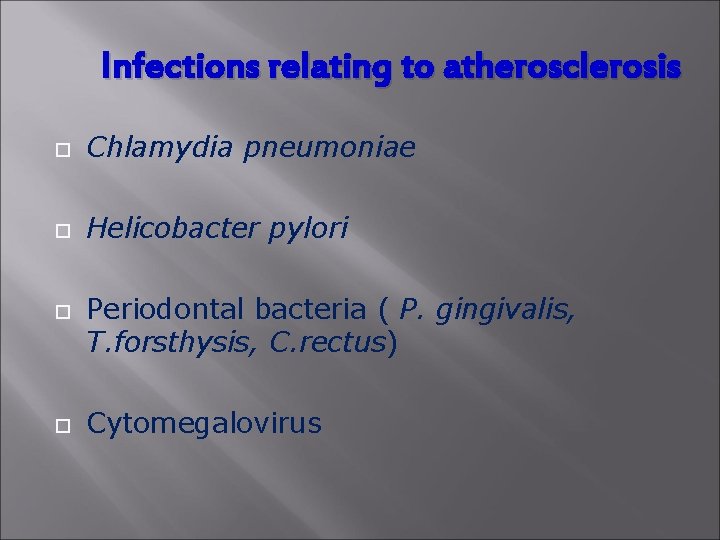
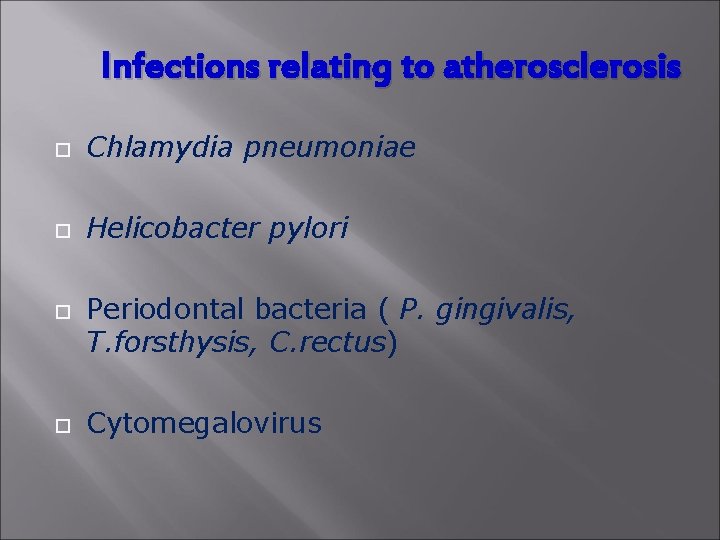
Infections relating to atherosclerosis Chlamydia pneumoniae Helicobacter pylori Periodontal bacteria ( P. gingivalis, T. forsthysis, C. rectus) Cytomegalovirus
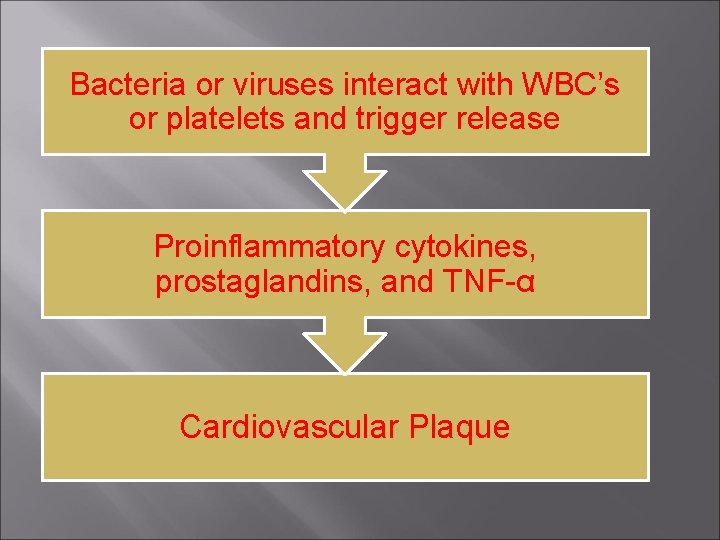
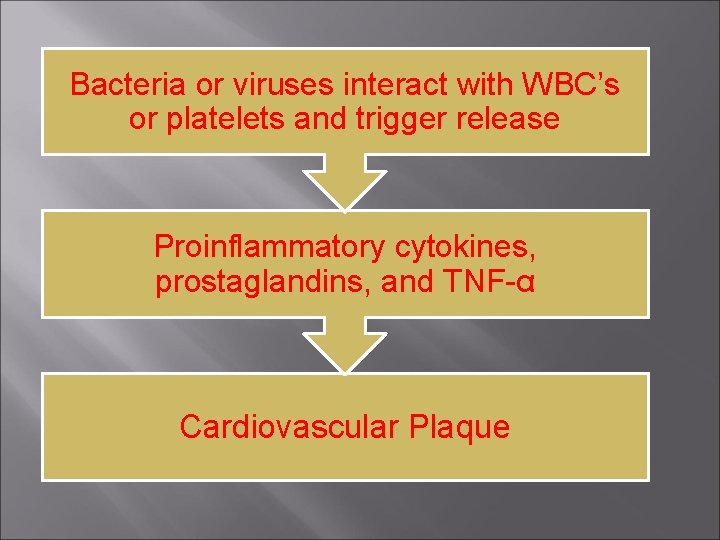
Bacteria or viruses interact with WBC’s or platelets and trigger release Proinflammatory cytokines, prostaglandins, and TNF-α Cardiovascular Plaque
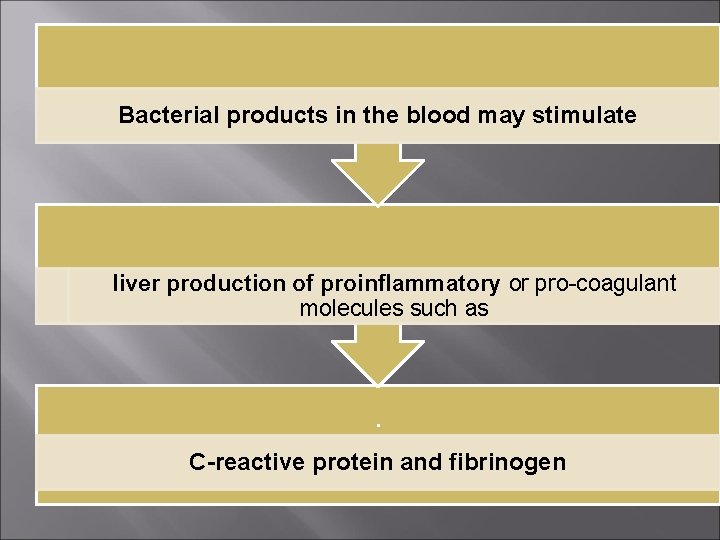
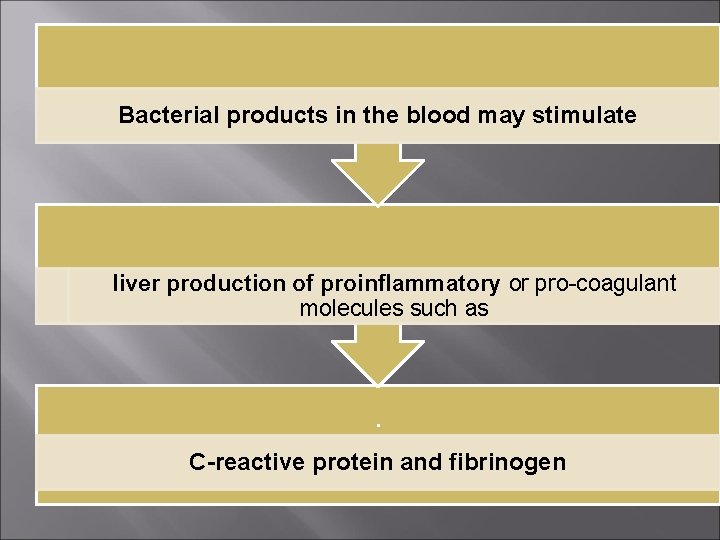
Bacterial products in the blood may stimulate liver production of proinflammatory or pro-coagulant molecules such as . C-reactive protein and fibrinogen
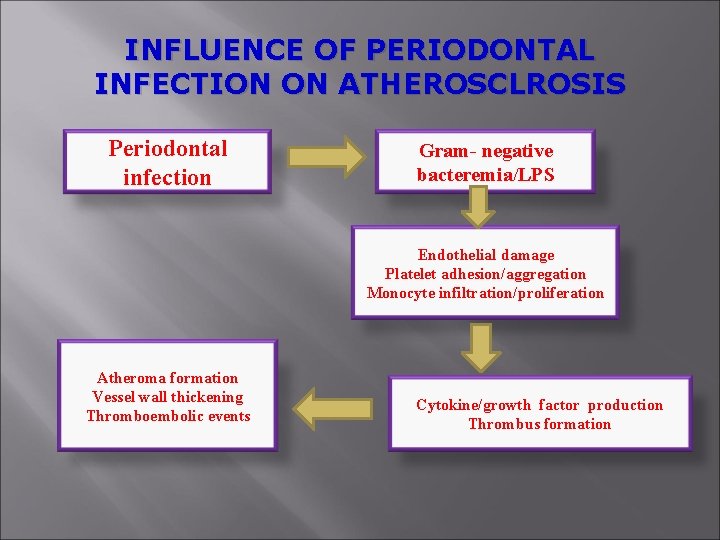
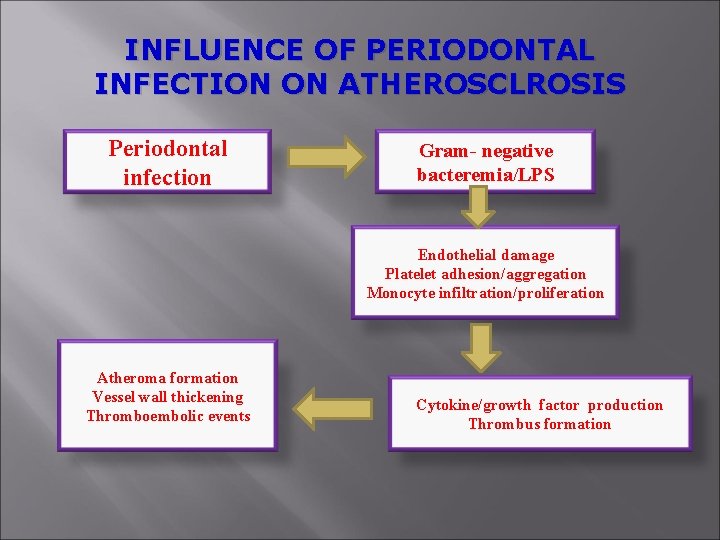
INFLUENCE OF PERIODONTAL INFECTION ON ATHEROSCLROSIS Periodontal infection Gram- negative bacteremia/LPS Endothelial damage Platelet adhesion/aggregation Monocyte infiltration/proliferation Atheroma formation Vessel wall thickening Thromboembolic events Cytokine/growth factor production Thrombus formation
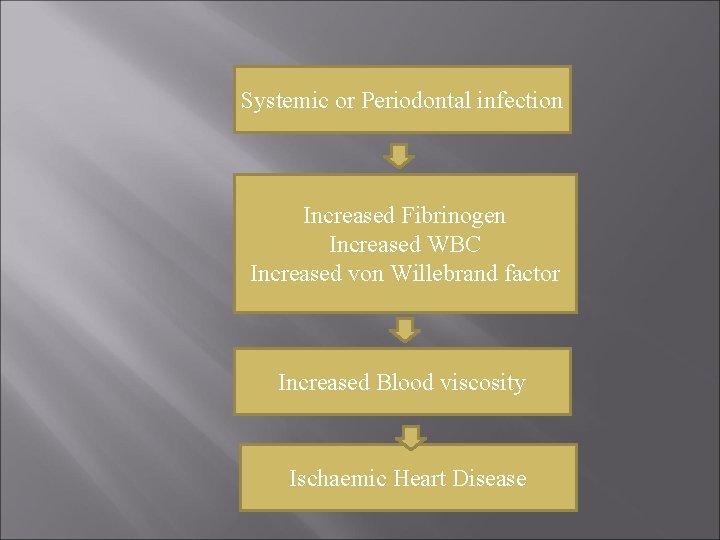
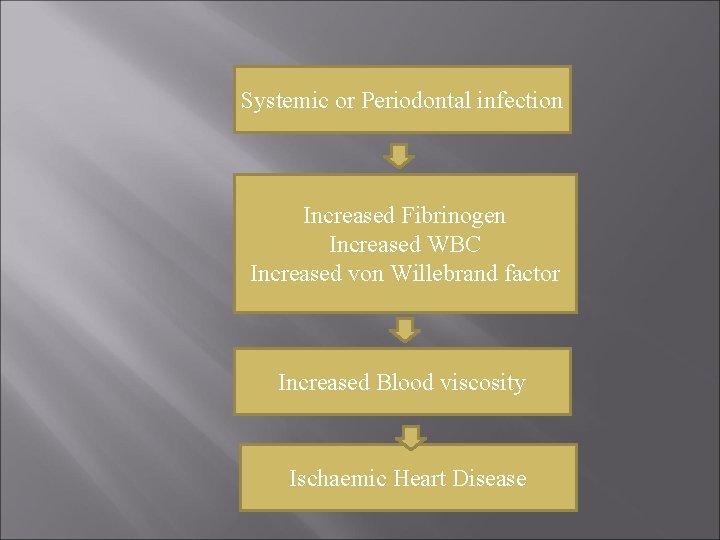
Systemic or Periodontal infection Increased Fibrinogen Increased WBC Increased von Willebrand factor Increased Blood viscosity Ischaemic Heart Disease
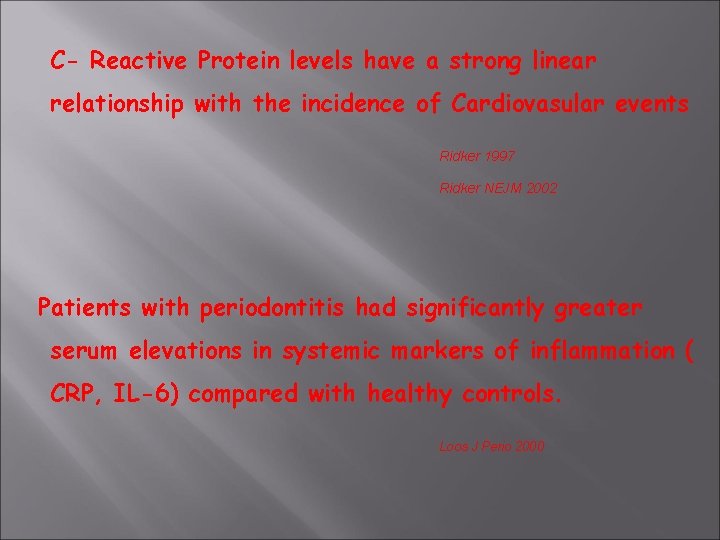
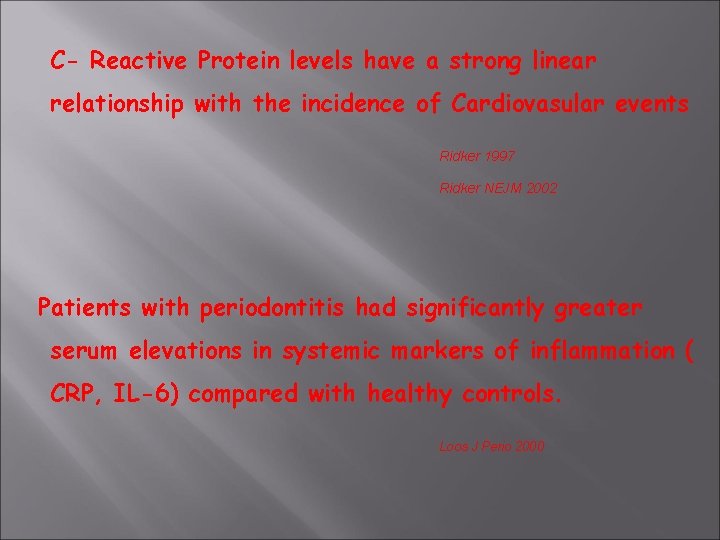
C- Reactive Protein levels have a strong linear relationship with the incidence of Cardiovasular events Ridker 1997 Ridker NEJM 2002 Patients with periodontitis had significantly greater serum elevations in systemic markers of inflammation ( CRP, IL-6) compared with healthy controls. Loos J Perio 2000
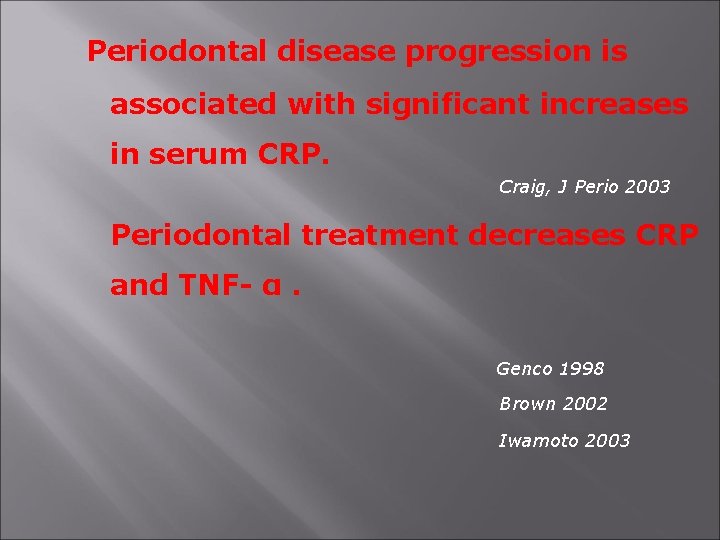
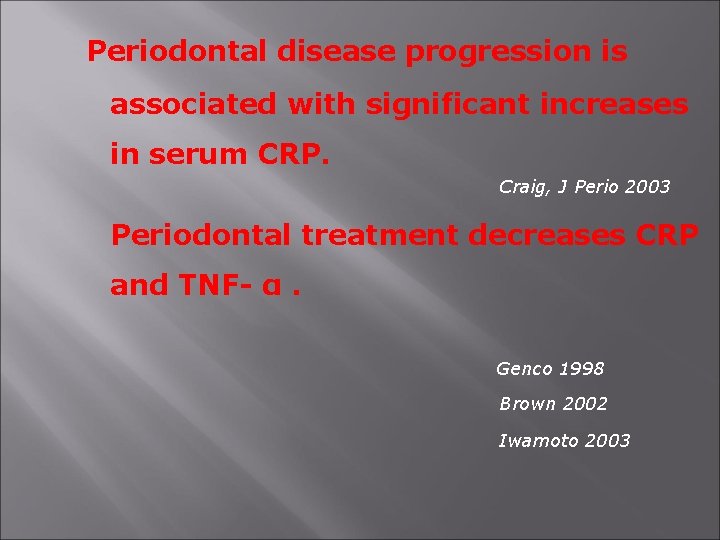
Periodontal disease progression is associated with significant increases in serum CRP. Craig, J Perio 2003 Periodontal treatment decreases CRP and TNF- α. Genco 1998 Brown 2002 Iwamoto 2003
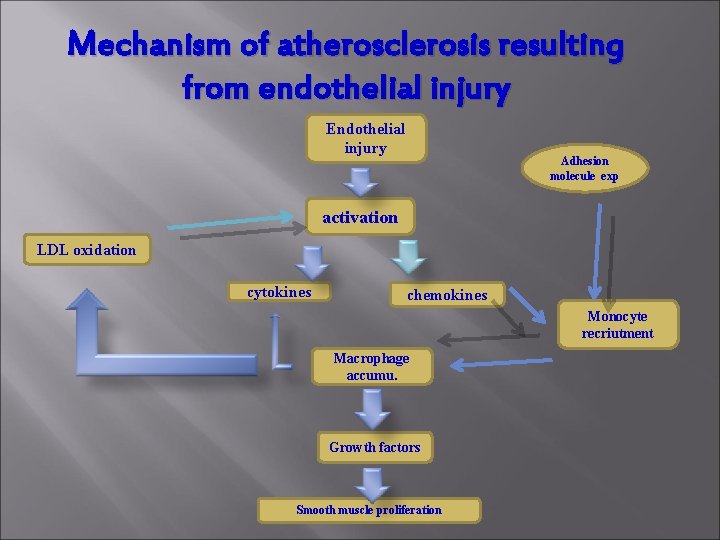
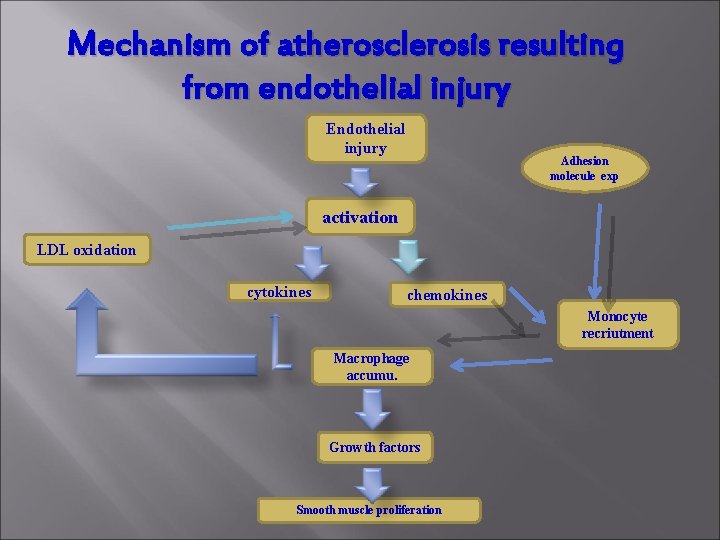
Mechanism of atherosclerosis resulting from endothelial injury Endothelial injury Adhesion molecule exp activation LDL oxidation cytokines chemokines Monocyte recriutment Macrophage accumu. Growth factors Smooth muscle proliferation
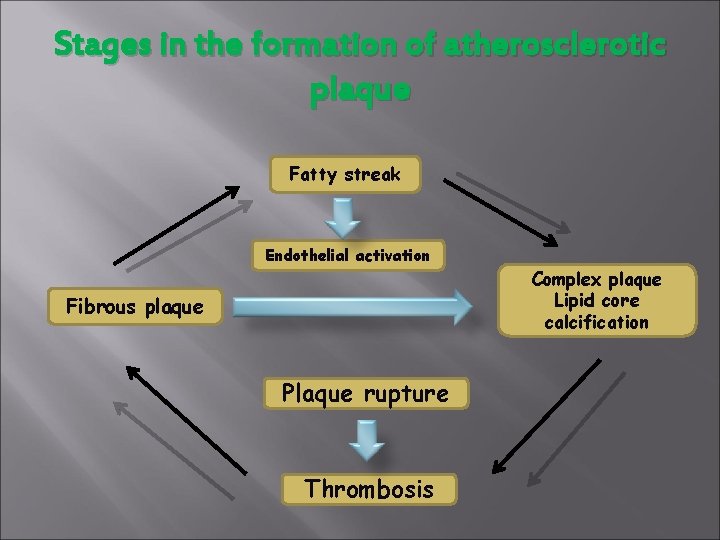
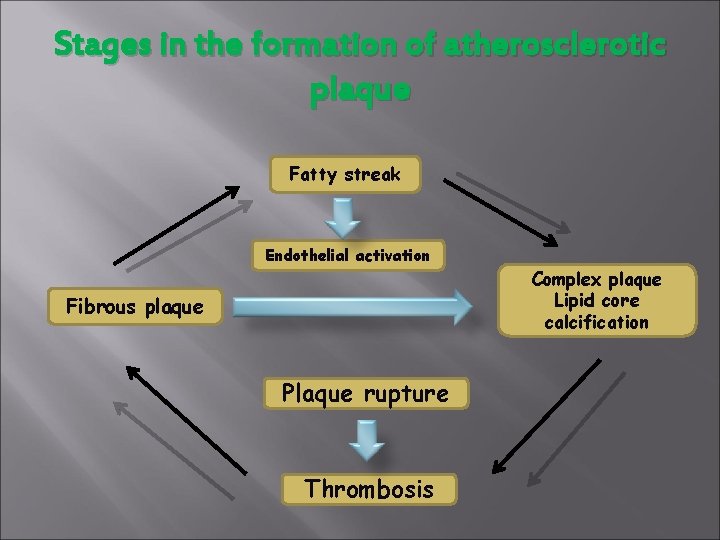
Stages in the formation of atherosclerotic plaque Fatty streak Endothelial activation Fibrous plaque Plaque rupture Thrombosis Complex plaque Lipid core calcification
Periodontitis and Pre-Term, Low Birth Weight Infants
PTLBW infant treatment in hospitals for respiratory distress, jaundice, malnutrition, anemia.
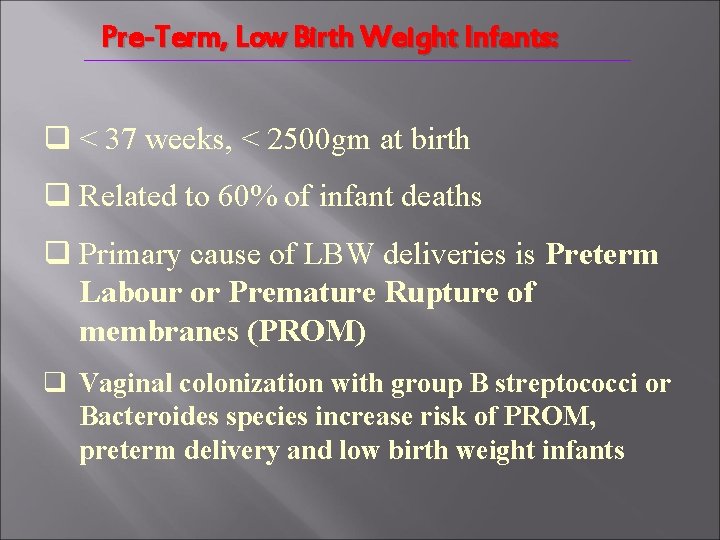
Pre-Term, Low Birth Weight Infants: q < 37 weeks, < 2500 gm at birth q Related to 60% of infant deaths q Primary cause of LBW deliveries is Preterm Labour or Premature Rupture of membranes (PROM) q Vaginal colonization with group B streptococci or Bacteroides species increase risk of PROM, preterm delivery and low birth weight infants
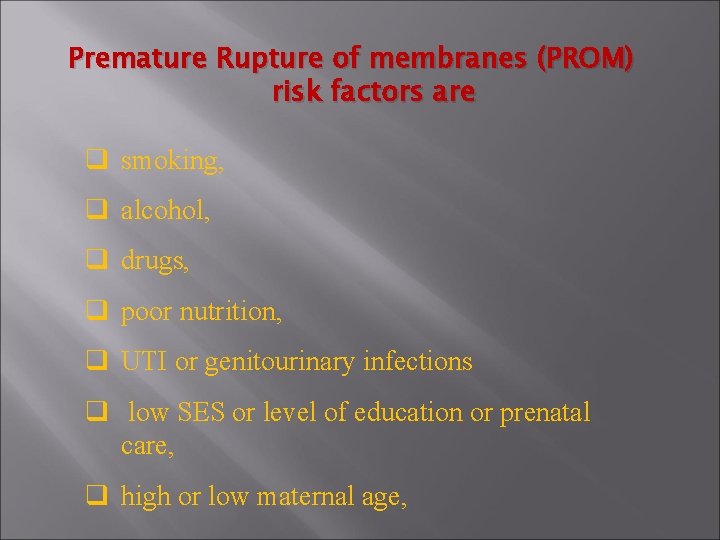
Premature Rupture of membranes (PROM) risk factors are q smoking, q alcohol, q drugs, q poor nutrition, q UTI or genitourinary infections q low SES or level of education or prenatal care, q high or low maternal age,
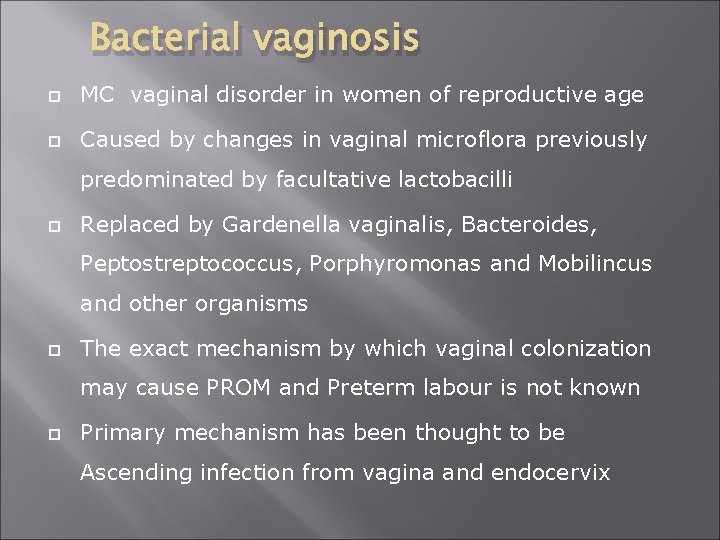
Bacterial vaginosis MC vaginal disorder in women of reproductive age Caused by changes in vaginal microflora previously predominated by facultative lactobacilli Replaced by Gardenella vaginalis, Bacteroides, Peptostreptococcus, Porphyromonas and Mobilincus and other organisms The exact mechanism by which vaginal colonization may cause PROM and Preterm labour is not known Primary mechanism has been thought to be Ascending infection from vagina and endocervix
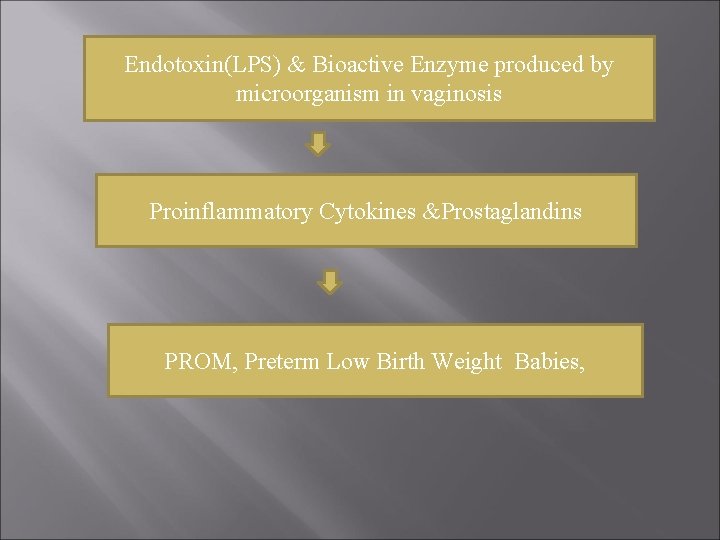
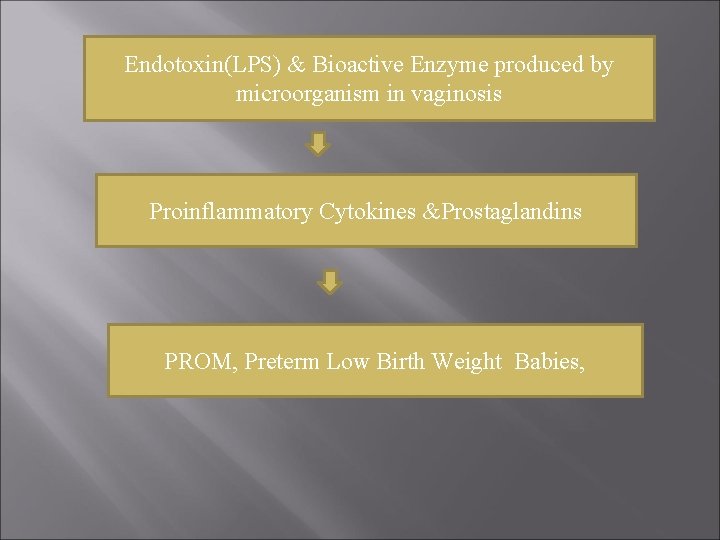
Endotoxin(LPS) & Bioactive Enzyme produced by microorganism in vaginosis Proinflammatory Cytokines &Prostaglandins PROM, Preterm Low Birth Weight Babies,
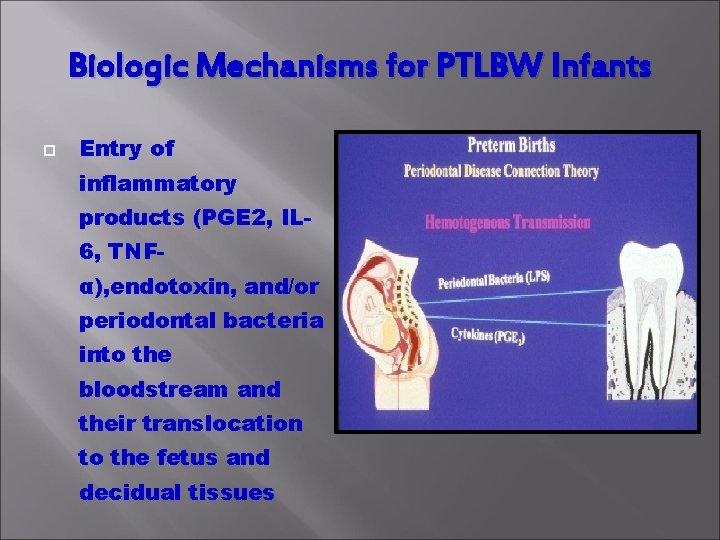
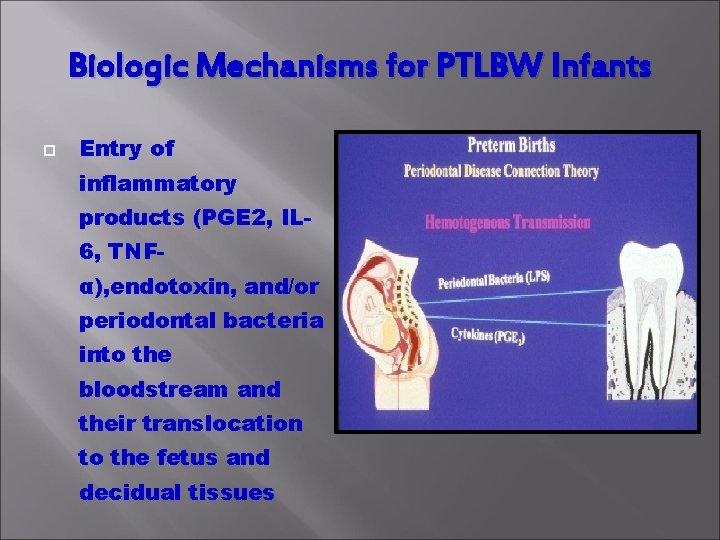
Biologic Mechanisms for PTLBW Infants Entry of inflammatory products (PGE 2, IL 6, TNFα), endotoxin, and/or periodontal bacteria into the bloodstream and their translocation to the fetus and decidual tissues
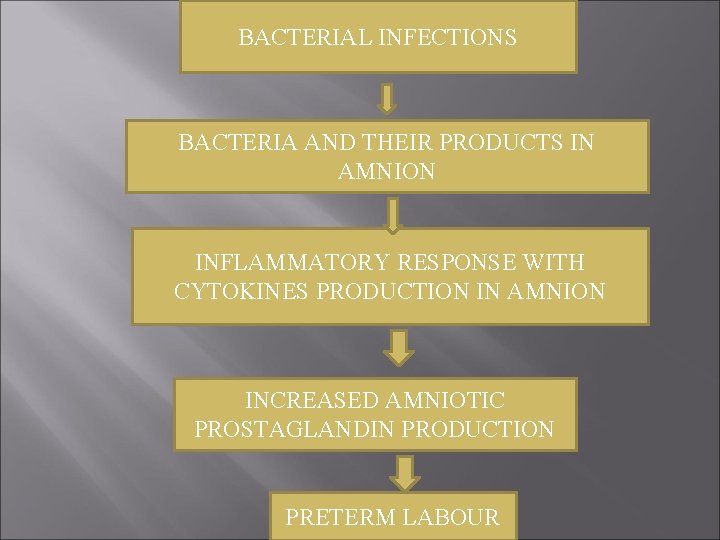
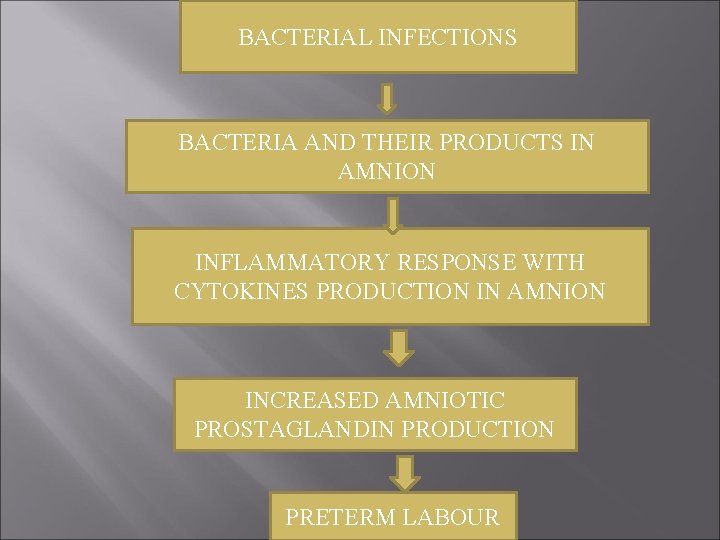
BACTERIAL INFECTIONS BACTERIA AND THEIR PRODUCTS IN AMNION INFLAMMATORY RESPONSE WITH CYTOKINES PRODUCTION IN AMNION INCREASED AMNIOTIC PROSTAGLANDIN PRODUCTION PRETERM LABOUR
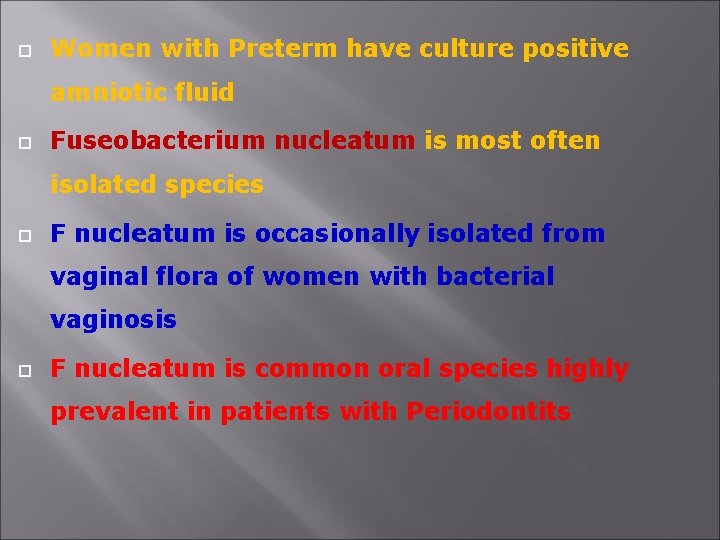
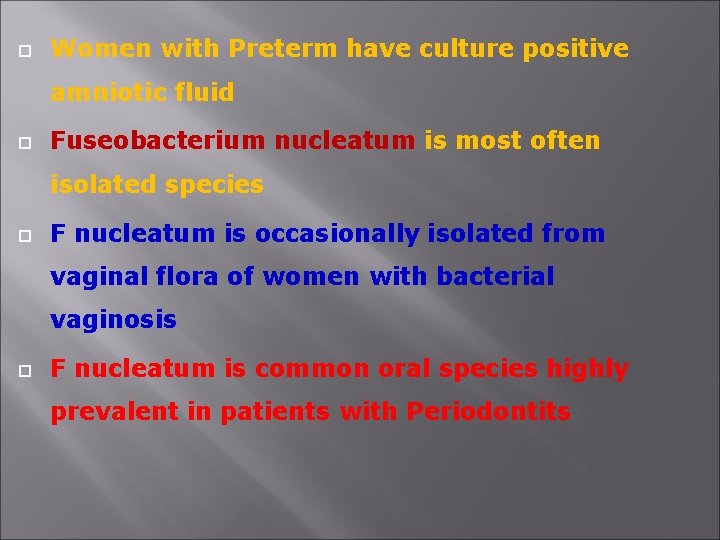
Women with Preterm have culture positive amniotic fluid Fuseobacterium nucleatum is most often isolated species F nucleatum is occasionally isolated from vaginal flora of women with bacterial vaginosis F nucleatum is common oral species highly prevalent in patients with Periodontits
q. Reaches amniotic fluid through haematogenous route q. Also Capnocytophaga, another periodontal pathogen is isolated from amniotic fluid of preterm females
Women with PLBW babies have significantly higher levels of periodontal pathogens like A a, Tf, Pg and T d in their subgingival plaque than controls having normal birth weight babies. Offenbaher, 1998 Women having PLBW babies have higher levels of IL-1 and PGE-2 in GCF
q. In Primiparous women GCF levels of PGE-2 inversely related to infant birth weight q. GCF LEVEL OF IL-1 AND PGE-2 HIGHLY CORRELATE WITH INTRAAMNIOTIC LEVELS
Preclampsia PERIODONTAL INFECTION MAY ALSO INCREASE RISK OF PRECLAMPSIA IN PREGNANT FEMALES
• Periodontitis appears to be an independent risk factor for pre-term delivery. • There is a clear need for more well designed observational and intervention studies to confirm observations. Expectant mothers should be counseled in the importance of oral health.
Periodontal disease and Acute Respiratory infections 1. Community-acquired bacterial pneumonia Streptococcus Haemophilus pneumonia influenza
Hospital acquired (Nosocomial) bacterial Pneumonia 2. Potential Respiratory pathogen (PRP) ØPredominantly found in GIT by Reflux esophagitis ØPRP may orignate in oral cavity, dental plaque serve as reservoir ØPRP isolated from subgingival plaque and buccal mucosa of patients intensive care units and in out patient settings
Selective Decontamination Employs Systemic Antibiotics with orally administered non-absorbable antibiotics in atempt to eradicate PRPs from the digestive tract and oropharyx and thereby minimize the risk of nosocomial respiratory infections.

 Chapter 26 infectious disease prevention and control
Chapter 26 infectious disease prevention and control Infectious disease quality controls
Infectious disease quality controls Stages of infection
Stages of infection Stages of infectious disease
Stages of infectious disease Stridor
Stridor Infectious disease
Infectious disease Hennepin county infectious disease manual
Hennepin county infectious disease manual Viruses are the smallest infectious agents
Viruses are the smallest infectious agents Iatrogenic factors in periodontal disease
Iatrogenic factors in periodontal disease Diagnosis of periodontal disease
Diagnosis of periodontal disease Periodontal disease
Periodontal disease Communicable disease and non communicable disease
Communicable disease and non communicable disease Oral disease
Oral disease Icd 10 morbus hansen
Icd 10 morbus hansen Hhps symbols
Hhps symbols Oral pathology
Oral pathology Waste management definition
Waste management definition Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious canine hepatitis in dogs
Infectious canine hepatitis in dogs Infectious nucleic acid
Infectious nucleic acid Blood smear
Blood smear Infectious mononucleosis
Infectious mononucleosis Epidemiological triad of malaria
Epidemiological triad of malaria Noncellular infectious protein particles are called
Noncellular infectious protein particles are called Infectious stunting syndrome
Infectious stunting syndrome Difference between local and systemic
Difference between local and systemic Systemic factors influencing wound healing
Systemic factors influencing wound healing Systemic pathology exam questions pdf
Systemic pathology exam questions pdf Arteries
Arteries Blood circulation system diagram
Blood circulation system diagram Principles of scaling and root planing
Principles of scaling and root planing Perimylolysis
Perimylolysis Politür lastiği
Politür lastiği Oxytalin
Oxytalin Eoe ioe dental
Eoe ioe dental Plaque index scoring criteria
Plaque index scoring criteria Ligamento periodontal
Ligamento periodontal Corrective phase periodontal therapy
Corrective phase periodontal therapy Indikasi gingivektomi
Indikasi gingivektomi Rationale of periodontal treatment
Rationale of periodontal treatment Junctional epitel
Junctional epitel Fibras oblicuas del ligamento periodontal
Fibras oblicuas del ligamento periodontal Glickman's concept
Glickman's concept Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Akut streptokokal gingivitis
Akut streptokokal gingivitis Ventajas de la técnica crown-down
Ventajas de la técnica crown-down Heliprobe 2 positivo
Heliprobe 2 positivo Viscoelastic theory of pdl
Viscoelastic theory of pdl Dişin embriyolojik gelişim evreleri
Dişin embriyolojik gelişim evreleri Non corticated
Non corticated Periapical granuloma vs abscess
Periapical granuloma vs abscess Periodontal abscess
Periodontal abscess Periodontal ligament injection definition
Periodontal ligament injection definition Kista residual
Kista residual Dental symbols for charting
Dental symbols for charting