Perinatal Asphyxia Hypoxic Ischemic Encephalopathy DR Tirupati 1




- Slides: 81
Perinatal Asphyxia & Hypoxic Ischemic Encephalopathy DR. Tirupati 1
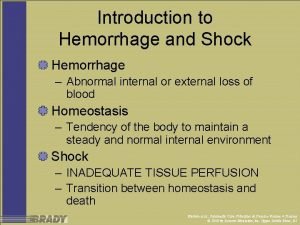
Definitions • Anoxia: – Complete lack of oxygen. • Hypoxia: – Decreased availability of oxygen • Hypoxemia: – Decreased arterial concentration of oxygen. • Ischemia: – Insufficient blood flow to cells or organ resulting in interrupted metabolism and death of the cell or organ affected. 2
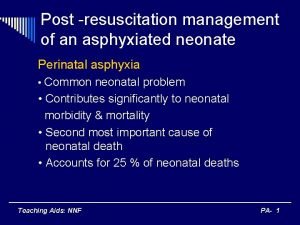
Perinatal Asphyxia (PA) Perinatal asphyxia, neonatal asphyxia, or birth asphyxia is the medical condition resulting from deprivation of oxygen to a newborn infant that causes physical harm, mainly to the brain. 3
Definition The Perinatal Asphyxia may be defined as hypoxic insult to the fetus severe enough to cause metabolic acidosis, neonatal encephalopathy, and multiorgan system dysfunction. 4
Perinatal Asphyxia The NNF of India has defined asphyxia as “gasping or ineffective breathing or lack of breathing at one minute of life” 5
AAP Criteria • Umbilical artery blood p. H < 7. 0. • 5 minute apgar score < 3, • Neonatal Encephalopathy manifesting as seizures, hypotonia or coma in the immediate neonatal period. • Evidence of multiorgan dysfunction. 6
Birth Asphyxia • Birth Asphyxia = Perinatal Asphyxia = Neonatal Asphyxia. • Incidence: 1 – 6 /1000 live births. 7
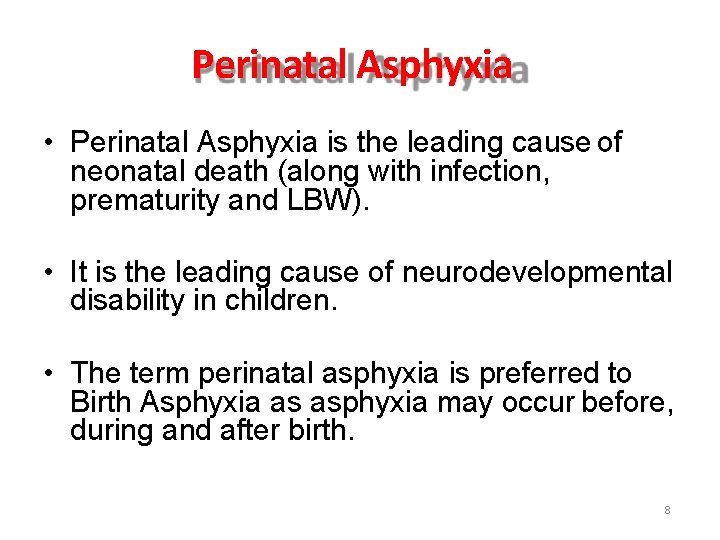
Perinatal Asphyxia • Perinatal Asphyxia is the leading cause of neonatal death (along with infection, prematurity and LBW). • It is the leading cause of neurodevelopmental disability in children. • The term perinatal asphyxia is preferred to Birth Asphyxia as asphyxia may occur before, during and after birth. 8

Why it is important? 9
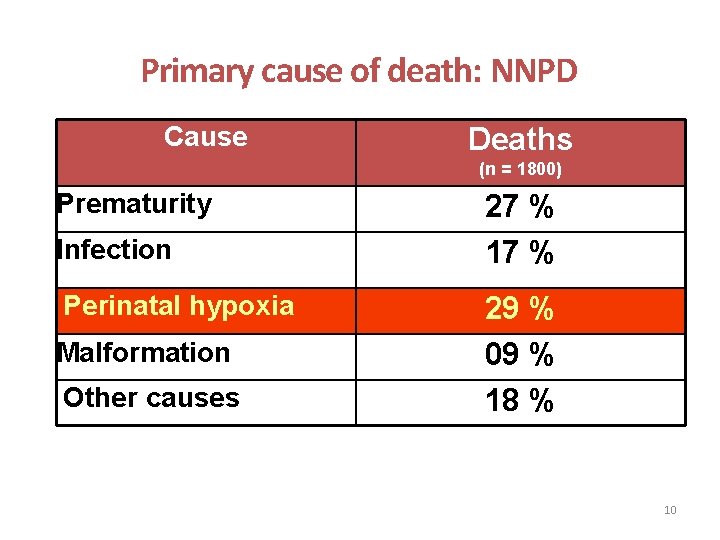
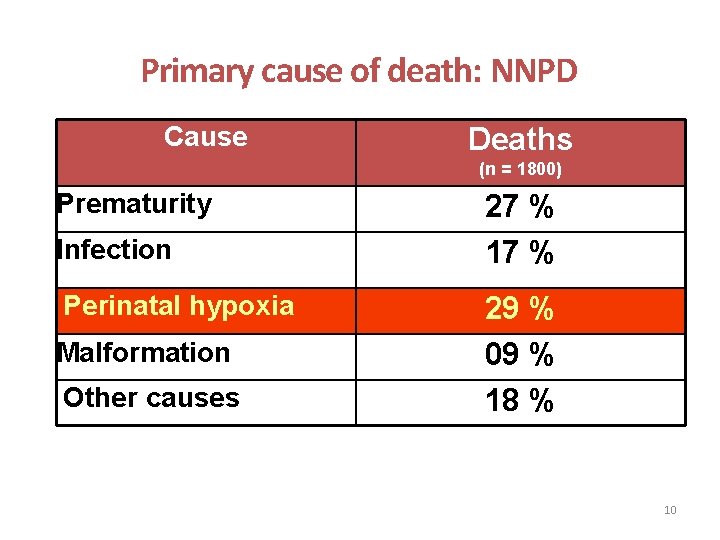
Primary cause of death: NNPD Cause Deaths (n = 1800) Prematurity Infection Perinatal hypoxia Malformation Other causes 27 % 17 % 29 % 09 % 18 % 10
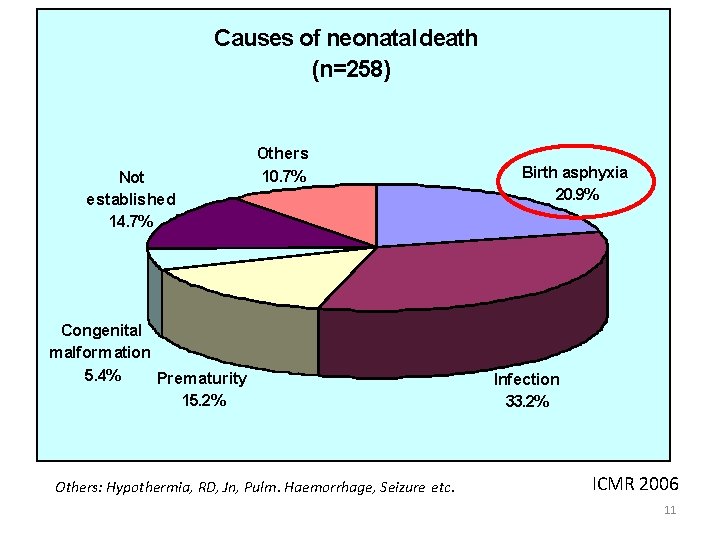
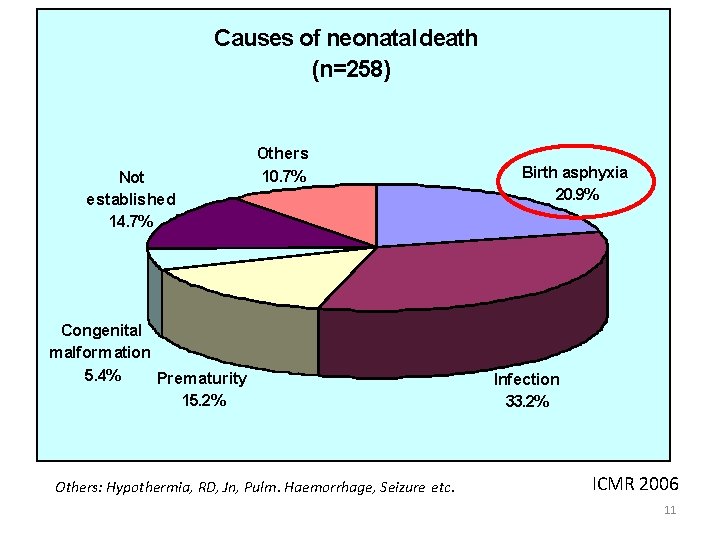
Causes of neonatal death (n=258) Not established 14. 7% Others 10. 7% Congenital malformation 5. 4% Prematurity 15. 2% Others: Hypothermia, RD, Jn, Pulm. Haemorrhage, Seizure etc. Birth asphyxia 20. 9% Infection 33. 2% ICMR 2006 11
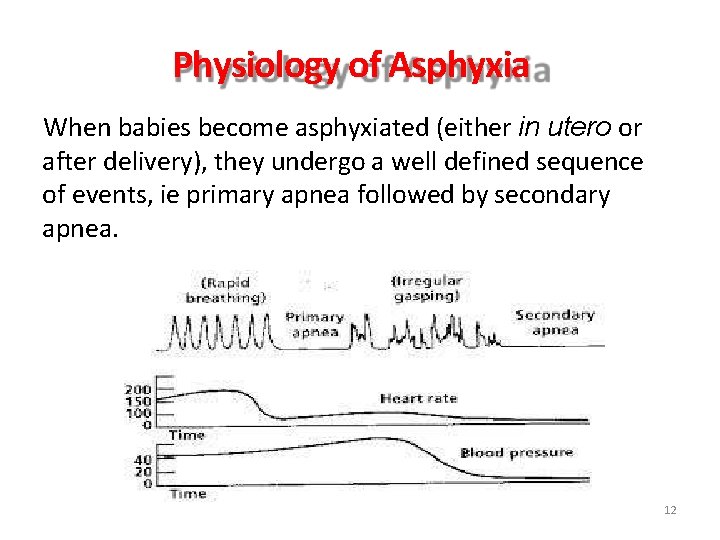
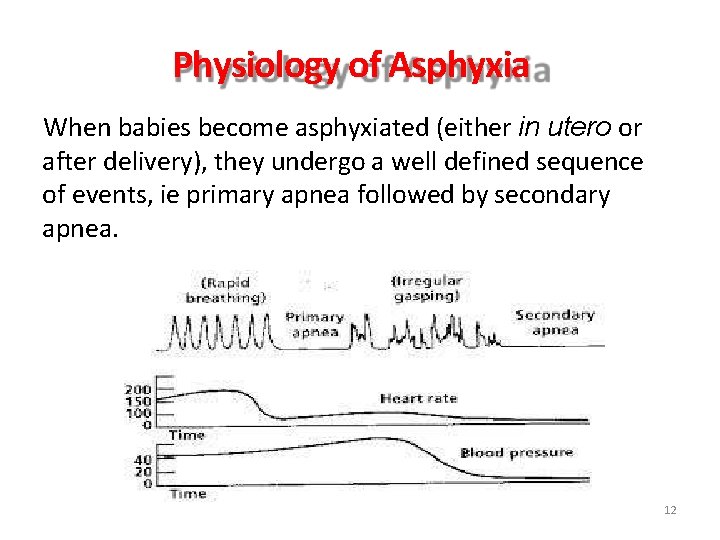
Physiology of Asphyxia When babies become asphyxiated (either in utero or after delivery), they undergo a well defined sequence of events, ie primary apnea followed by secondary apnea. 12
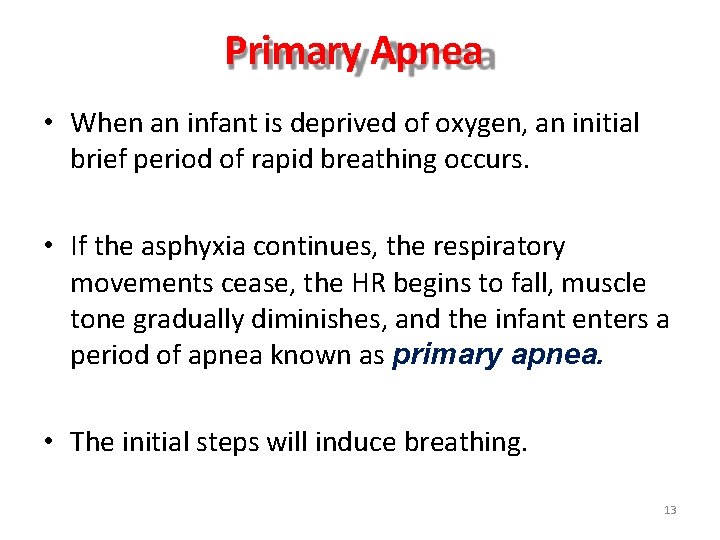
Primary Apnea • When an infant is deprived of oxygen, an initial brief period of rapid breathing occurs. • If the asphyxia continues, the respiratory movements cease, the HR begins to fall, muscle tone gradually diminishes, and the infant enters a period of apnea known as primary apnea. • The initial steps will induce breathing. 13
Secondary Apnea • If the asphyxia continues, the infant develops deep gasping respiration, the HR continues to decrease, the BP begins to fall, and the infant becomes nearly flaccid. • The respirations become weak and weaker until the infant takes a last gasp and enters a period of apnea called secondary apnea. • During secondary apnea the infant does not respond to initial steps. 14
Effects of PA • Hypoxic damage to most of the infant's organs (heart, lungs, liver, gut, kidneys), but brain damage is of most concern and perhaps the least likely to heal. • In more pronounced cases, an infant will survive, but with damage to the brain manifested as either mental or physical disability, such as developmental delay or intellectual disability, or physical, such as spasticity 15
Effects (continued) • Mental Disability: – Developmental Delay, – Intellectual Disability. • Physical Disability: – Spasticity, – Motor Deficit. • Cerebral Palsy. 16
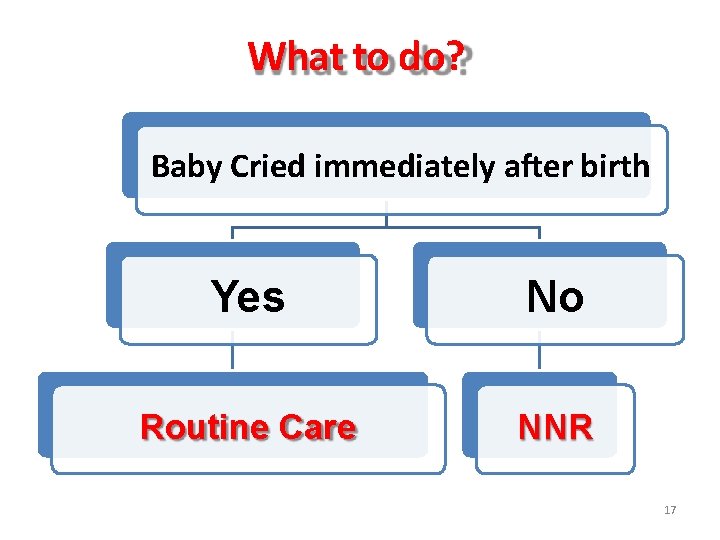
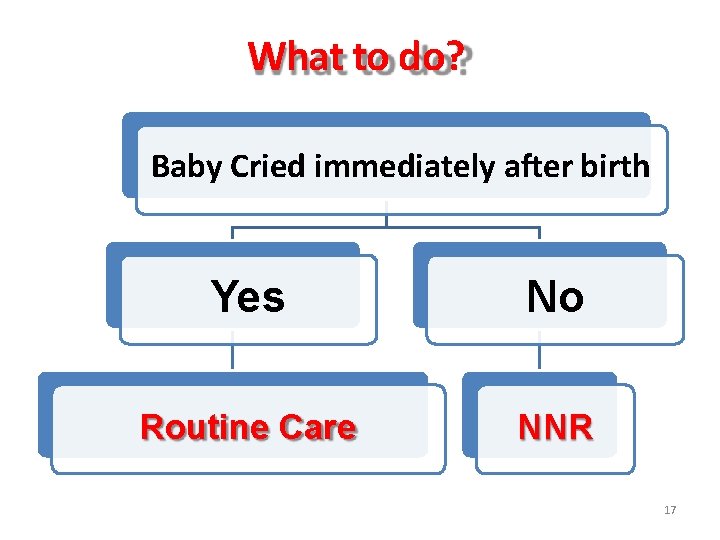
What to do? Baby Cried immediately after birth Yes No Routine Care NNR 17
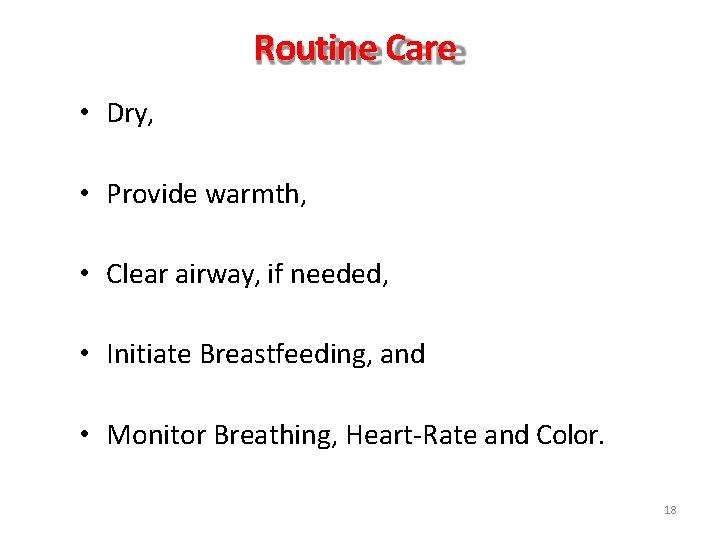
Routine Care • Dry, • Provide warmth, • Clear airway, if needed, • Initiate Breastfeeding, and • Monitor Breathing, Heart-Rate and Color. 18
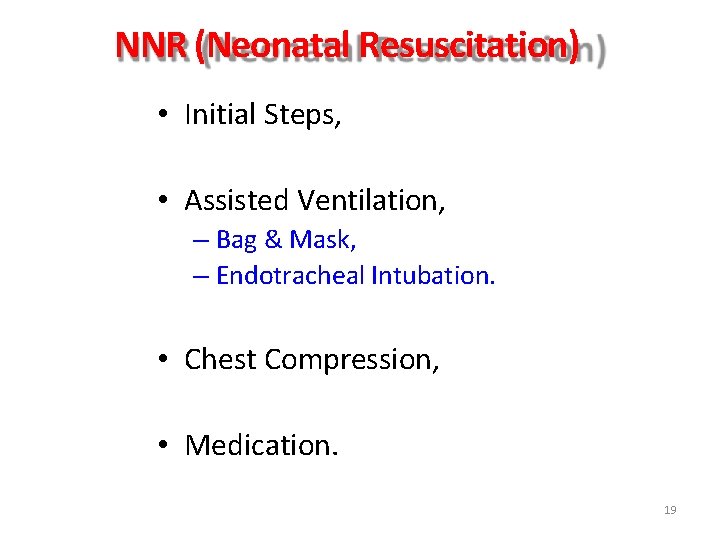
NNR (Neonatal Resuscitation) • Initial Steps, • Assisted Ventilation, – Bag & Mask, – Endotracheal Intubation. • Chest Compression, • Medication. 19
Global Hypoxic Ischemic Insult of Brain Hypoxic Ischemic Encephalopathy (HIE) 20
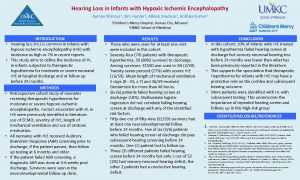
Hypoxic-Ischemic Encephalopathy (HIE) • The HIE refers to the characteristic neurological manifestations in term and near-term newborns which develop soon after birth following perinatal asphyxia. • Incidence: 3 -5 per 1000 full-term live births. • Half of them progress to moderate to severe HIE. 21
HIE • The encephalopathy resulting from hypoxia (low oxygen) and ischemia (low blood flow) mainly to the brain. • The HIE refers to the characteristic neurological manifestations in term and nearterm newborns which develop soon after birth following perinatal asphyxia. 22
Pathology • Lack of adequate breathing lack of oxygen supply to heart Inability of heart to pump adequate blood hypoxia + ischemia to organs (particularly brain). • Longer Arrest Infarct Brain Death. 23
Brain Regions vulnerable for damage • Hippocampus, • Purkinje Neurons in Cerebellum, • Basal Ganglia, and • Brain-stem. 24
Pathogenesis • Poorly understood, • Hypoxic Ischemic insult can damage periventricular white matter tracks. 25
Etiology • Perinatal Asphyxia, • Trauma, • Drowning, • Hanging, • Airway Obstruction, • Infection 26
Outcome • Immediate outcome: Death. • Late outcome (if survived): – Cerebral Palsy, – Developmental Delay, – Mental Retardation. 27
Further Outcome (complications) • Death, • Vegetative State, • Severe Disability, • SIRS, • Multiple Organ Dysfunction Syndrome. 28
Etiology of Perinatal Asphyxia • Multifactorial, • Antepartum: – Placental Insufficiency. • Intrapartum, and • Postpartum period. 29
Placental Insufficiency • Impaired maternal oxygenation, • Decreased blood flow from the mother to the placenta, • Decreased blood flow from placenta to fetus, • Impaired gas exchange across placenta or fetal tissues, • Increased fetal oxygen requirement. 30
Impaired Maternal Oxygenation • Anemia, • Pulmonary, or • Cardiac, or • Neurologic disease in mother. 31
Decreased Blood Flow from the mother to the placenta • Maternal Infection, • Shock, • Dehydration, and • Hypotension. 32
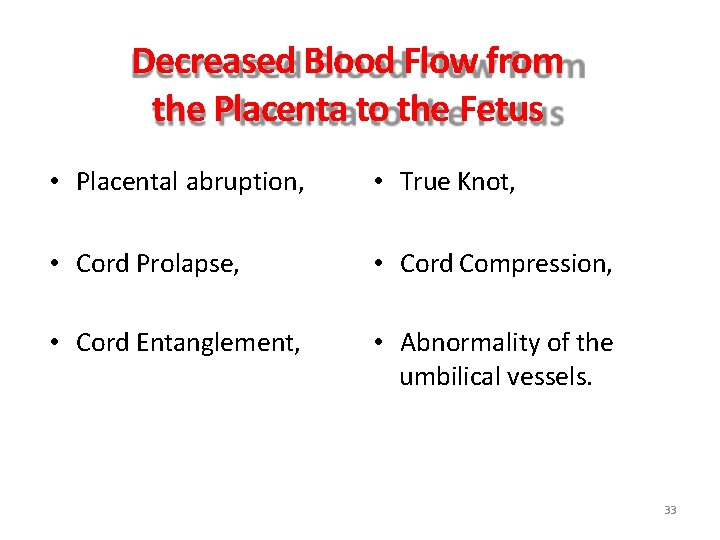
Decreased Blood Flow from the Placenta to the Fetus • Placental abruption, • True Knot, • Cord Prolapse, • Cord Compression, • Cord Entanglement, • Abnormality of the umbilical vessels. 33
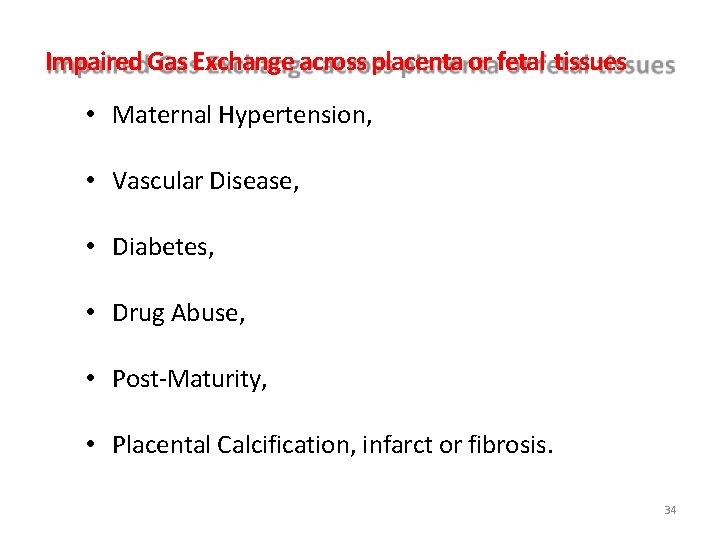
Impaired Gas Exchange across placenta or fetal tissues • Maternal Hypertension, • Vascular Disease, • Diabetes, • Drug Abuse, • Post-Maturity, • Placental Calcification, infarct or fibrosis. 34
Increased Fetal Oxygen Requirement • Fetal Anemia, • Fetal Infection, or • IUGR 35
Causes • Before Birth (Maternal Causes). – Inadequate oxygenation of maternal blood. – Low Maternal Blood Pressure. • At Birth (Fetal or Neonatal Causes). 36
Inadequate Oxygenation of maternal blood • Hypoventilation during anesthesia, • Cyanotic Heart Disease, • Respiratory Failure, • CO Poisoning. 37
Low Maternal BP • Acute Blood Loss, • Spinal Anesthesia, • Great Vessels compression by gravid uterus. • Uterine Tetany (oxytocin induced) 38
Low Maternal BP (continued) • Premature separation of placenta, • Compression of knotting of umbilical cord, • Placental insufficiency due to toxemia or postmaturity. 39
At Births • Failure of oxygenation: – Fetal Cyanotic Congenital Heart Disease, – Severe Pulmonary Distress. • Severe Anemia – Severe Hemorrhage, – Hemolytic Disease. • Shock 40
Shock • Sepsis, • Massive Blood Loss, • Intra-Cranial Hemorrhage, • Adrenal Hemorrhage. 41
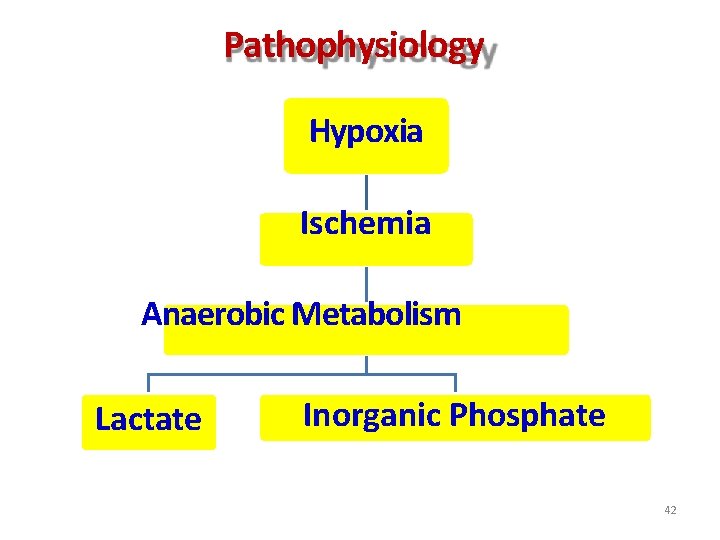
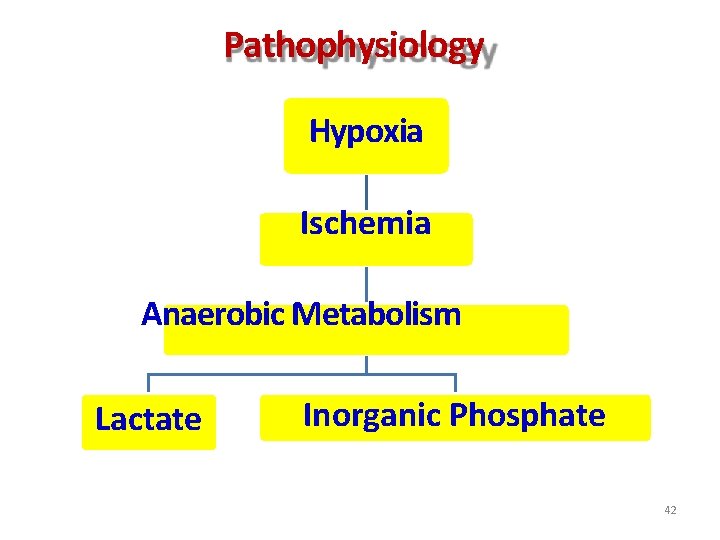
Pathophysiology Hypoxia Ischemia Anaerobic Metabolism Lactate Inorganic Phosphate 42
Vulnerable Organ • Brain, • Neonatal Brain has very high requirements for oxygen and baseline blood flow. • Hypoxic insult to the fetus initiates diving seal reflex. 43

Diving Seal Reflex • Shunting of blood to brain, heart and adrenals and away from lungs, gut, kidneys, liver, spleen and skin, in an attempt to maintain perfusion to more vital organs. 44
Pathophysiology • Accumulation of excitatory and toxic amino acids (glutamate) in the damaged tissue. • Increased production of free radicals and NO in damaged tissue. 45
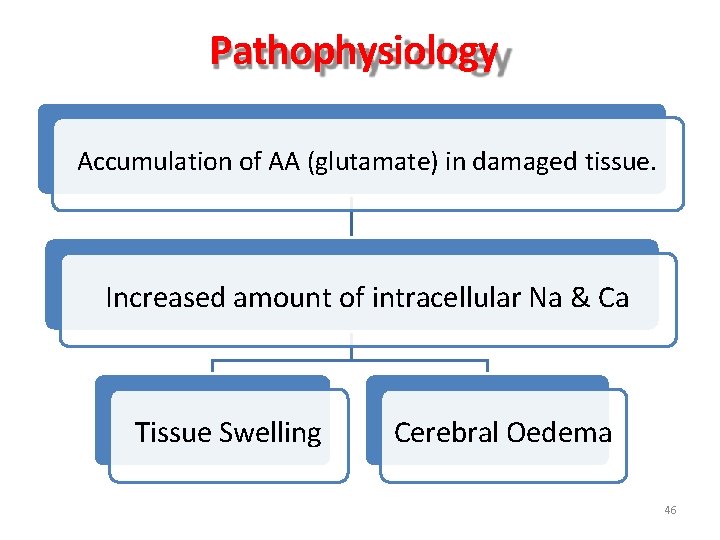
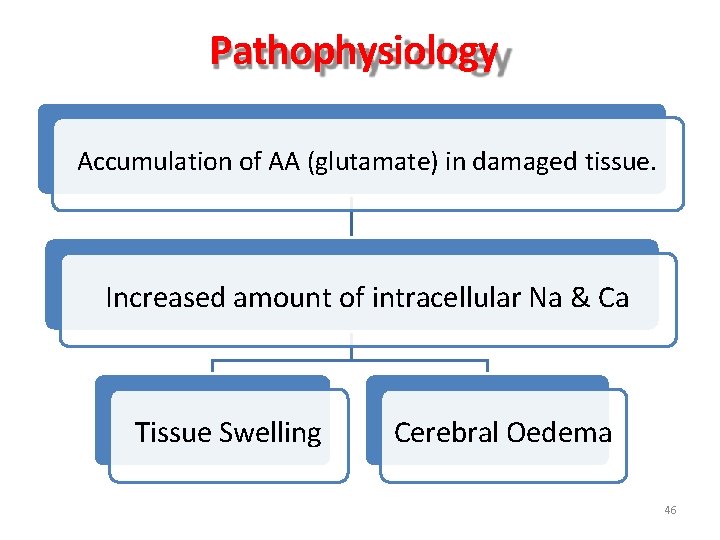
Pathophysiology Accumulation of AA (glutamate) in damaged tissue. Increased amount of intracellular Na & Ca Tissue Swelling Cerebral Oedema 46
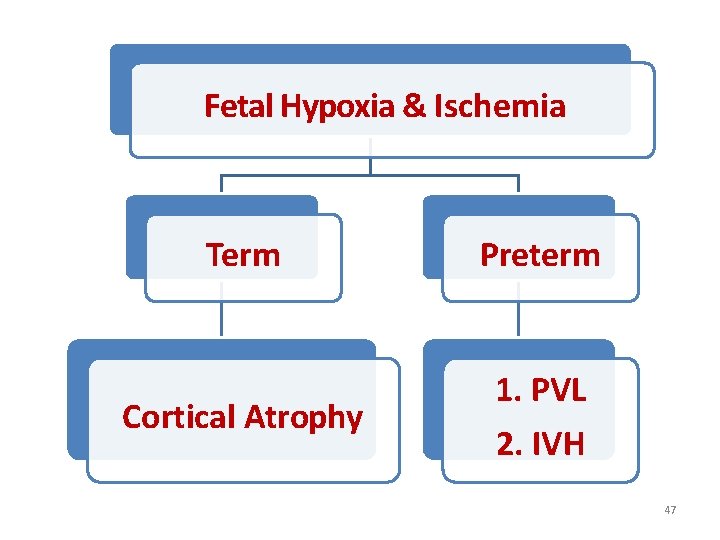
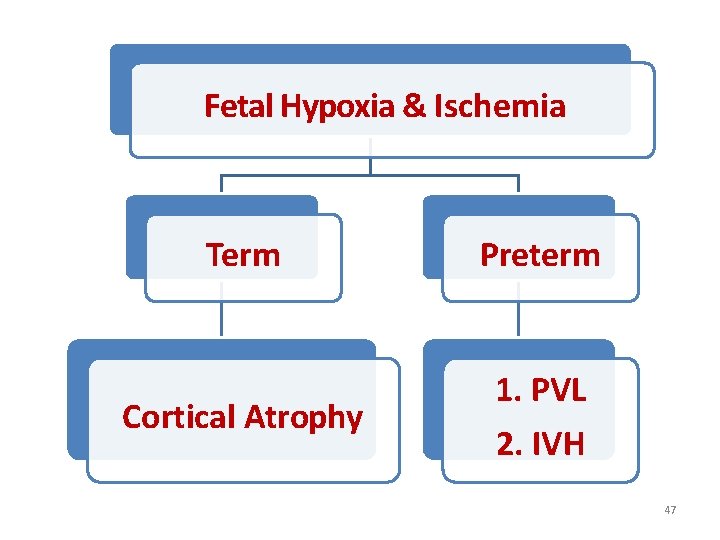
Fetal Hypoxia & Ischemia Term Preterm Cortical Atrophy 1. PVL 2. IVH 47
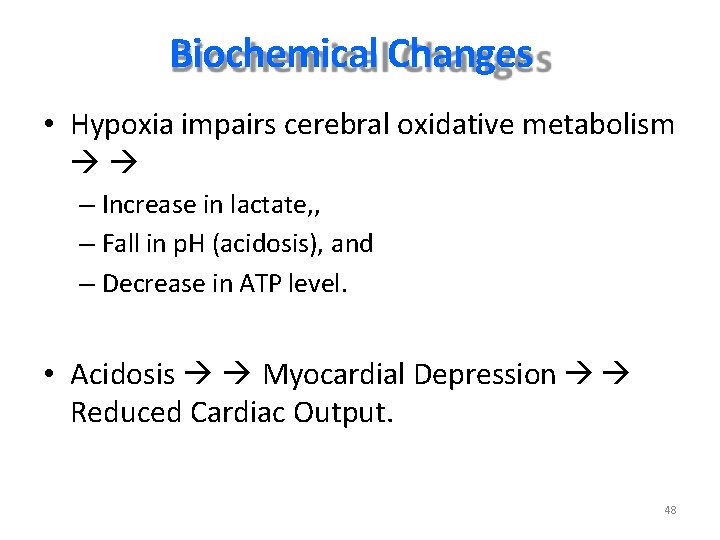
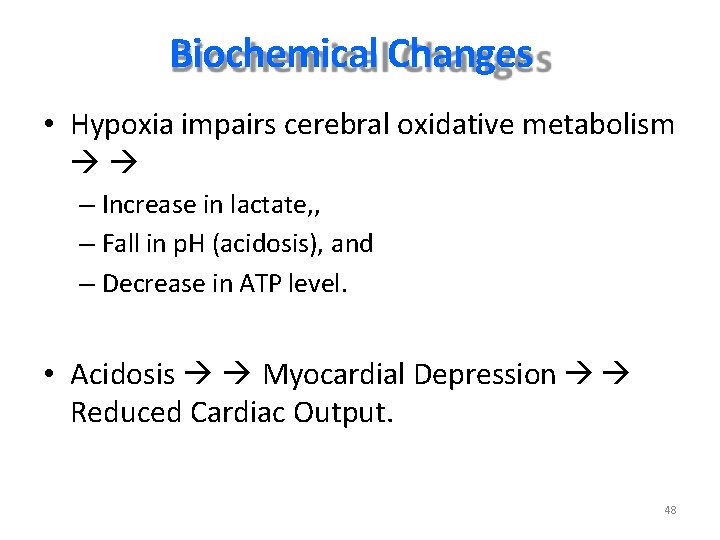
Biochemical Changes • Hypoxia impairs cerebral oxidative metabolism – Increase in lactate, , – Fall in p. H (acidosis), and – Decrease in ATP level. • Acidosis Myocardial Depression Reduced Cardiac Output. 48
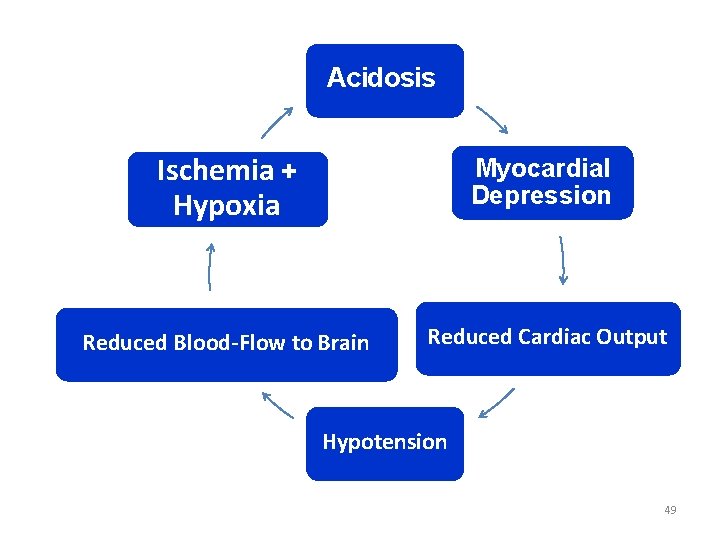
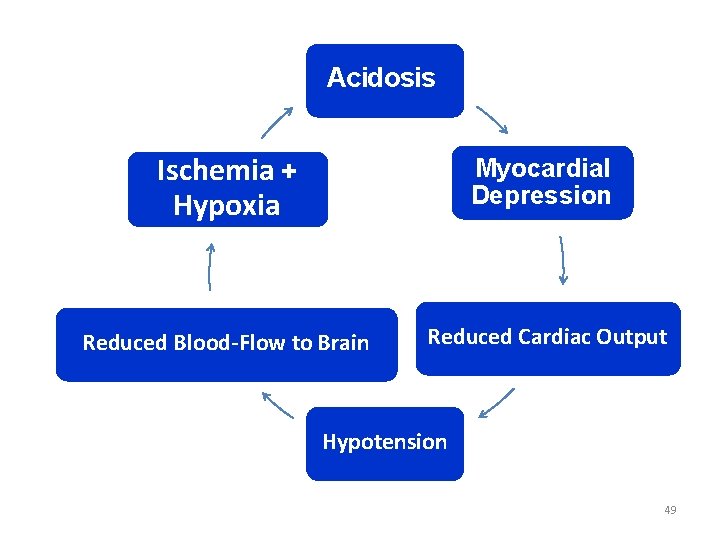
Acidosis Ischemia + Hypoxia Myocardial Depression Reduced Blood-Flow to Brain Reduced Cardiac Output Hypotension 49
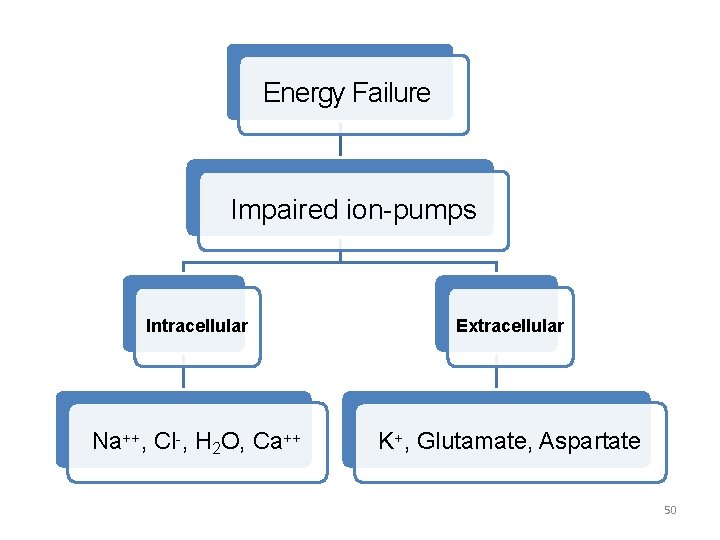
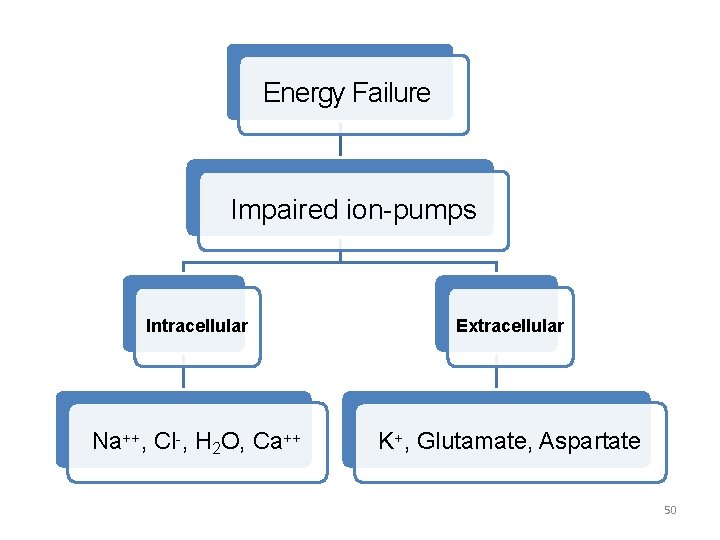
Energy Failure Impaired ion-pumps Intracellular Extracellular Na++, Cl-, H 2 O, Ca++ K+, Glutamate, Aspartate 50
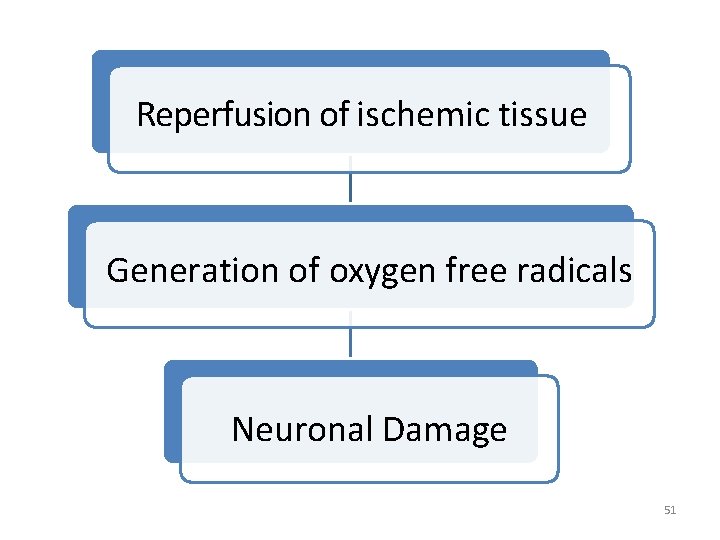
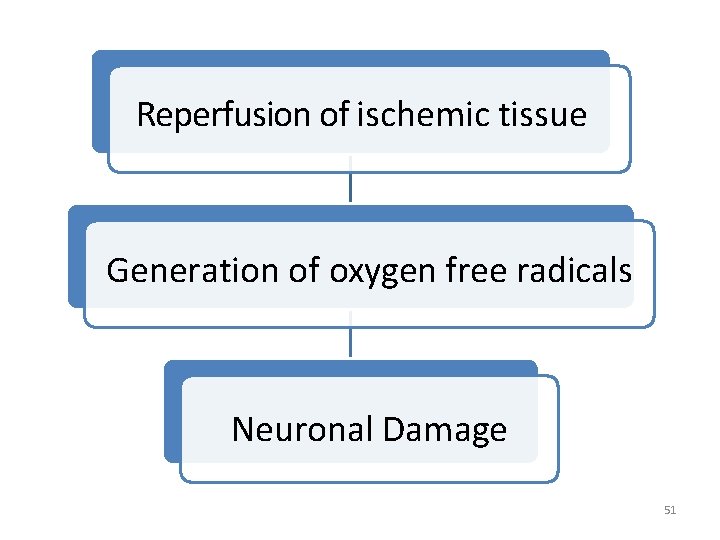
Reperfusion of ischemic tissue Generation of oxygen free radicals Neuronal Damage 51

Brain Damage • Term Newborn: – Cerebral Cortex, and – Basal Ganglia • Preterm Newborn: – Periventricular White Matter. 52
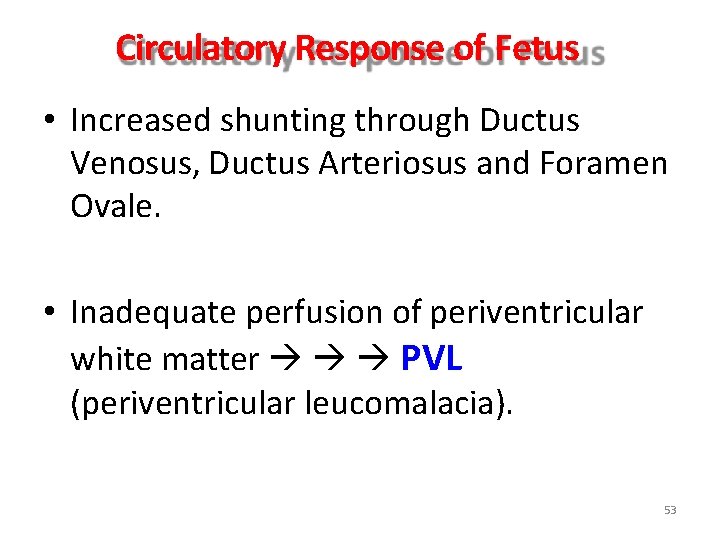
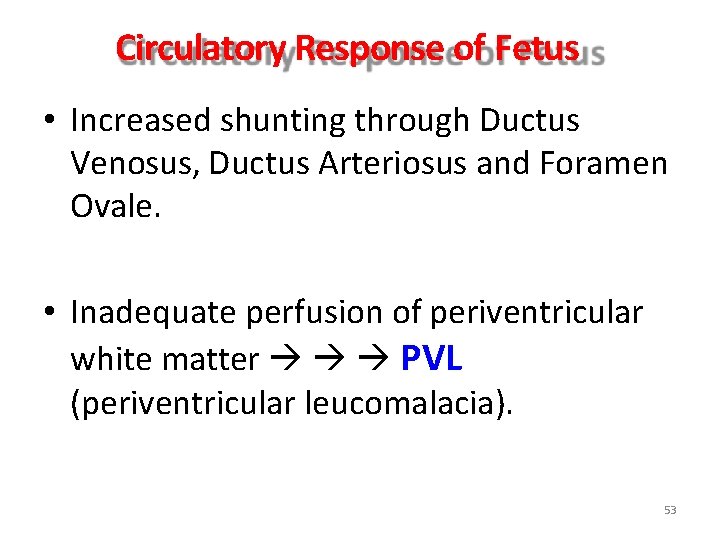
Circulatory Response of Fetus • Increased shunting through Ductus Venosus, Ductus Arteriosus and Foramen Ovale. • Inadequate perfusion of periventricular white matter PVL (periventricular leucomalacia). 53
Causes of Hypotension • Myocardial Dysfunction, • Capillary Leak Syndrome, and • Hypovolemia. 54
Clinical Features 55
Clinical Features • Perinatal Asphyxia (no breathing or difficult breathing at birth). • IUGR, • MSAF (Fetal Distress), Meconium Stained Amniotic Fluid • Hypotonic State. 56
Clinical Features • Mild HIE, • Moderate HIE, and • Severe HIE. 57
Mild HIE • Transient abnormalities, • Poor Feeding, • Irritability, or excessive crying, or sleepiness, • Slightly increased muscle-tone, • Brisk DTR. 58
Moderate HIE • Lethargic, • Significant hypotonia, • Diminished DTR, 59
Moderate HIE (continued) • Sluggish or absent Grasp, Moro and Sucking Reflexes. • Occasional Apnea, • Seizures. 60
Severe HIE • Coma, • Difficult breathing requiring ventilator support, • Decreased Tone, • Depressed DTR, • Absent neonatal reflexes. 61
Severe HIE (continued) • Disturbance of ocular motions, • Loss of “doll’s eye” movement, • Dilated and fixed pupils with poor LR, • Seizures, • Full & bulging AF, 62
Investigations • No confirmatory laboratory tests to diagnose perinatal asphyxia, • Tests are helpful to assess the severity of brain injury and to monitor the functional status of systemic organs. 63
Investigation • Blood Sugar, • Serum Electrolytes, • ABG, • Diffuse mediated MRI, • Sp. O 2 • US in preterm, • CT, • a. EEG 64
Investigations (continued) • Renal Function Tests: – Blood Urea, – Serum Creatinine. • Liver Function Tests, • Coagulation Profile – PT and – PTT. 65

Management 66
Goal of Treatment • Maintain TABC, • Optimize Cardiac Output and Cerebral Perfusion, • Maintain Sp. O 2 • Treat / Prevent Hypoglycemia, 67
Principles of Management • Supportive Therapy, • Anticonvulsants, • Cerebroprotective interventions, and • Monitoring. 68
Supportive Therapy • IV Fluid: – 10% Dextrose, – 60 ml/kg/day. • Treat Hypotension: – Dobutamine, and – Dopamine. • Temperature: – Cool Therapy (33 -340 C) 69
Supportive Therapy (continued) • Glucose: – Treat hypoglycemia, – Maintain BS at 75 to 100 mg/dl. • Calcium: – Calcium level should be kept in the normal range (9 – 11 mg/dl) 70
Anticonvulsants • Control Seizures: – Phenobarbitone: • Loading Dose: 20 mg/kg slowly • Maintenance Dose: 5 mg/kg/day – Phenytoin as a second line drug – Lorazepam • (0. 05 -0. 1 mg/kg/dose I. V. ) for seizures not responding to Phenobarbitone and/or Phenytoin. 71
Cerebroprotective Interventions • Therapeutic Hypothermia (cool therapy), • Free Radical Scavengers, • Antagonists of excitotoxic amino acids, • Calcium Channel Blockers. 72
Caution! • Drugs like mannitol, steroids, and furosemide used in past are no longer recommended. 73
Treatment • Selective Cerebral or Whole Body Therapeutic Hypothermia (Cool Therapy), • Control Seizures, – Phenobarbitone/Phenytoin/Midazolam. • Mechanical Ventilation, (or ECMO), • Volume Expansion, • Pressure Amines. 74
Monitoring • Regular clinical assessment, • Biochemical monitoring, • Sp. O 2. 75
Clinical Assessment • Respiratory Rate, • Temperature, • Heart Rate, • Oxygen Saturation, • CRT, • Urine Output. • BP 76
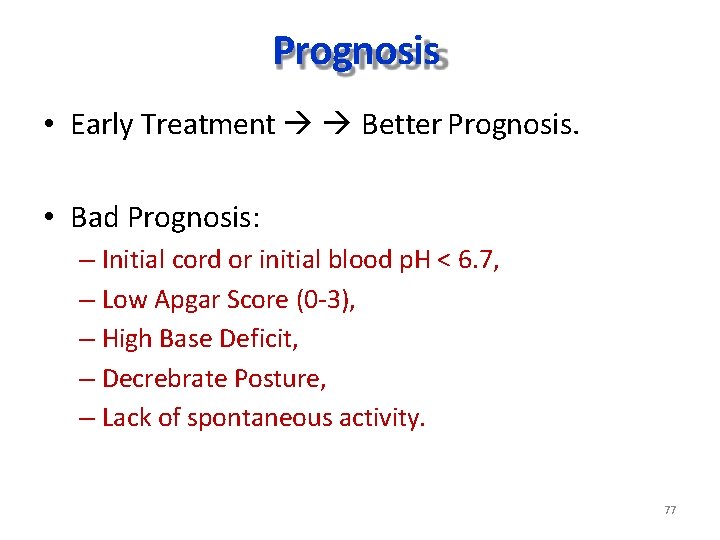
Prognosis • Early Treatment Better Prognosis. • Bad Prognosis: – Initial cord or initial blood p. H < 6. 7, – Low Apgar Score (0 -3), – High Base Deficit, – Decrebrate Posture, – Lack of spontaneous activity. 77
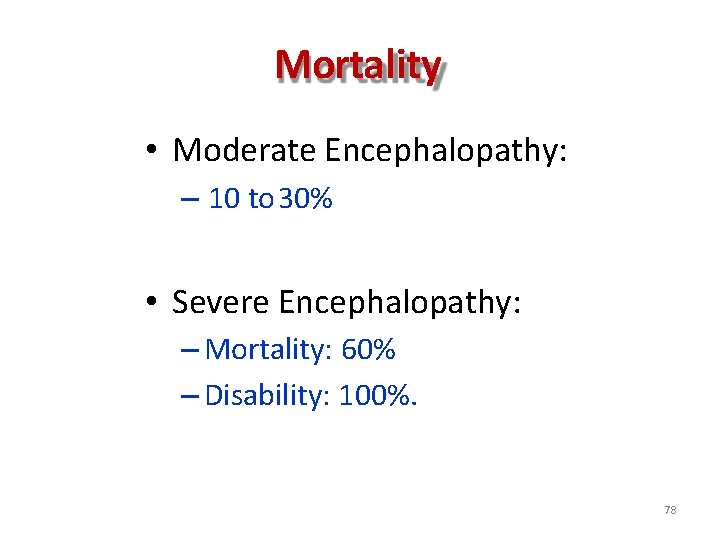
Mortality • Moderate Encephalopathy: – 10 to 30% • Severe Encephalopathy: – Mortality: 60% – Disability: 100%. 78
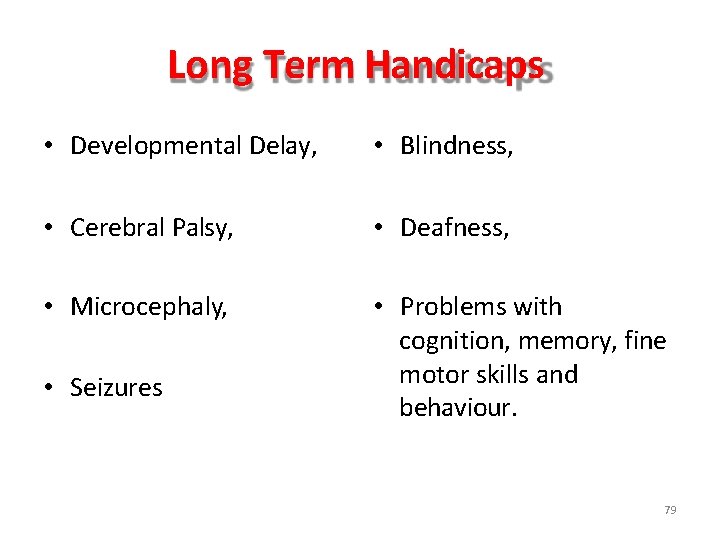
Long Term Handicaps • Developmental Delay, • Blindness, • Cerebral Palsy, • Deafness, • Microcephaly, • Problems with cognition, memory, fine motor skills and behaviour. • Seizures 79
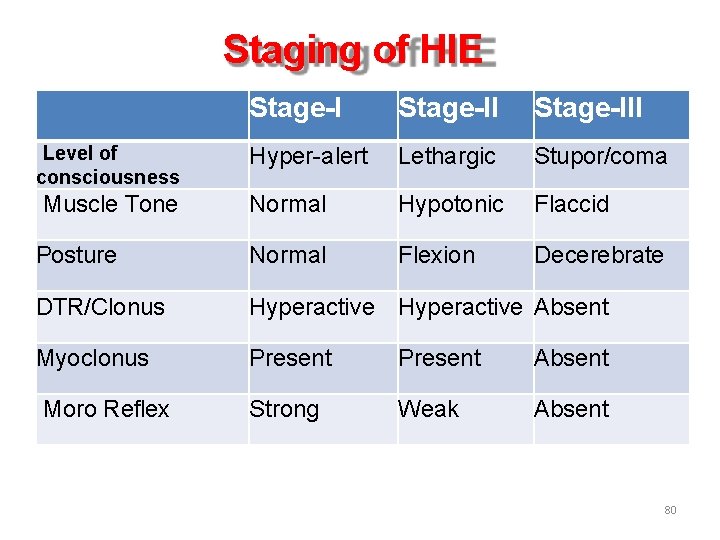
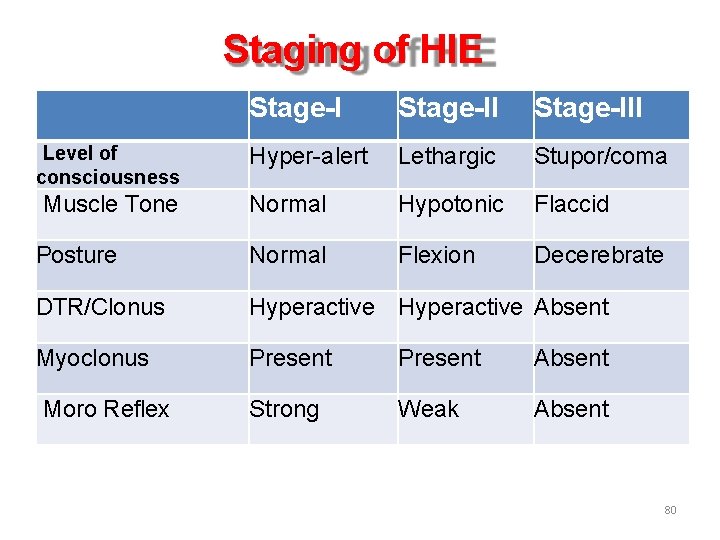
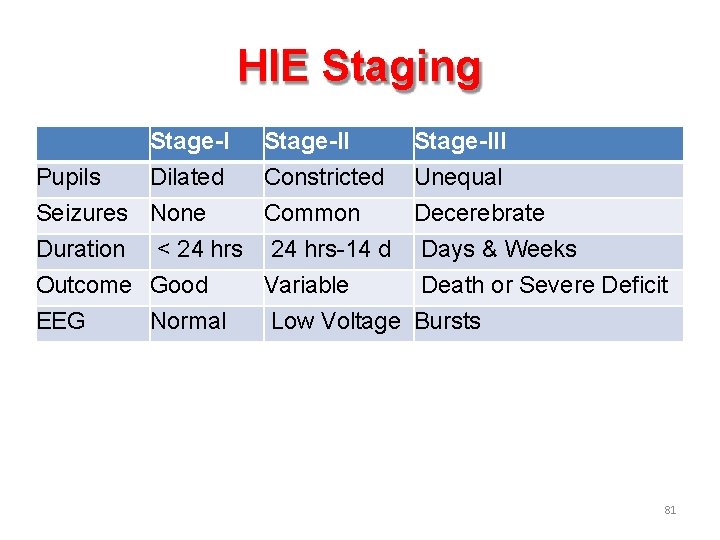
Staging of HIE Stage-III Hyper-alert Lethargic Stupor/coma Muscle Tone Normal Hypotonic Flaccid Posture Normal Flexion Decerebrate DTR/Clonus Hyperactive Absent Myoclonus Present Absent Moro Reflex Strong Weak Absent Level of consciousness 80
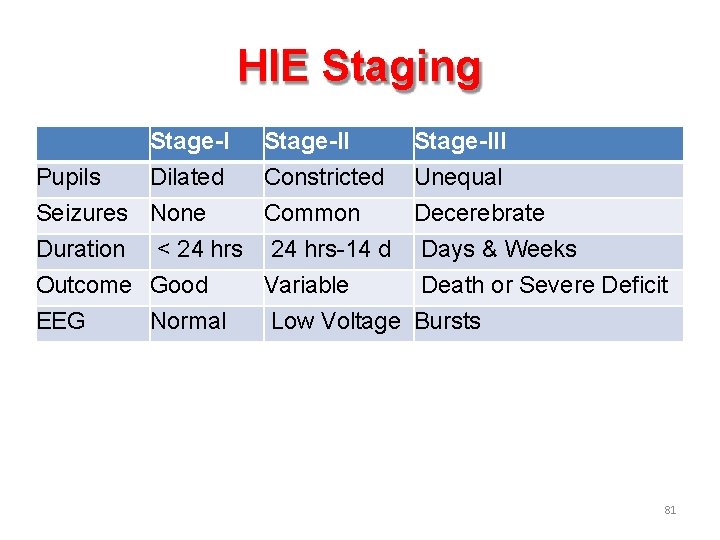
HIE Staging Stage-I Pupils Dilated Seizures None Duration < 24 hrs Outcome Good EEG Normal Stage-II Constricted Common 24 hrs-14 d Variable Low Voltage Stage-III Unequal Decerebrate Days & Weeks Death or Severe Deficit Bursts 81
 Classification of birth asphyxia
Classification of birth asphyxia Perinatal asphyxia
Perinatal asphyxia Perinatal asphyxia
Perinatal asphyxia Hypoxic hypoxia
Hypoxic hypoxia Hypoxic spells
Hypoxic spells Ischemic heart disease
Ischemic heart disease Ischemic bile duct injury
Ischemic bile duct injury Stroke algorithm
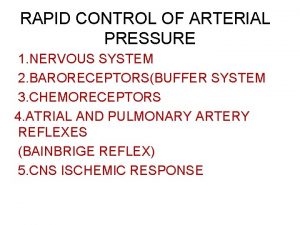
Stroke algorithm Cns ischemic response
Cns ischemic response Ischemic vs hemorrhagic stroke
Ischemic vs hemorrhagic stroke Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Tenecteplase stroke
Tenecteplase stroke Mechanism of ischemic stroke
Mechanism of ischemic stroke Cns ischemic response
Cns ischemic response Ischemic heart disease classification
Ischemic heart disease classification Optic ischemic neuropathy
Optic ischemic neuropathy Haemorrhage
Haemorrhage Cns ischemic response
Cns ischemic response Stages of asphyxia
Stages of asphyxia Silvery spots in asphyxia
Silvery spots in asphyxia Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation Questions on asphyxia
Questions on asphyxia Medical term for suffocation
Medical term for suffocation Hyponuria
Hyponuria Burking asphyxia
Burking asphyxia What does #ll mean when someone dies
What does #ll mean when someone dies Silvery spots in asphyxia
Silvery spots in asphyxia Hepatic encephalopathy symptoms
Hepatic encephalopathy symptoms Ruta materno perinatal
Ruta materno perinatal Bilirubn
Bilirubn Hepatic encephalopathy stages
Hepatic encephalopathy stages Clear perinatal quality
Clear perinatal quality Precipitants of hepatic encephalopathy
Precipitants of hepatic encephalopathy Acute toxic encephalopathy icd 10
Acute toxic encephalopathy icd 10 Fructose intolerance enzyme
Fructose intolerance enzyme Uremic encephalopathy
Uremic encephalopathy Uremic encephalopathy
Uremic encephalopathy Encephalopathy stages
Encephalopathy stages Waiter's tip deformity
Waiter's tip deformity Certain conditions originating in the perinatal period
Certain conditions originating in the perinatal period Encephalopathy stages
Encephalopathy stages Basic perinatal matrices
Basic perinatal matrices Malignant hypertension treatment
Malignant hypertension treatment Standing around crying
Standing around crying Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Hepatic encephalopathy staging
Hepatic encephalopathy staging Hepatic coma diet
Hepatic coma diet Increase bp
Increase bp Hashimoto encephalopathy diagnostic criteria
Hashimoto encephalopathy diagnostic criteria Ccqi perinatal standards
Ccqi perinatal standards Perinatal audit
Perinatal audit Encephalopathy stages
Encephalopathy stages Perinatal
Perinatal Post hepatic jaundice
Post hepatic jaundice Hepatic encephalopathy staging
Hepatic encephalopathy staging Transaminitis definition
Transaminitis definition Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Perinatal mortality rate
Perinatal mortality rate Childs pugh mdcalc
Childs pugh mdcalc South dakota perinatal association
South dakota perinatal association Uyarıcı zenginliği ve yoksunluğu nedir
Uyarıcı zenginliği ve yoksunluğu nedir