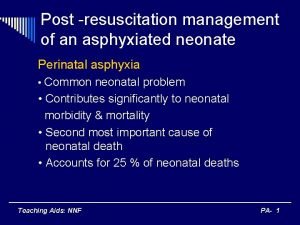
Post resuscitation management of an asphyxiated neonate Perinatal
- Slides: 19
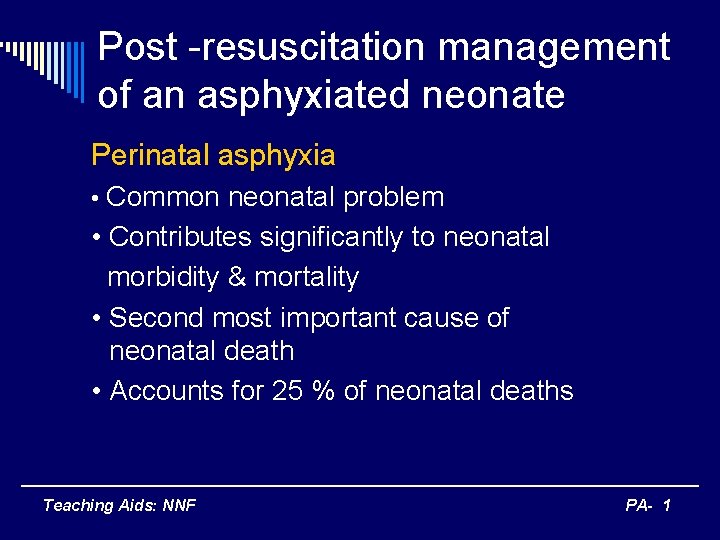
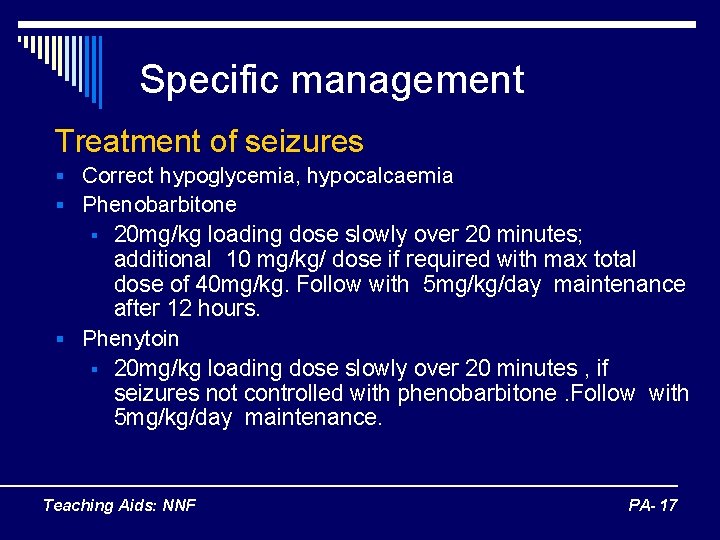
Post -resuscitation management of an asphyxiated neonate Perinatal asphyxia • Common neonatal problem • Contributes significantly to neonatal morbidity & mortality • Second most important cause of neonatal death • Accounts for 25 % of neonatal deaths Teaching Aids: NNF PA- 1
Perinatal asphyxia o Insult to the fetus / newborn n n Lack of oxygen - hypoxia &/or Lack of perfusion – ischemia o Effect of ischemia & hypoxia – inseparable o Both contribute to tissue injury Teaching Aids: NNF PA- 2
Definition of perinatal asphyxia o WHO : n A failure to initiate and sustain breathing at birth. o NNF : n Moderate asphyxia p Slow gasping breathing or an apgar score of 4 -6 at 1 minute of age n Severe asphyxia p No breathing or an apgar score of 0 -3 at 1 minute of age Teaching Aids: NNF PA- 3
Etiology o Intrapartum or ante partum ( 90%) Placental insufficiency o Post partum (10%) n Pulmonary n Cardiac n Teaching Aids: NNF PA- 4
Clinical consequences of perinatal asphyxia Brain ( Hypoxic Ischemic Encephalopathy, HIE ) o Altered sensorium Irritability, lethargy, deeply comatose o Tone disturbances - Hypotonia of proximal girdle muscles (lack of head control & weakness of shoulder muscle in term infants ) Teaching Aids: NNF PA- 5
Clinical consequences of perinatal asphyxia (contd. ) Brain ( Hypoxic Ischemic Encephalopathy, HIE ) o Autonomic disturbances eg. hypotension, increase salivation, abnormal pupillary reflex o Altered neonatal reflexes -Moro’s, sucking , swallowing o Seizures Teaching Aids: NNF PA- 6
Clinical consequences of perinatal asphyxia Heart Myocardial dysfunction resulting in hypotension or congestive cardiac failure Kidney Tubular damage may cause acute renal failure Teaching Aids: NNF PA- 7
Principles of management o Prevent further organ damage Maintain oxygenation, ventilation & perfusion n Correct & maintain normal metabolic & acid base milieu n Prompt management of complications n Teaching Aids: NNF PA- 8
Initial management o Admit in nursery, if -Apgar score <3 at 1 minute -Babies requiring intubation, chest compressions or medications o Nurse in thermo-neutral temperature to maintain skin o o temperature at 36. 5 o. C Secure IV line , fluids 2/3 rd of maintenance Fluid bolus if CRT > 3 secs or blood pressure low Inj vit k Stomach wash Teaching Aids: NNF PA- 9
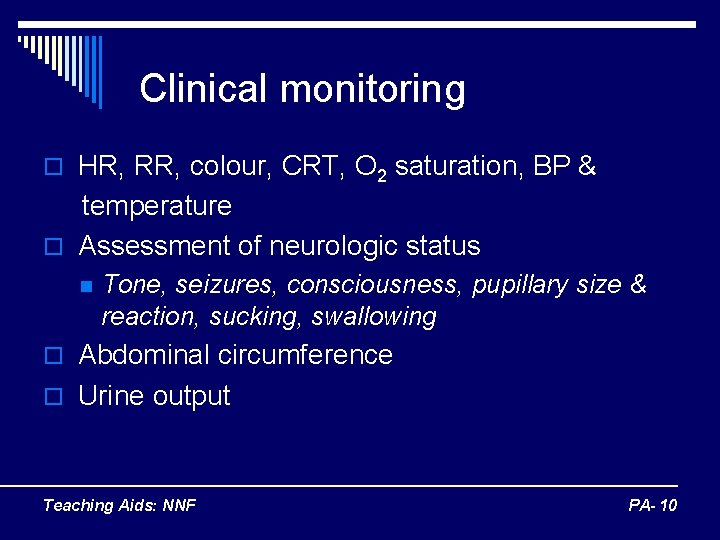
Clinical monitoring o HR, RR, colour, CRT, O 2 saturation, BP & temperature o Assessment of neurologic status n Tone, seizures, consciousness, pupillary size & reaction, sucking, swallowing o Abdominal circumference o Urine output Teaching Aids: NNF PA- 10
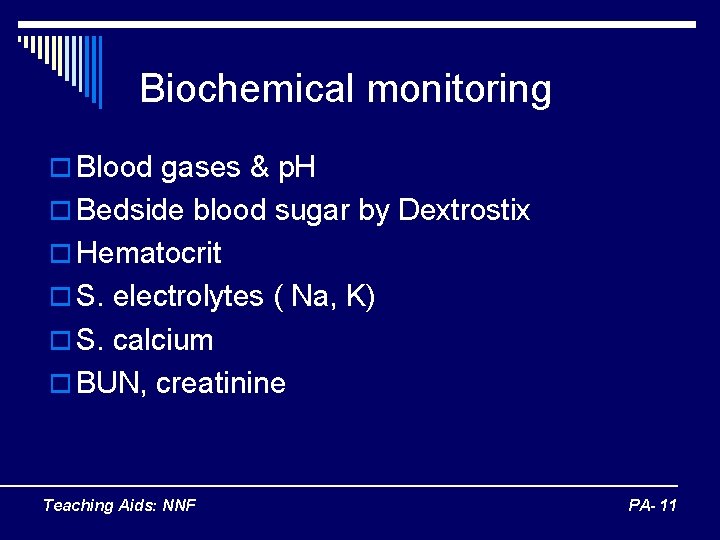
Biochemical monitoring o Blood gases & p. H o Bedside blood sugar by Dextrostix o Hematocrit o S. electrolytes ( Na, K) o S. calcium o BUN, creatinine Teaching Aids: NNF PA- 11
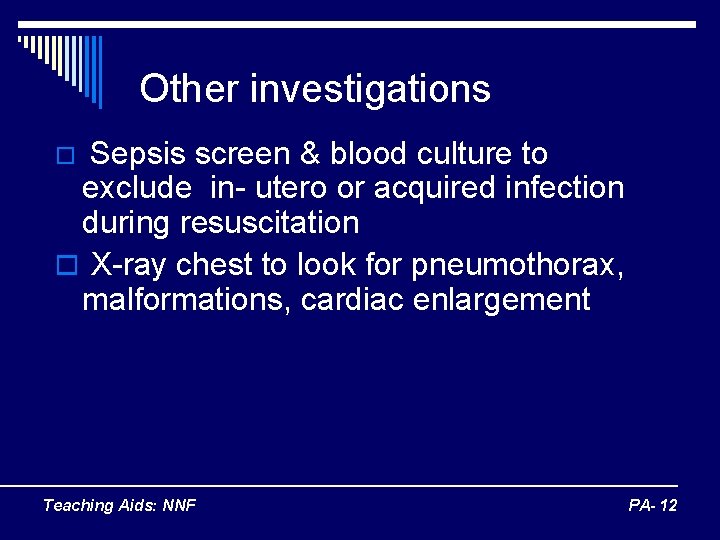
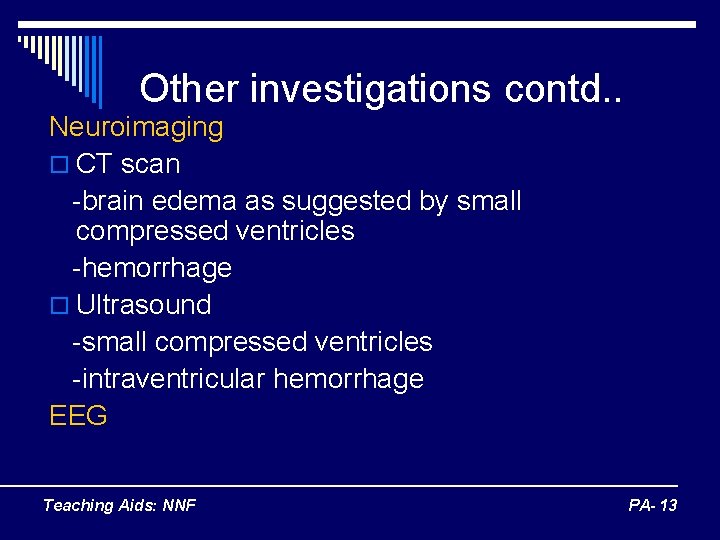
Other investigations Sepsis screen & blood culture to exclude in- utero or acquired infection during resuscitation o X-ray chest to look for pneumothorax, malformations, cardiac enlargement o Teaching Aids: NNF PA- 12
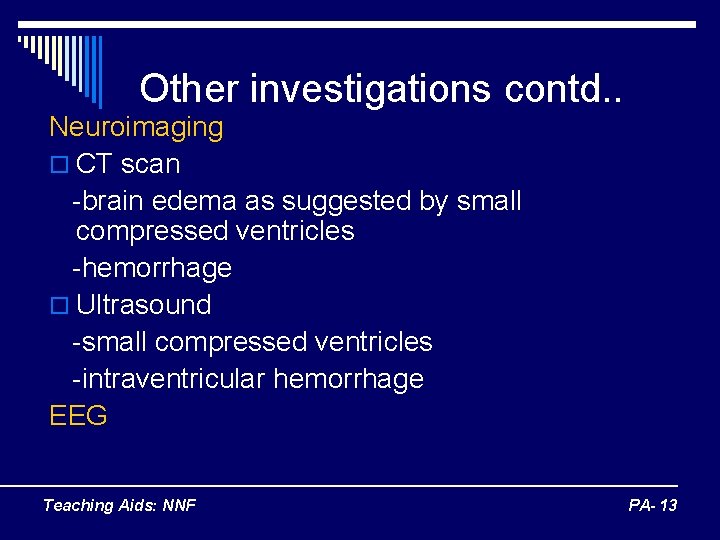
Other investigations contd. . Neuroimaging o CT scan -brain edema as suggested by small compressed ventricles -hemorrhage o Ultrasound -small compressed ventricles -intraventricular hemorrhage EEG Teaching Aids: NNF PA- 13
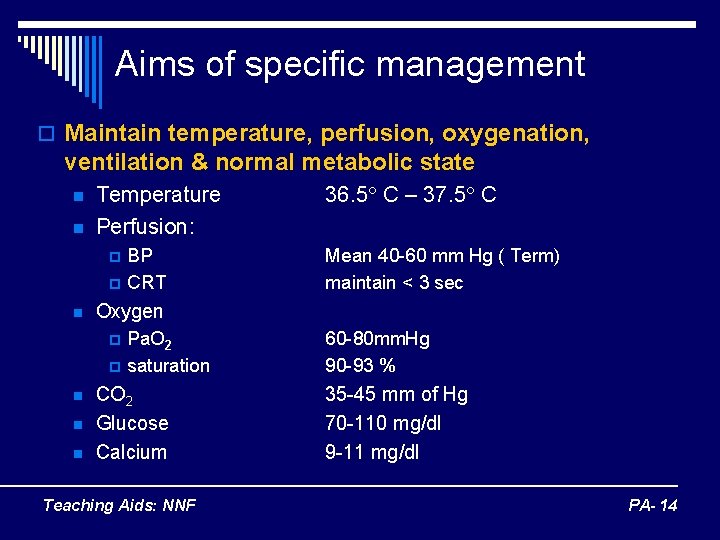
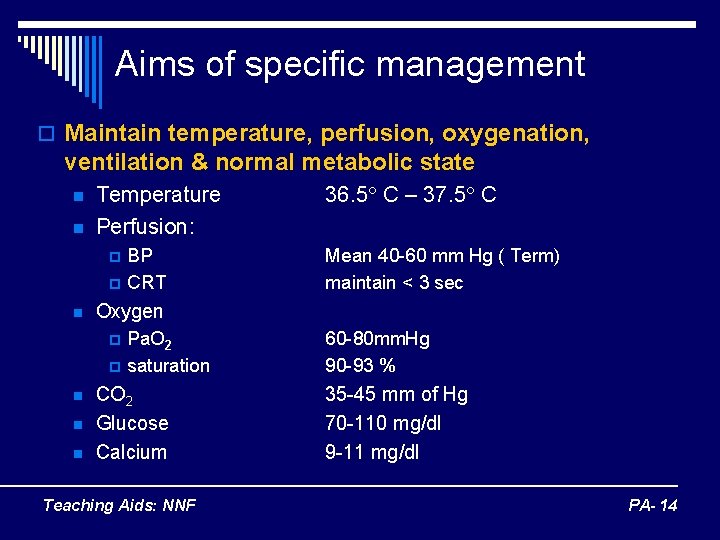
Aims of specific management o Maintain temperature, perfusion, oxygenation, ventilation & normal metabolic state n n Temperature Perfusion: p p n n Mean 40 -60 mm Hg ( Term) maintain < 3 sec Oxygen p n BP CRT 36. 5 C – 37. 5 C Pa. O 2 saturation CO 2 Glucose Calcium Teaching Aids: NNF 60 -80 mm. Hg 90 -93 % 35 -45 mm of Hg 70 -110 mg/dl 9 -11 mg/dl PA- 14
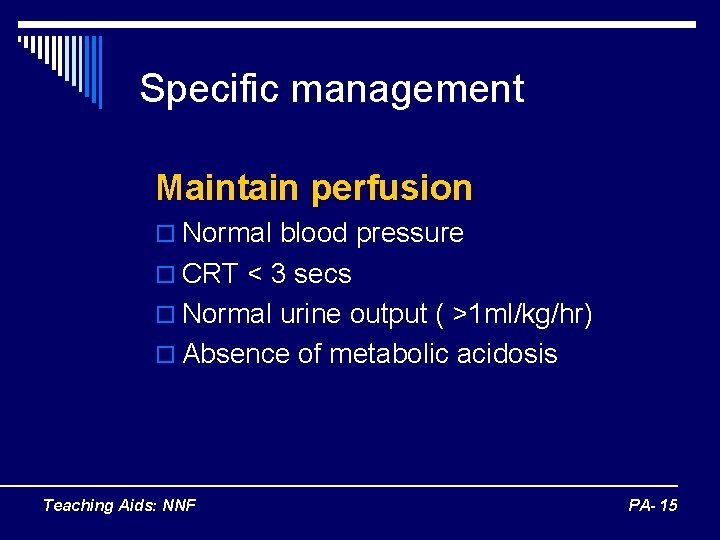
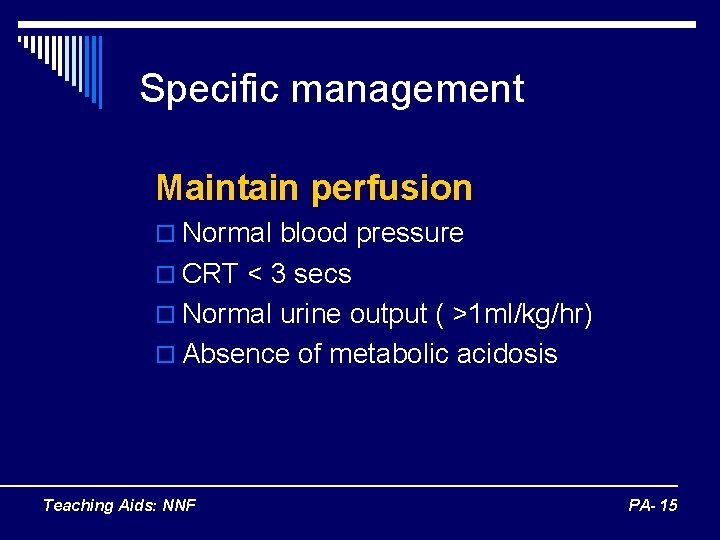
Specific management Maintain perfusion o Normal blood pressure o CRT < 3 secs o Normal urine output ( >1 ml/kg/hr) o Absence of metabolic acidosis Teaching Aids: NNF PA- 15
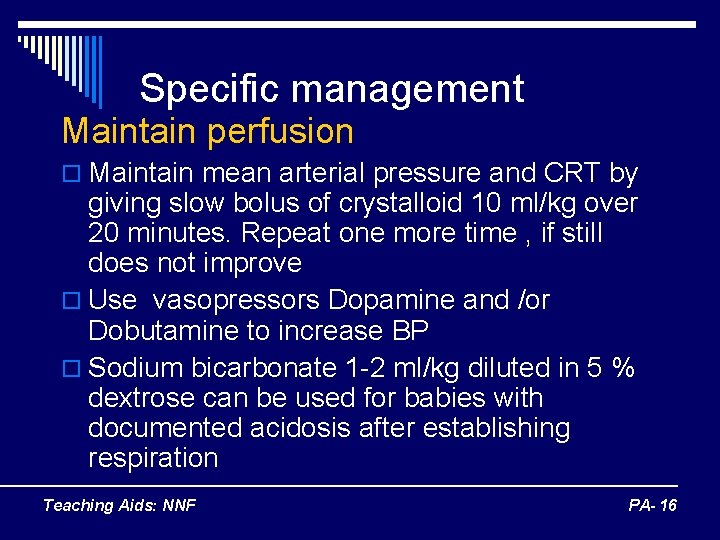
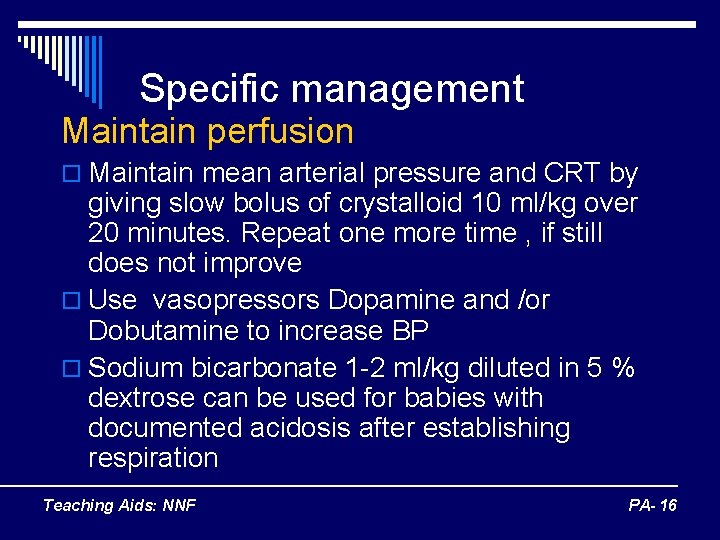
Specific management Maintain perfusion o Maintain mean arterial pressure and CRT by giving slow bolus of crystalloid 10 ml/kg over 20 minutes. Repeat one more time , if still does not improve o Use vasopressors Dopamine and /or Dobutamine to increase BP o Sodium bicarbonate 1 -2 ml/kg diluted in 5 % dextrose can be used for babies with documented acidosis after establishing respiration Teaching Aids: NNF PA- 16
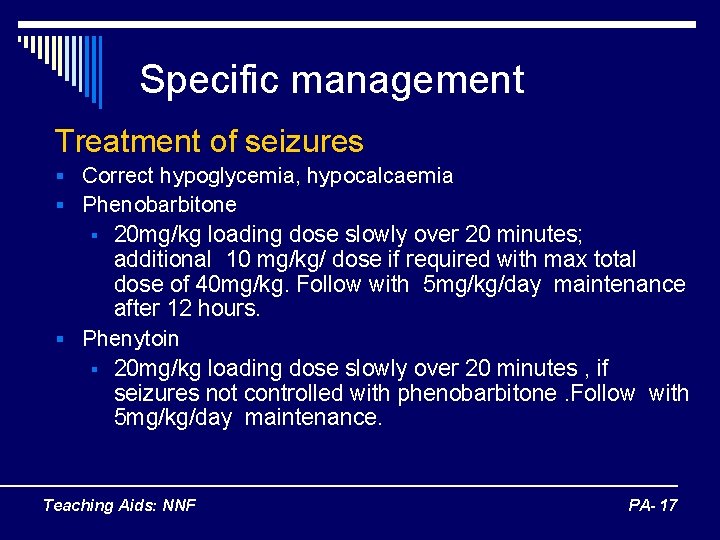
Specific management Treatment of seizures § Correct hypoglycemia, hypocalcaemia § Phenobarbitone 20 mg/kg loading dose slowly over 20 minutes; additional 10 mg/kg/ dose if required with max total dose of 40 mg/kg. Follow with 5 mg/kg/day maintenance after 12 hours. § Phenytoin § 20 mg/kg loading dose slowly over 20 minutes , if seizures not controlled with phenobarbitone. Follow with 5 mg/kg/day maintenance. § Teaching Aids: NNF PA- 17
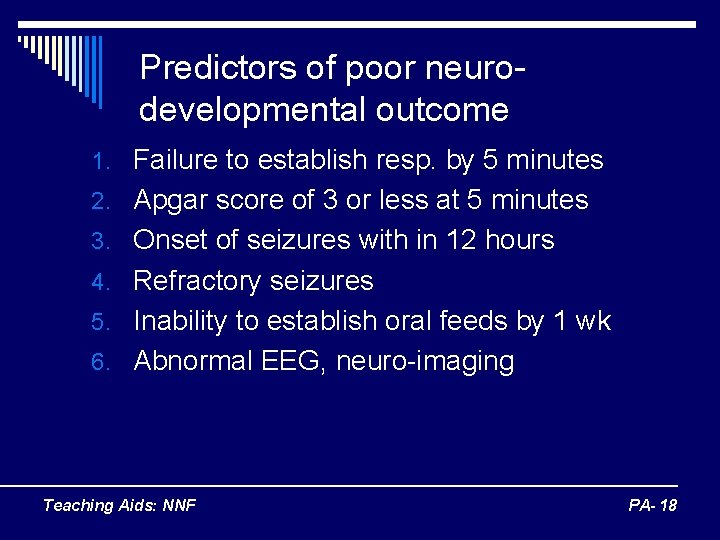
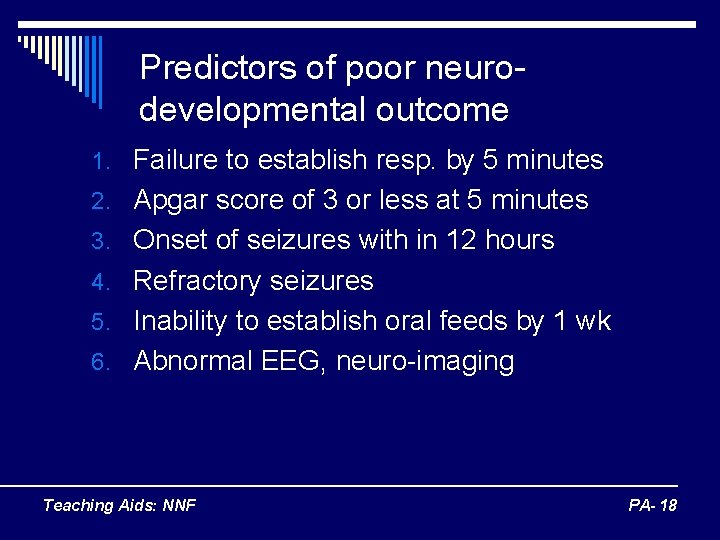
Predictors of poor neurodevelopmental outcome 1. Failure to establish resp. by 5 minutes 2. Apgar score of 3 or less at 5 minutes 3. Onset of seizures with in 12 hours 4. Refractory seizures 5. Inability to establish oral feeds by 1 wk 6. Abnormal EEG, neuro-imaging Teaching Aids: NNF PA- 18
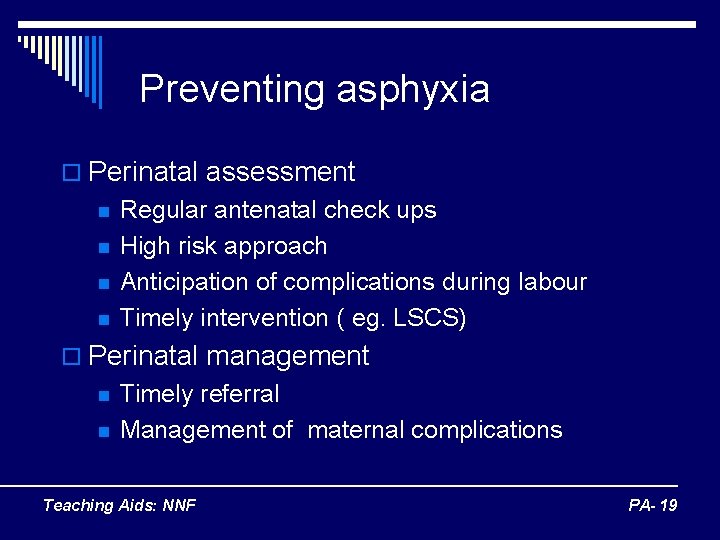
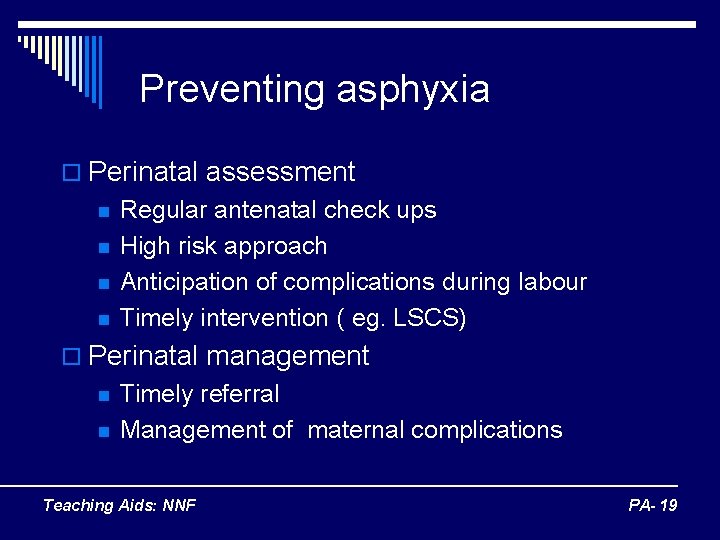
Preventing asphyxia o Perinatal assessment n n Regular antenatal check ups High risk approach Anticipation of complications during labour Timely intervention ( eg. LSCS) o Perinatal management n n Timely referral Management of maternal complications Teaching Aids: NNF PA- 19
 Neonatal resuscitation definition
Neonatal resuscitation definition Definition of high risk neonates
Definition of high risk neonates Petechiae neonate
Petechiae neonate Neonate skull
Neonate skull Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation Difference between resuscitation and resurrection
Difference between resuscitation and resurrection Srfac singapore
Srfac singapore Acute resuscitation plan form
Acute resuscitation plan form Site:slidetodoc.com
Site:slidetodoc.com Resuscitation of newborn procedure
Resuscitation of newborn procedure Amber care
Amber care Endpoint of resuscitation
Endpoint of resuscitation Pediatric color code
Pediatric color code Principle of resuscitation
Principle of resuscitation European resuscitation council
European resuscitation council Resuscitation cpr
Resuscitation cpr European resuscitation council
European resuscitation council Bls
Bls 17:6 providing first aid for burns
17:6 providing first aid for burns Cpr meaning medical
Cpr meaning medical