Paediatric Acute Resuscitation Plan Form Practicalities and sensitivities









- Slides: 58
Paediatric Acute Resuscitation Plan Form Practicalities and sensitivities around discussing resuscitation at the end of life: a clinical tool Dr Anthony Herbert Staff Specialist Paediatric Palliative Care Service Royal Children’s Hospital
PARP Implementation • • Case Study Background Components of the tool Summary w Overvie
Case Study • 7 year old boy • Lives in inner suburbs of Brisbane • Undiagnosed neurodegenerative condition – associated central hypotonia, macrocephaly and mild hydrocephalus • Long term prognosis felt to be guarded
Case Study • • PEG fed – no oral intake due to poor swallow Not mobile – uses specialised wheelchair Seizure disorder Recurrent severe lower respiratory tract infection related to aspiration and viral infections • Secretions problematic – suction machine at home
Case Study • Both parents are professionals • Younger brother aged 2 ½ years • Ongoing allied health input from a non government organisation at home (Physiotherapy and Speech Pathology)
Case Study • Severe LRTI in July 2010 • Family elected to continue standard paediatric cares after admission to hospital (e. g. Intravenous fluids and antibiotics, oxygen) • Parents open to limitations of invasive interventions such as intubation, ventilation or chest compressions; assumed also not for PICU • Parents were receptive to this discussion and were keen to be guided by health professionals, particularly their paediatrician • Discussion typed up by resident and filed in notes
Case Study • Further severe chest infection June 2011 – Difficulty locating typed summary of previous discussion in notes in the emergency department • Standard cares on ward but approximately 10 Litres / min oxygen required to maintain saturations and there was presence of increased work of breathing with associated fatigue

Case Study • Role of high flow oxygen discussed with family: non-invasive, could provide sufficient support to allow her to get through this inter-current illness, and may provide comfort • Patient still able to go to PICU even though not for CPR; went to PICU for 48 hours of high flow oxygen and returned to ward • Ultimately discharged home again
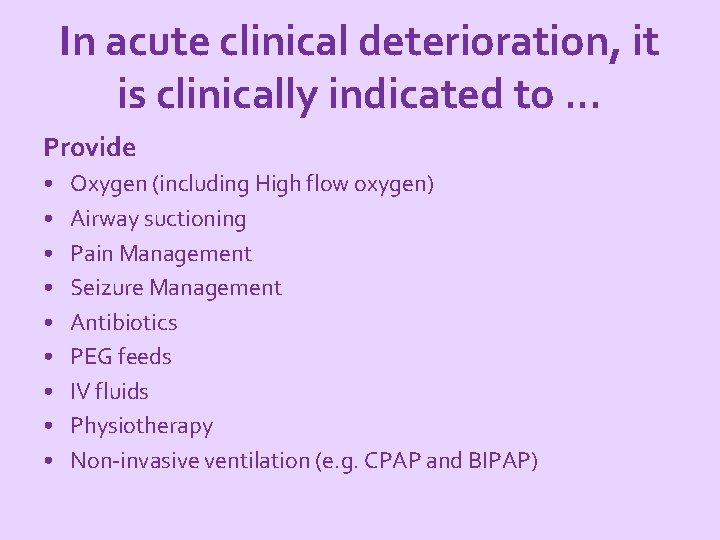
In acute clinical deterioration, it is clinically indicated to. . . Provide • • • Oxygen (including High flow oxygen) Airway suctioning Pain Management Seizure Management Antibiotics PEG feeds IV fluids Physiotherapy Non-invasive ventilation (e. g. CPAP and BIPAP)
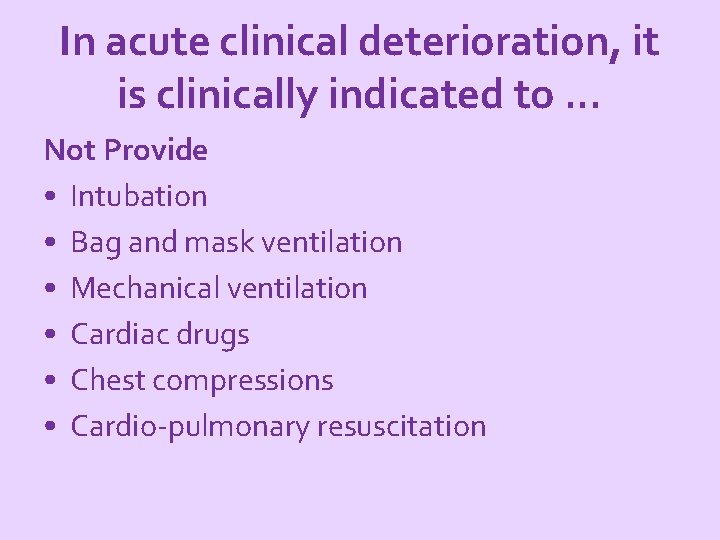
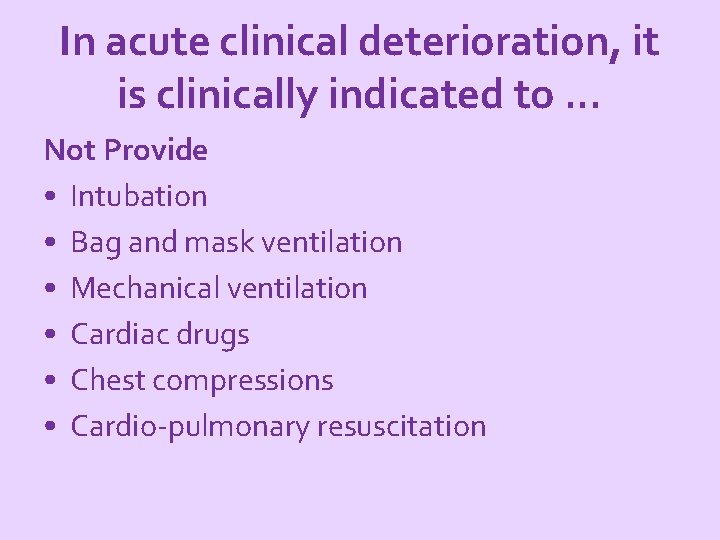
In acute clinical deterioration, it is clinically indicated to. . . Not Provide • Intubation • Bag and mask ventilation • Mechanical ventilation • Cardiac drugs • Chest compressions • Cardio-pulmonary resuscitation
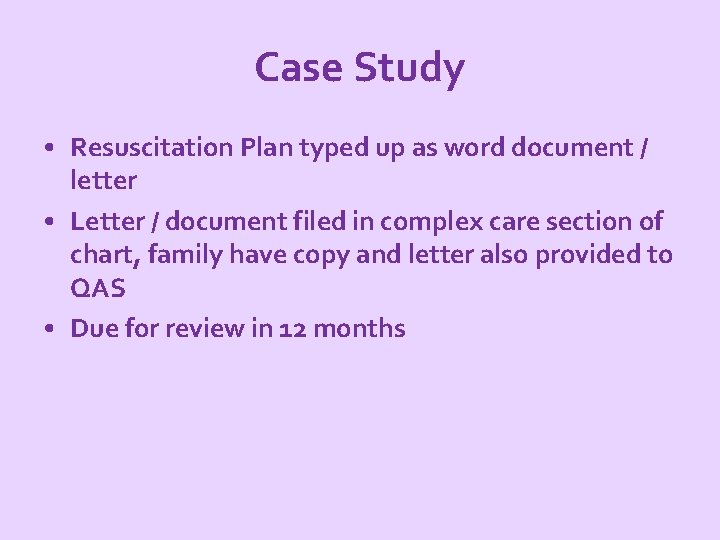
Case Study • Resuscitation Plan typed up as word document / letter • Letter / document filed in complex care section of chart, family have copy and letter also provided to QAS • Due for review in 12 months
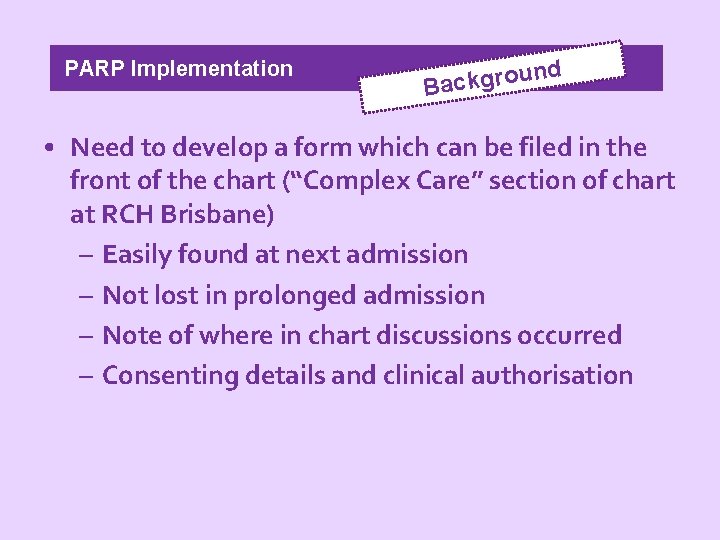
PARP Implementation d un Backgro • Need to develop a form which can be filed in the front of the chart (“Complex Care” section of chart at RCH Brisbane) – Easily found at next admission – Not lost in prolonged admission – Note of where in chart discussions occurred – Consenting details and clinical authorisation

PARP Implementation d un Backgro • Development of an adult “Acute Resuscitation Plan form” —Coronial inquests —End-of-Life Decision-Making Project —Need for state-wide consistency • Development of similar forms in other children’s hospitals around Australia • Need to demonstrate adolescent involvement in discussion
PARP Implementation Quote • “agreement on uniform standards of practice and documentation across public and private hospitals can only improve the quality of care for patients facing their likely demise. This would also help families understand treatment decisions. ” - Christine Clements, Deputy State Coroner
nd u Background o r g k c Ba PARP Implementation • Importance of language e. g. use of the term “Acute Resuscitation Plan” rather than “DNR” • Process to be followed if parents are to agree to a resuscitation plan for their child is complex and often requires time • Needs trust and acceptance in the clinicians by the parents / young person
PARP Version 1 Adults (34 versions)
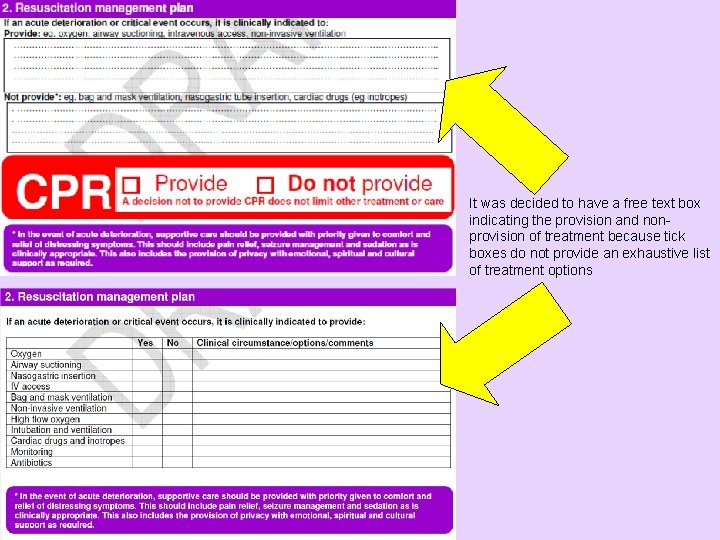
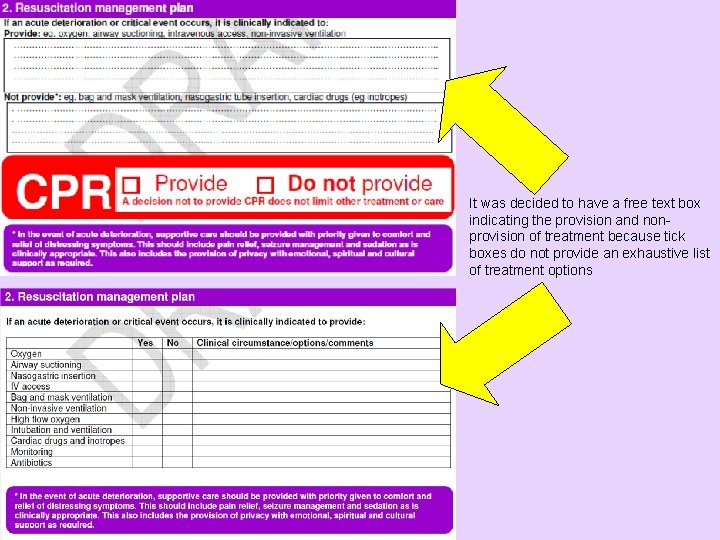
It was decided to have a free text box indicating the provision and nonprovision of treatment because tick boxes do not provide an exhaustive list of treatment options

PARP Welcome to version 14! Adults (34 versions)
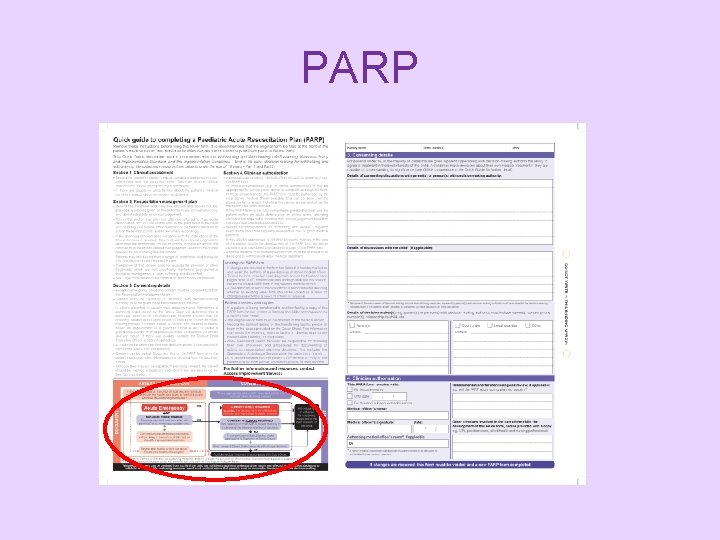
PARP
PARP Implementation ? RP A P e h t What is • a new form to document decisions to limit life-sustaining measures in children and young people. • filed at the front of the chart • replaces NFR or DNR orders • completed by a medical officer
PARP Implementation RP A P e h t d oul h s n e h W ? d e t e l p m be co ? • when a senior clinician considers there’s a risk of a cardiac or respiratory arrest where resuscitation may not be appropriate • a decision not to perform CPR does not limit the patient’s other treatment
PARP Implementation e w e v a h Why rm? o f e h t ed p o l e v e d Ensure that: • documentation is readily available if patient arrests • dying children and young people receive appropriate care and treatment for comfort and dignity • resuscitation is not commenced or continued when clinically inappropriate
ARP Implementation Quote If I am suffering from a treatable condition in which it is likely that a relatively short period of medical treatment will restore me to my present health and mental functioning, then I would like to receive such treatment. However, I would not wish my life to be artificially prolonged if thereby I am left in a terminal or vegetative state. . . Rev John Stott
PARP Implementation ed a e n e w Why do tric a i d e a p separate ent? docum • Legal – Guardianship law does not apply to children and young people aged less than 18 years • Role of the adolescent and young person in making decisions • Role of the Department of Child Safety in making decisions in some cases • Unique ethical aspects associated with decision making in children

n e e b s a Who h in d e v l o v in ? m r o f e h gt n i p o l e v de Who’s been involved PARP Implementation • Clinical Policy Unit • Palliative Care Working group (under auspices of the Child and Youth Network) • Presented at 2 Child and Youth Network Forums in 2010 and 2011 • Parents • Legal advice • Queensland Ambulance Service
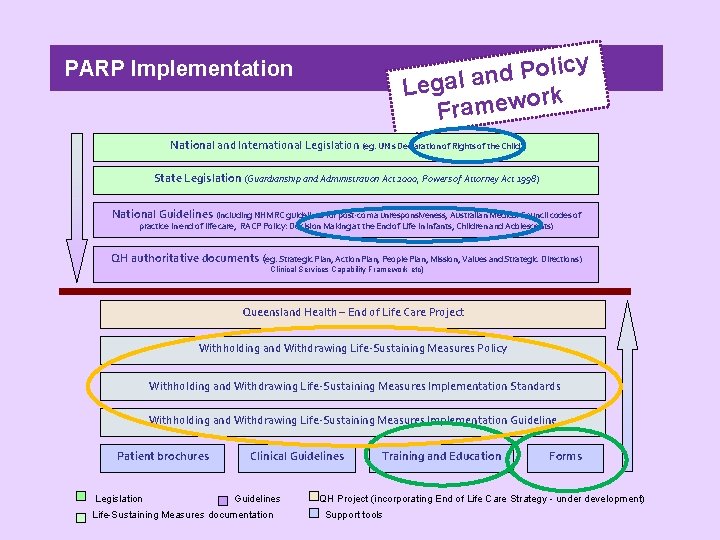
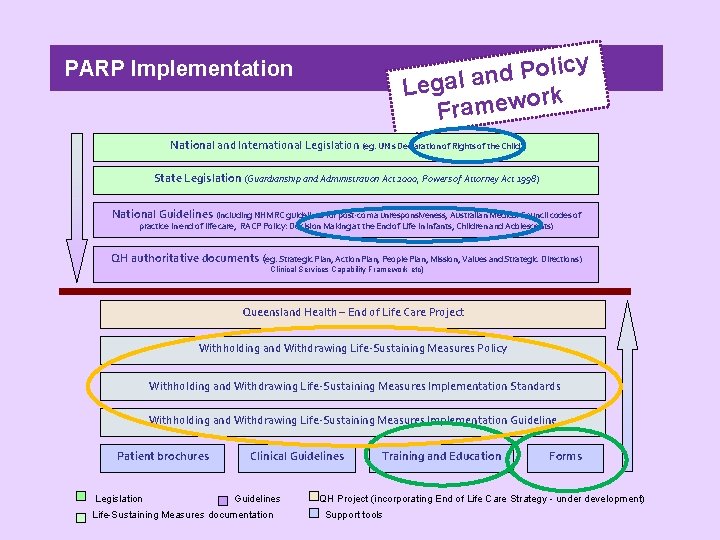
y c i l o P d Legal an ork Framew PARP Implementation National and International Legislation (eg. UN’s Declaration of Rights of the Child) State Legislation (Guardianship and Administration Act 2000, Powers of Attorney Act 1998) National Guidelines (including NHMRC guidelines for post-coma unresponsiveness, Australian Medical Council codes of practice in end of life care, RACP Policy: Decision Making at the End of Life in Infants, Children and Adolescents) QH authoritative documents (eg. Strategic Plan, Action Plan, People Plan, Mission, Values and Strategic Directions) Clinical Services Capability Framework etc) Queensland Health – End of Life Care Project Withholding and Withdrawing Life-Sustaining Measures Policy Withholding and Withdrawing Life-Sustaining Measures Implementation Standards Withholding and Withdrawing Life-Sustaining Measures Implementation Guideline Patient brochures Legislation Clinical Guidelines Life-Sustaining Measures documentation Training and Education Forms QH Project (incorporating End of Life Care Strategy - under development) Support tools
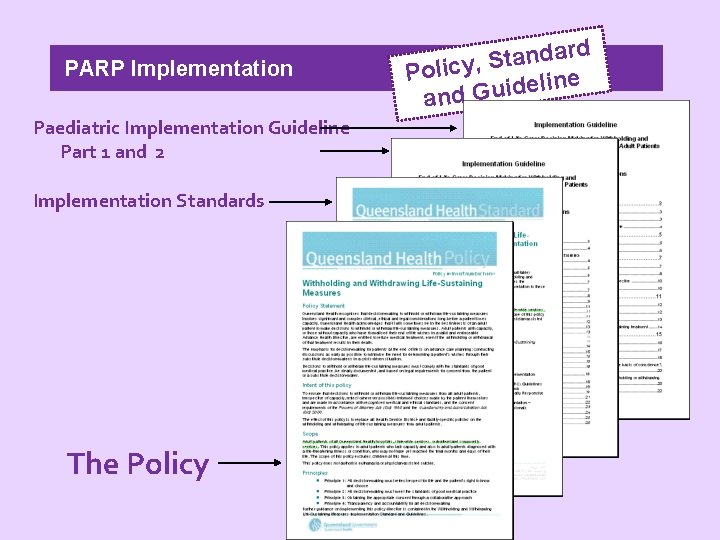
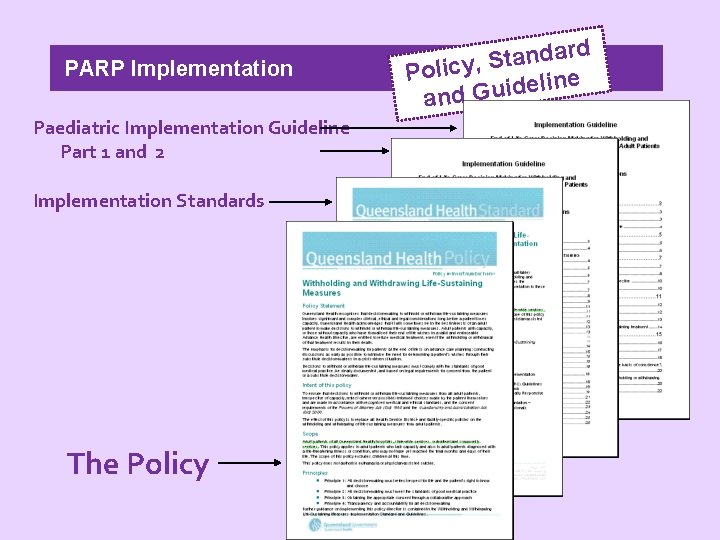
PARP Implementation Paediatric Implementation Guideline Part 1 and 2 Implementation Standards The Policy ard d n a t S , Policy e n i l e d i u and G
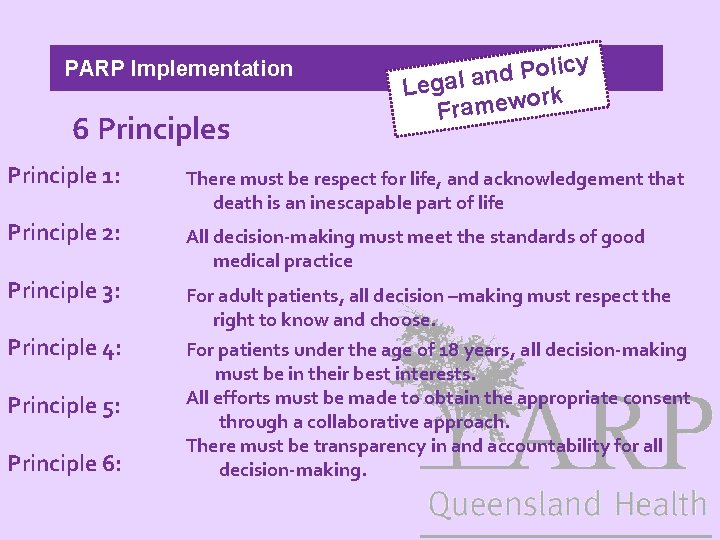
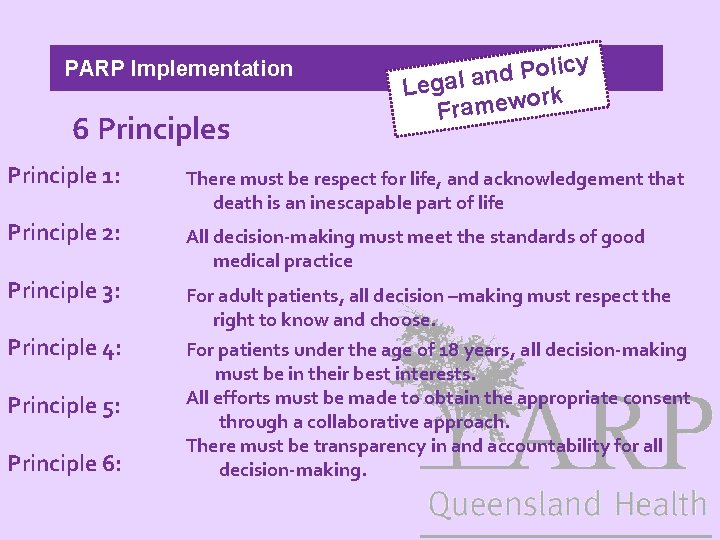
PARP Implementation 6 Principles y c i l o P d Legal an ork Framew Principle 1: There must be respect for life, and acknowledgement that death is an inescapable part of life Principle 2: All decision-making must meet the standards of good medical practice Principle 3: For adult patients, all decision –making must respect the right to know and choose. For patients under the age of 18 years, all decision-making must be in their best interests. All efforts must be made to obtain the appropriate consent through a collaborative approach. There must be transparency in and accountability for all decision-making. Principle 4: Principle 5: Principle 6:
PARP Implementation 1. Clinical Assessment f th o s t n e n Compo Form e
ARP Implementation Quote “Using the Paediatric Acute Resuscitation Plan form does not change good paediatric practice, it simply changes where a clinical plan is documented. ”

d un Backgro 2. Resuscitation Plan

d un Backgro 2. Resuscitation Plan - role of palliative care - documentation in chart - CPR as the key decision

Having the provide/ do not provide CPR box at the bottom: • follows human factors concepts • shows the decision-making pathway An earlier version of the form with tick boxes and the CPR box at the top of the page.
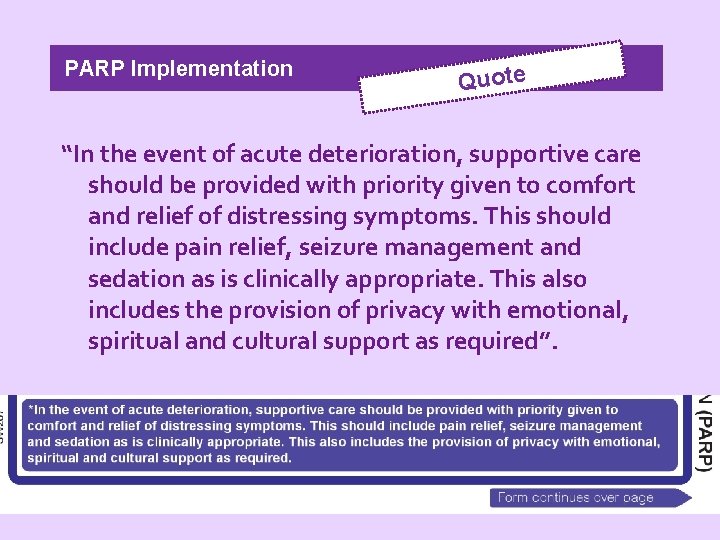
PARP Implementation Quote “In the event of acute deterioration, supportive care should be provided with priority given to comfort and relief of distressing symptoms. This should include pain relief, seizure management and sedation as is clinically appropriate. This also includes the provision of privacy with emotional, spiritual and cultural support as required”.
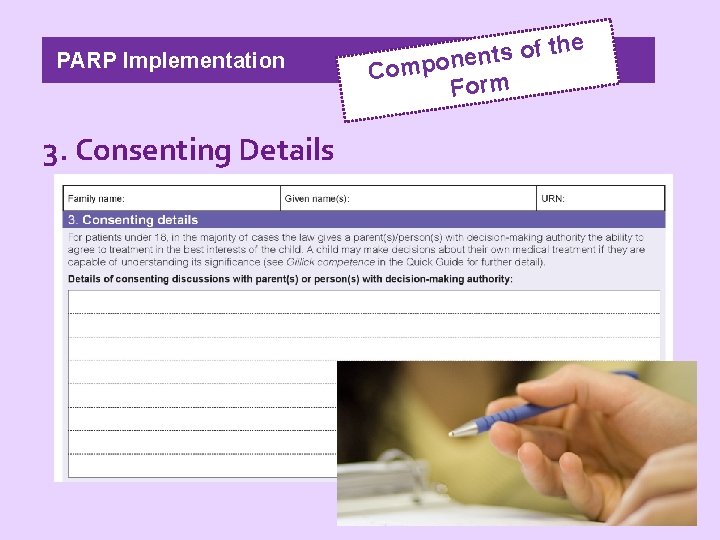
PARP Implementation 3. Consenting Details e h t f o s t en Compon Form
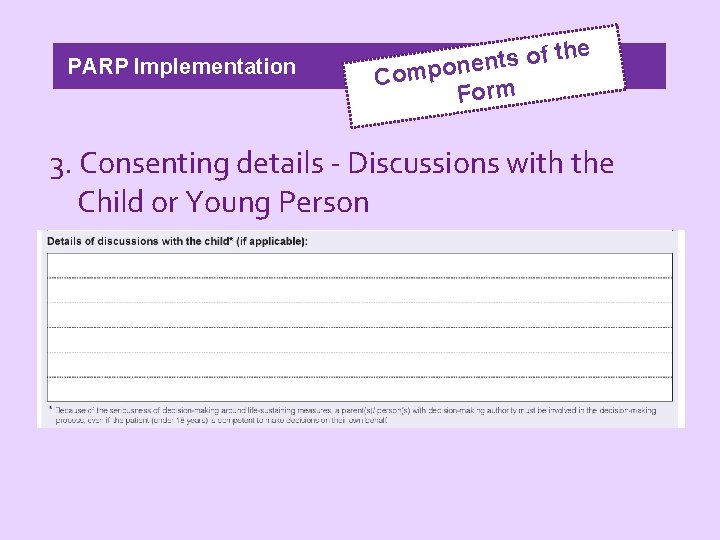
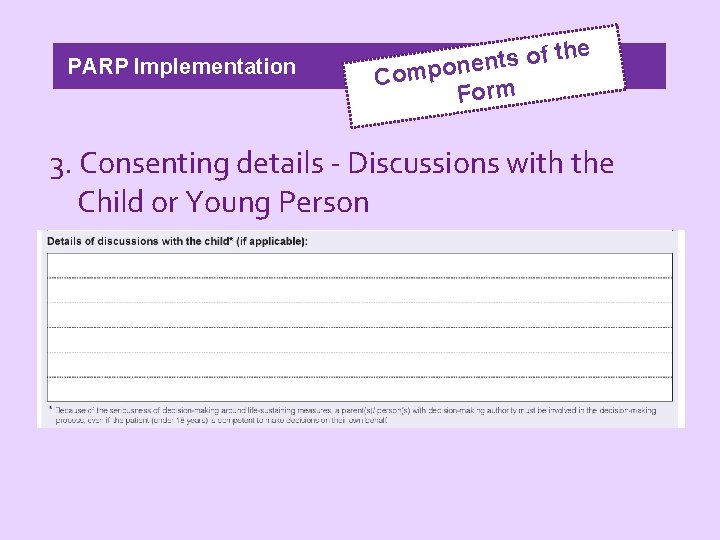
PARP Implementation h t f o s t n e Compon Form e 3. Consenting details - Discussions with the Child or Young Person
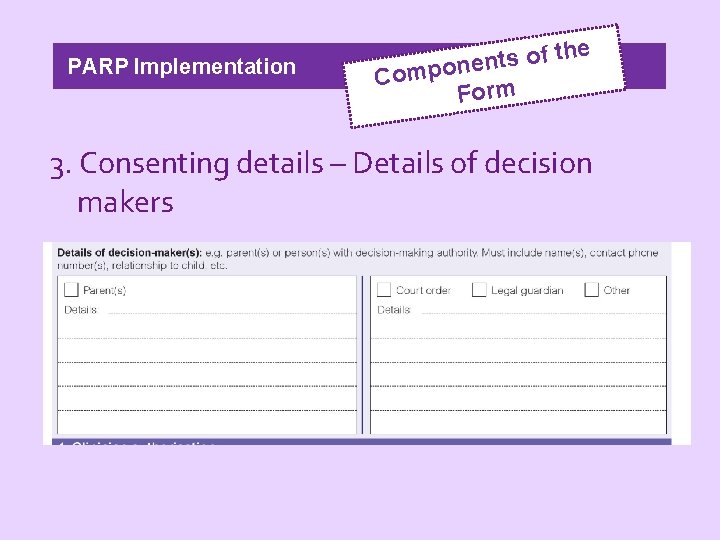
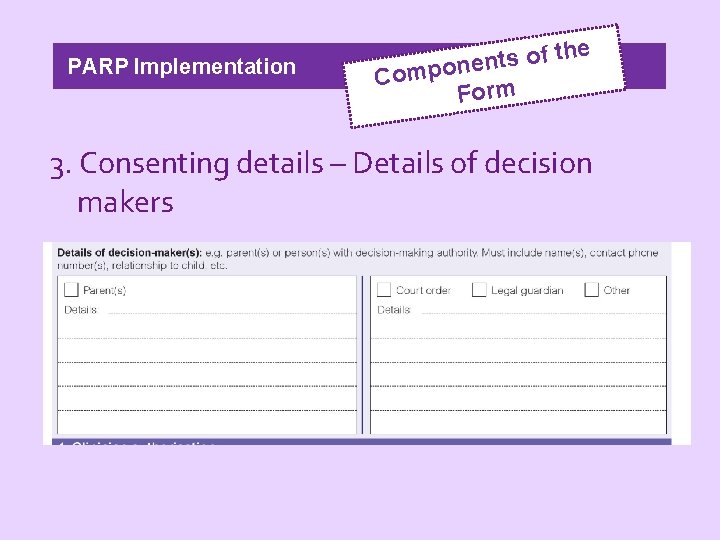
PARP Implementation h t f o s t n e Compon Form e 3. Consenting details – Details of decision makers
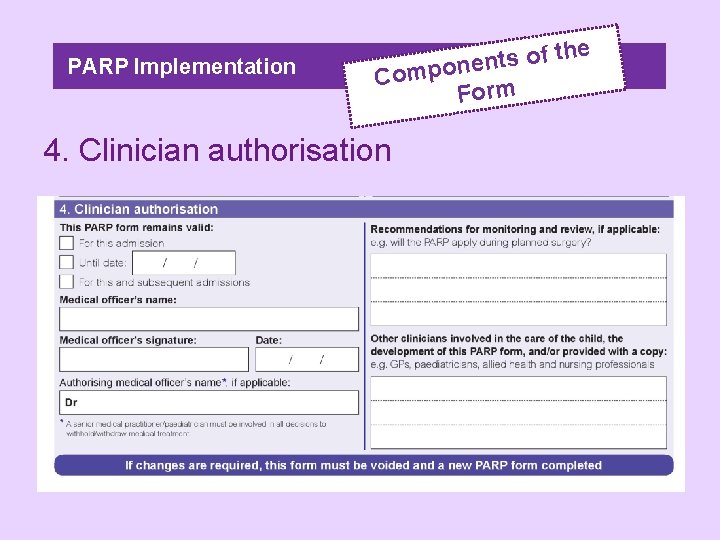
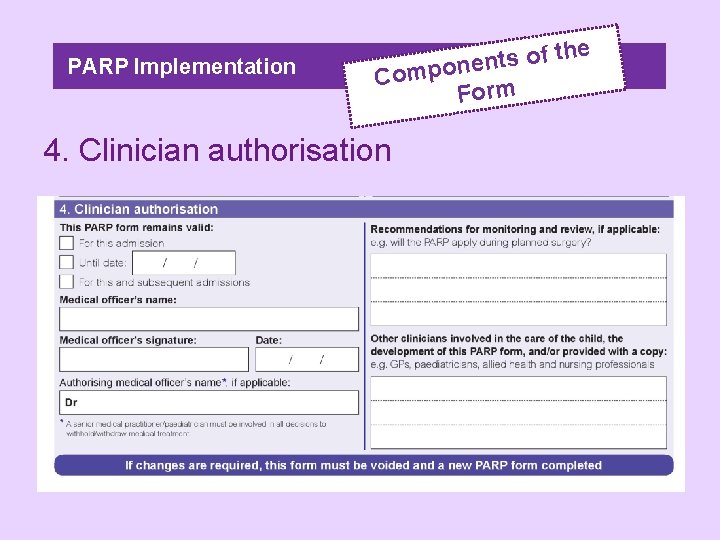
PARP Implementation h t f o s t n e Compon Form 4. Clinician authorisation e
PARP Implementation y c i l o P d Legal an ork Framew Why isn’t the PARP a “legally binding” form? — the parent / decision maker isn’t required to sign it — there are no witnessing provisions (as there are in an AHD or EPOA) • The PARP form is a clinical tool, a hospital form that provides evidence of the decision-making pathway (and discussions thereof) • The PARP does not replace, nor is it the same as, an Advance Health Directive!
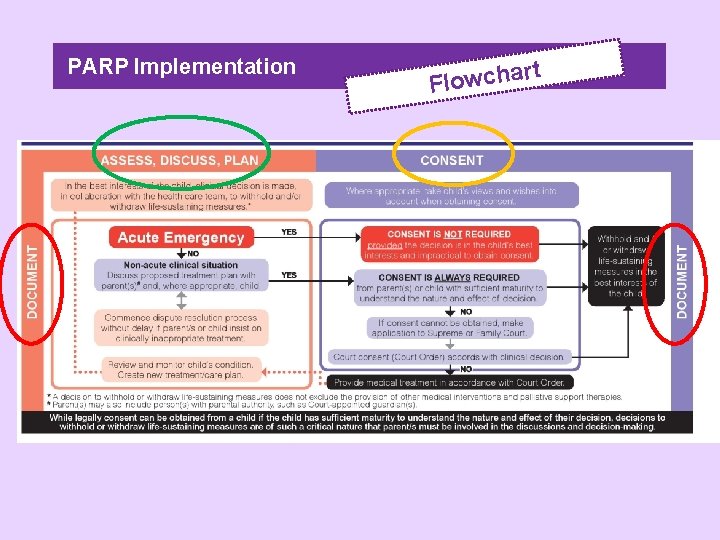
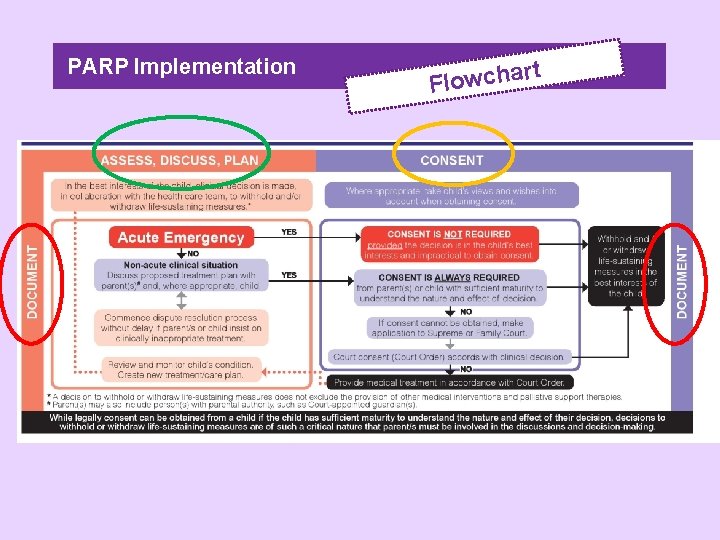
PARP Implementation rt a h c w o l F
ARP Implementation Quote “In the best interests of the child, clinical decision is made in collaboration with the health care team, to withold and/or withdraw life-sustaining measures”.
ARP Implementation Quote “Where appropriate, take the child’s views and wishes into account when obtaining consent”
ARP Implementation Quote “Although the interests of the patient are always primary, at the end of life there are times when the interests of the patient begin to wane, while those of the family intensify. ” Robert Truog
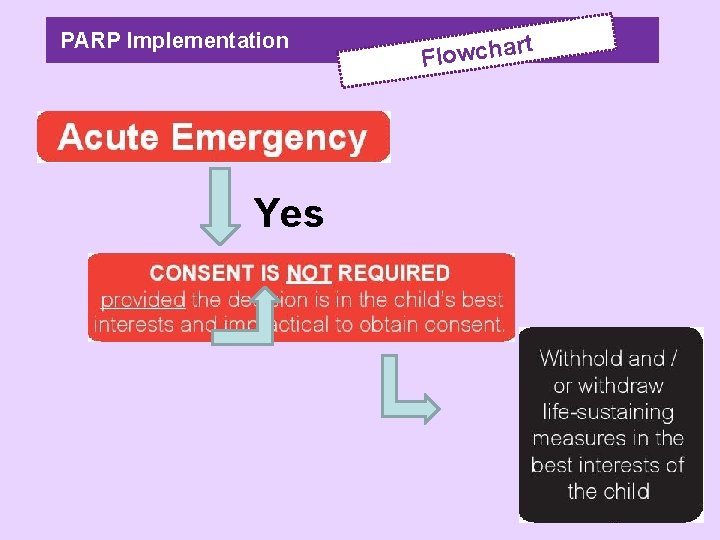
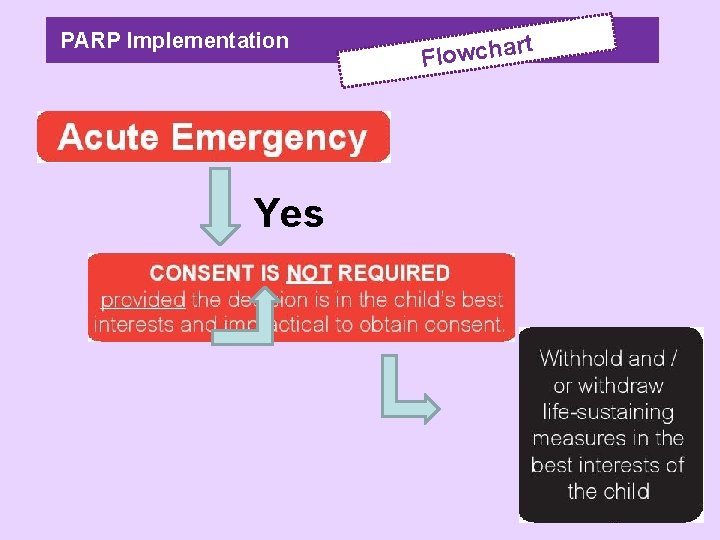
PARP Implementation Yes t r Flowcha
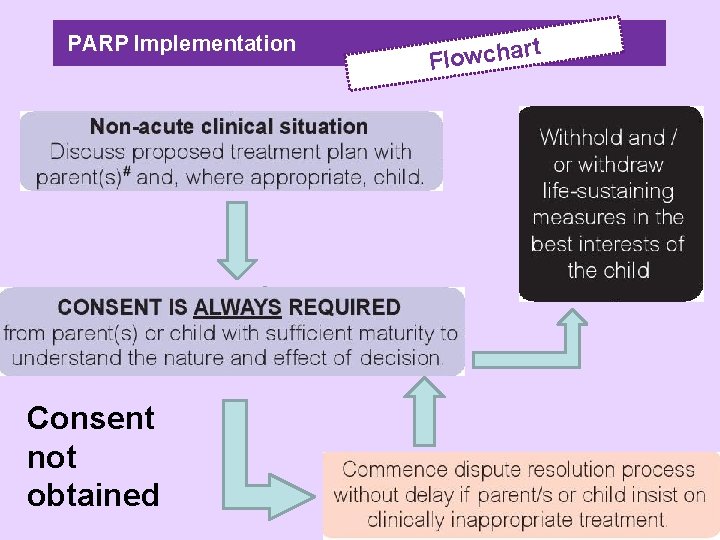
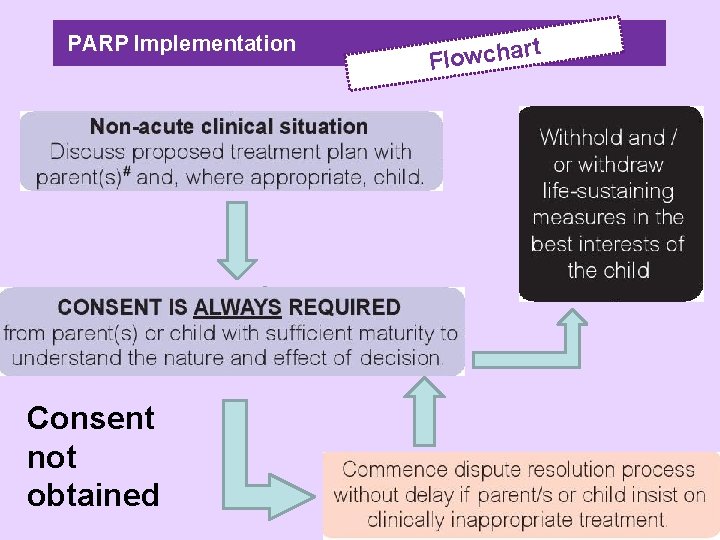
PARP Implementation Consent not obtained t r a h c w o Fl
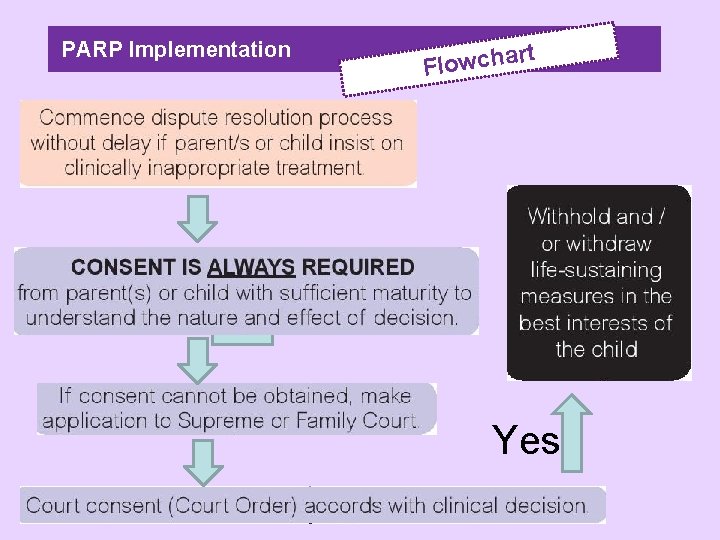
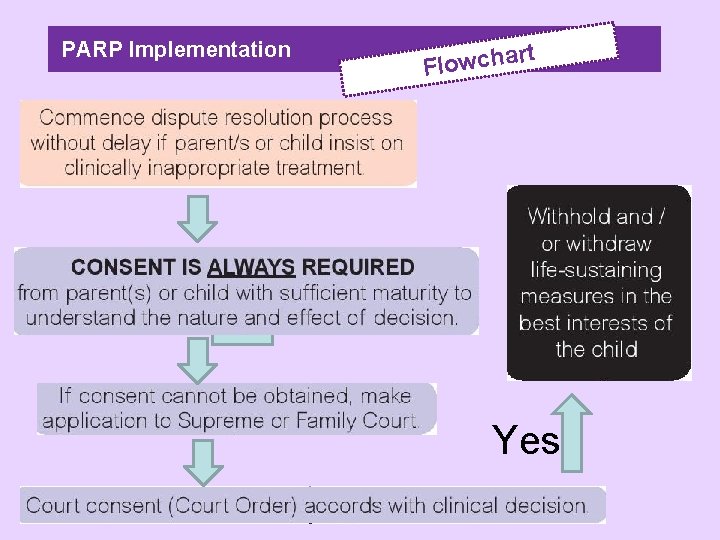
PARP Implementation rt Flowcha Yes

PARP Implementation rt a h c w o l F Withhold or withdraw life sustaining treatments In accordance with Court Order Provide medical treatment in accordance With Court Order
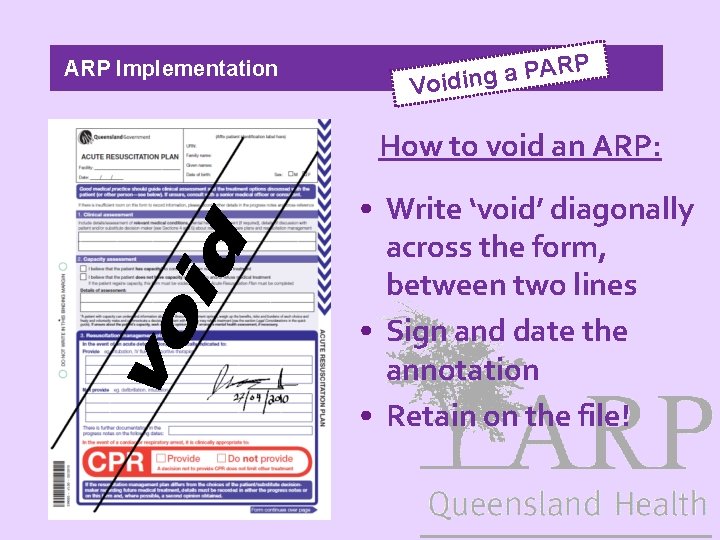
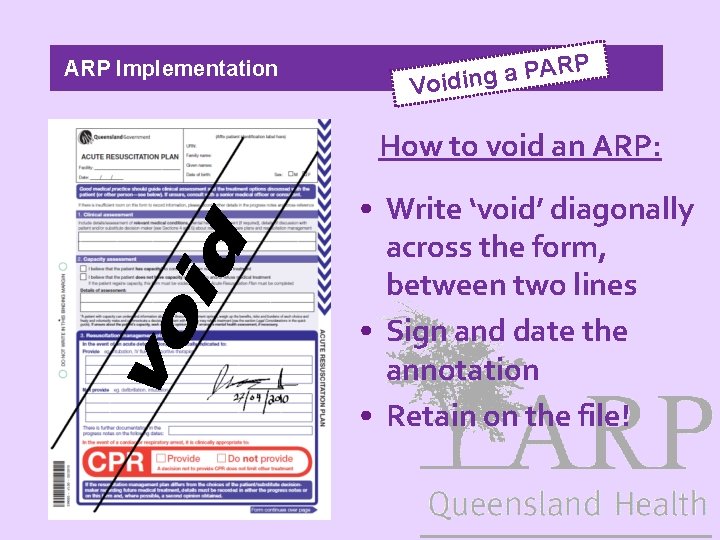
ARP Implementation P R A P a Voiding How to void an ARP: • Write ‘void’ diagonally across the form, between two lines • Sign and date the annotation • Retain on the file!
P ARP Implementation Stickers ed t e l p m o t-c i k l o o T The “Quick Guide”
P ARP Implementation d t i k l o o T e Th • Coversheet • Implementation Guide ete l p m o c – to be
P ARP Implementation er h t o – t i lk The Too ities possibil • Flip cards • Patient Information Sheets • On-line Training Module http: //apps. health. qld. gov. au/acp/login. Staff. aspx
P ARP Implementation Trial • The Trial PARP form has been endorsed by the Steering Group of the Child and Youth Network • Opportunity to modify (if needed) during the trial period • Being approved by the appropriate committees in local facilities (Royal Children’s, Mater Children’s, Gold Coast, Townsville) • Other sites can still be included in the trial
PARP Implementation n o i t a u l a Ev • Pre-implementation (baseline) audit • For deceased patients only, looking at resuscitation planning documentation (e. g. NFR orders) • Implementation audit • Use of ARP forms • Original form filed at start of chart • Arresting patient data • What are the best clinical indicators?
ARP Implementation ry Summa • State-wide Tool (or form) used to document resuscitation plans after appropriate clinical assessment and discussions with the parents or young person • Focus on what will be done rather than what won’t be done • Clear documentation of people involved in discussion • Can allow for complexity e. g. No CPR but can have high flow oxygen in the intensive care setting
PARP Ackowledgements Palliative Care Working Group of the Child and Youth Network -Dr Helen Irving, Paediatric Oncologist, Chair -Dr Anthony Herbert, Paediatrician, PPCS, RCH -Dr Will Cairns, Director of Palliative Care, TTH -Lee-anne Pedersen, Nurse Practitoner, PPCS, RCH -Leigh Kurth, Social Worker, PPCS, RCH -Liz Crowe, Social Worker, MCH -David Levitt, Paediatrician, MCH -Nicolette Thornton, Nurse Practitioner, GCH -Dr David van Gend, GP, Toowoomba -Sue Nancarrow, Manager and Nurse, Xavier Children’s Support Network -Registrars (Christine Smith, Jean Kelly)
PARP Ackowledgements Clinical Networks Elizabeth Chenoweth & Terry Lack, Principal Project Officers, Clinical Networks Team, Patient Safety and Quality Improvement Service, Centre for Healthcare Improvement Legal Advice Alessandra Liussi, Principal Lawyer, Legal Unit Nicole Sinclair, District Lawyer, RCH Julie White, Principal Lawyer, Access Improvement Service, Centre for Healthcare Improvement

PARP Ackowledgements End of Life Care Project Clinical Policy Team, Access Improvement Services, Centre for Healthcare Improvement Dr Wendy Corfield, Principal Policy Advisor Aurora Hodges, Policy Officer Julie White, Principal Lawyer