Pelvic Inflammatory Disease Risk Factors Diagnosis and Treatment


- Slides: 25
Pelvic Inflammatory Disease Risk Factors, Diagnosis and Treatment www. publichealth. columbus. gov

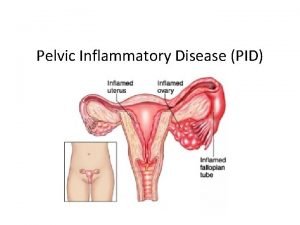
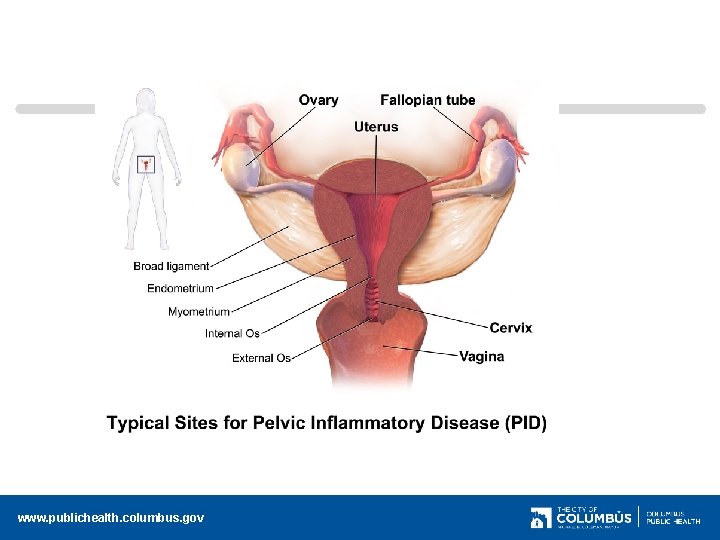
What is PID Pelvic inflammatory disease (PID) is a clinical syndrome that results from the ascension of microorganisms from the cervix and vagina to the upper genital tract. Approximately one million women are diagnosed yearly It is the most common serious STD complication . Acute PID is commonly caused by Chlamydia and Gonorrhea Most women with acute PID have Bacterial Vaginosis (BV) www. publichealth. columbus. gov
Center for Disease Control The CDC states it is an inflammatory disorder of the upper female genital tract, including any combination of fallopian tubes, uterine lining, ovaries, upper genital tract, uterus, throughout the pelvic area. Difficult to diagnose due to wide variation in symptoms www. publichealth. columbus. gov
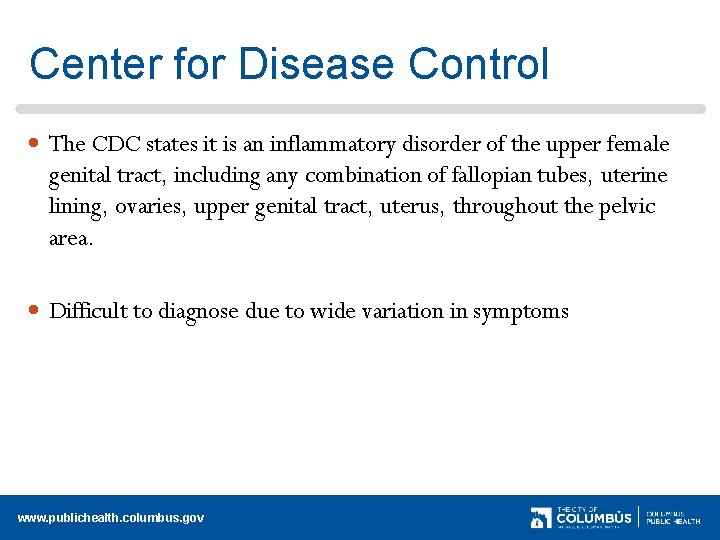
www. publichealth. columbus. gov
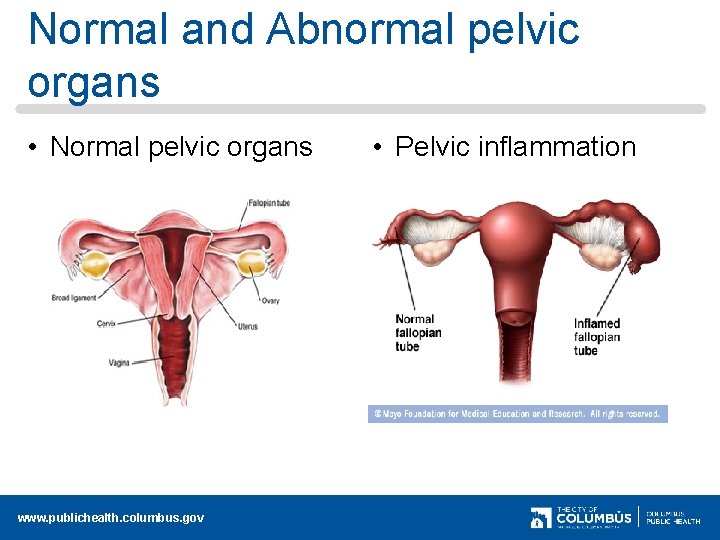
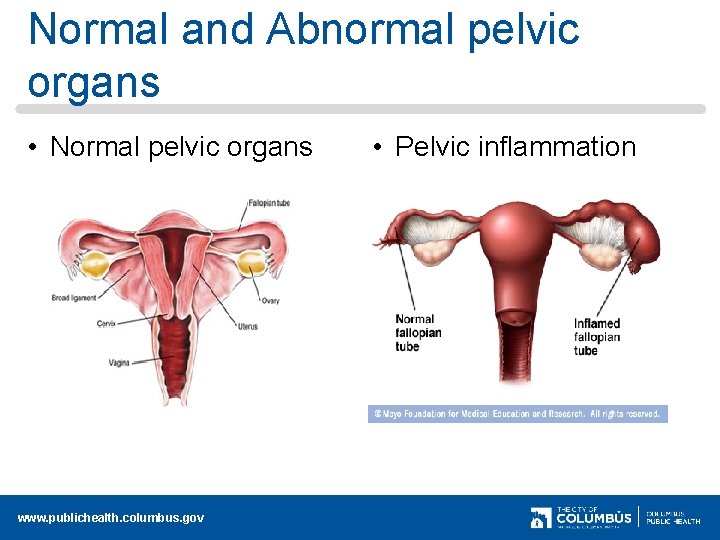
Normal and Abnormal pelvic organs • Normal pelvic organs www. publichealth. columbus. gov • Pelvic inflammation
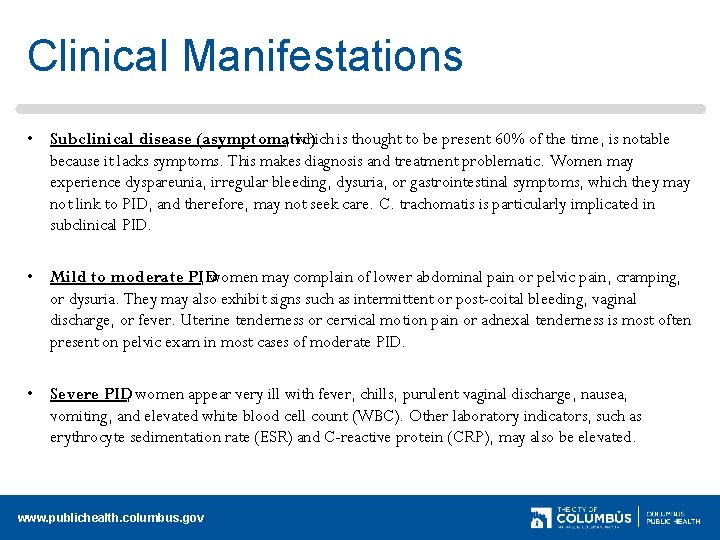
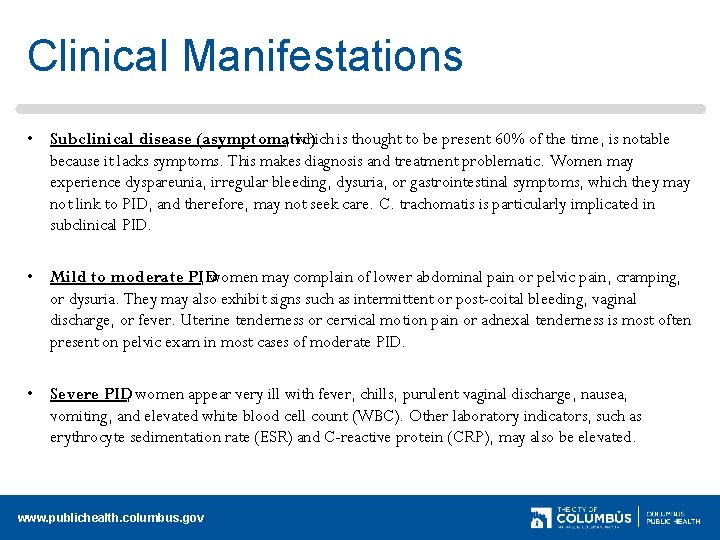
Clinical Manifestations • Subclinical disease (asymptomatic) , which is thought to be present 60% of the time, is notable because it lacks symptoms. This makes diagnosis and treatment problematic. Women may experience dyspareunia, irregular bleeding, dysuria, or gastrointestinal symptoms, which they may not link to PID, and therefore, may not seek care. C. trachomatis is particularly implicated in subclinical PID. • Mild to moderate PID , women may complain of lower abdominal pain or pelvic pain, cramping, or dysuria. They may also exhibit signs such as intermittent or post-coital bleeding, vaginal discharge, or fever. Uterine tenderness or cervical motion pain or adnexal tenderness is most often present on pelvic exam in most cases of moderate PID. • Severe PID, women appear very ill with fever, chills, purulent vaginal discharge, nausea, vomiting, and elevated white blood cell count (WBC). Other laboratory indicators, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), may also be elevated. www. publichealth. columbus. gov
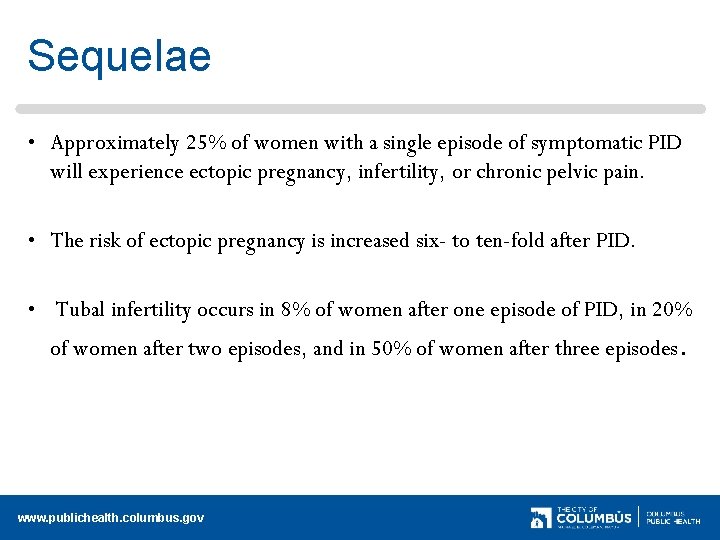
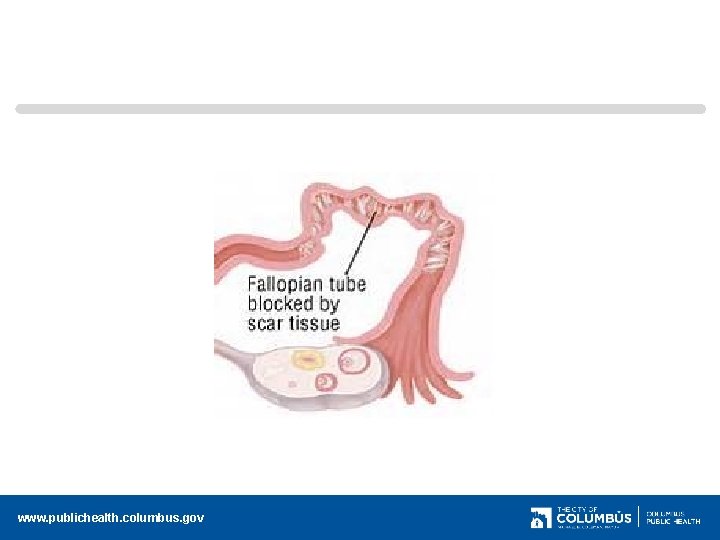
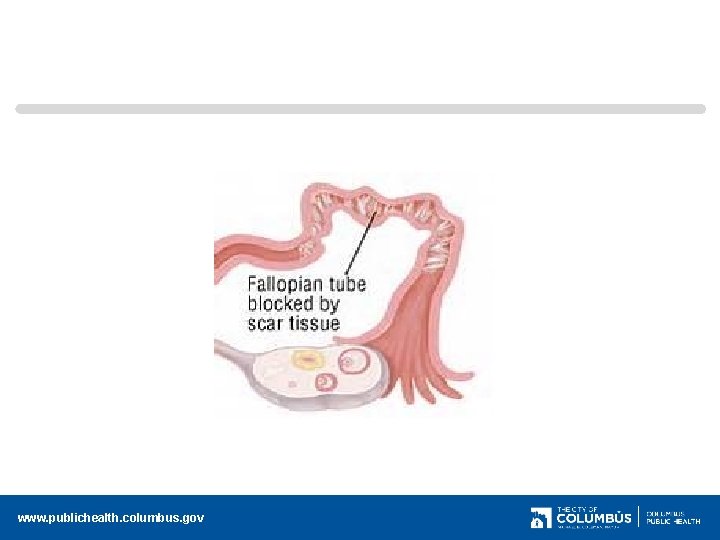
Sequelae • Approximately 25% of women with a single episode of symptomatic PID will experience ectopic pregnancy, infertility, or chronic pelvic pain. • The risk of ectopic pregnancy is increased six- to ten-fold after PID. • Tubal infertility occurs in 8% of women after one episode of PID, in 20% of women after two episodes, and in 50% of women after three episodes. www. publichealth. columbus. gov
www. publichealth. columbus. gov
Empiric treatment should be initiated in sexually active young women & women at risk if there is pelvic or lower abdominal pain, if no cause for the illness other than PID is identified and if one or more of the following minimum criteria are present on pelvic exam: 1) cervical motion tenderness 2) Uterine tenderness 3) adnexal tenderness www. publichealth. columbus. gov
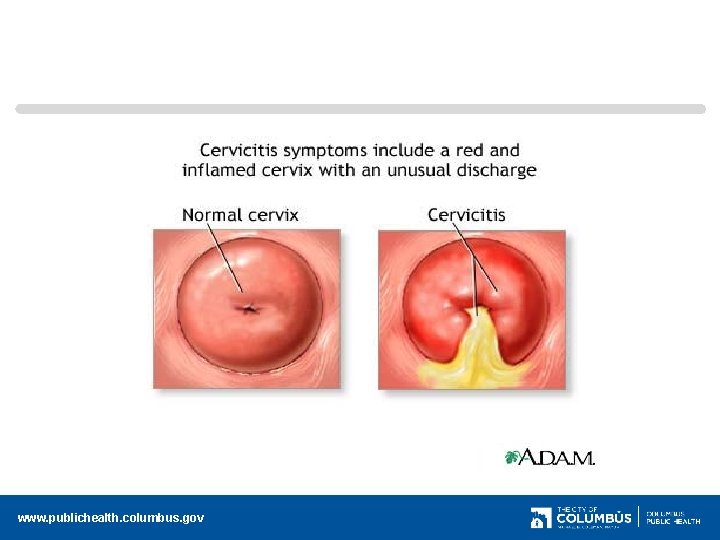
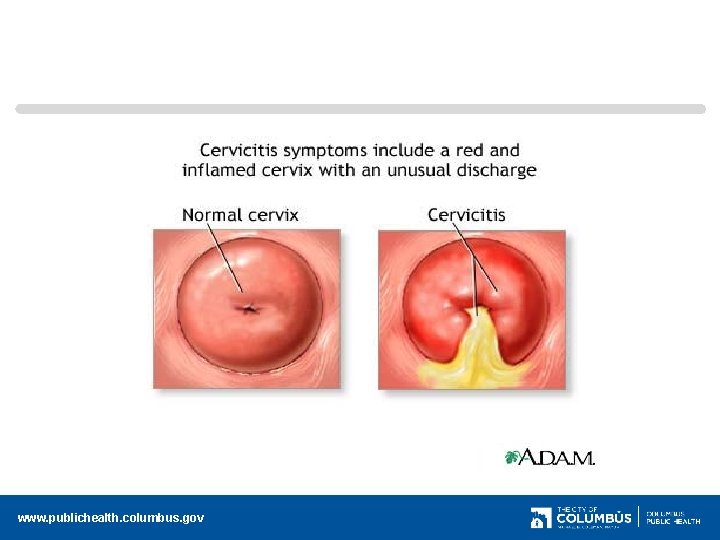
Requiring all three minimum criteria be present before treating can result in insufficient diagnosis of PID Most women with PID have either mucopurulent cervical discharge or increase WBC; s under microscope = infection The presence of signs of lower genital tract infection plusone of the three minimum diagnosis increases the specificity of the diagnosis If cervical discharge is normal and no WBC’s are present the diagnosis is unlikely and alternative causes of pain should be considered. www. publichealth. columbus. gov
www. publichealth. columbus. gov
Risk Factors PID is elevated in sexually active teens partially due to the immature cervical cells and frequently changing sex partners. Having multiple sex partners Women who douche Women with IUD’s Previous STD infections may elevate PID risk due to damage of reproductive organs from the initial infection www. publichealth. columbus. gov
Epidemology Diagnosed in 1 -5% of women in STD clinics in US Declining rates since the 1990’s Overt or subclinical PID is the most common cause of ectopic pregnancy and tubal infertility Incubation Period: Varies from 10 days to several months follow acquisition of Chlamydia or Gonorrhea www. publichealth. columbus. gov
Transmission • Exclusively by sexual contact or perinatal • Uncommon in Women having Sex with Women (WSW) with exclusively female sex partners www. publichealth. columbus. gov
Symptoms Abnormal or unusual vaginal discharge (yellow/green/malodorous) Abnormal vaginal bleeding Dull pain and tenderness in stomach Lower abdominal or pelvic pain nearly universal in symptomatic cases Pain with urination Pain with intercourse (dyspareunia) Pain in back Elevated temperature and fever Irregular menses Spotting and cramping with prolonged painful menses. (menorrhagia) www. publichealth. columbus. gov
Physical Exam • • • Pelvic adnexal tenderness usually bilaterally Uterine fundal and cervical motion tenderness Signs of MPC or BV Fever is common but often absent Lower quadrant abdominal tenderness, sometimes rebound tenderness present • Adnexal mass may be present • R upper quadrant tenderness may be present www. publichealth. columbus. gov
Diagnostic Criteria • In sexually active women, low abdominal pain with adnexal or cervical motion tenderness • Fever may be present • Mucopurulent cervicitis and discharge • Abundant WBC’s in cervical or vaginal discharge • Cervical infection with Chlamydia or Gonorrhea www. publichealth. columbus. gov
Lab diagnosis • Lab evidence of BV or MCP • Other tests: § Pelvic ultrasound § Laparoscopy may be indicated if diagnosis is uncertain § Endometrial Biopsy helpful with endometritis www. publichealth. columbus. gov
Differential diagnosis • • Appendicitis Ectopic pregnancy Septic abortion/miscarriage (associated with a serious uterine infection) Hemorrhagic, ruptured or twisted ovarian cysts Tumors Degeneration of a myoma Acute enteritis (inflammation small intestine) www. publichealth. columbus. gov
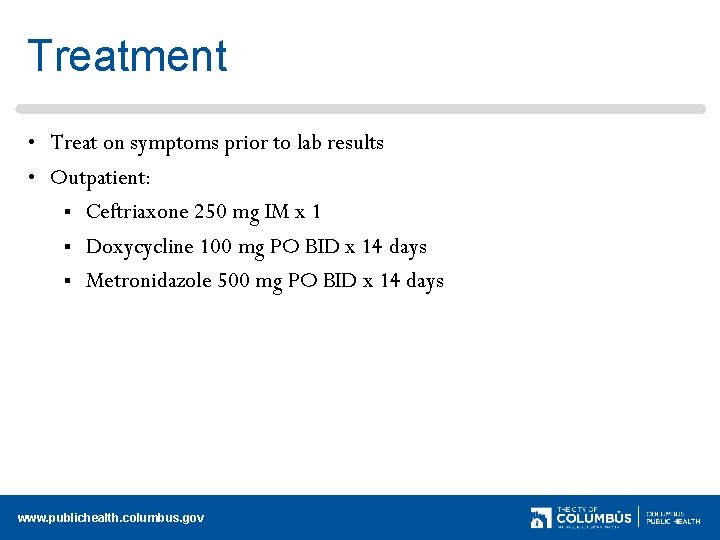
Treatment • Treat on symptoms prior to lab results • Outpatient: § Ceftriaxone 250 mg IM x 1 § Doxycycline 100 mg PO BID x 14 days § Metronidazole 500 mg PO BID x 14 days www. publichealth. columbus. gov
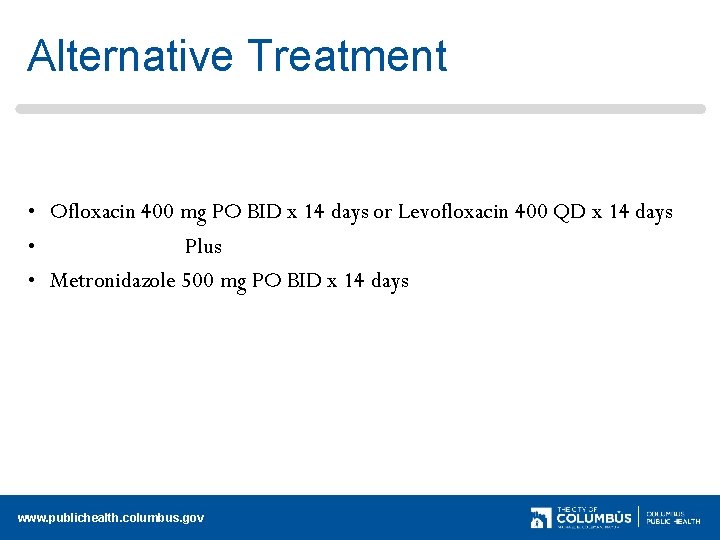
Alternative Treatment • Ofloxacin 400 mg PO BID x 14 days or Levofloxacin 400 QD x 14 days • Plus • Metronidazole 500 mg PO BID x 14 days www. publichealth. columbus. gov
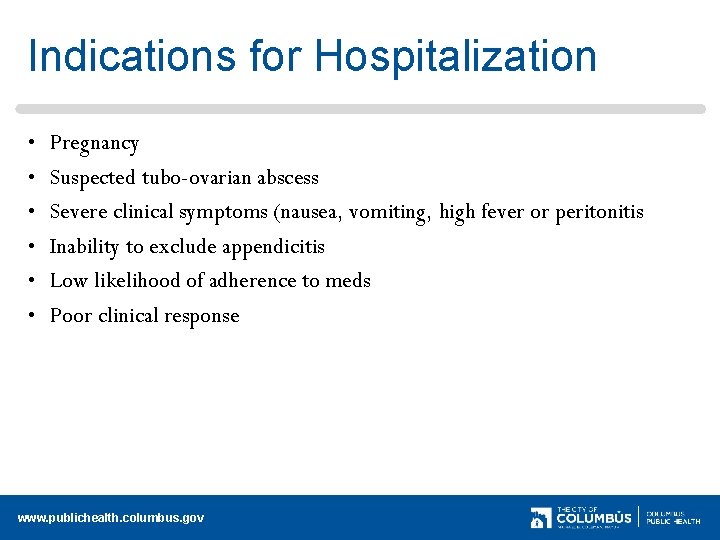
Indications for Hospitalization • • • Pregnancy Suspected tubo-ovarian abscess Severe clinical symptoms (nausea, vomiting, high fever or peritonitis Inability to exclude appendicitis Low likelihood of adherence to meds Poor clinical response www. publichealth. columbus. gov

Supportive therapy • • Consider removing IUD if present Bed rest in severe cases Abstain from sex until one week after completion of medication Partner treatment www. publichealth. columbus. gov
Follow up • Reexamine every 1 -3 days • Failure to improve within 3 -4 days requires hospitalization www. publichealth. columbus. gov
Bibliography • CDC. Pelvic Inflammatory Disease. Morbidity and Mortality Weekly Report 2010; 59 : 63 -67 • Handsfield, Hunter. H. Sexually Transmitted Diseases Third Edition. 2011; 267 -277 • Klausner, Jeffrey D. , Hook, Edward W III, Current Diagnosis and Treatment Sexually Transmitted Diseases. 2007; 46 -51 www. publichealth. columbus. gov
 Pelvic inflammatory disease men
Pelvic inflammatory disease men Pelvic girdle pain
Pelvic girdle pain Treatment of inflammatory breast cancer
Treatment of inflammatory breast cancer Ulcerative colitis vs crohn's
Ulcerative colitis vs crohn's Liquidity measures
Liquidity measures Steps of nursing process
Steps of nursing process Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Second phase of nursing process
Second phase of nursing process Nursing process and critical thinking
Nursing process and critical thinking Charting identification chapter 28
Charting identification chapter 28 House palate classification
House palate classification Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Oral diagnosis and treatment planning ppt
Oral diagnosis and treatment planning ppt Pro and anti inflammatory
Pro and anti inflammatory Bharathi viswanathan
Bharathi viswanathan Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Mucorrhea causes
Mucorrhea causes Mechanical vs inflammatory pain
Mechanical vs inflammatory pain Non odontogenic infection
Non odontogenic infection Inflammatory breast cancer pictures
Inflammatory breast cancer pictures Post inflammatory erythema
Post inflammatory erythema Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Predeksihkhariini
Predeksihkhariini Inflammatory cells
Inflammatory cells Acute inflammatory exudate
Acute inflammatory exudate Nursing diagnosis for vision impairment
Nursing diagnosis for vision impairment