PELVIC INFLAMMATORY DISEASE Nikolina Antonia Domoku Mentor A
- Slides: 9
PELVIC INFLAMMATORY DISEASE Nikolina Antonia Domokuš Mentor: A. Žmegač Horvat
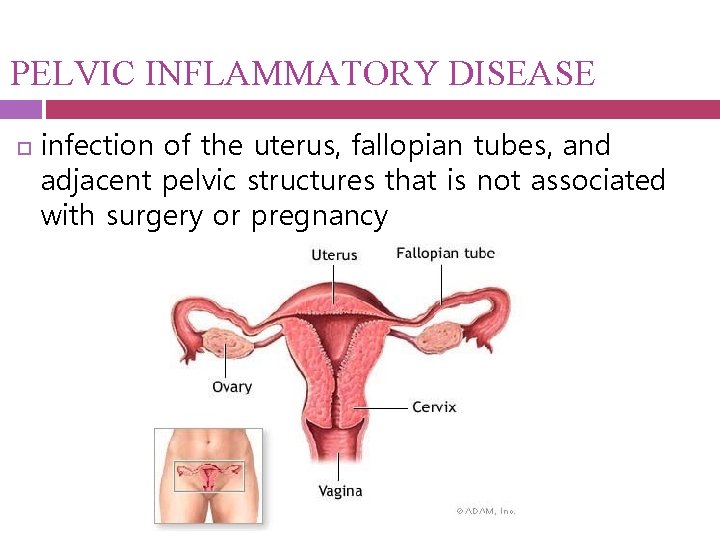
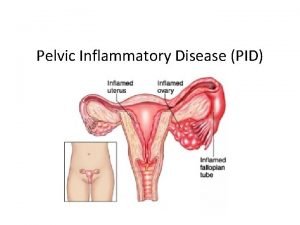
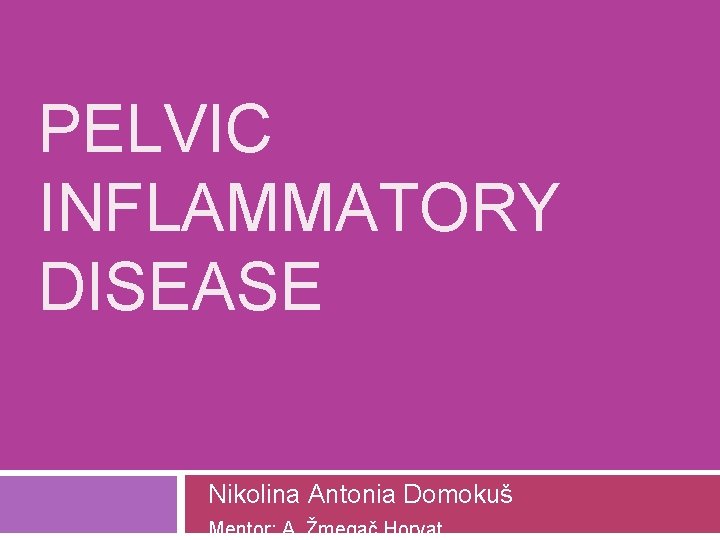
PELVIC INFLAMMATORY DISEASE infection of the uterus, fallopian tubes, and adjacent pelvic structures that is not associated with surgery or pregnancy
Etiology and Pathogenesis 2 stages of PID: -acquisition of a vaginal or cervical infection -direct ascent of micro-organisms from the vagina and cervix ORGANISMS MOST COMMONLY ISOLATED : • Neisseria gonorrhoeae and Chlamydia trachomatis • Gardnerella vaginalis, Mycoplasma hominis, Ureaplasma urealyticum, herpes simplex virus-2 (HSV-2), Trichomonas vaginalis, cytomegalovirus, Haemophilus influenzae, Streptococcus agalactiae
Risk factors young age multiple sexual partners certain methods of contraception previous history of chlamydia or another sexually transmitted infection delayed and decreased access to care
Symptoms lower abdominal pain abnormal vaginal discharge abnormal uterine bleeding dysuria dyspareunia nausea vomiting fever Gonococcal PID - dramatic symptoms of fever and peritoneal irritation
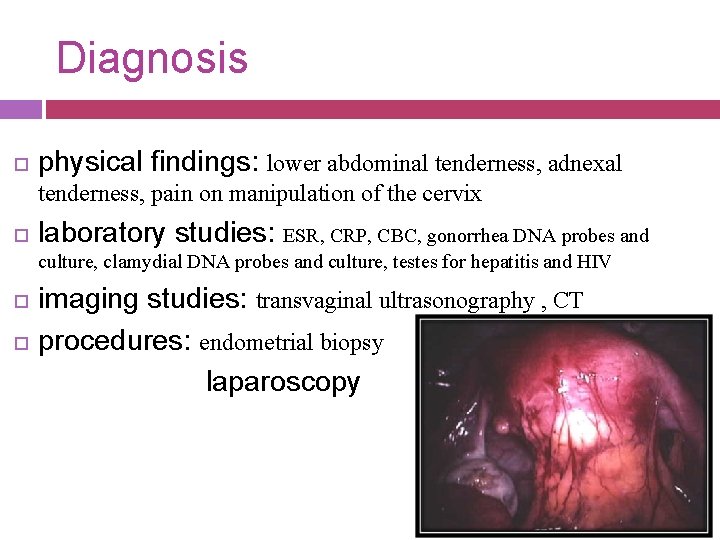
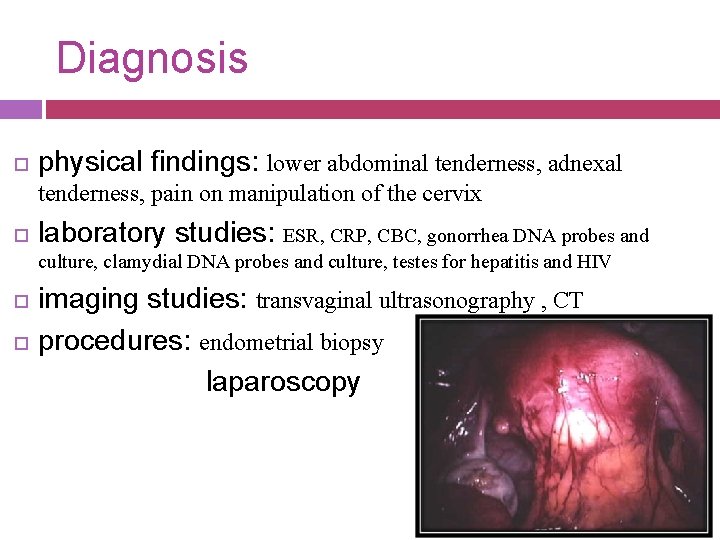
Diagnosis physical findings: lower abdominal tenderness, adnexal tenderness, pain on manipulation of the cervix laboratory studies: ESR, CRP, CBC, gonorrhea DNA probes and culture, clamydial DNA probes and culture, testes for hepatitis and HIV imaging studies: transvaginal ultrasonography , CT procedures: endometrial biopsy laparoscopy
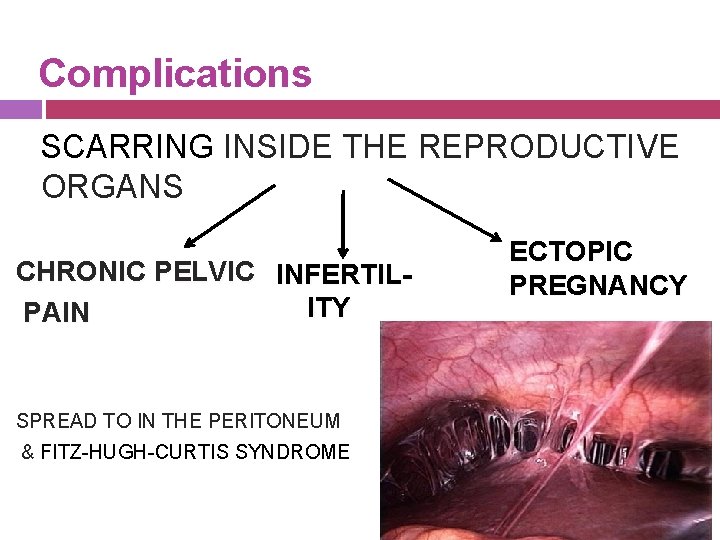
Complications SCARRING INSIDE THE REPRODUCTIVE ORGANS CHRONIC PELVIC INFERTILITY PAIN SPREAD TO IN THE PERITONEUM & FITZ-HUGH-CURTIS SYNDROME ECTOPIC PREGNANCY
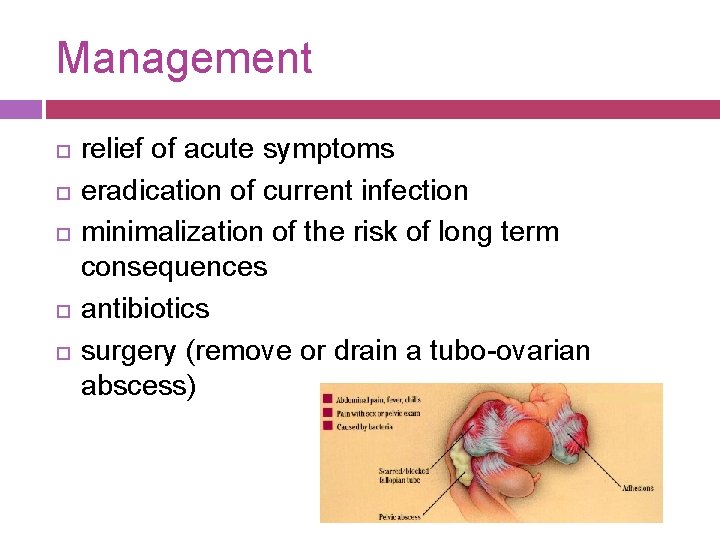
Management relief of acute symptoms eradication of current infection minimalization of the risk of long term consequences antibiotics surgery (remove or drain a tubo-ovarian abscess)
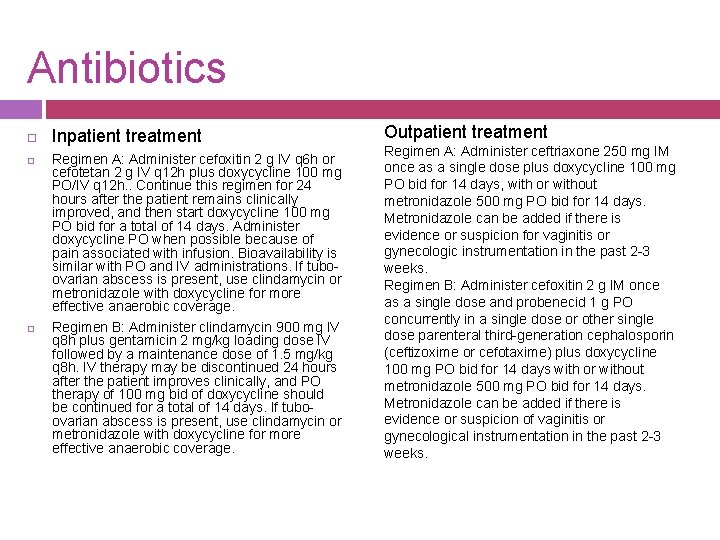
Antibiotics Inpatient treatment Regimen A: Administer cefoxitin 2 g IV q 6 h or cefotetan 2 g IV q 12 h plus doxycycline 100 mg PO/IV q 12 h. . Continue this regimen for 24 hours after the patient remains clinically improved, and then start doxycycline 100 mg PO bid for a total of 14 days. Administer doxycycline PO when possible because of pain associated with infusion. Bioavailability is similar with PO and IV administrations. If tuboovarian abscess is present, use clindamycin or metronidazole with doxycycline for more effective anaerobic coverage. Regimen B: Administer clindamycin 900 mg IV q 8 h plus gentamicin 2 mg/kg loading dose IV followed by a maintenance dose of 1. 5 mg/kg q 8 h. IV therapy may be discontinued 24 hours after the patient improves clinically, and PO therapy of 100 mg bid of doxycycline should be continued for a total of 14 days. If tuboovarian abscess is present, use clindamycin or metronidazole with doxycycline for more effective anaerobic coverage. Outpatient treatment Regimen A: Administer ceftriaxone 250 mg IM once as a single dose plus doxycycline 100 mg PO bid for 14 days, with or without metronidazole 500 mg PO bid for 14 days. Metronidazole can be added if there is evidence or suspicion for vaginitis or gynecologic instrumentation in the past 2 -3 weeks. Regimen B: Administer cefoxitin 2 g IM once as a single dose and probenecid 1 g PO concurrently in a single dose or other single dose parenteral third-generation cephalosporin (ceftizoxime or cefotaxime) plus doxycycline 100 mg PO bid for 14 days with or without metronidazole 500 mg PO bid for 14 days. Metronidazole can be added if there is evidence or suspicion of vaginitis or gynecological instrumentation in the past 2 -3 weeks.