Office Fracture Care TARA MASTERHUNTER M D DEPT

- Slides: 71
Office Fracture Care TARA MASTERHUNTER, M. D. DEPT. OF FAMILY MEDICINE UNIVERSITY OF MICHIGAN OCTOBER 2016
Objectives: To gain understanding of the risks of fracture care. To improve the ability to triage fractures and understand which ones may need orthopedic referral. To improve awareness of commonly missed injuries.
Refer to an orthopedist for any of the following: Intraarticular Severe comminution Inability to maintain reduction Nerve or vascular injury CRP Open Fractures Nonunion Pathologic fractures
Other fracture concepts Lack of tenderness to percussion is a sign of clinical healing In the elderly, immobilize as briefly as possible and rehab Check and document neurovascular status at every visit

Case #1: Fall on an Outstretched Hand 30 yo male injures his wrist after falling on an outstretched hand. He was learning how to roller blade (saw it on extreme sports channel).
Common FOOSH Injuries Distal Radius Fractures (Colles’ fracture) Scaphoid Injuries ouch
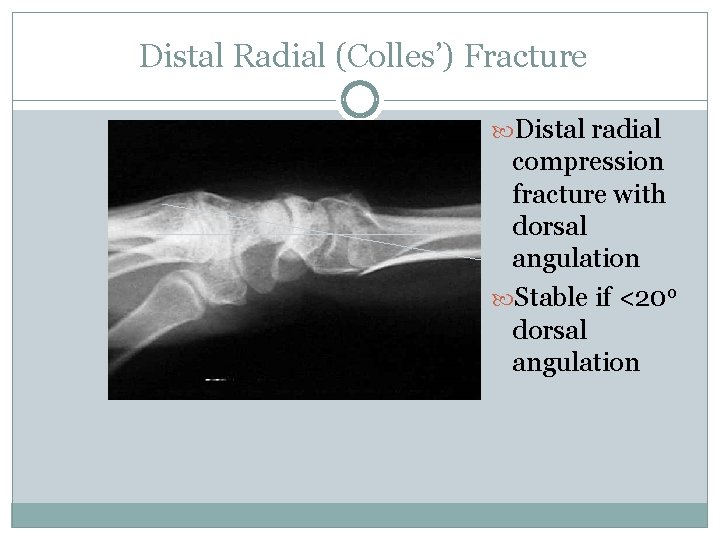
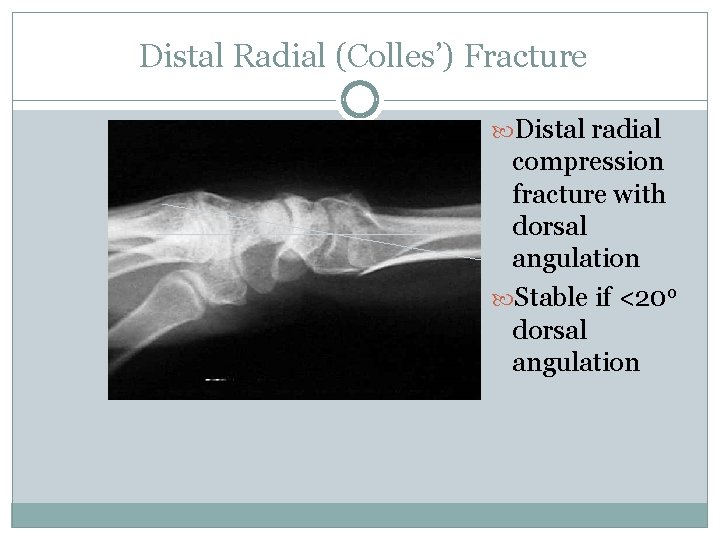
Distal Radial (Colles’) Fracture Distal radial compression fracture with dorsal angulation Stable if <20 o dorsal angulation
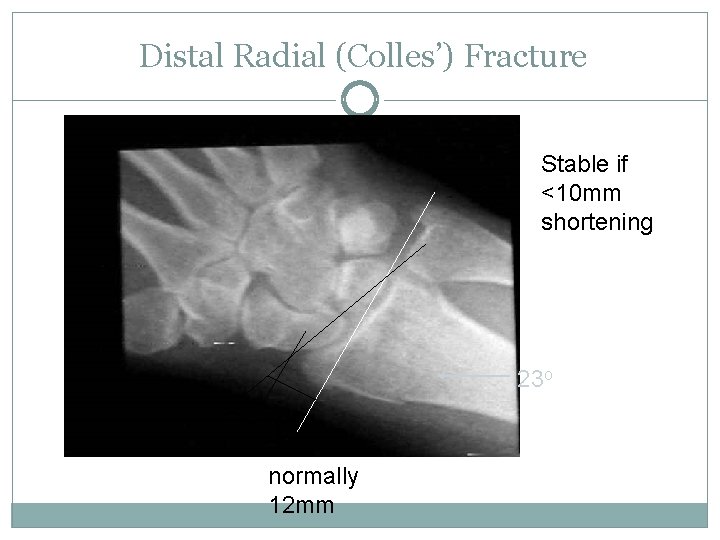
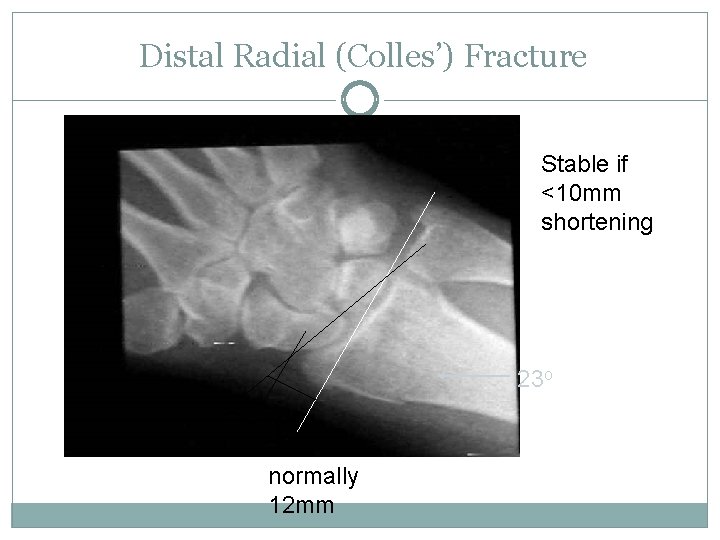
Distal Radial (Colles’) Fracture Stable if <10 mm shortening 23 o normally 12 mm
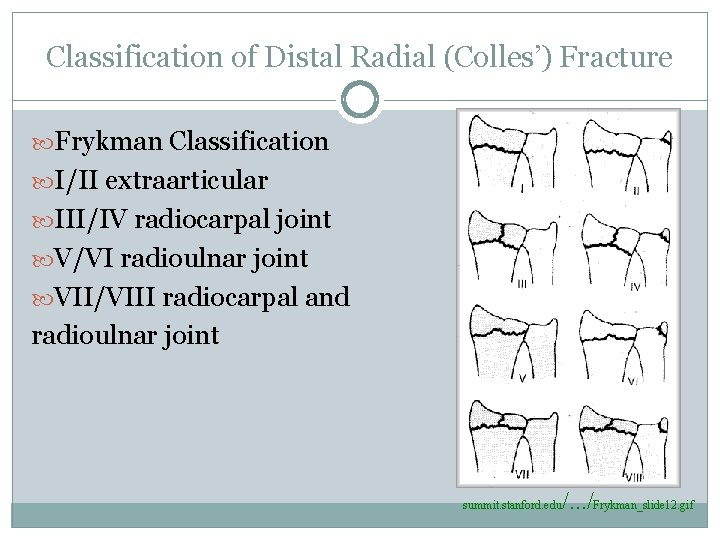
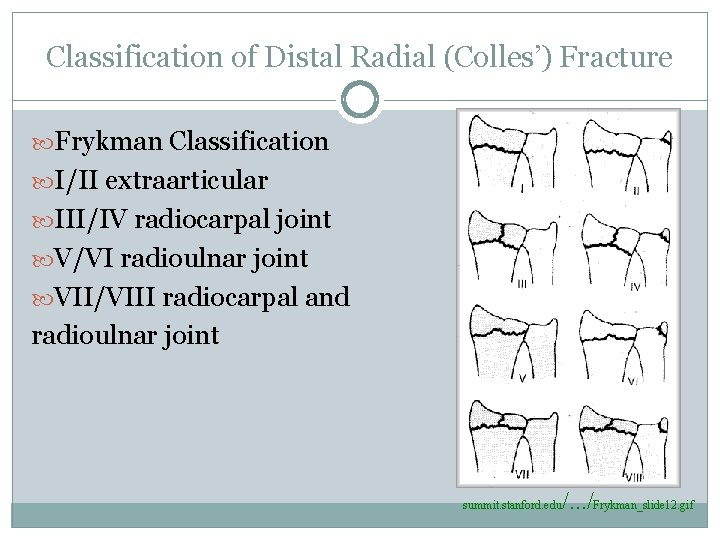
Classification of Distal Radial (Colles’) Fracture Frykman Classification I/II extraarticular III/IV radiocarpal joint V/VI radioulnar joint VII/VIII radiocarpal and radioulnar joint summit. stanford. edu /. . . /Frykman_slide 12. gif
Colles’ Fracture-Nondisplaced Acute Tx: Volar splint or sugar tong splint for 3 -5 days Definitive Tx: short arm cast (SAC) 4 -6 weeks X-ray every 2 -3 weeks
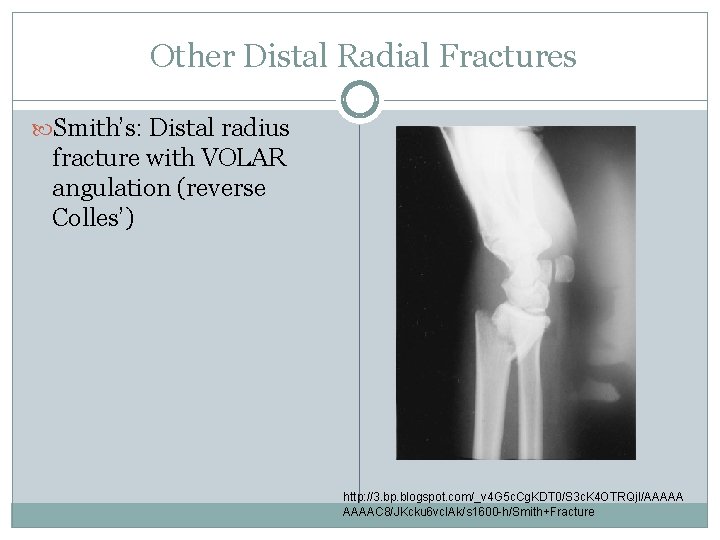
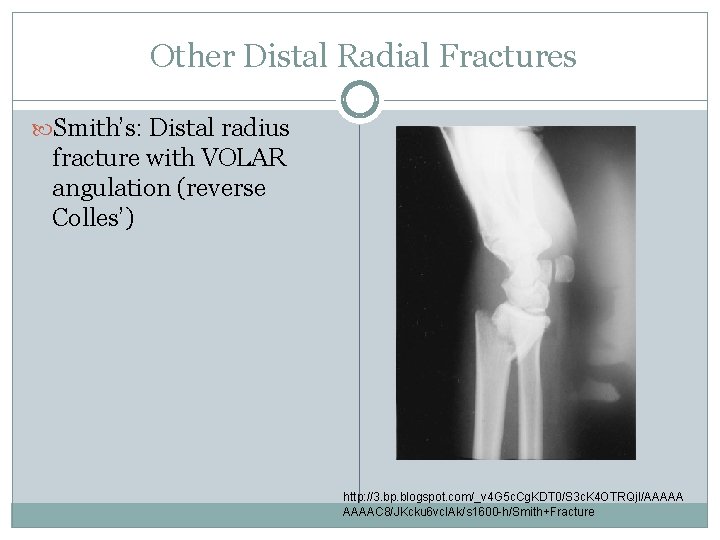
Other Distal Radial Fractures Smith’s: Distal radius fracture with VOLAR angulation (reverse Colles’) http: //3. bp. blogspot. com/_v 4 G 5 c. Cg. KDT 0/S 3 c. K 4 OTRQj. I/AAAAAC 8/JKcku 6 vc. IAk/s 1600 -h/Smith+Fracture
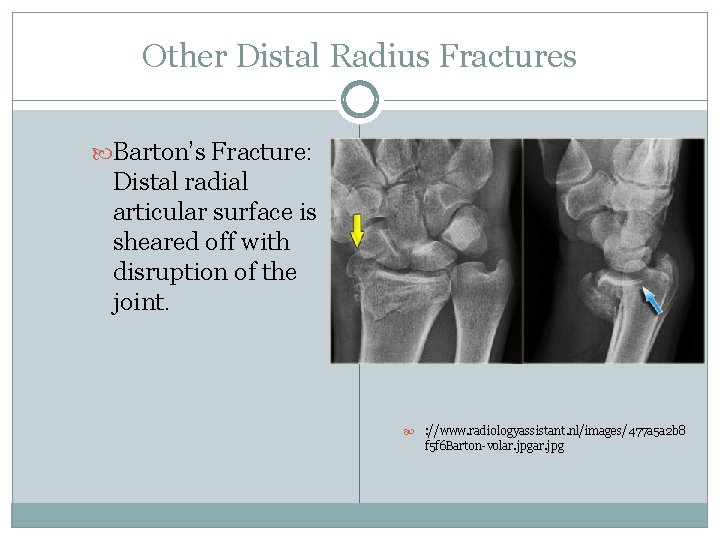
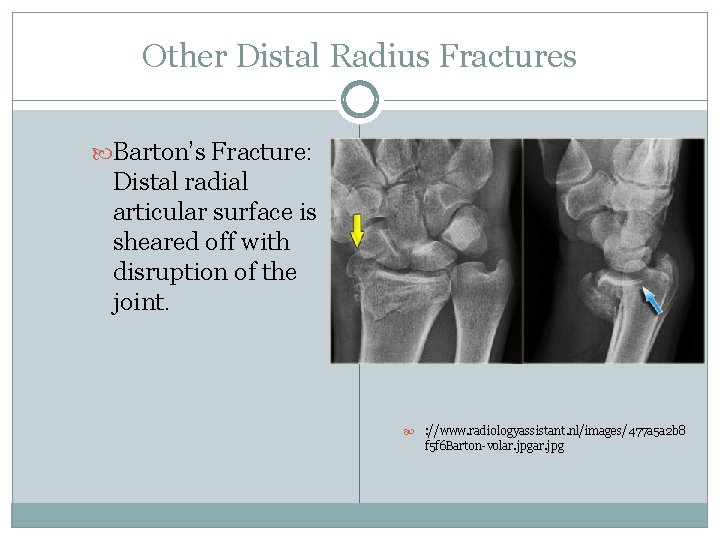
Other Distal Radius Fractures Barton’s Fracture: Distal radial articular surface is sheared off with disruption of the joint. : //www. radiologyassistant. nl/images/477 a 5 a 2 b 8 f 5 f 6 Barton-volar. jpg
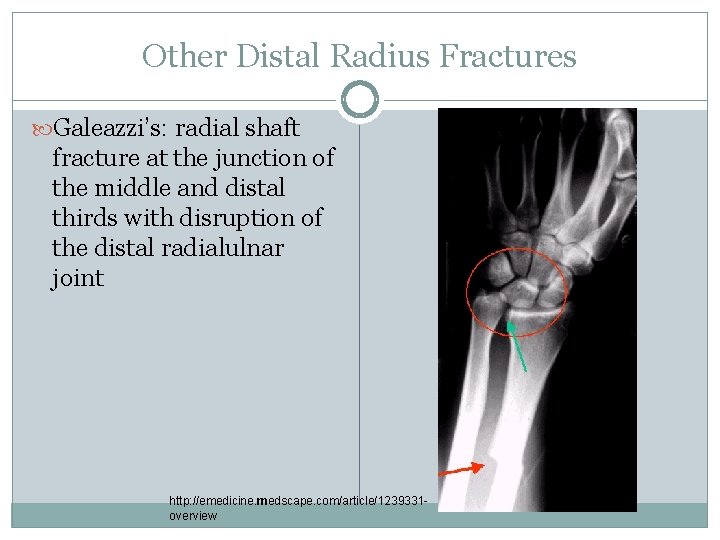
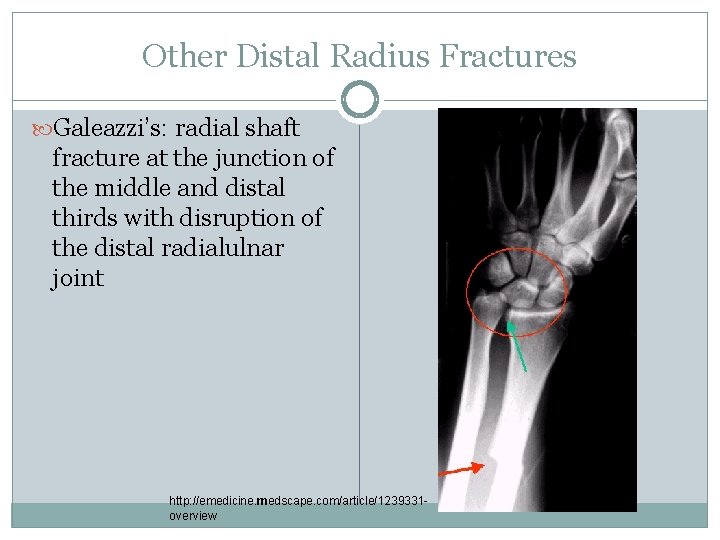
Other Distal Radius Fractures Galeazzi’s: radial shaft fracture at the junction of the middle and distal thirds with disruption of the distal radialulnar joint http: //emedicine. medscape. com/article/1239331 overview
Scaphoid Injuries OUCH
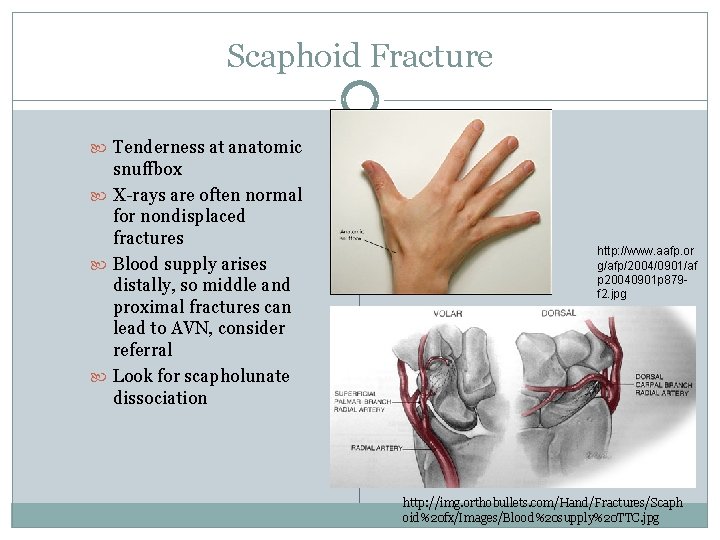
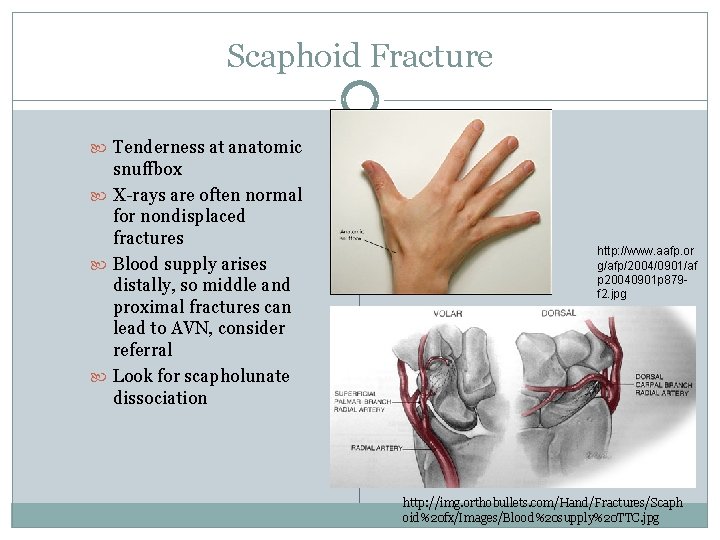
Scaphoid Fracture Tenderness at anatomic snuffbox X-rays are often normal for nondisplaced fractures Blood supply arises distally, so middle and proximal fractures can lead to AVN, consider referral Look for scapholunate dissociation http: //www. aafp. or g/afp/2004/0901/af p 20040901 p 879 f 2. jpg http: //img. orthobullets. com/Hand/Fractures/Scaph oid%20 fx/Images/Blood%20 supply%20 TTC. jpg
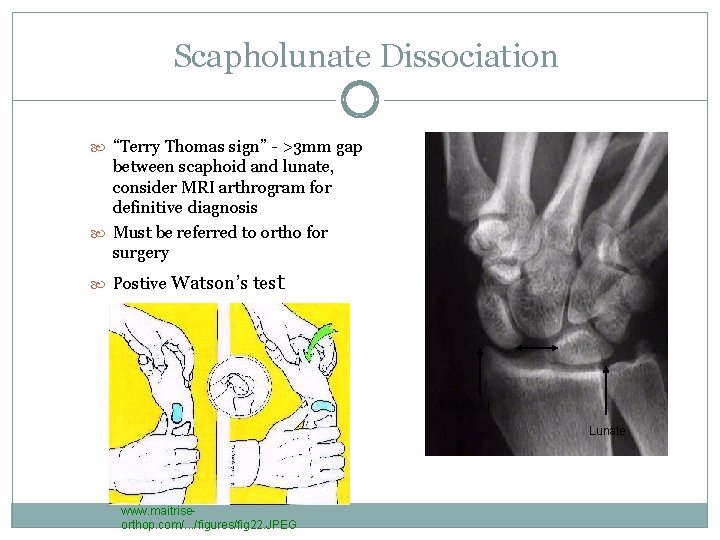
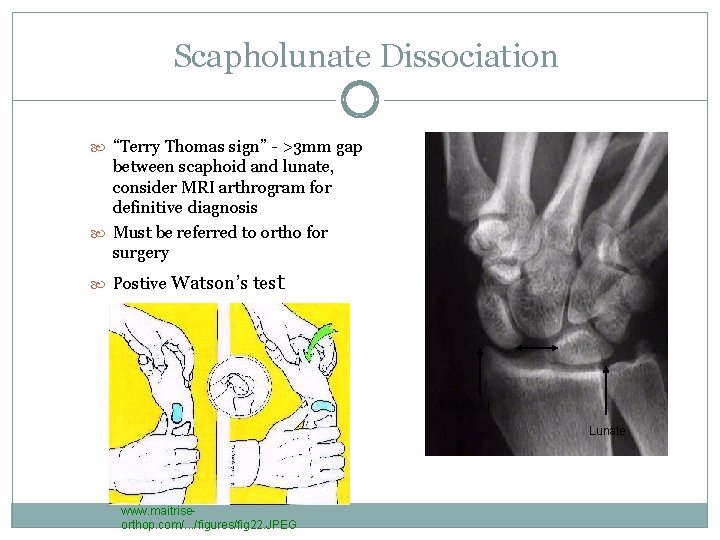
Scapholunate Dissociation “Terry Thomas sign” - >3 mm gap between scaphoid and lunate, consider MRI arthrogram for definitive diagnosis Must be referred to ortho for surgery Postive Watson’s test Scaphoid Lunate . www. maitriseorthop. com/. . . /figures/fig 22. JPEG
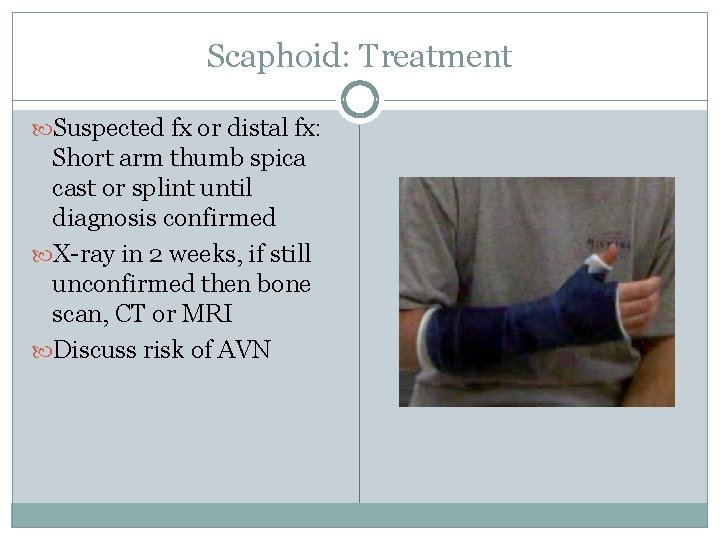
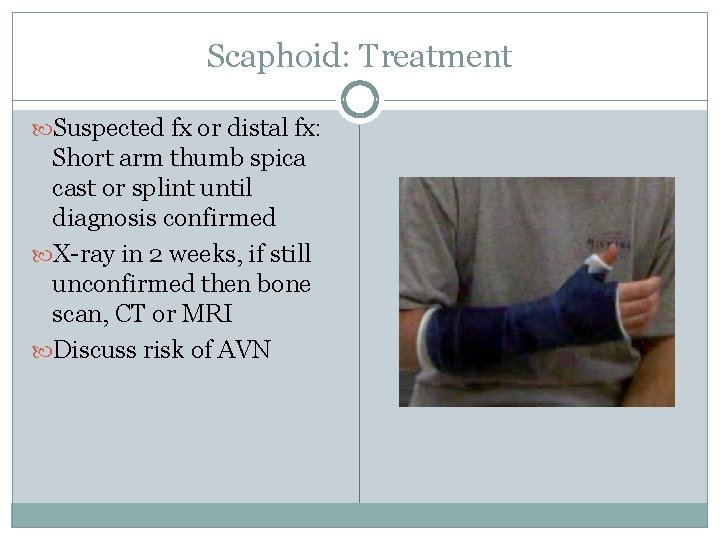
Scaphoid: Treatment Suspected fx or distal fx: Short arm thumb spica cast or splint until diagnosis confirmed X-ray in 2 weeks, if still unconfirmed then bone scan, CT or MRI Discuss risk of AVN
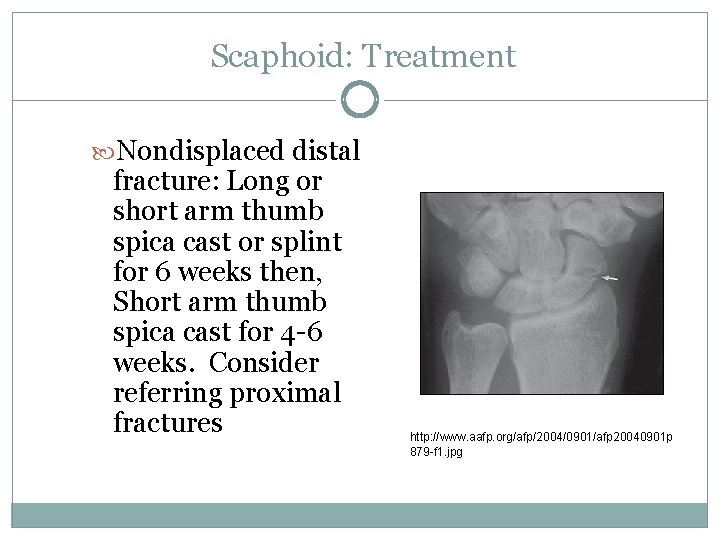
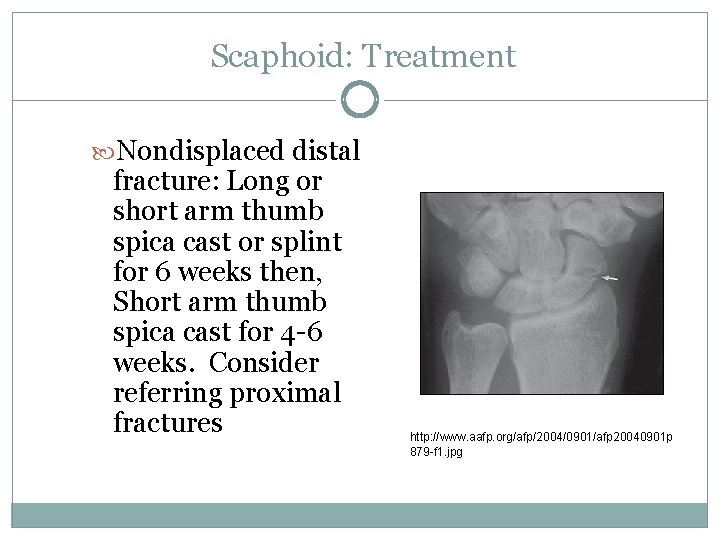
Scaphoid: Treatment Nondisplaced distal fracture: Long or short arm thumb spica cast or splint for 6 weeks then, Short arm thumb spica cast for 4 -6 weeks. Consider referring proximal fractures http: //www. aafp. org/afp/2004/0901/afp 20040901 p 879 -f 1. jpg
Case #2: Jim the Tool Man 30 yo male, well known to you, decides to give up sports, but, after watching many episodes of ‘The New Yankee Workshop, ’ wants to start building furniture. Guess what happens….
Common Hand Fractures Metacarpal Finger OUCH
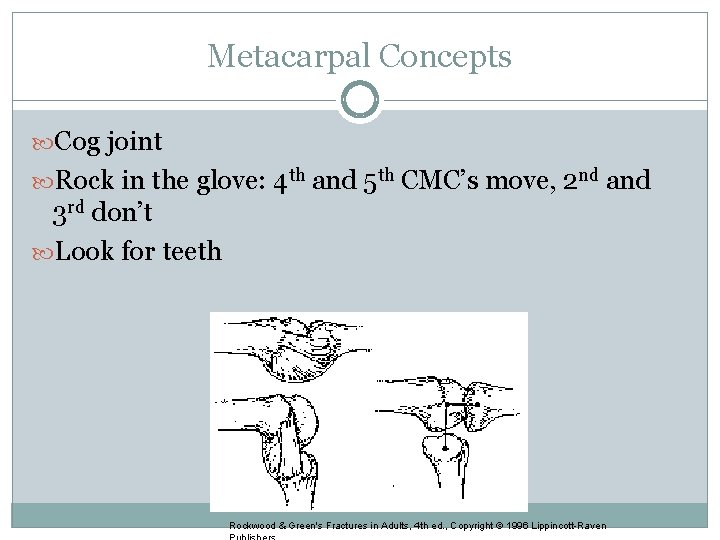
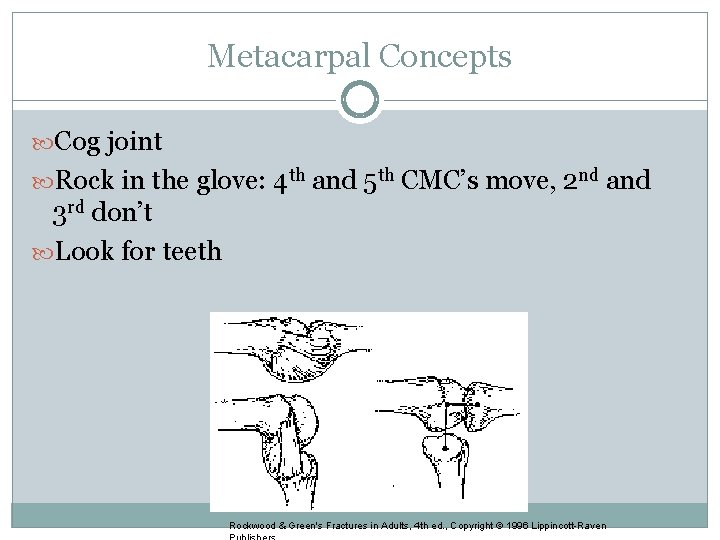
Metacarpal Concepts Cog joint Rock in the glove: 4 th and 5 th CMC’s move, 2 nd and 3 rd don’t Look for teeth Rockwood & Green's Fractures in Adults, 4 th ed. , Copyright © 1996 Lippincott-Raven
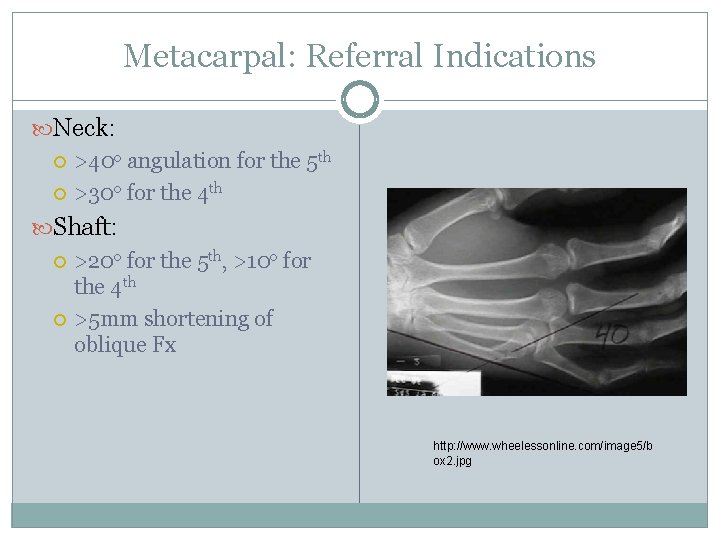
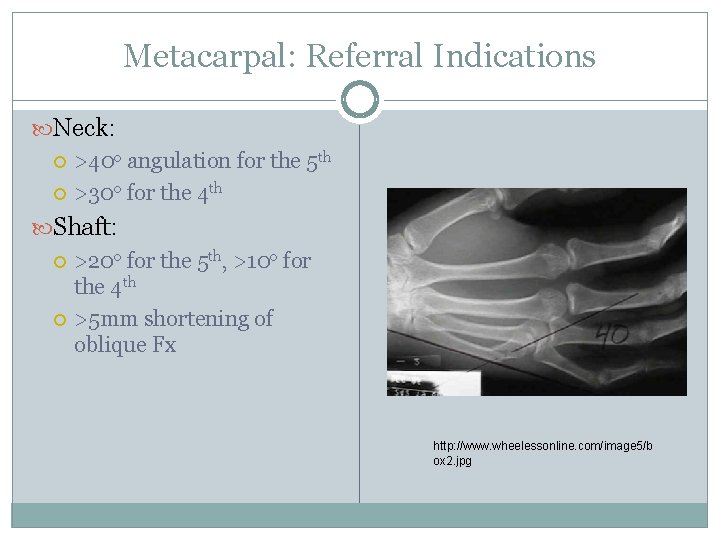
Metacarpal: Referral Indications Neck: >40 o angulation for the 5 th >30 o for the 4 th Shaft: >20 o for the 5 th, >10 o for the 4 th >5 mm shortening of oblique Fx http: //www. wheelessonline. com/image 5/b ox 2. jpg
Metacarpal: Referral Indications CANNOT TOLERATE ANY ANGULATION OF THE 2 ND OR 3 RD METACARPALS Base: 5 th metacarpal base is unstable
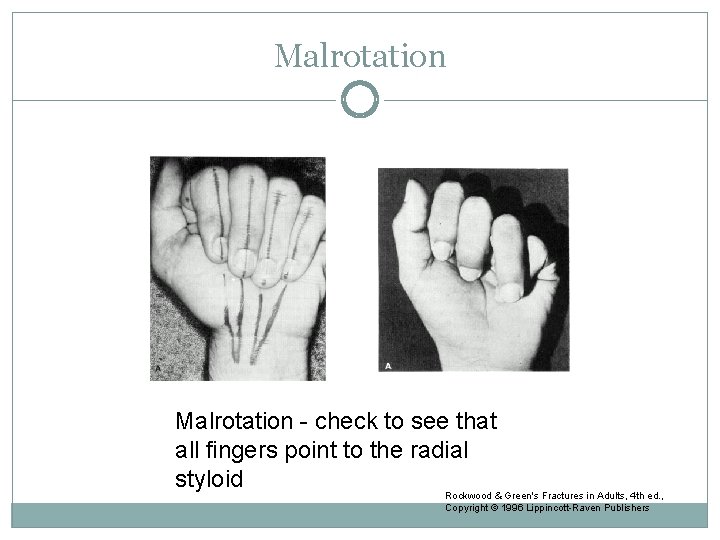
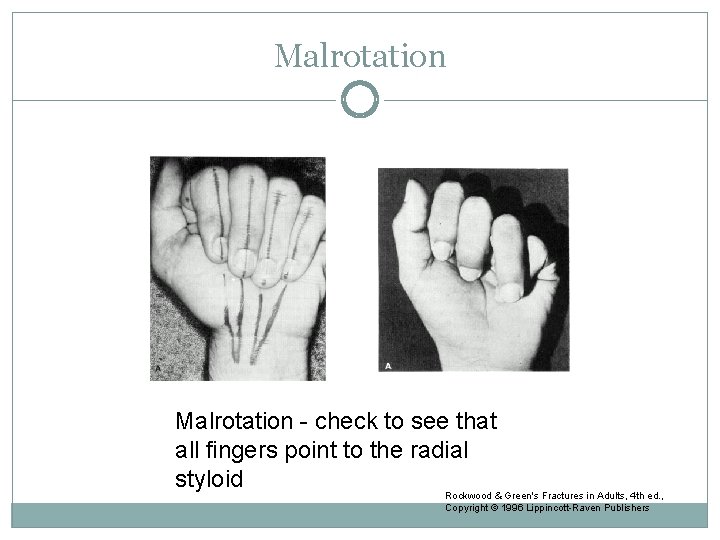
Malrotation - check to see that all fingers point to the radial styloid Rockwood & Green's Fractures in Adults, 4 th ed. , Copyright © 1996 Lippincott-Raven Publishers
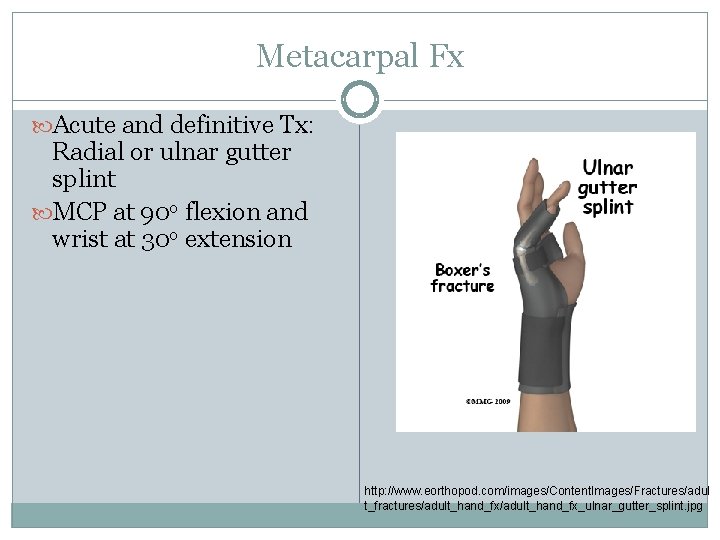
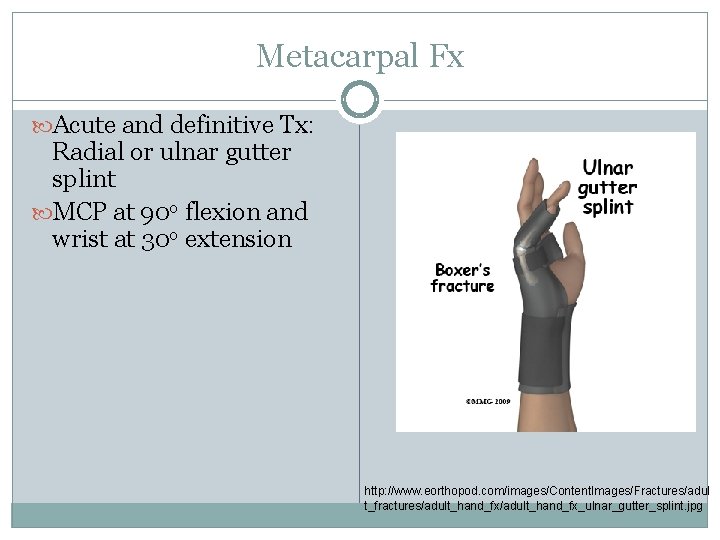
Metacarpal Fx Acute and definitive Tx: Radial or ulnar gutter splint MCP at 90 o flexion and wrist at 30 o extension http: //www. eorthopod. com/images/Content. Images/Fractures/adul t_fractures/adult_hand_fx_ulnar_gutter_splint. jpg
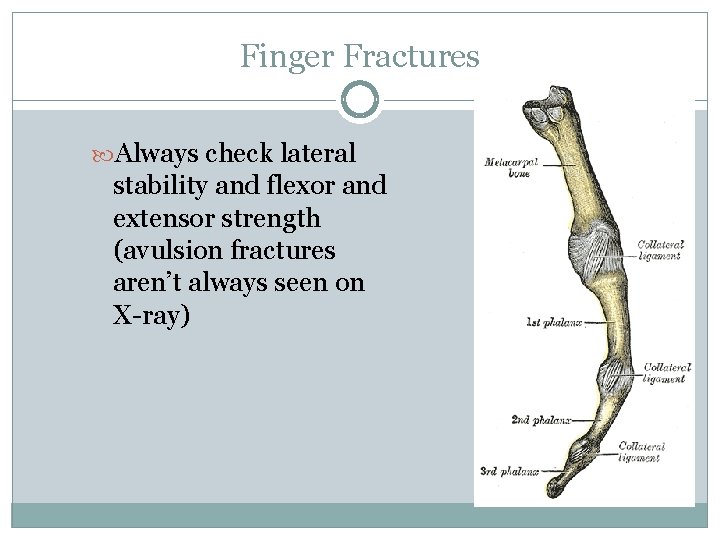
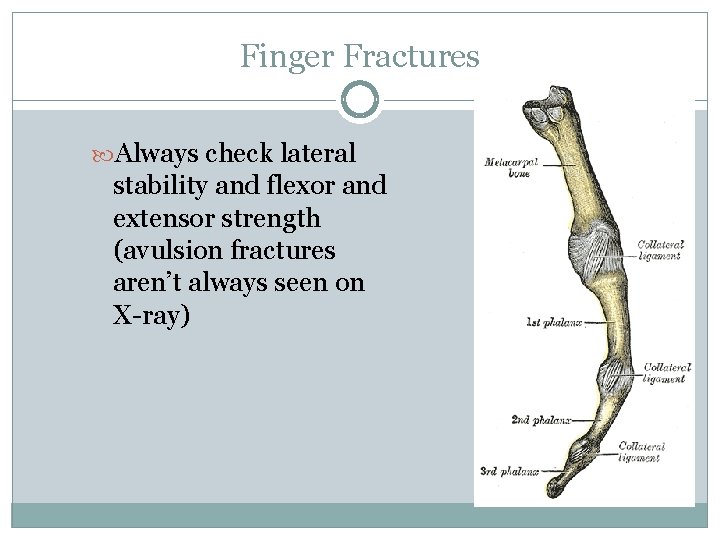
Finger Fractures Always check lateral stability and flexor and extensor strength (avulsion fractures aren’t always seen on X-ray)
Finger: Referral Indications Malrotation Oblique or spiral fractures >25 -30% articular involvement >2 mm displacement
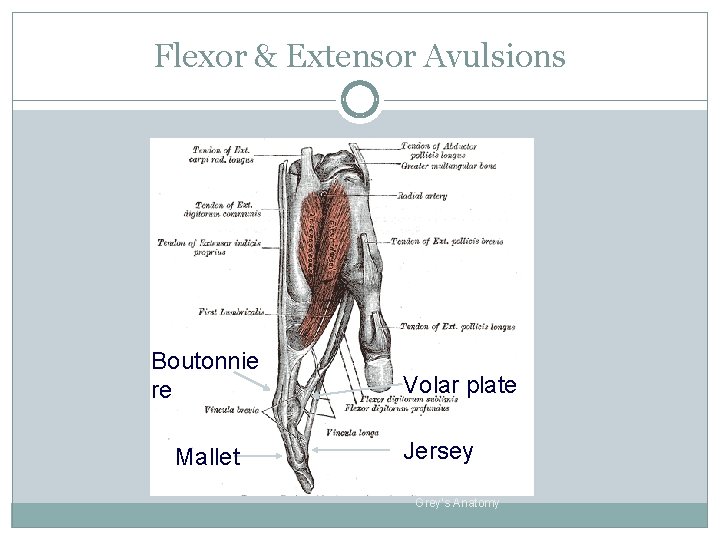
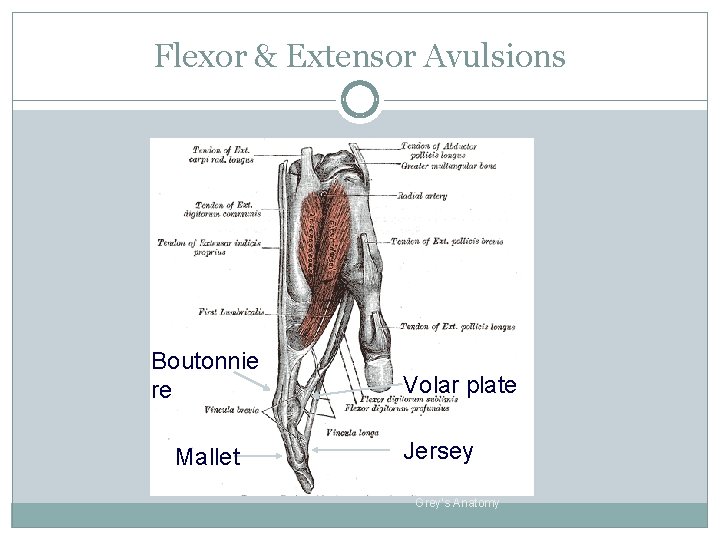
Flexor & Extensor Avulsions Boutonnie re Mallet Volar plate Jersey Grey’s Anatomy
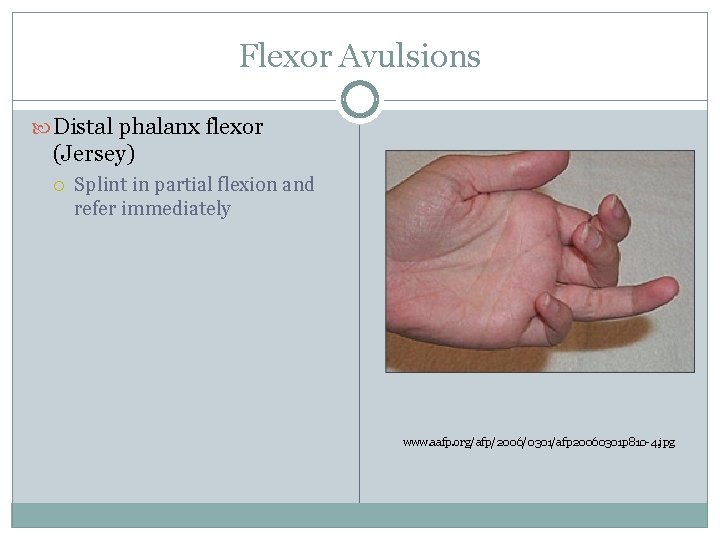
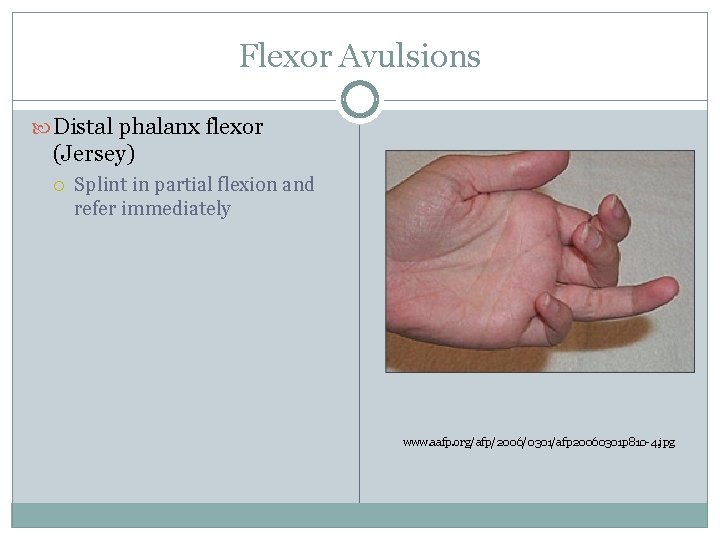
Flexor Avulsions Distal phalanx flexor (Jersey) Splint in partial flexion and refer immediately www. aafp. org/afp/2006/0301/afp 20060301 p 810 -4. jpg
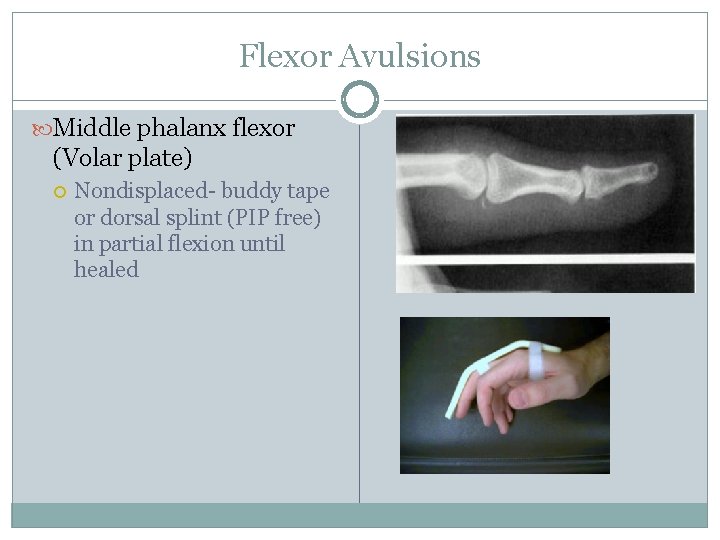
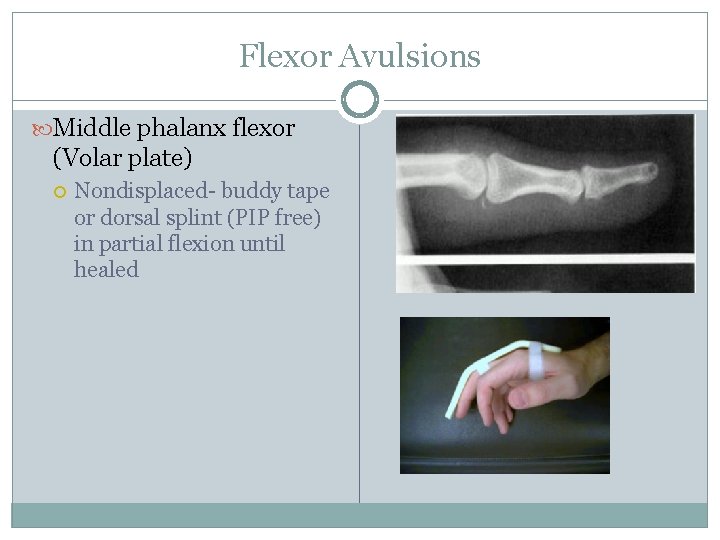
Flexor Avulsions Middle phalanx flexor (Volar plate) Nondisplaced- buddy tape or dorsal splint (PIP free) in partial flexion until healed
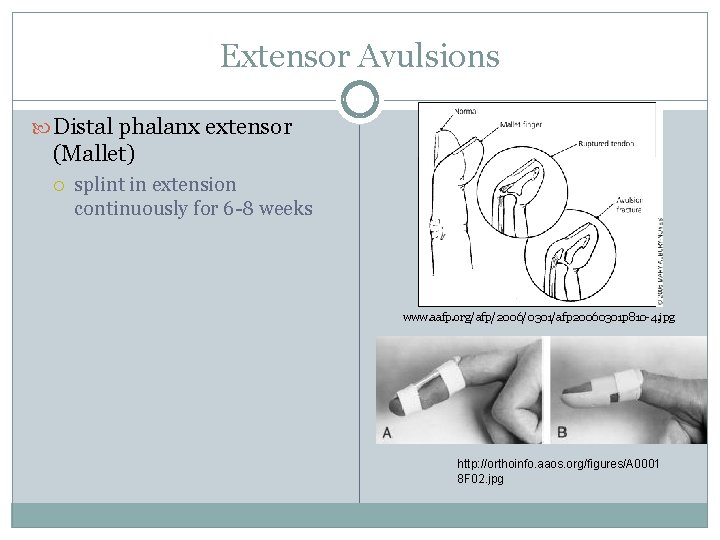
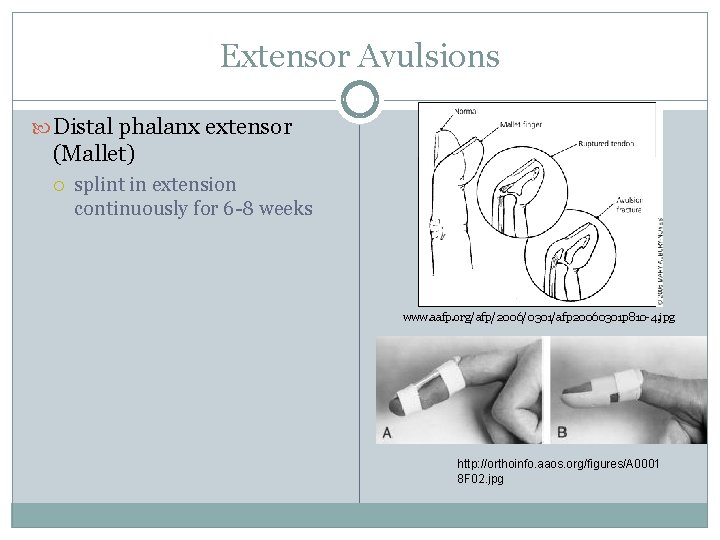
Extensor Avulsions Distal phalanx extensor (Mallet) splint in extension continuously for 6 -8 weeks www. aafp. org/afp/2006/0301/afp 20060301 p 810 -4. jpg http: //orthoinfo. aaos. org/figures/A 0001 8 F 02. jpg
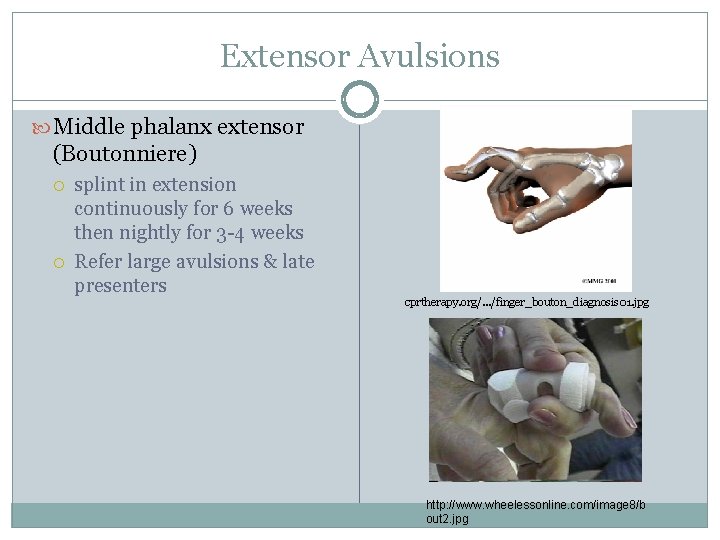
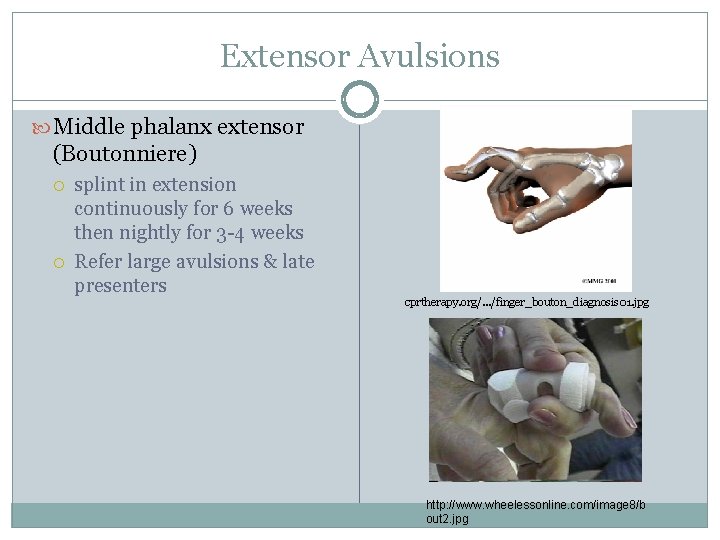
Extensor Avulsions Middle phalanx extensor (Boutonniere) splint in extension continuously for 6 weeks then nightly for 3 -4 weeks Refer large avulsions & late presenters cprtherapy. org/. . . /finger_bouton_diagnosis 01. jpg http: //www. wheelessonline. com/image 8/b out 2. jpg
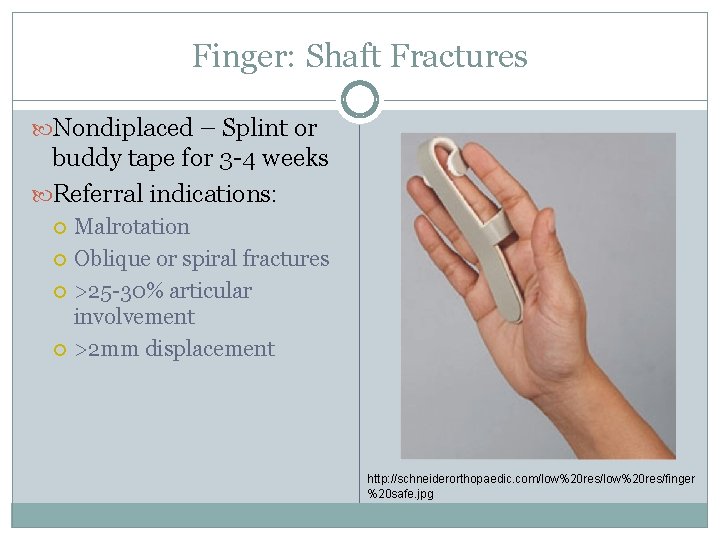
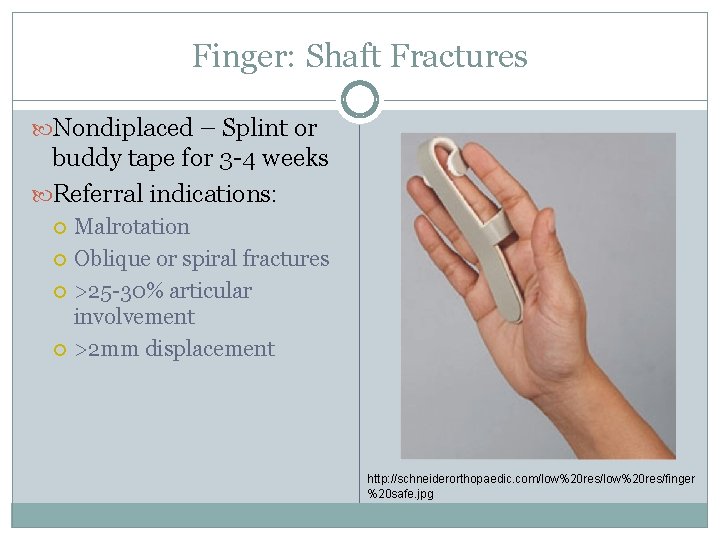
Finger: Shaft Fractures Nondiplaced – Splint or buddy tape for 3 -4 weeks Referral indications: Malrotation Oblique or spiral fractures >25 -30% articular involvement >2 mm displacement http: //schneiderorthopaedic. com/low%20 res/finger %20 safe. jpg
Case #3: Ankle Injury 29 yo female tries to train for her first marathon, but instead twists her ankle while walking out of her house.
Ankle Injuries Radiographs for ankle injuries comprise 10% of all x- rays taken in the ER Ankle injuries are the most common lower extremity injury seen in primary care practices Although injuries are common, evaluation can be far from simple
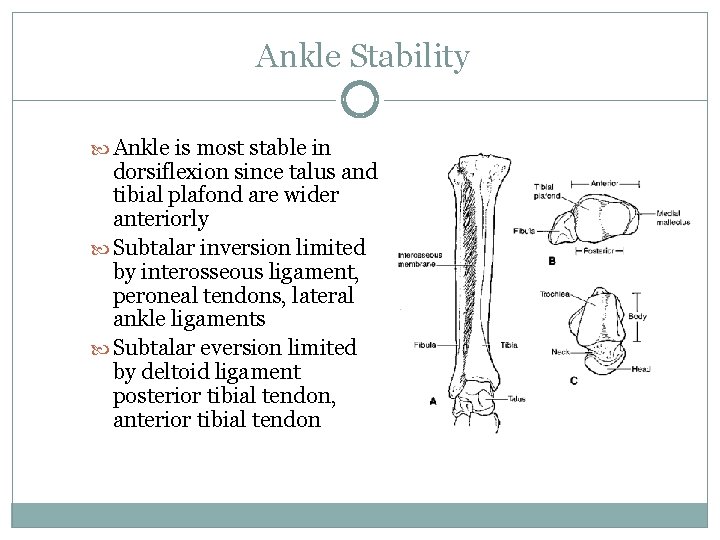
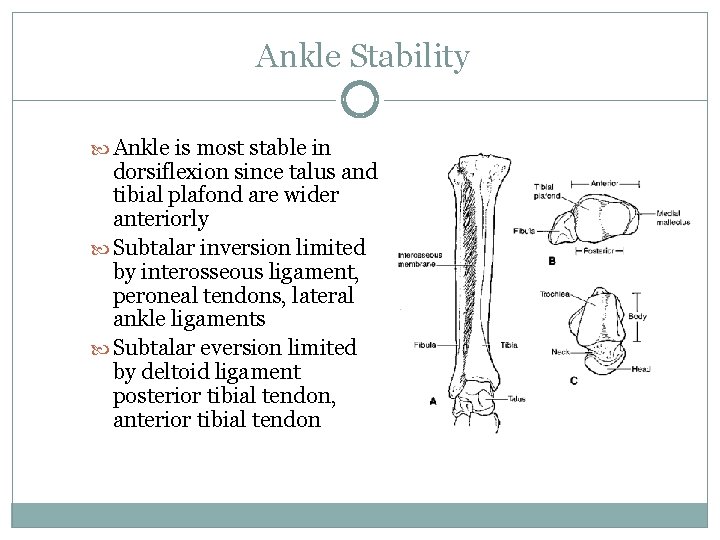
Ankle Stability Ankle is most stable in dorsiflexion since talus and tibial plafond are wider anteriorly Subtalar inversion limited by interosseous ligament, peroneal tendons, lateral ankle ligaments Subtalar eversion limited by deltoid ligament posterior tibial tendon, anterior tibial tendon
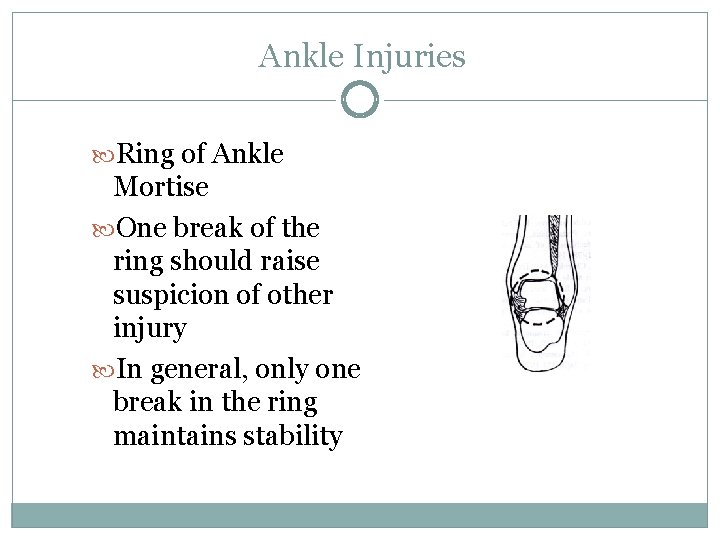
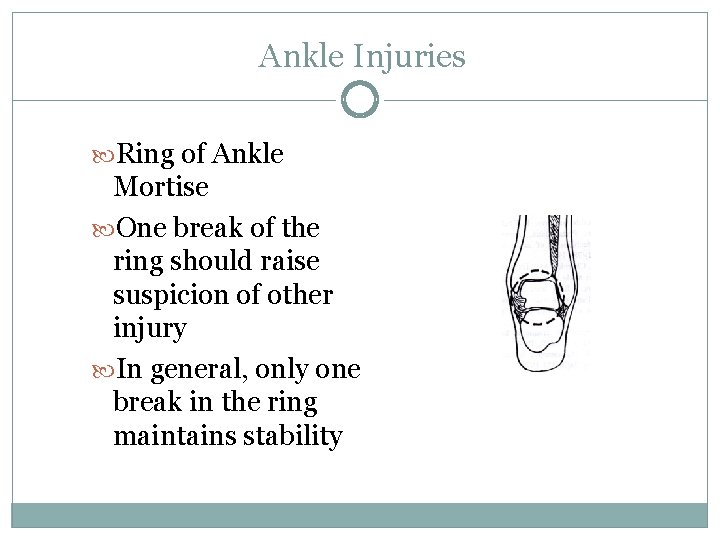
Ankle Injuries Ring of Ankle Mortise One break of the ring should raise suspicion of other injury In general, only one break in the ring maintains stability
Ankle Injury Mechanism of Injury Direction of force and position of foot often dictate pattern of injury Determining stability is key in managing and considering referral for ankle injuries
Physical Exam Areas of tenderness and swelling Check for significant medial or lateral pain Evaluate ability to stand or walk Anterior drawer test Talar tilt test Squeeze test External rotation stress test
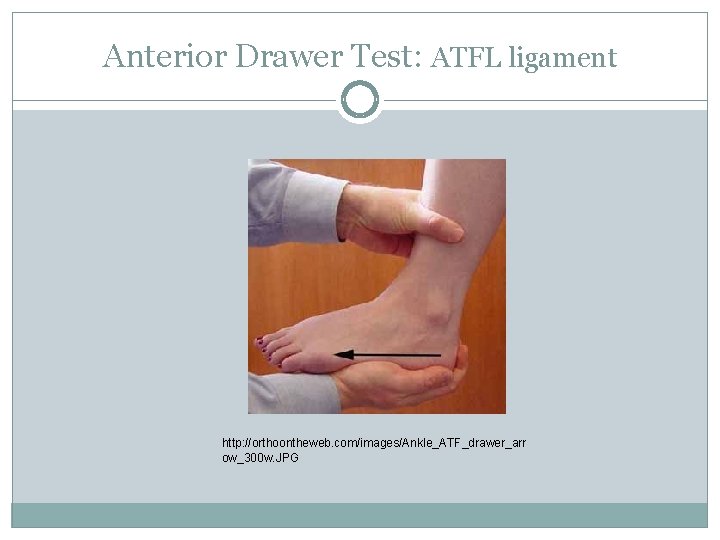
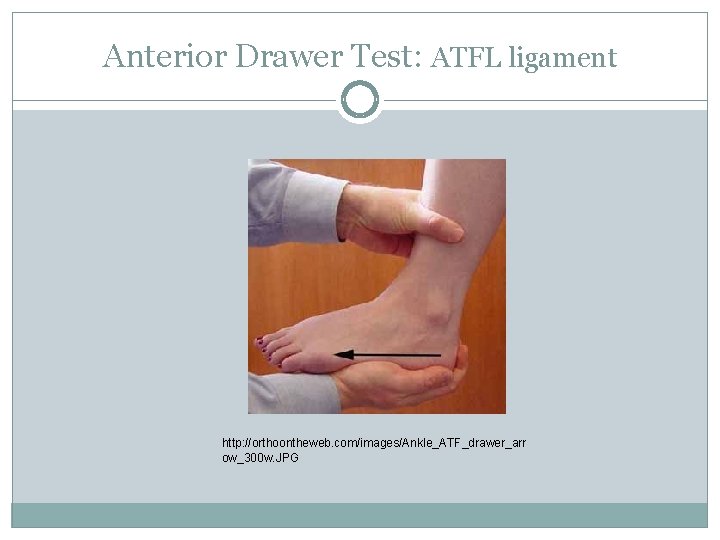
Anterior Drawer Test: ATFL ligament http: //orthoontheweb. com/images/Ankle_ATF_drawer_arr ow_300 w. JPG
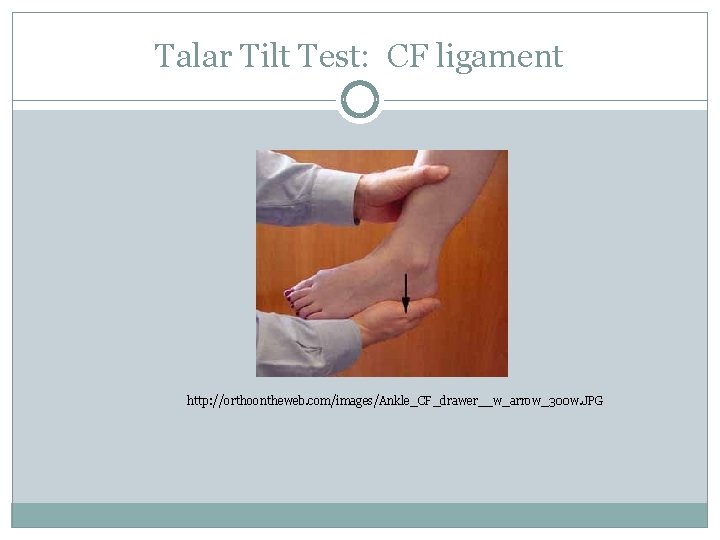
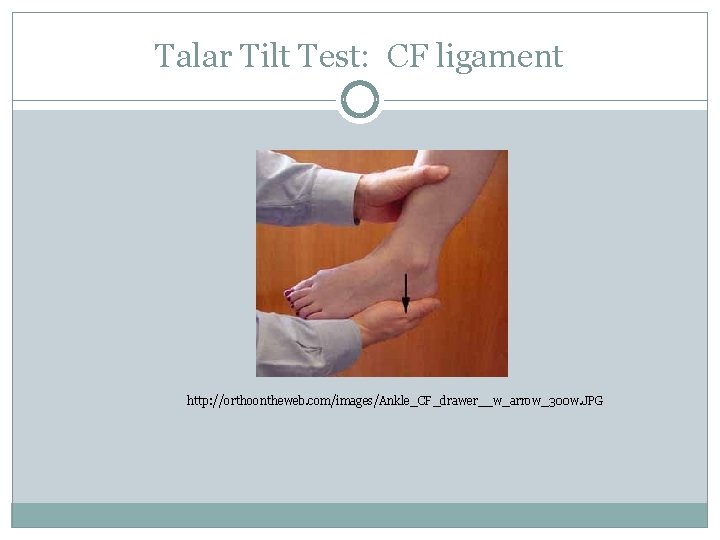
Talar Tilt Test: CF ligament http: //orthoontheweb. com/images/Ankle_CF_drawer__w_arrow_300 w. JPG
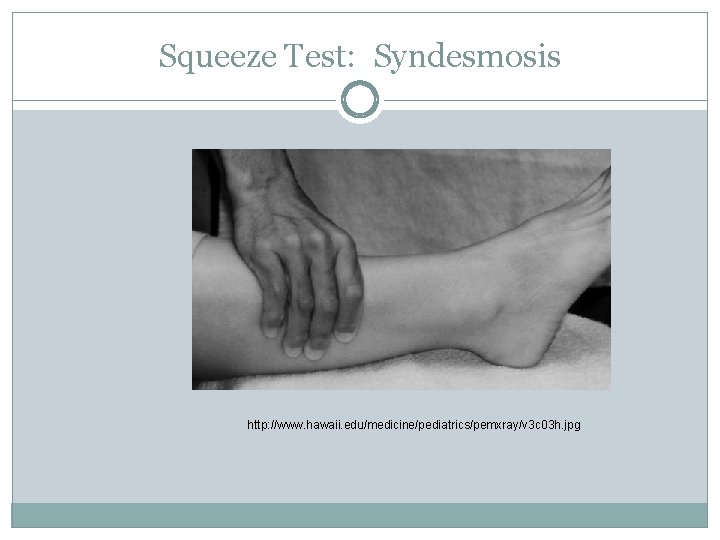
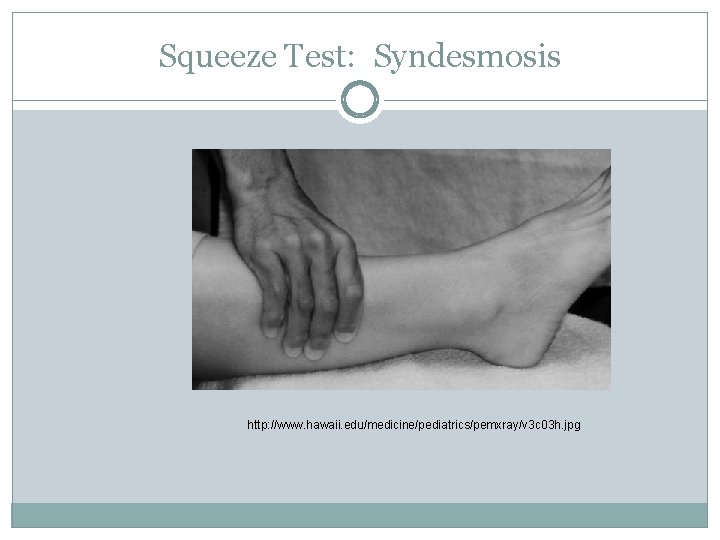
Squeeze Test: Syndesmosis http: //www. hawaii. edu/medicine/pediatrics/pemxray/v 3 c 03 h. jpg
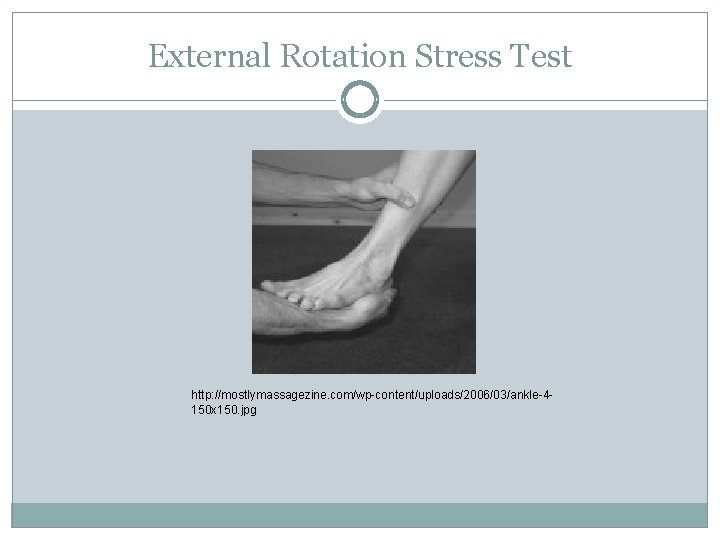
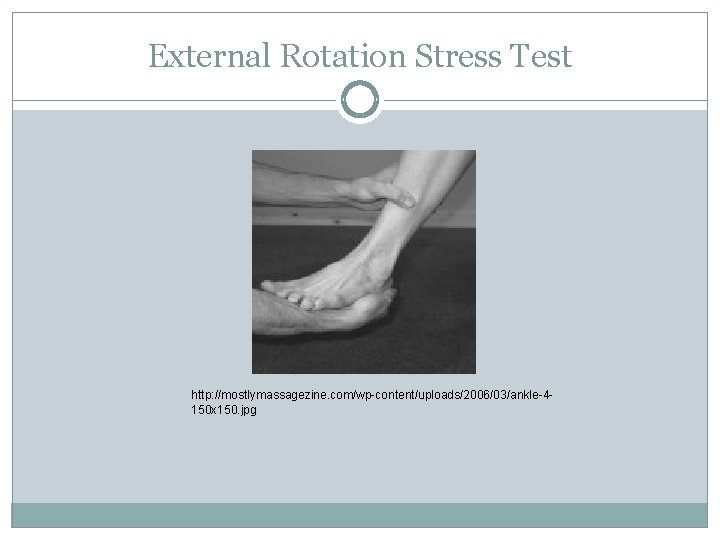
External Rotation Stress Test http: //mostlymassagezine. com/wp-content/uploads/2006/03/ankle-4150 x 150. jpg
Ottowa Rules Inability to bear weight (4 steps) immediately and in office Bony tenderness at posteror edges or tip (distal 6 cm) of either malleoli Bony tenderness at base of 5 th metatarsal or navicular (Pain in midfoot)
Ottowa Ankle Rules Not 100% sensitive, may miss small avulsion fractures More effective at ruling out fracture than ruling one in, negative predictive value 99% Intended to be applied in the acute setting
Radiographs Standard: AP, lateral, mortise Studies suggest 95% of fractures can be seen on lateral and either AP or mortise view Avulsion fractures are usually transverse, talar impact fractures are usually oblique
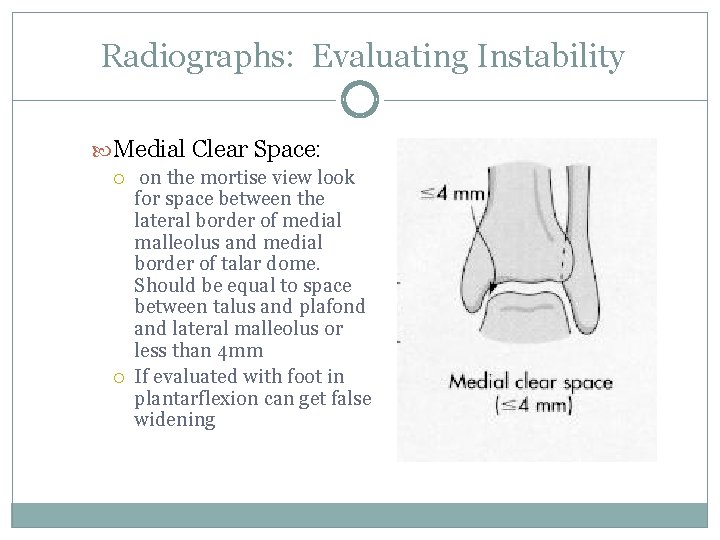
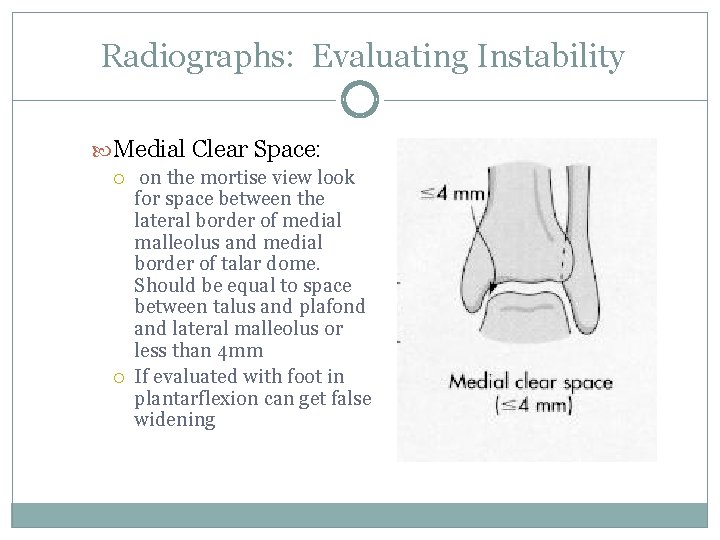
Radiographs: Evaluating Instability Medial Clear Space: on the mortise view look for space between the lateral border of medial malleolus and medial border of talar dome. Should be equal to space between talus and plafond and lateral malleolus or less than 4 mm If evaluated with foot in plantarflexion can get false widening
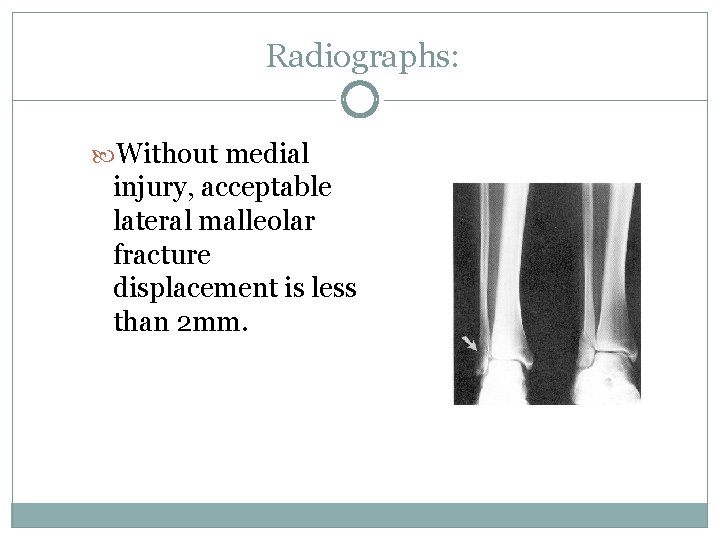
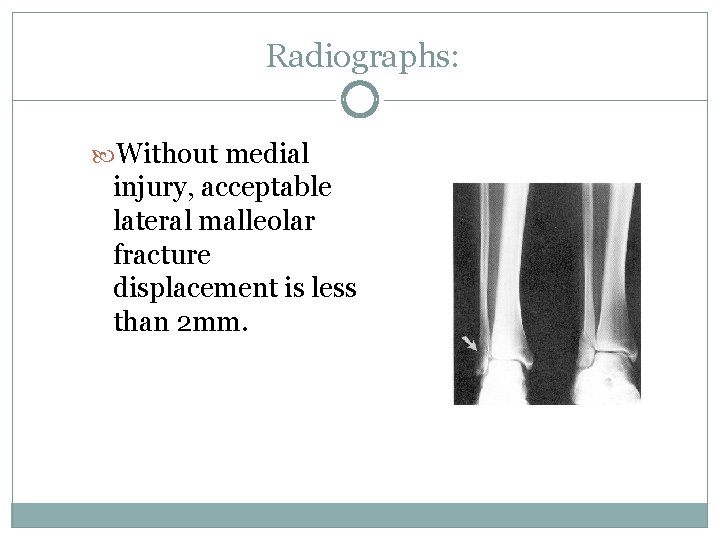
Radiographs: Without medial injury, acceptable lateral malleolar fracture displacement is less than 2 mm.
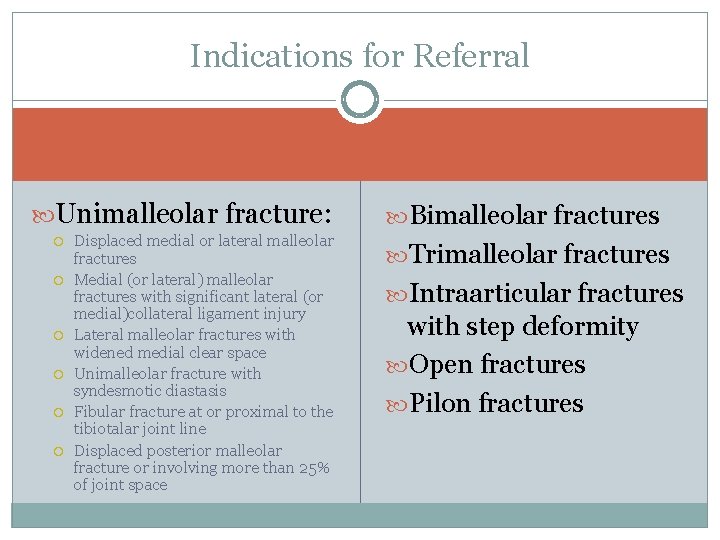
Indications for Referral Unimalleolar fracture: Displaced medial or lateral malleolar fractures Medial (or lateral) malleolar fractures with significant lateral (or medial)collateral ligament injury Lateral malleolar fractures with widened medial clear space Unimalleolar fracture with syndesmotic diastasis Fibular fracture at or proximal to the tibiotalar joint line Displaced posterior malleolar fracture or involving more than 25% of joint space Bimalleolar fractures Trimalleolar fractures Intraarticular fractures with step deformity Open fractures Pilon fractures
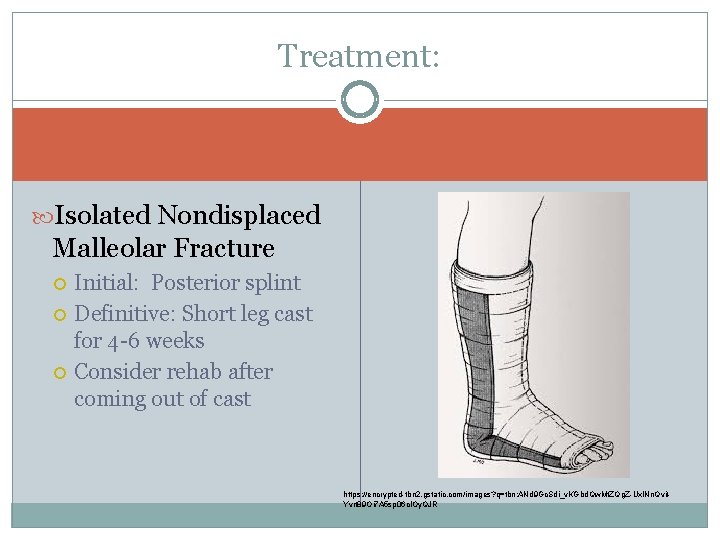
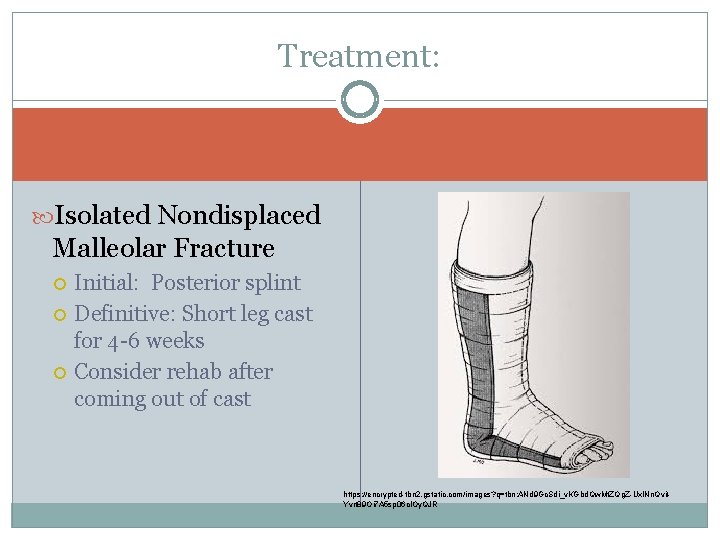
Treatment: Isolated Nondisplaced Malleolar Fracture Initial: Posterior splint Definitive: Short leg cast for 4 -6 weeks Consider rehab after coming out of cast https: //encrypted-tbn 2. gstatic. com/images? q=tbn: ANd 9 Gc. Sdi_v. KGbd. Qw. Mt. ZQg. Z-Uxl. Nn. Qvit. Yvrt 89 Oi 7 A 5 sp 06 cl. Oy. QJR
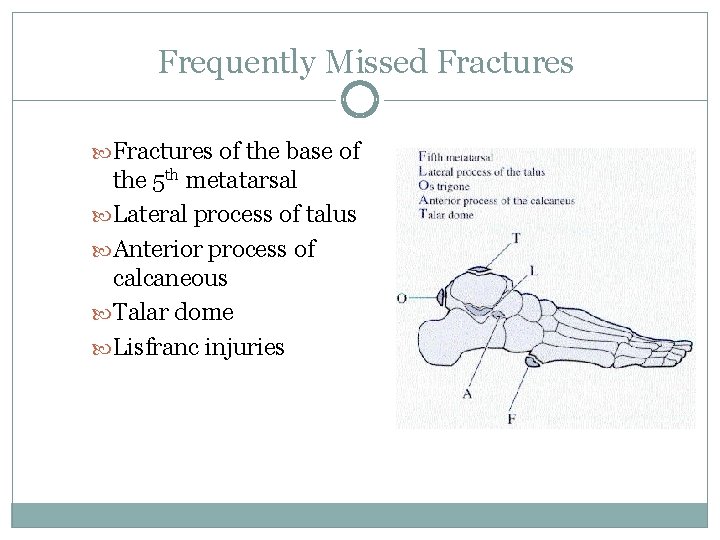
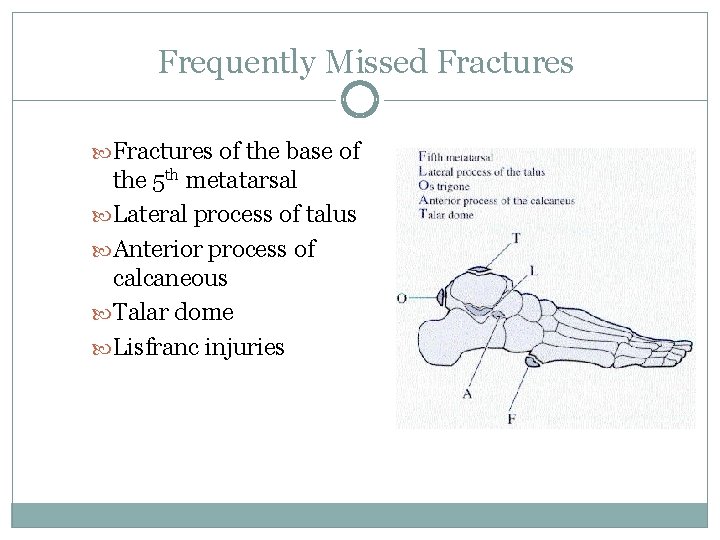
Frequently Missed Fractures of the base of the 5 th metatarsal Lateral process of talus Anterior process of calcaneous Talar dome Lisfranc injuries
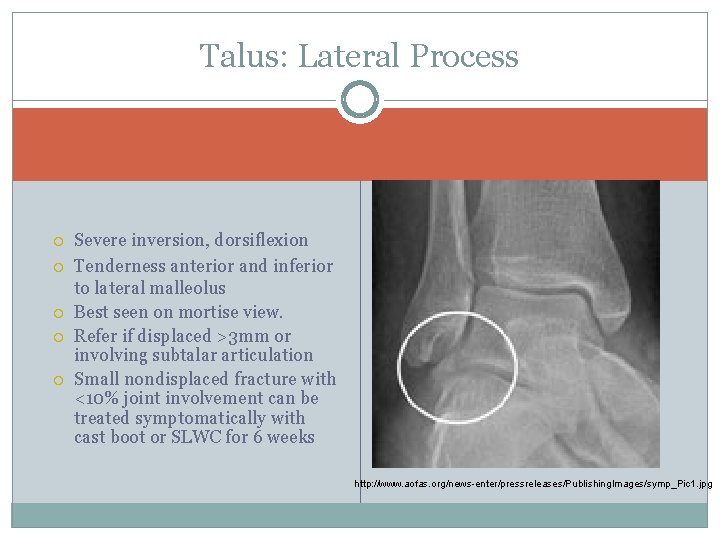
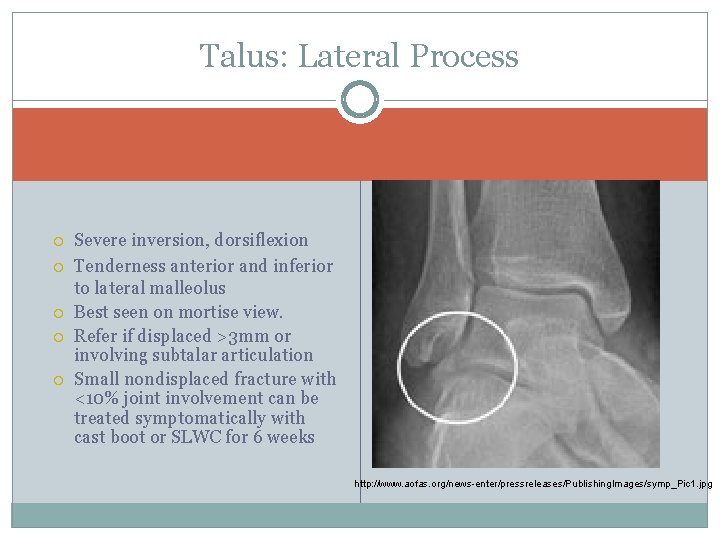
Talus: Lateral Process Severe inversion, dorsiflexion Tenderness anterior and inferior to lateral malleolus Best seen on mortise view. Refer if displaced >3 mm or involving subtalar articulation Small nondisplaced fracture with <10% joint involvement can be treated symptomatically with cast boot or SLWC for 6 weeks http: //www. aofas. org/news-enter/pressreleases/Publishing. Images/symp_Pic 1. jpg
Talar Dome Osteochondral Lesions 49% incidence of injury to articular cartilage of talar dome with malleolar fractures Suspect with persistant pain with weight bearing, persistant swelling, locking or crepitance Often need CT or MRI to determine extent of injury
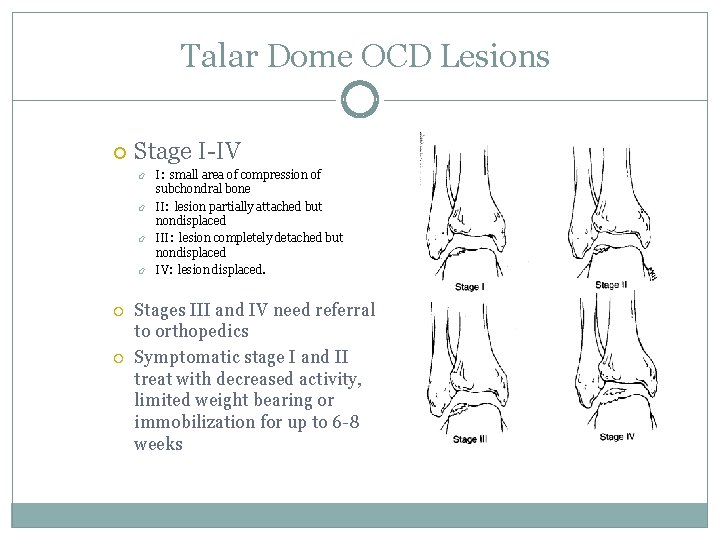
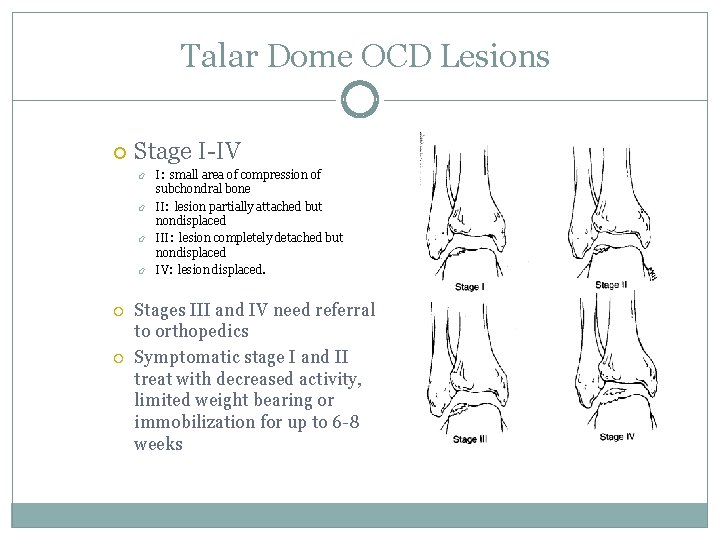
Talar Dome OCD Lesions Stage I-IV I: small area of compression of subchondral bone II: lesion partially attached but nondisplaced III: lesion completely detached but nondisplaced IV: lesion displaced. Stages III and IV need referral to orthopedics Symptomatic stage I and II treat with decreased activity, limited weight bearing or immobilization for up to 6 -8 weeks
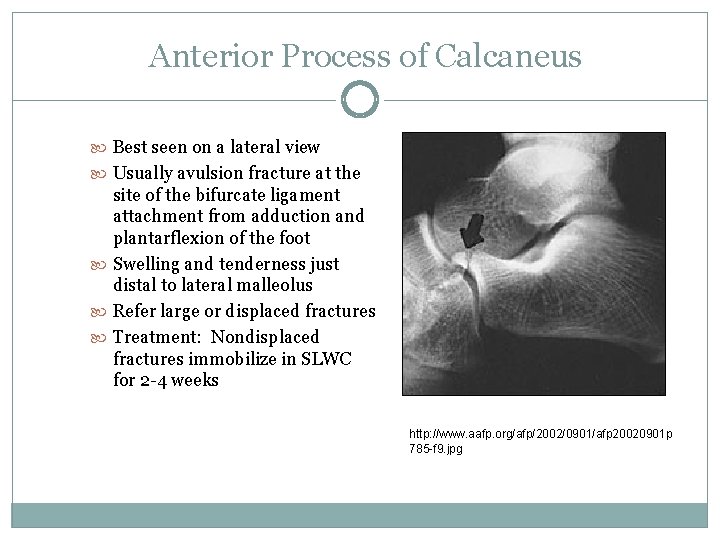
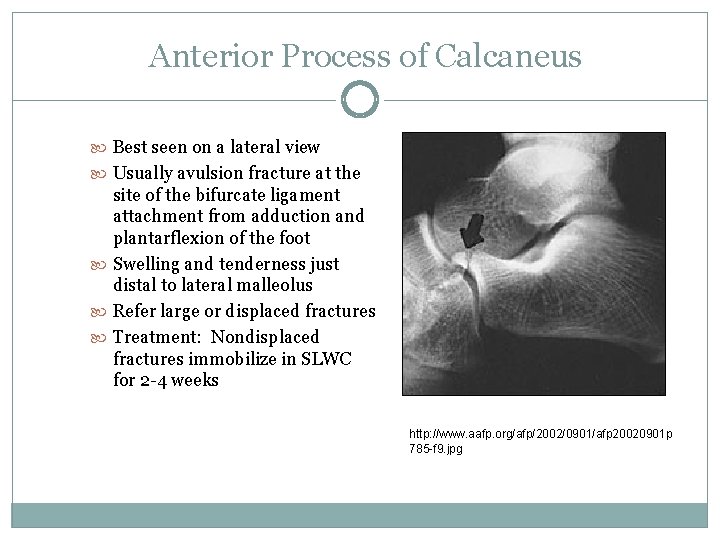
Anterior Process of Calcaneus Best seen on a lateral view Usually avulsion fracture at the site of the bifurcate ligament attachment from adduction and plantarflexion of the foot Swelling and tenderness just distal to lateral malleolus Refer large or displaced fractures Treatment: Nondisplaced fractures immobilize in SLWC for 2 -4 weeks http: //www. aafp. org/afp/2002/0901/afp 20020901 p 785 -f 9. jpg
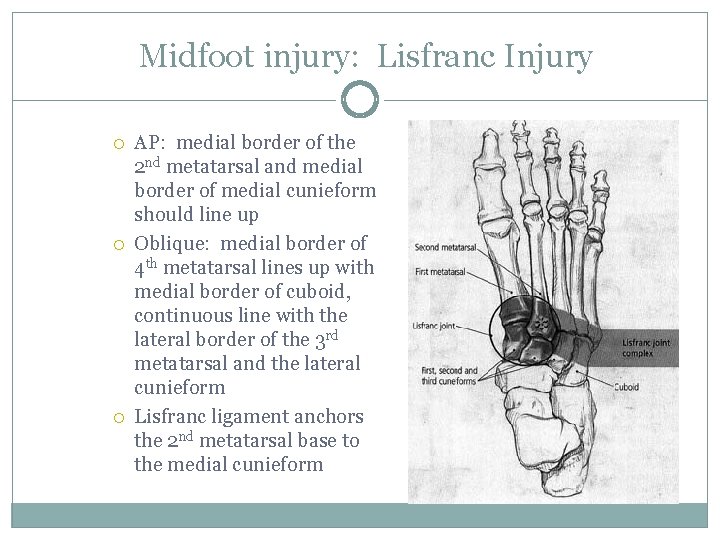
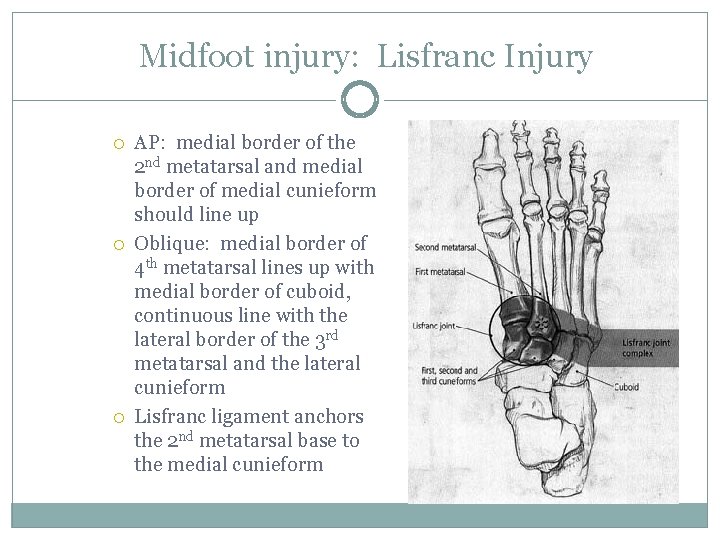
Midfoot injury: Lisfranc Injury AP: medial border of the 2 nd metatarsal and medial border of medial cunieform should line up Oblique: medial border of 4 th metatarsal lines up with medial border of cuboid, continuous line with the lateral border of the 3 rd metatarsal and the lateral cunieform Lisfranc ligament anchors the 2 nd metatarsal base to the medial cunieform
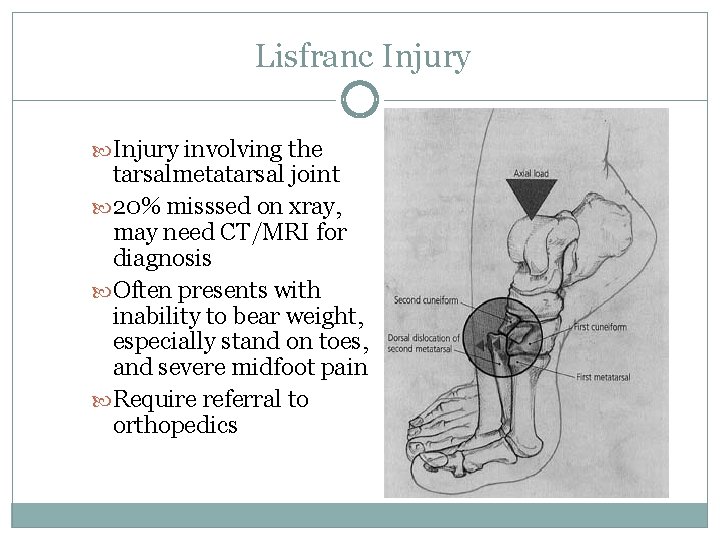
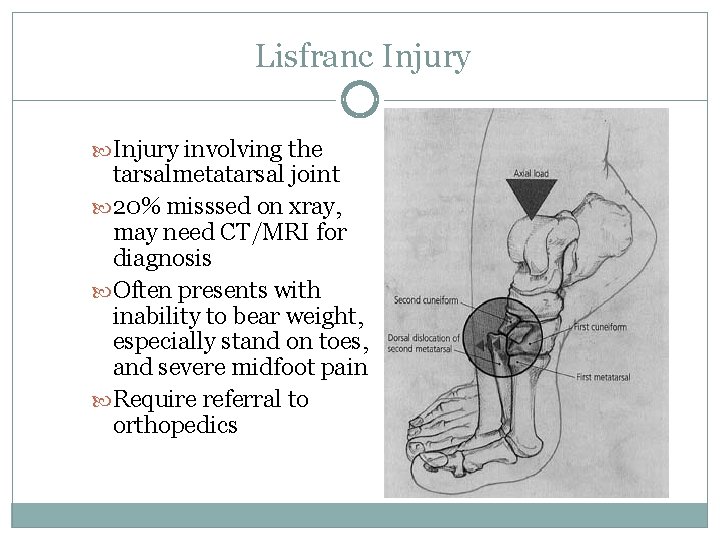
Lisfranc Injury involving the tarsalmetatarsal joint 20% misssed on xray, may need CT/MRI for diagnosis Often presents with inability to bear weight, especially stand on toes, and severe midfoot pain Require referral to orthopedics
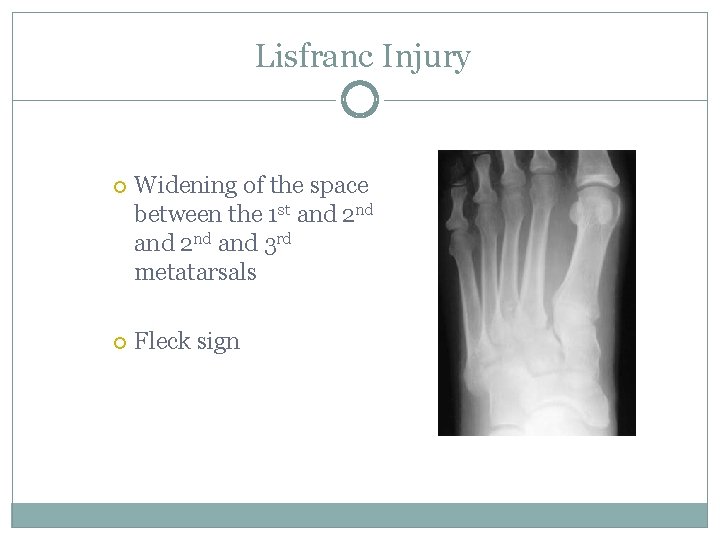
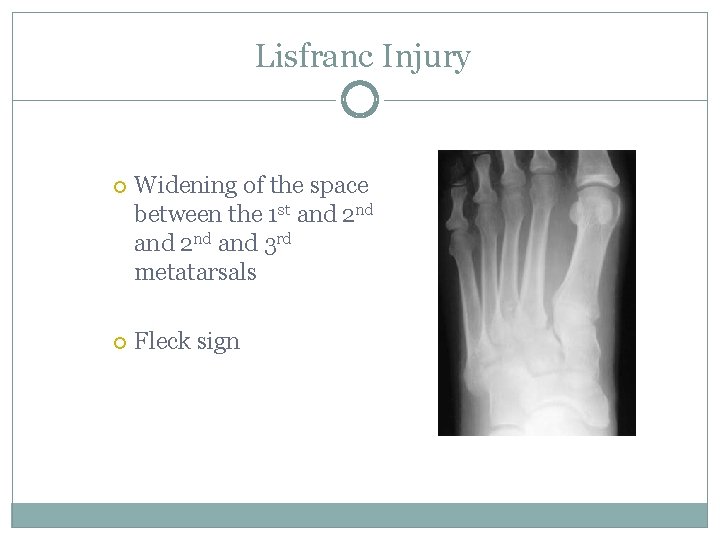
Lisfranc Injury Widening of the space between the 1 st and 2 nd and 3 rd metatarsals Fleck sign
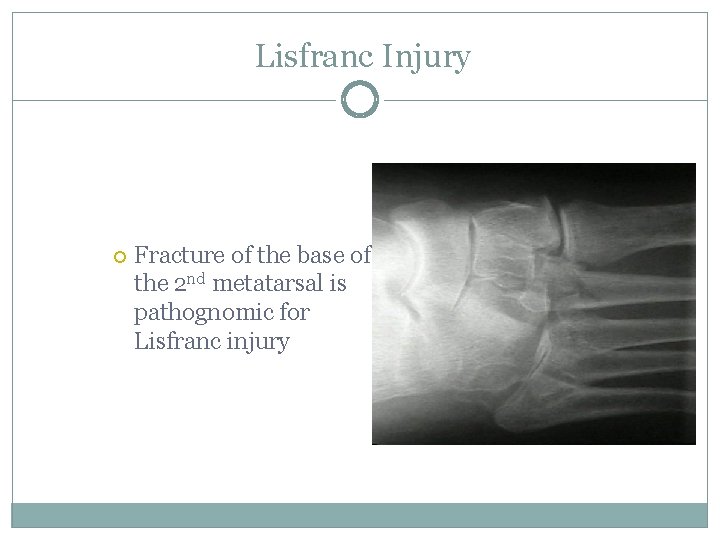
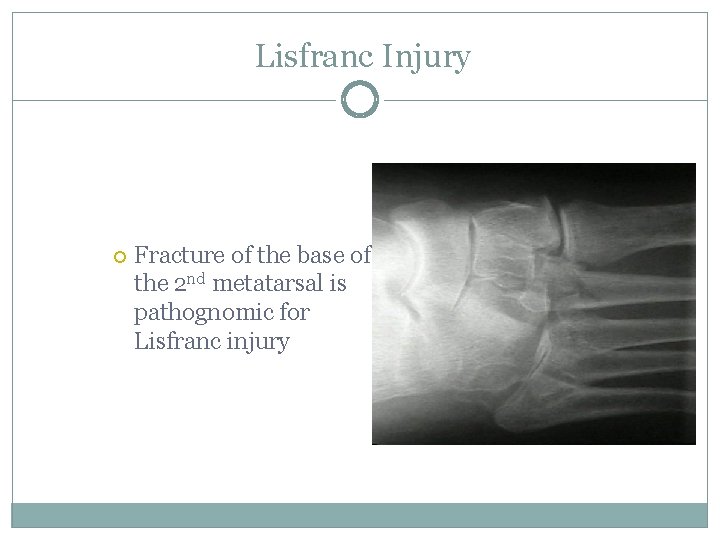
Lisfranc Injury Fracture of the base of the 2 nd metatarsal is pathognomic for Lisfranc injury
Case #4: Reading time 29 yo female after having her cast removed decided to get back to work…. . of course she injures herself when she drops her reading material on her foot.
Foot Fractures: Forefoot Metatarsal Phalangeal
Metatarsal Fractures Metatarsal Shaft Fractures Often due to direct blow or twisting Difficulty weight bearing and tenderness over fracture site Standard radiographs: AP, lateral and oblique
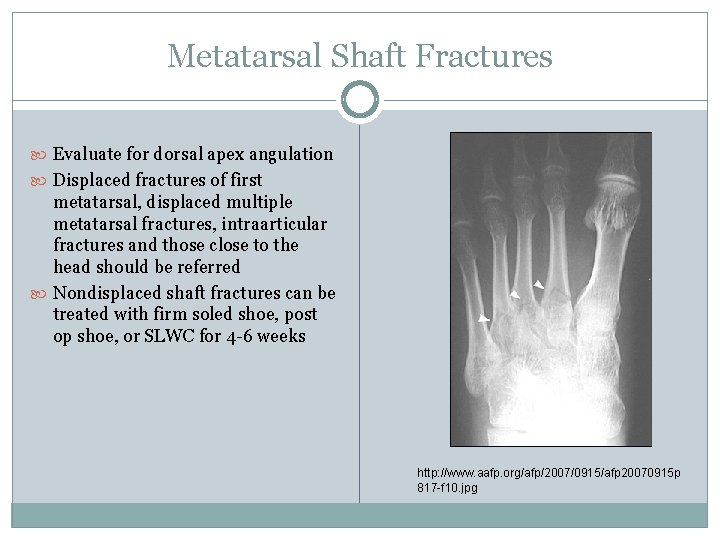
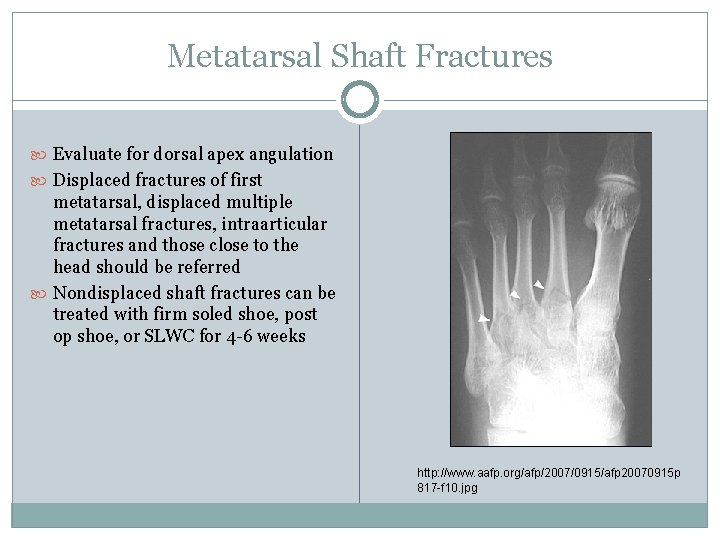
Metatarsal Shaft Fractures Evaluate for dorsal apex angulation Displaced fractures of first metatarsal, displaced multiple metatarsal fractures, intraarticular fractures and those close to the head should be referred Nondisplaced shaft fractures can be treated with firm soled shoe, post op shoe, or SLWC for 4 -6 weeks http: //www. aafp. org/afp/2007/0915/afp 20070915 p 817 -f 10. jpg
Proximal 5 th Metatarsal Fractures Proper triage of fractures of this area are key to successful treatment Evaluate with the standard foot series Determine which “zone’ area the fracture involves
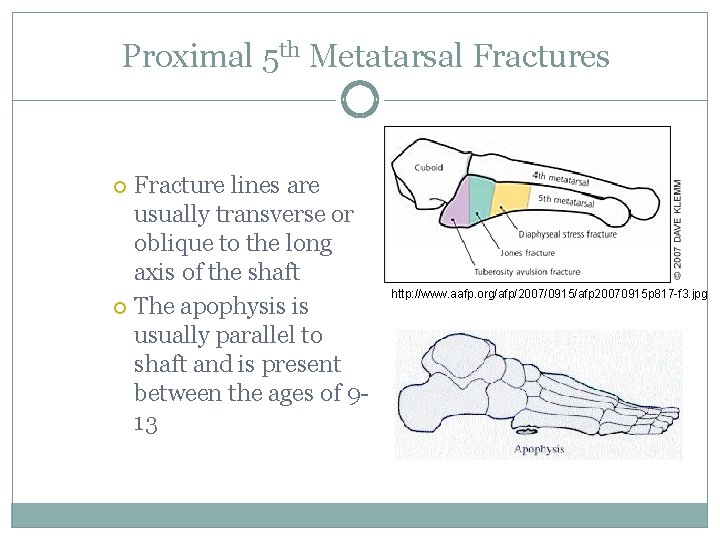
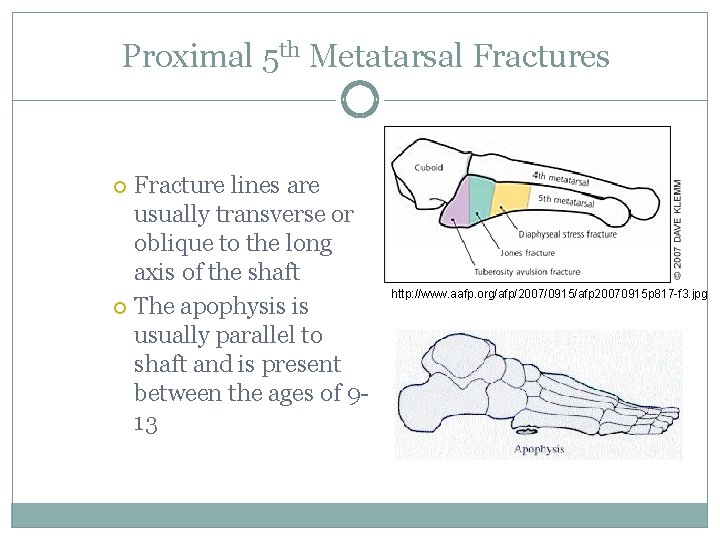
Proximal 5 th Metatarsal Fractures Fracture lines are usually transverse or oblique to the long axis of the shaft The apophysis is usually parallel to shaft and is present between the ages of 913 http: //www. aafp. org/afp/2007/0915/afp 20070915 p 817 -f 3. jpg
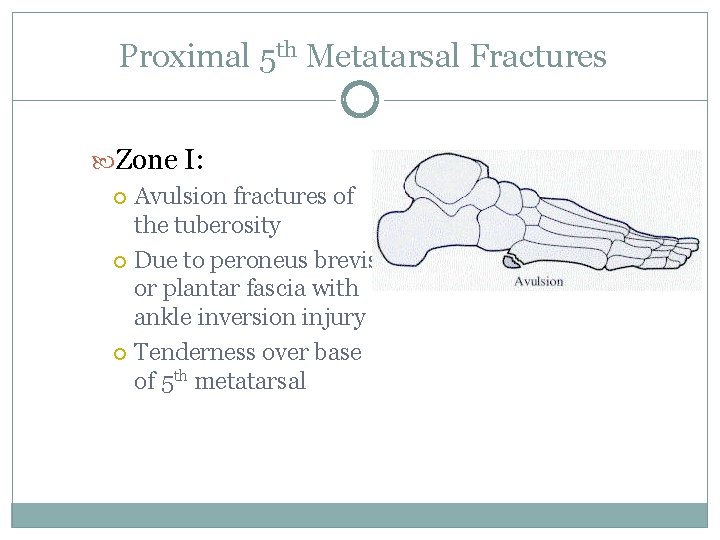
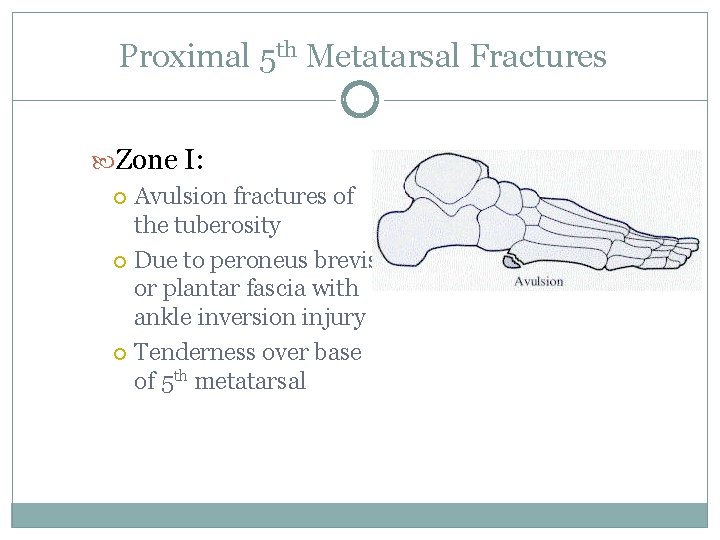
Proximal 5 th Metatarsal Fractures Zone I: Avulsion fractures of the tuberosity Due to peroneus brevis or plantar fascia with ankle inversion injury Tenderness over base of 5 th metatarsal
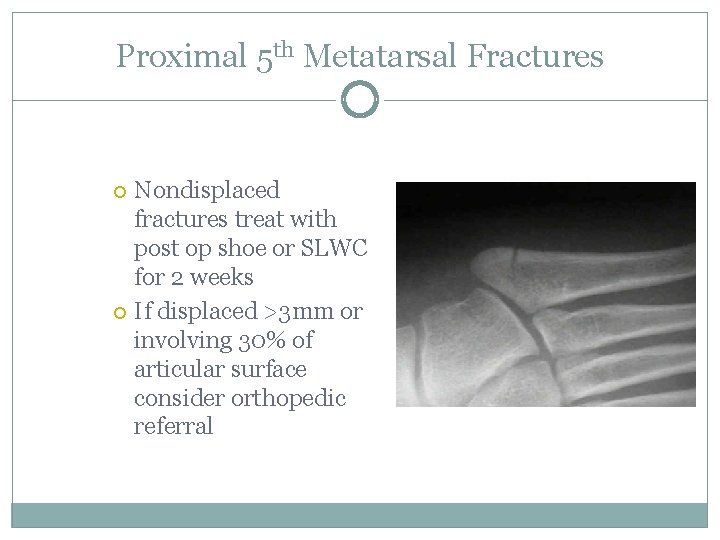
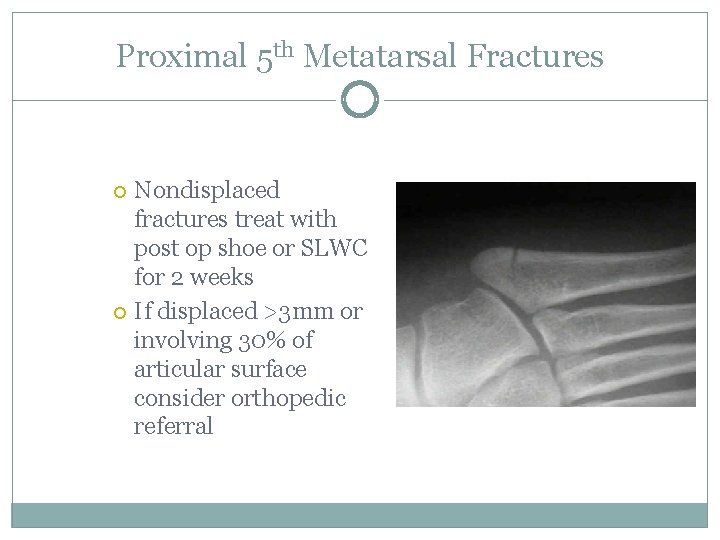
Proximal 5 th Metatarsal Fractures Nondisplaced fractures treat with post op shoe or SLWC for 2 weeks If displaced >3 mm or involving 30% of articular surface consider orthopedic referral
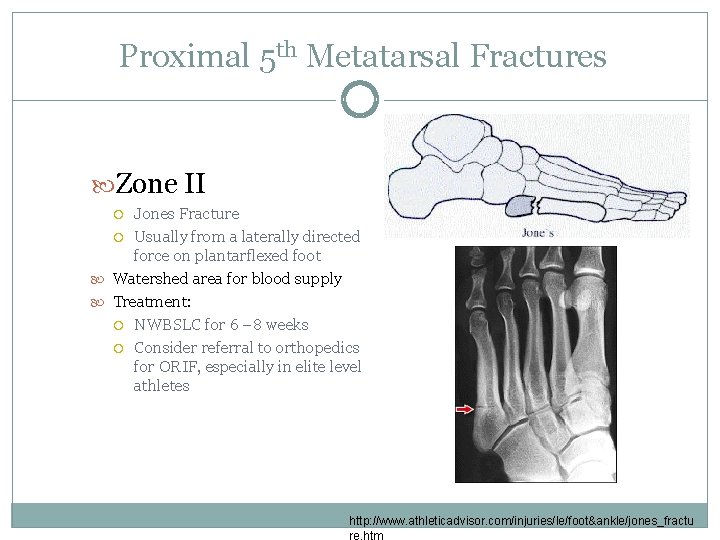
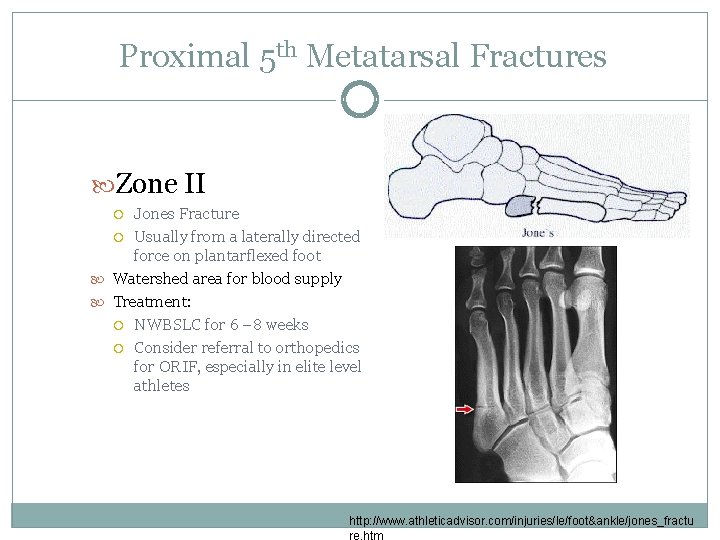
Proximal 5 th Metatarsal Fractures Zone II Jones Fracture Usually from a laterally directed force on plantarflexed foot Watershed area for blood supply Treatment: NWBSLC for 6 – 8 weeks Consider referral to orthopedics for ORIF, especially in elite level athletes http: //www. athleticadvisor. com/injuries/le/foot&ankle/jones_fractu re. htm
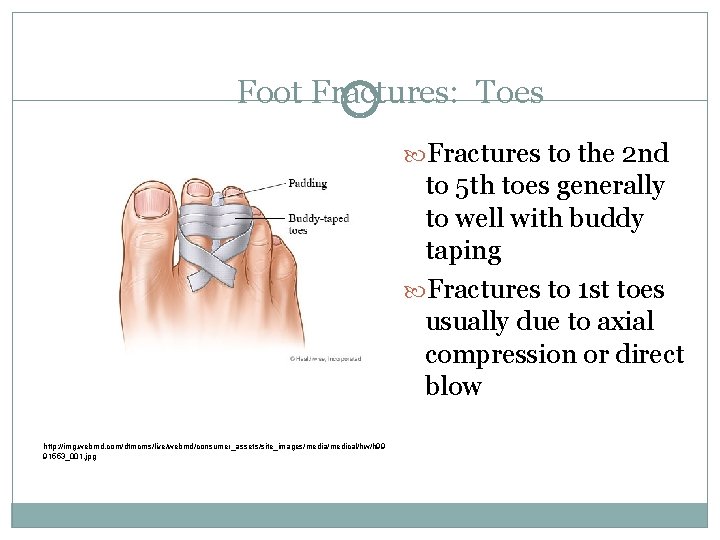
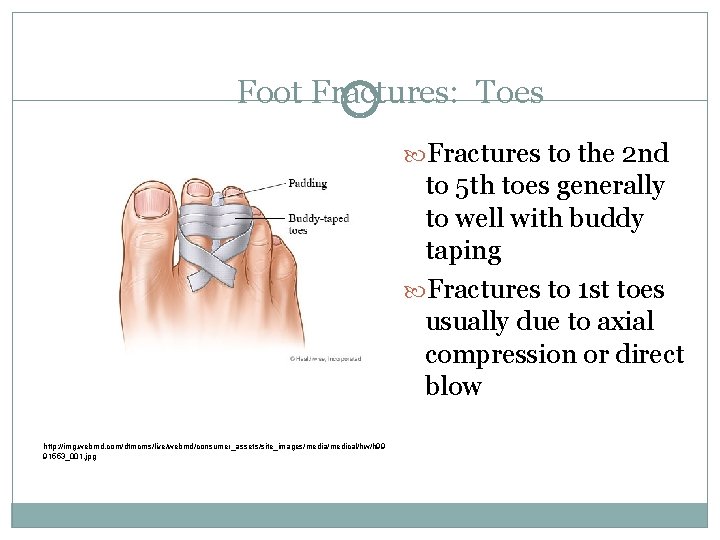
Foot Fractures: Toes Fractures to the 2 nd to 5 th toes generally to well with buddy taping Fractures to 1 st toes usually due to axial compression or direct blow http: //img. webmd. com/dtmcms/live/webmd/consumer_assets/site_images/media/medical/hw/h 99 91553_001. jpg
Refer to an orthopedist for any of the following: Intraarticular Severe comminution Inability to maintain reduction Nerve or vascular injury CRP Open Fractures Nonunion Pathologic fractures
Other Fracture Concepts Always look at the radiographs yourself Be aware of potential poor outcomes Manage fractures that you are comfortable with
 Hip fracture care clinical care standard
Hip fracture care clinical care standard Ductile fracture
Ductile fracture Primary care secondary care tertiary care
Primary care secondary care tertiary care Dept nmr spectroscopy
Dept nmr spectroscopy Department of agriculture consumer services
Department of agriculture consumer services Finance dept structure
Finance dept structure Worcester building department
Worcester building department Dept. name of organization
Dept. name of organization Mn dept of education
Mn dept of education Department of finance and administration
Department of finance and administration Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Ohio employment first
Ohio employment first Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Vaginal dept
Vaginal dept Gome dept
Gome dept Gome dept
Gome dept Nyttofunktion
Nyttofunktion Gome dept
Gome dept Hoe dept
Hoe dept Lafd interview score
Lafd interview score Maine department of agriculture conservation and forestry
Maine department of agriculture conservation and forestry Dept of education
Dept of education Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Dept a
Dept a Central islip fire department
Central islip fire department Rowan county medicaid transportation
Rowan county medicaid transportation Dept of education
Dept of education Tabella nmr
Tabella nmr Pt dept logistik
Pt dept logistik Nys department of homeland security
Nys department of homeland security Affiliate disclodures
Affiliate disclodures La geaux biz
La geaux biz Rewley house continuing education library
Rewley house continuing education library Nebraska dept of agriculture
Nebraska dept of agriculture Ee dept iitb
Ee dept iitb Dept ind onegov
Dept ind onegov Albany county dss
Albany county dss Proyecto tara
Proyecto tara Tara misra
Tara misra Tara cavarnei
Tara cavarnei Tara sullivan pt
Tara sullivan pt Tara dall md
Tara dall md Cod tara romania 642
Cod tara romania 642 Tara nilai baku adalah
Tara nilai baku adalah Tara shears
Tara shears Stefania koppel
Stefania koppel Tara stiles reebok
Tara stiles reebok Tara haughton
Tara haughton Tara and tiree fearless friends
Tara and tiree fearless friends Tara ristic biografija
Tara ristic biografija Tara brah
Tara brah Tara calabro
Tara calabro Tara thieme
Tara thieme Tara berladnicilor
Tara berladnicilor Tara reid
Tara reid Tara gentry
Tara gentry Tara noble
Tara noble Usc tara login
Usc tara login Tara tradelink private limited
Tara tradelink private limited Tara sfanta in vremea mantuitorului proiect didactic
Tara sfanta in vremea mantuitorului proiect didactic Mac renton tara
Mac renton tara Listen to a presentation about tara fashions
Listen to a presentation about tara fashions Tara reid
Tara reid Tara balakrishnan
Tara balakrishnan Tara worley
Tara worley Muntii din marea britanie
Muntii din marea britanie Tara bracco
Tara bracco Tara douglas-williams
Tara douglas-williams Tara bartee
Tara bartee Etlw
Etlw Tara hines
Tara hines