New challenge for students and staff Marijke van

- Slides: 47
New challenge for students and staff! Marijke van Santen-Hoeufft ass. prof. internal medicine/rheumatology, consultant in clinical education, curriculum development and assessment Maastricht, the Netherlands Clinical phase
The ambulatory and clinical environment in a modern medical curriculum Clinical phase
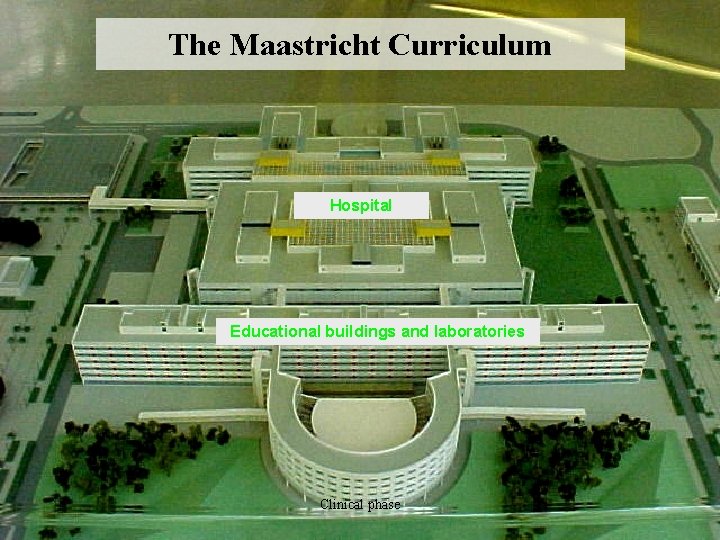
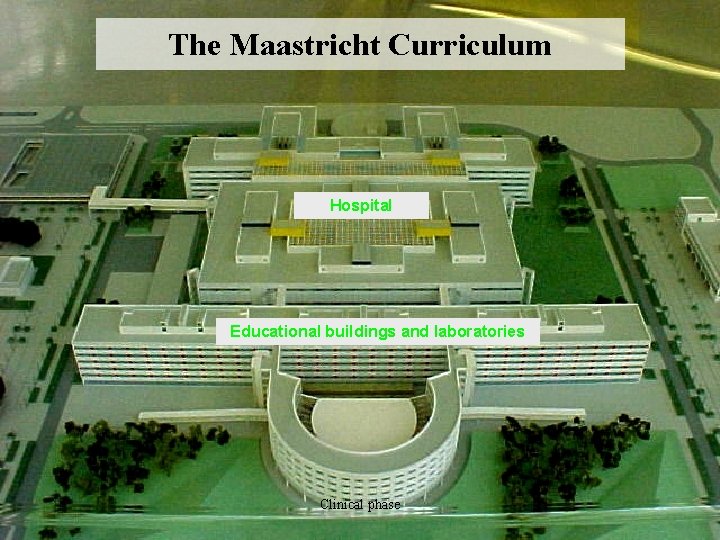
The Maastricht Curriculum Hospital Educational buildings and laboratories Clinical phase
How do we prepare our future doctors best for the challenges of the 21 st century? ‘The Maastricht experience’ Clinical phase
Outline of presentation • Motivation for curriculum change • Year 3 • Strenghts and weaknesses of clinical rotations • Conclusion Clinical phase
Many motivations for curriculum change in Maastricht 2001… The most important overall: The transition of preclinical to clinical phase is experienced as quite a shock of practice and… The transition of graduate to postgraduate training is experienced as… A tremendous ‘shock of practice’! Clinical phase
Why shock of practice? Post-graduate training requires: • Working under time pressure • Facing larger responsibility • Dealing with more complex problems • Having insufficient competencies Clinical phase
How to prevent shock of practices? • Critical appraisal of current content year 4 - 6 • Better preparation for the ‘real work’ in year 3 HOW TO DO THIS? • Start with real patient encounters in year 3 • Broadening of competencies other than medical expert Clinical phase
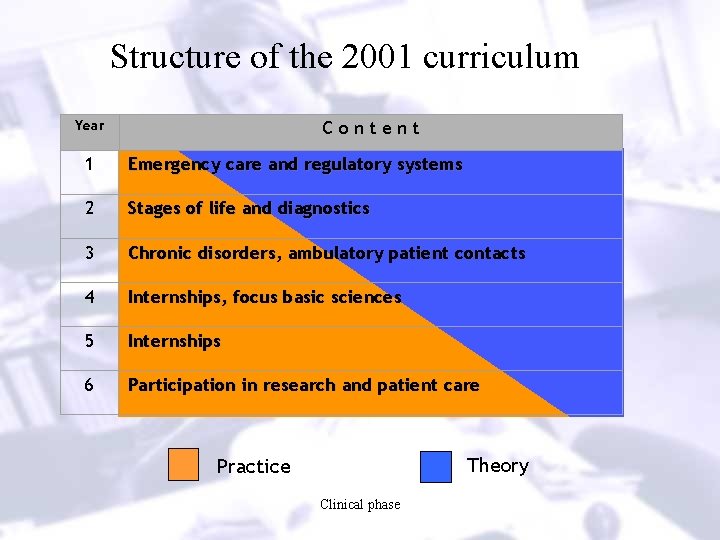
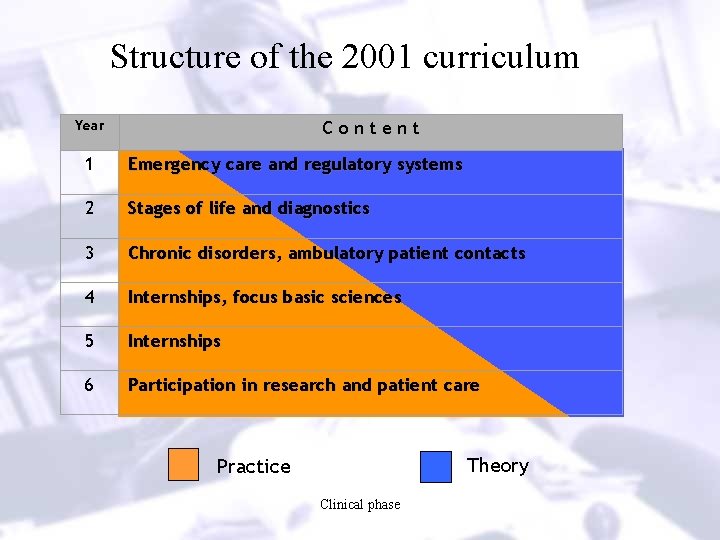
Structure of the 2001 curriculum Year Content 1 Emergency care and regulatory systems 2 Stages of life and diagnostics 3 Chronic disorders, ambulatory patient contacts 4 Internships, focus basic sciences 5 Internships 6 Participation in research and patient care Theory Practice Clinical phase
Why early patient contacts? Clinical phase
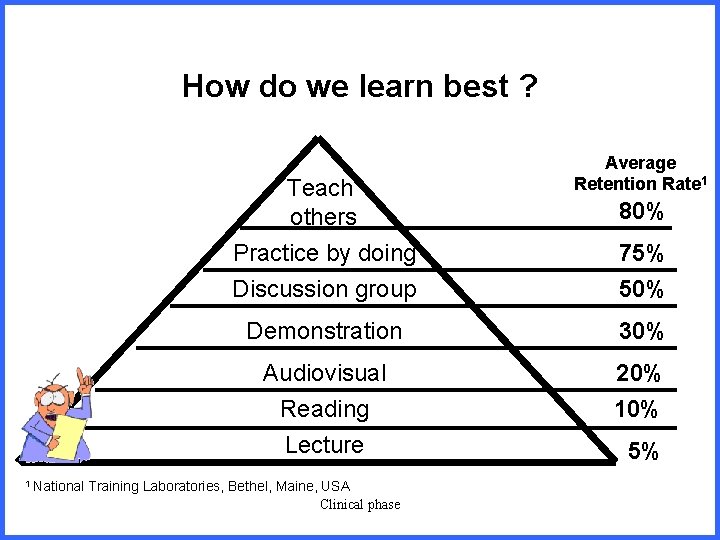
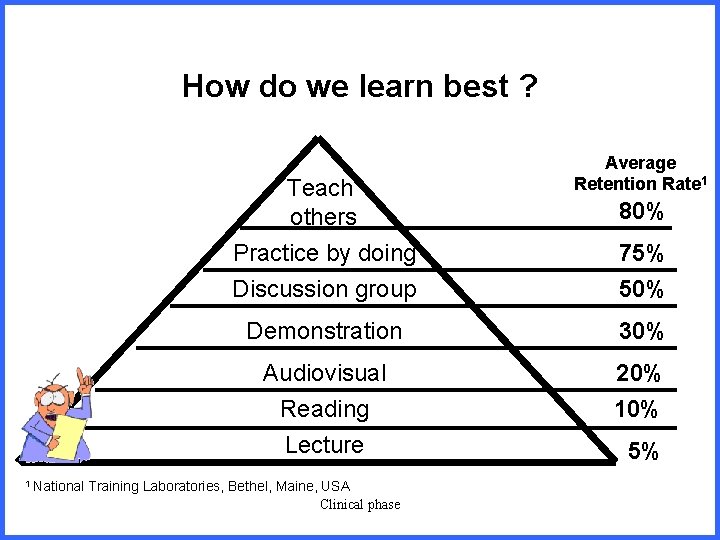
How do we learn best ? Teach others 1 National Average Retention Rate 1 80% Practice by doing Discussion group 75% 50% Demonstration 30% Audiovisual Reading Lecture 20% 10% Training Laboratories, Bethel, Maine, USA Clinical phase 5%
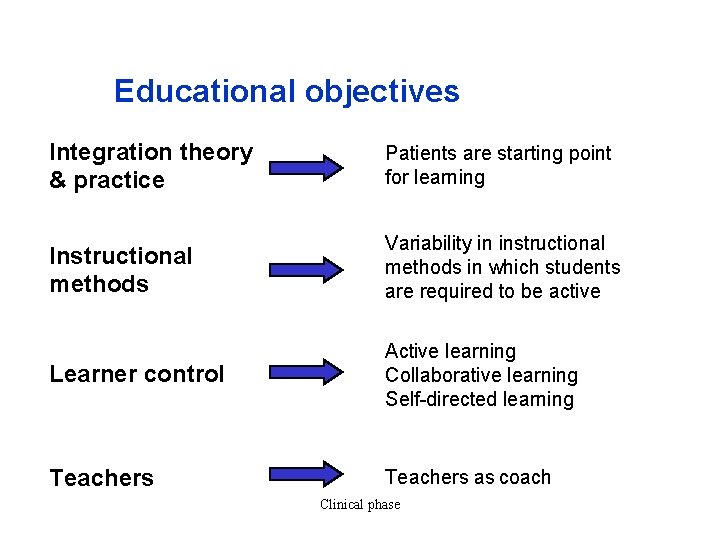
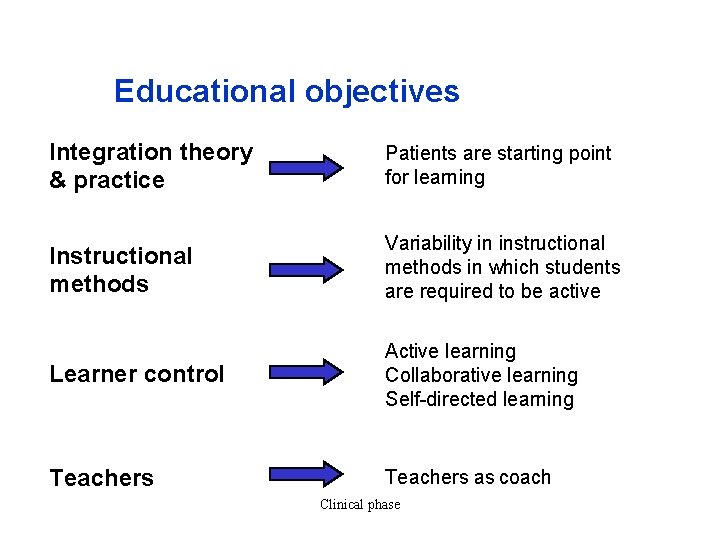
Educational objectives Integration theory & practice Patients are starting point for learning Instructional methods Variability in instructional methods in which students are required to be active Learner control Active learning Collaborative learning Self-directed learning Teachers as coach Clinical phase
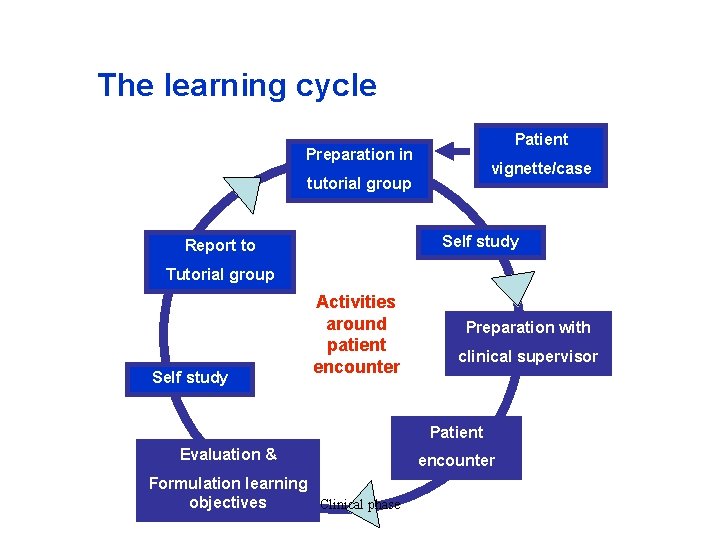
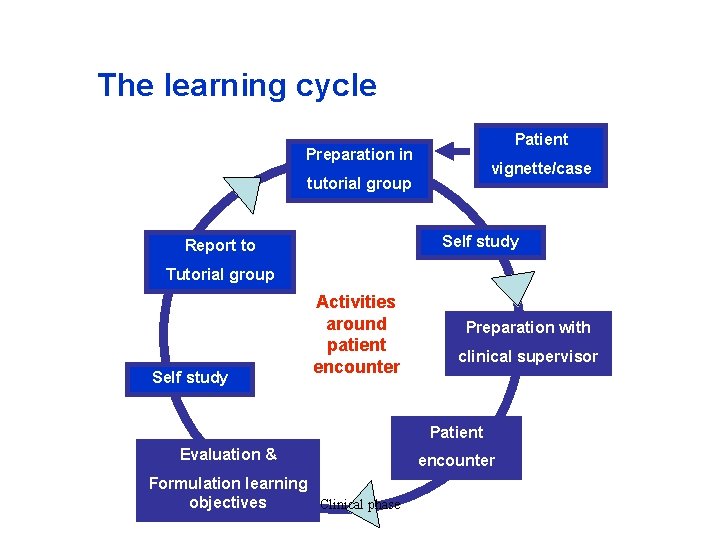
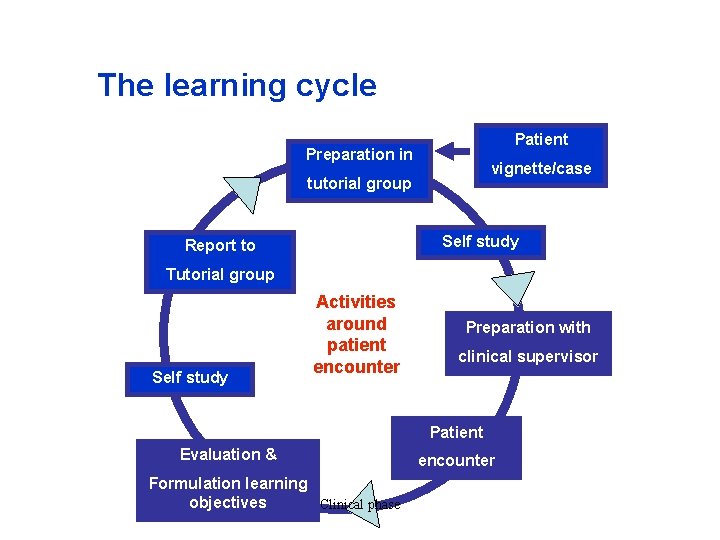
The learning cycle Patient Preparation in vignette/case tutorial group Self study Report to Tutorial group Self study Activities around patient encounter Preparation with clinical supervisor Patient Evaluation & Formulation learning objectives Clinical phase encounter
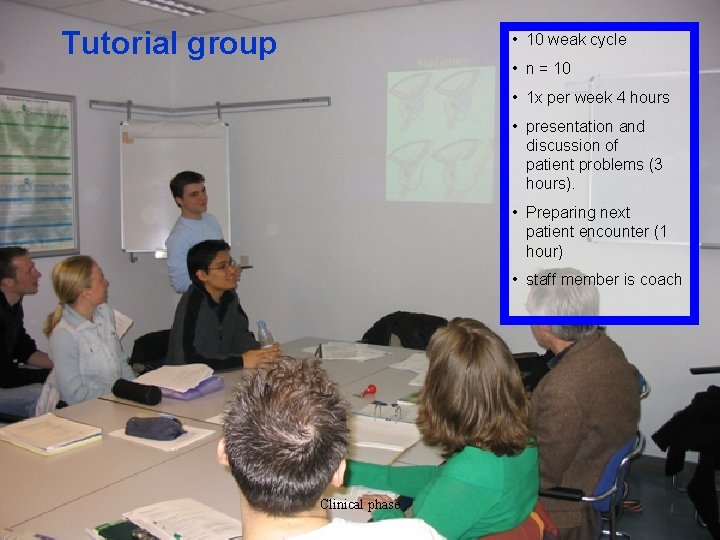
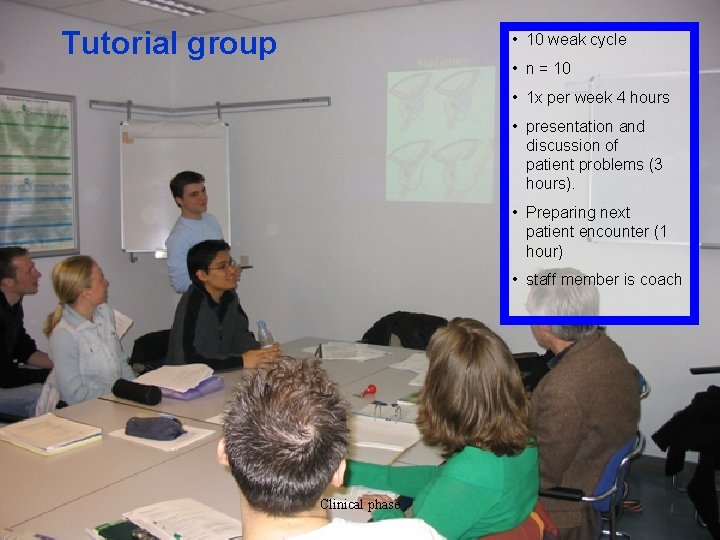
Tutorial group • 10 weak cycle • n = 10 • 1 x per week 4 hours • presentation and discussion of patient problems (3 hours). • Preparing next patient encounter (1 hour) • staff member is coach Clinical phase
Clinical phase
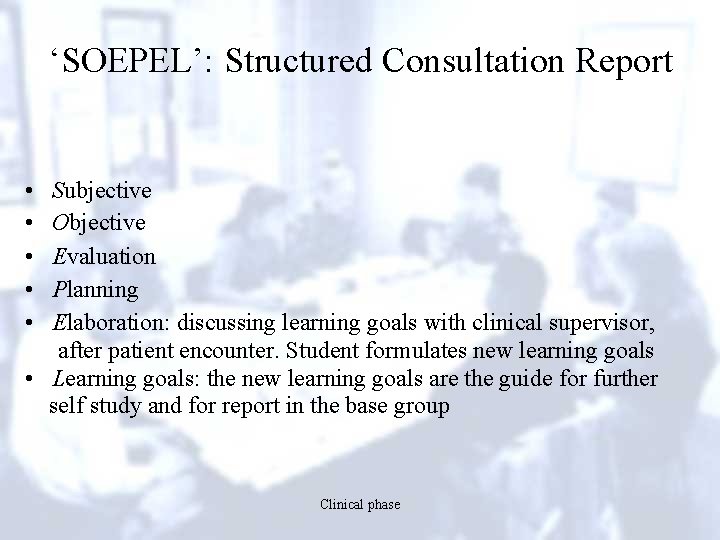
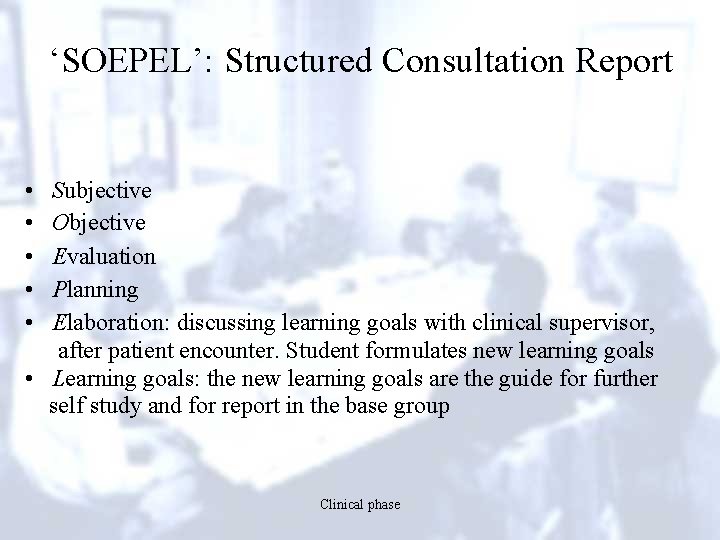
‘SOEPEL’: Structured Consultation Report • • • Subjective Objective Evaluation Planning Elaboration: discussing learning goals with clinical supervisor, after patient encounter. Student formulates new learning goals • Learning goals: the new learning goals are the guide for further self study and for report in the base group Clinical phase
Clinical phase
Clinical phase
Clinical phase
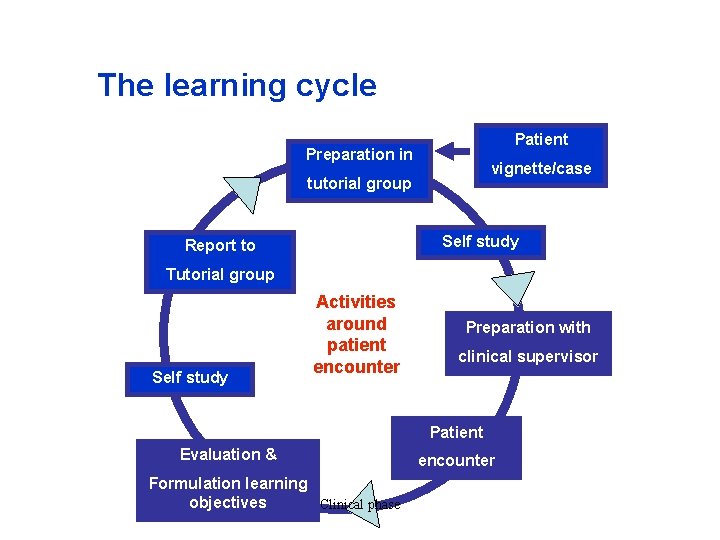
The learning cycle Patient Preparation in vignette/case tutorial group Self study Report to Tutorial group Self study Activities around patient encounter Preparation with clinical supervisor Patient Evaluation & Formulation learning objectives Clinical phase encounter
Formulating learning goals……. Clinical phase
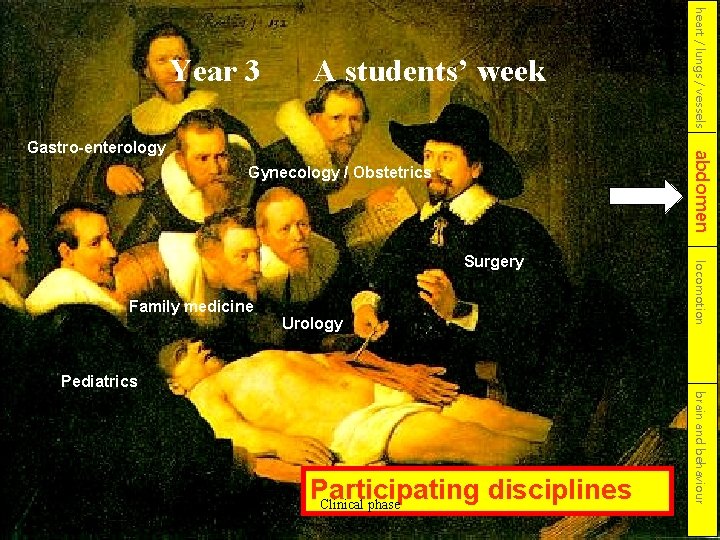
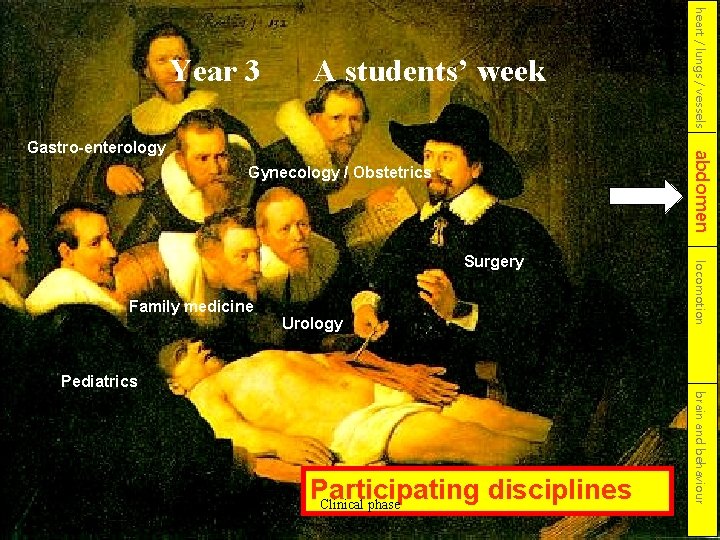
A students’ week abdomen Gastro-enterology Gynecology / Obstetrics Urology locomotion Surgery Family medicine heart / lungs / vessels Year 3 Pediatrics brain and behaviour Participating disciplines Clinical phase
Back to Brazil, back to the transition of students from the safe escola Pernambucana to the challenging IMIP environments… How to use PBL in a ambulatory and clinical context? Clinical phase
All medical faculties want to prepare their students the best they can for the 6 th year and post graduate education But what is the best way? Evidence for ‘best practice’? Clinical phase
“It may not be a perfect wheel, but it’s a state -of-the-art wheel. ” Clinical phase
Effectiveness of clinical rotations? ? Clinical phase
Strenghts of internships • • Learning in real, relevant context Integration of theory and workplace learning Active participation in practice Coping with increasing complex and diverse patient problems • Increasing self-reliance success depends on length of internship! Clinical phase
Unfortunately all internships have their weaknesses too… Why are internships generally less effective than ideally possible? Clinical phase
The effectiveness of internships is hampered by problems regarding: • • the teacher the workplace the students the elements of good clinical teaching Clinical phase
Common problems in clinical phase regarding the teacher(1): • Time pressures • Competing demands (clinical with parttime availability; administrative; research) • Teaching often opportunistic, making planning more difficult • Often under-resourced • Rewards and recognition for teachers poor • Good teaching needs intrinsic motivation of teacher Clinical phase
Common problems in clinical phase regarding the teacher(2): • Lack of knowledge about: • • • the effects of being a role model motivating students assessing competence giving constructive feedback the curriculum content, end-objectives… etc. • Lack of training in: • educational skills • evaluating his own teaching and asking feedback (self reflection) Clinical phase
Common problems in clinical phase regarding the workplace: • • Increasing numbers and types of students Fewer patients (shorter hospital stays; patients too ill or complex) Competing demands (patient-care related actions come first) Clinical environment not ‘teaching friendly’ (busy hospital ward; no suitable meetingplace with students; no learning climat) • Ambulatory care insufficiently involved in education Clinical phase
Common problems in clinical phase regarding the teacher(1): • Time pressures • Competing demands (clinical with parttime availability; administrative; research) • Teaching often opportunistic, making planning more difficult • Often under-resourced • Rewards and recognition for teachers poor • Good teaching needs intrinsic motivation of teacher Clinical phase
Common problems in clinical phase regarding the teacher(2): • Lack of knowledge about: • • • the effects of being a role model motivating students assessing competence giving constructive feedback the curriculum content, end-objectives… etc. • Lack of training in: • educational skills • evaluating his own teaching and asking feedback (self reflection) Clinical phase
Common problems in clinical phase regarding the workplace: • • Increasing numbers and types of students Fewer patients (shorter hospital stays; patients too ill or complex) Competing demands (patient-care related actions come first) Clinical environment not ‘teaching friendly’ (busy hospital ward; no suitable meetingplace with students; no learning climat) • Ambulatory care insufficiently involved in education Clinical phase
Common problems in clinical phase regarding the students: • Insufficiently prepared (knowledge, skills) • Don’t take the opportunities for examining patients independently • Stay passive observers in stead of active participants due to too short clerkships (no time for professional socialisation) Clinical phase
Common problems with clinical teaching(1): • Lack of clear objectives and expectations • Focus on factual recall rather than on development of problem solving skills and attitutes • Teaching pitched at the wrong level (too high or too specialistic) • Inadequate supervision and provision of feedback (due to lack of time, lack of skills or motivation, no continuity) Clinical phase
Isn’t it a wonder there are competent physicians anyway? ! At least we think we are…. Clinical phase
Important determinants of the effectiveness of student learning in a clinical environment: • • Patient mix Opportunities for examining patients independently Received supervision and feedback Organisational quality Student being part of a team Number of students at one time Educational sessions Positive attitude of staff towards students Clinical phase
Most important determinants of the effectiveness of student learning in a clinical environment: 1 - received supervision and feedback 2 - opportunities for examining patients independently 3 - patient mix Clinical phase
Measures to improve effectiveness of clerkships: • • • Clerkship study guides Teach the teachers trainings Create a positive learning environment More direct observation and feedback Include protected time for selfstudy Integration of learning and assessing on the workplace by using mini. CEX, logbooks etc. Clinical phase
Integration of learning and assessing by: • Observing multiple events during clerkship involving multiple people • Using mini CEX (Clinical Evaluation e. Xercise) or other ‘on the job assessment tools’ • Using the logbook in which structured clinical records are gathered of all patients seen by the student • Coaching • Critical incident analysis • Portfolio etc. Clinical phase

Integration in medical curricula Clinical phase Faculty of Medicine Universiteit Maastricht
Clinical phase
In summary, improvement of the effectiveness of the ambulatory and clinical phase can be achieved, but not without effort and lots of motivation of organisation, staff and students! Clinical phase
Thank you for your attention! Clinical phase
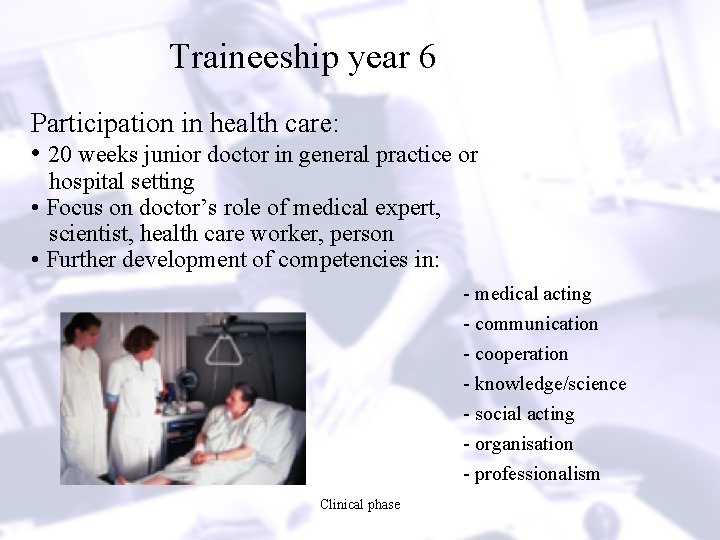
Traineeship year 6 Participation in health care: • 20 weeks junior doctor in general practice or hospital setting • Focus on doctor’s role of medical expert, scientist, health care worker, person • Further development of competencies in: - medical acting - communication - cooperation - knowledge/science - social acting - organisation - professionalism Clinical phase