Neonatal emergencies dr Miada Mahmoud Rady Definitions q










- Slides: 54
Neonatal emergencies dr. Miada Mahmoud Rady
Definitions q Newborn: within the first few hours after birth. q Neonate: within the first month after birth.
General Pathophysiology and Assessment of newborn and neonates • Neonatal resuscitation steps : ØThe same basic steps of adult resuscitation : 1. Airway 2. Breathing 3. Circulation • Newborn stabilization procedures : 1. Warming 2. Positioning 3. Clearing the airway 4. Drying and breathing stimualtion
General Pathophysiology and Assessment • Additional resuscitation steps that may be required in certain situations : 1. Supplemental oxygen 2. Positive pressure ventilatory assistance 3. Intubation 4. Chest compressions 5. Medications
Transition from Fetus to Newborn 1. First breath is triggered by mild hypoxia and hypercapnia. 2. Pulmonary vascular resistance drops as the lungs fill with air. 3. More blood flows to the lungs.
Transition from Fetus to Newborn 4. Delay in pulmonary pressure drop leads to: a. Delayed transition b. Hypoxia c. Brain injury d. Death

Arrival of the Newborn A. Obtain patient history and prepare environment. 1. Minimum needs: • Warm, dry blankets • Bulb syringe • Two small clamps or ties • A pair of clean scissors
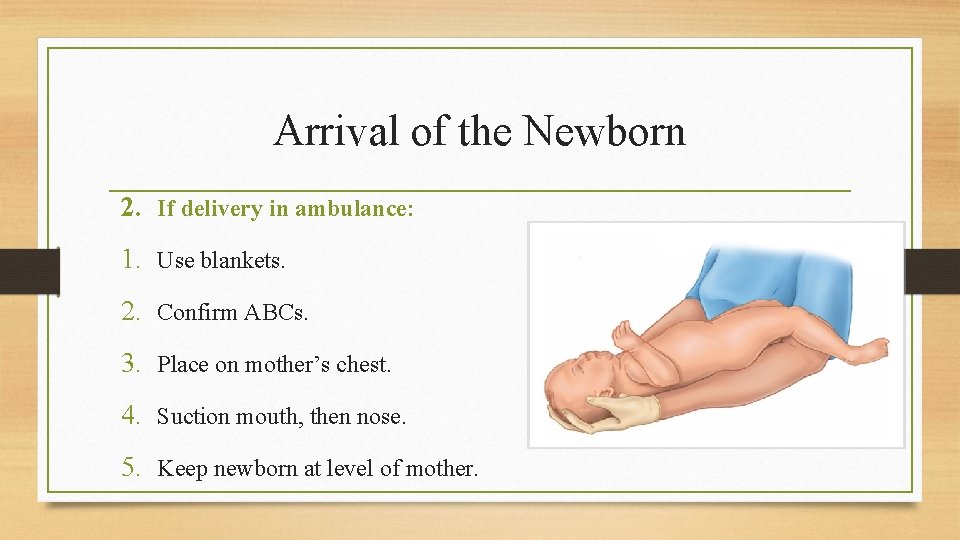
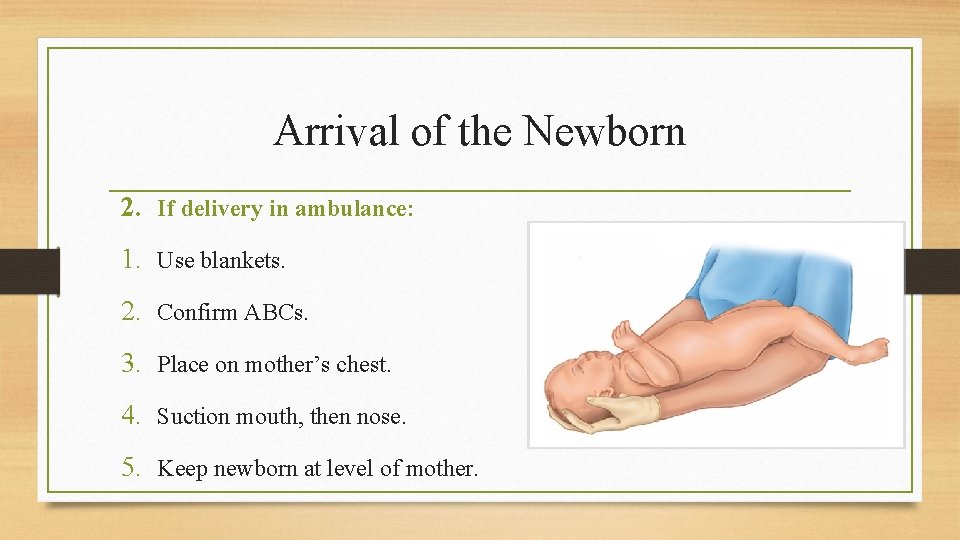
Arrival of the Newborn 2. If delivery in ambulance: 1. Use blankets. 2. Confirm ABCs. 3. Place on mother’s chest. 4. Suction mouth, then nose. 5. Keep newborn at level of mother.

Arrival of the Newborn 6. Clamp and cut the umbilical cord. 7. Do an initial rapid assessment. 8. Newborn is at risk for hyperthermia so Ensure thermoregulation. 9. Position the newborn, clear secretions, and assess the respiratory effort.
Arrival of the Newborn 10. If the newborn begins to turn pink in the first 5 minutes: • Maintain ongoing observation. • Continue thermoregulation with direct skin-to-skin contact with mother.
Apgar score

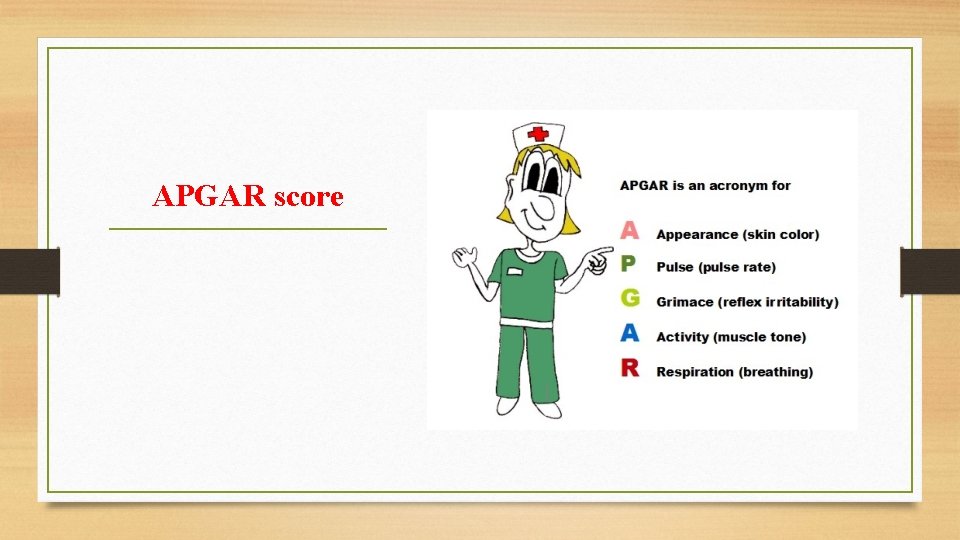
APGAR test q Definition : 1. A quick test performed on a baby at 1 and 5 minutes after birth. 2. The 1 -minute score determines how well the baby tolerated the birthing process. 3. The 5 -minute score determines how well the baby is doing outside the mother's womb.
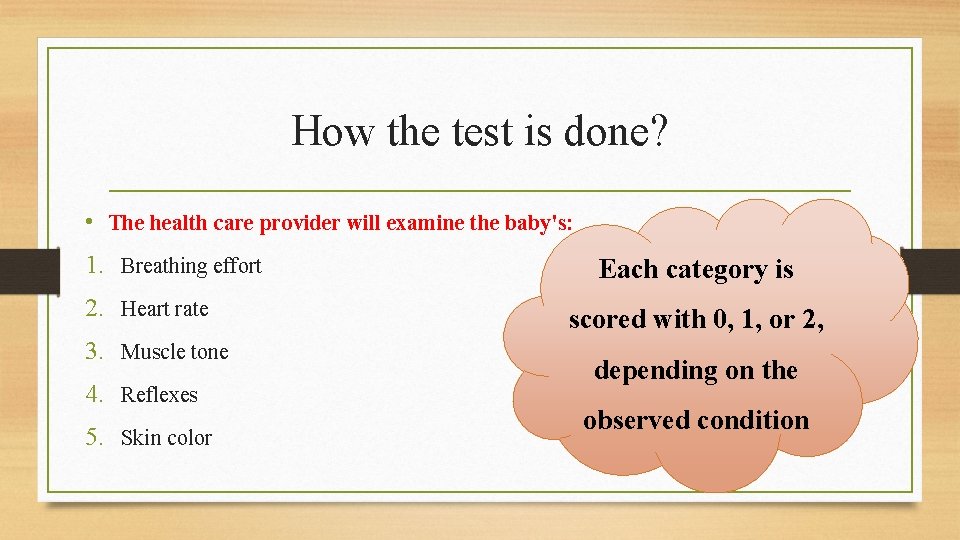
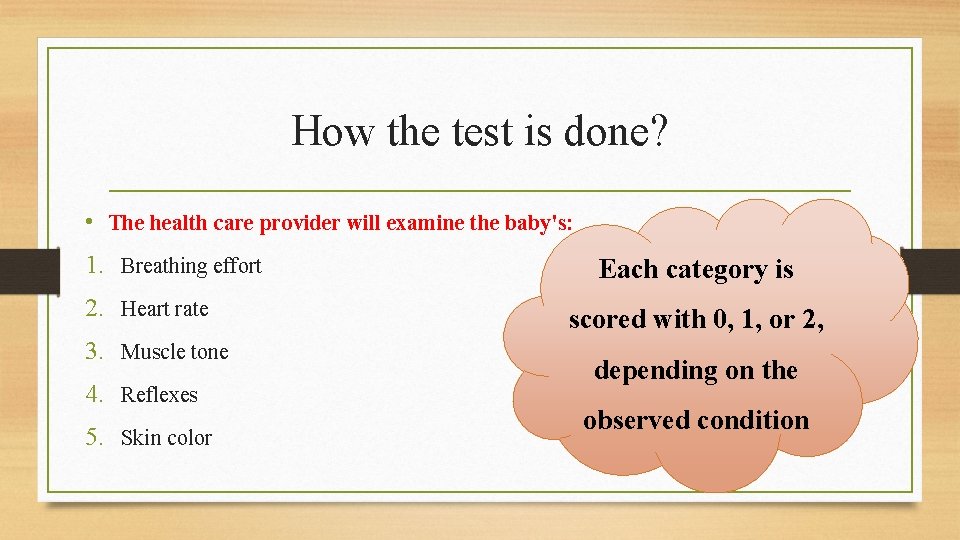
How the test is done? • The health care provider will examine the baby's: 1. Breathing effort 2. Heart rate 3. Muscle tone 4. Reflexes 5. Skin color Each category is scored with 0, 1, or 2, depending on the observed condition
• This test is done to determine whether a newborn needs help breathing or is having heart trouble. § Normal Results 1. The APGAR rating is based on a total score of 1 to 10. 2. The higher the score, the better the baby is doing after birth. 3. A score of 7, 8, or 9 is normal and is a sign that the newborn is in good health.
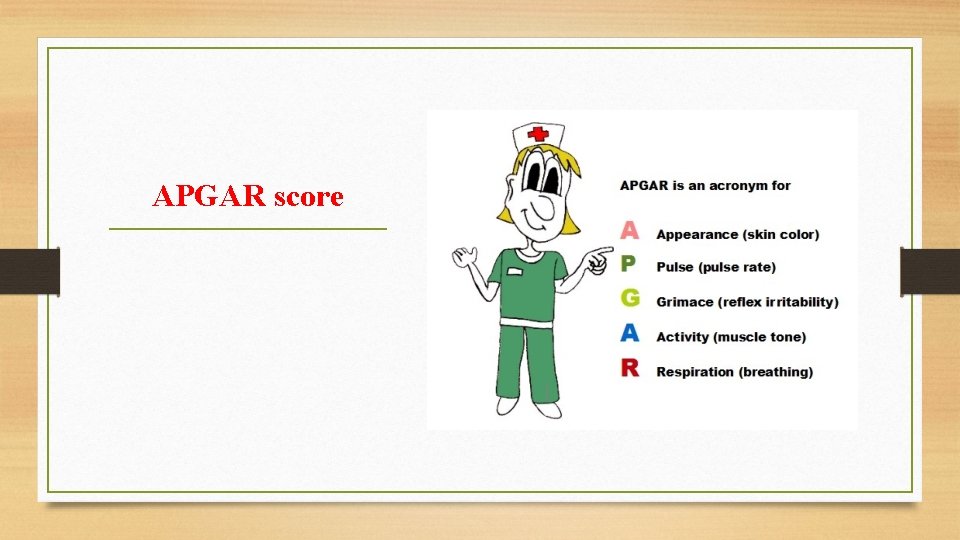
APGAR score
A for appearance 1. Appearance (Skin color): • If the skin color is pale blue, the infant scores 0 for color. • If the body is pink and the extremities are blue, the infant scores 1 for color. • If the entire body is pink, the infant scores 2 for color
P for pulse 2. Pulse (Heart rate) : Ø is evaluated by stethoscope , this is the most important assessment: • If there is no heartbeat, the infant scores 0 for heart rate. • If heart rate is less than 100 beats per minute, the infant scores 1 for heart rate. • If heart rate is greater than 100 beats per minute, the infant scores 2 for heart rate.
G for grimace 3. Grimace response ( reflex irritability ): It is a term describing response to stimulation such as a mild pinch : • If there is no reaction, the infant scores 0 for reflex irritability. • If there is grimacing, the infant scores 1 for reflex irritability. • If there is grimacing and a cough, sneeze, or vigorous cry, the infant scores 2 for reflex irritability.
A for activity 3. Activity ( Muscle tone): • If muscles are loose and floppy, the infant scores 0 for muscle tone. • If there is some muscle tone, the infant scores 1. • If there is active motion, the infant scores 2 for muscle tone.
R for respiration 1. Respiration ( Breathing )effort: • If the infant is not breathing, the respiratory score is 0. • If the respirations are slow or irregular, the infant scores 1 for respiratory effort. • If the infant cries well, the respiratory score is 2.



Drying and Stimulation • Nasal suctioning stimulates breathing: • Position on the back or side in sniffing position. • If airway is not clear, suction with the head turned to the side. • Flick the soles of the feet and rub the back.

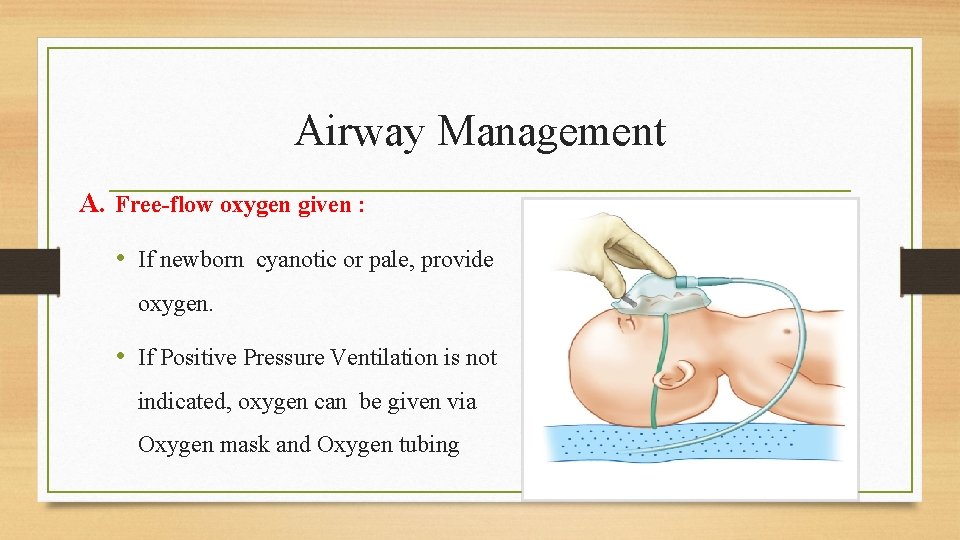
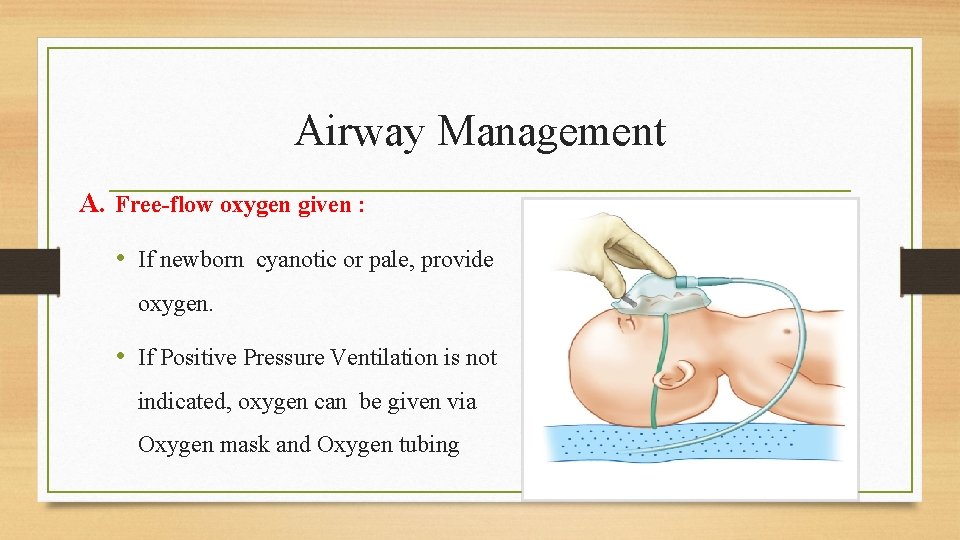
Airway Management A. Free-flow oxygen given : • If newborn cyanotic or pale, provide oxygen. • If Positive Pressure Ventilation is not indicated, oxygen can be given via Oxygen mask and Oxygen tubing
B. Oral airways Rarely used on newborns , Conditions that may require oral airways: 1. Bilateral choanal atresia 2. Pierre Robin sequence 3. Macroglossia (large tongue) 4. Craniofacial defects that affect the airway In all these cases (except bilateral choanal atresia), an ET tube is inserted down a nostril.

C. Bag-mask ventilation Indicated if newborn: 1. Is apneic 2. Has inadequate respiratory effort 3. Has a pulse rate of less than 100 beats/min after stimulation efforts
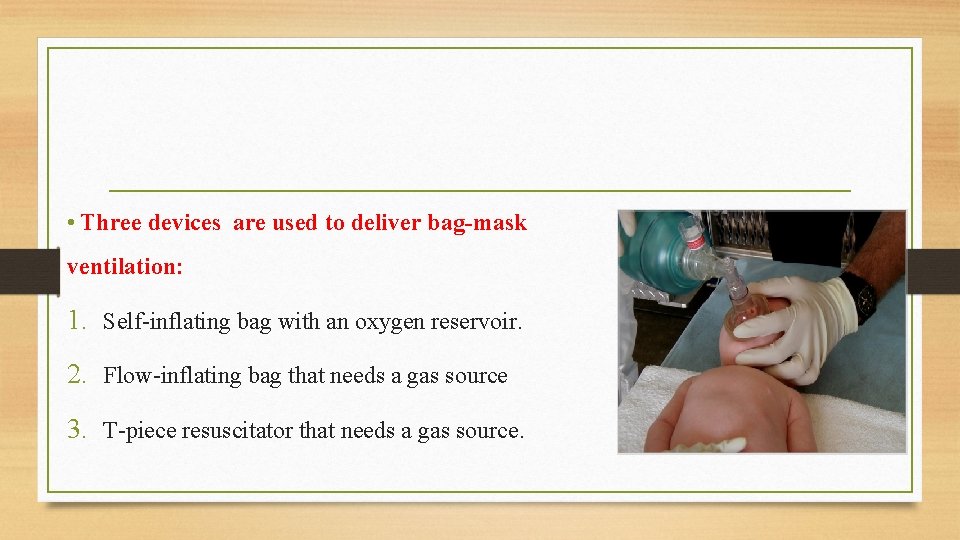
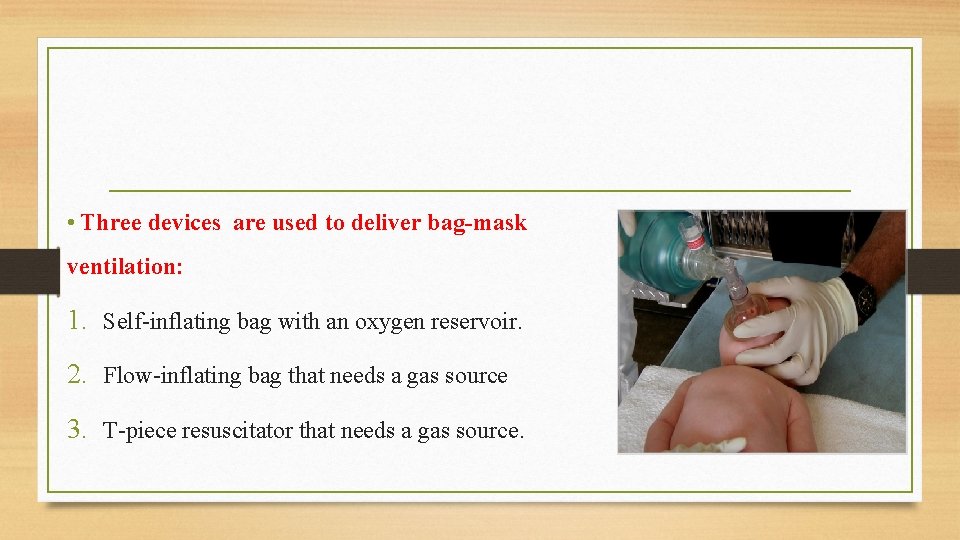
• Three devices are used to deliver bag-mask ventilation: 1. Self-inflating bag with an oxygen reservoir. 2. Flow-inflating bag that needs a gas source 3. T-piece resuscitator that needs a gas source.

• Correct ventilation time: 40 to 60 breaths/min • Causes of ineffective bag-mask ventilation: 1. Inadequate mask seal on the face and Equipment malfunction 2. Incorrect head position 3. Copious secretions 4. Pneumothorax
D. Intubation q Indications: 1. Meconium-stained fluid and non vigorous newborn 2. Congenital diaphragmatic hernia 3. ET administration of epinephrine is needed 4. Prolonged PPV needed 5. Craniofacial defects impeding airway
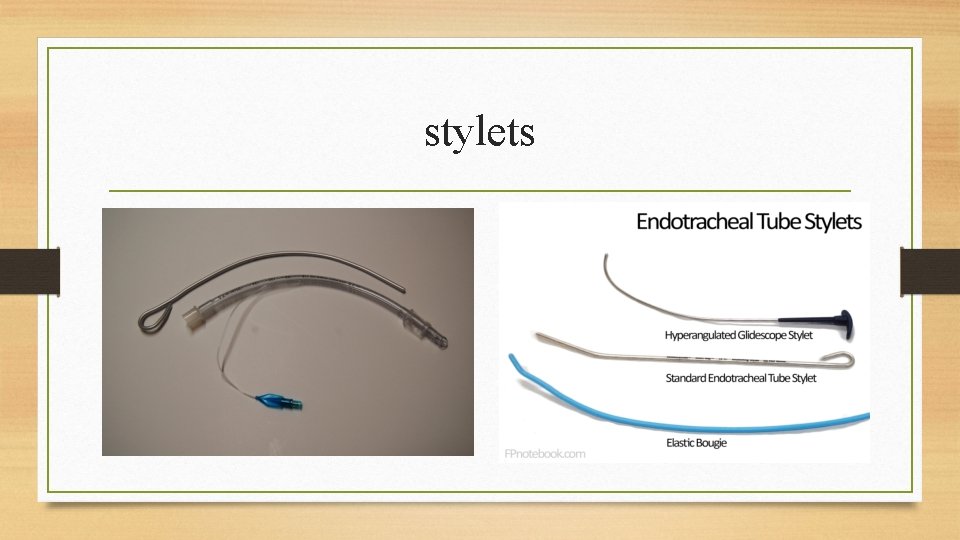
q Equipment needed: 1. Suction equipment 2. Laryngoscope 3. Blades 4. Shoulder roll and adhesive tape 5. ET tube and stylet
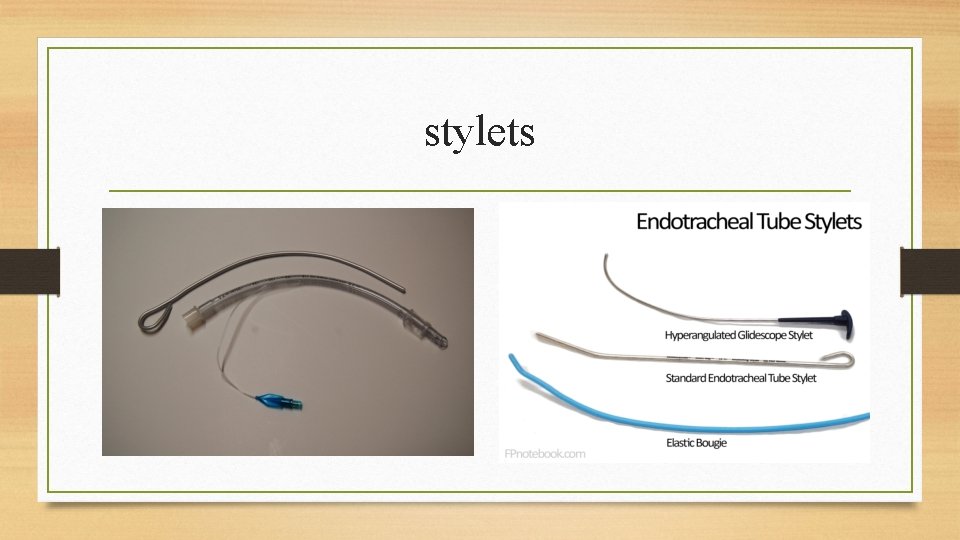
stylets
Gastric decompression q Indications: 1. Prolonged bag-mask ventilation 2. Abdominal distention impeding ventilation 3. Diaphragmatic hernia or gastrointestinal congenital anomaly
Circulation q Chest compressions 1. Indicated if pulse rate remains at less than 60 beats/min after resuscitation efforts 2. Two people needed 3. Depth: one third of the anteroposterior diameter 4. Do not deliver simultaneously with artificial ventilation. 5. Coordinate 90 compressions and 30 breaths/min
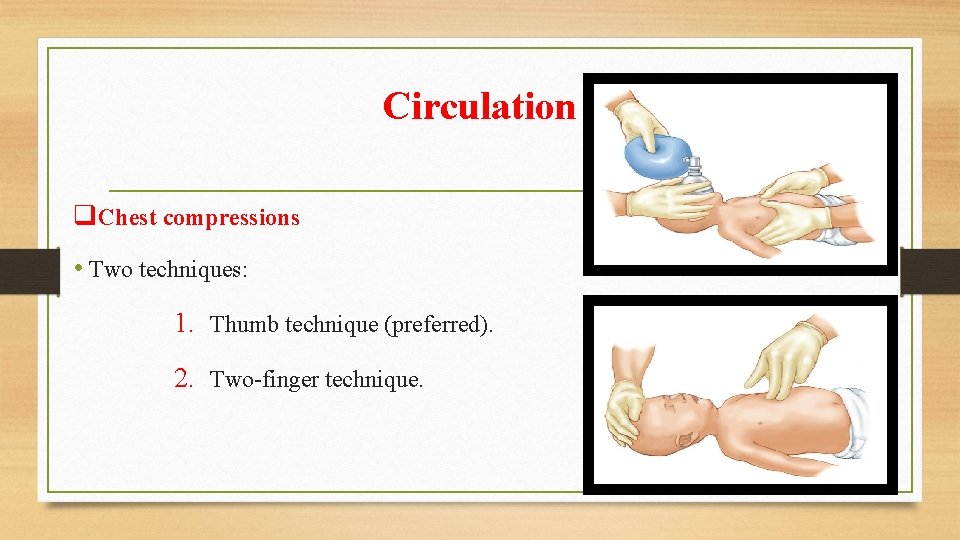
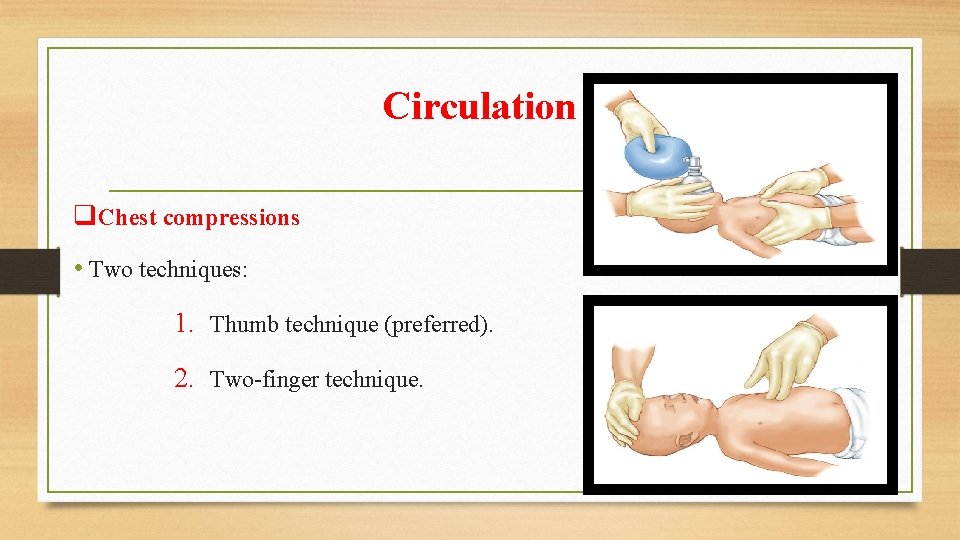
Circulation q. Chest compressions • Two techniques: 1. Thumb technique (preferred). 2. Two-finger technique.
Circulation q If pulse rate is above 60 beats/min: 1. Chest compressions can be stopped. 2. Continue ventilation at 40 to 60 breaths/min. 3. Recheck pulse rate after 30 seconds. q If rate goes above 100 beats/min, gradually slow the rate and decrease PPV pressure.
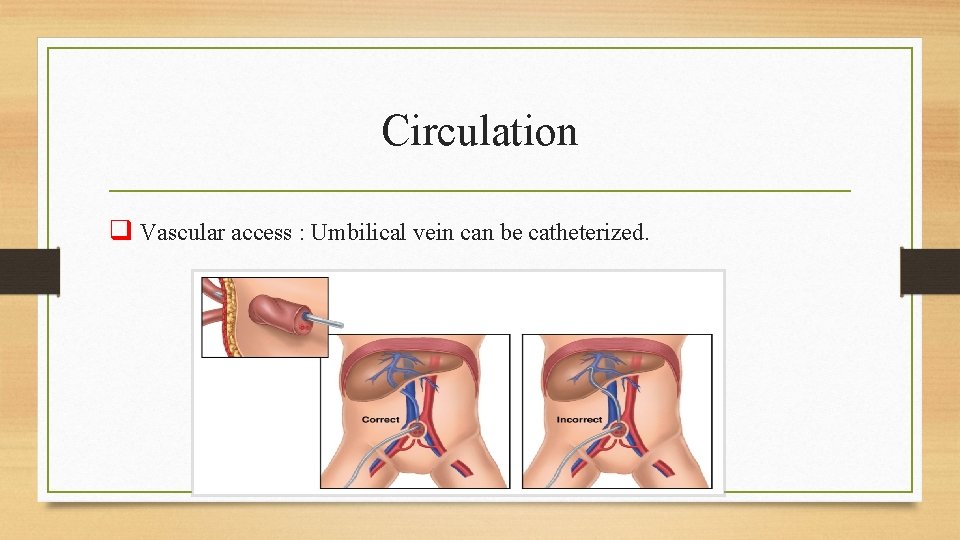
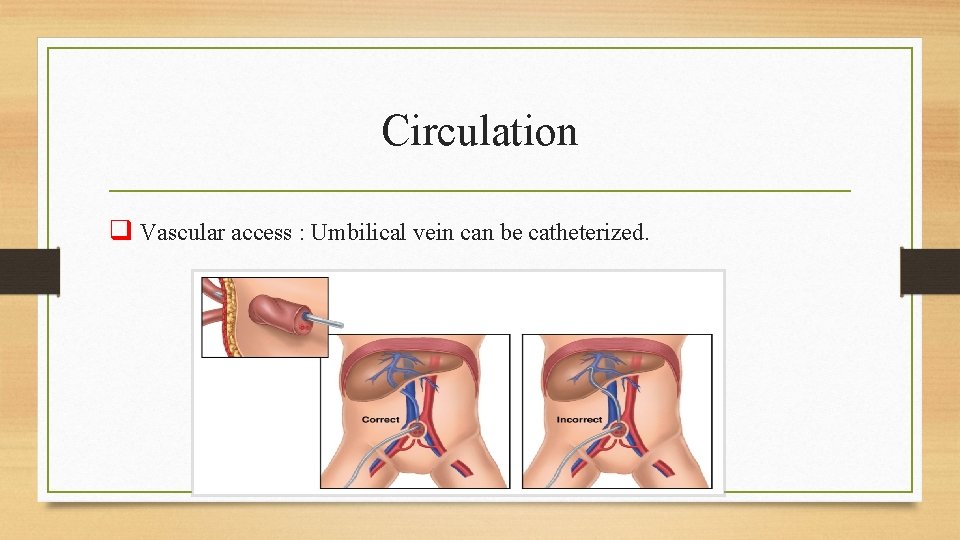
Circulation q Vascular access : Umbilical vein can be catheterized.
Pharmacologic Interventions q Rarely needed in newborn resuscitation q Medication dosages based on weight
Bradycardia q Mainly caused by hypoxia q Often will respond to PPV q Epinephrine administration is indicated for pulse rate of less than 60 beats/min with the following precautions : 1. Check pulse rate 1 minute after administration. 2. May repeat dose every 3 to 5 minutes
Bradycardia Assessment and management 1. Heart rate less than 100 beats/min provide PPV. 2. If still less than 60 beats/min Begin chest compressions. 3. If still less than 60 beats/min Administer epinephrine and Repeat every 3 to 5 minutes for persistent bradycardia.
Low Blood Volume q Signs of hypovolemia include: 1. Pallor Fluid resuscitation may be needed. 2. Persistently low pulse rate 3. Weak pulses 4. No improvement in circulatory status after resuscitation efforts
Low Blood Volume q Fluid bolus in a newborn is 10 m. L/kg given IV every 5 to 10 minutes of: 1. Saline 2. Lactated Ringer’s 3. O Rh-negative blood
Acidosis q Suspect acidosis if bradycardia persists after: 1. Adequate ventilations 2. Chest compressions 3. Volume expansion
Respiratory Depression from Narcotics • Management of respiratory suppression from use of narcotics: 1. Provide ventilator support. 2. Transport immediately. • Respiratory depression from acute treatment with narcotics: • Administer 0. 1 mg/kg of naloxone.
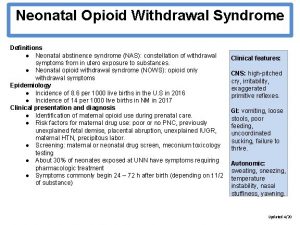
Hypoglycemia • Neurologic symptoms of hypoglycemia : 1. Decreased stimuli response 2. Hypotonia 3. Apnea 4. Poor feeding 5. seizures
Management of hypoglycemia A. Obtain baseline vital signs and oxygen saturation readings. B. If blood glucose level is less than 40 mg/d. L: 1. Give IV bolus of 10% dextrose solution. 2. Recheck level in about 30 minutes. 3. May need to follow with a 10% dextrose infusion
Family and Transport Considerations 1. Transport to nearest facility once newborn is stabilized as much as possible. 2. Provide ongoing communication with the family. 3. During transport, monitor the newborn.

 Sesja rady miasta skierniewice
Sesja rady miasta skierniewice Trofické řady
Trofické řady Rada pedagogiczna kompetencje
Rada pedagogiczna kompetencje Rady
Rady Umar ibn al khattab full name
Umar ibn al khattab full name Brzenica
Brzenica Trofické řady
Trofické řady Zložky časového radu
Zložky časového radu Dobre rady dla rodziców przedszkolaka
Dobre rady dla rodziców przedszkolaka Ocena pinokia
Ocena pinokia Hana mahmoud
Hana mahmoud Salman mustafa
Salman mustafa Mahmoud sarmini md
Mahmoud sarmini md Dr mahmoud khattab
Dr mahmoud khattab Mahmoud arafa
Mahmoud arafa Mahmoud abdelfattah age
Mahmoud abdelfattah age Mahmoud khattab md
Mahmoud khattab md Mahmoud boudarene
Mahmoud boudarene The passport mahmoud darwish
The passport mahmoud darwish Chapter 32 environmental emergencies
Chapter 32 environmental emergencies A behavioral crisis is most accurately defined as
A behavioral crisis is most accurately defined as Immunologic emergencies
Immunologic emergencies Gems diamond geriatric
Gems diamond geriatric Chapter 28 lesson 1
Chapter 28 lesson 1 Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Local area orientation dive
Local area orientation dive A 41 year old man presents with slow irregular breathing
A 41 year old man presents with slow irregular breathing Chapter 13 handling emergencies
Chapter 13 handling emergencies Environmental emergencies emt
Environmental emergencies emt Psychiatric emergencies
Psychiatric emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Qut security emergency extension number
Qut security emergency extension number Pumberton sign
Pumberton sign Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Tamiz neonatal
Tamiz neonatal Neonatal cholestasis definition
Neonatal cholestasis definition Lenticuloestriada
Lenticuloestriada Zonas de kramer
Zonas de kramer Sternal border
Sternal border Zonas de kramer ictericia neonatal
Zonas de kramer ictericia neonatal Neonatal kolestaz
Neonatal kolestaz Neonatal reflexes
Neonatal reflexes Hydrohepatosis definition
Hydrohepatosis definition 1-10 pain scale explained
1-10 pain scale explained Jaundice level
Jaundice level Riesgo de sepsis nanda
Riesgo de sepsis nanda Physiopathologie de l'ictère néonatal
Physiopathologie de l'ictère néonatal Kukonmaz
Kukonmaz