Necrotizing Fasciitis Current Concepts and review of the









- Slides: 36
Necrotizing Fasciitis: Current Concepts and review of the Literature Trauma Conference 4/28/2010 Emmanouil Palaios MD
Necrotizing Fasciitis: Current Concepts and Review of the Literature ü High mortality: 25 -35 % ü Mortality directly proportional to time of intervention. ü Purpose: review the microbiology, pathophysiology, diagnosis, and treatment of NSTI. ü Data from retrospective and nonblinded studies.
Necrotizing Fasciitis: Current Concepts and review of the Literature “Many were attacked by erysipelas all over the body when the exciting cause was a trivial accident…flesh, sinews, and bones fell away in large quantities…there were many deaths. ” Hippocrates ( 500 BC)
Necrotizing Fasciitis: Current Concepts and review of the Literature • As early as 1871 Dr. Joseph Jones: 2642 cases/ mortality 46% • (1883): Dr. Jean Alfred Fournier: NSTI of perineum in 5 male patients: Fournier’ s gangrene • (1951) Dr. Wilson : Necrotizing Fasciitis • Necrotizing Soft Tissue Infection
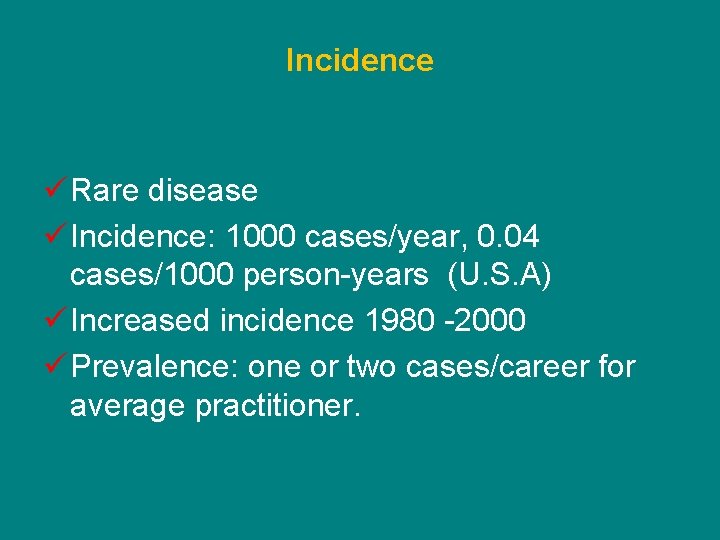
Incidence ü Rare disease ü Incidence: 1000 cases/year, 0. 04 cases/1000 person-years (U. S. A) ü Increased incidence 1980 -2000 ü Prevalence: one or two cases/career for average practitioner.

Classification Factor Comment Anatomic location Fournier’s gangrene perineum/scrotum Depth of Infection (correlates with mortality) Necrotizing adipositis (most common), fasciitis, myositis. Microbial cause Type I: polymicrobial (most common, 55 -75%) Type II: Monomicrobial: (staph, strep, clostridia). Type III: Vibrio vulnificus
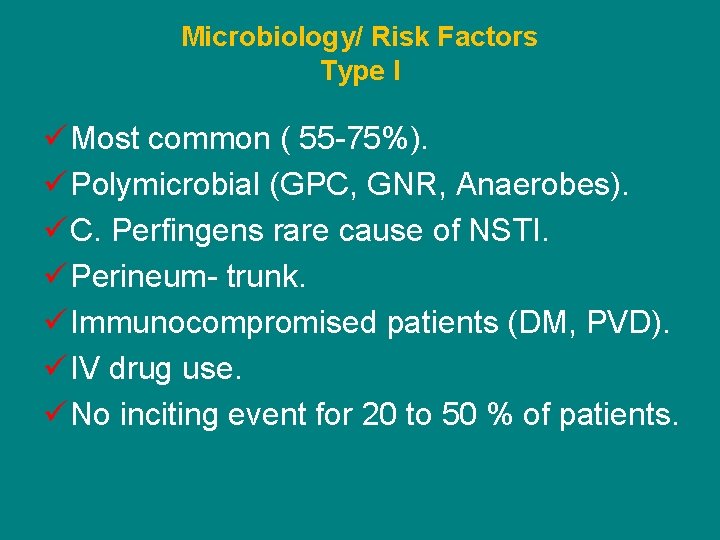
Microbiology/ Risk Factors Type I ü Most common ( 55 -75%). ü Polymicrobial (GPC, GNR, Anaerobes). ü C. Perfingens rare cause of NSTI. ü Perineum- trunk. ü Immunocompromised patients (DM, PVD). ü IV drug use. ü No inciting event for 20 to 50 % of patients.
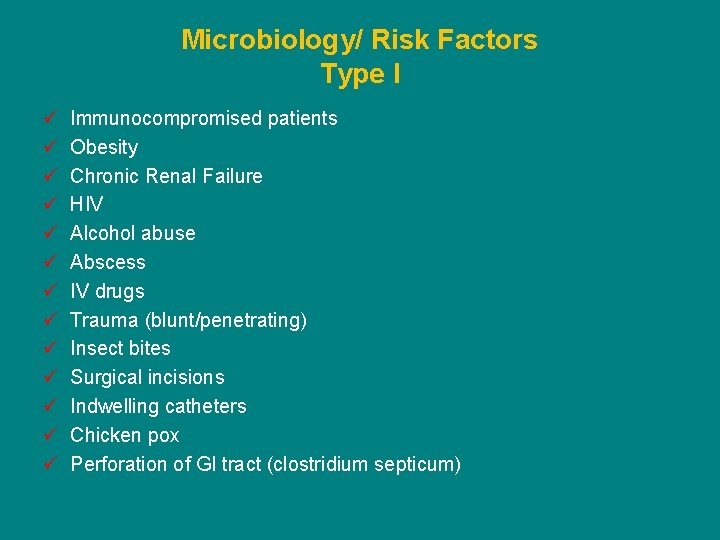
Microbiology/ Risk Factors Type I ü ü ü ü Immunocompromised patients Obesity Chronic Renal Failure HIV Alcohol abuse Abscess IV drugs Trauma (blunt/penetrating) Insect bites Surgical incisions Indwelling catheters Chicken pox Perforation of GI tract (clostridium septicum)
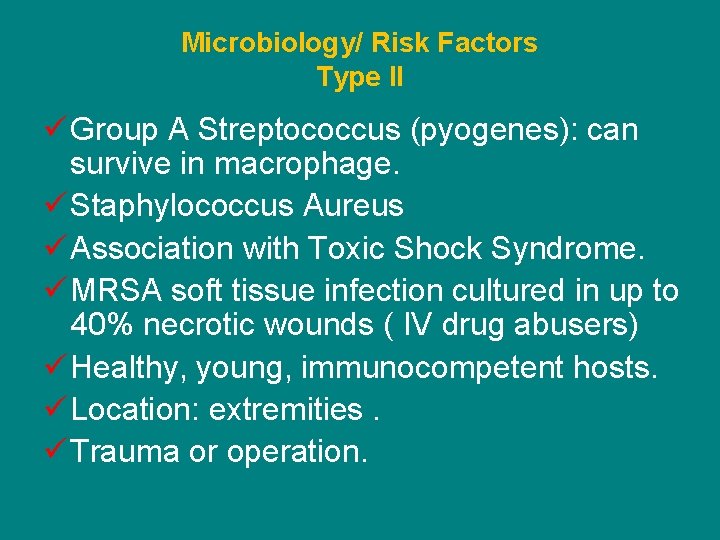
Microbiology/ Risk Factors Type II ü Group A Streptococcus (pyogenes): can survive in macrophage. ü Staphylococcus Aureus ü Association with Toxic Shock Syndrome. ü MRSA soft tissue infection cultured in up to 40% necrotic wounds ( IV drug abusers) ü Healthy, young, immunocompetent hosts. ü Location: extremities. ü Trauma or operation.
Microbiology/ Risk Factors Type III ü Least common type ü Vibrio vulnificus ü Skin break ü Warm sea water ü Coastal communities ü Risk factor: chronic HBV ü Fulminant course
Pathophysiology ü Invasion SC tissues ( trauma, perforated viscus) ü Production of toxins ü Tissue ischemia: thrombosis perforating skin vessels from local hypercoagulable state prevents adequate delivery of ABXS. ü Liquefactive necrosis ü Systemic illness. ü Extent of infection larger than that suggested by skin findings. ü Infection spread 1 inch/hour with little overlying skin change
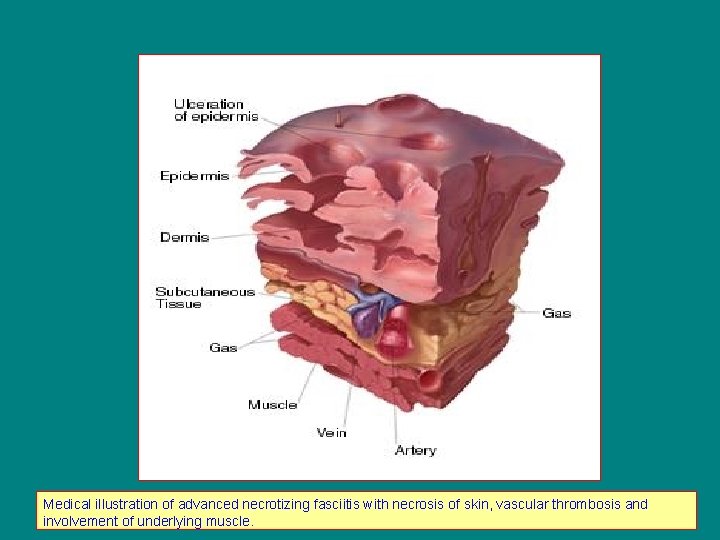
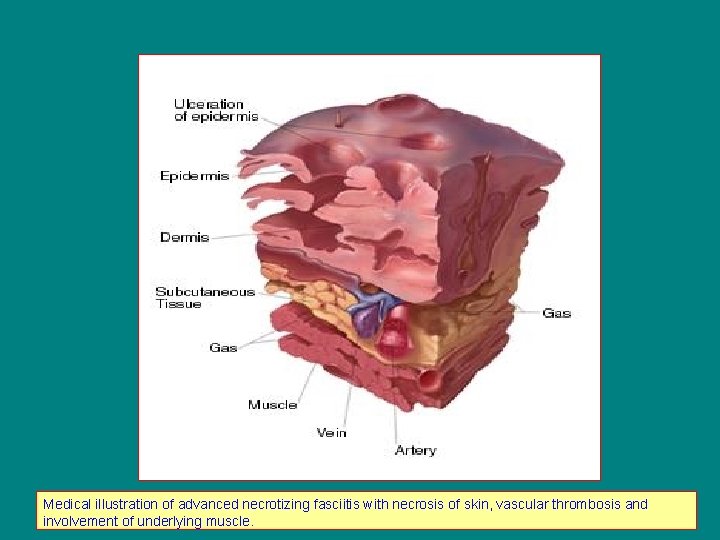
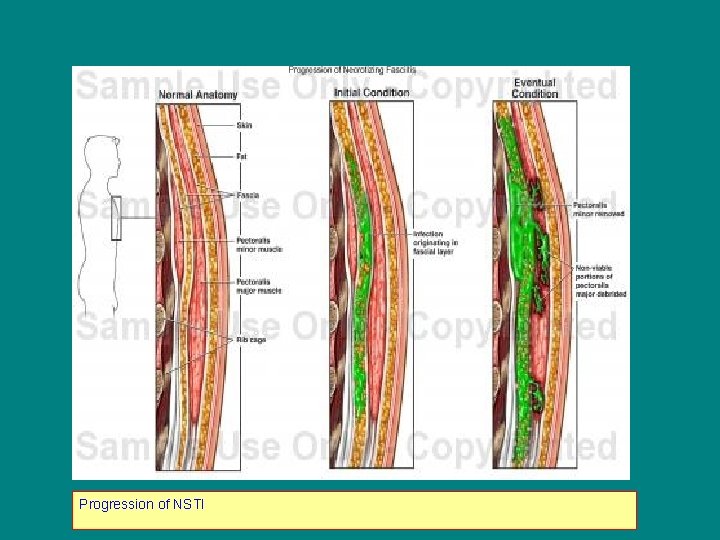
Medical illustration of advanced necrotizing fasciitis with necrosis of skin, vascular thrombosis and involvement of underlying muscle.
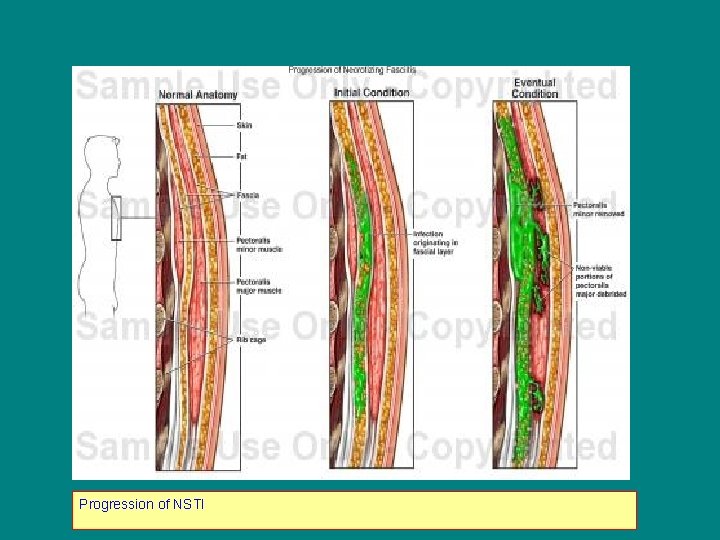
Progression of NSTI
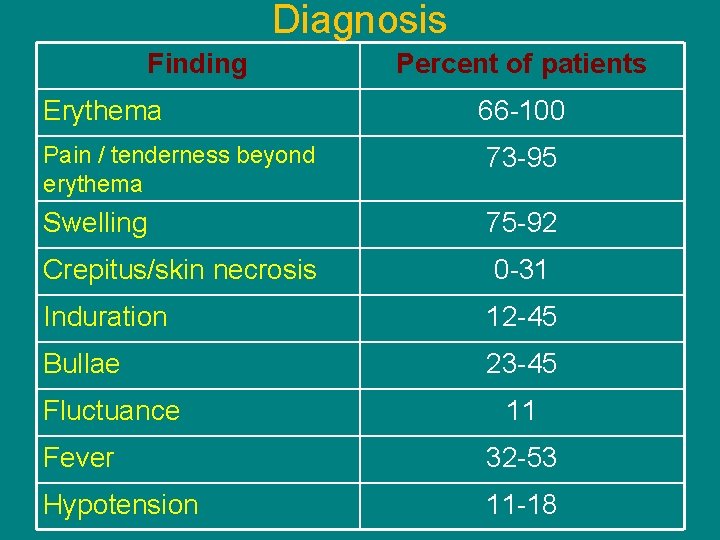
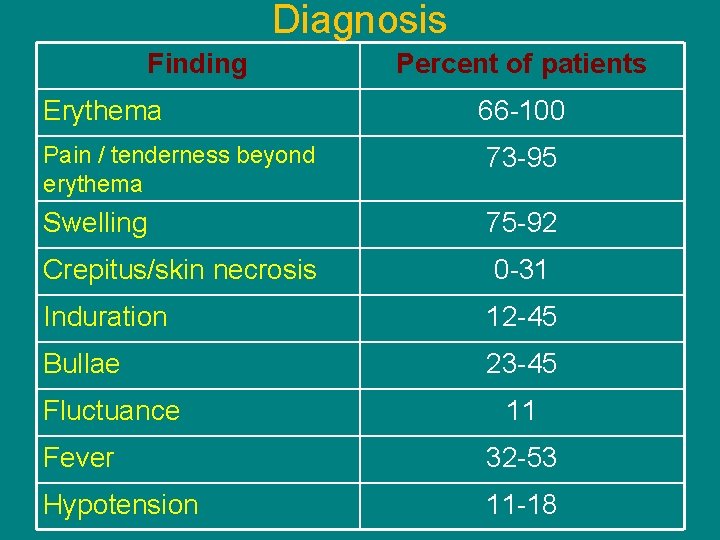
Diagnosis Finding Erythema Percent of patients 66 -100 Pain / tenderness beyond erythema 73 -95 Swelling 75 -92 Crepitus/skin necrosis 0 -31 Induration 12 -45 Bullae 23 -45 Fluctuance 11 Fever 32 -53 Hypotension 11 -18
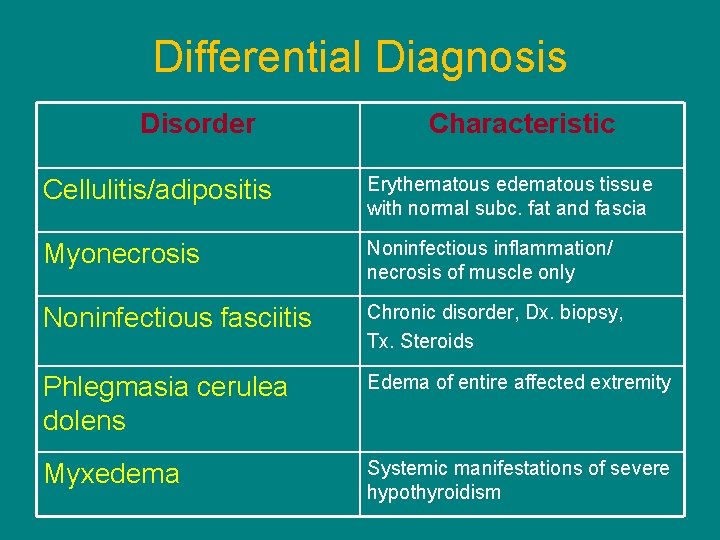
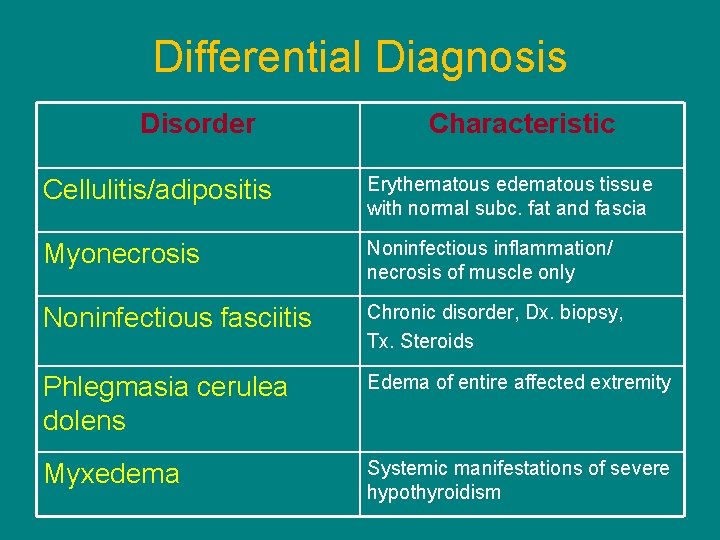
Differential Diagnosis Disorder Characteristic Cellulitis/adipositis Erythematous edematous tissue with normal subc. fat and fascia Myonecrosis Noninfectious inflammation/ necrosis of muscle only Noninfectious fasciitis Chronic disorder, Dx. biopsy, Tx. Steroids Phlegmasia cerulea dolens Edema of entire affected extremity Myxedema Systemic manifestations of severe hypothyroidism

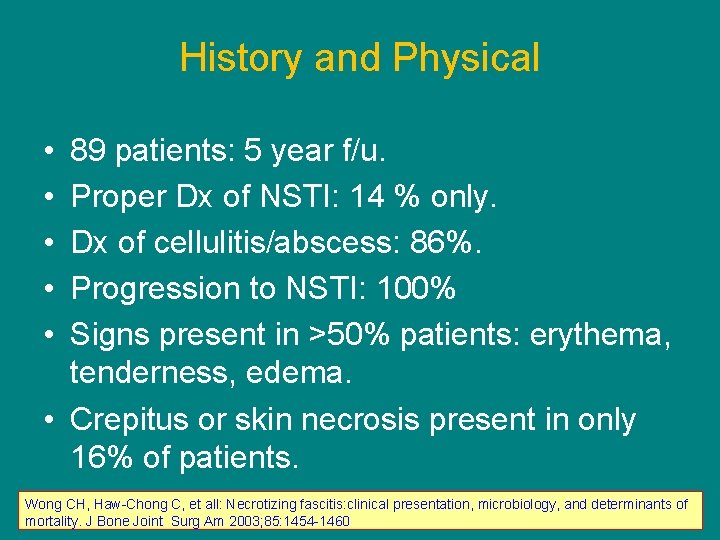
History and Physical ü Trauma/skin break 48 hrs. before symptoms (10 -40%) ü Local erythema ü Swelling with pain beyond the apparent confines of infection. ü Normal skin appearance in early stages. ü Crepitus or skin necrosis: 13 -31 % cases ü Vibrio vulnificus: fulminant NSTI ü Proper diagnosis as low as 14 % of cases.
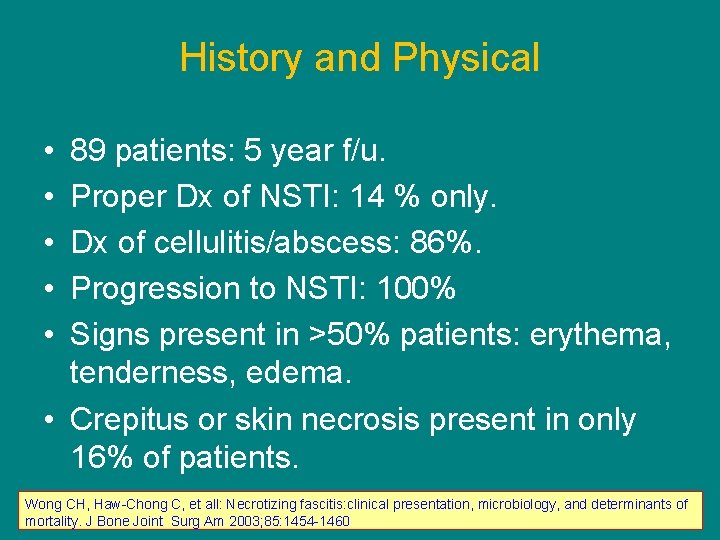
History and Physical • • • 89 patients: 5 year f/u. Proper Dx of NSTI: 14 % only. Dx of cellulitis/abscess: 86%. Progression to NSTI: 100% Signs present in >50% patients: erythema, tenderness, edema. • Crepitus or skin necrosis present in only 16% of patients. Wong CH, Haw-Chong C, et all: Necrotizing fascitis: clinical presentation, microbiology, and determinants of mortality. J Bone Joint Surg Am 2003; 85: 1454 -1460

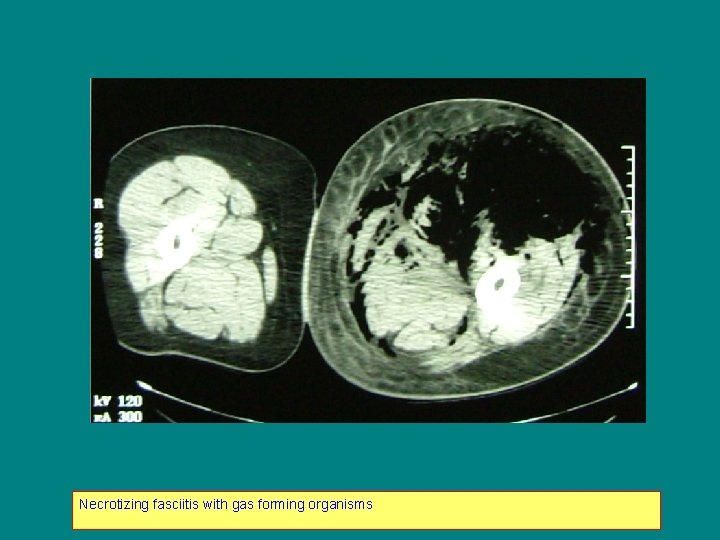
Radiographic Testing ü Plain x-ray: poor screening test. ü CT scan: more sensitive (plain) inflammatory changes gas formation fascial thickening: 80% sensitivity ü MRI: sensitivity 90 -100%, specificity 50 -85% prohibitive in critically ill, or unstable patients. (contrast-enhanced study)

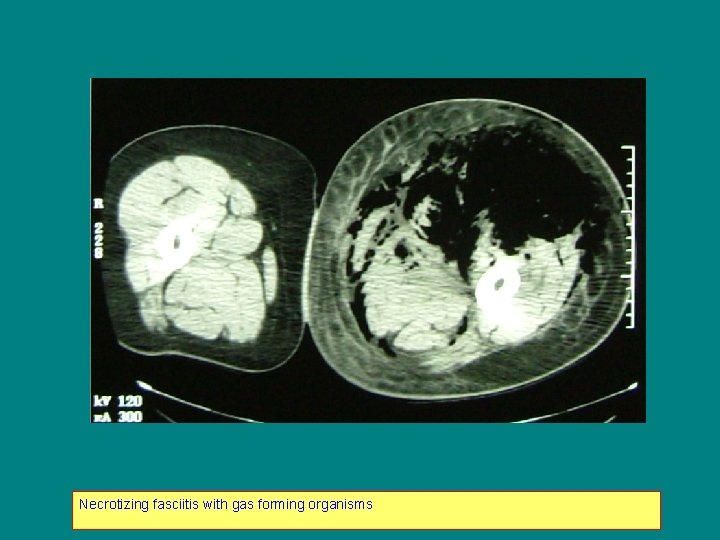
Necrotizing fasciitis with gas forming organisms
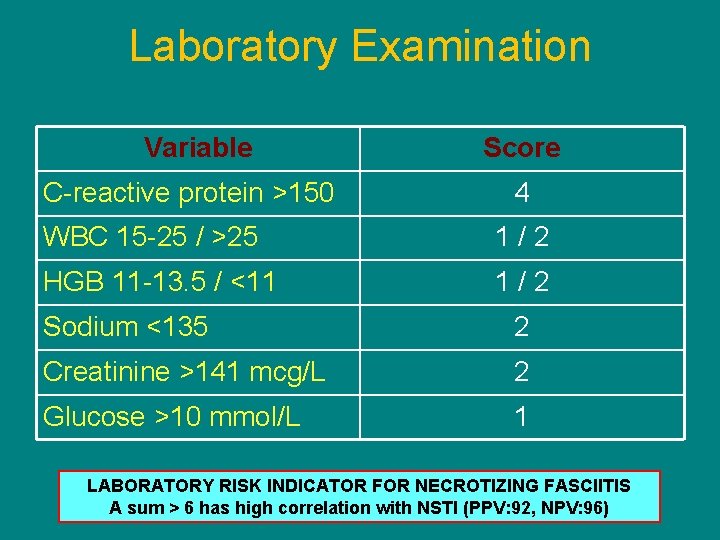
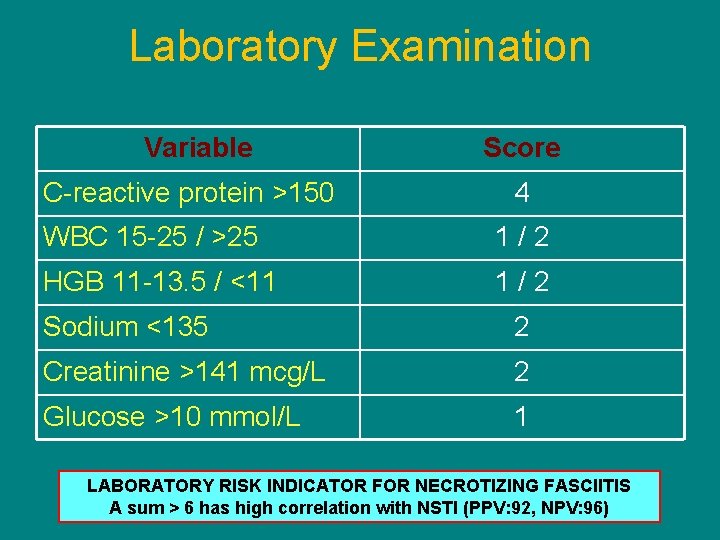
Laboratory Examination Variable C-reactive protein >150 Score 4 WBC 15 -25 / >25 1/2 HGB 11 -13. 5 / <11 1/2 Sodium <135 2 Creatinine >141 mcg/L 2 Glucose >10 mmol/L 1 LABORATORY RISK INDICATOR FOR NECROTIZING FASCIITIS A sum > 6 has high correlation with NSTI (PPV: 92, NPV: 96)
Operative Findings ü Operative exploration is the gold standard modality for diagnosis of NSTI ü “Dishwater” or foul-smelling discharge ü Necrosis ü Lack of bleeding ü Loss of normal resistance to the fascia. ü Biopsy from interface between live and dead tissue is rarely indicated.
Treatment Surgical Debridement (SD) ü Cornerstone of therapy. ü Delayed SD for more than 24 h is associated with a nine fold increase in mortality (Wong and colleagues) ü Wide excision to comprise healthy, bleeding tissue. ü Serial debridements ( 3 spaced 12 to 36 hrs. ) ü Amputation is a consideration ( IV drug users). ü Diverting colostomy for perineal/perianal NSTI ü Open wound , wet to dry dressings. ü Wound vac. ü Skin grafting for large wounds.
Treatment ü IV ABXs: Vancomycin, Linezolid, Daptomycin, quinupristin/dalfopristin, clindamycin ( G+) Clindamycin (anaerobes) Quinolones ( G-) ü IV IG: binds staph/strep toxins limiting SIRS. Not FDA approved. Critically ill patients from staph. or strept. ü Hyperbaric O 2: controversial and unproved. inhibits toxin elaboration by clostridia, increases local O 2 tension and killing ability of leukocytes.
Morbidity and Mortality ü Timing of operation the most critical determinant. ü Consider age, comorbidities, DM, shock, ARF, coagulopathy…. ü Morbidity as high as 82% (Eliot et all) ü Amputation rate 15 to 30% ü Complications: nosocomial infections, respiratory failure, ARDS, ARF, seizures, stroke, cardiac arrest….
Future efforts ü Monitor changes in microbiologic causes ü Enhance imaging techniques for early detection ü Role of adjunctive treatments

LLE NSTI in alcoholic patient from C. Perfingens
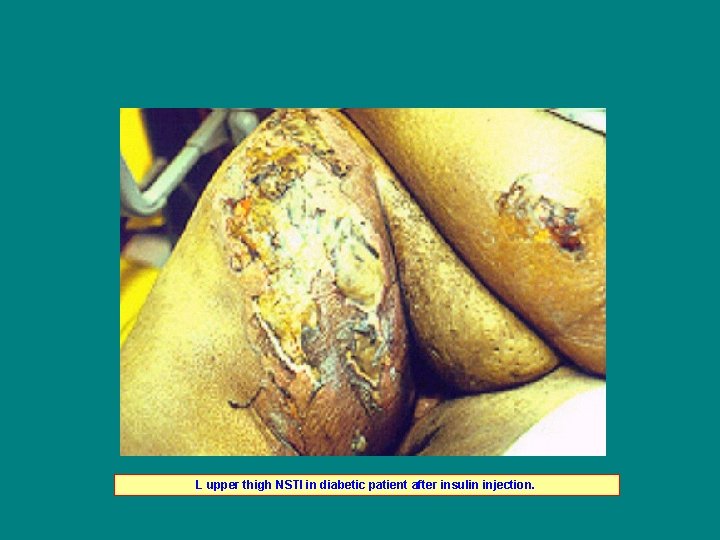
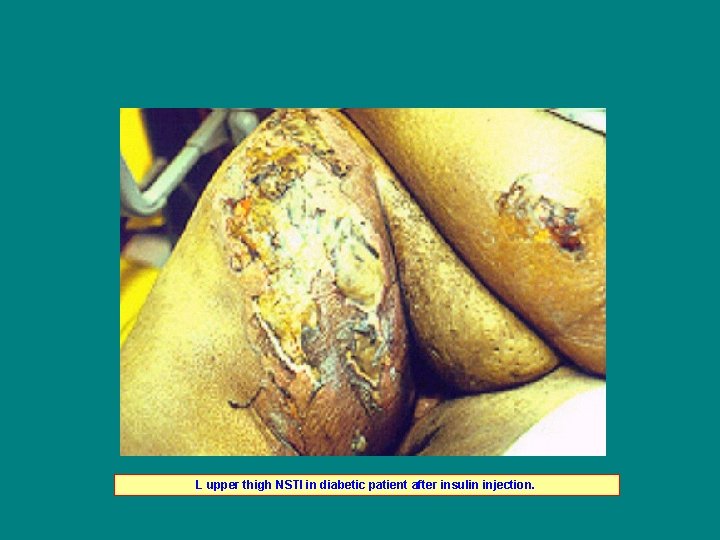
L upper thigh NSTI in diabetic patient after insulin injection.
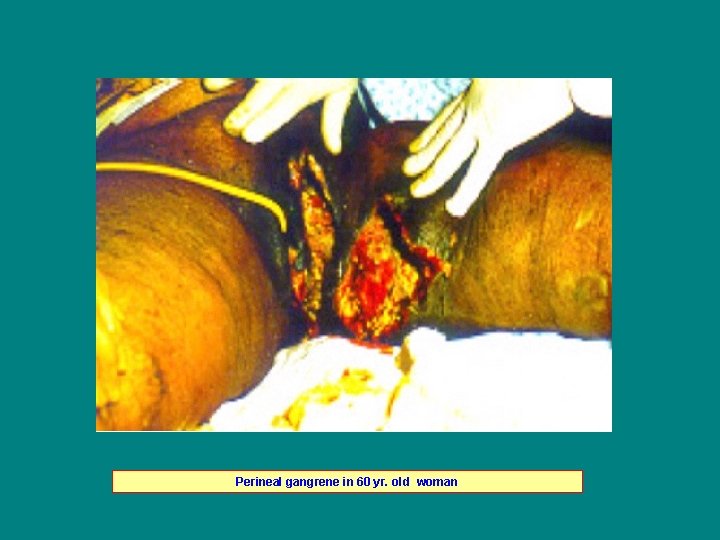
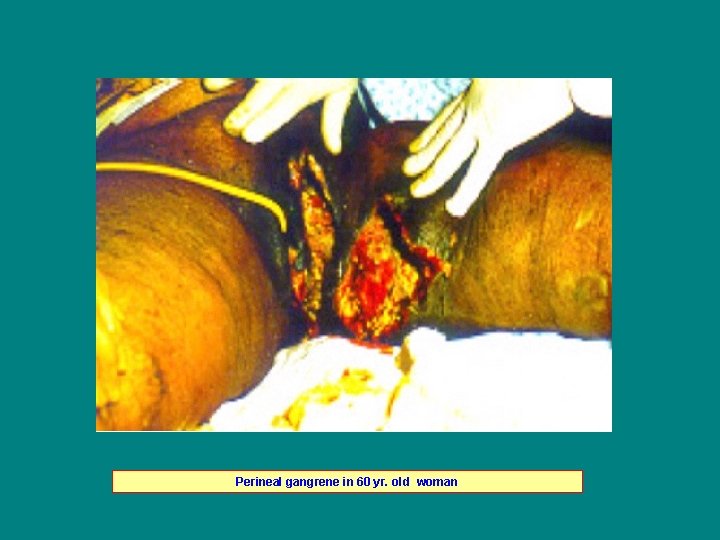
Perineal gangrene in 60 yr. old woman

L upper extremity NSTI from strep milleri
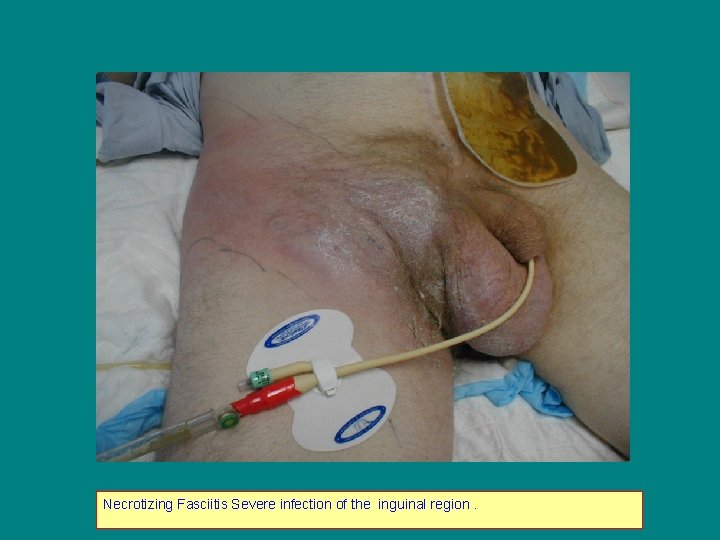
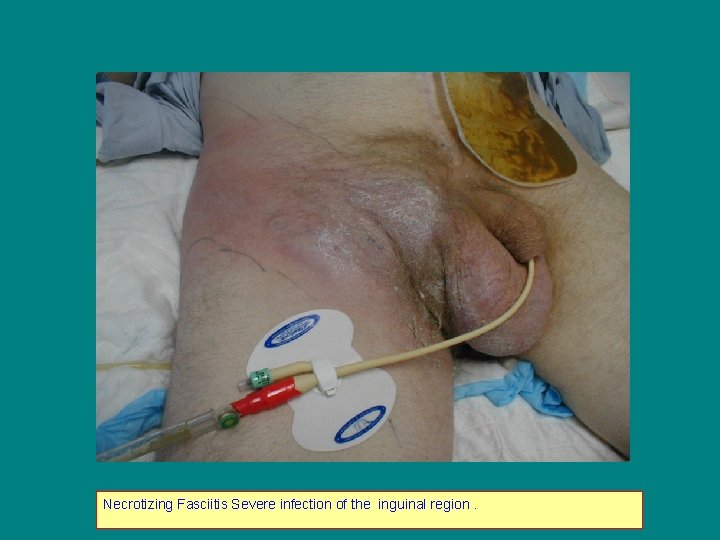
Necrotizing Fasciitis Severe infection of the inguinal region.
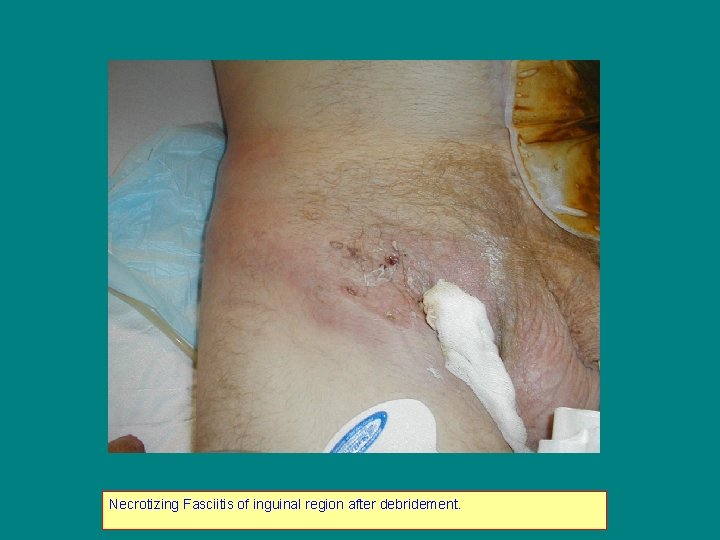
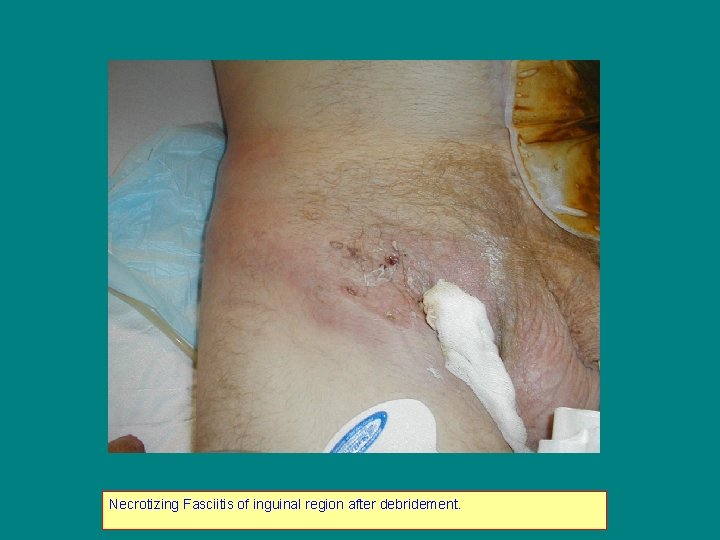
Necrotizing Fasciitis of inguinal region after debridement.

Necrotizing Fasciitis from group A Streptococcus (pyogenes)

L face debridement for Necrotizing Fasciitis

NSTI of R gluteal region after debridement.
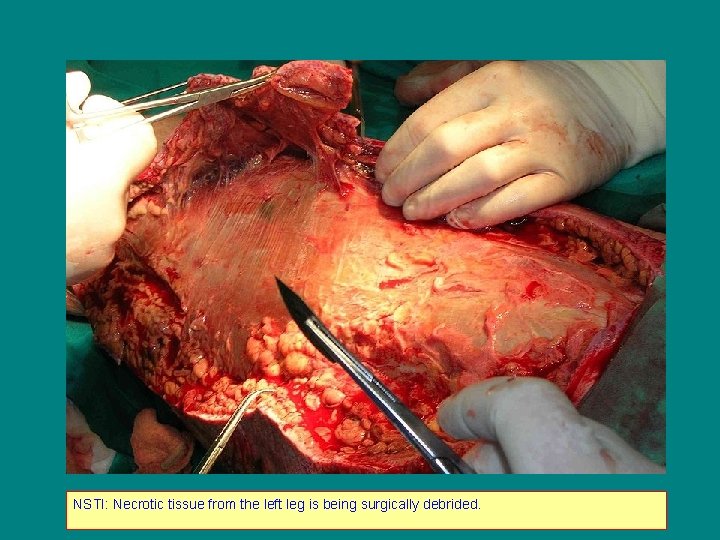
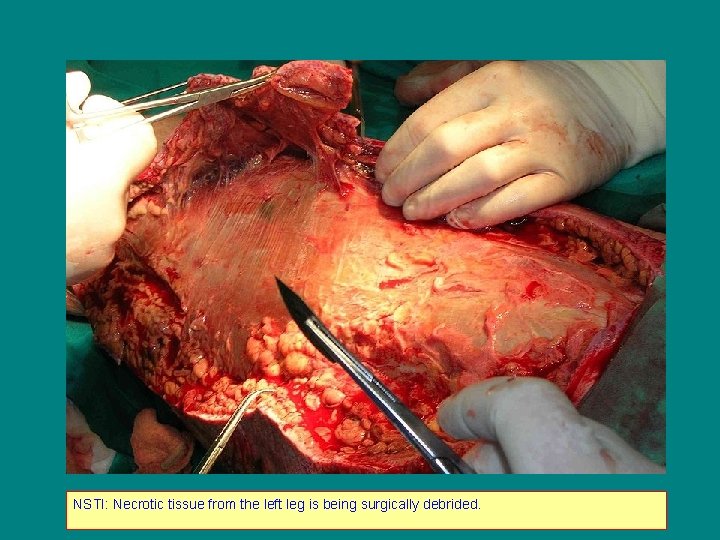
NSTI: Necrotic tissue from the left leg is being surgically debrided.
 Necrotizing fasciitis hemorrhagic bullae
Necrotizing fasciitis hemorrhagic bullae Necrotizing ulcerative gingivitis
Necrotizing ulcerative gingivitis Indication for exploratory laparotomy
Indication for exploratory laparotomy Nec disease
Nec disease Plantar fasciitis taping technique
Plantar fasciitis taping technique Acupressure tools dr berg
Acupressure tools dr berg Nodular fasciitis
Nodular fasciitis Nodular fasciitis
Nodular fasciitis Nodular fasciitis
Nodular fasciitis Nodular fasciitis
Nodular fasciitis Sugijanto fisioterapi
Sugijanto fisioterapi Prophylactic taping
Prophylactic taping Plantar fasciitis betekenis
Plantar fasciitis betekenis Line current and phase current
Line current and phase current Power formula three phase
Power formula three phase Semiconductor
Semiconductor Line current and phase current
Line current and phase current Drift vs diffusion current
Drift vs diffusion current Drift current and diffusion current in semiconductor
Drift current and diffusion current in semiconductor Wye delta diagram
Wye delta diagram Holding current and latching current
Holding current and latching current Diffusion current formula
Diffusion current formula The constant current area of a fet lies between
The constant current area of a fet lies between Dcep welding
Dcep welding Touch current vs leakage current
Touch current vs leakage current Kcl mesh analysis
Kcl mesh analysis Ssef price list
Ssef price list Bloomberg bmc solutions
Bloomberg bmc solutions Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Glasgow thang điểm
Glasgow thang điểm Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất