How to prevent gut disease in neonates Phillip


- Slides: 32
How to prevent gut disease in neonates Phillip Gordon Tulane
Topics we will cover �NEC (overview) �Term NEC �Preterm NEC associated with transfusions NEC associated with cows milk intolerance Catastrophic NEC �Spontaneous Intestinal Perforations
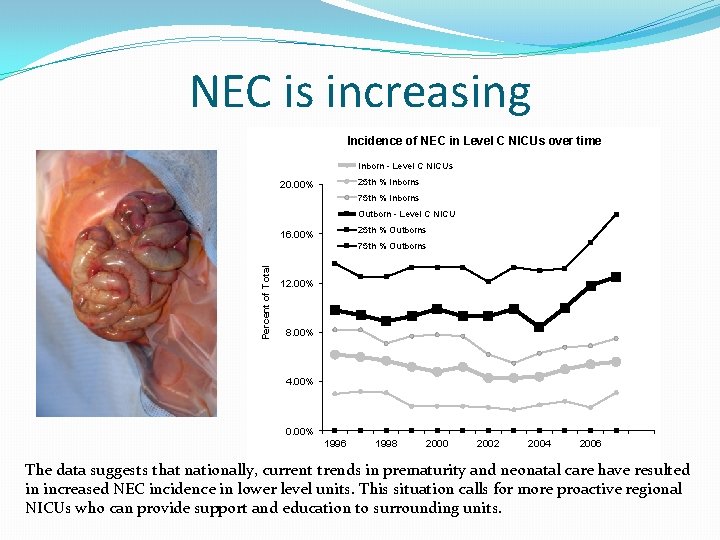
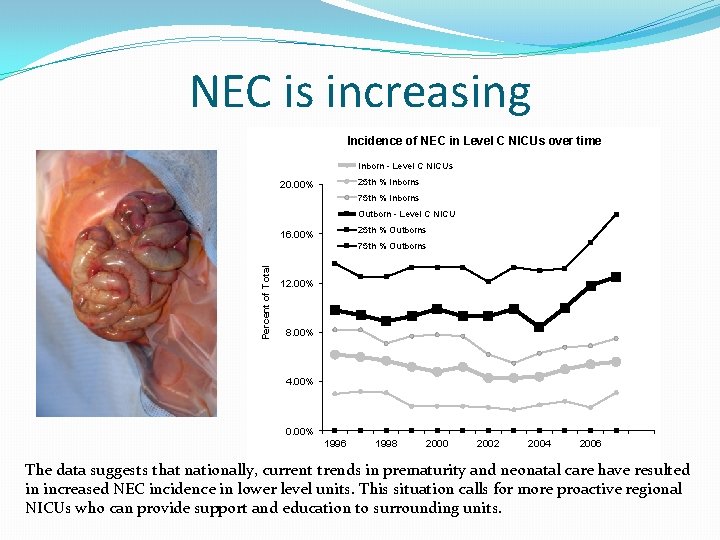
NEC is increasing Incidence of NEC in Level C NICUs over time Inborn - Level C NICUs 25 th % Inborns 20. 00% 75 th % Inborns Outborn - Level C NICU 25 th % Outborns 16. 00% Percent of Total 75 th % Outborns 12. 00% 8. 00% 4. 00% 0. 00% 1996 1998 2000 2002 2004 2006 The data suggests that nationally, current trends in prematurity and neonatal care have resulted in increased NEC incidence in lower level units. This situation calls for more proactive regional NICUs who can provide support and education to surrounding units.
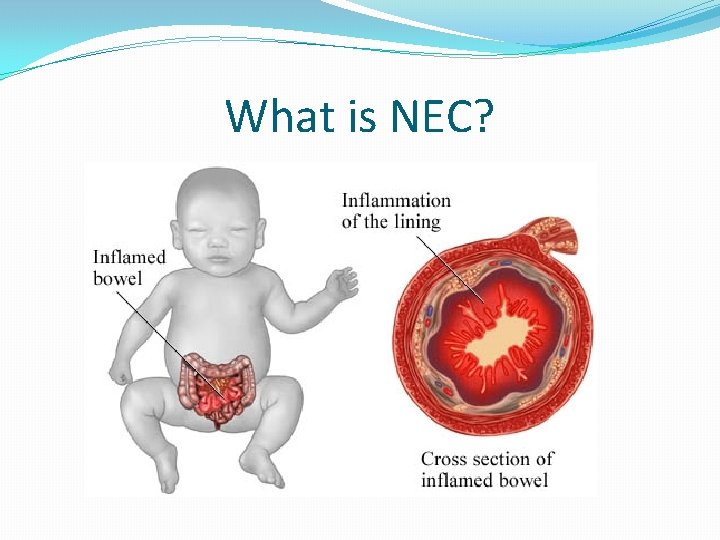
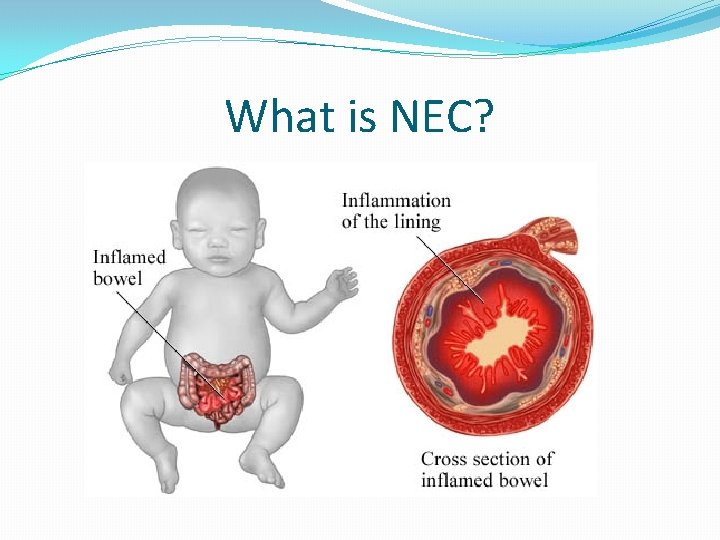
What is NEC?

It’s not just inflammation, it’s hemorrhagic necrosis Normal NEC The reason that this distinction is important is that the neonatal bowel is utilizing the innate immune system to modulate inflammation rather than adaptive immunity (which kicks in weeks to months later as we introduce food)
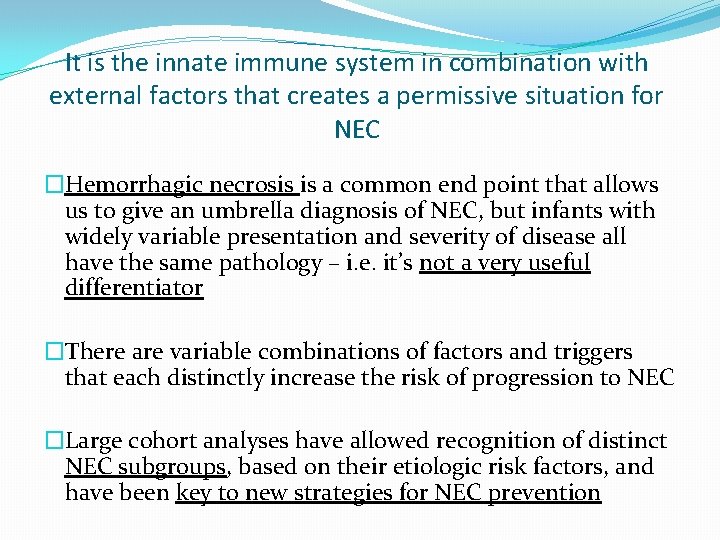
It is the innate immune system in combination with external factors that creates a permissive situation for NEC �Hemorrhagic necrosis is a common end point that allows us to give an umbrella diagnosis of NEC, but infants with widely variable presentation and severity of disease all have the same pathology – i. e. it’s not a very useful differentiator �There are variable combinations of factors and triggers that each distinctly increase the risk of progression to NEC �Large cohort analyses have allowed recognition of distinct NEC subgroups, based on their etiologic risk factors, and have been key to new strategies for NEC prevention

Review of term NEC risk factors Hypoxia / Ischemia Feeding a colonized gut Term NEC An immature and naive gut The Classic NEC Triad
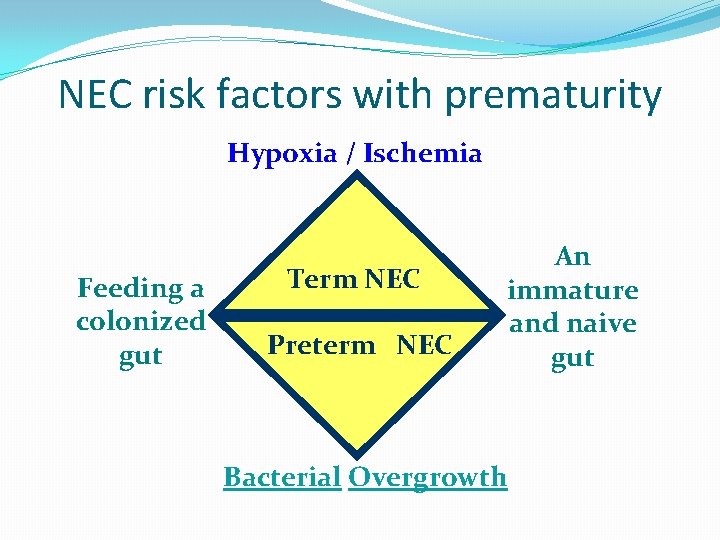
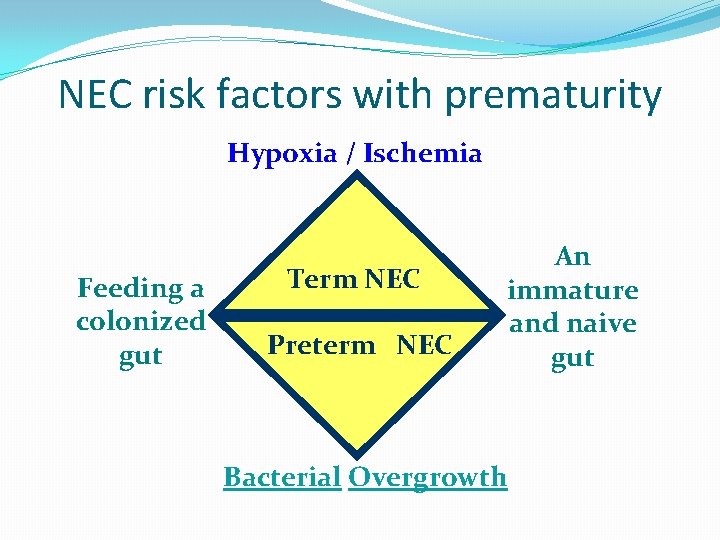
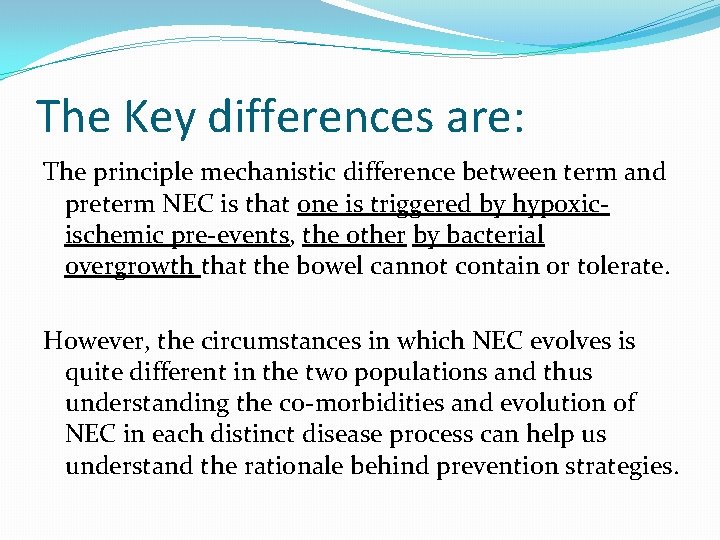
NEC risk factors with prematurity Hypoxia / Ischemia Feeding a colonized gut Term NEC Preterm NEC An immature and naive gut Bacterial Overgrowth
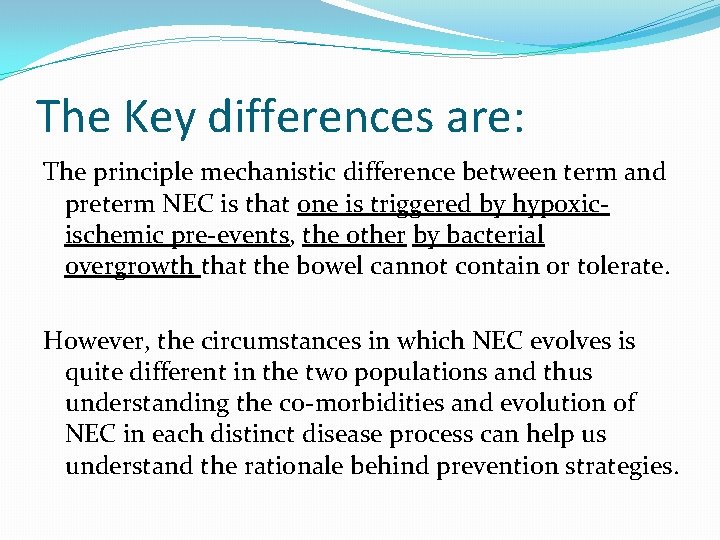
The Key differences are: The principle mechanistic difference between term and preterm NEC is that one is triggered by hypoxicischemic pre-events, the other by bacterial overgrowth that the bowel cannot contain or tolerate. However, the circumstances in which NEC evolves is quite different in the two populations and thus understanding the co-morbidities and evolution of NEC in each distinct disease process can help us understand the rationale behind prevention strategies.
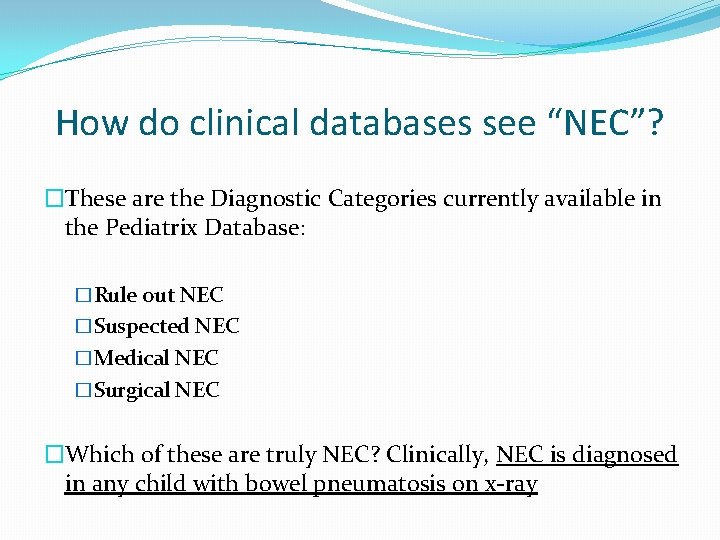
How do clinical databases see “NEC”? �These are the Diagnostic Categories currently available in the Pediatrix Database: �Rule out NEC �Suspected NEC �Medical NEC �Surgical NEC �Which of these are truly NEC? Clinically, NEC is diagnosed in any child with bowel pneumatosis on x-ray
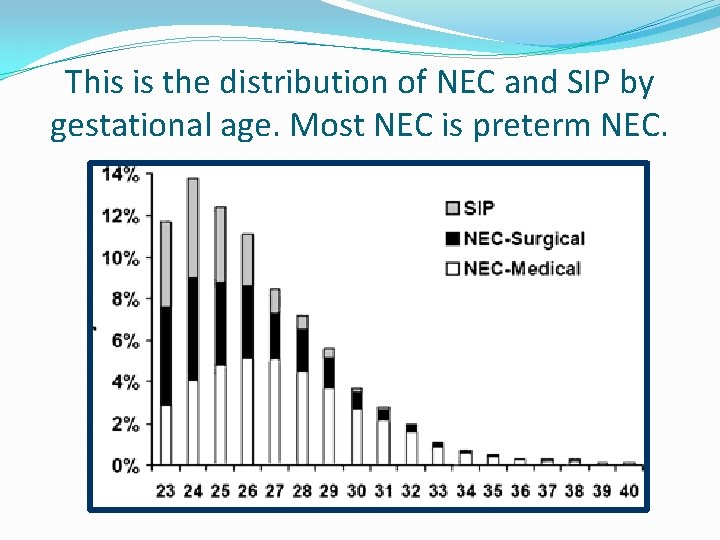
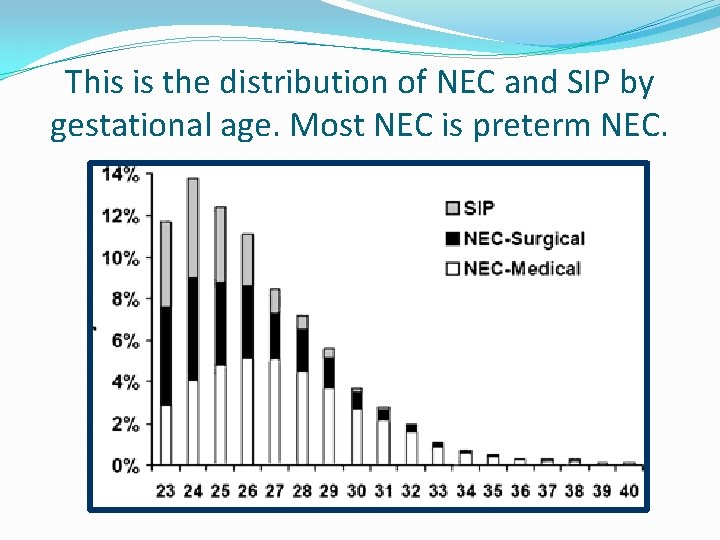
This is the distribution of NEC and SIP by gestational age. Most NEC is preterm NEC.
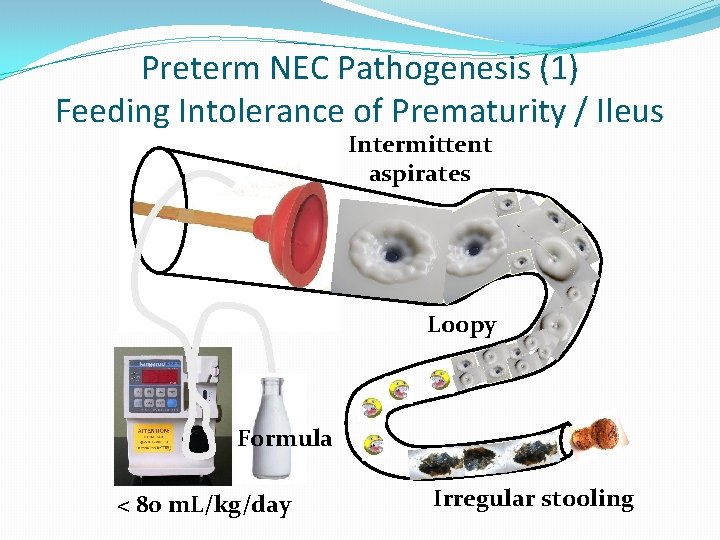
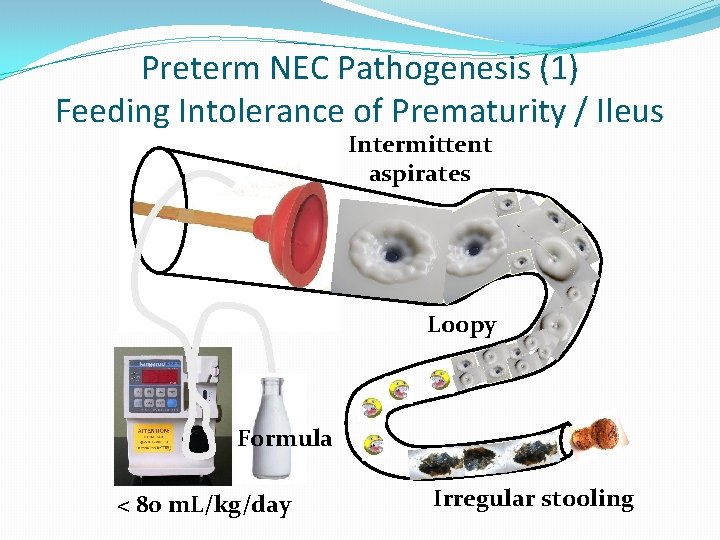
Preterm NEC Pathogenesis (1) Feeding Intolerance of Prematurity / Ileus Intermittent aspirates Loopy Formula < 80 m. L/kg/day Irregular stooling
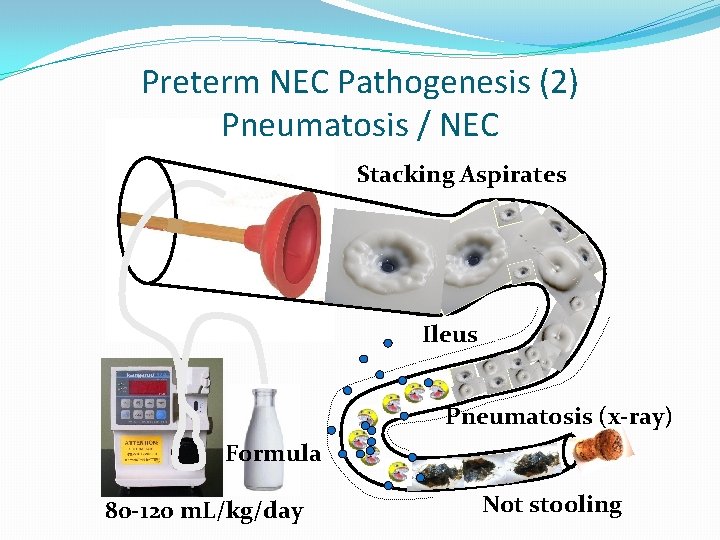
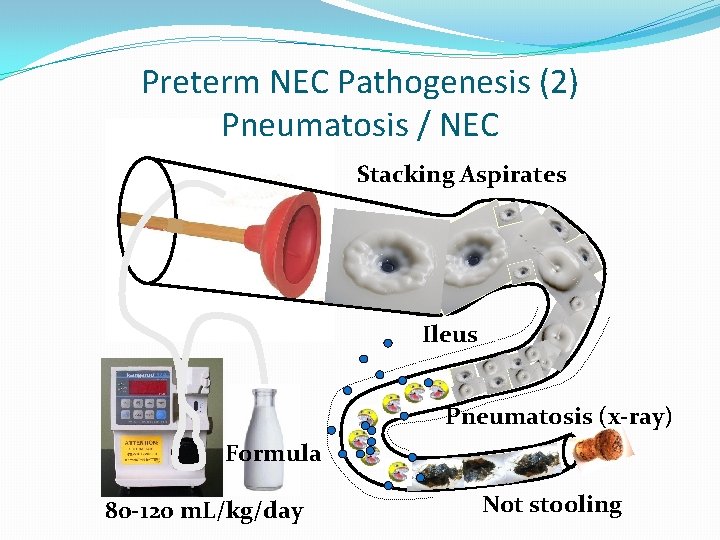
Preterm NEC Pathogenesis (2) Pneumatosis / NEC Stacking Aspirates Ileus Pneumatosis (x-ray) Formula 80 -120 m. L/kg/day Not stooling
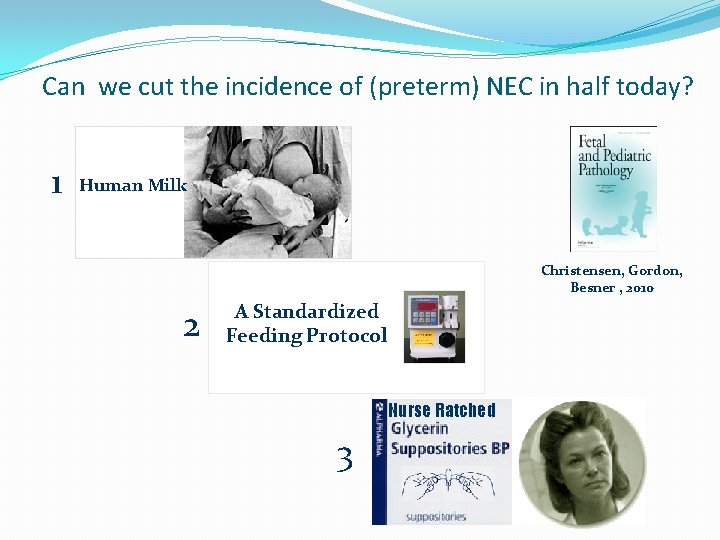
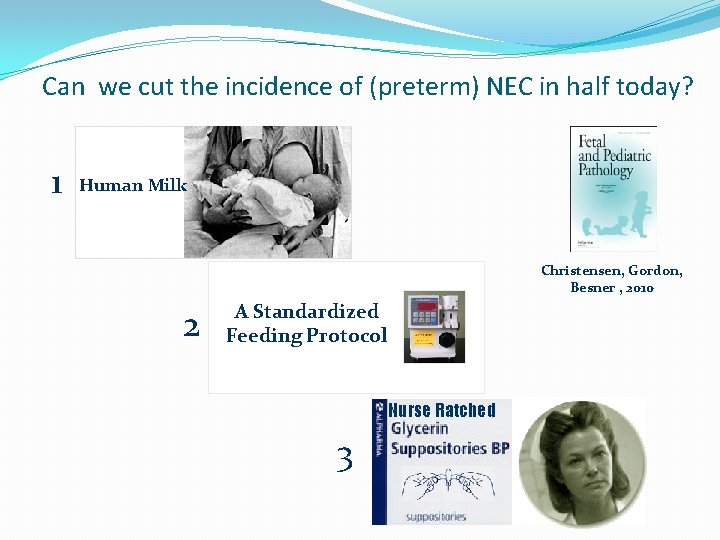
Can we cut the incidence of (preterm) NEC in half today? 1 Human Milk Christensen, Gordon, Besner , 2010 2 A Standardized Feeding Protocol Nurse Ratched 3
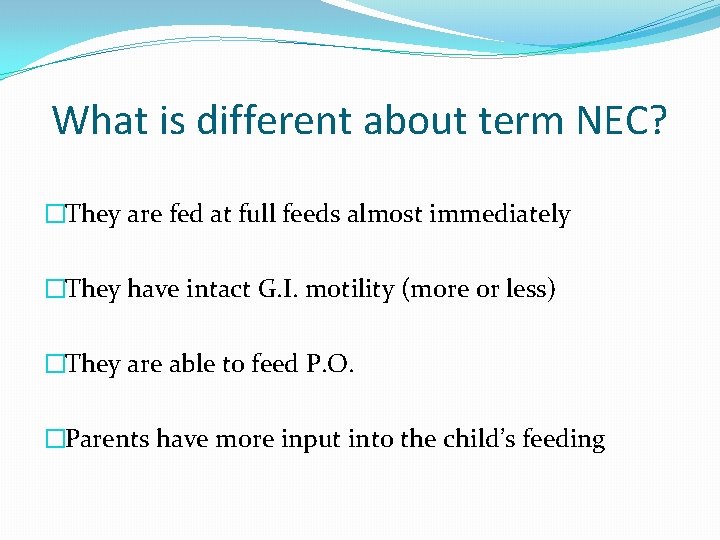
What is different about term NEC? �They are fed at full feeds almost immediately �They have intact G. I. motility (more or less) �They are able to feed P. O. �Parents have more input into the child’s feeding
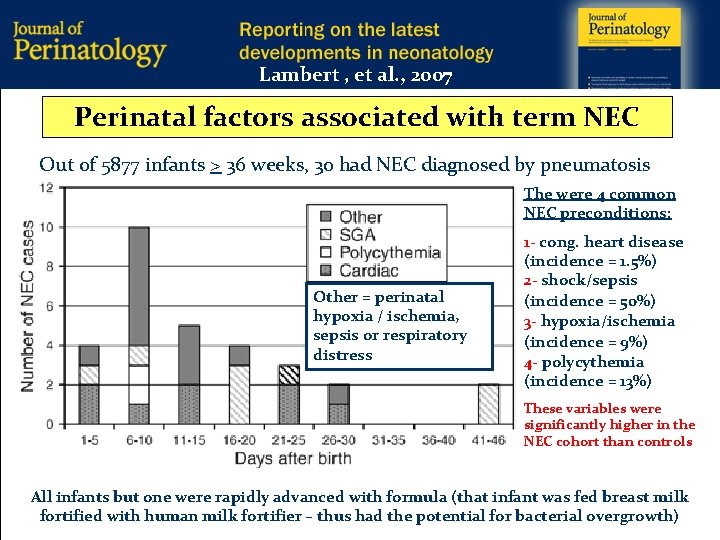
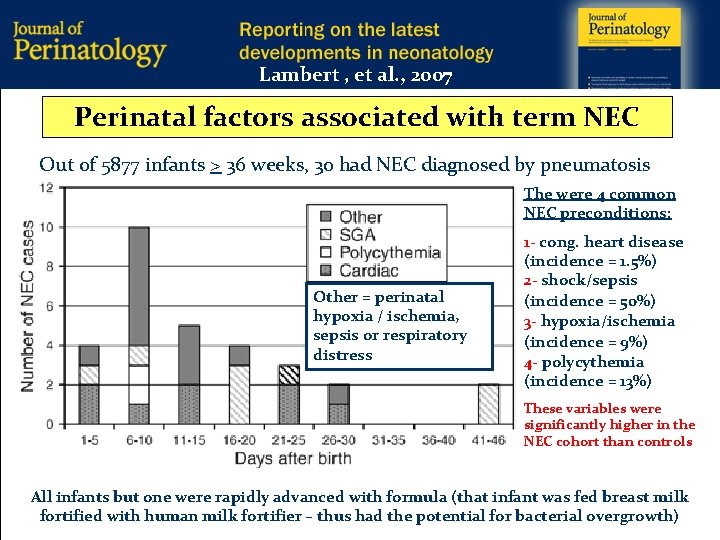
Lambert , et al. , 2007 Perinatal factors associated with term NEC Out of 5877 infants > 36 weeks, 30 had NEC diagnosed by pneumatosis The were 4 common NEC preconditions: Other = perinatal hypoxia / ischemia, sepsis or respiratory distress 1 - cong. heart disease (incidence = 1. 5%) 2 - shock/sepsis (incidence = 50%) 3 - hypoxia/ischemia (incidence = 9%) 4 - polycythemia (incidence = 13%) These variables were significantly higher in the NEC cohort than controls All infants but one were rapidly advanced with formula (that infant was fed breast milk fortified with human milk fortifier – thus had the potential for bacterial overgrowth)
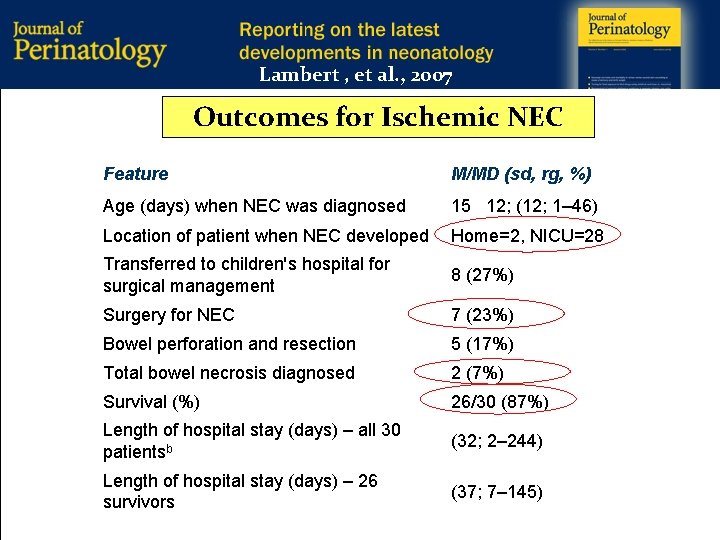
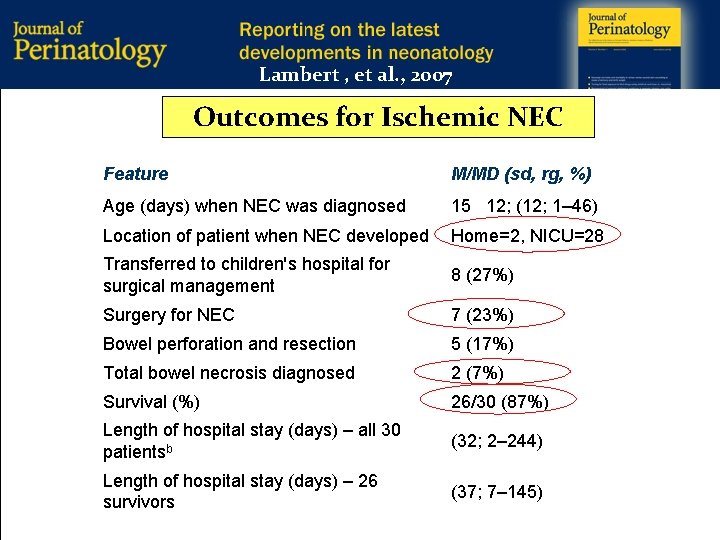
Lambert , et al. , 2007 Outcomes for Ischemic NEC Feature M/MD (sd, rg, %) Age (days) when NEC was diagnosed 15 12; (12; 1– 46) Location of patient when NEC developed Home=2, NICU=28 Transferred to children's hospital for surgical management 8 (27%) Surgery for NEC 7 (23%) Bowel perforation and resection 5 (17%) Total bowel necrosis diagnosed 2 (7%) Survival (%) 26/30 (87%) Length of hospital stay (days) – all 30 patientsb (32; 2– 244) Length of hospital stay (days) – 26 survivors (37; 7– 145)
Preventing term NEC �Term NEC has preconditions that place patient’s at risk. Exclusive feeding of human milk may reduce risk, but this population is rarer and more challenging to capture for standardized feeding protocols (especially in nontertiary NICUs) and thus may not be as amenable to prevention when compared to preterm NEC. �A high index of suspicion for a co-morbid, perinatal risk factors should prompt a controlled feeding advance (50 ml/kg/day on day 1 -> 100 ml/kg/day on day 2 -> 150 ml/kg/day on day 3) to facilitate observation during the period of greatest risk
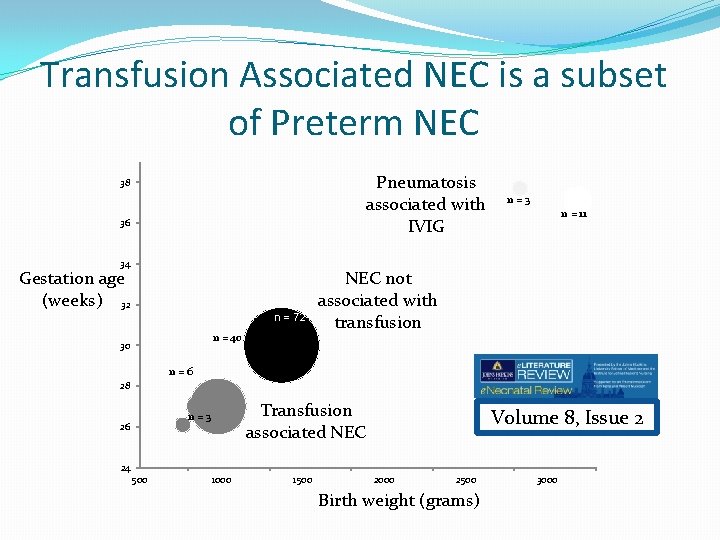
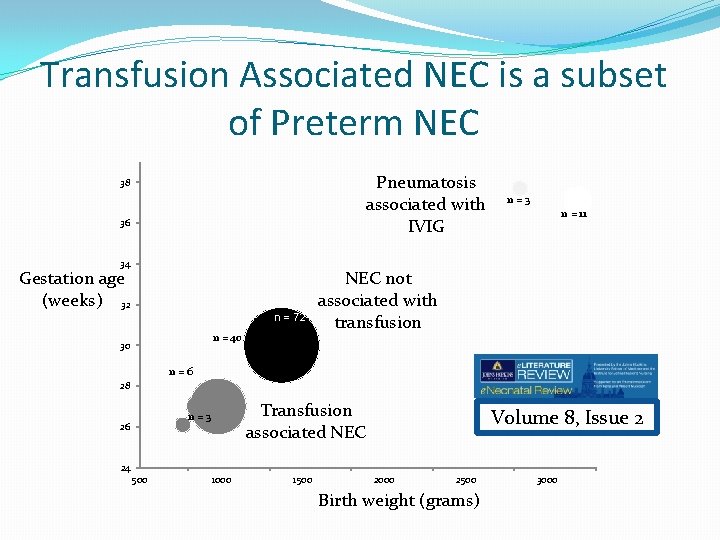
Transfusion Associated NEC is a subset of Preterm NEC Pneumatosis associated with IVIG 38 36 34 Gestation age (weeks) 32 n = 72 n = 40 30 n=3 n = 11 NEC not associated with transfusion n=6 28 Transfusion associated NEC n=3 26 Volume 8, Issue 2 24 500 1000 1500 2000 2500 Birth weight (grams) 3000
What are the co-travelers with transfusion-associated NEC? �Incidence is decreased in infants receiving breast milk �Incidence is decreased in infants whose feedings are held during the time of transfusion �Incidence is increased in infants with lowest HCTs �Incidence is increased in infants on exclusive formula feeds �Incidence is increased in infants who have had a previous transfusion �There is no relation to the age of the p. RBCs at time of transfusion
Cows Milk Allergy versus NEC We have known for some time that infants with cows milk allergy can present with pneumatosis. More recently, we have seen case studies and case series demonstrating premature infants with multiple episodes of pneumatosis that finally resolve with elemental formula and that are highlighted by eosinophilia in the stool and/or blood which also resolve with elemental formula. These infants have a milder form of NEC that is precipitated principally by relatively early onset of milk allergy (usually not before 4 weeks of life). Gordon et al. J. Perinatol, 2008
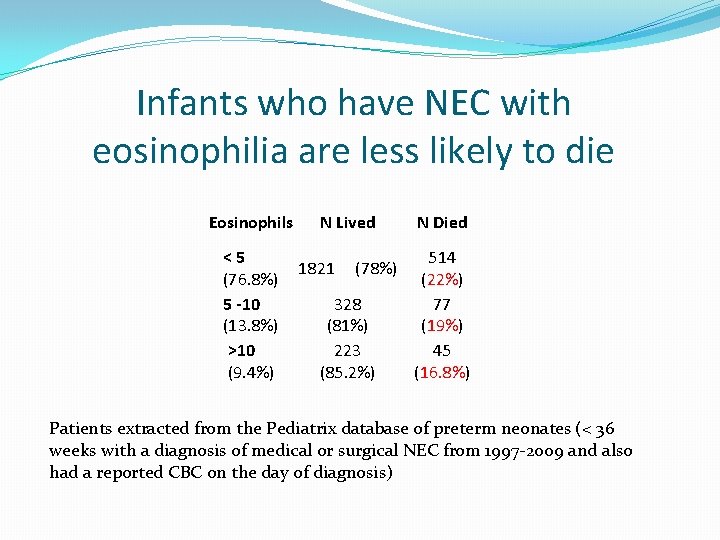
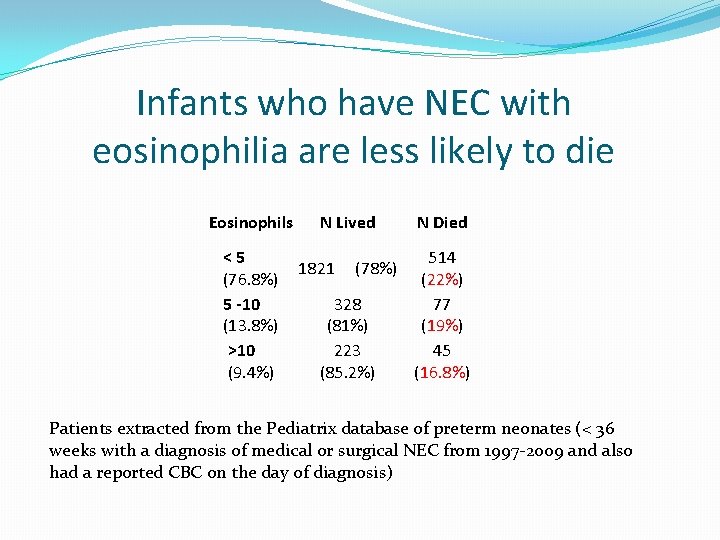
Infants who have NEC with eosinophilia are less likely to die Eosinophils <5 (76. 8%) 5 -10 (13. 8%) >10 (9. 4%) N Lived 1821 (78%) 328 (81%) 223 (85. 2%) N Died 514 (22%) 77 (19%) 45 (16. 8%) Patients extracted from the Pediatrix database of preterm neonates (< 36 weeks with a diagnosis of medical or surgical NEC from 1997 -2009 and also had a reported CBC on the day of diagnosis)
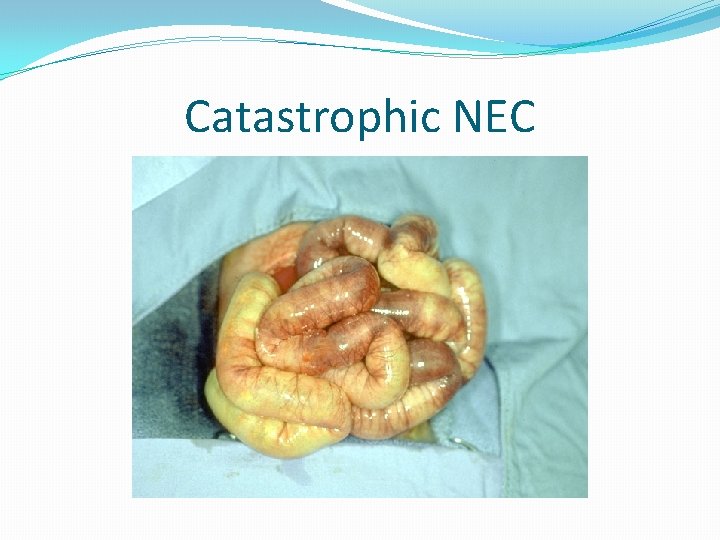
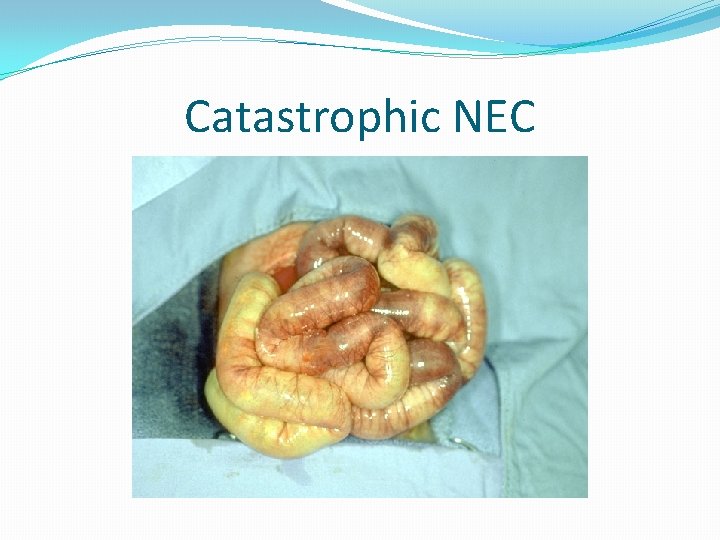
Catastrophic NEC
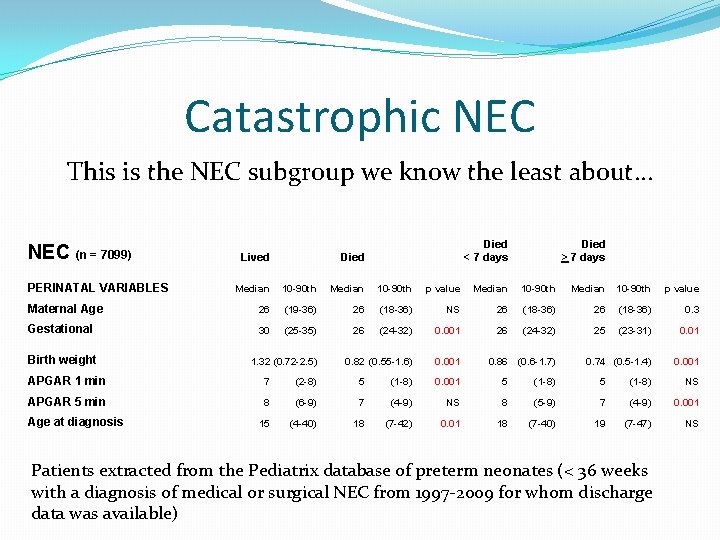
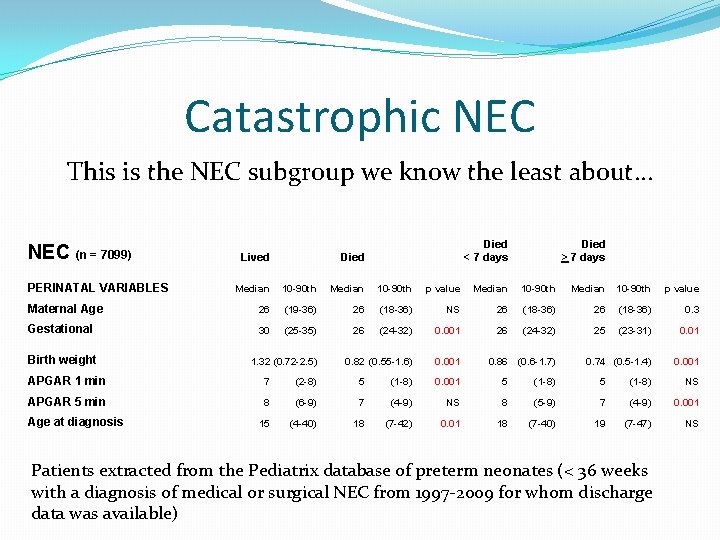
Catastrophic NEC This is the NEC subgroup we know the least about… NEC (n = 7099) PERINATAL VARIABLES Lived Died < 7 days Died > 7 days Median 10 -90 th p value Maternal Age 26 (19 -36) 26 (18 -36) NS 26 (18 -36) 0. 3 Gestational 30 (25 -35) 26 (24 -32) 0. 001 26 (24 -32) 25 (23 -31) 0. 01 0. 82 (0. 55 -1. 6) 0. 001 0. 74 (0. 5 -1. 4) 0. 001 Birth weight 1. 32 (0. 72 -2. 5) 0. 86 (0. 6 -1. 7) APGAR 1 min 7 (2 -8) 5 (1 -8) 0. 001 5 (1 -8) NS APGAR 5 min 8 (6 -9) 7 (4 -9) NS 8 (5 -9) 7 (4 -9) 0. 001 15 (4 -40) 18 (7 -42) 0. 01 18 (7 -40) 19 (7 -47) NS Age at diagnosis Patients extracted from the Pediatrix database of preterm neonates (< 36 weeks with a diagnosis of medical or surgical NEC from 1997 -2009 for whom discharge data was available)
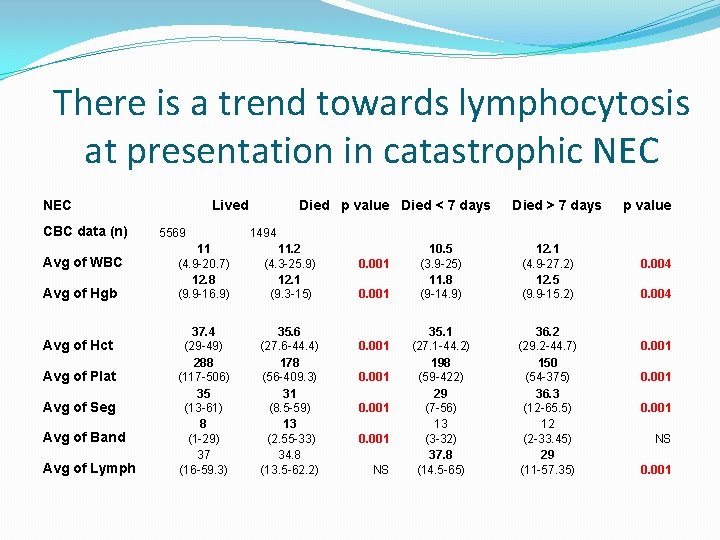
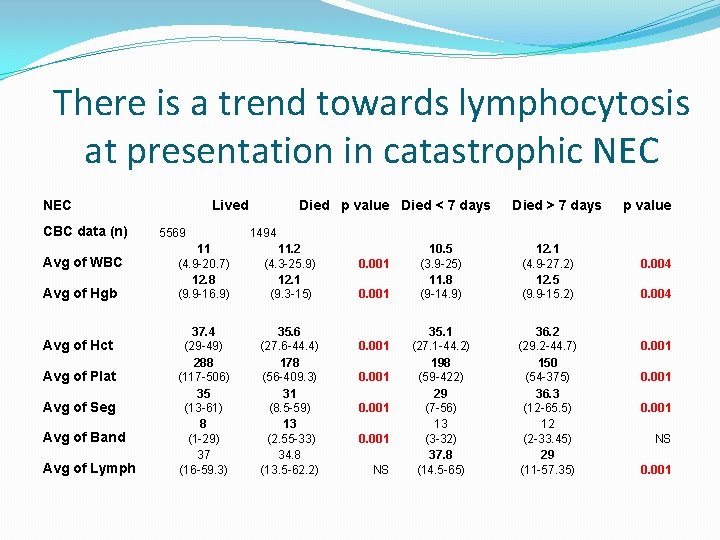
There is a trend towards lymphocytosis at presentation in catastrophic NEC CBC data (n) Avg of WBC Avg of Hgb Avg of Hct Avg of Plat Avg of Seg Avg of Band Avg of Lymph Lived 5569 Died p value Died < 7 days Died > 7 days p value 1494 11 (4. 9 -20. 7) 12. 8 (9. 9 -16. 9) 11. 2 (4. 3 -25. 9) 12. 1 (9. 3 -15) 37. 4 (29 -49) 288 (117 -506) 35 (13 -61) 8 (1 -29) 37 (16 -59. 3) 35. 6 (27. 6 -44. 4) 178 (56 -409. 3) 31 (8. 5 -59) 13 (2. 55 -33) 34. 8 (13. 5 -62. 2) 0. 001 NS 10. 5 (3. 9 -25) 11. 8 (9 -14. 9) 12. 1 (4. 9 -27. 2) 12. 5 (9. 9 -15. 2) 35. 1 (27. 1 -44. 2) 198 (59 -422) 29 (7 -56) 13 (3 -32) 37. 8 (14. 5 -65) 36. 2 (29. 2 -44. 7) 150 (54 -375) 36. 3 (12 -65. 5) 12 (2 -33. 45) 29 (11 -57. 35) 0. 004 0. 001 NS 0. 001
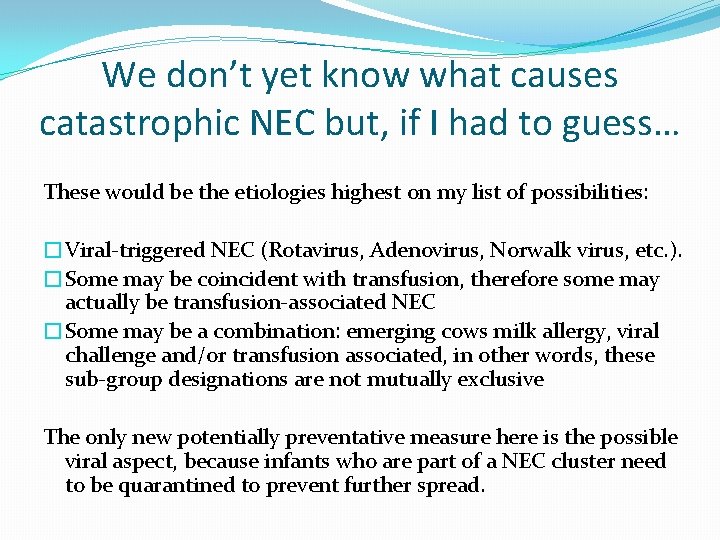
We don’t yet know what causes catastrophic NEC but, if I had to guess… These would be the etiologies highest on my list of possibilities: �Viral-triggered NEC (Rotavirus, Adenovirus, Norwalk virus, etc. ). �Some may be coincident with transfusion, therefore some may actually be transfusion-associated NEC �Some may be a combination: emerging cows milk allergy, viral challenge and/or transfusion associated, in other words, these sub-group designations are not mutually exclusive The only new potentially preventative measure here is the possible viral aspect, because infants who are part of a NEC cluster need to be quarantined to prevent further spread.
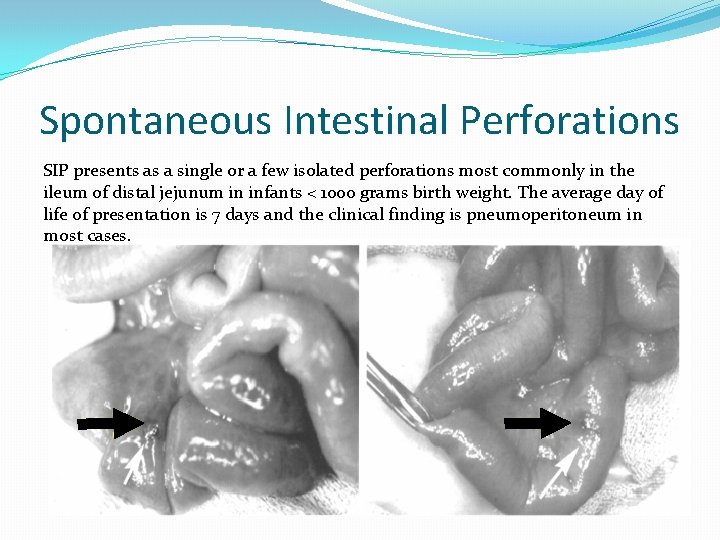
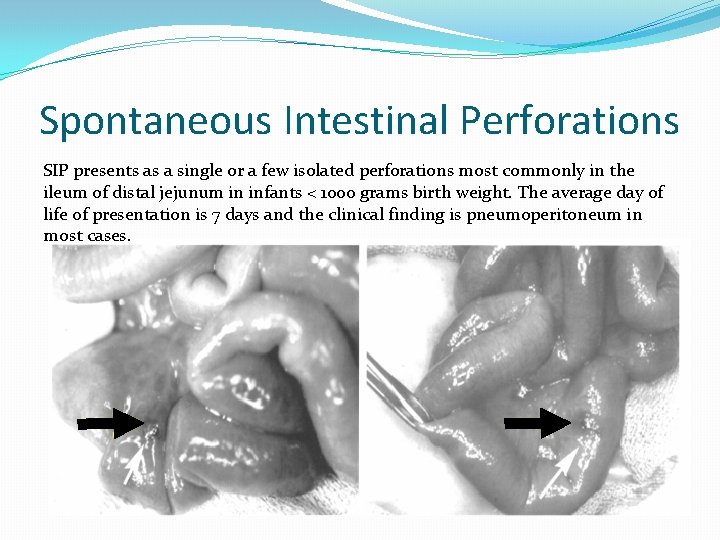
Spontaneous Intestinal Perforations SIP presents as a single or a few isolated perforations most commonly in the ileum of distal jejunum in infants < 1000 grams birth weight. The average day of life 0 f presentation is 7 days and the clinical finding is pneumoperitoneum in most cases.
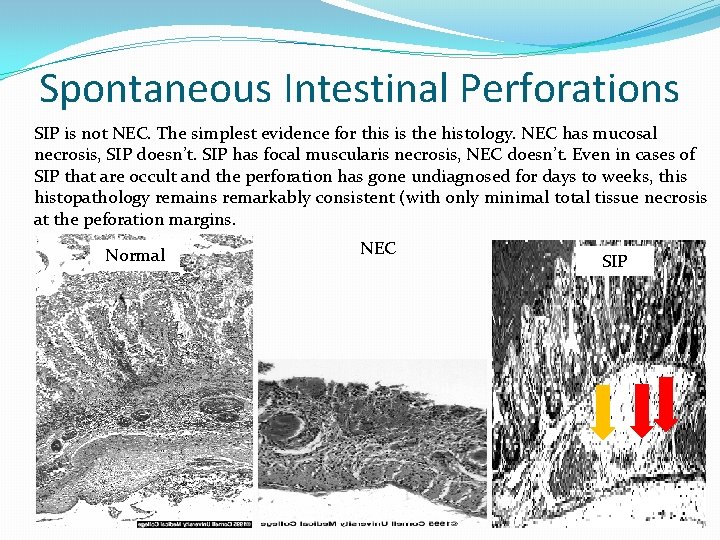
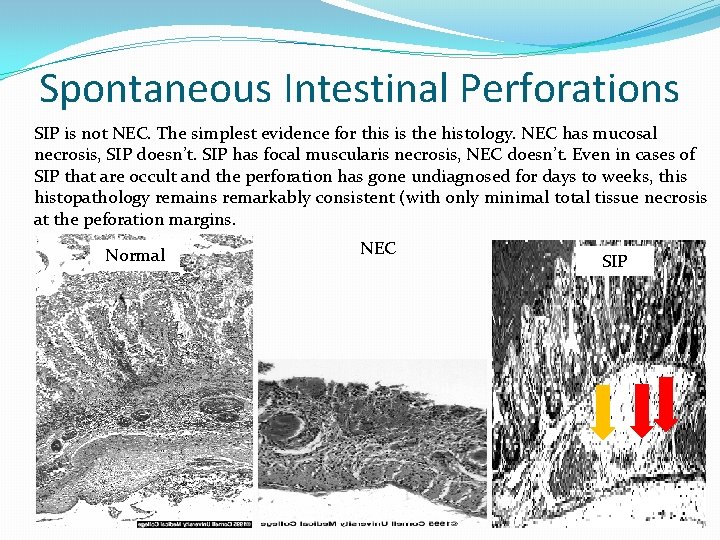
Spontaneous Intestinal Perforations SIP is not NEC. The simplest evidence for this is the histology. NEC has mucosal necrosis, SIP doesn’t. SIP has focal muscularis necrosis, NEC doesn’t. Even in cases of SIP that are occult and the perforation has gone undiagnosed for days to weeks, this histopathology remains remarkably consistent (with only minimal total tissue necrosis at the peforation margins. Normal NEC SIP
Risk factors associated with SIP �Extreme prematurity / low birth weight (< 100 o grams) �Early postnatal steroids (dexamethasone or hydrocortisone) �Early postnatal indomethacin (in the first 4 days of life) �The combination of early steroids and early indomethacin �Early postnatal ibuprofen �Prenatal indomethacin, given shortly before delivery of an extremely premature infant (for tocolysis) �SGA infants who are also premature. �High endogenous cortisol levels in the first days of life �Candida chorioamnionitis
Summary of surgical outcomes data for SIP & NEC �SIP preferentially treated by drain is associated with increased c. PVL and likely increased neurodevelopmental insult (NDI) compared to age matched controls �Surgical NEC has a higher mortality than SIP and has a greater risk of NDI when compared to SIP cohorts and controls, but all available data suffers from SIP contamination in currently published NEC cohorts. �It is probable that NDI associated with NEC and SIP could be improved by choosing primary laparotomy rather than drain. �It is imperative that future outcome studies differentiate SIP from NEC in the primary disease cohorts
SIP and NEC are preventable diseases �No early steroids or NSAIDs �Use feeding guidelines, initiate feeding advances early �Promote breast milk feeding at every opportunity �Use glycerin as appropriate �Minimize blood draws and transfusions (draw retics with HCTs) �Wash your hands between babies �Pay attention to aspirates that “stack”, ignore those that don’t, ignore all colors but dark green. �Don’t over wean the respiratory support or the isolette temp while advancing feeds �Quarantine infants with NEC to minimize the chance of NEC clusters (contact precautions).
The End
 Grading of jaundice in neonates
Grading of jaundice in neonates Thermoneutral environment for neonates
Thermoneutral environment for neonates Subcostal retractions
Subcostal retractions Grading of jaundice in neonates
Grading of jaundice in neonates Normal cbc in neonates
Normal cbc in neonates Facilitated tucking neonates
Facilitated tucking neonates Definition of high risk neonates
Definition of high risk neonates Thermoneutral environment for neonates
Thermoneutral environment for neonates Energy triangle neonates
Energy triangle neonates Bharathi viswanathan
Bharathi viswanathan Deacon and phillip
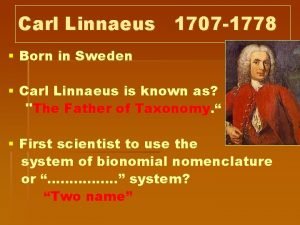
Deacon and phillip King phillip came over for good spaghetti
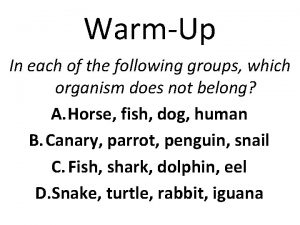
King phillip came over for good spaghetti Kingdom phylum class order
Kingdom phylum class order Philip lah
Philip lah Benefits of prokaryotes
Benefits of prokaryotes Philip bayard crosby
Philip bayard crosby Phillip gardiner tobacco
Phillip gardiner tobacco Rooikappie philip de vos
Rooikappie philip de vos Phillip garber
Phillip garber Phillip zimbardo
Phillip zimbardo Phillip a. scherrer
Phillip a. scherrer King phillip acronym
King phillip acronym Phillip crisp
Phillip crisp Organisms taxonomy
Organisms taxonomy 3rd person omniscient
3rd person omniscient The levels of classification
The levels of classification Phillip gilley
Phillip gilley Whale dichotomous key
Whale dichotomous key Phillip crisp
Phillip crisp Philip larkin they your mum and dad
Philip larkin they your mum and dad Math 2565
Math 2565 Dear king phillip came over
Dear king phillip came over Phillip crisp
Phillip crisp