NECROTIZING ENTEROCOLITIS Case Study Fall 2015 NECROTIZING ENTEROCOLITIS


- Slides: 26
NECROTIZING ENTEROCOLITIS Case Study Fall 2015
NECROTIZING ENTEROCOLITIS (NEC) • A condition that occurs mostly in premature or sick newborn infants where their intestinal tissue dies. 1 • The exact etiology is not clear but it is thought that the ischemic insult damages the intestinal lining. This leads to increased intestinal permeability and leaves the intestine subject to bacteria. 2
INCIDENCE • Most common severe neonatal gastrointestinal emergency that occurs in 1 to 8% of NICU admissions 2, 3 • Mortality rates range between 20 to 30%³ • 85% of very low birth weight premature infants (< 1, 500)3
RISK FACTORS AND CAUSE • Enteral Feedings • Aggressive and improper enteral feedings • Formula vs Breastmilk • Prematurity • 29 to 31 weeks post menstrual age • Immaturity of key gastrointestinal functions • Bacteria Colonization • Antibiotics • More than 10 days increased risk by 3 fold • Blood Transfusions • Prolonged rupture of the membranes • Birth Asphyxia • Congenital heart disease 3, 4, 5

SIGNS AND SYMPTOMS Intestinal Signs Systemic Signs • Feeding intolerance • Lethargy • Pre feeding gastric residuals • Hypotension • Emesis • Poor perfusion and pallor • Abdominal distention • Increased episode of apnea • Bloody stool • Worsening of respiratory function • Abdomen may appear shiny, distended, and erythematous • Temperature instability • Hyperglycemia or hypoglycemia⁴
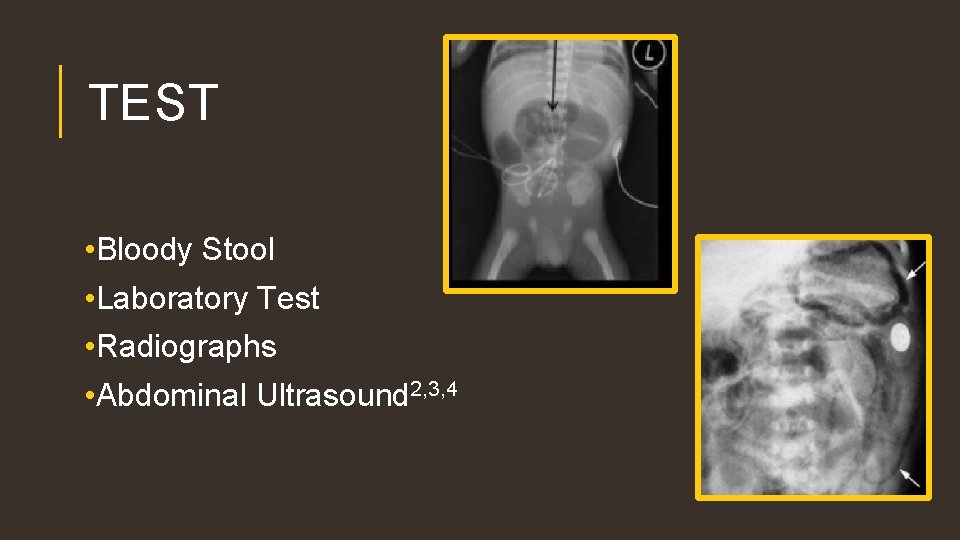
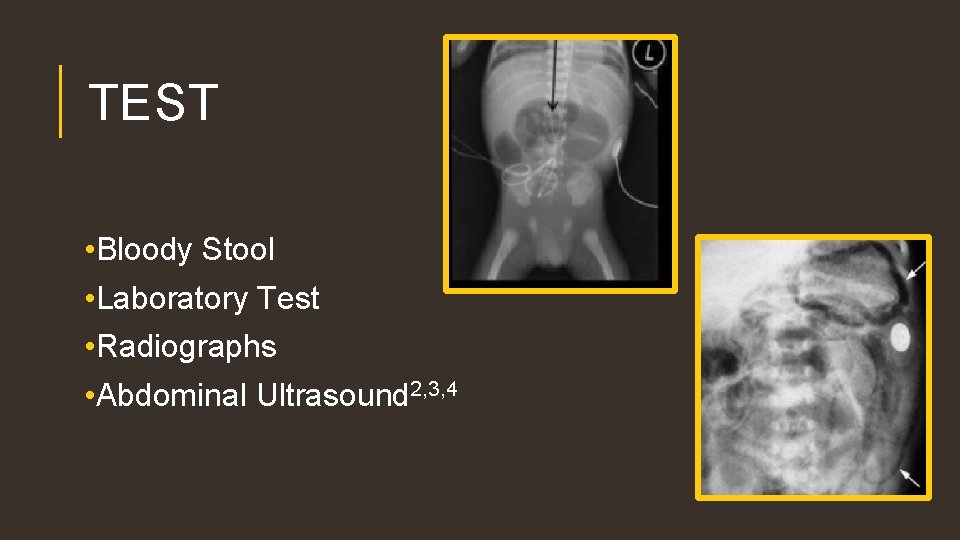
TEST • Bloody Stool • Laboratory Test • Radiographs • Abdominal Ultrasound 2, 3, 4
MEDICAL TREATMENT • All enteral feedings and medication discontinued • Decompression of the GI tract by lumen gastric tube • Monitoring of intravascular volume • Antibiotics • Surgery • Bowel perforation • Necrotic bowel • Clinical and laboratory condition worsen 3, 4, 6
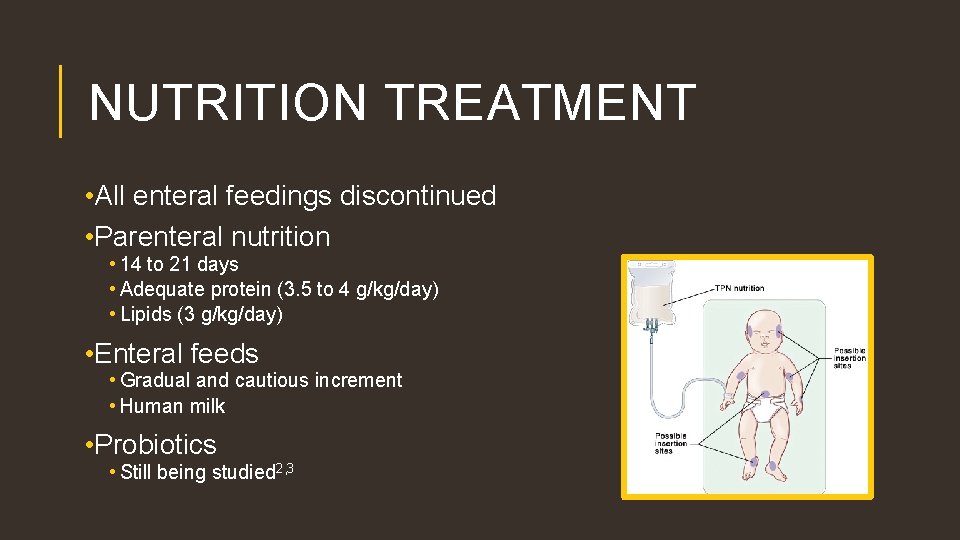
NUTRITION TREATMENT • All enteral feedings discontinued • Parenteral nutrition • 14 to 21 days • Adequate protein (3. 5 to 4 g/kg/day) • Lipids (3 g/kg/day) • Enteral feeds • Gradual and cautious increment • Human milk • Probiotics • Still being studied 2, 3
COMPLICATIONS • Intestinal strictures • Intra-abdominal abscess • Cholestasis • Short bowel syndrome • Higher cost and longer length of stay • Surgery • Increase of Comorbidities • Abnormal bowel function • Recurrences • Prolonged intravenous feeding • Death 3, 4, 6 • 5 to 6% of cases
PREVENTION Prevention of NEC is still being studied and there is no preventive or therapeutic approaches that have consistently shown to be effective • Human Milk • Amount/Advancement of Enteral Feedings • Probiotic Supplementation 2, 3, 6
PATIENT PROFILE & SOCIAL HISTORY • DA is a former 26 4/7 week male infant • Presented to the Hospital NICU on August 10, 2015 for prematurity, rule out sepsis, and respiratory distress syndrome (RDS) • 34 4/7 week PMA and day of life (DOL) 56 • PENUT study
MEDICAL PROBLEMS Current Medical Problems Resolved Medical Problems • Prematurity • Ruled out Sepsis • Mild Chronic Lung Disease • Hyponatremia • Apnea of Prematurity • Small Patent Ductus Arteriosus (PDA) • NEC • Anemia
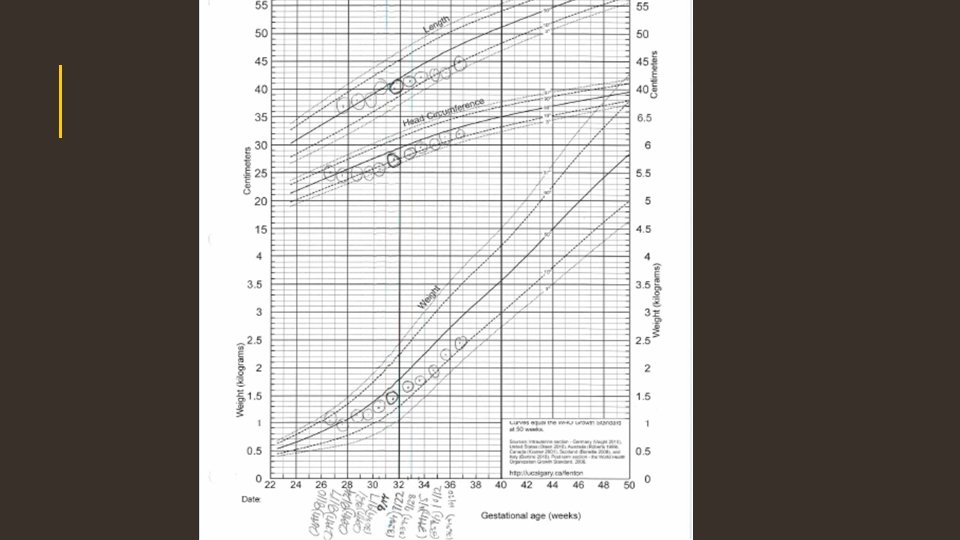
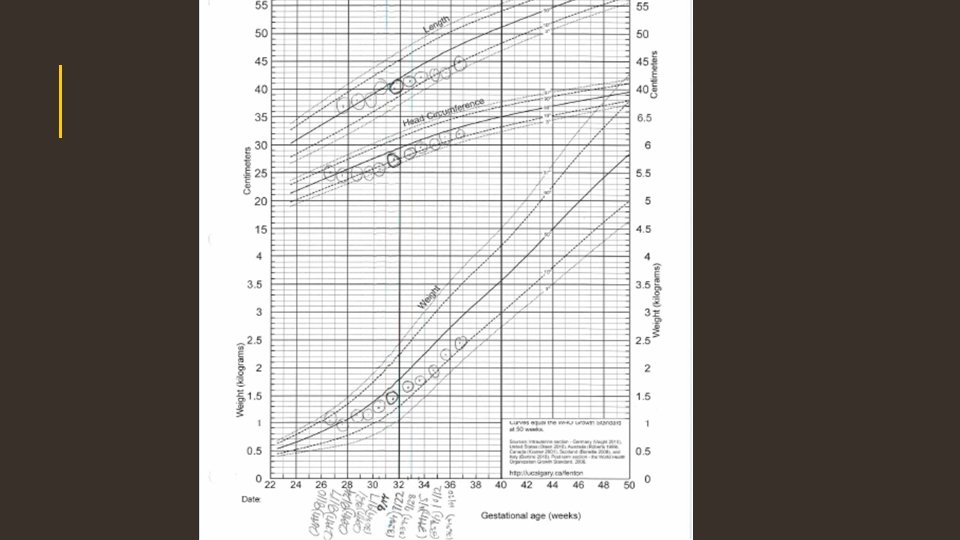
BIRTH ANTHROPOMETRICS • Birth Weight: • 1040 grams • 80 th percentile • Birth Length: • 37 centimeters (obtained on DOL 6) • 60 th percentile • Birth OFC: • 25 centimeters • 65 th percentile
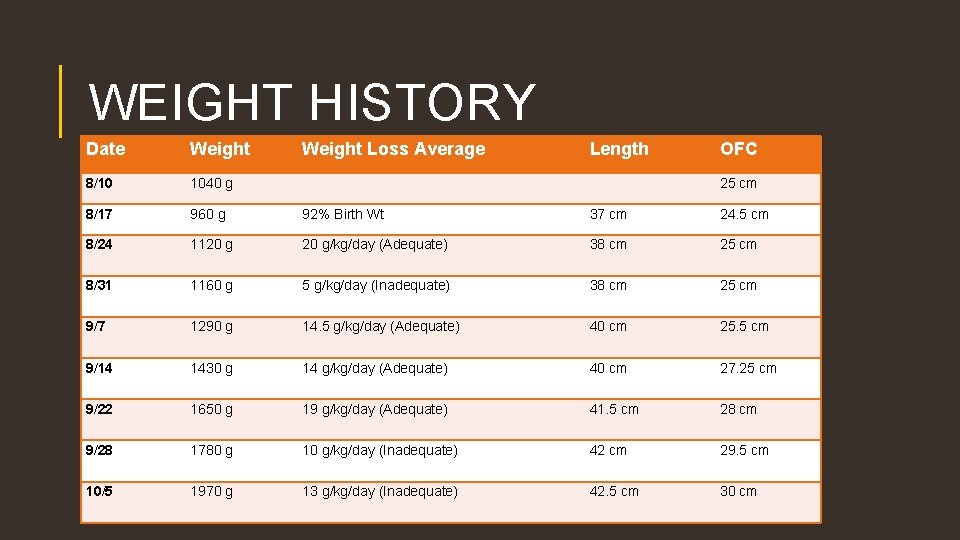
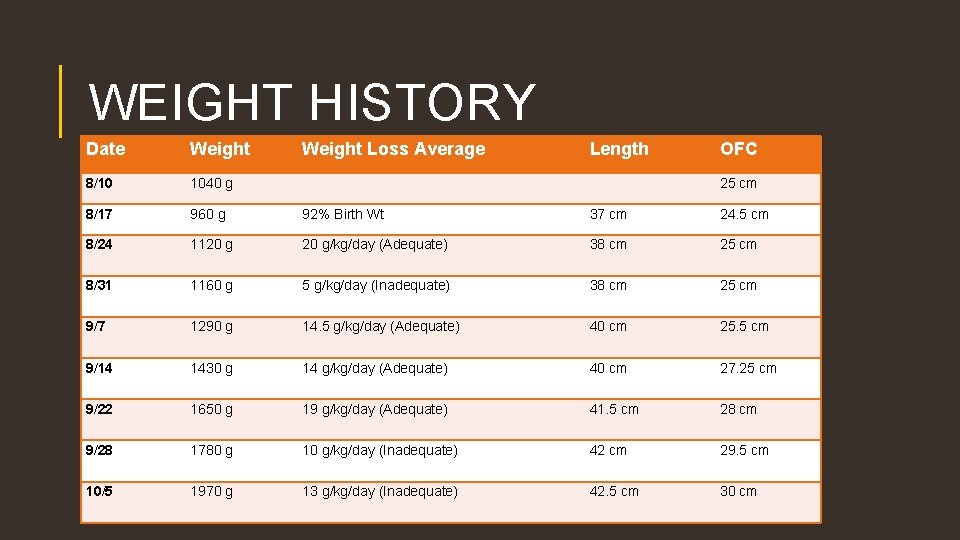
WEIGHT HISTORY Date Weight Loss Average Length OFC 8/10 1040 g 8/17 960 g 92% Birth Wt 37 cm 24. 5 cm 8/24 1120 g/kg/day (Adequate) 38 cm 25 cm 8/31 1160 g 5 g/kg/day (Inadequate) 38 cm 25 cm 9/7 1290 g 14. 5 g/kg/day (Adequate) 40 cm 25. 5 cm 9/14 1430 g 14 g/kg/day (Adequate) 40 cm 27. 25 cm 9/22 1650 g 19 g/kg/day (Adequate) 41. 5 cm 28 cm 9/28 1780 g 10 g/kg/day (Inadequate) 42 cm 29. 5 cm 10/5 1970 g 13 g/kg/day (Inadequate) 42. 5 cm 30 cm 25 cm
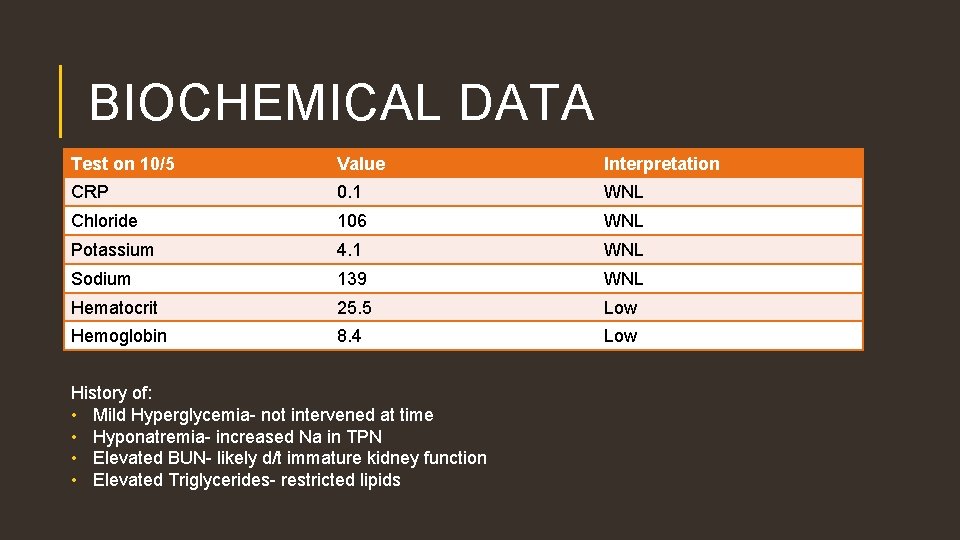
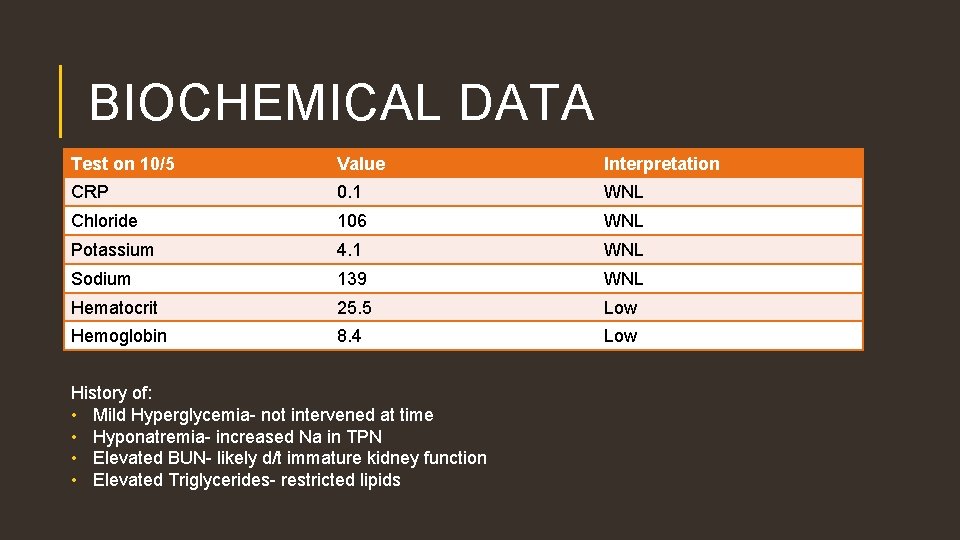
BIOCHEMICAL DATA Test on 10/5 Value Interpretation CRP 0. 1 WNL Chloride 106 WNL Potassium 4. 1 WNL Sodium 139 WNL Hematocrit 25. 5 Low Hemoglobin 8. 4 Low History of: • Mild Hyperglycemia- not intervened at time • Hyponatremia- increased Na in TPN • Elevated BUN- likely d/t immature kidney function • Elevated Triglycerides- restricted lipids

MEDICATION • Caffeine • Indocin Treatment • Zosyn • Poly-vi-sol + Iron • Zantac • Fer-in-sol • Started at birth • Discontinued on September 24 • Started October 5 • Last dose October 14 • In TPN • Ampicillin and Gentamicin • First 48 hours of life • Started on August 19 • Last dose on August 22 • 0. 5 ml daily • On hold • 6 mg/kg/day • On hold • IV Iron • 2 times per week
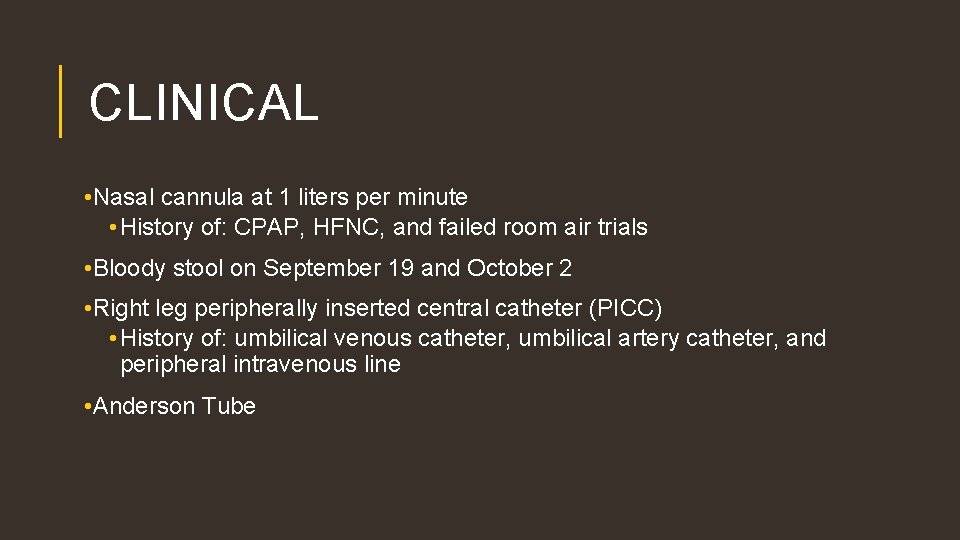
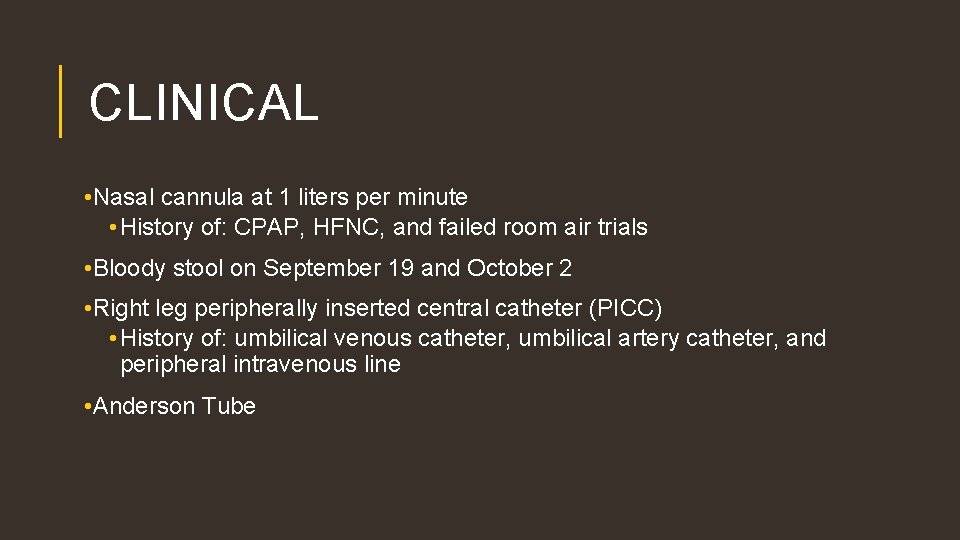
CLINICAL • Nasal cannula at 1 liters per minute • History of: CPAP, HFNC, and failed room air trials • Bloody stool on September 19 and October 2 • Right leg peripherally inserted central catheter (PICC) • History of: umbilical venous catheter, umbilical artery catheter, and peripheral intravenous line • Anderson Tube
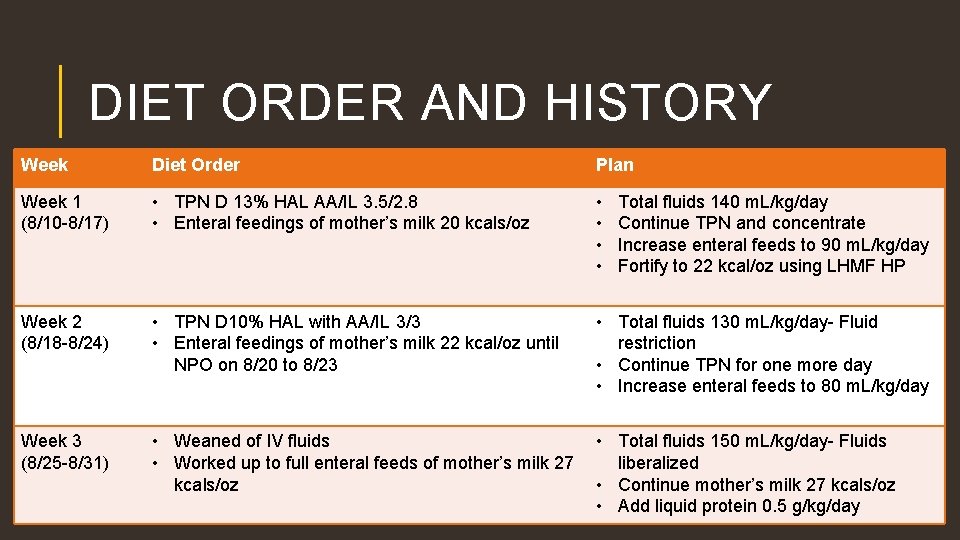
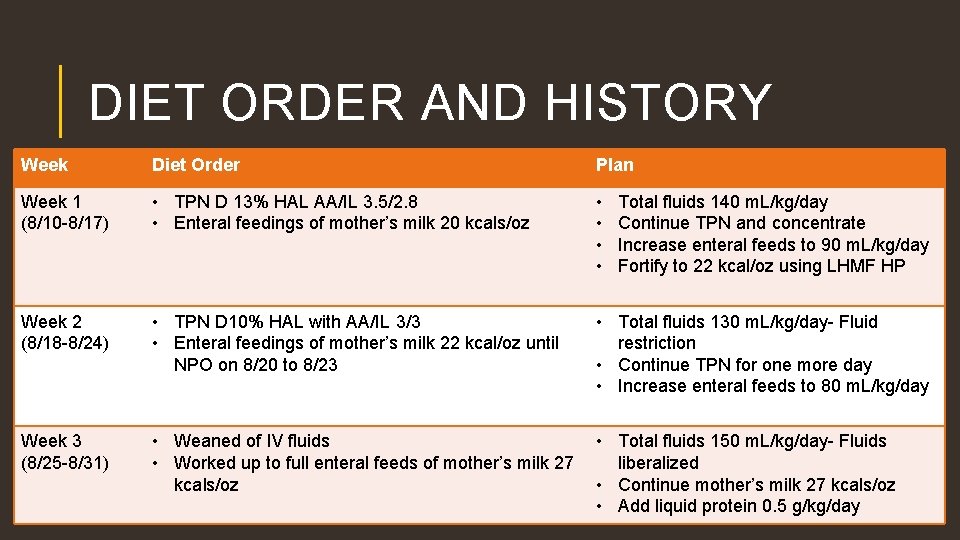
DIET ORDER AND HISTORY Week Diet Order Plan Week 1 (8/10 -8/17) • TPN D 13% HAL AA/IL 3. 5/2. 8 • Enteral feedings of mother’s milk 20 kcals/oz • • Week 2 (8/18 -8/24) • TPN D 10% HAL with AA/IL 3/3 • Enteral feedings of mother’s milk 22 kcal/oz until NPO on 8/20 to 8/23 • Total fluids 130 m. L/kg/day- Fluid restriction • Continue TPN for one more day • Increase enteral feeds to 80 m. L/kg/day Week 3 (8/25 -8/31) • Weaned of IV fluids • Worked up to full enteral feeds of mother’s milk 27 kcals/oz • Total fluids 150 m. L/kg/day- Fluids liberalized • Continue mother’s milk 27 kcals/oz • Add liquid protein 0. 5 g/kg/day Total fluids 140 m. L/kg/day Continue TPN and concentrate Increase enteral feeds to 90 m. L/kg/day Fortify to 22 kcal/oz using LHMF HP
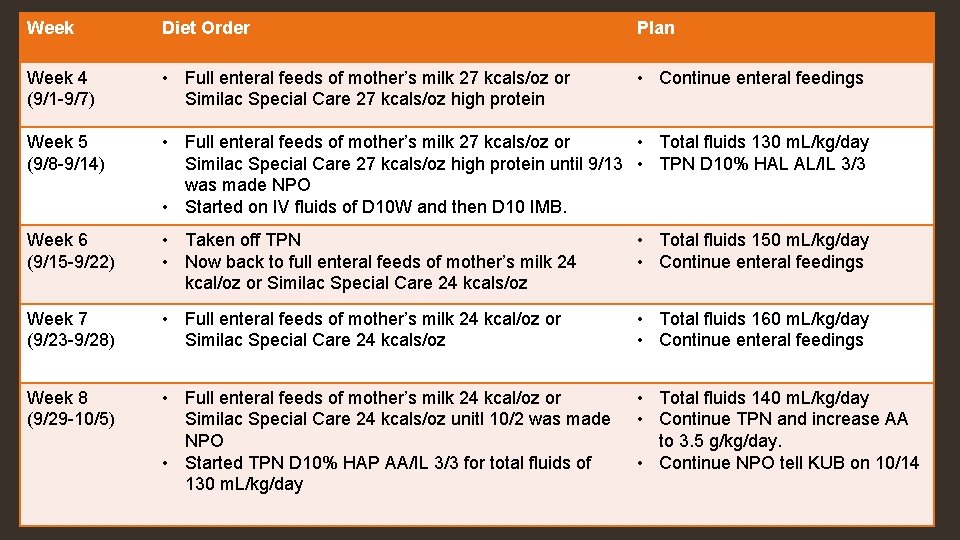
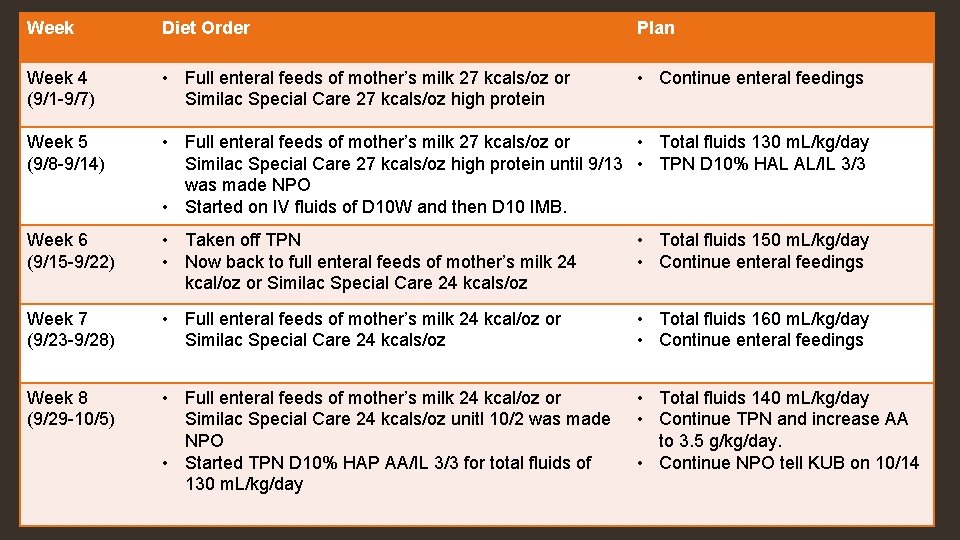
Week Diet Order Plan Week 4 (9/1 -9/7) • Full enteral feeds of mother’s milk 27 kcals/oz or Similac Special Care 27 kcals/oz high protein • Continue enteral feedings Week 5 (9/8 -9/14) • Full enteral feeds of mother’s milk 27 kcals/oz or • Total fluids 130 m. L/kg/day Similac Special Care 27 kcals/oz high protein until 9/13 • TPN D 10% HAL AL/IL 3/3 was made NPO • Started on IV fluids of D 10 W and then D 10 IMB. Week 6 (9/15 -9/22) • Taken off TPN • Now back to full enteral feeds of mother’s milk 24 kcal/oz or Similac Special Care 24 kcals/oz • Total fluids 150 m. L/kg/day • Continue enteral feedings Week 7 (9/23 -9/28) • Full enteral feeds of mother’s milk 24 kcal/oz or Similac Special Care 24 kcals/oz • Total fluids 160 m. L/kg/day • Continue enteral feedings Week 8 (9/29 -10/5) • Full enteral feeds of mother’s milk 24 kcal/oz or Similac Special Care 24 kcals/oz unitl 10/2 was made NPO • Started TPN D 10% HAP AA/IL 3/3 for total fluids of 130 m. L/kg/day • Total fluids 140 m. L/kg/day • Continue TPN and increase AA to 3. 5 g/kg/day. • Continue NPO tell KUB on 10/14
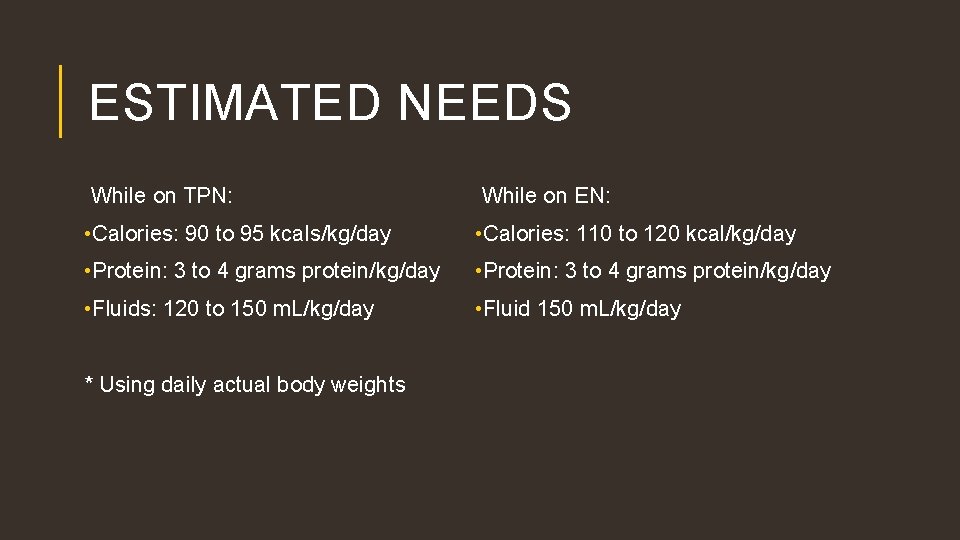
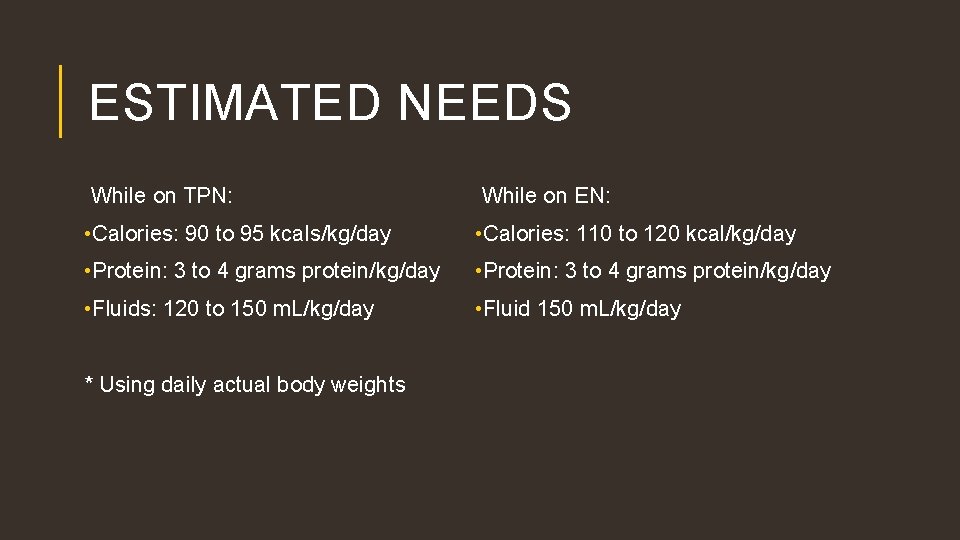
ESTIMATED NEEDS While on TPN: While on EN: • Calories: 90 to 95 kcals/kg/day • Calories: 110 to 120 kcal/kg/day • Protein: 3 to 4 grams protein/kg/day • Fluids: 120 to 150 m. L/kg/day • Fluid 150 m. L/kg/day * Using daily actual body weights
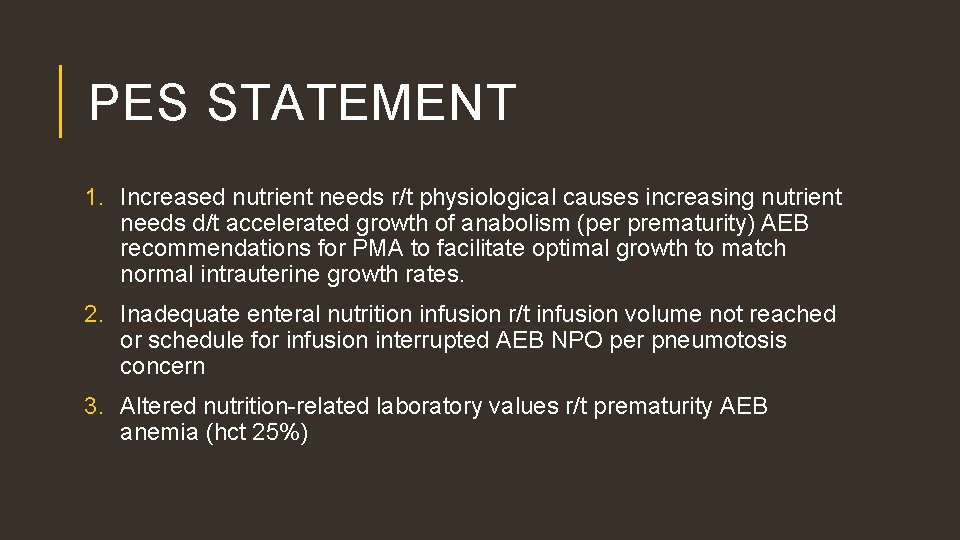
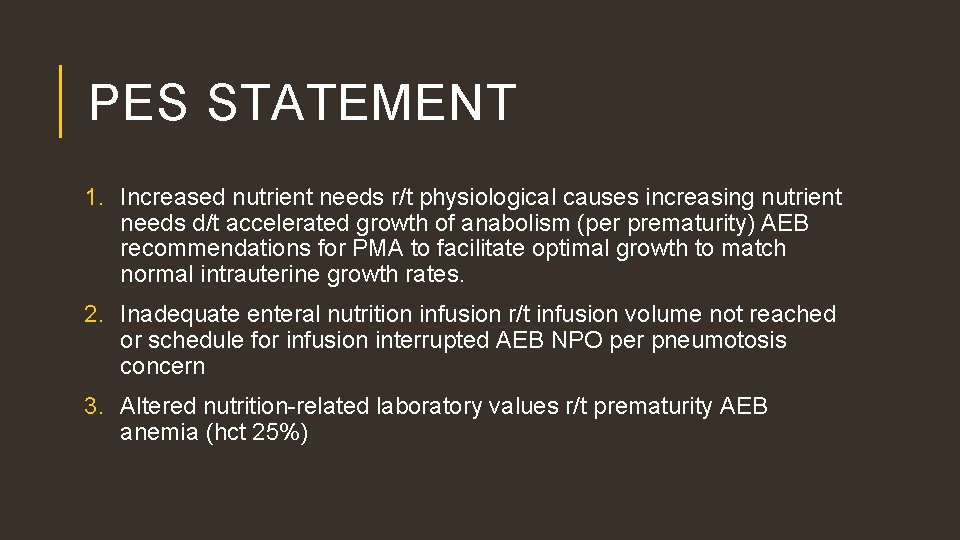
PES STATEMENT 1. Increased nutrient needs r/t physiological causes increasing nutrient needs d/t accelerated growth of anabolism (per prematurity) AEB recommendations for PMA to facilitate optimal growth to match normal intrauterine growth rates. 2. Inadequate enteral nutrition infusion r/t infusion volume not reached or schedule for infusion interrupted AEB NPO per pneumotosis concern 3. Altered nutrition-related laboratory values r/t prematurity AEB anemia (hct 25%)
INTERVENTION • IV rate 11. 5 m. L/hr to provide 140 m. L/kg/day. TPN D 11% 3. 5/3 to provide: 140 m. L/kg/day, 90 kcals/kg/day, and 3. 5 grams protein/kg/day. • Goals 1. Meet 100% of estimated nutritional needs via TPN 2. Re-establish enteral feedings 3. Promote optimal average weight gain of 15 to 20 g/kg/day 4. Promote optimal linear (1 cm/week) and head growth (0. 7 cm/week) 5. Nutrition related labs WNL
MONITORING AND EVALUATION • Weight, Length, and OFC Growth • Tolerance to TPN • Nutrition Related Lab Values • PENUT Study • Reticulocyte Hemoglobin • Zinc Protoporphryin • Ferritin
CONCLUSION • As of October 13 Anderson tube was pulled and was still being treated with Zosyn. Last dose of Zosyn was given on October 14 and then DA was going to have another KUB. Until results of KUB came back he was to stay on TPN for nutrition support. If KUB results allowed, enteral feeds could be attempted. • As of October 20 D 10 SPN was stopped and was tolerating re-advanced feedings. Was receiving mother’s milk 22 fortified with HMF or Neosure 22. DA feeds were changed to request feeds with a minimum of 120 m. L/kg/day. He was placed on a fluid restriction of 130 m. L/kg/day due to edema in the his legs. Restarted on Poly-vi-sol and ferrous sulfate to meet recommended nutritional needs for vitamin D and iron. Plan was to be discharged within the next week.
RESOURCES 1. Nelms M, Sucher KP, Lacey K, Roth SL. Nutrition Therapy & Pathophysiology Second Edition. Belmont, CA: Brooks/Cole Cengage Learning; 2011, 2007. 2. Porter RS, Kaplan JL. The Merck Manual Nineteenth Edition. Whitehouse Station, NJ: Merck Sharp & Dohme Corp; 2011. 3. Koletzko B, Poindexter B, Uauy R. Nutritional Care of Preterm Infants Volume 110. Basel, Switzerland: S. Karger AG; 2014 4. Sharma R, Hudak ML. A Clinical Perspective of Necrotizing Enterocolitis: Past, Present, and Future. Clin Perinatol. 2013; 40(1): 27 -51. doi: 10. 1016/j. clp. 2012. 5. Claud EC, Walker WA. Hypothesis: inappropriate colonization of the premature intestine can cause neonatal necrotizing enterocolitis. FASEB J. 2001; 15(8): 1398 -1403. doi: 10. 1096/fj. 000833 hyp. 6. Caplan MS. Probiotic and prebiotic supplementation for the prevention of neonatal necrotizing enterocolitis. J Perinatol. 2009; 29: S 2 -S 6. dio: 10. 1038/jp. 2009. 21.