TransfusionRelated Necrotizing Enterocolitis A Retrospective Review Diane Farley
- Slides: 1
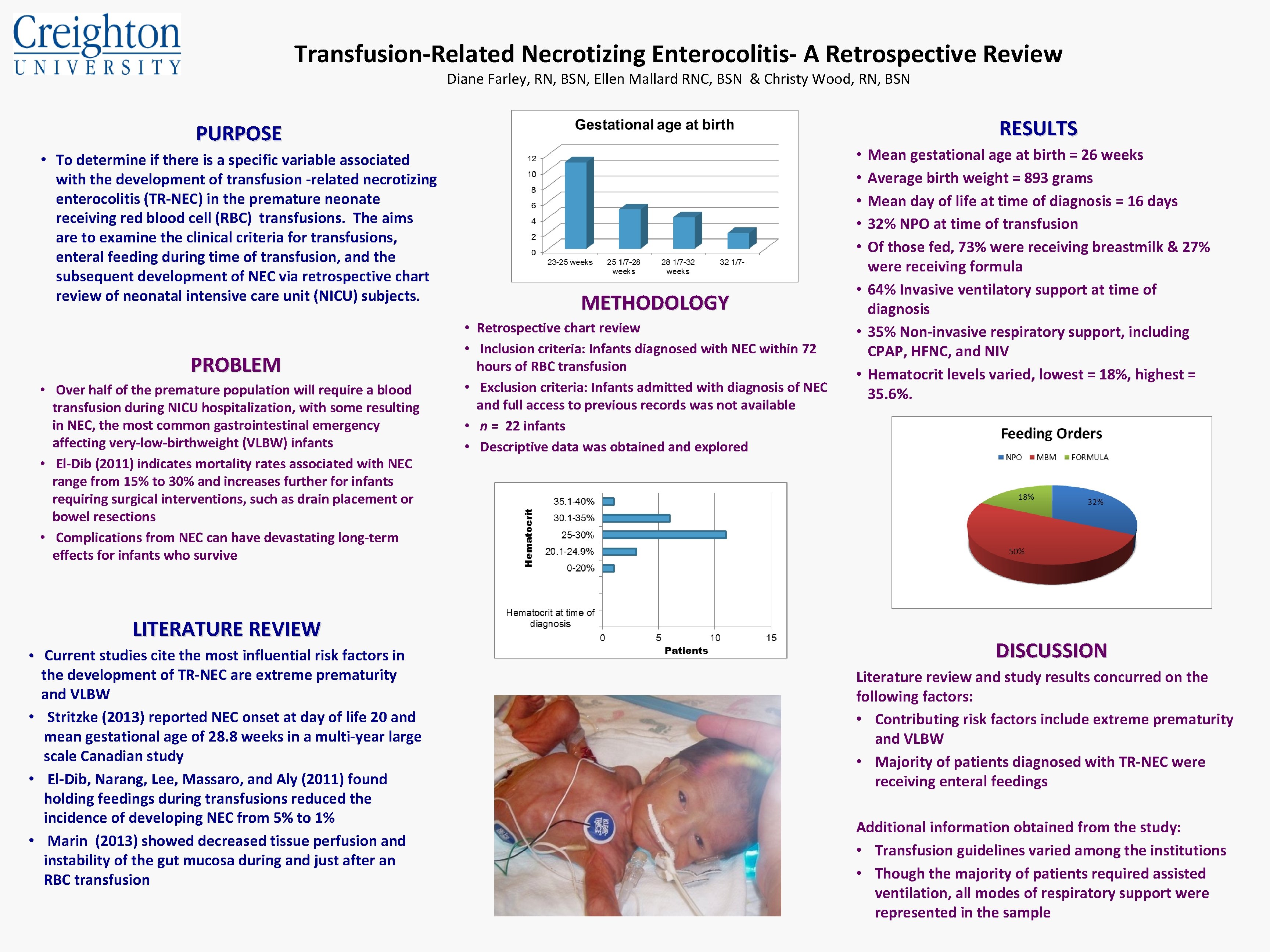
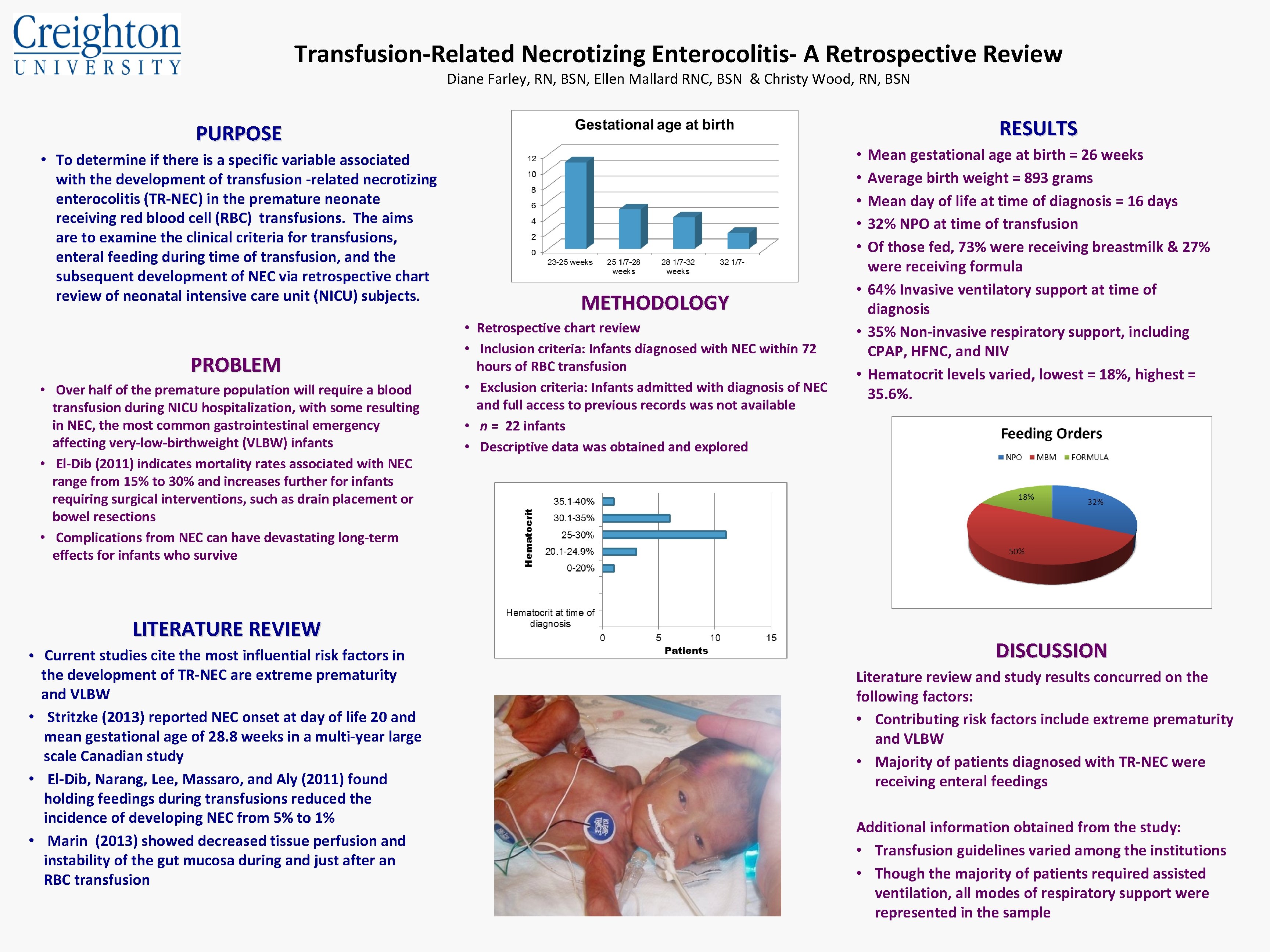
Transfusion-Related Necrotizing Enterocolitis- A Retrospective Review Diane Farley, RN, BSN, Ellen Mallard RNC, BSN & Christy Wood, RN, BSN RESULTS PURPOSE • To determine if there is a specific variable associated with the development of transfusion -related necrotizing enterocolitis (TR-NEC) in the premature neonate receiving red blood cell (RBC) transfusions. The aims are to examine the clinical criteria for transfusions, enteral feeding during time of transfusion, and the subsequent development of NEC via retrospective chart review of neonatal intensive care unit (NICU) subjects. PROBLEM • Over half of the premature population will require a blood transfusion during NICU hospitalization, with some resulting in NEC, the most common gastrointestinal emergency affecting very-low-birthweight (VLBW) infants • El-Dib (2011) indicates mortality rates associated with NEC range from 15% to 30% and increases further for infants requiring surgical interventions, such as drain placement or bowel resections • Complications from NEC can have devastating long-term effects for infants who survive LITERATURE REVIEW • Current studies cite the most influential risk factors in the development of TR-NEC are extreme prematurity and VLBW • Stritzke (2013) reported NEC onset at day of life 20 and mean gestational age of 28. 8 weeks in a multi-year large scale Canadian study • El-Dib, Narang, Lee, Massaro, and Aly (2011) found holding feedings during transfusions reduced the incidence of developing NEC from 5% to 1% • Marin (2013) showed decreased tissue perfusion and instability of the gut mucosa during and just after an RBC transfusion Mean gestational age at birth = 26 weeks Average birth weight = 893 grams Mean day of life at time of diagnosis = 16 days 32% NPO at time of transfusion Of those fed, 73% were receiving breastmilk & 27% were receiving formula • 64% Invasive ventilatory support at time of diagnosis • 35% Non-invasive respiratory support, including CPAP, HFNC, and NIV • Hematocrit levels varied, lowest = 18%, highest = 35. 6%. • • • METHODOLOGY • Retrospective chart review • Inclusion criteria: Infants diagnosed with NEC within 72 hours of RBC transfusion • Exclusion criteria: Infants admitted with diagnosis of NEC and full access to previous records was not available • n = 22 infants • Descriptive data was obtained and explored DISCUSSION Literature review and study results concurred on the following factors: • Contributing risk factors include extreme prematurity and VLBW • Majority of patients diagnosed with TR-NEC were receiving enteral feedings Additional information obtained from the study: • Transfusion guidelines varied among the institutions • Though the majority of patients required assisted ventilation, all modes of respiratory support were represented in the sample