Medidas de seguimiento para los nuevos genes de
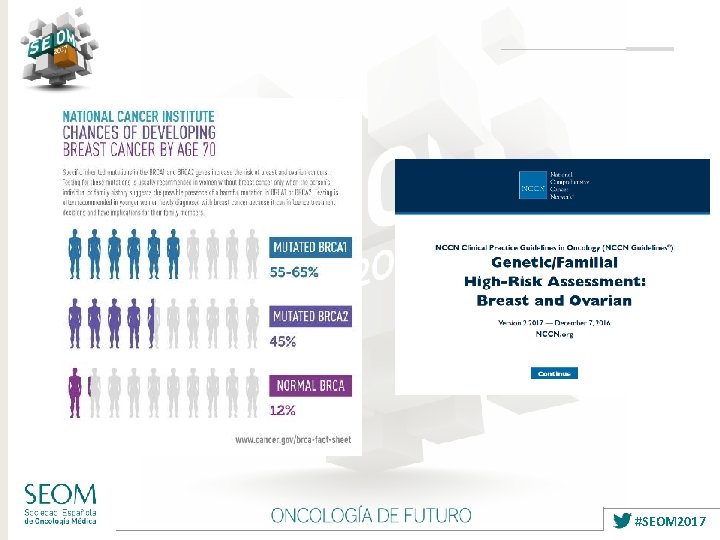


- Slides: 48
Medidas de seguimiento para los nuevos genes de predisposición hereditaria a cáncer LUIS ROBLES DÍAZ UNIDAD DE CÁNCER FAMILIAR SERVICIO DE ONCOLOGÍA MÉDICA #SEOM 2017
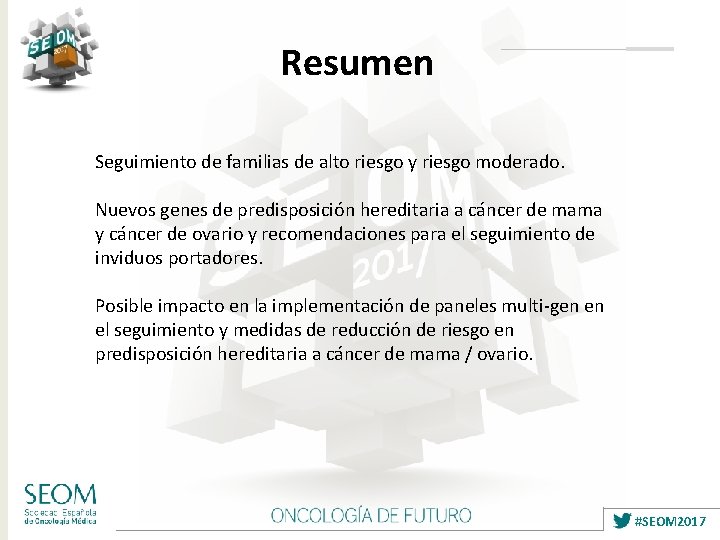
Resumen Seguimiento de familias de alto riesgo y riesgo moderado. Nuevos genes de predisposición hereditaria a cáncer de mama y cáncer de ovario y recomendaciones para el seguimiento de inviduos portadores. Posible impacto en la implementación de paneles multi-gen en el seguimiento y medidas de reducción de riesgo en predisposición hereditaria a cáncer de mama / ovario. #SEOM 2017
#SEOM 2017
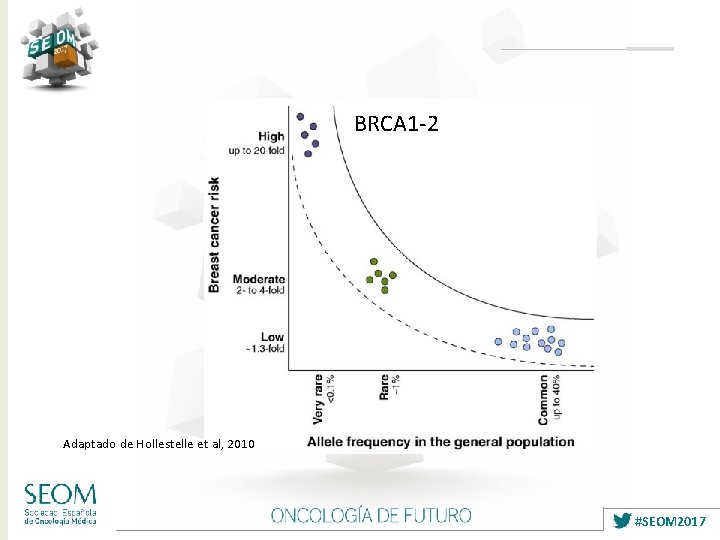
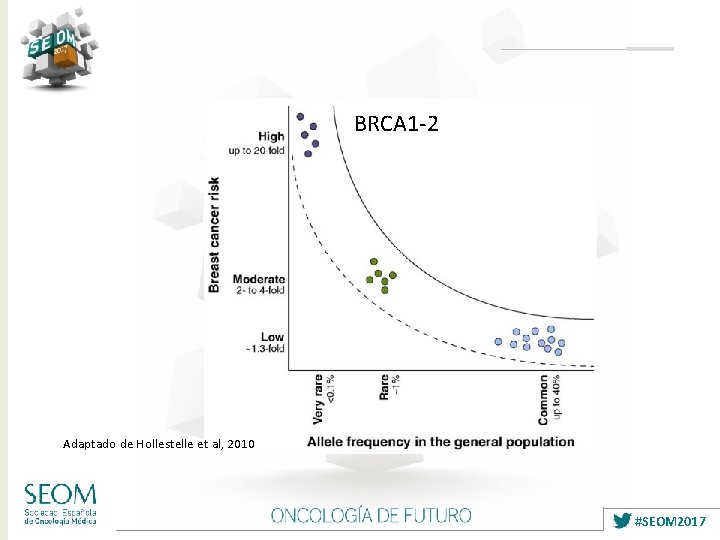
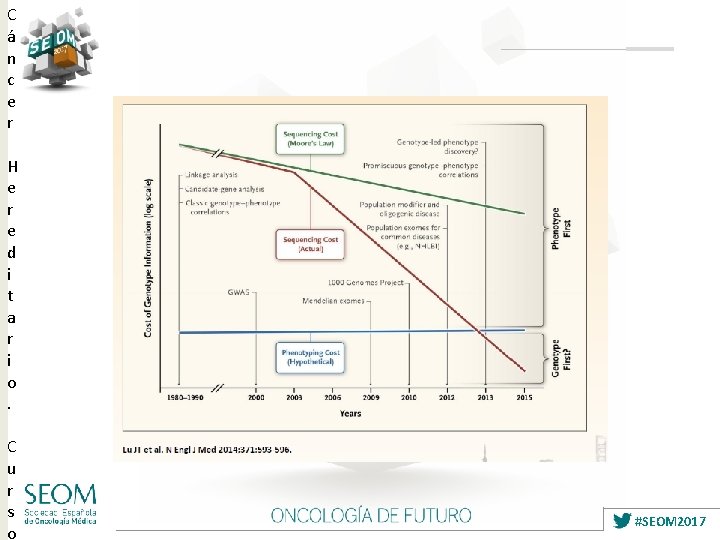
BRCA 1 -2 Adaptado de Hollestelle et al, 2010 #SEOM 2017

#SEOM 2017
C á n c e r H e r e d i t a r i o. C u r s o #SEOM 2017
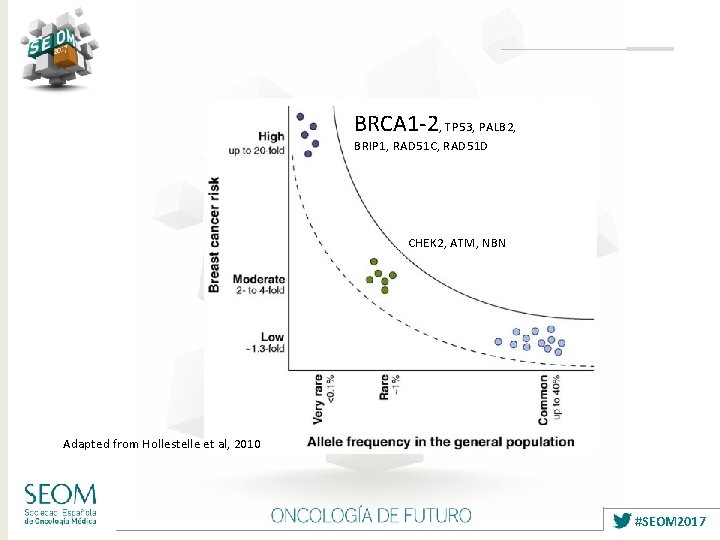
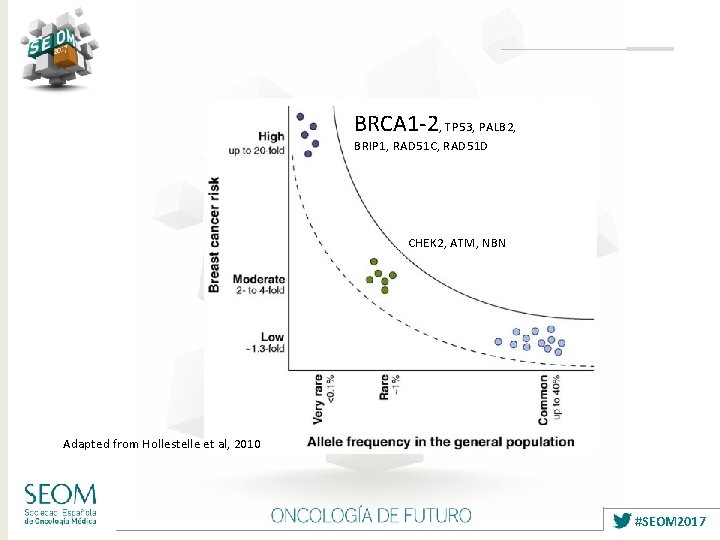
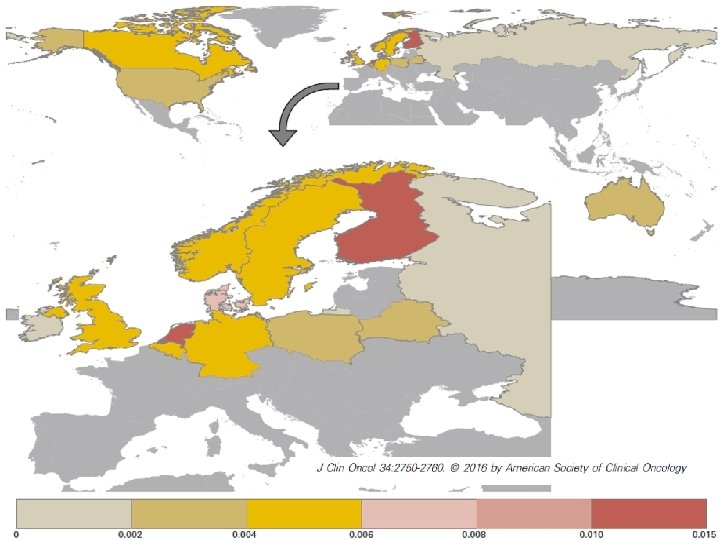
BRCA 1 -2, TP 53, PALB 2, BRIP 1, RAD 51 C, RAD 51 D CHEK 2, ATM, NBN Adapted from Hollestelle et al, 2010 #SEOM 2017
#SEOM 2017
#SEOM 2017

#SEOM 2017
Resumen Seguimiento de familias de alto riesgo y riesgo moderado. Nuevos genes de predisposición hereditaria a cáncer de mama y cáncer de ovario y recomendaciones para el seguimiento de inviduos portadores. Posible impacto en la implementación de paneles multi-gen en el seguimiento y medidas de reducción de riesgo en predisposición hereditaria a cáncer de mama / ovario. #SEOM 2017
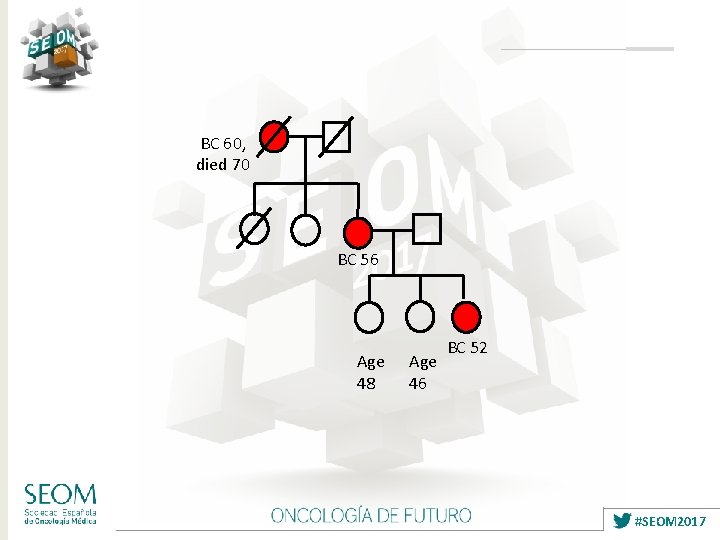
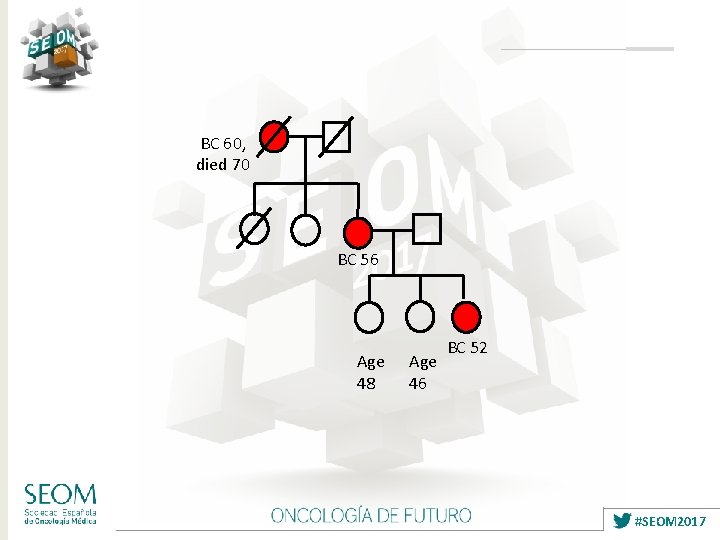
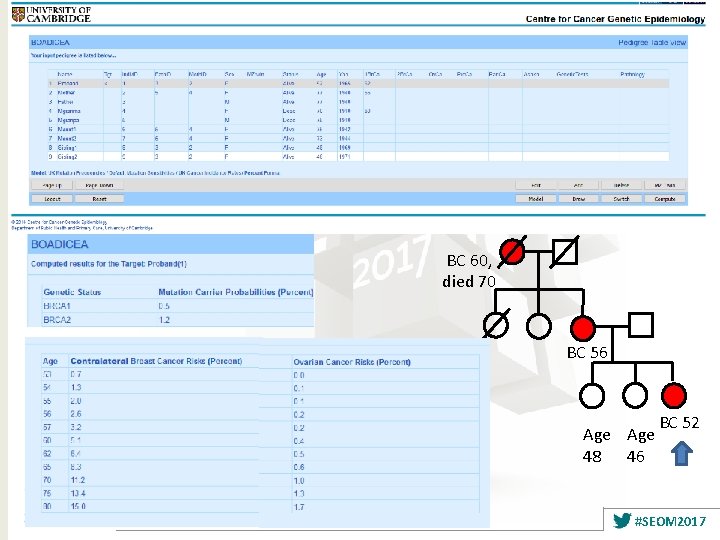
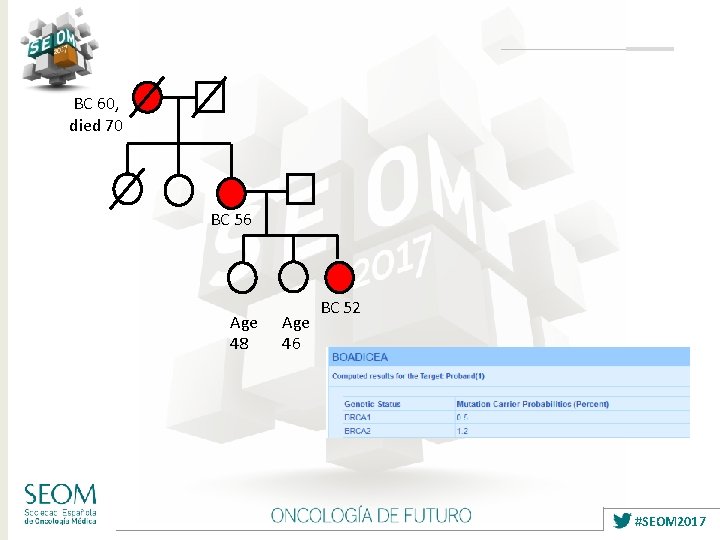
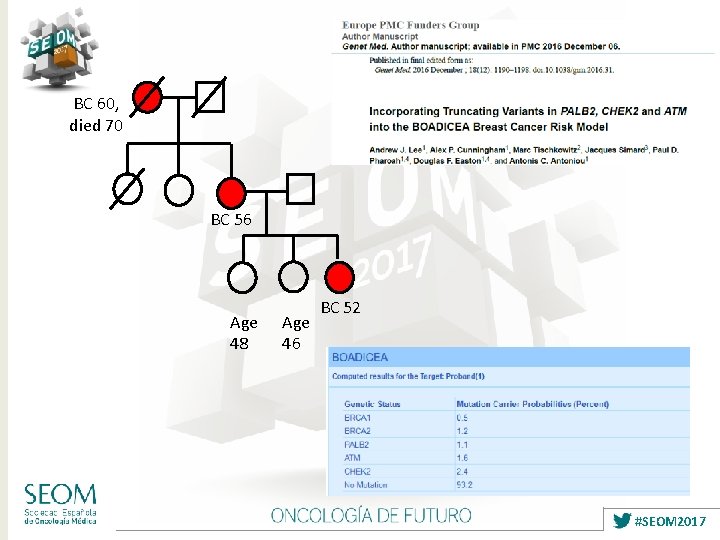
BC 60, died 70 BC 56 Age 48 Age 46 BC 52 #SEOM 2017
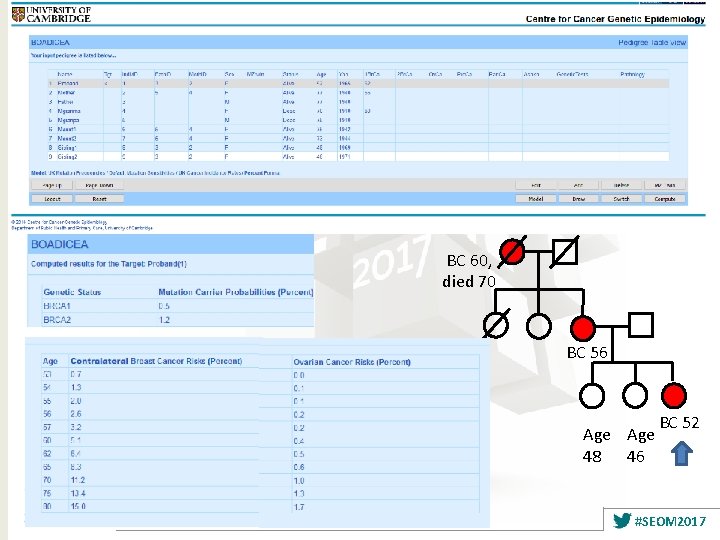
BC 60, died 70 BC 56 BC 52 Age 48 46 #SEOM 2017
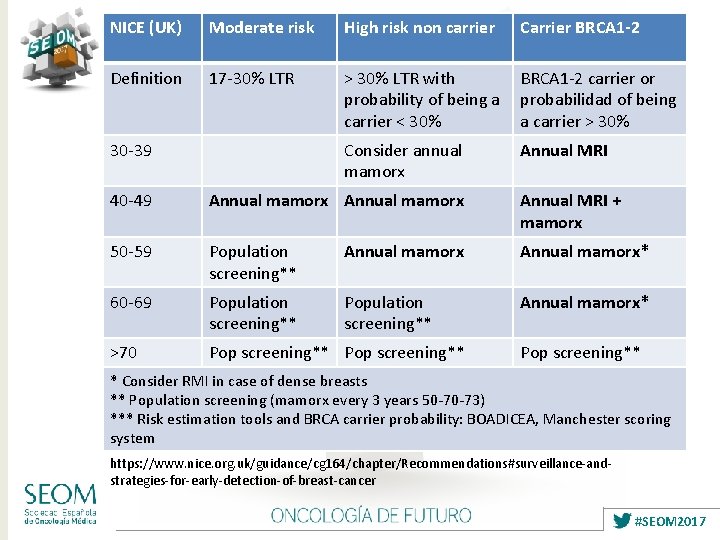
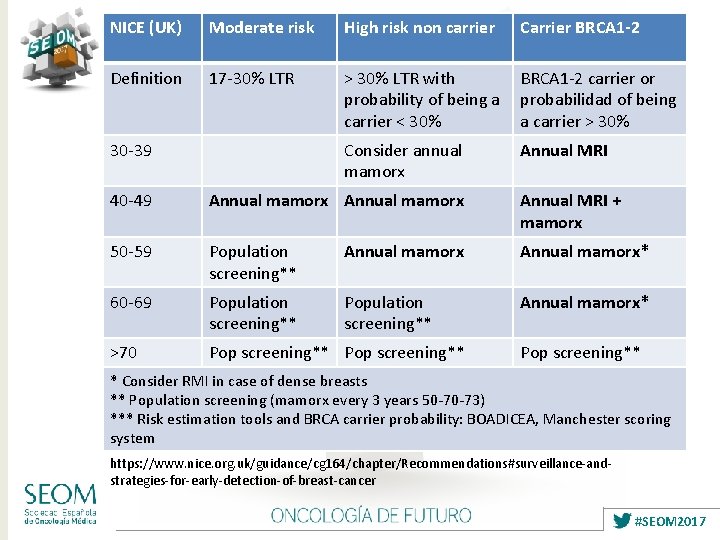
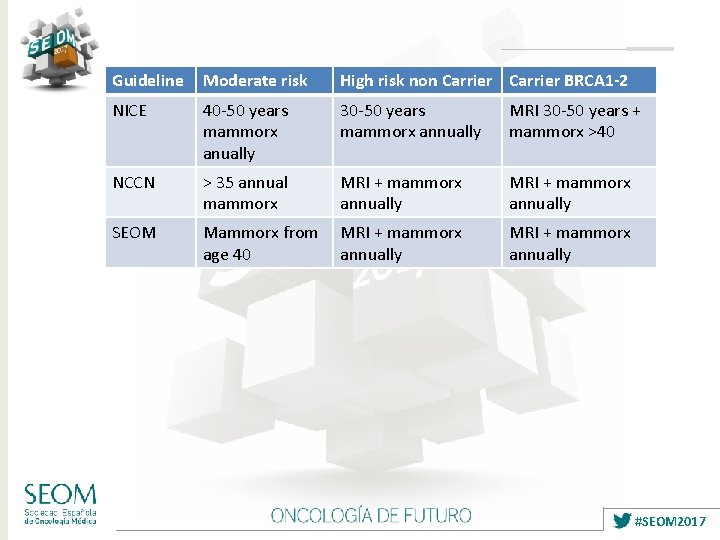
NICE (UK) Moderate risk High risk non carrier Carrier BRCA 1 -2 Definition 17 -30% LTR > 30% LTR with BRCA 1 -2 carrier or probability of being a probabilidad of being carrier < 30% a carrier > 30% 30 -39 Consider annual mamorx Annual MRI 40 -49 Annual mamorx Annual MRI + mamorx 50 -59 Population screening** Annual mamorx* 60 -69 Population screening** Annual mamorx* >70 Pop screening** * Consider RMI in case of dense breasts ** Population screening (mamorx every 3 years 50 -70 -73) *** Risk estimation tools and BRCA carrier probability: BOADICEA, Manchester scoring system https: //www. nice. org. uk/guidance/cg 164/chapter/Recommendations#surveillance-andstrategies-for-early-detection-of-breast-cancer #SEOM 2017
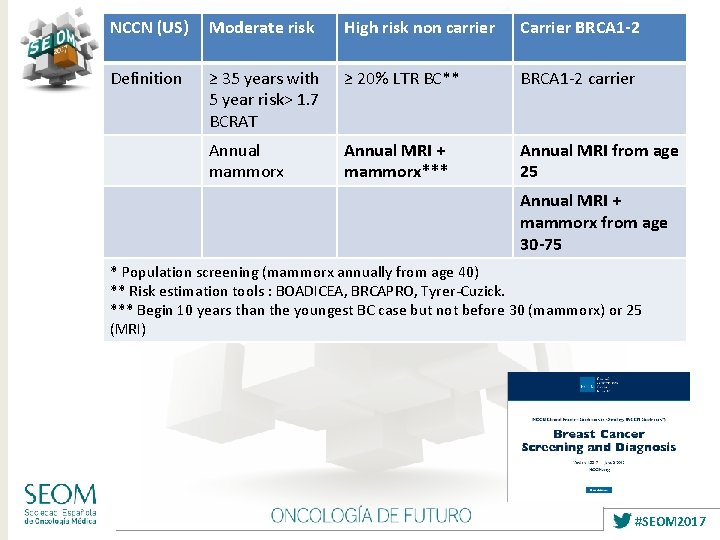
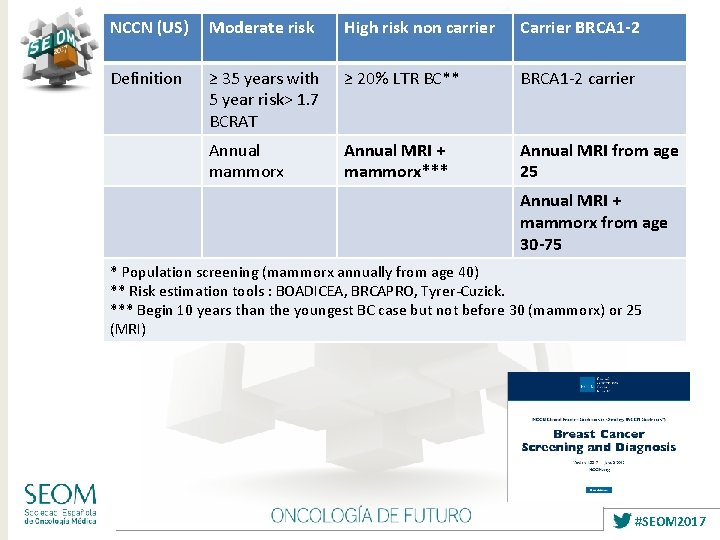
NCCN (US) Moderate risk High risk non carrier Carrier BRCA 1 -2 Definition ≥ 35 years with 5 year risk> 1. 7 BCRAT ≥ 20% LTR BC** BRCA 1 -2 carrier Annual mammorx Annual MRI + mammorx*** Annual MRI from age 25 Annual MRI + mammorx from age 30 -75 * Population screening (mammorx annually from age 40) ** Risk estimation tools : BOADICEA, BRCAPRO, Tyrer-Cuzick. *** Begin 10 years than the youngest BC case but not before 30 (mammorx) or 25 (MRI) #SEOM 2017
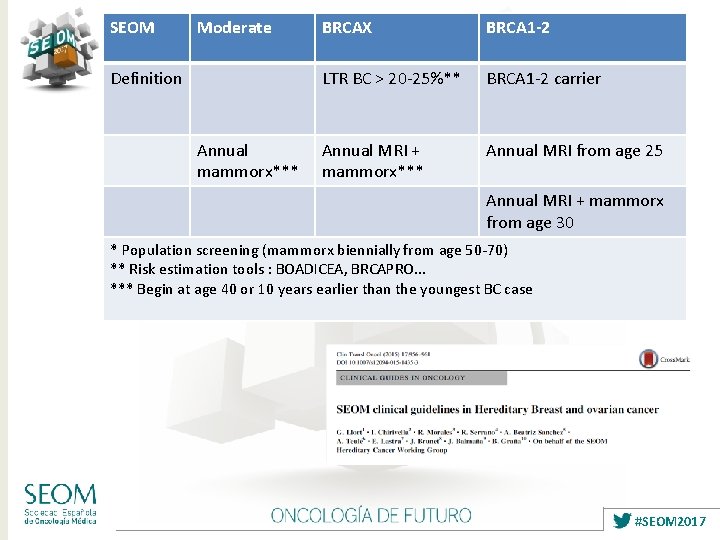
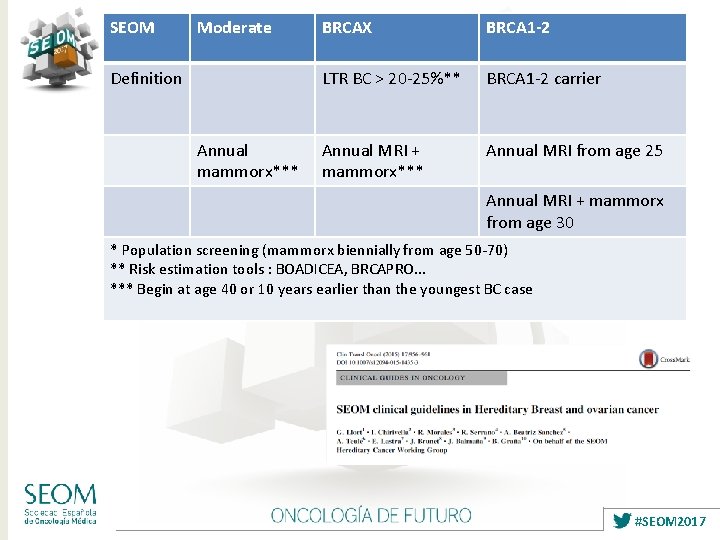
SEOM Moderate Definition Annual mammorx*** BRCAX BRCA 1 -2 LTR BC > 20 -25%** BRCA 1 -2 carrier Annual MRI + mammorx*** Annual MRI from age 25 Annual MRI + mammorx from age 30 * Population screening (mammorx biennially from age 50 -70) ** Risk estimation tools : BOADICEA, BRCAPRO. . . *** Begin at age 40 or 10 years earlier than the youngest BC case #SEOM 2017
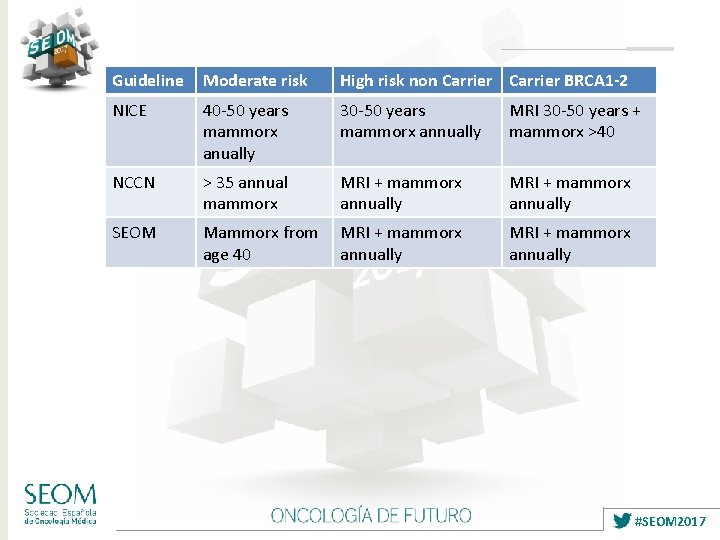
Guideline Moderate risk High risk non Carrier BRCA 1 -2 NICE 40 -50 years mammorx anually 30 -50 years mammorx annually MRI 30 -50 years + mammorx >40 NCCN > 35 annual mammorx MRI + mammorx annually SEOM Mammorx from MRI + mammorx age 40 annually MRI + mammorx annually #SEOM 2017
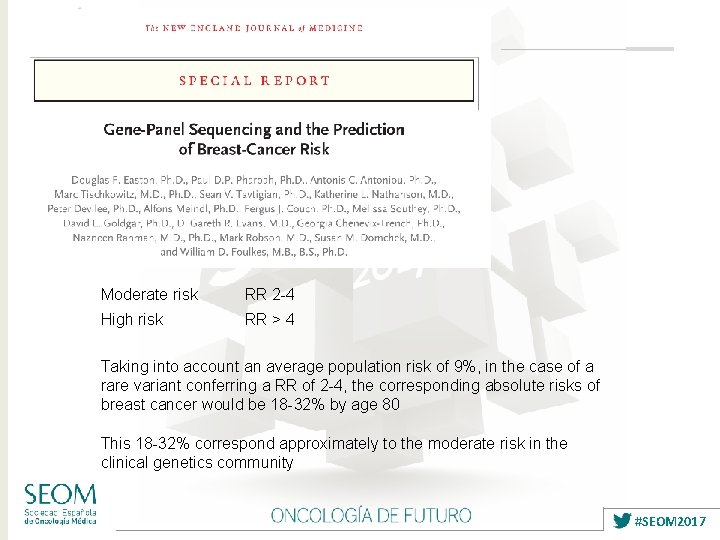
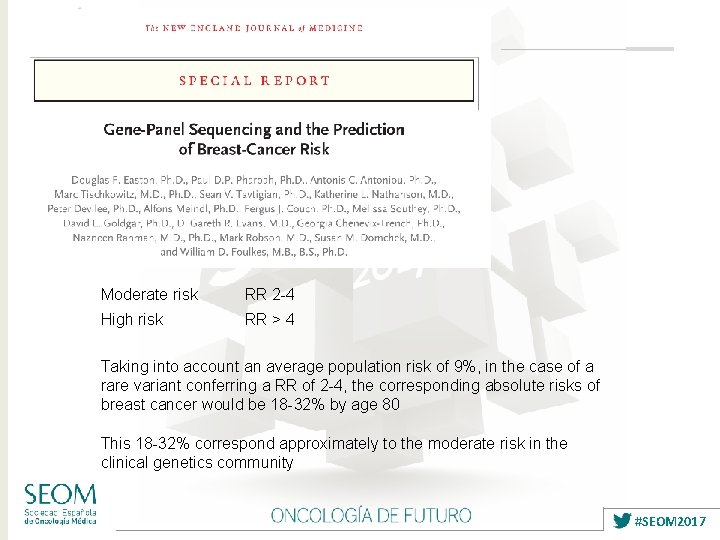
Moderate risk RR 2 -4 High risk RR > 4 Taking into account an average population risk of 9%, in the case of a rare variant conferring a RR of 2 -4, the corresponding absolute risks of breast cancer would be 18 -32% by age 80 This 18 -32% correspond approximately to the moderate risk in the clinical genetics community #SEOM 2017
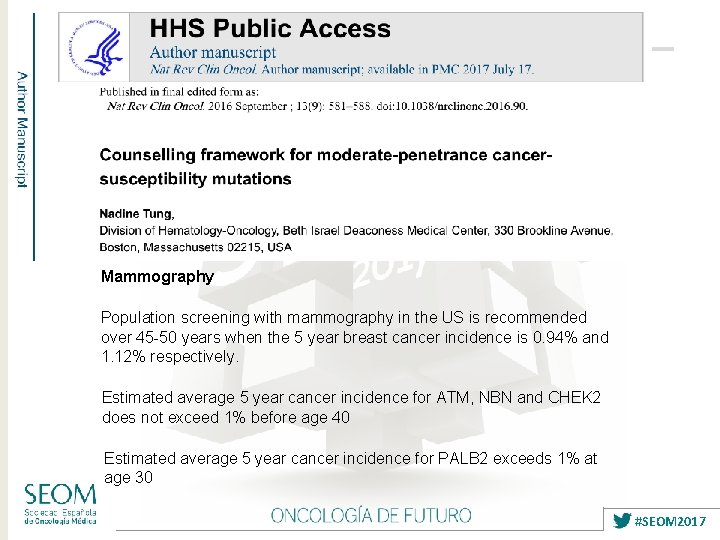
Mammography Population screening with mammography in the US is recommended over 45 -50 years when the 5 year breast cancer incidence is 0. 94% and 1. 12% respectively. Estimated average 5 year cancer incidence for ATM, NBN and CHEK 2 does not exceed 1% before age 40 Estimated average 5 year cancer incidence for PALB 2 exceeds 1% at age 30 #SEOM 2017
Resumen Seguimiento de familias de alto riesgo y riesgo moderado. Nuevos genes de predisposición hereditaria a cáncer de mama y cáncer de ovario y recomendaciones para el seguimiento de inviduos portadores. Posible impacto en la implementación de paneles multi-gen en el seguimiento y medidas de reducción de riesgo en predisposición hereditaria a cáncer de mama / ovario. #SEOM 2017
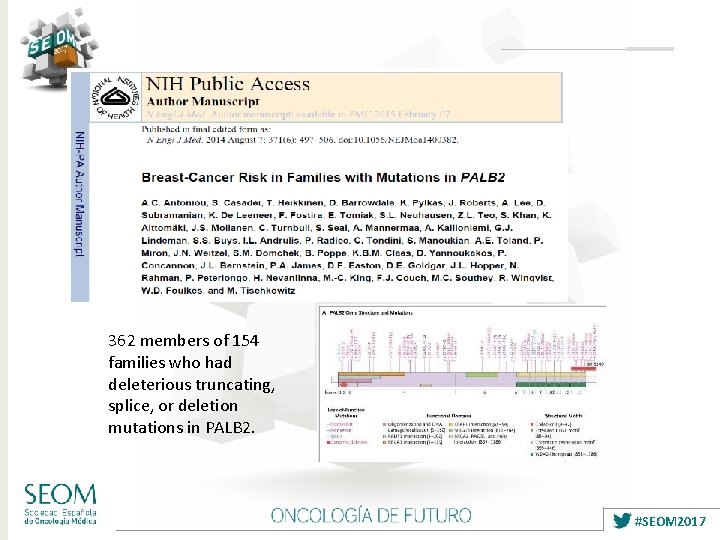
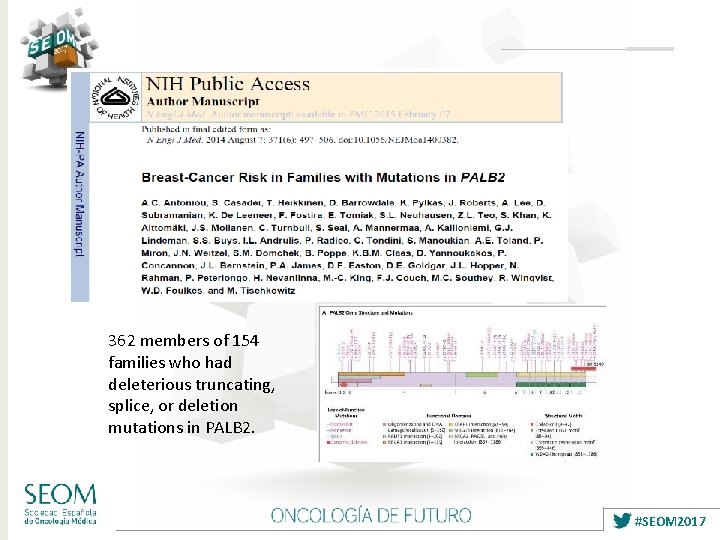
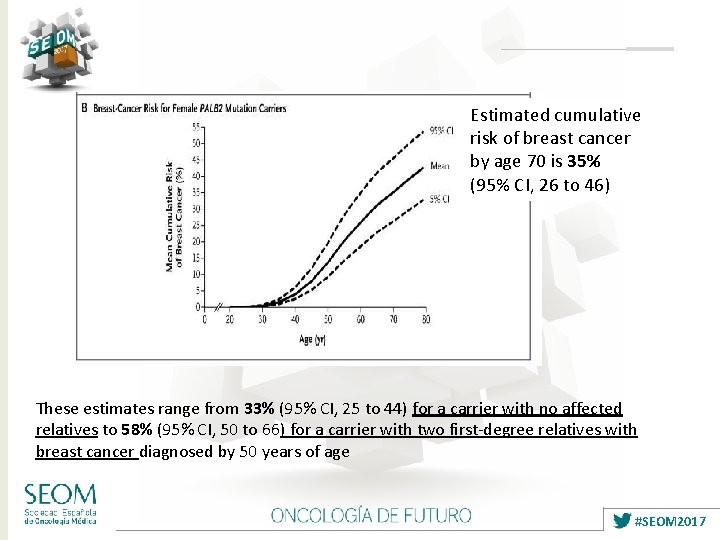
362 members of 154 families who had deleterious truncating, splice, or deletion mutations in PALB 2. #SEOM 2017
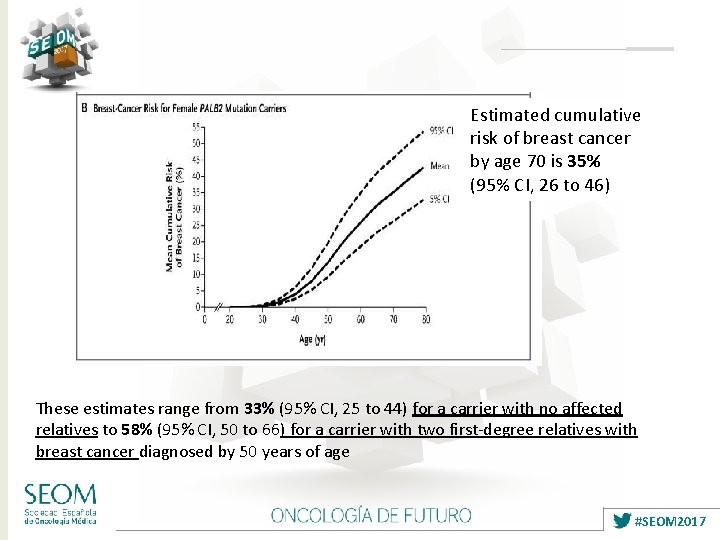
Estimated cumulative risk of breast cancer by age 70 is 35% (95% CI, 26 to 46) These estimates range from 33% (95% CI, 25 to 44) for a carrier with no affected relatives to 58% (95% CI, 50 to 66) for a carrier with two first-degree relatives with breast cancer diagnosed by 50 years of age #SEOM 2017
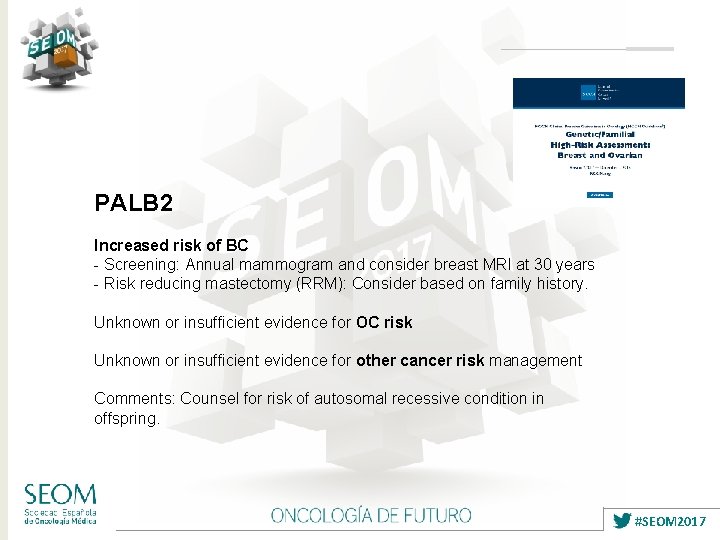
PALB 2 Increased risk of BC - Screening: Annual mammogram and consider breast MRI at 30 years - Risk reducing mastectomy (RRM): Consider based on family history. Unknown or insufficient evidence for OC risk Unknown or insufficient evidence for other cancer risk management Comments: Counsel for risk of autosomal recessive condition in offspring. #SEOM 2017
#SEOM 2017
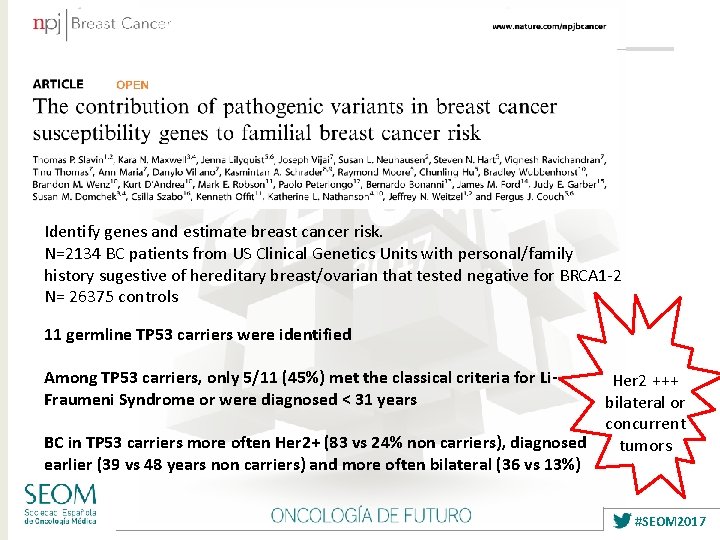
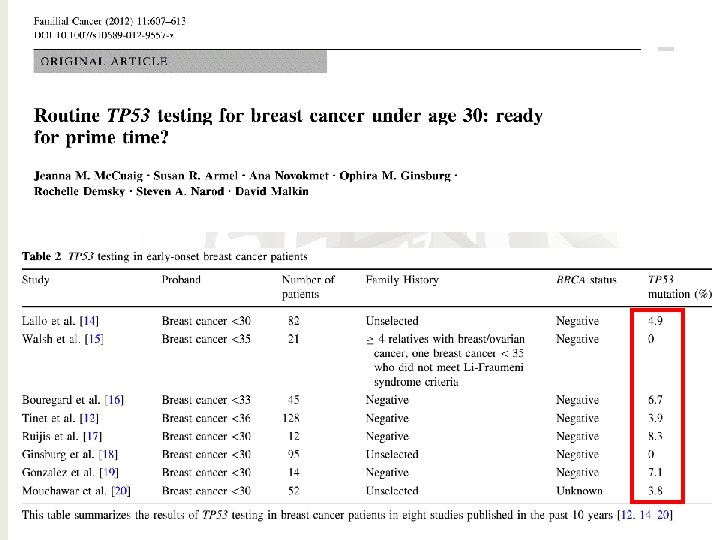
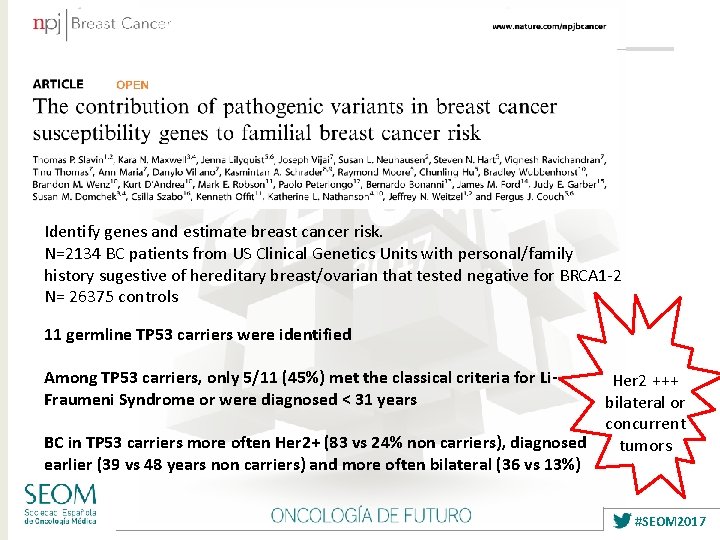
Identify genes and estimate breast cancer risk. N=2134 BC patients from US Clinical Genetics Units with personal/family history sugestive of hereditary breast/ovarian that tested negative for BRCA 1 -2 N= 26375 controls 11 germline TP 53 carriers were identified Among TP 53 carriers, only 5/11 (45%) met the classical criteria for Li. Fraumeni Syndrome or were diagnosed < 31 years Her 2 +++ bilateral or concurrent BC in TP 53 carriers more often Her 2+ (83 vs 24% non carriers), diagnosed tumors earlier (39 vs 48 years non carriers) and more often bilateral (36 vs 13%) #SEOM 2017
TP 53 Increased risk of BC - Screening: annual breast MRI with contrast starting at 20 years, try to avoid mammograms because of deletereus effect - RRM: Consider. Discuss on the Li-Fraumeni risks apart from BC No increased risk for OC Specific increase of risk for other Li-Fraumeni syndrome tumors: annual body MRI, endoscopy every 2 -5 years, dermatological examination yearly. #SEOM 2017
#SEOM 2017
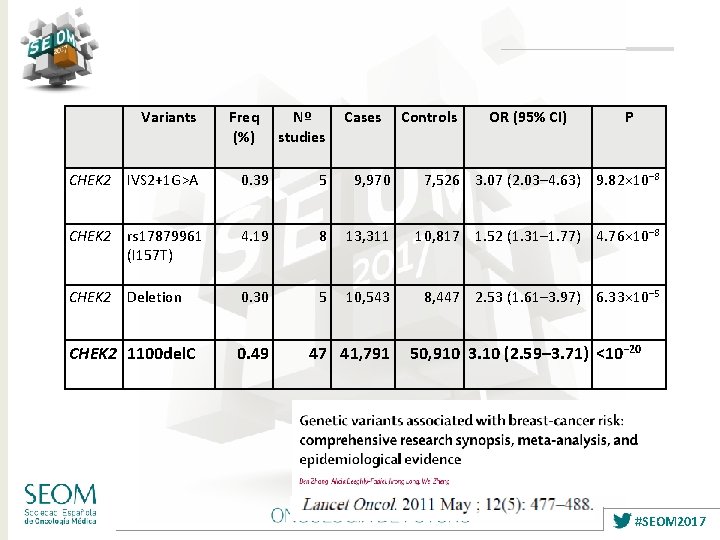
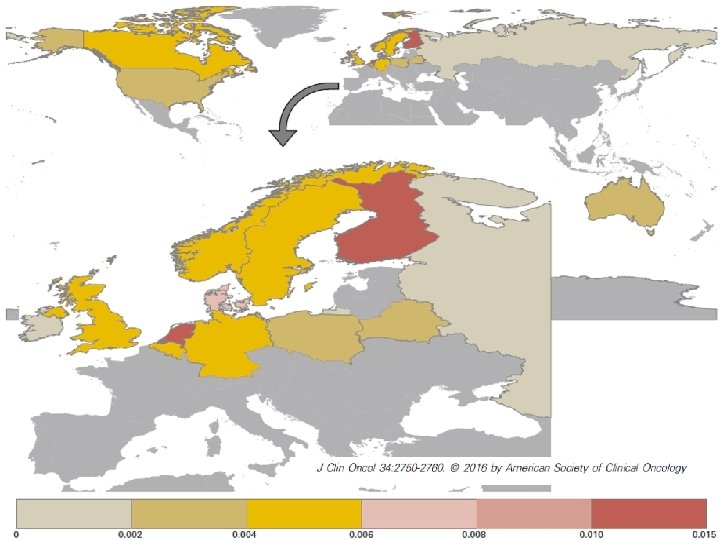
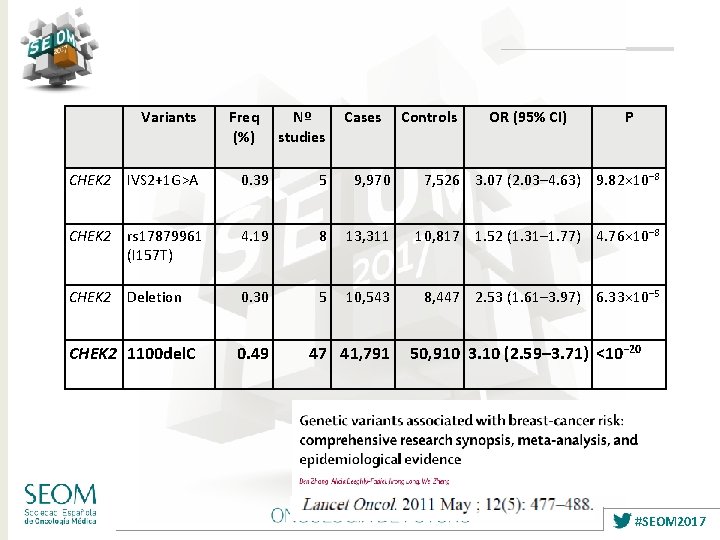
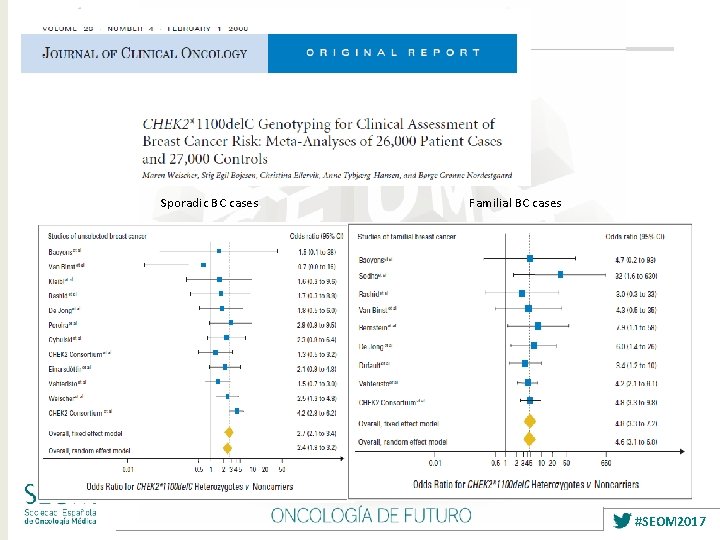
Variants Freq (%) Nº studies Cases Controls OR (95% CI) P CHEK 2 IVS 2+1 G>A 0. 39 5 9, 970 7, 526 3. 07 (2. 03– 4. 63) 9. 82× 10− 8 CHEK 2 rs 17879961 (I 157 T) 4. 19 8 13, 311 10, 817 1. 52 (1. 31– 1. 77) 4. 76× 10− 8 CHEK 2 Deletion 0. 30 5 10, 543 8, 447 2. 53 (1. 61– 3. 97) 6. 33× 10− 5 CHEK 2 1100 del. C 0. 49 47 41, 791 50, 910 3. 10 (2. 59– 3. 71) <10− 20 #SEOM 2017
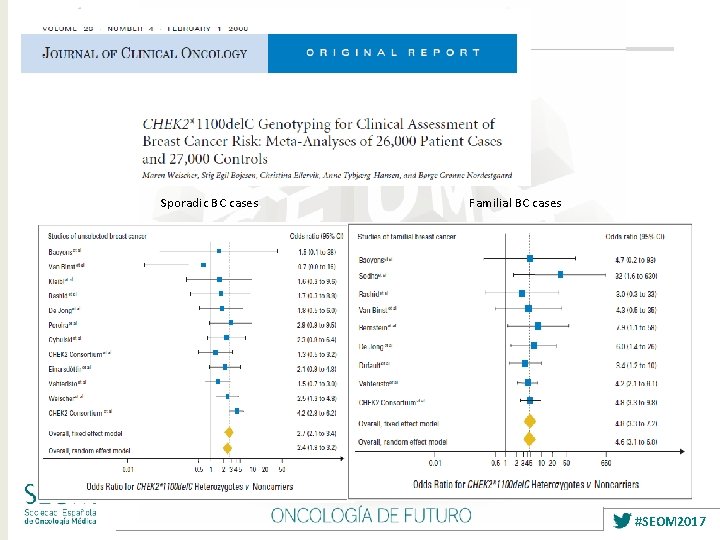
Sporadic BC cases Familial BC cases #SEOM 2017
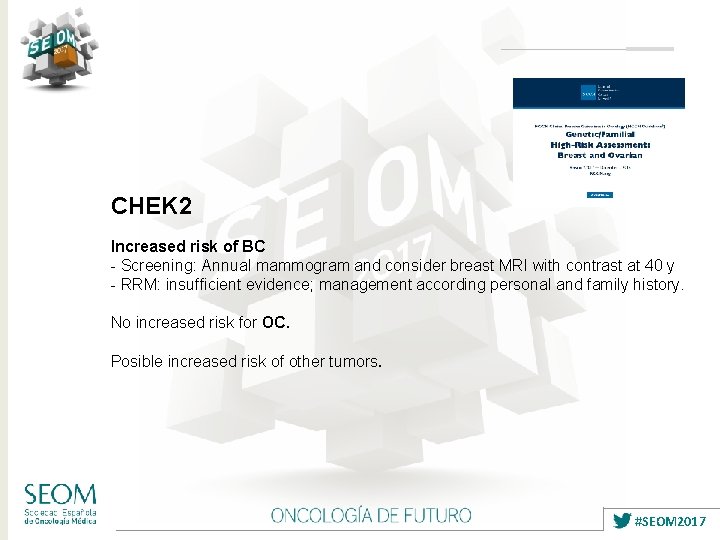
CHEK 2 Increased risk of BC - Screening: Annual mammogram and consider breast MRI with contrast at 40 y - RRM: insufficient evidence; management according personal and family history. No increased risk for OC. Posible increased risk of other tumors. #SEOM 2017
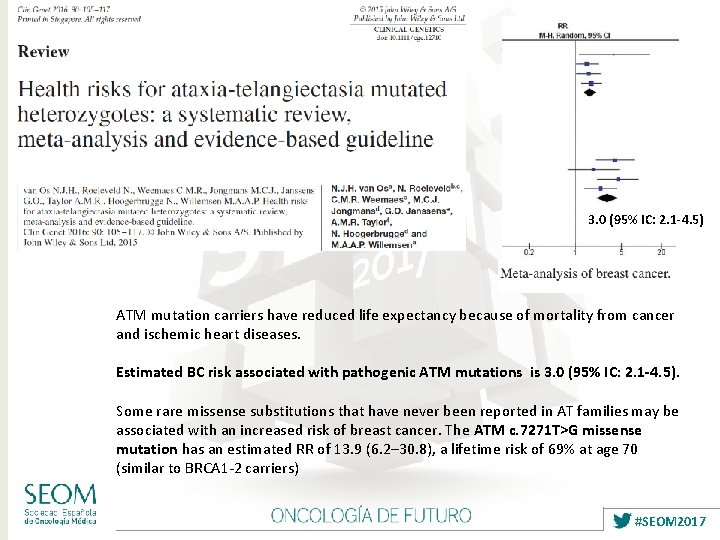
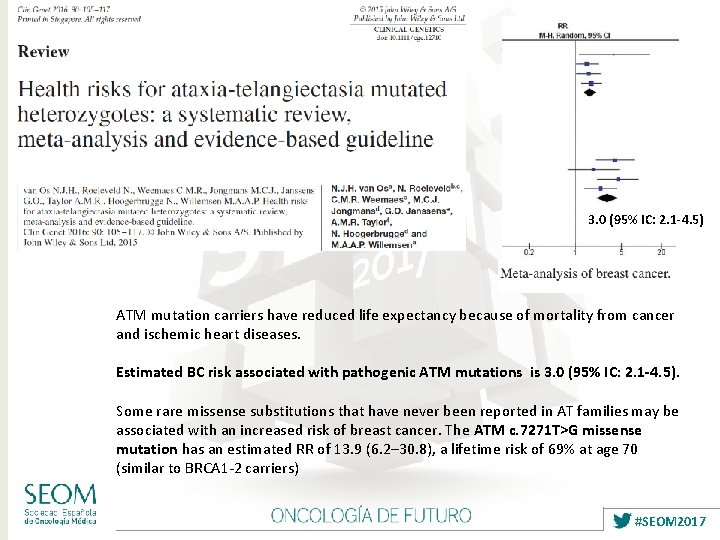
3. 0 (95% IC: 2. 1 -4. 5) ATM mutation carriers have reduced life expectancy because of mortality from cancer and ischemic heart diseases. Estimated BC risk associated with pathogenic ATM mutations is 3. 0 (95% IC: 2. 1 -4. 5). Some rare missense substitutions that have never been reported in AT families may be associated with an increased risk of breast cancer. The ATM c. 7271 T>G missense mutation has an estimated RR of 13. 9 (6. 2– 30. 8), a lifetime risk of 69% at age 70 (similar to BRCA 1 -2 carriers) #SEOM 2017
ATM Increased risk of BC - Screening: Annual mammogram and consider breast MRI with contrast at 40 y - RRM: Consider based on family history. No increased risk for OC. Unknown or insufficient evidence for other cancer risk management. Comments: The 7271 T>G missense mutation may act in a dominant– negative fashion, resulting in a lifetime breast cancer risk as high as 60% by age 80 (which is higher than truncating mutations, where risks are in the range of 30 -40%). Counsel for risk of autosomal recessive condition in offspring. #SEOM 2017
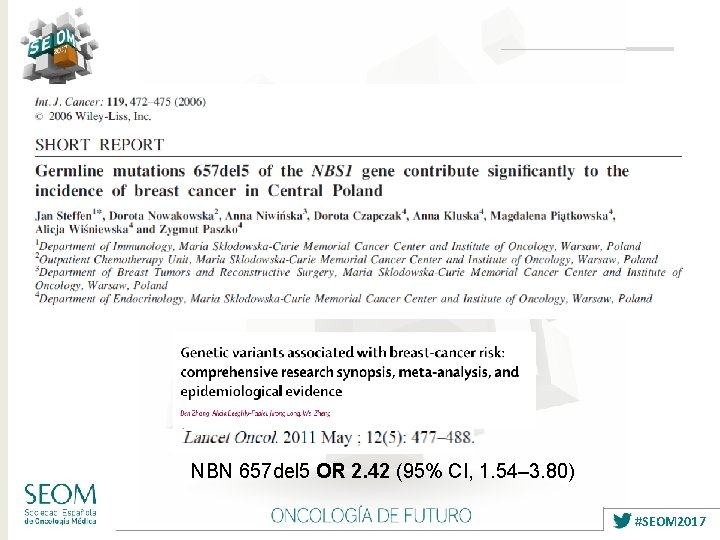
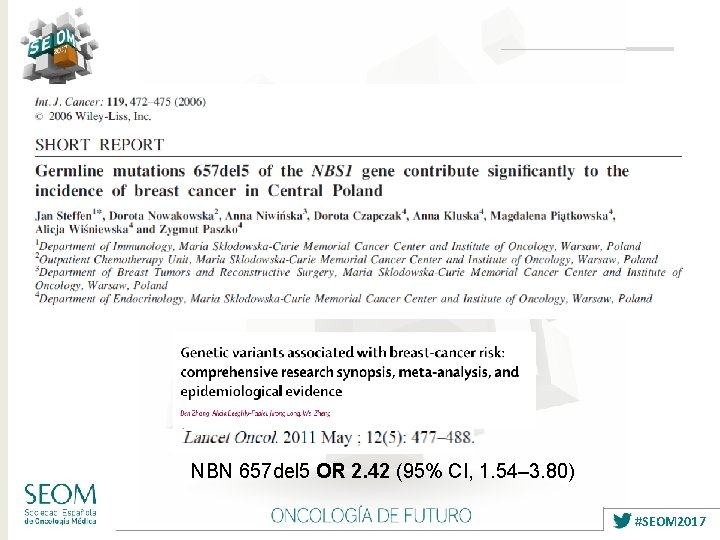
NBN 657 del 5 OR 2. 42 (95% CI, 1. 54– 3. 80) #SEOM 2017
NBN Increased risk of BC - Screening: Annual mammogram and consider breast MRI with contrast at 40 y - RRM: insufficient evidence; management according personal and family history. No increased risk for OC. Comments: Data on risk estimates are derived from the Slavic founder mutation 657 del 5. Counsel for risk of autosomal recessive condition in offspring (NBS) #SEOM 2017
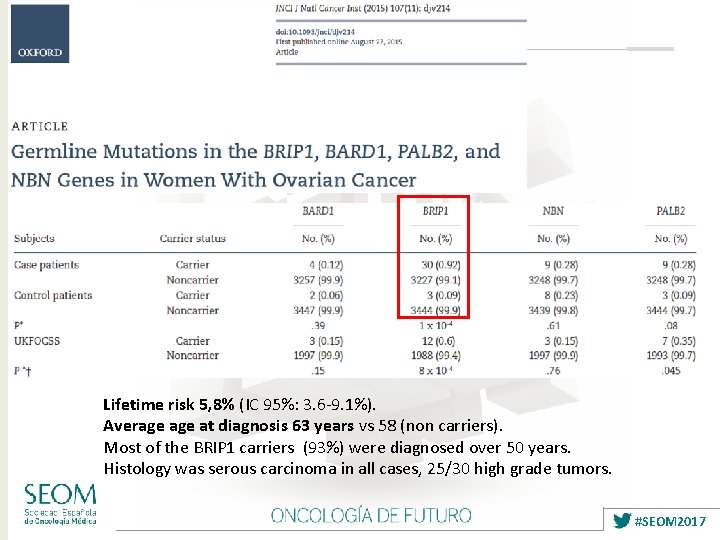
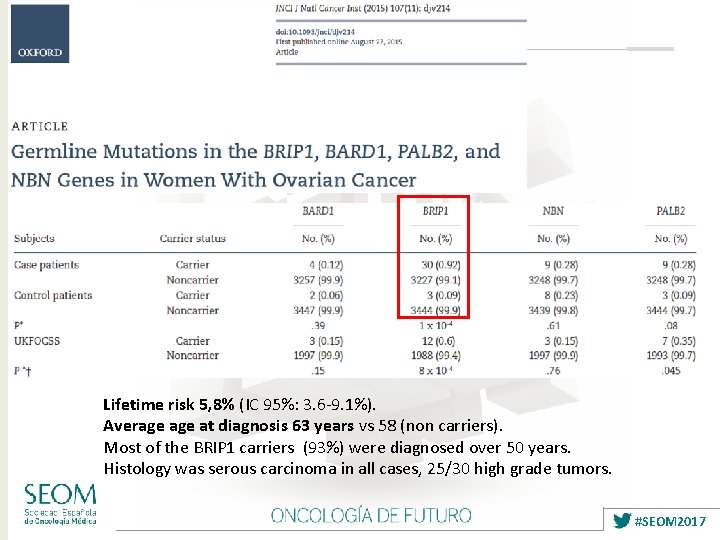
Lifetime risk 5, 8% (IC 95%: 3. 6 -9. 1%). Average at diagnosis 63 years vs 58 (non carriers). Most of the BRIP 1 carriers (93%) were diagnosed over 50 years. Histology was serous carcinoma in all cases, 25/30 high grade tumors. #SEOM 2017
BRIP 1 No increased risk for BC (Easton DF, J Med Genet 2016) Increased risk for OC risk: - Consider BSO from age 45 -50 or earlier depending on family history Unknown or insufficient evidence for other cancer risk management. Comments: Counsel for risk of autosomal recessive condition in offspring. #SEOM 2017
#SEOM 2017
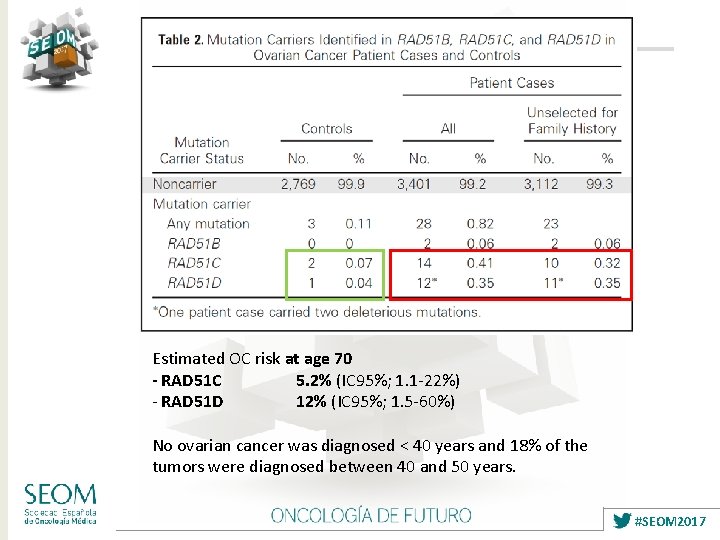
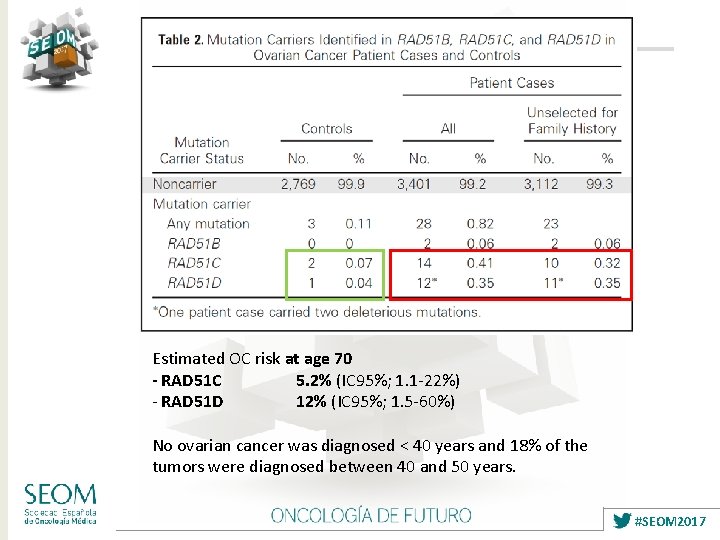
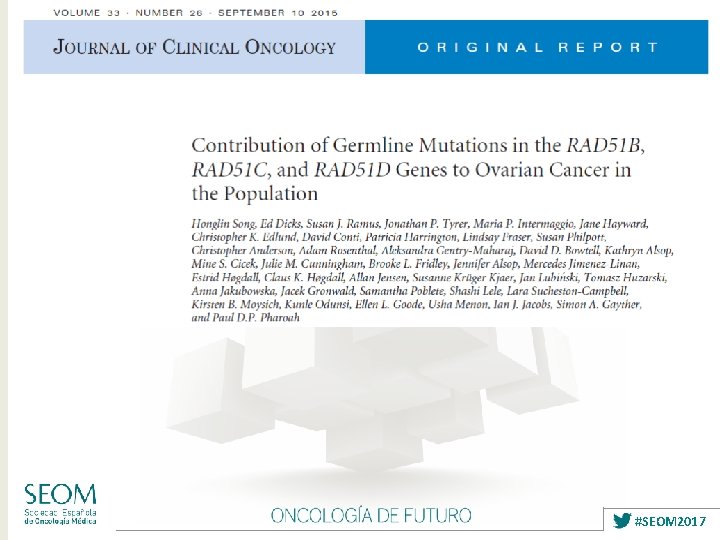
Estimated OC risk at age 70 - RAD 51 C 5. 2% (IC 95%; 1. 1 -22%) - RAD 51 D 12% (IC 95%; 1. 5 -60%) No ovarian cancer was diagnosed < 40 years and 18% of the tumors were diagnosed between 40 and 50 years. #SEOM 2017
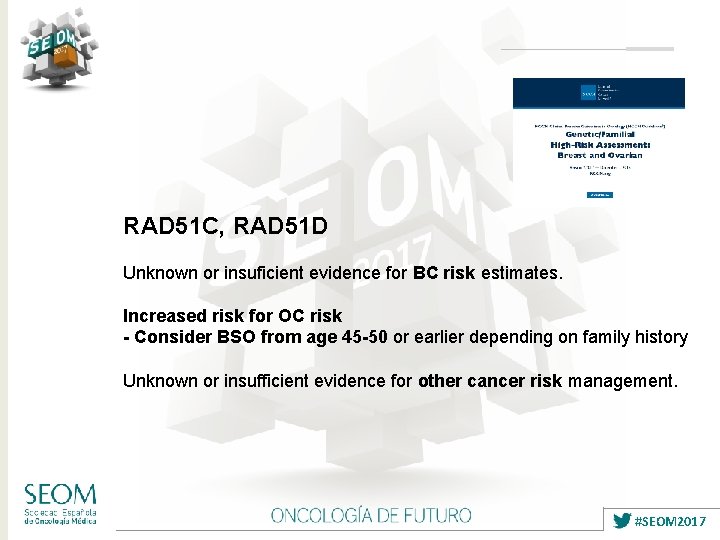
RAD 51 C, RAD 51 D Unknown or insuficient evidence for BC risk estimates. Increased risk for OC risk - Consider BSO from age 45 -50 or earlier depending on family history Unknown or insufficient evidence for other cancer risk management. #SEOM 2017
Resumen Seguimiento de familias de alto riesgo y riesgo moderado. Nuevos genes de predisposición hereditaria a cáncer de mama y cáncer de ovario y recomendaciones para el seguimiento de inviduos portadores. Posible impacto en la implementación de paneles multi-gen en el seguimiento y medidas de reducción de riesgo en predisposición hereditaria a cáncer de mama / ovario. #SEOM 2017
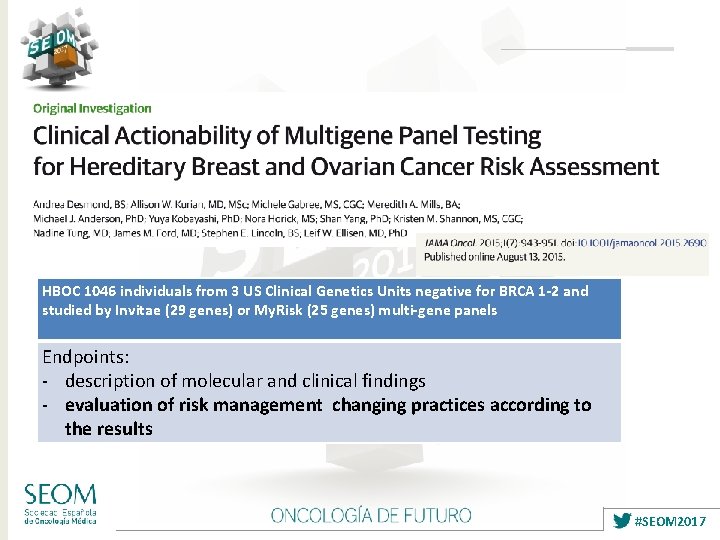
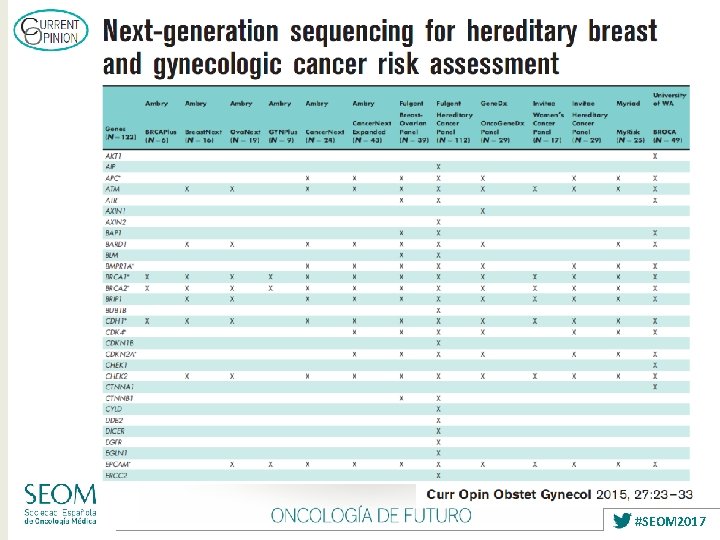
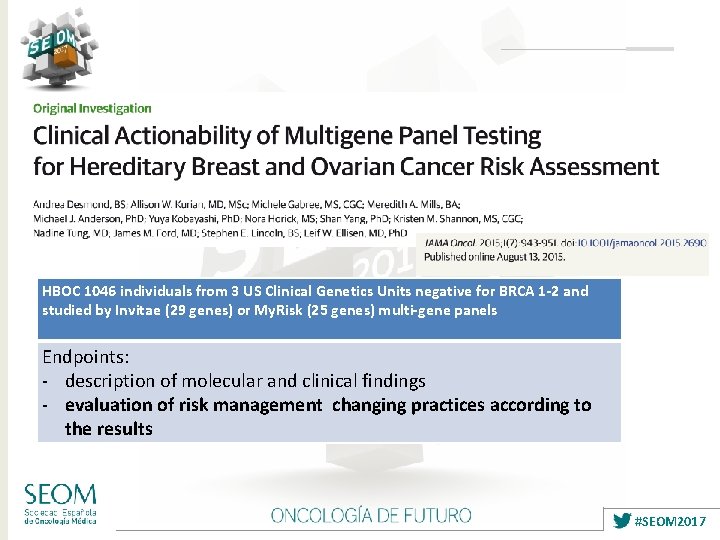
HBOC 1046 individuals from 3 US Clinical Genetics Units negative for BRCA 1 -2 and studied by Invitae (29 genes) or My. Risk (25 genes) multi-gene panels Endpoints: - description of molecular and clinical findings - evaluation of risk management changing practices according to the results #SEOM 2017
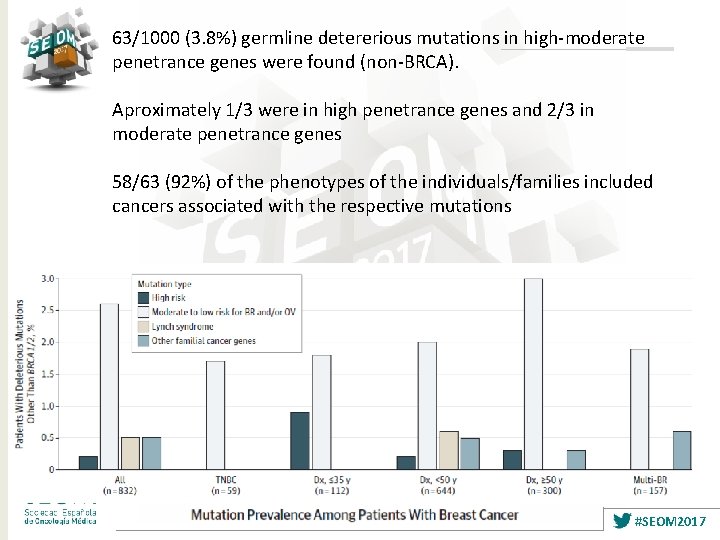
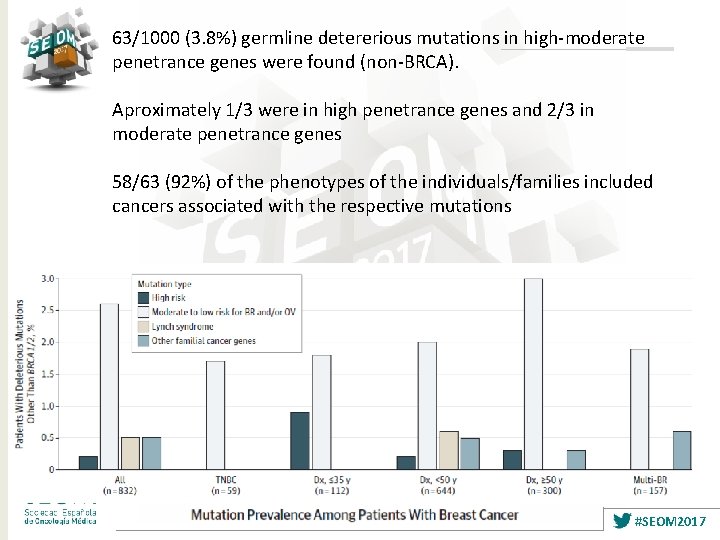
63/1000 (3. 8%) germline detererious mutations in high-moderate penetrance genes were found (non-BRCA). Aproximately 1/3 were in high penetrance genes and 2/3 in moderate penetrance genes 58/63 (92%) of the phenotypes of the individuals/families included cancers associated with the respective mutations #SEOM 2017
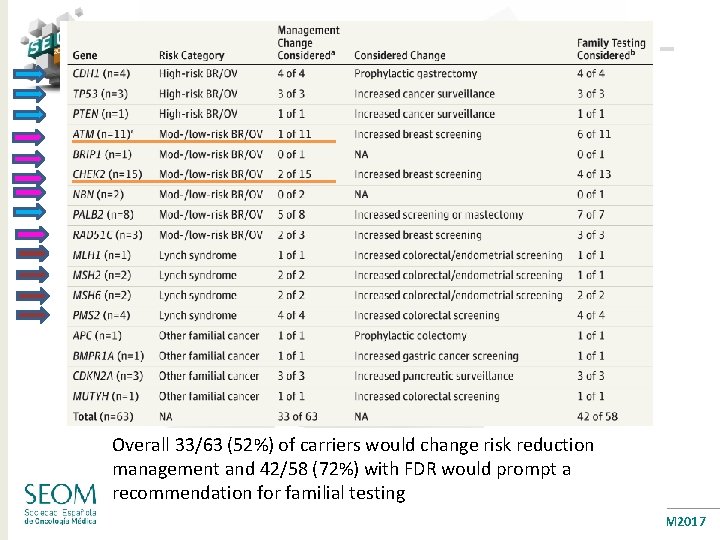
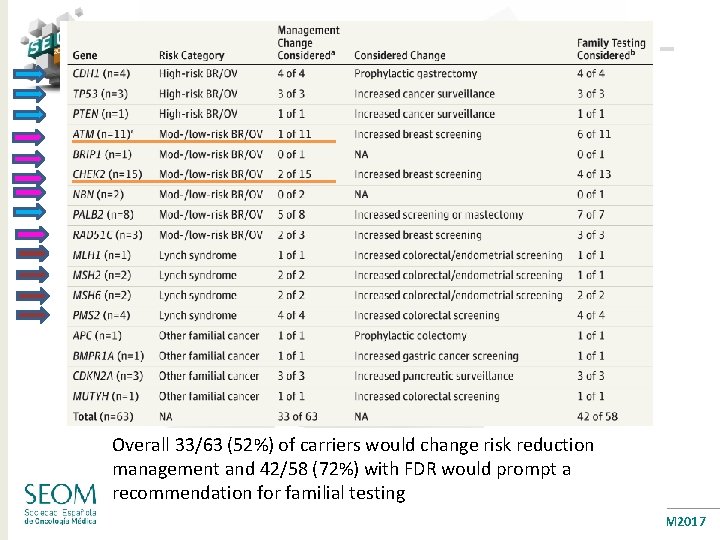
Overall 33/63 (52%) of carriers would change risk reduction management and 42/58 (72%) with FDR would prompt a recommendation for familial testing #SEOM 2017
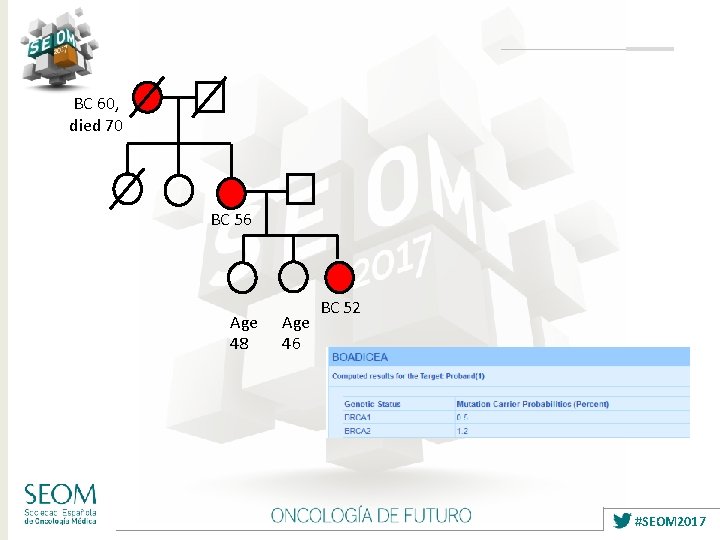
BC 60, died 70 BC 56 Age 48 Age 46 BC 52 #SEOM 2017
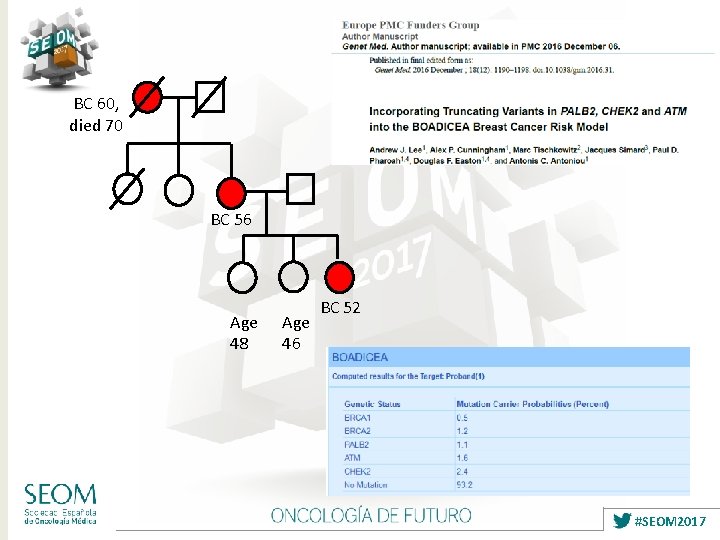
BC 60, died 70 BC 56 Age 48 Age 46 BC 52 #SEOM 2017
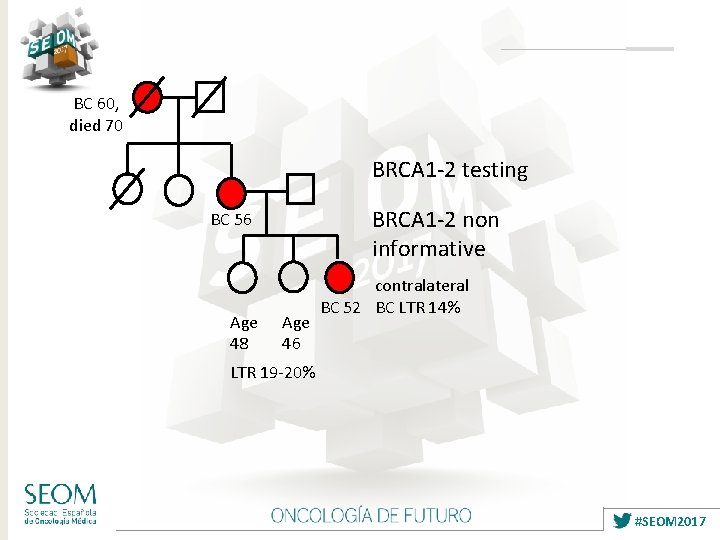
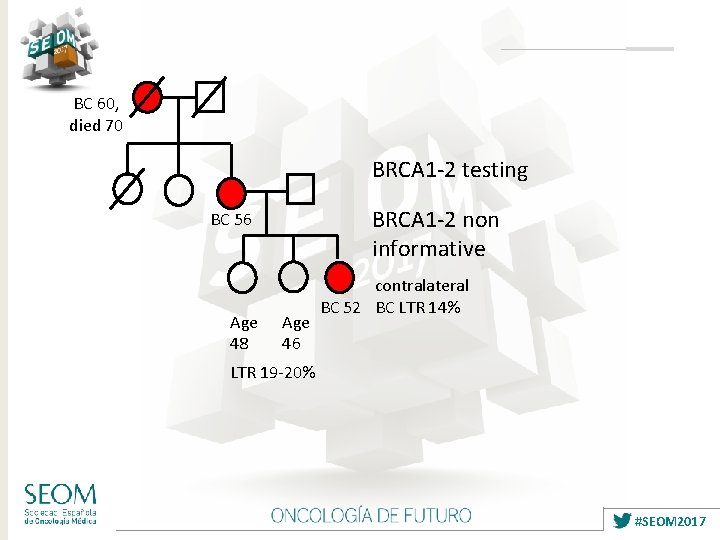
BC 60, died 70 BRCA 1 -2 testing BRCA 1 -2 non informative BC 56 Age 48 Age 46 contralateral BC 52 BC LTR 14% LTR 19 -20% #SEOM 2017
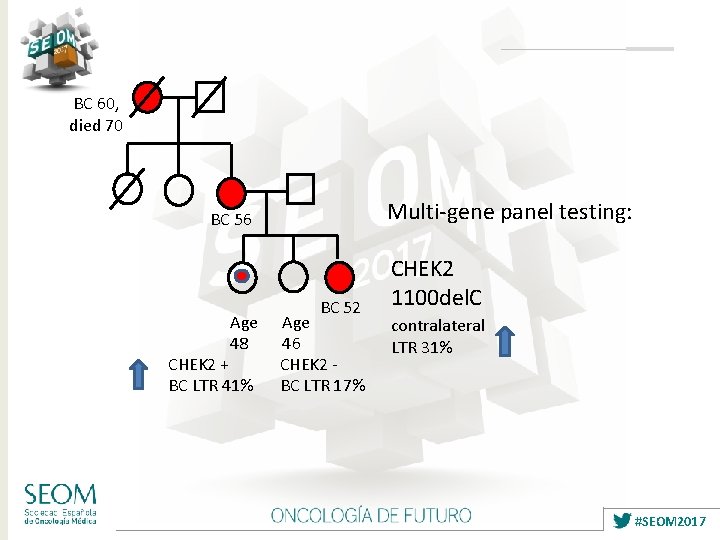
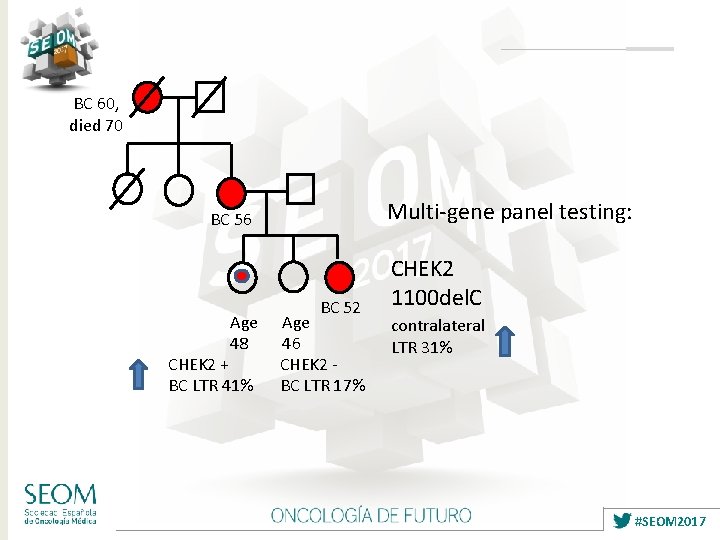
BC 60, died 70 Multi-gene panel testing: BC 56 Age 48 CHEK 2 + BC LTR 41% BC 52 Age 46 CHEK 2 BC LTR 17% CHEK 2 1100 del. C contralateral LTR 31% #SEOM 2017
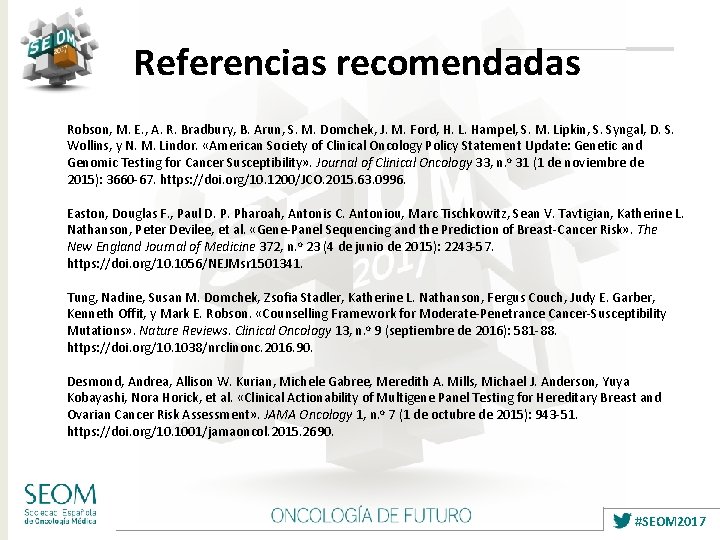
Referencias recomendadas Robson, M. E. , A. R. Bradbury, B. Arun, S. M. Domchek, J. M. Ford, H. L. Hampel, S. M. Lipkin, S. Syngal, D. S. Wollins, y N. M. Lindor. «American Society of Clinical Oncology Policy Statement Update: Genetic and Genomic Testing for Cancer Susceptibility» . Journal of Clinical Oncology 33, n. o 31 (1 de noviembre de 2015): 3660 -67. https: //doi. org/10. 1200/JCO. 2015. 63. 0996. Easton, Douglas F. , Paul D. P. Pharoah, Antonis C. Antoniou, Marc Tischkowitz, Sean V. Tavtigian, Katherine L. Nathanson, Peter Devilee, et al. «Gene-Panel Sequencing and the Prediction of Breast-Cancer Risk» . The New England Journal of Medicine 372, n. o 23 (4 de junio de 2015): 2243 -57. https: //doi. org/10. 1056/NEJMsr 1501341. Tung, Nadine, Susan M. Domchek, Zsofia Stadler, Katherine L. Nathanson, Fergus Couch, Judy E. Garber, Kenneth Offit, y Mark E. Robson. «Counselling Framework for Moderate-Penetrance Cancer-Susceptibility Mutations» . Nature Reviews. Clinical Oncology 13, n. o 9 (septiembre de 2016): 581 -88. https: //doi. org/10. 1038/nrclinonc. 2016. 90. Desmond, Andrea, Allison W. Kurian, Michele Gabree, Meredith A. Mills, Michael J. Anderson, Yuya Kobayashi, Nora Horick, et al. «Clinical Actionability of Multigene Panel Testing for Hereditary Breast and Ovarian Cancer Risk Assessment» . JAMA Oncology 1, n. o 7 (1 de octubre de 2015): 943 -51. https: //doi. org/10. 1001/jamaoncol. 2015. 2690. #SEOM 2017
 Linked genes and unlinked genes
Linked genes and unlinked genes Homeotic genes vs hox genes
Homeotic genes vs hox genes Linked genes and unlinked genes
Linked genes and unlinked genes Para vino nuevo odres nuevos
Para vino nuevo odres nuevos Ella necesita ir de compras para comprar calcetines nuevos.
Ella necesita ir de compras para comprar calcetines nuevos. Las tic y los nuevos paradigmas educativos
Las tic y los nuevos paradigmas educativos La verdad yo no comparto ese desprecio a los nuevos ricos
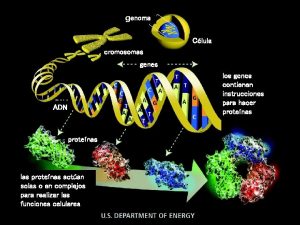
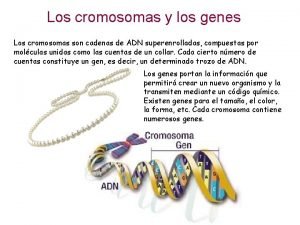
La verdad yo no comparto ese desprecio a los nuevos ricos Los transposones son genes móviles en un cromosoma
Los transposones son genes móviles en un cromosoma Expresión génica
Expresión génica Unos verbos
Unos verbos Etapas de desarrollo de nuevos productos
Etapas de desarrollo de nuevos productos Edad de cobre bronce y hierro
Edad de cobre bronce y hierro Cuentos creados
Cuentos creados Nuevos retos nuevas oportunidades
Nuevos retos nuevas oportunidades Nuevos comienzos en la biblia
Nuevos comienzos en la biblia Producto no buscados
Producto no buscados Nuevos inhibidores de betalactamasas
Nuevos inhibidores de betalactamasas Nuevos inhibidores de betalactamasas
Nuevos inhibidores de betalactamasas Nuevos grados
Nuevos grados Nuevos anticonvulsivantes
Nuevos anticonvulsivantes Cambios culturales
Cambios culturales Nuevos paradigmas educativos
Nuevos paradigmas educativos Nuevos paradigmas educativos
Nuevos paradigmas educativos Paradigma conductista
Paradigma conductista Nuevos ambientes de aprendizaje
Nuevos ambientes de aprendizaje Medida de tendencia central para datos agrupados
Medida de tendencia central para datos agrupados Lamela mediana
Lamela mediana Importancia de las plantas sin semilla
Importancia de las plantas sin semilla Cálculo de fórmula láctea por peso
Cálculo de fórmula láctea por peso Medidas de resumen para variables cuantitativas
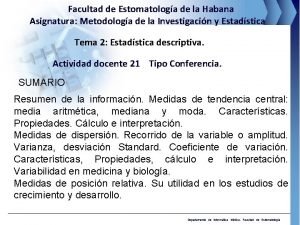
Medidas de resumen para variables cuantitativas Medidas de resumen para variables cuantitativas
Medidas de resumen para variables cuantitativas Seguridad en el techo
Seguridad en el techo Nimf 20
Nimf 20 Ojiva
Ojiva Medida de varas
Medida de varas Medidas de los triangulos
Medidas de los triangulos Figuras con ángulos obtusos
Figuras con ángulos obtusos Ejemplo de plan de monitoreo y seguimiento
Ejemplo de plan de monitoreo y seguimiento Objetivos y metas del pemc ejemplos
Objetivos y metas del pemc ejemplos Seguimiento y control fondef
Seguimiento y control fondef Seguimiento de mab
Seguimiento de mab Ejemplo de plan de monitoreo y seguimiento
Ejemplo de plan de monitoreo y seguimiento Seguimiento presupuestario
Seguimiento presupuestario Características del seguimiento a jesús
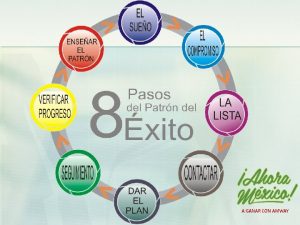
Características del seguimiento a jesús 8 pasos del patron del exito amway
8 pasos del patron del exito amway Rgp consultas
Rgp consultas Seguimiento etapa productiva sena
Seguimiento etapa productiva sena Seguimiento nominal
Seguimiento nominal Bloque de seguimiento
Bloque de seguimiento