LUTS NOCTURIA INCONTINENCE RECURRENT UTIS St George Education


- Slides: 63
LUTS – NOCTURIA & INCONTINENCE RECURRENT UTI’S St George Education Forum
Agenda • LUTS = Lower Urinary Tract Symptoms • OAB = Over. Active Bladder • Incontinence • Nocturia • Approach • Newer therapies • Recurrent Urinary Tract Infections • Strategy
LUTS • Overactive Bladder • Incontinence
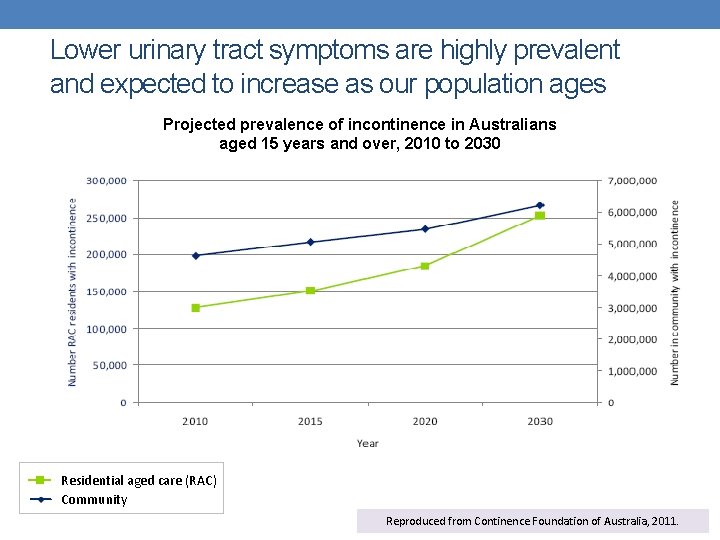
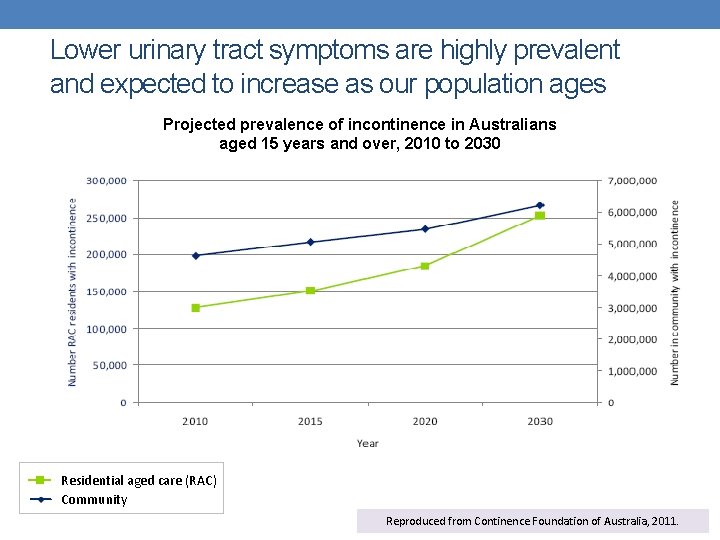
Lower urinary tract symptoms are highly prevalent and expected to increase as our population ages Projected prevalence of incontinence in Australians aged 15 years and over, 2010 to 2030 Residential aged care (RAC) Community Reproduced from Continence Foundation of Australia, 2011.
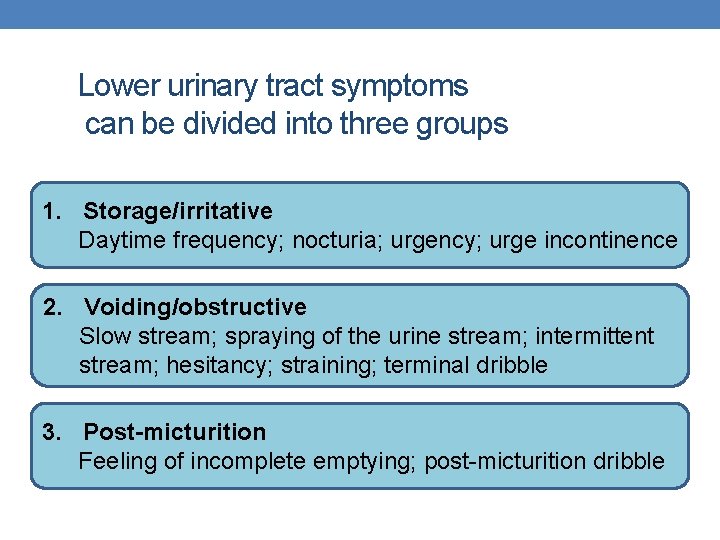
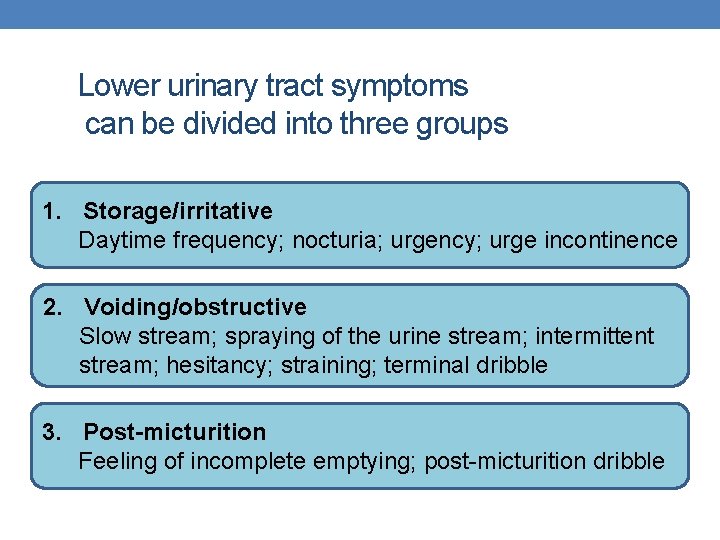
Lower urinary tract symptoms can be divided into three groups 1. Storage/irritative Daytime frequency; nocturia; urgency; urge incontinence 2. Voiding/obstructive Slow stream; spraying of the urine stream; intermittent stream; hesitancy; straining; terminal dribble 3. Post-micturition Feeling of incomplete emptying; post-micturition dribble
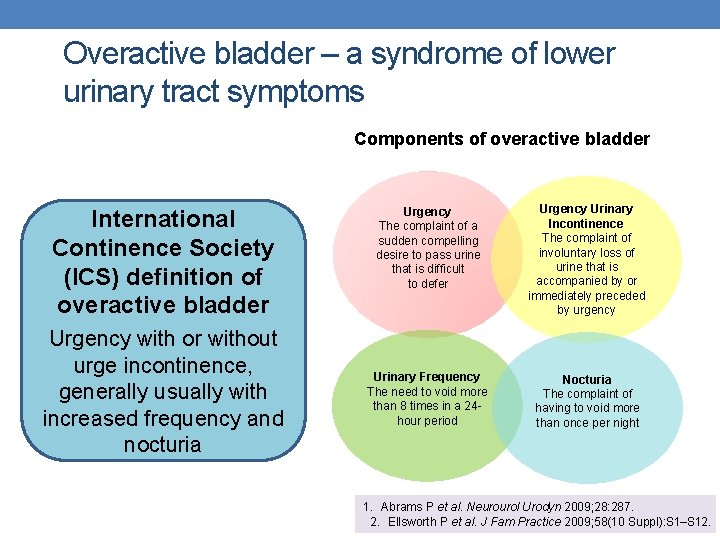
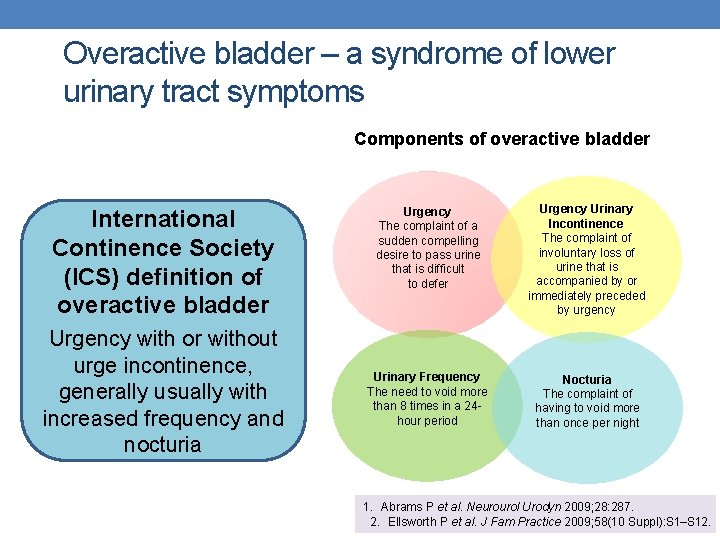
Overactive bladder – a syndrome of lower urinary tract symptoms Components of overactive bladder International Continence Society (ICS) definition of overactive bladder Urgency with or without urge incontinence, generally usually with increased frequency and nocturia Urgency The complaint of a sudden compelling desire to pass urine that is difficult to defer Urgency Urinary Incontinence The complaint of involuntary loss of urine that is accompanied by or immediately preceded by urgency Urinary Frequency The need to void more than 8 times in a 24 hour period Nocturia The complaint of having to void more than once per night 1. Abrams P et al. Neurourol Urodyn 2009; 28: 287. 2. Ellsworth P et al. J Fam Practice 2009; 58(10 Suppl): S 1–S 12.
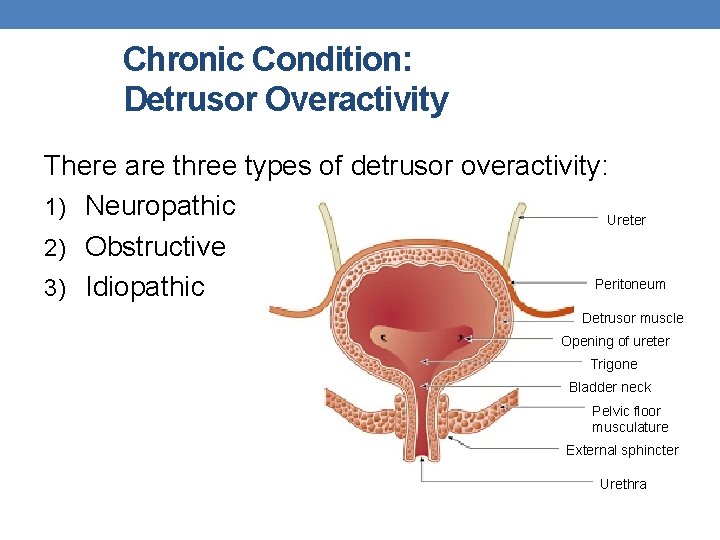
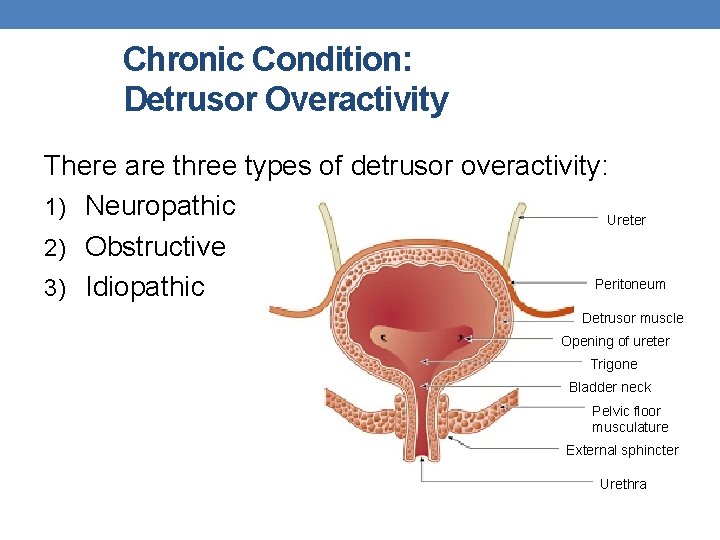
Chronic Condition: Detrusor Overactivity There are three types of detrusor overactivity: 1) Neuropathic Ureter 2) Obstructive Peritoneum 3) Idiopathic Detrusor muscle Opening of ureter Trigone Bladder neck Pelvic floor musculature External sphincter Urethra
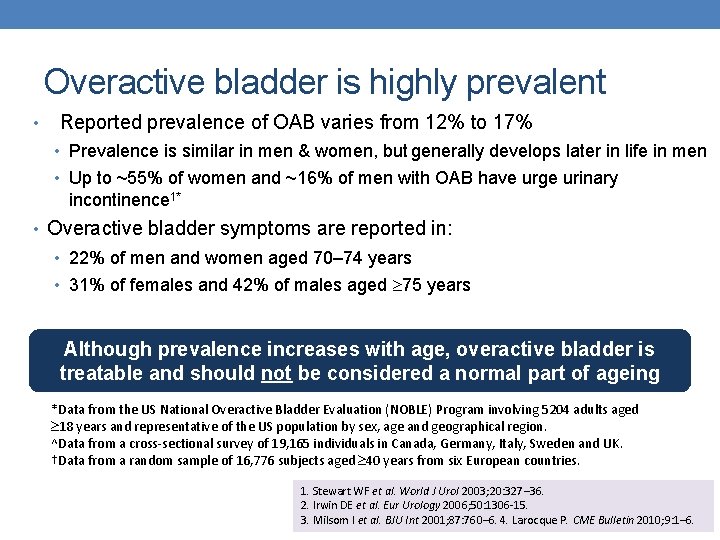
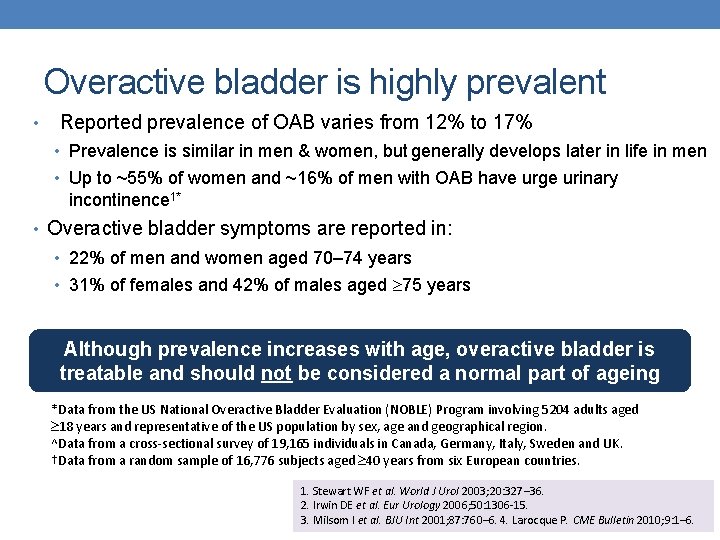
Overactive bladder is highly prevalent • Reported prevalence of OAB varies from 12% to 17% • Prevalence is similar in men & women, but generally develops later in life in men • Up to ~55% of women and ~16% of men with OAB have urge urinary incontinence 1* • Overactive bladder symptoms are reported in: • 22% of men and women aged 70– 74 years • 31% of females and 42% of males aged 75 years Although prevalence increases with age, overactive bladder is treatable and should not be considered a normal part of ageing *Data from the US National Overactive Bladder Evaluation (NOBLE) Program involving 5204 adults aged 18 years and representative of the US population by sex, age and geographical region. ^Data from a cross-sectional survey of 19, 165 individuals in Canada, Germany, Italy, Sweden and UK. †Data from a random sample of 16, 776 subjects aged 40 years from six European countries. 1. Stewart WF et al. World J Urol 2003; 20: 327– 36. 2. Irwin DE et al. Eur Urology 2006; 50: 1306 -15. 3. Milsom I et al. BJU Int 2001; 87: 760– 6. 4. Larocque P. CME Bulletin 2010; 9: 1– 6.
Risk factors for urinary incontinence • Female gender, in particular pre- and post-natal women • Advanced age • Menopause • Obesity • Recurrent urinary tract infections • Specific types of surgery such as prostatectomies, hysterectomies • Neurological diseases such as multiple sclerosis • Reduced mobility • Some medications Continence Foundation of Australia. The economic impact of incontinence in Australia 2011.
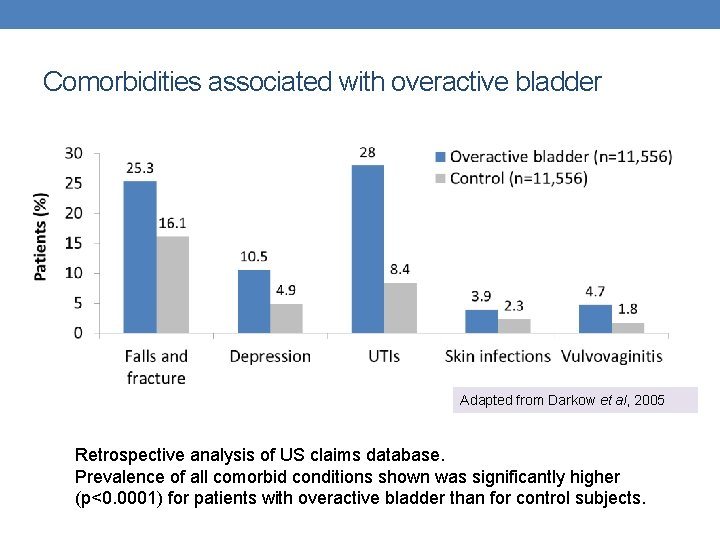
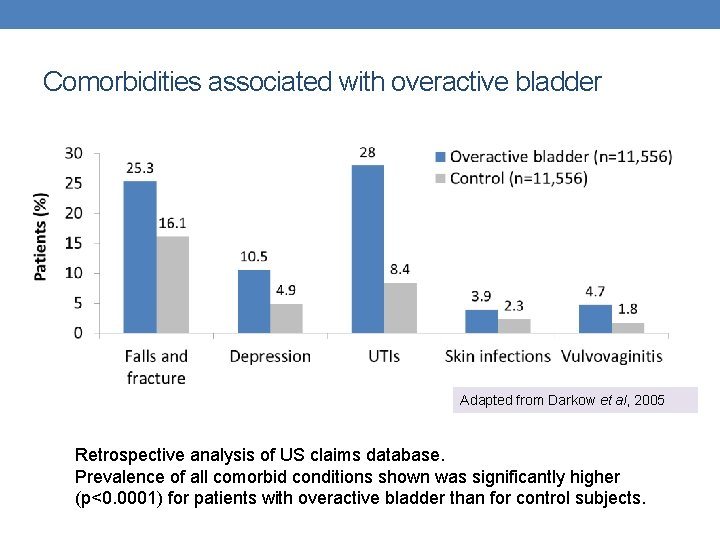
Comorbidities associated with overactive bladder Adapted from Darkow et al, 2005 Retrospective analysis of US claims database. Prevalence of all comorbid conditions shown was significantly higher (p<0. 0001) for patients with overactive bladder than for control subjects.
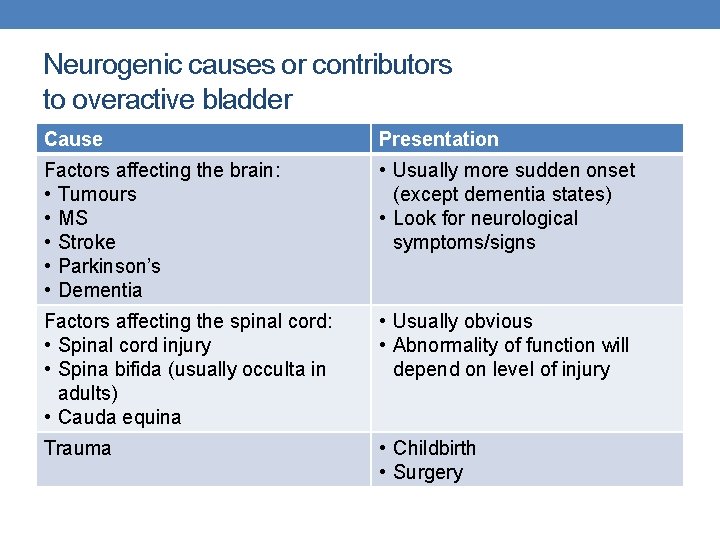
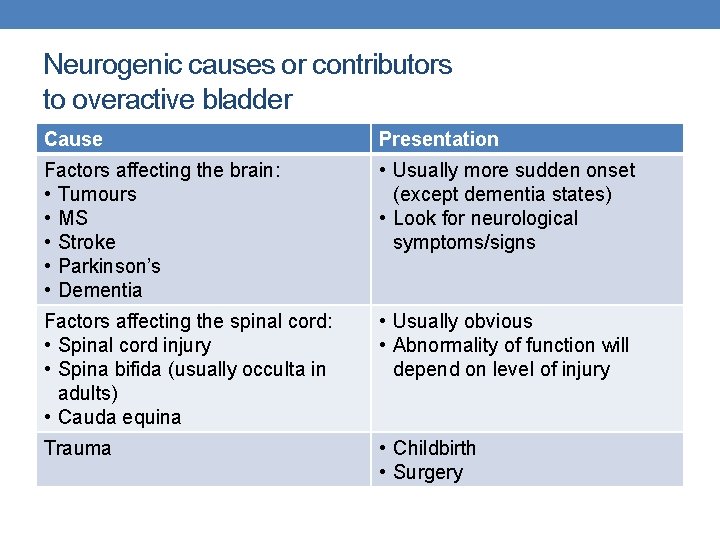
Neurogenic causes or contributors to overactive bladder Cause Presentation Factors affecting the brain: • Tumours • MS • Stroke • Parkinson’s • Dementia • Usually more sudden onset (except dementia states) • Look for neurological symptoms/signs Factors affecting the spinal cord: • Spinal cord injury • Spina bifida (usually occulta in adults) • Cauda equina • Usually obvious • Abnormality of function will depend on level of injury Trauma • Childbirth • Surgery
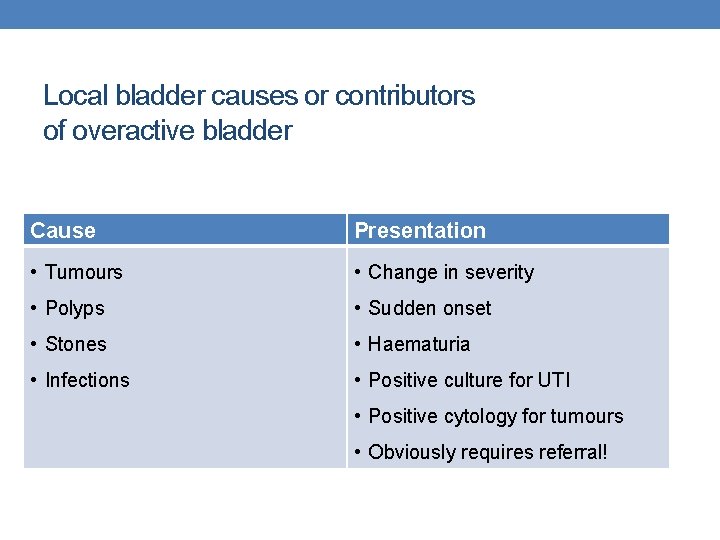
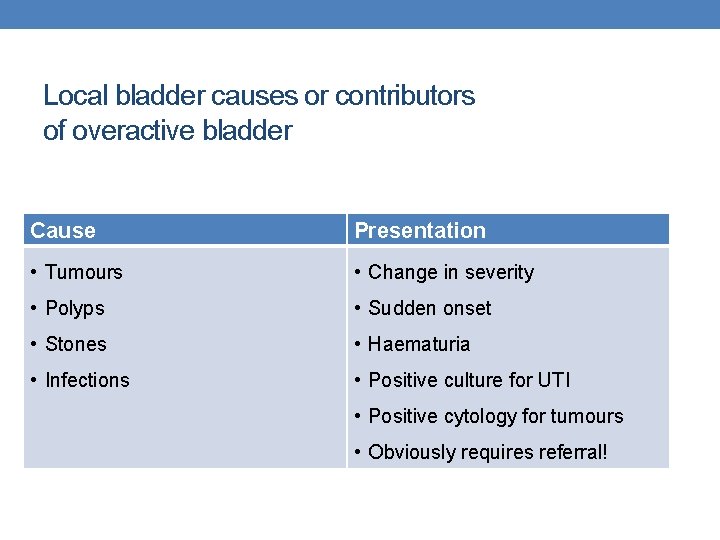
Local bladder causes or contributors of overactive bladder Cause Presentation • Tumours • Change in severity • Polyps • Sudden onset • Stones • Haematuria • Infections • Positive culture for UTI • Positive cytology for tumours • Obviously requires referral!
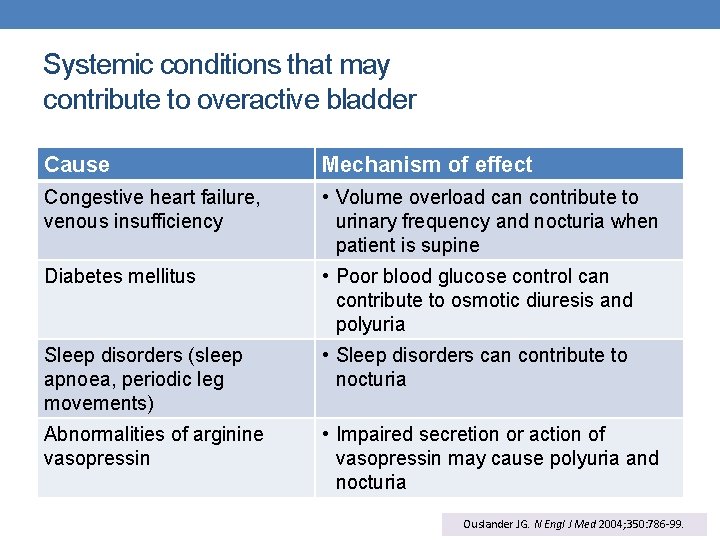
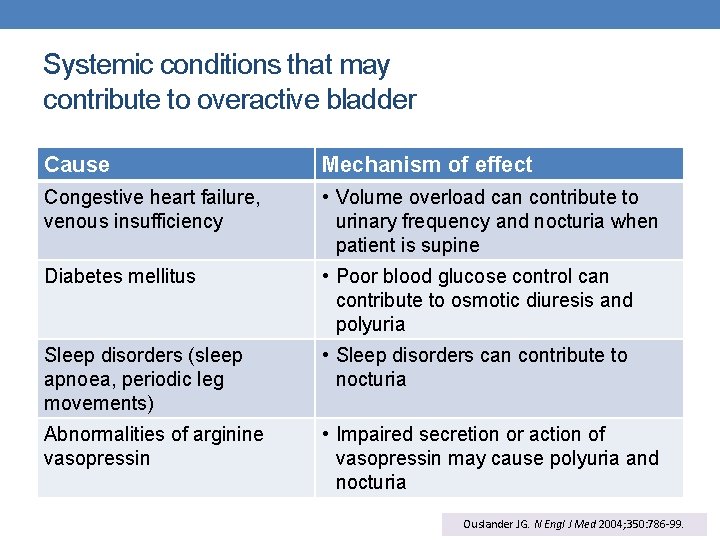
Systemic conditions that may contribute to overactive bladder Cause Mechanism of effect Congestive heart failure, venous insufficiency • Volume overload can contribute to urinary frequency and nocturia when patient is supine Diabetes mellitus • Poor blood glucose control can contribute to osmotic diuresis and polyuria Sleep disorders (sleep apnoea, periodic leg movements) • Sleep disorders can contribute to nocturia Abnormalities of arginine vasopressin • Impaired secretion or action of vasopressin may cause polyuria and nocturia Ouslander JG. N Engl J Med 2004; 350: 786 -99.
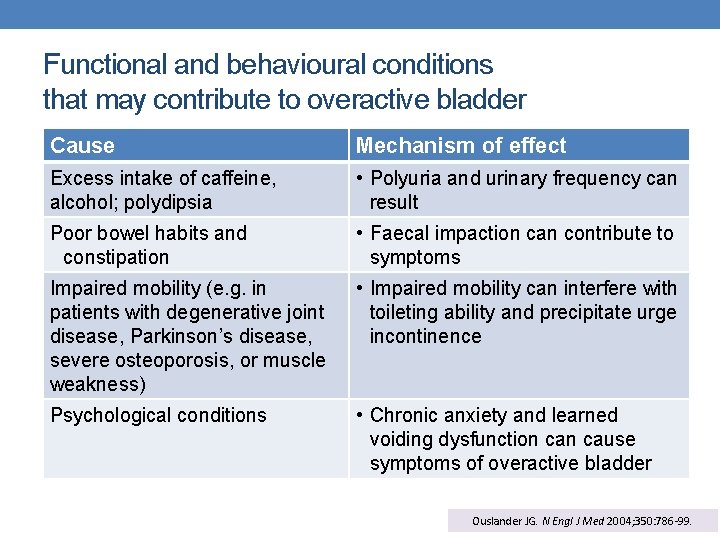
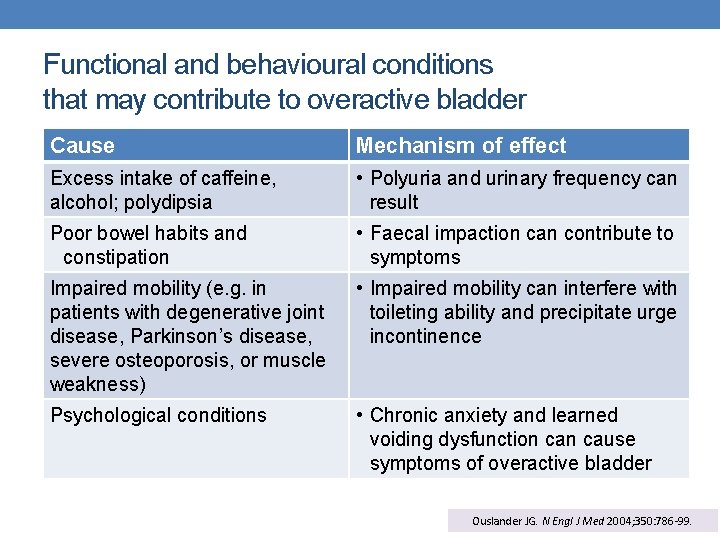
Functional and behavioural conditions that may contribute to overactive bladder Cause Mechanism of effect Excess intake of caffeine, alcohol; polydipsia • Polyuria and urinary frequency can result Poor bowel habits and constipation • Faecal impaction can contribute to symptoms Impaired mobility (e. g. in patients with degenerative joint disease, Parkinson’s disease, severe osteoporosis, or muscle weakness) • Impaired mobility can interfere with toileting ability and precipitate urge incontinence Psychological conditions • Chronic anxiety and learned voiding dysfunction cause symptoms of overactive bladder Ouslander JG. N Engl J Med 2004; 350: 786 -99.
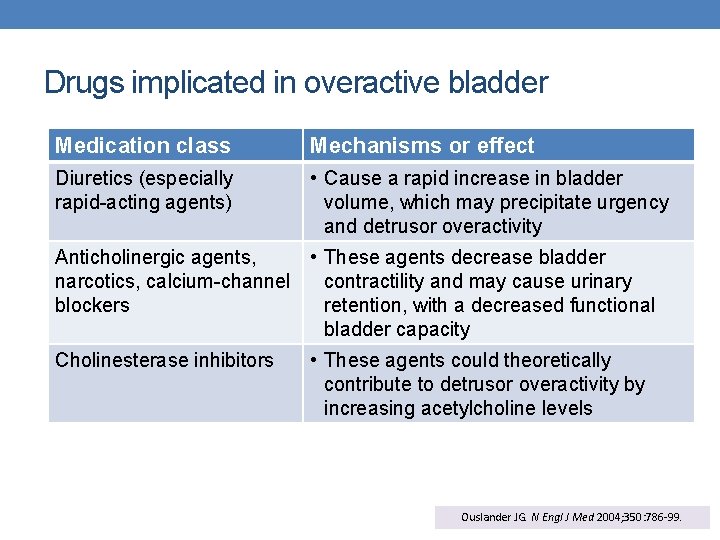
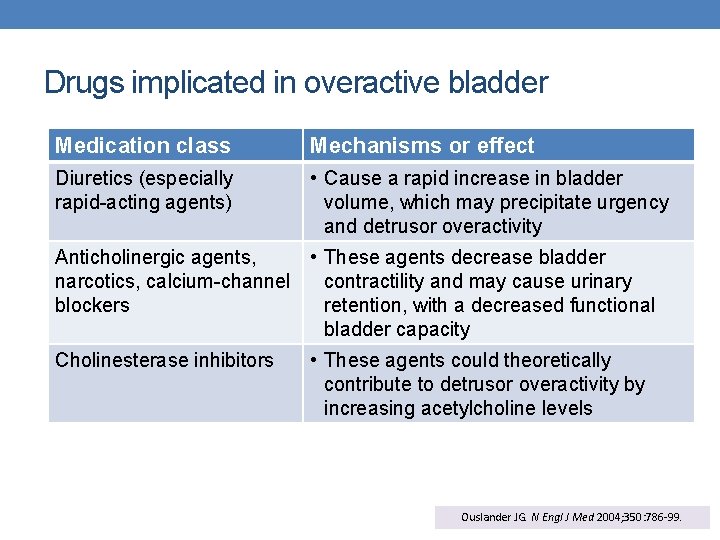
Drugs implicated in overactive bladder Medication class Mechanisms or effect Diuretics (especially rapid-acting agents) • Cause a rapid increase in bladder volume, which may precipitate urgency and detrusor overactivity Anticholinergic agents, • These agents decrease bladder narcotics, calcium-channel contractility and may cause urinary blockers retention, with a decreased functional bladder capacity Cholinesterase inhibitors • These agents could theoretically contribute to detrusor overactivity by increasing acetylcholine levels Ouslander JG. N Engl J Med 2004; 350: 786 -99.
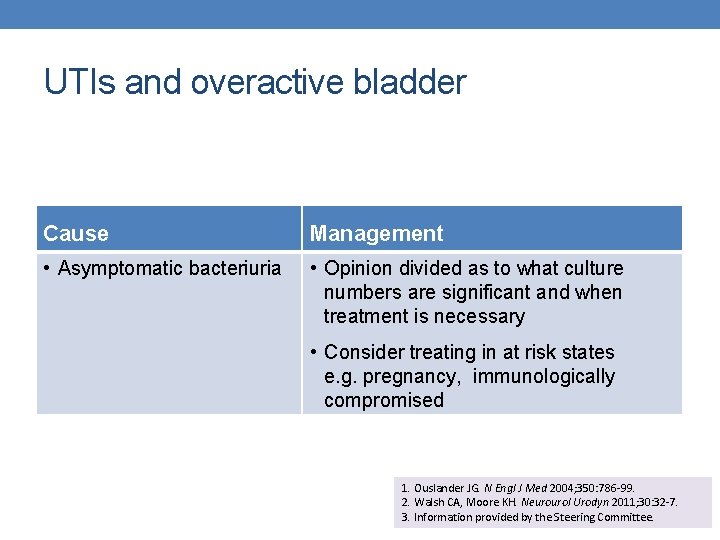
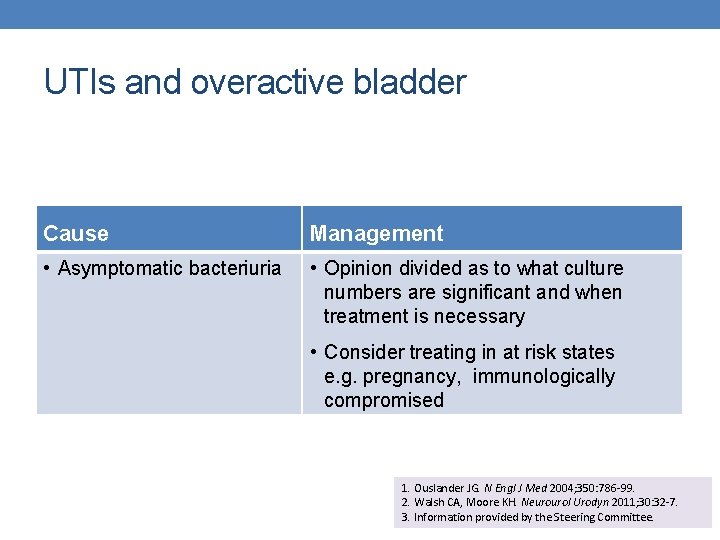
UTIs and overactive bladder Cause Management • Asymptomatic bacteriuria • Opinion divided as to what culture numbers are significant and when treatment is necessary • Consider treating in at risk states e. g. pregnancy, immunologically compromised 1. Ouslander JG. N Engl J Med 2004; 350: 786 -99. 2. Walsh CA, Moore KH. Neurourol Urodyn 2011; 30: 32 -7. 3. Information provided by the Steering Committee.
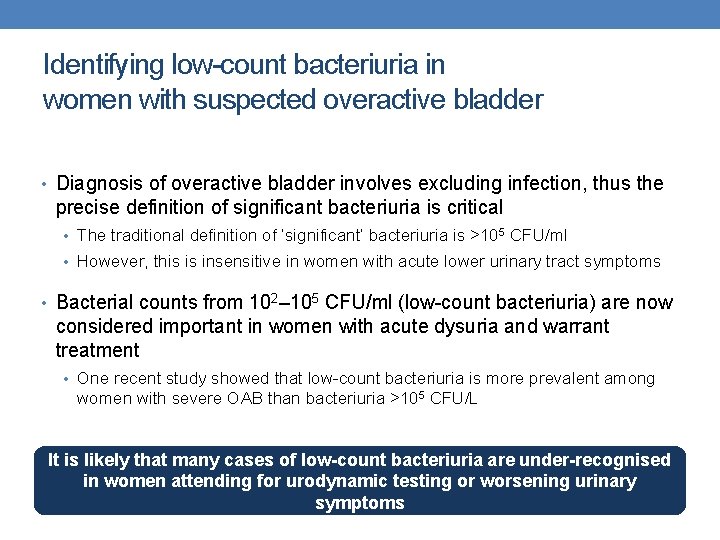
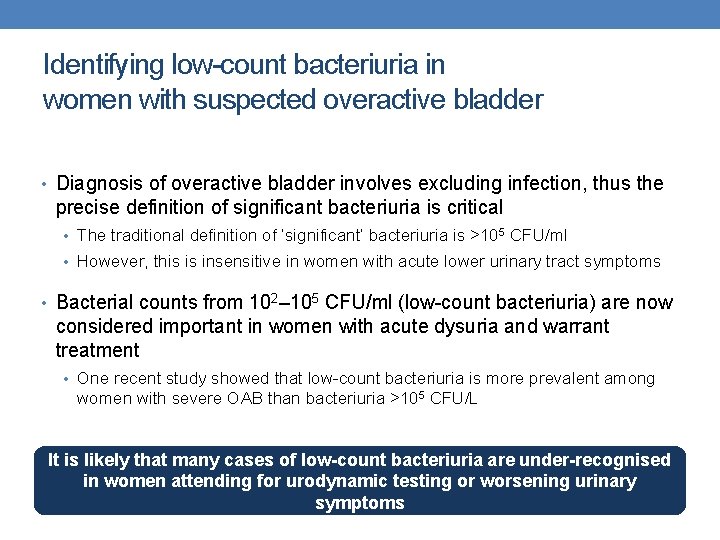
Identifying low-count bacteriuria in women with suspected overactive bladder • Diagnosis of overactive bladder involves excluding infection, thus the precise definition of significant bacteriuria is critical • The traditional definition of ‘significant’ bacteriuria is >105 CFU/ml • However, this is insensitive in women with acute lower urinary tract symptoms • Bacterial counts from 102– 105 CFU/ml (low-count bacteriuria) are now considered important in women with acute dysuria and warrant treatment • One recent study showed that low-count bacteriuria is more prevalent among women with severe OAB than bacteriuria >105 CFU/L It is likely that many cases of low-count bacteriuria are under-recognised in women attending for urodynamic testing or worsening urinary symptoms
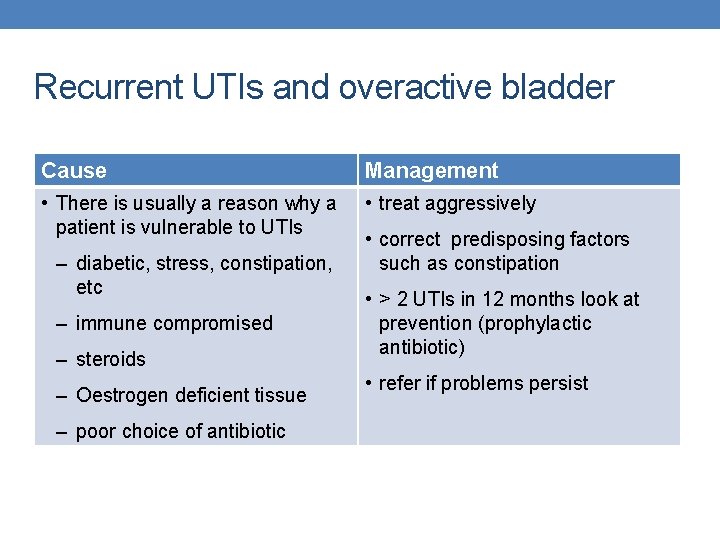
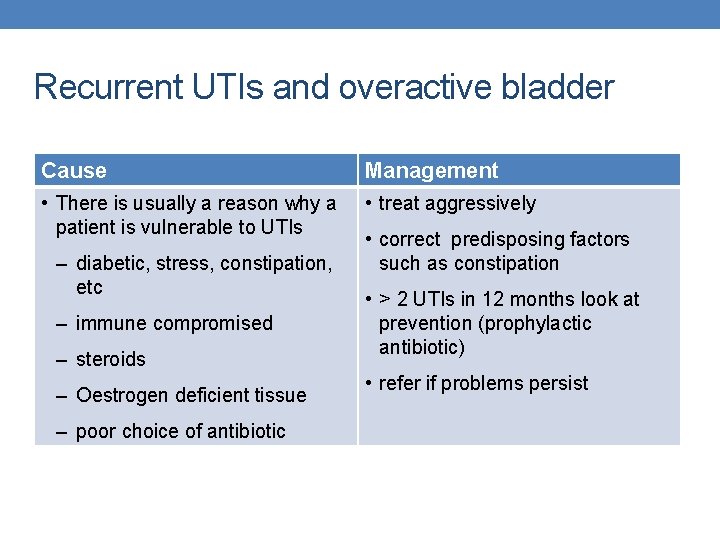
Recurrent UTIs and overactive bladder Cause Management • There is usually a reason why a patient is vulnerable to UTIs • treat aggressively – diabetic, stress, constipation, etc – immune compromised – steroids – Oestrogen deficient tissue – poor choice of antibiotic • correct predisposing factors such as constipation • > 2 UTIs in 12 months look at prevention (prophylactic antibiotic) • refer if problems persist
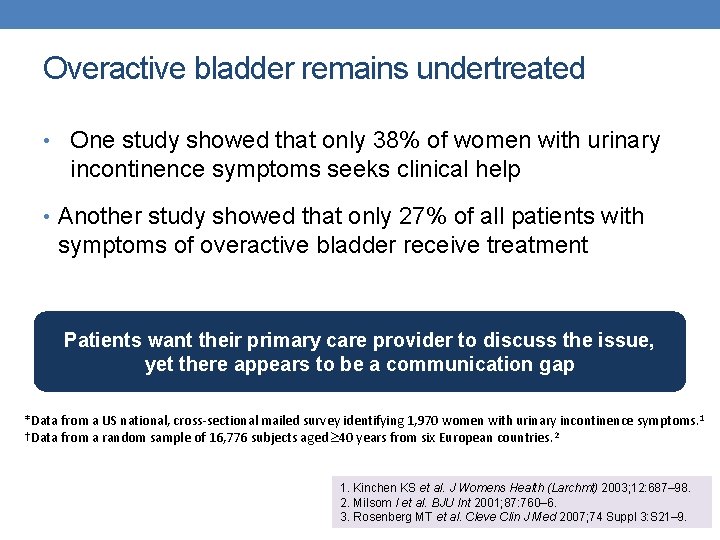
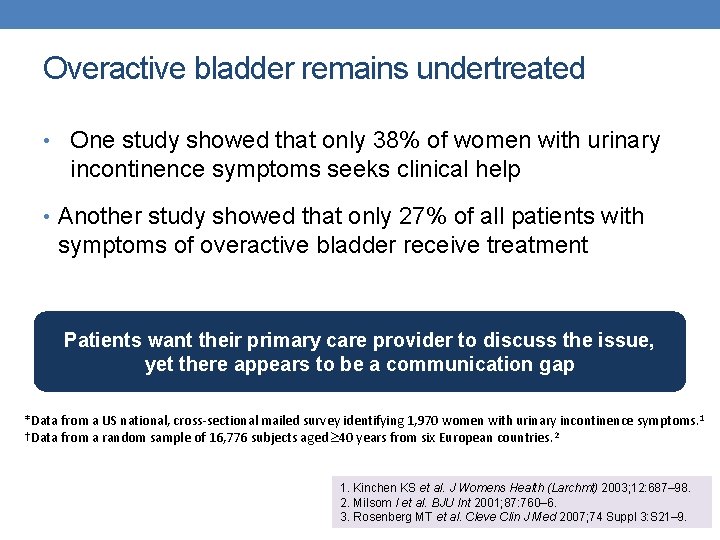
Overactive bladder remains undertreated • One study showed that only 38% of women with urinary incontinence symptoms seeks clinical help • Another study showed that only 27% of all patients with symptoms of overactive bladder receive treatment Patients want their primary care provider to discuss the issue, yet there appears to be a communication gap *Data from a US national, cross-sectional mailed survey identifying 1, 970 women with urinary incontinence symptoms. 1 †Data from a random sample of 16, 776 subjects aged 40 years from six European countries. 2 1. Kinchen KS et al. J Womens Health (Larchmt) 2003; 12: 687– 98. 2. Milsom I et al. BJU Int 2001; 87: 760– 6. 3. Rosenberg MT et al. Cleve Clin J Med 2007; 74 Suppl 3: S 21– 9.
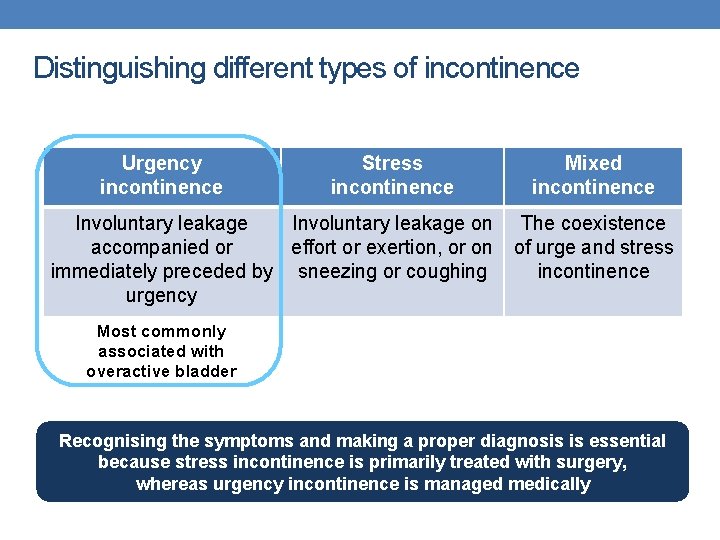
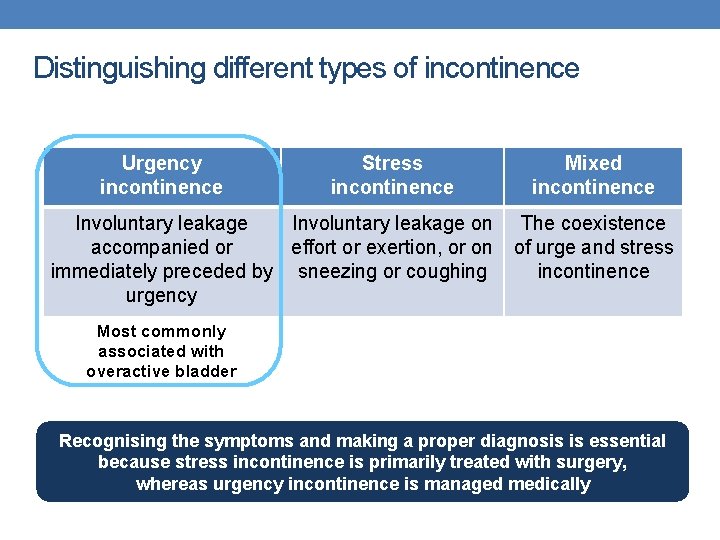
Distinguishing different types of incontinence Urgency incontinence Stress incontinence Involuntary leakage on accompanied or effort or exertion, or on immediately preceded by sneezing or coughing urgency Mixed incontinence The coexistence of urge and stress incontinence Most commonly associated with overactive bladder Recognising the symptoms and making a proper diagnosis is essential because stress incontinence is primarily treated with surgery, whereas urgency incontinence is managed medically
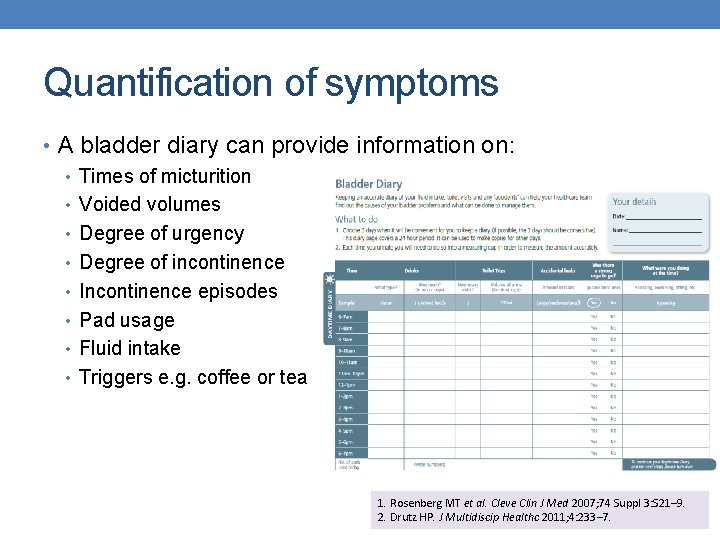
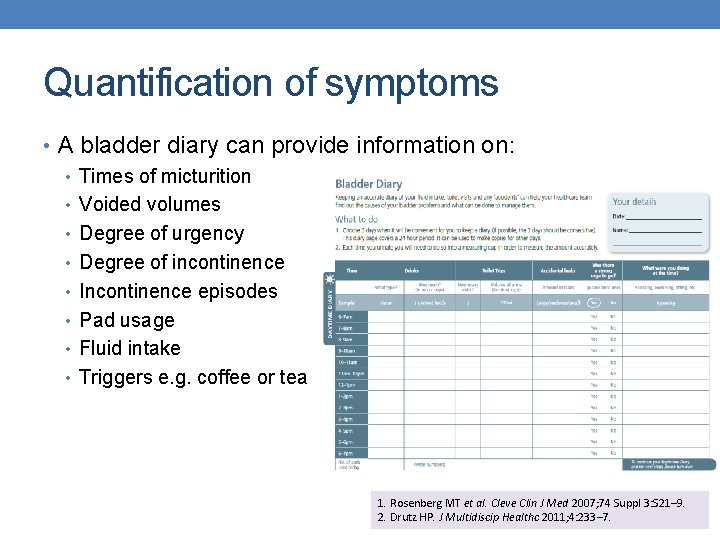
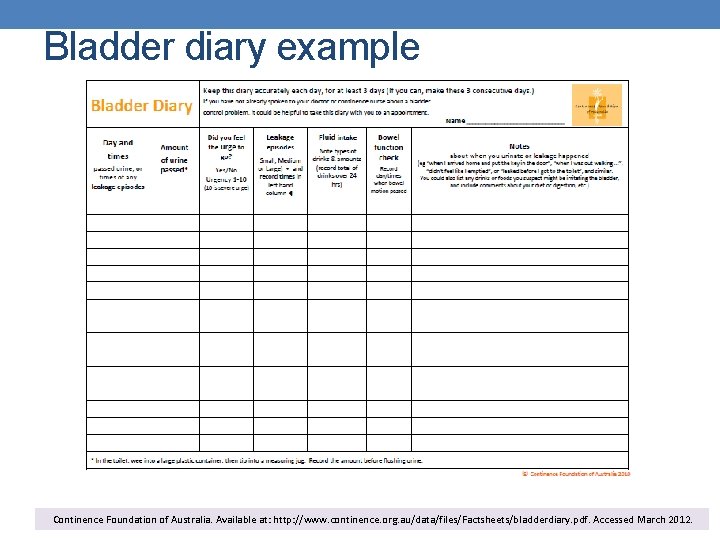
Quantification of symptoms • A bladder diary can provide information on: • Times of micturition • Voided volumes • Degree of urgency • Degree of incontinence • Incontinence episodes • Pad usage • Fluid intake • Triggers e. g. coffee or tea 1. Rosenberg MT et al. Cleve Clin J Med 2007; 74 Suppl 3: S 21– 9. 2. Drutz HP. J Multidiscip Healthc 2011; 4: 233– 7.
MANAGEMENT -OAB
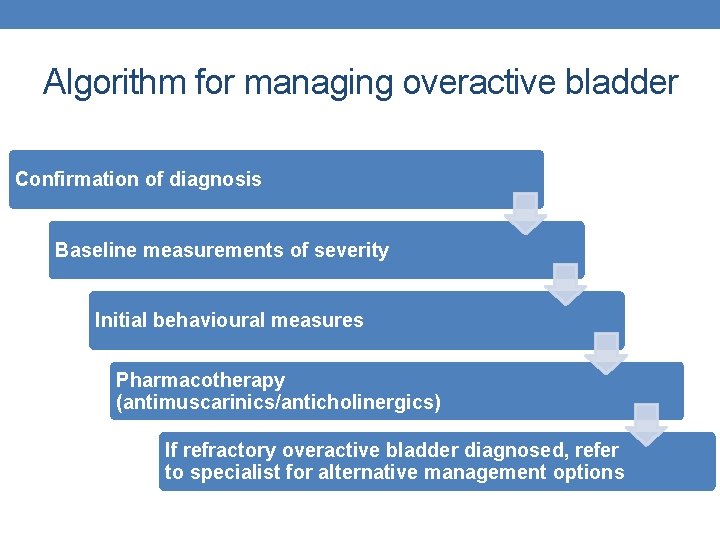
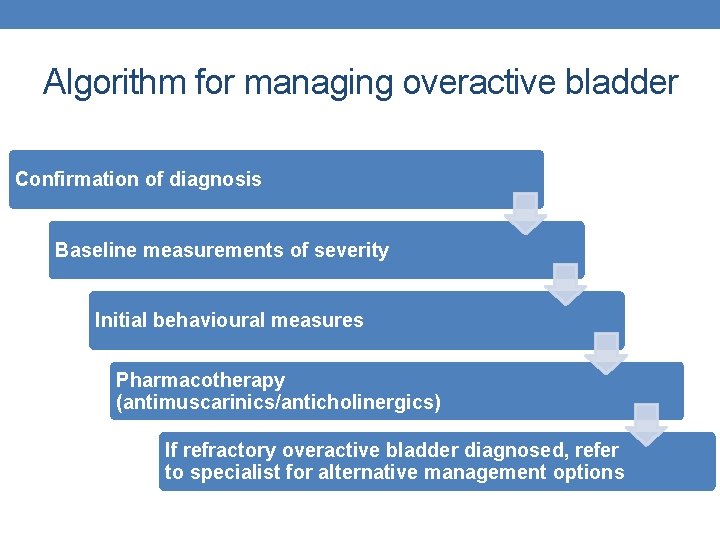
Algorithm for managing overactive bladder Confirmation of diagnosis Baseline measurements of severity Initial behavioural measures Pharmacotherapy (antimuscarinics/anticholinergics) If refractory overactive bladder diagnosed, refer to specialist for alternative management options
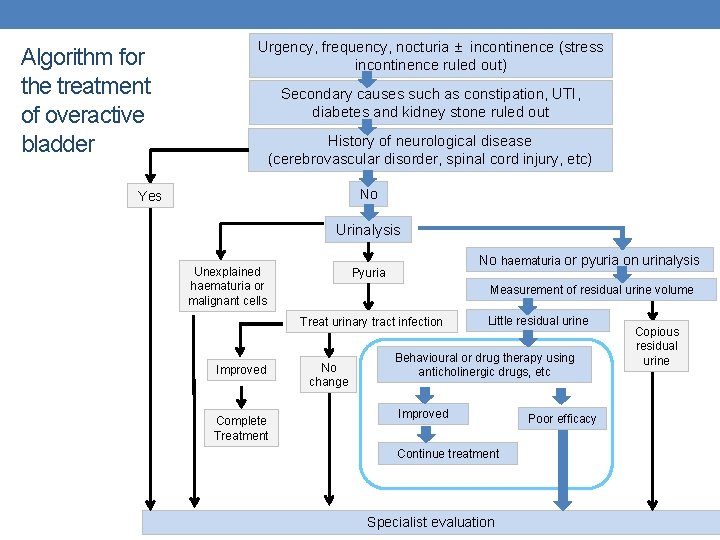
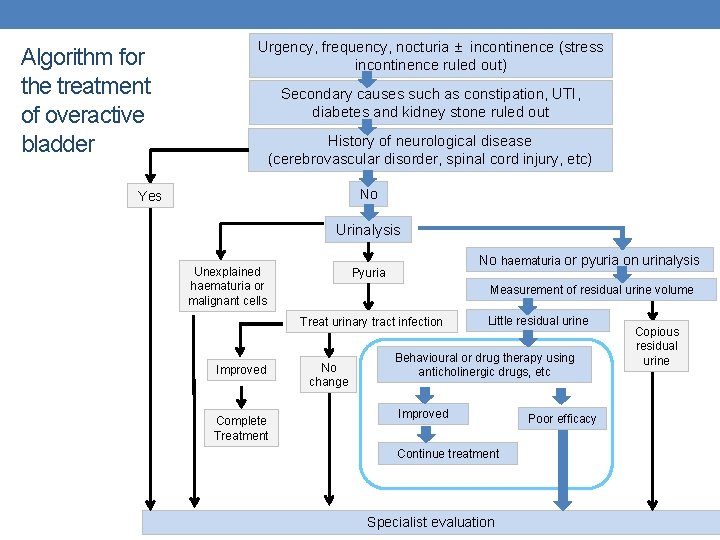
Algorithm for the treatment of overactive bladder Urgency, frequency, nocturia ± incontinence (stress incontinence ruled out) Secondary causes such as constipation, UTI, diabetes and kidney stone ruled out History of neurological disease (cerebrovascular disorder, spinal cord injury, etc) No Yes Urinalysis Unexplained haematuria or malignant cells No haematuria or pyuria on urinalysis Pyuria Measurement of residual urine volume Treat urinary tract infection Improved Complete Treatment No change Little residual urine Behavioural or drug therapy using anticholinergic drugs, etc Improved Continue treatment Specialist evaluation Poor efficacy Copious residual urine
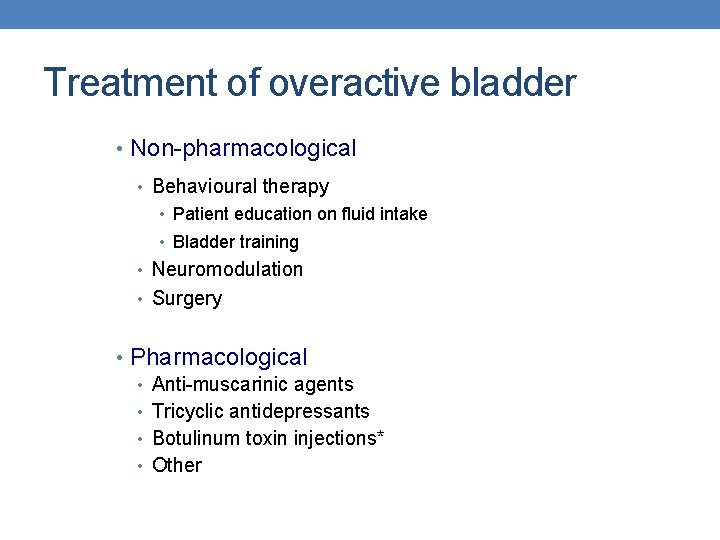
Treatment of overactive bladder • Non-pharmacological • Behavioural therapy • Patient education on fluid intake • Bladder training • Neuromodulation • Surgery • Pharmacological • Anti-muscarinic agents • Tricyclic antidepressants • Botulinum toxin injections* • Other
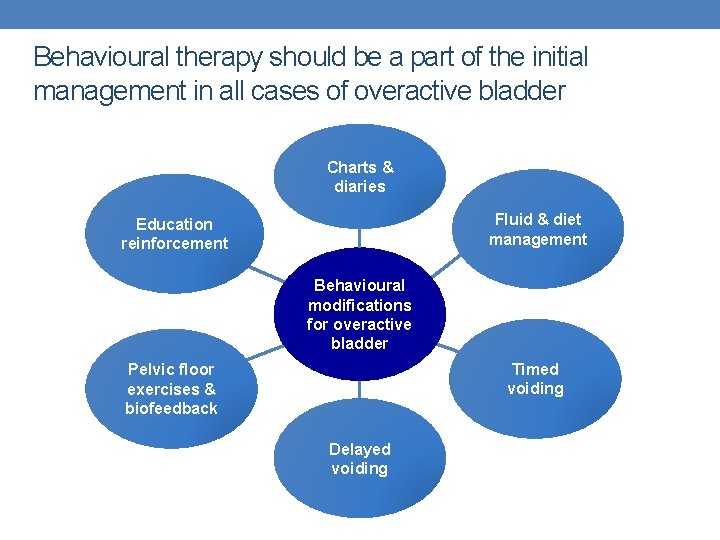
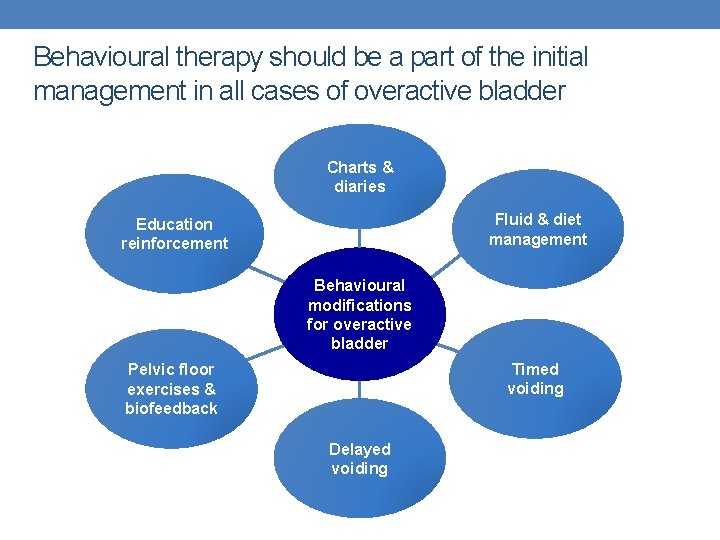
Behavioural therapy should be a part of the initial management in all cases of overactive bladder Charts & diaries Fluid & diet management Education reinforcement Behavioural modifications for overactive bladder Timed voiding Pelvic floor exercises & biofeedback Delayed voiding
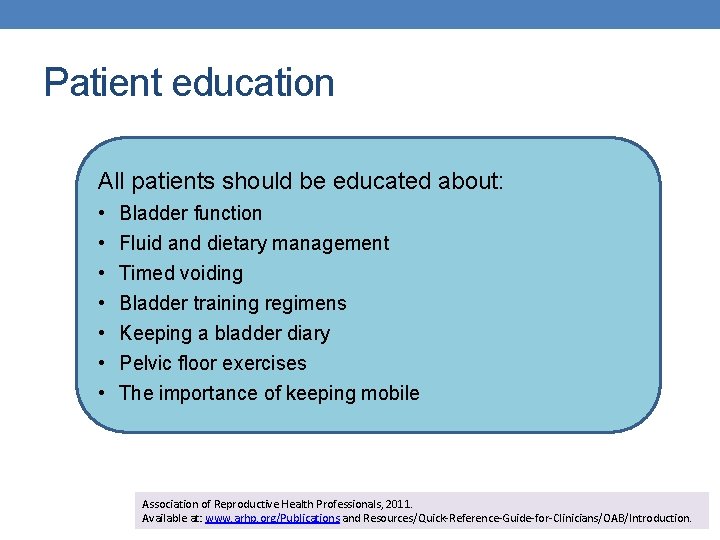
Patient education All patients should be educated about: • • Bladder function Fluid and dietary management Timed voiding Bladder training regimens Keeping a bladder diary Pelvic floor exercises The importance of keeping mobile Association of Reproductive Health Professionals, 2011. Available at: www. arhp. org/Publications and Resources/Quick-Reference-Guide-for-Clinicians/OAB/Introduction.
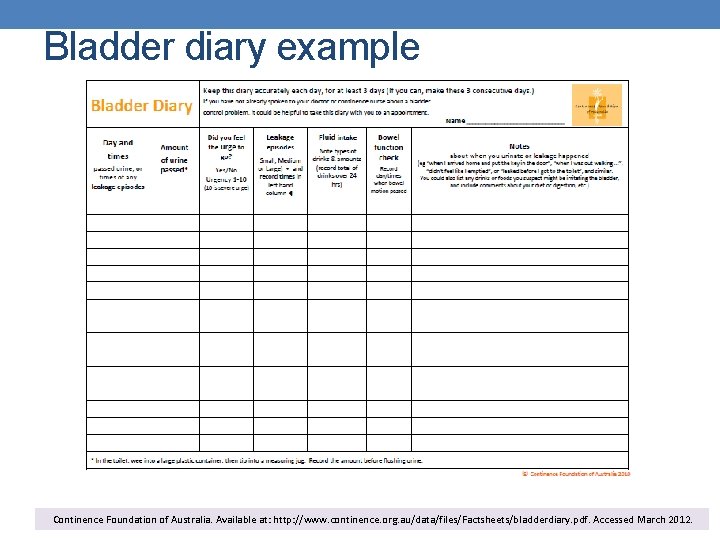
Bladder diary example Continence Foundation of Australia. Available at: http: //www. continence. org. au/data/files/Factsheets/bladderdiary. pdf. Accessed March 2012.
Reviewing lifestyle changes as part of a bladder training program • Reduce or cease intake of caffeine, alcohol and sweet drinks • Manage constipation • Only go to the toilet when needed (i. e. don’t go “just-in-case”) • Drink ~1. 5 L of fluid per day (mostly water) • Aim to regularly pass 300 ml or more of urine • Exercise pelvic floor muscles • Maintain a healthy weight
PHARMACOLOGICAL MX Anti-Muscarinics Beta-3 Agonist
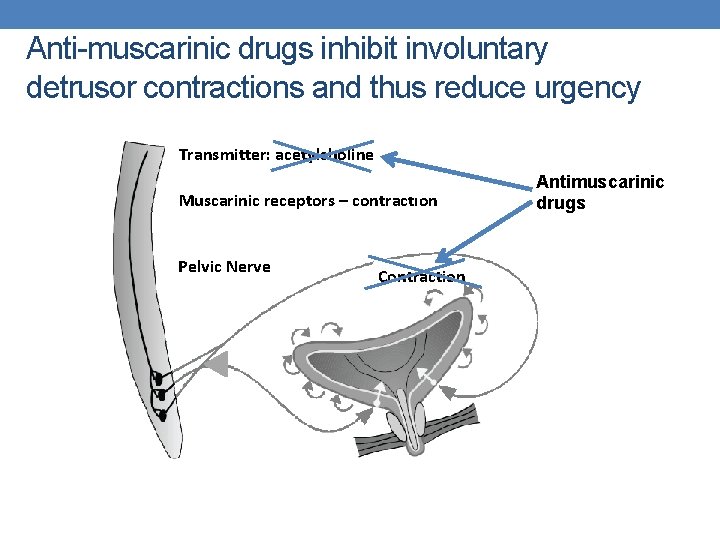
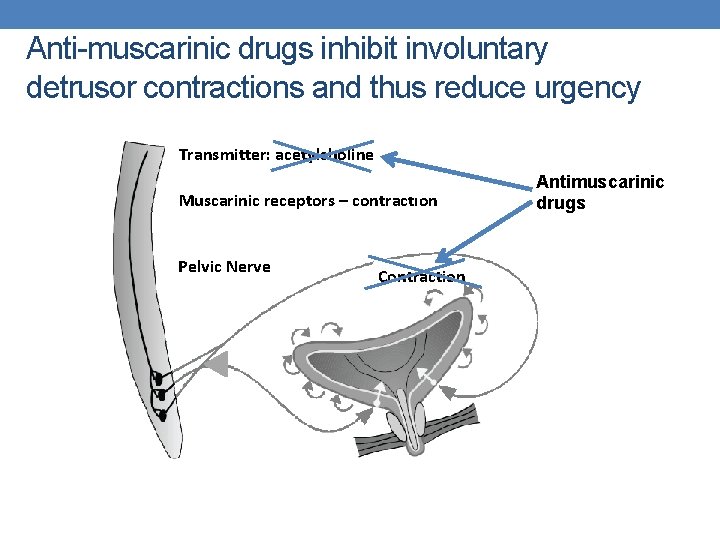
Anti-muscarinic drugs inhibit involuntary detrusor contractions and thus reduce urgency Transmitter: acetylcholine Muscarinic receptors – contraction Pelvic Nerve Contraction Antimuscarinic drugs
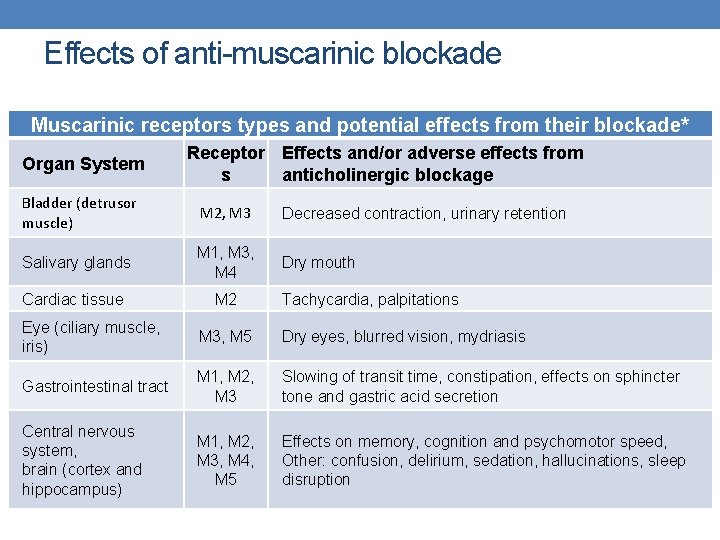
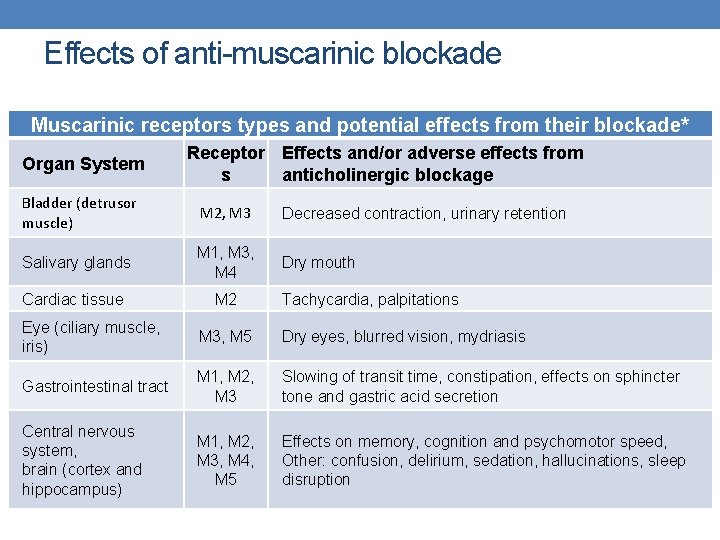
Effects of anti-muscarinic blockade Muscarinic receptors types and potential effects from their blockade* Organ System Receptor Effects and/or adverse effects from s anticholinergic blockage Bladder (detrusor muscle) M 2, M 3 Decreased contraction, urinary retention Salivary glands M 1, M 3, M 4 Dry mouth Cardiac tissue M 2 Tachycardia, palpitations Eye (ciliary muscle, iris) M 3, M 5 Dry eyes, blurred vision, mydriasis Gastrointestinal tract M 1, M 2, M 3 Slowing of transit time, constipation, effects on sphincter tone and gastric acid secretion Central nervous system, brain (cortex and hippocampus) M 1, M 2, M 3, M 4, M 5 Effects on memory, cognition and psychomotor speed, Other: confusion, delirium, sedation, hallucinations, sleep disruption
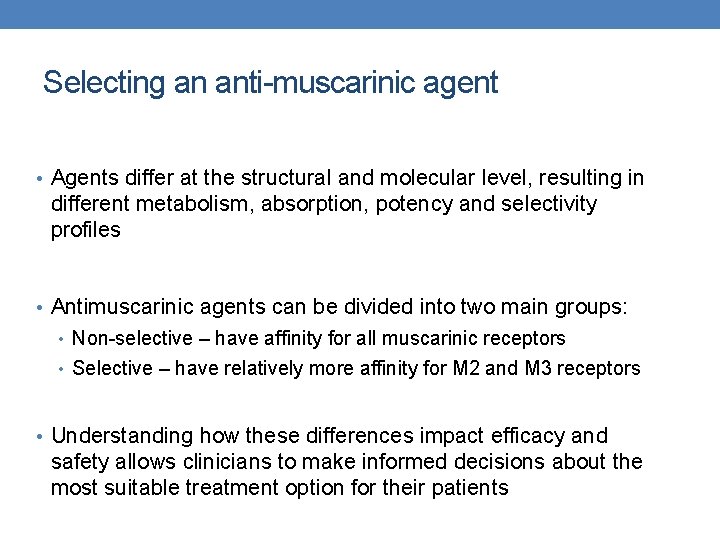
Selecting an anti-muscarinic agent • Agents differ at the structural and molecular level, resulting in different metabolism, absorption, potency and selectivity profiles • Antimuscarinic agents can be divided into two main groups: • Non-selective – have affinity for all muscarinic receptors • Selective – have relatively more affinity for M 2 and M 3 receptors • Understanding how these differences impact efficacy and safety allows clinicians to make informed decisions about the most suitable treatment option for their patients
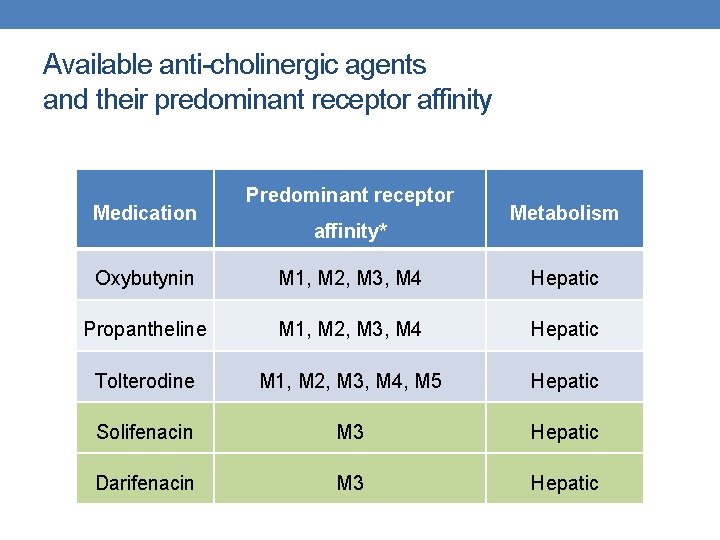
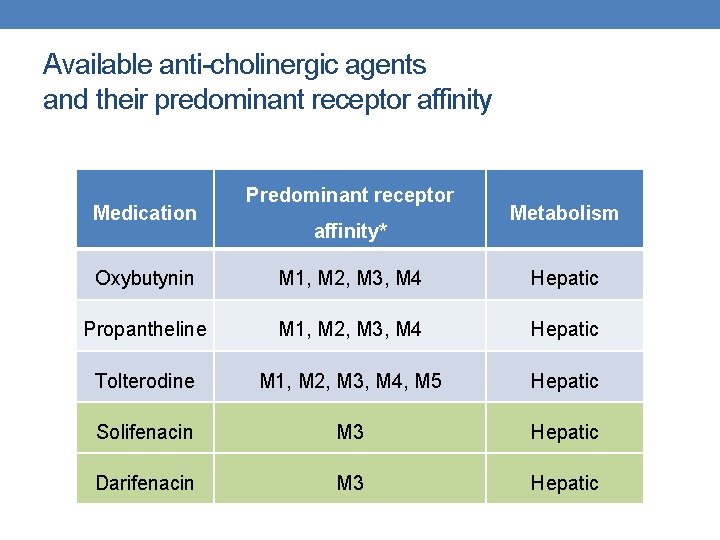
Available anti-cholinergic agents and their predominant receptor affinity Medication Predominant receptor affinity* Metabolism Oxybutynin M 1, M 2, M 3, M 4 Hepatic Propantheline M 1, M 2, M 3, M 4 Hepatic Tolterodine M 1, M 2, M 3, M 4, M 5 Hepatic Solifenacin M 3 Hepatic Darifenacin M 3 Hepatic
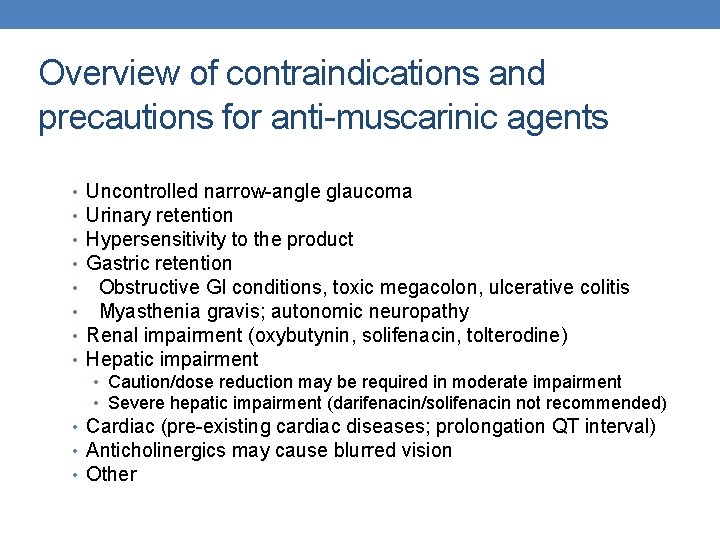
Overview of contraindications and precautions for anti-muscarinic agents • • Uncontrolled narrow-angle glaucoma Urinary retention Hypersensitivity to the product Gastric retention Obstructive GI conditions, toxic megacolon, ulcerative colitis Myasthenia gravis; autonomic neuropathy Renal impairment (oxybutynin, solifenacin, tolterodine) Hepatic impairment • Caution/dose reduction may be required in moderate impairment • Severe hepatic impairment (darifenacin/solifenacin not recommended) • Cardiac (pre-existing cardiac diseases; prolongation QT interval) • Anticholinergics may cause blurred vision • Other
BETA 3 AGONIST Mirabegron
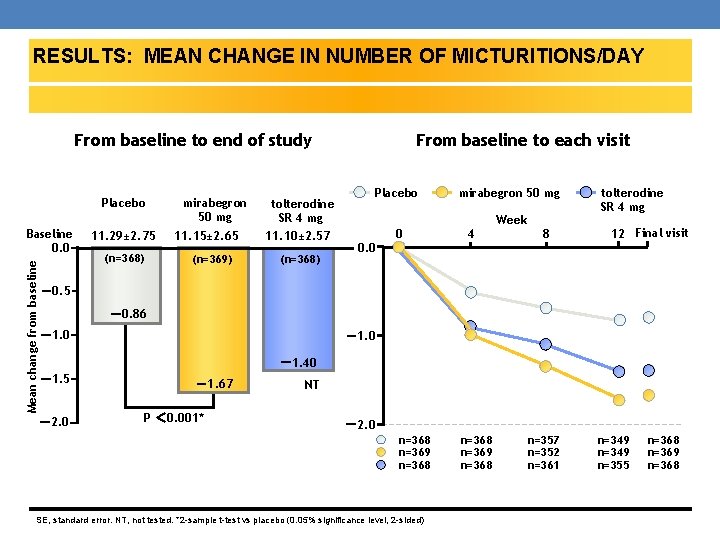
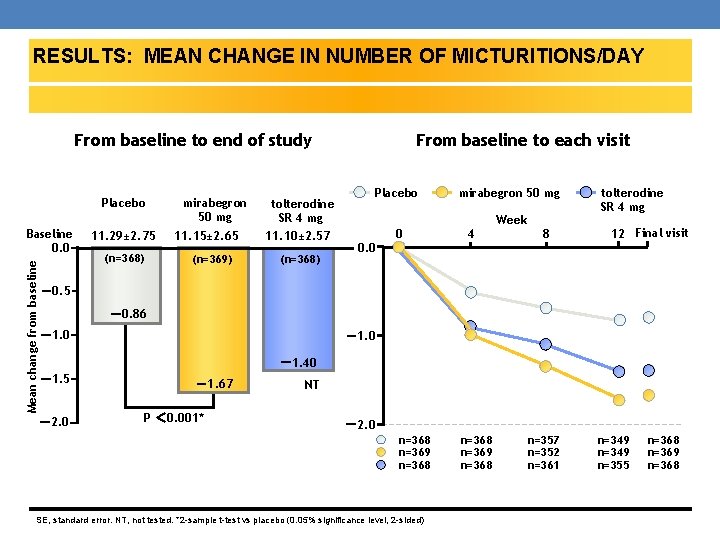
RESULTS: MEAN CHANGE IN NUMBER OF MICTURITIONS/DAY RESULTS: PRIMARY ENDPOINTS From baseline to end of study Placebo Mean change from baseline Baseline 0. 0 11. 29± 2. 75 (n=368) mirabegron 50 mg 11. 15± 2. 65 (n=369) tolterodine SR 4 mg 11. 10± 2. 57 (n=368) From baseline to each visit Placebo mirabegron 50 mg Week 0. 0 0 4 8 tolterodine SR 4 mg 12 Final visit -0. 5 -0. 86 -1. 0 -1. 40 -1. 5 -2. 0 -1. 67 P < 0. 001* NT -2. 0 n=368 n=369 n=368 SE, standard error. NT, not tested. *2 -sample t-test vs placebo (0. 05% significance level, 2 -sided) n=368 n=369 n=368 n=357 n=352 n=361 n=349 n=355 n=368 n=369 n=368
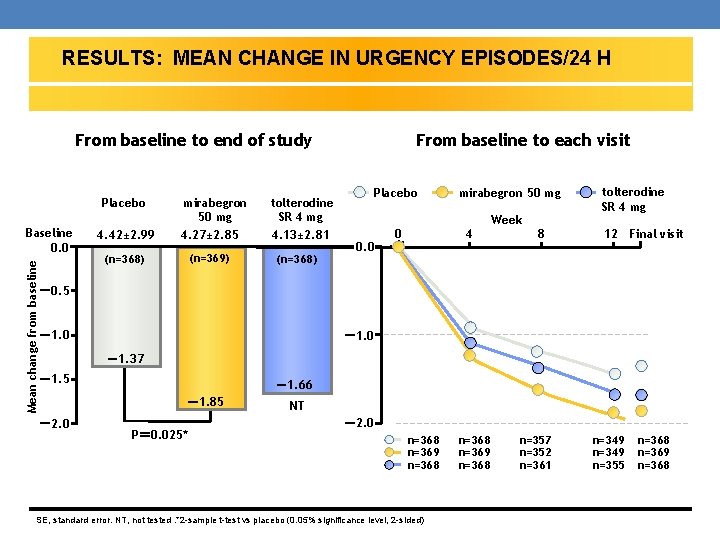
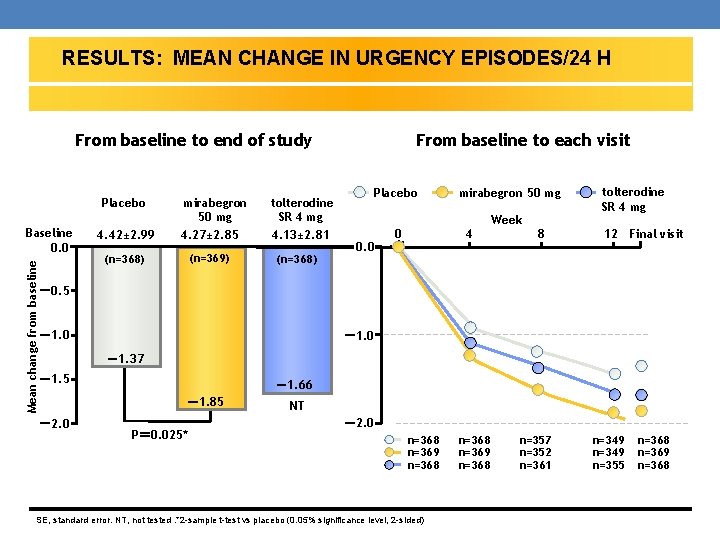
RESULTS: MEAN CHANGE IN URGENCY EPISODES/24 H From baseline to end of study Placebo Mean change from baseline Baseline 0. 0 4. 42± 2. 99 mirabegron 50 mg 4. 27± 2. 85 (n=369) (n=368) tolterodine SR 4 mg 4. 13± 2. 81 (n=368) From baseline to each visit Placebo mirabegron 50 mg Week 0. 0 0 4 8 tolterodine SR 4 mg 12 Final visit -0. 5 -1. 0 -1. 37 -1. 5 -1. 66 -1. 85 -2. 0 P= 0. 025* NT -2. 0 n=368 n=369 n=368 SE, standard error. NT, not tested. *2 -sample t-test vs placebo (0. 05% significance level, 2 -sided) n=368 n=369 n=368 n=357 n=352 n=361 n=349 n=355 n=368 n=369 n=368
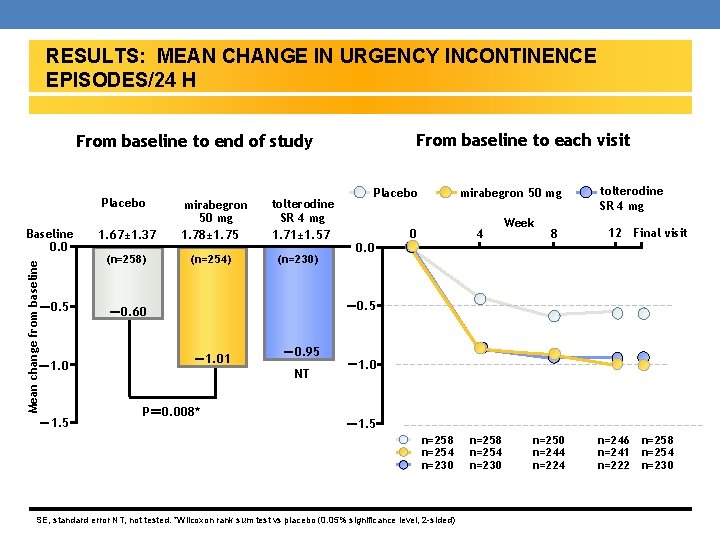
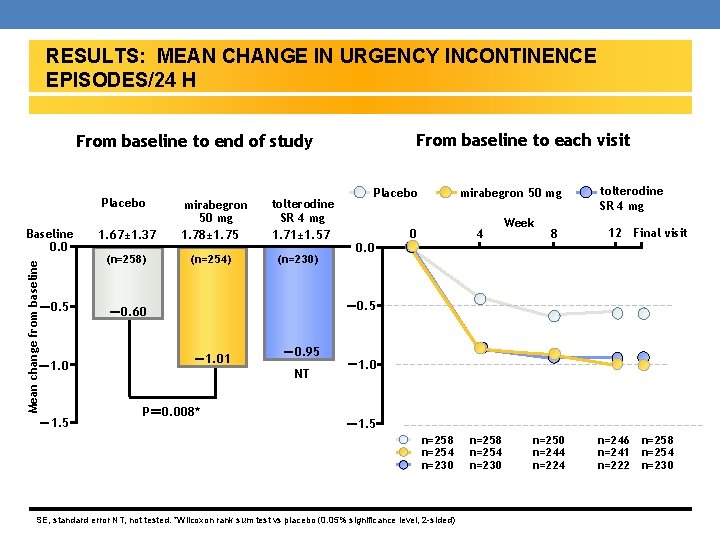
RESULTS: MEAN CHANGE IN URGENCY INCONTINENCE EPISODES/24 H From baseline to each visit From baseline to end of study Placebo Mean change from baseline Baseline 0. 0 -0. 5 -1. 0 -1. 5 1. 67± 1. 37 mirabegron 50 mg 1. 78± 1. 75 (n=258) (n=254) tolterodine SR 4 mg 1. 71± 1. 57 (n=230) Placebo 0. 0 mirabegron 50 mg 0 4 Week 8 tolterodine SR 4 mg 12 Final visit -0. 5 -0. 60 -1. 01 -0. 95 NT P= 0. 008* -1. 0 -1. 5 n=258 n=254 n=230 SE, standard error NT, not tested. *Wilcoxon rank sum test vs placebo (0. 05% significance level, 2 -sided) n=258 n=254 n=230 n=250 n=244 n=224 n=246 n=241 n=222 n=258 n=254 n=230
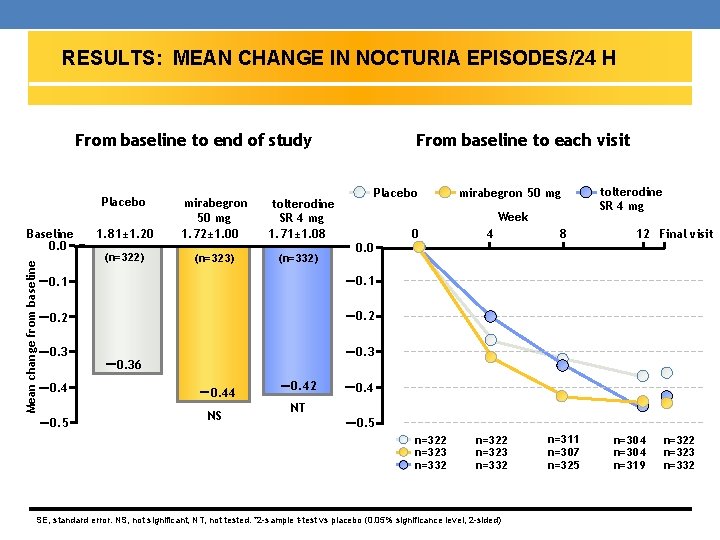
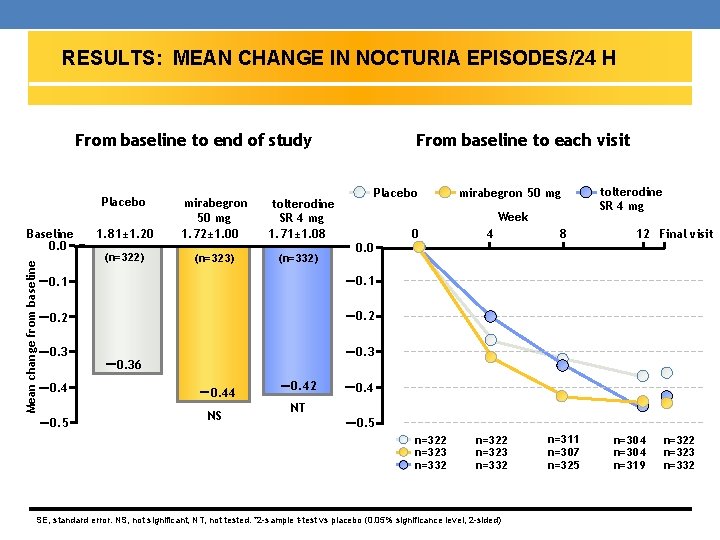
RESULTS: MEAN CHANGE IN NOCTURIA EPISODES/24 H From baseline to end of study Placebo Mean change from baseline Baseline 0. 0 1. 81± 1. 20 mirabegron 50 mg 1. 72± 1. 00 tolterodine SR 4 mg 1. 71± 1. 08 (n=322) (n=323) (n=332) From baseline to each visit Placebo mirabegron 50 mg Week 0. 0 -0. 1 -0. 2 0 4 8 n=322 n=323 n=332 n=311 n=307 n=325 tolterodine SR 4 mg 12 Final visit -0. 36 -0. 4 -0. 5 -0. 44 NS -0. 42 -0. 4 NT -0. 5 n=322 n=323 n=332 SE, standard error. NS, not significant, NT, not tested. *2 -sample t-test vs placebo (0. 05% significance level, 2 -sided) n=304 n=319 n=322 n=323 n=332
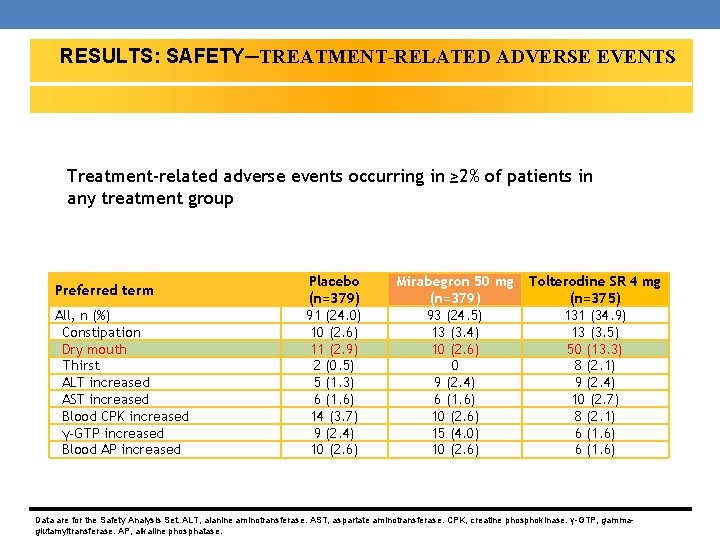
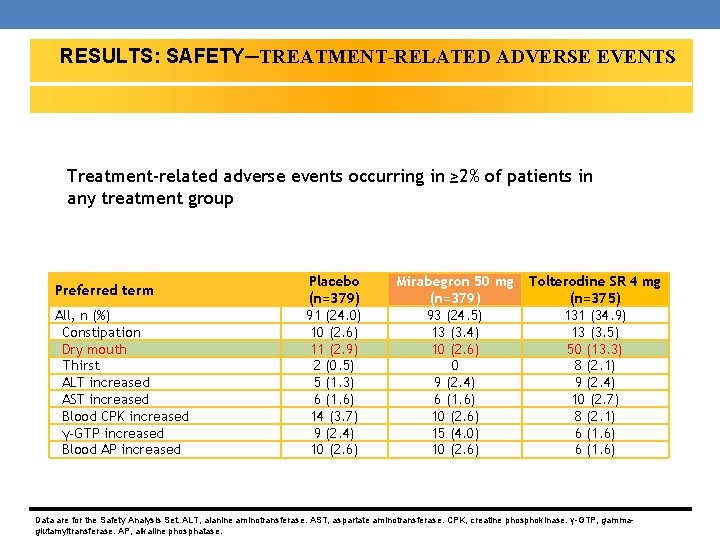
RESULTS: SAFETY─TREATMENT-RELATED ADVERSE EVENTS Treatment-related adverse events occurring in ≥ 2% of patients in any treatment group Preferred term All, n (%) Constipation Dry mouth Thirst ALT increased AST increased Blood CPK increased γ-GTP increased Blood AP increased Placebo (n=379) 91 (24. 0) 10 (2. 6) 11 (2. 9) 2 (0. 5) 5 (1. 3) 6 (1. 6) 14 (3. 7) 9 (2. 4) 10 (2. 6) Mirabegron 50 mg (n=379) 93 (24. 5) 13 (3. 4) 10 (2. 6) 0 9 (2. 4) 6 (1. 6) 10 (2. 6) 15 (4. 0) 10 (2. 6) Tolterodine SR 4 mg (n=375) 131 (34. 9) 13 (3. 5) 50 (13. 3) 8 (2. 1) 9 (2. 4) 10 (2. 7) 8 (2. 1) 6 (1. 6) Data are for the Safety Analysis Set. ALT, alanine aminotransferase. AST, aspartate aminotransferase. CPK, creatine phosphokinase. γ-GTP, gammaglutamyltransferase. AP, alkaline phosphatase.
OTHER …
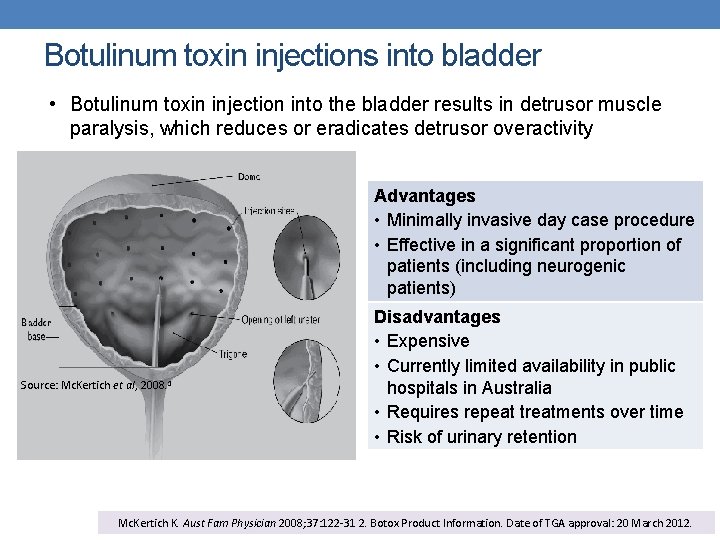
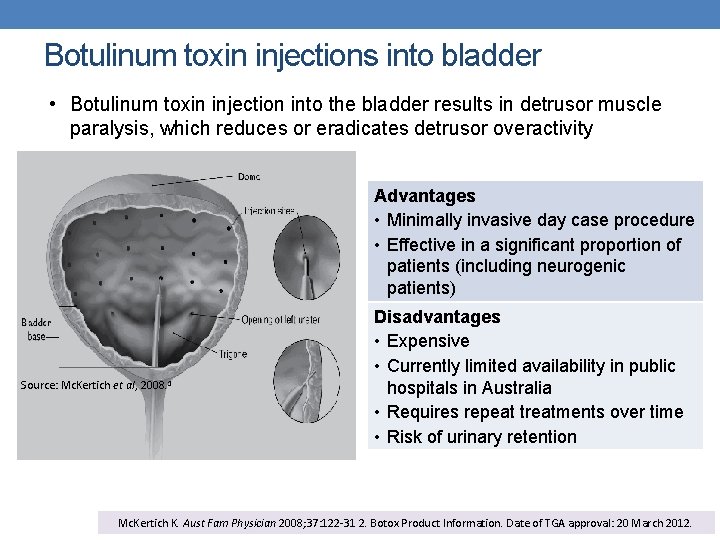
Botulinum toxin injections into bladder • Botulinum toxin injection into the bladder results in detrusor muscle paralysis, which reduces or eradicates detrusor overactivity Advantages • Minimally invasive day case procedure • Effective in a significant proportion of patients (including neurogenic patients) Source: Mc. Kertich et al, 2008. 1 Disadvantages • Expensive • Currently limited availability in public hospitals in Australia • Requires repeat treatments over time • Risk of urinary retention Mc. Kertich K. Aust Fam Physician 2008; 37: 122 -31 2. Botox Product Information. Date of TGA approval: 20 March 2012.
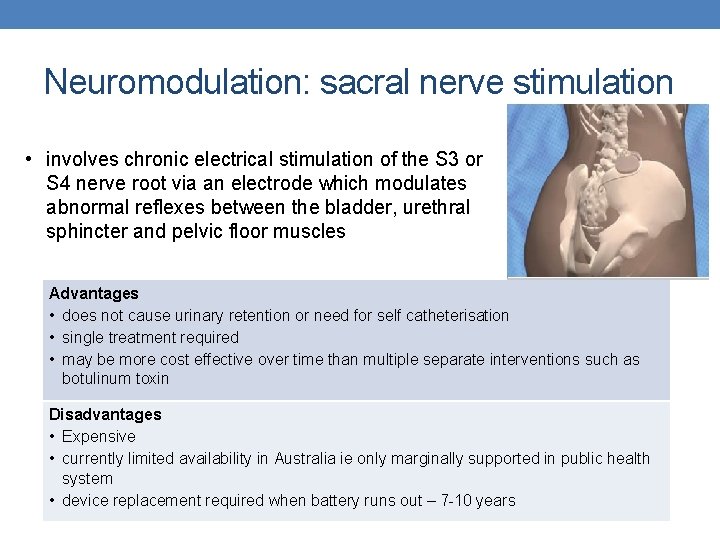
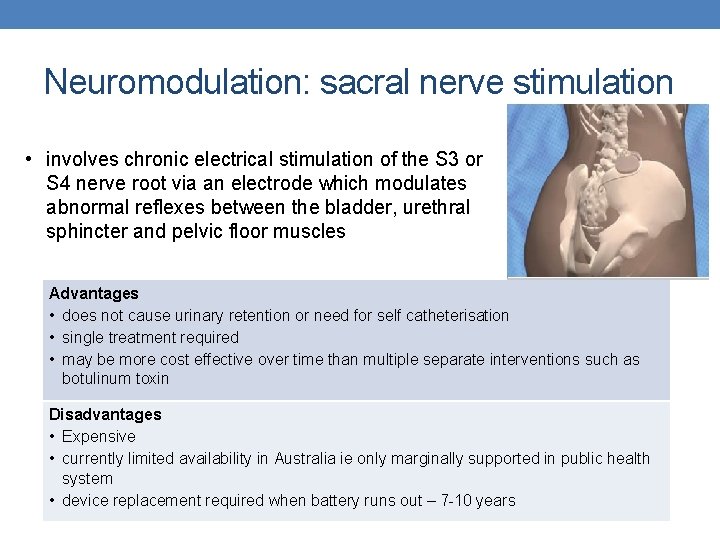
Neuromodulation: sacral nerve stimulation • involves chronic electrical stimulation of the S 3 or S 4 nerve root via an electrode which modulates abnormal reflexes between the bladder, urethral sphincter and pelvic floor muscles Advantages • does not cause urinary retention or need for self catheterisation • single treatment required • may be more cost effective over time than multiple separate interventions such as botulinum toxin Disadvantages • Expensive • currently limited availability in Australia ie only marginally supported in public health system • device replacement required when battery runs out – 7 -10 years
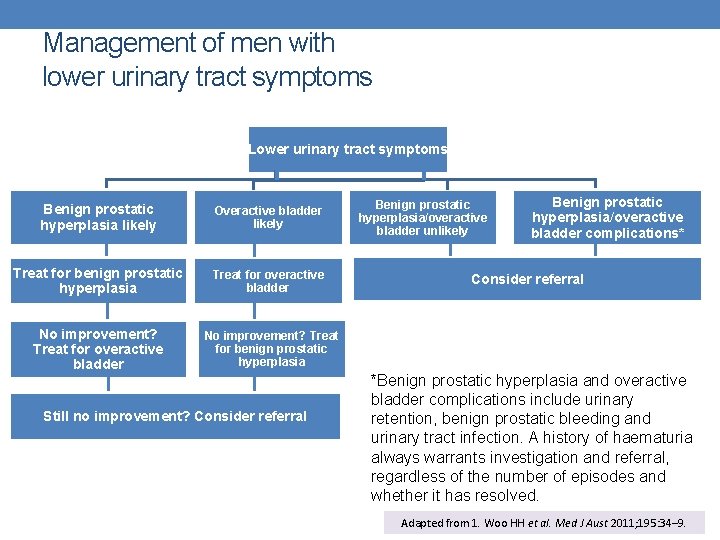
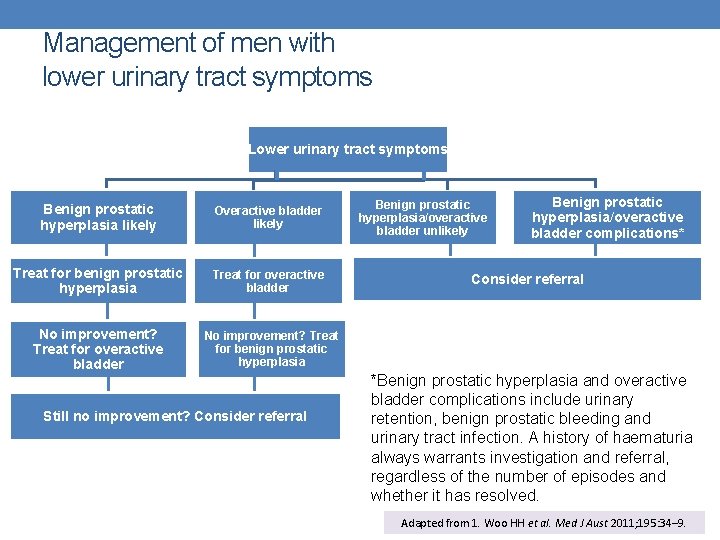
Management of men with lower urinary tract symptoms Lower urinary tract symptoms Benign prostatic hyperplasia likely Overactive bladder likely Treat for benign prostatic hyperplasia Treat for overactive bladder No improvement? Treat for benign prostatic hyperplasia Still no improvement? Consider referral Benign prostatic hyperplasia/overactive bladder unlikely Benign prostatic hyperplasia/overactive bladder complications* Consider referral *Benign prostatic hyperplasia and overactive bladder complications include urinary retention, benign prostatic bleeding and urinary tract infection. A history of haematuria always warrants investigation and referral, regardless of the number of episodes and whether it has resolved. Adapted from 1. Woo HH et al. Med J Aust 2011; 195: 34– 9.
NOCTURIA


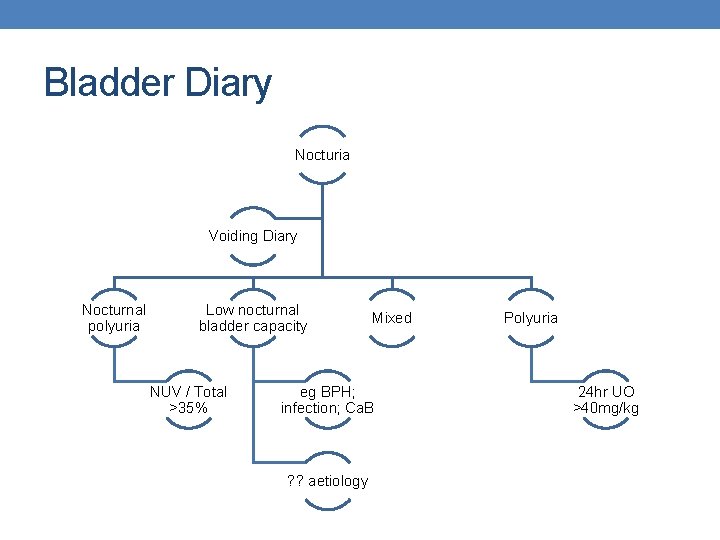
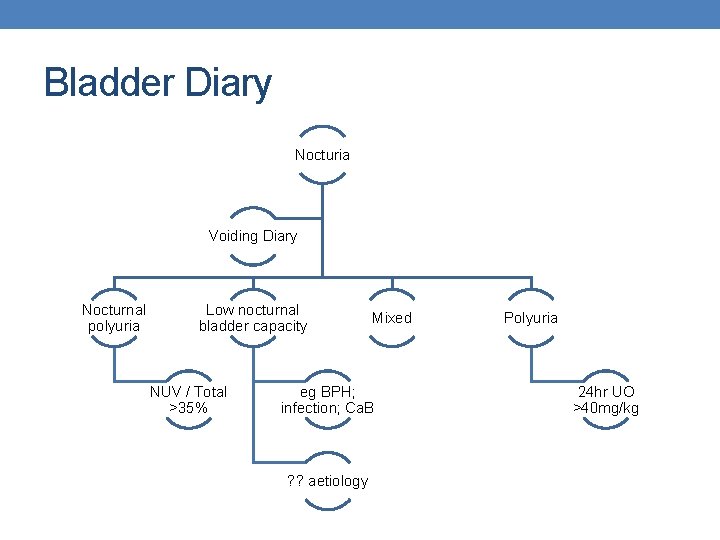
Bladder Diary Nocturia Voiding Diary Nocturnal polyuria Low nocturnal bladder capacity NUV / Total >35% Mixed eg BPH; infection; Ca. B ? ? aetiology Polyuria 24 hr UO >40 mg/kg
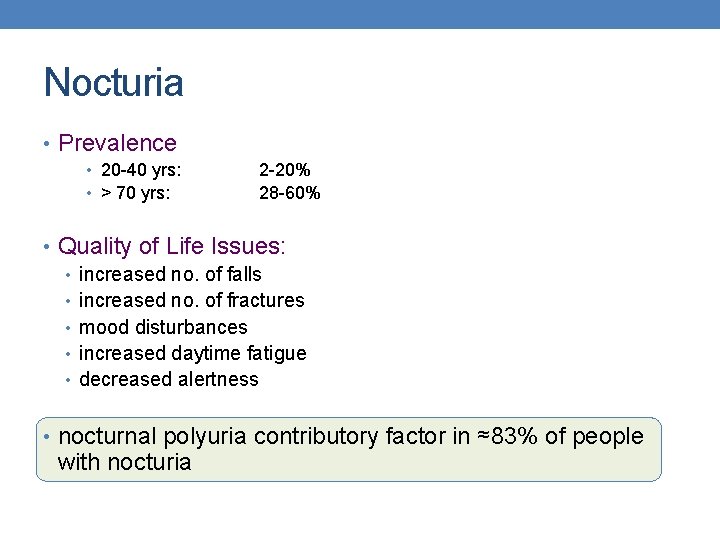
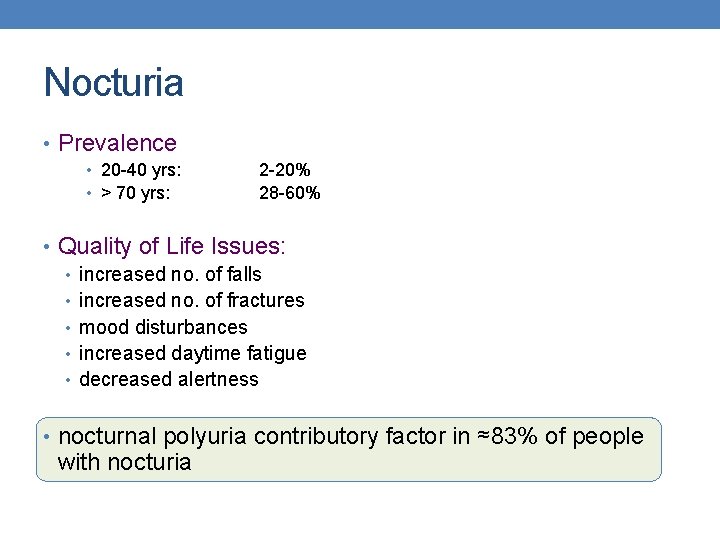
Nocturia • Prevalence • 20 -40 yrs: • > 70 yrs: 2 -20% 28 -60% • Quality of Life Issues: • increased no. of falls • increased no. of fractures • mood disturbances • increased daytime fatigue • decreased alertness • nocturnal polyuria contributory factor in ≈83% of people with nocturia
Investigations • Bladder diary • Ultrasound • Urinary tract • MSU • Cystoscopy • exclude local pathology • not every patient
Management Strategy • attempt to categorise patient • review bladder diary • review medications • consider intake • caffeine • alcohol • treat ancillary conditions: • CCF • sleep apnoea • UTI • BPH
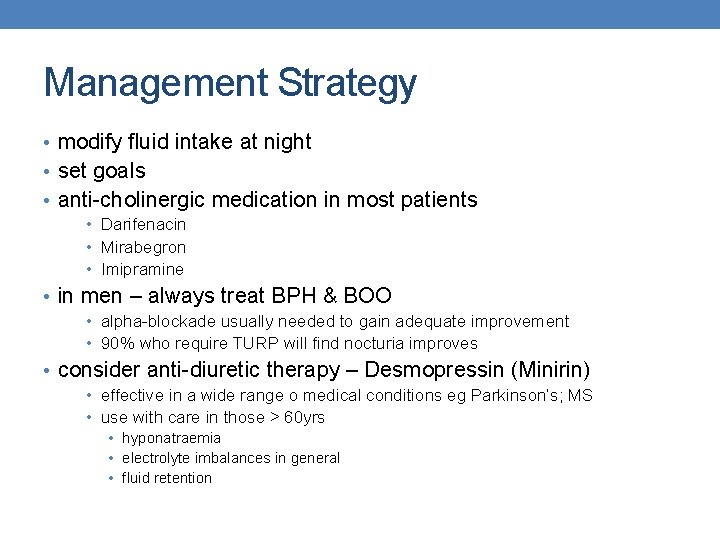
Management Strategy • modify fluid intake at night • set goals • anti-cholinergic medication in most patients • Darifenacin • Mirabegron • Imipramine • in men – always treat BPH & BOO • alpha-blockade usually needed to gain adequate improvement • 90% who require TURP will find nocturia improves • consider anti-diuretic therapy – Desmopressin (Minirin) • effective in a wide range o medical conditions eg Parkinson’s; MS • use with care in those > 60 yrs • hyponatraemia • electrolyte imbalances in general • fluid retention
RECURRENT UTI’S
UTI’s • most common human bacterial infection • result in significant: • hospitalisation • sepsis • morbidity • divided into 2 categories: • upper tract (U/T) • lower tract (L/T)
Recurrent UTI’s (r. UTI) • Definition: • 3 separate UTIs in a 12 month period • 2 separate UTI’s in a 6 month period • Persistent: • Recurrence of same bacterial UTI in ≤ 2 weeks • Criteria: • different bacteria • negative MSU between infections • more than 2 weeks between symptoms
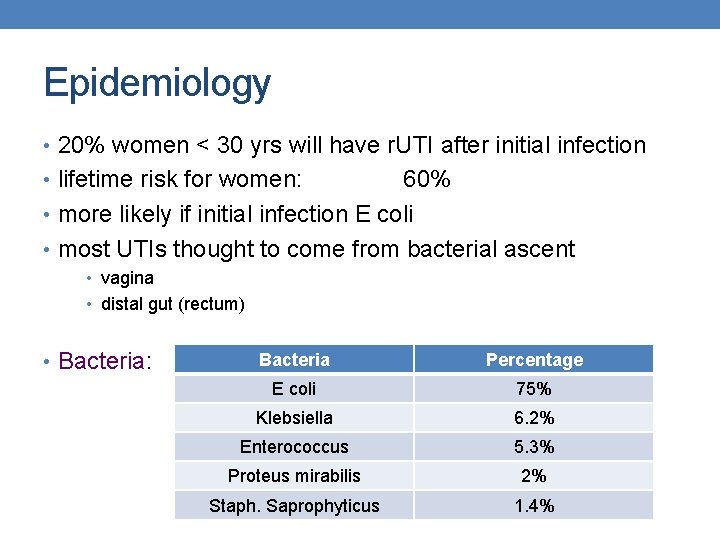
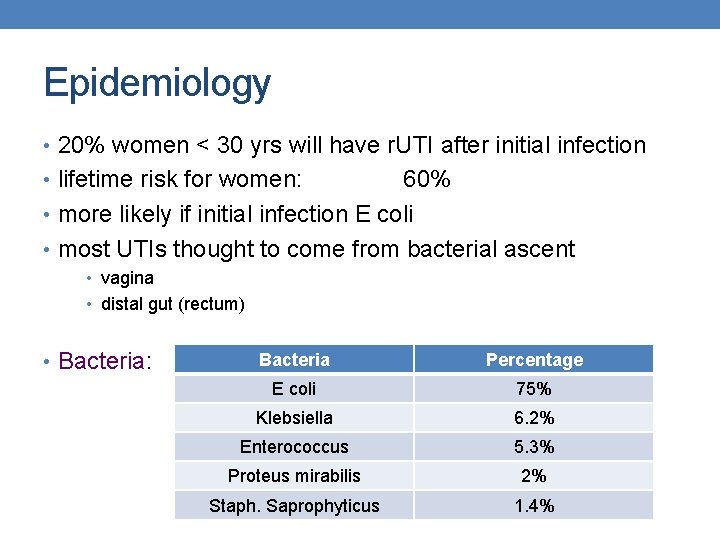
Epidemiology • 20% women < 30 yrs will have r. UTI after initial infection • lifetime risk for women: 60% • more likely if initial infection E coli • most UTIs thought to come from bacterial ascent • vagina • distal gut (rectum) • Bacteria: Bacteria Percentage E coli 75% Klebsiella 6. 2% Enterococcus 5. 3% Proteus mirabilis 2% Staph. Saprophyticus 1. 4%
Risk Factors • Anatomical Variations • Age • distance from urethra to anus • incontinence • distance from posterior • cystocoele fourchette to anus • urethral length - NOT • post void residual • Genetic • FHx - strong +ve predictor • not sure of mechanism • Behavioural • sexual practises • use of spermicidials • use of barrier contraceptives • post-menopausal changes in vaginal lining • decreased lactobacilli • reduces acidic hostile environment for bacteria
Management Strategies • Evaluation: • exclude obvious anatomical possibilities • Eg: • cystocoele • urethral diverticulum • Skene’s glands • MSU – document • bacteria • number of +ve MSU’s over time period • Ultrasound • assess PVR • exclude other anatomical abnormalities
Prevention • Behavioural Modification: • revise sexual behaviour • change contraceptive • no spermicidals / barrier contraception • Hiprex • Metabolised to NH 3 & formaldehyde • 1 g bd • Taken with OJ or Ascorbic Acid • Prophylactic Antibiotics • Nitrofurantoin: • Trimethoprim: • Keflex: 50 mg nocte 300 mg nocte 250 mg nocte
Prevention • Cranberry • Proanthocyanodin • inhibits p-fimbriae binding to cell wall • tablets better than juice • avoids taste, acidity & calorie issues • Oestrogen Replacement • atrophic vaginal changes increase suscepability • topical oestrogen only • NO benefit to oral configuration
New Options - ? The Future • GAG Replenishment • • poor or defective GAG layer postulated in some women i. Alu. Ril – combination Hyaluronic acid & Chondroitin Series of instillations Bit expensive • Anti-adhesives: • prevention of Fim. H binding to highly mannosylated residues on bladder surface • D-Mannose – orally available can prevent this • More on the way • Probiotics / Essential Oils: • some evidence suggesting can help restore normal healthy flora to vagina • Vaccination • early trials
THANK YOU!
 White blood
White blood Kaupo voormansik
Kaupo voormansik Oab luts
Oab luts Coital incontinence
Coital incontinence Acfi assessment
Acfi assessment Acupuncture for incontinence
Acupuncture for incontinence Sacral reflex
Sacral reflex George washington vs king george iii venn diagram
George washington vs king george iii venn diagram George washington vs king george iii venn diagram
George washington vs king george iii venn diagram Cricothyroid muscle.
Cricothyroid muscle. Visualizing and understanding recurrent networks
Visualizing and understanding recurrent networks Termination of brachial artery
Termination of brachial artery Rima glottidis
Rima glottidis Lstm andrew ng
Lstm andrew ng Recurrent strokes
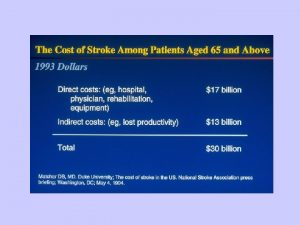
Recurrent strokes Recurrent stroke causes
Recurrent stroke causes Recurrent artery of huebner
Recurrent artery of huebner Extensions of recurrent neural network language model
Extensions of recurrent neural network language model Cs 7643 github
Cs 7643 github Visualizing and understanding recurrent networks
Visualizing and understanding recurrent networks Bert question generation
Bert question generation Pixelrnn
Pixelrnn Recurrent neural network based language model
Recurrent neural network based language model Lines positioned between horizontal and vertical
Lines positioned between horizontal and vertical Coarcotation
Coarcotation A recurrent image in a literary work is the
A recurrent image in a literary work is the Part 135 recurrent training
Part 135 recurrent training Abduction of larynx
Abduction of larynx Recurrent laryngeal nerve
Recurrent laryngeal nerve Recurrent connection
Recurrent connection Vestibule nasal
Vestibule nasal Foot arteries
Foot arteries Rolo object tracking
Rolo object tracking Simple recurrent network
Simple recurrent network How formal education differ from als
How formal education differ from als Difference between health promotion and health education
Difference between health promotion and health education Backbone of extension education
Backbone of extension education King george cousins family tree
King george cousins family tree George herbert mead i'' and me
George herbert mead i'' and me George royce uno
George royce uno Conway v george wimpey
Conway v george wimpey Bryant acar
Bryant acar Local vertical local horizontal frame
Local vertical local horizontal frame Peter hadley the veldt
Peter hadley the veldt George siscoe
George siscoe George w. mclaurin
George w. mclaurin Curious george smoking a pipe
Curious george smoking a pipe George mbti
George mbti Summary chapter 2 great gatsby
Summary chapter 2 great gatsby Pis cyprus
Pis cyprus Hoologanism
Hoologanism Alexander friedmann ve georges lemaitre
Alexander friedmann ve georges lemaitre Where is george
Where is george George washington bottle buddy
George washington bottle buddy Pengambilan keputusan menurut george r terry
Pengambilan keputusan menurut george r terry George alleyne
George alleyne George and tamara (doesn't don't) want to see that movie
George and tamara (doesn't don't) want to see that movie Kznu radio
Kznu radio Example of anticipatory socialization
Example of anticipatory socialization George cosbuc scoala
George cosbuc scoala High value resistances or rehostats are made by
High value resistances or rehostats are made by Title of pygmalion
Title of pygmalion Possessive and demonstrative pronouns
Possessive and demonstrative pronouns George nees
George nees