Urinary Incontinence r UTIs R Hamid FRCSEd FRCS












- Slides: 52
Urinary Incontinence & r. UTI’s R Hamid FRCSEd FRCS (Urol), MD(Res) Consultant Urological Surgeon Female, Reconstruction & Neuro-Urologist National Hospital for Neurology & Neurosurgery, University College London Hospitals & Londo. N Spinal Injuries Unit Royal National Orthopaedic Hospital Stanmore
The Normal Bladder Holds 400 - 500 mls The pressure at end fill is <15 cm. H 20 Can hold on for as long as needed! No pain on filling No incontinence Bladder empties with no residual volume With normal pressure and high flow No abdominal straining No UTI
Definition Incontinence - The complaint of any involuntary urinary leakage 1 Overactive bladder - urgency, with or without urge incontinence, usually in the presence of frequency and nocturia Stress incontinence – urinary leakage on effort, exertion, sneezing or coughing without a desire to pass urine Mixed incontinence - a combination of the above 2 types 1 Abrams et al (2002). Standardisation Subcommittee of the International Continence Society. Neurourol & Urodyn. 21: 167 -78
Types of urinary incontinence Urge incontinence Stress incontinence Neuropathic incontinence Mixed incontinence Male Incontinence Overflow incontinence 3 4
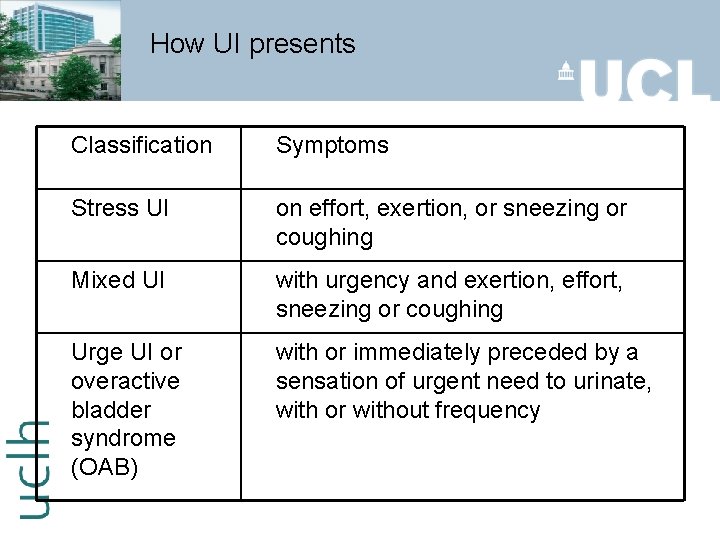
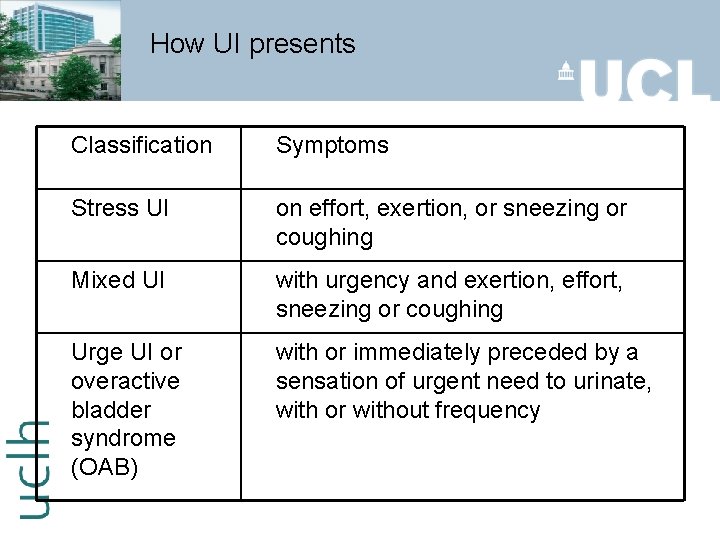
How UI presents Classification Symptoms Stress UI on effort, exertion, or sneezing or coughing Mixed UI with urgency and exertion, effort, sneezing or coughing Urge UI or overactive bladder syndrome (OAB) with or immediately preceded by a sensation of urgent need to urinate, with or without frequency
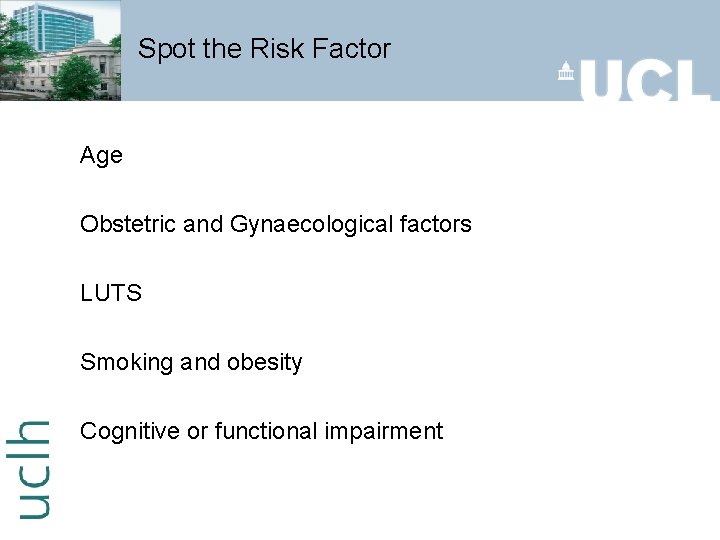
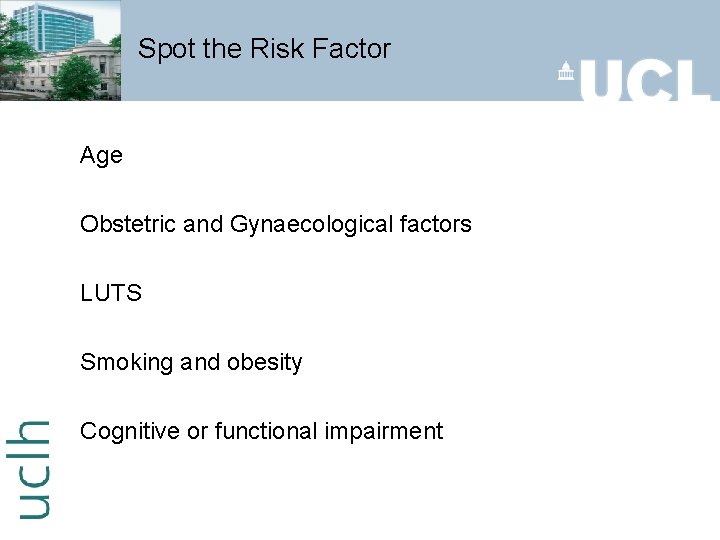
Spot the Risk Factor Age Obstetric and Gynaecological factors LUTS Smoking and obesity Cognitive or functional impairment
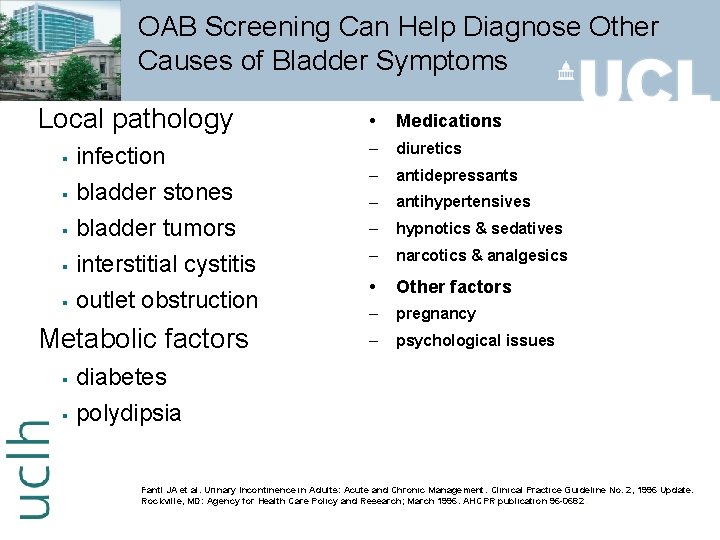
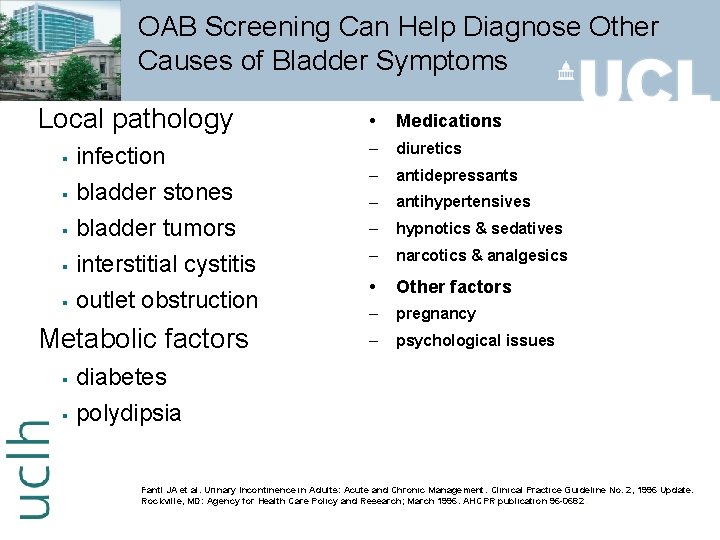
OAB Screening Can Help Diagnose Other Causes of Bladder Symptoms Local pathology § § § infection bladder stones bladder tumors interstitial cystitis outlet obstruction Metabolic factors § § • Medications – diuretics – antidepressants – antihypertensives – hypnotics & sedatives – narcotics & analgesics • Other factors – pregnancy – psychological issues diabetes polydipsia Fantl JA et al. Urinary Incontinence in Adults: Acute and Chronic Management. Clinical Practice Guideline No. 2, 1996 Update. Rockville, MD: Agency for Health Care Policy and Research; March 1996. AHCPR publication 96 -0682.
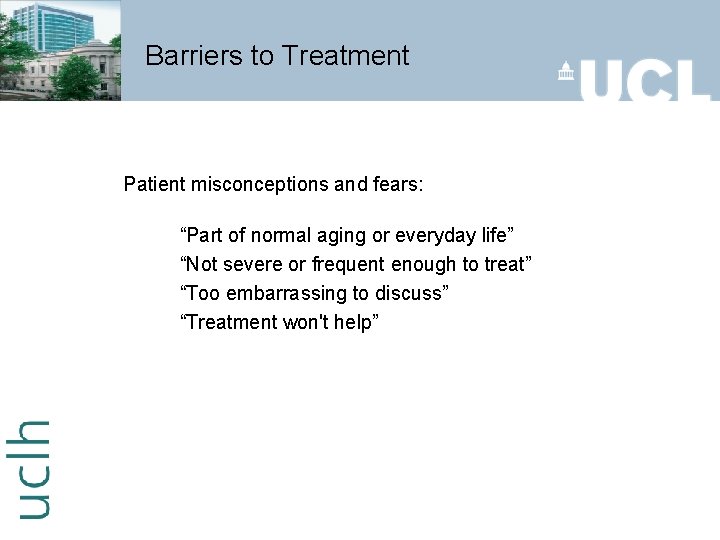
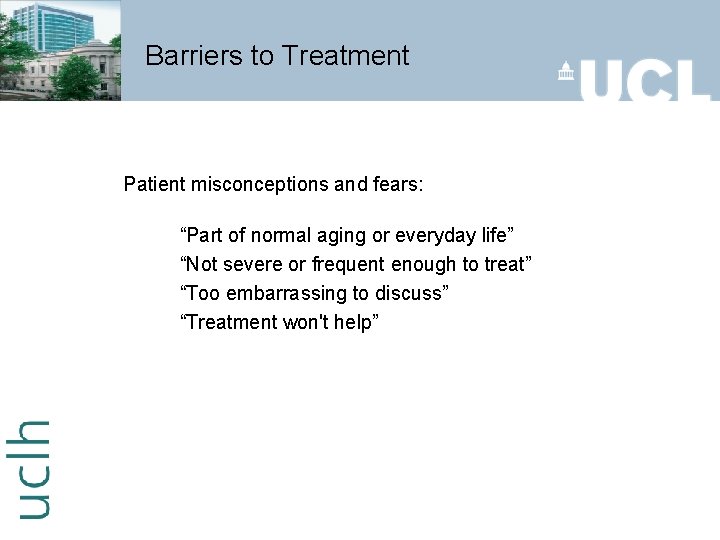
Barriers to Treatment Patient misconceptions and fears: “Part of normal aging or everyday life” “Not severe or frequent enough to treat” “Too embarrassing to discuss” “Treatment won't help”
Triggers to Bladder Overactivity Key in the door Running water Telephone boxes (red ones!) Proximity to the toilet Stress i. e. giving lectures, exams etc!
Assessment & Initial management Categorise UI as SUI / UUI or OAB / mixed UI Use urine dipstick tests to detect blood, glucose, protein, leucocytes and nitrites Ask the woman to complete a bladder diary for at least 3 days, covering variations in usual activities (e. g. working and leisure days) Flow rate & PVR? Start treatment on this basis Identify factors that may require referral

Suggested Reasons for Referral Symptoms do not respond to initial treatment within 2 to 3 months Hematuria without infection on urinalysis Recurrent symptomatic UTI Symptoms suggestive of poor bladder emptying Pelvic bladder, vaginal, or urethral pain • Evidence of complicated neurologic or metabolic disease • Failed previous incontinence surgery • Elevated PVR volume • Radical pelvic surgery • Symptomatic prolapse • Prostate problems • Surgery planned (2 nd opinion) Abrams P. Wein AJ. The Overactive Bladder – A Widespread and Treatable Condition. 1998.
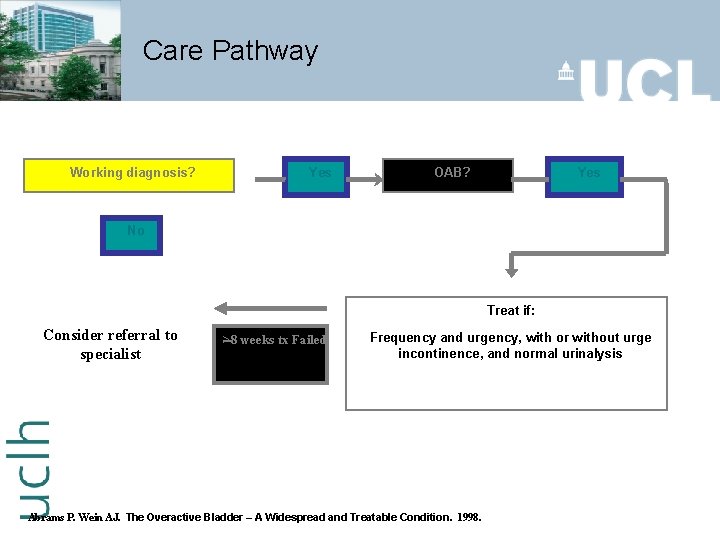
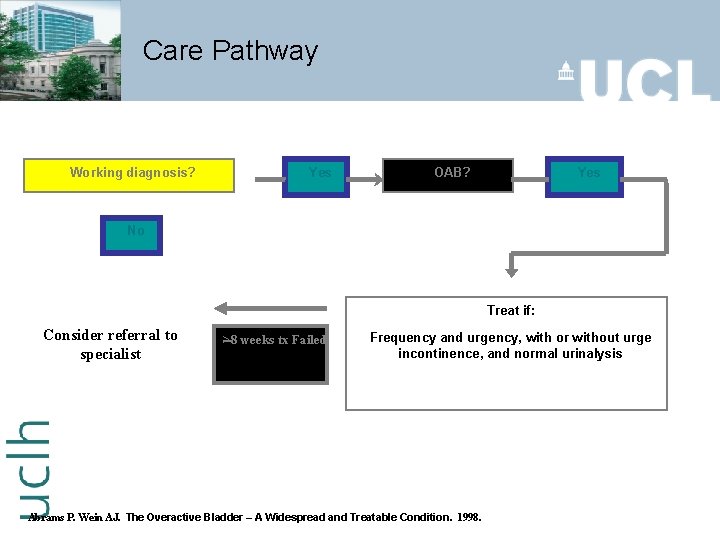
Care Pathway Working diagnosis? Yes OAB? Yes No Treat if: Consider referral to specialist >8 weeks tx Failed Frequency and urgency, with or without urge incontinence, and normal urinalysis Abrams P. Wein AJ. The Overactive Bladder – A Widespread and Treatable Condition. 1998.
Treatment options for OAB - (PC) Life style changes Recommend caffeine reduction First-line treatment is Bladder re-training lasting at least 6 weeks Antimuscarinic drug - oxybutynin If oxybutynin is not tolerated, alternatives are solifenacin, tolterodine, trospium, or different oxybutynin formulations Carry out an early treatment review after any change in drug

Conservative Management Behaviour modification Dietary changes / weight loss Advice on fluid management Reduction in caffeine intake Reduction in alcohol intake
Behavioural Therapy Bladder Re-training Described by Frewen Timed voiding Bladder Training Voiding Diary Fluid management Successful in > 50% Reduced success longterm Payne CK. Urology 2000: 55 (Suppl 5 A); 3 -5 Burgio KL, Burgio LD. Clin Geriatri Med 1986: 2 (4); 809 -827

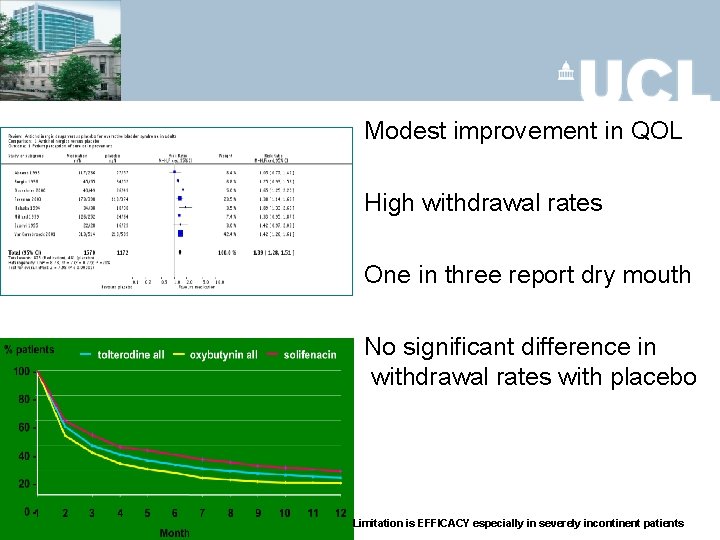
Drugs - Antimuscuranics
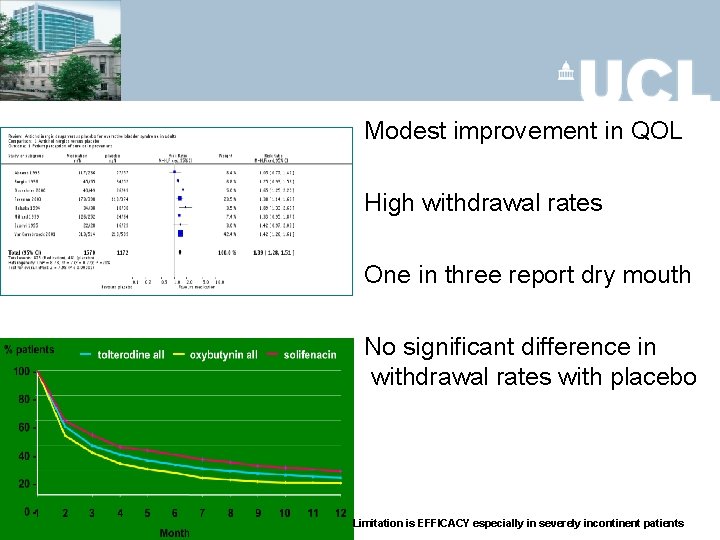
Modest improvement in QOL High withdrawal rates One in three report dry mouth No significant difference in withdrawal rates with placebo Limitation is EFFICACY especially in severely incontinent patients
New Therapy - Mirabegron β-3 adrenoreceptors in the bladder are known to have a role in bladder relaxation Mirabegron (β-3 adrenoreceptors) reduces the number of micturitions and incontinence episodes in a 24 -h period compared with placebo Dry mouth and gastrointestinal disturbances are the most common side effects, but these have been rated as mild to moderate A small rise in mean heart rate and blood pressure has been shown Mirabegron - is it a promising alternative or supplement to antimuscarinics? Bhindee A. Int J Urogynae. 2012 Oct; 23(10): 1345 -8
OAB + / - urge UI (PC) In postmenopausal women with vaginal atrophy offer intravaginal oestrogens for OAB symptoms In women with UI who also have cognitive impairment prompted and timed toileting programmes may help reduce leakage episodes Do not routinely use electrical stimulation in OAB

OAB + / - urge UI (SC) If conservative treatments have fail consider referring to secondary care for: Botulinum toxin A p. TENS Sacral nerve stimulation Augmentation cystoplasty Urinary diversion

Intravesical Botulinum Toxin
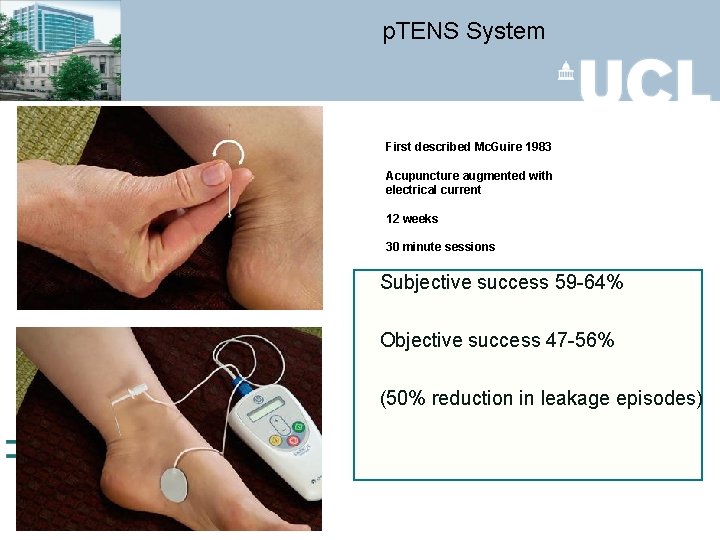
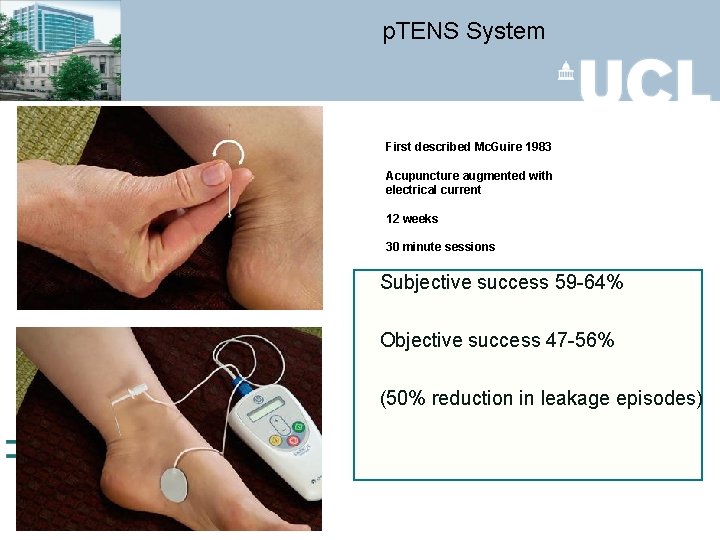
p. TENS System First described Mc. Guire 1983 Acupuncture augmented with electrical current 12 weeks 30 minute sessions Subjective success 59 -64% Objective success 47 -56% (50% reduction in leakage episodes)
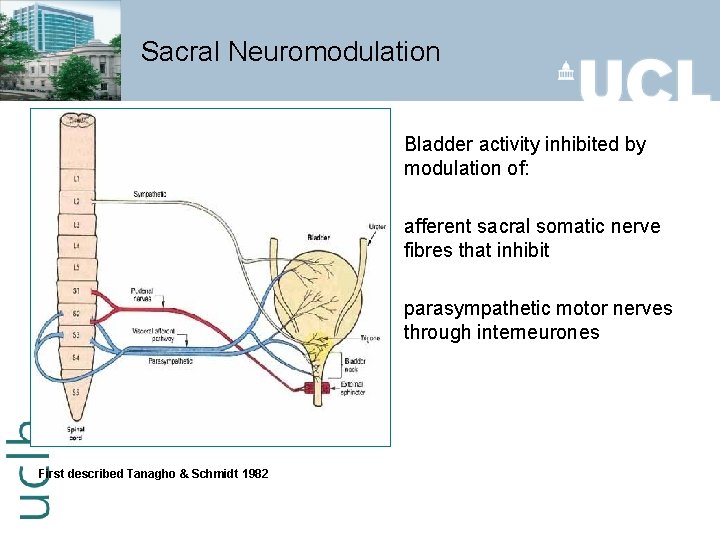
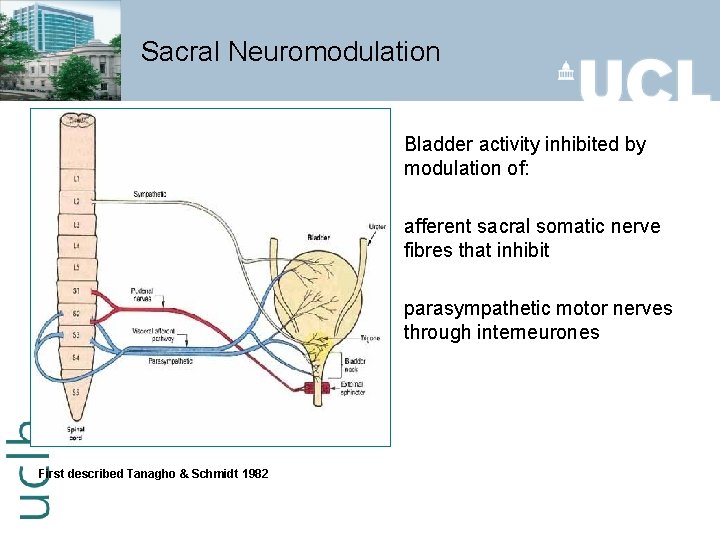
Sacral Neuromodulation Bladder activity inhibited by modulation of: afferent sacral somatic nerve fibres that inhibit parasympathetic motor nerves through interneurones First described Tanagho & Schmidt 1982
Clam Cystoplasty Described in 1888 in Italian dogs Popularised for IDO by Bramble in 1980 s 85% cure
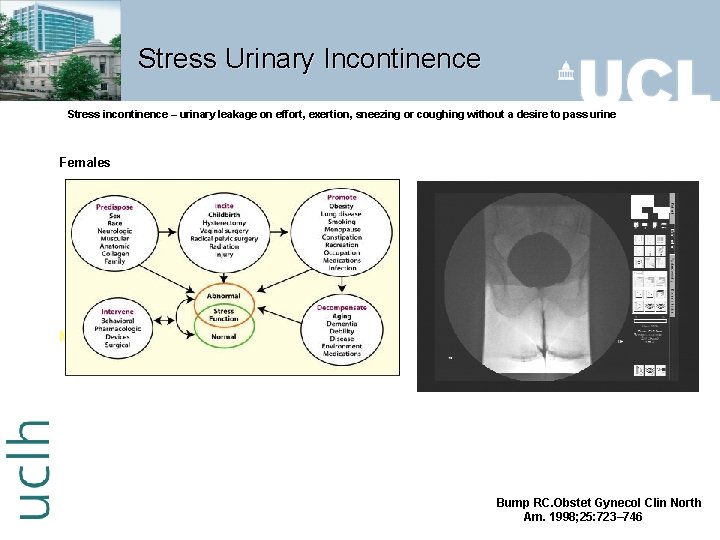
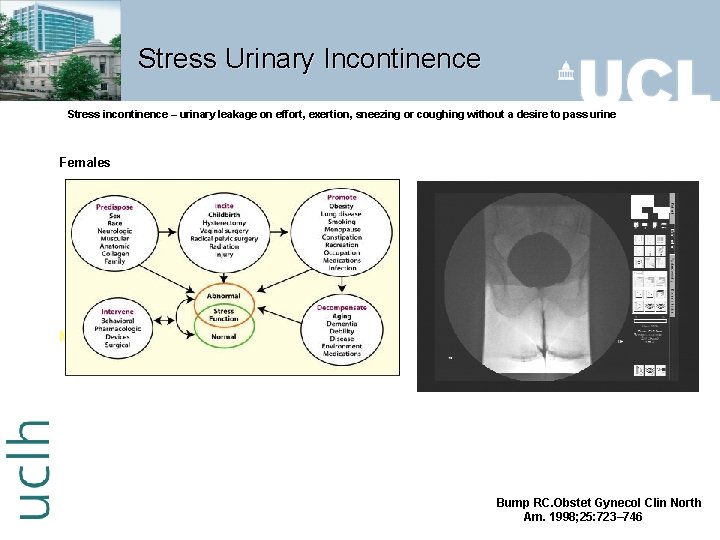
Stress Urinary Incontinence Stress incontinence – urinary leakage on effort, exertion, sneezing or coughing without a desire to pass urine Females Males – Post prostatic surgery Bump RC. Obstet Gynecol Clin North Am. 1998; 25: 723– 746
Pad testing - Definition International Continence Society – 1 g loss / hour – 8 -10 g loss / 24 hour
Stress UI Management (PC) First-line treatment for stress or mixed UI should be pelvic floor muscle training (PFMT) lasting at least 3 months PFMT should consist of at least eight contractions (slow & fast) three times a day If PFMT is beneficial, continue an exercise programme

Drugs - Duloxetine Ten randomised trials 3944 adults § 50% reduction in Incontinence Episode Frequency § 3% improvement in subjective cure (improved QOL) ie small effect § High incidence ‘mild’ side effects nausea (33%) § No advantage of combination PFE over either treatment alone Duloxetine Should not be used as 1 st line Not to used as 2 nd line May be offered as alternative to surgery Counsel about side effects P Mariappan, AA Alhasso, A Grant, JMO N'Dow Serotonin andnoradrenaline reuptake inhibitors (SNRI) for stress urinary incontinence in adults Cochrane Database of Systematic Reviews 2005
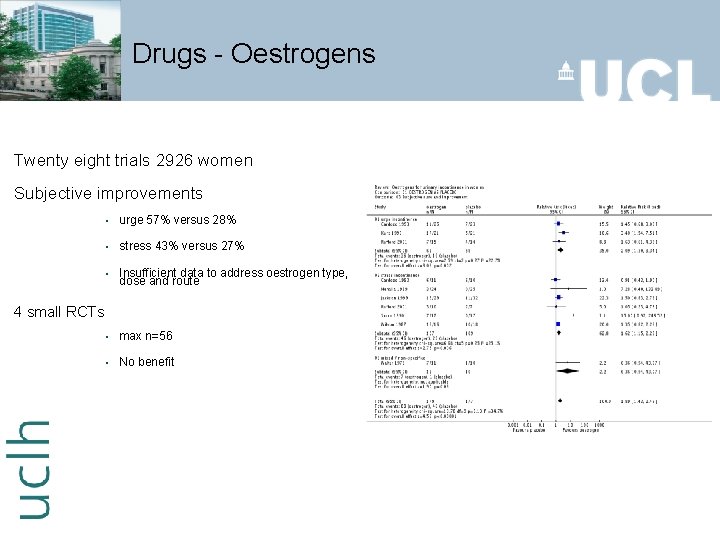
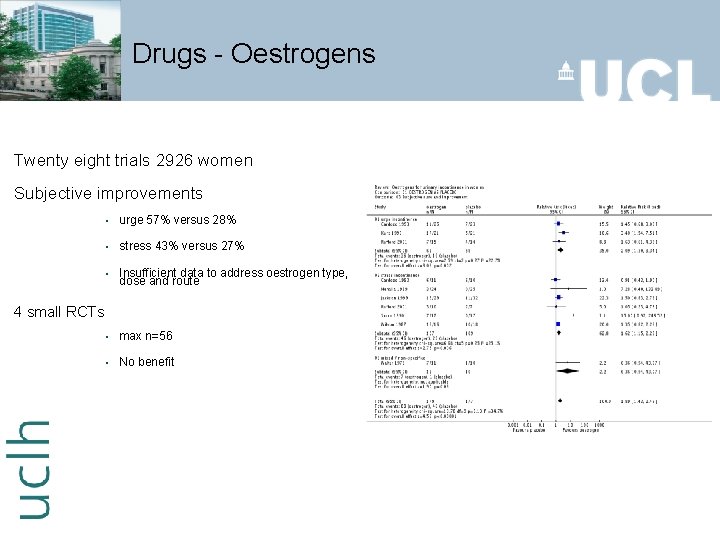
Drugs - Oestrogens Twenty eight trials 2926 women Subjective improvements § urge 57% versus 28% § stress 43% versus 27% § Insufficient data to address oestrogen type, dose and route § max n=56 § No benefit 4 small RCTs

Conservative treatment - Summary Strength: Safe Challenges: Compliance ↓ over time No fast outcomes More RCTs needed Consistency in PFMT programs Consistency in outcome assessment
Surgical management SUI (SC) Intramural bulking agents Synthetic slings using a retropubic ‘top-down’ or a transobturator foramen approach Autologous slings Retropubic operations - open/lap colposuspension Artificial urinary sphincter Bladder neck closure / Mitrofanoff / Ileal conduit

Results Generally >80% in 1 yr >70% long term Well tolerated High satisfaction rates Need for SIC BUT Increasing concern re long term issues i. e. erosion 50 33
Mixed UI Determine treatment according to whether stress or urge UI is the dominant symptom Generally treat urge component first

Neuropathic Bladder
Management of Neuropathic incontinence Upper motor neuron type injury Anticholinergic medications & self catheterization Intravesical Botox Clam cystoplasty Sacral anterior root stimulator Indwelling catheters Condom sheaths

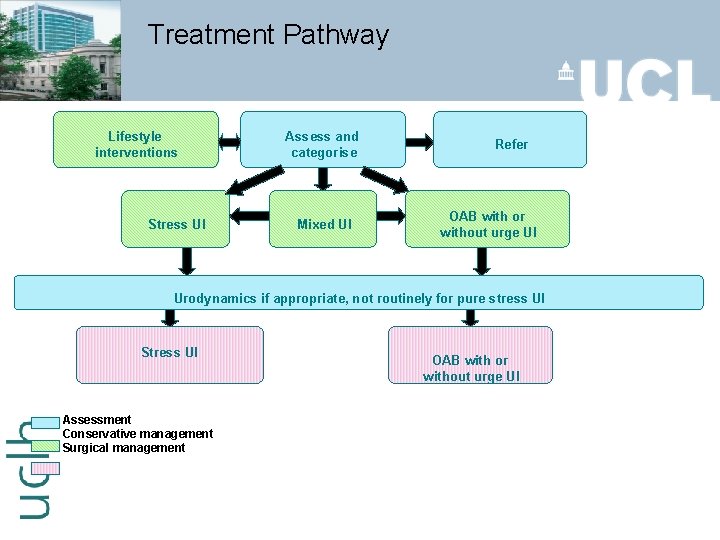
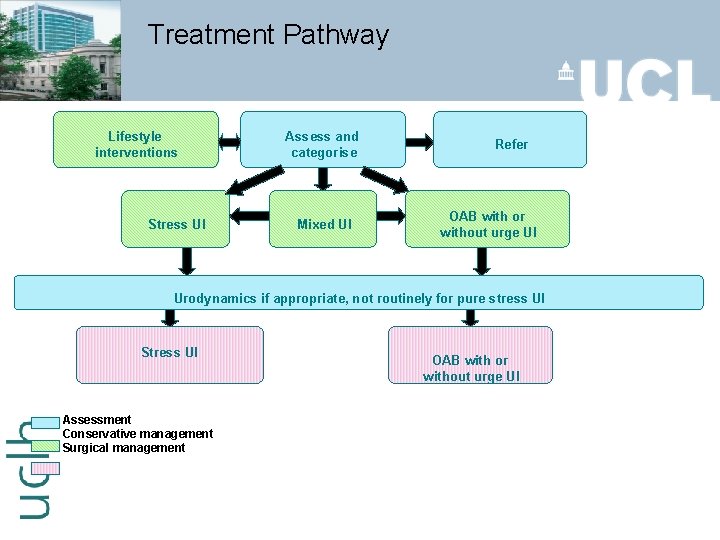
Treatment Pathway Lifestyle interventions Stress UI Assess and categorise Mixed UI Refer OAB with or without urge UI Urodynamics if appropriate, not routinely for pure stress UI Stress UI Assessment Conservative management Surgical management OAB with or without urge UI
Conclusions Urinary incontinence is a significant problem It has a considerable impact on Qo. L The treatments are generally effective Patient wishes must be taken into account
Conclusions Lifestyle and bladder training Anticholinergics Botulinum Toxin Sacral Neuromodulation Stress UI – Midurethral tapes of abdominal operations
r. Urinary Tract Infection

Types of UTI’s Uncomplicated lower UTI (cystitis) Uncomplicated pyelonephritis Complicated UTI with or without pyelonephritis Urosepsis 63 42
History Subjective § dysuria, urgency, frequency, nocturia Personal § scented products, hygiene, fluid intake Sexual § frequency, number of partners, use of latex or spermicides, routes Obstetric and gynecological § last menstrual period, symptoms of atrophic changes Medication § anticholinergics, psychotropics, immunosuppressives

Diagnosis Dipstick analysis p. H and Specific Gravity Blood Protein Nitrites Leukocyte esterase (Howes, 2005) specificity 94% specificity 74 -95%
History Predisposition to r. UTI § Previous diagnosis § Diabetes mellitus § Pregnancy § Elderly Hillebrand L, Harmanli OH, Whiteman V, Khandelwal M. Urinary tract infections in pregnant women with bacterial vaginosis. Am J Obstet Gynecol. 2002 May; 186(5): 916 -7
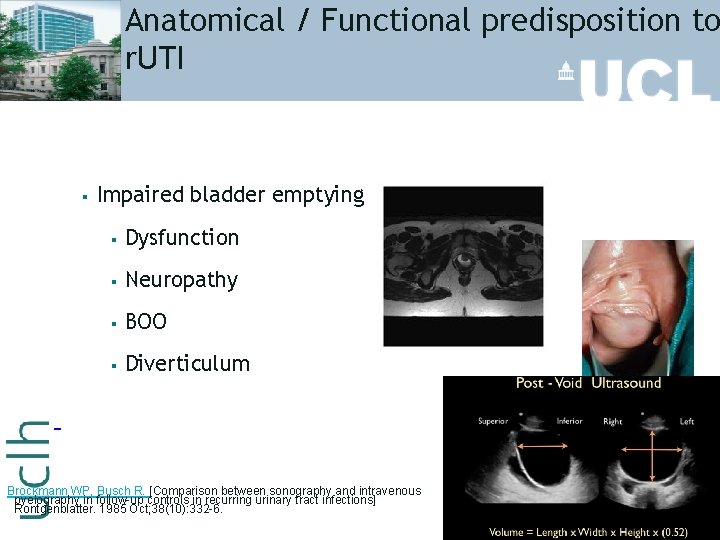
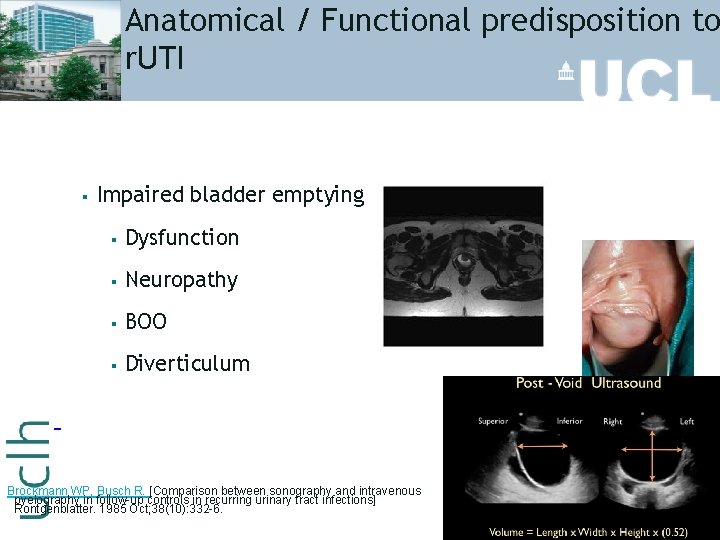
Anatomical / Functional predisposition to r. UTI § Impaired bladder emptying § Dysfunction § Neuropathy § BOO § Diverticulum Brockmann WP, Busch R. [Comparison between sonography and intravenous pyelography in follow-up controls in recurring urinary tract infections] Rontgenblatter. 1985 Oct; 38(10): 332 -6.
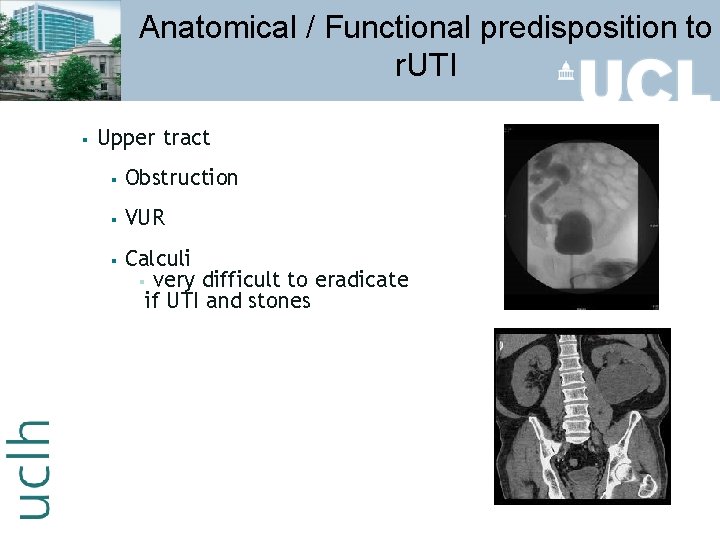
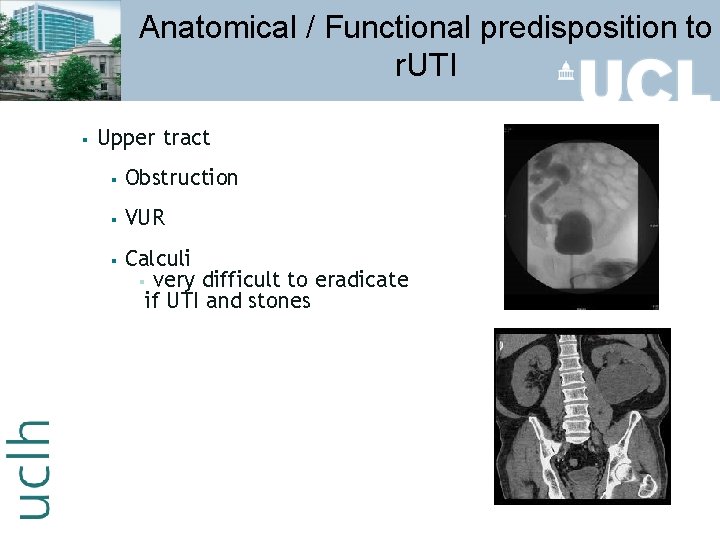
Anatomical / Functional predisposition to r. UTI § Upper tract § Obstruction § VUR § Calculi § very difficult to eradicate if UTI and stones
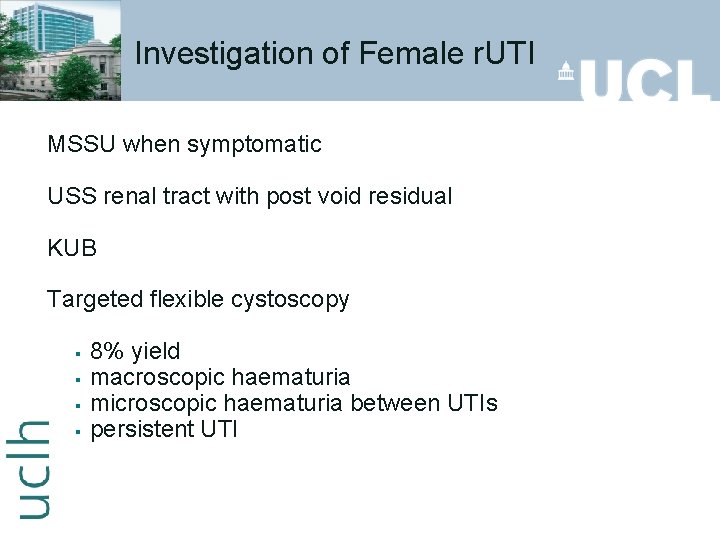
Investigation of Female r. UTI MSSU when symptomatic USS renal tract with post void residual KUB Targeted flexible cystoscopy § § 8% yield macroscopic haematuria microscopic haematuria between UTIs persistent UTI
Treatment of Female UTI 3 days oral antibiotics or x 1 high dose § § 1 day regimes have been associated with high failure rates Greater than 3 days have been deemed unnecessary (Delzell & Fitzsimmons, 2005; NGC, 2000). 14 days antibiotics if pyelonephritis Ronald A, Nicolle LE, Harding G. Single dose treatment failure in women with acute cystitis. Infection. 1992; 20 Suppl 4: S 2769. Lutters M, Vogt N. Antibiotic duration for treating uncomplicated, symptomatic lower urinary tract infections in elderly women. Cochrane Database Syst Rev. 2002; (3): CD 001535. Roberts JA. Management of pyelonephritis and upper urinary tract infections. Urol Clin North Am. 1999 Nov; 26(4): 753 -63.
Treatment of Female r. UTI Topical oestrogen (postmenopausal) General advice § § § Hygiene increase fluid intake Double voiding Void after sexual intercourse Cranberry juice Live yoghurt Xu R, Wu Y, Hu Y. [Prevention and treatment of recurrent urinary system infection with estrogen cream in postmenopausal women] Zhonghua Fu Chan Ke Za Zhi. 2001 Sep; 36(9): 531 -3. Stothers L. A randomized trial to evaluate effectiveness and cost effectiveness of naturopathic cranberry products as prophylaxis against urinary tract infection in women. Can J Urol. 2002 Jun; 9(3): 1558 -62
Treatment of Recurrent UTI Self-start antibiotic therapy 6 months low dose prophylactic antibiotics Nitrofurantoin 50 -100 mgs nocte Trimethoprim 100 mg nocte BREAKTHROUGH INFECTIONS Ciprofloxacin 125 mg/day Nicolle LE, Harding GK, Thompson M, Kennedy J, Urias B, Ronald AR. Prospective, randomized, placebocontrolled trial of norfloxacin for the prophylaxis of recurrent urinary tract infection in women. Antimicrob Agents Chemother. 1989 Jul; 33(7): 1032 -5 Schaeffer AJ, Stuppy BA. Efficacy and safety of self-start therapy in women with recurrent urinary tract infections. J Urol. 1999 Jan ; 161(1): 207 -11
Thank you
 Acupuncture for incontinence
Acupuncture for incontinence Bulbocavernosus reflex
Bulbocavernosus reflex Coital incontinence
Coital incontinence Acfi answer appraisal pack
Acfi answer appraisal pack Frcsed meaning
Frcsed meaning Titul frcs(t)
Titul frcs(t) Frcs viva
Frcs viva Frcsed meaning
Frcsed meaning Frcsed meaning
Frcsed meaning Hamid d. ismail
Hamid d. ismail Hamid vazin
Hamid vazin Dr hamid rabiee
Dr hamid rabiee Seyed hamid reza sanei
Seyed hamid reza sanei Hamid khattak
Hamid khattak Rania hamid
Rania hamid Hamid rashid finterra
Hamid rashid finterra Lovostatin
Lovostatin Alia hamid
Alia hamid Doc zainul abidin hamid
Doc zainul abidin hamid Hamid mahini
Hamid mahini Hamid vakilzadian
Hamid vakilzadian Edy suandi hamid
Edy suandi hamid Hamid harroud
Hamid harroud Hamid rahim
Hamid rahim Cognitive psychology ppt
Cognitive psychology ppt Hamid yeşilyayla
Hamid yeşilyayla R4funds
R4funds Edy suandi hamid
Edy suandi hamid Hamid yunis
Hamid yunis Ardian shajkovci
Ardian shajkovci Hamid sebaly
Hamid sebaly Osteichthyes
Osteichthyes Urinary infection symptoms
Urinary infection symptoms Urinary system fun fact
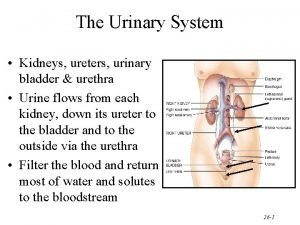
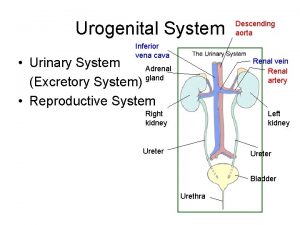
Urinary system fun fact Urinary system
Urinary system Urinary system
Urinary system Complicated urinary tract infection
Complicated urinary tract infection Urised otc
Urised otc Fetal pig excretory system diagram
Fetal pig excretory system diagram Superior surface of urinary bladder
Superior surface of urinary bladder Homework
Homework Youtube urinary system
Youtube urinary system Anatomical structure of urinary system
Anatomical structure of urinary system Nur 102
Nur 102 Lith-oh-trip-see
Lith-oh-trip-see Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Urinary system histology
Urinary system histology Classification of urinary antiseptics
Classification of urinary antiseptics Hyperproteinuria word parts
Hyperproteinuria word parts Inferior vena cava urinary system
Inferior vena cava urinary system The urinary system consists of
The urinary system consists of Spill of dye
Spill of dye