Longterm Complications of Immune suppression after liver transplantation








- Slides: 60
Long-term Complications of Immune suppression after liver transplantation Isabelle Colle MD Ph. D Dept. of Hepatology and Gastroenterology Ghent University Hospital Ghent 10 th of March 2005 UNIVERSITEIT GENT
1. Metabolic and endocrinological disorders - Diabetes mellitus => increased mortality after 2 y - Metabolic bone disease - Obesity - Hyperlipidemia => 40% 2. Cardiovascular diseases => 0 -20% mortality after 3 y 3. Renal failure after LTx => ESRD: 4. 6 x increased risk of death 4. Malignancies - solid tumors - lymphoma and PTLD - skin tumors 5. Infectious complications => 68% cause of death
Overall Summary of Safety Physician’s Desk Reference Kahan DB and Ponticelli, C. Principles and Practice of Renal Transplantation, ed Martin Dunitz, 2000
Metabolic complications after liver transplantation -Diabetes -Metabolic bone disorders -Obesity -Hyperlipidemia
Diabetes mellitus • DM if present before LTx => more infectious, renal and cardiovascular complications, more malignancies, 5 y survival is less (34% in DM vs 67% in non-DM). John. Hepatology 2001. • 1/3 have transient glucose intolerance within 1°y • 13 -30% develop de novo DM Eur FK 506 multicentre Liver study group. Lancet 1994. Stegall. Transplantation 1995. Heisel. Am J Transplantation 2004. Reasons: -Ciclosporin A (8%) < tacrolimus (18%): insulin resistance, insulin secretion - Prednisolone: withdrawal => better glucose metabolism - Weight gain

Obesity • Obesity occurs early after LTx • 20 - 40% develop BMI > 30 kg/m 2 Stegall. Transplantation 1995. Everhart. Liver Tx Surg 1998. Munoz. Transplant Proc 1991 Causes: ? - Hepatic denervation - Hunger feeling - Increased sense of taste and smelling - Ciclosporin A > tacrolimus: ? - Prednisolone: no difference in dose Treatment: dietary counseling, daily exercise (2 miles within 25 min)
Hyperlipidemia (1) • Hypercholesterolemia > 250 mg/dl - 24% in ciclosporin - 5% in tacrolimus • High levels of Tg > 500 mg/dl => plasma Cl of ciclo • Sirolimus: blocks insulin-stimulated lipoprotein lipase, reduction in catabolism of apo. B 100 -containing lipoproteins • Corticosteroids: hyperinsulinemia mediated stimulation VLDL synthesis + down-regulation LDL-receptors • Cyclosporin: total and LDL chol and HDL chol Adverse effects of hyperlipidemia: - heart attack: especially in KTx and HTx - stroke Mor E. Transpl Proc 1995. Canzanello. Liver Transpl Surg 1997. Kraemer. Metabolism 1998. Hoogeveen. Tx 2001. Groth. Tx 1999. Kreis. Tx 2000.

Cardiovascular complications after liver transplantation
Arterial hypertension (AHT) • AHT very common after LTx • 80% exhibit AHT at one timepoint after LTx • 50% patients require chronic antihypertensive treatment Cause: - direct effects of IS on vascular endothelium: SVR - drug induced renal changes: RVR - cyclo 62% > FK 38% - corticosteroids, weight gain Sheiner. Transplantation 2000. Eur FK 506 multicentre Liver study group. Lancet 1994. Rabkin. Am J Surg 2002. US FK 506 multicentre Liver study group. NEJM 1994. Canzanello. Liver Tx Surg 1998.
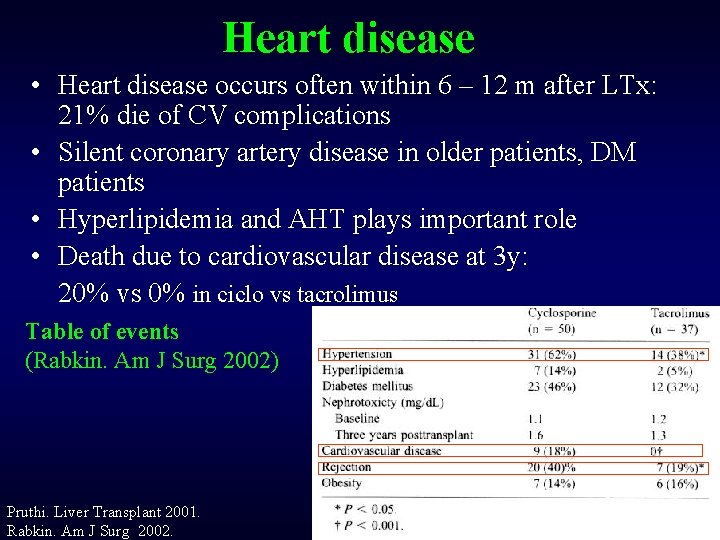
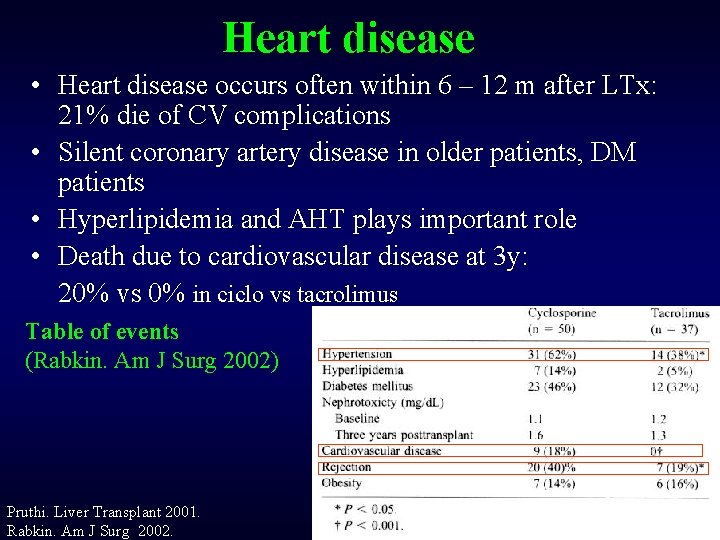
Heart disease • Heart disease occurs often within 6 – 12 m after LTx: 21% die of CV complications • Silent coronary artery disease in older patients, DM patients • Hyperlipidemia and AHT plays important role • Death due to cardiovascular disease at 3 y: 20% vs 0% in ciclo vs tacrolimus Table of events (Rabkin. Am J Surg 2002) Pruthi. Liver Transplant 2001. Rabkin. Am J Surg 2002.

Renal complications after liver transplantation
Survival after Liver Tx • Survival in patients with HRS before Tx is lower than no HRS => renal failure improves but 710% will develop ESRD • Patients with pre-LTx renal failure => 10% need hemodialysis post-LTx vs 2% who did not have renal failure before • Indication combined KTx and LTx: => proven parenchymal kidney disease => genetic diseases: oxalosis; polycystic disease
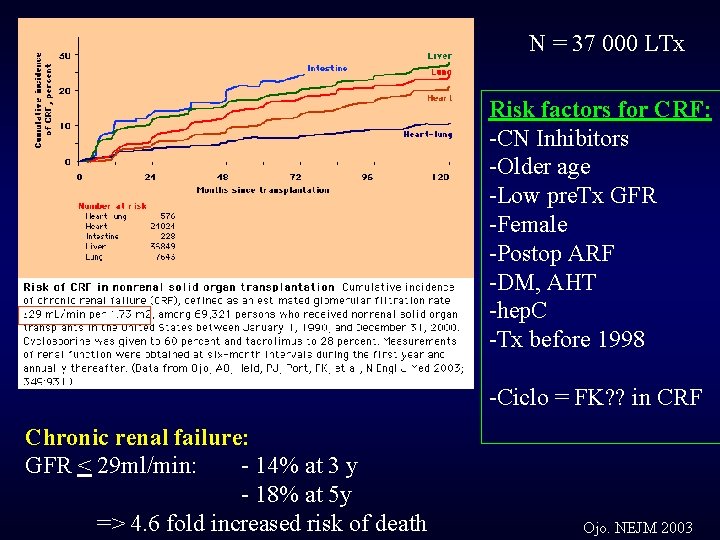
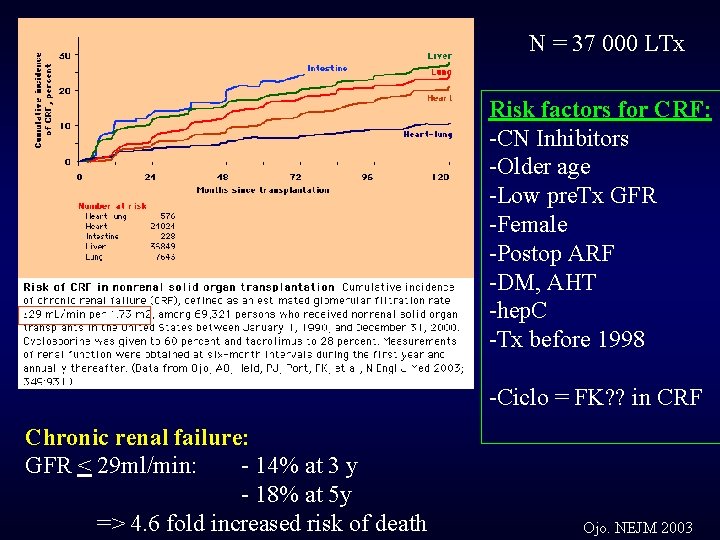
N = 37 000 LTx Risk factors for CRF: -CN Inhibitors -Older age -Low pre. Tx GFR -Female -Postop ARF -DM, AHT -hep. C -Tx before 1998 -Ciclo = FK? ? in CRF Chronic renal failure: GFR < 29 ml/min: - 14% at 3 y - 18% at 5 y => 4. 6 fold increased risk of death Ojo. NEJM 2003
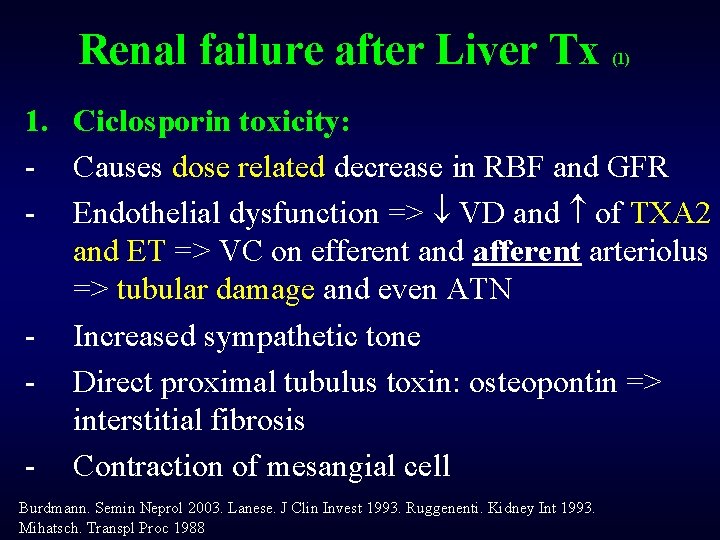
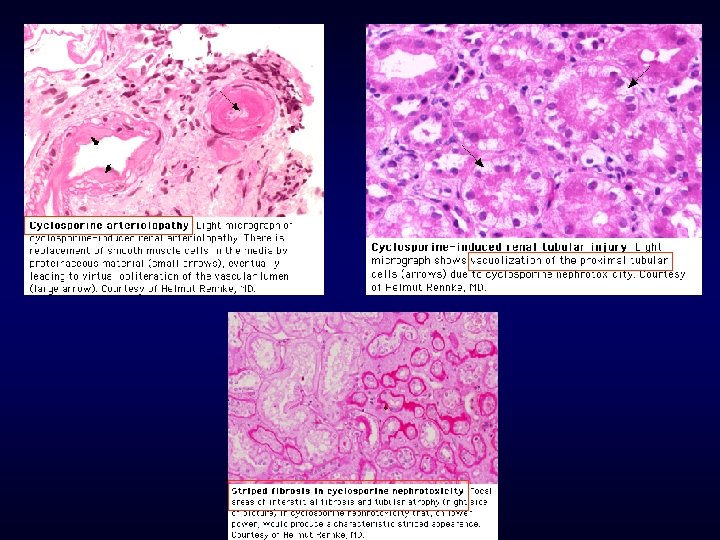
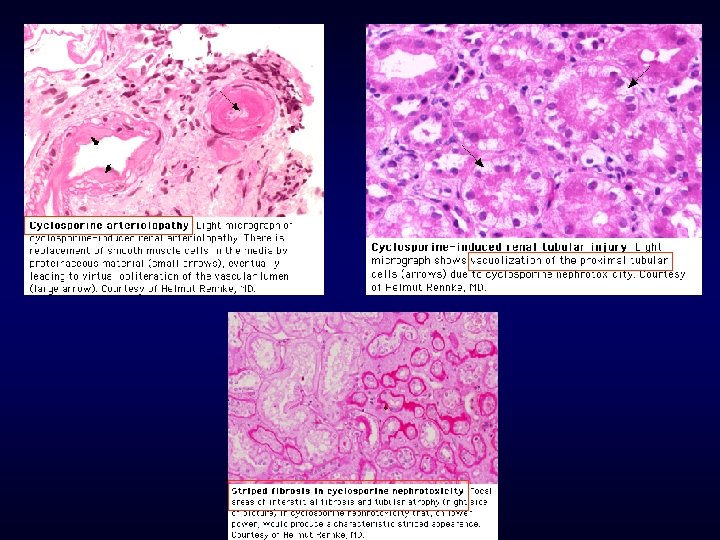
Renal failure after Liver Tx (1) 1. Ciclosporin toxicity: - Causes dose related decrease in RBF and GFR - Endothelial dysfunction => VD and of TXA 2 and ET => VC on efferent and afferent arteriolus => tubular damage and even ATN - Increased sympathetic tone - Direct proximal tubulus toxin: osteopontin => interstitial fibrosis - Contraction of mesangial cell Burdmann. Semin Neprol 2003. Lanese. J Clin Invest 1993. Ruggenenti. Kidney Int 1993. Mihatsch. Transpl Proc 1988
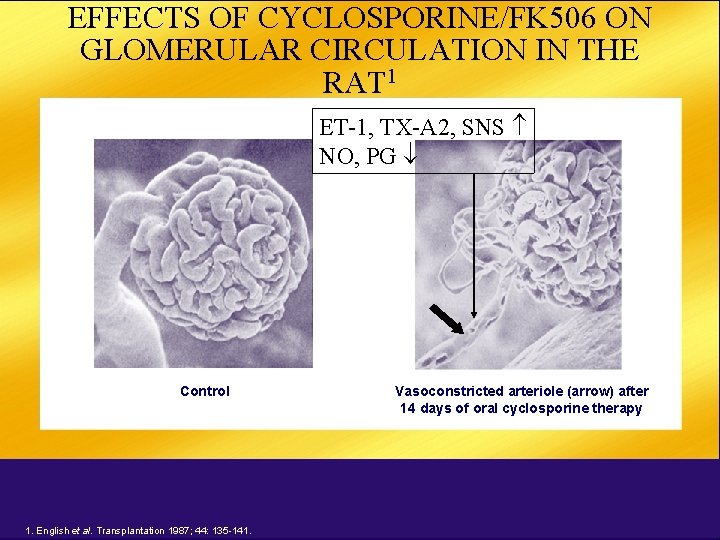
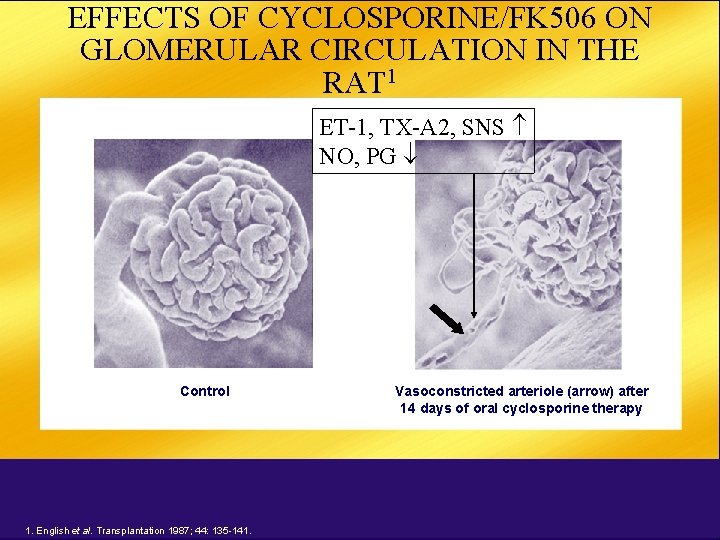
EFFECTS OF CYCLOSPORINE/FK 506 ON GLOMERULAR CIRCULATION IN THE RAT 1 ET-1, TX-A 2, SNS NO, PG Control 1. English et al. Transplantation 1987; 44: 135 -141. Vasoconstricted arteriole (arrow) after 14 days of oral cyclosporine therapy
Renal failure after Liver Tx (2) 1. Ciclosporin toxicity: - Acute nephrotoxicity: endothelial damage, fibrin thrombi in capillary loops, eo’s, patchy necrosis of SMC malignant HT, thrombotic thrombocytopenic purpura
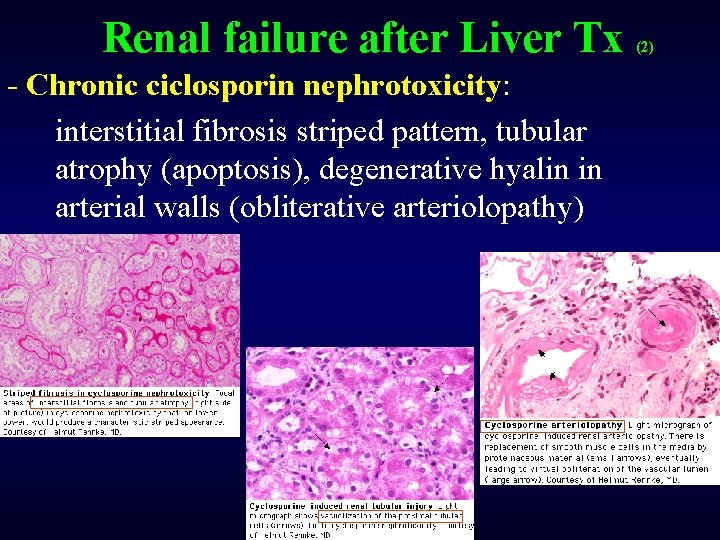
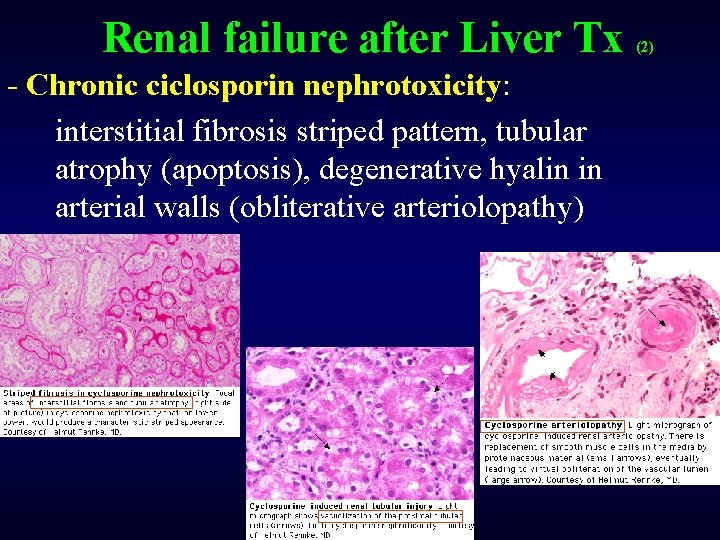
Renal failure after Liver Tx - Chronic ciclosporin nephrotoxicity: interstitial fibrosis striped pattern, tubular atrophy (apoptosis), degenerative hyalin in arterial walls (obliterative arteriolopathy) (2)
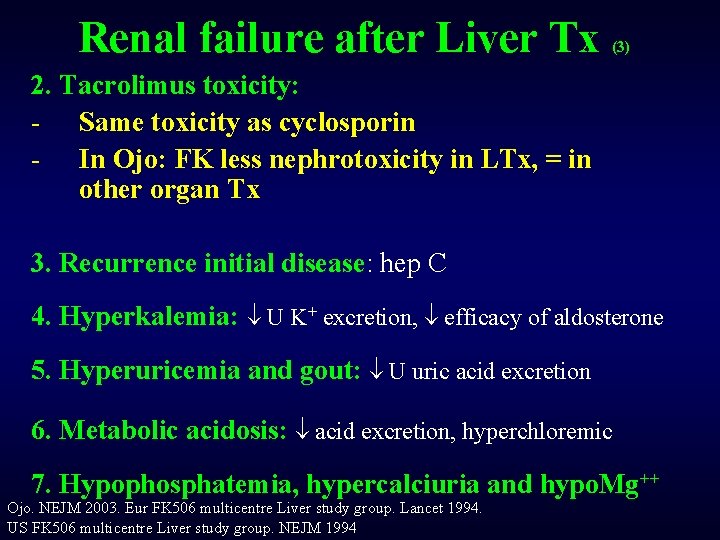
Renal failure after Liver Tx 2. Tacrolimus toxicity: - Same toxicity as cyclosporin - In Ojo: FK less nephrotoxicity in LTx, = in other organ Tx 3. Recurrence initial disease: hep C Ojo. NEJM 2003. Eur FK 506 multicentre Liver study group. Lancet 1994. US FK 506 multicentre Liver study group. NEJM 1994 (3)
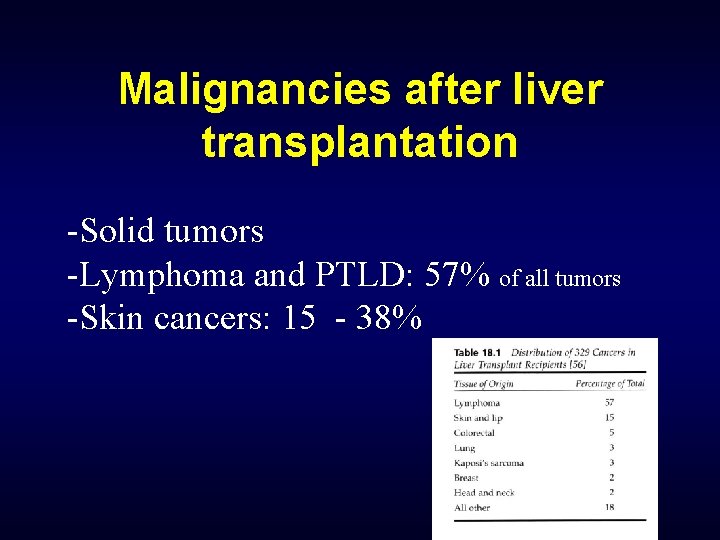
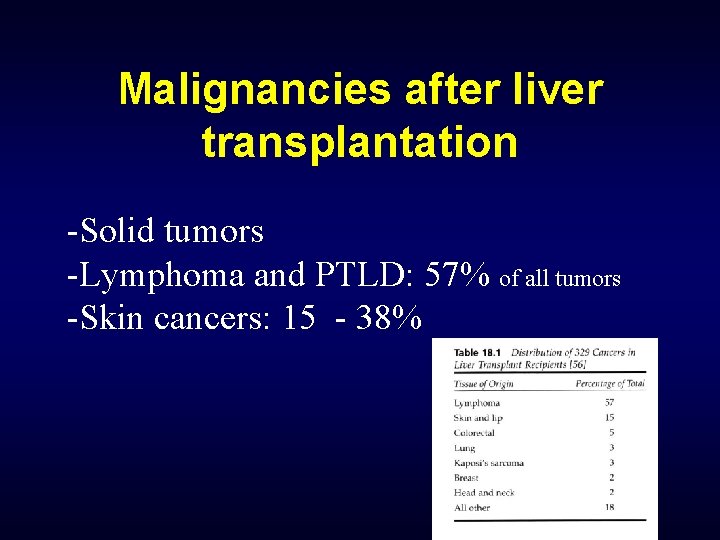
Malignancies after liver transplantation -Solid tumors -Lymphoma and PTLD: 57% of all tumors -Skin cancers: 15 - 38%
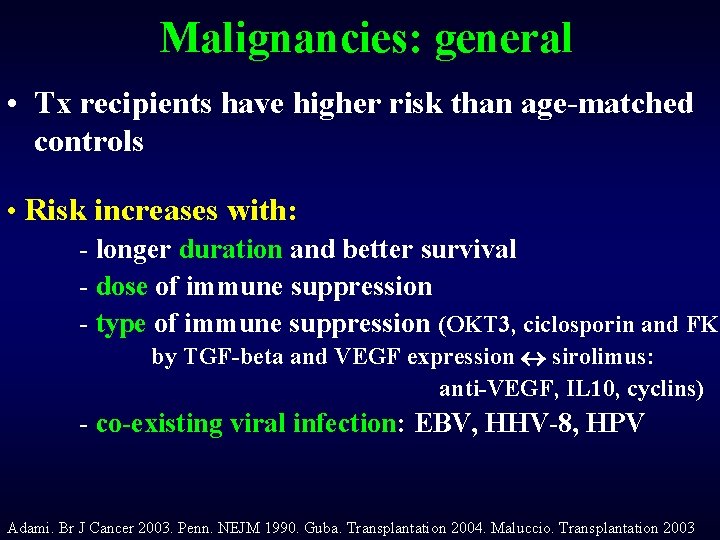
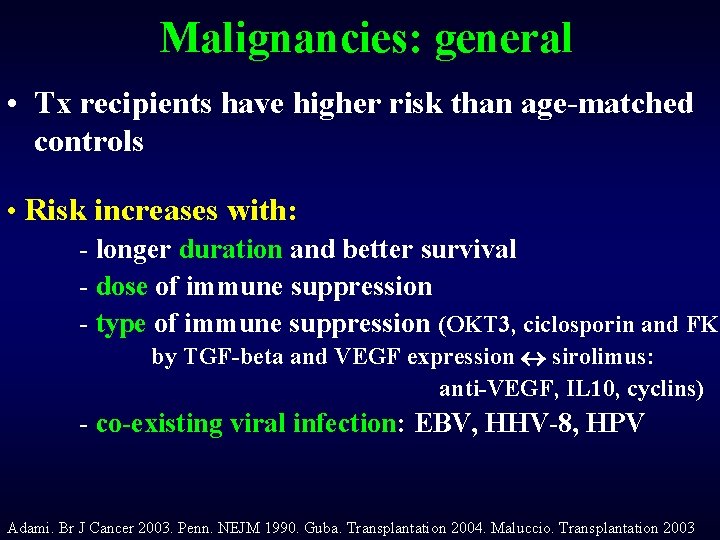
Malignancies: general • Tx recipients have higher risk than age-matched controls • Risk increases with: - longer duration and better survival - dose of immune suppression - type of immune suppression (OKT 3, ciclosporin and FK by TGF-beta and VEGF expression sirolimus: anti-VEGF, IL 10, cyclins) - co-existing viral infection: EBV, HHV-8, HPV Adami. Br J Cancer 2003. Penn. NEJM 1990. Guba. Transplantation 2004. Maluccio. Transplantation 2003
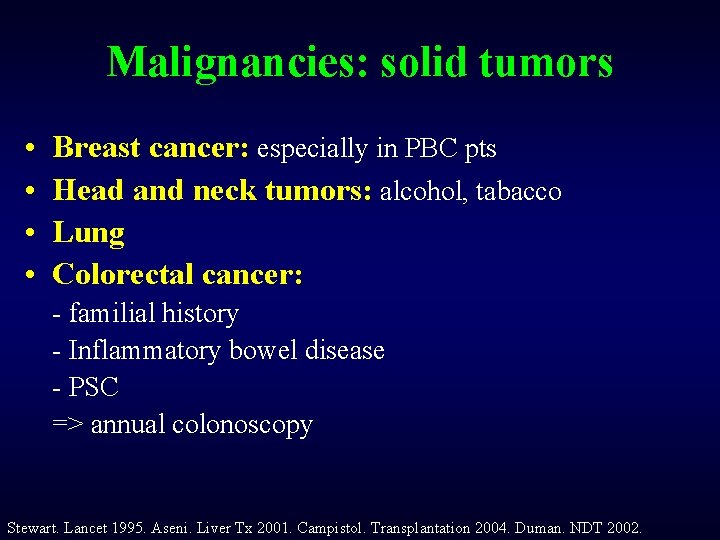
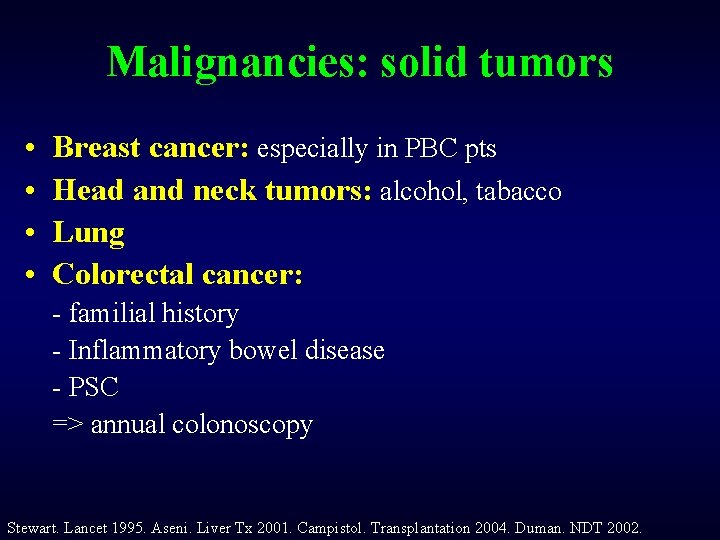
Malignancies: solid tumors • • Breast cancer: especially in PBC pts Head and neck tumors: alcohol, tabacco Lung Colorectal cancer: - familial history - Inflammatory bowel disease - PSC => annual colonoscopy Stewart. Lancet 1995. Aseni. Liver Tx 2001. Campistol. Transplantation 2004. Duman. NDT 2002.
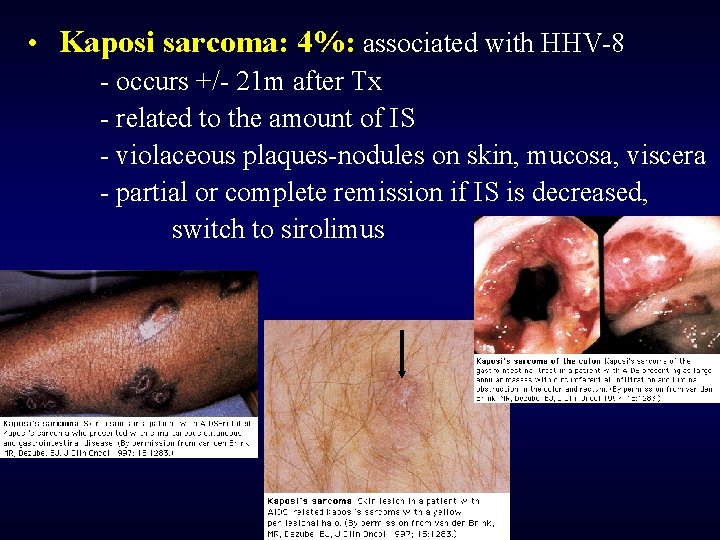
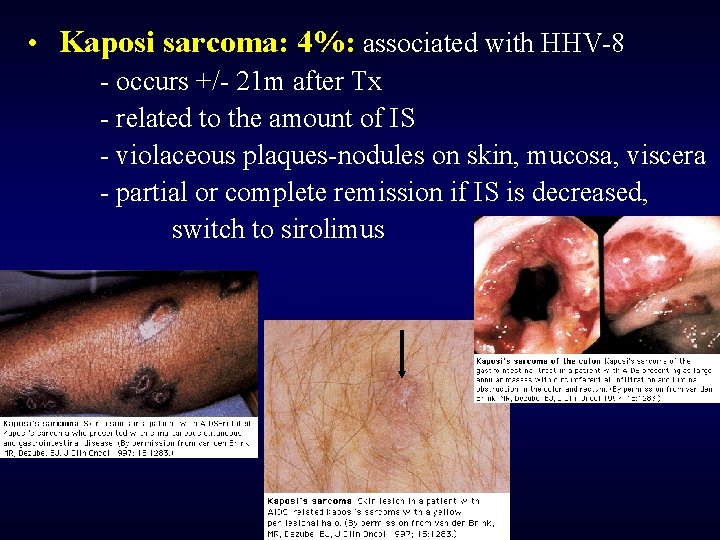
• Kaposi sarcoma: 4%: associated with HHV-8 - occurs +/- 21 m after Tx - related to the amount of IS - violaceous plaques-nodules on skin, mucosa, viscera - partial or complete remission if IS is decreased, switch to sirolimus
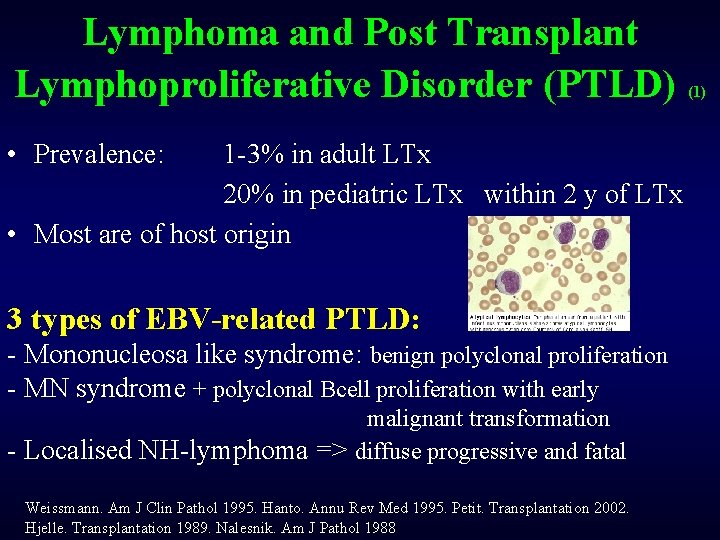
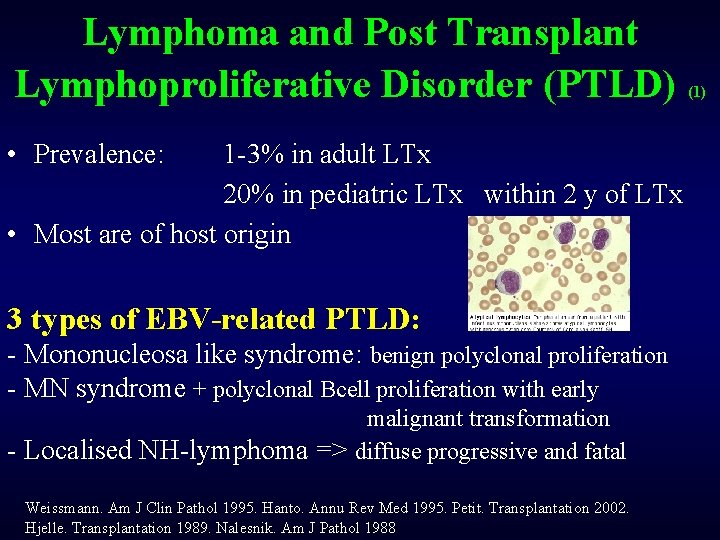
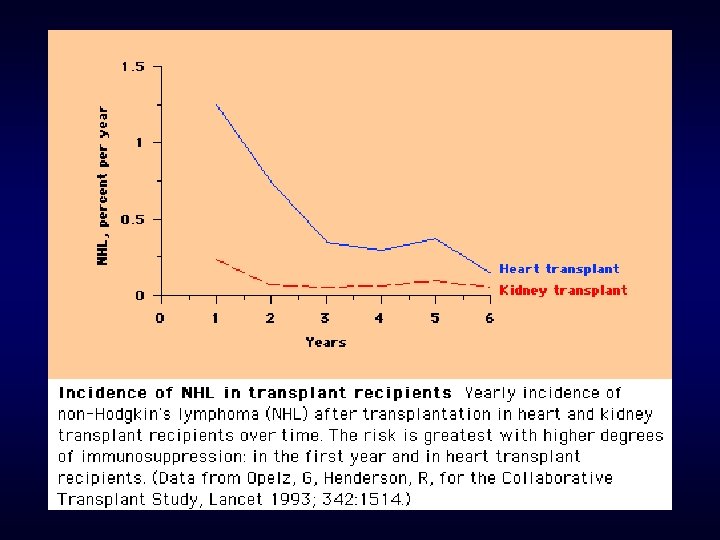
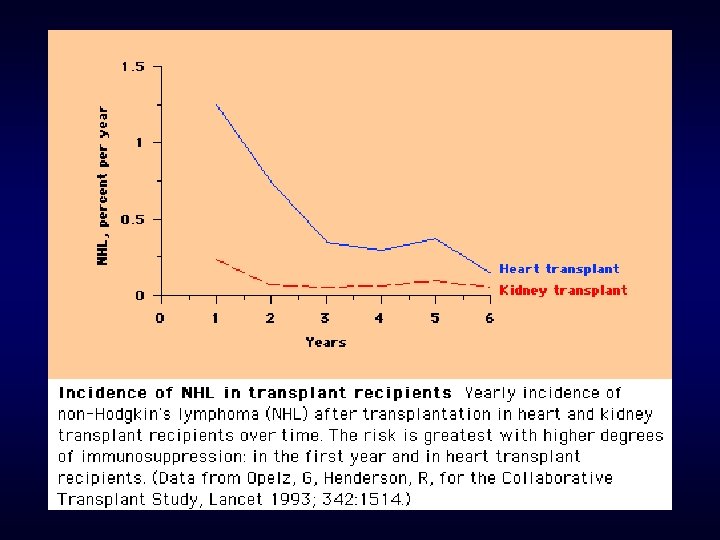
Lymphoma and Post Transplant Lymphoproliferative Disorder (PTLD) • Prevalence: 1 -3% in adult LTx 20% in pediatric LTx within 2 y of LTx • Most are of host origin 3 types of EBV-related PTLD: - Mononucleosa like syndrome: benign polyclonal proliferation - MN syndrome + polyclonal Bcell proliferation with early malignant transformation - Localised NH-lymphoma => diffuse progressive and fatal Weissmann. Am J Clin Pathol 1995. Hanto. Annu Rev Med 1995. Petit. Transplantation 2002. Hjelle. Transplantation 1989. Nalesnik. Am J Pathol 1988 (1)
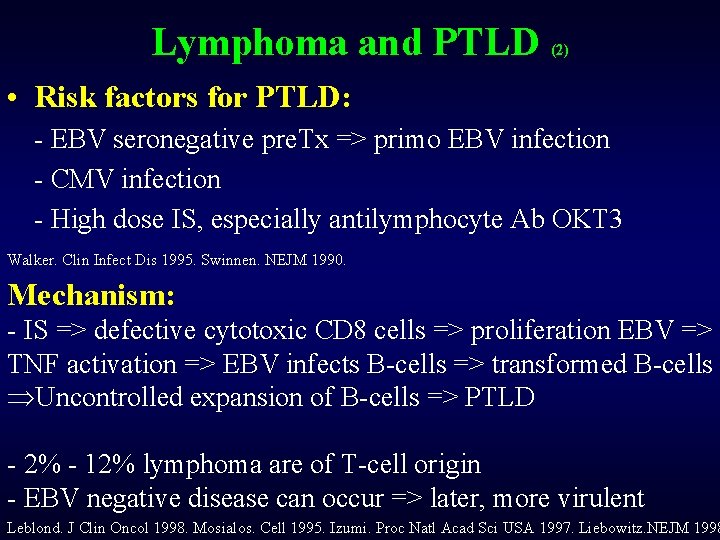
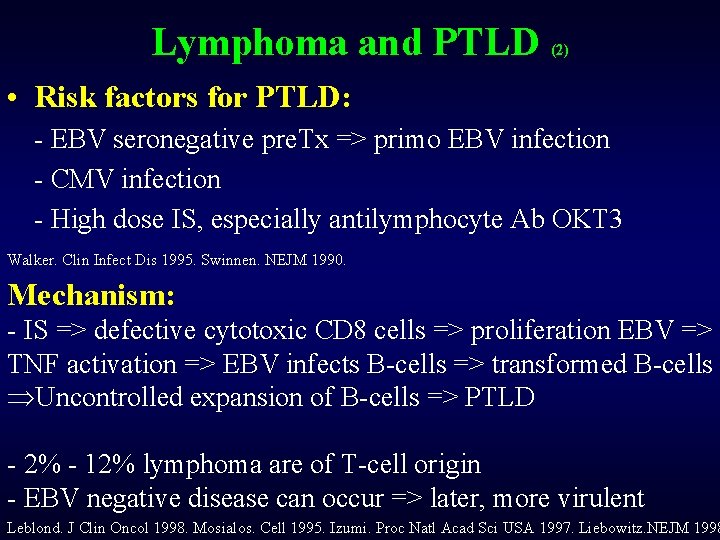
Lymphoma and PTLD (2) • Risk factors for PTLD: - EBV seronegative pre. Tx => primo EBV infection - CMV infection - High dose IS, especially antilymphocyte Ab OKT 3 Walker. Clin Infect Dis 1995. Swinnen. NEJM 1990. Mechanism: - IS => defective cytotoxic CD 8 cells => proliferation EBV => TNF activation => EBV infects B-cells => transformed B-cells ÞUncontrolled expansion of B-cells => PTLD - 2% - 12% lymphoma are of T-cell origin - EBV negative disease can occur => later, more virulent Leblond. J Clin Oncol 1998. Mosialos. Cell 1995. Izumi. Proc Natl Acad Sci USA 1997. Liebowitz. NEJM 1998
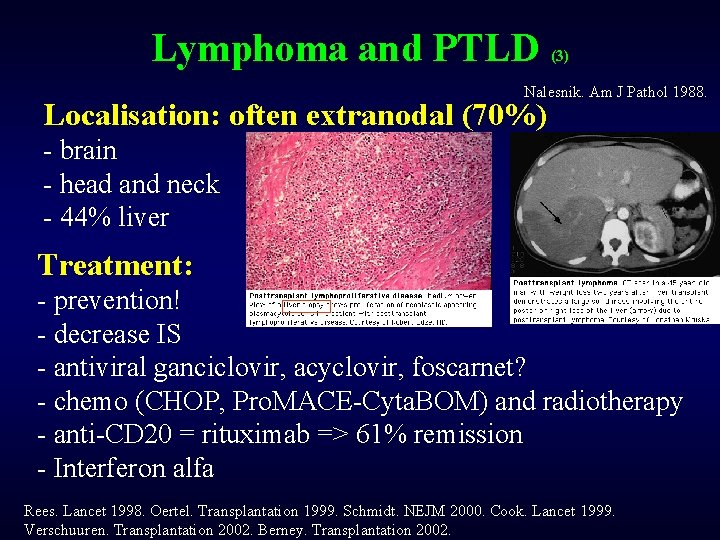
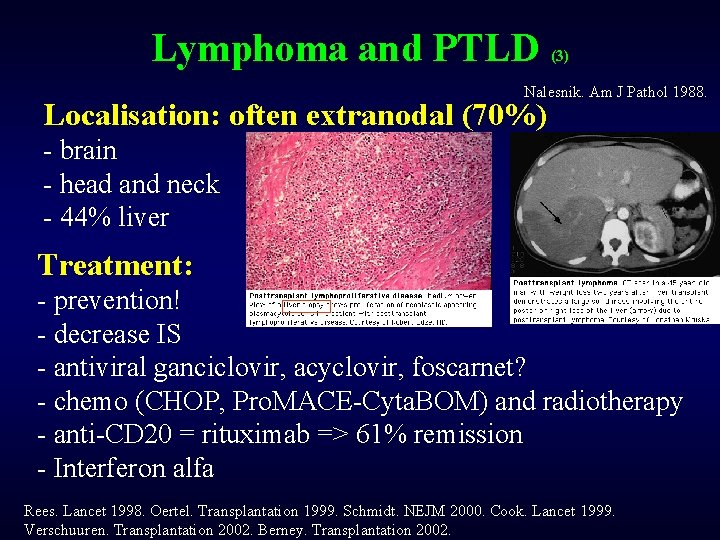
Lymphoma and PTLD (3) Nalesnik. Am J Pathol 1988. Localisation: often extranodal (70%) - brain - head and neck - 44% liver Treatment: - prevention! - decrease IS - antiviral ganciclovir, acyclovir, foscarnet? - chemo (CHOP, Pro. MACE-Cyta. BOM) and radiotherapy - anti-CD 20 = rituximab => 61% remission - Interferon alfa Rees. Lancet 1998. Oertel. Transplantation 1999. Schmidt. NEJM 2000. Cook. Lancet 1999. Verschuuren. Transplantation 2002. Berney. Transplantation 2002.
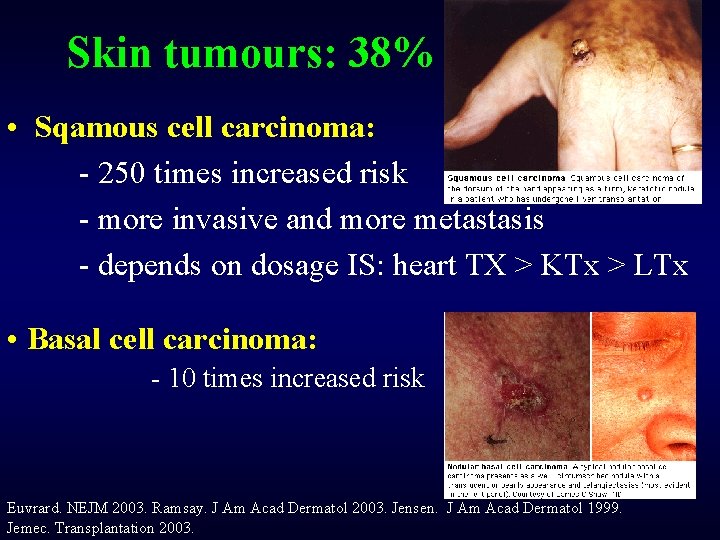
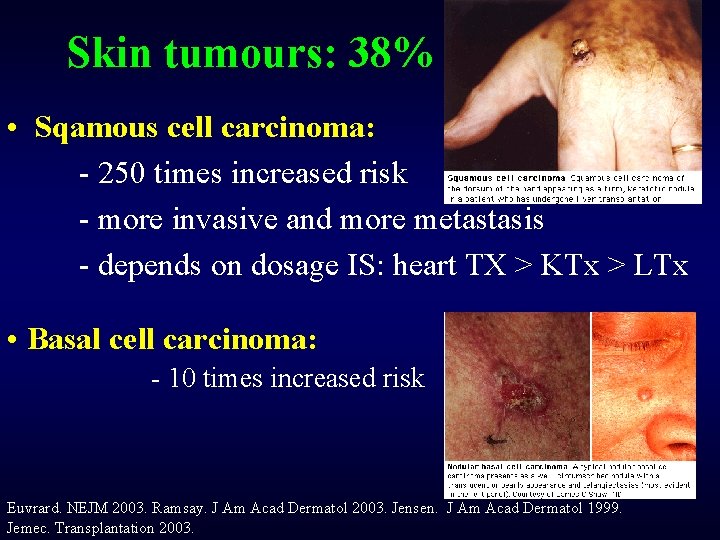
Skin tumours: 38% • Sqamous cell carcinoma: - 250 times increased risk - more invasive and more metastasis - depends on dosage IS: heart TX > KTx > LTx • Basal cell carcinoma: - 10 times increased risk Euvrard. NEJM 2003. Ramsay. J Am Acad Dermatol 2003. Jensen. J Am Acad Dermatol 1999. Jemec. Transplantation 2003.
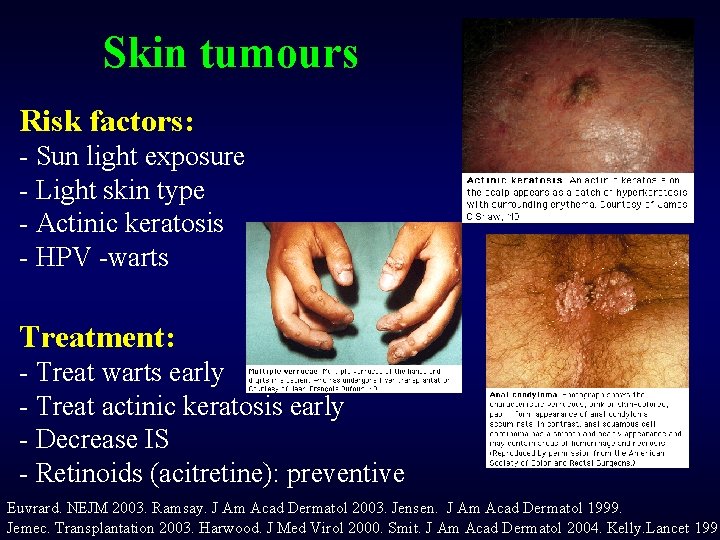
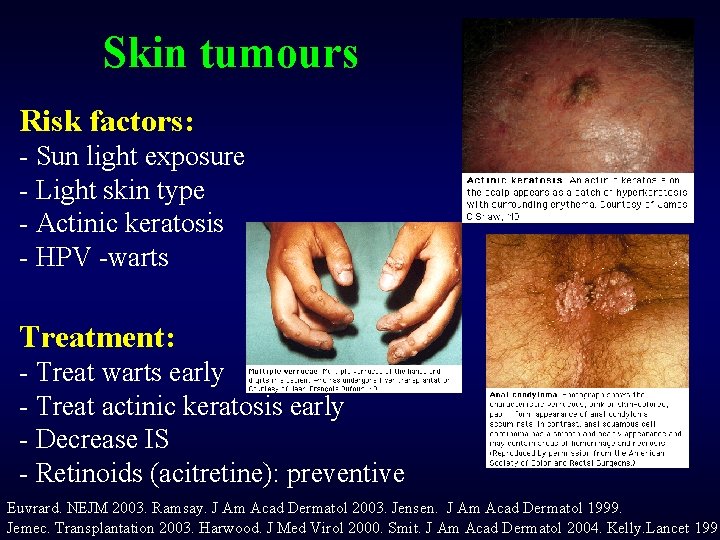
Skin tumours Risk factors: - Sun light exposure - Light skin type - Actinic keratosis - HPV -warts Treatment: - Treat warts early - Treat actinic keratosis early - Decrease IS - Retinoids (acitretine): preventive Euvrard. NEJM 2003. Ramsay. J Am Acad Dermatol 2003. Jensen. J Am Acad Dermatol 1999. Jemec. Transplantation 2003. Harwood. J Med Virol 2000. Smit. J Am Acad Dermatol 2004. Kelly. Lancet 1991

Infectious complications after liver transplantation
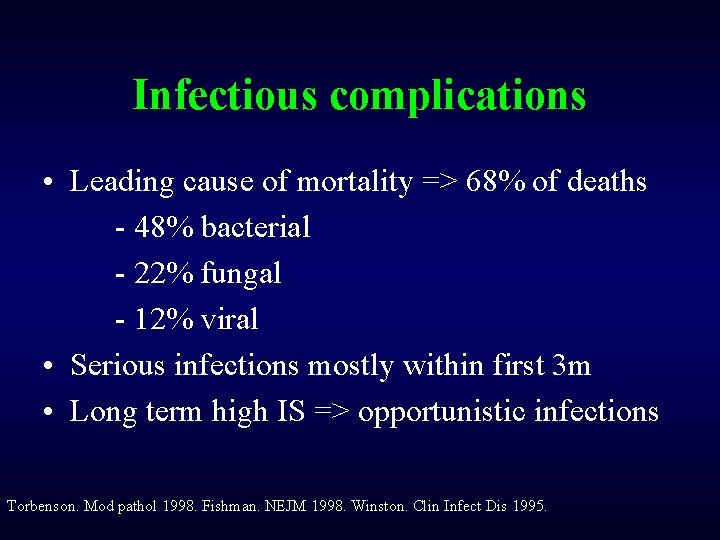
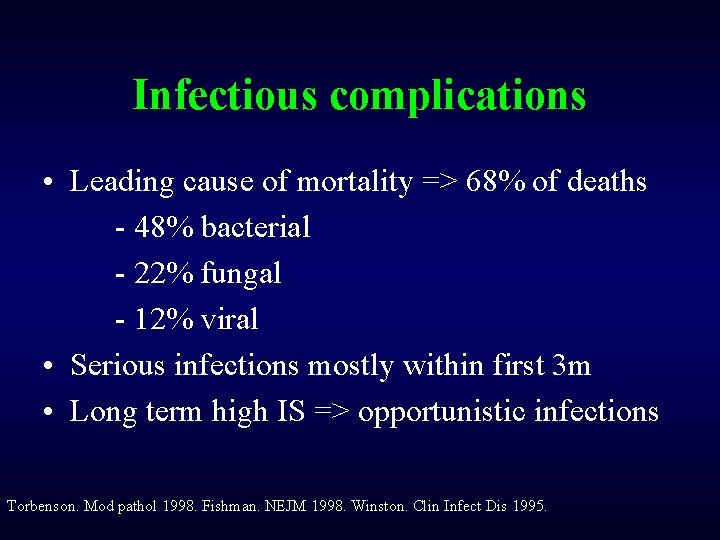
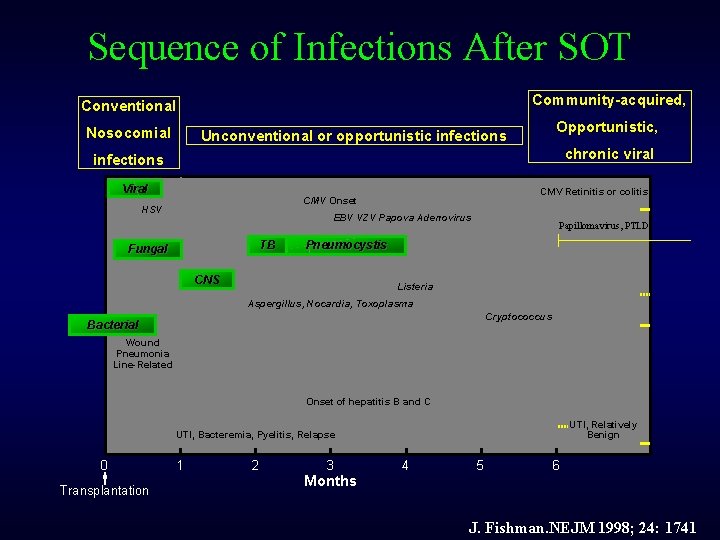
Infectious complications • Leading cause of mortality => 68% of deaths - 48% bacterial - 22% fungal - 12% viral • Serious infections mostly within first 3 m • Long term high IS => opportunistic infections Torbenson. Mod pathol 1998. Fishman. NEJM 1998. Winston. Clin Infect Dis 1995.
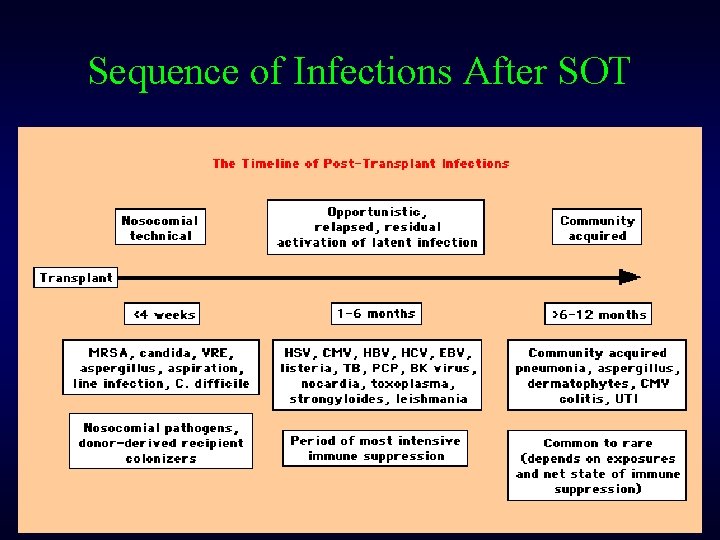
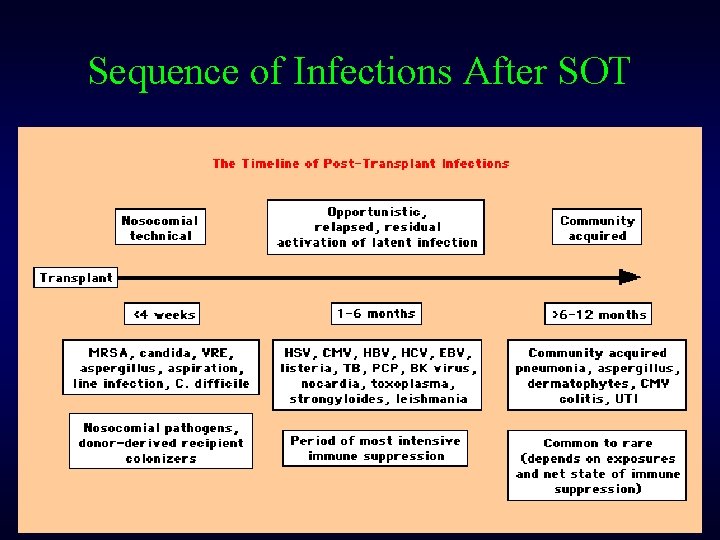
Sequence of Infections After SOT
Bacterial infections • Legionella: pneumonia, diarrhea, pulmonary cavitations • Listeria: in milk, meat => bacteremia, meningitis => ampicillin • Nocardia: lung, CNS, skin => sulfonamide • TBC: 0. 9 – 2. 3% after LTx Torbenson. Mod pathol 1998. Fishman. NEJM 1998. Winston. Clin Infect Dis 1995.
Fungal infections Risk factors for fungal infections: - Re-transplantation - High need of peroperative blood transfusion - Creatinine > 2 mg/dl - Bilirubin > 10 mg/dl - Choledocho-jejunostomy - Previous colonisation • Candida: abdominal infections • Aspergillus: lung and brain => profylaxis fluconazole: 23% => 5. 6% • Pneumocystic carinii: 2 -6 m post-Tx dyspnea, hypoxia, fever, cough =>TMP/SMZ, dapsone, pentamidine Collins. J Infect Dis 1994. Paya. Clin Infect Dis 1993. Fishman. NEJM 1998. Winston. Clin Infect Dis 1995.
Viral infections (1) • CMV: - Primo infection by donated allograft or sero+ blood products - Reactivation endogenous CMV • Risk for CMV infection: - D+ /R- High IS, especially antilymphocyte OKT 3 • Mechanism: infection, rejection, IS , OKT 3 => increase in TNFalfa => reactivation CMV => direct immunosuppressive properties => increased risk for bacterial, fungal and EBV infection + risk rejection Torbenson. Mod pathol 1998. Fishman. NEJM 1998. Winston. Clin Infect Dis 1995. Paya. J Hepatol 1993.
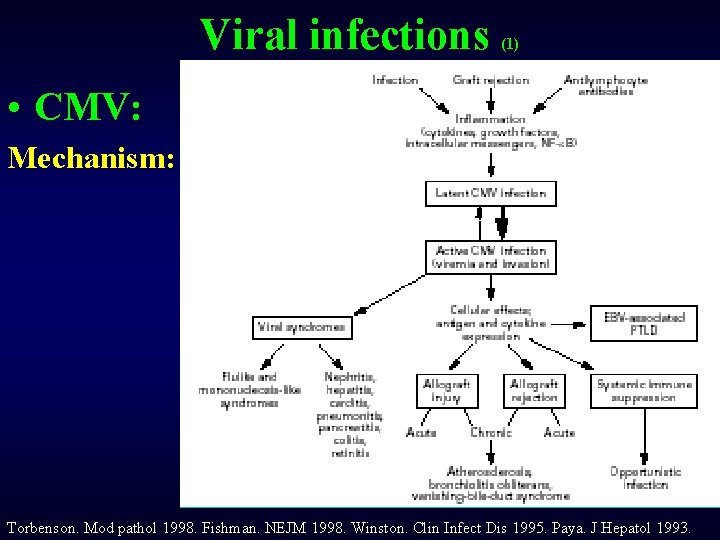
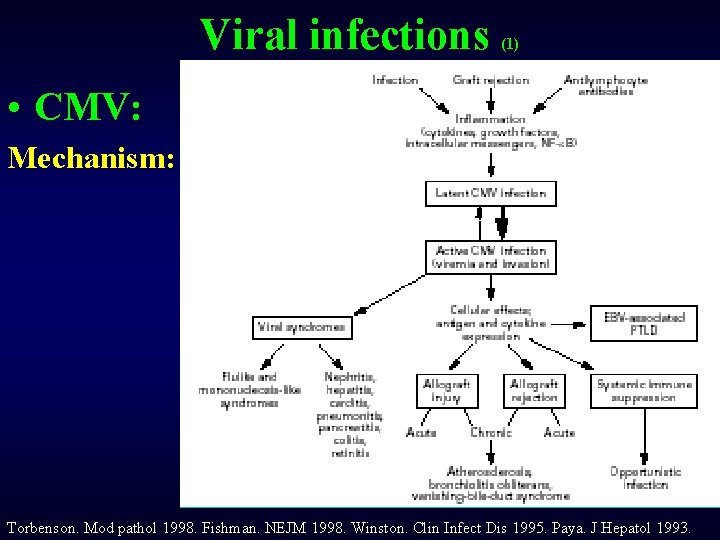
Viral infections (1) • CMV: Mechanism: Torbenson. Mod pathol 1998. Fishman. NEJM 1998. Winston. Clin Infect Dis 1995. Paya. J Hepatol 1993.
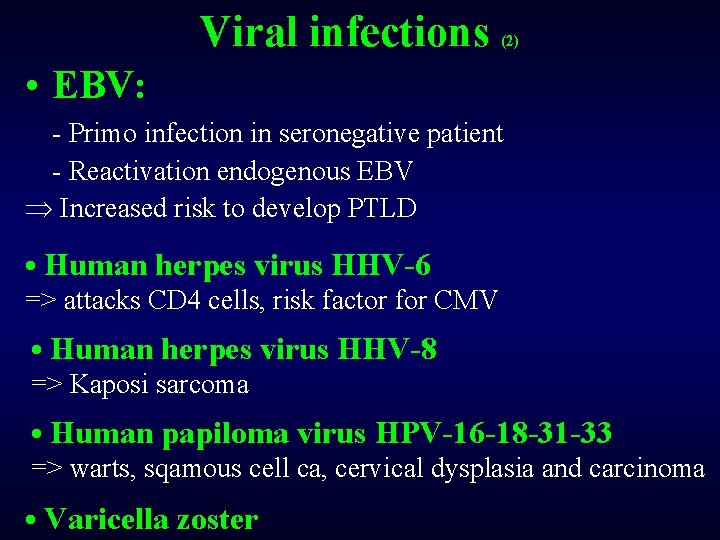
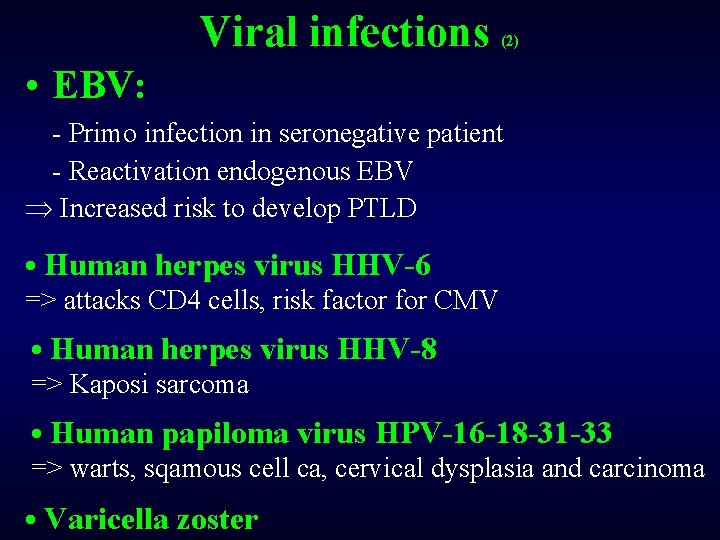
Viral infections (2) • EBV: - Primo infection in seronegative patient - Reactivation endogenous EBV Þ Increased risk to develop PTLD • Human herpes virus HHV-6 => attacks CD 4 cells, risk factor for CMV • Human herpes virus HHV-8 => Kaposi sarcoma • Human papiloma virus HPV-16 -18 -31 -33 => warts, sqamous cell ca, cervical dysplasia and carcinoma • Varicella zoster
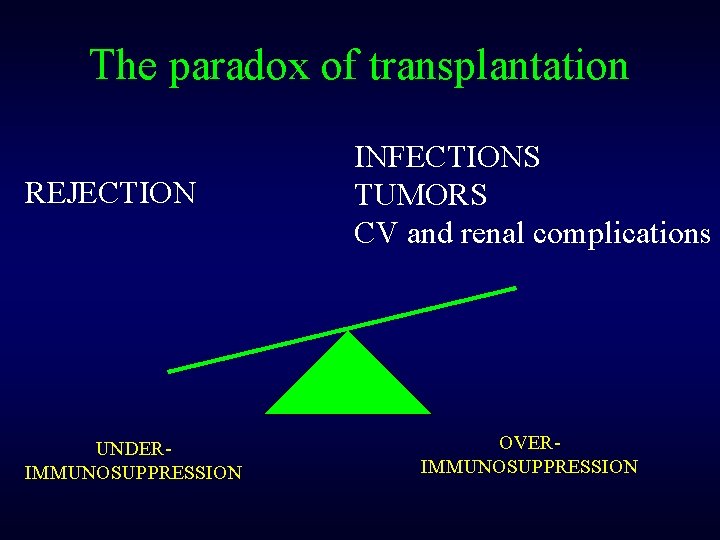
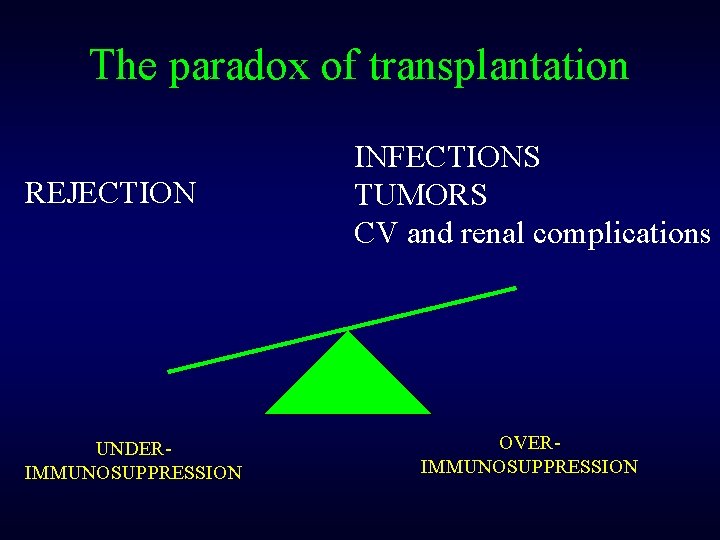
The paradox of transplantation REJECTION UNDERIMMUNOSUPPRESSION INFECTIONS TUMORS CV and renal complications OVERIMMUNOSUPPRESSION
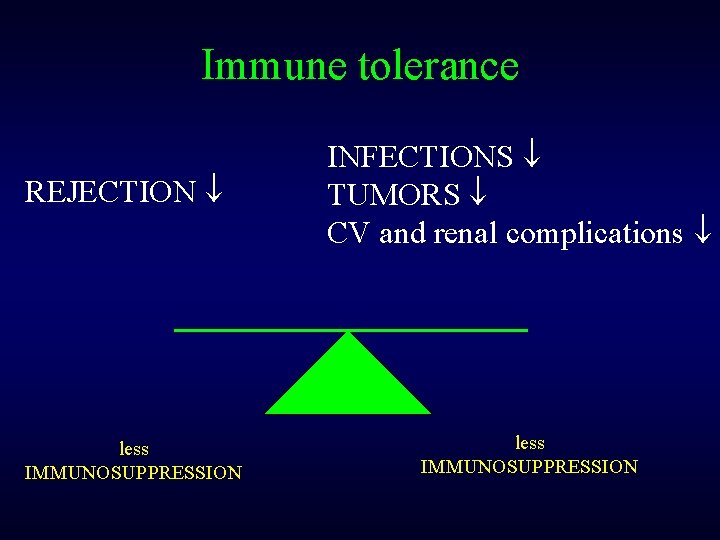
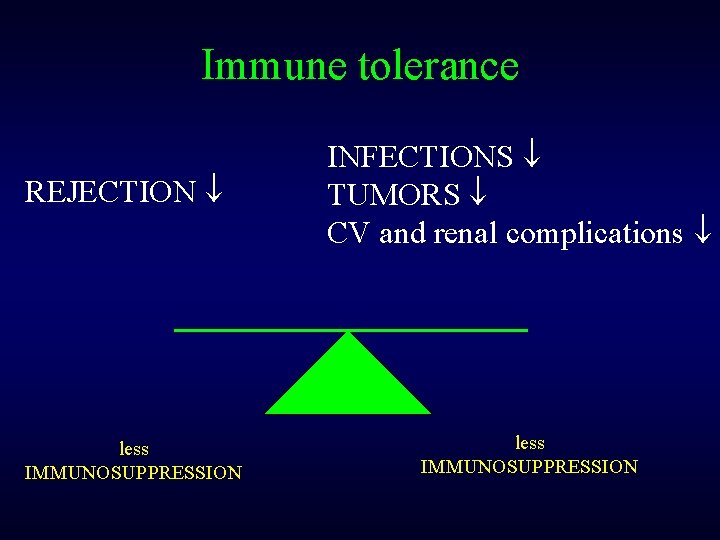
Immune tolerance REJECTION less IMMUNOSUPPRESSION INFECTIONS TUMORS CV and renal complications less IMMUNOSUPPRESSION
Renal function measurements • Creatinine: false low due to muscle atrophy => Cockeroft and Gault: overestimation of GFR • Cr EDTA
Neurological complications after liver transplantation
Neurological disorders • 10 -50% neurological complications post LTx first week Etiologies: - Vascular events: 52% - Infections: 18% - IS associated leuko-encephalopathy: 12% - Central pontine myelinolyse: 8% - Malignancy: 3% - Miscellaneous: 7% Bonham. Transplantation 1998. Adams. Lancet 1987
Neurological disorders Causes: - IV administration immune suppression - Postop hypercoagulability - Periop cardiovascular instability Symptoms: -ciclo / FK: peripheral neuropathie: tremor, shooting pain in limbs, carpal tunnel syndrome (6% in PBC) - headache/migraine: not always relieved by IS Treatment: Calcium antagonists, beta-blockers, tricyclic antidepressants

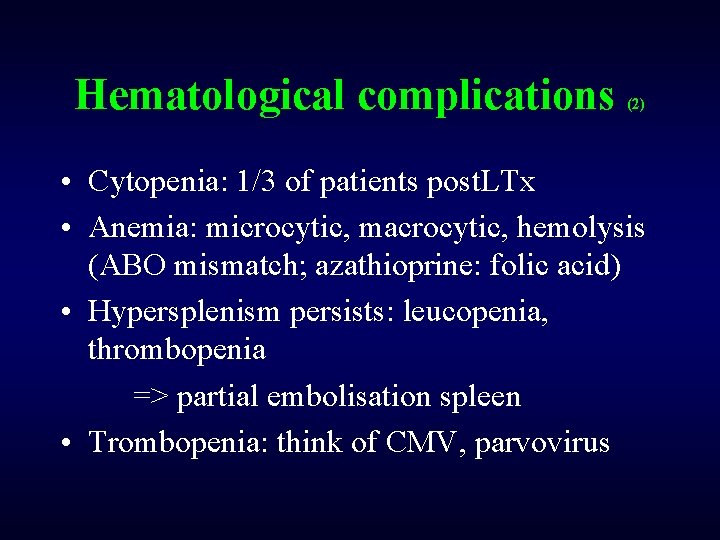
Hematological complications after liver transplantation
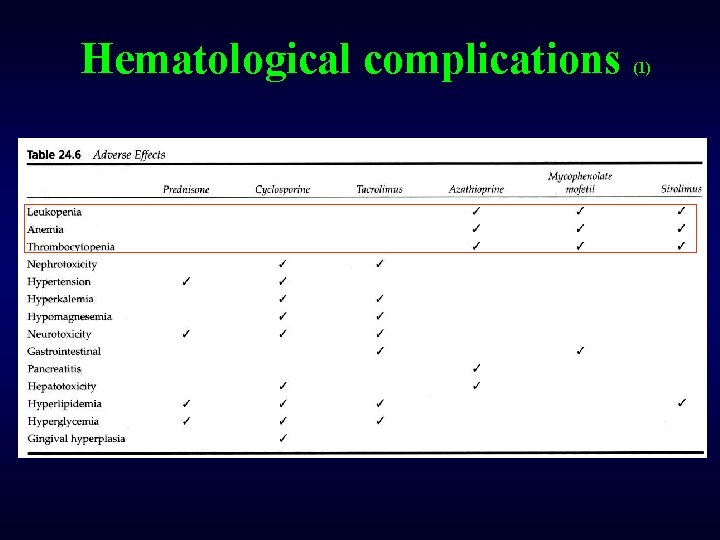
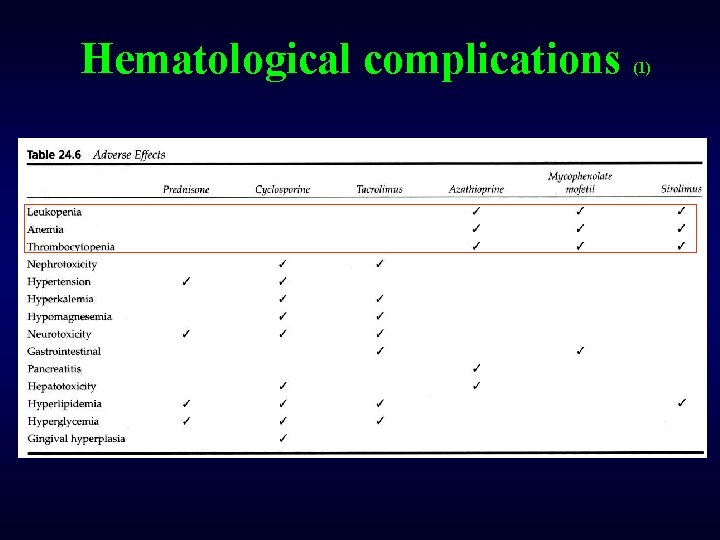
Hematological complications (1)
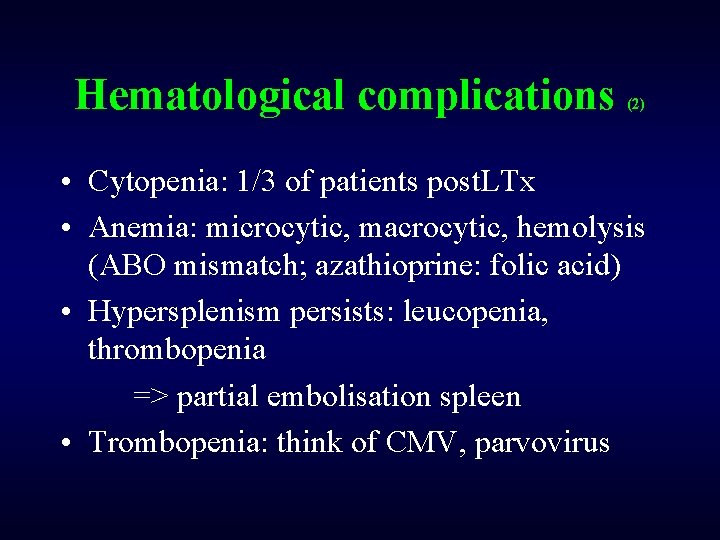
Hematological complications (2) • Cytopenia: 1/3 of patients post. LTx • Anemia: microcytic, macrocytic, hemolysis (ABO mismatch; azathioprine: folic acid) • Hypersplenism persists: leucopenia, thrombopenia => partial embolisation spleen • Trombopenia: think of CMV, parvovirus
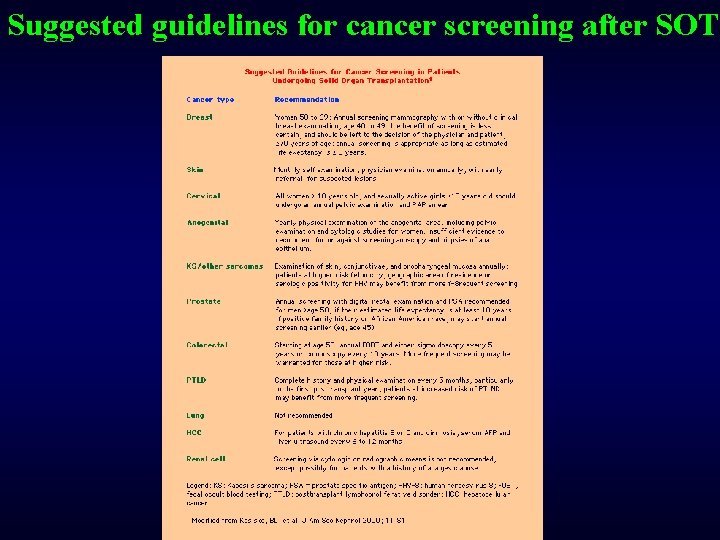
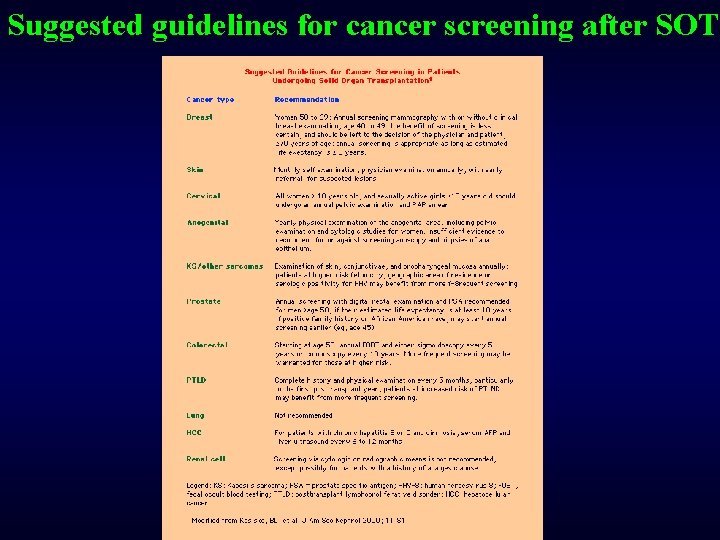
Suggested guidelines for cancer screening after SOT
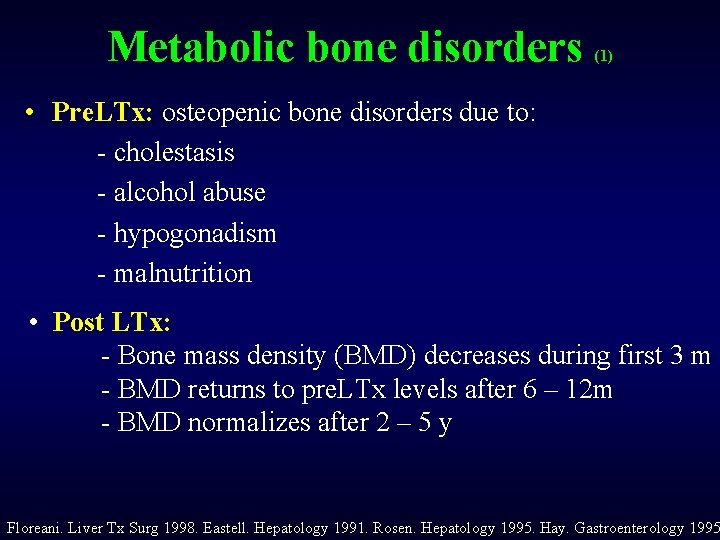
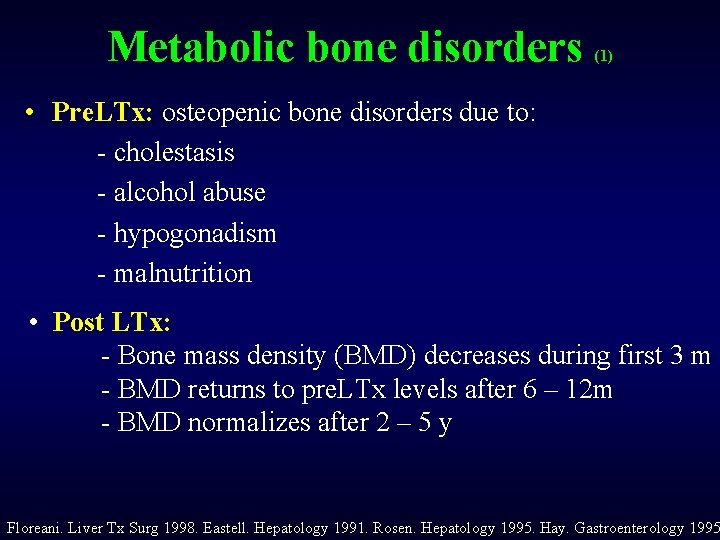
Metabolic bone disorders (1) • Pre. LTx: osteopenic bone disorders due to: - cholestasis - alcohol abuse - hypogonadism - malnutrition • Post LTx: - Bone mass density (BMD) decreases during first 3 m - BMD returns to pre. LTx levels after 6 – 12 m - BMD normalizes after 2 – 5 y Floreani. Liver Tx Surg 1998. Eastell. Hepatology 1991. Rosen. Hepatology 1995. Hay. Gastroenterology 1995

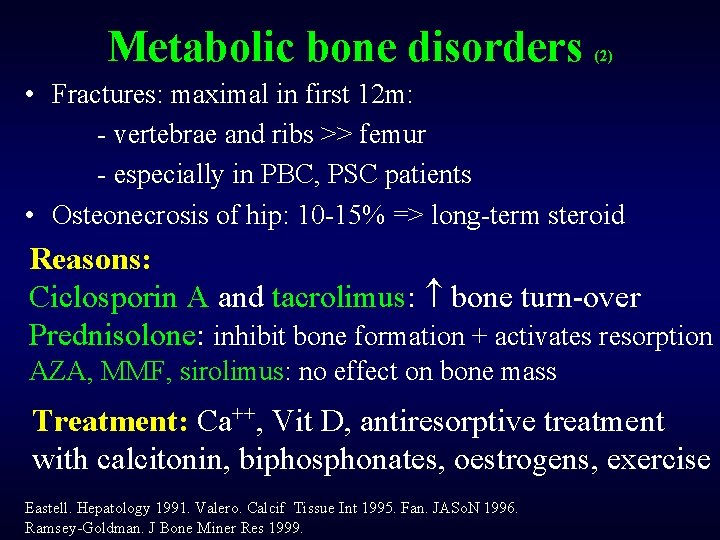
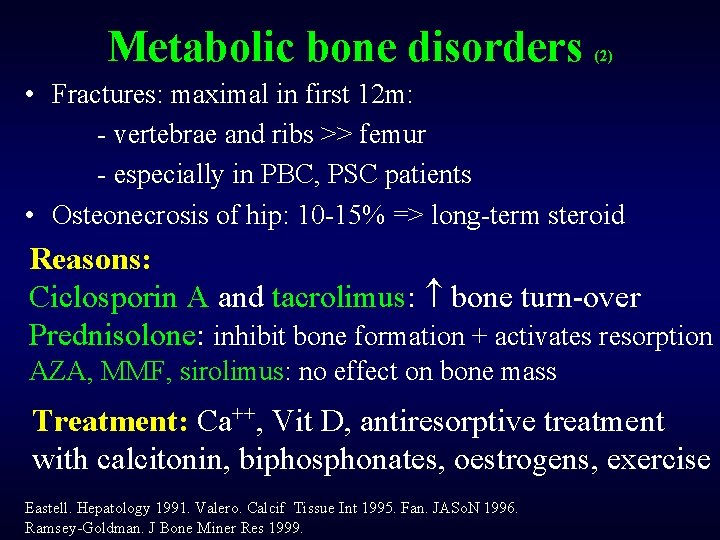
Metabolic bone disorders (2) • Fractures: maximal in first 12 m: - vertebrae and ribs >> femur - especially in PBC, PSC patients • Osteonecrosis of hip: 10 -15% => long-term steroid Reasons: Ciclosporin A and tacrolimus: bone turn-over Prednisolone: inhibit bone formation + activates resorption AZA, MMF, sirolimus: no effect on bone mass Treatment: Ca++, Vit D, antiresorptive treatment with calcitonin, biphosphonates, oestrogens, exercise Eastell. Hepatology 1991. Valero. Calcif Tissue Int 1995. Fan. JASo. N 1996. Ramsey-Goldman. J Bone Miner Res 1999.

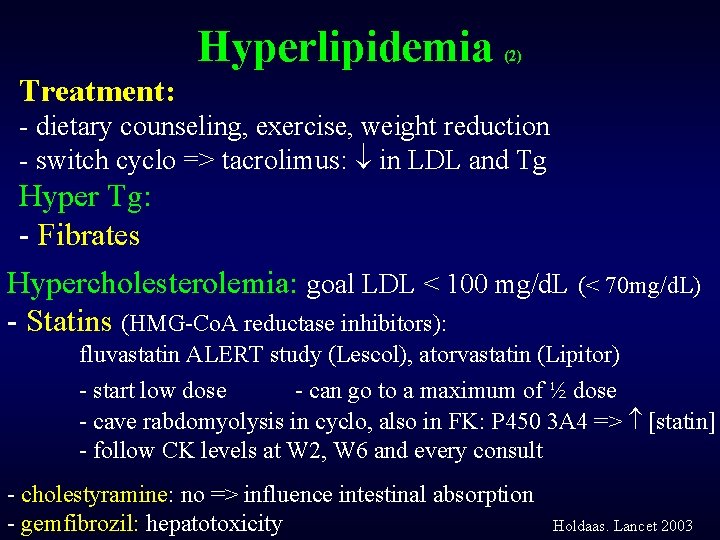
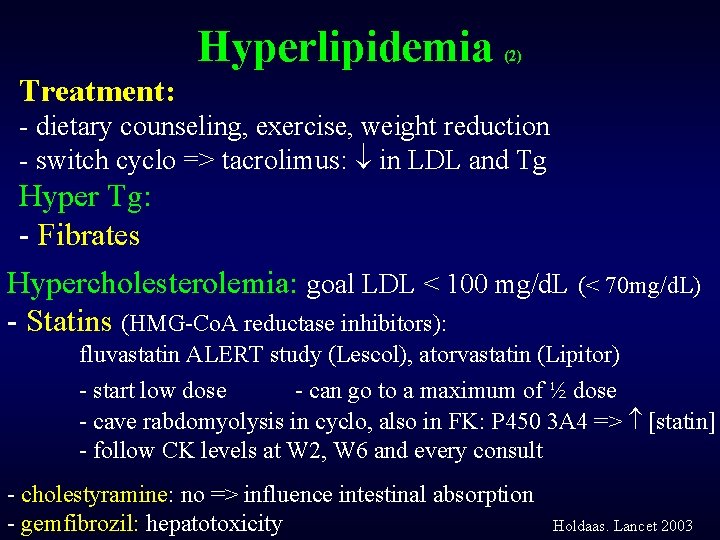
Hyperlipidemia (2) Treatment: - dietary counseling, exercise, weight reduction - switch cyclo => tacrolimus: in LDL and Tg Hyper Tg: - Fibrates Hypercholesterolemia: goal LDL < 100 mg/d. L (< 70 mg/d. L) - Statins (HMG-Co. A reductase inhibitors): fluvastatin ALERT study (Lescol), atorvastatin (Lipitor) - start low dose - can go to a maximum of ½ dose - cave rabdomyolysis in cyclo, also in FK: P 450 3 A 4 => [statin] - follow CK levels at W 2, W 6 and every consult - cholestyramine: no => influence intestinal absorption - gemfibrozil: hepatotoxicity Holdaas. Lancet 2003
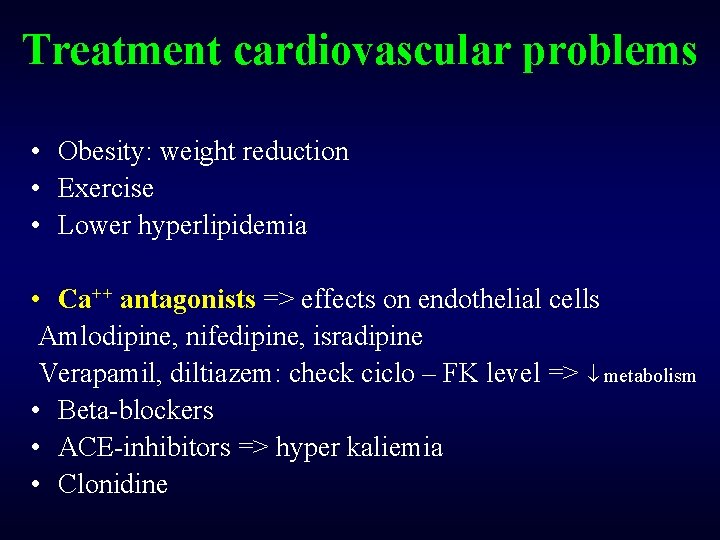
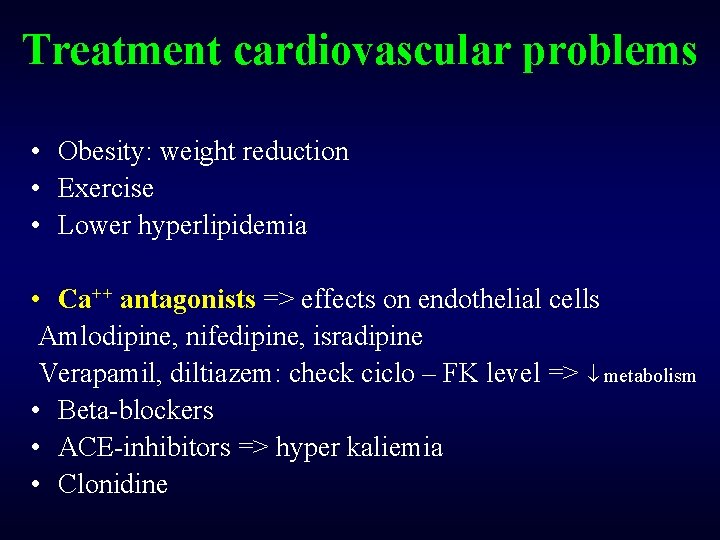
Treatment cardiovascular problems • Obesity: weight reduction • Exercise • Lower hyperlipidemia • Ca++ antagonists => effects on endothelial cells Amlodipine, nifedipine, isradipine Verapamil, diltiazem: check ciclo – FK level => metabolism • Beta-blockers • ACE-inhibitors => hyper kaliemia • Clonidine
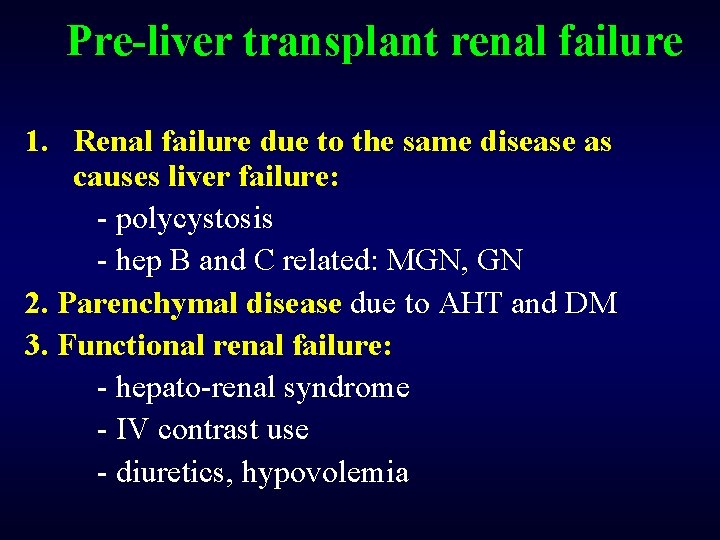
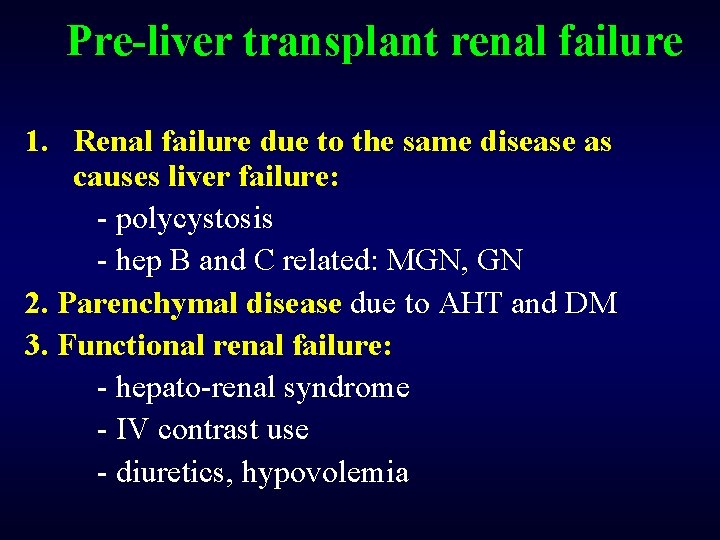
Pre-liver transplant renal failure 1. Renal failure due to the same disease as causes liver failure: - polycystosis - hep B and C related: MGN, GN 2. Parenchymal disease due to AHT and DM 3. Functional renal failure: - hepato-renal syndrome - IV contrast use - diuretics, hypovolemia
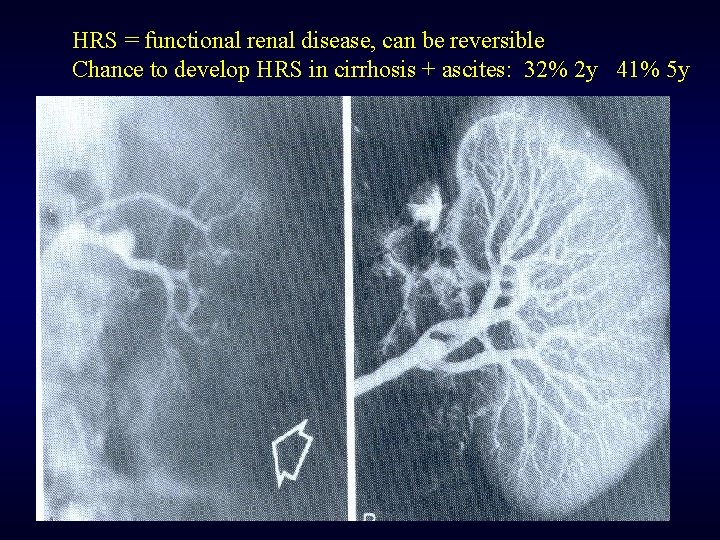
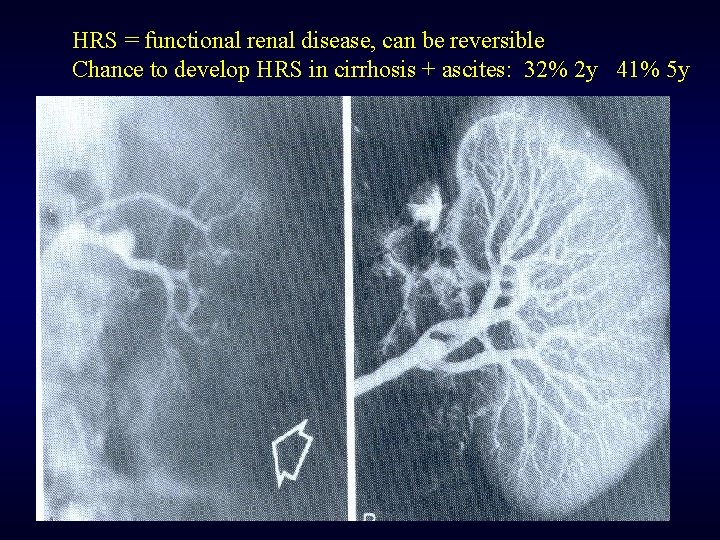
HRS = functional renal disease, can be reversible Chance to develop HRS in cirrhosis + ascites: 32% 2 y 41% 5 y
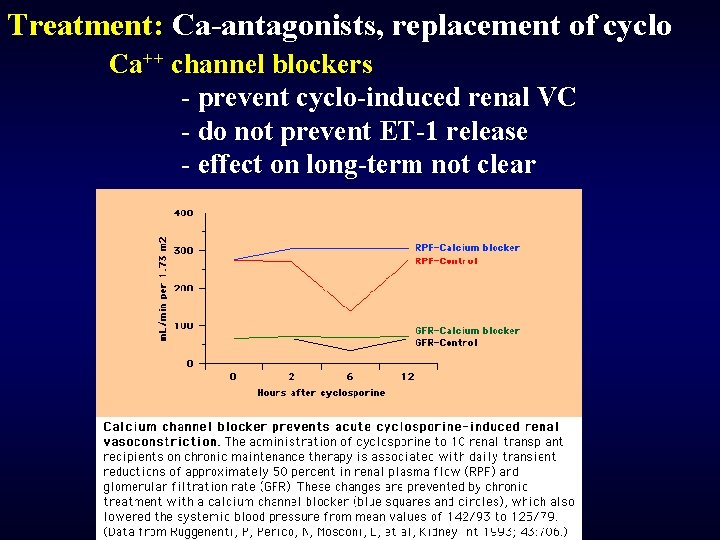
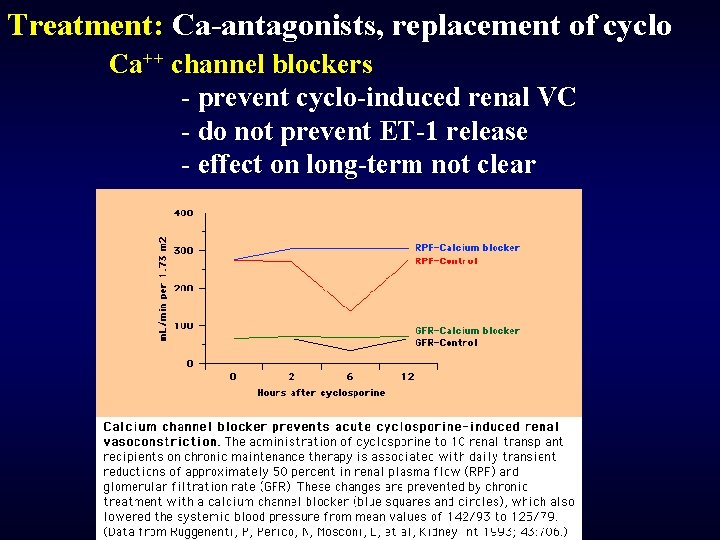
Treatment: Ca-antagonists, replacement of cyclo Ca++ channel blockers - prevent cyclo-induced renal VC - do not prevent ET-1 release - effect on long-term not clear
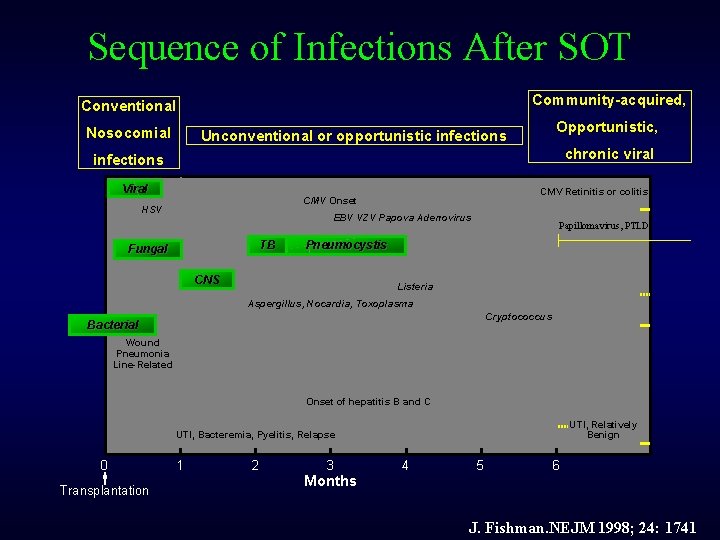
Sequence of Infections After SOT Community-acquired, Conventional Nosocomial Opportunistic, Unconventional or opportunistic infections chronic viral infections Viral CMV Retinitis or colitis CMV Onset HSV EBV VZV Papova Adenovirus TB Fungal Papillomavirus, PTLD Pneumocystis CNS Listeria Aspergillus, Nocardia, Toxoplasma Cryptococcus Bacterial Wound Pneumonia Line-Related Onset of hepatitis B and C UTI, Relatively Benign UTI, Bacteremia, Pyelitis, Relapse 0 Transplantation 1 2 3 Months 4 5 6 J. Fishman. NEJM 1998; 24: 1741

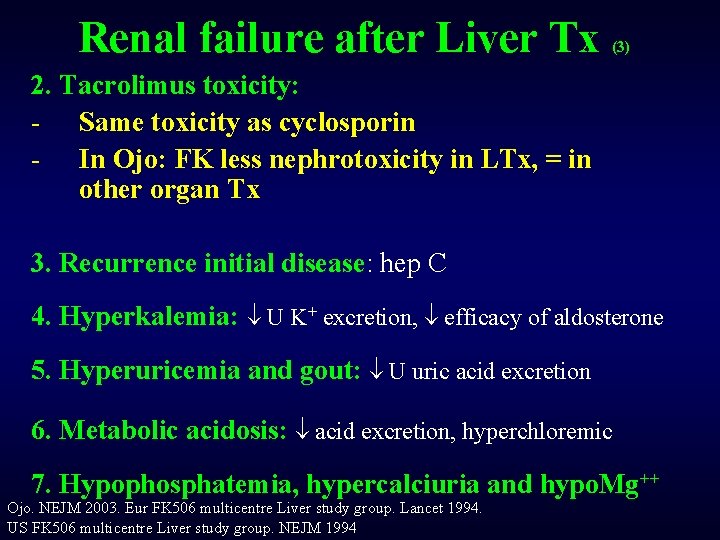
Renal failure after Liver Tx (3) 2. Tacrolimus toxicity: - Same toxicity as cyclosporin - In Ojo: FK less nephrotoxicity in LTx, = in other organ Tx 3. Recurrence initial disease: hep C 4. Hyperkalemia: U K+ excretion, efficacy of aldosterone 5. Hyperuricemia and gout: U uric acid excretion 6. Metabolic acidosis: acid excretion, hyperchloremic 7. Hypophosphatemia, hypercalciuria and hypo. Mg++ Ojo. NEJM 2003. Eur FK 506 multicentre Liver study group. Lancet 1994. US FK 506 multicentre Liver study group. NEJM 1994
 Primary immune response and secondary immune response
Primary immune response and secondary immune response Lts stable
Lts stable Thomas silverstein art
Thomas silverstein art After me after me after me
After me after me after me If anyone desires to come after me
If anyone desires to come after me Stem cell phuket
Stem cell phuket Patrick evrard mont godinne
Patrick evrard mont godinne Cultural transposition
Cultural transposition Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Transplant
Transplant Law of transplantation
Law of transplantation Complications after cesarean section
Complications after cesarean section Fike water mist
Fike water mist Fire suppression rating schedule
Fire suppression rating schedule Nitin ventures fze
Nitin ventures fze Cephalosporins
Cephalosporins Suppression clothes
Suppression clothes Superegooo
Superegooo Dexamethasone suppression test
Dexamethasone suppression test Piranha fire suppression system
Piranha fire suppression system Pyrogen fire suppression
Pyrogen fire suppression Articulatory suppression
Articulatory suppression Novec vs inergen
Novec vs inergen Foam suppression system
Foam suppression system Kiwiblog's david farrar
Kiwiblog's david farrar Reinforced robot humor suppression pump
Reinforced robot humor suppression pump Superheterodyne wave analyzer
Superheterodyne wave analyzer Any substance capable of provoking an immune response
Any substance capable of provoking an immune response Innate immunity first line of defense
Innate immunity first line of defense Muscle type
Muscle type A pericardiophrenica
A pericardiophrenica Unsaturated alcohol crossword clue
Unsaturated alcohol crossword clue Overreactions of the immune system
Overreactions of the immune system Oobean
Oobean Hit heparin
Hit heparin Ap biology immune system
Ap biology immune system Immune reconstitution therapy
Immune reconstitution therapy Cellular immune response
Cellular immune response Lupus
Lupus Defination of immune system
Defination of immune system Immune checkpoint inhibitors mechanism of action
Immune checkpoint inhibitors mechanism of action Chapter 35 immune system and disease
Chapter 35 immune system and disease Maladie auto immune connectivite
Maladie auto immune connectivite Lymph diagram
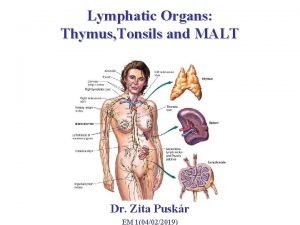
Lymph diagram Hepatite auto immune fmc
Hepatite auto immune fmc Immune system def
Immune system def Lymphatic vs immune system
Lymphatic vs immune system Chapter 24 the immune and lymphatic systems and cancer
Chapter 24 the immune and lymphatic systems and cancer Spalding sign
Spalding sign Immune complex
Immune complex What is the third line of defense in the immune system
What is the third line of defense in the immune system The main function of immune system
The main function of immune system Adcc immune
Adcc immune Primary immune response
Primary immune response Immune reconstitution inflammatory syndrome
Immune reconstitution inflammatory syndrome Immune thrombocytopenia vaccine
Immune thrombocytopenia vaccine Chapter 55 care of the patient with an immune disorder
Chapter 55 care of the patient with an immune disorder Immune thrombocytopenic purpura
Immune thrombocytopenic purpura Thymus
Thymus Immune defintion
Immune defintion Mbg453
Mbg453