Learning aim D Investigate the roles of professionals
- Slides: 32
Learning aim D: Investigate the roles of professionals and how they work together to provide the care and support necessary to meet individual needs ©Outstanding Resources 2017
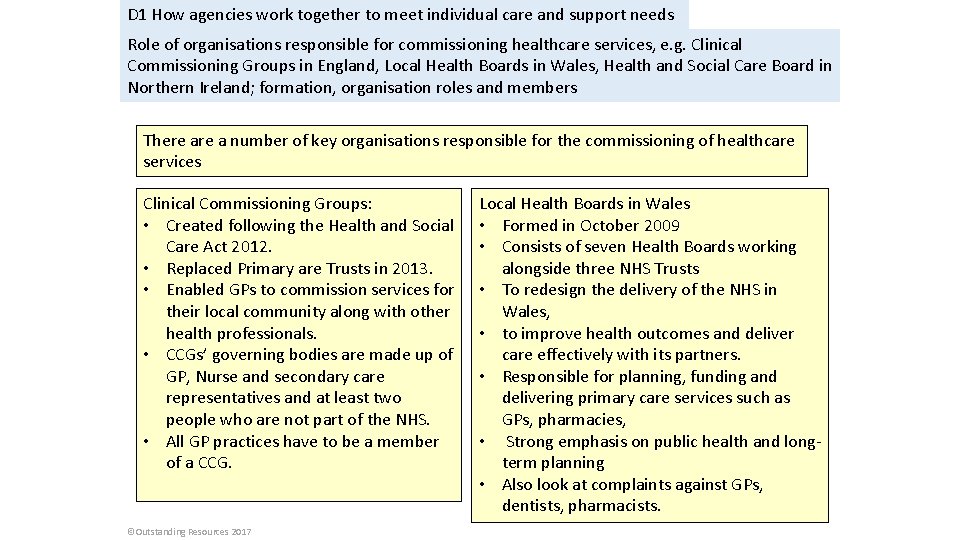
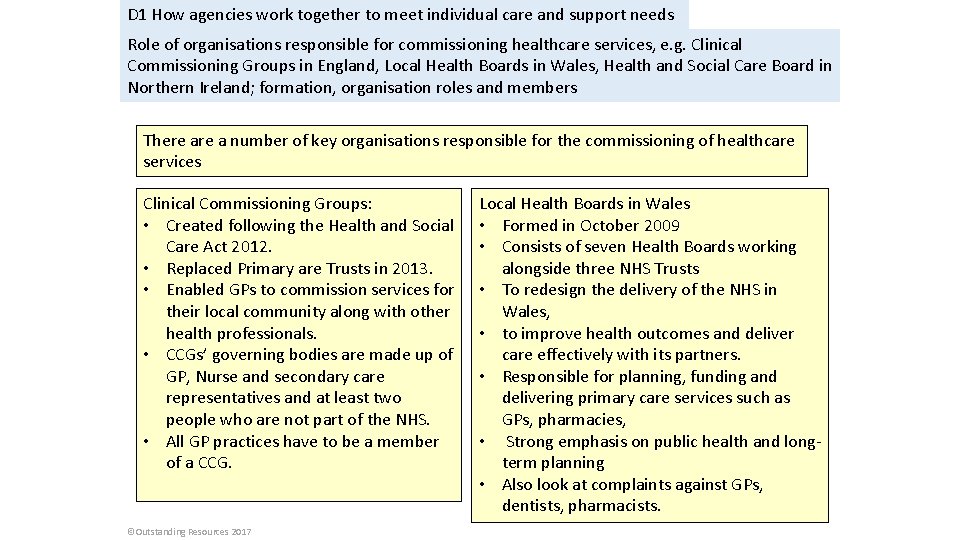
D 1 How agencies work together to meet individual care and support needs Role of organisations responsible for commissioning healthcare services, e. g. Clinical Commissioning Groups in England, Local Health Boards in Wales, Health and Social Care Board in Northern Ireland; formation, organisation roles and members There a number of key organisations responsible for the commissioning of healthcare services Clinical Commissioning Groups: • Created following the Health and Social Care Act 2012. • Replaced Primary are Trusts in 2013. • Enabled GPs to commission services for their local community along with other health professionals. • CCGs’ governing bodies are made up of GP, Nurse and secondary care representatives and at least two people who are not part of the NHS. • All GP practices have to be a member of a CCG. ©Outstanding Resources 2017 Local Health Boards in Wales • Formed in October 2009 • Consists of seven Health Boards working alongside three NHS Trusts • To redesign the delivery of the NHS in Wales, • to improve health outcomes and deliver care effectively with its partners. • Responsible for planning, funding and delivering primary care services such as GPs, pharmacies, • Strong emphasis on public health and longterm planning • Also look at complaints against GPs, dentists, pharmacists.
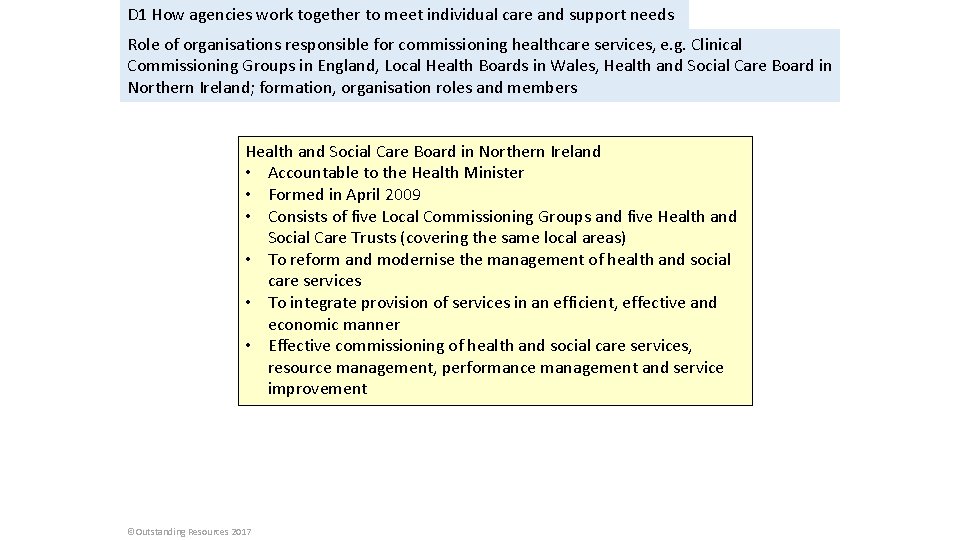
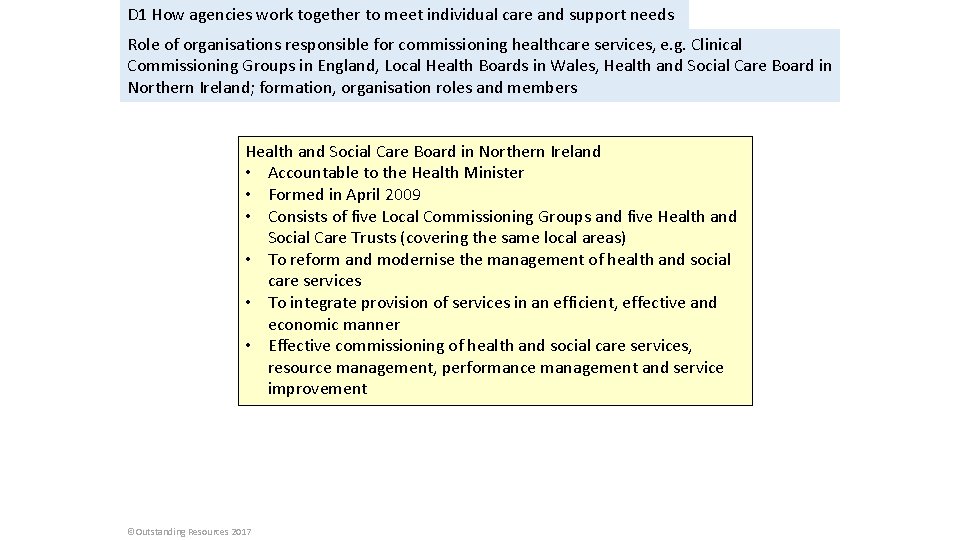
D 1 How agencies work together to meet individual care and support needs Role of organisations responsible for commissioning healthcare services, e. g. Clinical Commissioning Groups in England, Local Health Boards in Wales, Health and Social Care Board in Northern Ireland; formation, organisation roles and members Health and Social Care Board in Northern Ireland • Accountable to the Health Minister • Formed in April 2009 • Consists of five Local Commissioning Groups and five Health and Social Care Trusts (covering the same local areas) • To reform and modernise the management of health and social care services • To integrate provision of services in an efficient, effective and economic manner • Effective commissioning of health and social care services, resource management, performance management and service improvement ©Outstanding Resources 2017
D 1 How agencies work together to meet individual care and support needs Role of organisations responsible for commissioning social care services, e. g. local authorities. • Local authorities’ statutory responsibilities for public health services are set out in the Health and Social Care Act 2012 • Local authorities commission social services to achieve personalised, community based support that promotes health and wellbeing by using evidence, local knowledge, skills and resources as best they can. • Local authorities work in close partnership with other organisations, such as housing and NHS partners, using guidance such as the Adult Social Care Outcomes Framework, Making it Real statements and the Public Health Outcomes Framework. ©Outstanding Resources 2017
D 1 How agencies work together to meet individual care and support needs Role of bodies responsible for integrating health and social care, e. g. Health and Wellbeing Boards (HWB). • Health and wellbeing boards were established under the Health and Social Care Act 2012 to act as a forum in which key leaders from the local health and care system could work together to improve the health and wellbeing of their local population. • The HWBs enable different organisations to work together in planning and delivering local services. For example, the NHS, Adult social care services, Children’s services and Youth services. • Health and Wellbeing Boards are where representatives from the health and social care sector work together to improve the health and well-being of their local population. • They report to the clinical commissioning groups and local authorities. • These boards are at the centre of the Care and Health Improvement Programme, introduced in April 2015, which aims to help HWBs develop their leadership and better support the integration of services https: //www. kingsfund. org. uk/publications/health-wellbeing-boards-explained Read the information in the link and add to the notes that you have. ©Outstanding Resources 2017
D 1 How agencies work together to meet individual care and support needs Role of assessment and eligibility frameworks, to include Common Assessment Framework (CAF), the National Eligibility Criteria (Care Act 2014), Department of Health, National Framework for NHS Continuing Healthcare. The Education, Health and Care plan (EHC http: //greatermanchesterscb. proceduresonline. c om/pdfs/caf_guidance_practitioners. pdf Additional reading https: //www. youtube. com/watch? v=ZFb_lvqz. JX w CAF Training video dorsetforyou webteam Watch the clip and make notes. What is CAF? Try to record some of the examples given about some of the people they have helped, why that person needed help, what help they received etc. The Department of Health • Sets national policy • Creates legislation • Allocates funding for health care https: //www. gov. uk/government/organisations/department-of -health/about (Additional information) ©Outstanding Resources 2017 National Eligibility Criteria (Care Act 2014) or the Care and Support (Eligibility Criteria) Regulations 2014. Sets out national eligibility criteria for access to adult care and support and for access to carer support. http: //www. legislation. gov. uk/ukdsi/201 4/9780111124185 Additional reading https: //www. youtube. com/watch? v=Ki 5 20 q. Aj. NTg Education, Health and Care plans Educationgovuk Make notes from the clip.
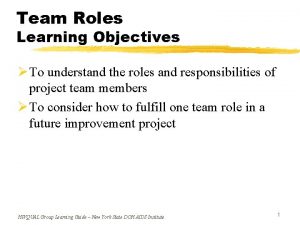
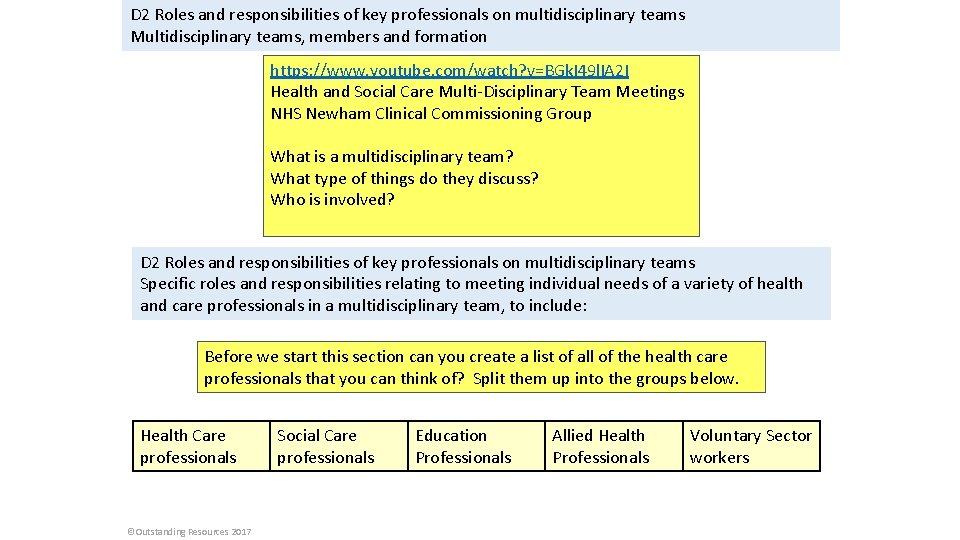
D 2 Roles and responsibilities of key professionals on multidisciplinary teams Multidisciplinary teams, members and formation https: //www. youtube. com/watch? v=BGk. I 49 l. IA 2 I Health and Social Care Multi-Disciplinary Team Meetings NHS Newham Clinical Commissioning Group What is a multidisciplinary team? What type of things do they discuss? Who is involved? D 2 Roles and responsibilities of key professionals on multidisciplinary teams Specific roles and responsibilities relating to meeting individual needs of a variety of health and care professionals in a multidisciplinary team, to include: Before we start this section can you create a list of all of the health care professionals that you can think of? Split them up into the groups below. Health Care professionals ©Outstanding Resources 2017 Social Care professionals Education Professionals Allied Health Professionals Voluntary Sector workers
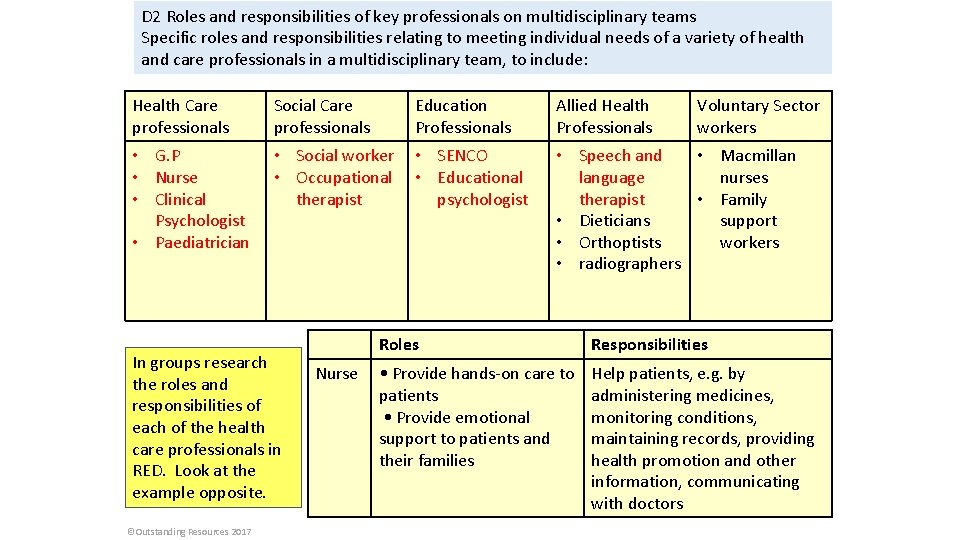
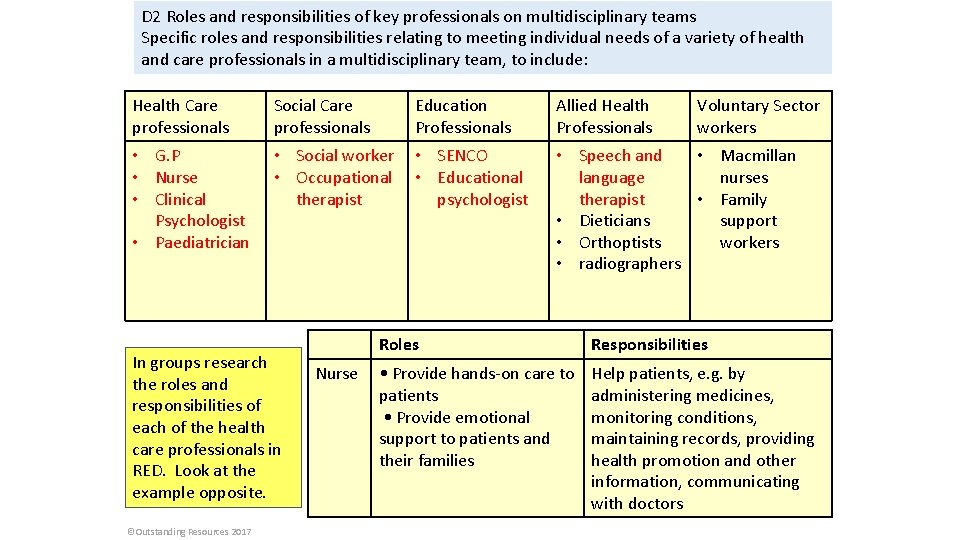
D 2 Roles and responsibilities of key professionals on multidisciplinary teams Specific roles and responsibilities relating to meeting individual needs of a variety of health and care professionals in a multidisciplinary team, to include: Health Care professionals Social Care professionals • G. P • Nurse • Clinical Psychologist • Paediatrician • Social worker • SENCO • Occupational • Educational therapist psychologist In groups research the roles and responsibilities of each of the health care professionals in RED. Look at the example opposite. ©Outstanding Resources 2017 Nurse Education Professionals Allied Health Professionals Voluntary Sector workers • Speech and • Macmillan language nurses therapist • Family • Dieticians support • Orthoptists workers • radiographers Roles Responsibilities • Provide hands-on care to patients • Provide emotional support to patients and their families Help patients, e. g. by administering medicines, monitoring conditions, maintaining records, providing health promotion and other information, communicating with doctors
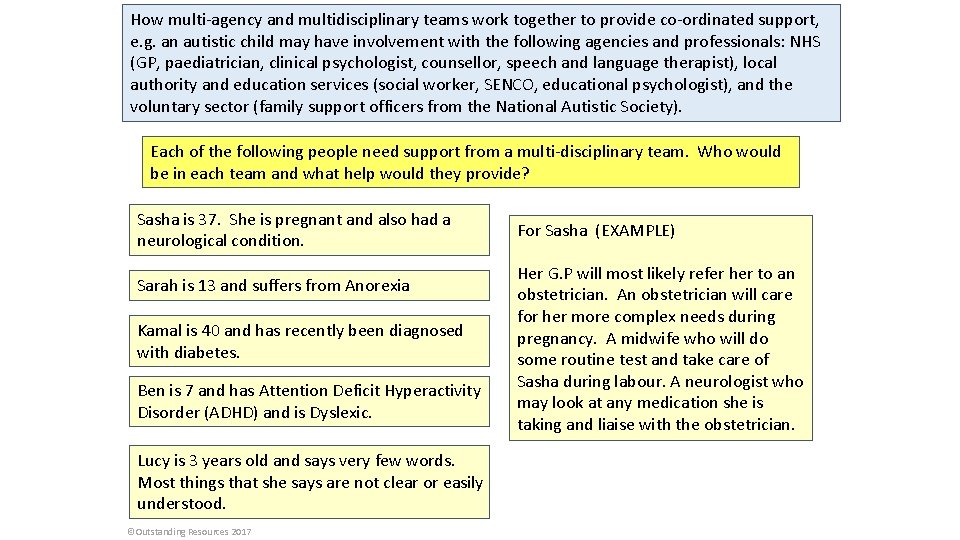
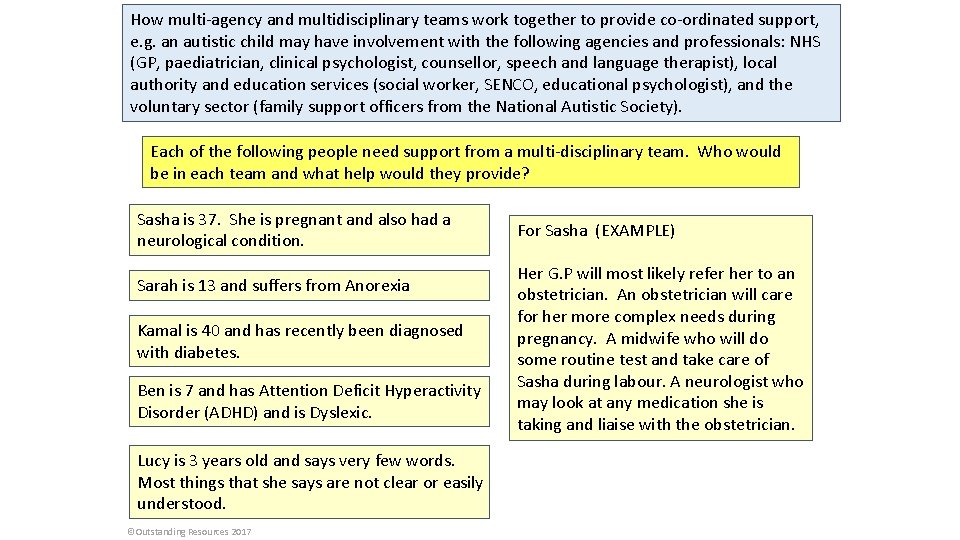
How multi-agency and multidisciplinary teams work together to provide co-ordinated support, e. g. an autistic child may have involvement with the following agencies and professionals: NHS (GP, paediatrician, clinical psychologist, counsellor, speech and language therapist), local authority and education services (social worker, SENCO, educational psychologist), and the voluntary sector (family support officers from the National Autistic Society). Each of the following people need support from a multi-disciplinary team. Who would be in each team and what help would they provide? Sasha is 37. She is pregnant and also had a neurological condition. Sarah is 13 and suffers from Anorexia Kamal is 40 and has recently been diagnosed with diabetes. Ben is 7 and has Attention Deficit Hyperactivity Disorder (ADHD) and is Dyslexic. Lucy is 3 years old and says very few words. Most things that she says are not clear or easily understood. ©Outstanding Resources 2017 For Sasha (EXAMPLE) Her G. P will most likely refer her to an obstetrician. An obstetrician will care for her more complex needs during pregnancy. A midwife who will do some routine test and take care of Sasha during labour. A neurologist who may look at any medication she is taking and liaise with the obstetrician.
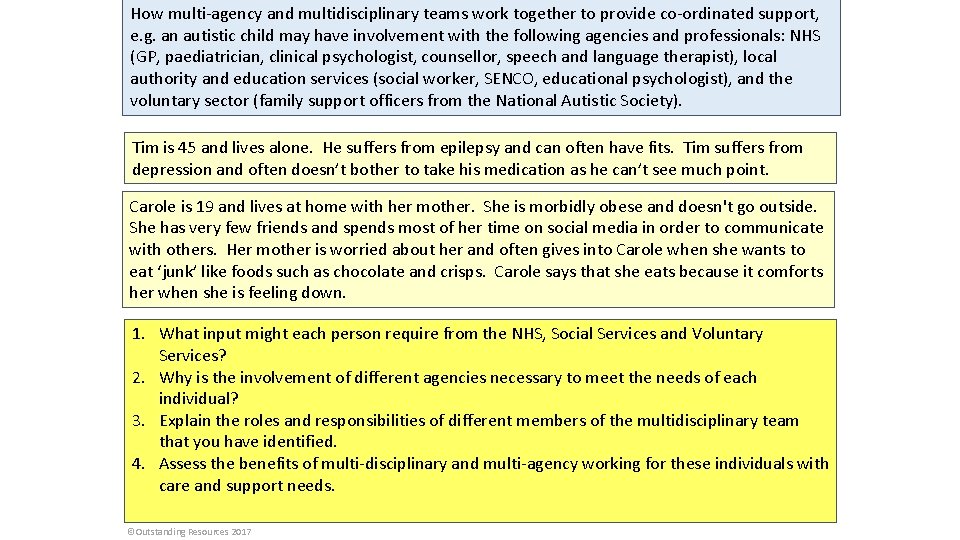
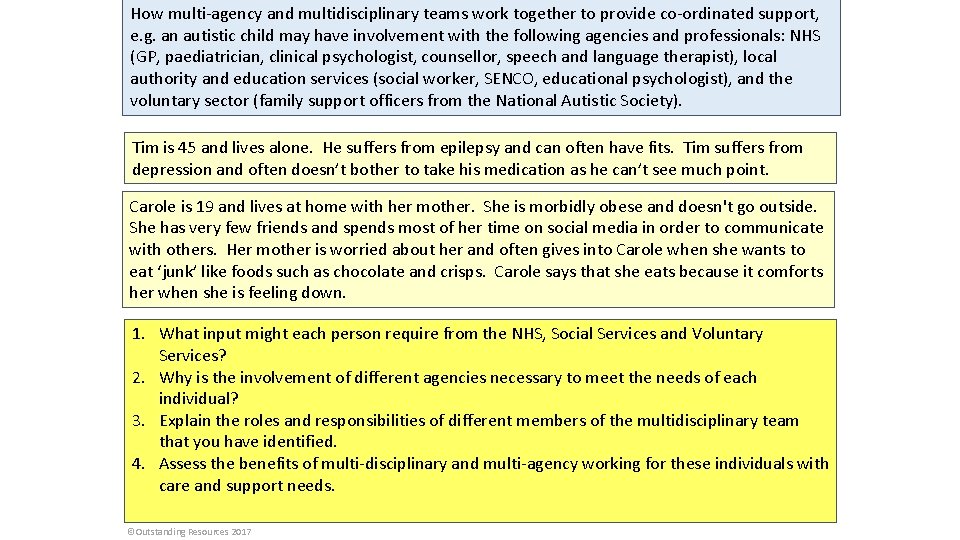
How multi-agency and multidisciplinary teams work together to provide co-ordinated support, e. g. an autistic child may have involvement with the following agencies and professionals: NHS (GP, paediatrician, clinical psychologist, counsellor, speech and language therapist), local authority and education services (social worker, SENCO, educational psychologist), and the voluntary sector (family support officers from the National Autistic Society). Tim is 45 and lives alone. He suffers from epilepsy and can often have fits. Tim suffers from depression and often doesn’t bother to take his medication as he can’t see much point. Carole is 19 and lives at home with her mother. She is morbidly obese and doesn't go outside. She has very few friends and spends most of her time on social media in order to communicate with others. Her mother is worried about her and often gives into Carole when she wants to eat ‘junk’ like foods such as chocolate and crisps. Carole says that she eats because it comforts her when she is feeling down. 1. What input might each person require from the NHS, Social Services and Voluntary Services? 2. Why is the involvement of different agencies necessary to meet the needs of each individual? 3. Explain the roles and responsibilities of different members of the multidisciplinary team that you have identified. 4. Assess the benefits of multi-disciplinary and multi-agency working for these individuals with care and support needs. ©Outstanding Resources 2017
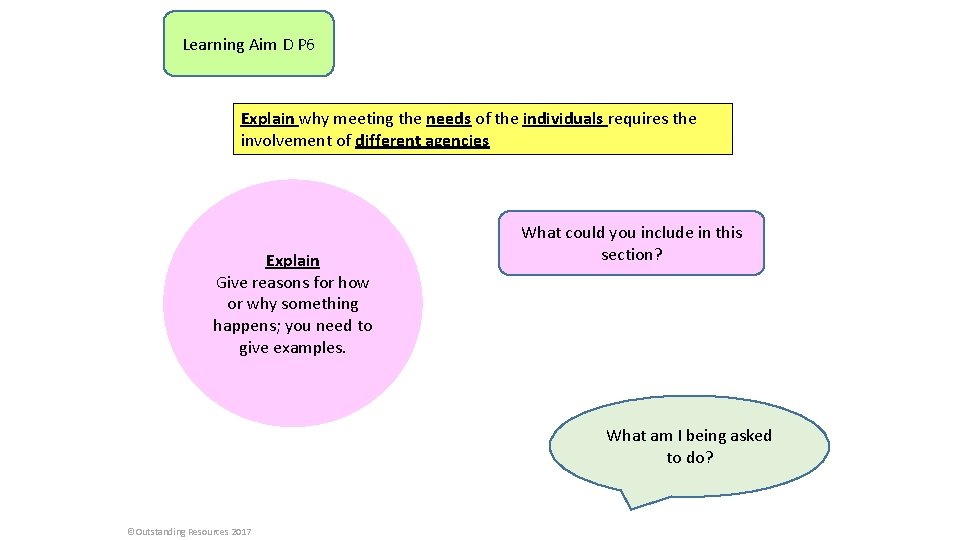
Learning Aim D P 6 Explain why meeting the needs of the individuals requires the involvement of different agencies Explain Give reasons for how or why something happens; you need to give examples. What could you include in this section? What am I being asked to do? ©Outstanding Resources 2017
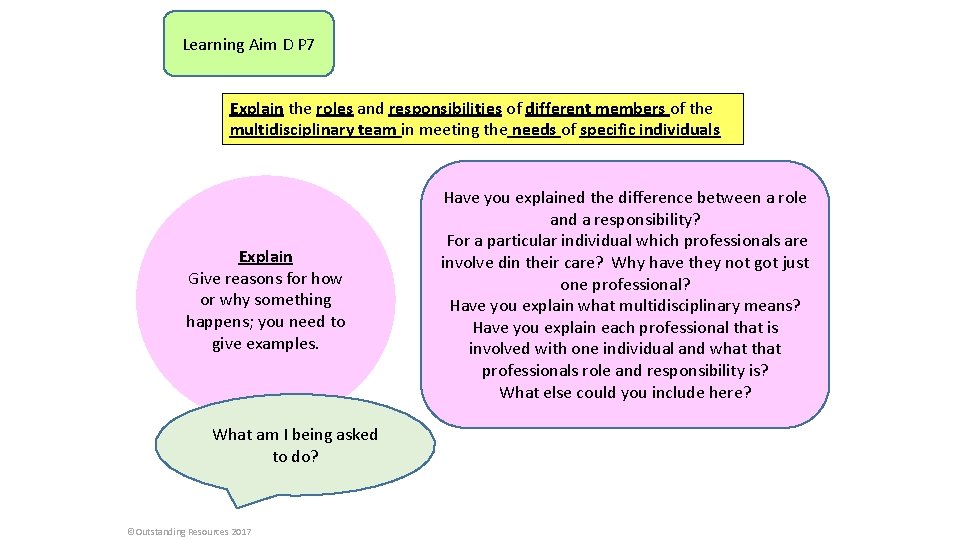
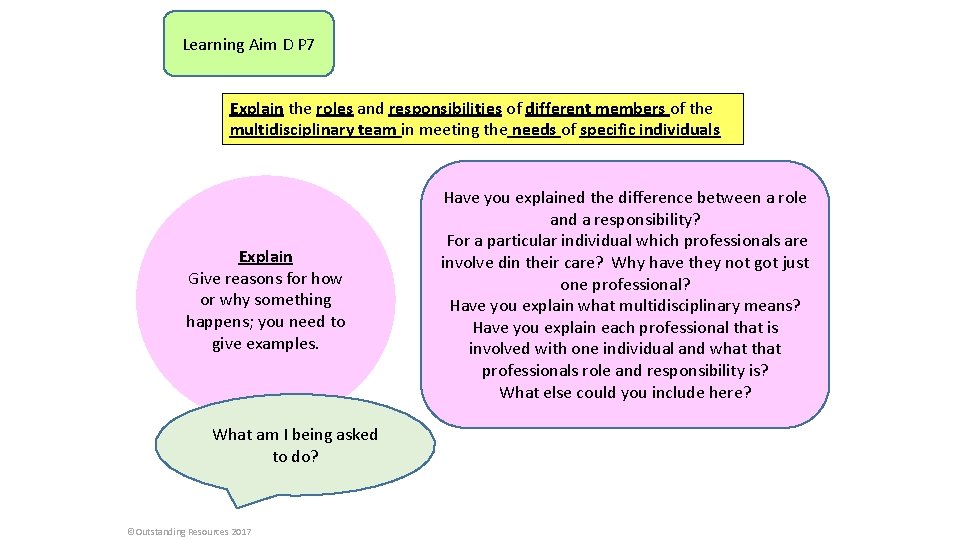
Learning Aim D P 7 Explain the roles and responsibilities of different members of the multidisciplinary team in meeting the needs of specific individuals Explain Give reasons for how or why something happens; you need to give examples. What am I being asked to do? ©Outstanding Resources 2017 Have you explained the difference between a role and a responsibility? For a particular individual which professionals are involve din their care? Why have they not got just one professional? Have you explain what multidisciplinary means? Have you explain each professional that is involved with one individual and what that professionals role and responsibility is? What else could you include here?
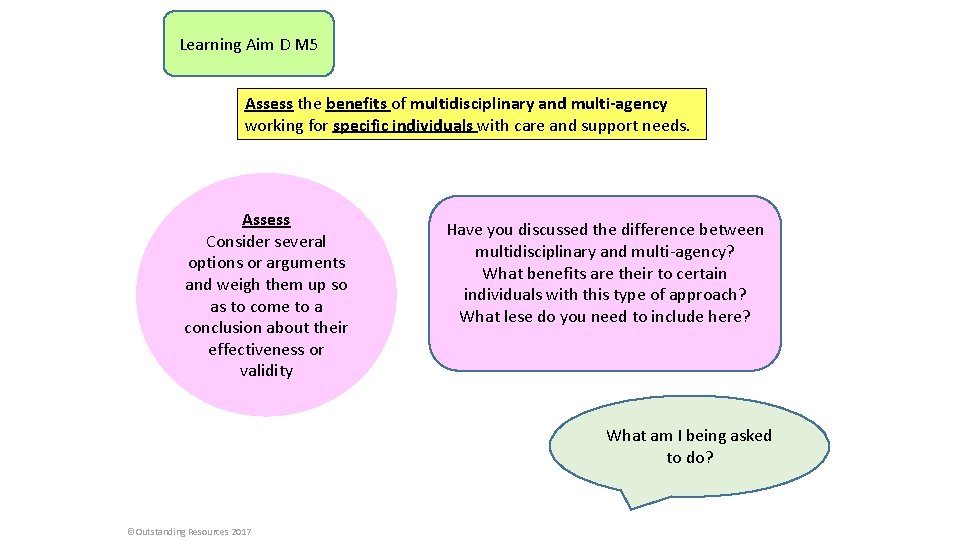
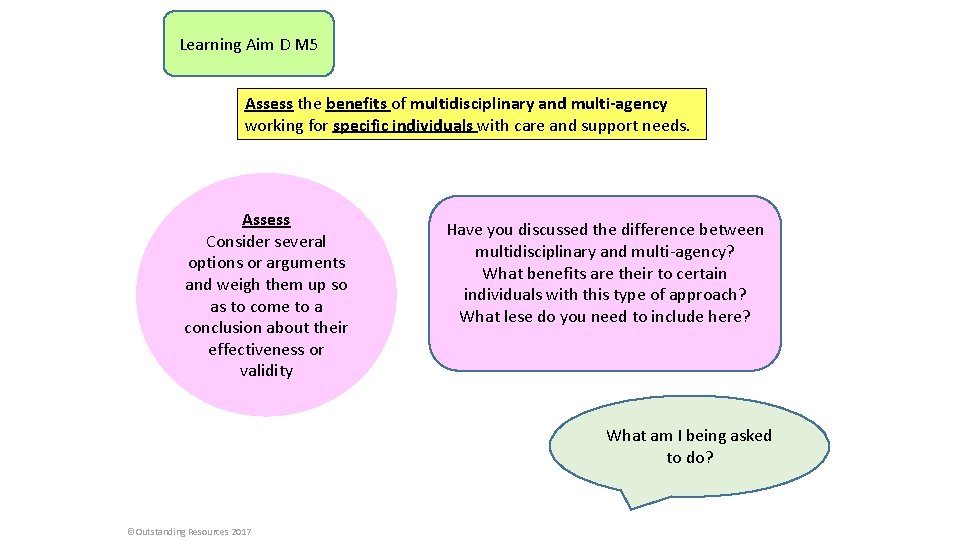
Learning Aim D M 5 Assess the benefits of multidisciplinary and multi-agency working for specific individuals with care and support needs. Assess Consider several options or arguments and weigh them up so as to come to a conclusion about their effectiveness or validity Have you discussed the difference between multidisciplinary and multi-agency? What benefits are their to certain individuals with this type of approach? What lese do you need to include here? What am I being asked to do? ©Outstanding Resources 2017
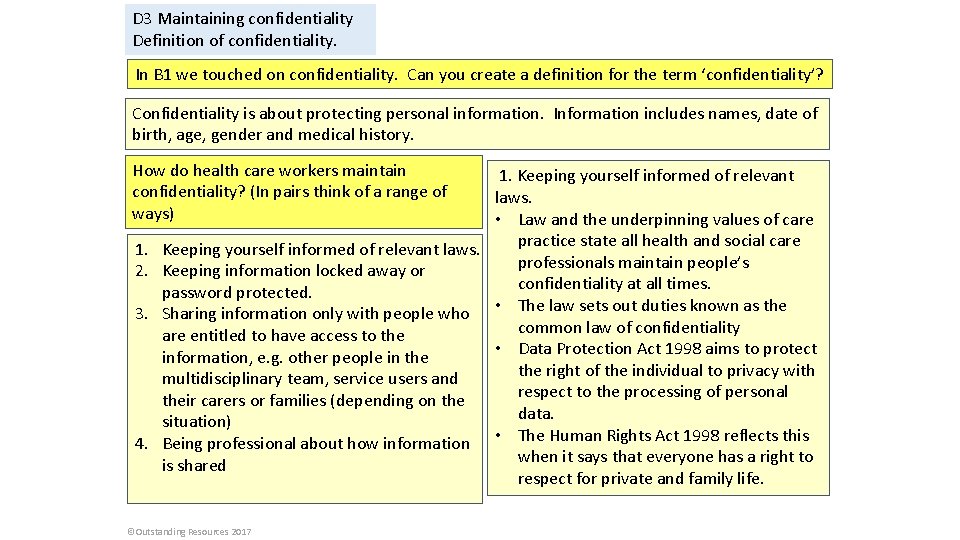
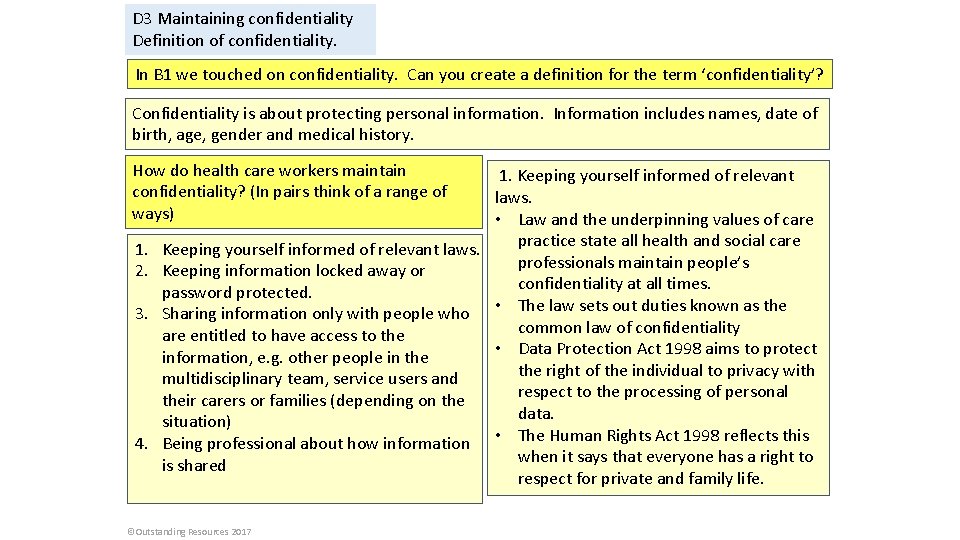
D 3 Maintaining confidentiality Definition of confidentiality. In B 1 we touched on confidentiality. Can you create a definition for the term ‘confidentiality’? Confidentiality is about protecting personal information. Information includes names, date of birth, age, gender and medical history. How do health care workers maintain confidentiality? (In pairs think of a range of ways) 1. Keeping yourself informed of relevant laws. • Law and the underpinning values of care practice state all health and social care 1. Keeping yourself informed of relevant laws. professionals maintain people’s 2. Keeping information locked away or confidentiality at all times. password protected. 3. Sharing information only with people who • The law sets out duties known as the common law of confidentiality are entitled to have access to the • Data Protection Act 1998 aims to protect information, e. g. other people in the right of the individual to privacy with multidisciplinary team, service users and respect to the processing of personal their carers or families (depending on the data. situation) 4. Being professional about how information • The Human Rights Act 1998 reflects this when it says that everyone has a right to is shared respect for private and family life. ©Outstanding Resources 2017
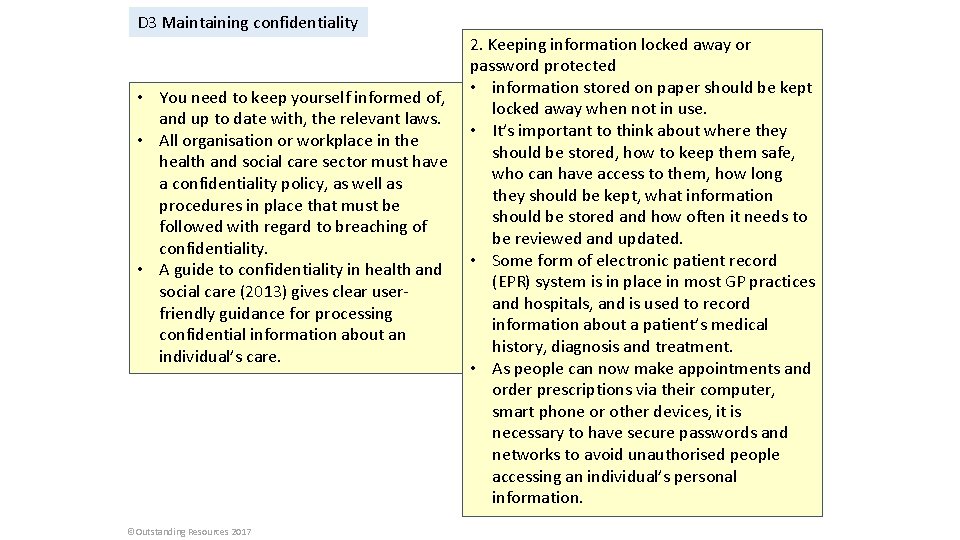
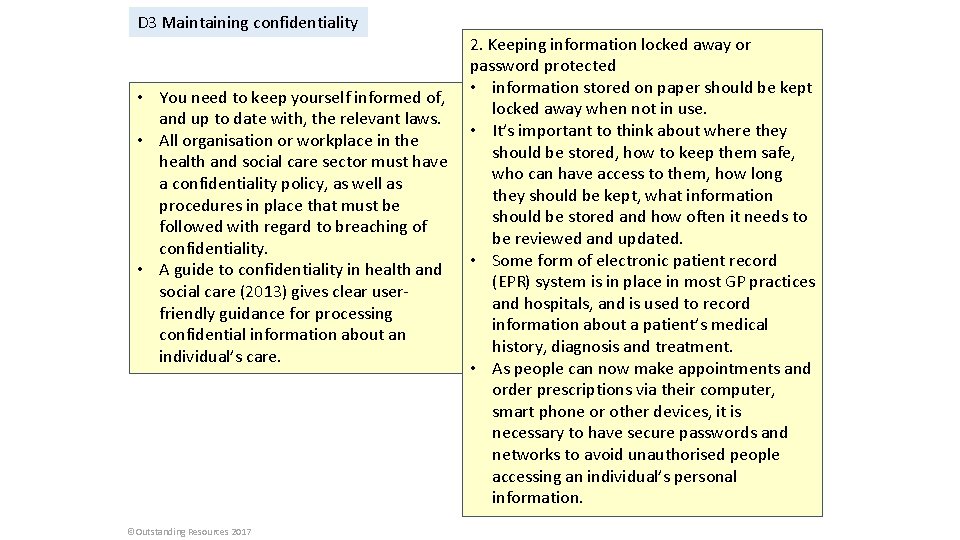
D 3 Maintaining confidentiality • You need to keep yourself informed of, and up to date with, the relevant laws. • All organisation or workplace in the health and social care sector must have a confidentiality policy, as well as procedures in place that must be followed with regard to breaching of confidentiality. • A guide to confidentiality in health and social care (2013) gives clear userfriendly guidance for processing confidential information about an individual’s care. ©Outstanding Resources 2017 2. Keeping information locked away or password protected • information stored on paper should be kept locked away when not in use. • It’s important to think about where they should be stored, how to keep them safe, who can have access to them, how long they should be kept, what information should be stored and how often it needs to be reviewed and updated. • Some form of electronic patient record (EPR) system is in place in most GP practices and hospitals, and is used to record information about a patient’s medical history, diagnosis and treatment. • As people can now make appointments and order prescriptions via their computer, smart phone or other devices, it is necessary to have secure passwords and networks to avoid unauthorised people accessing an individual’s personal information.
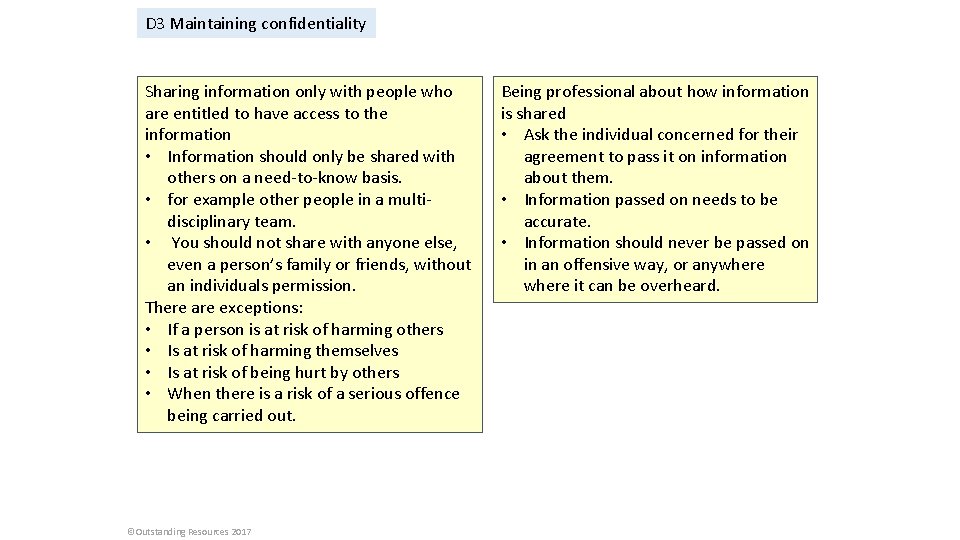
D 3 Maintaining confidentiality Sharing information only with people who are entitled to have access to the information • Information should only be shared with others on a need-to-know basis. • for example other people in a multidisciplinary team. • You should not share with anyone else, even a person’s family or friends, without an individuals permission. There are exceptions: • If a person is at risk of harming others • Is at risk of harming themselves • Is at risk of being hurt by others • When there is a risk of a serious offence being carried out. ©Outstanding Resources 2017 Being professional about how information is shared • Ask the individual concerned for their agreement to pass it on information about them. • Information passed on needs to be accurate. • Information should never be passed on in an offensive way, or anywhere it can be overheard.
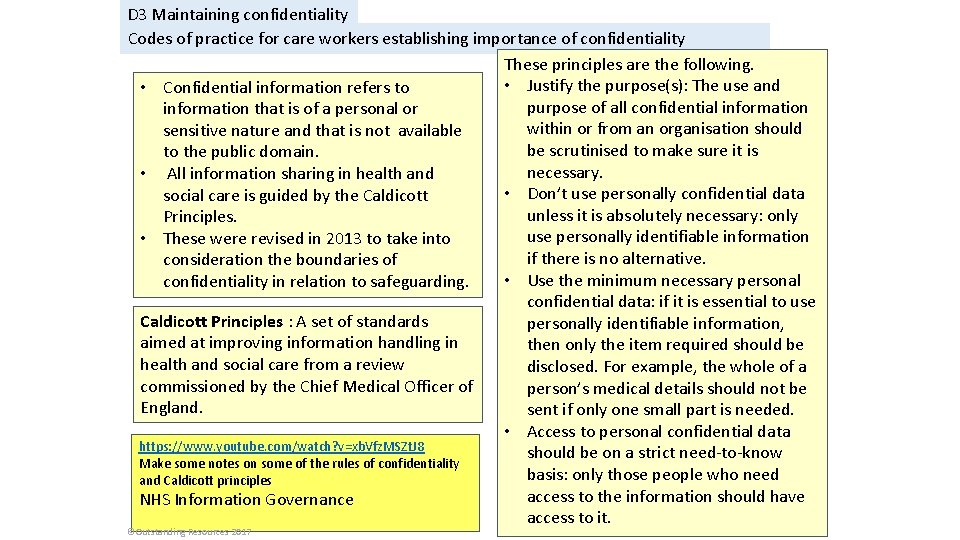
D 3 Maintaining confidentiality Codes of practice for care workers establishing importance of confidentiality These principles are the following. • Justify the purpose(s): The use and • Confidential information refers to purpose of all confidential information that is of a personal or within or from an organisation should sensitive nature and that is not available be scrutinised to make sure it is to the public domain. necessary. • All information sharing in health and • Don’t use personally confidential data social care is guided by the Caldicott unless it is absolutely necessary: only Principles. use personally identifiable information • These were revised in 2013 to take into if there is no alternative. consideration the boundaries of • Use the minimum necessary personal confidentiality in relation to safeguarding. confidential data: if it is essential to use Caldicott Principles : A set of standards personally identifiable information, aimed at improving information handling in then only the item required should be health and social care from a review disclosed. For example, the whole of a commissioned by the Chief Medical Officer of person’s medical details should not be England. sent if only one small part is needed. • Access to personal confidential data https: //www. youtube. com/watch? v=xb. Vfz. MSZt. J 8 should be on a strict need-to-know Make some notes on some of the rules of confidentiality basis: only those people who need and Caldicott principles access to the information should have NHS Information Governance access to it. ©Outstanding Resources 2017
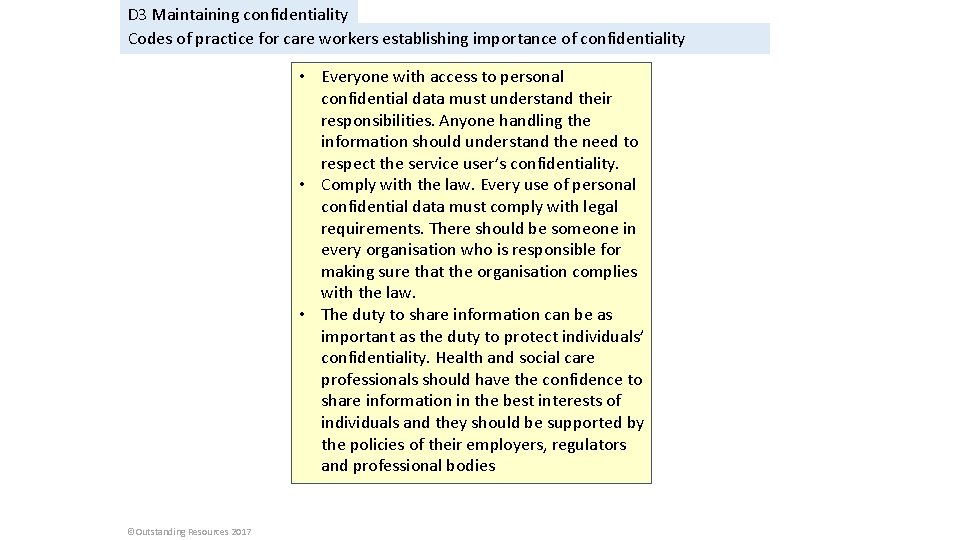
D 3 Maintaining confidentiality Codes of practice for care workers establishing importance of confidentiality • Everyone with access to personal confidential data must understand their responsibilities. Anyone handling the information should understand the need to respect the service user’s confidentiality. • Comply with the law. Every use of personal confidential data must comply with legal requirements. There should be someone in every organisation who is responsible for making sure that the organisation complies with the law. • The duty to share information can be as important as the duty to protect individuals’ confidentiality. Health and social care professionals should have the confidence to share information in the best interests of individuals and they should be supported by the policies of their employers, regulators and professional bodies ©Outstanding Resources 2017
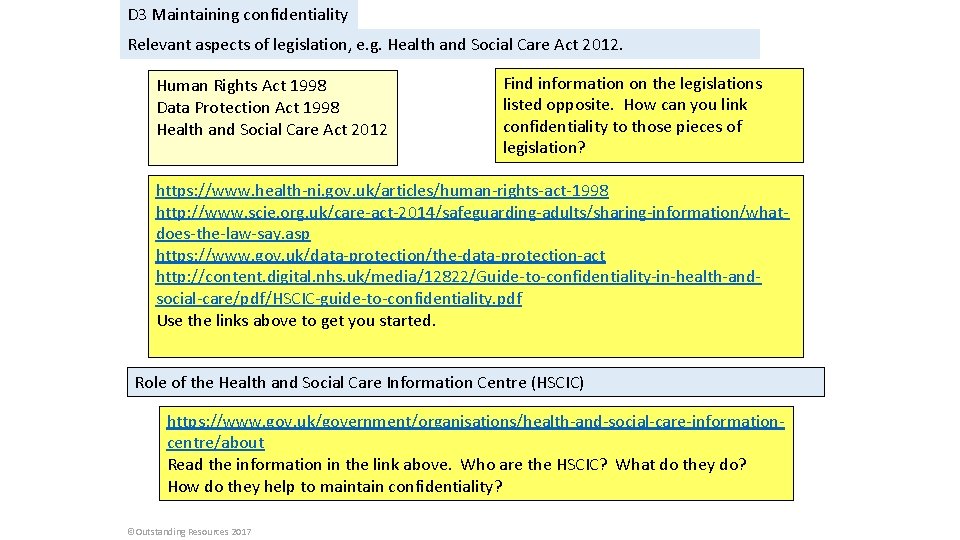
D 3 Maintaining confidentiality Relevant aspects of legislation, e. g. Health and Social Care Act 2012. Human Rights Act 1998 Data Protection Act 1998 Health and Social Care Act 2012 Find information on the legislations listed opposite. How can you link confidentiality to those pieces of legislation? https: //www. health-ni. gov. uk/articles/human-rights-act-1998 http: //www. scie. org. uk/care-act-2014/safeguarding-adults/sharing-information/whatdoes-the-law-say. asp https: //www. gov. uk/data-protection/the-data-protection-act http: //content. digital. nhs. uk/media/12822/Guide-to-confidentiality-in-health-andsocial-care/pdf/HSCIC-guide-to-confidentiality. pdf Use the links above to get you started. Role of the Health and Social Care Information Centre (HSCIC) https: //www. gov. uk/government/organisations/health-and-social-care-informationcentre/about Read the information in the link above. Who are the HSCIC? What do they do? How do they help to maintain confidentiality? ©Outstanding Resources 2017
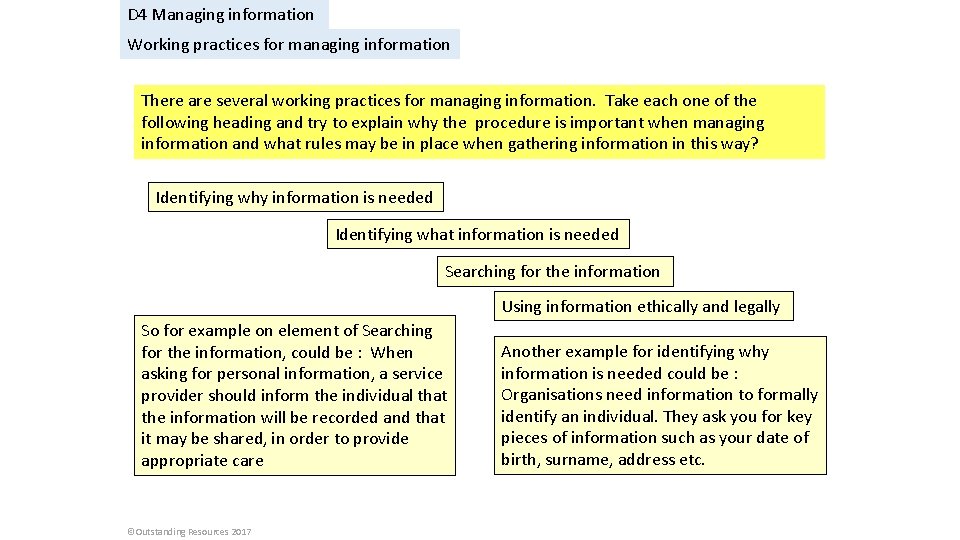
D 4 Managing information Working practices for managing information There are several working practices for managing information. Take each one of the following heading and try to explain why the procedure is important when managing information and what rules may be in place when gathering information in this way? Identifying why information is needed Identifying what information is needed Searching for the information Using information ethically and legally So for example on element of Searching for the information, could be : When asking for personal information, a service provider should inform the individual that the information will be recorded and that it may be shared, in order to provide appropriate care ©Outstanding Resources 2017 Another example for identifying why information is needed could be : Organisations need information to formally identify an individual. They ask you for key pieces of information such as your date of birth, surname, address etc.
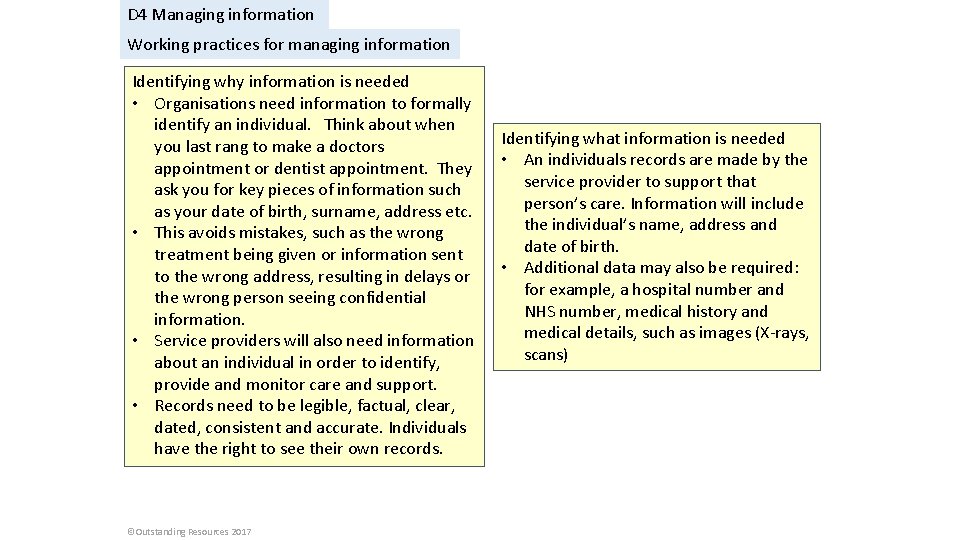
D 4 Managing information Working practices for managing information Identifying why information is needed • Organisations need information to formally identify an individual. Think about when you last rang to make a doctors appointment or dentist appointment. They ask you for key pieces of information such as your date of birth, surname, address etc. • This avoids mistakes, such as the wrong treatment being given or information sent to the wrong address, resulting in delays or the wrong person seeing confidential information. • Service providers will also need information about an individual in order to identify, provide and monitor care and support. • Records need to be legible, factual, clear, dated, consistent and accurate. Individuals have the right to see their own records. ©Outstanding Resources 2017 Identifying what information is needed • An individuals records are made by the service provider to support that person’s care. Information will include the individual’s name, address and date of birth. • Additional data may also be required: for example, a hospital number and NHS number, medical history and medical details, such as images (X-rays, scans)
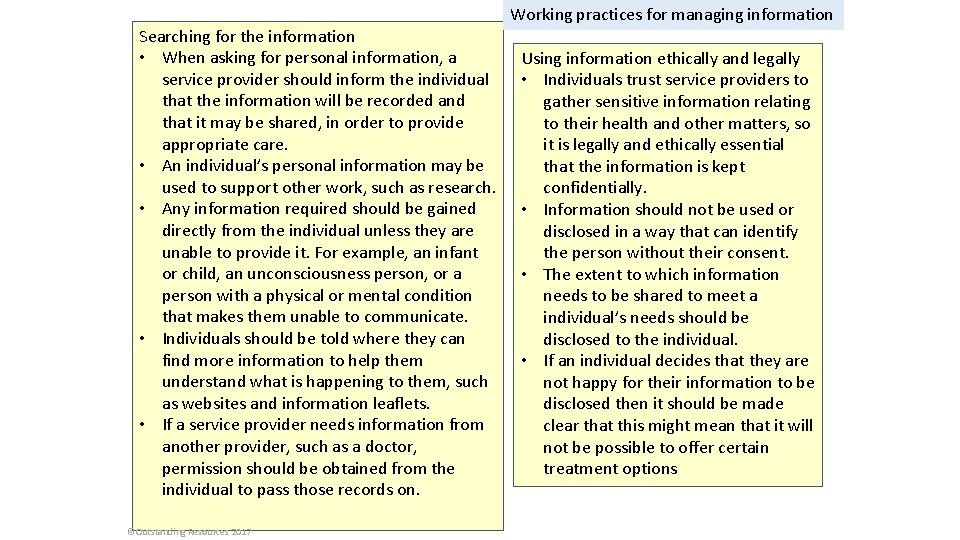
Searching for the information • When asking for personal information, a service provider should inform the individual that the information will be recorded and that it may be shared, in order to provide appropriate care. • An individual’s personal information may be used to support other work, such as research. • Any information required should be gained directly from the individual unless they are unable to provide it. For example, an infant or child, an unconsciousness person, or a person with a physical or mental condition that makes them unable to communicate. • Individuals should be told where they can find more information to help them understand what is happening to them, such as websites and information leaflets. • If a service provider needs information from another provider, such as a doctor, permission should be obtained from the individual to pass those records on. ©Outstanding Resources 2017 Working practices for managing information Using information ethically and legally • Individuals trust service providers to gather sensitive information relating to their health and other matters, so it is legally and ethically essential that the information is kept confidentially. • Information should not be used or disclosed in a way that can identify the person without their consent. • The extent to which information needs to be shared to meet a individual’s needs should be disclosed to the individual. • If an individual decides that they are not happy for their information to be disclosed then it should be made clear that this might mean that it will not be possible to offer certain treatment options
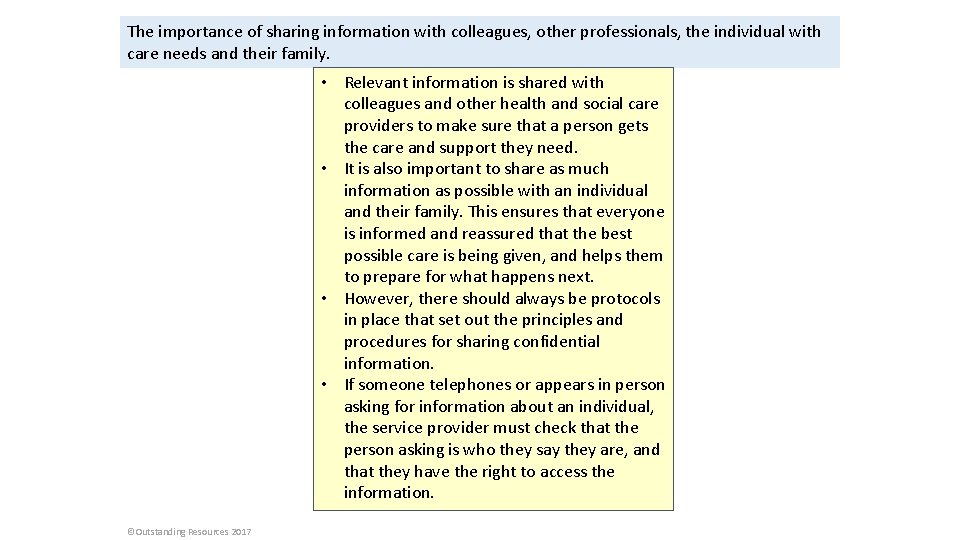
The importance of sharing information with colleagues, other professionals, the individual with care needs and their family. • Relevant information is shared with colleagues and other health and social care providers to make sure that a person gets the care and support they need. • It is also important to share as much information as possible with an individual and their family. This ensures that everyone is informed and reassured that the best possible care is being given, and helps them to prepare for what happens next. • However, there should always be protocols in place that set out the principles and procedures for sharing confidential information. • If someone telephones or appears in person asking for information about an individual, the service provider must check that the person asking is who they say they are, and that they have the right to access the information. ©Outstanding Resources 2017
D 4 Managing information Impact of new technologies on managing information https: //www. youtube. com/watch? v=s. D 4 Qiqu. LZiw We share because we care: sharing health records in the NHS What are the advantages of electronic patient records? What happens when you ring your doctors surgery to make an appointment? https: //www. youtube. com/watch? v=p 2 eii. Buj. Iv 4 Taking the hassle out of healthcare ©Outstanding Resources 2017 • The HSCIC’s vision is that, by 2020, there will be full service user access to national and local dat. • Individuals will be able to view and manage their own records, communicate with care providers and increasingly manage their own health, care and wellbeing. • The HSCIC has set out a strategy with five objectives towards achieving this vision • Ensure that every citizen’s data is protected. • Establish shared architecture and standards so that everyone benefits. • Implement services that meet national and local needs. • Support health and care organisations in getting the best from technology, data and information. • Make better use of health and care information
D 4 Managing information Bodies that control the management of information, e. g. the National Adult Social Care Intelligence Service (NASCIS) • The National Adult Social Care Intelligence Service (NASCIS) • single national resource of social care information for England. • Website has a collection of data, tools and resources designed to meet the needs of service planners, managers, researchers and policy makers and others. You can view and download data on: • Referrals, assessments and packages of care • Adult social care activity • Social care expenditure • Abuse of vulnerable adults • Adult and Social Care Outcomes Framework • User experience survey • Joint strategic needs assessment • The Information Commissioner’s Office (ICO) • Upholds information rights in the public interest, promoting openness by public bodies and data privacy for individuals. • https: //ico. org. uk/about-the-ico/whatwe-do/ • Additional reading ©Outstanding Resources 2017
D 4 Managing information Legislation and codes of practice that relate to the storage and sharing of information in health and social care. Legislation and codes of practice must be current and applicable to England, Wales or Northern Ireland Data Protection Act 1998 • Main piece of legislation that governs the protection of personal data in the UK • Controls how your personal information is used by everyone responsible for using data, by providing rules called data protection principles • Provides legal protection for more sensitive personal data • Gives you the right to access to your own personal data • Enables health and social care providers to share information with other professionals directly involved in providing clinical care ©Outstanding Resources 2017 Freedom of Information Act 2000 • Provides public access to information held by public authorities in England, Wales and Northern Ireland, and UKwide public authorities based in Scotland • Does not give access to your own personal data • Makes public authorities accountable for their actions. Allows public debate to be better informed and, therefore, more productive
D 4 Managing information Legislation and codes of practice that relate to the storage and sharing of information in health and social care. Legislation and codes of practice must be current and applicable to England, Wales or Northern Ireland Mental Health Act 2007 • Allows people in England Wales to be admitted to hospital, detained and treated against their consent, for their own health and safety and for that of others, so allows the storing and sharing of their personal information without their consent Mental Capacity Act 2005 • Requires professionals to consider a person’s mental capacity to consent to share information • Outlines correct procedures for making decisions in the best interest of a person who lacks the mental capacity to consent ©Outstanding Resources 2017 • Care Quality Commission (CQC) codes of practice • CQC is an independent body that speaks up for the rights of people who use care services, their families and carers, and checks that services stick to the Health and Social Care Act 2008 • One example is the 2010 code of practice for health and adult social services in England, which: • sets out the practices to be followed in obtaining, handling, using and disclosing confidential personal information • is based on a set of nine principles • includes a necessity test to decide whether it is necessary to obtain, use or disclose personal information
D 4 Managing information Legislation and codes of practice that relate to the storage and sharing of information in health and social care. Legislation and codes of practice must be current and applicable to England, Wales or Northern Ireland The Health and Care Professions Council (HCPC) codes of practice • HCPC is a regulator set up to protect the public, by keeping a register of health and social care professionals who meet HCPC standards for training, professional skills, behaviour and health • Confidentiality – guidance for registrants 2008, slightly amended in 2012, sets out the standards of conduct, performance and ethics expected from the professionals it regulates, including management of information ©Outstanding Resources 2017
Learning Aim D P 8 Explain the arrangements for managing information between professionals. Explain Give reasons for how or why something happens; you need to give examples. What am I being asked to do? ©Outstanding Resources 2017 What arrangements are in place for professionals when it comes to passing information from one person to another? For each arrangement state why this is important. Does this link to any other areas you have studied, for example confidentiality? What else can you include in this section.
Learning Aim D M 6 Analyse the impact of legislation and codes of practice relating to information management on multidisciplinary working. Analyse Break an issue into its separate parts. Look in depth at each part using supporting arguments and evidence for and against as well as how these interrelate (connect) to one another. What am I being asked to do? ©Outstanding Resources 2017
Learning Aim D D 3 Justify how organisations and professionals work together to meet individual needs while managing information and maintaining confidentiality. Justify Give a reason to support an argument/ give an explanation for something/ defend a point of view. This might reasonably involve discussing and discounting alternative views or actions. There may be positives and negatives. What do you need to include in this section? What am I being asked to do? ©Outstanding Resources 2017
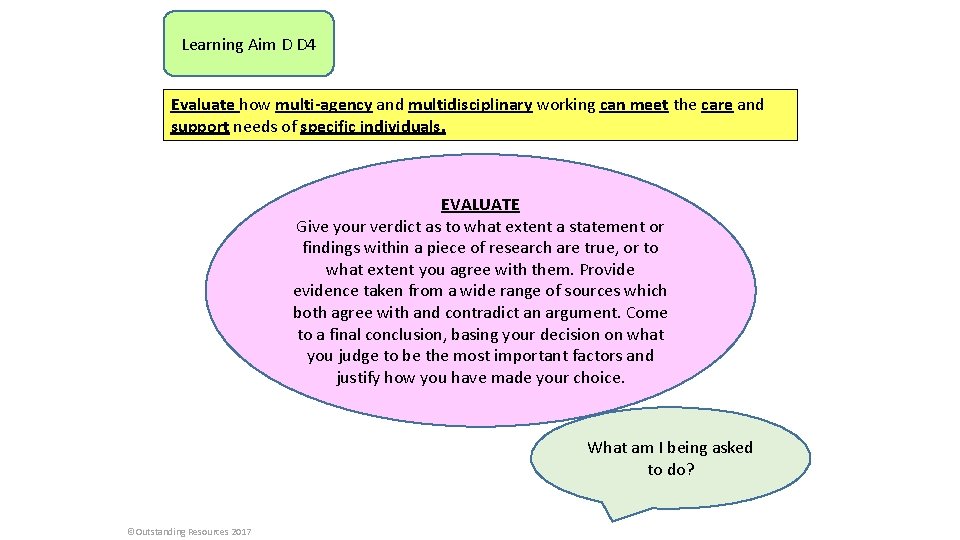
Learning Aim D D 4 Evaluate how multi-agency and multidisciplinary working can meet the care and support needs of specific individuals. EVALUATE Give your verdict as to what extent a statement or findings within a piece of research are true, or to what extent you agree with them. Provide evidence taken from a wide range of sources which both agree with and contradict an argument. Come to a final conclusion, basing your decision on what you judge to be the most important factors and justify how you have made your choice. What am I being asked to do? ©Outstanding Resources 2017
 Lesson 4 parameters and return make
Lesson 4 parameters and return make What made oedipus go to the oracle when he was young?
What made oedipus go to the oracle when he was young? Initial rate of reaction
Initial rate of reaction How to investigate a problem
How to investigate a problem Investigate bivariate measurement data
Investigate bivariate measurement data Investigate reflection
Investigate reflection Cuadro comparativo de e-learning
Cuadro comparativo de e-learning Health and social care unit 5 learning aim d
Health and social care unit 5 learning aim d Learning aim c btec business
Learning aim c btec business Unit 14 learning aim d
Unit 14 learning aim d Unit 14 physiological disorders assignment 2
Unit 14 physiological disorders assignment 2 Health and social care component 2 learning aim b example
Health and social care component 2 learning aim b example Learning targets helping students aim for understanding
Learning targets helping students aim for understanding Learning aim d health and social care
Learning aim d health and social care Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Hát lên người ơi alleluia
Hát lên người ơi alleluia Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống