Introduction to Carotid Ultrasound and Transcranial Doppler Ultrasound
- Slides: 39
Introduction to Carotid Ultrasound and Transcranial Doppler Ultrasound Ryan Hakimi, DO, MS Director, Critical Care Neurology Assistant Professor Department of Neurology The University of Oklahoma Health Sciences Center January 16, 2015 OU Neurology
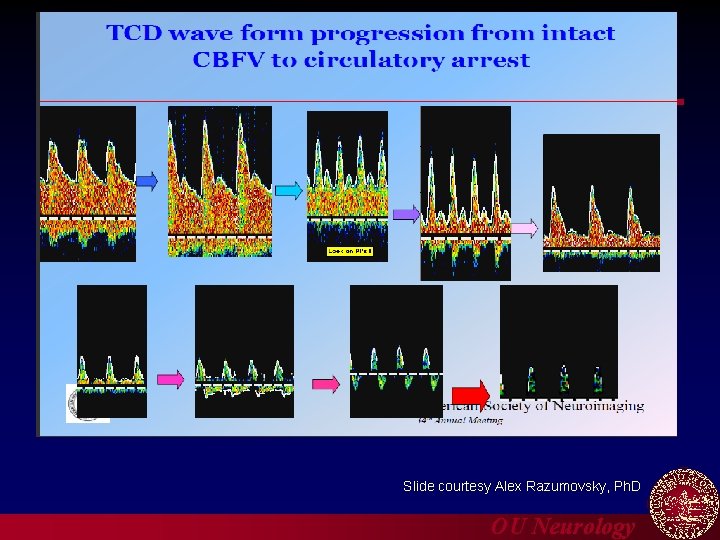
Disclosures n Many of the slides have been adapted from slides presented at the American Society for Neuroimaging Annual Meetings by my mentors Andre Alexandrov, MD n n Zsolt Garami, MD Charles Tegeler, MD Alex Razumovsky, Ph. D FINANCIAL DISCLOSURE Ø Nothing to disclose UNLABELED/UNAPPROVED USES DISCLOSURE Ø Nothing to disclose OU Neurology
Objectives n Review the basic principles of carotid ultrasound (CUS) and transcranial Doppler ultrasound (TCD) n Illustrate the process of plaque morphology and assignment of range of carotid stenosis n Illustrate the process of determining vasospasm by TCD n Discuss some of the current applications of TCD OU Neurology
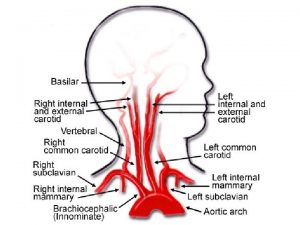
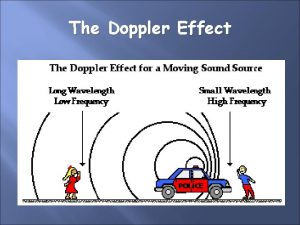
Principles of Ultrasound n Blood flow velocity through a cross sectional area of a particular vessel (cm/s) n Blood flow velocity is directly related to Doppler shift ØIf you measure the Doppler shift you can derive the blood flow velocity § Carotid ultrasound and transcranial Doppler ultrasound can accomplish this OU Neurology
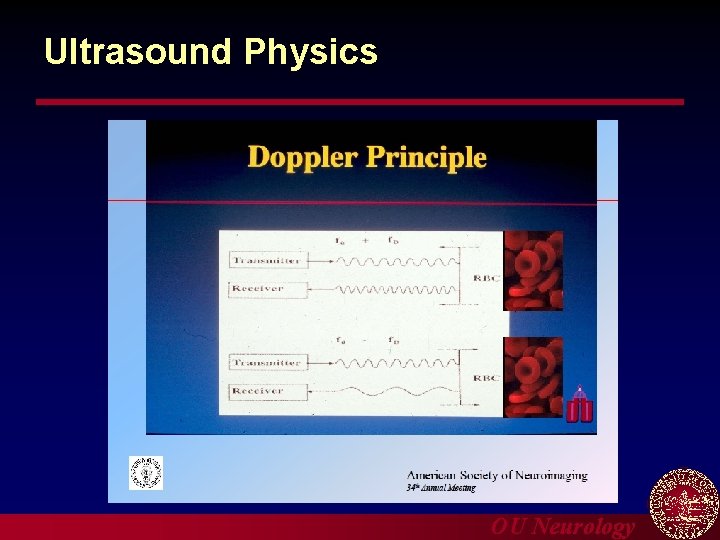
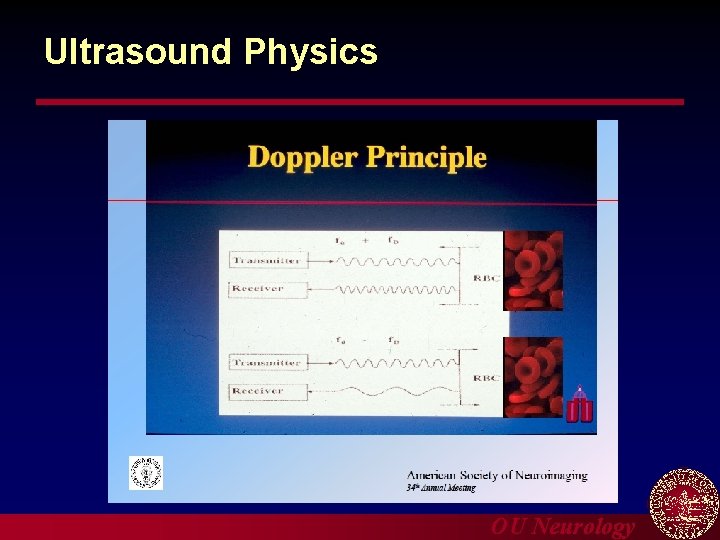
Ultrasound Physics OU Neurology
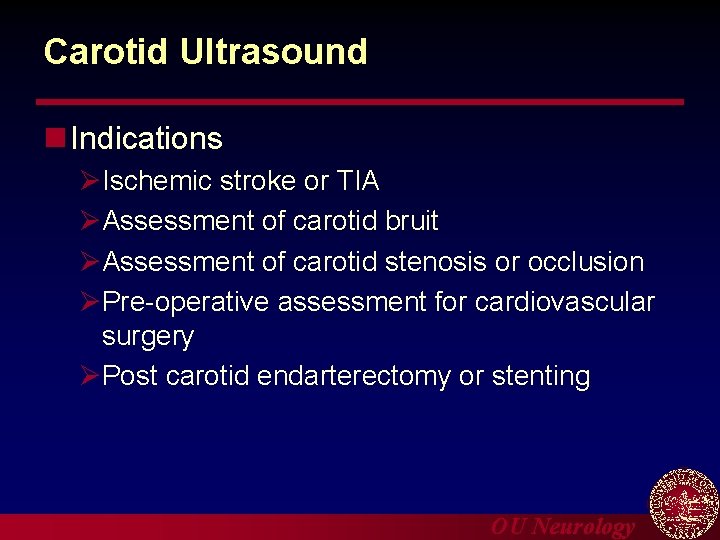
Carotid Ultrasound n Indications ØIschemic stroke or TIA ØAssessment of carotid bruit ØAssessment of carotid stenosis or occlusion ØPre-operative assessment for cardiovascular surgery ØPost carotid endarterectomy or stenting OU Neurology
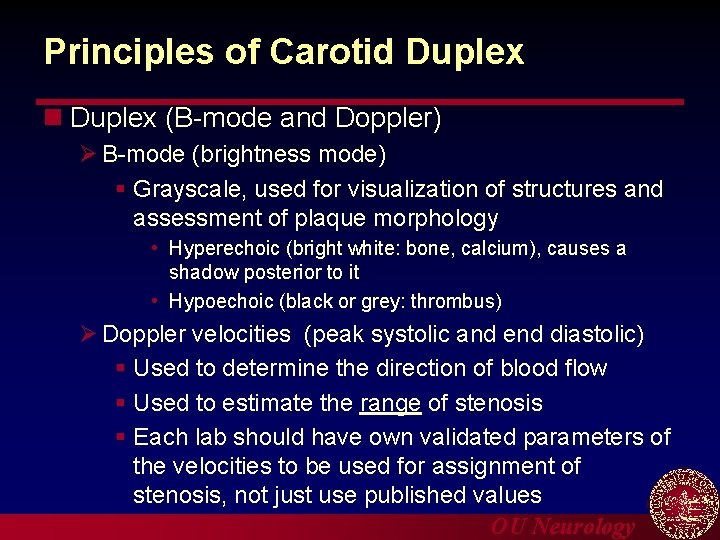
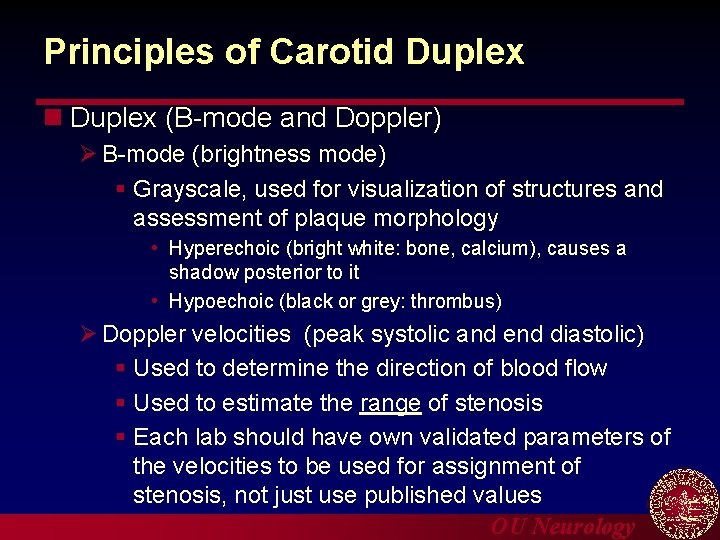
Principles of Carotid Duplex n Duplex (B-mode and Doppler) Ø B-mode (brightness mode) § Grayscale, used for visualization of structures and assessment of plaque morphology • Hyperechoic (bright white: bone, calcium), causes a shadow posterior to it • Hypoechoic (black or grey: thrombus) Ø Doppler velocities (peak systolic and end diastolic) § Used to determine the direction of blood flow § Used to estimate the range of stenosis § Each lab should have own validated parameters of the velocities to be used for assignment of stenosis, not just use published values OU Neurology
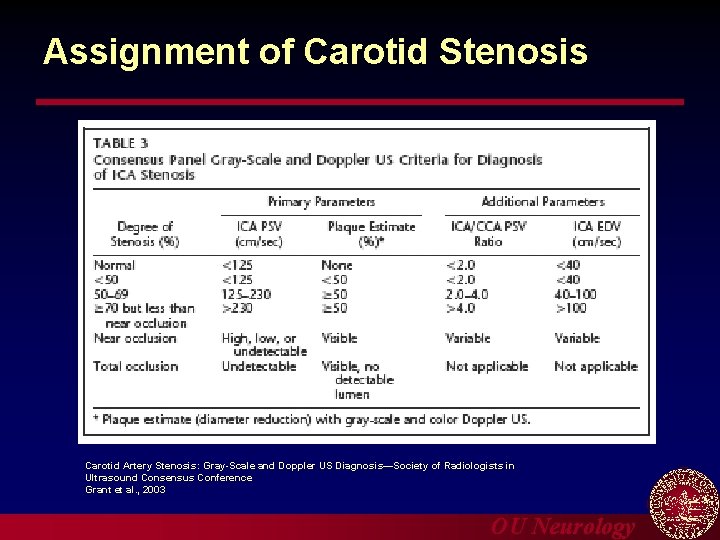
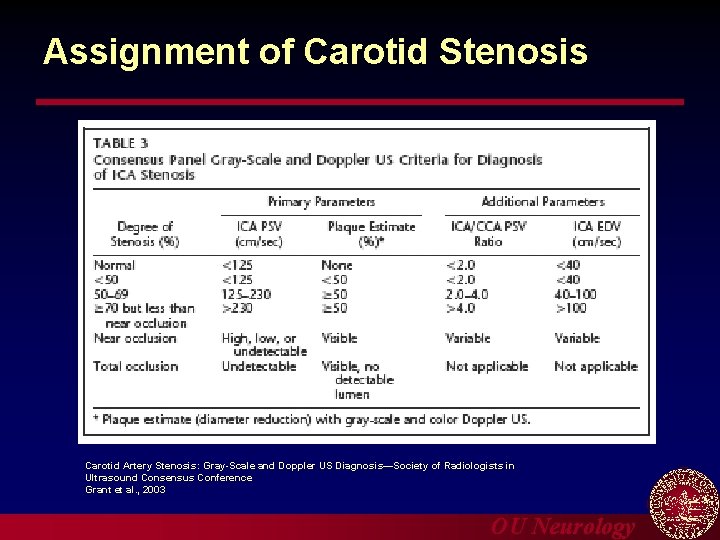
Assignment of Carotid Stenosis Carotid Artery Stenosis: Gray-Scale and Doppler US Diagnosis—Society of Radiologists in Ultrasound Consensus Conference Grant et al. , 2003 OU Neurology
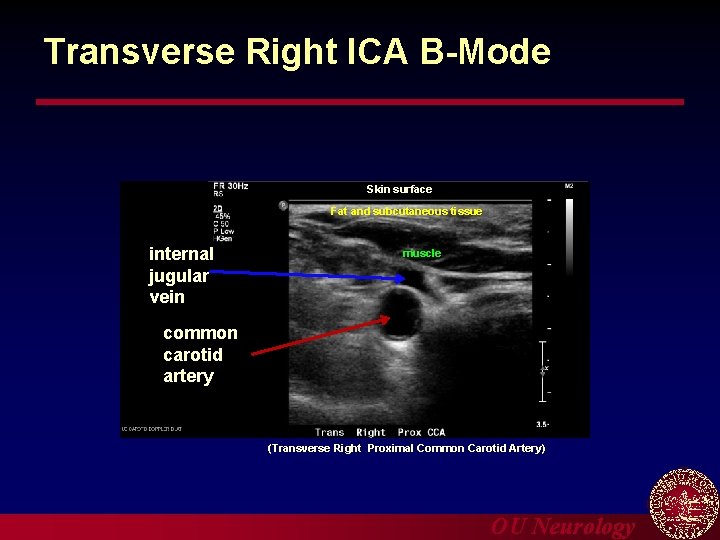
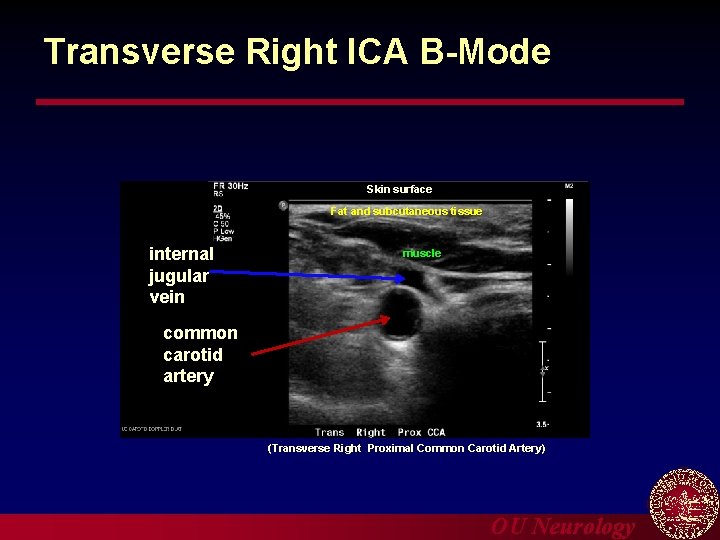
Transverse Right ICA B-Mode Skin surface Fat and subcutaneous tissue internal jugular vein muscle common carotid artery (Transverse Right Proximal Common Carotid Artery) OU Neurology
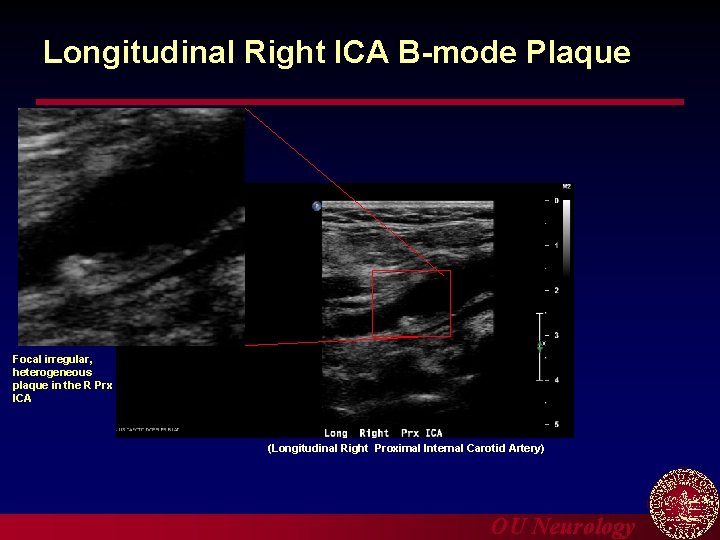
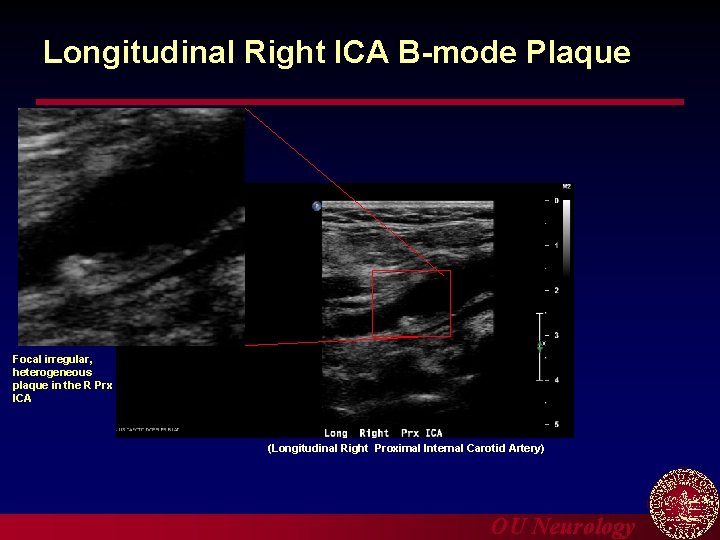
Longitudinal Right ICA B-mode Plaque Focal irregular, heterogeneous plaque in the R Prx ICA (Longitudinal Right Proximal Internal Carotid Artery) OU Neurology
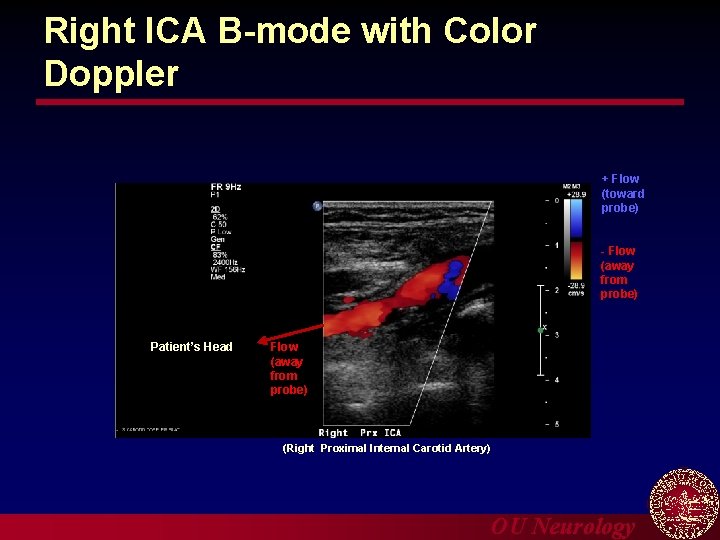
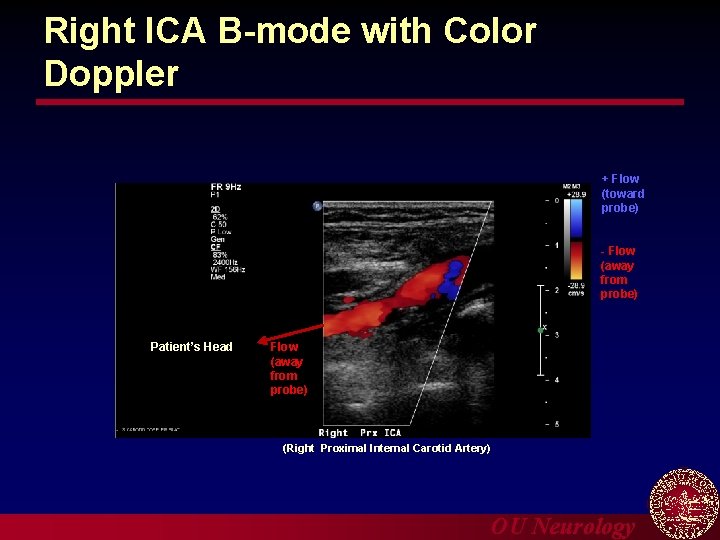
Right ICA B-mode with Color Doppler + Flow (toward probe) - Flow (away from probe) Patient’s Head Flow (away from probe) (Right Proximal Internal Carotid Artery) OU Neurology
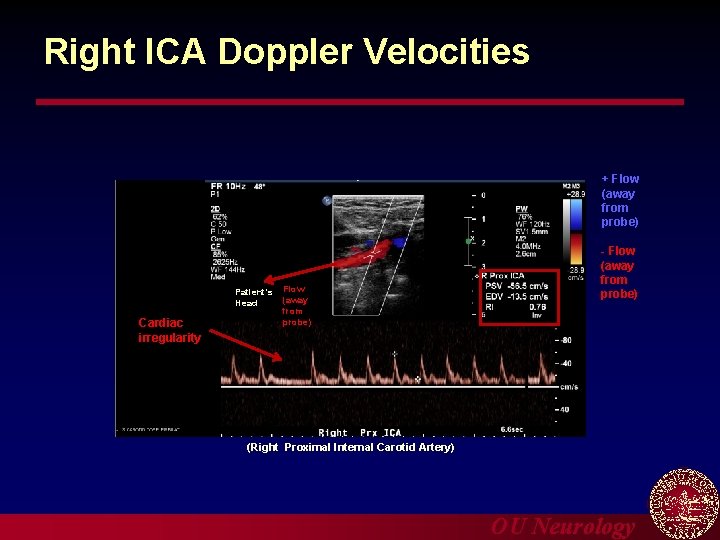
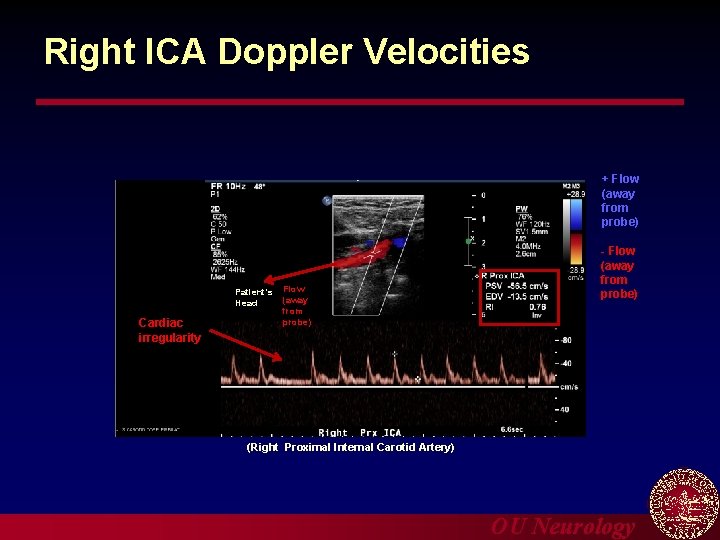
Right ICA Doppler Velocities + Flow (away from probe) Patient’s Head Cardiac irregularity Flow (away from probe) - Flow (away from probe) (Right Proximal Internal Carotid Artery) OU Neurology
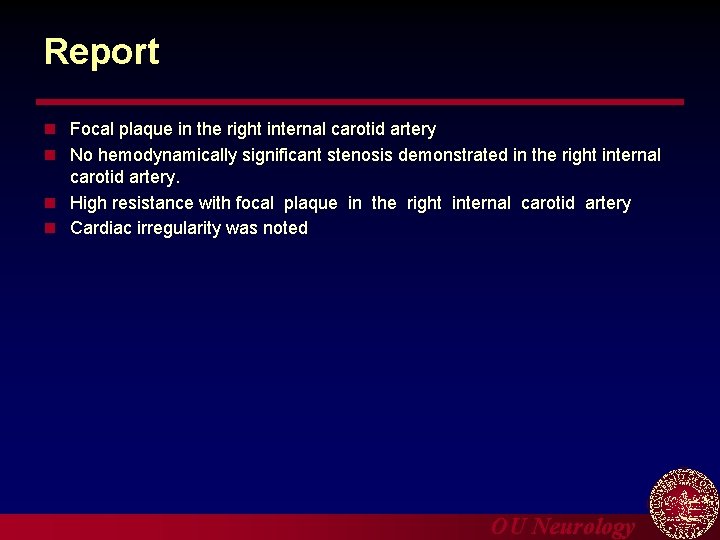
Report n Focal plaque in the right internal carotid artery n No hemodynamically significant stenosis demonstrated in the right internal carotid artery. n High resistance with focal plaque in the right internal carotid artery n Cardiac irregularity was noted OU Neurology
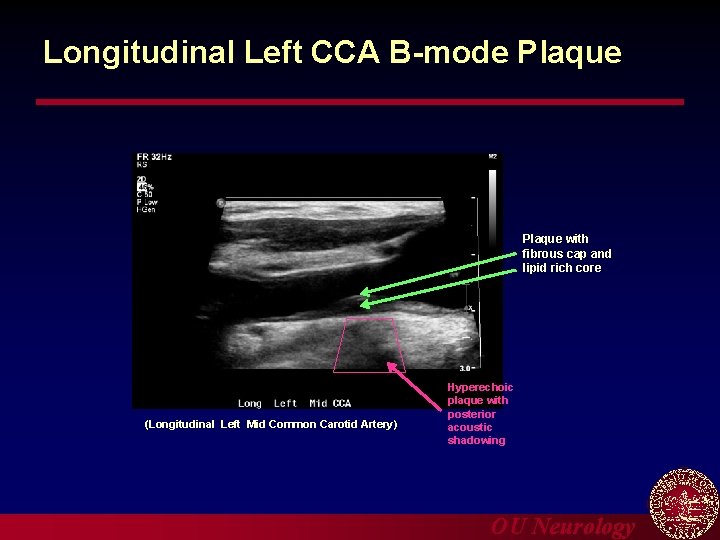
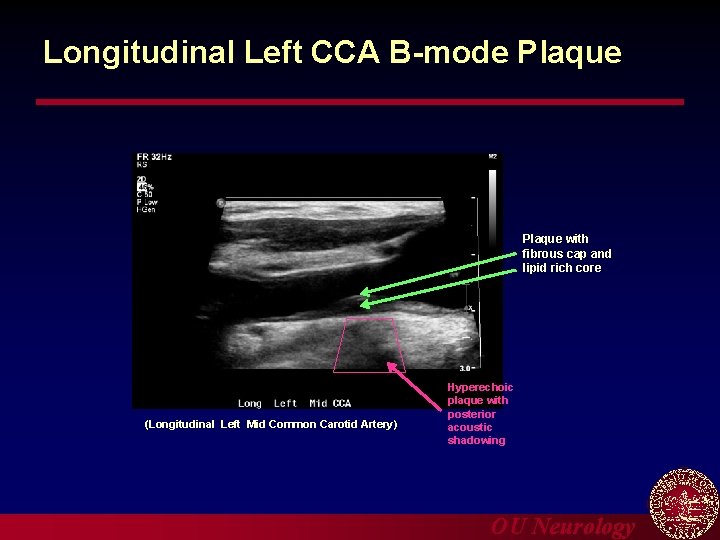
Longitudinal Left CCA B-mode Plaque with fibrous cap and lipid rich core (Longitudinal Left Mid Common Carotid Artery) Hyperechoic plaque with posterior acoustic shadowing OU Neurology
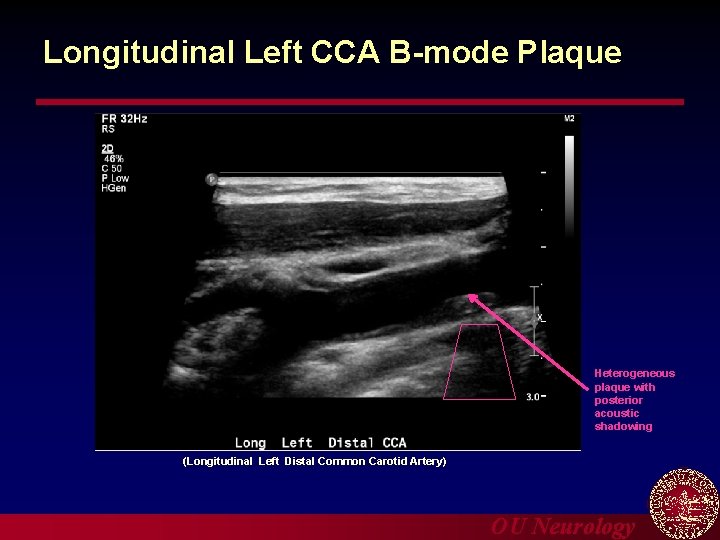
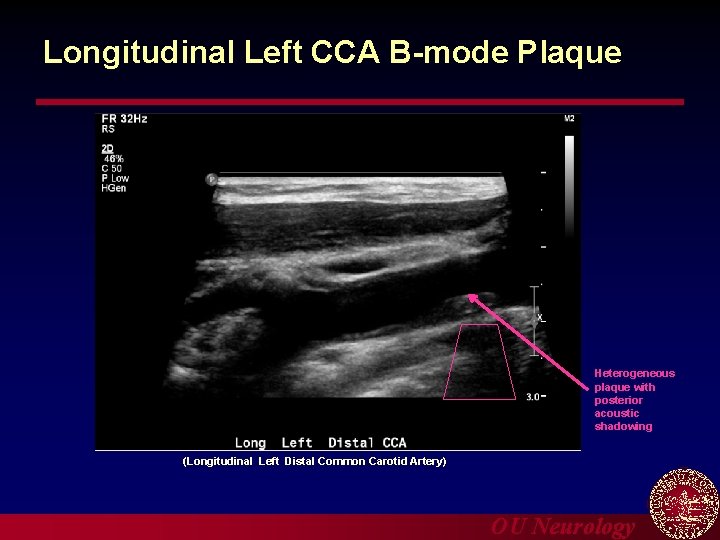
Longitudinal Left CCA B-mode Plaque Heterogeneous plaque with posterior acoustic shadowing (Longitudinal Left Distal Common Carotid Artery) OU Neurology
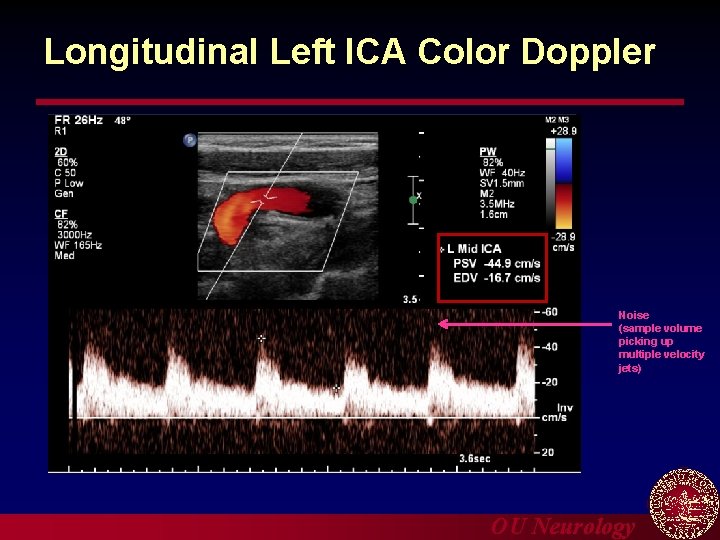
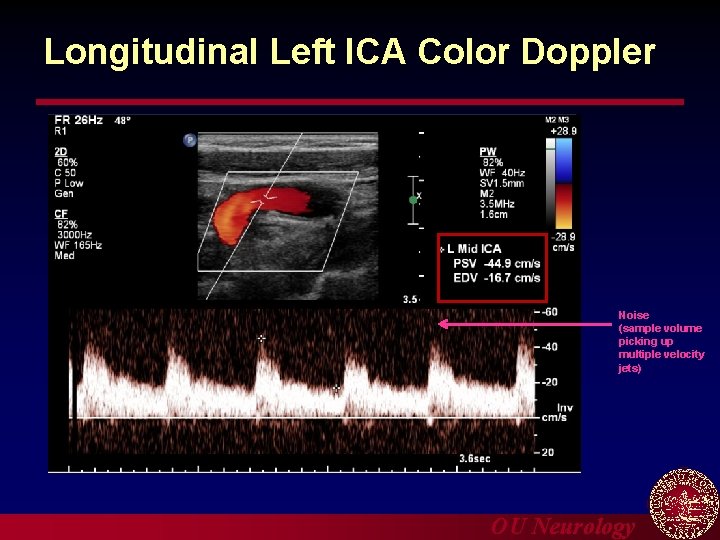
Longitudinal Left ICA Color Doppler Noise (sample volume picking up multiple velocity jets) OU Neurology
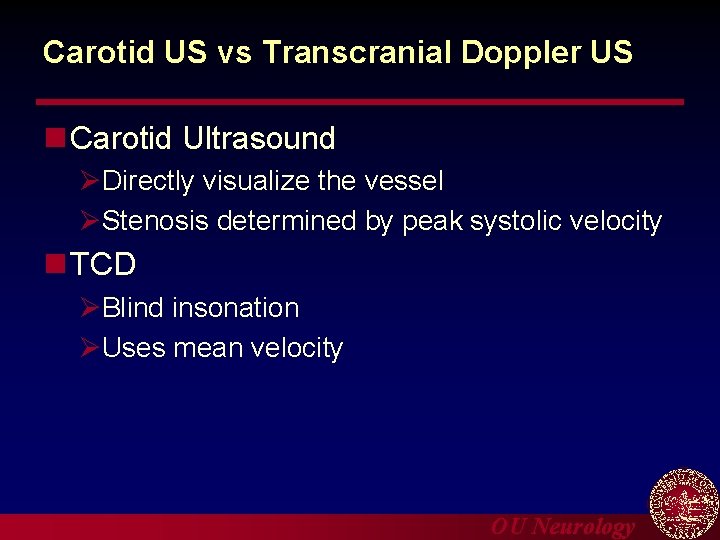
Carotid US vs Transcranial Doppler US n Carotid Ultrasound ØDirectly visualize the vessel ØStenosis determined by peak systolic velocity n TCD ØBlind insonation ØUses mean velocity OU Neurology
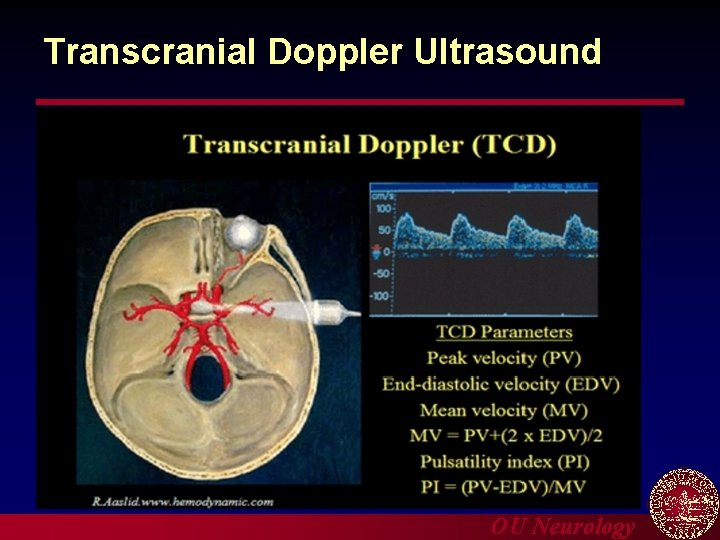
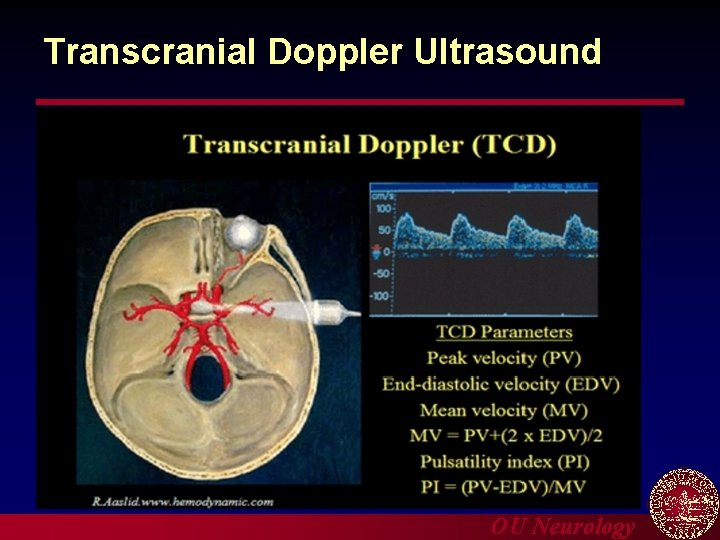
Transcranial Doppler Ultrasound OU Neurology
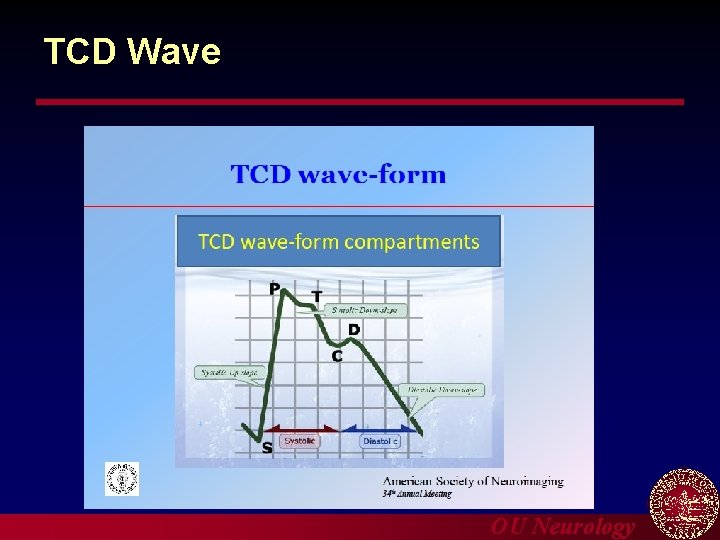
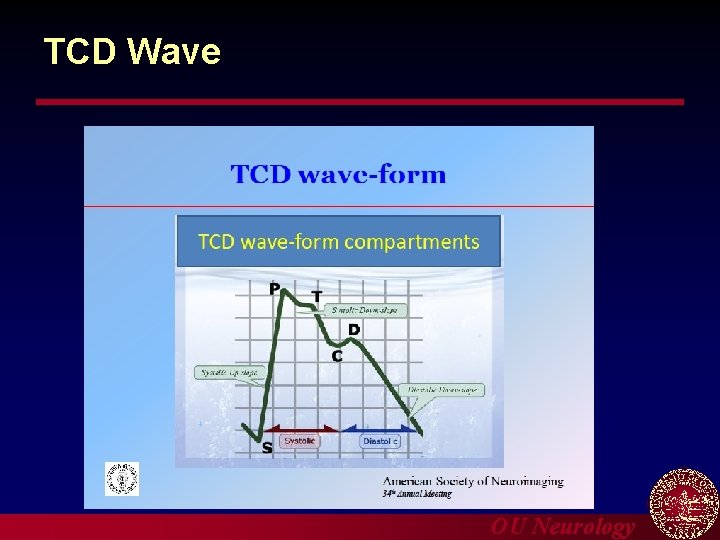
TCD Wave OU Neurology
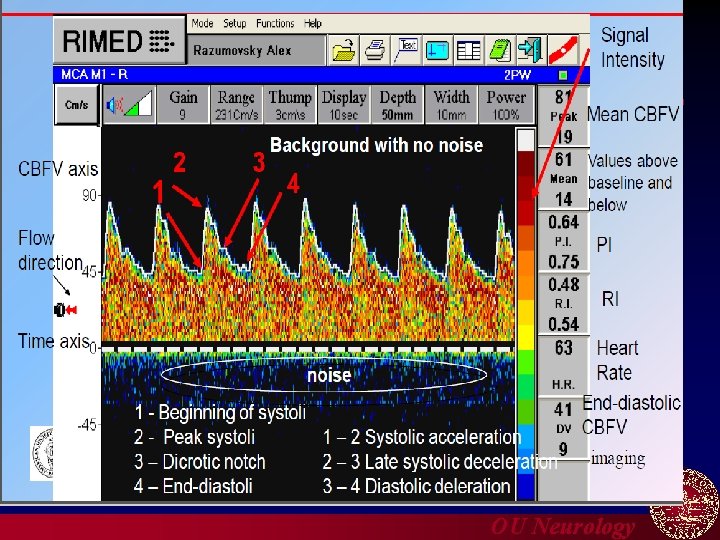
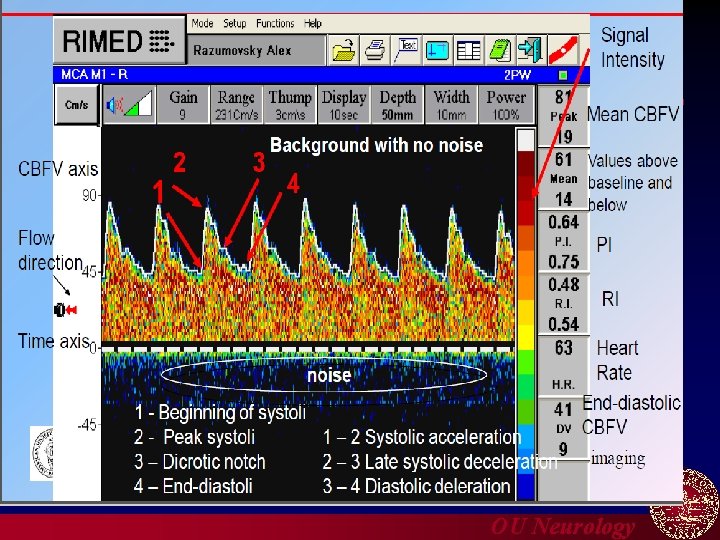
OU Neurology
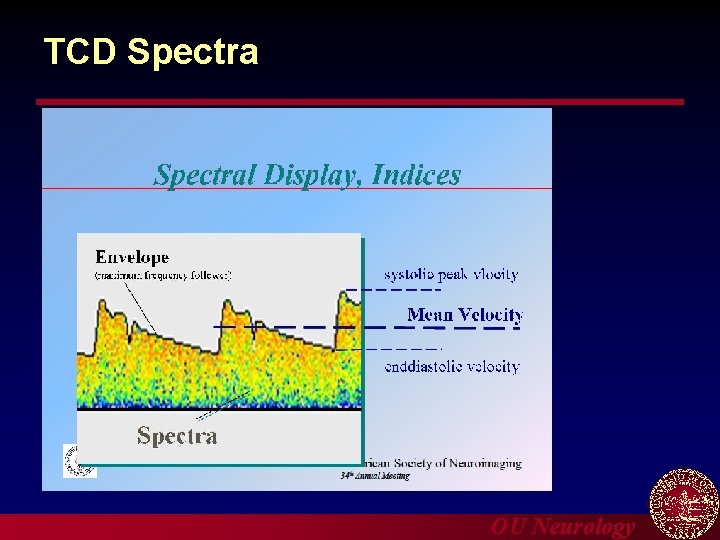
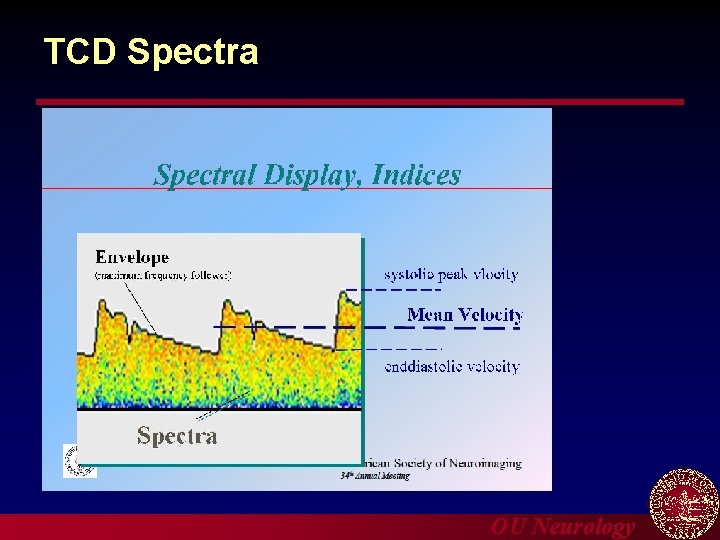
TCD Spectra OU Neurology
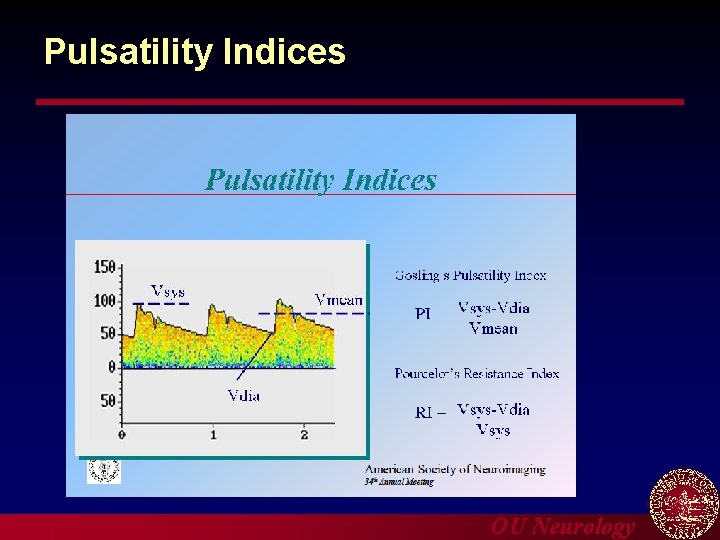
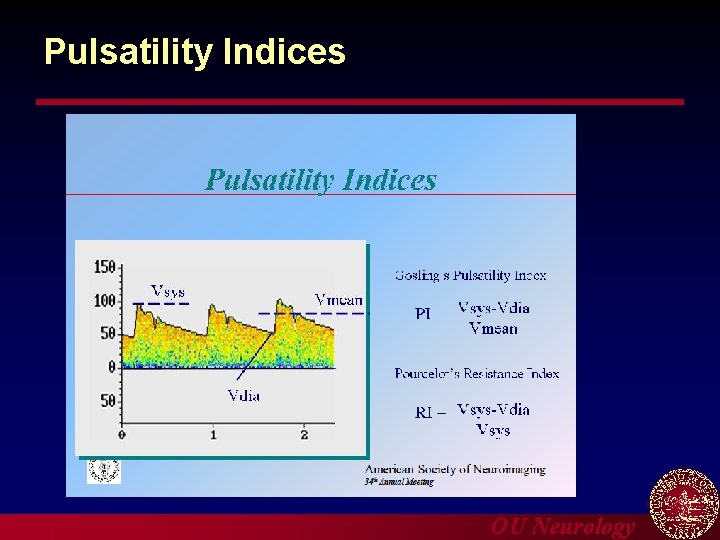
Pulsatility Indices OU Neurology
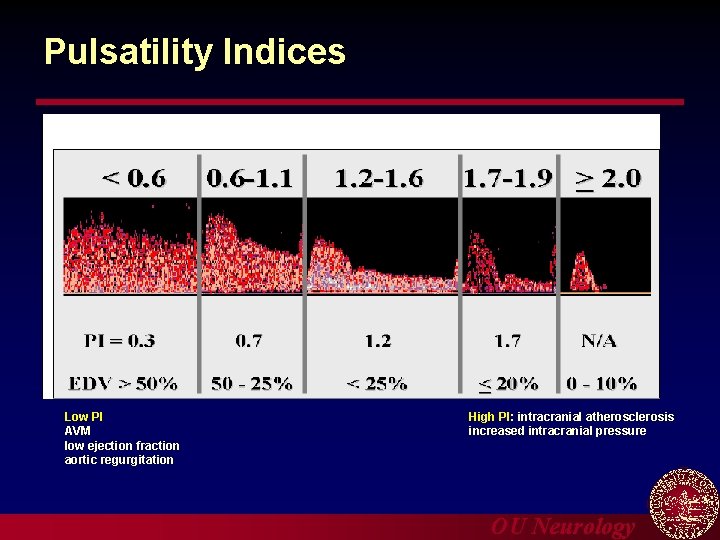
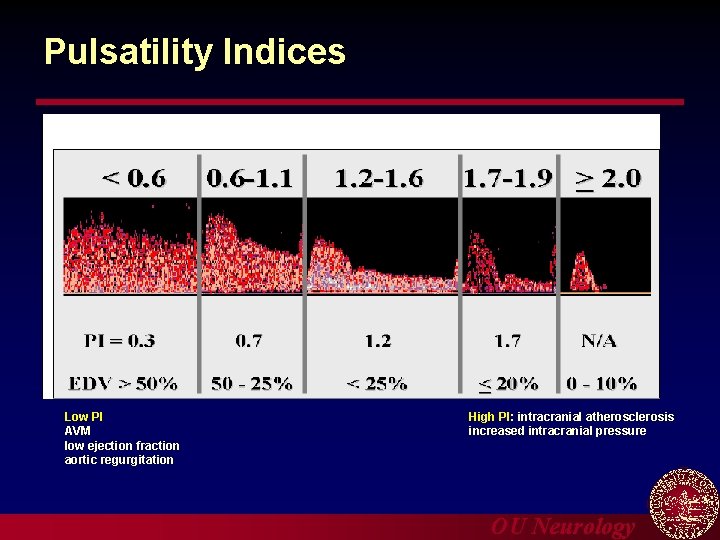
Pulsatility Indices Low PI AVM low ejection fraction aortic regurgitation High PI: intracranial atherosclerosis increased intracranial pressure OU Neurology
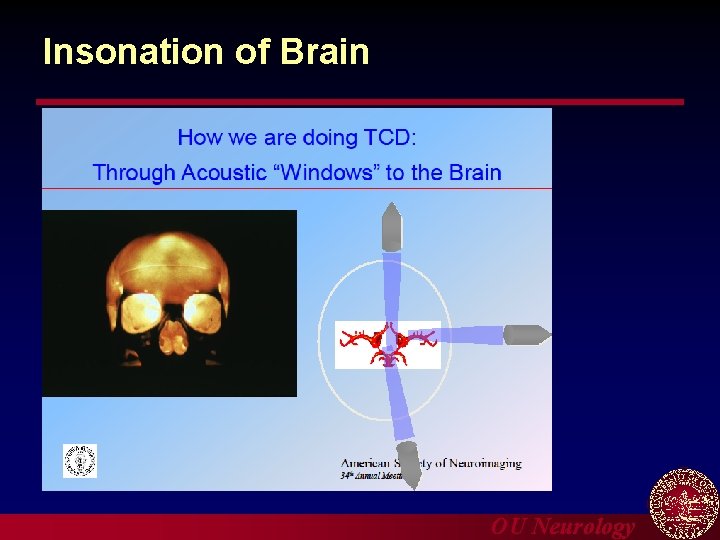
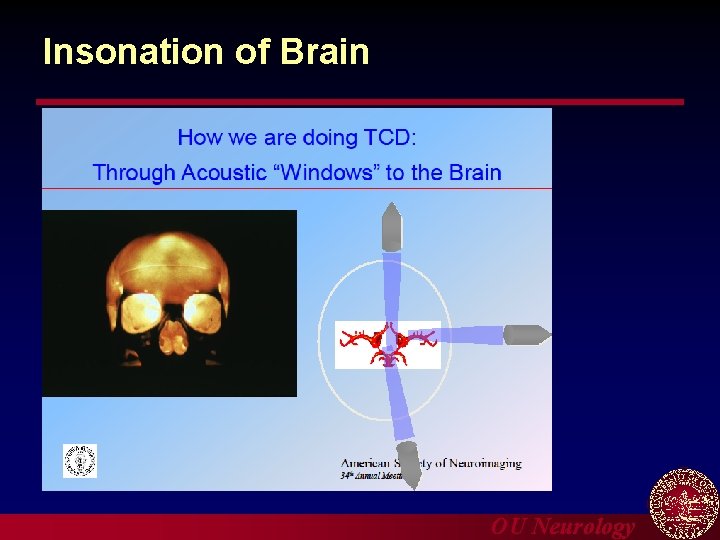
Insonation of Brain OU Neurology
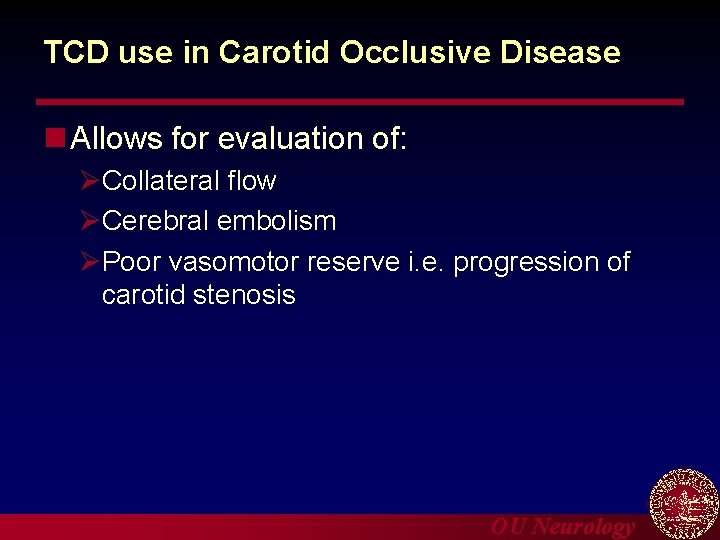
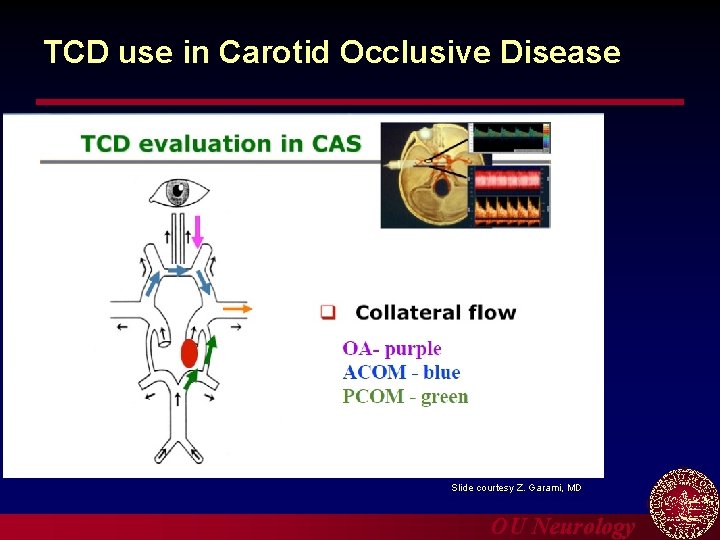
TCD use in Carotid Occlusive Disease n Allows for evaluation of: ØCollateral flow ØCerebral embolism ØPoor vasomotor reserve i. e. progression of carotid stenosis OU Neurology
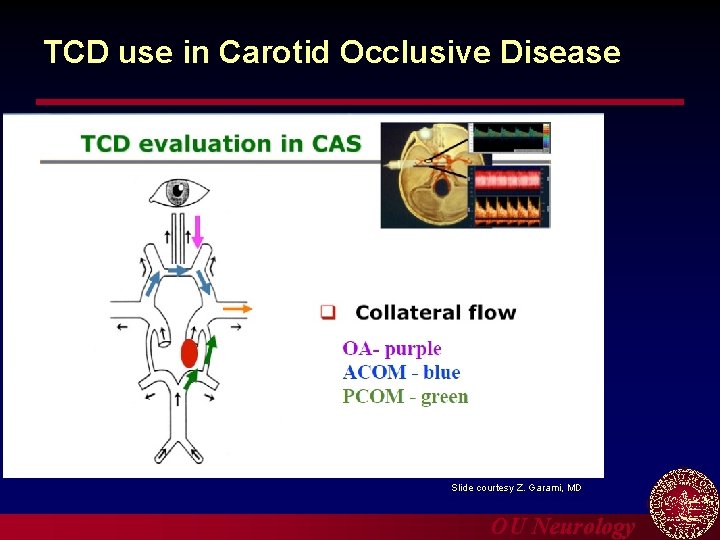
TCD use in Carotid Occlusive Disease Slide courtesy Z. Garami, MD OU Neurology
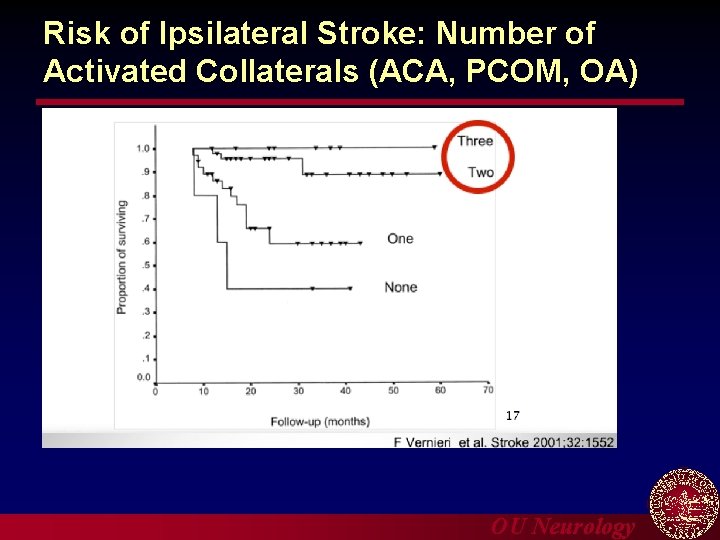
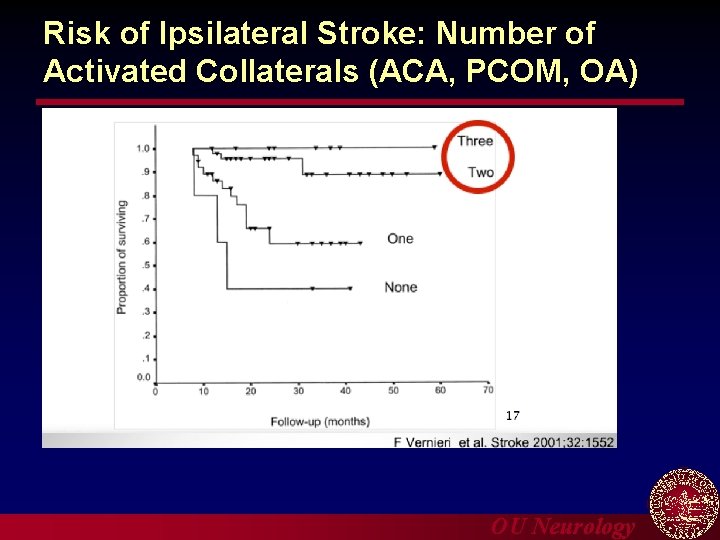
Risk of Ipsilateral Stroke: Number of Activated Collaterals (ACA, PCOM, OA) OU Neurology
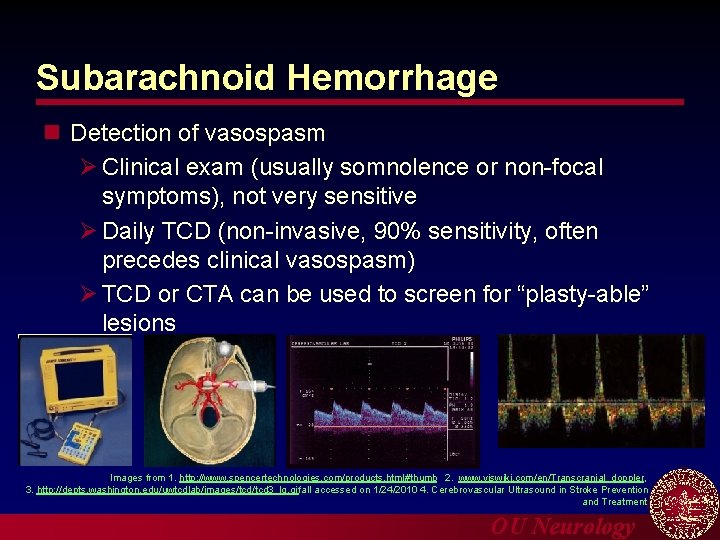
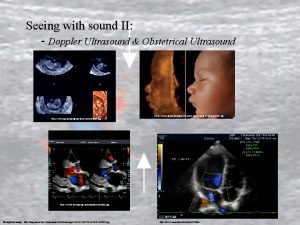
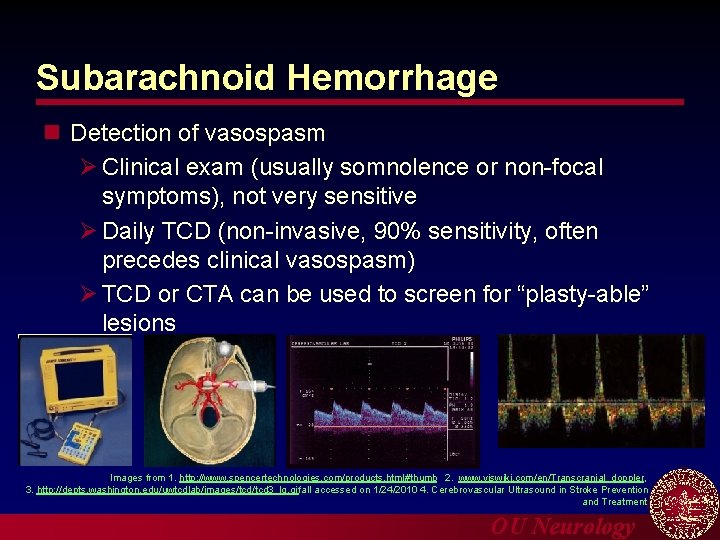
Subarachnoid Hemorrhage n Detection of vasospasm Ø Clinical exam (usually somnolence or non-focal symptoms), not very sensitive Ø Daily TCD (non-invasive, 90% sensitivity, often precedes clinical vasospasm) Ø TCD or CTA can be used to screen for “plasty-able” lesions Images from 1. http: //www. spencertechnologies. com/products. html#thumb 2. www. viswiki. com/en/Transcranial_doppler, 3. http: //depts. washington. edu/uwtcdlab/images/tcd 3_lg. gif all accessed on 1/24/2010 4. Cerebrovascular Ultrasound in Stroke Prevention and Treatment OU Neurology
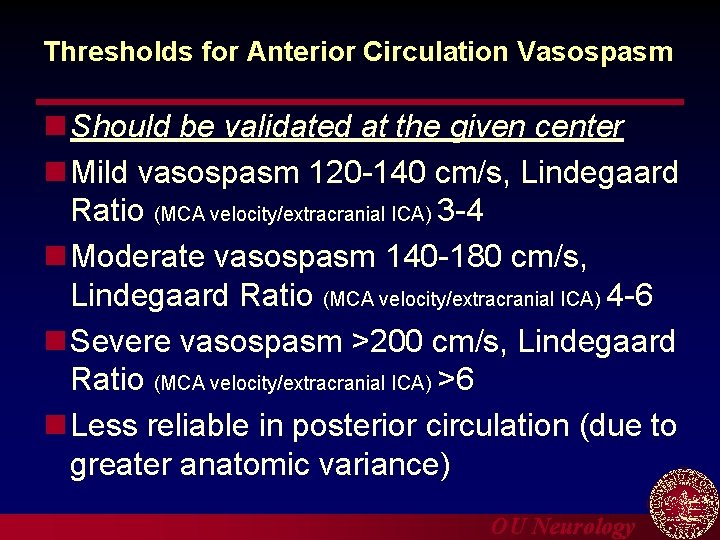
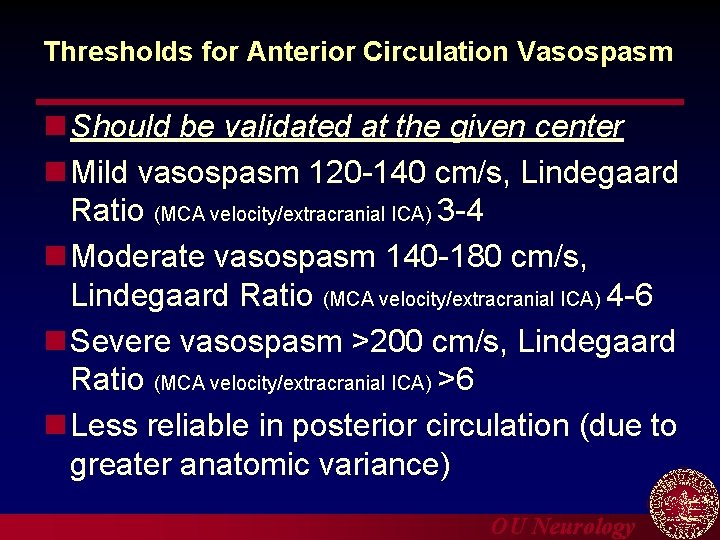
Thresholds for Anterior Circulation Vasospasm n Should be validated at the given center n Mild vasospasm 120 -140 cm/s, Lindegaard Ratio (MCA velocity/extracranial ICA) 3 -4 n Moderate vasospasm 140 -180 cm/s, Lindegaard Ratio (MCA velocity/extracranial ICA) 4 -6 n Severe vasospasm >200 cm/s, Lindegaard Ratio (MCA velocity/extracranial ICA) >6 n Less reliable in posterior circulation (due to greater anatomic variance) OU Neurology
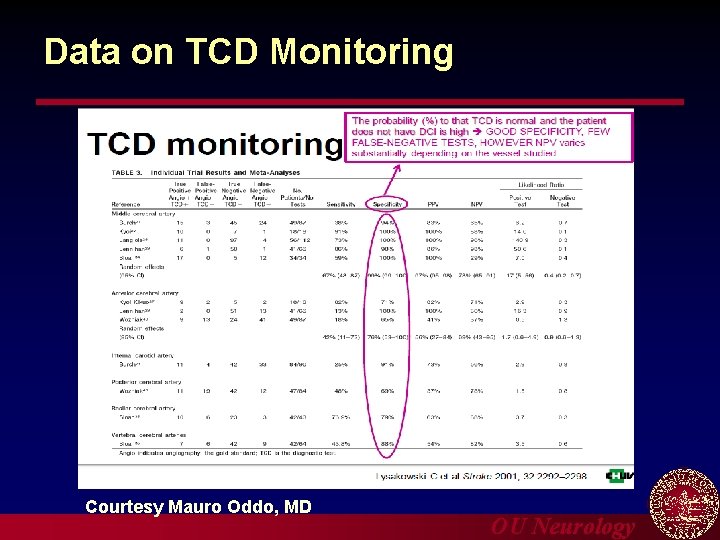
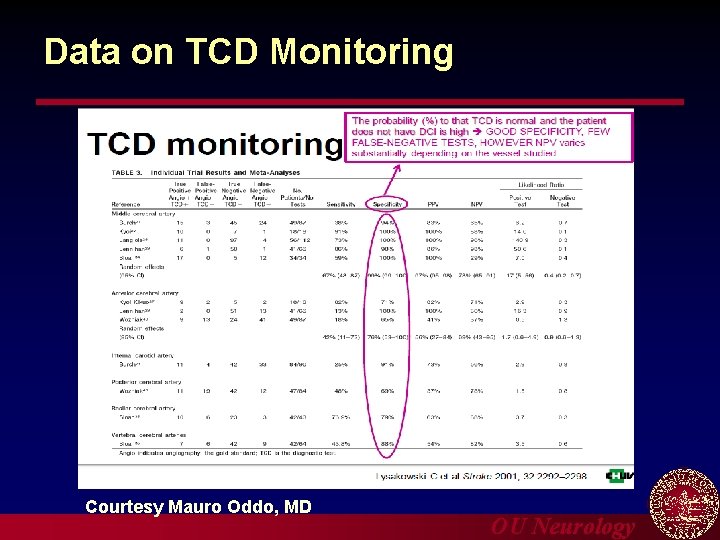
Data on TCD Monitoring Courtesy Mauro Oddo, MD OU Neurology
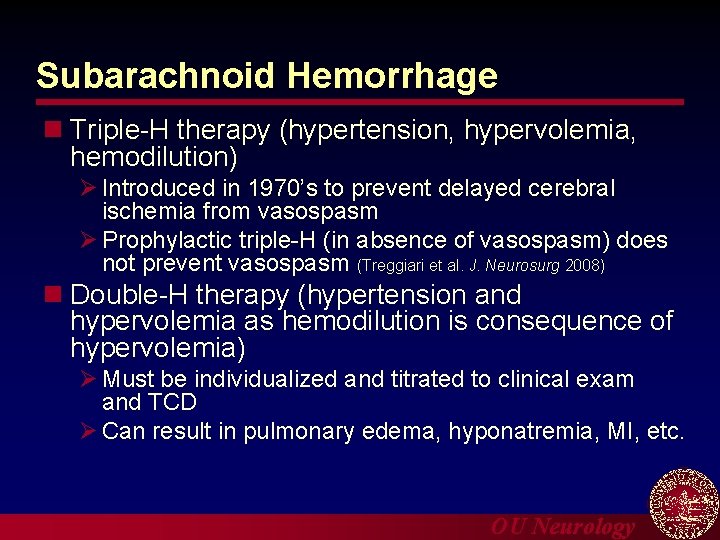
Subarachnoid Hemorrhage n Triple-H therapy (hypertension, hypervolemia, hemodilution) Ø Introduced in 1970’s to prevent delayed cerebral ischemia from vasospasm Ø Prophylactic triple-H (in absence of vasospasm) does not prevent vasospasm (Treggiari et al. J. Neurosurg 2008) n Double-H therapy (hypertension and hypervolemia as hemodilution is consequence of hypervolemia) Ø Must be individualized and titrated to clinical exam and TCD Ø Can result in pulmonary edema, hyponatremia, MI, etc. OU Neurology
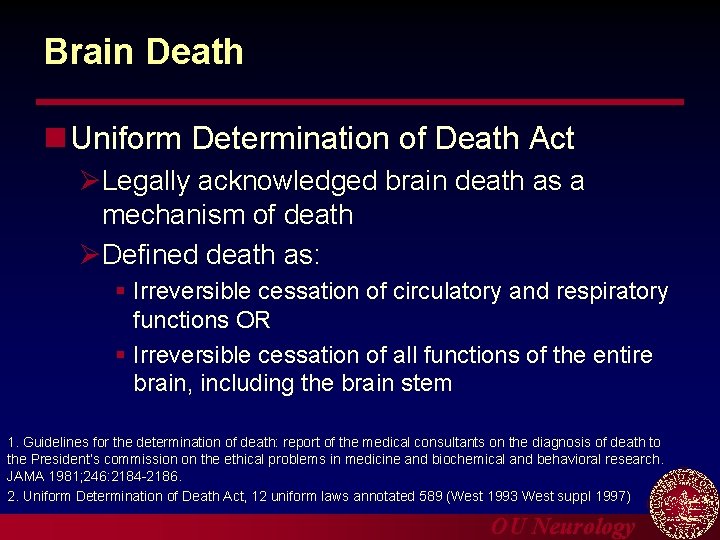
Brain Death n Uniform Determination of Death Act ØLegally acknowledged brain death as a mechanism of death ØDefined death as: § Irreversible cessation of circulatory and respiratory functions OR § Irreversible cessation of all functions of the entire brain, including the brain stem 1. Guidelines for the determination of death: report of the medical consultants on the diagnosis of death to the President’s commission on the ethical problems in medicine and biochemical and behavioral research. JAMA 1981; 246: 2184 -2186. 2. Uniform Determination of Death Act, 12 uniform laws annotated 589 (West 1993 West suppl 1997) OU Neurology
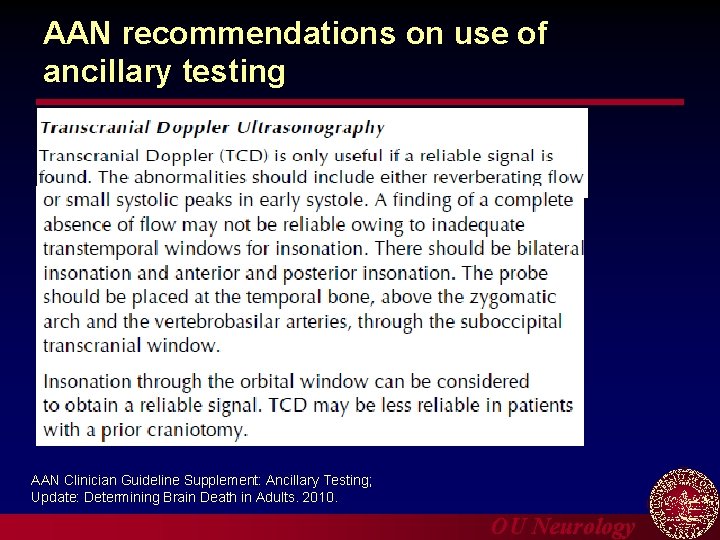
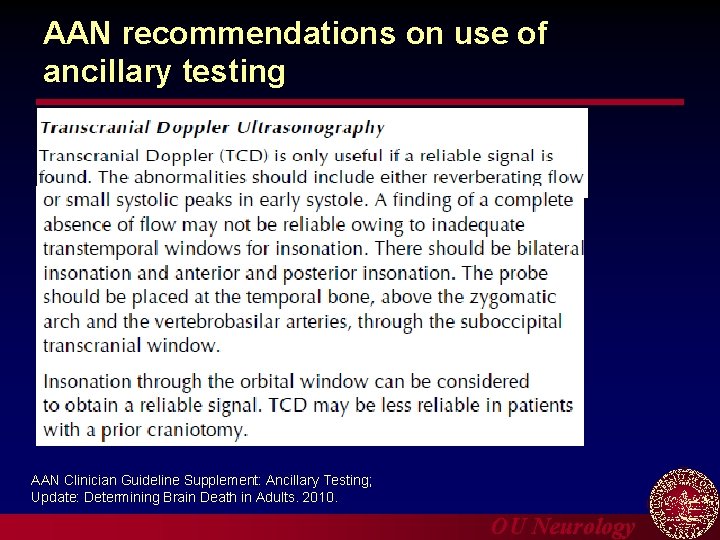
AAN recommendations on use of ancillary testing AAN Clinician Guideline Supplement: Ancillary Testing; Update: Determining Brain Death in Adults. 2010. OU Neurology
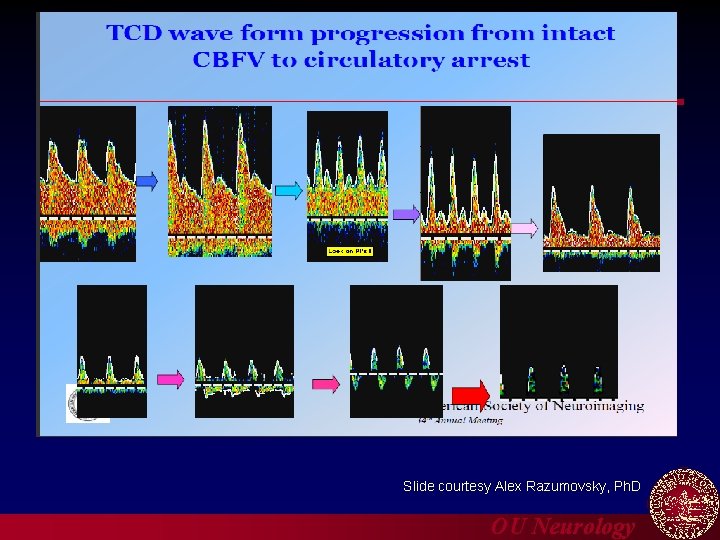
Diagnosis of Patent Foramen Ovale (PFO) Slide courtesy Alex Razumovsky, Ph. D OU Neurology
Diagnosis of Patent Foramen Ovale (PFO) n PFO is a residual channel between the right and left atrium which originally allowed oxygenated placental blood to pass from the right to left atrium bypassing the fetal lungs n Usually closes by age 2, but can persist in 25 -30% of the general population OU Neurology
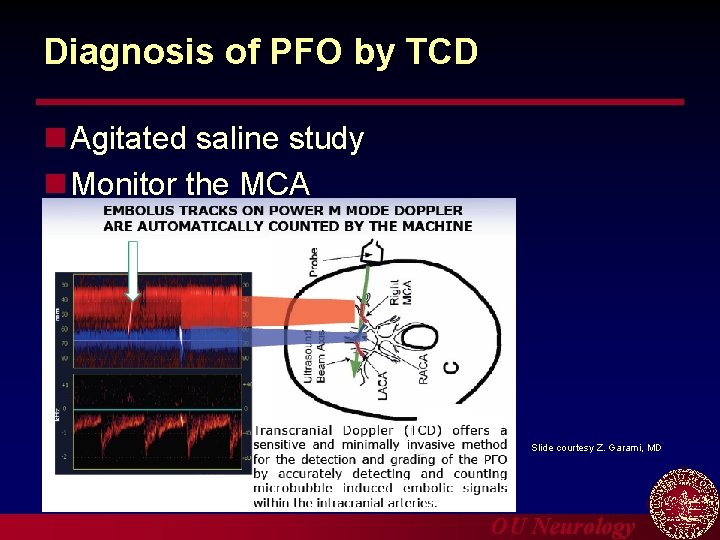
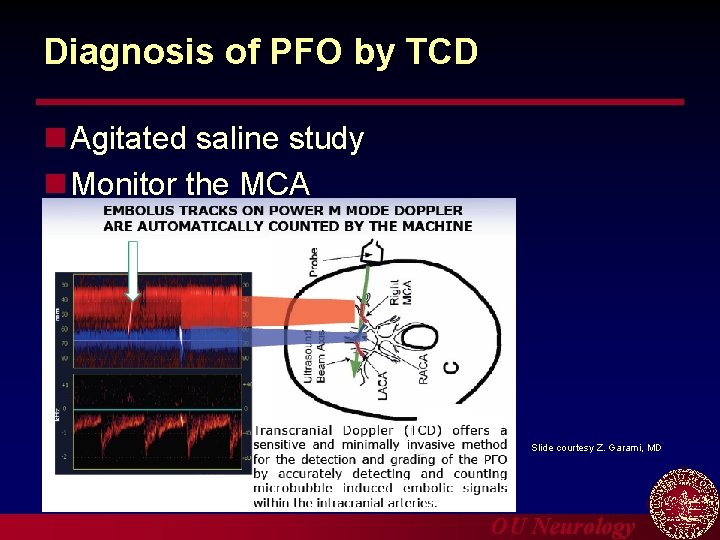
Diagnosis of PFO by TCD n Agitated saline study n Monitor the MCA Slide courtesy Z. Garami, MD OU Neurology
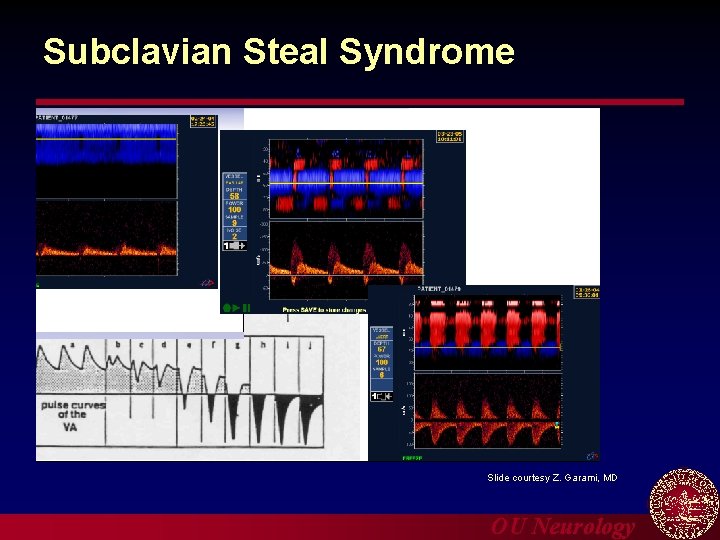
Diagnosing subclavian steal by TCD n Image the vertebral artery n Ischemic cuff test OU Neurology
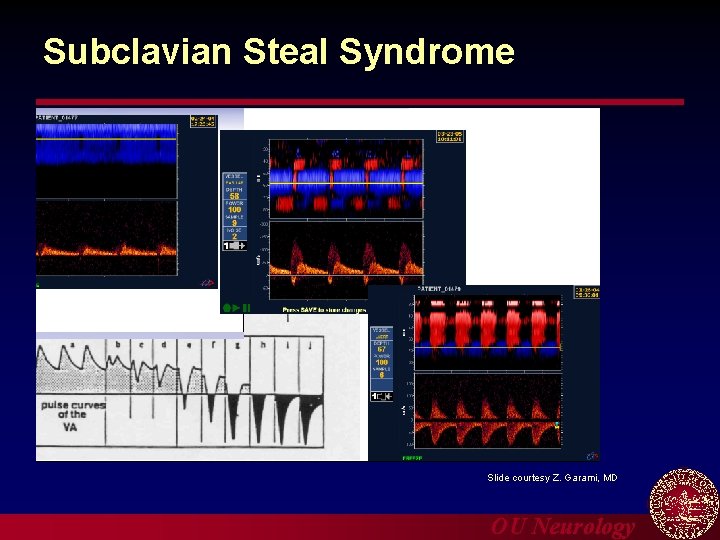
Subclavian Steal Syndrome Slide courtesy Z. Garami, MD OU Neurology
Questions Thank you OU Neurology
 Duplex ultrasound vs doppler
Duplex ultrasound vs doppler Seioh
Seioh As a baby emerges from the darkness of the womb
As a baby emerges from the darkness of the womb Testicular torsion doppler ultrasound
Testicular torsion doppler ultrasound Difference between doppler and duplex
Difference between doppler and duplex Duplex doppler ultrasound
Duplex doppler ultrasound Ferriman-gallwey score
Ferriman-gallwey score Lana schumacher md
Lana schumacher md Carotid sinus hypersensitivity
Carotid sinus hypersensitivity Facial foramen
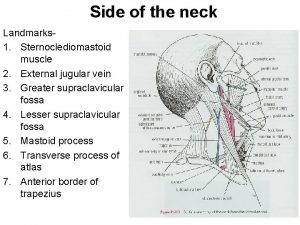
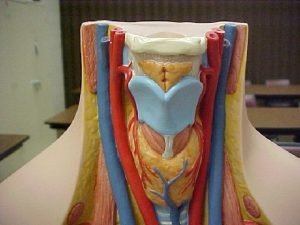
Facial foramen Contents of carotid sheath
Contents of carotid sheath Jugular vs carotid
Jugular vs carotid Parotid fascia
Parotid fascia Occipital artery
Occipital artery Carotid triangle contents
Carotid triangle contents Components of carotid sheath
Components of carotid sheath Thyrocervical trunk branches
Thyrocervical trunk branches Combat lifesaver powerpoint
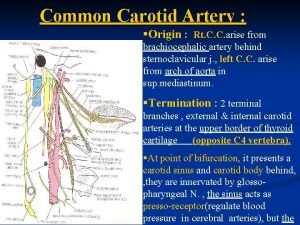
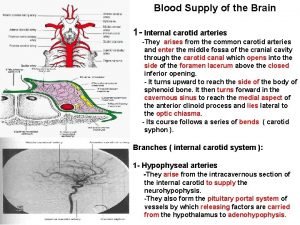
Combat lifesaver powerpoint Internal carotid artery supply
Internal carotid artery supply Triangle
Triangle Mastoid air cells
Mastoid air cells Carotid cana
Carotid cana Carotid cavernous fistula
Carotid cavernous fistula Carotid cana
Carotid cana Cat dissection labeled
Cat dissection labeled Hepatic portal vein model
Hepatic portal vein model Swollen cervical lymph nodes
Swollen cervical lymph nodes Amourosis fugax
Amourosis fugax Brain arterial supply
Brain arterial supply Carotid cochlear dehiscence
Carotid cochlear dehiscence Carotid sinus
Carotid sinus Inferior phrenic vein
Inferior phrenic vein Carotid body
Carotid body Carotid artery pulse
Carotid artery pulse Site:slidetodoc.com
Site:slidetodoc.com Eca branches
Eca branches Carotid anatomy
Carotid anatomy Mti radar with power amplifier transmitter
Mti radar with power amplifier transmitter Delay line canceller in radar
Delay line canceller in radar Laser doppler electrophoresis
Laser doppler electrophoresis