Diagnostic Medical Sonography Program Lecture 20 Transcranial Doppler

- Slides: 19
Diagnostic Medical Sonography Program • Lecture 20: Transcranial Doppler (TCD) Holdorf
Transcranial Doppler (TCD) • Capabilities: – Detect intracranial stenosis, occlusions, and assess collateral circulation – Evaluate onset, severity, and time course of vasoconstriction from subarachnoid hemorrhage – Evaluate intracranial arteriovenous malformations – Assess patients with suspected brain death
Limitations • Recent eye surgery may eliminate trans-orbital approach • Adequate penetration of temporal bone • Inaccurate vessel identification with nonimaging technique
• Patient Positioning – Patient supine and avoids speaking during examination • Physical principles – Same as pulsed Doppler
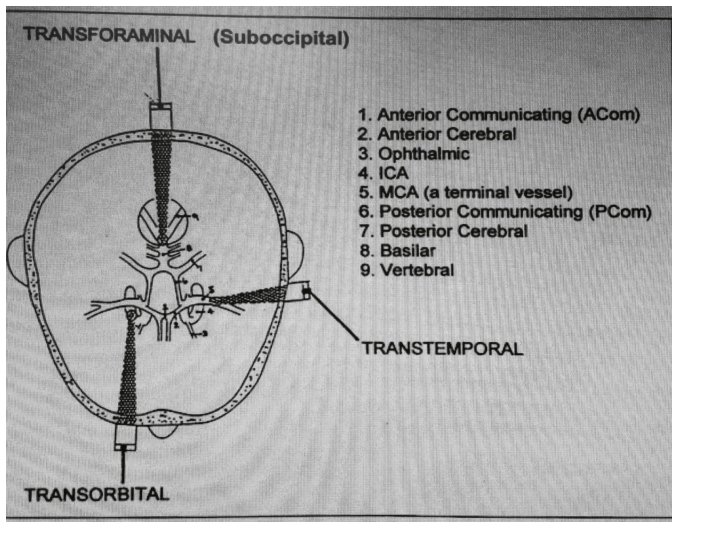
Important Points • 2 MHz pulsed Doppler used with spectrum analysis • Zero angle of insonation is assumed • Three acoustic windows used: – Trans-temporal – Trans-orbital – Trans-foraminal / sub-occipital
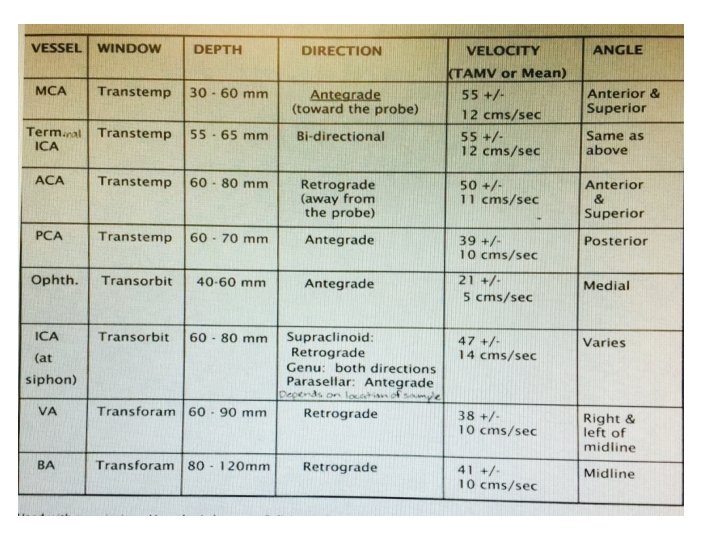
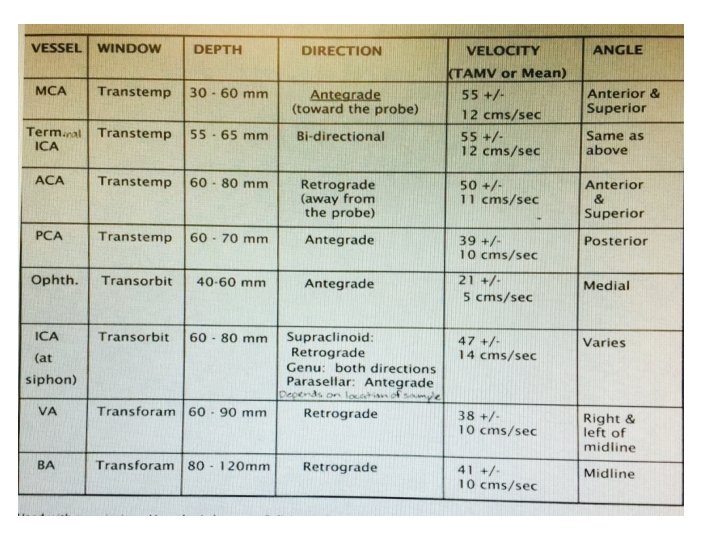
Important Points • Accurate vessel identification requires: – Depth of sample volume – Velocity of the blood flow – Direction of blood flow – Relationship of flow patterns to one another • Time averaged maximum velocity (TAMV) or mean velocity used
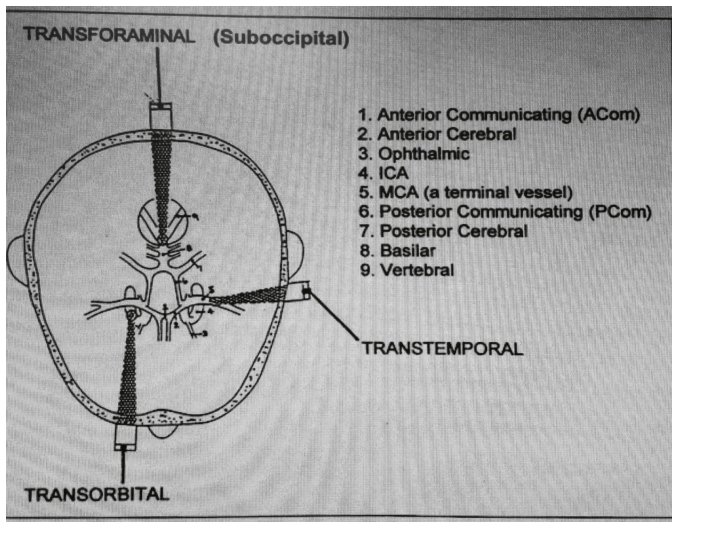
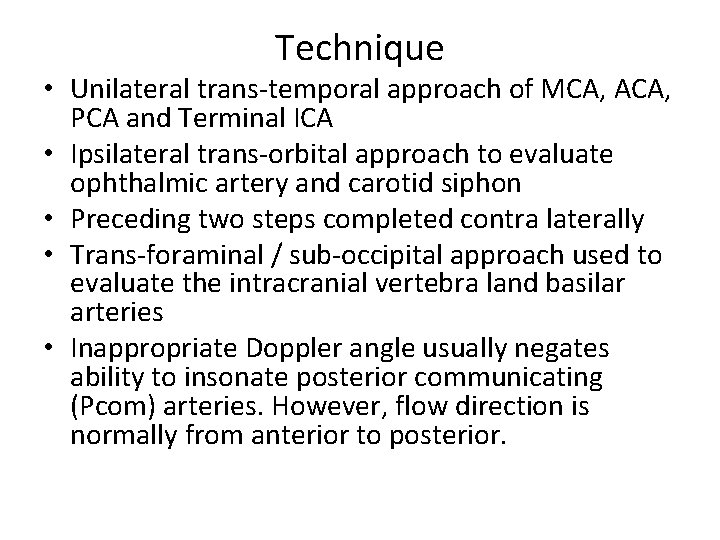
Technique • Unilateral trans-temporal approach of MCA, ACA, PCA and Terminal ICA • Ipsilateral trans-orbital approach to evaluate ophthalmic artery and carotid siphon • Preceding two steps completed contra laterally • Trans-foraminal / sub-occipital approach used to evaluate the intracranial vertebra land basilar arteries • Inappropriate Doppler angle usually negates ability to insonate posterior communicating (Pcom) arteries. However, flow direction is normally from anterior to posterior.
Interpretation • Based on flow characteristics: – Direction – Velocity – Turbulence – Pulsatility – Systolic upstroke
• Collateral Pathways – Cross-over: antegrade flow in anterior cerebral artery (ACA) from cross-over collateralization, e. g. , flow from contralateral ACA via anterior communicating artery – External-to-internal: Retrograde flow in ophthalmic artery (OA) – Posterior-to-anterior: Increased flow in posterior cerebral artery (PCA), reversing direction of flow in the Pcom artery.
• Factors that may alter intracranial blood flow, e. g. , age, sex, hematocrit, blood gases, metabolism • Occlusion: – Most accurate in ICA or MCA – Criterial similar to those used in other vessels • Vasospasm – Most accurate in MCA – Serial recordings necessary – Mean velocities > 120 cm/sec. Severe vasospasm = > 200 cm/sec
• Arteriovenous malformations – Increased systolic and diastolic flow velocities – Very low pulsatility indices – Reduced flow in adjacent arteries
Intraoperative monitoring • Capabilities: Identification of flow abnormalities may warrant change in surgical technique, e. g. , carotid endarterectomy or coronary artery bypass grafting • Technique – Headset utilized for continuous monitoring – Not working in sterile field • Interpretation – Significant decrease in MCA flow velocities during crossclamping of vessels may indicate need for shunting – Audible signals related to micro-emboli may alter surgical technique
Additional Notes: Lecture 20 Transcranial Doppler (TCD) • TCD does not image.
Collaterals: MCA: if the ipsilateral ICA is occluded Antegrade flow in the ACA means ipsilateral ICA is occluded. The monster chart • ACA- Direction is supposed to be Retrograde-away from the probe • PCA-Direction is supposed to be Antegrade- towards the probe • Ophthalmic artery- Direction is supposed to be antegrade- towards the probe • ICA at the siphon-retrograde and antegrade flow patterns. • Vertebral artery- retrograde • Basilar Artery- retrograde • DEPTH is an important question; usually asked only for the ID of the MCA. 30 -60 mm
Collateral pathways are important!!! But, can be confusing. • At this point, you need to know what the expected flow directions are (antegradetoward the probe or retrograde-away from the probe). Ex. if the MCA demonstrates retrograde flow, you know that something is not right and that there is collateral flow occurring, and that this is due to save parts of the brain that may otherwise not receive blood.
Homework • Textbook: Chapter 21: Transcranial Doppler – Pages 239 – 248 • SDMS Assignments
