Diagnostic Medical Sonography Program Lecture 12 Duplex Scanning

- Slides: 33
Diagnostic Medical Sonography Program • Lecture 12: Duplex Scanning and Color Flow Imaging of the Lower Extremities • Holdorf
Duplex / Color Flow Imaging of the Lower Extremities • Capabilities: – Determines presence or absence of > 50% diameter reduction of occlusion – Determines presence or absence of aneurysms – Follow-up of bypass grafts – To localize the stenotic lesion prior to balloon angioplasty
Limitations • Presence of dressings, skin staples, sutures, open wounds • Incisional tenderness, hematomas • Obesity- may be difficult to image vessels • Calcific shadowing from diabetes and or atherosclerosis
Patient Positioning • Patient supine with head on pillow • Extremity positioned close to the examiner • Patient’s hip minimally rotated externally, with knee flexed • Prone or lateral decubitus position may be required for assessment of popliteal artery
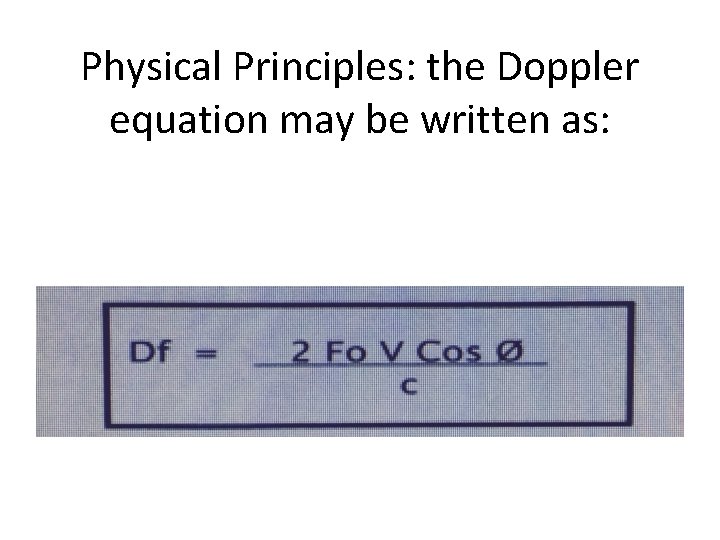
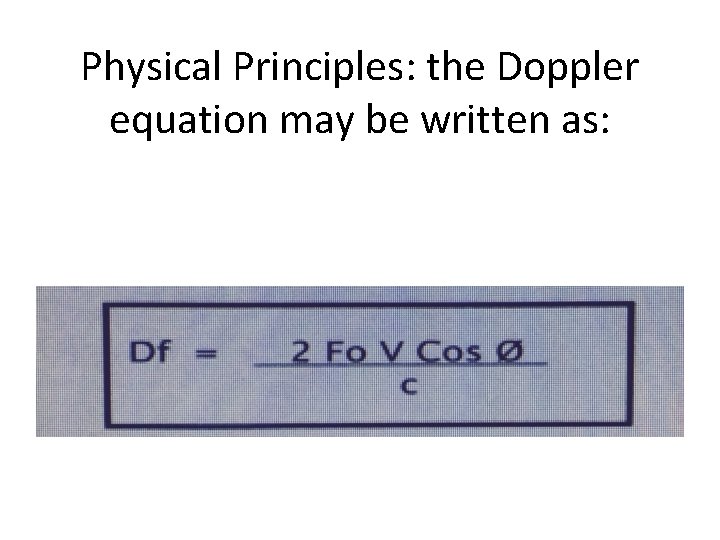
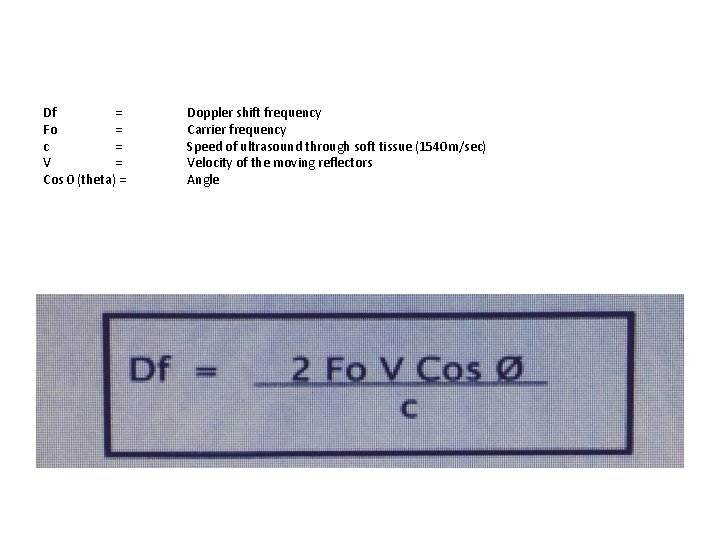
Physical Principles: the Doppler equation may be written as:
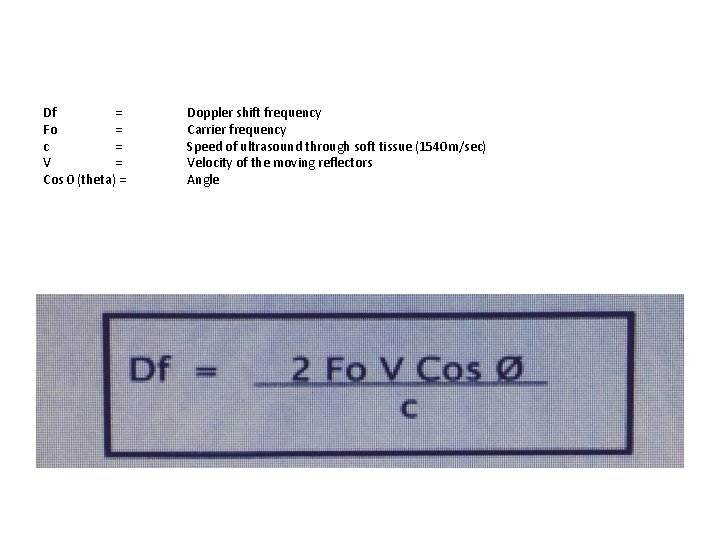
Df = Fo = c = V = Cos 0 (theta) = Doppler shift frequency Carrier frequency Speed of ultrasound through soft tissue (1540 m/sec) Velocity of the moving reflectors Angle
• Ideal Doppler angle for vascular exams is 60 degrees, obtained center-stream, parallel to walls. • Vessel tortuosity and other conditions will cause the Doppler angle to be < 60 degrees, which IS usable. • Not reliable: Doppler angle > than 60 degrees.
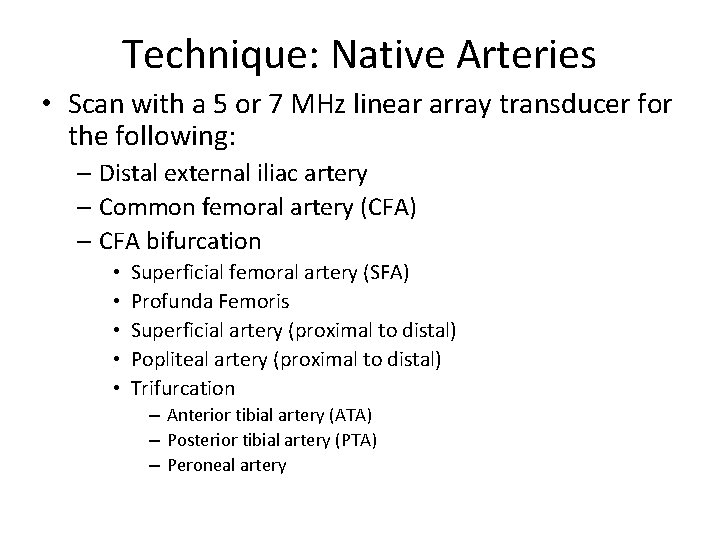
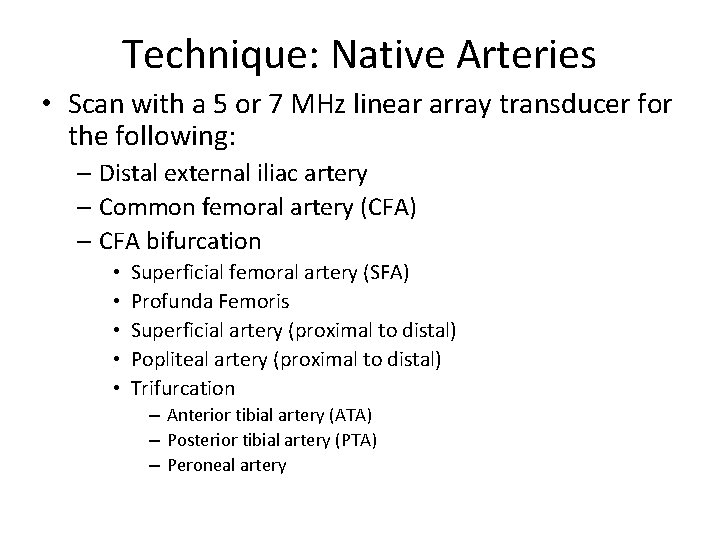
Technique: Native Arteries • Scan with a 5 or 7 MHz linear array transducer for the following: – Distal external iliac artery – Common femoral artery (CFA) – CFA bifurcation • • • Superficial femoral artery (SFA) Profunda Femoris Superficial artery (proximal to distal) Popliteal artery (proximal to distal) Trifurcation – Anterior tibial artery (ATA) – Posterior tibial artery (PTA) – Peroneal artery
• Observe gray scale for plaque or other abnormalities • Observe color flow patterns • Obtain peak systolic velocities (PSV) from each major vessel (proximal, mid and distal if vessel is long) and more if disease suspected – Characterize the Doppler signals: triphasic (normal). Biphasic, or monophasic (abnormal) – Observe wave form for any spectral broadening
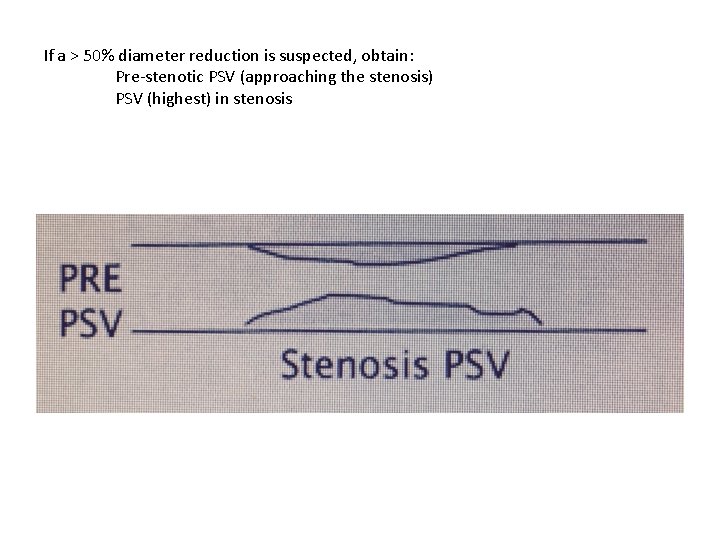
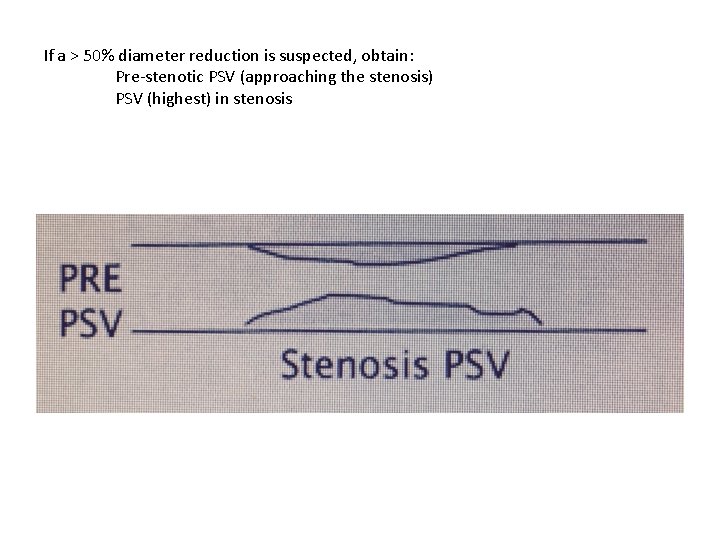
If a > 50% diameter reduction is suspected, obtain: Pre-stenotic PSV (approaching the stenosis) PSV (highest) in stenosis
• Post –Stenotic turbulence signals – Document as previously described for UE
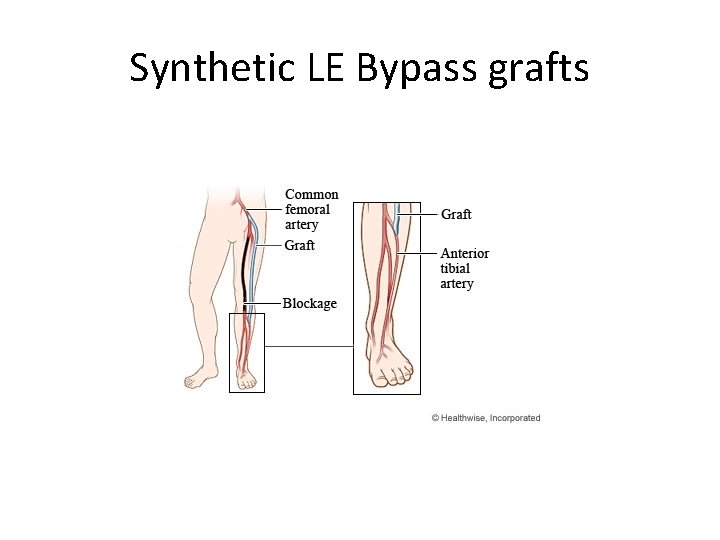
Technique: Bypass Grafts A. Know type, Location , and age: – Synthetic (e. g. Gortex)
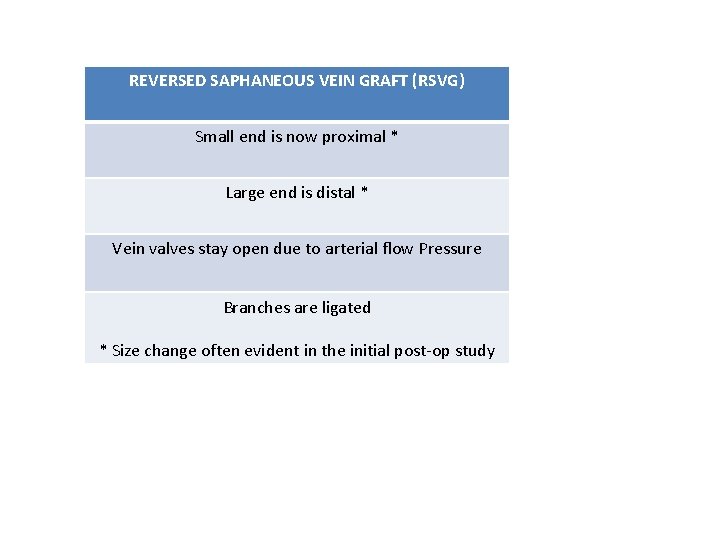
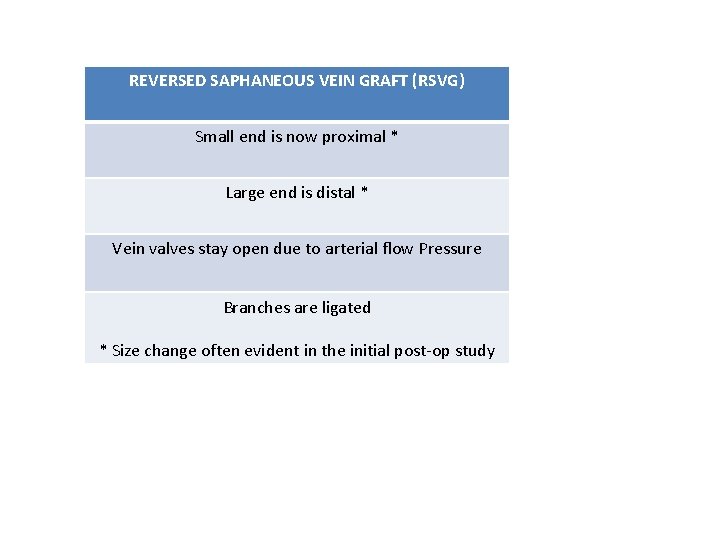
REVERSED SAPHANEOUS VEIN GRAFT (RSVG) Small end is now proximal * Large end is distal * Vein valves stay open due to arterial flow Pressure Branches are ligated * Size change often evident in the initial post-op study
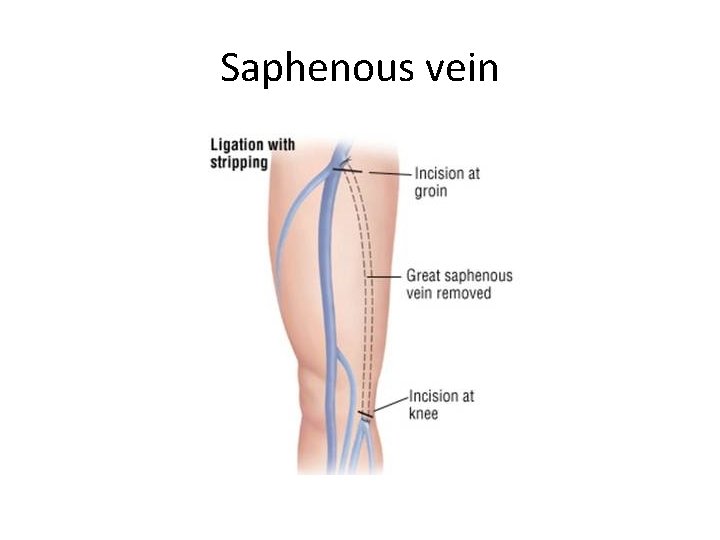
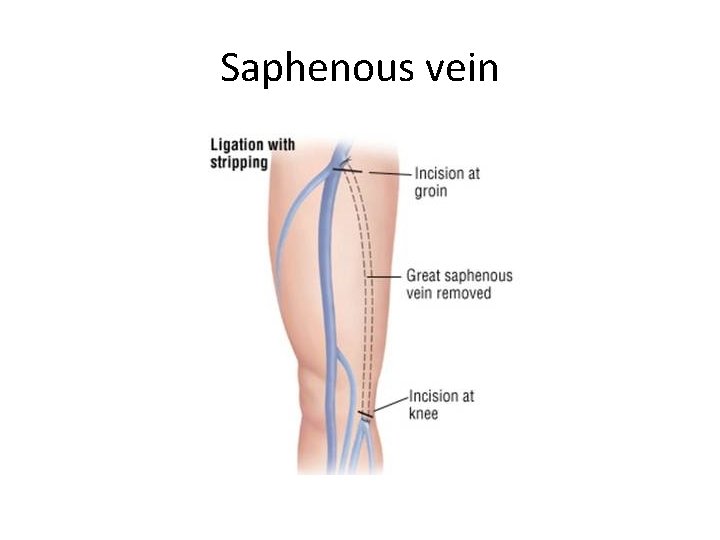
Saphenous vein
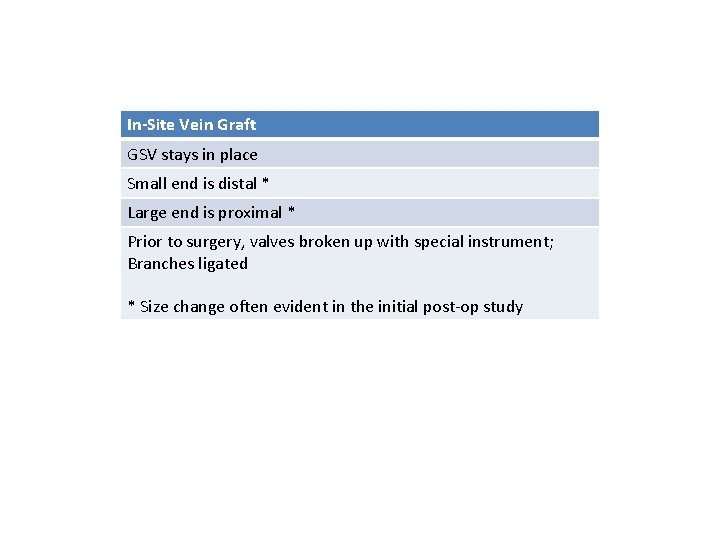
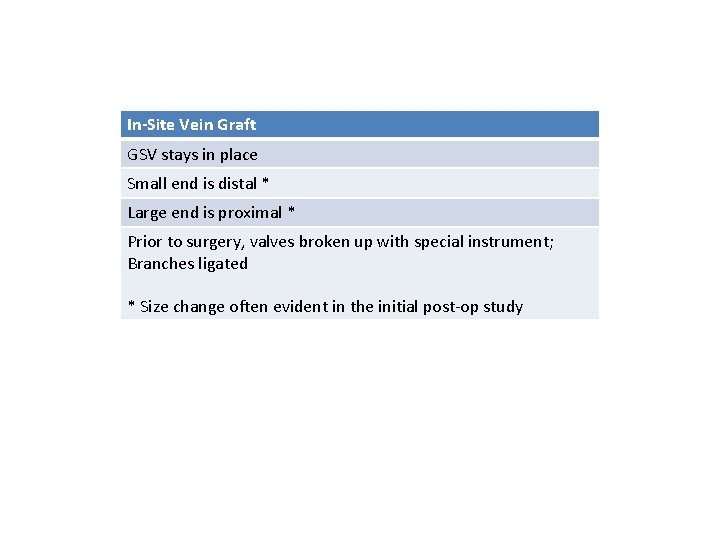
In-Site Vein Graft GSV stays in place Small end is distal * Large end is proximal * Prior to surgery, valves broken up with special instrument; Branches ligated * Size change often evident in the initial post-op study
Technique Continued… B. Protocol usually combined with ABIs. C. Vein bypass graft evaluation includes: Observation of gray scale, color flow, and PSVs of the following: Inflow artery Proximal Anastomosis Entire Length of the vein bypass graft Distal Anastomosis Outflow artery Also check for branches (that could form AV Fistulas), valves, and or other abnormalities
Technique continued… D. Synthetic bypass graft evaluation include observations of gray scale, color image, PSVs of the following: Inflow artery Proximal anastomosis Mid Graft Distal anastomosis Outflow artery
Interpretation: Native Arteries • A. Normal – Doppler signals are triphasic; a change to biphasic can be significant: however, some patients normally have biphasic flow without evidence of disease
B. Abnormal findings Compare stenotic PSV to Pre-Stenotic PSV • 2: 1 ratio = > 50% diameter reduction • 4: 1 ratio = > 75% diameter reduction • >400 cm/sec PSV = > 75% diameter reduction • Never accept the value of numbers alone; post -stenotic turbulence should be present • Observe for occlusions and aneurysms
• Pre-stenotic Doppler spectra demonstrates a waveform that is – Monophasic – Dampened • Doppler spectra obtained AT the stenosis – Documents the highest PSVs • Post-Stenotic Doppler spectra demonstrates a waveform that shows turbulence (Usually distal to a > 50% stenosis
Interpretation: Bypass Grafts A. Normal: – Lower resistance flow patterns may normally be expected. – Some retrograde flow in the native artery may be evident at the distal anastomosis of a Reversed Saphenous Vein Graft (RSVG), which provides an additional source of collateral flow. (Retrograde flow results from a pressure gradient)
B. Abnormal Findings Compare results with previous studies and observe for changes such as: • Decrease of 30 cm/sec in any graft segment • Reduced PSVs in smallest graft diameter that were greater previously • Change from Triphasic to biphasic signals • Decrease in ABI of >. 15 • Observe for post-complications such as: AV fistula (can siphon off graft flow); valve cusp • Can also apply previous data used for native artery stenosis
C. Synthetic Grafts Can loosely apply the previous data to determine whether a > 50% diameter reduction exists. Anastomotic sites should be evaluated well for aneurysm and or stenosis Observe for graft occlusion
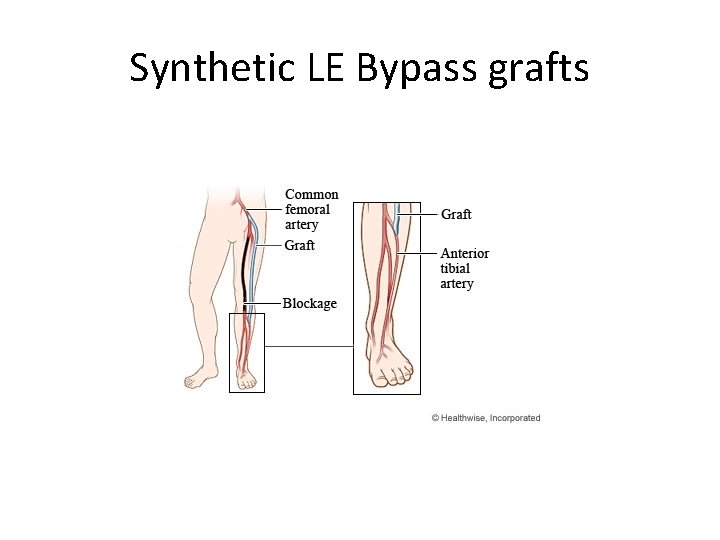
Synthetic LE Bypass grafts
Post Endovascular Intervention • In general, normal stented arteries may have elevated peak systolic velocities • Greatly elevated peak systolic velocities are abnormal and suggest a hemodynamically significant diameter reduction
Intraoperative monitoring • Used for checking patency of anastomotic sites • Evaluate any suspicious stenotic or turbulent areas that can occur in vein bypass grafts (e. g. , valve cusp sites or suspected branch sites) • Use highest frequency imaging transducer available
Additional Notes Lecture 12 Duplex / Color flow imaging (LE) • Calculating for velocity is the only thing that we do not know. • Calculation is based on your angle. • Doppler angle of greater than 60 degrees is not good
Bypass grafts • For In-situ Vein Graft, will use as an artery • All braches must be ligated. • Now arterial. • For synthetic bypass graft • Looking at prox and distal ends.
Pay close attention to the ratios 2: 1 4: 1 difference is bad. Telling the story • Systole: Proximal issues • Diastole: distal issues. • Blood flows because of a pressure gradient. High to low pressure.
Interpretation of bypass grafts Normal splash of blue color in systole (reversal) is normal due to mixed pressure gradient. If Velocity 1 (study one) showed a peak systolic Velocity PSV of. 89 and the second study shows a PSV of 5. 56, then this is a greater than 4: 1 ratio, which is bad. AV fistula: two things are connected that normally would not be.
Homework • Chapter 13: – Pages 127 -138 • SDMS assignments
