Uncommon Disorders Affecting the Carotid Arteries Lana Schumacher

- Slides: 35
Uncommon Disorders Affecting the Carotid Arteries Lana Schumacher, M. D. Surgery Resident 5/22/06
Uncommon Carotid Disorders • • • Carotid Kinks and Coils Carotid Body Tumors Carotid Sinus Syndrome Carotid Dissection Vasculitis Moyamoya
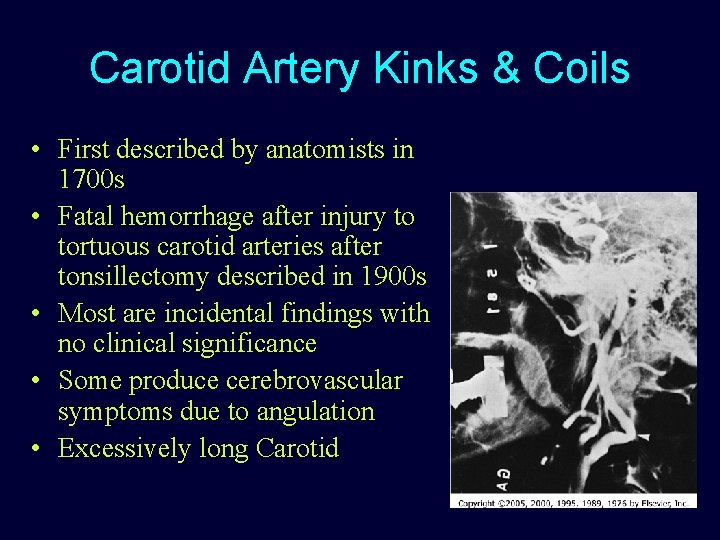
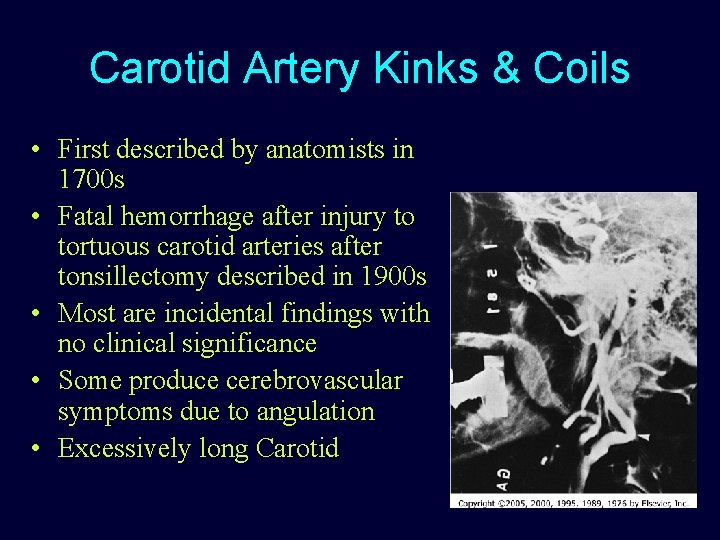
Carotid Artery Kinks & Coils • First described by anatomists in 1700 s • Fatal hemorrhage after injury to tortuous carotid arteries after tonsillectomy described in 1900 s • Most are incidental findings with no clinical significance • Some produce cerebrovascular symptoms due to angulation • Excessively long Carotid
Carotid Artery Kinks & Coils • Congenital (usually bilateral ~50%) – Faulty descent of heart and great vessels – Excessive lengthening of carotid as cervical spine elongates • Aquired (usually unilateral) – Carotid elongates with age – Elderly with atherosclerosis, thinning of media, fragmenting of elastic lamina, plaques that fix vessel – Fascial band • ICA is usually affected – S shape, single, double complete loops have all been described – Acute angle/kinks often are associated with plaque or stenosis • Kinks - Women: Men - 4: 1 • Incidence?
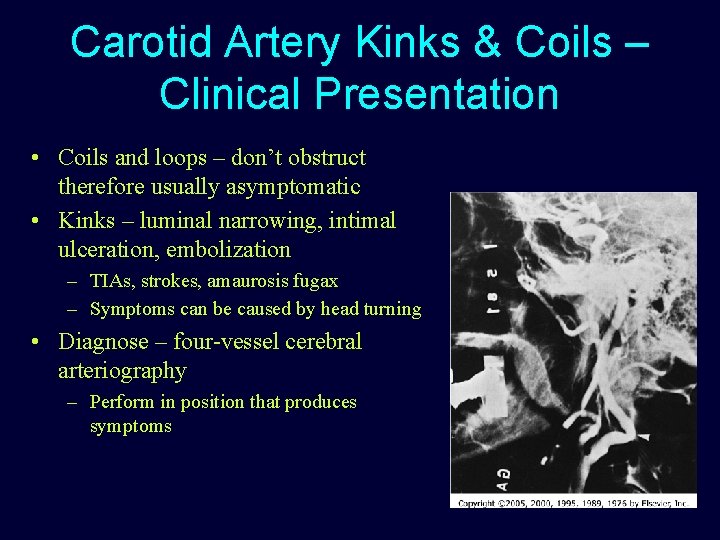
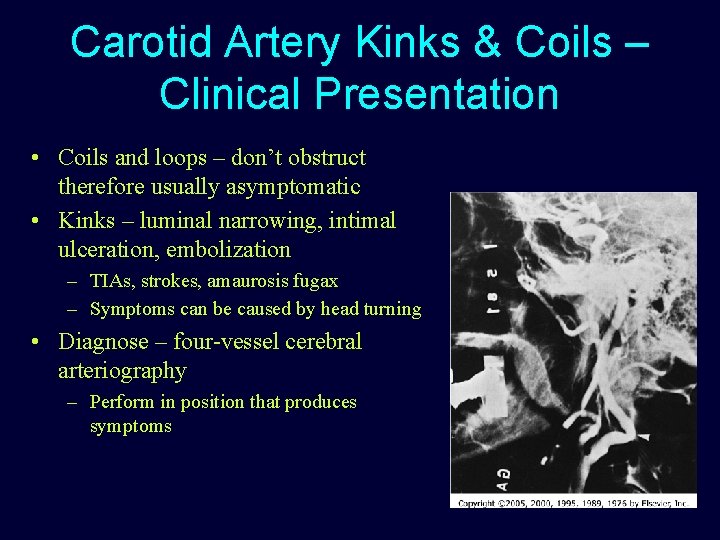
Carotid Artery Kinks & Coils – Clinical Presentation • Coils and loops – don’t obstruct therefore usually asymptomatic • Kinks – luminal narrowing, intimal ulceration, embolization – TIAs, strokes, amaurosis fugax – Symptoms can be caused by head turning • Diagnose – four-vessel cerebral arteriography – Perform in position that produces symptoms
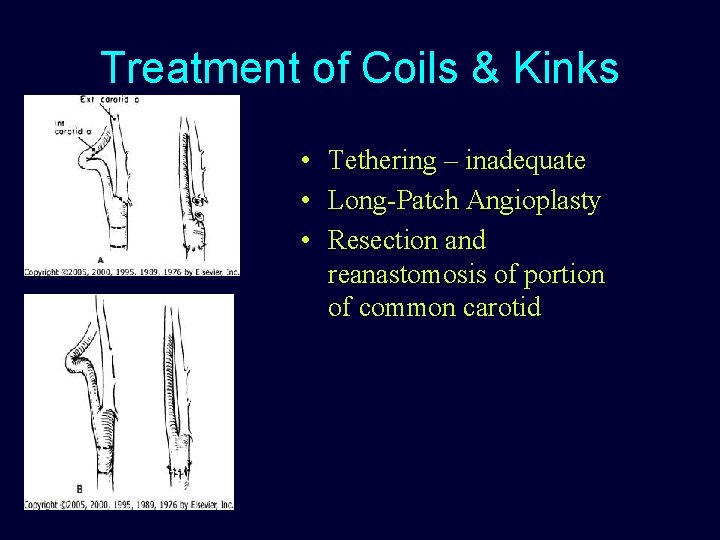
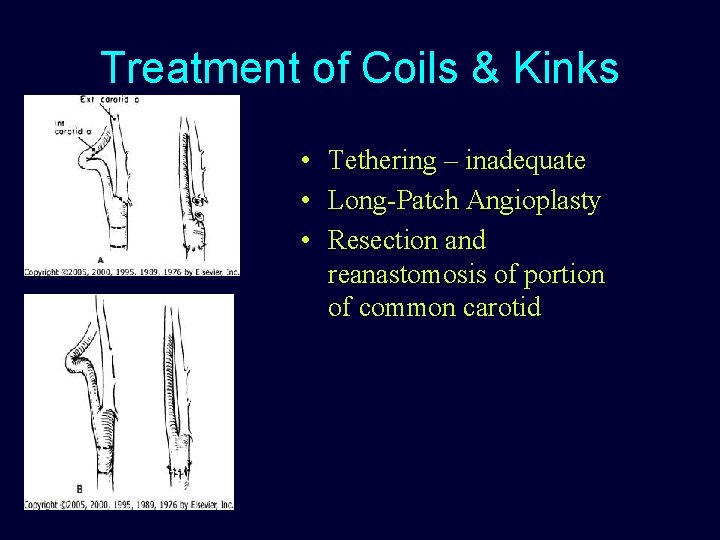
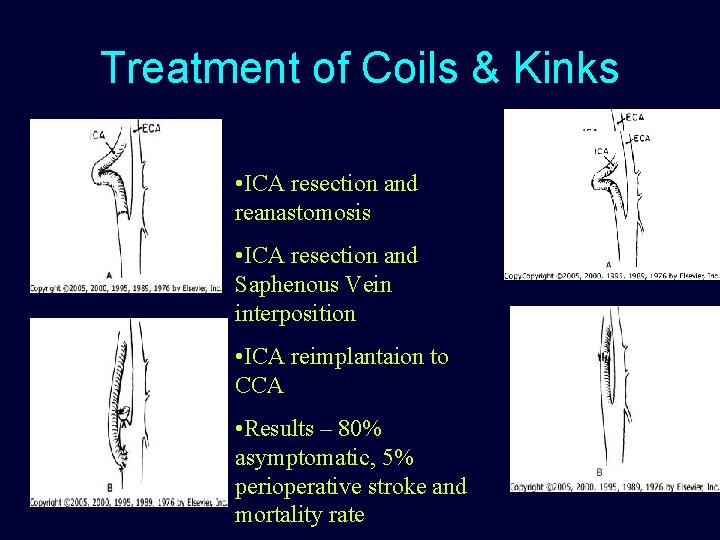
Treatment of Coils & Kinks • Tethering – inadequate • Long-Patch Angioplasty • Resection and reanastomosis of portion of common carotid
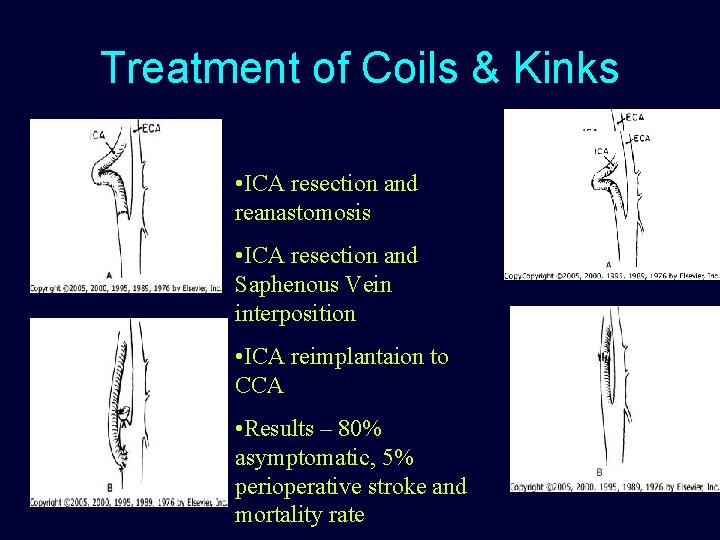
Treatment of Coils & Kinks • ICA resection and reanastomosis • ICA resection and Saphenous Vein interposition • ICA reimplantaion to CCA • Results – 80% asymptomatic, 5% perioperative stroke and mortality rate
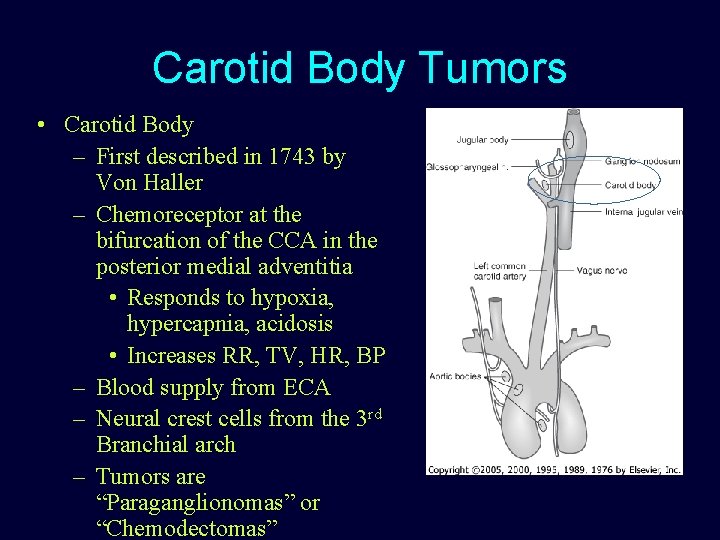
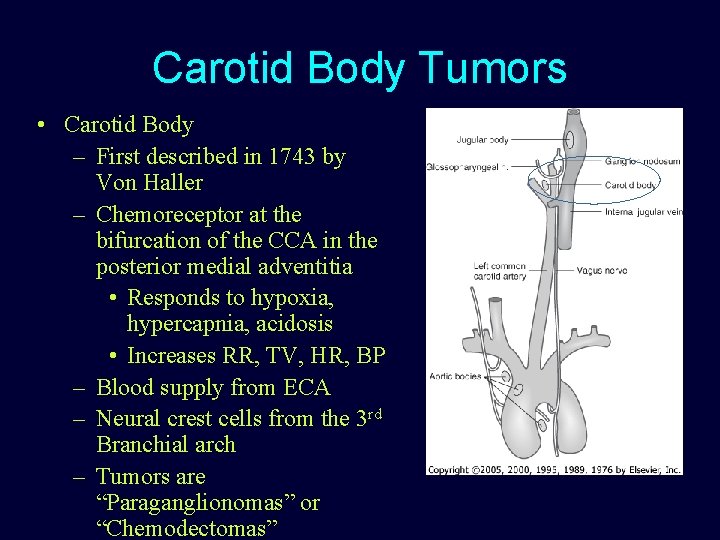
Carotid Body Tumors • Carotid Body – First described in 1743 by Von Haller – Chemoreceptor at the bifurcation of the CCA in the posterior medial adventitia • Responds to hypoxia, hypercapnia, acidosis • Increases RR, TV, HR, BP – Blood supply from ECA – Neural crest cells from the 3 rd Branchial arch – Tumors are “Paraganglionomas” or “Chemodectomas”
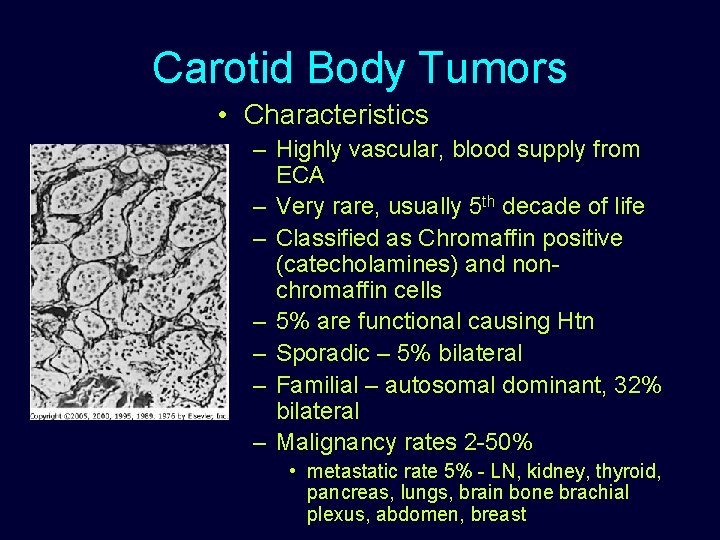
Carotid Body Tumors • Characteristics – Highly vascular, blood supply from ECA – Very rare, usually 5 th decade of life – Classified as Chromaffin positive (catecholamines) and nonchromaffin cells – 5% are functional causing Htn – Sporadic – 5% bilateral – Familial – autosomal dominant, 32% bilateral – Malignancy rates 2 -50% • metastatic rate 5% - LN, kidney, thyroid, pancreas, lungs, brain bone brachial plexus, abdomen, breast
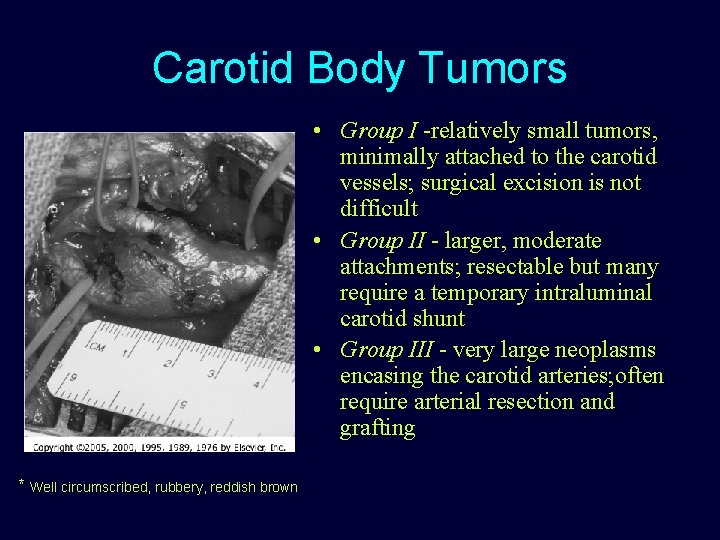
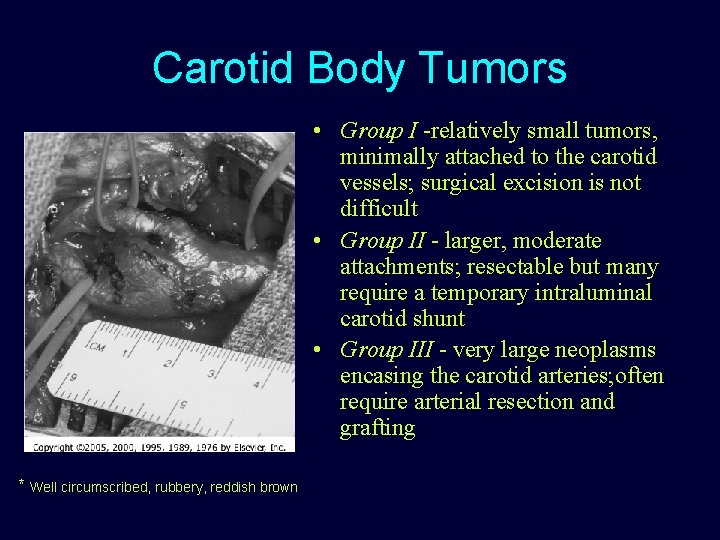
Carotid Body Tumors • Group I -relatively small tumors, minimally attached to the carotid vessels; surgical excision is not difficult • Group II - larger, moderate attachments; resectable but many require a temporary intraluminal carotid shunt • Group III - very large neoplasms encasing the carotid arteries; often require arterial resection and grafting * Well circumscribed, rubbery, reddish brown

Clinical presentation and diagnosis • Most common presentation - Painless swelling in neck at angle of mandible • Neck or ear pain, local tenderness, hoarse, dysphasia, tinnitus • If functional – symptoms of dizziness, flushing, palpitations, tachycardia, arrhythmias, headache, diaphoresis, photophobia • Bruit if tumor is impinging the artery • Diagnosis – • Duplex scan – highly vascular mass at bifurcation • Angiography – gold standard • CTA, MRA – size and extent of tumor • Avoid FNA – massive hemorrhage, pseudoaneurysm, carotid thrombosis
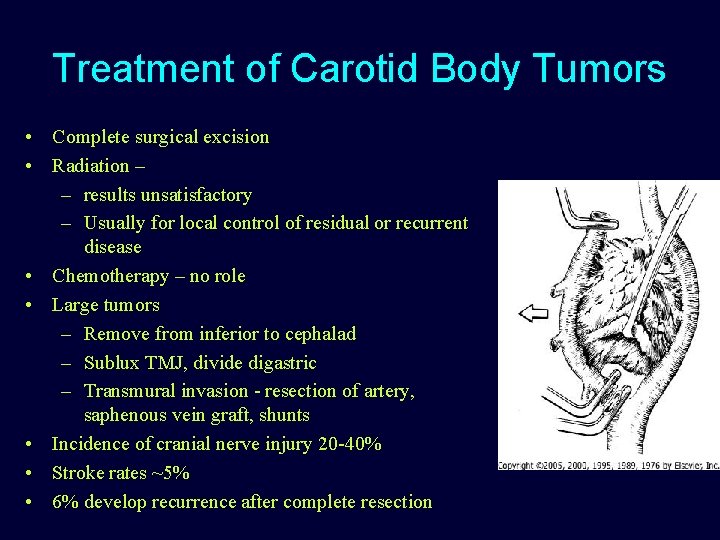
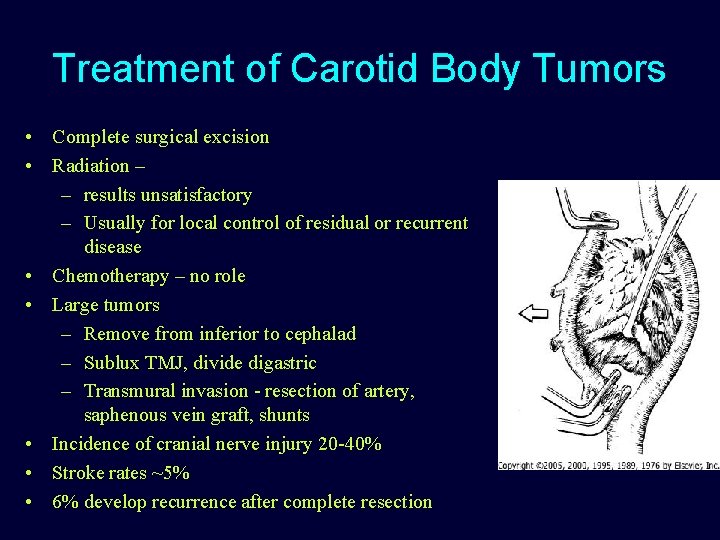
Treatment of Carotid Body Tumors • Complete surgical excision • Radiation – – results unsatisfactory – Usually for local control of residual or recurrent disease • Chemotherapy – no role • Large tumors – Remove from inferior to cephalad – Sublux TMJ, divide digastric – Transmural invasion - resection of artery, saphenous vein graft, shunts • Incidence of cranial nerve injury 20 -40% • Stroke rates ~5% • 6% develop recurrence after complete resection
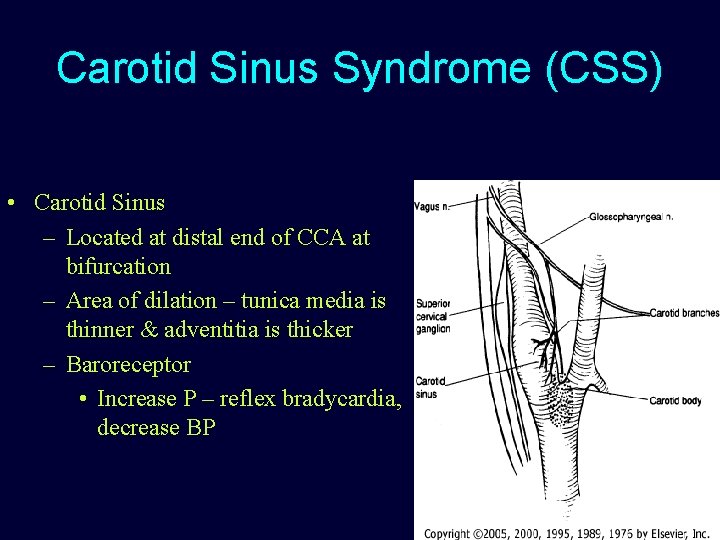
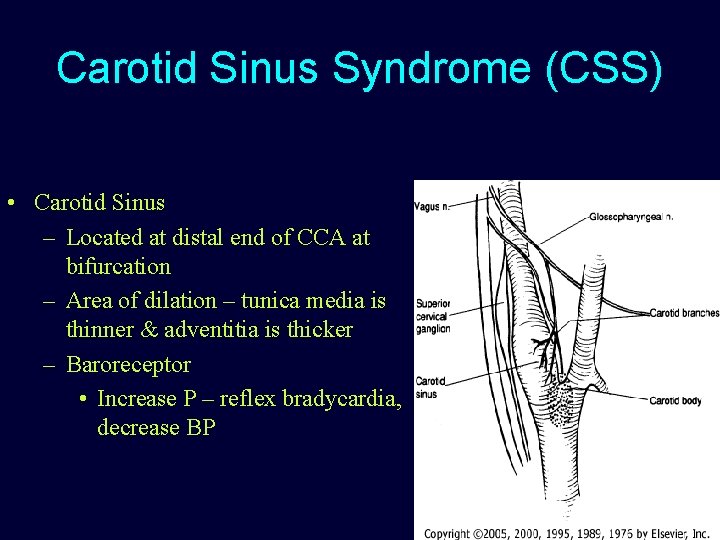
Carotid Sinus Syndrome (CSS) • Carotid Sinus – Located at distal end of CCA at bifurcation – Area of dilation – tunica media is thinner & adventitia is thicker – Baroreceptor • Increase P – reflex bradycardia, decrease BP
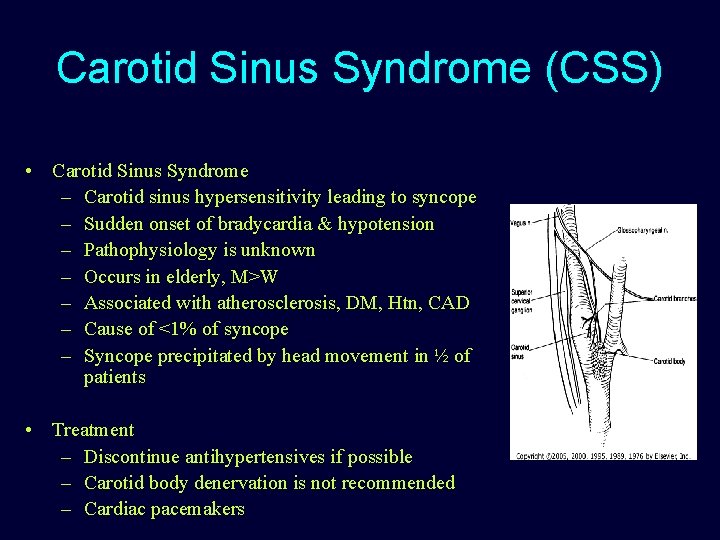
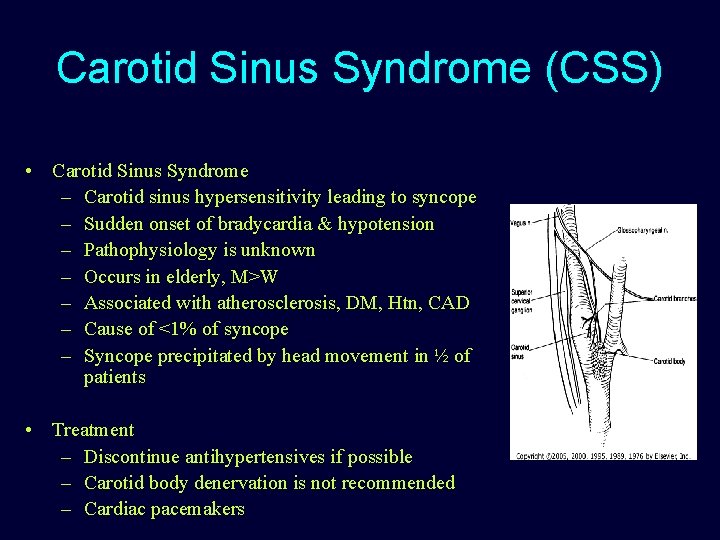
Carotid Sinus Syndrome (CSS) • Carotid Sinus Syndrome – Carotid sinus hypersensitivity leading to syncope – Sudden onset of bradycardia & hypotension – Pathophysiology is unknown – Occurs in elderly, M>W – Associated with atherosclerosis, DM, Htn, CAD – Cause of <1% of syncope – Syncope precipitated by head movement in ½ of patients • Treatment – Discontinue antihypertensives if possible – Carotid body denervation is not recommended – Cardiac pacemakers
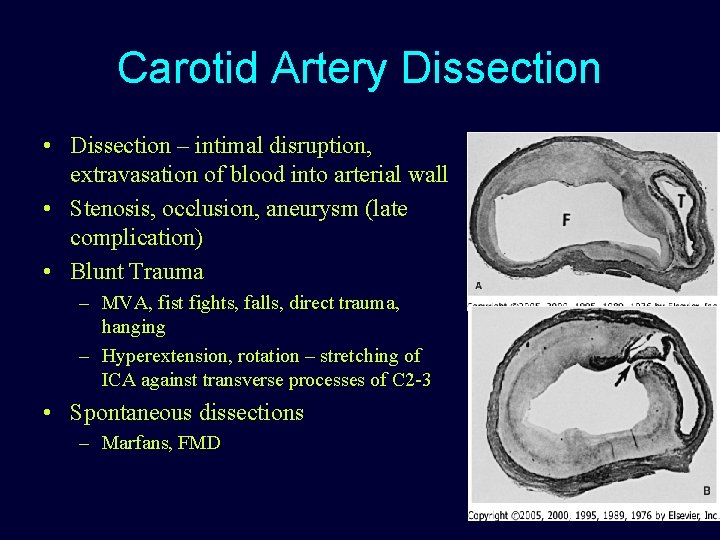
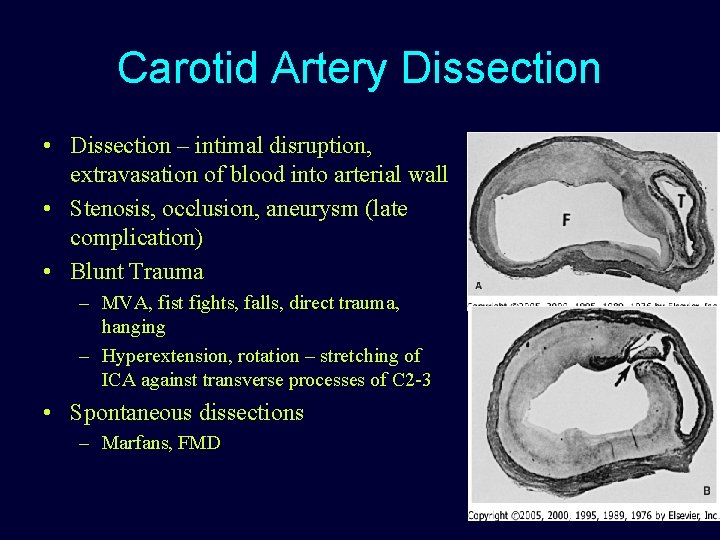
Carotid Artery Dissection • Dissection – intimal disruption, extravasation of blood into arterial wall • Stenosis, occlusion, aneurysm (late complication) • Blunt Trauma – MVA, fist fights, falls, direct trauma, hanging – Hyperextension, rotation – stretching of ICA against transverse processes of C 2 -3 • Spontaneous dissections – Marfans, FMD
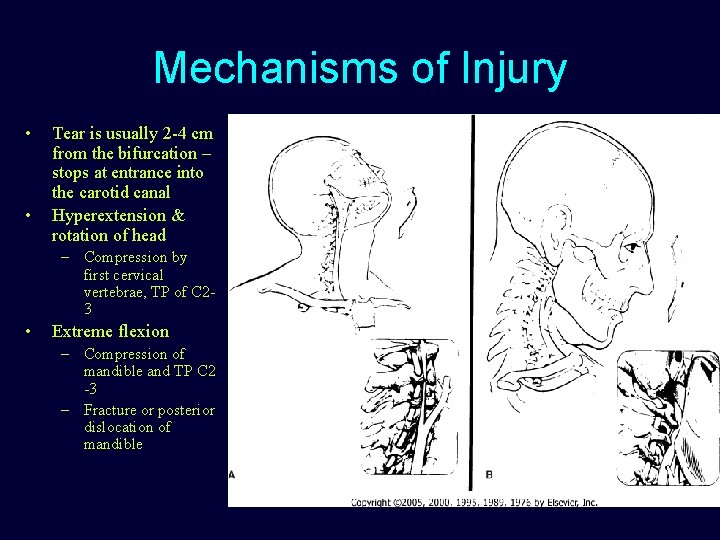
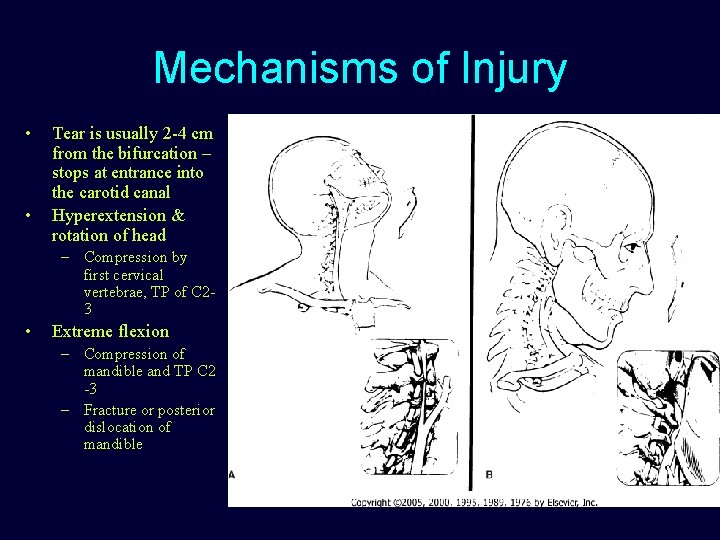
Mechanisms of Injury • • Tear is usually 2 -4 cm from the bifurcation – stops at entrance into the carotid canal Hyperextension & rotation of head – Compression by first cervical vertebrae, TP of C 23 • Extreme flexion – Compression of mandible and TP C 2 -3 – Fracture or posterior dislocation of mandible
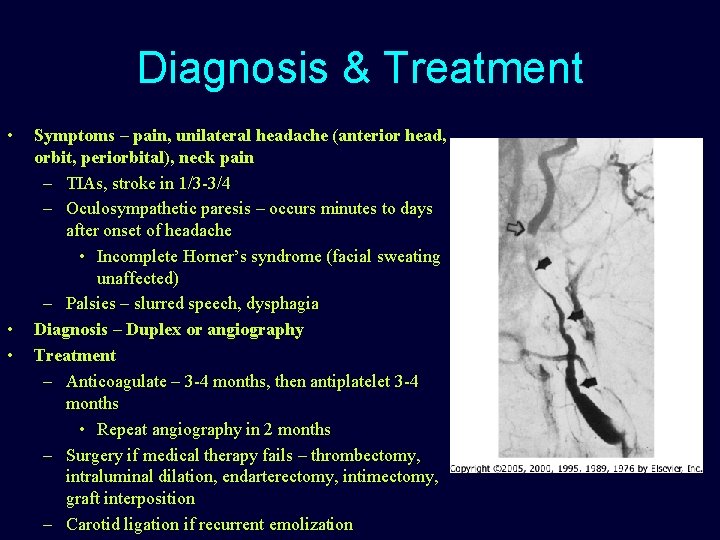
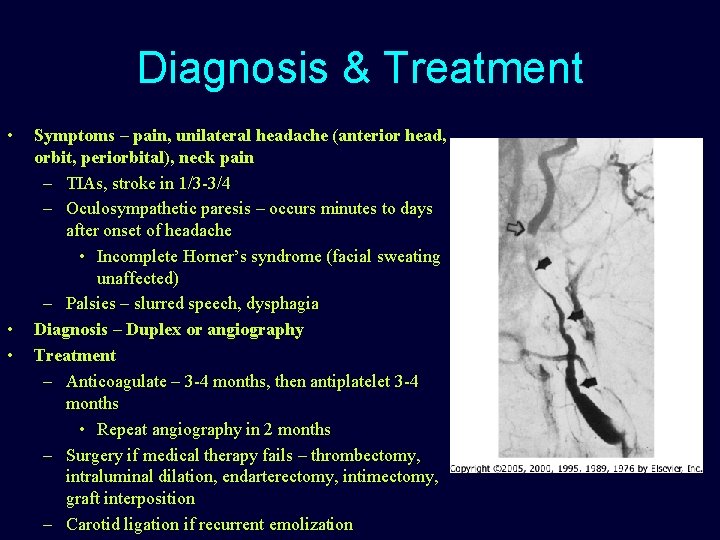
Diagnosis & Treatment • • • Symptoms – pain, unilateral headache (anterior head, orbit, periorbital), neck pain – TIAs, stroke in 1/3 -3/4 – Oculosympathetic paresis – occurs minutes to days after onset of headache • Incomplete Horner’s syndrome (facial sweating unaffected) – Palsies – slurred speech, dysphagia Diagnosis – Duplex or angiography Treatment – Anticoagulate – 3 -4 months, then antiplatelet 3 -4 months • Repeat angiography in 2 months – Surgery if medical therapy fails – thrombectomy, intraluminal dilation, endarterectomy, intimectomy, graft interposition – Carotid ligation if recurrent emolization
Radiation-Induced Carotid Arteritis and Stenosis • Two patterns of disease 1. Luminal occlusion – 7 -24 years after radiation – Pathophysiology – plaque-like thickening of intima, fibrosis of media and adventitia – Can lead to accelerated athlerosclerosis 2. Arterial Disruption – Usually after primary resection of tumor followed by radiation – Associated with tissue infection/wound breakdown
Radiation-Induced Carotid Arteritis and Stenosis – When to Operate? • Transmural radiation damage – • Recommend bypass graft of diseased segments Late presentation – usually accelerated atherosclerosis – – Endarterectomy – technically more difficult due to periarterial fibrosis and strong adherence of plaque to vessel wall Sometimes segmental resection and reconstruction is required due to wall attenuation v Important to consider life expectancy, healing of irradiated tissue/infection
Radiation-Induced Carotid Arteritis and Stenosis – When to Operate? • Carotid artery rupture – Poor prognosis – Present with sentinel bleed then exsanguinating hemorrhage – Prompt surgical exploration, carotid ligation or EC-IC bypass
Vasculitis • Inflammatory process resulting in necrosis of structural elements of vessel wall • Obliteration of lumen leads to ischemia • Variable course and variable presentation • No definitive lab tests or clinical signs • Primary or secondary due to underslying disease • Women usually > men 2: 1 • Vasculitis cannot be excluded based on negative angiogram
Giant Cell Arteritis • • Affects medium and large arteries Elderly women Usually presents as temporal arteritis Can affect aortic arch and extracranial carotid arteries • findings include disruptions of elastic lamina and media, granulomatous degeneration • Lesions are short and segmental with normal artery between lesions
Temporal Arteritis • Involves branches of external carotid artery – especially superficial temporal arteries, posterior ciliary, ophtalmic arteries • Flu-like syndrome, low-grade fever, Headache, scalp tenderness, jaw claudication, visual changes (amaursosis fugax, diplopia, permanent visual loss) • ESR may be elevated • vessels can be tender to palpation, cordlike and difficult to compress • Sudden and complete visual loss in 62% – Loss of blood supply to ophthalmic artery – Can progress to blindness in less than 24 hrs
Temporal Arteritis • Diagnosis – 4 -7 cm biopsy – Biopsy contralateral artery if first biopsy is negative – (14% incidence of positive contralateral biopsies) • Treatment – – “medical emergency” – start steroids immediately – Prognosis is good if treated expeditiously and does not influence life expectancy
Takayasu’s Arteritis • “Pulseless Disease” • “Obliterative brachiocephalic Arteries” – Margagni (1761) • “autopsy findings in a 40 yo F with absent radial pulses, thickened proximal aorta, lower thoracic aortic stenosis, cardiac hyperthrophy and pulmonary edema – Takayasu (1908) • “young Japanese woman with progressive visual loss, vertigo, syncope, conjunctival injection, retinal arteriovenous anastomoses, alopecia” • Occurs in all races and age groups, women 2 nd-3 rd decades • Involves the aortic arch and great vessels • Cerebral ischemia is the most life-threatening complications – Can involve more distal aortic segments as well as pulmonary and coronary arteries
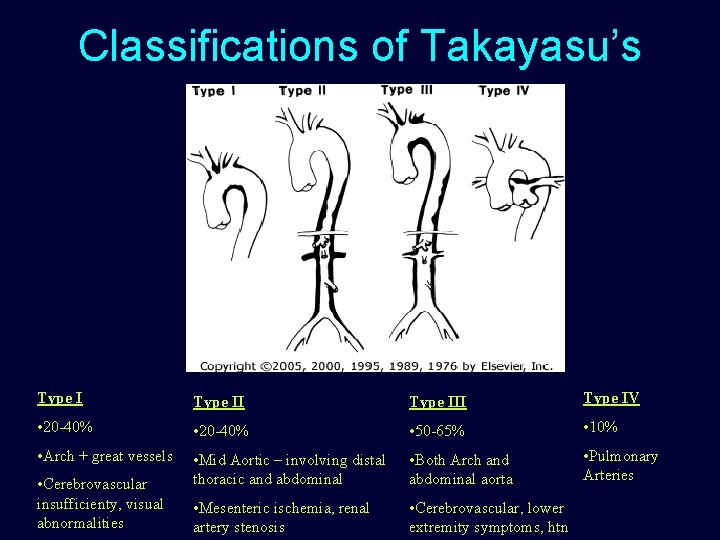
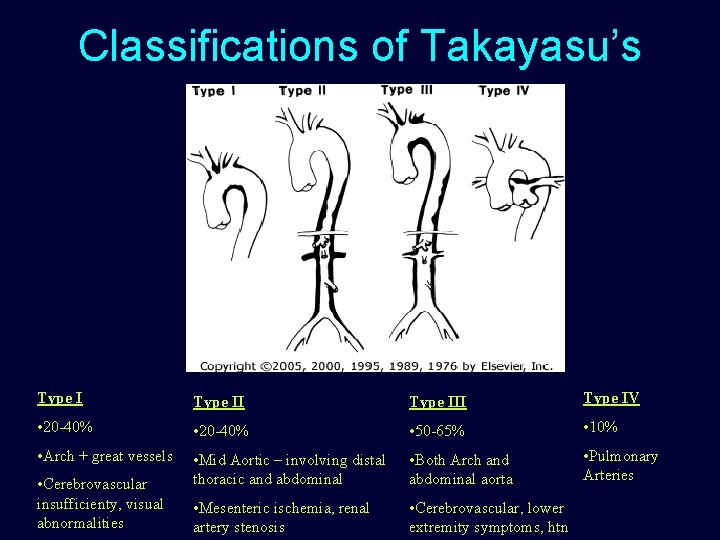
Classifications of Takayasu’s Type III Type IV • 20 -40% • 50 -65% • 10% • Arch + great vessels • Mid Aortic – involving distal thoracic and abdominal • Both Arch and abdominal aorta • Pulmonary Arteries • Mesenteric ischemia, renal artery stenosis • Cerebrovascular, lower extremity symptoms, htn • Cerebrovascular insufficienty, visual abnormalities
Clinical Presentation • Phase I – Prodrome of “malaise, anorexia, fatigue, weight loss, anemia, myalgias, fevers, night sweats” • Phase II – Inflammation of blood vessels – discomfort • Phase III – Symptoms of ischemia depending on location • TIAs, visual impairment – diplopia, amaurosis fugax, blurred vission, stroke, effort fatigue of upper extremities • Renovascular hypertension, mesenteric ischemia, lower extremity insufficiency • Pulmonary hypertension, dyspnea on exertion, pleuritic chest pain – Arterial stenosis, embolization, occlusion, aneurysm
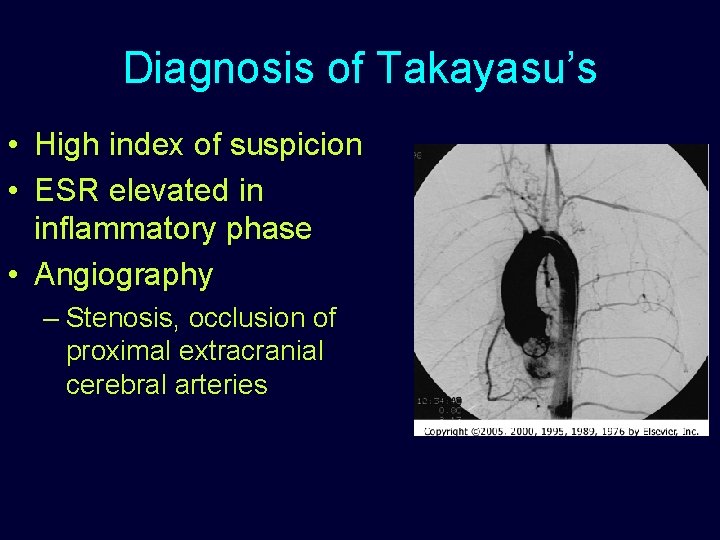
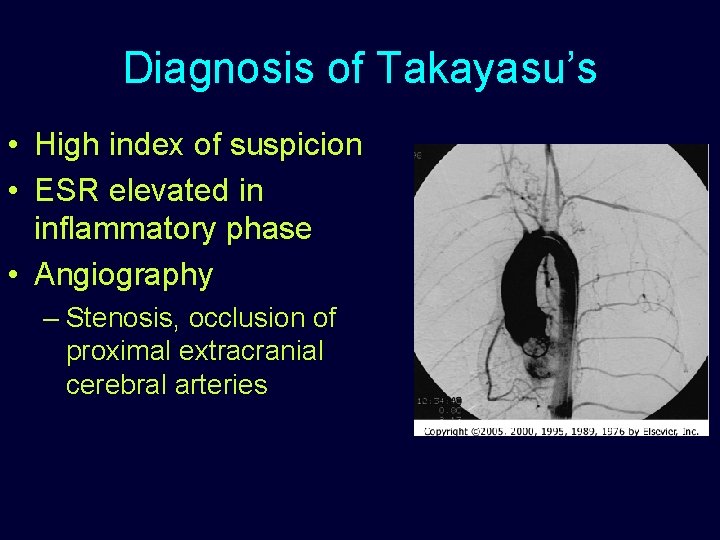
Diagnosis of Takayasu’s • High index of suspicion • ESR elevated in inflammatory phase • Angiography – Stenosis, occlusion of proximal extracranial cerebral arteries
Treatment of Takayasu’s • Course is unpredictable – Prognosis can be dependent on the presence of complications and severity of disease – Death usually due to CHF, stroke, MI, Renal failue – 5 year survival rate 55 -98% • Steroids and anti-inflammatories – high dose, then taper – may be on steroids for many years • Cyclophosphamide – if no response to steroid after 3 months • Long-term anticoagulation
Surgery for Takayasu’s • Surgery required in up to 1/3 of patients with chronic advanced Takayasu’s • Surgery should be delayed past active phase • Transmural disease with all layers – endarterectomy or patch angioplasty is not recommended – Interposition graft • Multiple operations are required • Close postoperative surveillance due to frequent development of anastomotic stenosis in first 1 -2 years
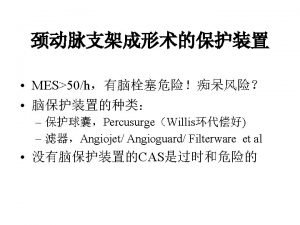
Moyamoya • Rare cerebrovacular disorder leading to progressive stenosis in the arteries of the circle of Willis • Ischemic strokes in children • Hemorrhages in adults • Described by Takeuchi & Shimizu in 1957 – “bilateral hypogenesis of the ICAs” – Moyamoya = “puff of smoke”
Moyamoya • Cause is unknown • Episode of infection/URI is frequently antecedent • Does not affect large vessels • Begins with carotid artery in cavernous sinus and progresses • Familial cases and higher incidence in Down Syndrome
Presentation of Moyamoya • Biphasic age – 1 st & 4 th decades • Female to male 1: 5 • Children – ischemic sx, TIAs, stroke – Induced by crying, coughing, straining, seizures – Mortality 4% • Adults – hemorrhage usually into ventricles, thalamus, basal ganglia – Worse prognosis - Mortality 10%
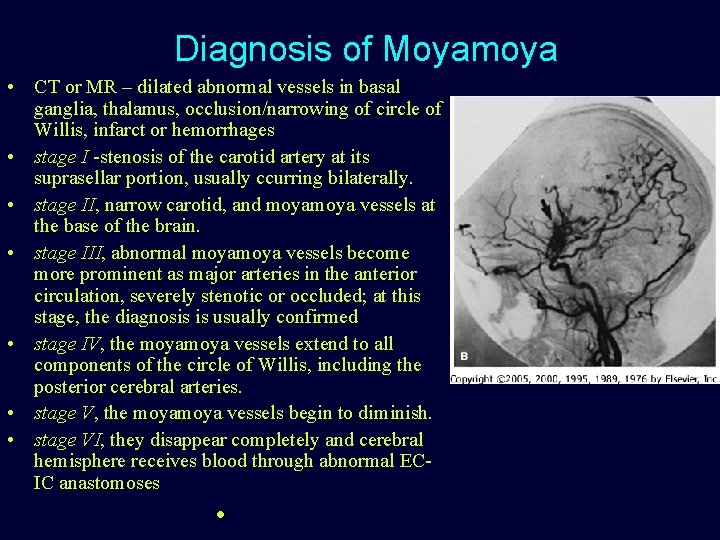
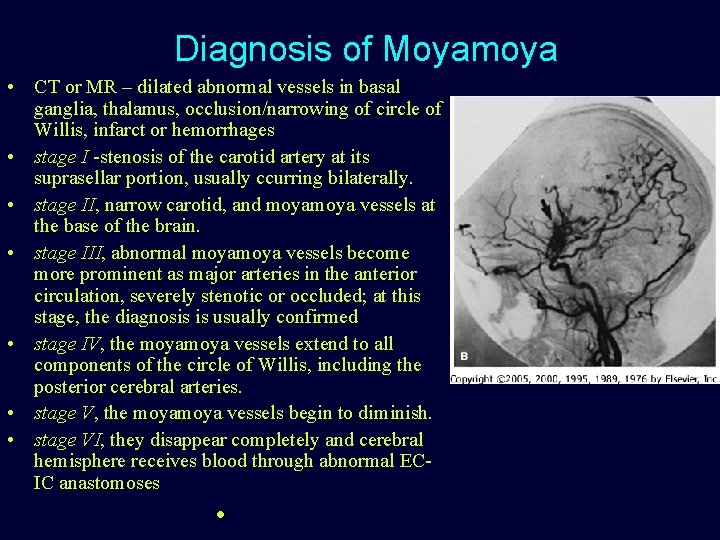
Diagnosis of Moyamoya • CT or MR – dilated abnormal vessels in basal ganglia, thalamus, occlusion/narrowing of circle of Willis, infarct or hemorrhages • stage I -stenosis of the carotid artery at its suprasellar portion, usually ccurring bilaterally. • stage II, narrow carotid, and moya vessels at the base of the brain. • stage III, abnormal moya vessels become more prominent as major arteries in the anterior circulation, severely stenotic or occluded; at this stage, the diagnosis is usually confirmed • stage IV, the moya vessels extend to all components of the circle of Willis, including the posterior cerebral arteries. • stage V, the moya vessels begin to diminish. • stage VI, they disappear completely and cerebral hemisphere receives blood through abnormal ECIC anastomoses •
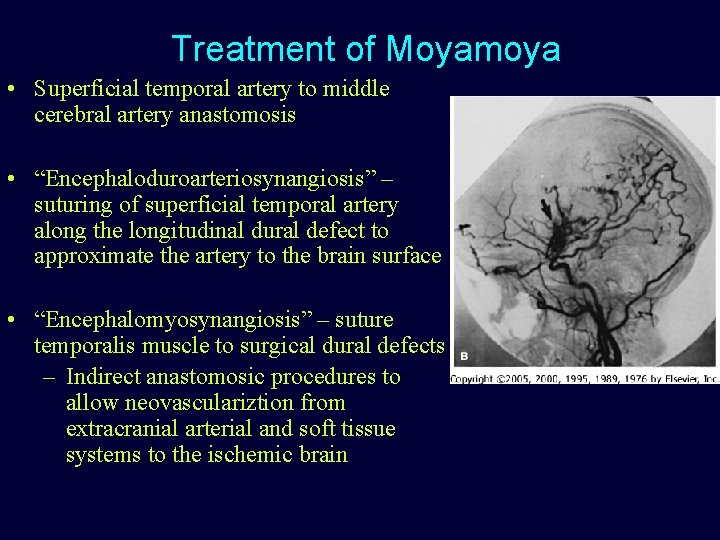
Treatment of Moyamoya • Superficial temporal artery to middle cerebral artery anastomosis • “Encephaloduroarteriosynangiosis” – suturing of superficial temporal artery along the longitudinal dural defect to approximate the artery to the brain surface • “Encephalomyosynangiosis” – suture temporalis muscle to surgical dural defects – Indirect anastomosic procedures to allow neovasculariztion from extracranial arterial and soft tissue systems to the ischemic brain
 Dr. lana schumacher
Dr. lana schumacher Definition of solubility product constant
Definition of solubility product constant The uncommon practice
The uncommon practice Uncommon logic digital
Uncommon logic digital Michael schumacher geburtsort
Michael schumacher geburtsort Benjamin schumacher
Benjamin schumacher Pacific puddle jump
Pacific puddle jump 10 examples of litotes
10 examples of litotes Anne schumacher
Anne schumacher Tyler schumacher
Tyler schumacher Jeroen schumacher
Jeroen schumacher Leon schumacher
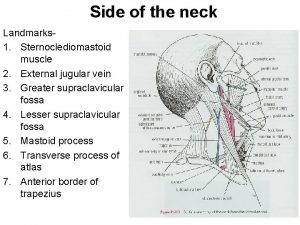
Leon schumacher Sternoclediomastoid
Sternoclediomastoid Lingual artery
Lingual artery Site:slidetodoc.com
Site:slidetodoc.com Cat dissection digestive system
Cat dissection digestive system Amourosis fugax
Amourosis fugax Pulse site and location
Pulse site and location Phrenic vein
Phrenic vein Pharynx
Pharynx Carotid triangle contents
Carotid triangle contents Duplex ultrasound vs doppler
Duplex ultrasound vs doppler Celiac trunk
Celiac trunk Brain
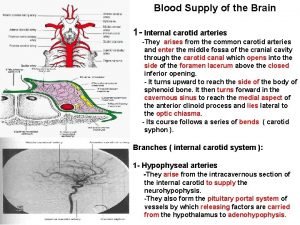
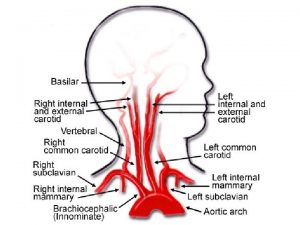
Brain Internal carotid artery branches
Internal carotid artery branches Vasovagal reaction
Vasovagal reaction Left subclavian vein
Left subclavian vein Organ of zuckerkandl
Organ of zuckerkandl Carotid cavernous fistula
Carotid cavernous fistula Glossopharyngeal nerve branches
Glossopharyngeal nerve branches Eca branches
Eca branches Carotid cochlear dehiscence
Carotid cochlear dehiscence Carotid sheath contents
Carotid sheath contents Infraorbital foramen
Infraorbital foramen Fascia parotidea
Fascia parotidea Carotid artery pulse
Carotid artery pulse