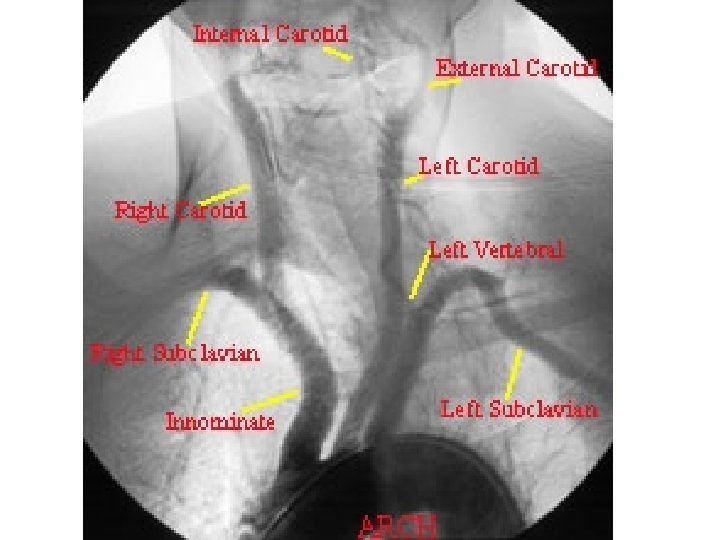
Towne Carotid Lateral Carotid 1 Internal Carotid 2







![MR venogram - sagittal view [rght image]; A = Lateral (transverse) sinus; B: Sigmoid MR venogram - sagittal view [rght image]; A = Lateral (transverse) sinus; B: Sigmoid](https://slidetodoc.com/presentation_image_h2/3d990da964354bbaa02d5eb54b25877b/image-13.jpg)















- Slides: 53

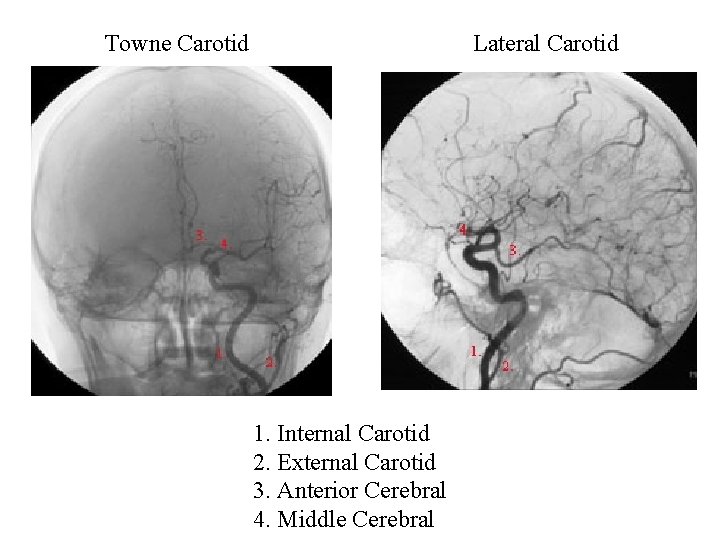
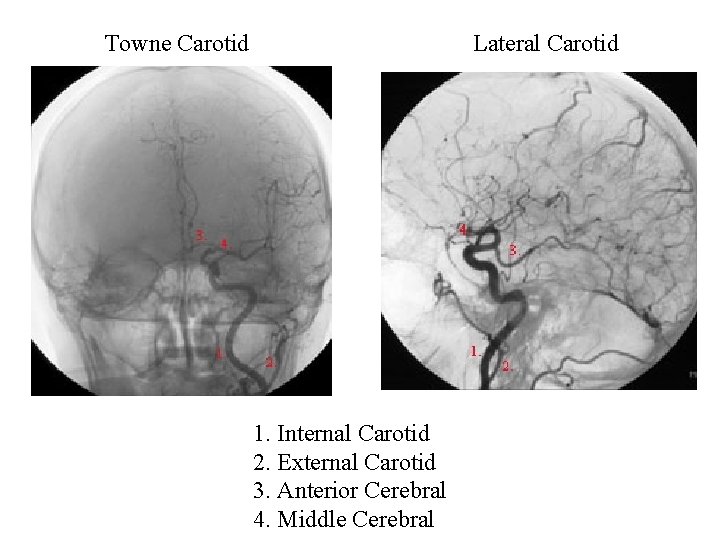
Towne Carotid Lateral Carotid 1. Internal Carotid 2. External Carotid 3. Anterior Cerebral 4. Middle Cerebral

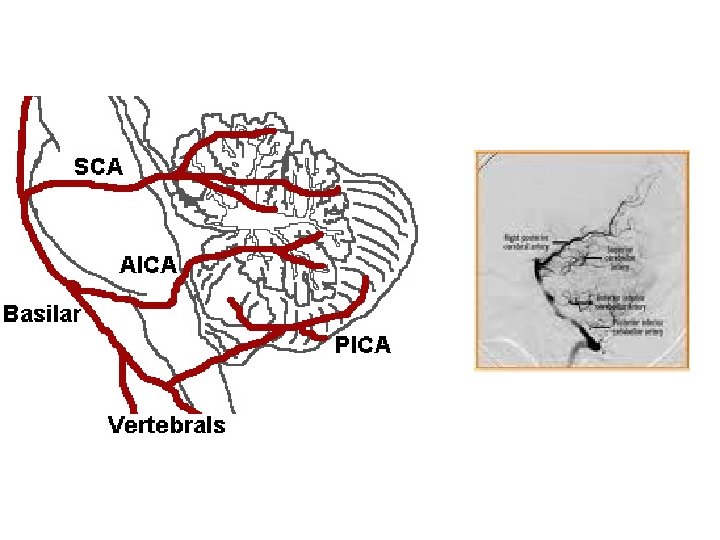
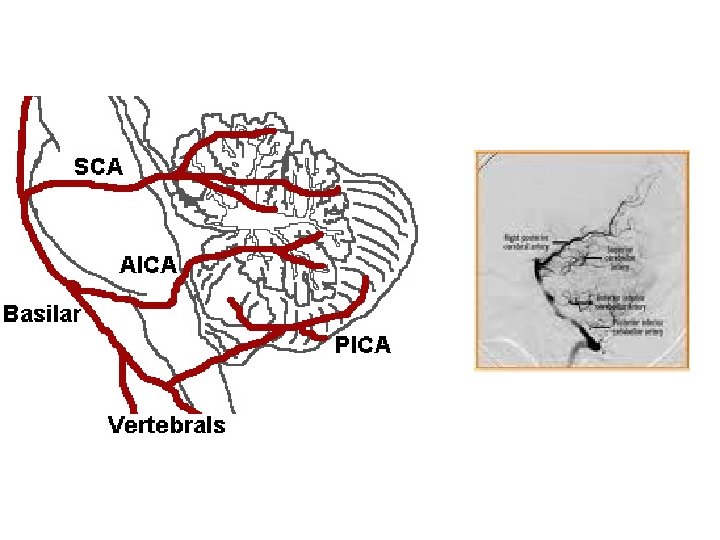
Towne Vertebral 1. Vertebral 2. Posterior Inferior Cerebellar 3. Anterior Inferior Cerebellar 4. Basilar 5. Posterior Cerebral Lateral Vertebral 1. Vertebral 2. Posterior Inferior Cerebellar 3. Basilar 4. Superior Cerebellar 5. Posterior Cerebral 6. Occipital 7. Posterior Temporal
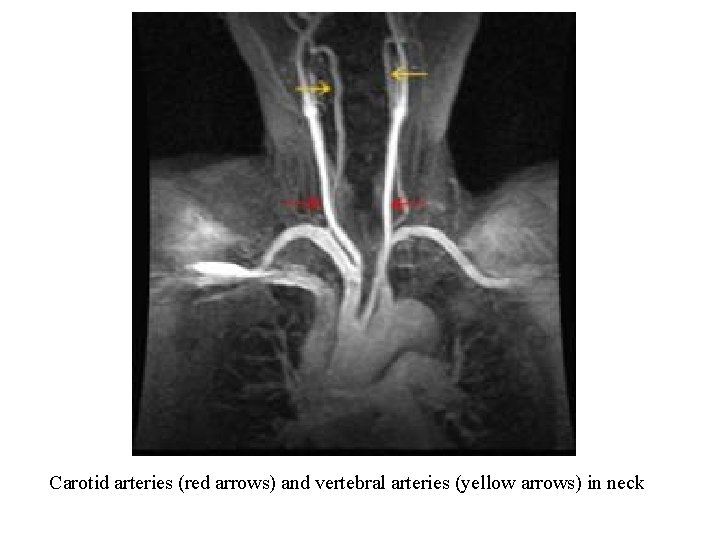
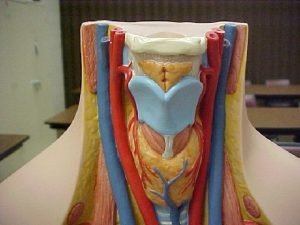
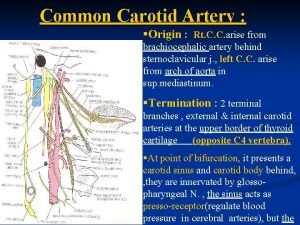
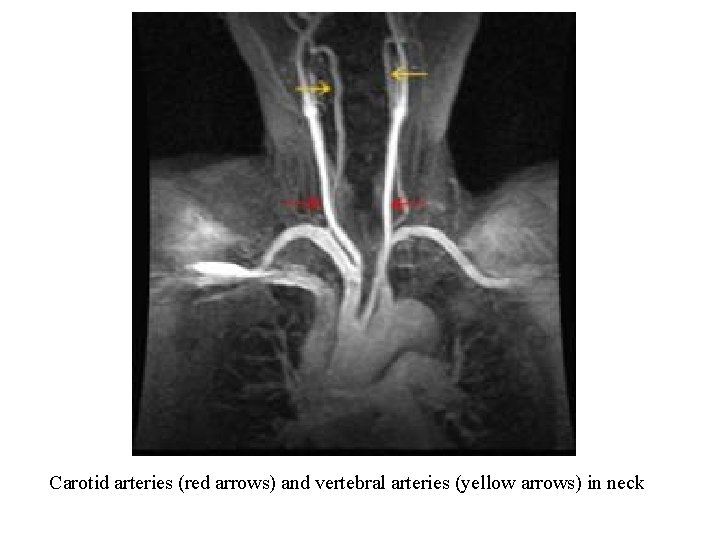
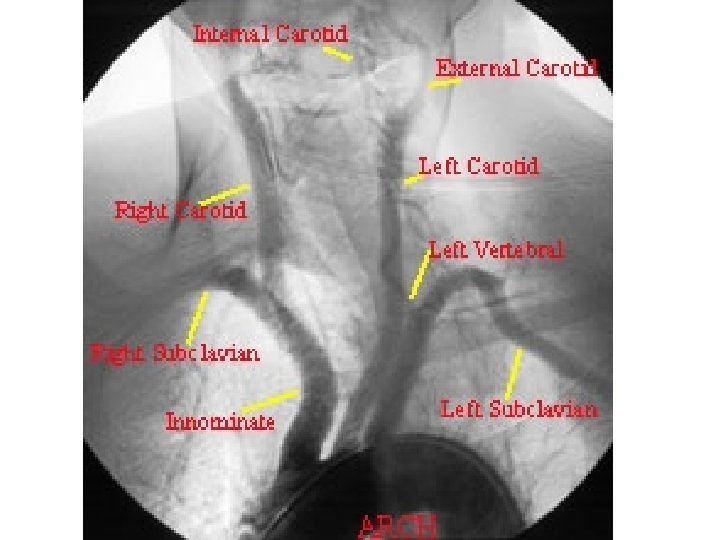
Carotid arteries (red arrows) and vertebral arteries (yellow arrows) in neck

Common (blue arrow), Internal (red arrow), and External (yellow arrow) branches of the Left Carotid Artery
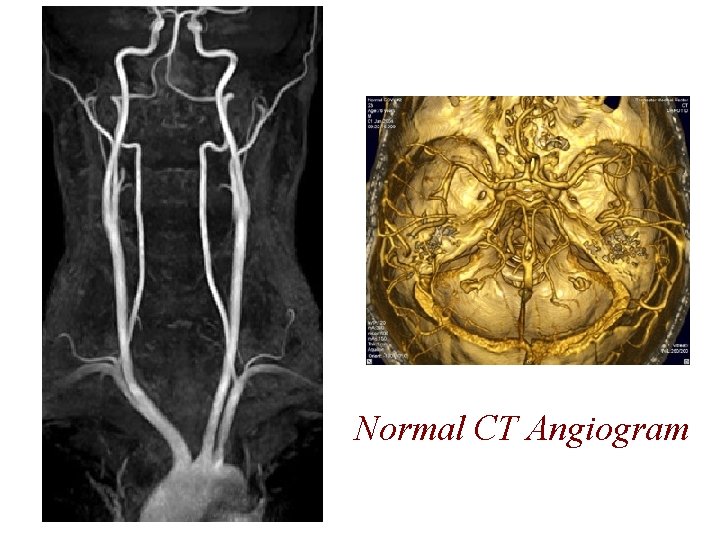
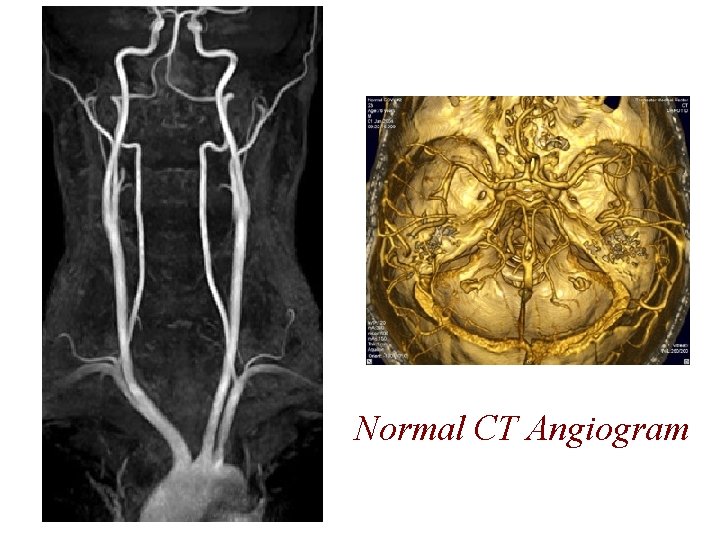
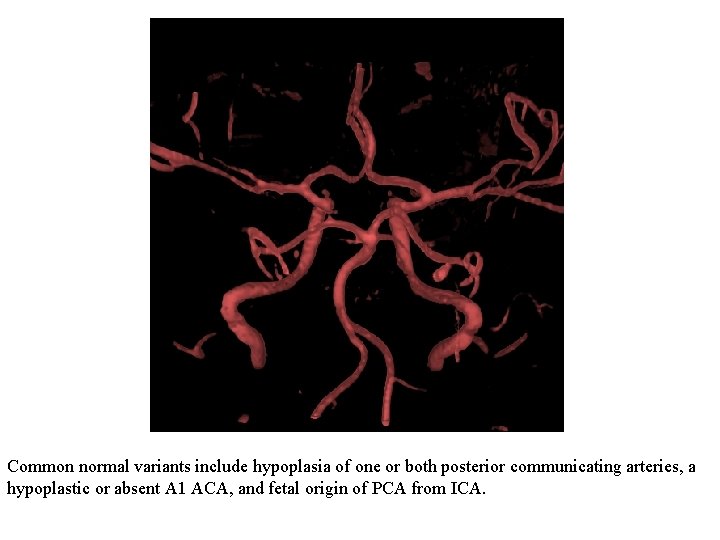
Normal CT Angiogram




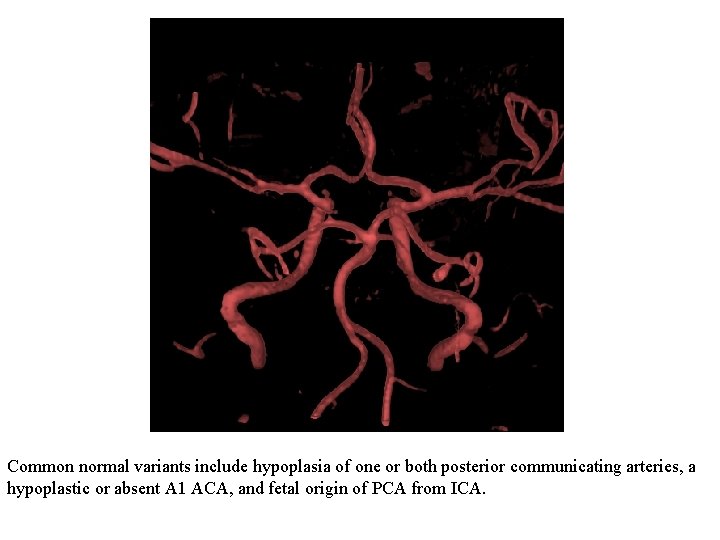
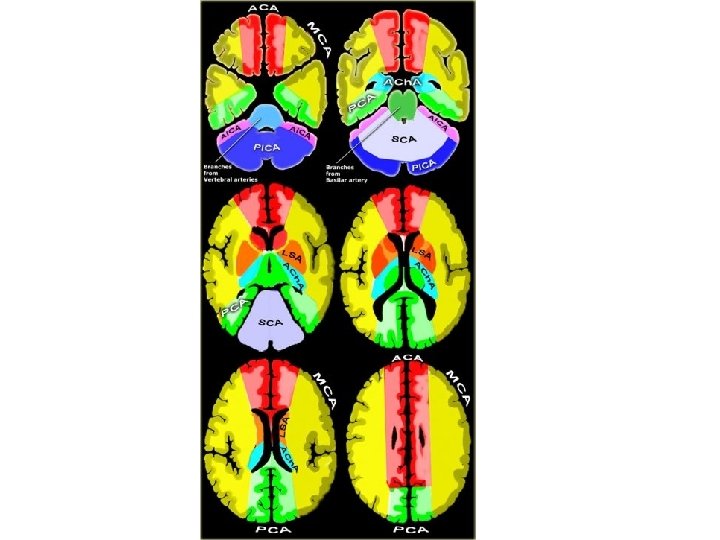
Common normal variants include hypoplasia of one or both posterior communicating arteries, a hypoplastic or absent A 1 ACA, and fetal origin of PCA from ICA.
![MR venogram sagittal view rght image A Lateral transverse sinus B Sigmoid MR venogram - sagittal view [rght image]; A = Lateral (transverse) sinus; B: Sigmoid](https://slidetodoc.com/presentation_image_h2/3d990da964354bbaa02d5eb54b25877b/image-13.jpg)
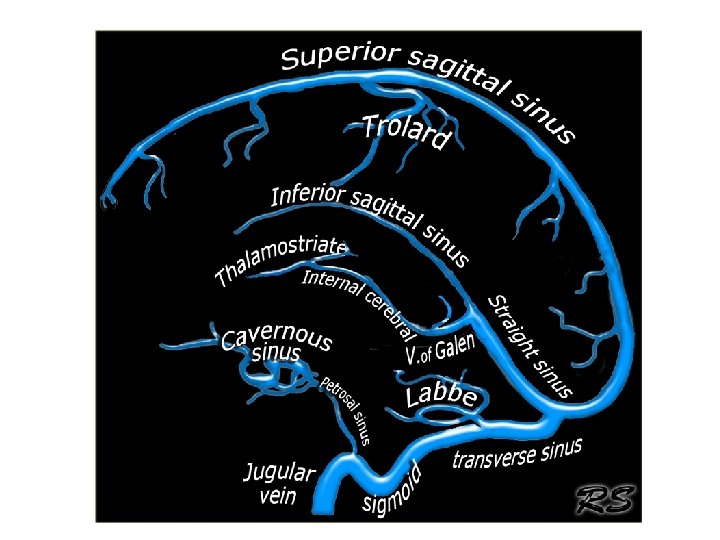
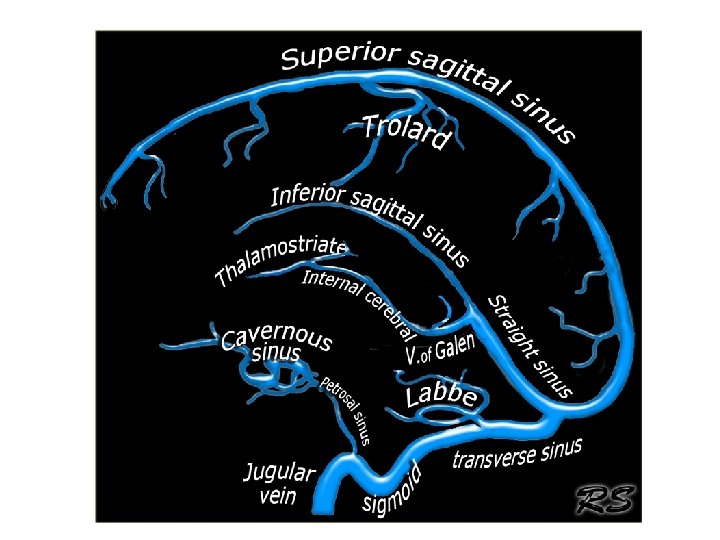
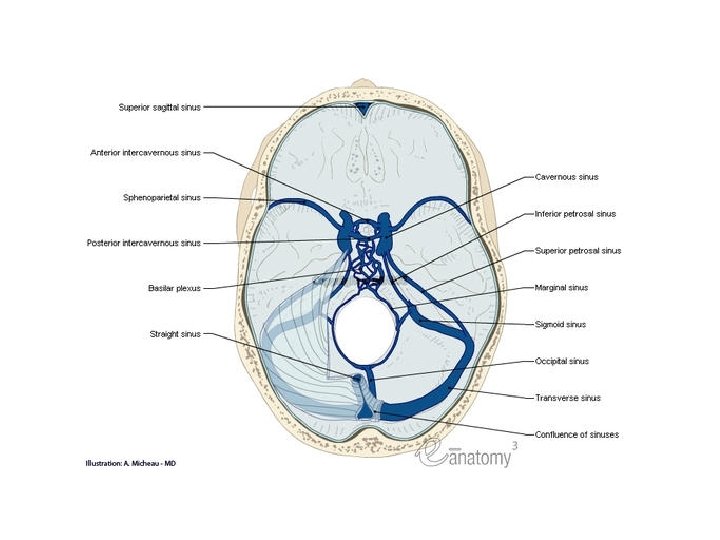
MR venogram - sagittal view [rght image]; A = Lateral (transverse) sinus; B: Sigmoid sinus C = Confluence of sinuses; D = Superior sagittal sinus; and E = Straight sinus.



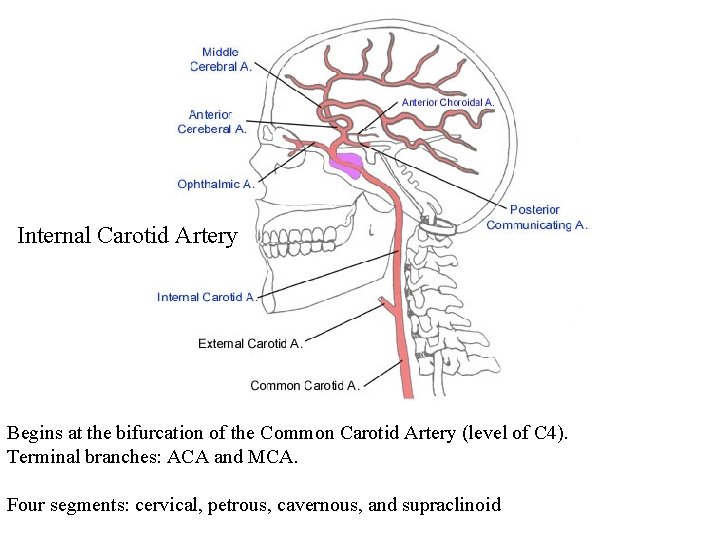
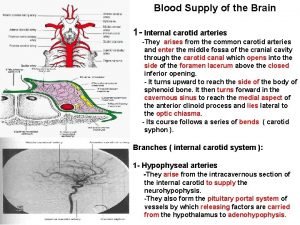
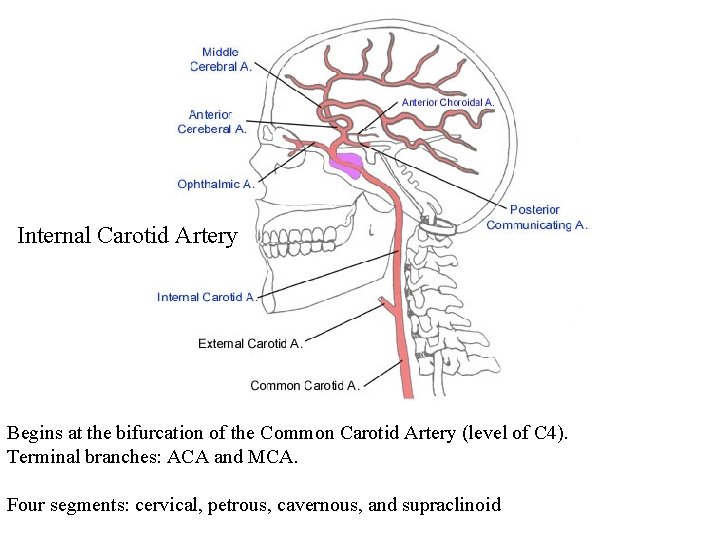
Internal Carotid Artery Begins at the bifurcation of the Common Carotid Artery (level of C 4). Terminal branches: ACA and MCA. Four segments: cervical, petrous, cavernous, and supraclinoid

Cervical Segment Petrous Segment Internal Carotid Artery Extends from base of skull to apex of petrous bone Enters cranial vault via foramen lacerum.
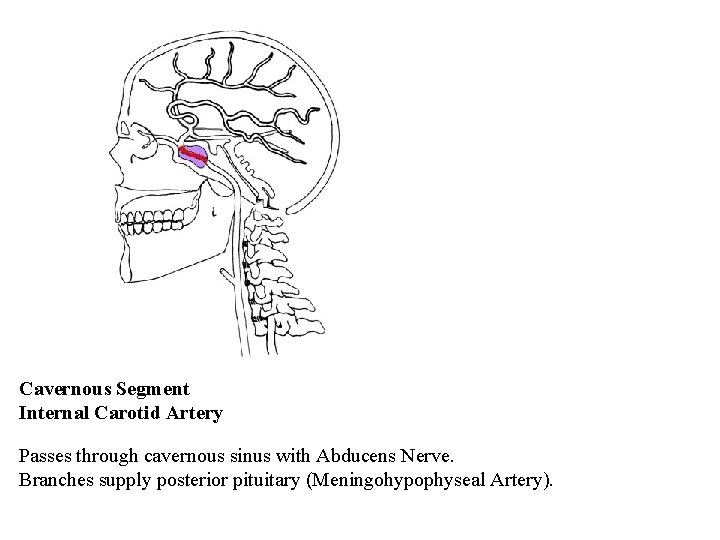
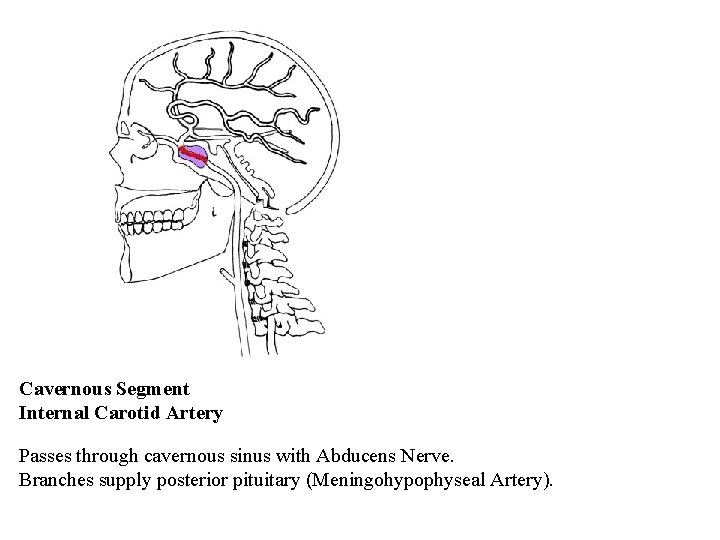
Cavernous Segment Internal Carotid Artery Passes through cavernous sinus with Abducens Nerve. Branches supply posterior pituitary (Meningohypophyseal Artery).
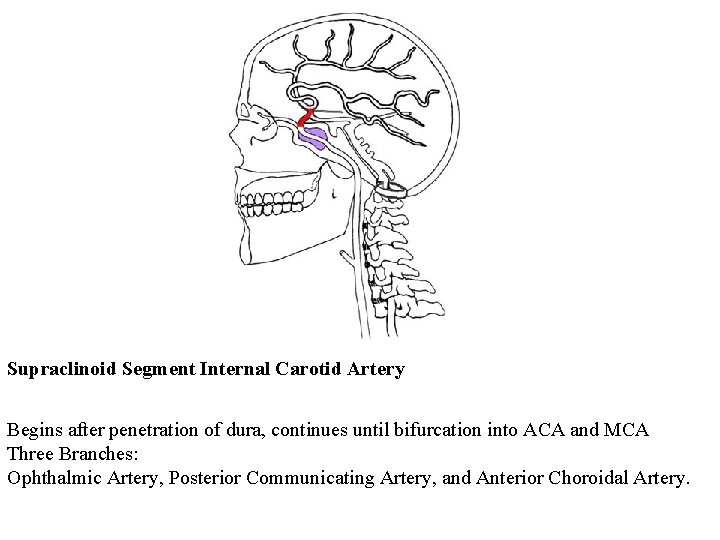
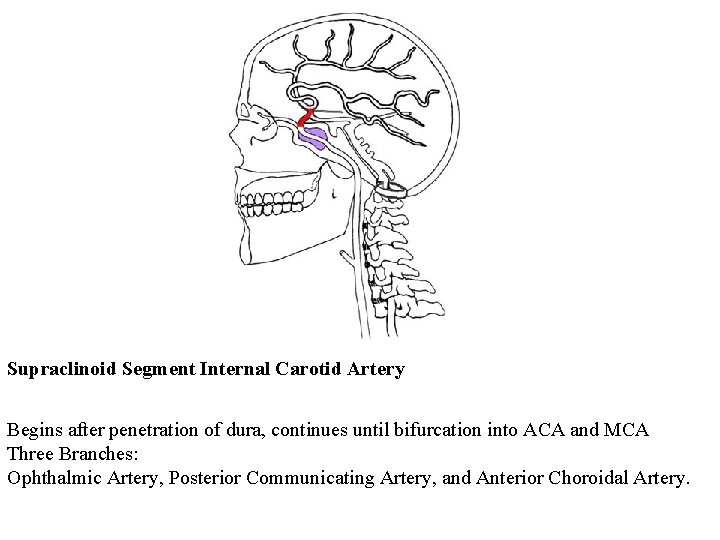
Supraclinoid Segment Internal Carotid Artery Begins after penetration of dura, continues until bifurcation into ACA and MCA Three Branches: Ophthalmic Artery, Posterior Communicating Artery, and Anterior Choroidal Artery.
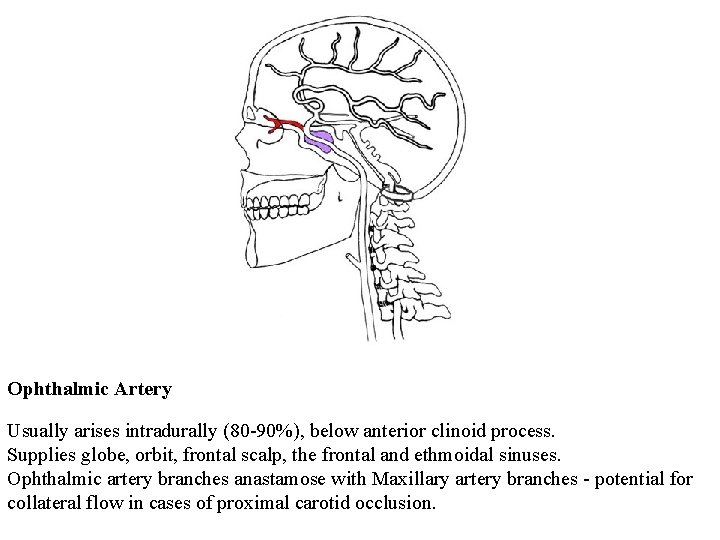
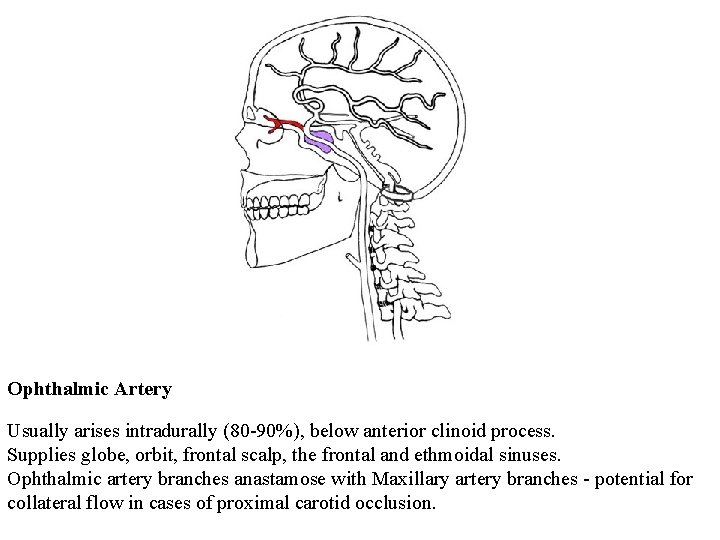
Ophthalmic Artery Usually arises intradurally (80 -90%), below anterior clinoid process. Supplies globe, orbit, frontal scalp, the frontal and ethmoidal sinuses. Ophthalmic artery branches anastamose with Maxillary artery branches - potential for collateral flow in cases of proximal carotid occlusion.
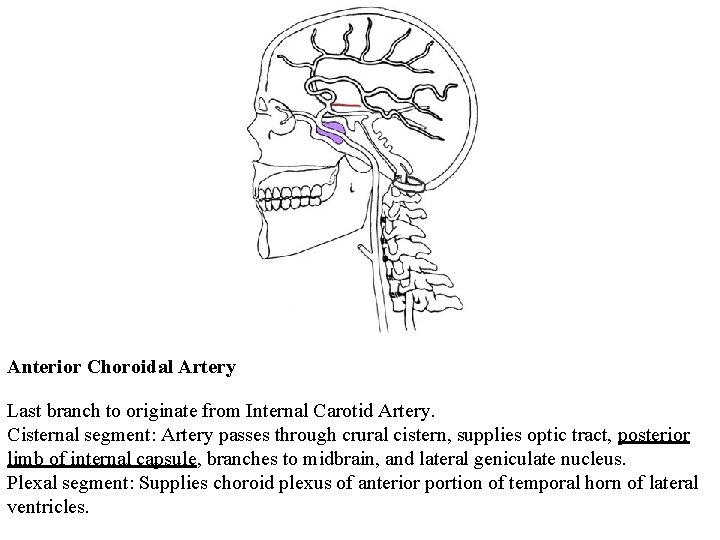
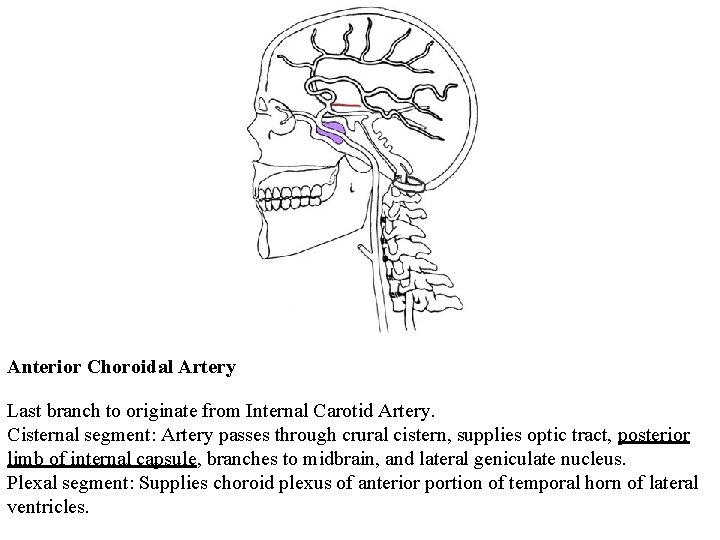
Anterior Choroidal Artery Last branch to originate from Internal Carotid Artery. Cisternal segment: Artery passes through crural cistern, supplies optic tract, posterior limb of internal capsule, branches to midbrain, and lateral geniculate nucleus. Plexal segment: Supplies choroid plexus of anterior portion of temporal horn of lateral ventricles.
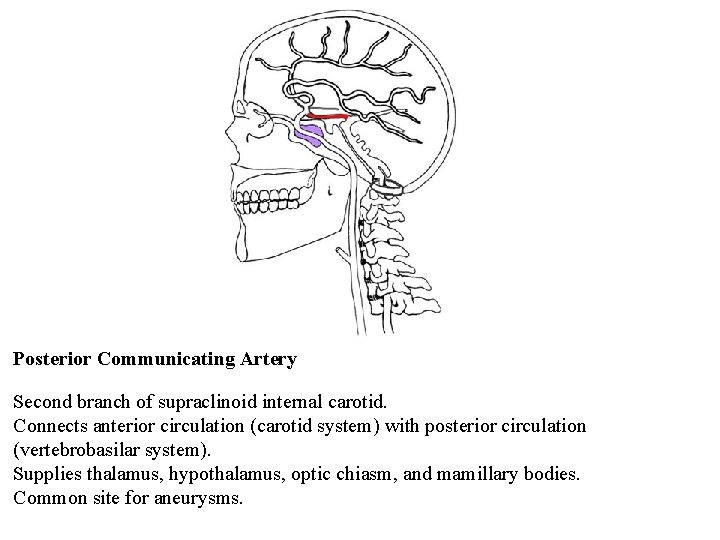
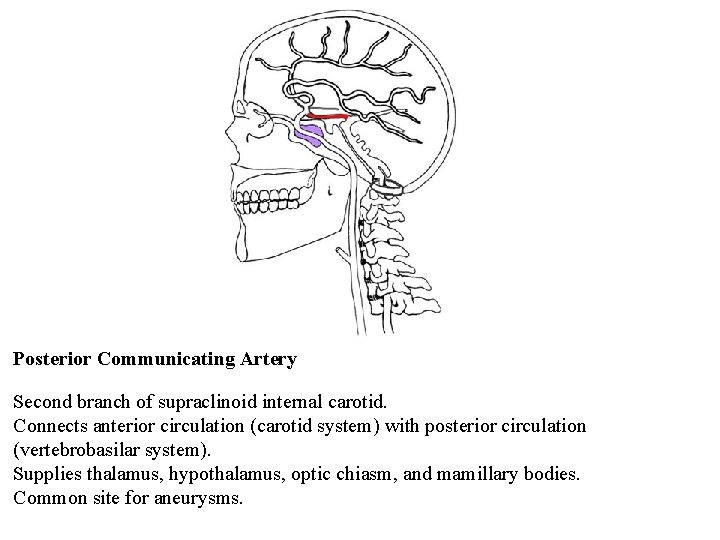
Posterior Communicating Artery Second branch of supraclinoid internal carotid. Connects anterior circulation (carotid system) with posterior circulation (vertebrobasilar system). Supplies thalamus, hypothalamus, optic chiasm, and mamillary bodies. Common site for aneurysms.
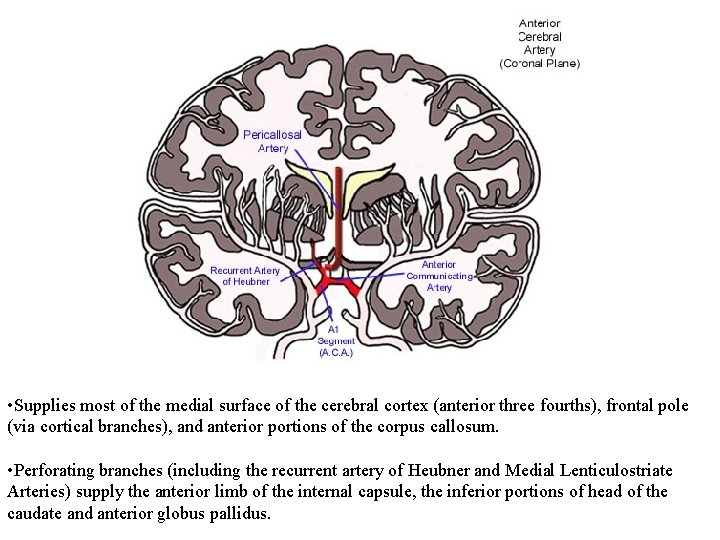
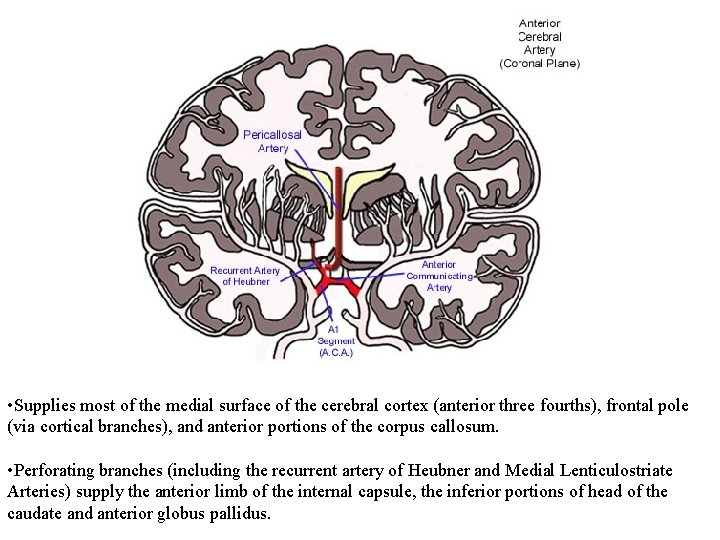
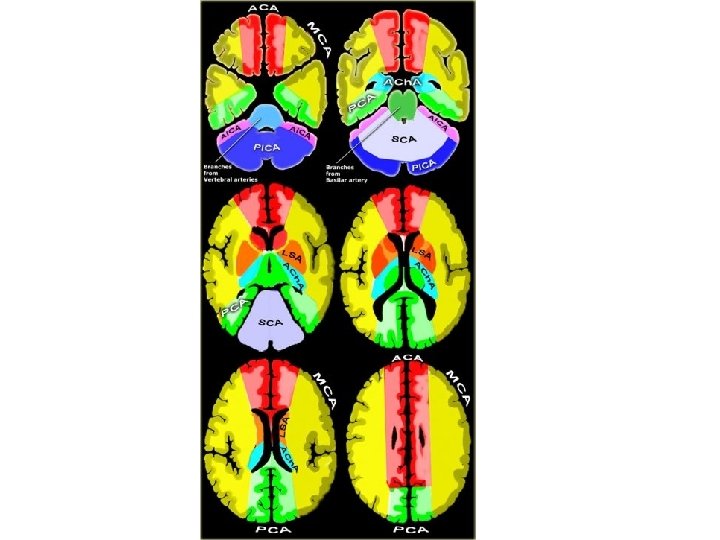
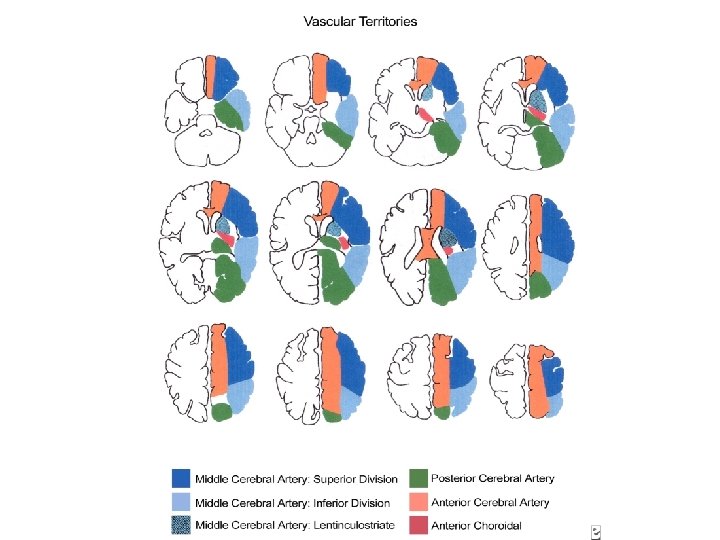
• Supplies most of the medial surface of the cerebral cortex (anterior three fourths), frontal pole (via cortical branches), and anterior portions of the corpus callosum. • Perforating branches (including the recurrent artery of Heubner and Medial Lenticulostriate Arteries) supply the anterior limb of the internal capsule, the inferior portions of head of the caudate and anterior globus pallidus.
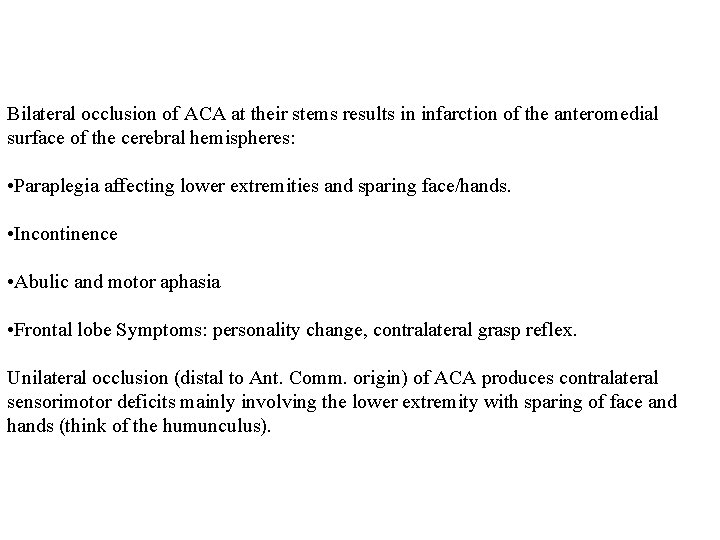
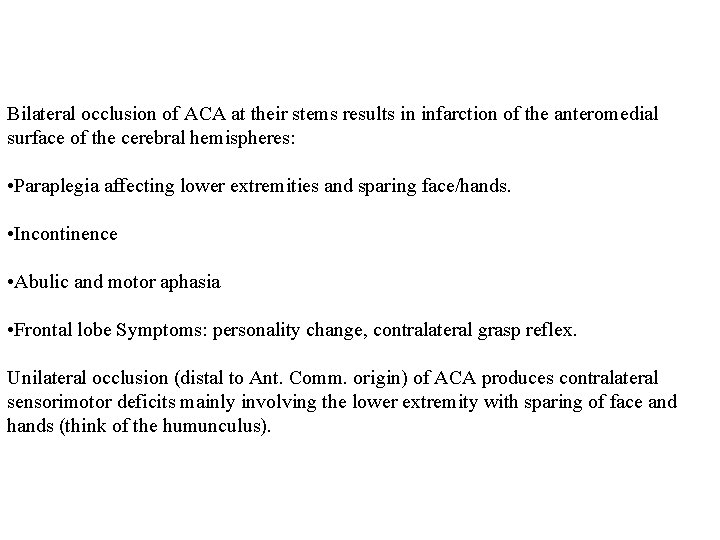
Bilateral occlusion of ACA at their stems results in infarction of the anteromedial surface of the cerebral hemispheres: • Paraplegia affecting lower extremities and sparing face/hands. • Incontinence • Abulic and motor aphasia • Frontal lobe Symptoms: personality change, contralateral grasp reflex. Unilateral occlusion (distal to Ant. Comm. origin) of ACA produces contralateral sensorimotor deficits mainly involving the lower extremity with sparing of face and hands (think of the humunculus).
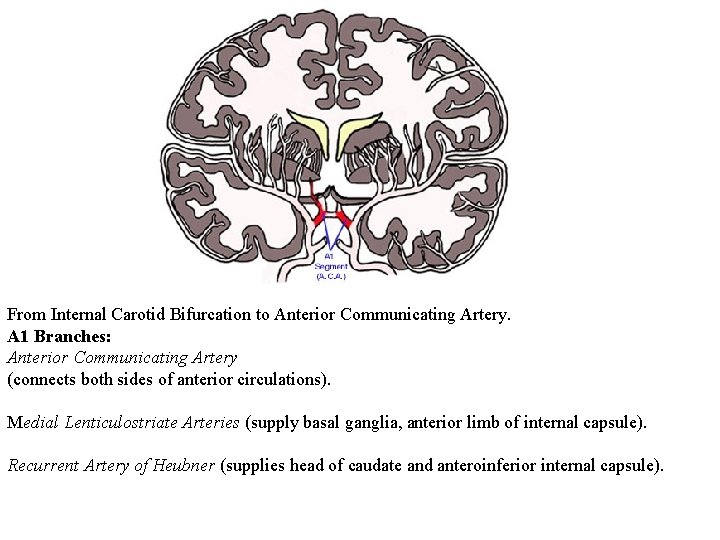
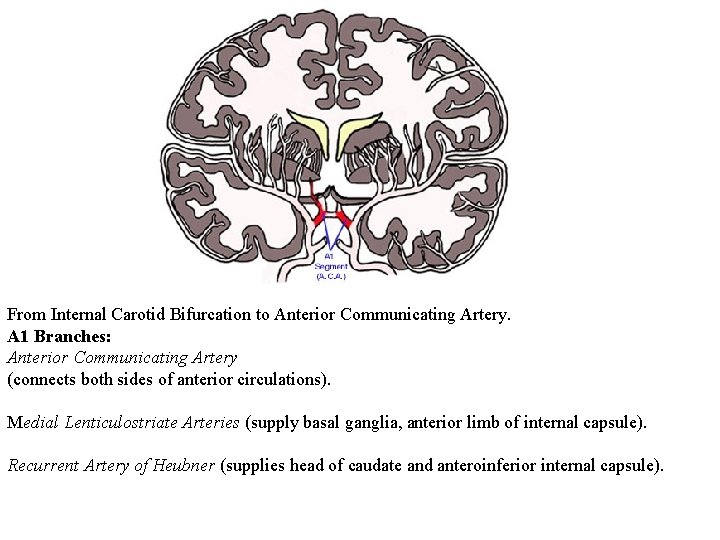
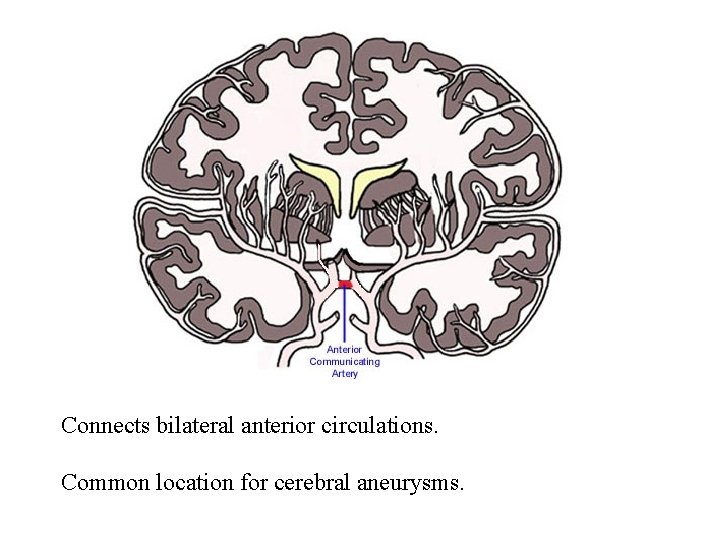
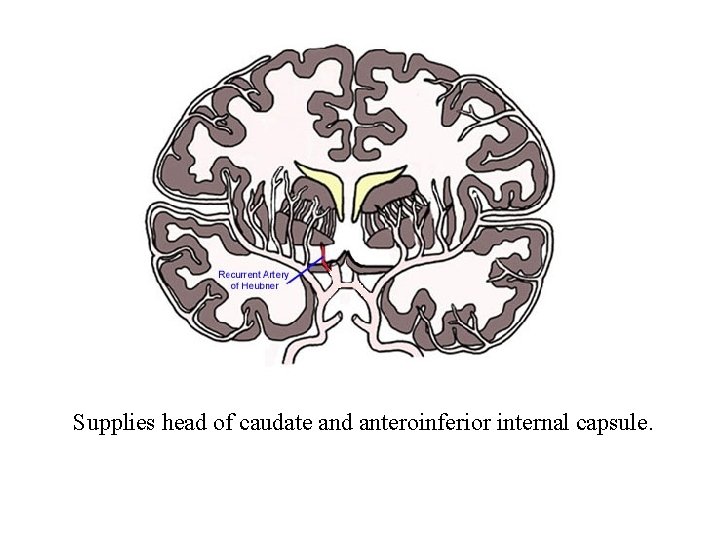
From Internal Carotid Bifurcation to Anterior Communicating Artery. A 1 Branches: Anterior Communicating Artery (connects both sides of anterior circulations). Medial Lenticulostriate Arteries (supply basal ganglia, anterior limb of internal capsule). Recurrent Artery of Heubner (supplies head of caudate and anteroinferior internal capsule).
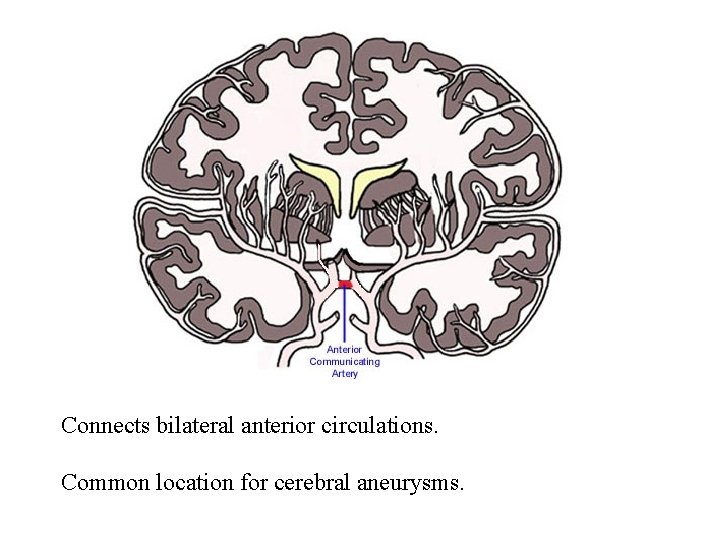
Connects bilateral anterior circulations. Common location for cerebral aneurysms.
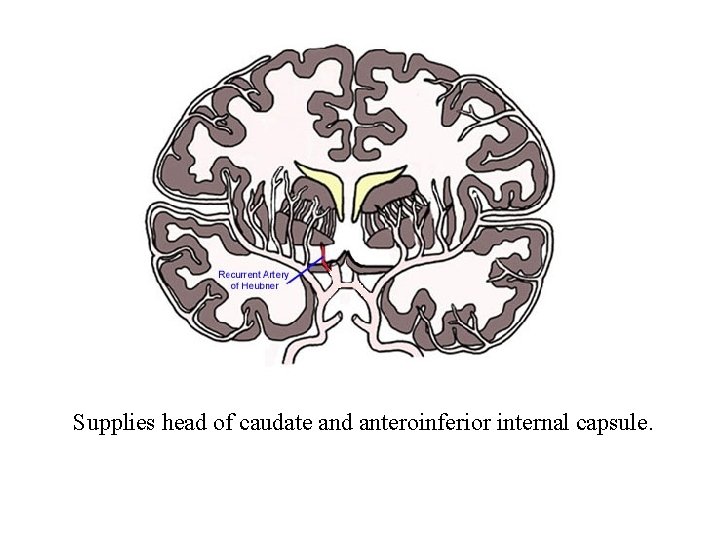
Supplies head of caudate and anteroinferior internal capsule.

Pericallosal Artery Continuation of the ACA as it arches superiorly and posteriorly. Supplies the medial surface of the cerebral hemispheres and corpus callosum.

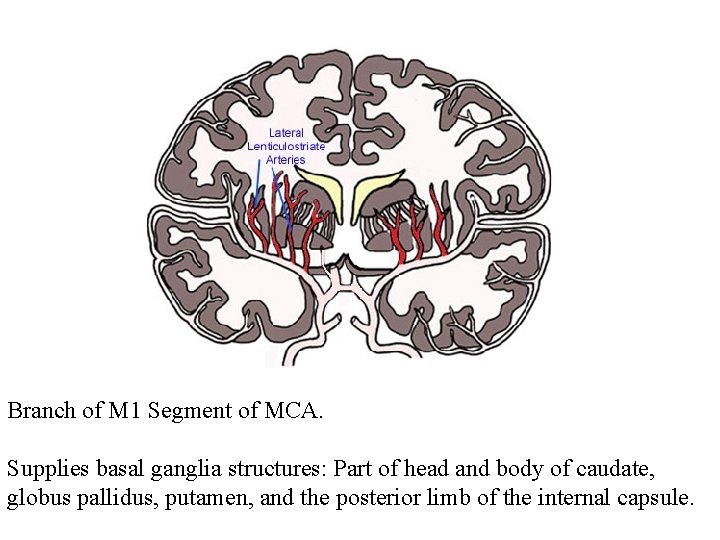
Supplies most of the temporal lobe, anterolateral frontal lobe, and parietal lobe. Perforating branches supply the posterior limb of the internal capsule, part of the head and body of the caudate and globus pallidus.
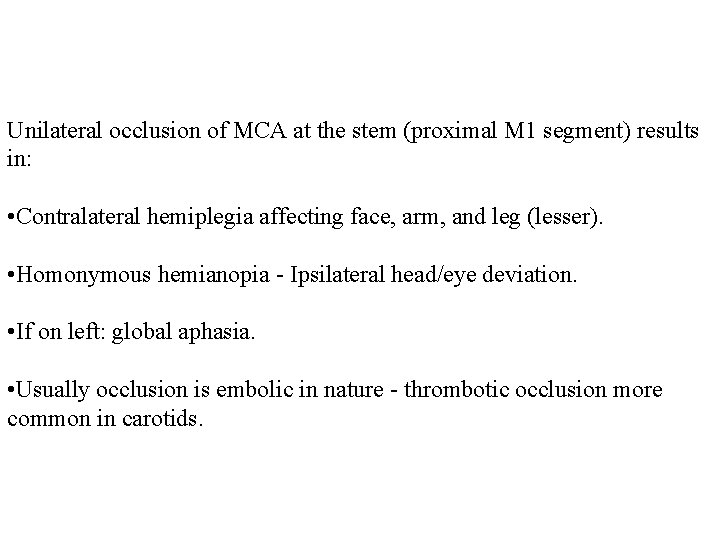
Unilateral occlusion of MCA at the stem (proximal M 1 segment) results in: • Contralateral hemiplegia affecting face, arm, and leg (lesser). • Homonymous hemianopia - Ipsilateral head/eye deviation. • If on left: global aphasia. • Usually occlusion is embolic in nature - thrombotic occlusion more common in carotids.

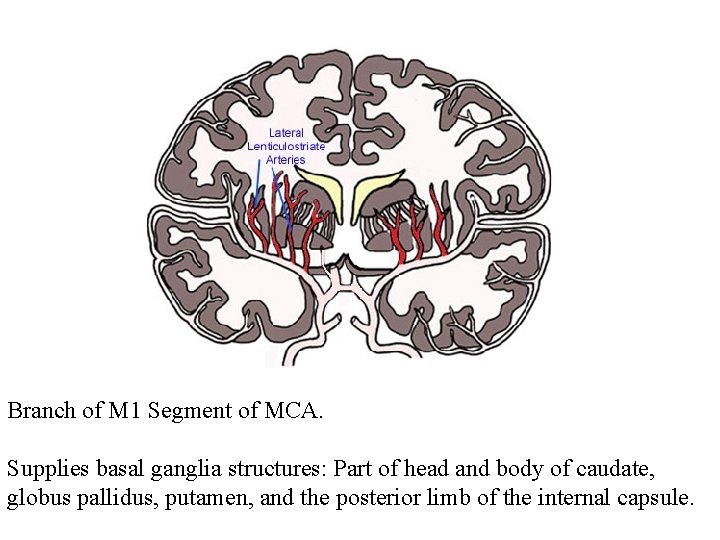
Branch of M 1 Segment of MCA. Supplies basal ganglia structures: Part of head and body of caudate, globus pallidus, putamen, and the posterior limb of the internal capsule.

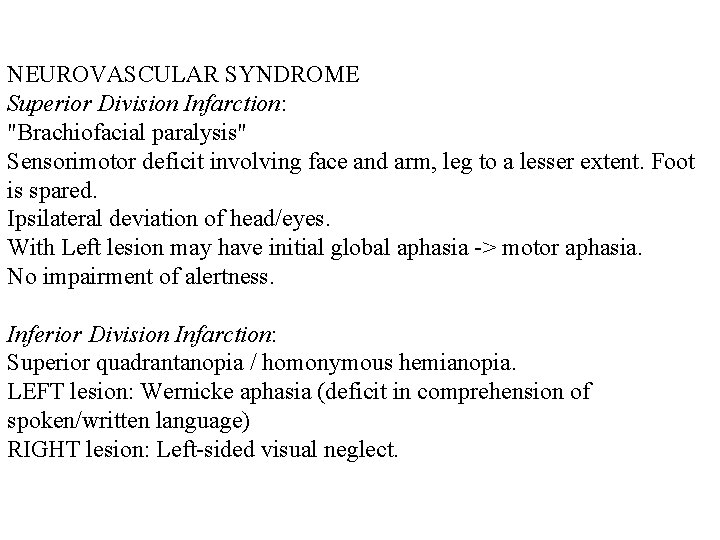
Sylvian (M 2) Segment MCA Segment divides into superior and inferior divisions which can be a site for an embolus to lodge. Branches supply: Temporal Lobe and Insular Cortex (sensory language area of Wernicke) Parietal Lobe, (Sensory cortical areas), Inferolateral frontal lobe.
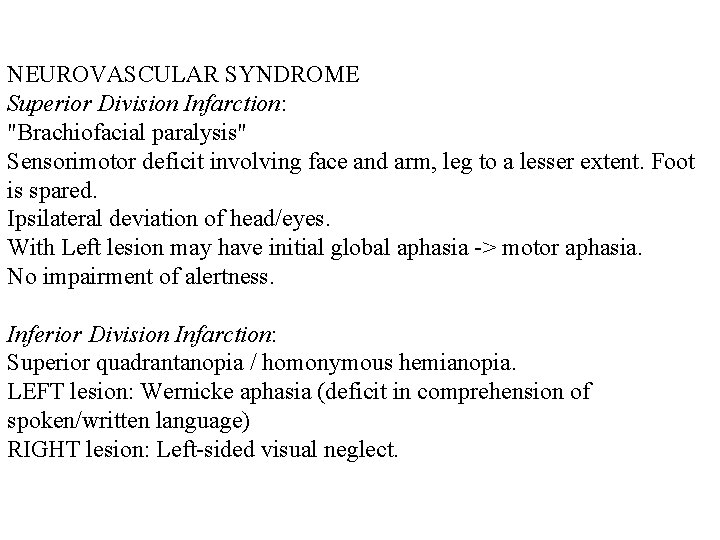
NEUROVASCULAR SYNDROME Superior Division Infarction: "Brachiofacial paralysis" Sensorimotor deficit involving face and arm, leg to a lesser extent. Foot is spared. Ipsilateral deviation of head/eyes. With Left lesion may have initial global aphasia -> motor aphasia. No impairment of alertness. Inferior Division Infarction: Superior quadrantanopia / homonymous hemianopia. LEFT lesion: Wernicke aphasia (deficit in comprehension of spoken/written language) RIGHT lesion: Left-sided visual neglect.
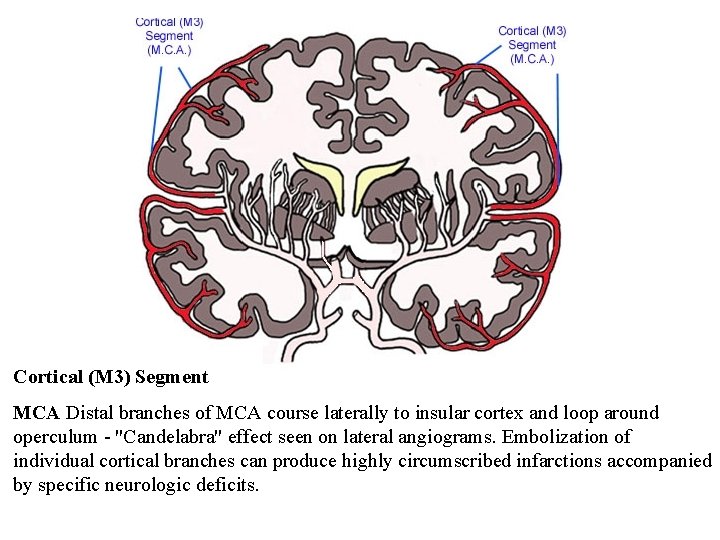
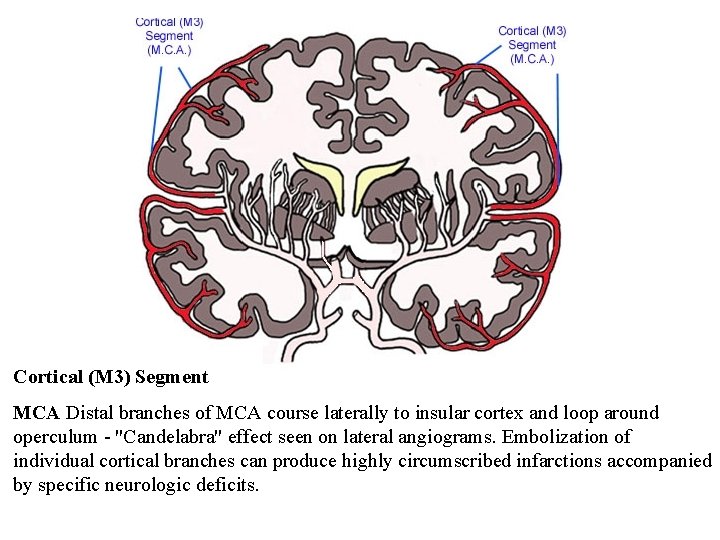
Cortical (M 3) Segment MCA Distal branches of MCA course laterally to insular cortex and loop around operculum - "Candelabra" effect seen on lateral angiograms. Embolization of individual cortical branches can produce highly circumscribed infarctions accompanied by specific neurologic deficits.

Vertebral Artery
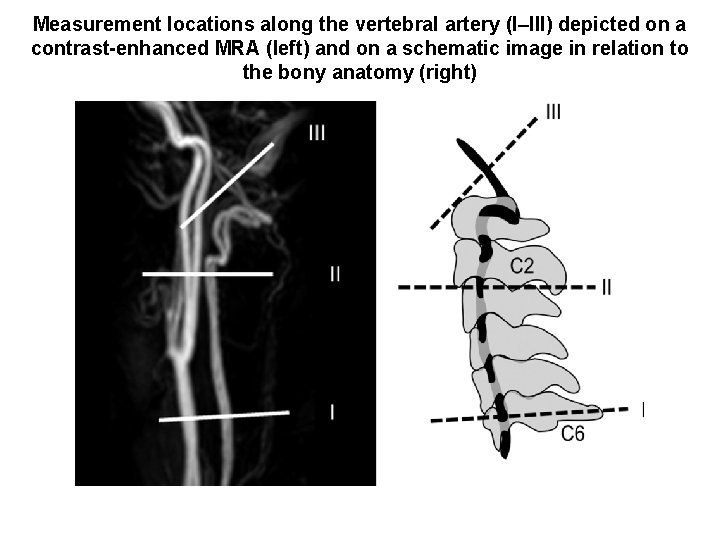
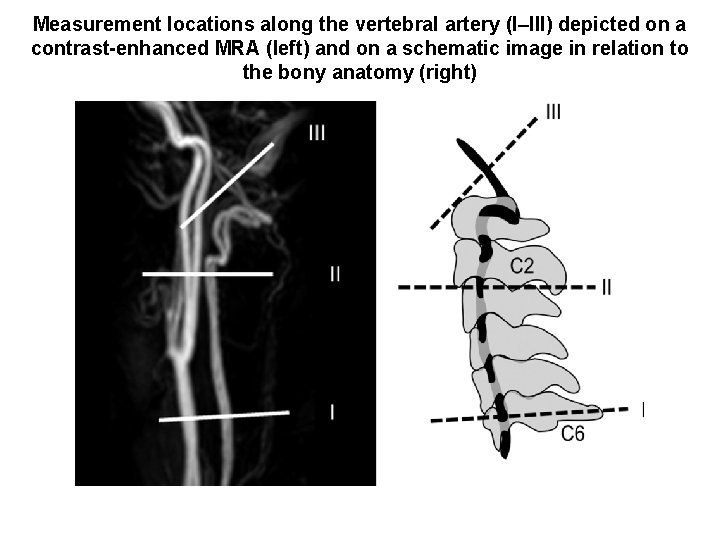
Measurement locations along the vertebral artery (I–III) depicted on a contrast-enhanced MRA (left) and on a schematic image in relation to the bony anatomy (right)

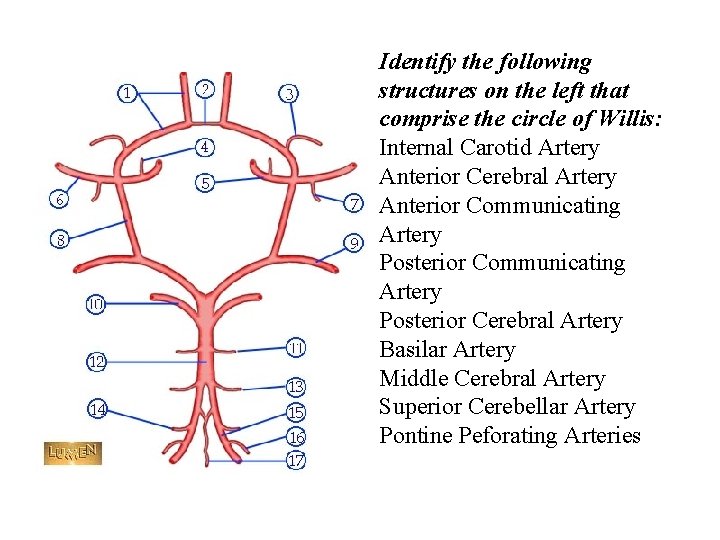
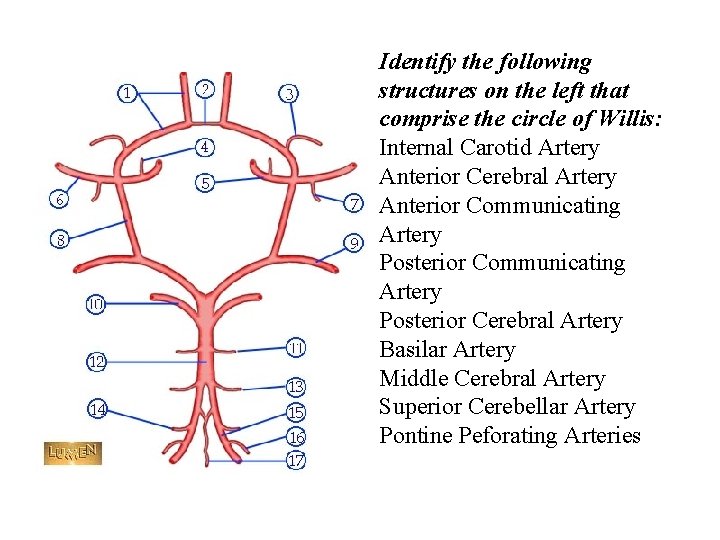
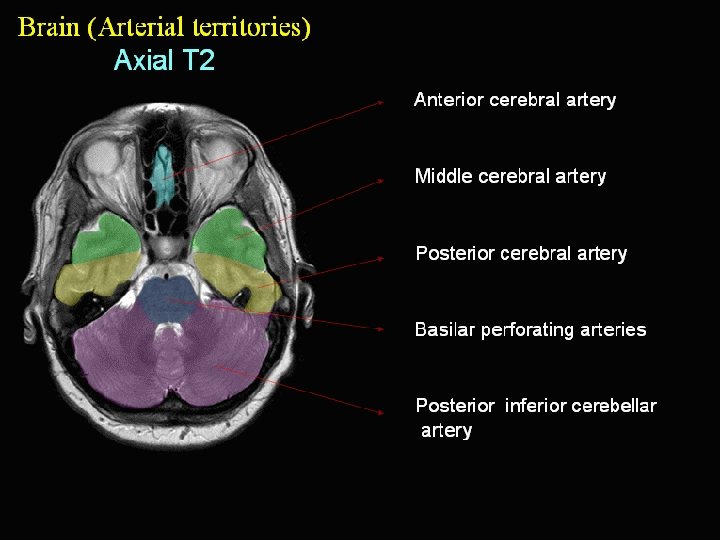
Identify the following structures on the left that comprise the circle of Willis: Internal Carotid Artery Anterior Cerebral Artery Anterior Communicating Artery Posterior Cerebral Artery Basilar Artery Middle Cerebral Artery Superior Cerebellar Artery Pontine Peforating Arteries
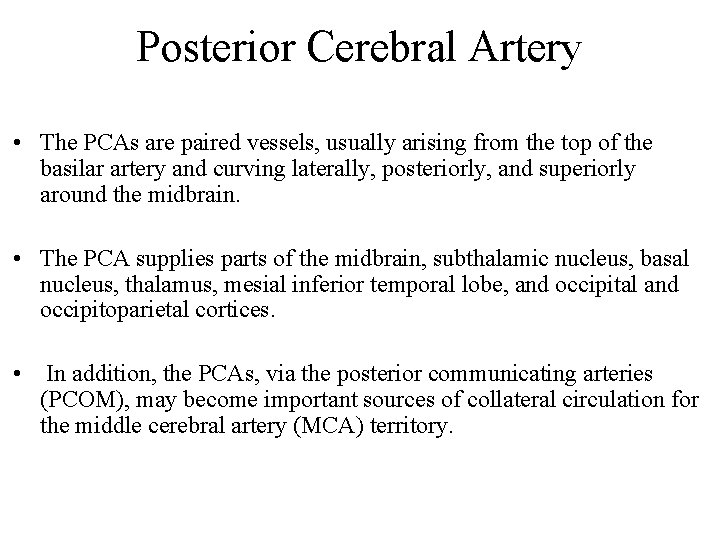
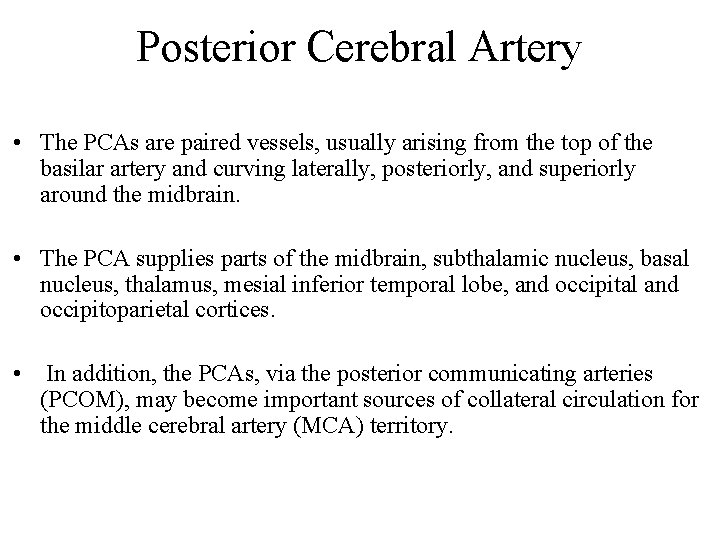
Posterior Cerebral Artery • The PCAs are paired vessels, usually arising from the top of the basilar artery and curving laterally, posteriorly, and superiorly around the midbrain. • The PCA supplies parts of the midbrain, subthalamic nucleus, basal nucleus, thalamus, mesial inferior temporal lobe, and occipital and occipitoparietal cortices. • In addition, the PCAs, via the posterior communicating arteries (PCOM), may become important sources of collateral circulation for the middle cerebral artery (MCA) territory.

Posterior Cerebral Artery • The PCA is divided into P 1 and P 2 segments by the PCOM. Penetrating branches to the mesencephalon, subthalamic, basal structures, and thalamus arise primarily from the P 1 segment and the PCOM. These penetrating arteries include thalamogeniculate, splenial (posterior paricallosal artery), and lateral and medial posterior choroidal arteries. • The P 2 segment bifurcates into the posterior temporal artery and the internal occipital artery. The posterior temporal artery further divides into anterior, middle, posterior, and hippocampal branches. The internal occipital artery divides into calcarine and occipitoparietal branches.




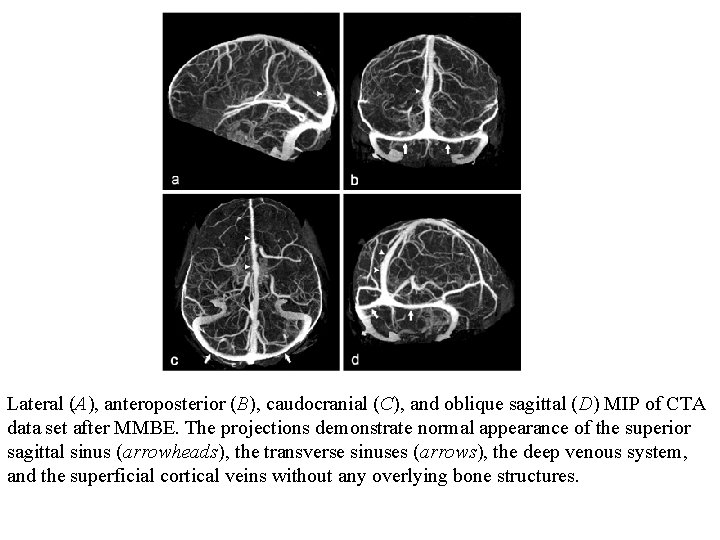
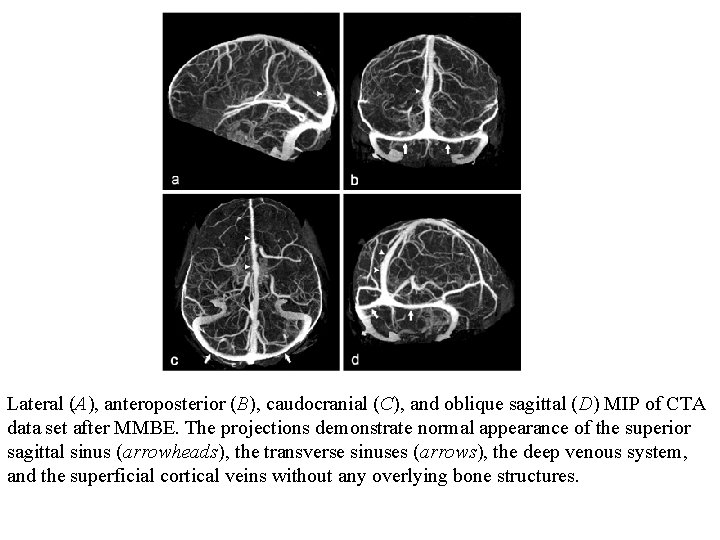
Lateral (A), anteroposterior (B), caudocranial (C), and oblique sagittal (D) MIP of CTA data set after MMBE. The projections demonstrate normal appearance of the superior sagittal sinus (arrowheads), the transverse sinuses (arrows), the deep venous system, and the superficial cortical veins without any overlying bone structures.
 Lllkk
Lllkk Basilar artery course
Basilar artery course Posterior auricular vein
Posterior auricular vein Internal carotid artery blood supply
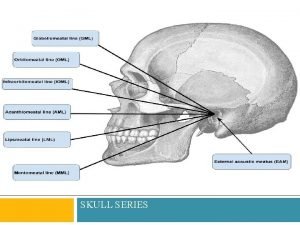
Internal carotid artery blood supply Chapter 42 extraoral imaging
Chapter 42 extraoral imaging Reverse towne projeksiyonu
Reverse towne projeksiyonu Lateral cephalometric radiograph
Lateral cephalometric radiograph Anthropological baseline
Anthropological baseline Adler and towne
Adler and towne Lom craneo
Lom craneo James towne village
James towne village Petrous ridge
Petrous ridge Anatomia tc encefalo
Anatomia tc encefalo Reverse townes view positioning
Reverse townes view positioning Radiografia stenvers
Radiografia stenvers X ray mastoid towne's view position
X ray mastoid towne's view position Open mouth towne's view
Open mouth towne's view What is the area of lateral faces
What is the area of lateral faces System of internal controls
System of internal controls Vouching in auditing
Vouching in auditing Neurology sonography
Neurology sonography Interior trunk
Interior trunk Carotid sheath contents
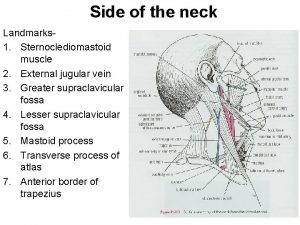
Carotid sheath contents Pulse site and location
Pulse site and location Lana schumacher md
Lana schumacher md Pheocromocytoma
Pheocromocytoma Carotid cavernous fistula
Carotid cavernous fistula Antihelix
Antihelix Preauricular lymph node
Preauricular lymph node Sternocleidomastoid
Sternocleidomastoid Tympanic branch of glossopharyngeal nerve
Tympanic branch of glossopharyngeal nerve Carotid sinus hypersensitivity
Carotid sinus hypersensitivity Retract defintion
Retract defintion Carotid artery pulse
Carotid artery pulse Carotid cana
Carotid cana Parotid fascia
Parotid fascia Carotid cochlear dehiscence
Carotid cochlear dehiscence Tympanic cavity
Tympanic cavity Carotid terminus
Carotid terminus Facial foramen
Facial foramen Carotid anatomy
Carotid anatomy V
V Ileocecal junction cat
Ileocecal junction cat Maxillary artery branches
Maxillary artery branches Carotid sinus
Carotid sinus Salpingopalatine fold
Salpingopalatine fold Contents of carotid sheath
Contents of carotid sheath Jaringan pengangkut
Jaringan pengangkut Posisi lateral
Posisi lateral Passive earth pressure
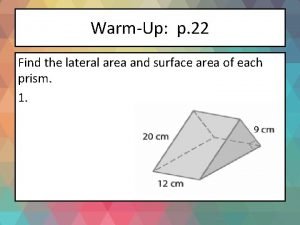
Passive earth pressure Find the lateral area and surface area of each prism
Find the lateral area and surface area of each prism Vista superior
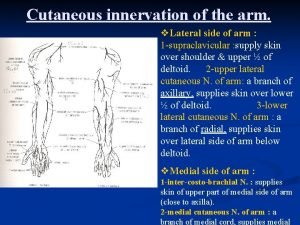
Vista superior Arm cutaneous innervation
Arm cutaneous innervation Pola komunikasi lateral
Pola komunikasi lateral