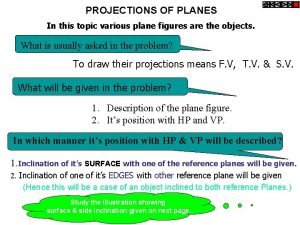
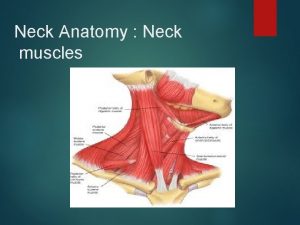
Side of the neck Landmarks 1 Sternoclediomastoid muscle
- Slides: 26
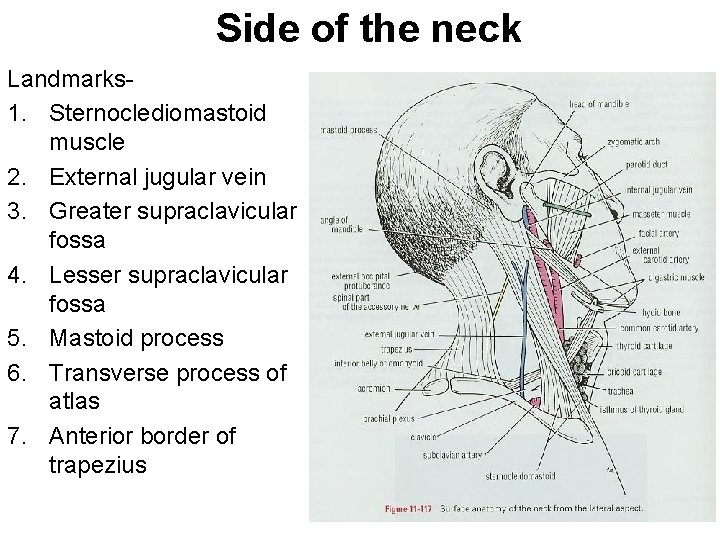
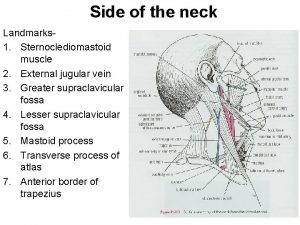
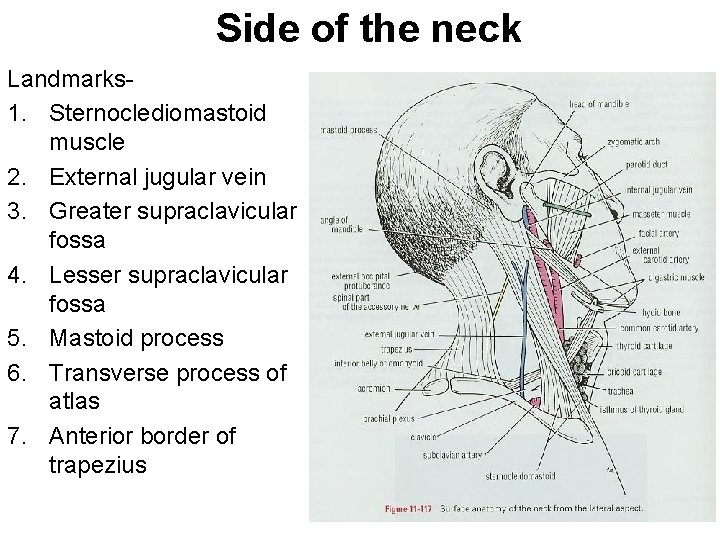
Side of the neck Landmarks 1. Sternoclediomastoid muscle 2. External jugular vein 3. Greater supraclavicular fossa 4. Lesser supraclavicular fossa 5. Mastoid process 6. Transverse process of atlas 7. Anterior border of trapezius
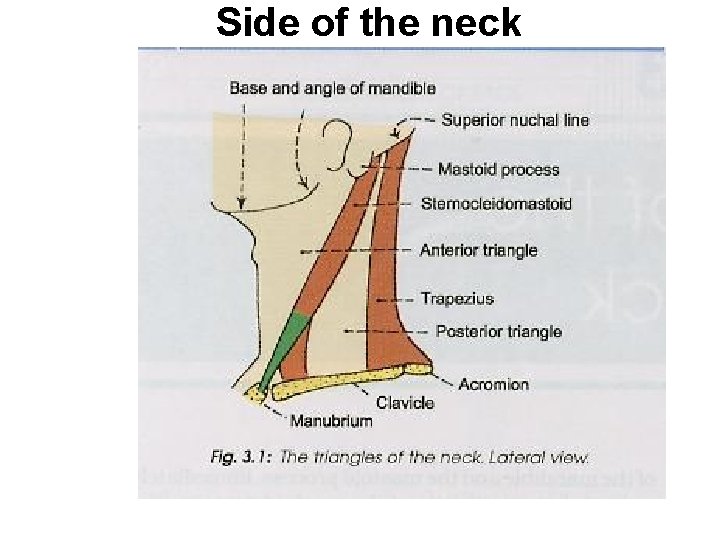
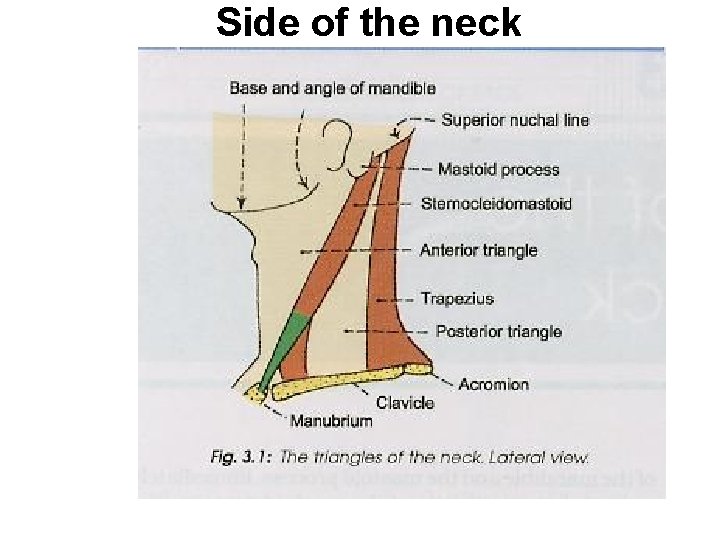
Side of the neck
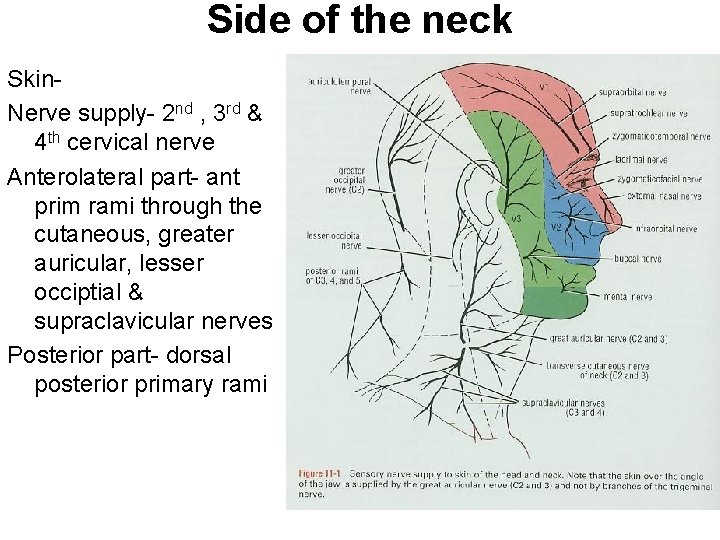
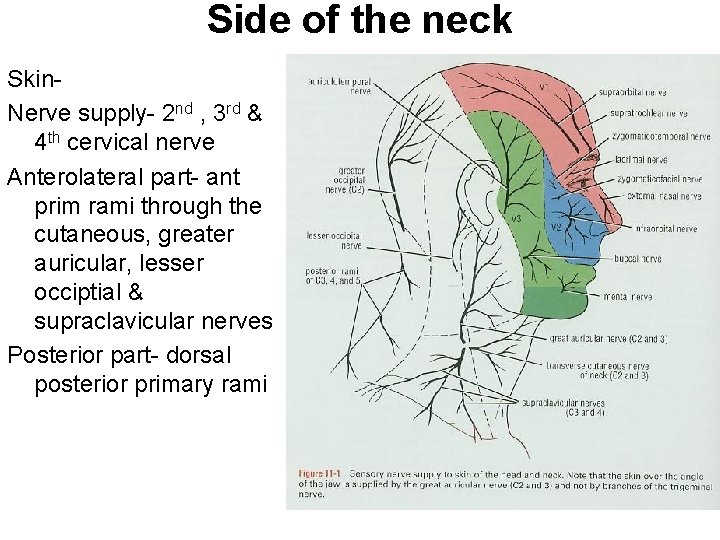
Side of the neck Skin. Nerve supply- 2 nd , 3 rd & 4 th cervical nerve Anterolateral part- ant prim rami through the cutaneous, greater auricular, lesser occiptial & supraclavicular nerves Posterior part- dorsal posterior primary rami
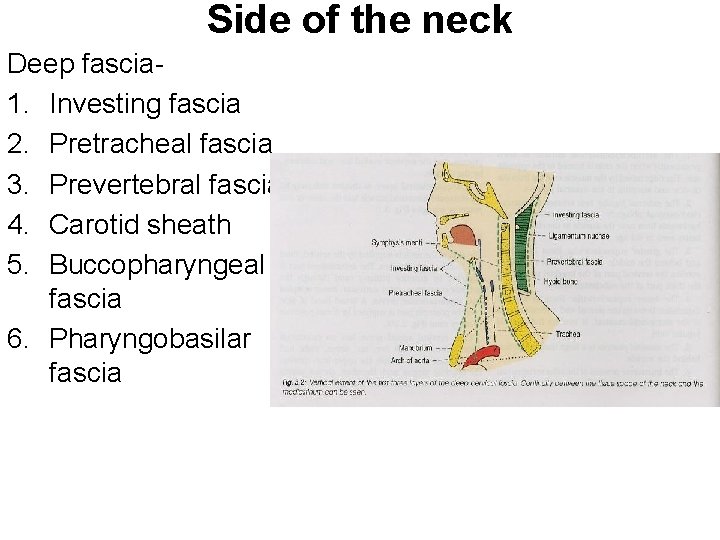
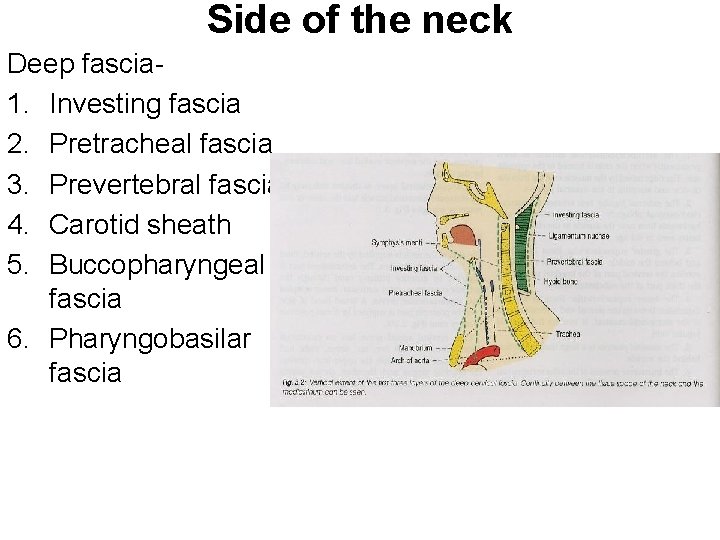
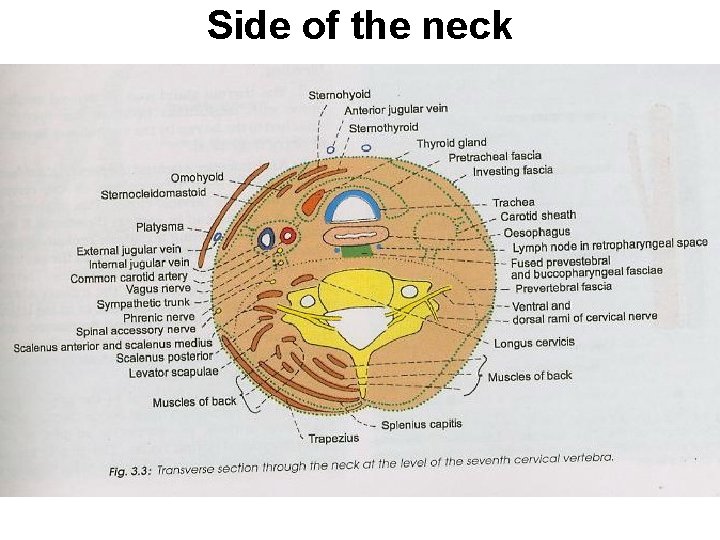
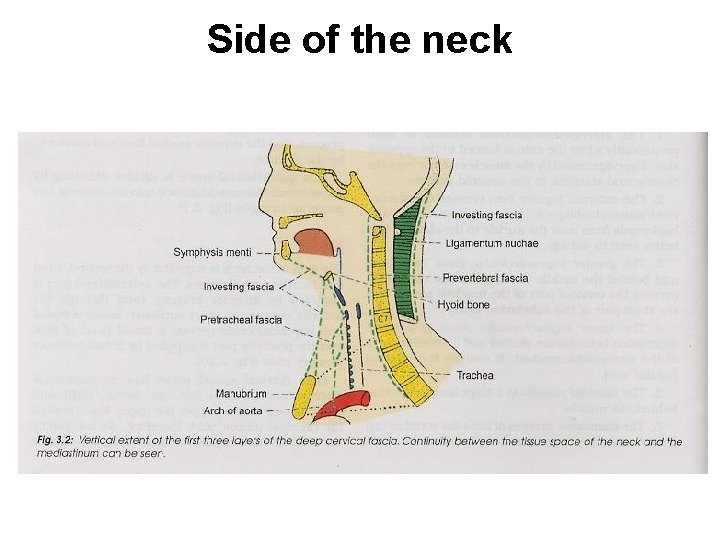
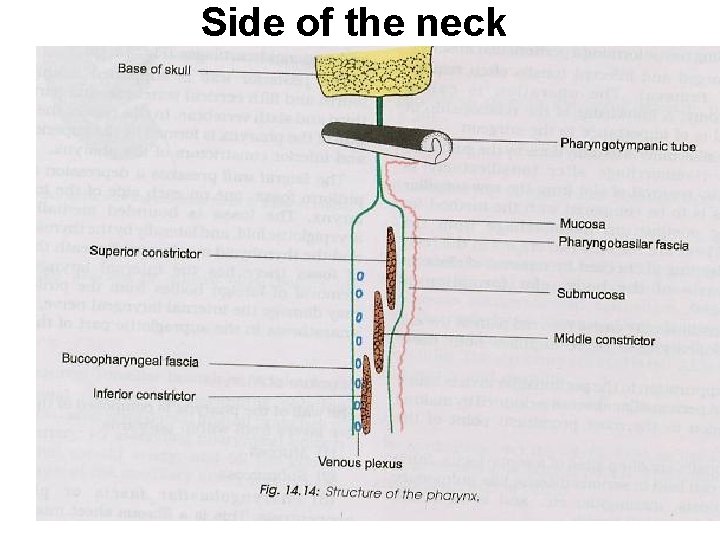
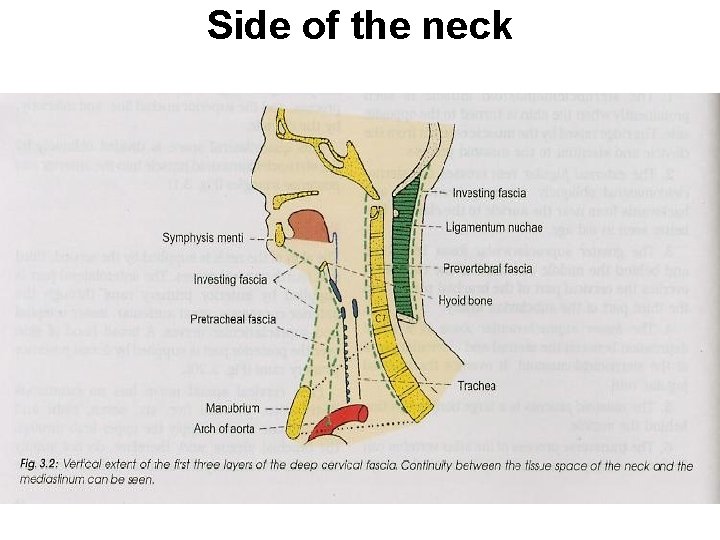
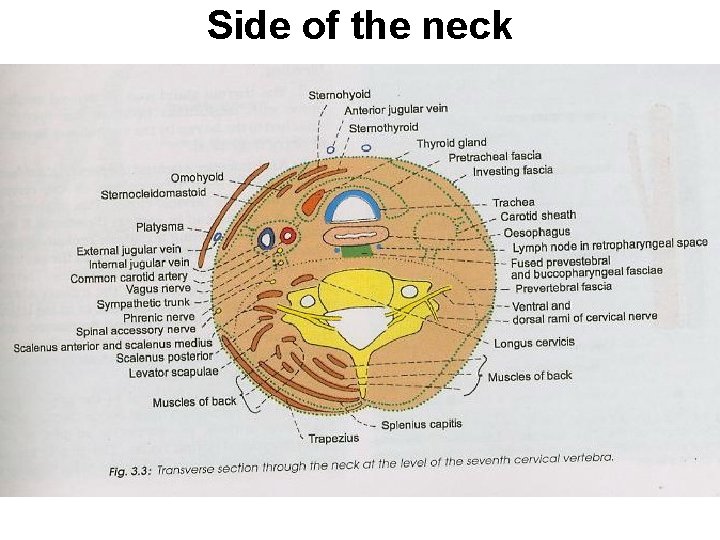
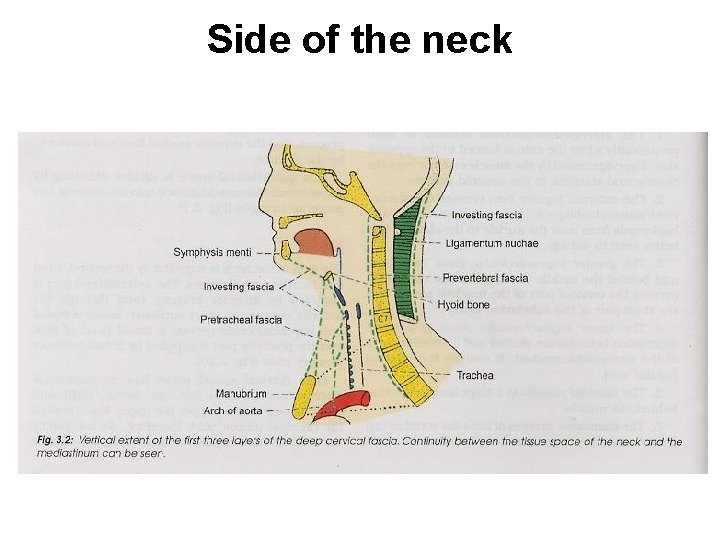
Side of the neck Deep fascia 1. Investing fascia 2. Pretracheal fascia 3. Prevertebral fascia 4. Carotid sheath 5. Buccopharyngeal fascia 6. Pharyngobasilar fascia
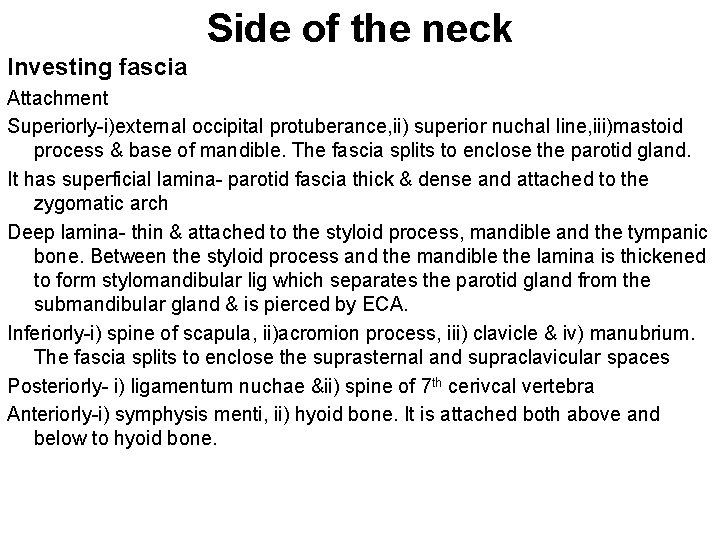
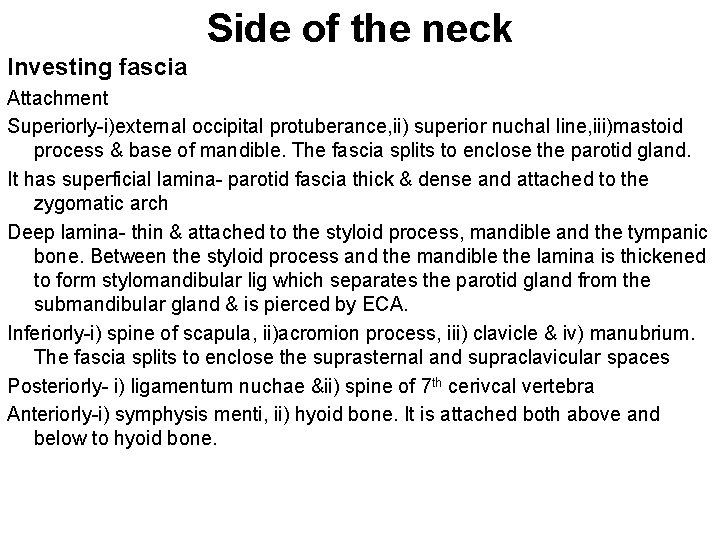
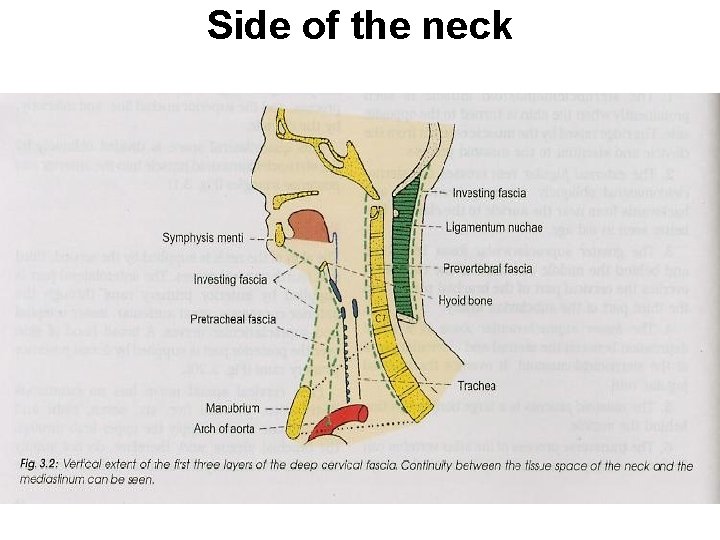
Side of the neck Investing fascia Attachment Superiorly-i)external occipital protuberance, ii) superior nuchal line, iii)mastoid process & base of mandible. The fascia splits to enclose the parotid gland. It has superficial lamina- parotid fascia thick & dense and attached to the zygomatic arch Deep lamina- thin & attached to the styloid process, mandible and the tympanic bone. Between the styloid process and the mandible the lamina is thickened to form stylomandibular lig which separates the parotid gland from the submandibular gland & is pierced by ECA. Inferiorly-i) spine of scapula, ii)acromion process, iii) clavicle & iv) manubrium. The fascia splits to enclose the suprasternal and supraclavicular spaces Posteriorly- i) ligamentum nuchae &ii) spine of 7 th cerivcal vertebra Anteriorly-i) symphysis menti, ii) hyoid bone. It is attached both above and below to hyoid bone.
Side of the neck
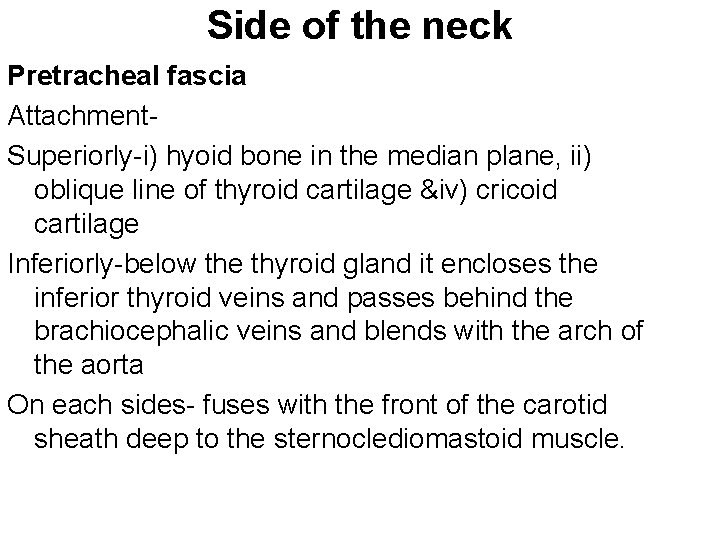
Side of the neck Pretracheal fascia Attachment. Superiorly-i) hyoid bone in the median plane, ii) oblique line of thyroid cartilage &iv) cricoid cartilage Inferiorly-below the thyroid gland it encloses the inferior thyroid veins and passes behind the brachiocephalic veins and blends with the arch of the aorta On each sides- fuses with the front of the carotid sheath deep to the sternoclediomastoid muscle.
Side of the neck
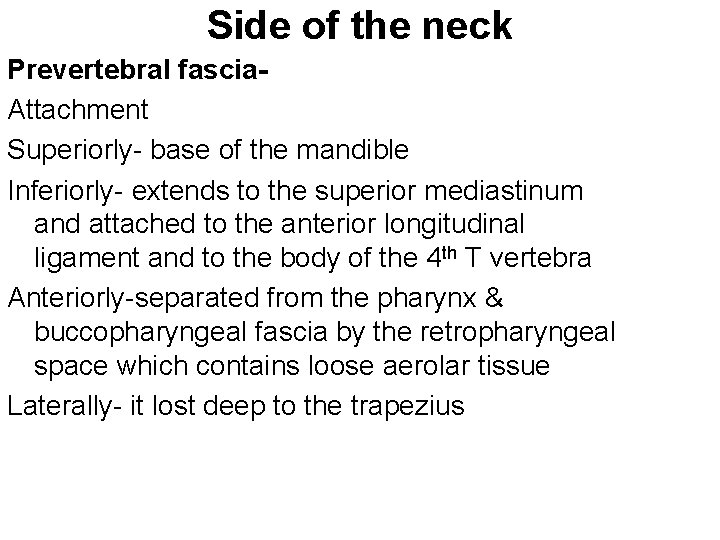
Side of the neck Prevertebral fascia. Attachment Superiorly- base of the mandible Inferiorly- extends to the superior mediastinum and attached to the anterior longitudinal ligament and to the body of the 4 th T vertebra Anteriorly-separated from the pharynx & buccopharyngeal fascia by the retropharyngeal space which contains loose aerolar tissue Laterally- it lost deep to the trapezius
Side of the neck
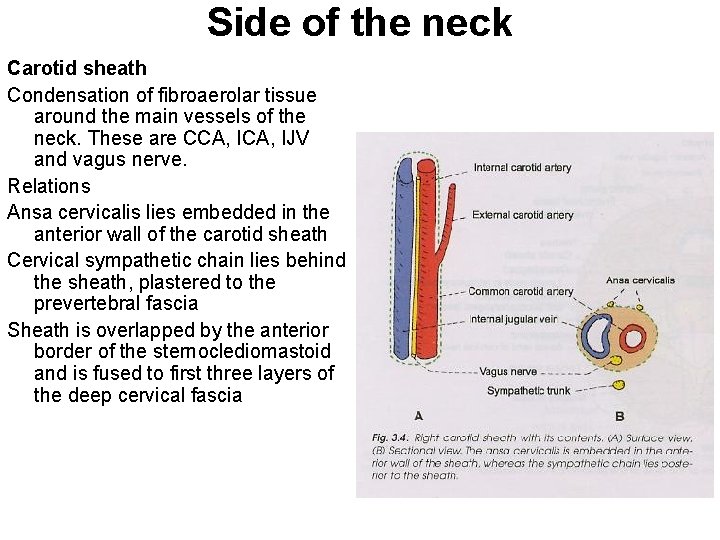
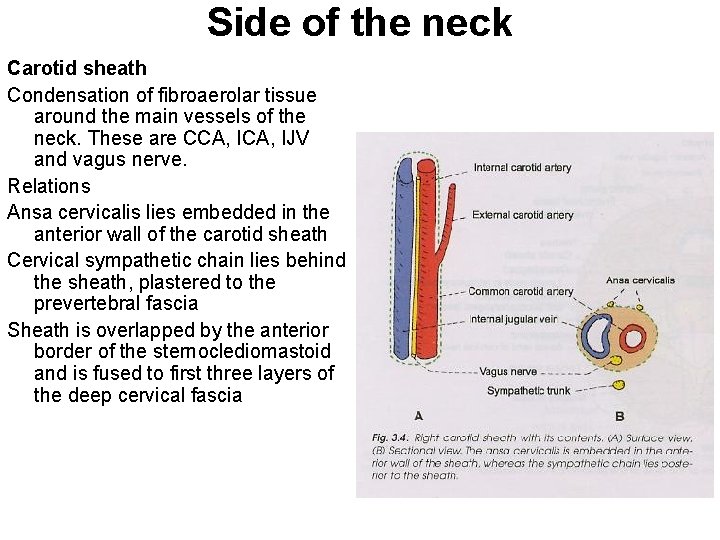
Side of the neck Carotid sheath Condensation of fibroaerolar tissue around the main vessels of the neck. These are CCA, IJV and vagus nerve. Relations Ansa cervicalis lies embedded in the anterior wall of the carotid sheath Cervical sympathetic chain lies behind the sheath, plastered to the prevertebral fascia Sheath is overlapped by the anterior border of the sternoclediomastoid and is fused to first three layers of the deep cervical fascia
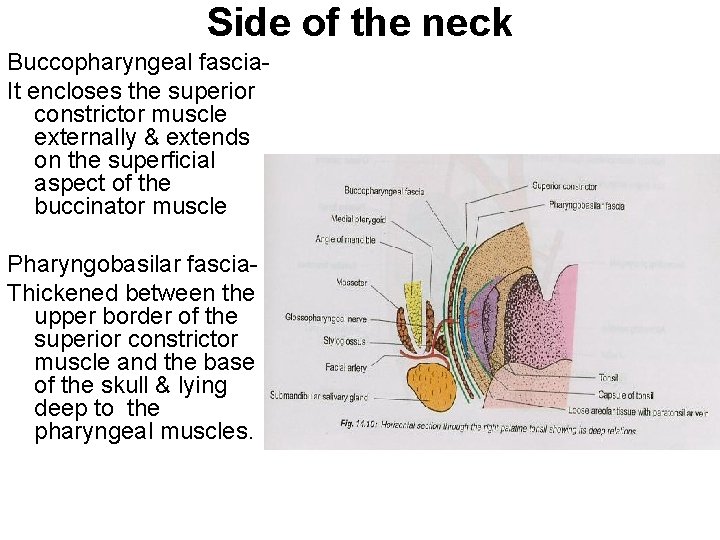
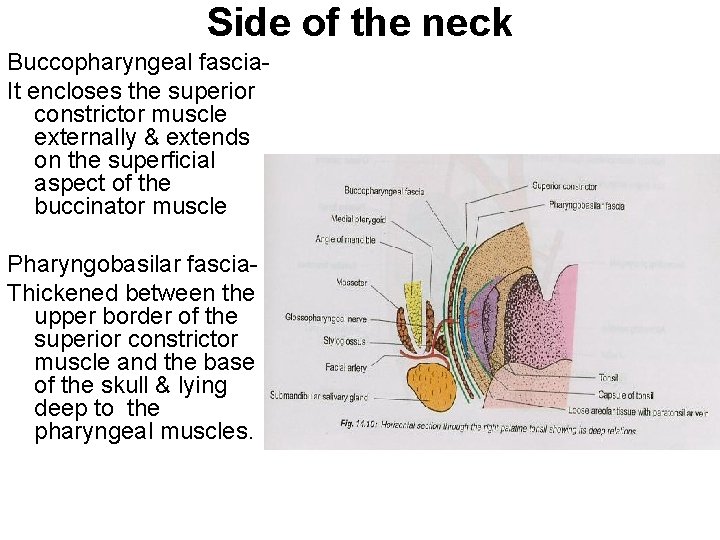
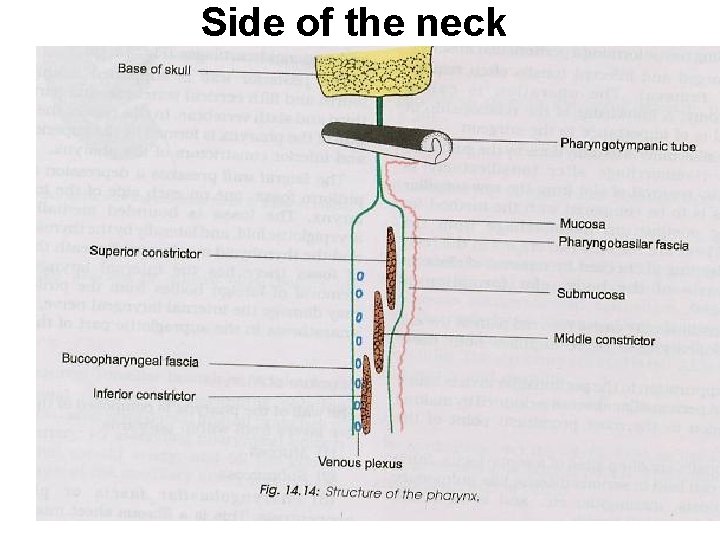
Side of the neck Buccopharyngeal fascia. It encloses the superior constrictor muscle externally & extends on the superficial aspect of the buccinator muscle Pharyngobasilar fascia. Thickened between the upper border of the superior constrictor muscle and the base of the skull & lying deep to the pharyngeal muscles.
Side of the neck
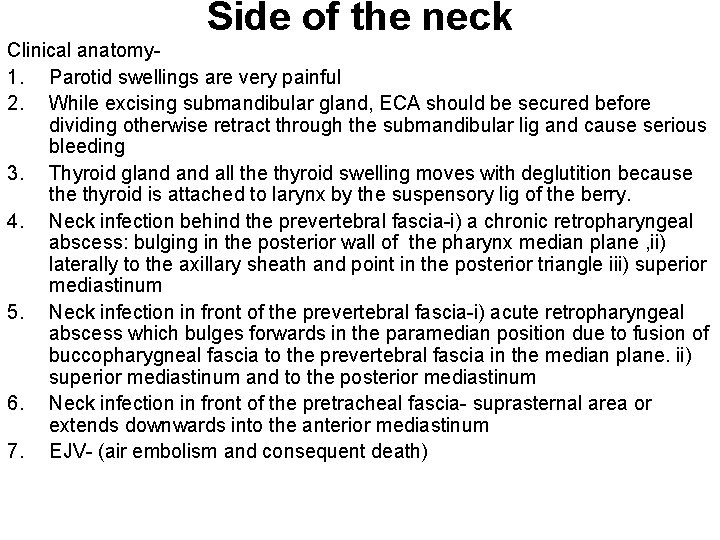
Side of the neck Clinical anatomy 1. Parotid swellings are very painful 2. While excising submandibular gland, ECA should be secured before dividing otherwise retract through the submandibular lig and cause serious bleeding 3. Thyroid gland all the thyroid swelling moves with deglutition because thyroid is attached to larynx by the suspensory lig of the berry. 4. Neck infection behind the prevertebral fascia-i) a chronic retropharyngeal abscess: bulging in the posterior wall of the pharynx median plane , ii) laterally to the axillary sheath and point in the posterior triangle iii) superior mediastinum 5. Neck infection in front of the prevertebral fascia-i) acute retropharyngeal abscess which bulges forwards in the paramedian position due to fusion of buccopharygneal fascia to the prevertebral fascia in the median plane. ii) superior mediastinum and to the posterior mediastinum 6. Neck infection in front of the pretracheal fascia- suprasternal area or extends downwards into the anterior mediastinum 7. EJV- (air embolism and consequent death)
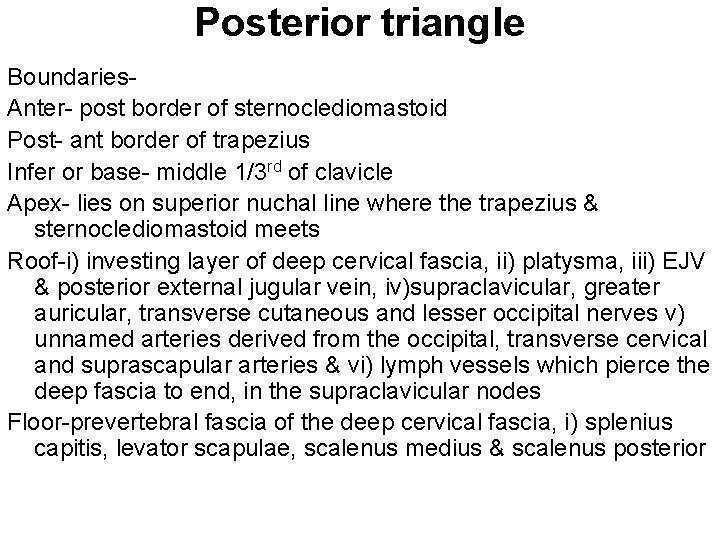
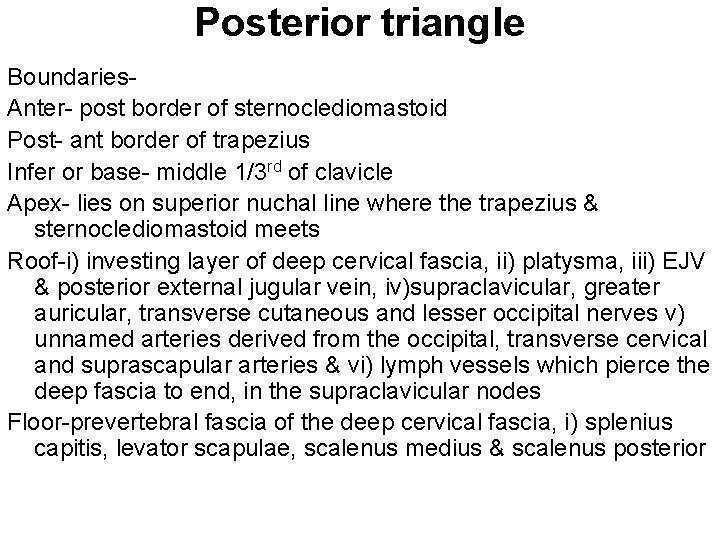
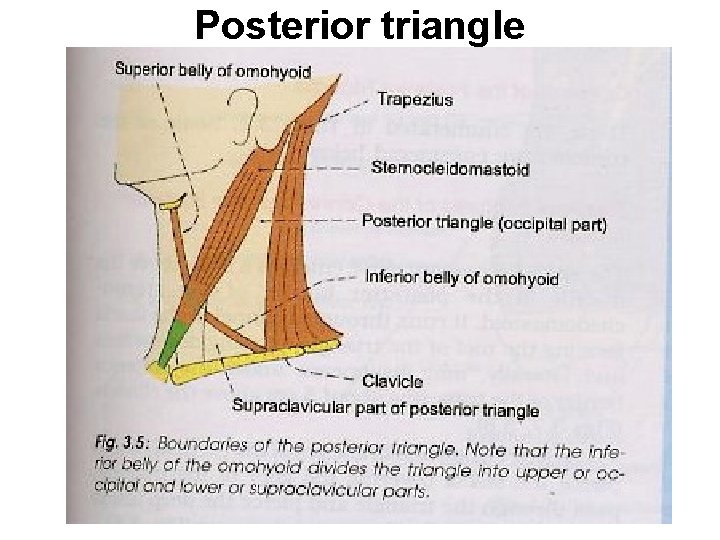
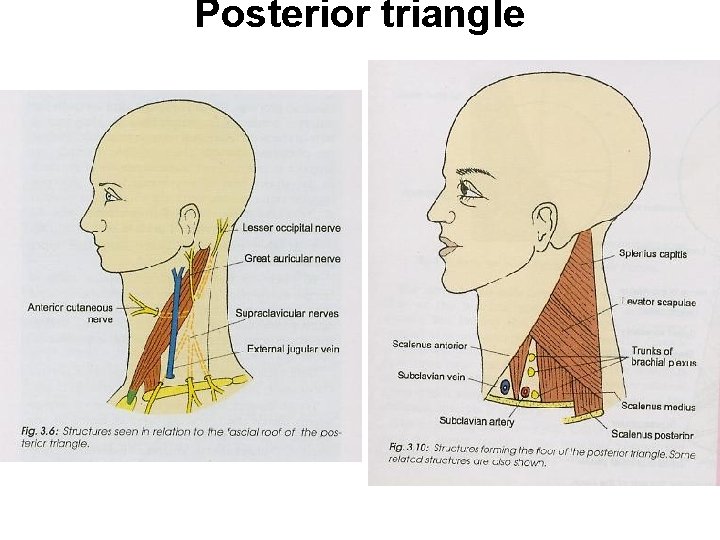
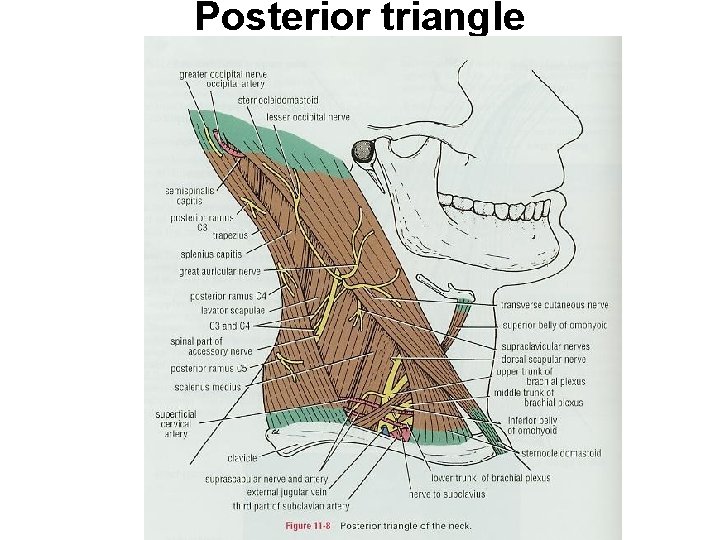
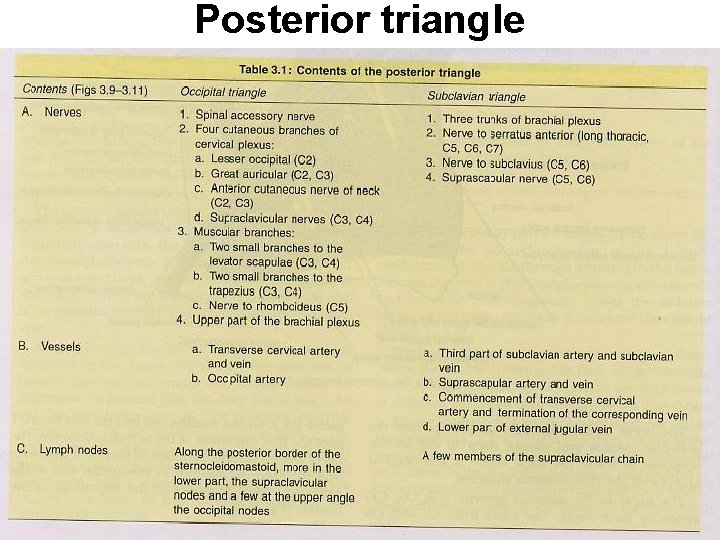
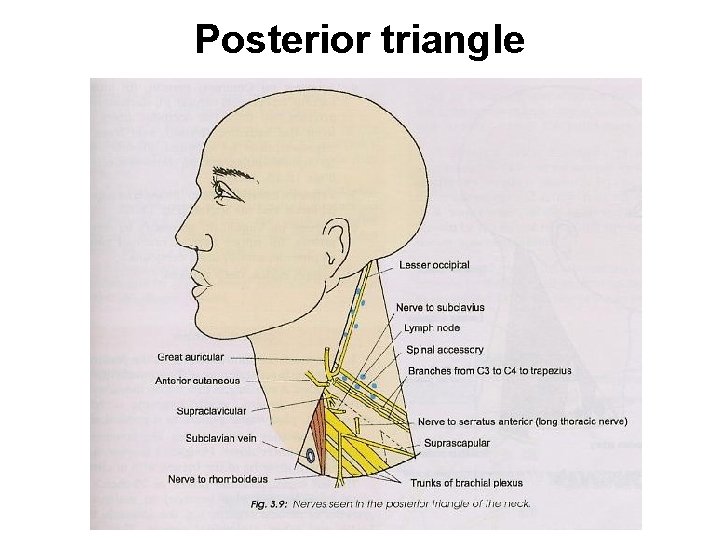
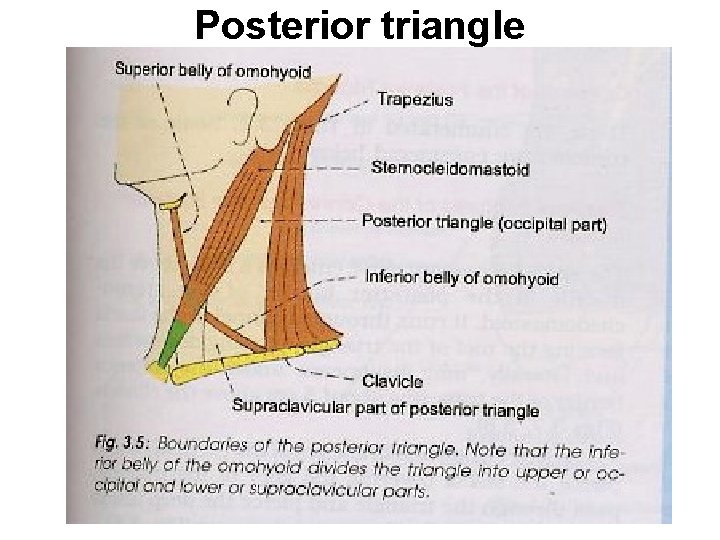
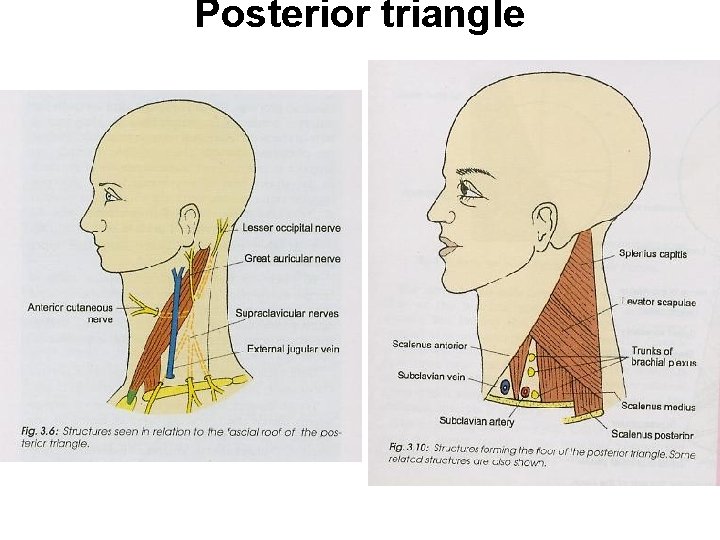
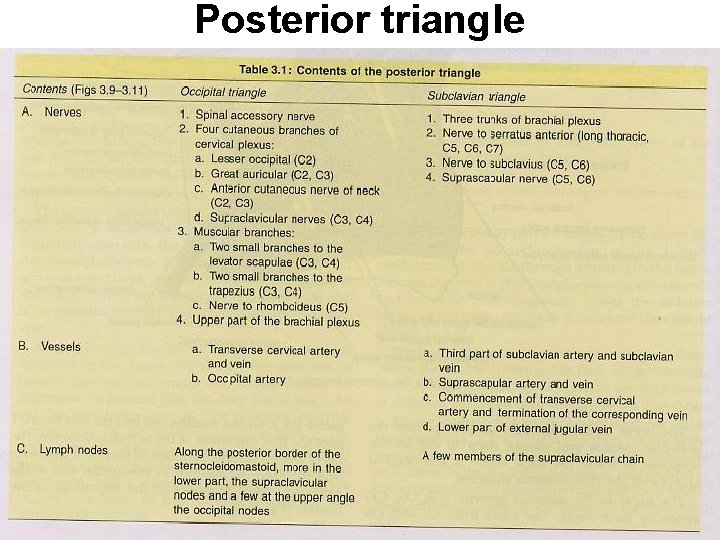
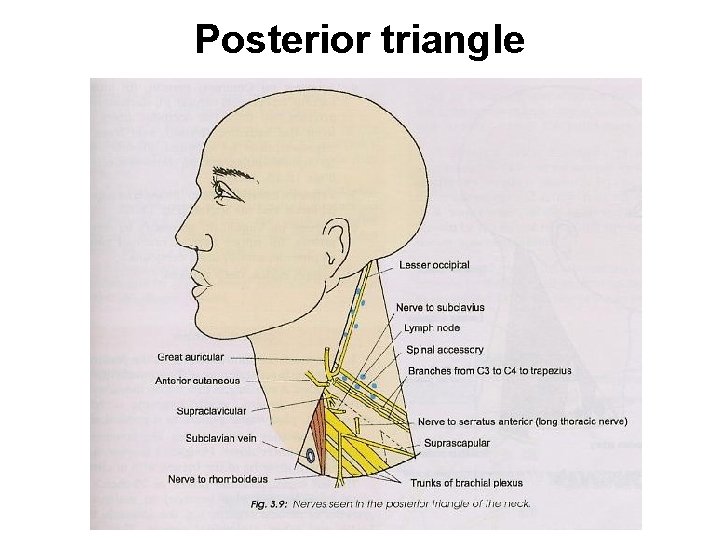
Posterior triangle Boundaries. Anter- post border of sternoclediomastoid Post- ant border of trapezius Infer or base- middle 1/3 rd of clavicle Apex- lies on superior nuchal line where the trapezius & sternoclediomastoid meets Roof-i) investing layer of deep cervical fascia, ii) platysma, iii) EJV & posterior external jugular vein, iv)supraclavicular, greater auricular, transverse cutaneous and lesser occipital nerves v) unnamed arteries derived from the occipital, transverse cervical and suprascapular arteries & vi) lymph vessels which pierce the deep fascia to end, in the supraclavicular nodes Floor-prevertebral fascia of the deep cervical fascia, i) splenius capitis, levator scapulae, scalenus medius & scalenus posterior
Posterior triangle
Posterior triangle
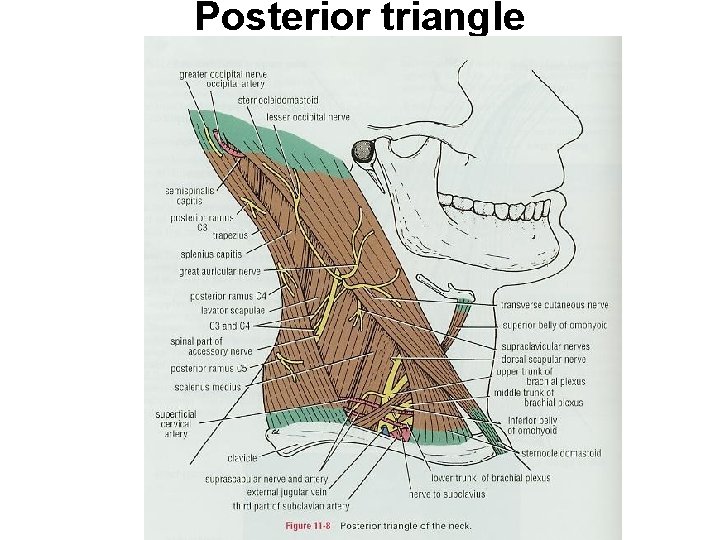
Posterior triangle
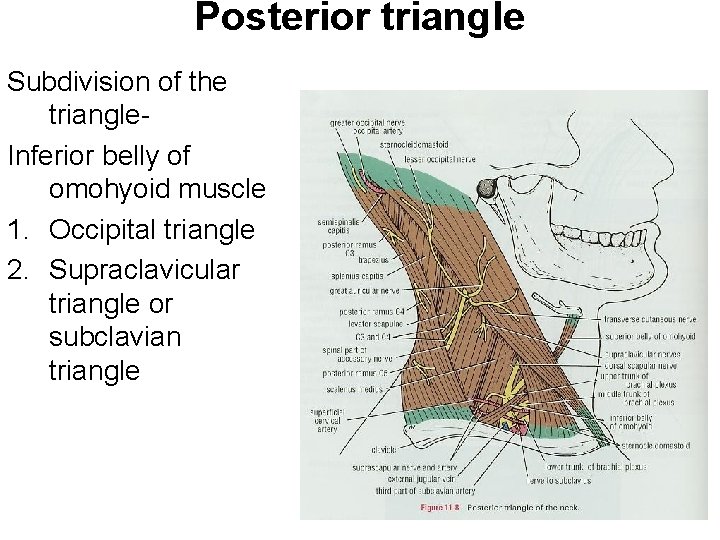
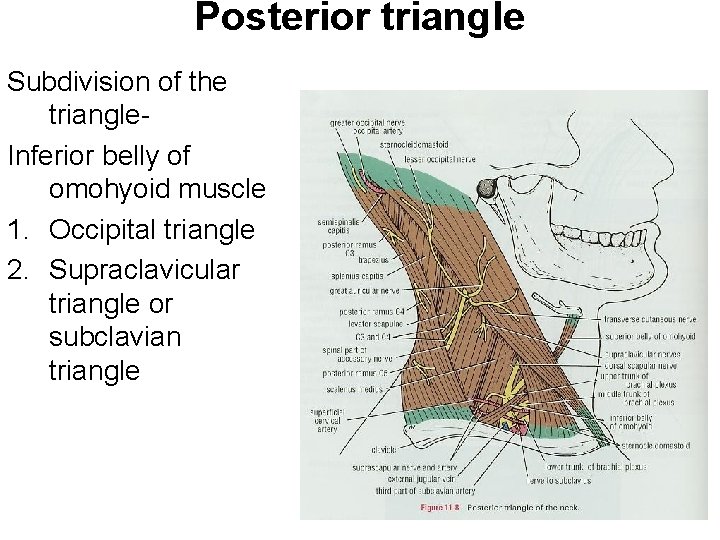
Posterior triangle Subdivision of the triangle. Inferior belly of omohyoid muscle 1. Occipital triangle 2. Supraclavicular triangle or subclavian triangle
Posterior triangle
Posterior triangle
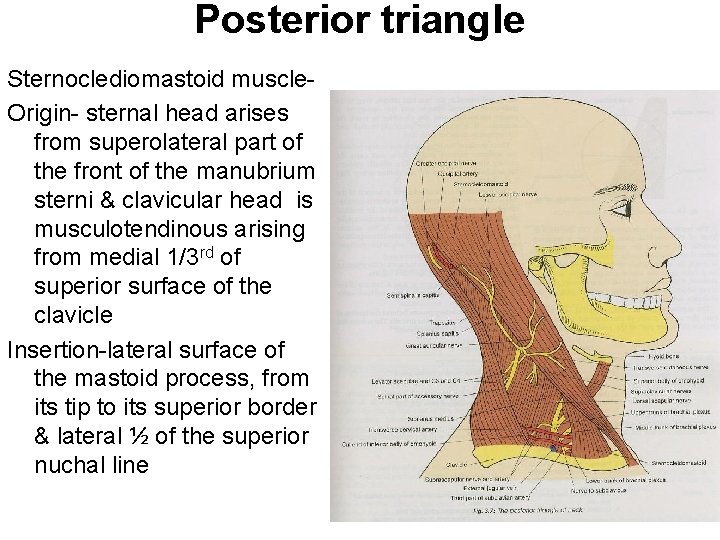
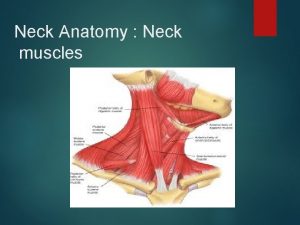
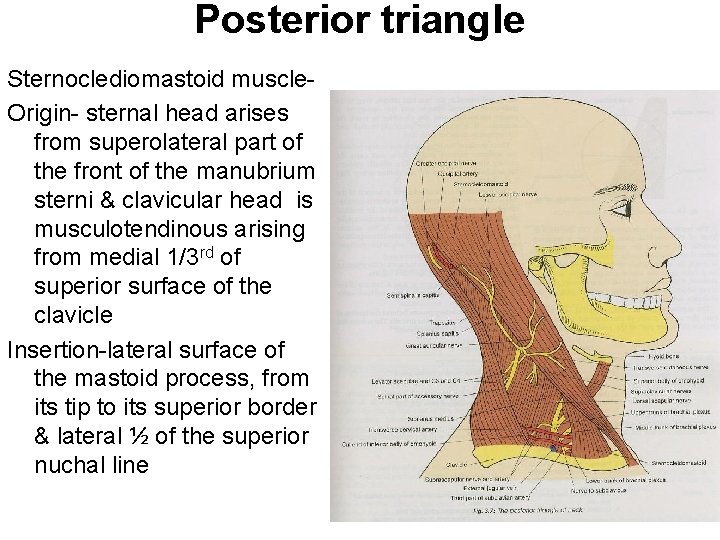
Posterior triangle Sternoclediomastoid muscle. Origin- sternal head arises from superolateral part of the front of the manubrium sterni & clavicular head is musculotendinous arising from medial 1/3 rd of superior surface of the clavicle Insertion-lateral surface of the mastoid process, from its tip to its superior border & lateral ½ of the superior nuchal line
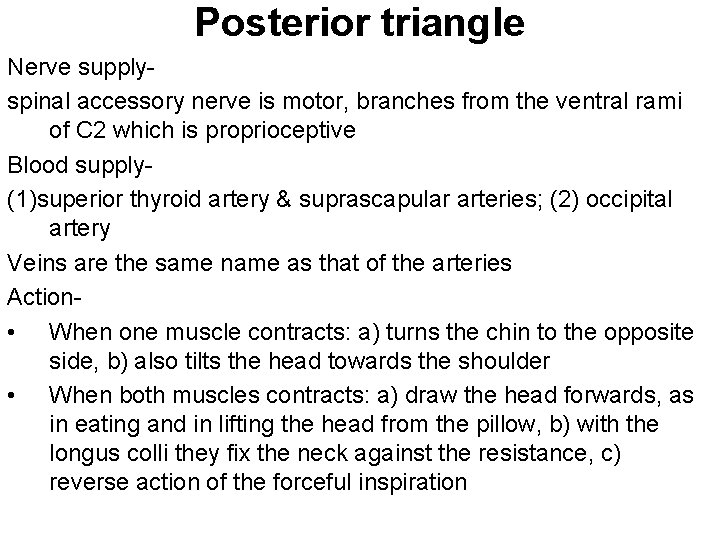
Posterior triangle Nerve supplyspinal accessory nerve is motor, branches from the ventral rami of C 2 which is proprioceptive Blood supply(1)superior thyroid artery & suprascapular arteries; (2) occipital artery Veins are the same name as that of the arteries Action • When one muscle contracts: a) turns the chin to the opposite side, b) also tilts the head towards the shoulder • When both muscles contracts: a) draw the head forwards, as in eating and in lifting the head from the pillow, b) with the longus colli they fix the neck against the resistance, c) reverse action of the forceful inspiration
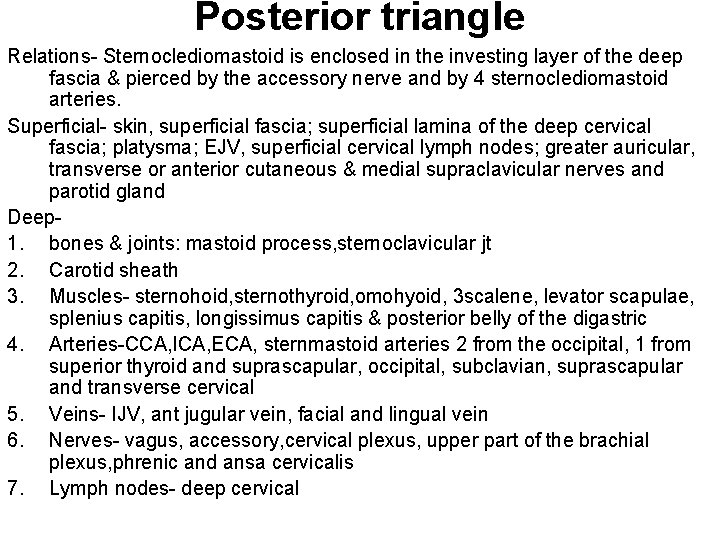
Posterior triangle Relations- Sternoclediomastoid is enclosed in the investing layer of the deep fascia & pierced by the accessory nerve and by 4 sternoclediomastoid arteries. Superficial- skin, superficial fascia; superficial lamina of the deep cervical fascia; platysma; EJV, superficial cervical lymph nodes; greater auricular, transverse or anterior cutaneous & medial supraclavicular nerves and parotid gland Deep 1. bones & joints: mastoid process, sternoclavicular jt 2. Carotid sheath 3. Muscles- sternohoid, sternothyroid, omohyoid, 3 scalene, levator scapulae, splenius capitis, longissimus capitis & posterior belly of the digastric 4. Arteries-CCA, ICA, ECA, sternmastoid arteries 2 from the occipital, 1 from superior thyroid and suprascapular, occipital, subclavian, suprascapular and transverse cervical 5. Veins- IJV, ant jugular vein, facial and lingual vein 6. Nerves- vagus, accessory, cervical plexus, upper part of the brachial plexus, phrenic and ansa cervicalis 7. Lymph nodes- deep cervical
Posterior triangle Clinical anatomy 1. Swelling in the posterior triangle is due enlargement of supraclaviular lymph nodes. Lipoma, cystic hygroma or lymphangioma, pharyngeal pouch or a cervical rib. Supraclavicular lymph nodes are commonly enlarged in tuberculosis, Hodgkin’s disease and in malignant growth of the breast, arm or chest. 2. Left supraclavicular nodes or Virchow’s or Scalene nodes are mostly involved in malignant growths of distant organs, eg stomach, testis and other abdominal organs. Because of the drainage to the thoracic duct 3. Torticollis or wry neck- deformity in which the head bent to one side and the chin points to the other side. a) Rehumatic torticollis- due to exposure to cold or draught b) Reflex torticollis- due to inflamed or suppurating cervical lymph nodes which irritate the spinal accessory nerve c) Congenital torticollis- due to birth injury d) Spasmodic torticollis- due to central irritation 4. Block dissection of the neck- (malignant disease) removal of cervical lymph nodes along with other structures involved in the growth.
Posterior triangle 5. Cervical rib may compress the subclavian artery. Decrease in the radial pulse or obliterated on turning the patient head upwards and to the affected side after a deep breath blood( Adson’s test) 6. Dysphagia caused by compression of the oesophagus by an abnormal subsclavian artery is called dysphagia lusoria 7. Blalock’s operation for fallot’s tetratogy right subsclavian artery is anastomosed end to side short circuit the pulmonary stenosis
 Sternoclediomastoid
Sternoclediomastoid Aa theorem
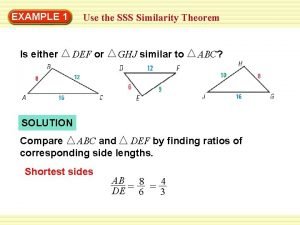
Aa theorem Sss similarity theorem examples
Sss similarity theorem examples Identify the similar triangles.
Identify the similar triangles. Sss
Sss Depressor labii inferioris
Depressor labii inferioris Lumber triangle
Lumber triangle Fusiform muscle
Fusiform muscle Powerful shoulder abductor used to raise the arm overhead
Powerful shoulder abductor used to raise the arm overhead Occlusion in cd
Occlusion in cd Two wheels roll side by side
Two wheels roll side by side Client side and server side
Client side and server side M&a process timeline
M&a process timeline Platzbedarf side by side melkstand
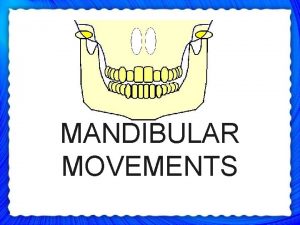
Platzbedarf side by side melkstand Muscle for protrusion of mandible
Muscle for protrusion of mandible Glass will break first on the weaker side, the side:
Glass will break first on the weaker side, the side: Weld root
Weld root Side by side stuff
Side by side stuff Perfect competition side by side graphs
Perfect competition side by side graphs Videocon refrigerator temperature settings
Videocon refrigerator temperature settings Smtyk
Smtyk A regular hexagonal lamina of side a
A regular hexagonal lamina of side a Sin = adjacent or opposite
Sin = adjacent or opposite Uil tea side by side
Uil tea side by side Red side blue side
Red side blue side Diễn thế sinh thái là
Diễn thế sinh thái là Thế nào là giọng cùng tên
Thế nào là giọng cùng tên