Transcranial Doppler TCD scan Stroke risk assessment Dr


- Slides: 32
Transcranial Doppler (TCD) scan & Stroke risk assessment Dr. Ijeoma N. Akinwumi (FMCPaed, MSc. Haemoglobinopathy) Lagos State University College of Medicine/ Teaching Hospital, Ikeja Lagos
Stroke risk assessment Stroke is a vascular event with neurological sequelae. Only the ischaemic type predominant in childhood SCD can be predicted. Comprehensive care & hence routine practice - UK, USA and other countries dealing with SCD includes TCD ischaemic stroke risk assessment/ screening. 1. Identify asymptomatic children at greatest risk for ischaemic stroke 2. Prevent an initial stroke by offering preventive intervention = Primary stroke prevention 3. Secondary stroke prevention – prevention of recurrence
Cost of Stroke Morbidity • Prevents achievement of expected independence and full potential • Adversely affects the quality of life • Imposes emotional, physical, psychosocial and financial burdens on their family, society • Financial burden to the healthcare system Mortality PREVENTION IS DESIRABLE!! Stroke risk assessment is EXTREMELY IMPORTANT. Steinlin et al, 2012
Epidemiology of childhood Stroke • Rare worldwide, approx 0. 003% • SCD is a major contributor - Hb. SS>>Hb. SC. • Ischaemic or haemorrhagic or combined In SCD • Peak incidence of 1 st stroke age 2 -5 yrs • Most before 10 yrs and rare below age 1 yr • By age 20 years – 11%. (Ganesan et al, 2002; Kirkham et al, 2004; Mallick and O’Callaghan, 2010; Ohene-Frempong et al, 1998)
SCD related stroke in Nigeria Clinical stroke rate is 5 -8. 4% of affected children 14 -20% of children die. Recurrence rate 26 - 75% 2/3 rd survivors - lifelong handicaps 28% stroke related epilepsy & 26% school dropout rate (hosp based data) • Also unreported strokes & deaths in community • • • Fatunde, 2005; Kehinde, 2008; Lagunju &Brown, 2012
History of Stroke risk assessment • Aaslid et al, 1982, 1 st recommended time averaged mean max velocity (TAMMV) in cm/sec for occlusive cerebral artery disease - less vulnerable to haemodynamic changes - corresponds better to cerebral perfusion & ideal for categorization of stroke risk. • Adams et al, 1992 predicted stroke risk using nonimaging transcranial Doppler techniques • Ohene-Frempong et al 1998 – Risk factors for CVA in SCD from 20 yr natural hx study of 4, 000 pts (0 - 45 yrs) • Adams et al, 1998 (STOP trial)-RCT blood transfusion vs standard treatment, outcome – stroke • Nichols et al, 2001 developed STOP Guidelines categorising and indicating need for intervention
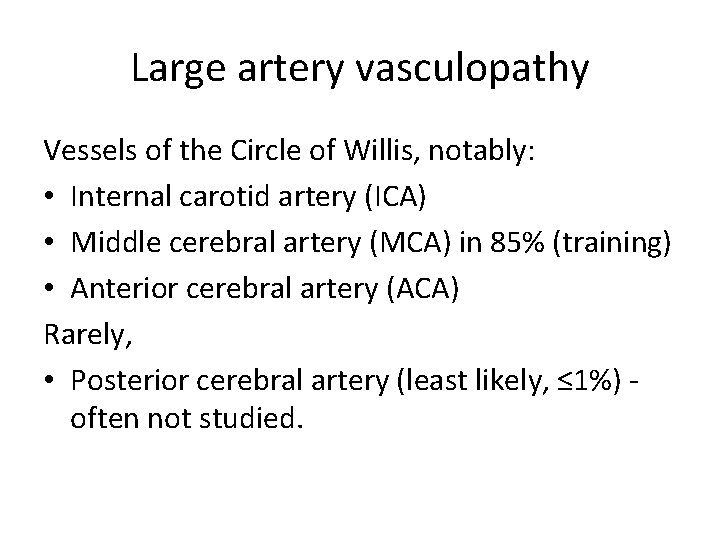
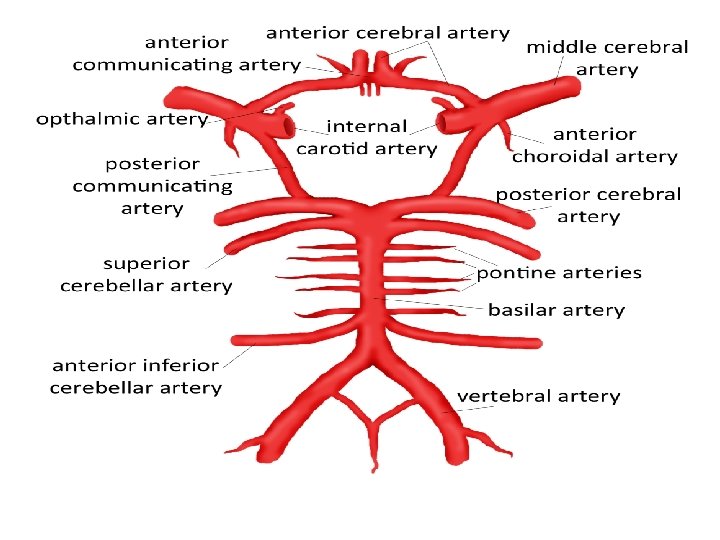
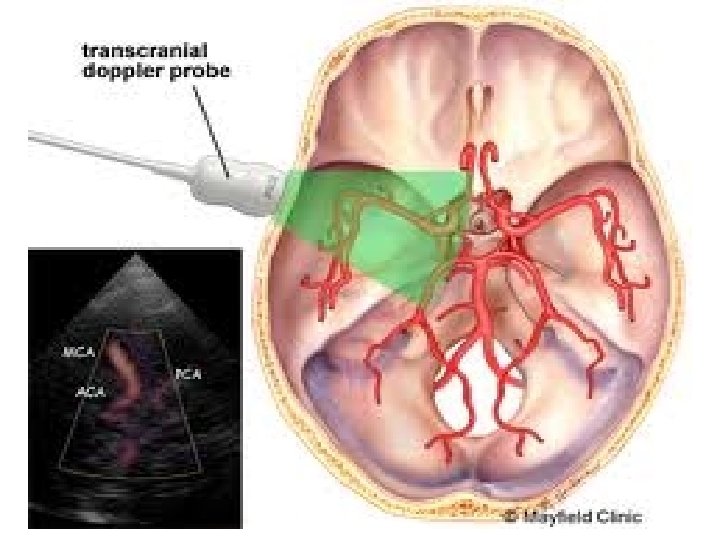
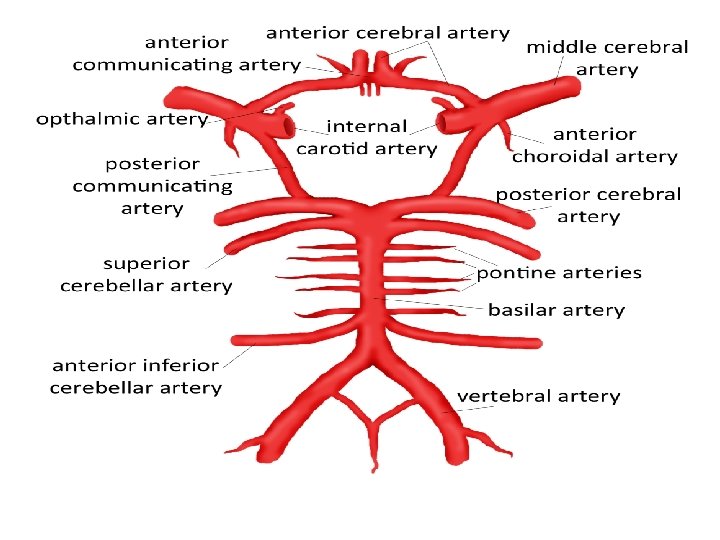
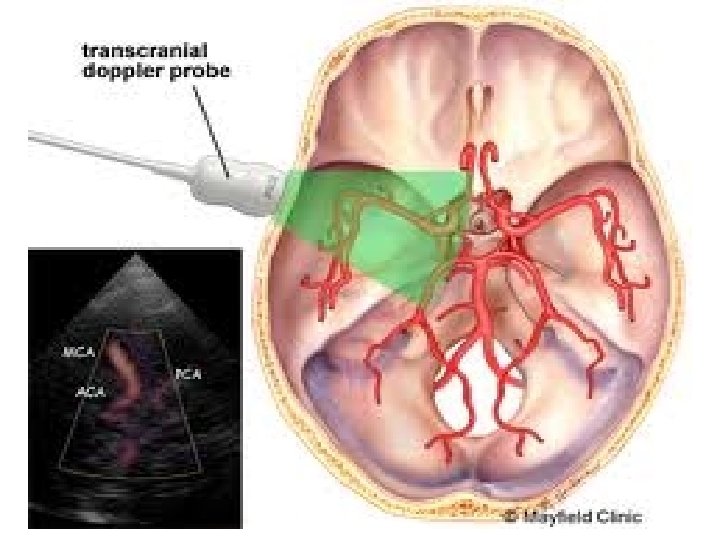
Large artery vasculopathy Vessels of the Circle of Willis, notably: • Internal carotid artery (ICA) • Middle cerebral artery (MCA) in 85% (training) • Anterior cerebral artery (ACA) Rarely, • Posterior cerebral artery (least likely, ≤ 1%) often not studied.
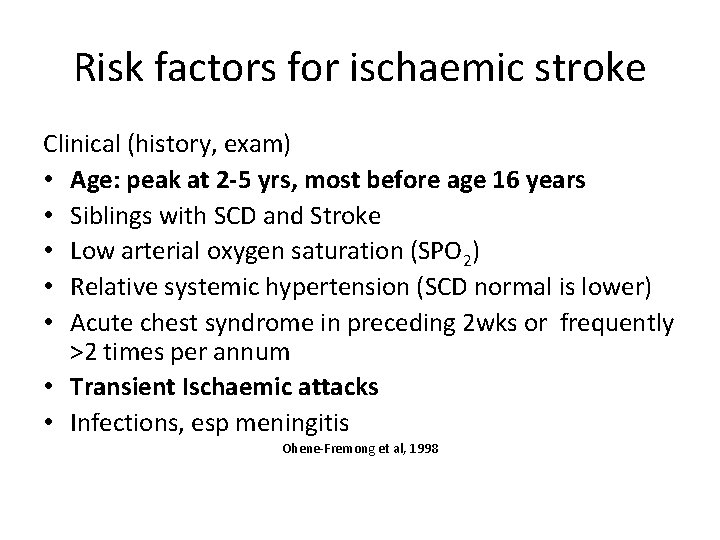
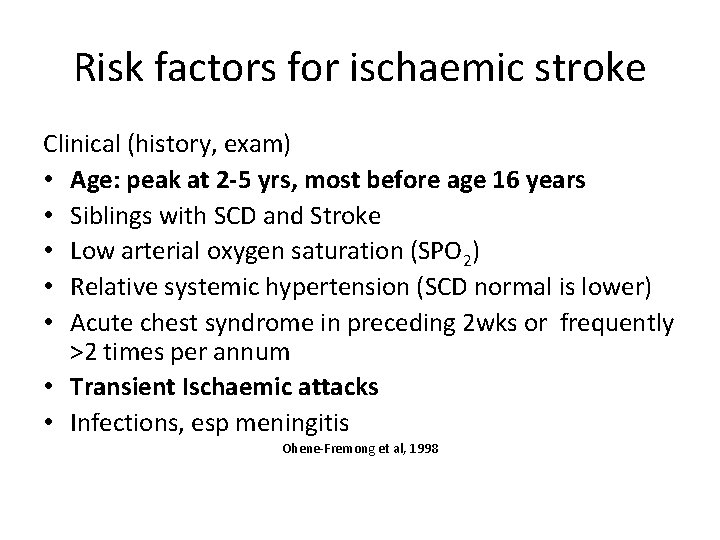
Risk factors for ischaemic stroke Clinical (history, exam) • Age: peak at 2 -5 yrs, most before age 16 years • Siblings with SCD and Stroke • Low arterial oxygen saturation (SPO 2) • Relative systemic hypertension (SCD normal is lower) • Acute chest syndrome in preceding 2 wks or frequently >2 times per annum • Transient Ischaemic attacks • Infections, esp meningitis Ohene-Fremong et al, 1998
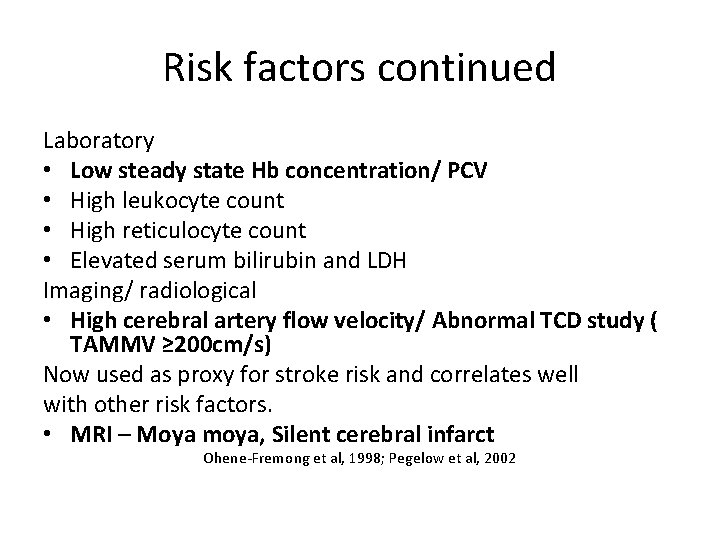
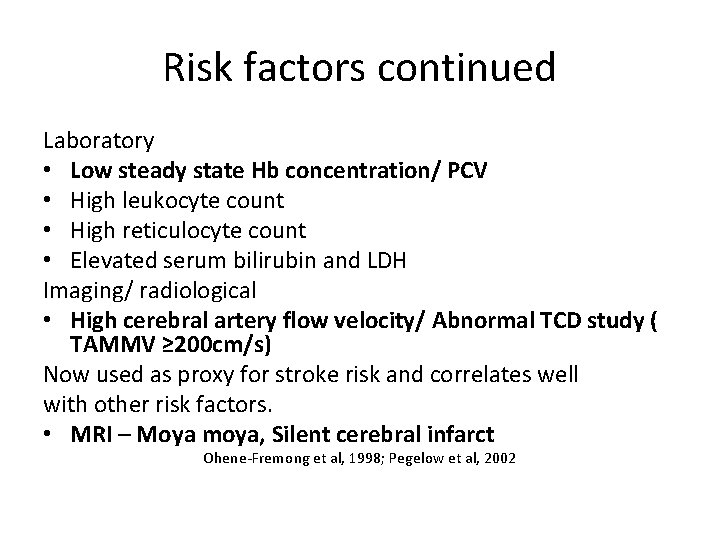
Risk factors continued Laboratory • Low steady state Hb concentration/ PCV • High leukocyte count • High reticulocyte count • Elevated serum bilirubin and LDH Imaging/ radiological • High cerebral artery flow velocity/ Abnormal TCD study ( TAMMV ≥ 200 cm/s) Now used as proxy for stroke risk and correlates well with other risk factors. • MRI – Moya moya, Silent cerebral infarct Ohene-Fremong et al, 1998; Pegelow et al, 2002
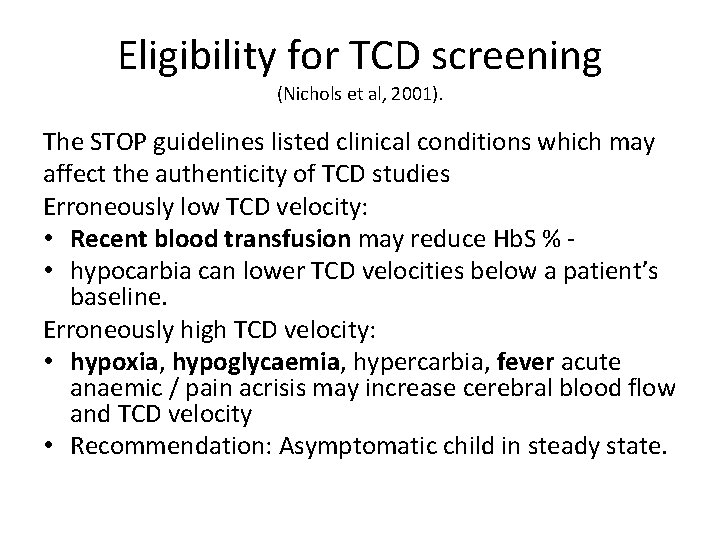
Eligibility for TCD screening (Nichols et al, 2001). The STOP guidelines listed clinical conditions which may affect the authenticity of TCD studies Erroneously low TCD velocity: • Recent blood transfusion may reduce Hb. S % • hypocarbia can lower TCD velocities below a patient’s baseline. Erroneously high TCD velocity: • hypoxia, hypoglycaemia, hypercarbia, fever acute anaemic / pain acrisis may increase cerebral blood flow and TCD velocity • Recommendation: Asymptomatic child in steady state.
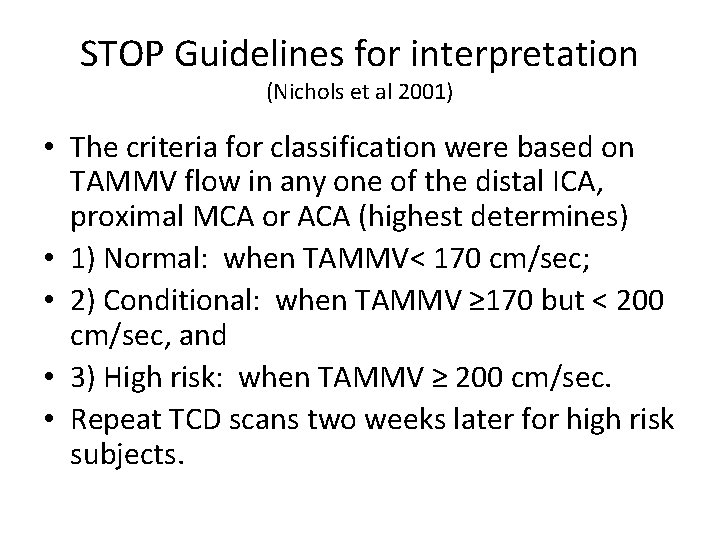
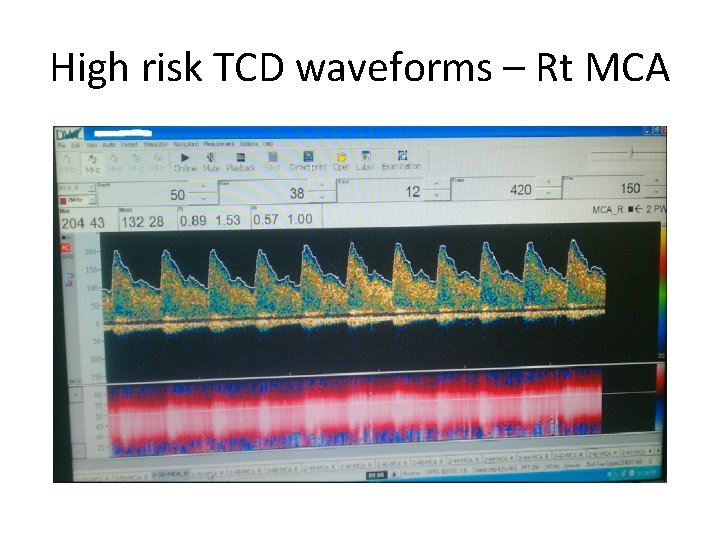
STOP Guidelines for interpretation (Nichols et al 2001) • The criteria for classification were based on TAMMV flow in any one of the distal ICA, proximal MCA or ACA (highest determines) • 1) Normal: when TAMMV< 170 cm/sec; • 2) Conditional: when TAMMV ≥ 170 but < 200 cm/sec, and • 3) High risk: when TAMMV ≥ 200 cm/sec. • Repeat TCD scans two weeks later for high risk subjects.
Interpretation of TCD • Highest TAMMV in any studied artery determines category • TAMMV ≥ 200 cm/s (high risk/ abnormal TCD)40% risk of stroke in 2 yrs • TAMMV ≥ 170 cm/s but < 199 cm/s (conditional risk) – 7% • standard 2% stroke risk as in the general SCD population was reported in children with TAMMV <170 cm/s (normal TCD) (Adams et al, 1997; Adams et al, 1998).
Interpretation contd • Subjects prone to overt stroke could also have a TAMMV <70 cm/s in their MCA velocity • Inadequate study despite adequate temporal window or A comparison of non-imaging TCD and MRI/ MRA suggest these findings are indicative of vasculopathy. • This category not included in STOP guidelines • Use to MRI/ MRA to confirm vascular stenosis before transfusions therapy is commenced (Adams et al, 1992; Seibert et al, 1993; Seibert et al, 1998).
Non-imaging TCD - Procedure • Well patient (steady state if possible) supine, awake and quiet, not sedated • 2 MHz ultrasound probe aligned with a specific cerebral artery blindly • via thin temporal bone (window) above the zygomatic arch - Temporal insonation window
Optimization The machine records and saves the TAMMV in the ICA, ACA and MCA at maximal sound pitch. For accuracy probe angle is adjusted manually & depth and penetration power of ultrasound waves adjusted by hand held remote Control until highest sound pitch is obtained diff for each vessel • The amplitude of the wave form measured & recorded on a screen over time correlates directly with the speed of the blood in cm/sec • Corresponds to time averaged maximum mean velocity (TAMMV)

TCD equipment

EQUIPMENT (CONTD)
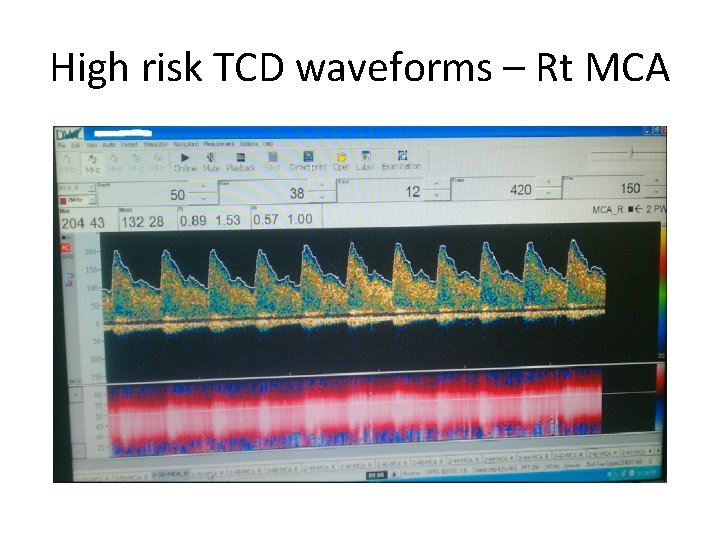
High risk TCD waveforms – Rt MCA
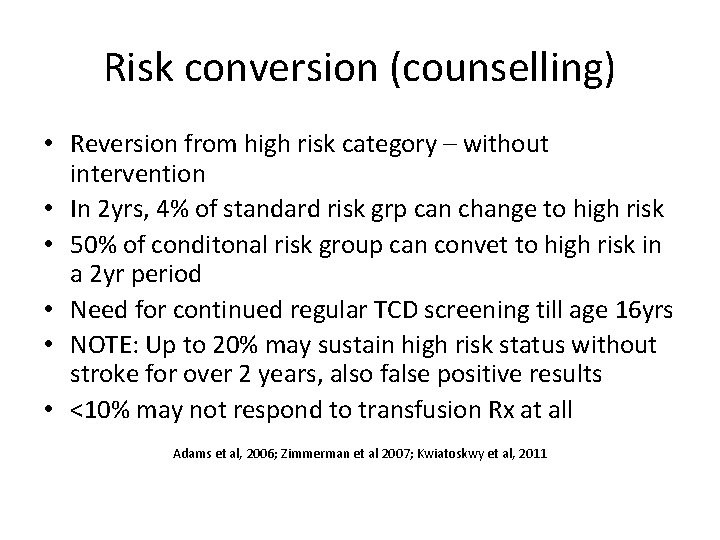
Risk conversion (counselling) • Reversion from high risk category – without intervention • In 2 yrs, 4% of standard risk grp can change to high risk • 50% of conditonal risk group can convet to high risk in a 2 yr period • Need for continued regular TCD screening till age 16 yrs • NOTE: Up to 20% may sustain high risk status without stroke for over 2 years, also false positive results • <10% may not respond to transfusion Rx at all Adams et al, 2006; Zimmerman et al 2007; Kwiatoskwy et al, 2011
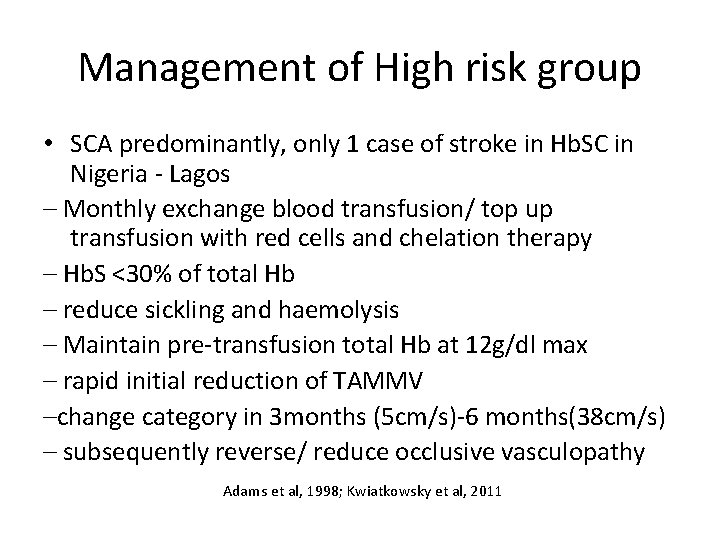
Management of High risk group • SCA predominantly, only 1 case of stroke in Hb. SC in Nigeria - Lagos – Monthly exchange blood transfusion/ top up transfusion with red cells and chelation therapy – Hb. S <30% of total Hb – reduce sickling and haemolysis – Maintain pre-transfusion total Hb at 12 g/dl max – rapid initial reduction of TAMMV –change category in 3 months (5 cm/s)-6 months(38 cm/s) – subsequently reverse/ reduce occlusive vasculopathy Adams et al, 1998; Kwiatkowsky et al, 2011
Ischaemic stroke prevention • Transcranial Doppler Ultrasound identifies asymptomatic high risk patients in children 216 yrs old (epidemiology, co-operation, temporal insonation window) • Pre- an post-TCD counselling • Chronic episodic red cell transfusion prevents up to 90% of initial ischaemic strokes • Hydroxyurea (HU)/ Hydroxycarbamide
Update of management of high stroke risk • Hydroxyurea (HU)/ Hydroxycarbamide escalated to maximal tolerable dose (MTD) Works and very useful, • trials underway for exact figures, • Galadanci et al, 2016 -acceptable & efficacious. • Ware et al, 2016 - HU vs. Chr Transf Tx Nichols et al, 2001 – STOP guidelines for stroke risk assessment and primary stroke prevention
Stopping blood transfusions (counselling) STOP 2 trial to determine at when to stop bld Tx and SWi. TCH trial – stop blood Hydroxyurea – high stroke rate, death – overwhelming evidence of adverse outcome – trial discontinued prematurely These were RCTs. Recommendation remains – continue blood Tx till at least age 16 -18 yrs. Adams et al, 2005; Ware et al, 2004
Stopping Blood transfusion: 2016 update • For high-risk children with sickle cell anaemia and abnormal TCD velocities who have received at least 1 year of transfusions, and have no MRA-defined severe vasculopathy, hydroxycarbamide treatment can substitute for chronic transfusions to maintain TCD velocities and help to prevent primary stroke. – Ware et el, 2016 1 yr OVERLAP of both red cell transfusions & HU
Stroke risk assessment in Nigeria Standard practice in UK, USA, some other SCD burdened countries. Stroke risk assessment & chronic blood transfusion has drastically reduced America’s childhood SCD stroke rate Efforts to standardize SCD care underway in Nigeria • Not available in most dedicated SCD clinics in Nigeria • Relatively new to Nigeria, not practiced routinely Standard stroke risk assessment resources – SCD – 3 places in Nigeria (Sickle cell Foundation, Idia-Araba, Gbagada General hospital both in Lagos & UCH Ibadan) Fullerton, 2004; Galadanchi et al, 2013
Non- imaging TCD Studies in South west Nigeria High risk patients to STOP guidelines using similar equipment and protocol: • 4. 7% - 8% in Ibadan – Lagunju et al, 2011, 2013. • 9. 6% - Ojewumi & Adeyemo et al 2016, • 9. 8%–, Diaku-Akinwumi et al, & 11% in Lagos Adekunle & Diaku-Akinwumi et al • Blood transfusion not acceptable/ sustainable All studies • Conditional risk – 20% and • Majority are standard risk ≥ 70%
Caution! • Interpretations discussed are for NON-IMAGING TCD - quick procedure with portable , relatively inexpensive TCD unit - easy to teach non-clinical staff in few days, skills improve with time • IMAGING TCD using a colour Doppler machine - can be achieved with most standard ultrasound equipment if performed by an expert - visualizes and identifies vessels more confidently BUT - expensive machines with larger transducers-not suitable for small temporal windows of children. Bullas, 2005; Padayachee et al, 2011
Caution! continued RCTs were with age 2 -16 yrs, using non-imaging TCD – Imaging and non-imaging TCD correlate well BUT Results (actual cerebral flow velocity figures) are NOT interchangeable – no known formula to interconvert yet Padayachee et al, 2011
APPEAL 1. SEEK TO GET TCD MACHINES & EXPERTISE • POLITICAL WILL • FUNDING 2. SEEK ALTERNATIVE WAYS
Thank you for listening