Hypertrophic Cardiomyopathy Ahmad Yousre Msc cardiology Hypertrophic Cardiomyopathy











- Slides: 48
Hypertrophic Cardiomyopathy Ahmad Yousre Msc cardiology

Hypertrophic Cardiomyopathy
Definition: WHO: left and/or right ventricular hypertrophy, usually asymmetric and involves the interventricular septum.
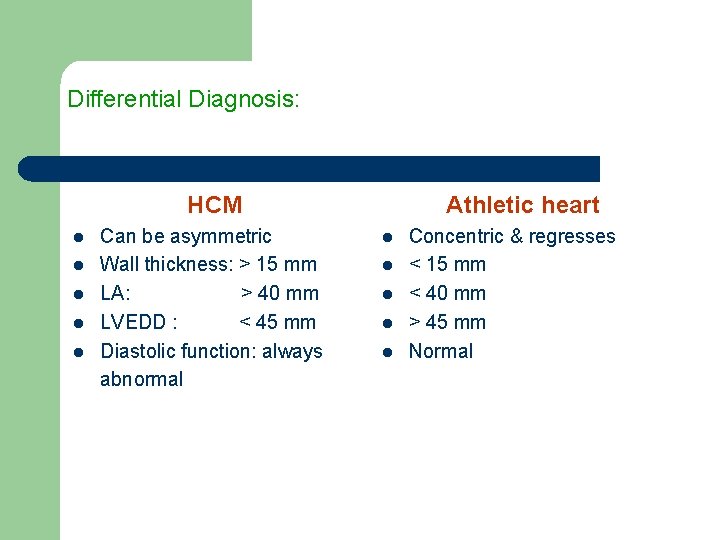
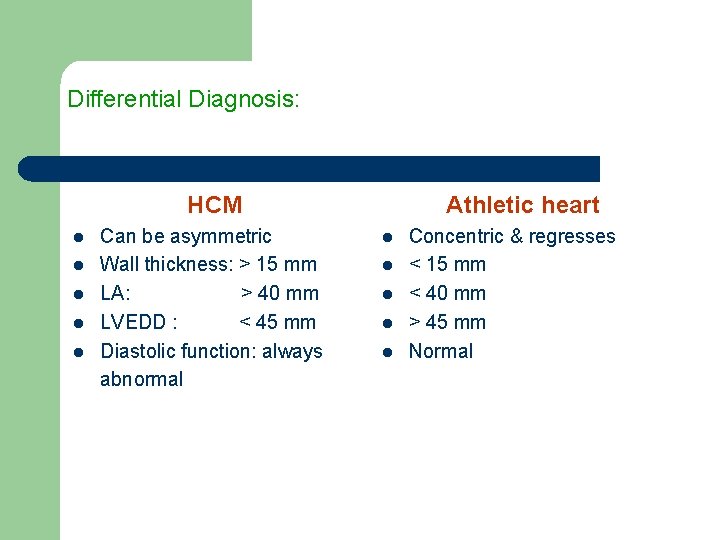
Differential Diagnosis: HCM l l l Can be asymmetric Wall thickness: > 15 mm LA: > 40 mm LVEDD : < 45 mm Diastolic function: always abnormal Athletic heart l l l Concentric & regresses < 15 mm < 40 mm > 45 mm Normal
Stimulus: l l Unknown Disorder of intracellular calcium metabolism Neural crest disorder Papillary muscle malpositioned and misoriented
Genetic abnormality: l l Autosomal dominant. Mutations in genes for cardiac sarcomeric proteins. Polymorphism of ACE gene. ß-myosin heavy chain gene on chromosome 14.
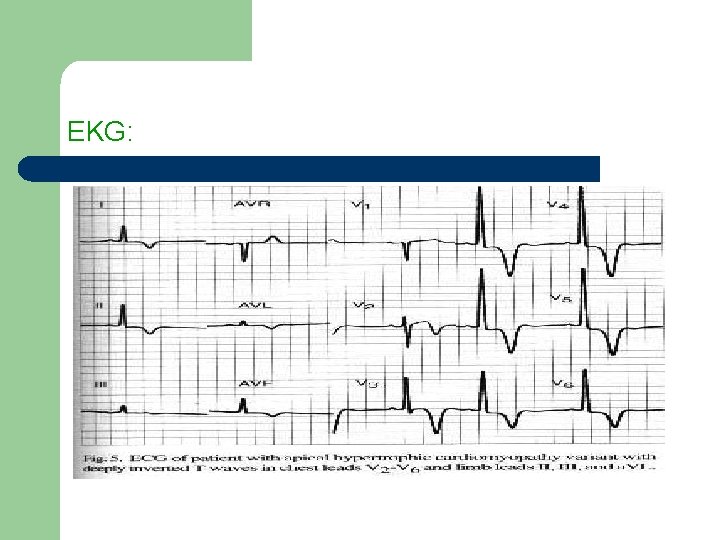
Most common Variants of location: HCM: subaortic , septal, and ant. wall. l Asymmetric hypertrophy (septum and ant. wall): 70 %. l Basal septal hypertrophy: 15 - 20 %. l Concentric LVH: 8 -10 %. l Apical or lateral wall: < 2 % (25 % in Japan/Asia): characteristic giant T-wave inversion laterally & spade-like left ventricular cavity: more benign.

Hypertensive hypertrophic Cardiomyopathy l l l Elderly women Simulates HCM Prognosis better than non-hypertensive HCM
Pathophysiology of HCM l l l Dynamic LV outflow tract obstruction Diastolic dysfunction Myocardial ischemia Mitral regurgitation Arrhythmias
Left ventricular outflow tract gradient l ↑ with decreased preload, decreased afterload, or increased contractility. l Venturi effect: anterior mitral valve leaflets & chordae sucked into outflow tract → ↑ obstruction, eccentric jet of MR in mid-late systole. l
Maneuvers that ↓ end-diastolic volume (↓ venous return & afterload, ↑ contractility) l Vasodilators l Inotropes l Dehydration l Valsalva l Amyl nitrite l Exercise → ↑ HCM murmur

Arrhythmias: l Sustained V-Tach and V-Fib: most likely mechanism of syncope/ sudden death. l Dependant on atrial kick: CO ↓ by 40 % if A. Fib present.
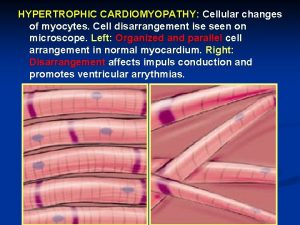
Histology: l l l Myocardial fiber disarray, endocardial plaques. Abnormal relaxation and diversely oriented myocardial fibers. Intimal hyperplasia of intramural coronary arteries, endothelial dysfunction, myocardial perfusion defects.
Clinical presentation: l l l Any age Leading cause of sudden death in competitive athletes Triad: DOE, angina, presyncope/syncope.


Physical exam: l l l l Apex localized, sustained Palpable S 4 Tripple Prominent “a” wave Rapid upstroke carotid pulse, “jerky” bifid (spike-anddome pulse) Harsh systolic ejection murmur across entire precordium → apex & heart base MR: separate murmur: severity of MR related to degree of outflow obstruction
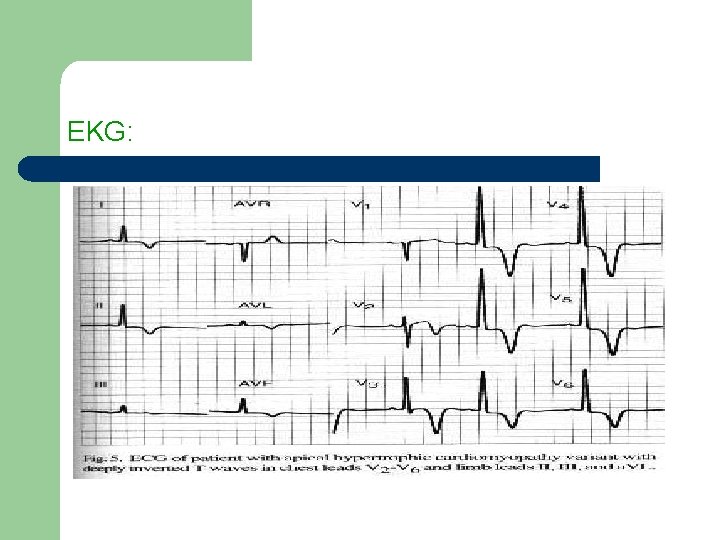
EKG:
Echocardiography: 2 D-echo: l Asymmetric septal hypertrophy l Diffuse concentric or localized to apex/anterior wall l Systolic anterior motion of MV (SAM)
Doppler Echocardiocraphy: l Typical appearance: late-peaking signal “dagger-shaped” l Bernoulli for peak systolic gradient (+ maneuvers) l Obstructive or non-obstructive l Distinguish MR and intra-cavitary obstruction (looking for the aortic closure signal)


Cardiac cath: l Not necessary
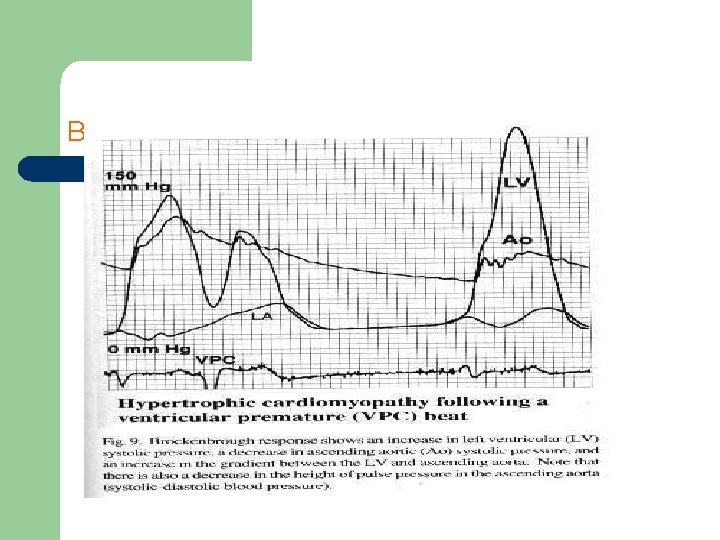
Brockenbrough response l l l ↑ LV systolic pressure ↓ Ao systolic pressure ↑ gradient between LV & Ao Post PVC
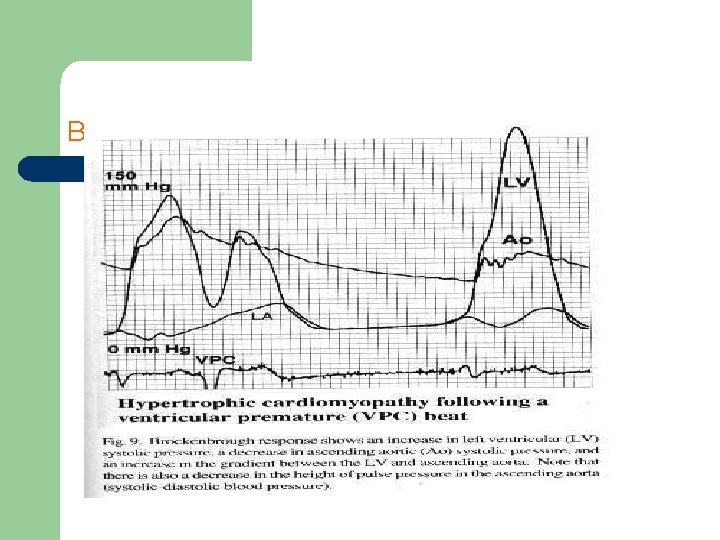
Brockenbrough response

Imitator of HCM Amyloidosis: Thickened walls & low voltage on EKG. l
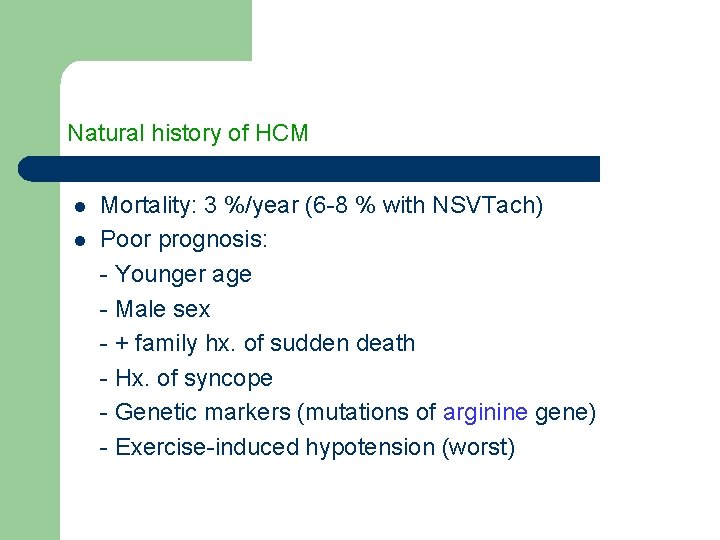
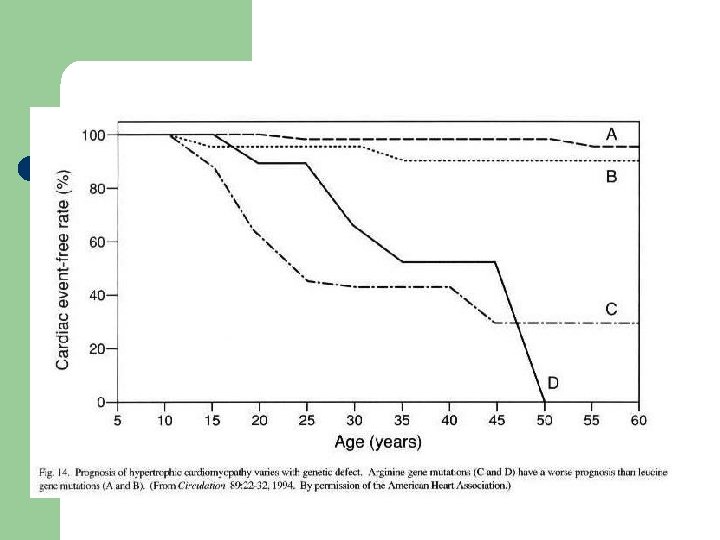
Natural history of HCM l l Mortality: 3 %/year (6 -8 % with NSVTach) Poor prognosis: - Younger age - Male sex - + family hx. of sudden death - Hx. of syncope - Genetic markers (mutations of arginine gene) - Exercise-induced hypotension (worst)

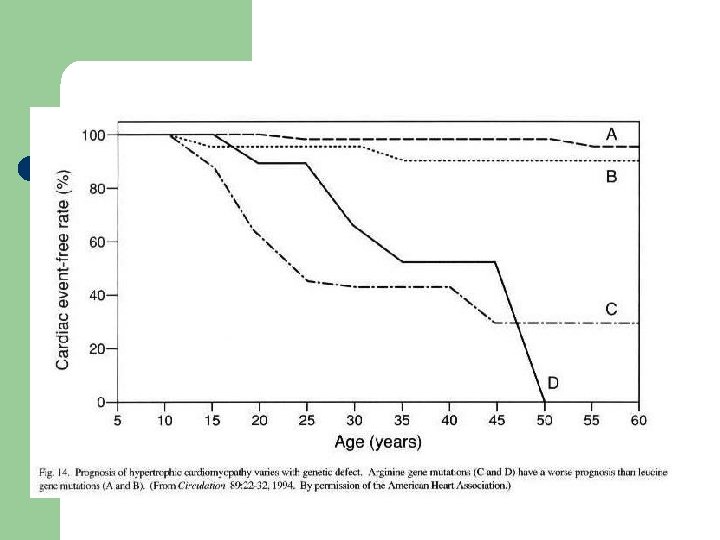
Genetic defect and prognosis
Management l l All first degree relatives: screening… echocardiography/genetic counseling Avoid competitive athletics Prophylactic antibiotics before medical & dental procedures Holter x 48 hours
β- Blockers: Propranolol 200 -400 mg/d (large doses)/ Selective β- B lose selectivity at high doses: Slow HR → longer diastolic filling time → ↓ myocardial O 2 consumption → ↓ myocardial ischemia & LVOT obstruction l Ca. Ch- Blockers: Verapamil 240 -320 mg/d (with caution for hemodynamic deterioration) l Combination of both l
l Disopyramide: class I antiarrhythmic + strong –ive inotropic effect
Non-responders to Medical therapy ? ? ? 1 - Surgery (Myotomy/Myectomy) +/- MVR 2 - ICD 3 - DDD pacemaker 4 - NSRT (alcohol septal ablation)
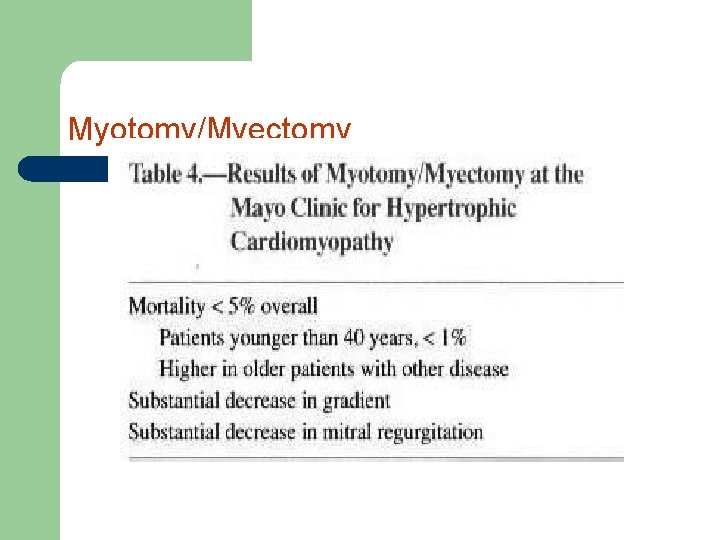
1 - Surgery: Septal myotomy/myectomy: l Patients < 40 years: mortality < 1 % l Patients > 65 years: mortality 10 -15 % l Survival better than medically treated patients l Should be considered in: resting gradient > 50 mm. Hg, or refractory to medical Rx. l Young patients, particularly those with severe disease l Additional structural abnormalities affecting the mitral valve or coronary arteries. l Complication (rare): Aortic incompetence
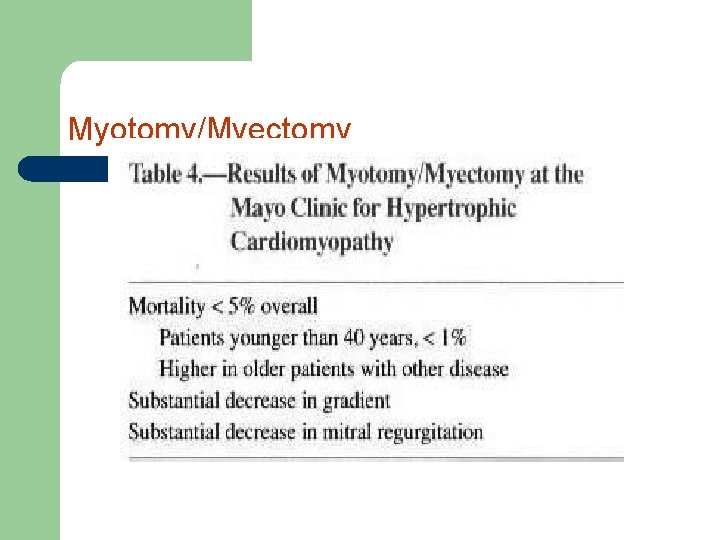
Myotomy/Myectomy
2 - ICD: l l l Previous sudden death High risk of sudden death EPS use ?
3 - DDD pacemaker Substantial ↓ gradient(~ 50 %)
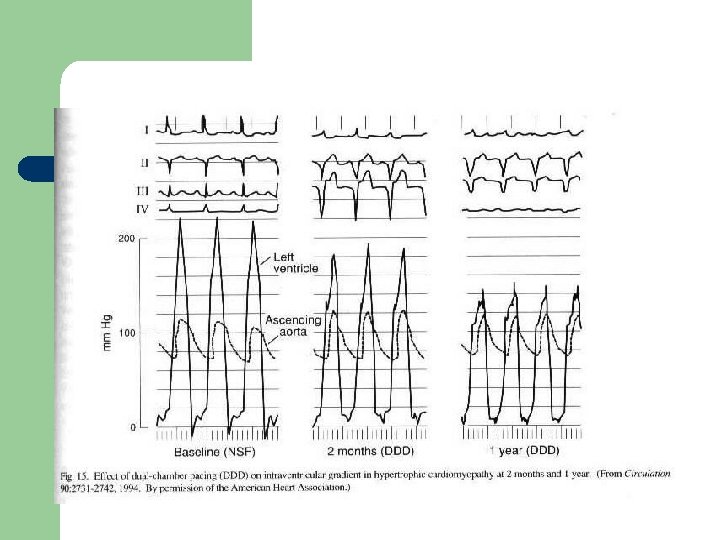
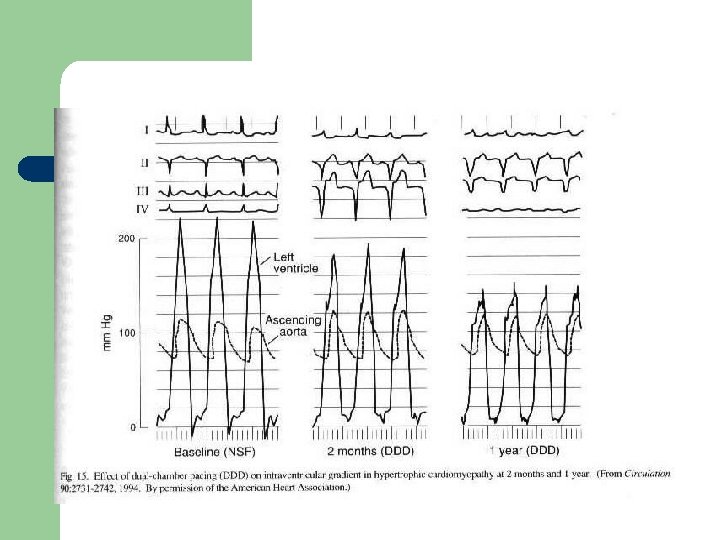
Effect of DDD pacemaker in HCM

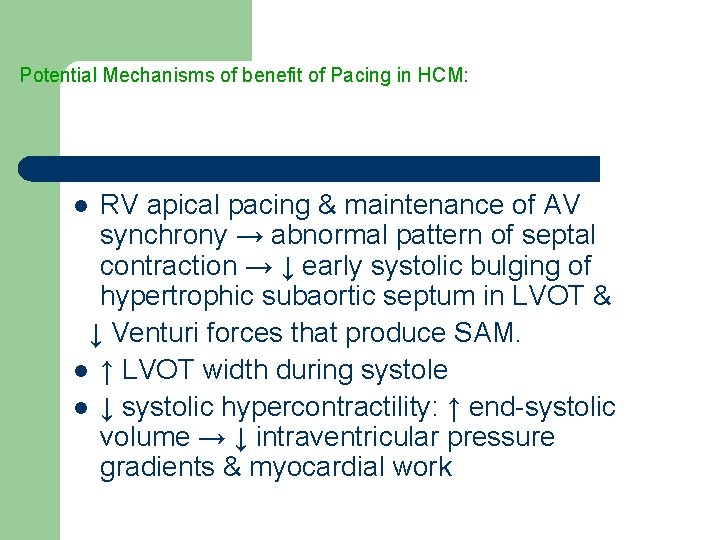
Potential Mechanisms of benefit of Pacing in HCM: RV apical pacing & maintenance of AV synchrony → abnormal pattern of septal contraction → ↓ early systolic bulging of hypertrophic subaortic septum in LVOT & ↓ Venturi forces that produce SAM. l ↑ LVOT width during systole l ↓ systolic hypercontractility: ↑ end-systolic volume → ↓ intraventricular pressure gradients & myocardial work l
l l l ↓ MR May favorably alter diastolic function LVH regression
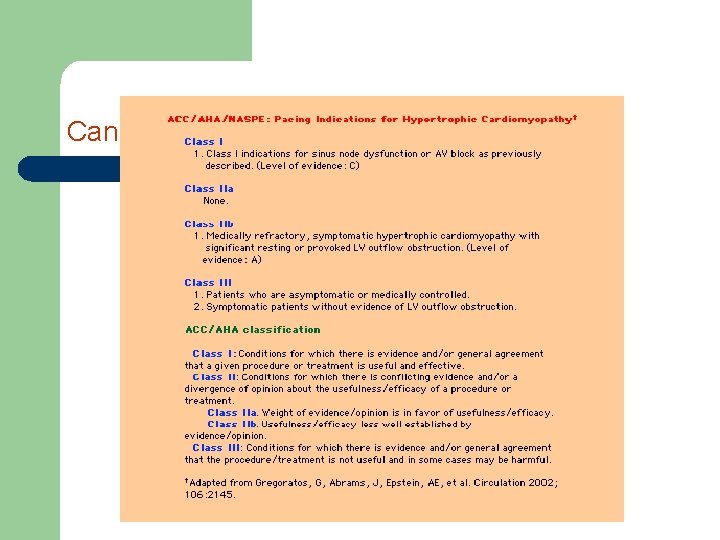
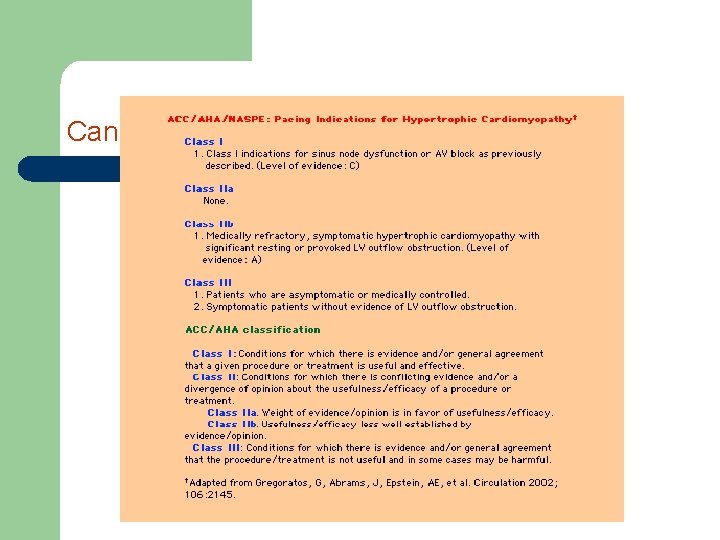
Candidates for DDD
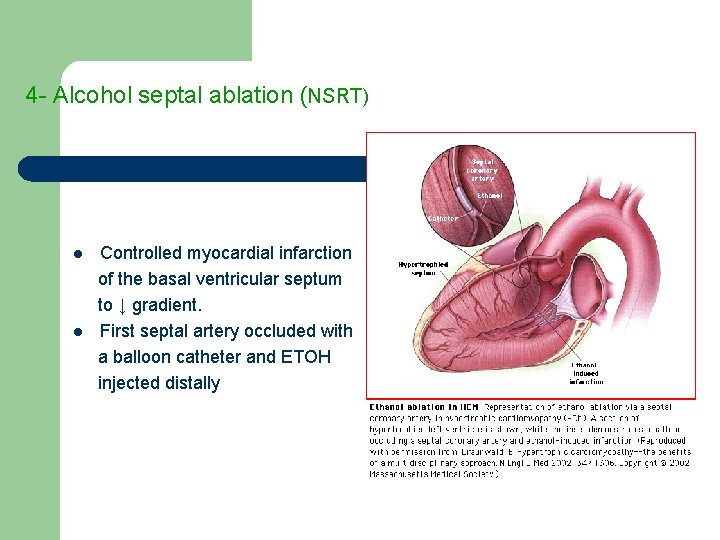
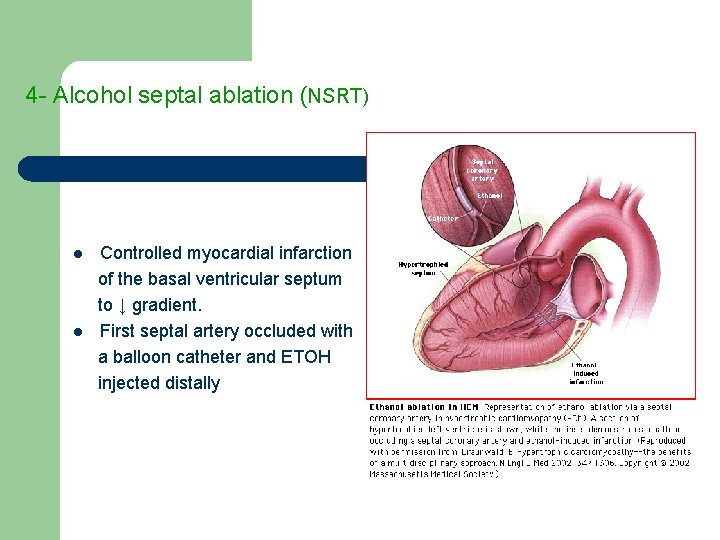
4 - Alcohol septal ablation (NSRT) l l Controlled myocardial infarction of the basal ventricular septum to ↓ gradient. First septal artery occluded with a balloon catheter and ETOH injected distally
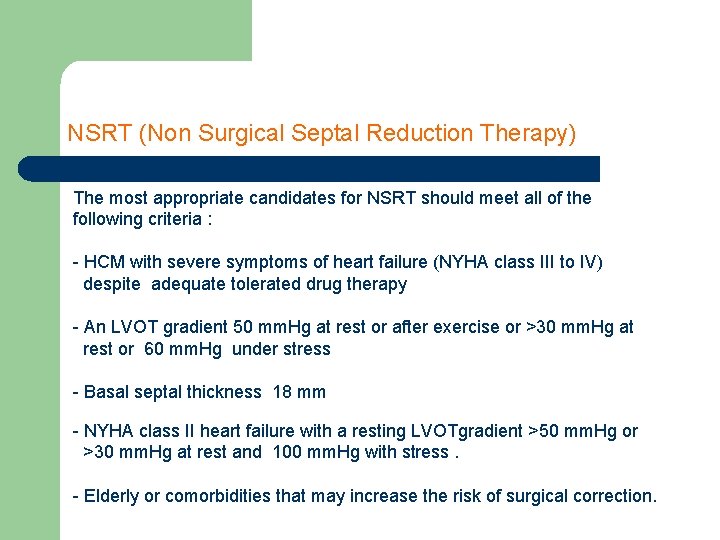
NSRT (Non Surgical Septal Reduction Therapy) The most appropriate candidates for NSRT should meet all of the following criteria : - HCM with severe symptoms of heart failure (NYHA class III to IV) despite adequate tolerated drug therapy - An LVOT gradient 50 mm. Hg at rest or after exercise or >30 mm. Hg at rest or 60 mm. Hg under stress - Basal septal thickness 18 mm - NYHA class II heart failure with a resting LVOTgradient >50 mm. Hg or >30 mm. Hg at rest and 100 mm. Hg with stress. - Elderly or comorbidities that may increase the risk of surgical correction.

Thank you
 Feline
Feline Dilated cardiomyopathy dog
Dilated cardiomyopathy dog Icd 10 eksim
Icd 10 eksim Hypertrophic obesity definition
Hypertrophic obesity definition Hypertrophic pyloric stenosis
Hypertrophic pyloric stenosis Eczema icd 10
Eczema icd 10 Craig ainsworth cardiology
Craig ainsworth cardiology Cardiology procedures chapter 47
Cardiology procedures chapter 47 Structured reporting cardiology
Structured reporting cardiology Dr nick gall cardiologist
Dr nick gall cardiologist Hall-garcia cardiology associates
Hall-garcia cardiology associates Accp cardiology prn
Accp cardiology prn Accp cardiology prn journal club
Accp cardiology prn journal club Muse cardiology
Muse cardiology Westcliffe cardiology service
Westcliffe cardiology service Enloe cardiology
Enloe cardiology Acc sports cardiology
Acc sports cardiology Elias hanna cardiology
Elias hanna cardiology Clinical documentation improvement for cardiology
Clinical documentation improvement for cardiology Justin davies md
Justin davies md Service line management in healthcare
Service line management in healthcare Msc finance and banking tor vergata
Msc finance and banking tor vergata Msc eir
Msc eir Jma msc
Jma msc Msc pelago
Msc pelago Nsozvn
Nsozvn Scan barcode msc
Scan barcode msc Msc
Msc Phsc in erythropoiesis
Phsc in erythropoiesis Msc direccionamiento
Msc direccionamiento Ship construction file
Ship construction file Plasmin
Plasmin Dynamic positioning classes
Dynamic positioning classes Grenoble msc finance
Grenoble msc finance Solid-state lighting (ssl)
Solid-state lighting (ssl) Struktur msc
Struktur msc Rna transfer
Rna transfer Msc
Msc Meteorological satellite center of jma
Meteorological satellite center of jma Msc circular 1206
Msc circular 1206 Msc sandra
Msc sandra Medgulf msc
Medgulf msc Msc.252(83)
Msc.252(83) 7 aplikasi perdana msc
7 aplikasi perdana msc Msc olga
Msc olga Msc rini iii
Msc rini iii Um interface in gsm
Um interface in gsm Humánkineziológia msc
Humánkineziológia msc Actuarial management
Actuarial management