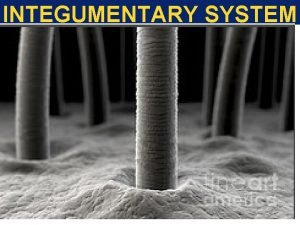
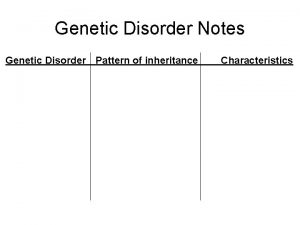
GENETIC DISORDER Integumentary System INTEGUMENTARY SYSTEM DISORDERS Is











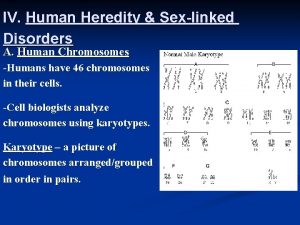
- Slides: 94

GENETIC DISORDER Integumentary System
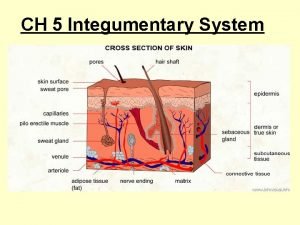
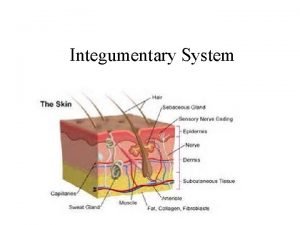
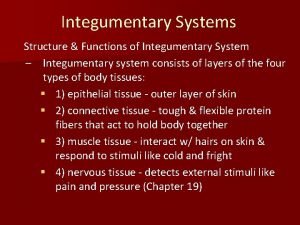
INTEGUMENTARY SYSTEM DISORDERS • Is a disorder affecting the skin • Skin is largest organ in the body
ALBINISM • A genetic disorder in which there is complete or partial congenital absence of pigment in the skin, hair, and eyes. • Is found in all races • The most common type is recessively inherited oculocutaneous albinism
2 BROAD CATEGORIES 1. Oculocutaneous (OCA) (absence in pigments in hair, eyes and skin) • Tyrosinase (+) • Tyrosinase (-) 2. Ocular (absence of pigments within the eyes) • Subtypes • Autosomal Recessive • Sex-linked Recessive
ALBINISM • Incidence • Rare Disorder • 1 in 40, 000 (Oculocutaneous) • 1 in 15, 000 males (ocular) • Less common in females X-linked; most females are carriers • Risk Factors • Permanent poor vision • Heightened risk of skin cancer • Etiology • Caused by the inheritance of homozygous recessive allele
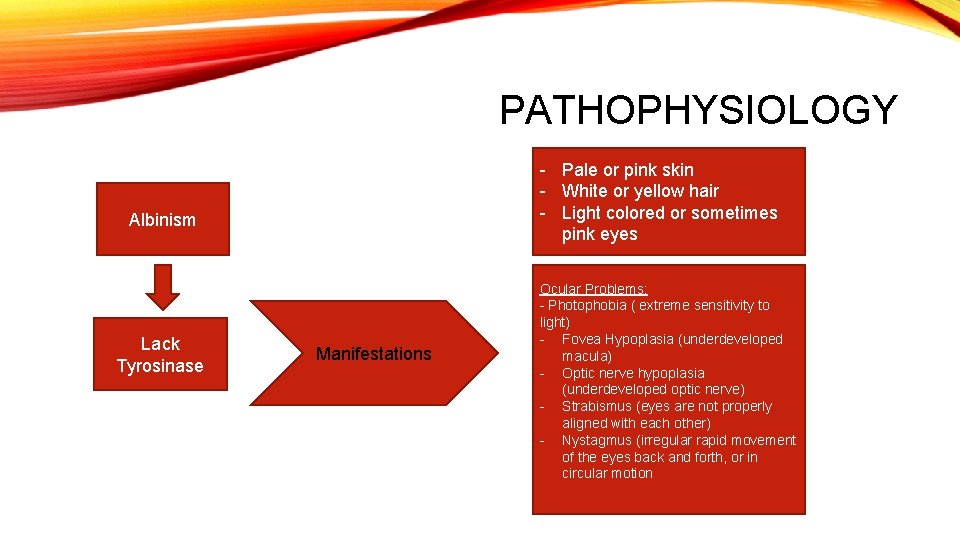
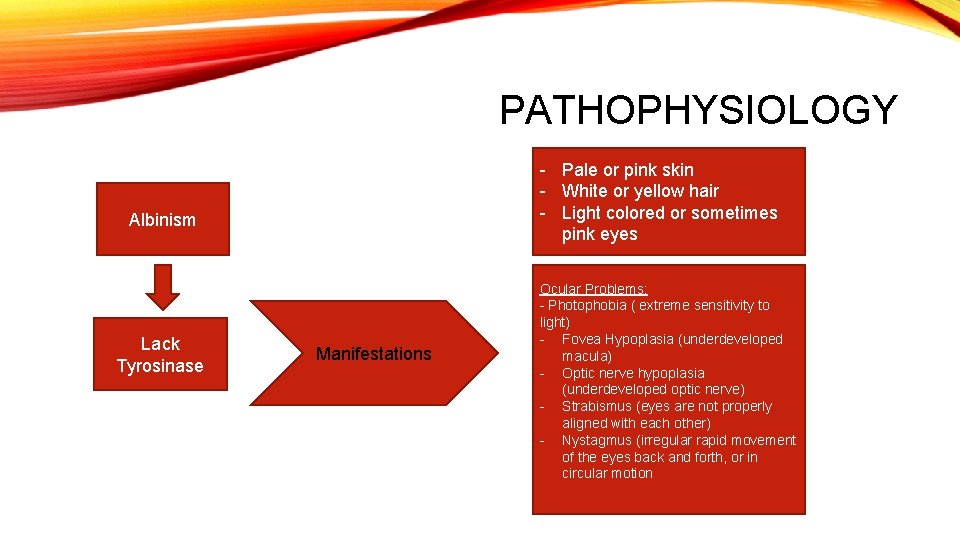
PATHOPHYSIOLOGY - Pale or pink skin - White or yellow hair - Light colored or sometimes pink eyes Albinism Lack Tyrosinase Manifestations Ocular Problems: - Photophobia ( extreme sensitivity to light) - Fovea Hypoplasia (underdeveloped macula) - Optic nerve hypoplasia (underdeveloped optic nerve) - Strabismus (eyes are not properly aligned with each other) - Nystagmus (irregular rapid movement of the eyes back and forth, or in circular motion
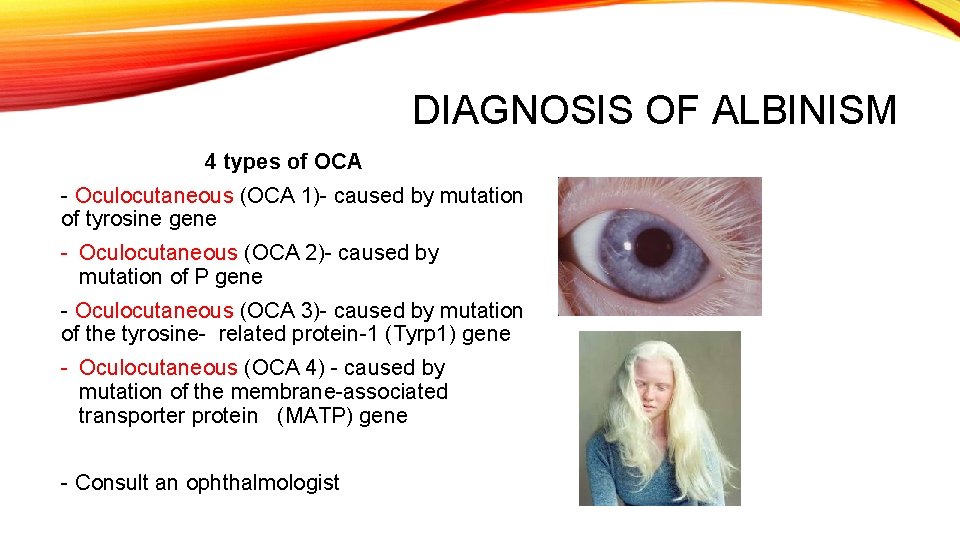
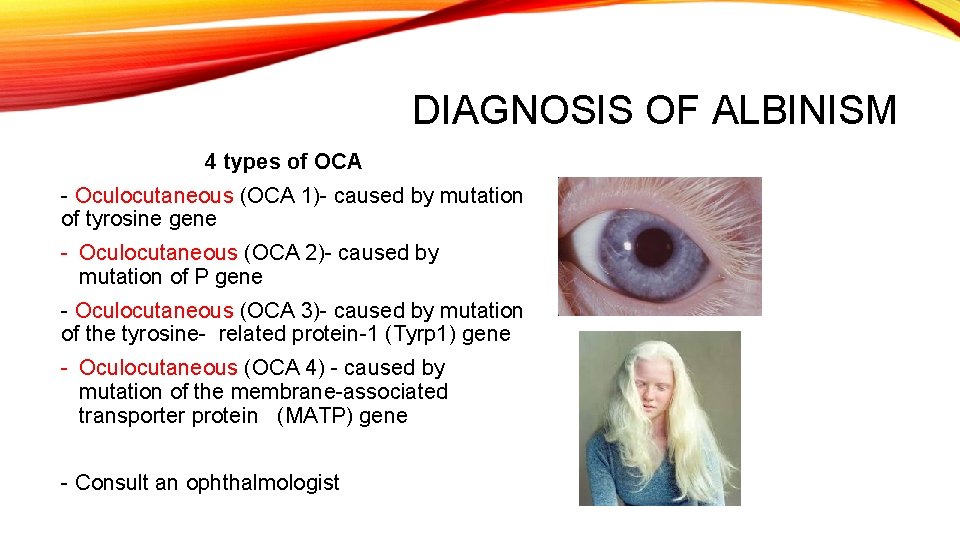
DIAGNOSIS OF ALBINISM 4 types of OCA - Oculocutaneous (OCA 1)- caused by mutation of tyrosine gene - Oculocutaneous (OCA 2)- caused by mutation of P gene - Oculocutaneous (OCA 3)- caused by mutation of the tyrosine- related protein-1 (Tyrp 1) gene - Oculocutaneous (OCA 4) - caused by mutation of the membrane-associated transporter protein (MATP) gene - Consult an ophthalmologist
PREVENTION • Cannot be prevented • Incurable • Avoid sunlight • Cover up when going outdoors • Use Sun Protection Factor, (SPF) 30 or greater
TREATMENT • Reduced their risk for skin cancer through protection from solar radiation and screening for malignant changes. • Efforts to reduce the visual impact are important, such as glasses, preferential setting in classrooms and large- print books.
NURSING DIAGNOSIS • Ineffective Coping related to chronic condition • Body Image Disturbance related to pale or white skin brought about by absence of melanin pigment • Risk for Activity Intolerance: Poor Vision related to alterations in nerve connections between the retina and brain brought about by absence of melanin pigment • Risk for impaired skin integrity related to absence of melanin pigment

ICHTHYOSIS VULGARIS • also known as "Autosomal dominant ichthyosis, " and "Ichthyosis simplex“ or a fish scale disease • is a skin disorder causing dry, scaly skin. • It is the most common form of ichthyosis affecting around 1 in 250 people. • For this reason it is known as common ichthyosis. • It is usually an autosomal dominant inherited disease
PRESENTATION • Not present at birth but generally develop between 3 months and 5 years of age • Often improve with age but grow more severe in old age. • Not life threatening • Mild cases • scaly patches on the shins, fine white scales on the forearms and upper arms, and rough palms
SEVERE CASES • build up of scales everywhere • Less affected areas: • areas of the body that have a concentration of sweat glands • Areas where the skin rubs against each other • armpits, the groin • "folded" areas of the elbow and knees • When the build up of scales is bad, the person with a severe case suffers from "prickly itch" when he or she needs to sweat but cannot because of the scales.
CAUSES • autosomal dominant pattern, • meaning that only one parent needs to possess the mutated gene in order to pass it onto his or her child. • caused by mutations to the gene encoding profilaggrin • a protein which is converted to filaggrin which plays a vital role in the structure of the skin.
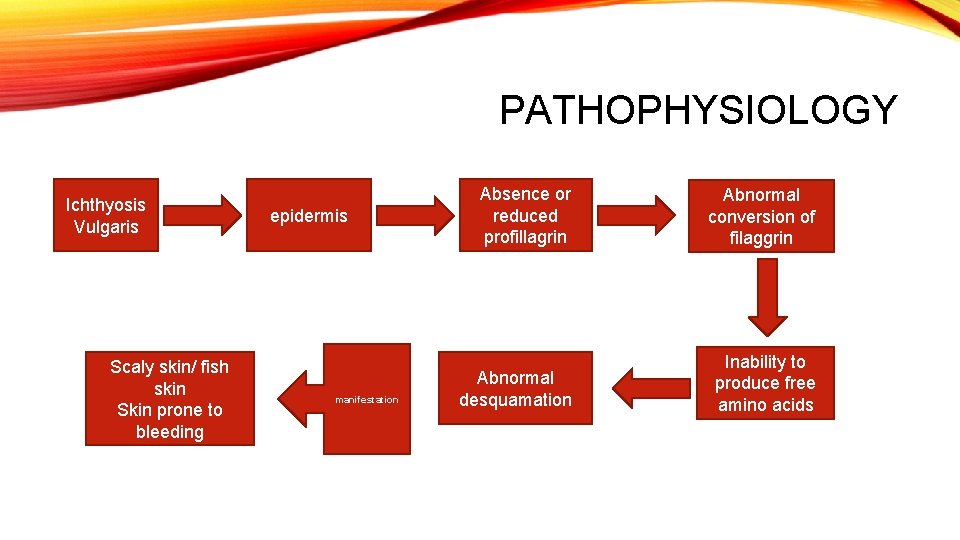
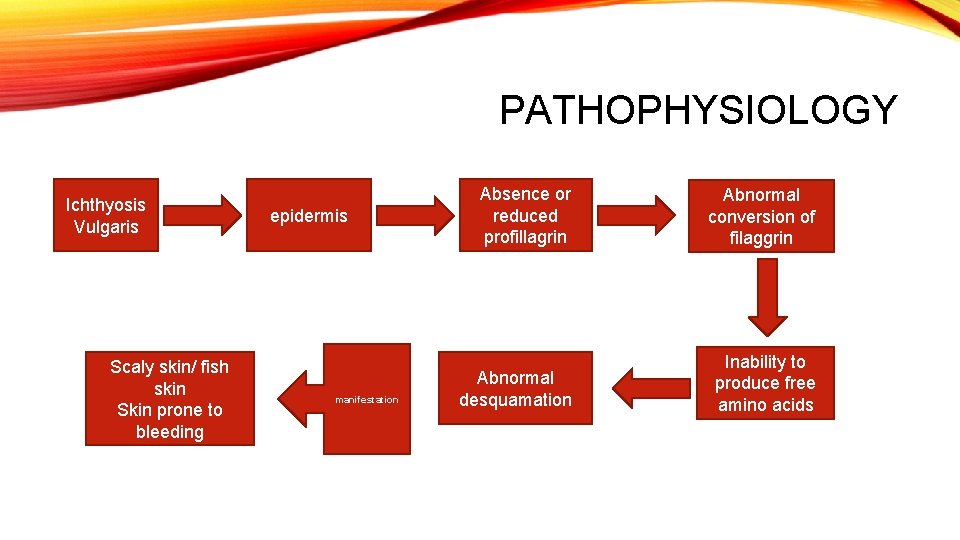
PATHOPHYSIOLOGY Ichthyosis Vulgaris Scaly skin/ fish skin Skin prone to bleeding epidermis manifestation Absence or reduced profillagrin Abnormal conversion of filaggrin Abnormal desquamation Inability to produce free amino acids
DIAGNOSIS • A dermatologist —a doctor specializing in skin disorders can typically diagnose ichthyosis vulgaris by sight. • Your doctor will ask you about; • family history of skin diseases, • the age you first experienced symptoms, • whether you suffer from any other skin disorders

TREATMENT • Various topical treatments are available to "exfoliate" the scales. • These include lotions that contain alpha-hydroxy acids.
COPING • Living with ichthyosis vulgaris and similar skin conditions is difficult at times, especially for children. • If the cosmetic impact of the condition becomes too much, you may want to attend a support group or see a mental health professional. • These therapies can help you to regain your confidence and deal with any emotional difficulties you may encounter.

NURSING DIAGNOSIS • Impaired Skin Integrity related to scaly skin • Risk for Self-care Deficit related to bleeding tendencies • Body Image Disturbance related to body skin appearance • Risk for Ineffective Coping related to chronic condition

RESPIRATORY SYSTEM
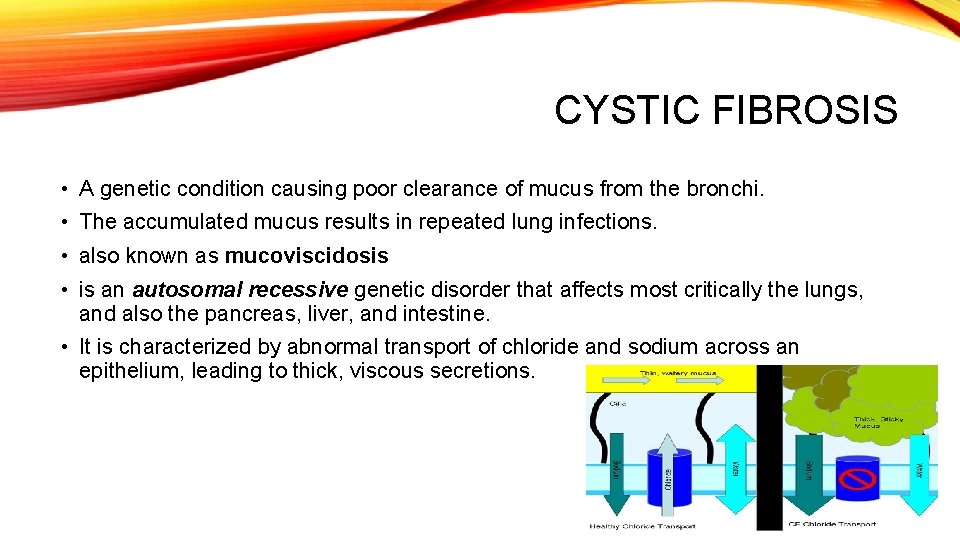
CYSTIC FIBROSIS • A genetic condition causing poor clearance of mucus from the bronchi. • The accumulated mucus results in repeated lung infections. • also known as mucoviscidosis • is an autosomal recessive genetic disorder that affects most critically the lungs, and also the pancreas, liver, and intestine. • It is characterized by abnormal transport of chloride and sodium across an epithelium, leading to thick, viscous secretions.
GENETIC EXPLANATION • Mutation in the CFTR gene on chromosome 7 • Encodes a protein known as the cystic fibrosis transmembrane regulator • Abnormal proteins leads to disruption of chloride on the cells. Remember: CFTR= C- cystic, F- fibrosis, T- transmembrane, Rregulator - Genes mutated in cystic fibrosis
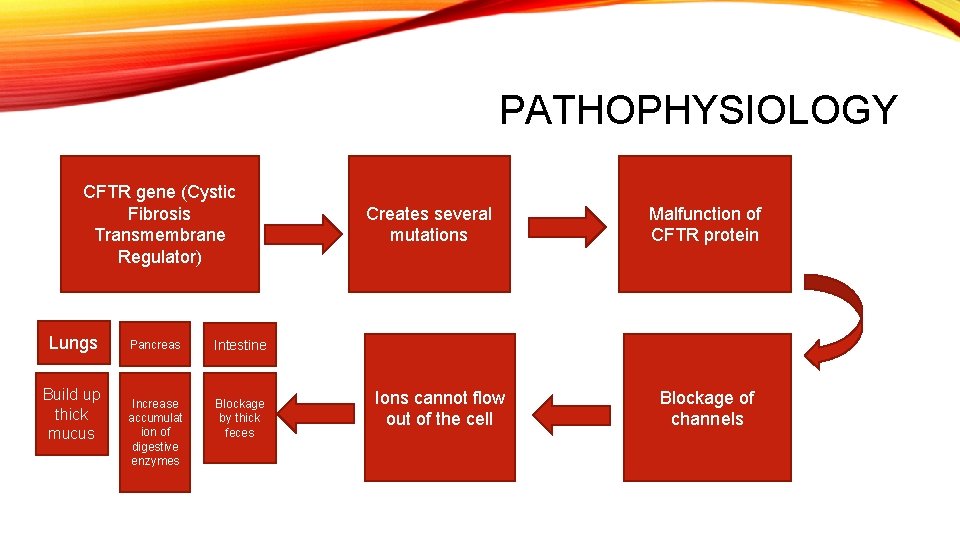
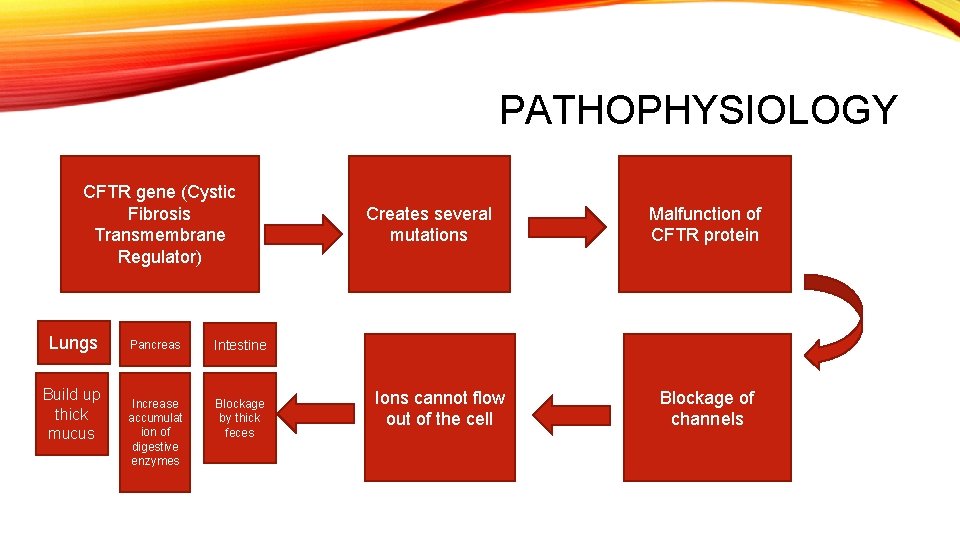
PATHOPHYSIOLOGY CFTR gene (Cystic Fibrosis Transmembrane Regulator) Lungs Build up thick mucus Pancreas Intestine Increase accumulat ion of digestive enzymes Blockage by thick feces Creates several mutations Ions cannot flow out of the cell Malfunction of CFTR protein Blockage of channels
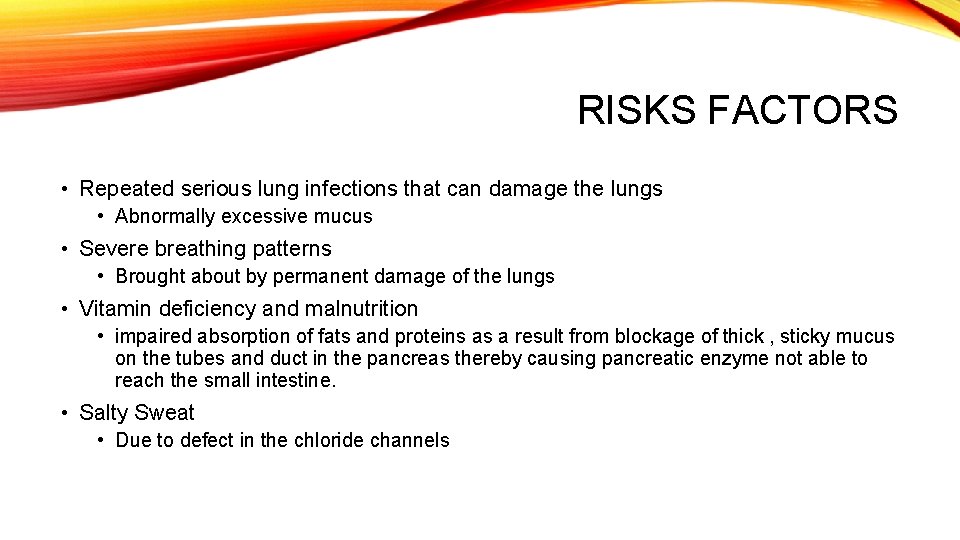
RISKS FACTORS • Repeated serious lung infections that can damage the lungs • Abnormally excessive mucus • Severe breathing patterns • Brought about by permanent damage of the lungs • Vitamin deficiency and malnutrition • impaired absorption of fats and proteins as a result from blockage of thick , sticky mucus on the tubes and duct in the pancreas thereby causing pancreatic enzyme not able to reach the small intestine. • Salty Sweat • Due to defect in the chloride channels
DAIGNOSING AND MONITORING • Newborn Screening • The newborn screen initially measures for raised blood concentration of immunoreactive trypsinogen. • Sweat testing • Infants with an abnormal newborn screen need a sweat test to confirm the CF diagnosis. In many cases, a parent makes the diagnosis because the infant tastes salty. • The resultant sweat is then collected on filter paper or in a capillary tube and analyzed for abnormal amounts of sodium and chloride. People with CF have increased amounts of sodium and chloride in their sweat • Genetic testing • Trypsinogen levels can be increased in individuals who have a single mutated copy of the CFTR gene (carriers) or, in rare instances, in individuals with two normal copies of the CFTR gene.
PRENATAL • Couples who are pregnant or planning a pregnancy can have themselves tested for the CFTR gene mutations to determine the risk that their child will be born with cystic fibrosis. • Testing is typically performed first on one or both parents and, if the risk of CF is high, testing on the fetus is performed. • During pregnancy, testing can be performed • the placenta (chorionic villus sampling) • fluid around the fetus (amniocentesis).
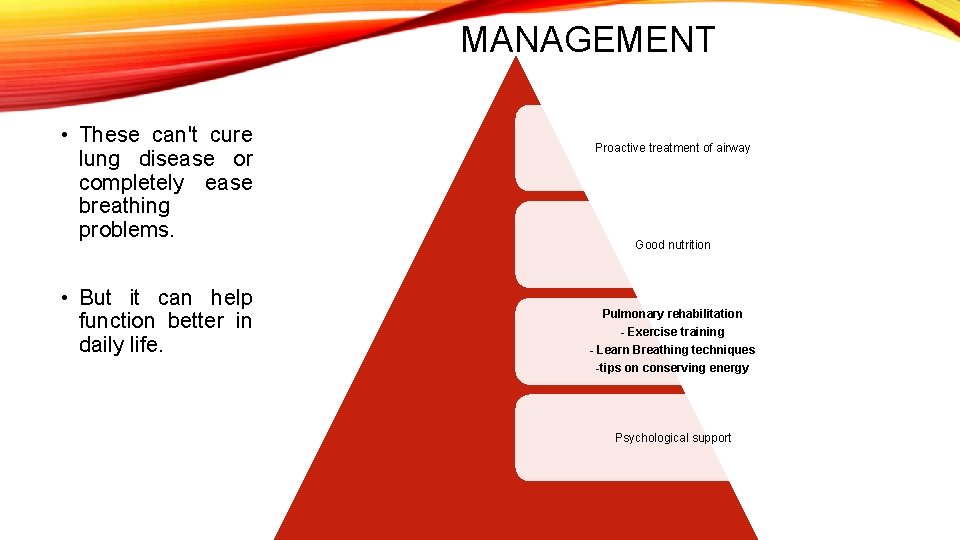
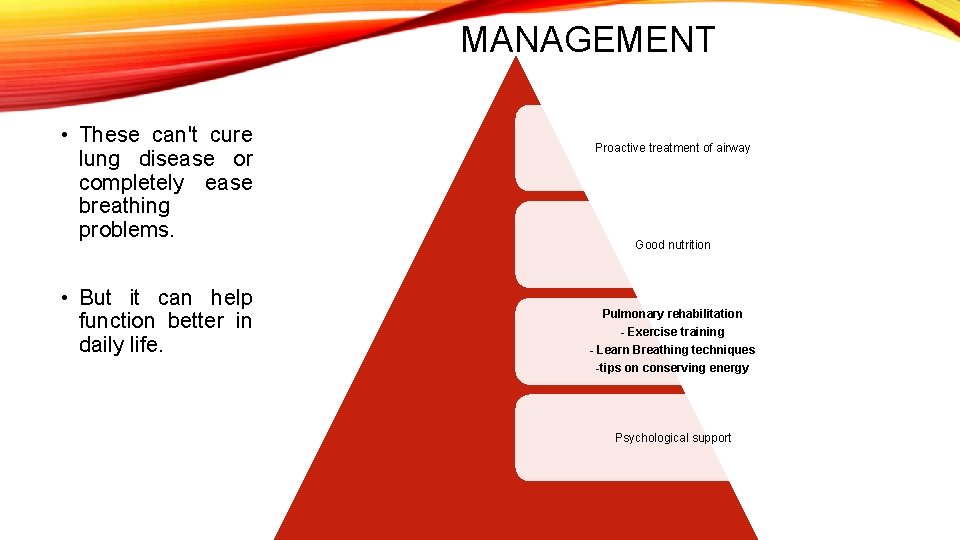
MANAGEMENT • These can't cure lung disease or completely ease breathing problems. • But it can help function better in daily life. Proactive treatment of airway Good nutrition Pulmonary rehabilitation - Exercise training - Learn Breathing techniques -tips on conserving energy Psychological support
Chronic and acute infections. • Intravenous, inhaled, and oral antibiotics Inhaled therapy with antibiotics such as tobramycin, colistin, and aztreonam is often given for months at a time to improve lung function by impeding the growth of colonized bacteria. Used to alter and clear the thickened mucus • Mechanical devices and inhalation medications

GOAL QUALITY OF LIFE
NURSING DIAGNOSIS • Ineffective Airway Clearance related to increase mucus secretions • Ineffective Breathing Pattern related to increase mucus secretions secondary to lung inflammation • Impaired Gas Exchange related to increase mucus secretions brought about by permanent damage of the lungs • Imbalanced Nutrition: Less than body requirement related to vitamin deficiency • Activity Intolerance related to shortness of breath • Ineffective Coping related to chronic condition • Hopelessness related to chronic condition
GENETIC CARDIOVASCULAR DISORDER Hypertrophic Cardiomyopathy
HYPERTROPHIC CARDIOMYOPATHY • A primary disease of the myocardium (the muscle of the heart) • Portion of myocardium is hypertrophied (thickened) without any obvious cause. • Leading cause of sudden cardiac death in young athletes. • Sudden unexpected cardiac death in any age group and a cause of disabling cardiac symptoms. • Younger people are likely to have a more severe for of hyperthropic cardiomyopathy. • Frequently asymptomatic until sudden cardiac death. (routine screening is necessary)
PREVALENCE • European, American, and Japanese populations, HCM appears in all racial groups. • The prevalence of HCM is about 0. 2% to 0. 5% of the general population
SIGNS AND SYMPTOMS • Asymptomatic or mildly asymptomatic • Dyspnea • Is largely due to increased stiffness of the left ventricle, which impairs filling of the ventricles and leads to elevated pressure in the left ventricle and left atrium. • Chest pain (angina) • Uncomfortable awareness of the heart beat • Lightheadedness • Fatigue • Fainting (called syncope) • Sudden cardiac death

MAJOR RISK FACTORS • Prior history of cardiac arrest or ventricular fibrillation • Spontaneous sustained ventricular tachycardia • The arrhythmia lasts ≥ 30 seconds or causes hemodynamic collapse in <30 seconds • Family history of premature sudden death • Unexplained syncope • LV thickness greater than or equal to 30 mm • Abnormal blood pressure • Nonsustained ventricular tachycardia(NSVT) • is defined as 3 or more consecutive beats at a rate of > beats/min and lasting < 30 s
GENETIC EXPLANATION • Autosomal dominant trait • Children of a single HCM parent have 50% chance of inheriting the disease-causing mutation • Mutations in one of a number of genes that encode for one of the sarcomere proteins. (1 of 9 sarcomeric genes) • Approximately 45% of these mutations occur in the β myosin heavy chain gene on chromosome 14 q 11. 2 -3 • 35% involve the cardiac myosin binding protein C gene.

INDIVIDUALS WITH NO FAMILY HISTORY • The cause of disease is due to de novo mutation of the gene that produces the β -myosin heavy chain. • An insertion/ deletion polymorphism in the gene encoding for angiotensin converting enzyme (ACE) alters the clinical phenotype of the disease. • The D/D (deletion/deletion) genotype of ACE is associated with more marked hypertrophy of the left ventricle and may be associated with higher risk of adverse outcomes
PATHOPHYSIOLOGY • A complex type of heart disease that affects the heart muscle • Thickening of the heart muscle (myocardium) • Occurs at the septum • Thickened septum cause a narrowing that can block or reduce the blood flow from the left ventricle to the aorta = “outflow tract obstruction” • The ventricles must pump harder to overcome the narrowing or blockage • Called as hyperthrophic obstructive caridomyopathy (HOCM).
• Stiffness in the left ventricle • Occurs as a result of cellular changes that occur in the heart muscle when it thickens. • The left ventricle is unable to relax normally and fill with blood. • Less blood at the end of filling – less oxygen- rich blood pumped to the organs and muscles. • The stiffness in the left ventricle causes pressure to increase inside the heart and may lead to mitral valve changes. • Mitral Valve Changes • The narrowing of the left ventricular outflow tract disrupts the proper function of the mitral valve • outflow obstruction • Increased pressure in the left ventricle.

MITRAL VALVE CHANGES
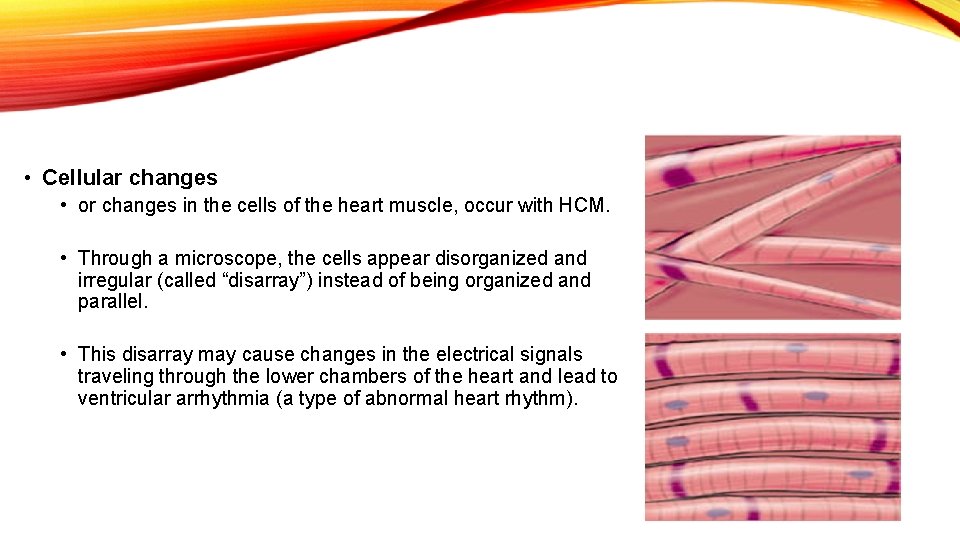
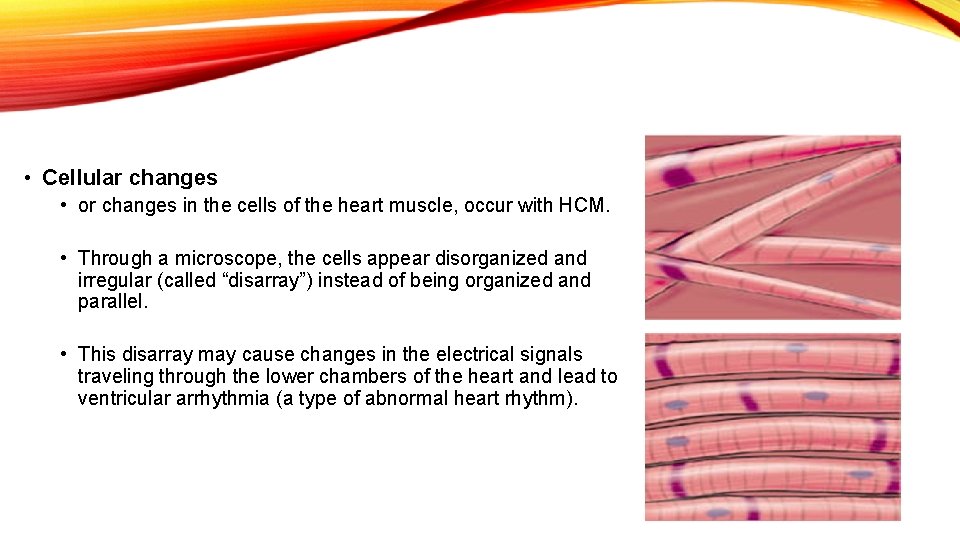
• Cellular changes • or changes in the cells of the heart muscle, occur with HCM. • Through a microscope, the cells appear disorganized and irregular (called “disarray”) instead of being organized and parallel. • This disarray may cause changes in the electrical signals traveling through the lower chambers of the heart and lead to ventricular arrhythmia (a type of abnormal heart rhythm).
THE DIAGNOSIS OF HCM IS BASED ON • Medical history: Your doctor will ask you questions about your symptoms and family history. • Physical exam: Your doctor will listen to your heart and lungs. Patients with hypertrophic obstructive cardiomyopathy (HOCM) may have a heart murmur. • Tests: An echocardiogram is the most common test used to diagnose HCM, as the characteristic thickening of the heart walls is usually visible on the echo. Other tests may include blood tests, electrocardiogram, chest X-ray, exercise stress echo test, cardiac catheterization and magnetic resonance imaging (MRI).
MEDICATIONS • BETA-BLOCKERS AND CALCIUM CHANNEL BLOCKERS • relax the heart muscle, allowing it to fill better and pump more effectively. • Other medications may be prescribed as needed to control your heart rate or decrease the occurrence of arrhythmias. • Avoid certain medications: - nitrates, because they lower blood pressure - digoxin, because it increases the force of the heart’s contraction. • Antibiotic medications may be prescribed to reduce the risk of bacterial endocarditis, a potentially life-threatening condition. • Antitussives- to avoid coughing
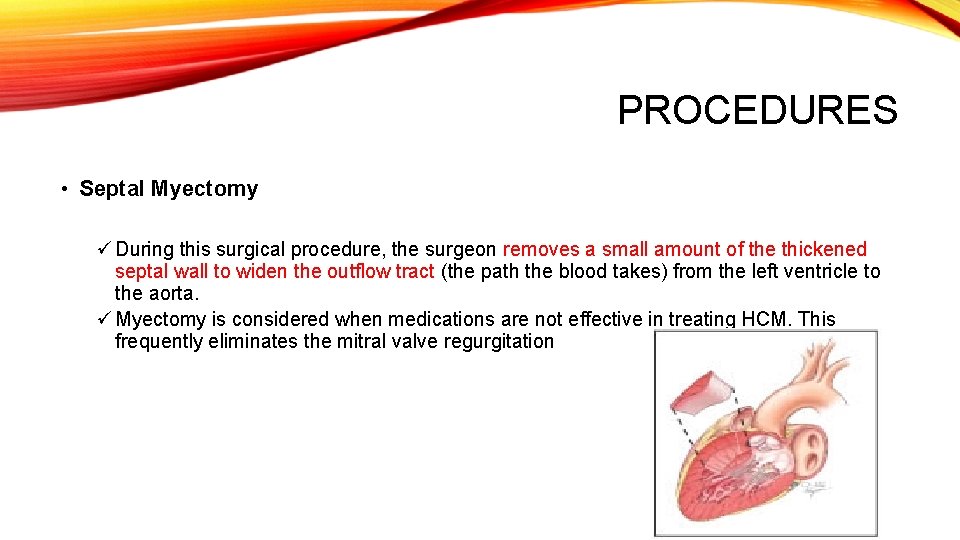
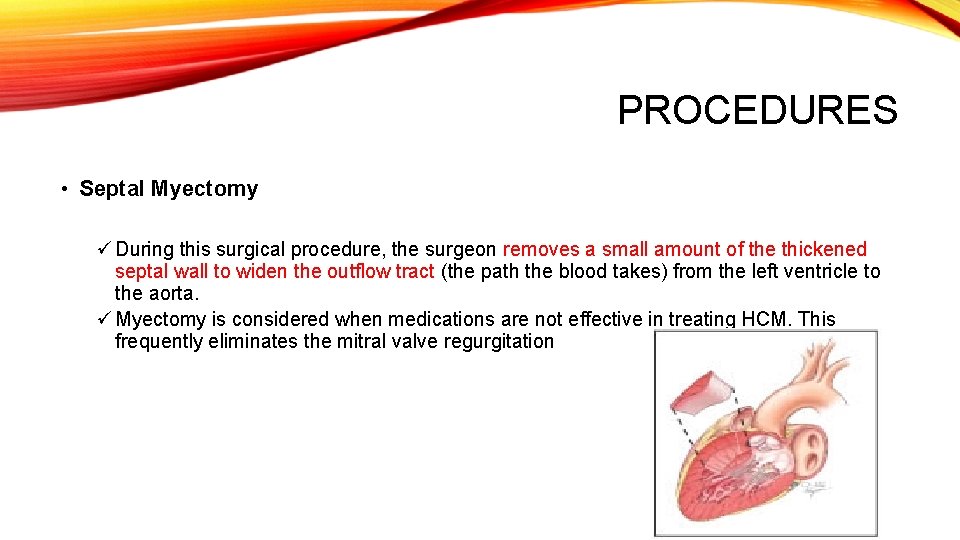
PROCEDURES • Septal Myectomy ü During this surgical procedure, the surgeon removes a small amount of the thickened septal wall to widen the outflow tract (the path the blood takes) from the left ventricle to the aorta. ü Myectomy is considered when medications are not effective in treating HCM. This frequently eliminates the mitral valve regurgitation
ETHANOL ABLATION • This procedure, also called septal ablation, is reserved for patients who are not eligible candidates for septal myectomy. • The ablation procedure is performed in the cardiac catheterization laboratory. • First, the small coronary artery that supplies blood flow to the upper part of the septum is located during a cardiac catheterization procedure. • A balloon catheter is inserted into the artery and inflated. • A contrast agent is injected to locate thickened septal wall that narrows the passageway from the left ventricle to the aorta. • When the bulge is located, a tiny amount of pure alcohol is injected through the catheter. • The alcohol kills the cells on contact, causing the septum to shrink back to a more normal size over the following months, widening the passage for blood flow.
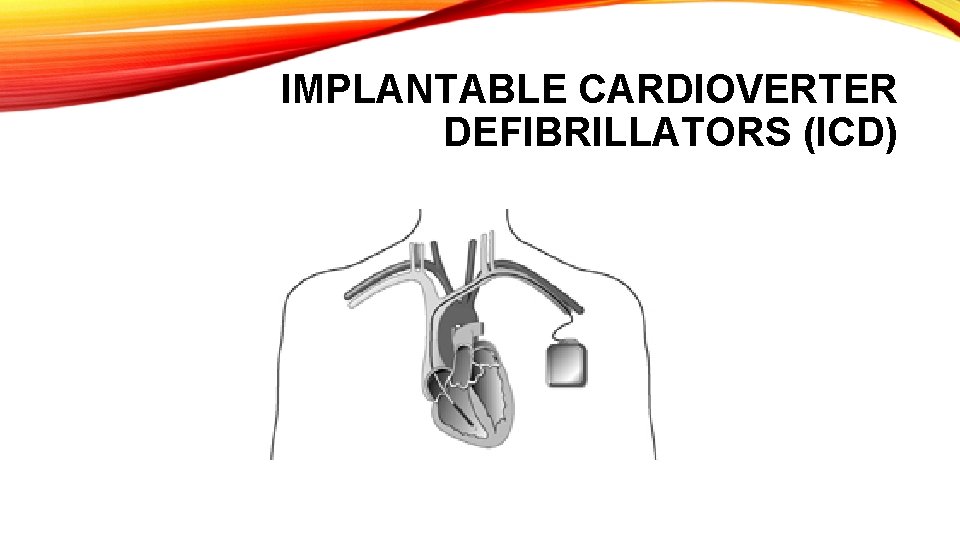
IMPLANTABLE CARDIOVERTER DEFIBRILLATORS (ICD) • ICDs are suggested for people at risk for life-threatening arrhythmias or sudden cardiac death. • The ICD is a small device placed just under the skin and is connected to wire leads that are threaded through the vein to the heart. • An ICD constantly monitors the heart rhythm. • When it detects a very fast, abnormal heart rhythm, it delivers energy (a small but powerful shock) to the heart muscle to cause the heart to beat in a normal rhythm again.
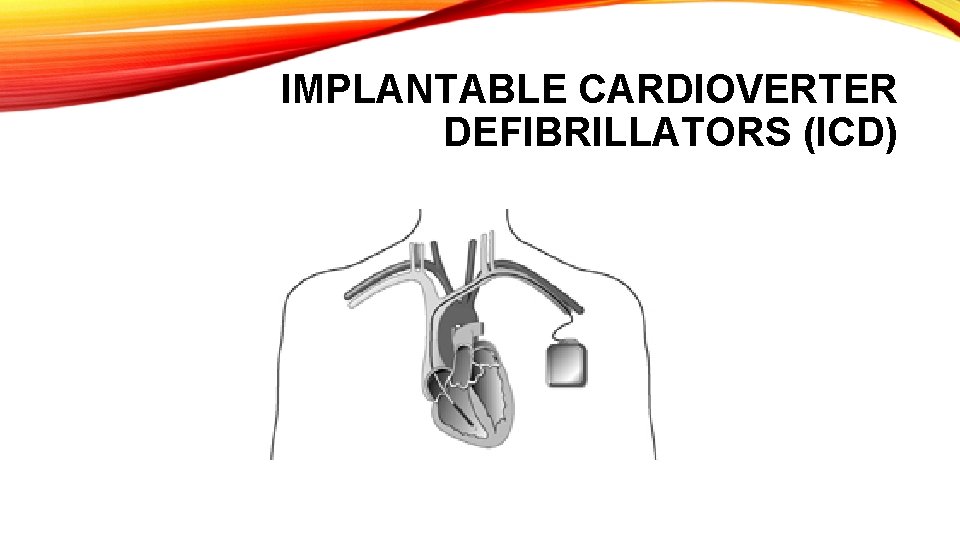
IMPLANTABLE CARDIOVERTER DEFIBRILLATORS (ICD)
LIFESTYLE CHANGES: • Certain lifestyle changes, as listed below, are essential for properly managing HCM. • Fluid and sodium restrictions may be necessary for some patients if heart failure symptoms are present. Ask the doctor for specific fluid and dietary guidelines, including information about alcoholic beverages and caffeinated products. • Exercise. • The doctor will discuss exercise guidelines with the patient. • Most people with hypertrophic cardiomyopathy are able to participate in noncompetitive aerobic activities. • Heavy weight lifting and many high-intensity sports are not recommended.
• Regular Follow-Up Visits. • Patients with HCM should follow up regularly with their cardiologist, as recommended, to monitor their condition. • Reduce Risk for Infection
TO REDUCE RISK FOR INFECTION: • Practice good oral hygiene habits every day. • Take good care of your teeth and gums by seeking professional dental care every six months • regularly brushing and flossing your teeth • making sure dentures fit properly.
TO REDUCE RISK FOR INFECTION • Call the doctor if there are symptoms of an infection like: • • • fever over 100 degrees F; sweats or chills; skin rash; pain, tenderness, redness or swelling; wound or cut that won’t heal; red, warm or draining wound; sore throat, scratchy throat or pain when swallowing; sinus drainage, nasal congestion, headaches or tenderness along upper cheekbones; persistent dry or moist cough that lasts more than two days; white patches in your mouth or on your tongue; • nausea, vomiting or diarrhea.
TO REDUCE RISK FOR INFECTION • Don’t wait to seek treatment. • Colds and the flu do not cause endocarditis, but infections, which may have the same symptoms, do cause endocarditis. • To be safe, call the doctor.
NURSING DIAGNOSIS • Activity Intolerance related arrhythmias • Ineffective breathing pattern related to dyspnea • Decreased cardiac output related to mitral valve changes • Situational low self esteem related to chronic condition • Ineffective sexuality pattern: risk • Fear related to chronic condition • Impaired comfort related to chest pain
GENETIC DISORDER IN NEUROLOGICAL SYSTEM
ALZHEIMER’S DISEASE (AD) • AD is an illness of the brain, It causes large numbers of nerve cells in the brain to die. • A progressive, irreversible brain disease that destroys memory and thinking skills. • Most common dementia in adults.
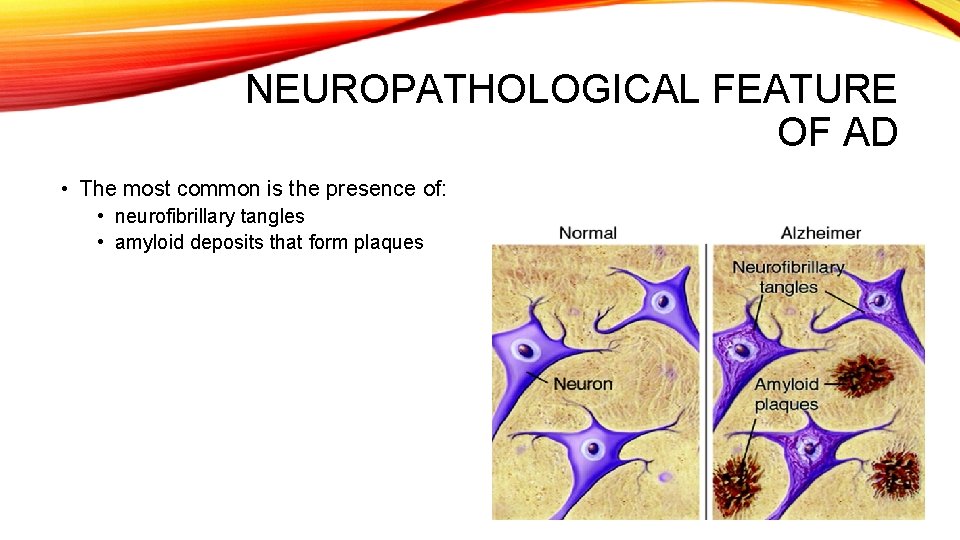
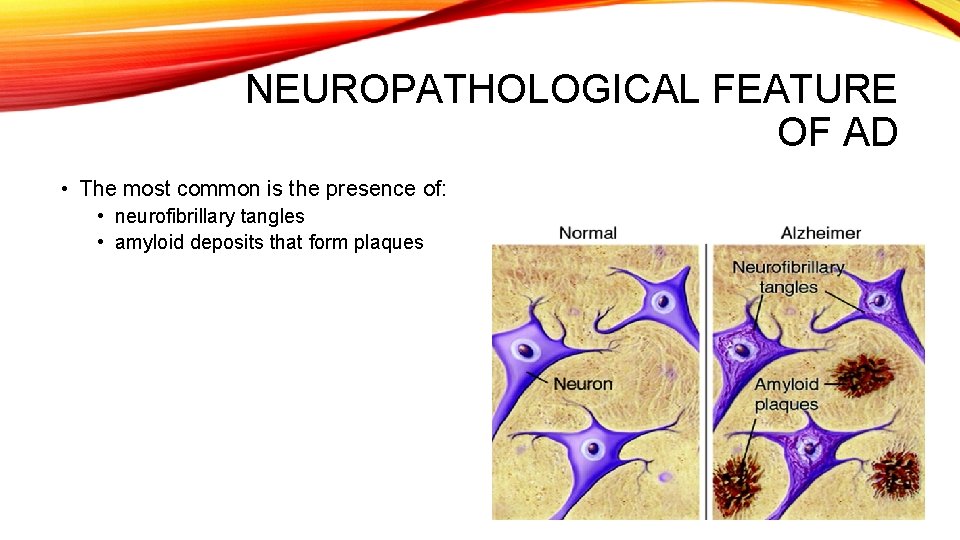
NEUROPATHOLOGICAL FEATURE OF AD • The most common is the presence of: • neurofibrillary tangles • amyloid deposits that form plaques
SIGNS AND SYMPTOMS • • • Memory loss Difficulty performing familiar tasks Problems with language Disorientation to time and place Poor or decreased judgement Problems with abstract thinking Misplace things Changes in mood or behavior Changes in personality Loss of initiative
RISK FACTORS • Age • After age 65 and rises sharply after age 75 • Genetics • Family history of AD • Sex • Women > men • Having Down Syndrome
FORMS OF AD • Familial • Sporadic
• Familial forms • When more than one person in a family is affected • Approximately 25% of AD is familial • Sporadic Forms • Refers to AD cases when no other cases have been seen in close family members. • The remaining 75% is sporadic
DIFFERENT ONSET • Early onset forms • Denotes onset of the disease before age 65 years • Less than 10% of all AD cases are familial early onset • Late onset forms • Denotes onset after age 65 years. • Almost all cases of Sporadic AD are late onset • Approximately 90% of familial AD is late onset.
GENETIC EXPLANATION Familial onset Sporadic onset

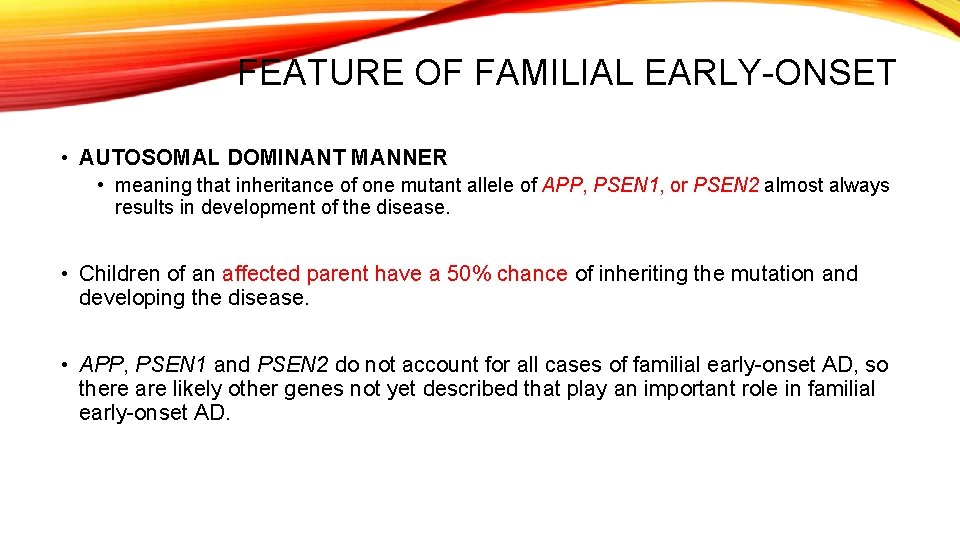
FEATURE OF FAMILIAL EARLY-ONSET • AUTOSOMAL DOMINANT MANNER • meaning that inheritance of one mutant allele of APP, PSEN 1, or PSEN 2 almost always results in development of the disease. • Children of an affected parent have a 50% chance of inheriting the mutation and developing the disease. • APP, PSEN 1 and PSEN 2 do not account for all cases of familial early-onset AD, so there are likely other genes not yet described that play an important role in familial early-onset AD.
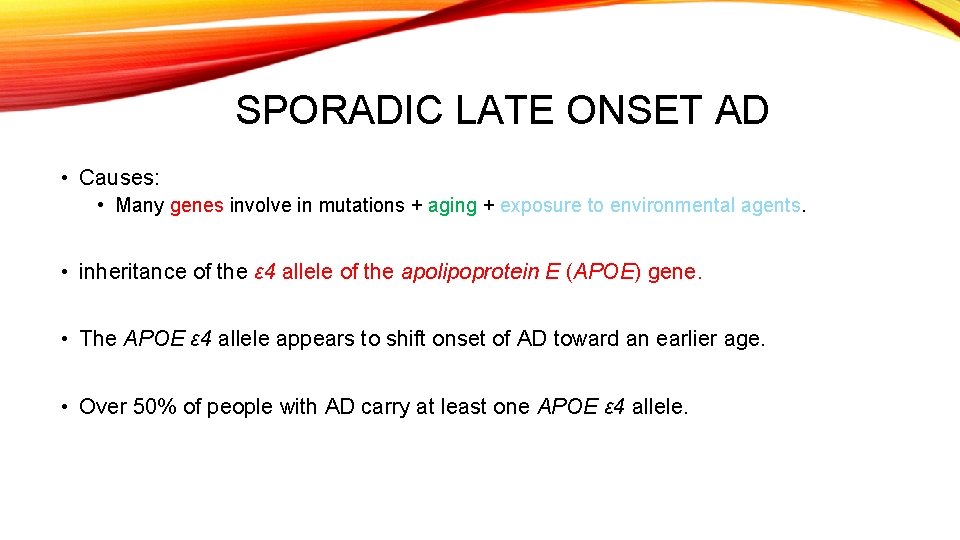
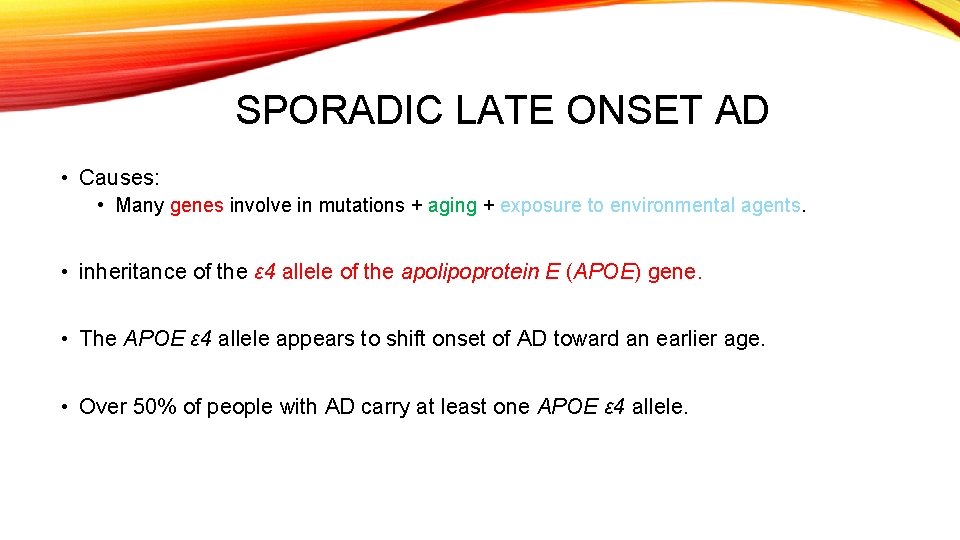
SPORADIC LATE ONSET AD • Causes: • Many genes involve in mutations + aging + exposure to environmental agents. • inheritance of the ε 4 allele of the apolipoprotein E (APOE) gene. • The APOE ε 4 allele appears to shift onset of AD toward an earlier age. • Over 50% of people with AD carry at least one APOE ε 4 allele.
• A person carrying two APOE ε 4 alleles has a 30% chance of developing sporadic late-onset AD. • First degree relatives of a person with sporadic late-onset AD have an approximately 2. 5 times greater risk of developing sporadic late-onset AD.
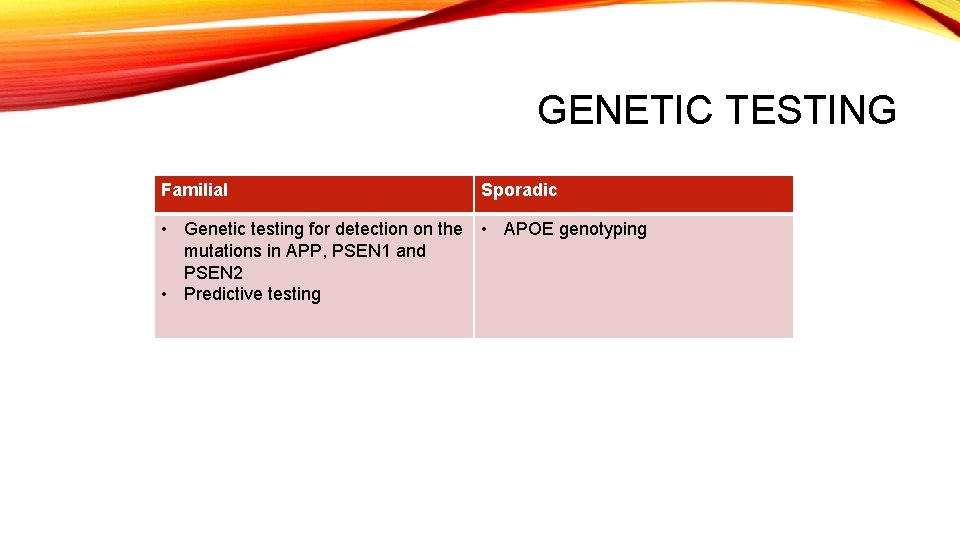
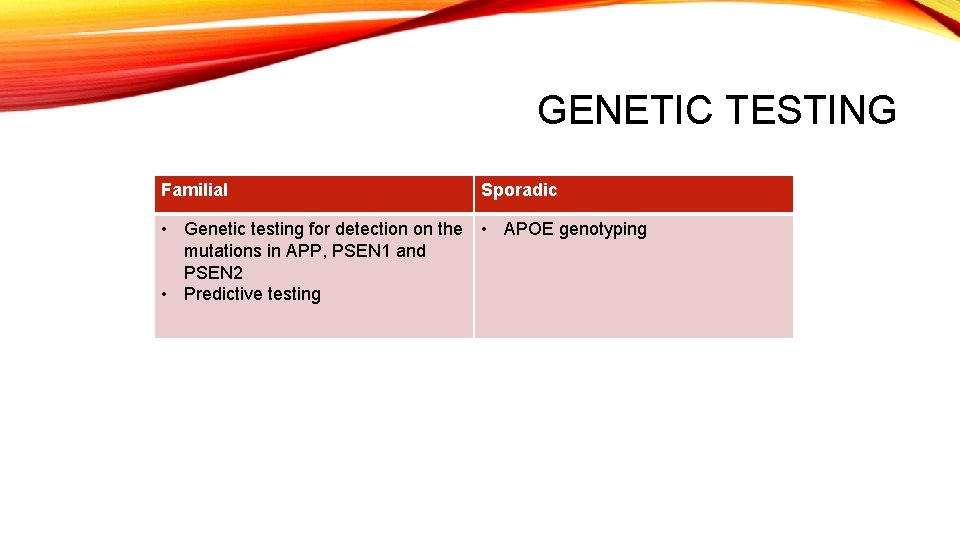
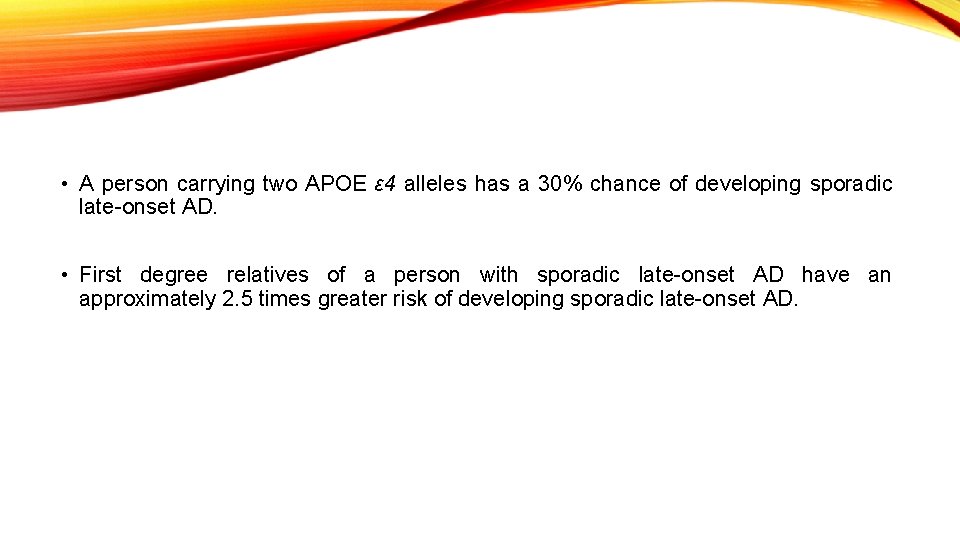
GENETIC TESTING Familial Sporadic • Genetic testing for detection on the mutations in APP, PSEN 1 and PSEN 2 • Predictive testing • APOE genotyping

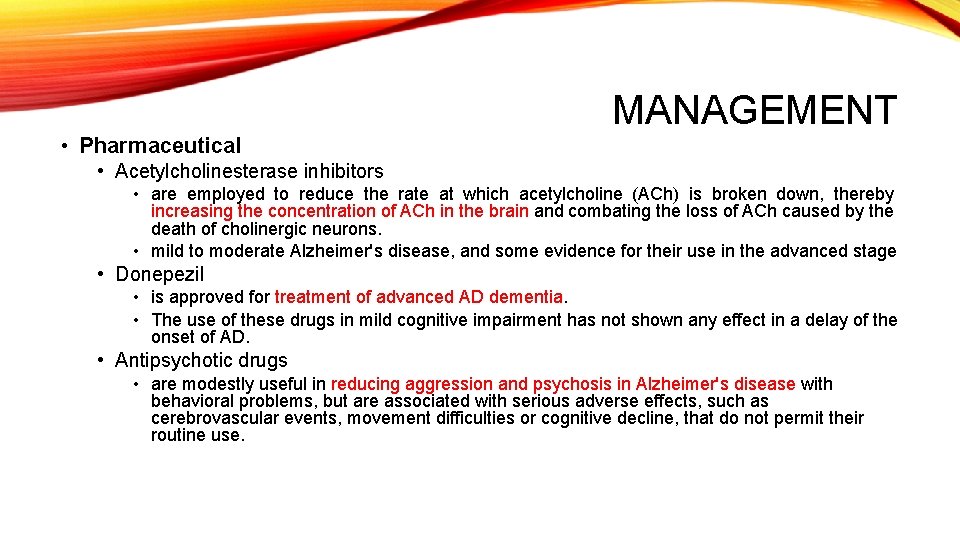
• Pharmaceutical MANAGEMENT • Acetylcholinesterase inhibitors • are employed to reduce the rate at which acetylcholine (ACh) is broken down, thereby increasing the concentration of ACh in the brain and combating the loss of ACh caused by the death of cholinergic neurons. • mild to moderate Alzheimer's disease, and some evidence for their use in the advanced stage • Donepezil • is approved for treatment of advanced AD dementia. • The use of these drugs in mild cognitive impairment has not shown any effect in a delay of the onset of AD. • Antipsychotic drugs • are modestly useful in reducing aggression and psychosis in Alzheimer's disease with behavioral problems, but are associated with serious adverse effects, such as cerebrovascular events, movement difficulties or cognitive decline, that do not permit their routine use.
PSYCHOSOCIAL INTERVENTION • used as an adjunct to pharmaceutical treatment and can be classified within behavior-, emotion-, cognition- or stimulation-oriented approaches. 1. Behavioral interventions • identify and reduce the antecedents and consequences of problem behaviors. • This approach has not shown success in improving overall functioning, but can help to reduce some specific problem behaviors, such as incontinence • There is a lack of high quality data on the effectiveness
• Emotion-oriented interventions include • • • reminiscence therapy validation therapy supportive psychotherapy sensory integration simulated presence therapy • Stimulation-oriented treatments include • art, music and pet therapies, exercise, and any other kind of recreational activities. • support for improving behavior, mood, and, to a lesser extent, function. • the main support for the use of stimulation therapies is the change in the person's routine.
CAREGIVING • Modifications of the living environment • Patient’s safety • Simplified routines
NURSING DIAGNOSIS • Ineffective coping • Risk for fall • Activity intolerance • Impaired thought process • Inadequate nutrition: less than body requirements • Helplessness
ENDOCRINE AND RENAL SYSTEM
NEPHROGENIC DIABETES INSIPIDUS • A disorder of water balance • Produce too much urine (polyuria) which causes them to be excessively thirsty (polydipsia) • Affected individuals can quickly become dehydrated if they do not drink enough water especially in hot weather or when they are sick. • Can either be acquired or hereditary • Acquired- certain drugs or chronic diseases and occur at any time during life. • Hereditary – genetic mutations, and its signs and symptoms usually become apparent within first few months.
• Eat poorly INFANTS WITH HEREDITARY NEPHROGENIC DIABETES INSIPIDUS • Fail to gain weight • Grow at the expected rate (failure to thrive) • Irritable • Fever • Diarrhea- recurrent episodes can lead to slow growth and delayed development. • Vomiting
IF NOT MANAGED • Damaged of bladder and kidneys • Pain • Infections • Kidney failure • With appropriate treatment, affected individuals usually have few complications and a normal lifespan.
HOW COMMON? • Prevalence – unknown • Rare • Hereditary
GENETIC EXPLANATION HEREDITARY FORM • Mutations in at least two genes • 90% of all cases of hereditary results from mutations in the AVPR 2 gene. • 10% of cases are caused by mutations in the AQP 2 gene. • AVPR 2 and AQP 2 genes • Provides instructions for making proteins that help determine how much water is excreted in urine.
ACQUIRED FORM • Results from chronic kidney disease • Medications such as lithium, low levels of potassium in the blood (hypokalemia), high levels of calcium in the blood (hypercalcemia), or an obstruction of the urinary tract.
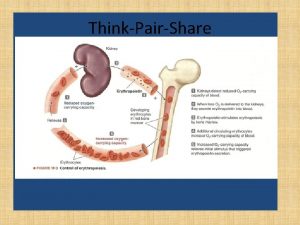
PHYSIOLOGY • The kidneys filter the blood to remove waste and excess fluid, which are stored in the bladder as urine. • The balance between fluid intake and urine excretion is controlled by a hormone called vasopressin or antidiuretic hormone (ADH). • ADH directs the kidneys to concentrate urine by reabsorbing some of the water into the bloodstream. • Normally, when a person's fluid intake is low or when a lot of fluid is lost (for example, through sweating), increased levels of ADH in the blood tell the kidneys to make less urine. • When fluid intake is adequate, lower levels of ADH tell the kidneys to make more urine.
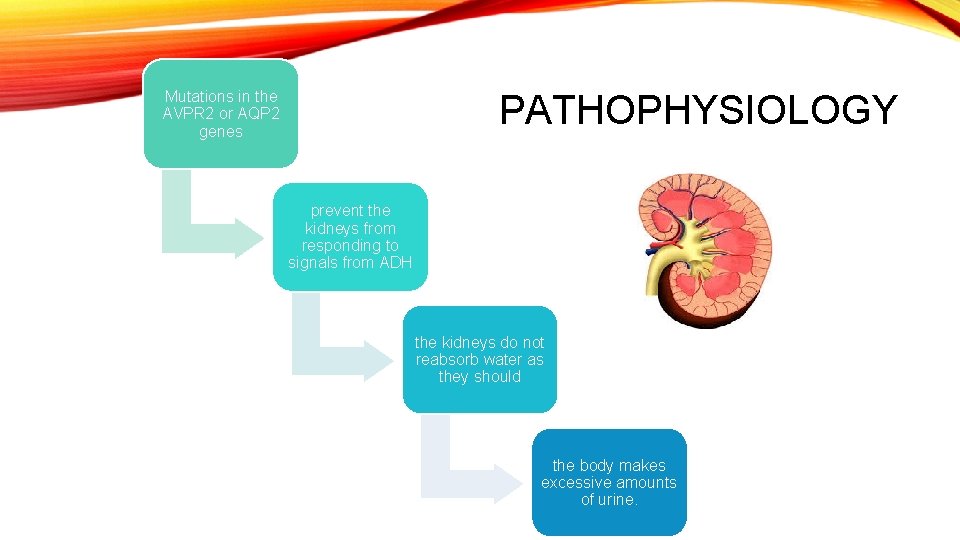
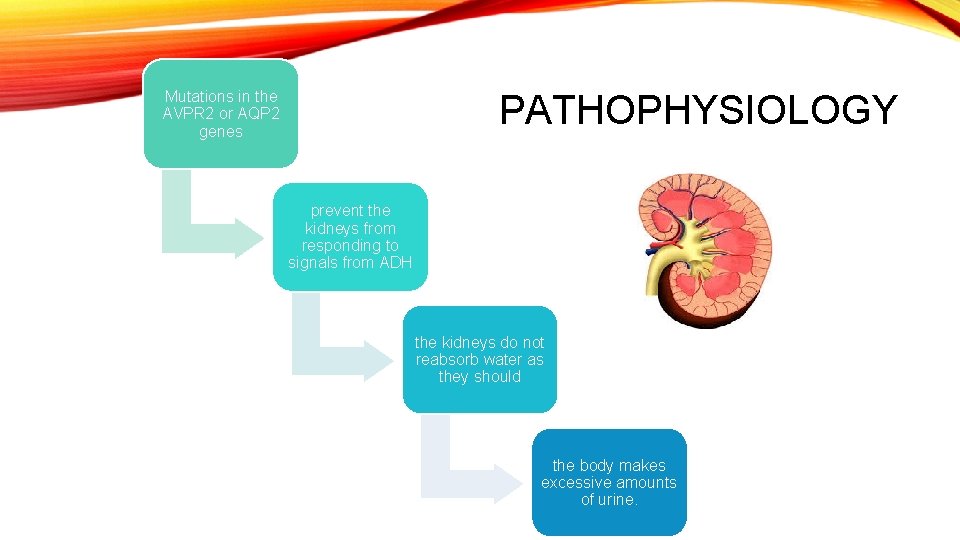
Mutations in the AVPR 2 or AQP 2 genes PATHOPHYSIOLOGY prevent the kidneys from responding to signals from ADH the kidneys do not reabsorb water as they should the body makes excessive amounts of urine.
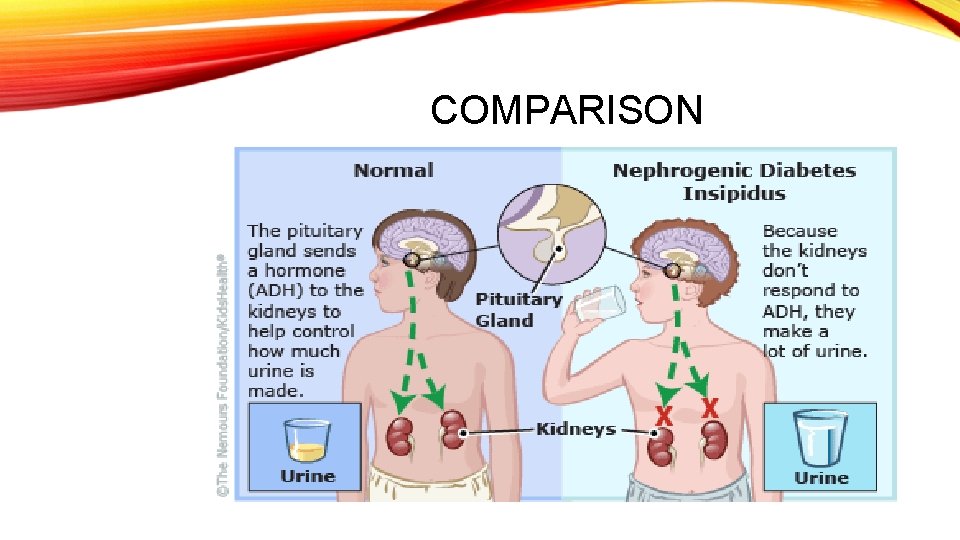
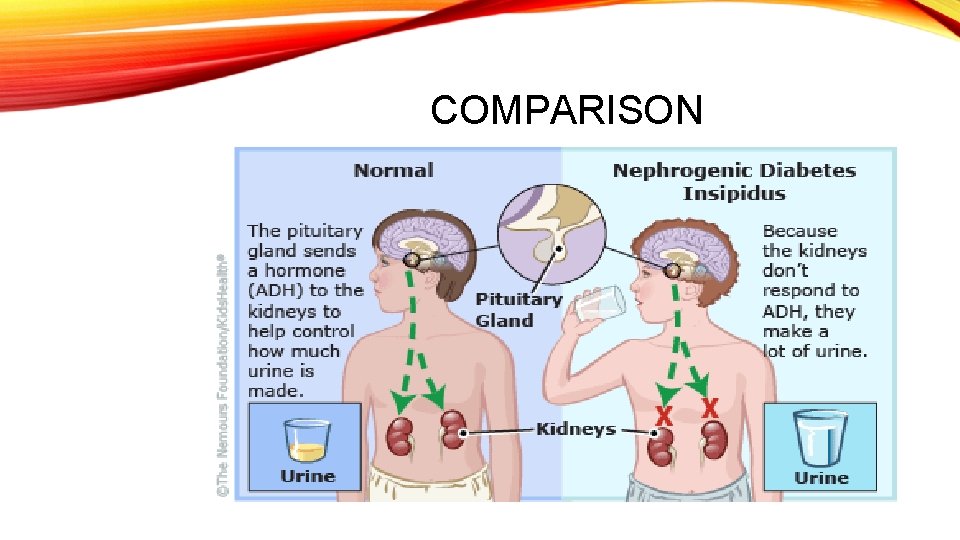
COMPARISON
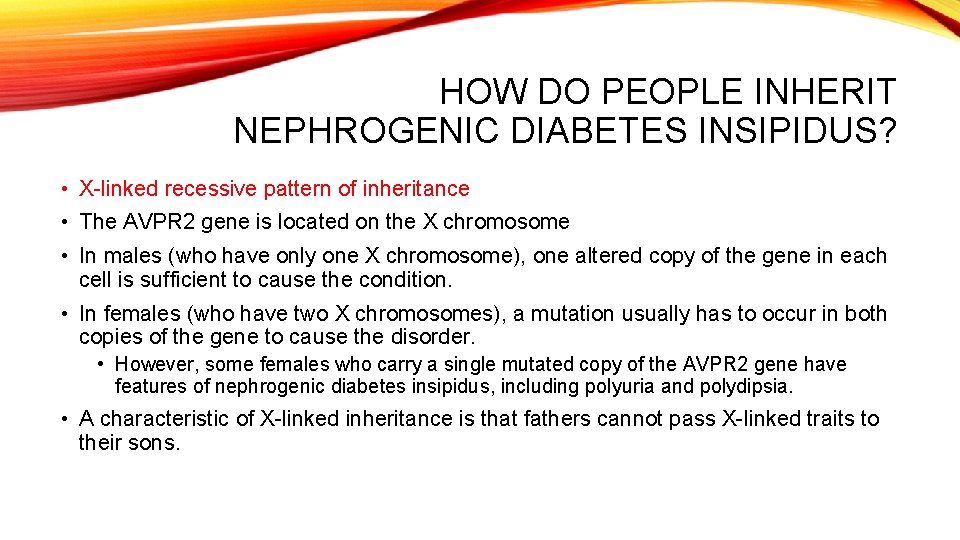
HOW DO PEOPLE INHERIT NEPHROGENIC DIABETES INSIPIDUS? • X-linked recessive pattern of inheritance • The AVPR 2 gene is located on the X chromosome • In males (who have only one X chromosome), one altered copy of the gene in each cell is sufficient to cause the condition. • In females (who have two X chromosomes), a mutation usually has to occur in both copies of the gene to cause the disorder. • However, some females who carry a single mutated copy of the AVPR 2 gene have features of nephrogenic diabetes insipidus, including polyuria and polydipsia. • A characteristic of X-linked inheritance is that fathers cannot pass X-linked traits to their sons.
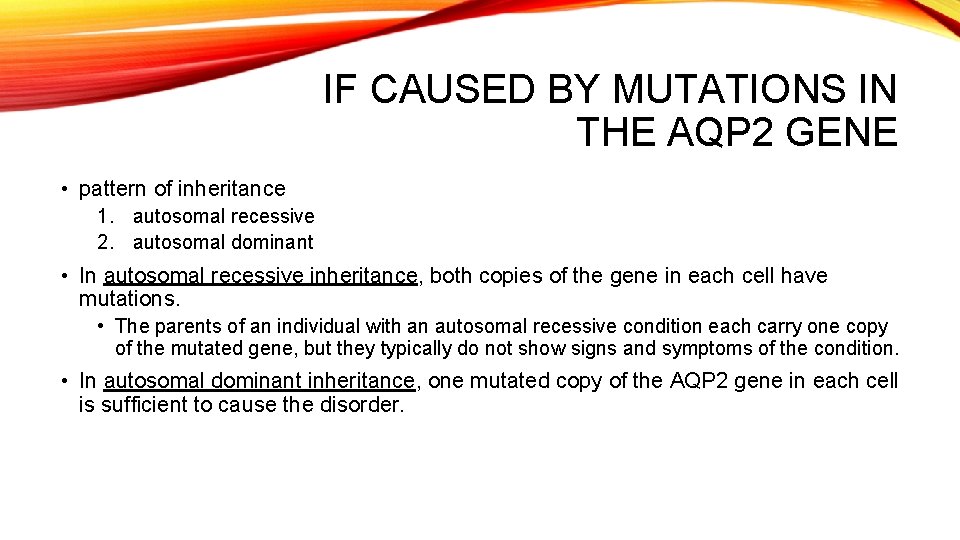
IF CAUSED BY MUTATIONS IN THE AQP 2 GENE • pattern of inheritance 1. autosomal recessive 2. autosomal dominant • In autosomal recessive inheritance, both copies of the gene in each cell have mutations. • The parents of an individual with an autosomal recessive condition each carry one copy of the mutated gene, but they typically do not show signs and symptoms of the condition. • In autosomal dominant inheritance, one mutated copy of the AQP 2 gene in each cell is sufficient to cause the disorder.
NURSING MANAGEMENT • • • Goal: Maintenance of fluid and electrolyte balance Early detection Maintenance of adequate hydration Patient teaching for long term management Dietary measures • low sodium diet – limiting sodium intake to no more than 3 g/day • Help decrease urine output • Medication- may reduce flow to the ADH- sensitive distal nephrons • Thiazide diuretics • Hydrochlorothiazide (Hydro. DIURIL) • Chlorothiazide (Diuril)
• Indomethacin (Indocin) • May be prescribed if low sodium diet and thiazide is not effective • A non steroidal anti-inflammatory drug (NSAID) • Help increase renal responsiveness to ADH
NURSING DIAGNOSIS • Deficient fluid volume related to compromised endocrine regulatory mechanism Neurohypophyseal dysfunction Hypopituitarism Hypophysectomy Nephrogenic DI • Common Expected Outcome: • Patient experiences normal fluid volume as evidenced by absence of thirst, normal serum sodium level, and stable weight. • NIC Interventions • Fluid Monitoring; • Fluid Management; • Electrolyte Management
• Risk for Impaired Skin Integrity related to urinary frequency with high volume output and the potential for incontinence • Common Expected • Patient’s skin remains intact. • NIC Interventions • Skin Surveillance; • Skin Care: • Topical Treatments
• Deficient Knowledge related to new condition, unfamiliarity with disease and treatment • Questions Requests for more information verbalized misconceptions or misinterpretation • Common Expected • Patient verbalizes correct understanding of DI and the medications used in treatment. • Nursing Interventions Teaching: • Disease Process; • Teaching: • Prescribed Medication
GROUP PRESENTATION • Outline: • • • Disease Overview Signs and Symptoms Risk Factors Genetic Explanation Mode and Type of Inheritance Medical and Nursing Management • Treatment • Nursing diagnosis at least 2
THANK YOU
 Chorionic villus
Chorionic villus Dominant vs recessive genetic disorders
Dominant vs recessive genetic disorders Using karyotypes to diagnose genetic disorders
Using karyotypes to diagnose genetic disorders Chromosomal mutation
Chromosomal mutation Gene pool
Gene pool Genetic programming vs genetic algorithm
Genetic programming vs genetic algorithm Genetic programming vs genetic algorithm
Genetic programming vs genetic algorithm Genetic drift
Genetic drift Gene flow vs genetic drift
Gene flow vs genetic drift Marfan syndrome genetics
Marfan syndrome genetics Genetic disorder brochure project answers
Genetic disorder brochure project answers Dsm 5 munchausen by proxy
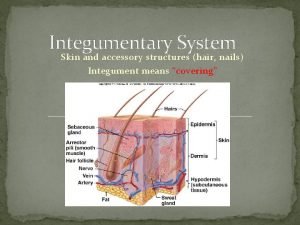
Dsm 5 munchausen by proxy Glands in integumentary system
Glands in integumentary system Integumentary system vocabulary
Integumentary system vocabulary Integumentary system of pig
Integumentary system of pig Definisi sistem integumen
Definisi sistem integumen Integumentary system facts
Integumentary system facts Exercise 7 the integumentary system
Exercise 7 the integumentary system Integumentary system vocab
Integumentary system vocab Exfoliative dermatitis
Exfoliative dermatitis The integumentary system
The integumentary system Integumentary system assessment
Integumentary system assessment Excretory system analogy
Excretory system analogy The integumentary system
The integumentary system The integumentary system
The integumentary system Integumentary system components
Integumentary system components Effects of aging on the integumentary system
Effects of aging on the integumentary system Section 36-3 the integumentary system
Section 36-3 the integumentary system Integumentary system
Integumentary system Integumentary system
Integumentary system Unit 3 integumentary system
Unit 3 integumentary system Skin homeostatic imbalances
Skin homeostatic imbalances Cells in stratum spinosum
Cells in stratum spinosum 6 functions of the integumentary system
6 functions of the integumentary system Integumentary system psoriasis
Integumentary system psoriasis Urinary system interesting facts
Urinary system interesting facts Integumentary system
Integumentary system Large organ of the body
Large organ of the body Integumentary system cpt coding guidelines ppt
Integumentary system cpt coding guidelines ppt Duct of merocrine sweat gland
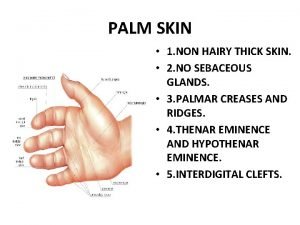
Duct of merocrine sweat gland Palm without skin
Palm without skin Nails integumentary system
Nails integumentary system Integumentary system
Integumentary system Excretory and integumentary system
Excretory and integumentary system Squid integumentary system
Squid integumentary system Digestive system foldable
Digestive system foldable Chapter 6 integumentary system
Chapter 6 integumentary system Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders Disorders of the nervous system
Disorders of the nervous system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Chapter 10 lymphatic system diseases and disorders
Chapter 10 lymphatic system diseases and disorders Chapter 36 skeletal muscular and integumentary systems
Chapter 36 skeletal muscular and integumentary systems Free nerve endings and encapsulated
Free nerve endings and encapsulated How to pronounce integumentary
How to pronounce integumentary Integumentary interactions with other systems
Integumentary interactions with other systems Unit 14 physiological disorders and their care
Unit 14 physiological disorders and their care Unit 14 task 1
Unit 14 task 1 Neurocognitive disorders
Neurocognitive disorders Bipolar and other related disorders
Bipolar and other related disorders Bipolar and other related disorders
Bipolar and other related disorders Flinders model of care
Flinders model of care Assistive technology for emotional disturbance
Assistive technology for emotional disturbance Nursing diagnosis for somatoform disorder
Nursing diagnosis for somatoform disorder Coprophilic disorder
Coprophilic disorder Types of sensory disorders
Types of sensory disorders Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Section 4-1 mental disorders answers
Section 4-1 mental disorders answers Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Chapter 18 psychological disorders
Chapter 18 psychological disorders Diathesis stress model
Diathesis stress model Cluster b personality disorders
Cluster b personality disorders Axis 1 and axis 2 disorders
Axis 1 and axis 2 disorders Dramatic personality disorders
Dramatic personality disorders Dsm v personality disorders
Dsm v personality disorders Inflexible personality
Inflexible personality Cluster c
Cluster c Cluster b traits
Cluster b traits What are the 3 clusters of personality disorders
What are the 3 clusters of personality disorders Yorkshire centre for eating disorders
Yorkshire centre for eating disorders Neurotic, stress-related and somatoform disorders
Neurotic, stress-related and somatoform disorders Neurocognitive disorders
Neurocognitive disorders Immunoproliferative disorders examples
Immunoproliferative disorders examples Mood disorders
Mood disorders Prpp
Prpp Purine disorders
Purine disorders Monosomy disorders
Monosomy disorders Sex linked disorders
Sex linked disorders Unit 14 physiological disorders assignment 1
Unit 14 physiological disorders assignment 1 Ctc added authorization
Ctc added authorization Gross features
Gross features Hemodynamic disorders
Hemodynamic disorders Hemodynamic disorders
Hemodynamic disorders Hemodynamic disorders
Hemodynamic disorders