Figure 26 1 An Introduction to the Urinary



- Slides: 68
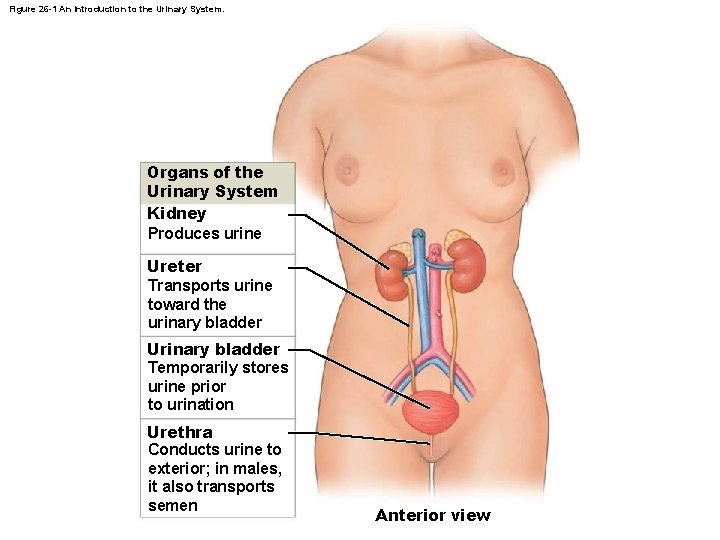
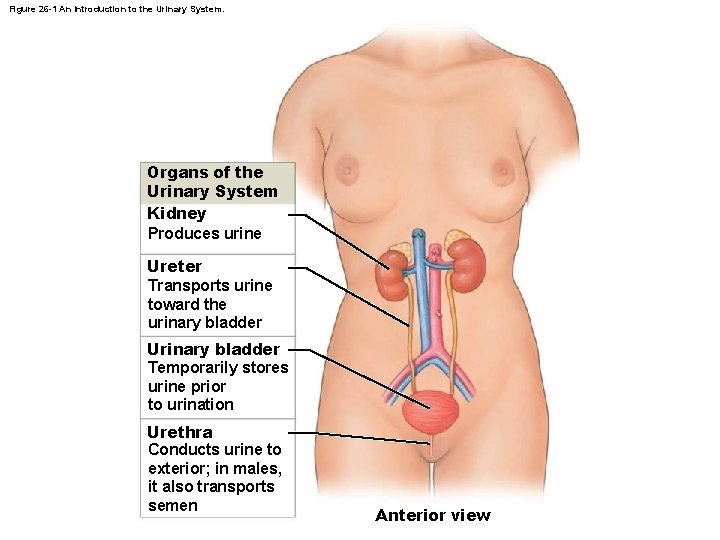
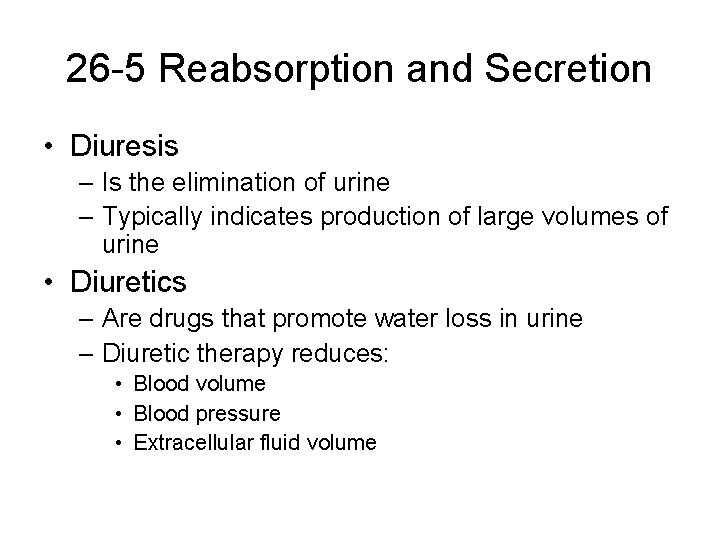
Figure 26 -1 An Introduction to the Urinary System. Organs of the Urinary System Kidney Produces urine Ureter Transports urine toward the urinary bladder Urinary bladder Temporarily stores urine prior to urination Urethra Conducts urine to exterior; in males, it also transports semen Anterior view
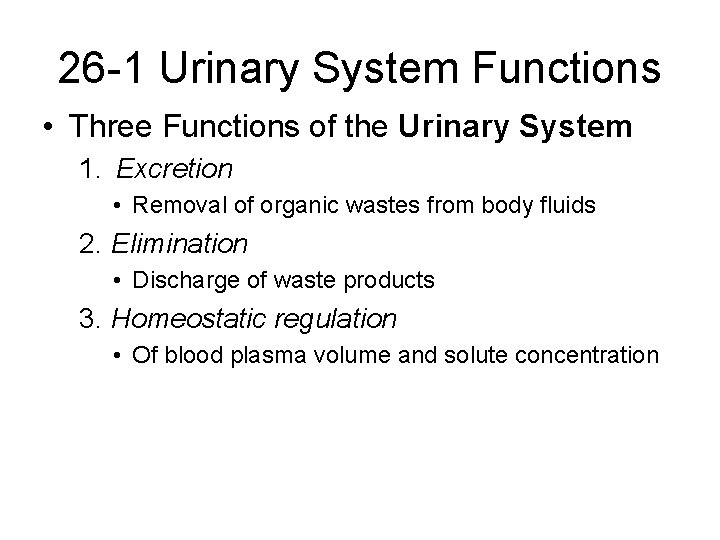
26 -1 Urinary System Functions • Three Functions of the Urinary System 1. Excretion • Removal of organic wastes from body fluids 2. Elimination • Discharge of waste products 3. Homeostatic regulation • Of blood plasma volume and solute concentration
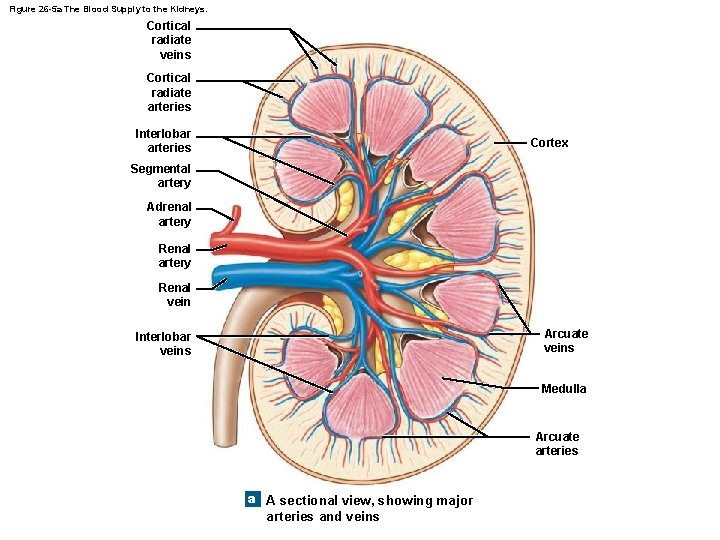
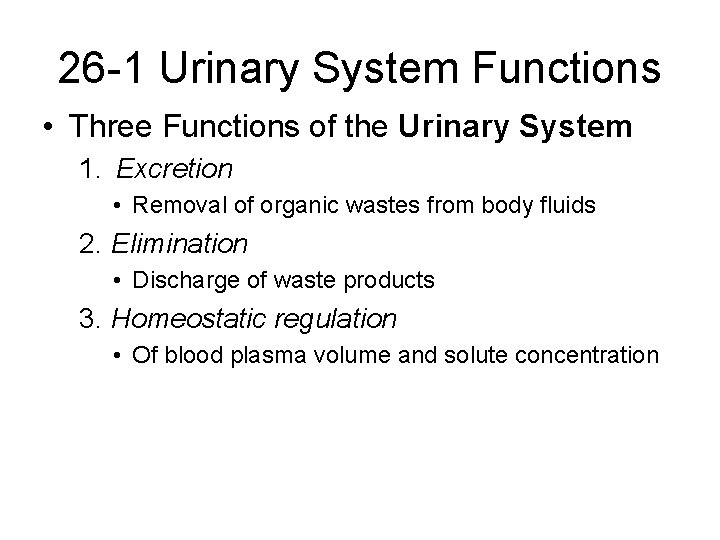
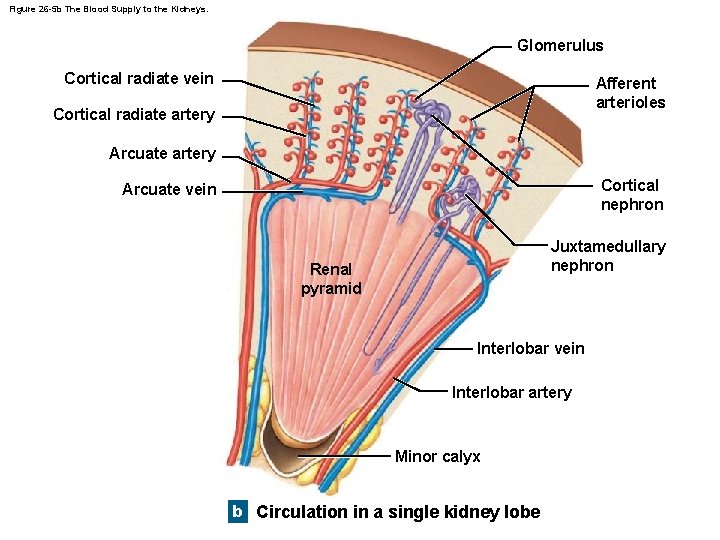
Figure 26 -5 a The Blood Supply to the Kidneys. Cortical radiate veins Cortical radiate arteries Interlobar arteries Cortex Segmental artery Adrenal artery Renal vein Arcuate veins Interlobar veins Medulla Arcuate arteries a A sectional view, showing major arteries and veins
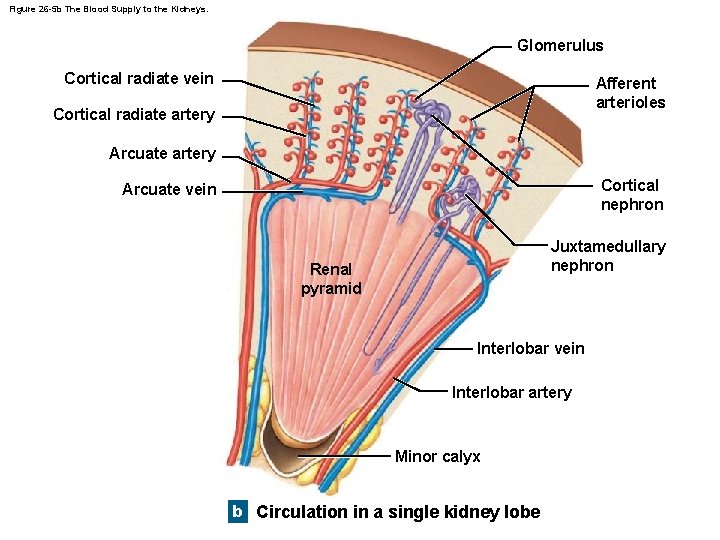
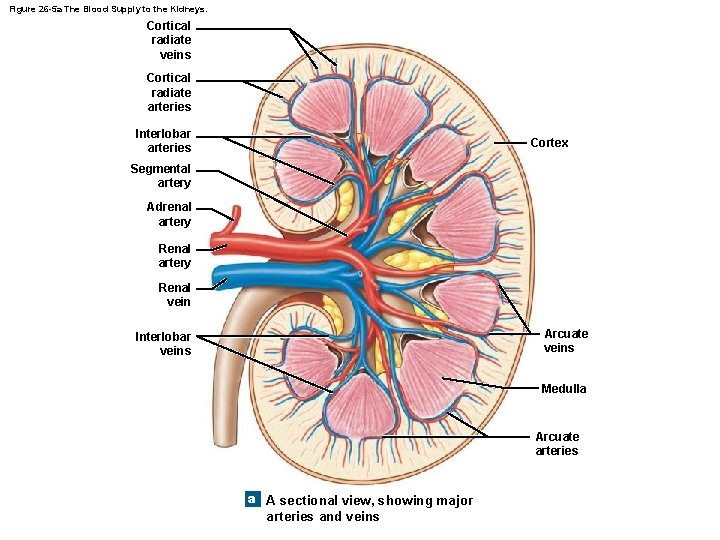
Figure 26 -5 b The Blood Supply to the Kidneys. Glomerulus Cortical radiate vein Afferent arterioles Cortical radiate artery Arcuate artery Cortical nephron Arcuate vein Juxtamedullary nephron Renal pyramid Interlobar vein Interlobar artery Minor calyx b Circulation in a single kidney lobe
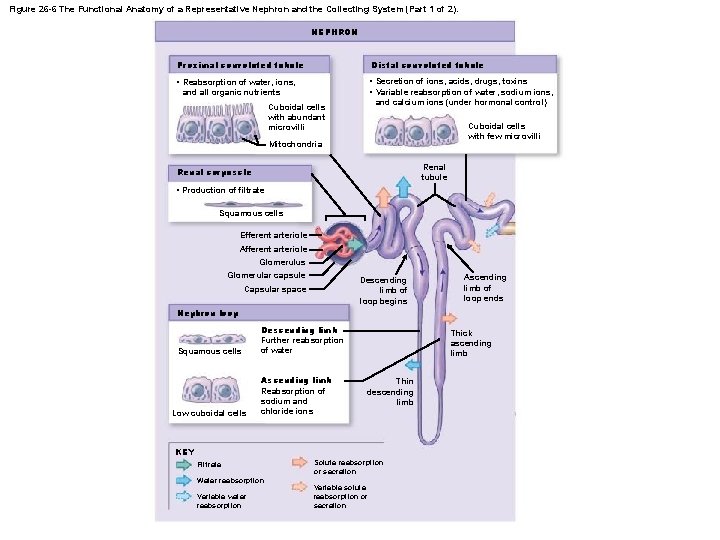
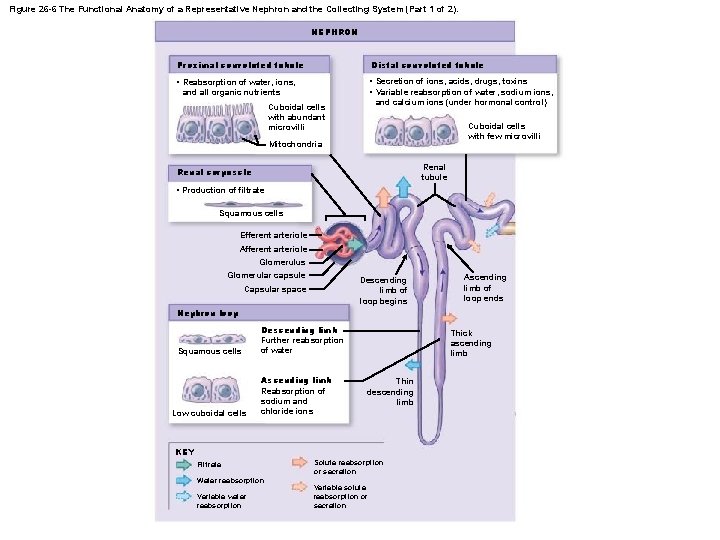
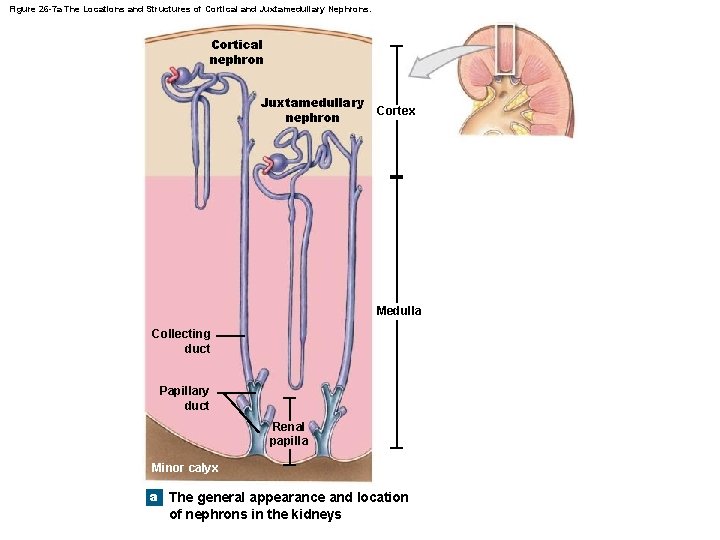
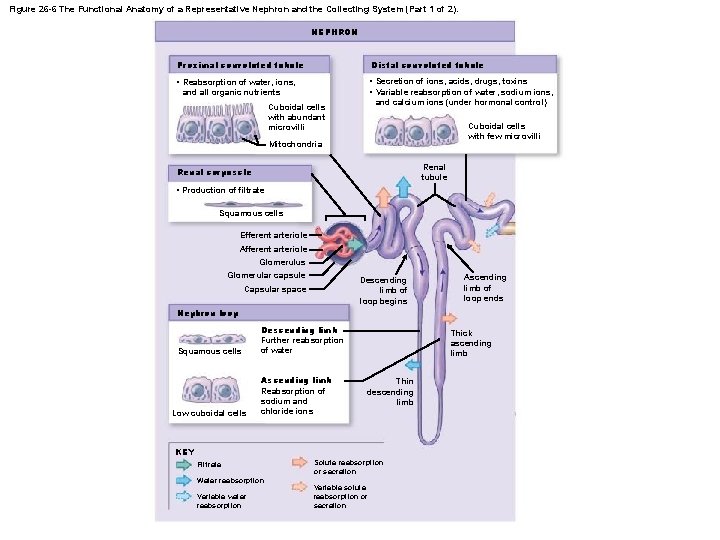
Figure 26 -6 The Functional Anatomy of a Representative Nephron and the Collecting System (Part 1 of 2). NEPHRON Proximal convoluted tubule Distal convoluted tubule • Reabsorption of water, ions, and all organic nutrients • Secretion of ions, acids, drugs, toxins • Variable reabsorption of water, sodium ions, and calcium ions (under hormonal control) Cuboidal cells with abundant microvilli Cuboidal cells with few microvilli Mitochondria Renal tubule Renal corpuscle • Production of filtrate Squamous cells Efferent arteriole Afferent arteriole Glomerulus Glomerular capsule Descending limb of loop begins Capsular space Ascending limb of loop ends Nephron loop Squamous cells Low cuboidal cells Descending limb Further reabsorption of water Ascending limb Reabsorption of sodium and chloride ions Thick ascending limb Thin descending limb KEY Filtrate Water reabsorption Variable water reabsorption Solute reabsorption or secretion Variable solute reabsorption or secretion
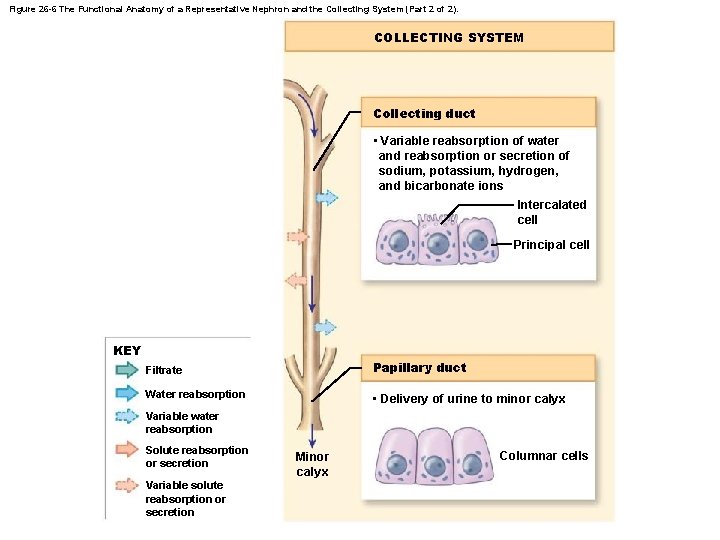
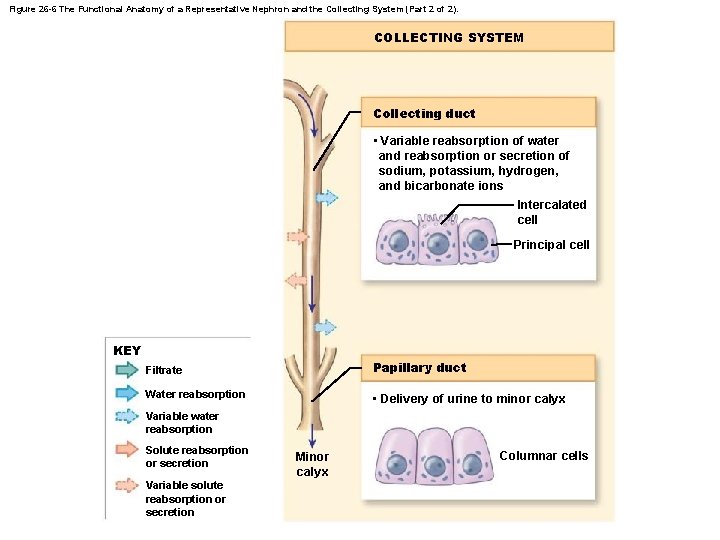
Figure 26 -6 The Functional Anatomy of a Representative Nephron and the Collecting System (Part 2 of 2). COLLECTING SYSTEM Collecting duct • Variable reabsorption of water and reabsorption or secretion of sodium, potassium, hydrogen, and bicarbonate ions Intercalated cell Principal cell KEY Filtrate Papillary duct Water reabsorption • Delivery of urine to minor calyx Variable water reabsorption Solute reabsorption or secretion Variable solute reabsorption or secretion Minor calyx Columnar cells

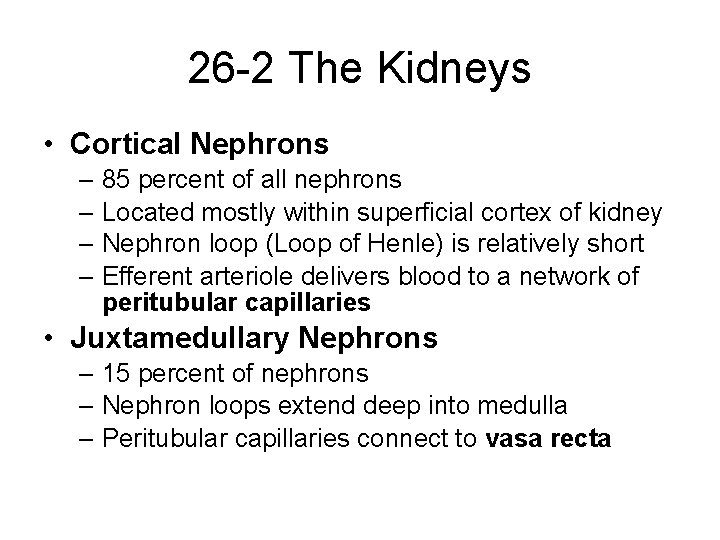
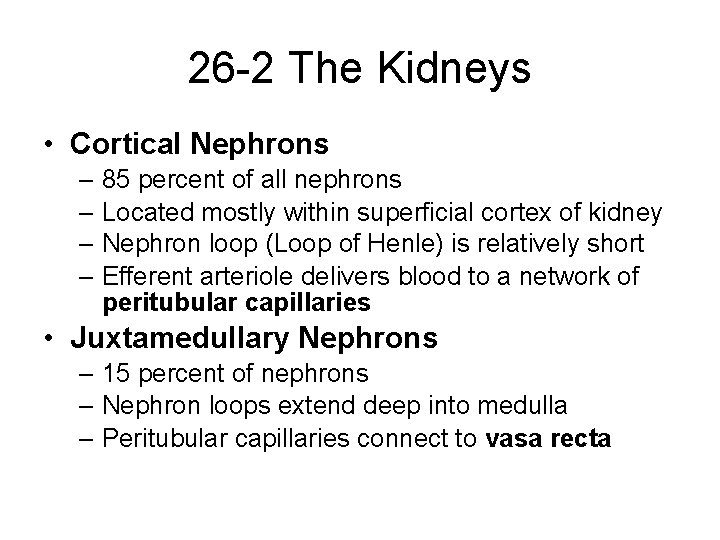
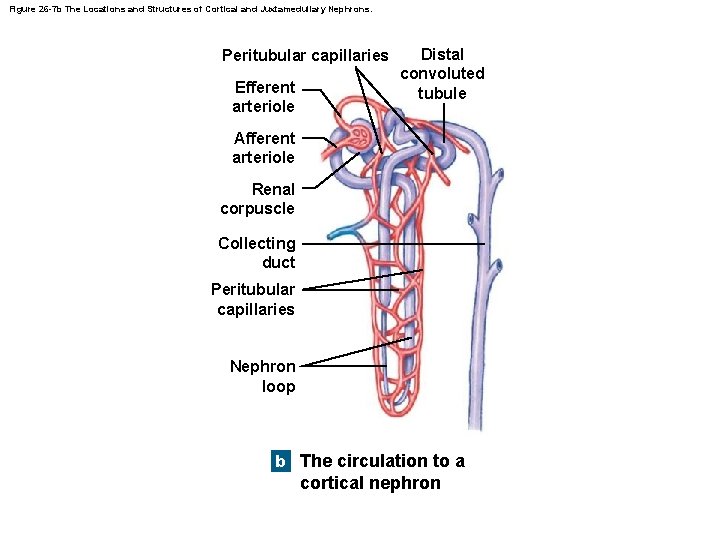
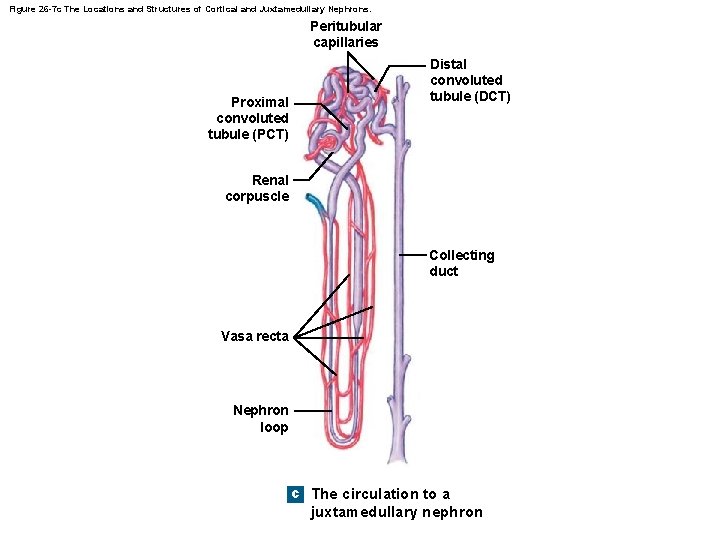
26 -2 The Kidneys • Cortical Nephrons – 85 percent of all nephrons – Located mostly within superficial cortex of kidney – Nephron loop (Loop of Henle) is relatively short – Efferent arteriole delivers blood to a network of peritubular capillaries • Juxtamedullary Nephrons – 15 percent of nephrons – Nephron loops extend deep into medulla – Peritubular capillaries connect to vasa recta
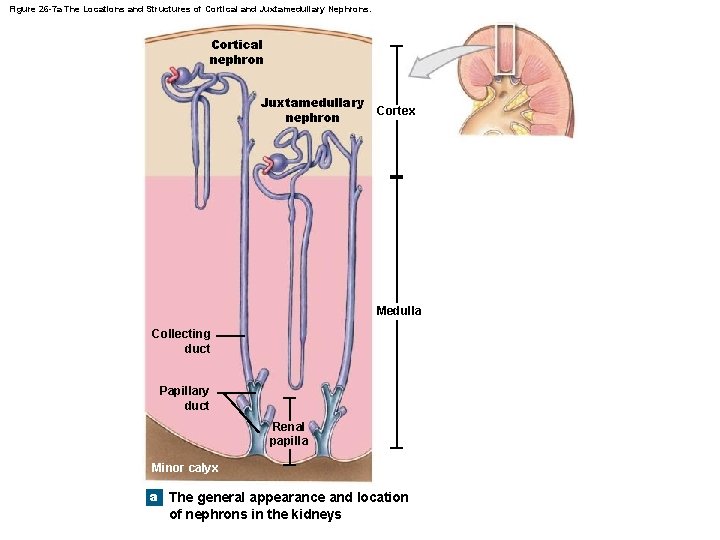
Figure 26 -7 a The Locations and Structures of Cortical and Juxtamedullary Nephrons. Cortical nephron Juxtamedullary nephron Cortex Medulla Collecting duct Papillary duct Renal papilla Minor calyx a The general appearance and location of nephrons in the kidneys
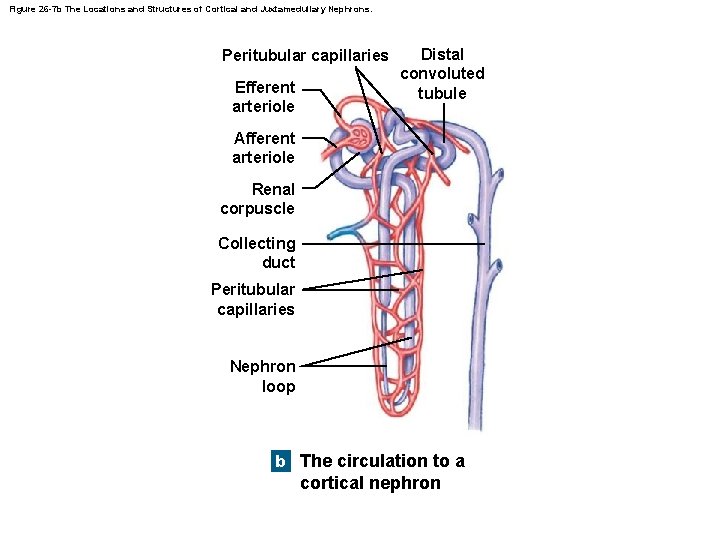
Figure 26 -7 b The Locations and Structures of Cortical and Juxtamedullary Nephrons. Peritubular capillaries Efferent arteriole Distal convoluted tubule Afferent arteriole Renal corpuscle Collecting duct Peritubular capillaries Nephron loop b The circulation to a cortical nephron
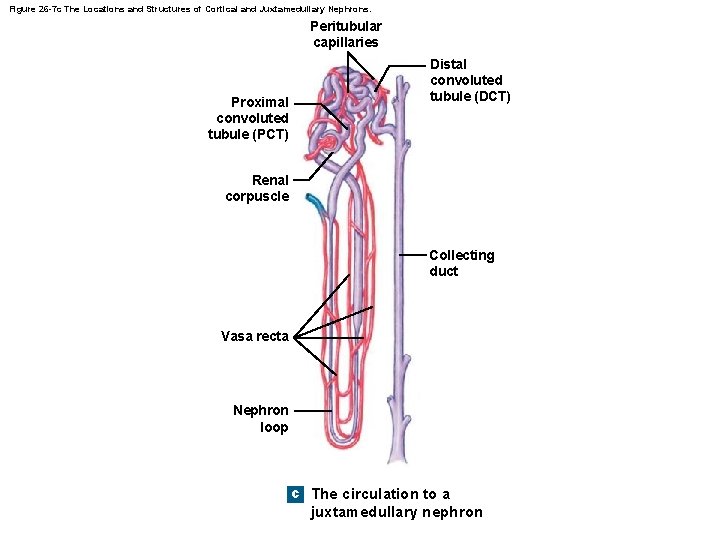
Figure 26 -7 c The Locations and Structures of Cortical and Juxtamedullary Nephrons. Peritubular capillaries Proximal convoluted tubule (PCT) Distal convoluted tubule (DCT) Renal corpuscle Collecting duct Vasa recta Nephron loop c The circulation to a juxtamedullary nephron
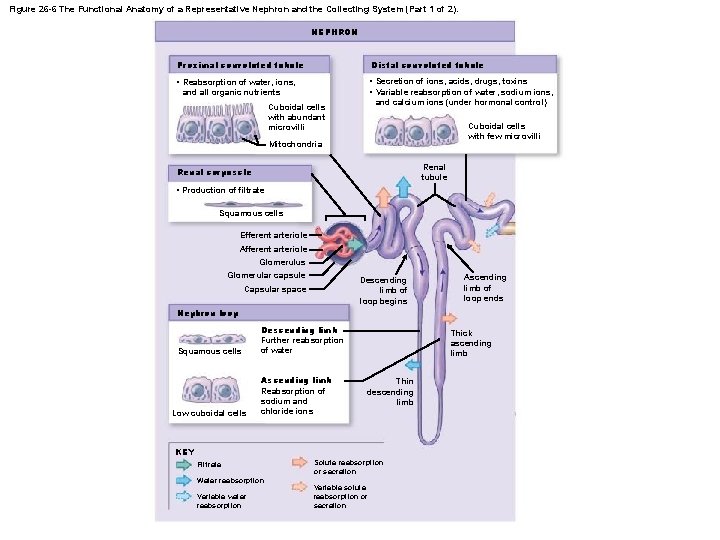
Figure 26 -6 The Functional Anatomy of a Representative Nephron and the Collecting System (Part 1 of 2). NEPHRON Proximal convoluted tubule Distal convoluted tubule • Reabsorption of water, ions, and all organic nutrients • Secretion of ions, acids, drugs, toxins • Variable reabsorption of water, sodium ions, and calcium ions (under hormonal control) Cuboidal cells with abundant microvilli Cuboidal cells with few microvilli Mitochondria Renal tubule Renal corpuscle • Production of filtrate Squamous cells Efferent arteriole Afferent arteriole Glomerulus Glomerular capsule Descending limb of loop begins Capsular space Ascending limb of loop ends Nephron loop Squamous cells Low cuboidal cells Descending limb Further reabsorption of water Ascending limb Reabsorption of sodium and chloride ions Thick ascending limb Thin descending limb KEY Filtrate Water reabsorption Variable water reabsorption Solute reabsorption or secretion Variable solute reabsorption or secretion
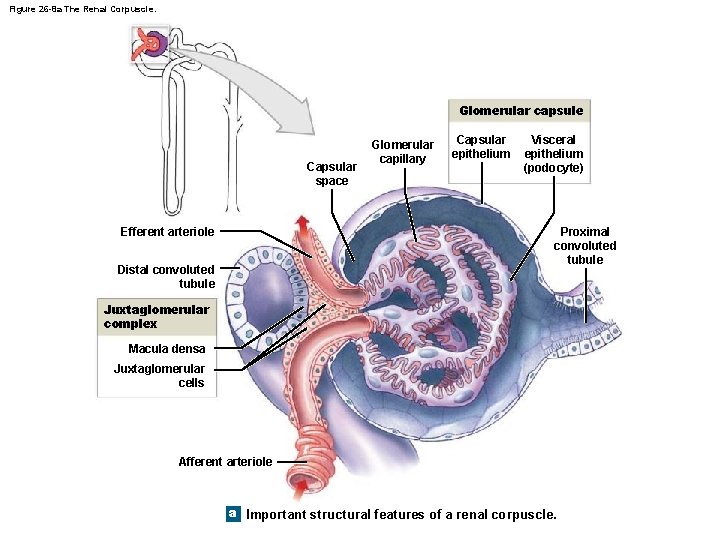
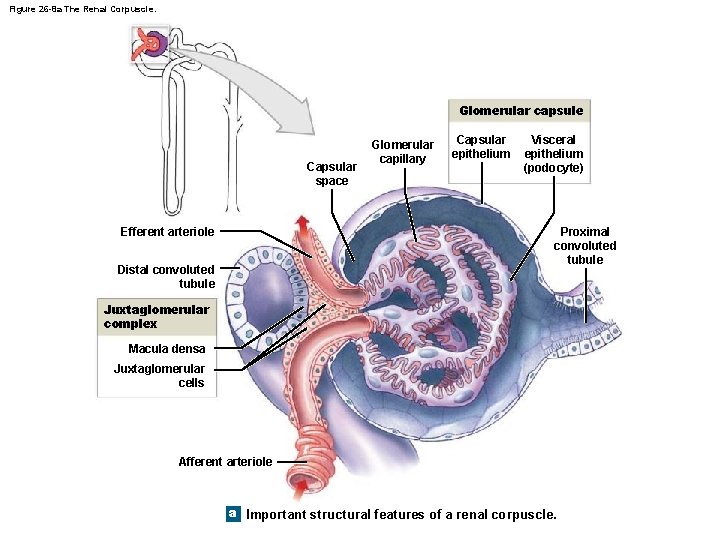
Figure 26 -8 a The Renal Corpuscle. Glomerular capsule Capsular space Efferent arteriole Glomerular capillary Capsular epithelium Visceral epithelium (podocyte) Proximal convoluted tubule Distal convoluted tubule Juxtaglomerular complex Macula densa Juxtaglomerular cells Afferent arteriole a Important structural features of a renal corpuscle.
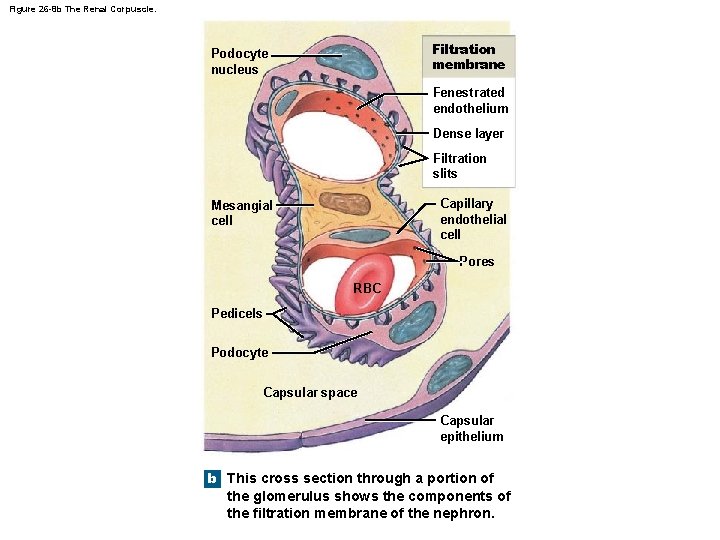
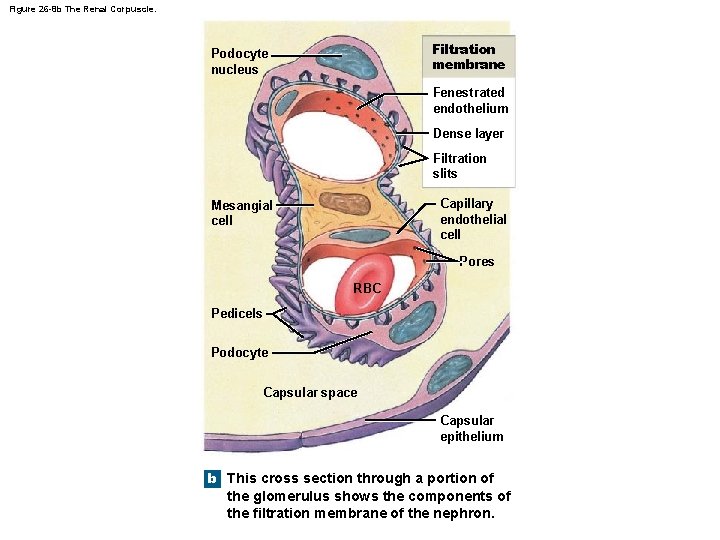
Figure 26 -8 b The Renal Corpuscle. Filtration membrane Podocyte nucleus Fenestrated endothelium Dense layer Filtration slits Capillary endothelial cell Mesangial cell Pores RBC Pedicels Podocyte Capsular space Capsular epithelium b This cross section through a portion of the glomerulus shows the components of the filtration membrane of the nephron.
26 -2 The Kidneys • The Glomerular Capillaries – Are fenestrated capillaries • Endothelium contains large-diameter pores • Blood Flow Control – Special supporting cells (mesangial cells) • Between adjacent capillaries • Control diameter and rate of capillary blood flow
26 -2 The Kidneys • The Filtration Membrane – Consists of: • Fenestrated endothelium • Dense layer • Filtration slits
26 -2 The Kidneys • The Juxtaglomerular Complex (JGC) – An endocrine structure that secretes: • Hormone erythropoietin • Enzyme renin – Formed by: • Macula densa • Juxtaglomerular cells
26 -2 The Kidneys • Macula Densa – Epithelial cells of DCT, near renal corpuscle – Tall cells with densely clustered nuclei • Juxtaglomerular Cells – Smooth muscle fibers in wall of afferent arteriole • Associated with cells of macula densa • Together with macula densa forms juxtaglomerular complex (JGC)
26 -2 The Kidneys • Filtration – Blood pressure • Forces water and small solutes across membrane into capsular space – Larger solutes, such as plasma proteins, are excluded
26 -2 The Kidneys • Filtration at Renal Corpuscle – Is passive – Solutes enter capsular space • Metabolic wastes and excess ions • Glucose, free fatty acids, amino acids, and vitamins • Reabsorption – Useful materials are recaptured before filtrate leaves kidneys – Reabsorption occurs in proximal convoluted tubule
26 -2 The Kidneys • The Proximal Convoluted Tubule (PCT) – Is the first segment of renal tubule – Entrance to PCT lies opposite point of connection of afferent and efferent arterioles with glomerulus • Epithelial Lining of PCT – Is simple cuboidal – Has microvilli on apical surfaces – Functions in reabsorption – Secretes substances into lumen
26 -2 The Kidneys • Tubular Cells – Absorb organic nutrients, ions, water, and plasma proteins from tubular fluid – Release them into peritubular fluid (interstitial fluid around renal tubule)
26 -2 The Kidneys • The Nephron Loop (Loop of Henle) – Renal tubule turns toward renal medulla – Descending limb • Fluid flows toward renal pelvis – Ascending limb • Fluid flows toward renal cortex – Each limb contains: • Thick segment • Thin segment
26 -2 The Kidneys • The Thick Descending Limb – Has functions similar to PCT • Pumps sodium and chloride ions out of tubular fluid • Ascending Limbs – Of juxtamedullary nephrons in medulla • Create high solute concentrations in peritubular fluid
26 -2 The Kidneys • The Thin Segments – Are freely permeable to water • Not to solutes – Water movement helps concentrate tubular fluid • The Thick Ascending Limb – Ends at a sharp angle near the renal corpuscle • Where DCT begins
26 -2 The Kidneys • The Distal Convoluted Tubule (DCT) – The third segment of the renal tubule – Initial portion passes between afferent and efferent arterioles – Has a smaller diameter than PCT – Epithelial cells lack microvilli
26 -2 The Kidneys • Three Processes at the DCT 1. Active secretion of ions, acids, drugs, and toxins 2. Selective reabsorption of sodium and calcium ions from tubular fluid 3. Selective reabsorption of water • Concentrates tubular fluid
26 -2 The Kidneys • The Collecting System – The distal convoluted tubule opens into the collecting system – Individual nephrons drain into a nearby collecting duct – Several collecting ducts: • Converge into a larger papillary duct • Which empties into a minor calyx – Transports tubular fluid from nephron to renal pelvis – Adjusts fluid composition – Determines final osmotic concentration and volume of urine

26 -3 Renal Physiology • The Goal of Urine Production – Is to maintain homeostasis • By regulating volume and composition of blood • Including excretion of metabolic waste products
26 -3 Renal Physiology • Three Organic Waste Products 1. Urea 2. Creatinine 3. Uric acid • Organic Waste Products – Are dissolved in bloodstream – Are eliminated only while dissolved in urine – Removal is accompanied by water loss
26 -3 Renal Physiology • Basic Processes of Urine Formation 1. Filtration 2. Reabsorption 3. Secretion
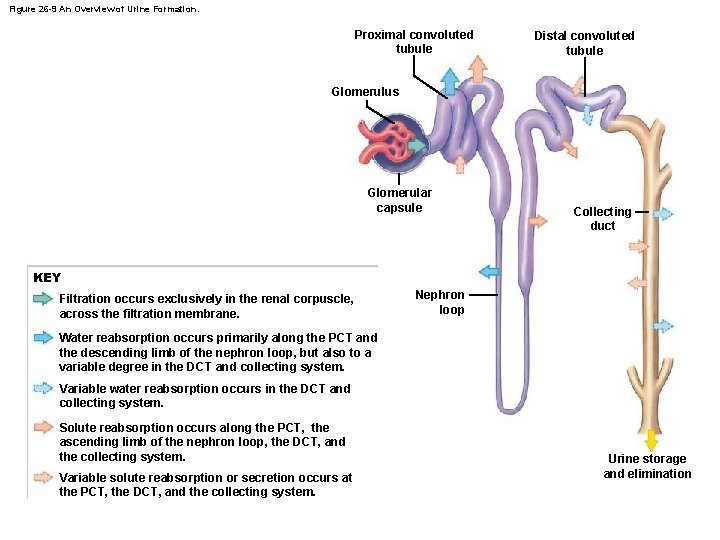
26 -3 Renal Physiology • An Overview of Renal Function – Water and solute reabsorption • Primarily along proximal convoluted tubules – Active secretion • Primarily at proximal and distal convoluted tubules – Long loops of juxtamedullary nephrons and collecting system • Regulate final volume and solute concentration of urine
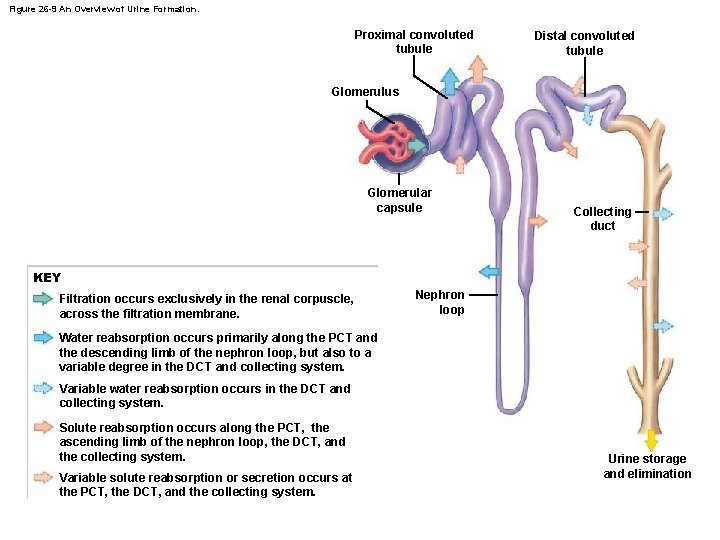
Figure 26 -9 An Overview of Urine Formation. Proximal convoluted tubule Distal convoluted tubule Glomerulus Glomerular capsule Collecting duct KEY Filtration occurs exclusively in the renal corpuscle, across the filtration membrane. Nephron loop Water reabsorption occurs primarily along the PCT and the descending limb of the nephron loop, but also to a variable degree in the DCT and collecting system. Variable water reabsorption occurs in the DCT and collecting system. Solute reabsorption occurs along the PCT, the ascending limb of the nephron loop, the DCT, and the collecting system. Variable solute reabsorption or secretion occurs at the PCT, the DCT, and the collecting system. Urine storage and elimination
26 -3 Renal Physiology • Filtration – Hydrostatic pressure forces water through membrane pores • Small solute molecules pass through pores • Larger solutes and suspended materials are retained – Occurs across capillary walls • As water and dissolved materials are pushed into interstitial fluids
26 -3 Renal Physiology • Reabsorption and Secretion – At the kidneys, it involves: • • Diffusion Osmosis Channel-mediated diffusion Carrier-mediated transport
26 -3 Renal Physiology • Renal Threshold – Is the plasma concentration at which: • A specific compound or ion begins to appear in urine – Varies with the substance involved
26 -3 Renal Physiology • Renal Threshold for Glucose – Is approximately 180 mg/d. L – If plasma glucose is greater than 180 mg/d. L: • Tm of tubular cells is exceeded • Glucose appears in urine – Glycosuria
26 -3 Renal Physiology • Renal Threshold for Amino Acids – Is lower than glucose (65 mg/d. L) – Amino acids commonly appear in urine • After a protein-rich meal • Aminoaciduria
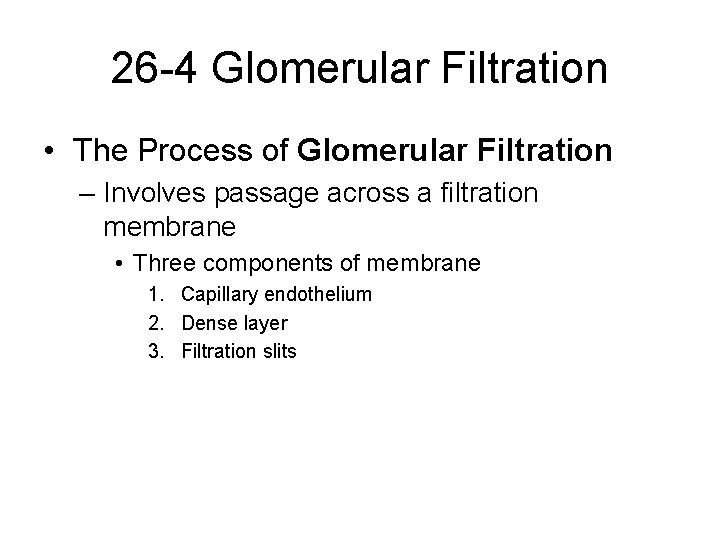
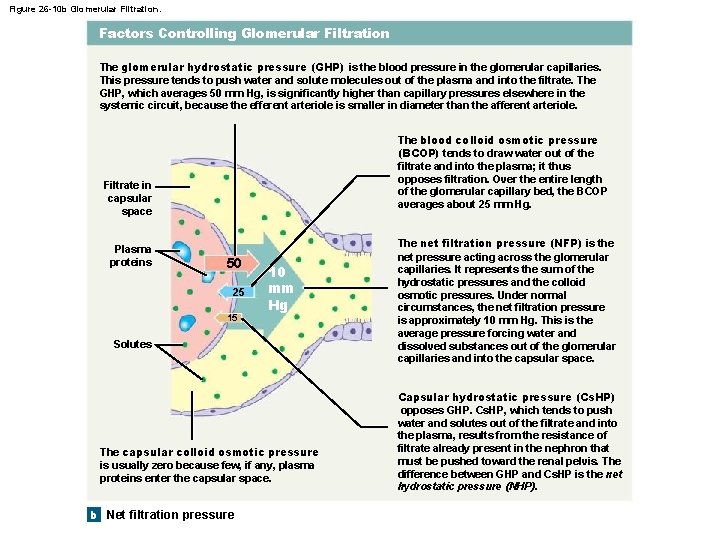
26 -4 Glomerular Filtration • The Process of Glomerular Filtration – Involves passage across a filtration membrane • Three components of membrane 1. Capillary endothelium 2. Dense layer 3. Filtration slits
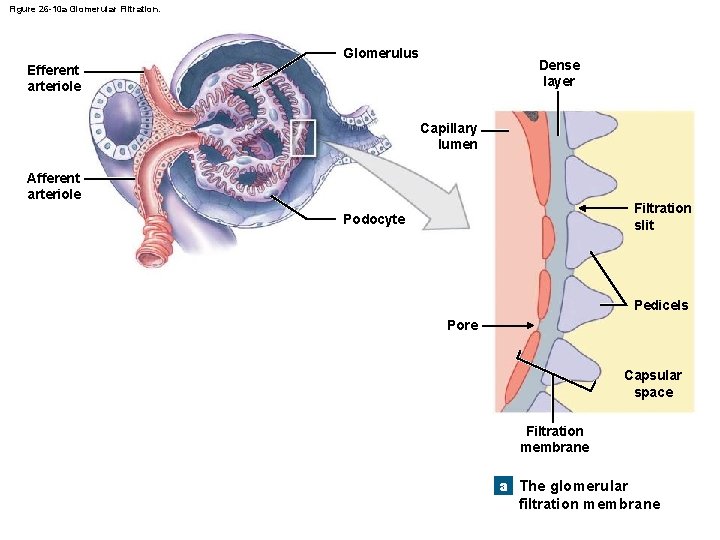
Figure 26 -10 a Glomerular Filtration. Glomerulus Dense layer Efferent arteriole Capillary lumen Afferent arteriole Filtration slit Podocyte Pedicels Pore Capsular space Filtration membrane a The glomerular filtration membrane
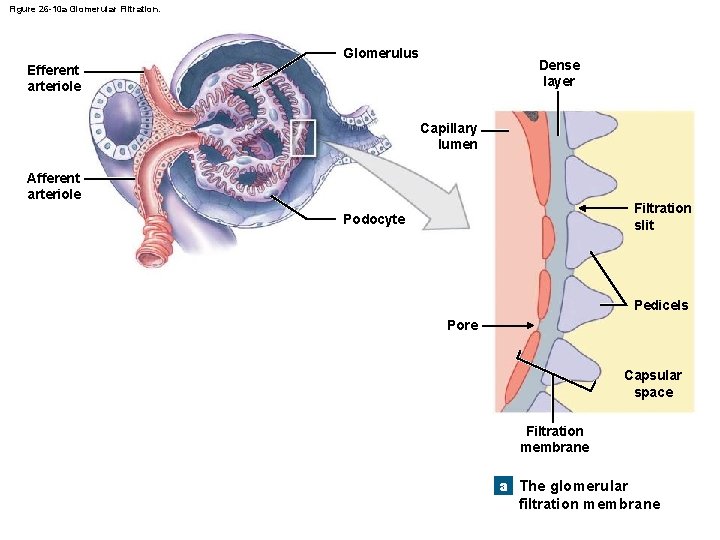
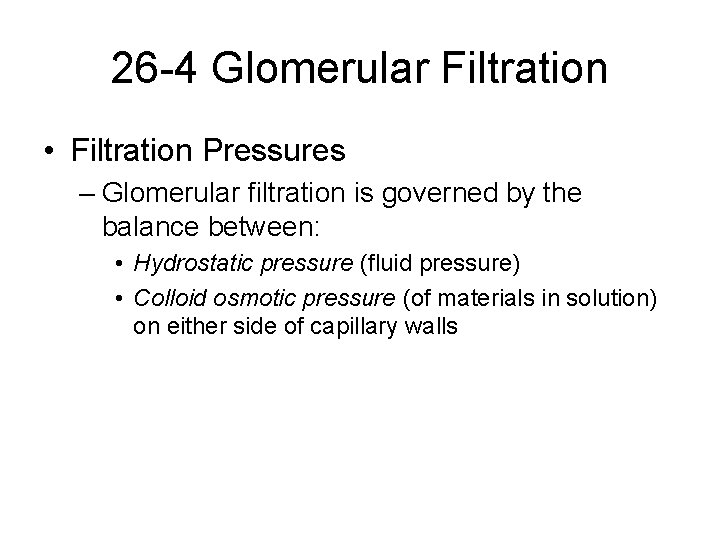
26 -4 Glomerular Filtration • Filtration Pressures – Glomerular filtration is governed by the balance between: • Hydrostatic pressure (fluid pressure) • Colloid osmotic pressure (of materials in solution) on either side of capillary walls
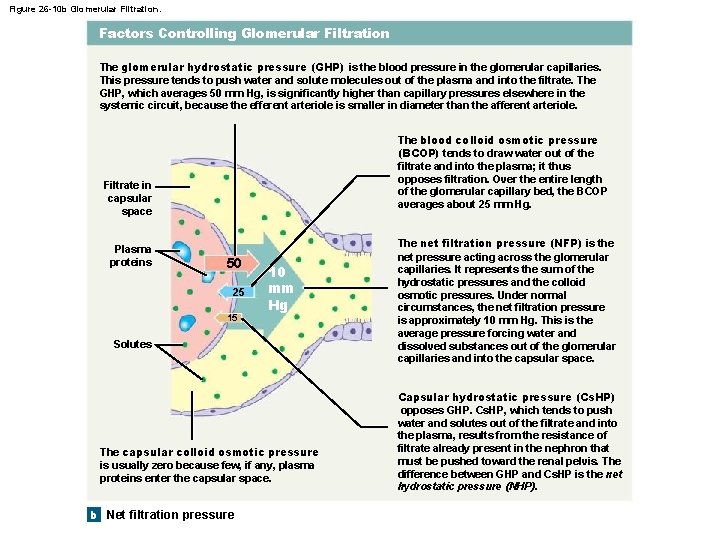
Figure 26 -10 b Glomerular Filtration. Factors Controlling Glomerular Filtration The glomerular hydrostatic pressure (GHP) is the blood pressure in the glomerular capillaries. This pressure tends to push water and solute molecules out of the plasma and into the filtrate. The GHP, which averages 50 mm Hg, is significantly higher than capillary pressures elsewhere in the systemic circuit, because the efferent arteriole is smaller in diameter than the afferent arteriole. The blood colloid osmotic pressure (BCOP) tends to draw water out of the filtrate and into the plasma; it thus opposes filtration. Over the entire length of the glomerular capillary bed, the BCOP averages about 25 mm Hg. Filtrate in capsular space Plasma proteins 50 25 15 10 mm Hg Solutes The capsular colloid osmotic pressure is usually zero because few, if any, plasma proteins enter the capsular space. b Net filtration pressure The net filtration pressure (NFP) is the net pressure acting across the glomerular capillaries. It represents the sum of the hydrostatic pressures and the colloid osmotic pressures. Under normal circumstances, the net filtration pressure is approximately 10 mm Hg. This is the average pressure forcing water and dissolved substances out of the glomerular capillaries and into the capsular space. Capsular hydrostatic pressure (Cs. HP) opposes GHP. Cs. HP, which tends to push water and solutes out of the filtrate and into the plasma, results from the resistance of filtrate already present in the nephron that must be pushed toward the renal pelvis. The difference between GHP and Cs. HP is the net hydrostatic pressure (NHP).
26 -4 Glomerular Filtration • The Glomerular Filtration Rate (GFR) – Is the amount of filtrate kidneys produce each minute – Averages 125 m. L/min – About 10 percent of fluid delivered to kidneys • Leaves bloodstream • Enters capsular spaces
26 -4 Glomerular Filtration • Creatinine (waste product of muscle metabolism of creatinine) Clearance Test – Is used to estimate GFR – A more accurate GFR test uses inulin (naturally occurring plant polysaccharide) • Which is not metabolized • Filtrate – Glomeruli generate about 180 liters of filtrate per day • 99 percent is reabsorbed in renal tubules
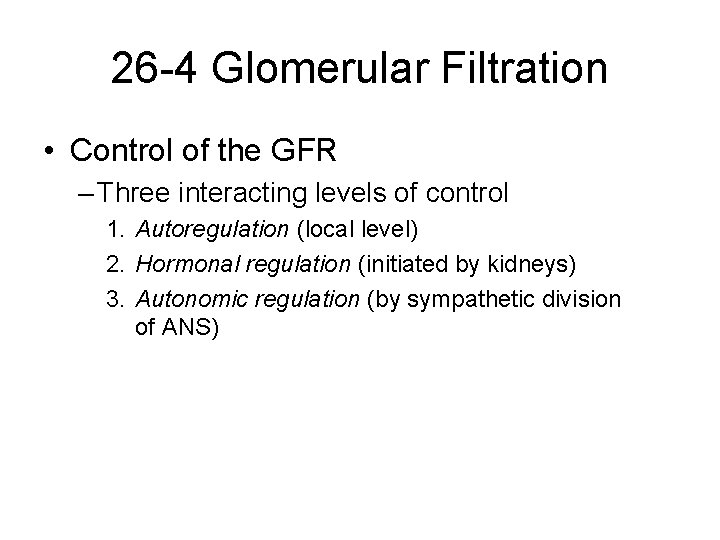
26 -4 Glomerular Filtration • Control of the GFR – Three interacting levels of control 1. Autoregulation (local level) 2. Hormonal regulation (initiated by kidneys) 3. Autonomic regulation (by sympathetic division of ANS)
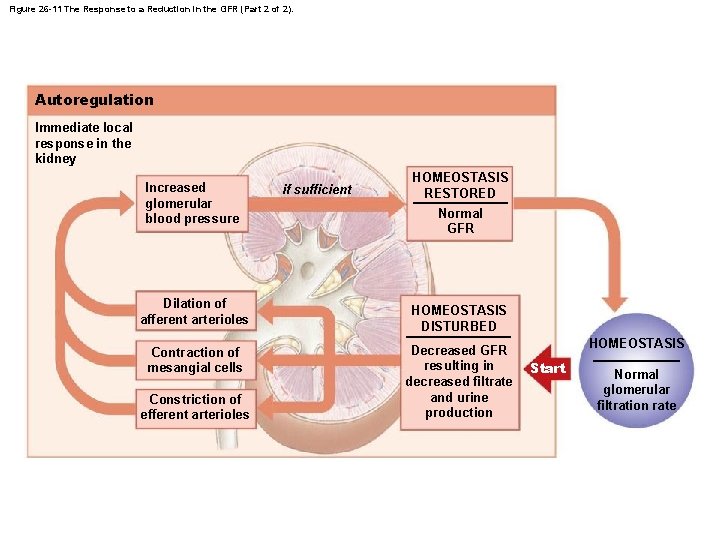
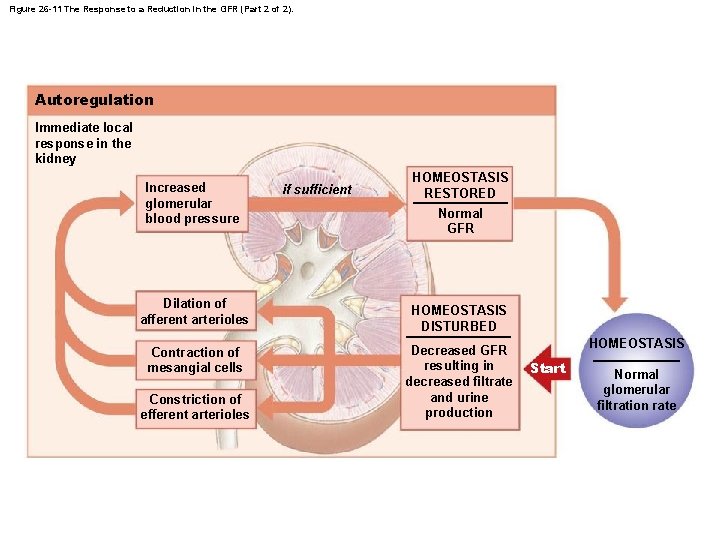
Figure 26 -11 The Response to a Reduction in the GFR (Part 2 of 2). Autoregulation Immediate local response in the kidney Increased glomerular blood pressure Dilation of afferent arterioles Contraction of mesangial cells Constriction of efferent arterioles if sufficient HOMEOSTASIS RESTORED Normal GFR HOMEOSTASIS DISTURBED Decreased GFR resulting in decreased filtrate and urine production HOMEOSTASIS Start Normal glomerular filtration rate
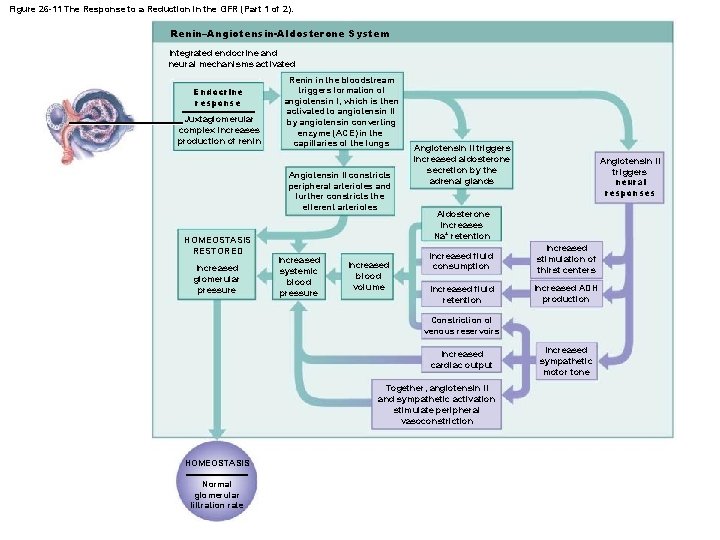
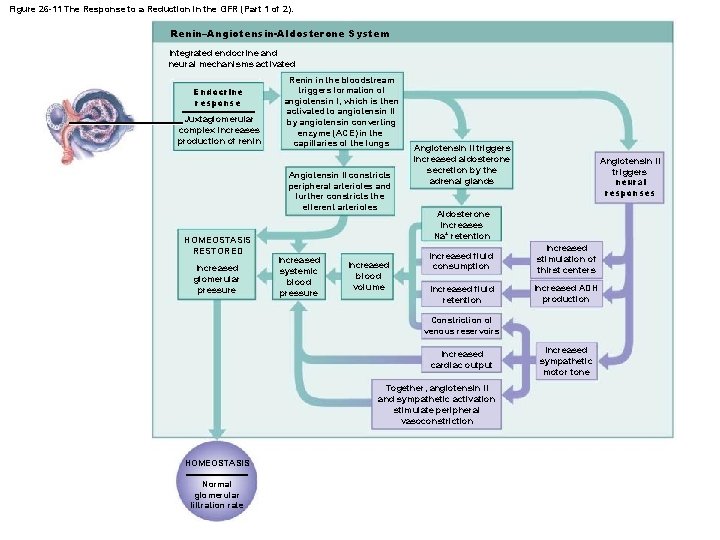
Figure 26 -11 The Response to a Reduction in the GFR (Part 1 of 2). Renin–Angiotensin-Aldosterone System Integrated endocrine and neural mechanisms activated Endocrine response Juxtaglomerular complex increases production of renin Renin in the bloodstream triggers formation of angiotensin I, which is then activated to angiotensin II by angiotensin converting enzyme (ACE) in the capillaries of the lungs Angiotensin II constricts peripheral arterioles and further constricts the efferent arterioles HOMEOSTASIS RESTORED Increased glomerular pressure Increased systemic blood pressure Increased blood volume Angiotensin II triggers increased aldosterone secretion by the adrenal glands Angiotensin II triggers neural responses Aldosterone increases Na+ retention Increased fluid consumption Increased stimulation of thirst centers Increased fluid retention Increased ADH production Constriction of venous reservoirs Increased cardiac output Together, angiotensin II and sympathetic activation stimulate peripheral vasoconstriction HOMEOSTASIS Normal glomerular filtration rate Increased sympathetic motor tone
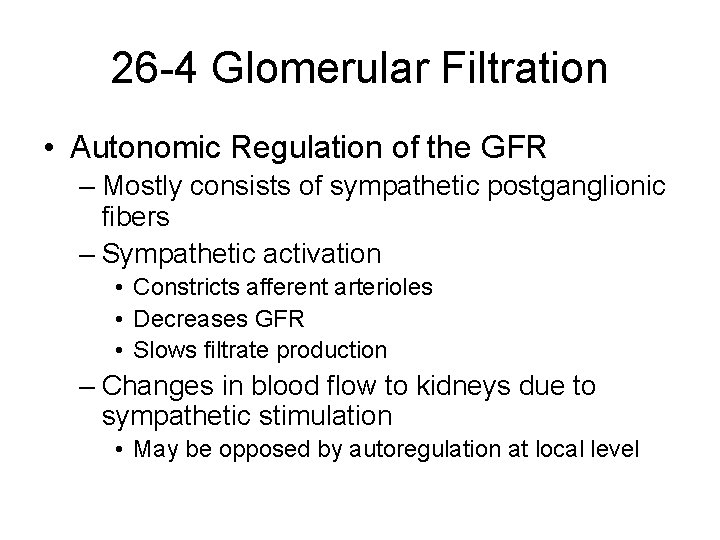
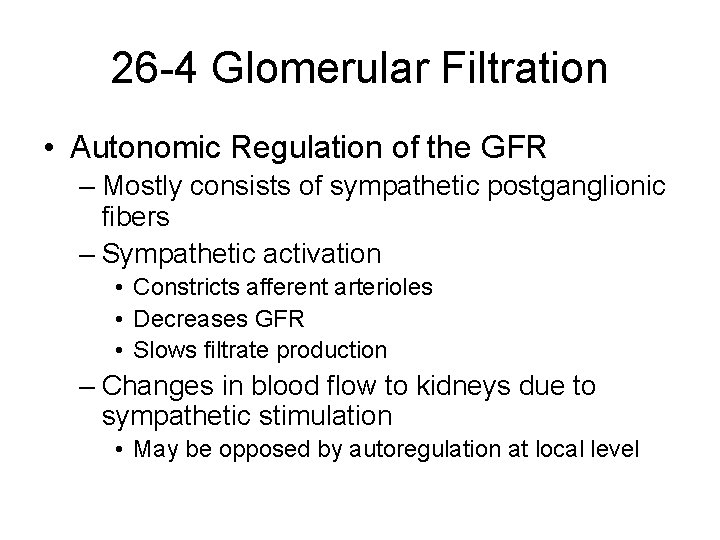
26 -4 Glomerular Filtration • Autonomic Regulation of the GFR – Mostly consists of sympathetic postganglionic fibers – Sympathetic activation • Constricts afferent arterioles • Decreases GFR • Slows filtrate production – Changes in blood flow to kidneys due to sympathetic stimulation • May be opposed by autoregulation at local level
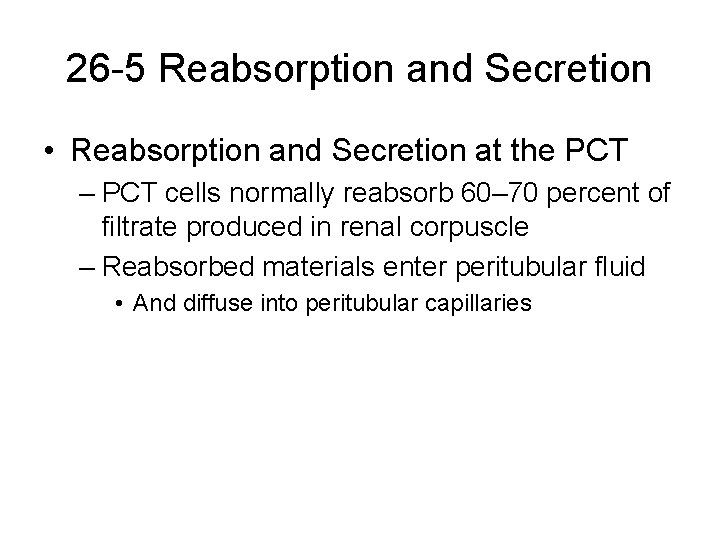
26 -5 Reabsorption and Secretion • Reabsorption and Secretion at the PCT – PCT cells normally reabsorb 60– 70 percent of filtrate produced in renal corpuscle – Reabsorbed materials enter peritubular fluid • And diffuse into peritubular capillaries
26 -5 Reabsorption and Secretion • Five Functions of the PCT 1. 2. 3. 4. 5. Reabsorption of organic nutrients Active reabsorption of ions Reabsorption of water Passive reabsorption of ions Secretion
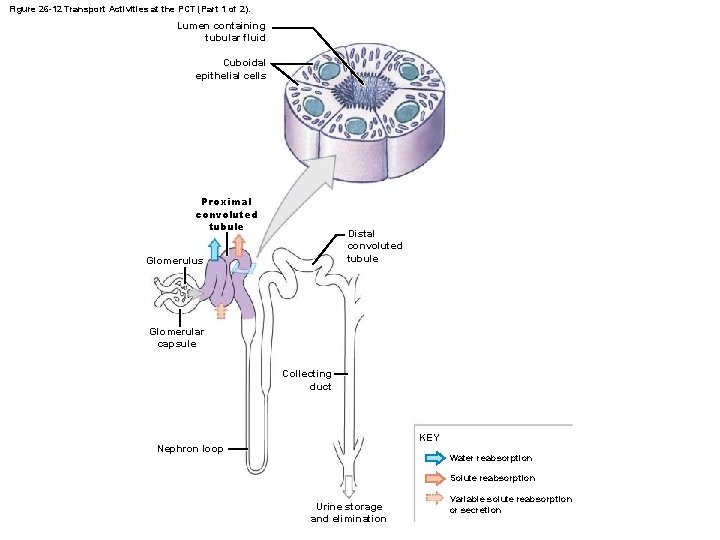
Figure 26 -12 Transport Activities at the PCT (Part 1 of 2). Lumen containing tubular fluid Cuboidal epithelial cells Proximal convoluted tubule Distal convoluted tubule Glomerulus Glomerular capsule Collecting duct KEY Nephron loop Water reabsorption Solute reabsorption Urine storage and elimination Variable solute reabsorption or secretion
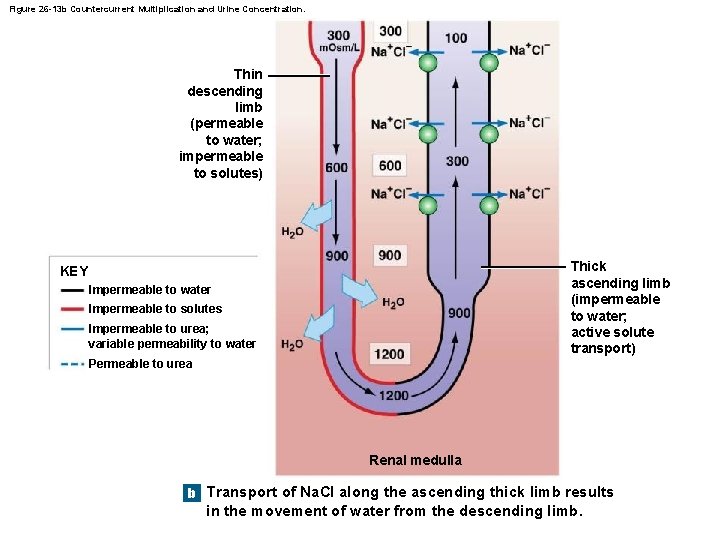
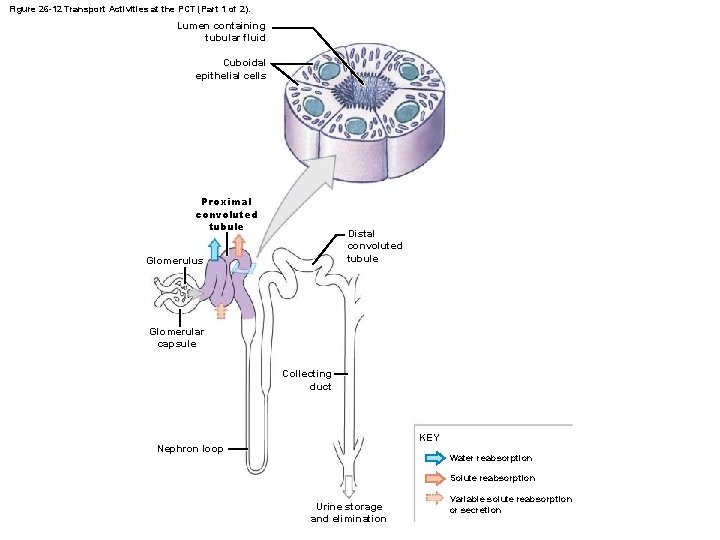
Figure 26 -13 b Countercurrent Multiplication and Urine Concentration. Thin descending limb (permeable to water; impermeable to solutes) Thick ascending limb (impermeable to water; active solute transport) KEY Impermeable to water Impermeable to solutes Impermeable to urea; variable permeability to water Permeable to urea Renal medulla b Transport of Na. Cl along the ascending thick limb results in the movement of water from the descending limb.
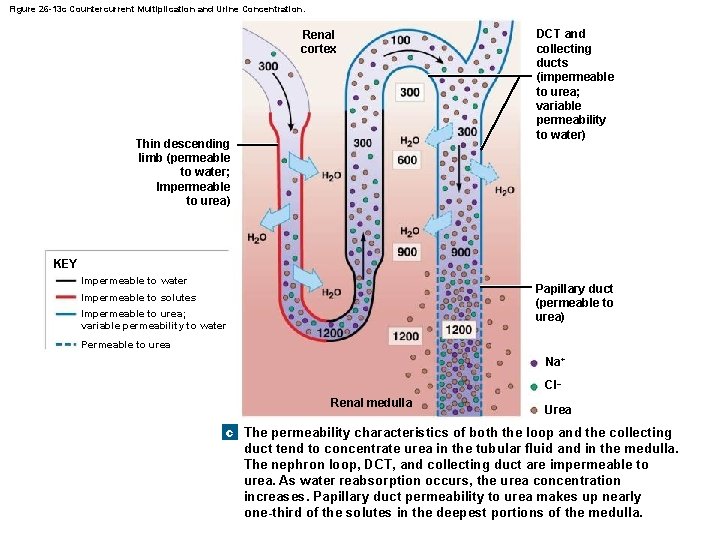
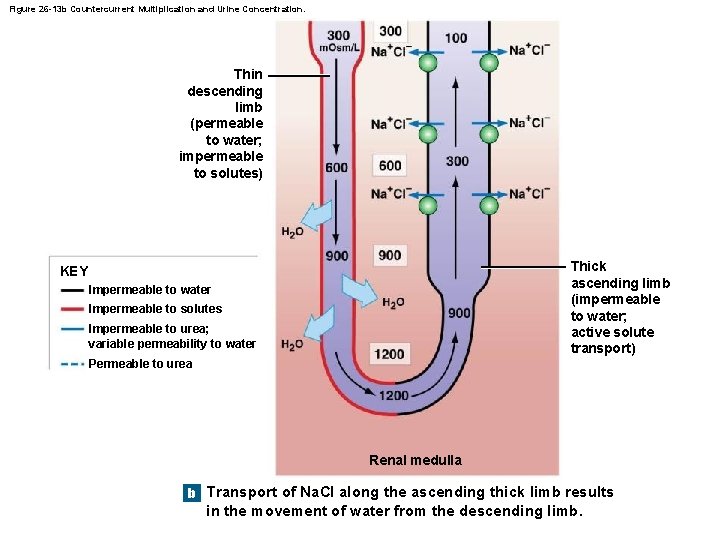
Figure 26 -13 c Countercurrent Multiplication and Urine Concentration. Renal cortex Thin descending limb (permeable to water; Impermeable to urea) DCT and collecting ducts (impermeable to urea; variable permeability to water) KEY Impermeable to water Papillary duct (permeable to urea) Impermeable to solutes Impermeable to urea; variable permeability to water Permeable to urea Na+ Cl– Renal medulla Urea c The permeability characteristics of both the loop and the collecting duct tend to concentrate urea in the tubular fluid and in the medulla. The nephron loop, DCT, and collecting duct are impermeable to urea. As water reabsorption occurs, the urea concentration increases. Papillary duct permeability to urea makes up nearly one-third of the solutes in the deepest portions of the medulla.
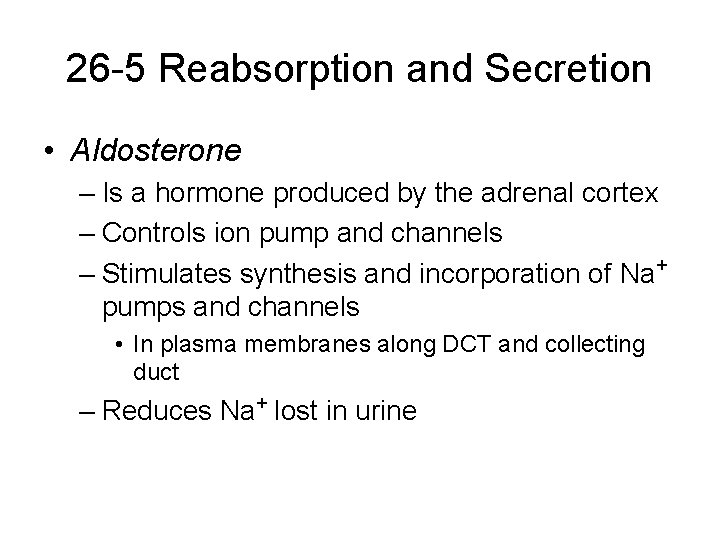
26 -5 Reabsorption and Secretion • Aldosterone – Is a hormone produced by the adrenal cortex – Controls ion pump and channels – Stimulates synthesis and incorporation of Na+ pumps and channels • In plasma membranes along DCT and collecting duct – Reduces Na+ lost in urine
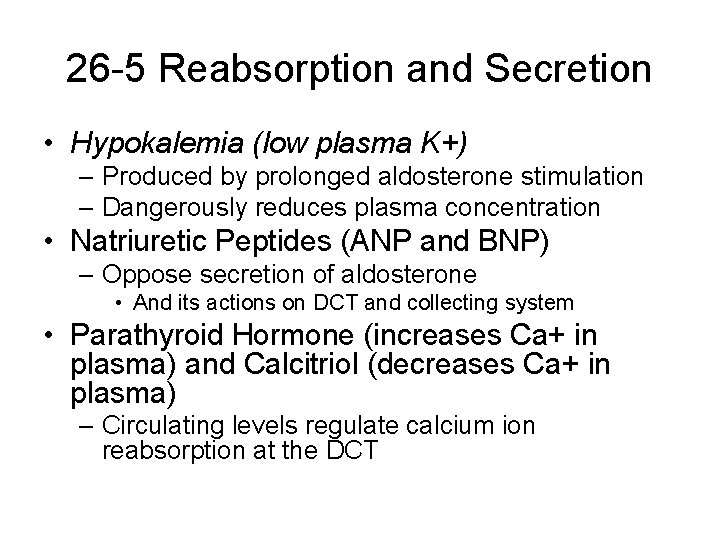
26 -5 Reabsorption and Secretion • Hypokalemia (low plasma K+) – Produced by prolonged aldosterone stimulation – Dangerously reduces plasma concentration • Natriuretic Peptides (ANP and BNP) – Oppose secretion of aldosterone • And its actions on DCT and collecting system • Parathyroid Hormone (increases Ca+ in plasma) and Calcitriol (decreases Ca+ in plasma) – Circulating levels regulate calcium ion reabsorption at the DCT
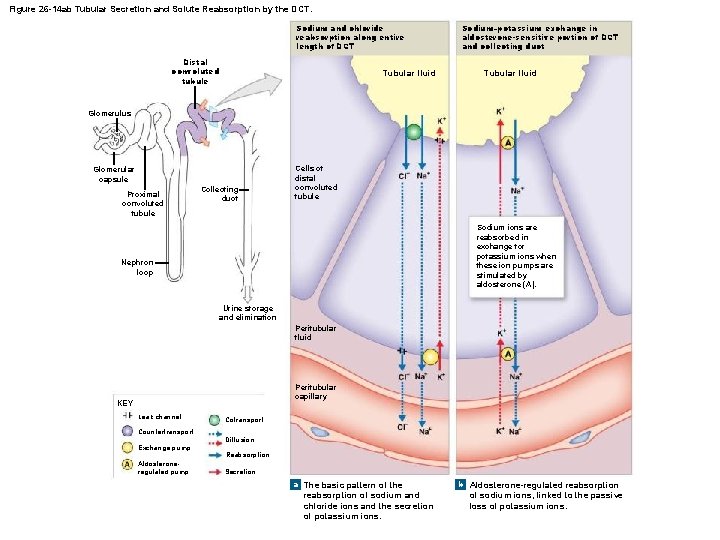
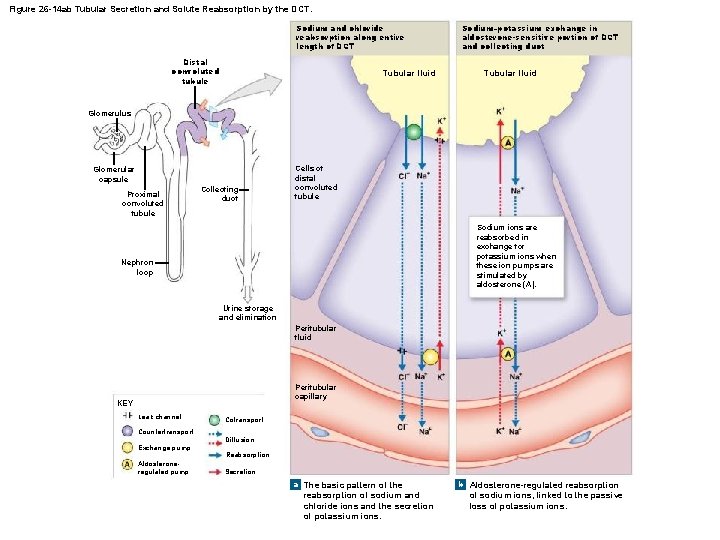
Figure 26 -14 ab Tubular Secretion and Solute Reabsorption by the DCT. Sodium and chloride reabsorption along entire length of DCT Distal convoluted tubule Tubular fluid Sodium–potassium exchange in aldosterone-sensitive portion of DCT and collecting duct Tubular fluid Glomerulus Glomerular capsule Proximal convoluted tubule Collecting duct Cells of distal convoluted tubule Sodium ions are reabsorbed in exchange for potassium ions when these ion pumps are stimulated by aldosterone (A). Nephron loop Urine storage and elimination Peritubular fluid Peritubular capillary KEY Leak channel Countertransport Exchange pump Aldosteroneregulated pump Cotransport Diffusion Reabsorption Secretion a The basic pattern of the reabsorption of sodium and chloride ions and the secretion of potassium ions. b Aldosterone-regulated reabsorption of sodium ions, linked to the passive loss of potassium ions.
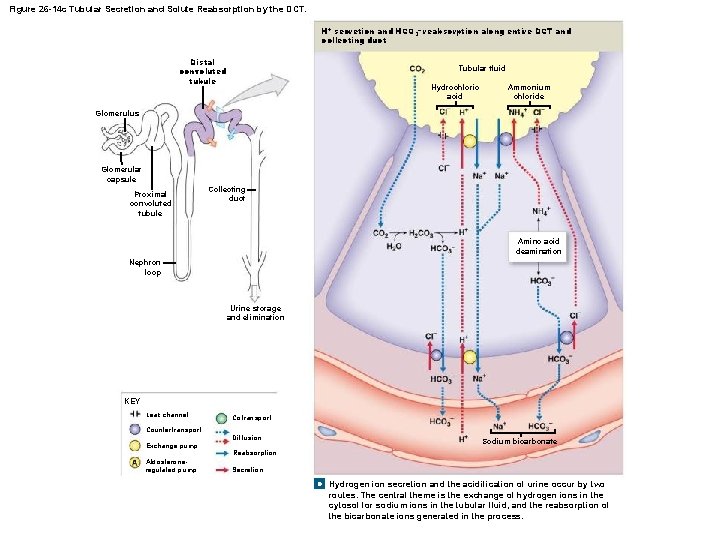
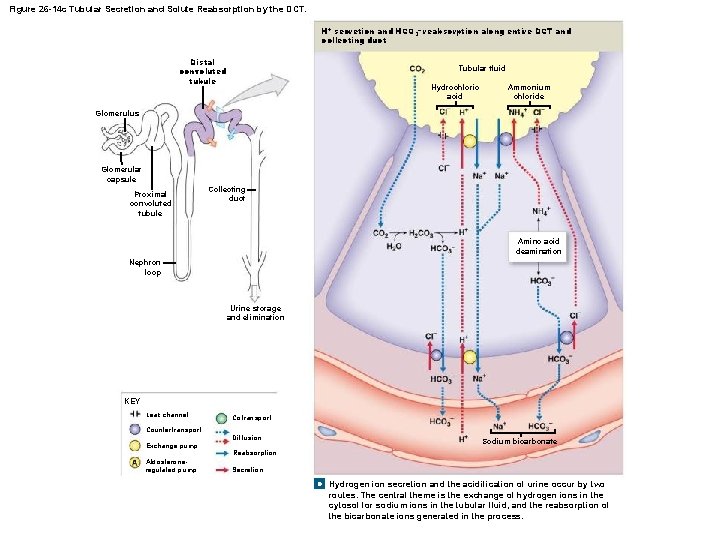
Figure 26 -14 c Tubular Secretion and Solute Reabsorption by the DCT. H+ secretion and HCO 3– reabsorption along entire DCT and collecting duct Distal convoluted tubule Tubular fluid Hydrochloric acid Ammonium chloride Glomerulus Glomerular capsule Proximal convoluted tubule Collecting duct Amino acid deamination Nephron loop Urine storage and elimination KEY Leak channel Countertransport Exchange pump Aldosteroneregulated pump Cotransport Diffusion Sodium bicarbonate Reabsorption Secretion c Hydrogen ion secretion and the acidification of urine occur by two routes. The central theme is the exchange of hydrogen ions in the cytosol for sodium ions in the tubular fluid, and the reabsorption of the bicarbonate ions generated in the process.
26 -5 Reabsorption and Secretion • Acidosis – Lactic acidosis • Develops after exhaustive muscle activity – Ketoacidosis • Develops in starvation or diabetes mellitus
26 -5 Reabsorption and Secretion • Water Reabsorption – Occurs when osmotic concentration of peritubular fluid exceeds that of tubular fluid – 1– 2 percent of water in original filtrate is recovered • During sodium ion reabsorption • In distal convoluted tubule and collecting system
26 -5 Reabsorption and Secretion • Obligatory Water Reabsorption – Is water movement that cannot be prevented – Usually recovers 85 percent of filtrate produced • Facultative Water Reabsorption – Controls volume of water reabsorbed along DCT and collecting system • 15 percent of filtrate volume (27 liters/day) • Segments are relatively impermeable to water • Except in presence of ADH
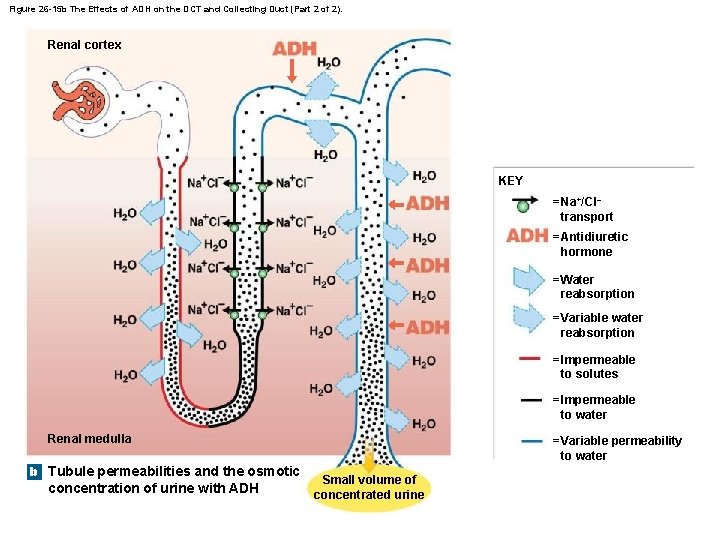
26 -5 Reabsorption and Secretion • ADH – Hormone that causes special water channels (aquaporins) to appear in apical cell membranes – Increases rate of osmotic water movement – Higher levels of ADH increase: • Number of water channels • Water permeability of DCT and collecting system
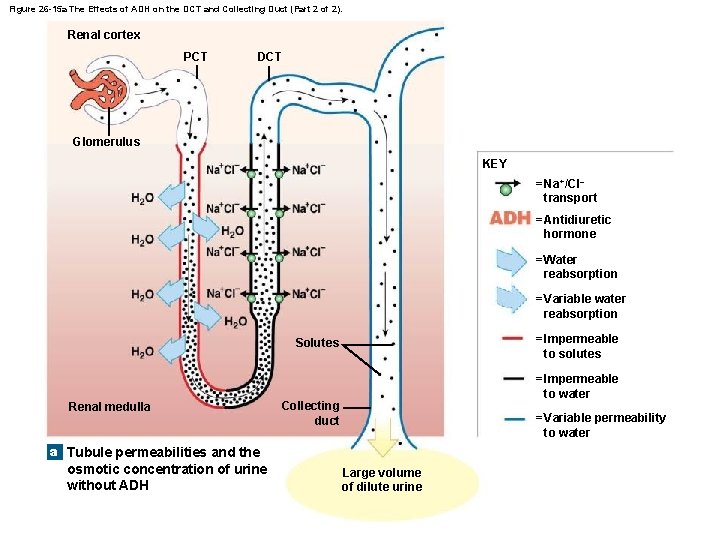
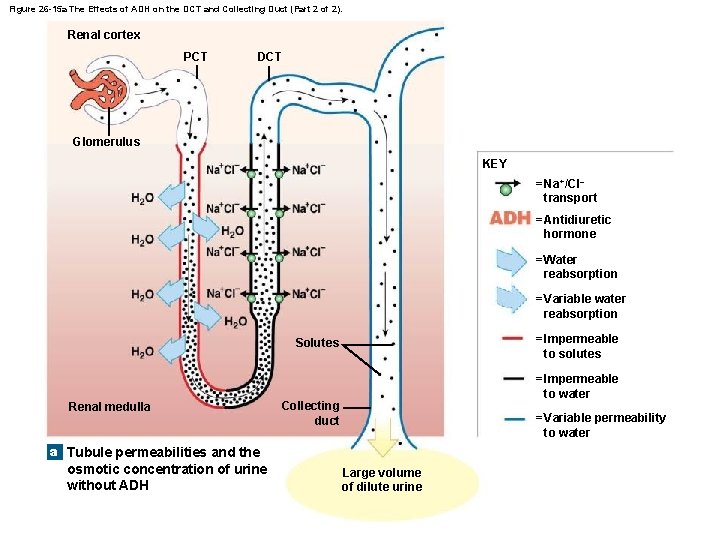
Figure 26 -15 a The Effects of ADH on the DCT and Collecting Duct (Part 2 of 2). Renal cortex PCT DCT Glomerulus KEY = Na+/Cl– transport = Antidiuretic hormone = Water reabsorption = Variable water reabsorption = Impermeable to solutes Solutes Renal medulla = Impermeable to water Collecting duct = Variable permeability to water a Tubule permeabilities and the osmotic concentration of urine without ADH Large volume of dilute urine
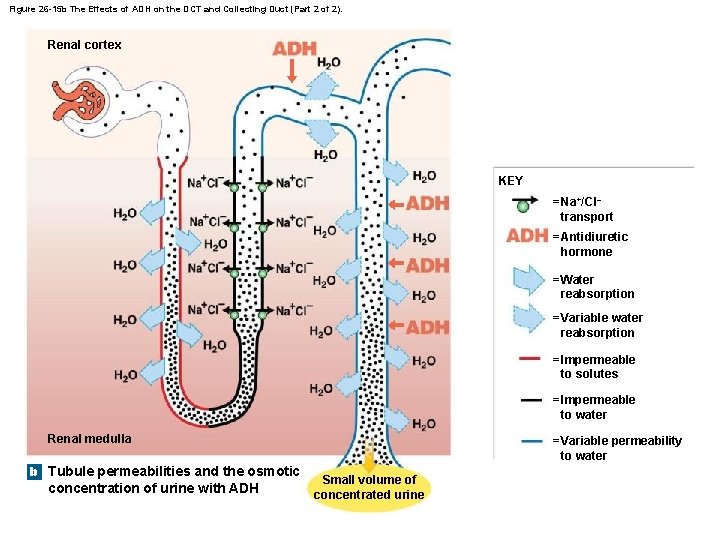
Figure 26 -15 b The Effects of ADH on the DCT and Collecting Duct (Part 2 of 2). Renal cortex KEY = Na+/Cl– transport = Antidiuretic hormone = Water reabsorption = Variable water reabsorption = Impermeable to solutes = Impermeable to water Renal medulla b Tubule permeabilities and the osmotic concentration of urine with ADH = Variable permeability to water Small volume of concentrated urine

26 -5 Reabsorption and Secretion • The Hypothalamus – Continuously secretes low levels of ADH • DCT and collecting system are always permeable to water – At normal ADH levels • Collecting system reabsorbs 16. 8 liters/day (9. 3 percent of filtrate)
26 -5 Reabsorption and Secretion • Urine Production – A healthy adult produces: • 1200 m. L per day (0. 6 percent of filtrate) • With osmotic concentration of 855– 1335 m. Osm/L
26 -5 Reabsorption and Secretion • Diuresis – Is the elimination of urine – Typically indicates production of large volumes of urine • Diuretics – Are drugs that promote water loss in urine – Diuretic therapy reduces: • Blood volume • Blood pressure • Extracellular fluid volume