Dr Tushar Shah M D Ped Convener Dr









- Slides: 74

Dr. Tushar Shah M. D. (Ped. ) Convener Dr. Bakulesh Chauhan M. D. (Ped. ) Dr. Rakesh Sharma M. D. (Ped. ) Coordinators Scientific Grant: Sanofi Pasteur, 4 Care
Three Tire Module Immunization Growth monitoring Diet- Nutrition related issues 2

Paramedic Skill – upgradation Initiative Beneficiary: Practicing pediatrician Adding value to practice Target audience: Front end person of hospital (receptionists) Dietician Empowerment Assistant doctor Counselors 3
Aims: • To enhance quality practice and improve standard of care • To empower front end staff of the hospital to deal with frequently asked questions of parents regarding immunization, Diet - nutrition and growth related issues • To improve vaccine uptake of the hospital • Hand’s on experience at various workstations giving them practical demonstration. 4
Motto • To decrease Mortality indicators(NMR/IMR/U 5 MR)by improving vaccination in private practice. • Early pick up of growth defaulters by adequate screening of weight and height with proper charting and thus decrease malnutrition • Promote exclusive breast feeding for first 6 months and rightful complementary feeding and other proper guidance of nutrition 5
SAKSHAM Module • • Manual –Reading material PPT Pretest Post test Feedback forms Certificate Work Stations material 6

Program Agenda ( TOT): Sr. no. Time Topic Faculty 1. 9: 00 am -9: 30 am Registration & Breakfast 2. 9: 30 am – 10: 05 am Inauguration and concept of Dr. Nishchal Bhatt workshop AOP Gujarat President 3. 10: 05 – 10: 15 am Orientation Dr. Tushar Shah 4. 10: 15 – 10: 30 am Pre test 5. 10: 30 am – 10: 45 am Counselling Concepts Dr. Satish Pandya 6. 10: 45 to 11: 45 noon Good immunization practices Dr. Tushar Shah 7. 11: 45 – 12: 00 noon Tea break 8. 12: 00 – 12: 30 pm Growth Monitoring Dr. Bakulesh Chauhan 9. 12: 30 pm to 1: 00 pm Diet and Nutrition Dr. Rakesh Sharma 10. 1: 00 pm – 1: 45 pm Lunch 11. 1: 45 pm-2: 45 pm Workstations (two) by rotation 30 min. each 12. 2: 45 – 3: 15 pm Posttest , Feedback & Certificate distribution. Trainees…… 13. 3: 15 pm to 4: 00 pm Chai Pe Charcha Discussion with Pediatricians (with Tea and cookies being served) 7
Work Stations: Work station 1. Immunization: Ø A. Vaccine boxes (dummy) - Schedule, Ø B. cold chain Concepts: Vaccine Vial monitor, vaccine carrier, syringe/needle, Mannequin, chart of fridge with various vaccine logo for arranging in fridge (to teach immunization concept, Injection technique, and cold chain concept) and prepared charts for demo. Ø C. FAQs Ø D. Biomedical waste mx (needle cutter) Work station 2. Ø Growth monitoring: infantometer (length measurement), stadiometer(height chart), head circumference(measure tape) Growth charts ( To teach how to measure weight and length, height and head circumference and plotting) Ø Nutrition: Visual aid, food plate, pyramid (some aid) to teach food concept ( to teach about breast feeding, complementary feeding and balance diet) 8
Pre – Training Evaluation: 9
Good immunization practices Dr. Tushar Shah M. D. (Ped. ), LL. b Navkar Children Hospital, Vadodara 10
Agenda • Importance of Immunization – Counsellor’s role • Concept of Immunization • Indian Scenario • Effective Counselling about Vaccine benefits and Risks • Practical Aspects of Vaccination • Vaccine Schedule with some details of each vaccine • Storage of Vaccine • Bio – Medical Waste Management • ADR – Emergency management 11

WHY IS IT IMPORTANT TO TALK ABOUT IMMUNIZATION? 12
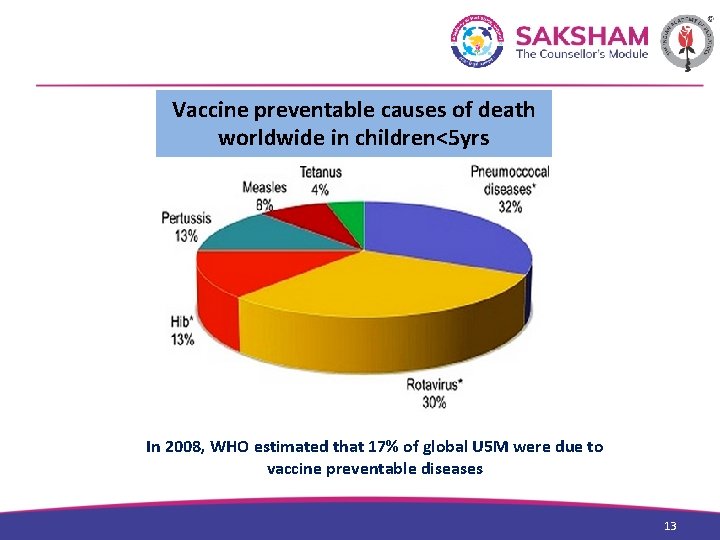
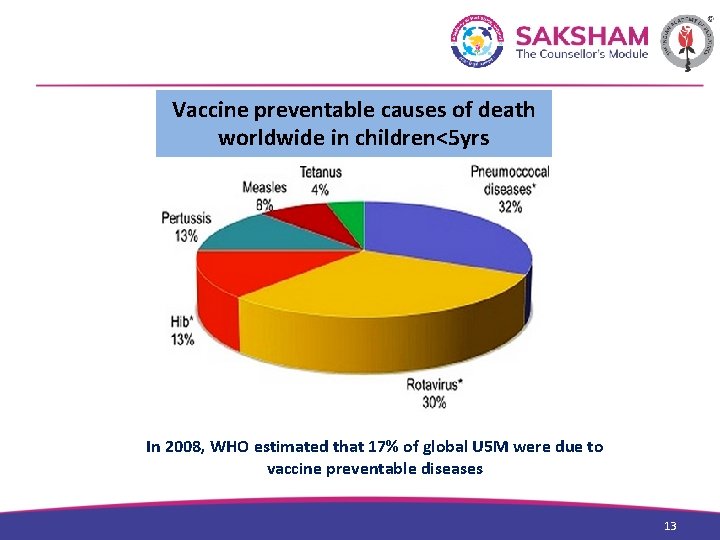
Vaccine preventable causes of death worldwide in children<5 yrs In 2008, WHO estimated that 17% of global U 5 M were due to vaccine preventable diseases 13
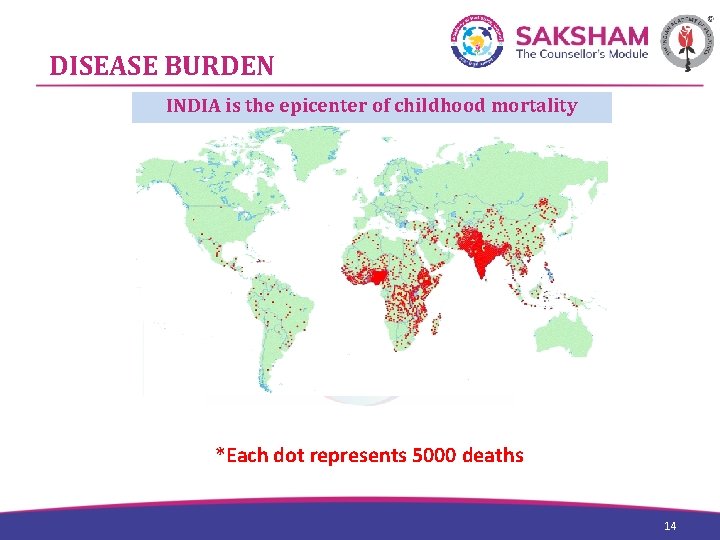
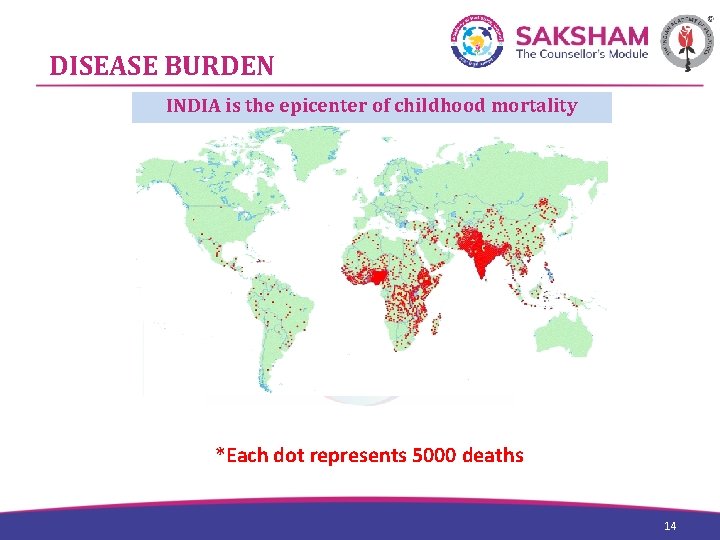
DISEASE BURDEN INDIA is the epicenter of childhood mortality *Each dot represents 5000 deaths 14
Relevance of Immunization • Important tool to decrease the childhood mortality • Immunization coverage in India continues to remain very poor Only 61% of children between 12 -23 months were fully vaccinated(BCG, Measles, 3 doses DPT and polio) • Large scope to improve the immunization acceptance rate with your help 15
COUNSELLOR’S ROLE Vital link in the immunization chain You play a vital role- counseling, preparing, motivating for immunization 16
Counsellor’s ROLE • First point of contact for most patients, Patient’s Comfort. • Explain things in a simple but accurate manner. • New dimension to your existing role. • Contribution in reducing the Childhood mortality and morbidity. 17

CONCEPT OF IMMUNIZATION 18
IMMUNIZATION AGAINST SMALLPOX • Most cost-effective healthcare interventions. • Rupee spent is rupees saved. • The success of smallpox eradication and now of polio eradication programs in the country are testimony to this. 19
Vaccination scene in India • At crossroads • Public sector v/s Private sector • Exaggeration of adverse events by press/lay people • All vaccines do have inherent risk of AEFI, but the benefits are undoubtedly immense, and clearly outweigh the risks. 20
Effective Communication about Vaccine benefits and risks 21 21
1. Risk of developing disease • Not possible to evaluate risk of disease in an individual child, but figures from literature may be quoted, – e. g. the risk of Invasive Pneumococcal Disease (IPD) in a healthy child aged less than 1 year is roughly 200 per 100, 000 (as per Western data). • Some general statements are also helpful. – Water or food-borne infections are preventable to some extent but not airborne droplet infections. • Risk of complications of disease is higher in infants and younger children and in undernourished population. 22
2. Efficacy of vaccine • No vaccine provides 100% protection though most of the vaccines do offer high degree of protection. • Vaccines significantly decrease chance of disease and even partial protection is useful to prevent complications. • Occasional failure of vaccine protection is no reason to consider against its use. 23
3. Safety of vaccine • Vaccines are very safe and serious adverse reactions are extremely rare. • Media outbursts of fatal reactions to vaccines are mostly due to programmatic errors and not due to vaccine itself. • Thus benefits of vaccines far outweigh the risk of side effects caused by vaccines. 24
4. Economics of vaccine • Decision of affordability should be left to parents after discussing all vaccine options. – For example, DTw. P and DTa. P are equally efficacious though differ in reactogenicity. • Cost of vaccine in clinics and its logical reasons – Cold chain maintenance/ stock maintenance/ breakage/expiry/administration cost/consultation charges etc. 25
5. Dynamic Process • It is important to emphasize that above discussion is based on the current understanding. • With increasing experience over time, there can be a change in the recommendations of individual vaccine and it is necessary to adapt to such changes. – For example, second dose of Varicella, three doses of MMR etc. is now recommended. 26
Practical Aspects of Vaccination 27
Injection procedure • Hands should be washed with soap and water for 2 minutes using WHO's 6 steps technique. Alternately, alcohol-based waterless antiseptic hand rub can be used. • Gloves need not be worn, unless the person administering the vaccine has open lesions on hands. • Syringe and needles used must be sterile and disposable. • If multi-dose vials are used, the septum should be swabbed with alcohol prior to each withdrawal and the needle should not be left in the stopper in between uses. 28
Cont. • Different vaccines should never be mixed in the same syringe • Vaccine doses should not be drawn into a syringe until immediately before administration. • To prevent inadvertent needle-stick injury or reuse, needles and syringes should be discarded immediately after use in labeled, puncture-proof containers located in the same room where the vaccine is administered. 29
General Instructions on Immunization • At birth: as early as possible, within 24 to 72 hours after birth or at least not later than one week after birth. • The recommended age in weeks/months/years mean completed weeks/months/years. • Combination vaccine generally is preferred over separate injections • When two or more live parenteral vaccines are not administered on the same day, they should be given at least 28 days (4 weeks) apart; this rule does not apply to live oral vaccines. 30
Cont. • Any number of vaccines can be given on the same day. • Anterolateral aspect of the thigh is the preferred site for IM injections because of its greater muscle mass. • Patients should be observed for allergic reaction for 15 to 20 minutes after immunization(s). • When necessary, 2 vaccines can be given in the same limb. – The distance separating the 2 injections is arbitrary but should be at least 1 inch so that local reactions are unlikely to overlap. 31
Cont. • Inform the parents regarding vaccine benefits and their anticipated reactions. Take informed Consent. • Avoid fomentation/ vigorous rubbing after vaccination • Document every vaccination 32
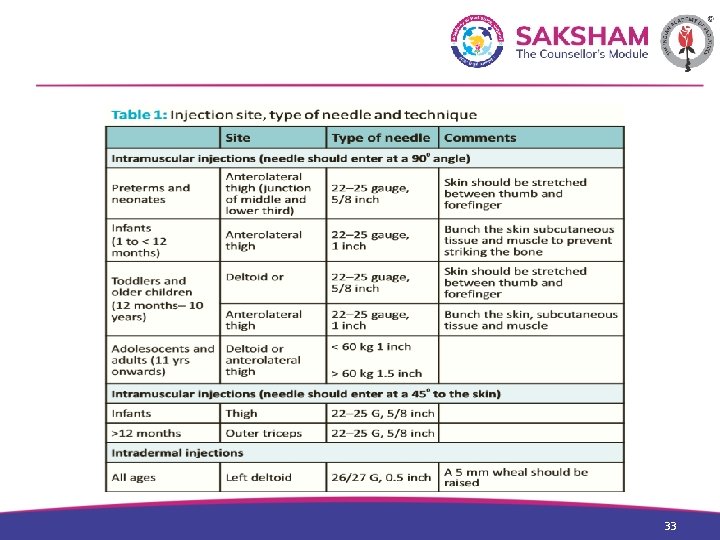
33
Vaccination Schedule 34
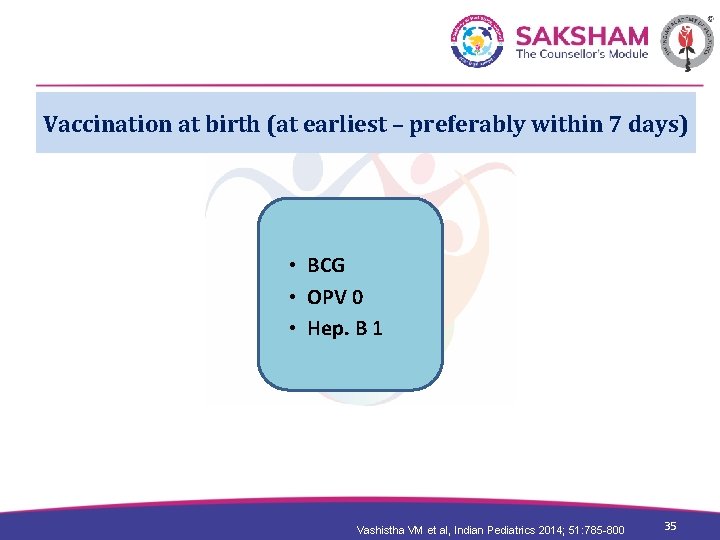
Vaccination at birth (at earliest – preferably within 7 days) • BCG • OPV 0 • Hep. B 1 Vashistha VM et al, Indian Pediatrics 2014; 51: 785 -800 35
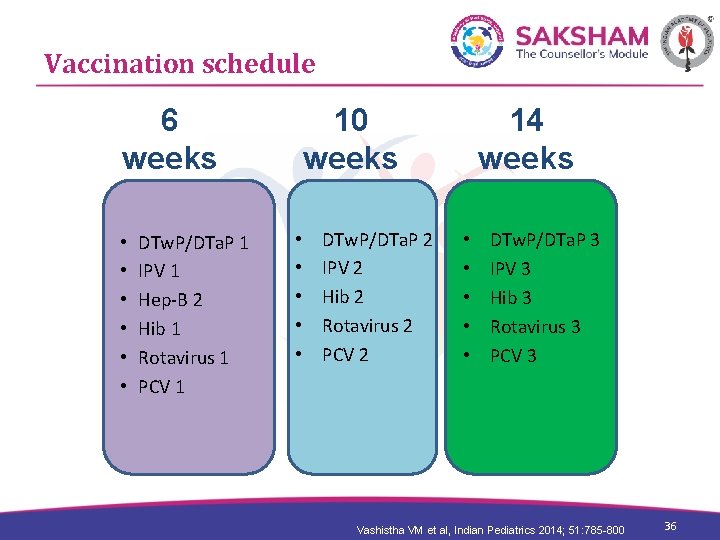
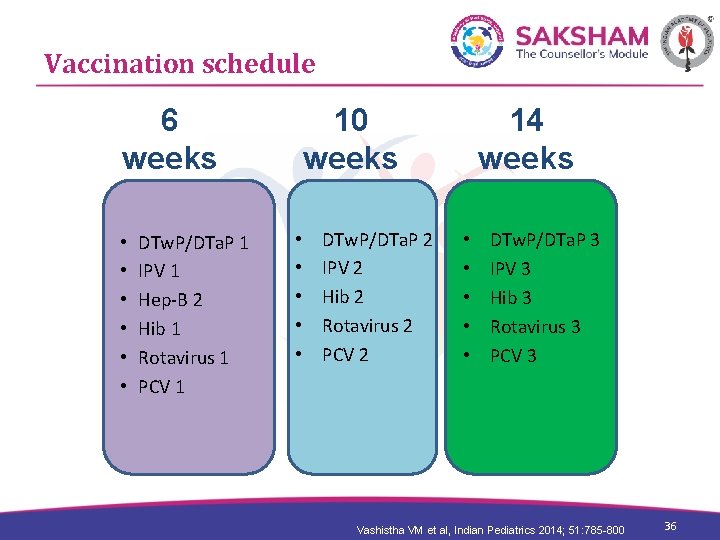
Vaccination schedule 6 weeks • • • DTw. P/DTa. P 1 IPV 1 Hep-B 2 Hib 1 Rotavirus 1 PCV 1 10 weeks • • • DTw. P/DTa. P 2 IPV 2 Hib 2 Rotavirus 2 PCV 2 14 weeks • • • DTw. P/DTa. P 3 IPV 3 Hib 3 Rotavirus 3 PCV 3 Vashistha VM et al, Indian Pediatrics 2014; 51: 785 -800 36
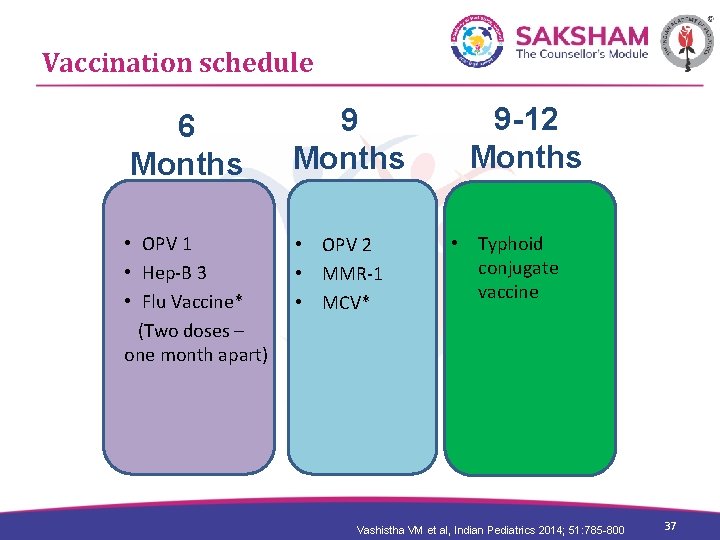
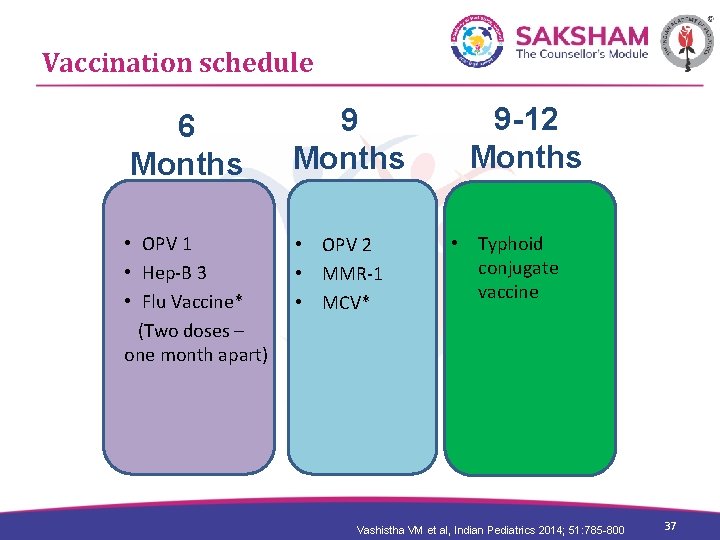
Vaccination schedule 6 Months 9 Months • OPV 1 • OPV 2 • Hep-B 3 • MMR-1 • Flu Vaccine* • MCV* (Two doses – one month apart) 9 -12 Months • Typhoid conjugate vaccine Vashistha VM et al, Indian Pediatrics 2014; 51: 785 -800 37
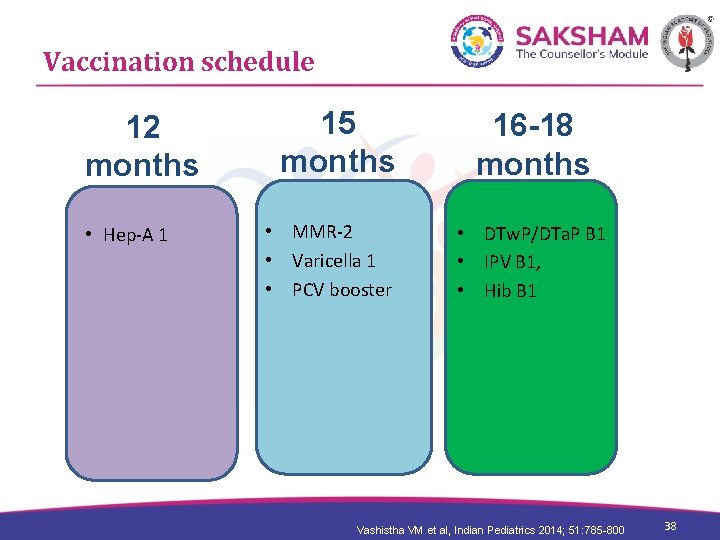
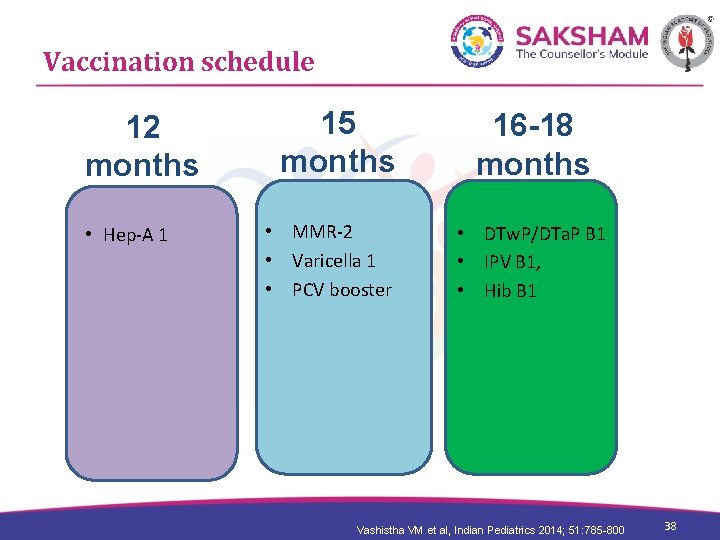
Vaccination schedule 12 months • Hep-A 1 15 months • MMR-2 • Varicella 1 • PCV booster 16 -18 months • DTw. P/DTa. P B 1 • IPV B 1, • Hib B 1 Vashistha VM et al, Indian Pediatrics 2014; 51: 785 -800 38
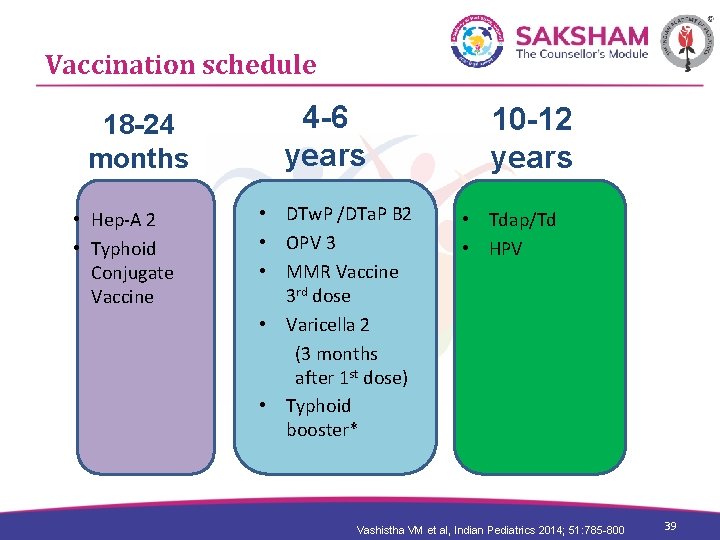
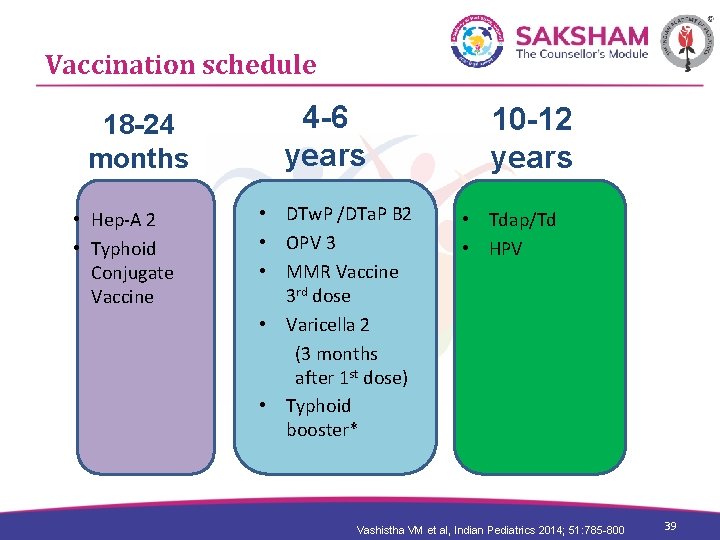
Vaccination schedule 18 -24 months • Hep-A 2 • Typhoid Conjugate Vaccine 4 -6 years • DTw. P /DTa. P B 2 • OPV 3 • MMR Vaccine 3 rd dose • Varicella 2 (3 months after 1 st dose) • Typhoid booster* 10 -12 years • Tdap/Td • HPV Vashistha VM et al, Indian Pediatrics 2014; 51: 785 -800 39
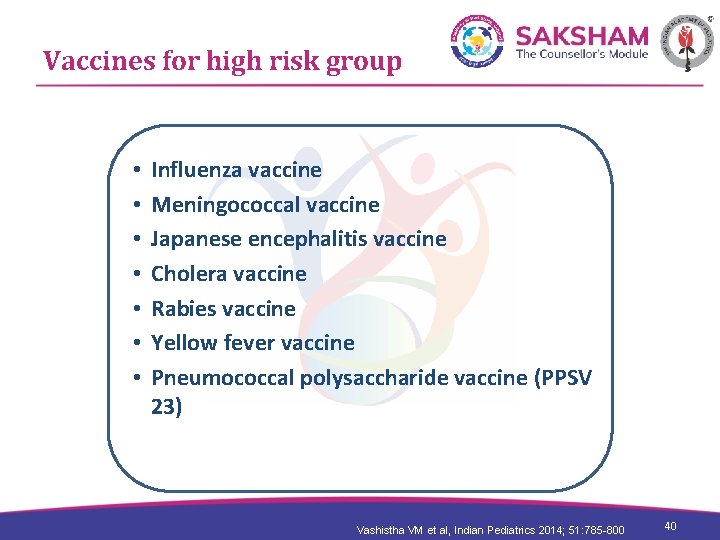
Vaccines for high risk group • • Influenza vaccine Meningococcal vaccine Japanese encephalitis vaccine Cholera vaccine Rabies vaccine Yellow fever vaccine Pneumococcal polysaccharide vaccine (PPSV 23) Vashistha VM et al, Indian Pediatrics 2014; 51: 785 -800 40
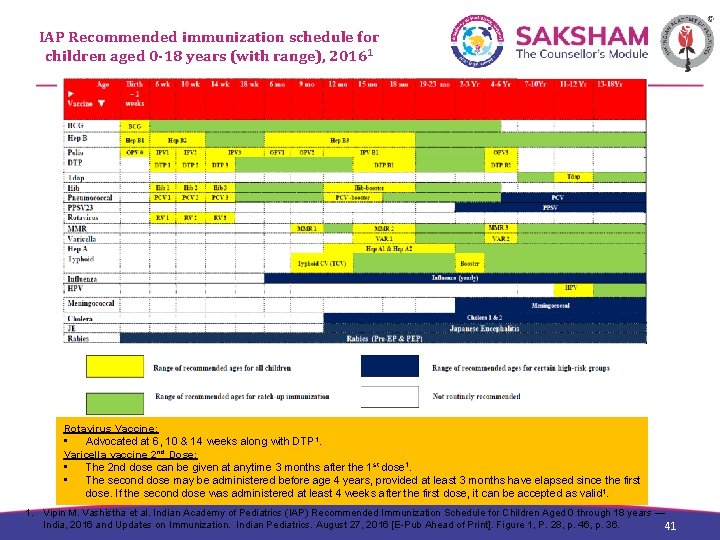
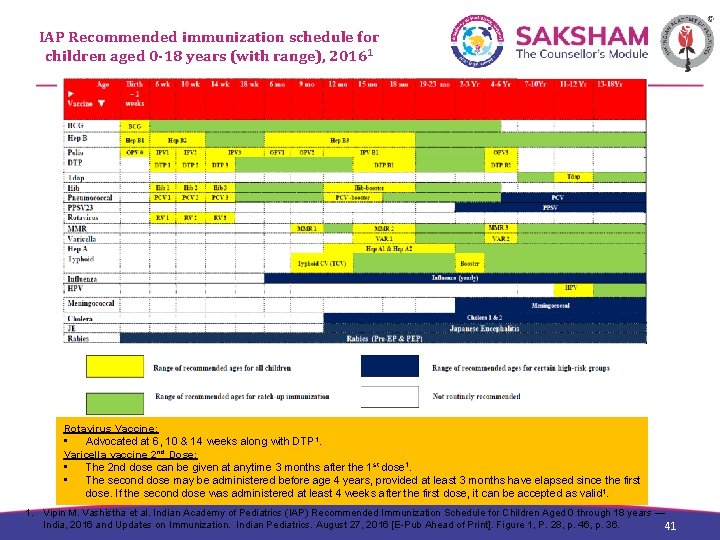
IAP Recommended immunization schedule for children aged 0 -18 years (with range), 20161 Rotavirus Vaccine: • Advocated at 6, 10 & 14 weeks along with DTP 1. Varicella vaccine 2 nd Dose: • The 2 nd dose can be given at anytime 3 months after the 1 st dose 1. • The second dose may be administered before age 4 years, provided at least 3 months have elapsed since the first dose. If the second dose was administered at least 4 weeks after the first dose, it can be accepted as valid 1. 1. Vipin M. Vashistha et al. Indian Academy of Pediatrics (IAP) Recommended Immunization Schedule for Children Aged 0 through 18 years — India, 2016 and Updates on Immunization. Indian Pediatrics. August 27, 2016 [E-Pub Ahead of Print]. Figure 1, P. 28, p. 46, p. 36. 41
Storage of vaccine 42 42
WHAT IS COLD CHAIN? • System of transporting, storing and distributing vaccines • Ensuring proper temperature maintenance from point of manufacture till end user • Important to maintain the chain without breaks • You have vital role in ensuring the cold chain in your hospital 43
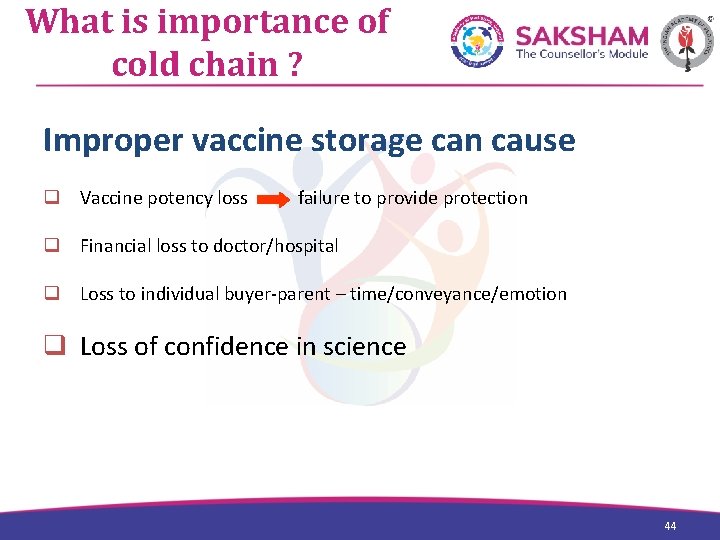
What is importance of cold chain ? Improper vaccine storage can cause q Vaccine potency loss failure to provide protection q Financial loss to doctor/hospital q Loss to individual buyer-parent – time/conveyance/emotion q Loss of confidence in science 44
Vaccines can be damaged by q Freezing q Exposure to § Heat § Sunlight Light- UV rays § Fluorescent /neon light. 45
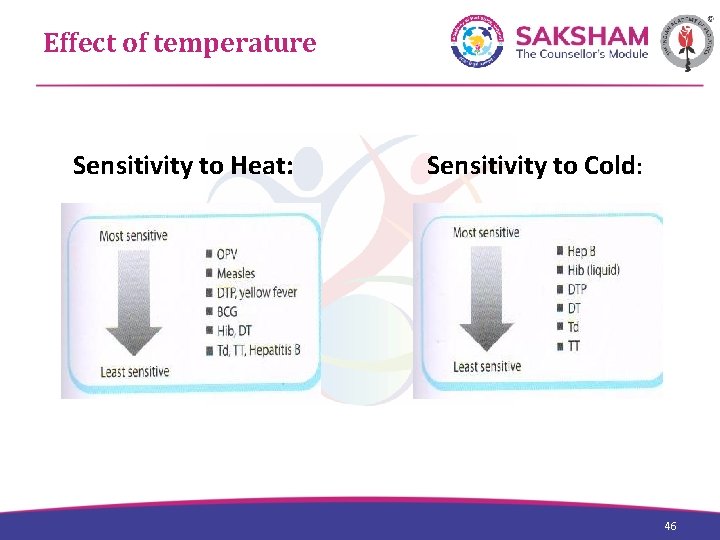
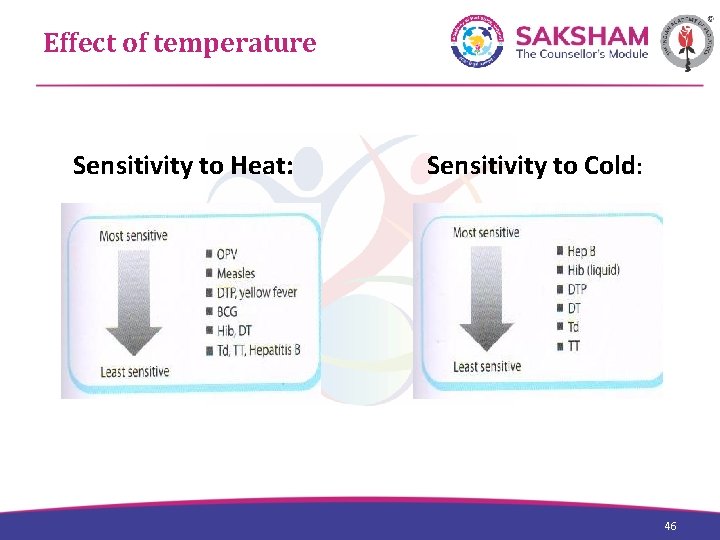
Effect of temperature Sensitivity to Heat: Sensitivity to Cold: 46
Effect of light on vaccines • Direct sunlight exposure is harmful • Also, fluorescent neon light, ultraviolet light, any strong light • Vaccines easily damaged by light exposure include BCG, MMR, Measles, Rotavirus, HPV, DTa. P 47
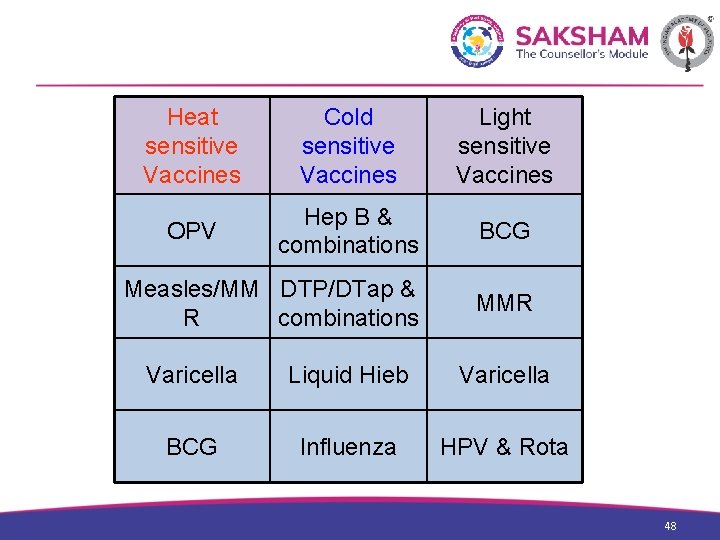
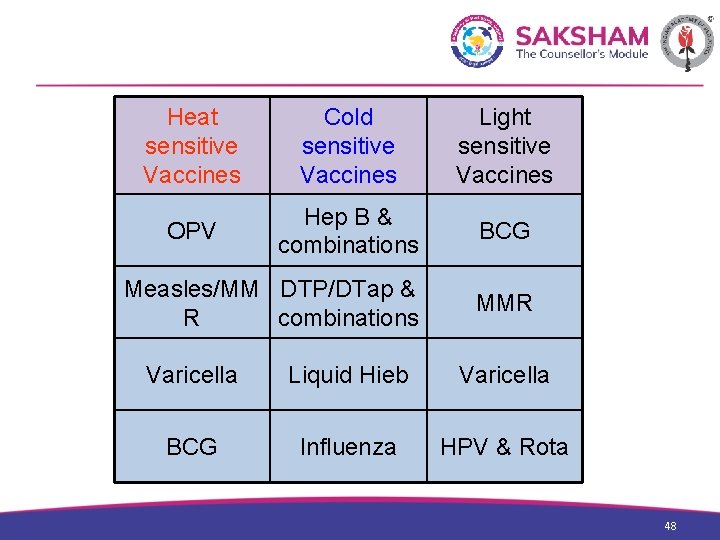
Heat sensitive Vaccines Cold sensitive Vaccines Light sensitive Vaccines OPV Hep B & combinations BCG Measles/MM DTP/DTap & R combinations MMR Varicella Liquid Hieb Varicella BCG Influenza HPV & Rota 48
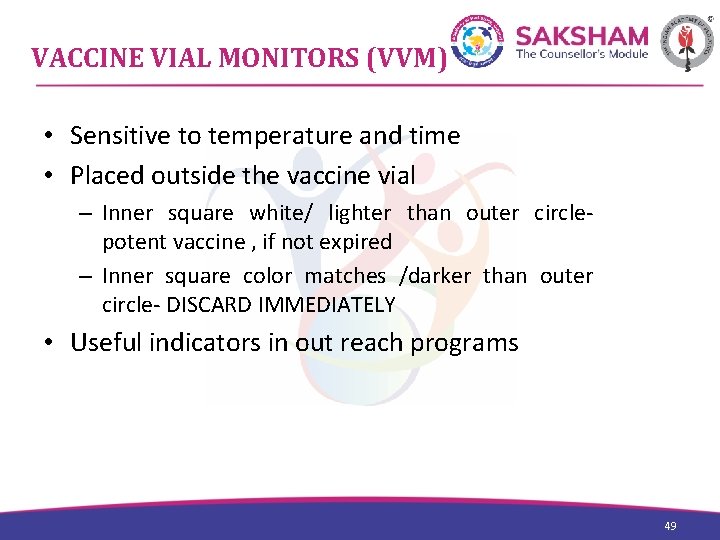
VACCINE VIAL MONITORS (VVM) • Sensitive to temperature and time • Placed outside the vaccine vial – Inner square white/ lighter than outer circle- potent vaccine , if not expired – Inner square color matches /darker than outer circle- DISCARD IMMEDIATELY • Useful indicators in out reach programs 49

VACCINE VIAL MONITORS 50
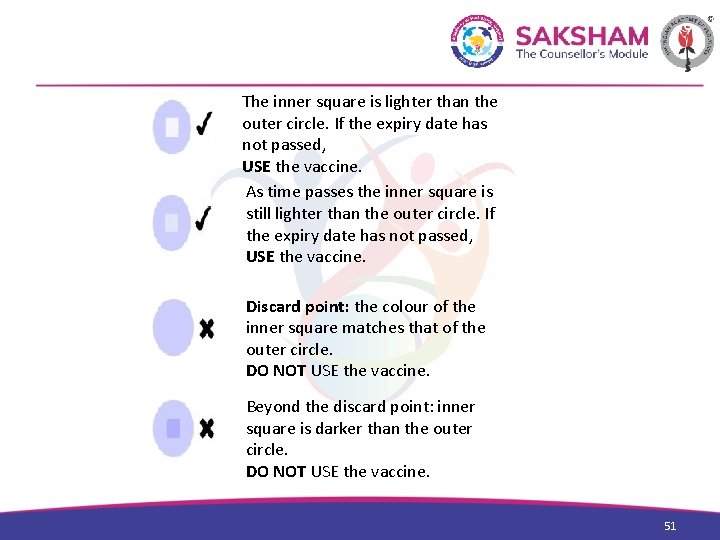
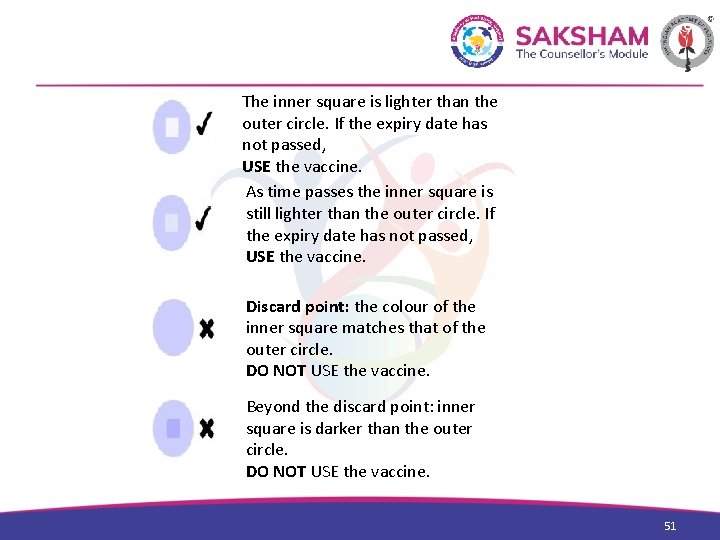
The inner square is lighter than the outer circle. If the expiry date has not passed, USE the vaccine. As time passes the inner square is still lighter than the outer circle. If the expiry date has not passed, USE the vaccine. Discard point: the colour of the inner square matches that of the outer circle. DO NOT USE the vaccine. Beyond the discard point: inner square is darker than the outer circle. DO NOT USE the vaccine. 51

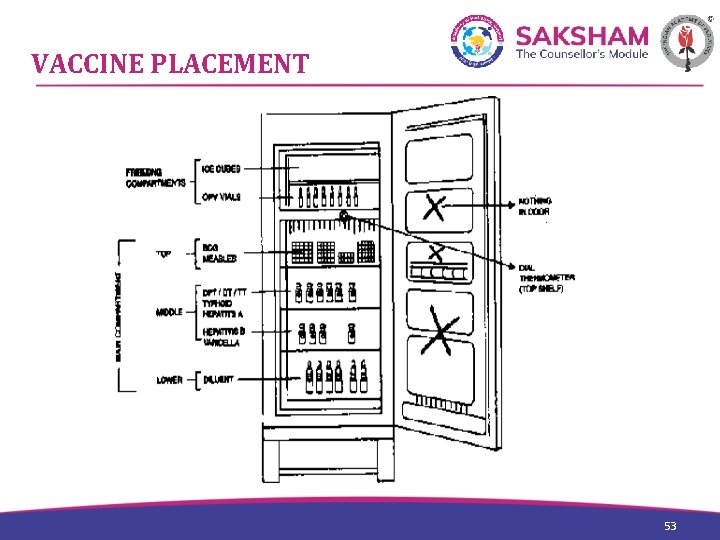
VACCINE PLACEMENT NO VACCINES ON THE DOOR Freezer: OPV Top shelf: BCG, Measles, MMR Middle: DTw. P, DTa. P, HPV, DT, TT, IPV, PCV, HAV, Influenza, Rota, Combination vaccines • Lower: HBV, Varicella • Crispator: Diluents • Baffle tray: EMPTY • • 52
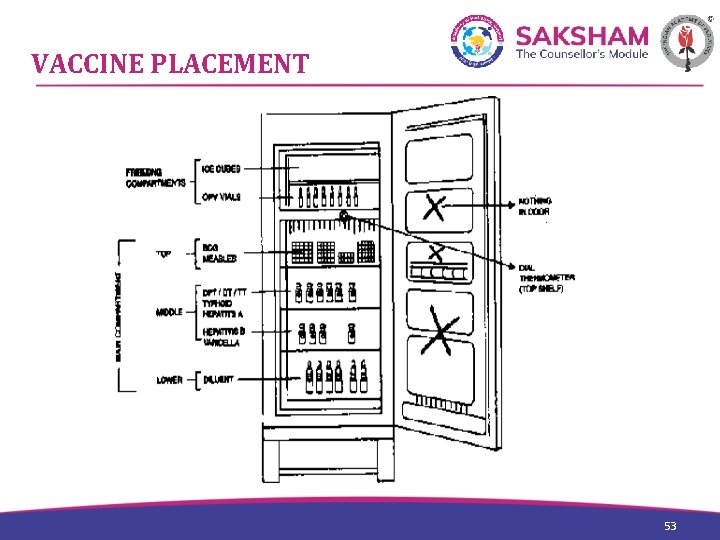
VACCINE PLACEMENT 53

COLD BOXES, VACCINE CARRIERS 54
VACCINE STORAGE Protect from direct sunlight Safe storage in original packs till use Temperature 2 -8°C for 24 months Live vaccines kept frozen for longer use- MMR, OPV, BCG, Measles • DISCARD accidentally frozen vaccines • NEVER freeze diluents • • 55
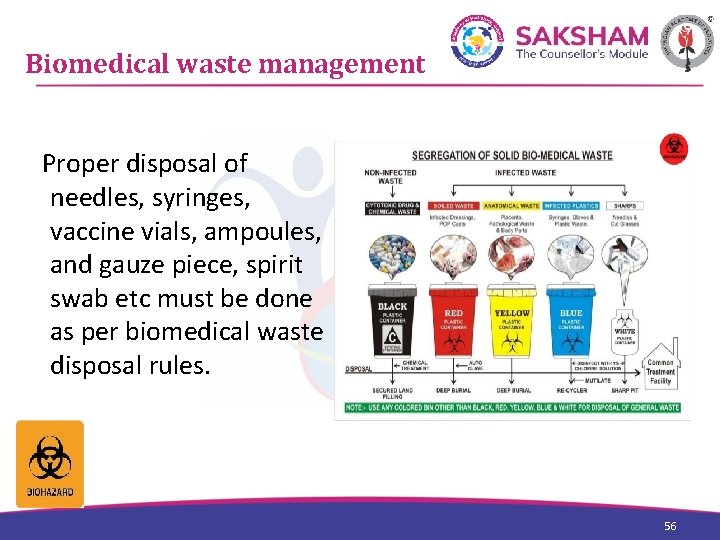
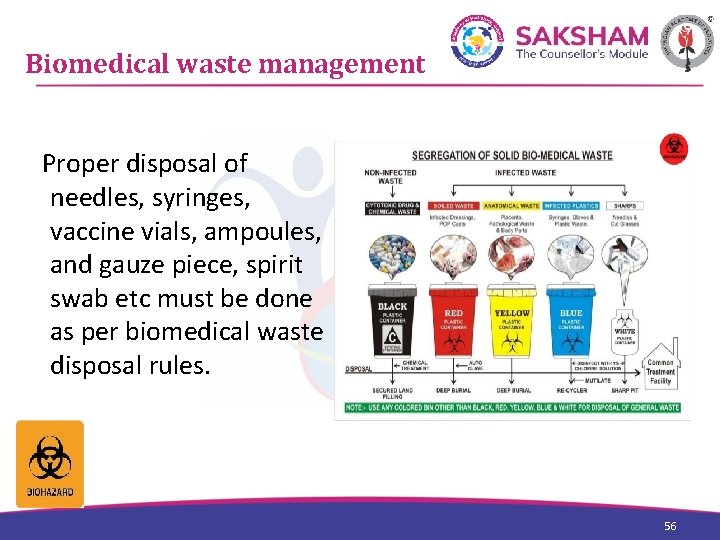
Biomedical waste management Proper disposal of needles, syringes, vaccine vials, ampoules, and gauze piece, spirit swab etc must be done as per biomedical waste disposal rules. 56
Adverse reaction – emergency management • No vaccine is perfectly safe • Emergency tray – preparedness – Effective resuscitation facilities should be available to tackle any adverse event. • Medico legal implications – Proper consent (informed) would help to prevent litigation. 57
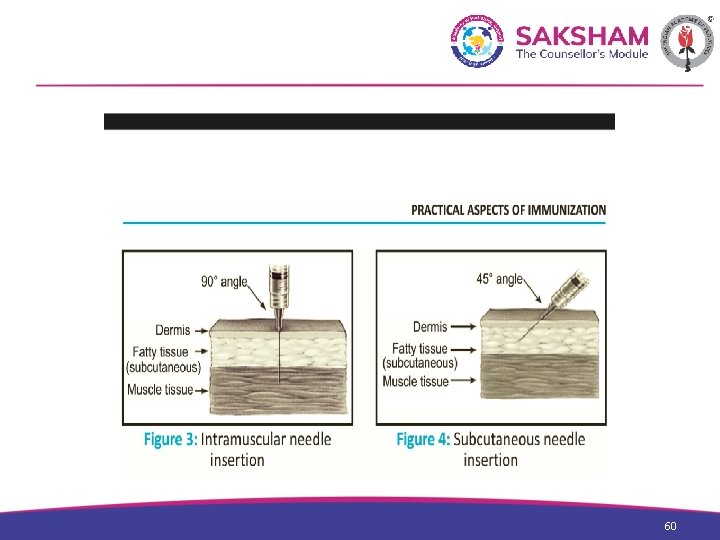
Work station 1. Immunization 59
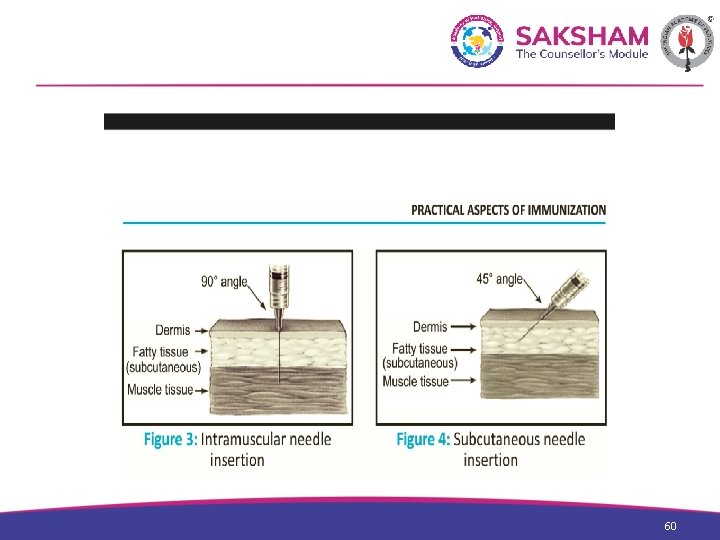
60
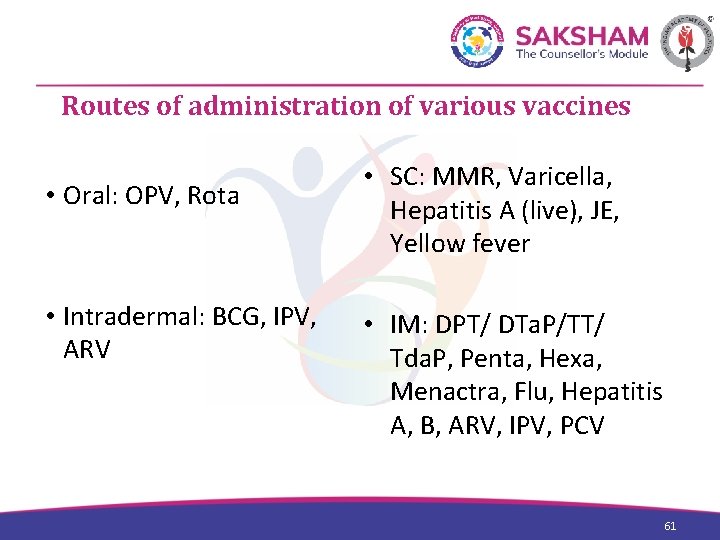
Routes of administration of various vaccines • Oral: OPV, Rota • Intradermal: BCG, IPV, ARV • SC: MMR, Varicella, Hepatitis A (live), JE, Yellow fever • IM: DPT/ DTa. P/TT/ Tda. P, Penta, Hexa, Menactra, Flu, Hepatitis A, B, ARV, IPV, PCV 61
DOUBTS AND MYTHS IN IMMUNIZATION 62 62
Doubts and Myths 1. In the old days, there weren’t so many vaccines, yet children were healthy. Is it essential to give so many vaccines to my child? - Vaccines protect against deadly diseases - Medical science advances- more vaccines produced - Herd immunity 63

Doubts and Myths 2. Is it necessary to start immunization soon after birth? - Some vaccines must be given at birth - Maximum protection against dangerous diseases - Early protection essential 64
Doubts and Myths 3. My baby is premature. When can I start immunizations? Will it be able to tolerate the immunizations - Poor innate immunity - Adequate protection essential - Start immunization when infant is stable and age appropriate preferably at the time of discharge from the NICU - Live vaccines at discharge 65
Doubts and Myths 4. My baby has cold, fever and diarrhea. Is it alright to vaccinate my baby now, or do I have to delay it? - Few specific contraindications to immunization - CDC recommendations- no need to delay vaccines for mild URI, diarrhea and fever 66
Doubts and Myths 5. Are all vaccines compulsory or are there some which are optional vaccines? - Prevention is better than cure - Vaccines protect against disease responsible for U-5 mortality - No concept of optional vaccines 67
Doubts and Myths 6. Combination vaccines contain antigens against several diseases. Will my child be able to tolerate these vaccines? - Combination vaccines protect against common infections - They require repeated doses for complete protection - Reduced number of pricks - Decreased physician contact 68
Doubts and Myths 7. Are there any side effects of immunization? - Introduces antigens which stimulate antibodies in the host - Protect against infection in future - All vaccines can cause side effects – usually mild - No serious side effects usually 69
Doubts and Myths 8. My child is recovering from an infection and is on medication at present. Can I give the scheduled immunization now or do I have to postpone it? - CDC recommends no delay in case of minor illness or convalescence - Reasons for delay- Nephrotic syndrome on steroids Bronchial asthma on steroids Immunosuppressants Blood products administered 70
Doubts and Myths 9. My child’s vaccines have been delayed. Do I need to restart the entire course again? - No need to restart - Age appropriate vaccines - Catch up vaccination 71
Doubts and Myths 10. I have to travel on the day of immunization. Can I take the vaccine two days earlier? - Ideal interval 4 -8 weeks - Delay vaccine in case of short travel - If long delay is anticipated, administer upto 4 days earlier 72
Doubts and Myths 11. My granny says that unless the baby develops fever after immunization, the vaccine will not be effective. Is this true? - Vaccine induces immune response in host Vaccine induces local and systemic adverse effects like pain, fever, swelling No correlation between fever and body immune response. 73