Dr Rakhi R 2 Dept of Radiodiagnosis Medical










- Slides: 94
Dr Rakhi , R 2 Dept of Radiodiagnosis , Medical college , Vadodara. 1
Case - 1 2
n n Fifty-nine-year-old male with unknown past medical history complaining of vomiting and severe chest pain. There was no record of him having had any recent procedures 3
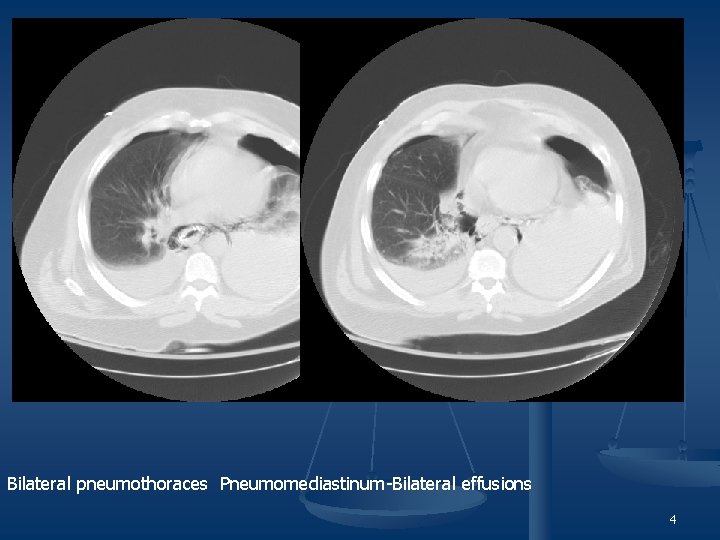
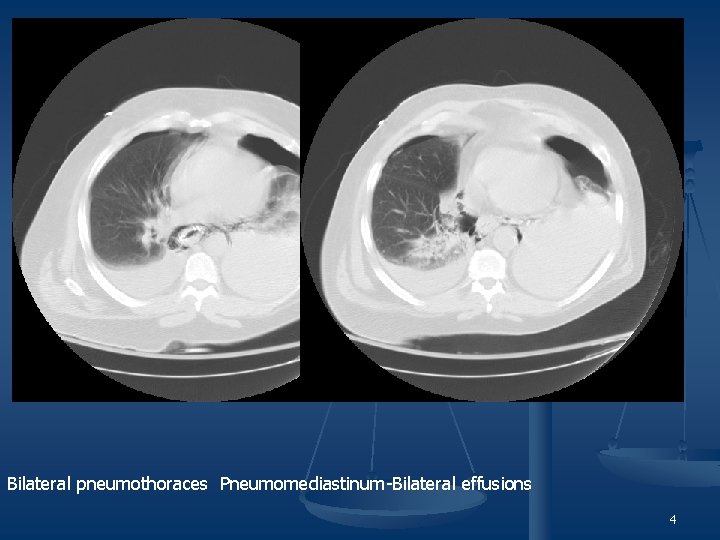
Bilateral pneumothoraces Pneumomediastinum-Bilateral effusions 4
n n n Boerhaave’s Syndrome Foreign Body Perforation of the Esophagus Mallory- wiess tear 5

Contrast extravasation from the distal esophagus into both pleural cavities--The 6 exam was subsequently terminated
n n n n Esophageal perforation is a rare, albeit lifethreatening, event. It has been a reported complication in about one per 1000 patients who undergo endoscopic examination. 55% - iatrogenic, 15% - spontaneous, 14% - foreign body ingestion, and 10% - traumatic. Cervical esophagus most commonly perforated by endoscopic procedures & Thoracic esophagus may be perforated during stenting or dilatation procedures. 7
n n n The spontaneous esophageal rupture after a violent vomiting episode (ie, Boerhaave syndrome) is typically located in the left posterolateral esophagus, near the left diaphragmatic crus. About 10 -15% of perforation are caused by ingested foreign bodies such as chicken and meat bones. When an intra-abdominal segment of the esophagus is perforated by an endoscope, then the perforation is usually into the lesser sac. 8
Boerhaave’s Syndrome n Spontaneous esophageal perforation is secondary to phenomena that increase intraluminal pressure within the esophagus such that all three layers of wall are disrupted (as opposed to a Mallory-Weiss tear, which only involves the mucosa). n The condition is grave secondary to subsequent development of mediastinitis & retropharyngeal or mediastinal abscess. n The syndrome is most common in adults (particularly males), in whom the most common location of the tear (90%) is the site least protected from herniation by adjacent structures--that is, the left posterolateral wall of the distal esophagus. n In neonates, the syndrome is more common in females and usually involves the right distal esophagus. n Clinically, vomiting, severe chest pain, and subcutaneous air in an adult should alert one to the diagnosis, although patients may present without this “textbook” pattern. 9
n On a conventional chest radiograph, pneumothorax, pneumomediastinum, mediastinal widening, and subcutaneous air are common findings. n A delayed radiograph twelve to twenty-four hours after the inciting event may reveal a left pleural effusion or left pneumothorax (reflecting the fact that most ruptures occur on the left). n The Nacleiro sign represents air dissecting from the mediastinum down to the left diaphragmatic pleura and appears as a “V”-shaped lucency. n CT, while it may not be as good at identifying the exact site of perforation, rules out other causes of chest pain and/or nausea and vomiting. 10
n The other primary modality for evaluating Boerhaave’s syndrome is the contrast esophagram. n A water-soluble contrast such as gastrografin is the agent of choice initially, because barium is known to cause a severe mediastinitis. However, if the exam is negative and if esophageal rupture is still suspected, barium should be used to confirm the diagnosis as well as to aid the surgeon by delineating the location and length of the perforation. n Management is primarily surgical/interventional (e. g. primary repair, diversion procedures, T-tube drainage, or expanding stents) but also includes antibiotics and supportive measures such as fluid resuscitation. 11
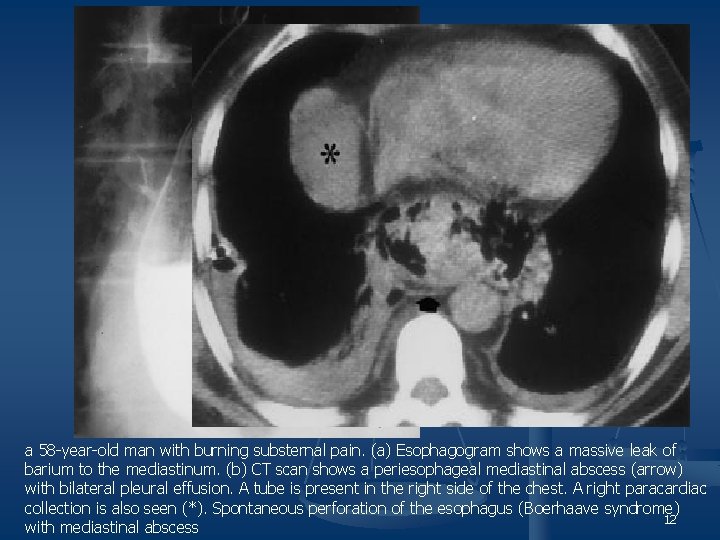
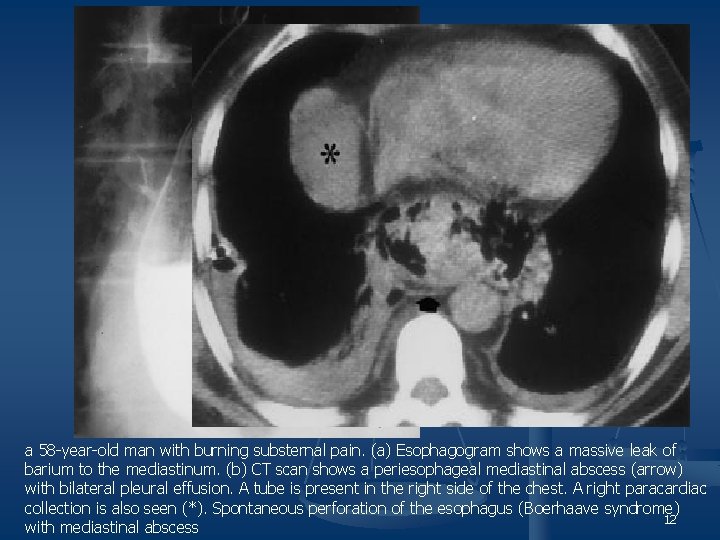
a 58 -year-old man with burning substernal pain. (a) Esophagogram shows a massive leak of barium to the mediastinum. (b) CT scan shows a periesophageal mediastinal abscess (arrow) with bilateral pleural effusion. A tube is present in the right side of the chest. A right paracardiac collection is also seen (*). Spontaneous perforation of the esophagus (Boerhaave syndrome) 12 with mediastinal abscess
n Radiological examination: n Chest x-ray n n Extraluminal gas, which forms a radiolucent triangle behind the heart - earliest chest x-ray feature , extraluminal gas is easier to recognize when it spreads and lifts the visceral pleura from the margin of heart and aorta. Surgical emphysema in neck and upper thorax Mediasinitis cause sympathetic pleural effusion, or mediasinal pleura may rupture to produce a hydropneumothorax, which is more common on left side where the mediastinal pleura is closely applied to the distal esophagus. However plain radiograph may be completely normal. 13
n n n Contrast examination: It is important to obtain decubitus films with horizontal x-ray beam to detect small leaks. Common practice is to start with a nonionic water soluble agent and, if this shows no evidence of significant leakage, then a little dilute barium can be used to obtain best mucosal detail. 14
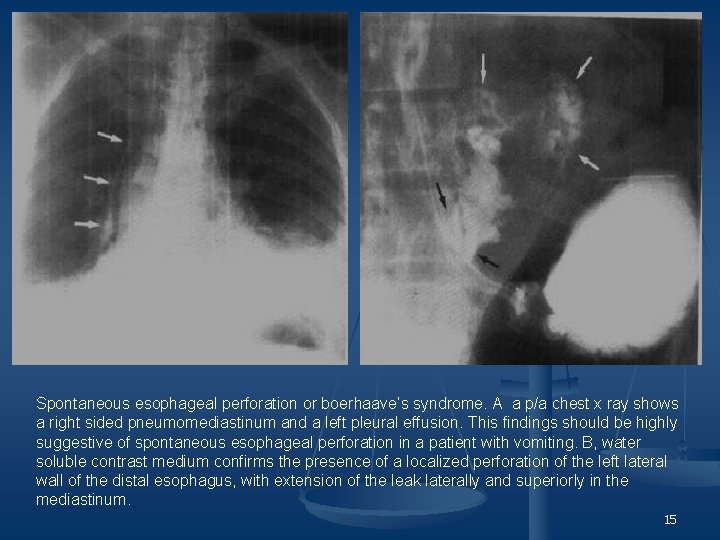
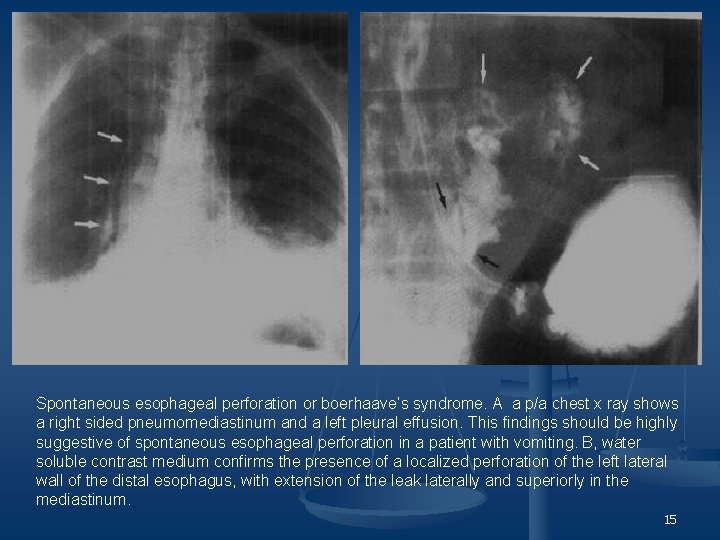
Spontaneous esophageal perforation or boerhaave’s syndrome. A a p/a chest x ray shows a right sided pneumomediastinum and a left pleural effusion. This findings should be highly suggestive of spontaneous esophageal perforation in a patient with vomiting. B, water soluble contrast medium confirms the presence of a localized perforation of the left lateral wall of the distal esophagus, with extension of the leak laterally and superiorly in the mediastinum. 15
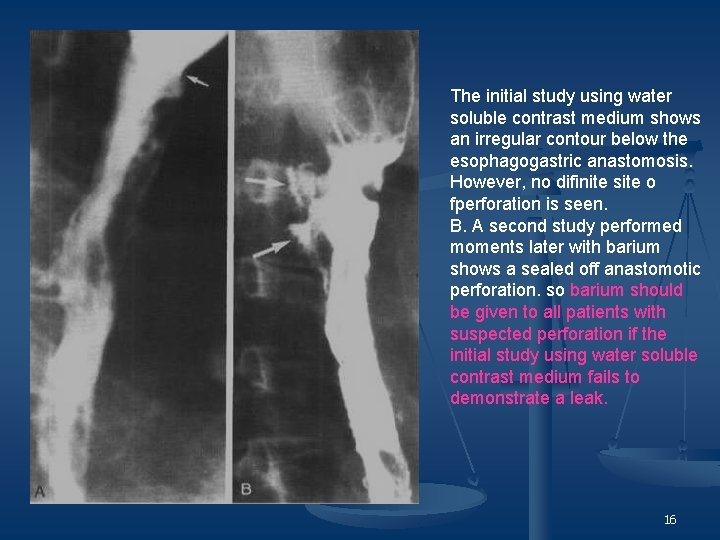
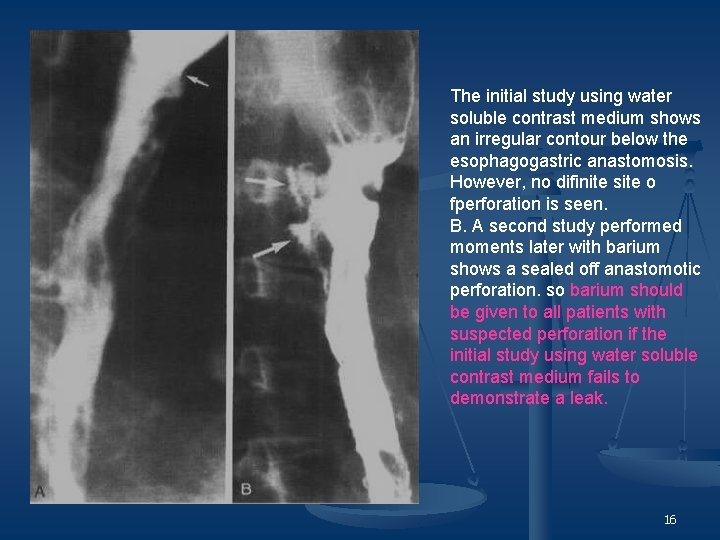
The initial study using water soluble contrast medium shows an irregular contour below the esophagogastric anastomosis. However, no difinite site o fperforation is seen. B. A second study performed moments later with barium shows a sealed off anastomotic perforation. so barium should be given to all patients with suspected perforation if the initial study using water soluble contrast medium fails to demonstrate a leak. 16
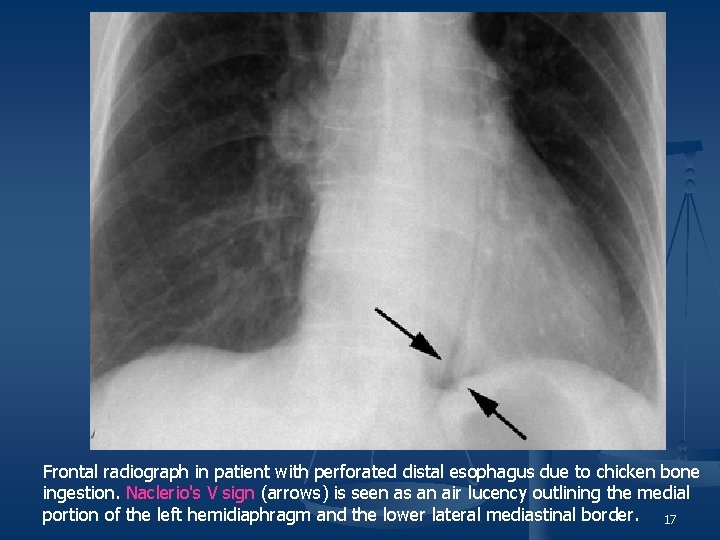
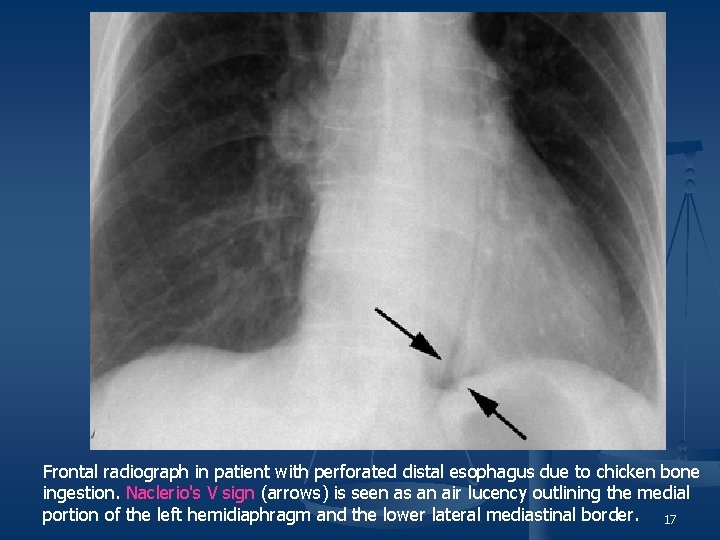
Frontal radiograph in patient with perforated distal esophagus due to chicken bone ingestion. Naclerio's V sign (arrows) is seen as an air lucency outlining the medial portion of the left hemidiaphragm and the lower lateral mediastinal border. 17
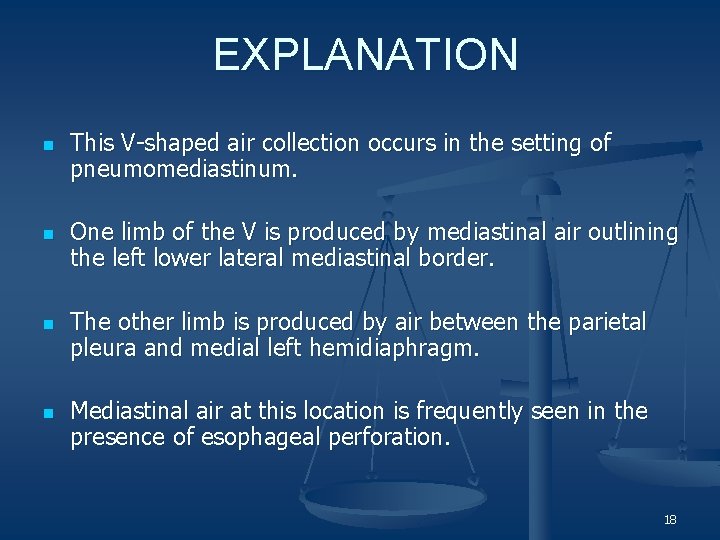
EXPLANATION n n This V-shaped air collection occurs in the setting of pneumomediastinum. One limb of the V is produced by mediastinal air outlining the left lower lateral mediastinal border. The other limb is produced by air between the parietal pleura and medial left hemidiaphragm. Mediastinal air at this location is frequently seen in the presence of esophageal perforation. 18
n On chest radiographs, pneumomediastinum is seen as multiple lucent streaks of air outlining mediastinal structures. n It may be extensive, with air tracking up into the neck or chest wall n Pneumomediastinum can be secondary to alveolar rupture, which leads to pulmonary interstitial emphysema that travels centrally back to the mediastinum. n Other conditions that can produce pneumomediastinum include asthma, chest trauma, and barotrauma. n Tracheobronchial injury and esophageal perforation are less common causes of pneumomediastinum. 19
n n n Naclerio described the V sign in patients with spontaneous esophageal rupture. Leakage of air from the perforated or ruptured distal esophagus produces pneumomediastinum, which results in outlining of the medial left hemidiaphragm and left lower lateral mediastinal area on radiographs. Naclerio attributed the finding to air "dissecting along diaphragmatic and mediastinal fascial planes in the region of the lower esophagus". Iatrogenic and traumatic perforations, usually occurring in the proximal esophagus, may not produce the V sign. Naclerio's V sign is not entirely specific to that condition. Regardless, the presence of Naclerio's V sign in an appropriate clinical scenario may provide an early radiologic clue to the presence of esophageal rupture 20
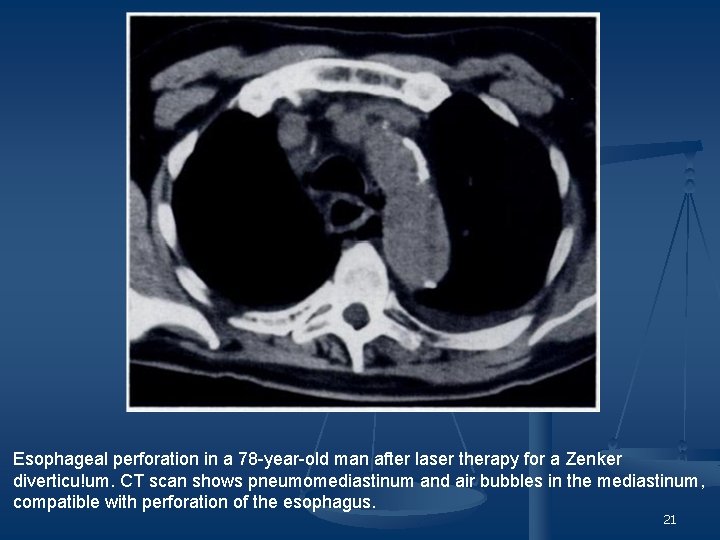
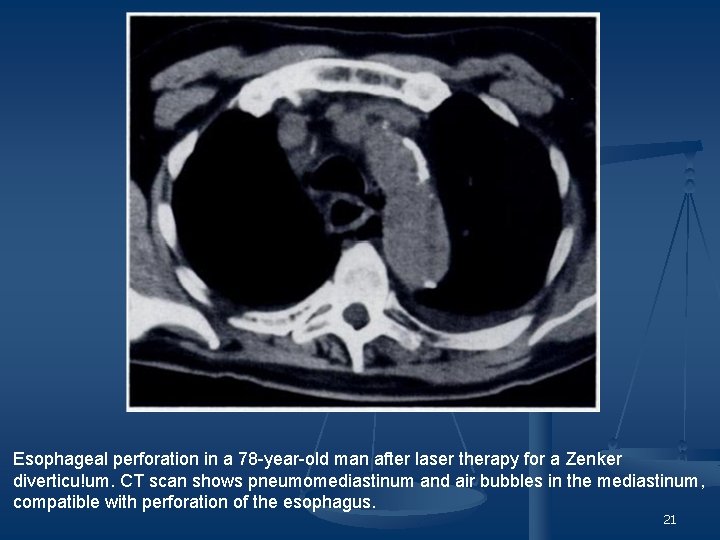
Esophageal perforation in a 78 -year-old man after laser therapy for a Zenker diverticu!um. CT scan shows pneumomediastinum and air bubbles in the mediastinum, compatible with perforation of the esophagus. 21
Mallory – Weiss tear n n The tear result from a sudden increase in intraesophageal pressure, as may occur from vomiting or retching. This tear may cause severe haematemesis. Endoscopically the mucosal tear is above the gastro- esophageal junction. On DC barium study the tear can sometimes be seen as a short vertical white line. 22
n n Esophageal tear can also result from the ingestion of foreign bodies or from endoscopy. Hemorrhage may strip the mucosa from the underlying circular muscle coat to produce a smooth, broad-based filling defect which bulge into the lumen. Esophageal haematoma that spread circumferentially produce an annular stricture, whereas those that spread longitudinally narrow the esophageal lumen. Barium may enter the tear and dissect under the mucosa. 23
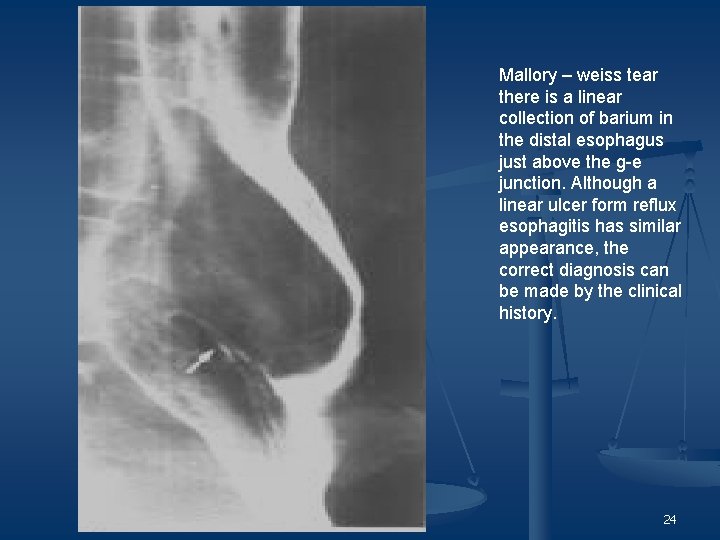
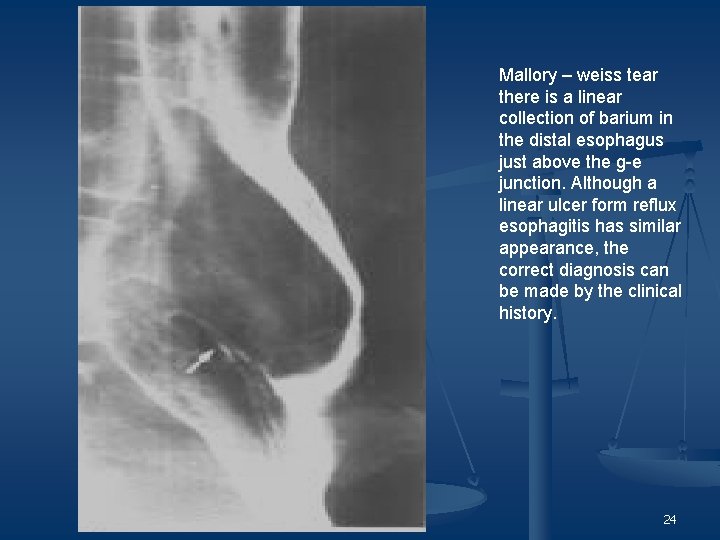
Mallory – weiss tear there is a linear collection of barium in the distal esophagus just above the g-e junction. Although a linear ulcer form reflux esophagitis has similar appearance, the correct diagnosis can be made by the clinical history. 24
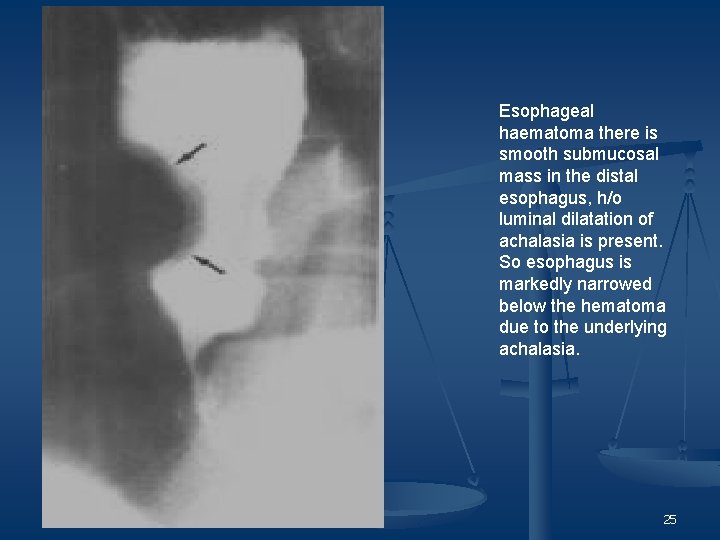
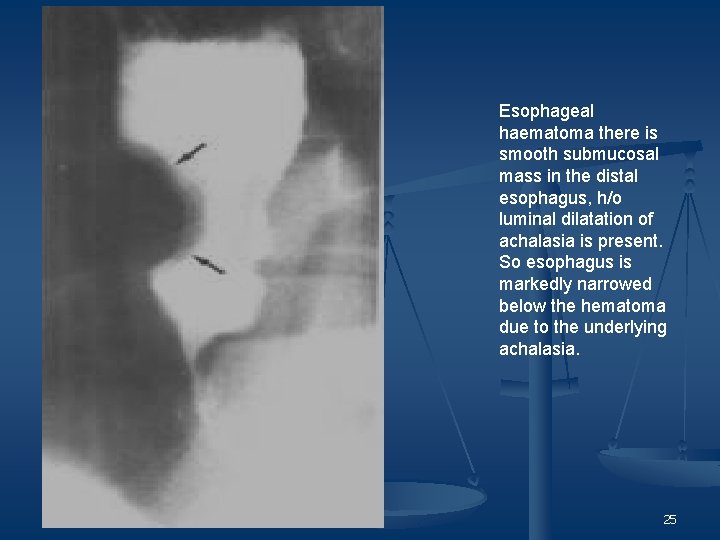
Esophageal haematoma there is smooth submucosal mass in the distal esophagus, h/o luminal dilatation of achalasia is present. So esophagus is markedly narrowed below the hematoma due to the underlying achalasia. 25
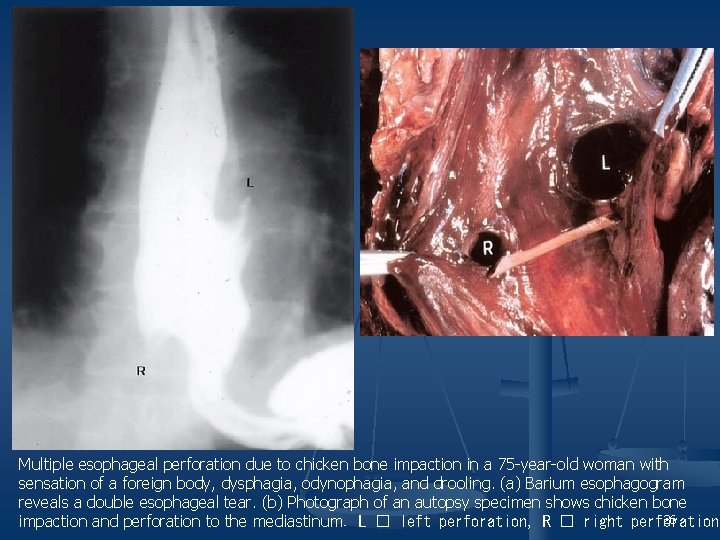
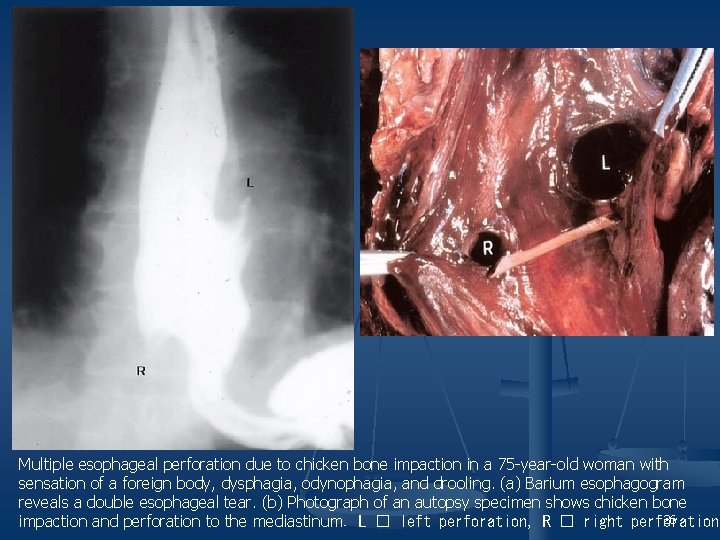
Multiple esophageal perforation due to chicken bone impaction in a 75 -year-old woman with sensation of a foreign body, dysphagia, odynophagia, and drooling. (a) Barium esophagogram reveals a double esophageal tear. (b) Photograph of an autopsy specimen shows chicken bone 26 impaction and perforation to the mediastinum. L � left perforation, R � right perforation
Case - 2 27
n n n 30 yr old female with h/o prior small-bowel resection presented with left upper quadrant abdominal pain. She was afebrile with a normal WBC. No signs of peritonitis were noted on clinical examination. 28

29
30

31

32
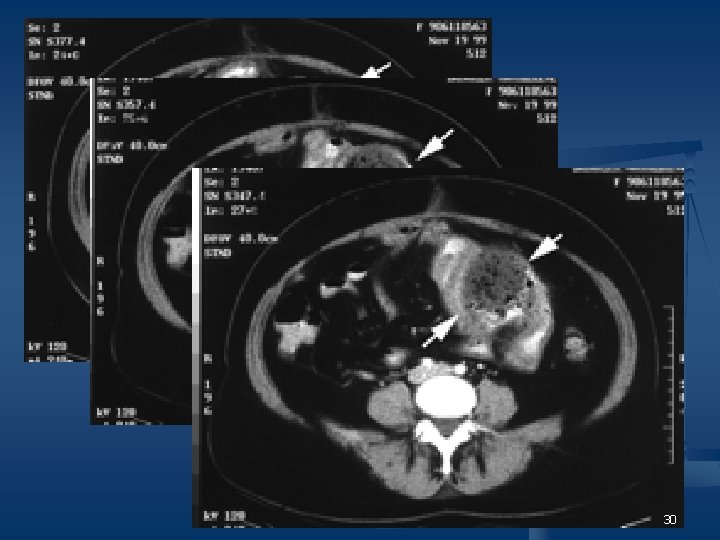
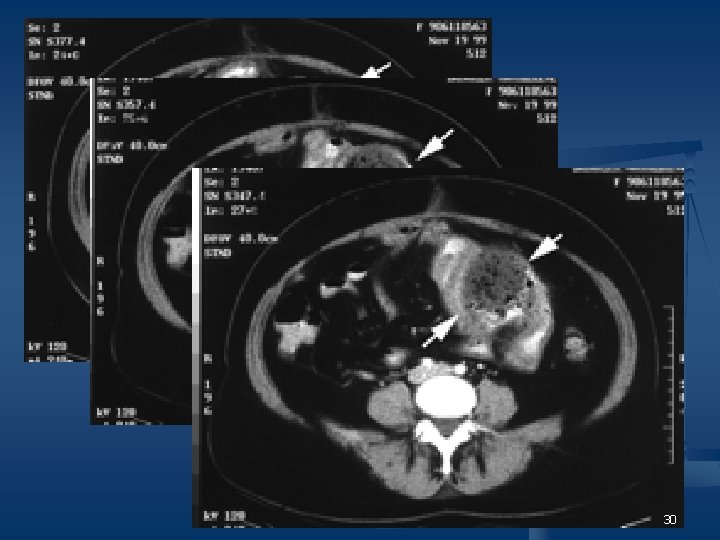
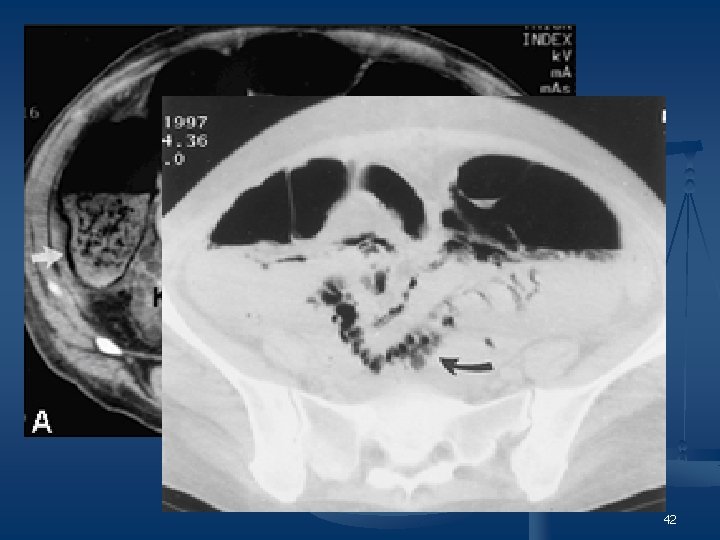
n n The abdominal radiograph obtained at presentation with left abdominal pain shows a large mottled gas and debris collection in left upper quadrant. CECT scans show a large mass proximal to the jejunostomy site. The mass has multiple air bubbles, fluid, and debris scattered throughout, giving it a mottled appearance. Oral contrast material is noted surrounding the mass. The abdominal radiograph obtained 1 day after CT shows a large mottled gas collection with contrast material. Axial CT scans obtained 5 months before presentation show focal dilatation of the jejunum proximal to the jejunostomy. 33
n n n Oral contrast material was noted to surround the mass, suggesting the mass was intraluminal. No thick enhancing wall was identified to suggest an abscess. The gas was noted to be diffusely scattered in the mass and not in the wall of the bowel, excluding pneumatosis. The most likely diagnosis of this case is small-bowel bezoar. Exploratory laparotomy showed an intraluminal mass at the site of the previous jejunostomy. Pathology revealed a phytobezoar of the small bowel with vegetable products in the small-bowel lumen. 34
DISCUSSION n n n Bezoars of the gastrointestinal tract are most often found in the stomach as persistent concretions of substances such as plant and vegetable fibers (phytobezoar), persimmons (disopyrobezoar), or hair (trichobezoar). Phytobezoars are the most common and are characterized by concretions of poorly digested fibers, fruit seeds, and pulpy fruits, especially oranges and persimmons. A primary small-bowel bezoar without associated gastric bezoars is uncommon. 35
n n Usually, bezoar fragments from the stomach or bolus of food small enough to pass through the pylorus will enter the small bowel where they absorb water, increase in size, and become impacted. Complete mechanical intestinal obstruction is the most frequent clinical presentation of bezoar. Small-bowel obstruction caused by bezoar is rarely diagnosed preoperatively. 36
n n n Small-bowel bezoars can arise in small-bowel diverticula, in a segment of bowel associated with stricture formation, or proximal to smallbowel tumors. They almost always present with obstruction and rarely with perforation. If a small-bowel bezoar is found, the stomach should be inspected closely. Concurrent gastric bezoar is found in 17 -21% of patients with small -bowel bezoar. 37
n n CT reveals a well-defined ovoid intraluminal mass with a mottled gas pattern in the dilated small bowel at the site of obstruction and an abruptly collapsed lumen beyond the lesion. The mottled appearance is a result of air bubbles retained in the interstices of the mass. The site of impaction is usually the narrowest portion of the small bowel 50 -75 cm from the ileocaecal valve or at the valve itself. Any part can be affected, especially in patients with postoperative adhesions. 38
D/D: n n n Small-bowel pneumatosis -gas in the wall of the intestine-usually occurs in the setting of bowel ischemia or infarction. CT findings of pneumatosis are curvilinear, serpiginous, bubbly collections of gas that occur circumferentially or in peripheral or dependent portions of the bowel wall. Long segments of the bowel are usually involved. 39
Pneumatosis Intestinalis n Cystic or linear collections of gas can be located in subserosa or submucosa of small bowel or colon Causes of air in the bowel wall – -Disruption of the bowel mucosa (eg, bowel obstruction, inflammatory bowel disease), -Increased bowel permeability (eg, graft-versus-host disease, acquired immunodeficiency syndrome, steroid therapy), and n -Pulmonary disease (eg, chronic obstructive pulmonary disease) n Diagnosis on plain x-ray & CT ( mainly) n Important to recognise ischaemic, inflammatory, ulcerative & traumatic conditions 40 40
n Abscesses usually develop as a complication of intraabdominal inflammatory processes or after laparotomy. n Patients usually present with fever and elevated WBC. n On CT, abscesses appear as circumscribed round or oval soft tissue-density masses with an attenuation of 10 -30 H. n n If a well-formed capsule is present, it often shows contrast enhancement, whereas the central area of the abscess, which contains necrotic material. Intracavitary gas is a suggestive finding in 40 -50% of abscesses. The gas may be distributed as finely dispersed air bubbles throughout the collection or as an air-fluid level. 41
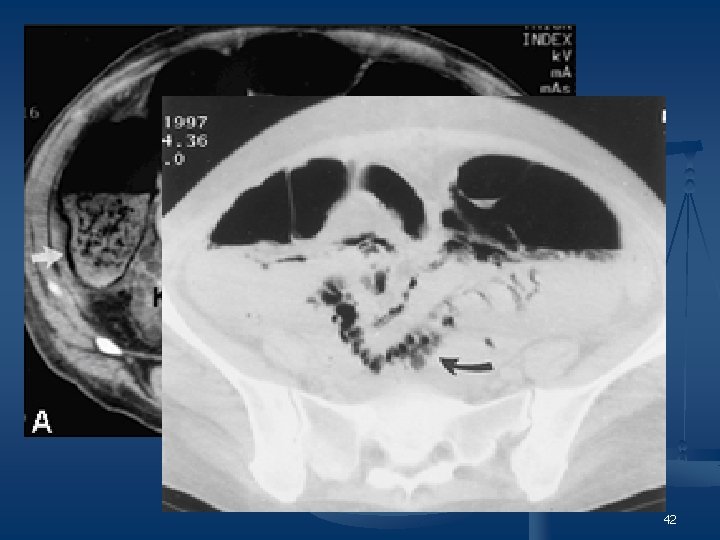
42
Case - 3 43

n 53 -year-old patient presented with recurrent headaches 44
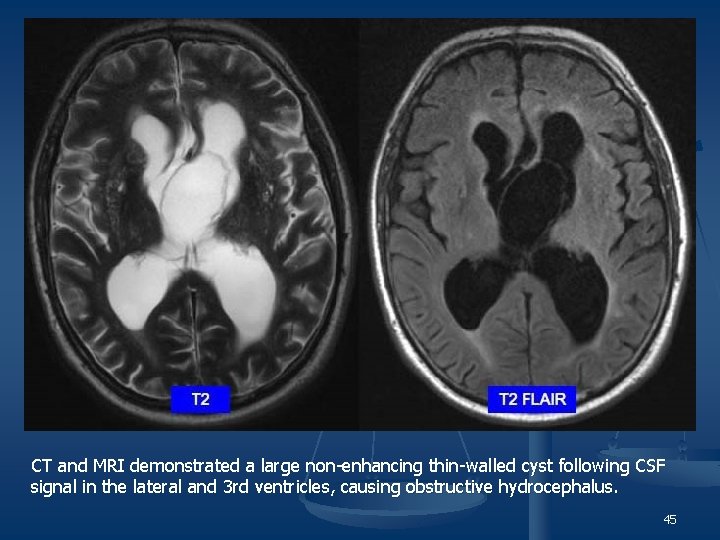
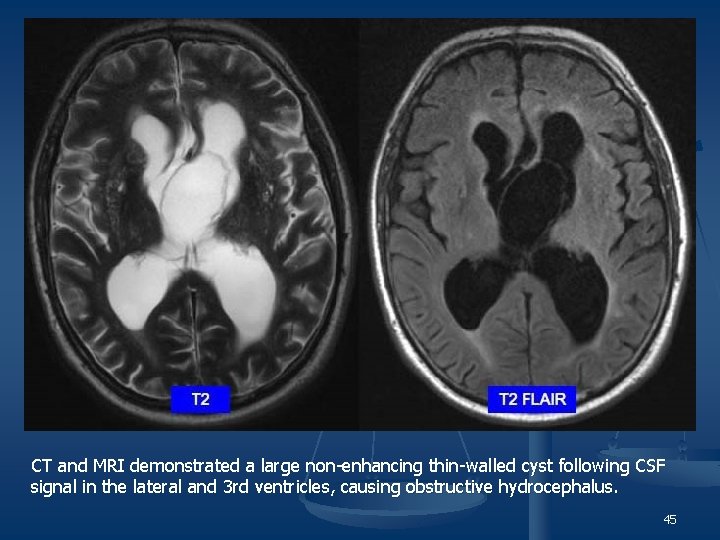
CT and MRI demonstrated a large non-enhancing thin-walled cyst following CSF signal in the lateral and 3 rd ventricles, causing obstructive hydrocephalus. 45
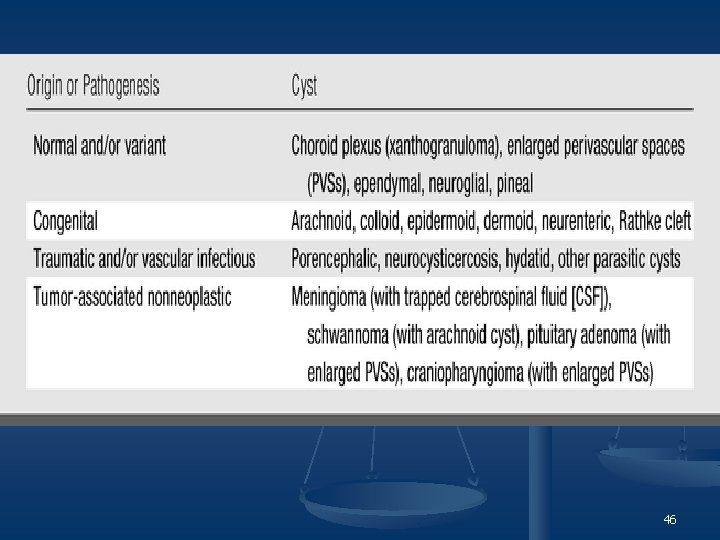
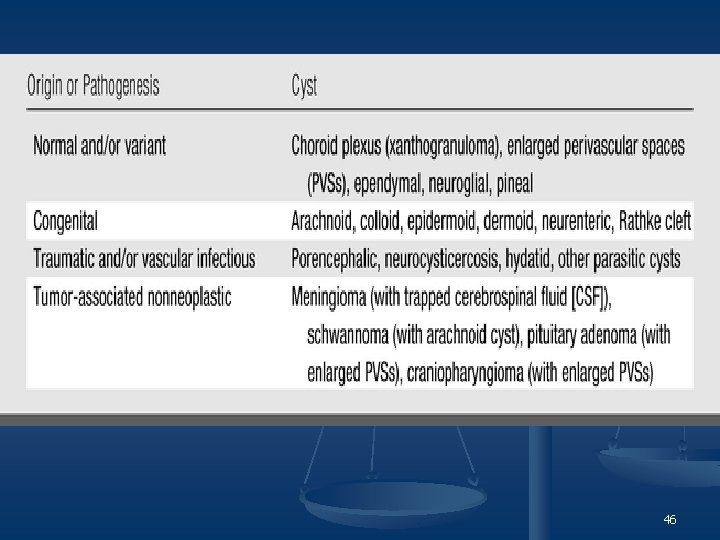
46
47
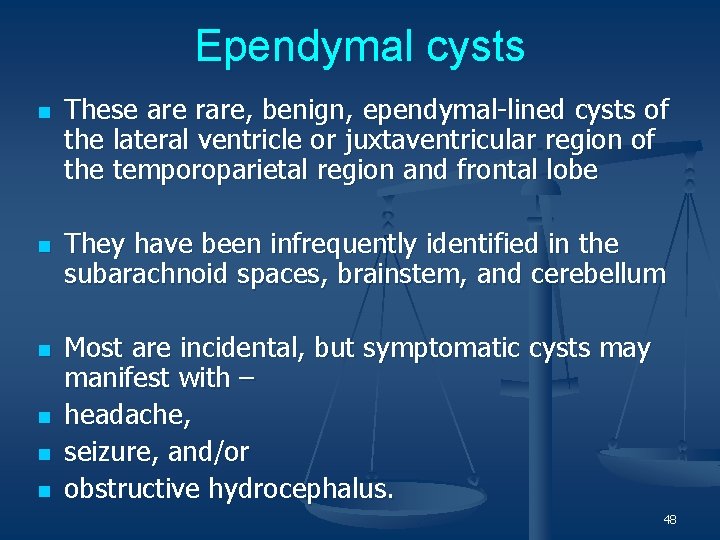
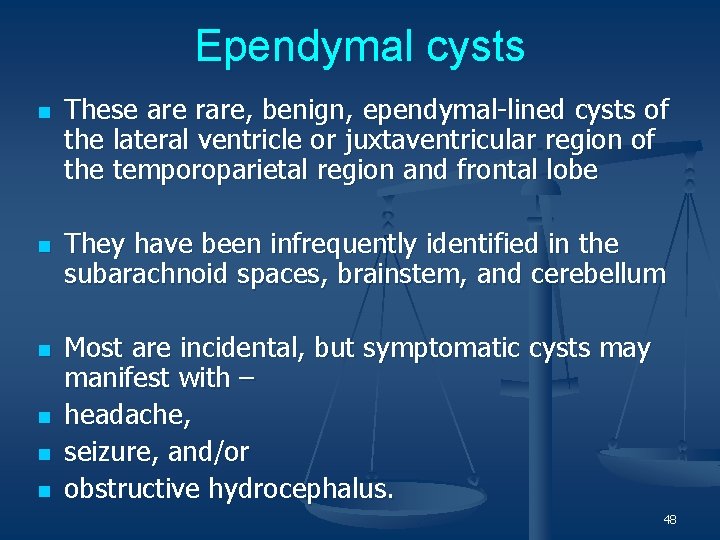
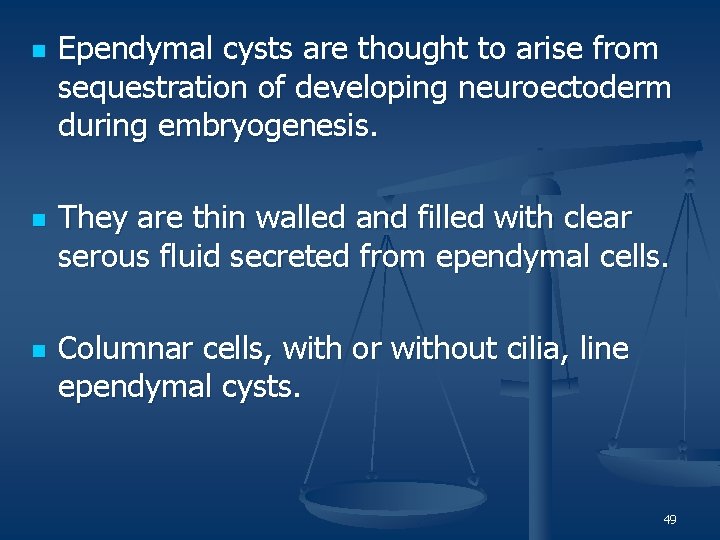
Ependymal cysts n n n These are rare, benign, ependymal-lined cysts of the lateral ventricle or juxtaventricular region of the temporoparietal region and frontal lobe They have been infrequently identified in the subarachnoid spaces, brainstem, and cerebellum Most are incidental, but symptomatic cysts may manifest with – headache, seizure, and/or obstructive hydrocephalus. 48
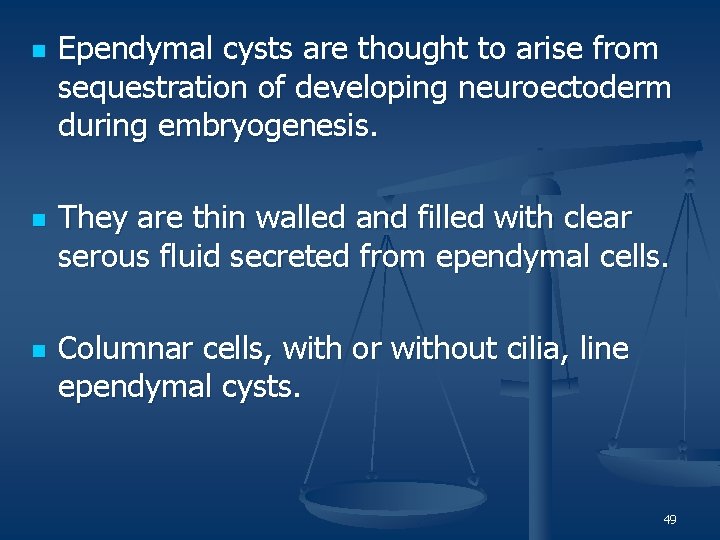
n n n Ependymal cysts are thought to arise from sequestration of developing neuroectoderm during embryogenesis. They are thin walled and filled with clear serous fluid secreted from ependymal cells. Columnar cells, with or without cilia, line ependymal cysts. 49
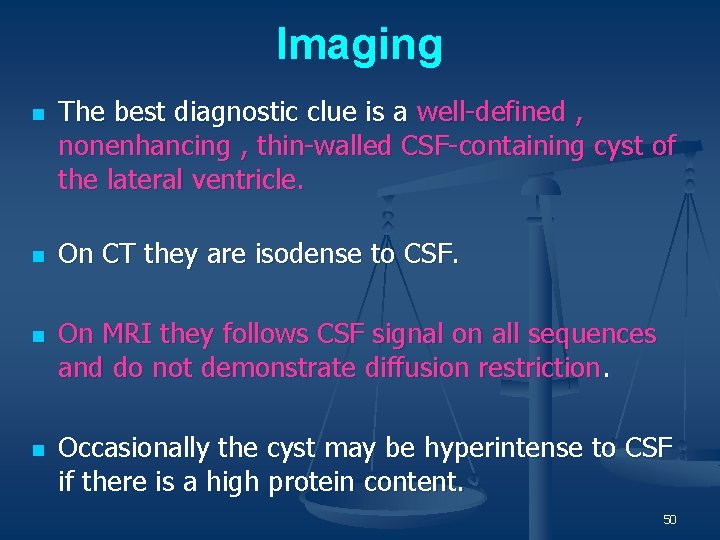
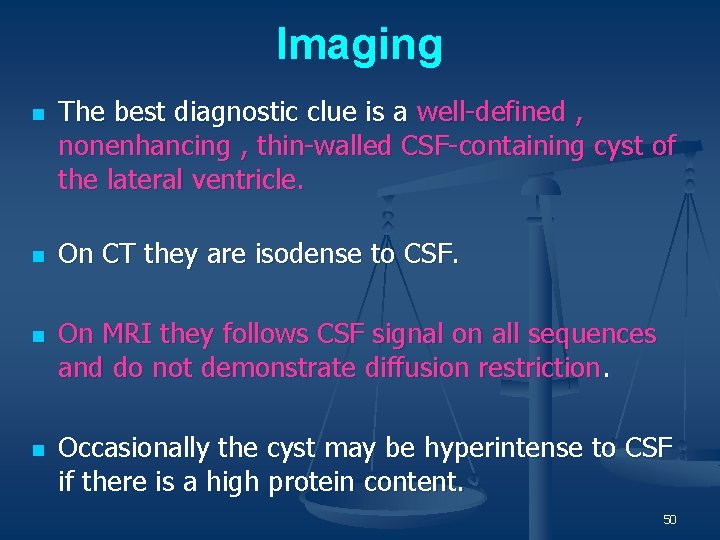
Imaging n n The best diagnostic clue is a well-defined , nonenhancing , thin-walled CSF-containing cyst of the lateral ventricle. On CT they are isodense to CSF. On MRI they follows CSF signal on all sequences and do not demonstrate diffusion restriction. Occasionally the cyst may be hyperintense to CSF if there is a high protein content. 50
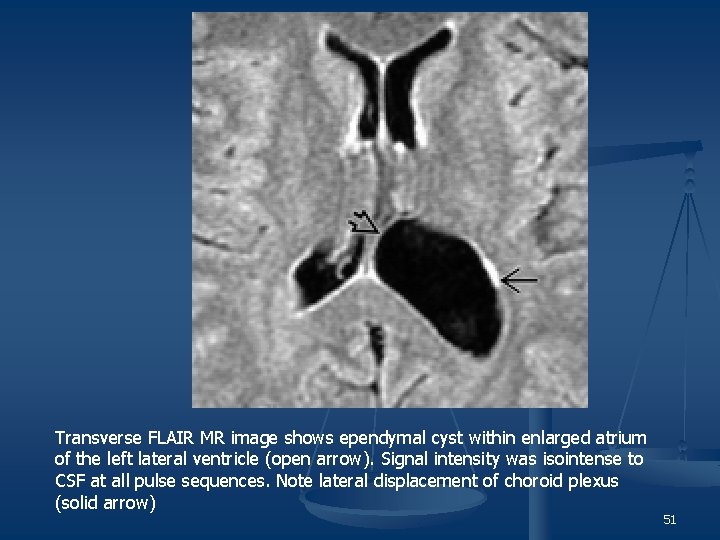
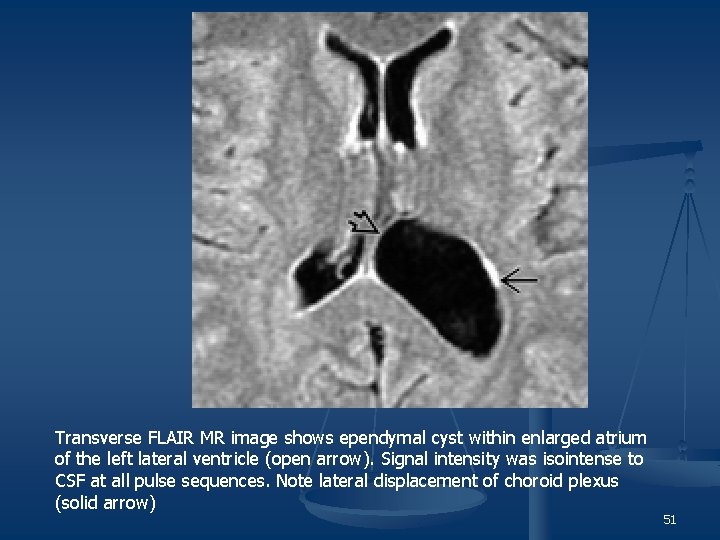
Transverse FLAIR MR image shows ependymal cyst within enlarged atrium of the left lateral ventricle (open arrow). Signal intensity was isointense to CSF at all pulse sequences. Note lateral displacement of choroid plexus (solid arrow) 51
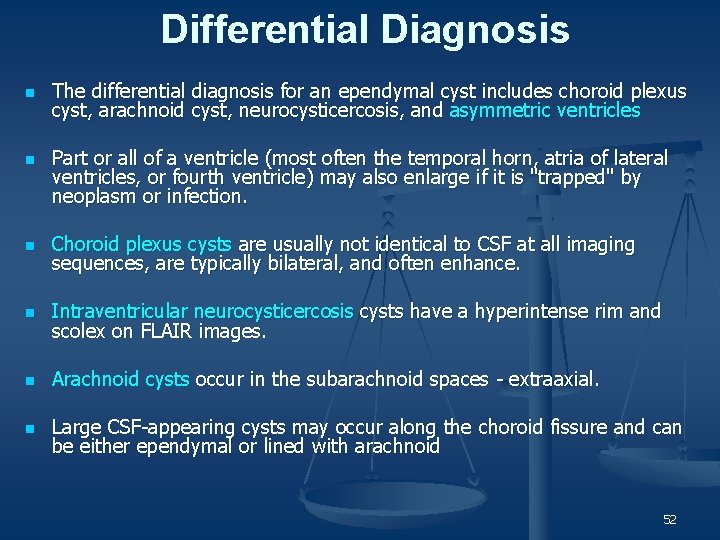
Differential Diagnosis n n The differential diagnosis for an ependymal cyst includes choroid plexus cyst, arachnoid cyst, neurocysticercosis, and asymmetric ventricles Part or all of a ventricle (most often the temporal horn, atria of lateral ventricles, or fourth ventricle) may also enlarge if it is "trapped" by neoplasm or infection. n Choroid plexus cysts are usually not identical to CSF at all imaging sequences, are typically bilateral, and often enhance. n Intraventricular neurocysticercosis cysts have a hyperintense rim and scolex on FLAIR images. n Arachnoid cysts occur in the subarachnoid spaces - extraaxial. n Large CSF-appearing cysts may occur along the choroid fissure and can be either ependymal or lined with arachnoid 52
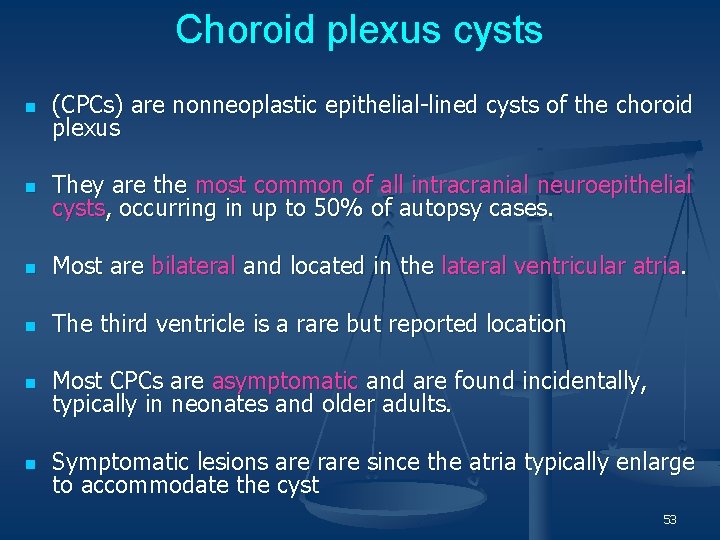
Choroid plexus cysts n (CPCs) are nonneoplastic epithelial-lined cysts of the choroid plexus n They are the most common of all intracranial neuroepithelial cysts, occurring in up to 50% of autopsy cases. n Most are bilateral and located in the lateral ventricular atria. n The third ventricle is a rare but reported location n Most CPCs are asymptomatic and are found incidentally, typically in neonates and older adults. n Symptomatic lesions are rare since the atria typically enlarge to accommodate the cyst 53
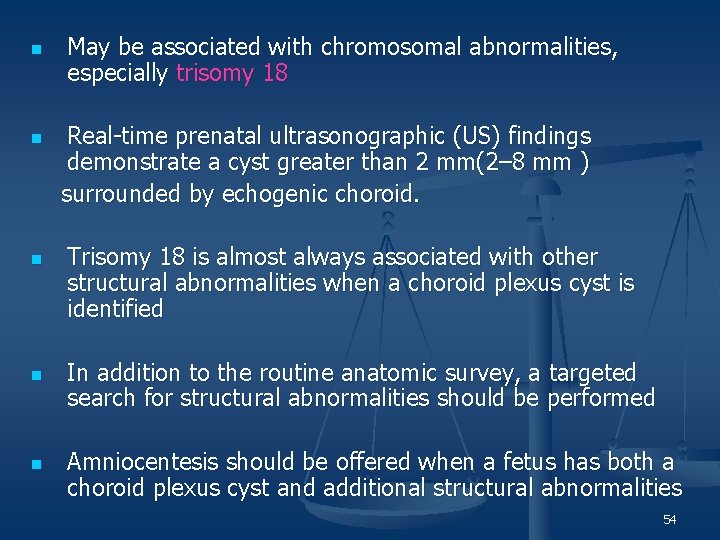
n May be associated with chromosomal abnormalities, especially trisomy 18 Real-time prenatal ultrasonographic (US) findings demonstrate a cyst greater than 2 mm(2– 8 mm ) surrounded by echogenic choroid. n n Trisomy 18 is almost always associated with other structural abnormalities when a choroid plexus cyst is identified In addition to the routine anatomic survey, a targeted search for structural abnormalities should be performed Amniocentesis should be offered when a fetus has both a choroid plexus cyst and additional structural abnormalities 54
Imaging n n n CPCs are iso- to slightly hyperattenuated on nonenhanced CT scans compared with CSF & show enhancement that varies from none to striking. Peripheral calcification is common. Signal intensity on MR images is variable. Most are iso- or hyperintense on precontrast T 1 -weighted MR images compared with CSF and show rim or nodular contrast enhancement. Hyperintense to CSF on T 2 -weighted images The majority do not become completely hypointense (suppress) on fluidattenuated inversion-recovery (FLAIR) images and remain slightly or moderately hyperintense to CSF. Two-thirds show restriction (high signal intensity) on diffusion-weighted images 55
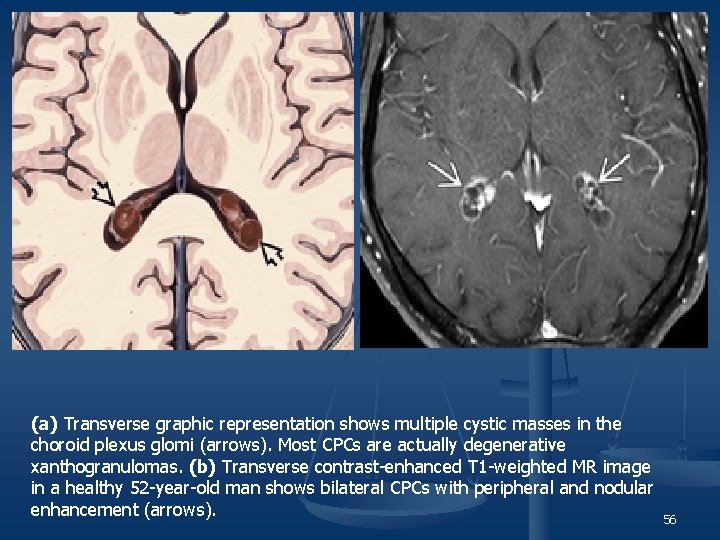
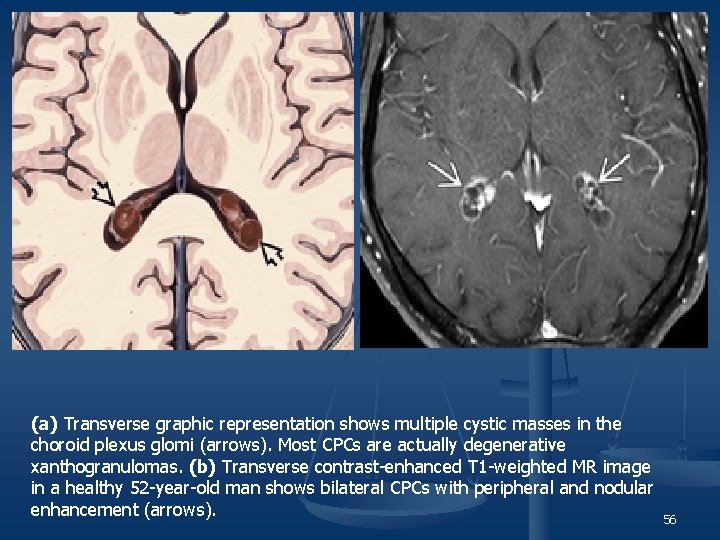
(a) Transverse graphic representation shows multiple cystic masses in the choroid plexus glomi (arrows). Most CPCs are actually degenerative xanthogranulomas. (b) Transverse contrast-enhanced T 1 -weighted MR image in a healthy 52 -year-old man shows bilateral CPCs with peripheral and nodular enhancement (arrows). 56
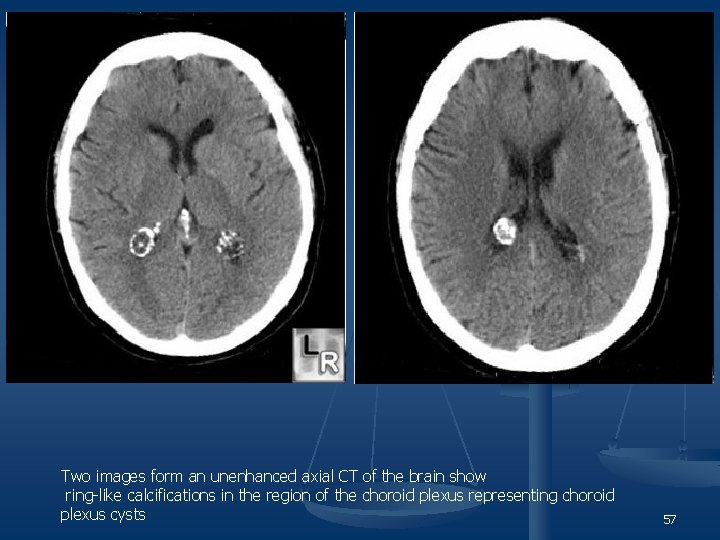
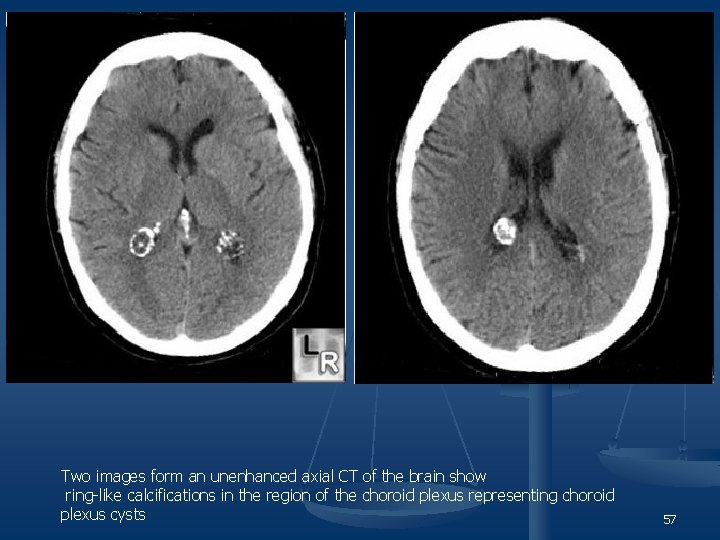
Two images form an unenhanced axial CT of the brain show ring-like calcifications in the region of the choroid plexus representing choroid plexus cysts 57
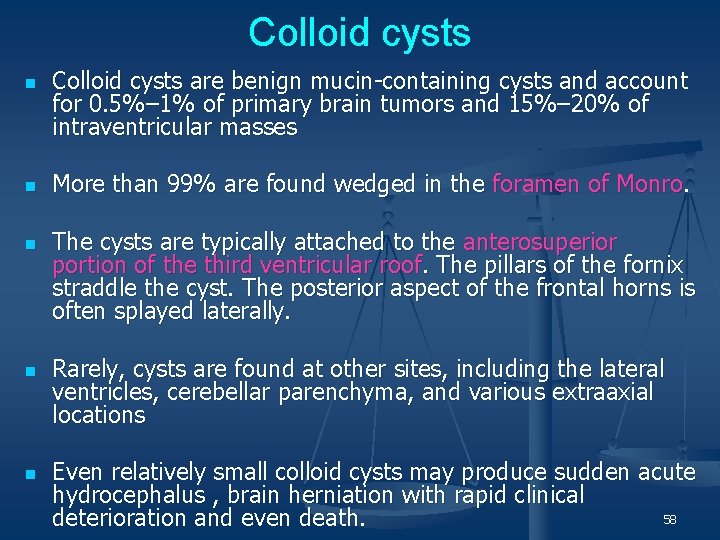
Colloid cysts n n n Colloid cysts are benign mucin-containing cysts and account for 0. 5%– 1% of primary brain tumors and 15%– 20% of intraventricular masses More than 99% are found wedged in the foramen of Monro. The cysts are typically attached to the anterosuperior portion of the third ventricular roof. The pillars of the fornix straddle the cyst. The posterior aspect of the frontal horns is often splayed laterally. Rarely, cysts are found at other sites, including the lateral ventricles, cerebellar parenchyma, and various extraaxial locations Even relatively small colloid cysts may produce sudden acute hydrocephalus , brain herniation with rapid clinical 58 deterioration and even death.
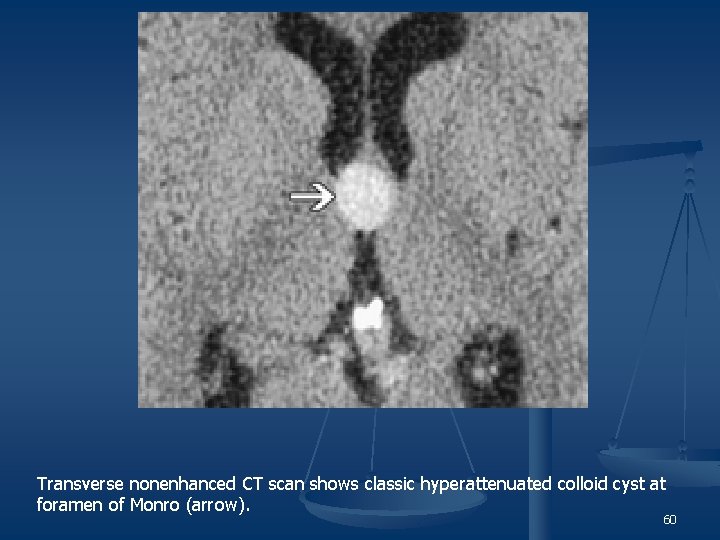
Imaging n n The best diagnostic clue to a colloid cyst is its location at the foramen of Monro. The classic colloid cyst appears as a well-delineated smooth and spherical, hyperattenuated mass on nonenhanced CT scans varying in size from 0. 3 cm to more than 4 cm in diameter. mean size is 1. 5 cm. n Attenuation correlates inversely with hydration state. n On T 1 -weighted MR images, two-thirds of colloid cysts are hyperintense. The majority are isointense to brain on T 2 -weighted images. n Some demonstrate peripheral rim enhancement n Occasionally, colloid cysts expand rapidly. These colloid cysts typically have a higher water content, which reflects ongoing cyst expansion. Thus, it is hypothesized that potentially the most "dangerous" lesions are hypointense on T 1 - and hyperintense on T 2 -weighted images 59
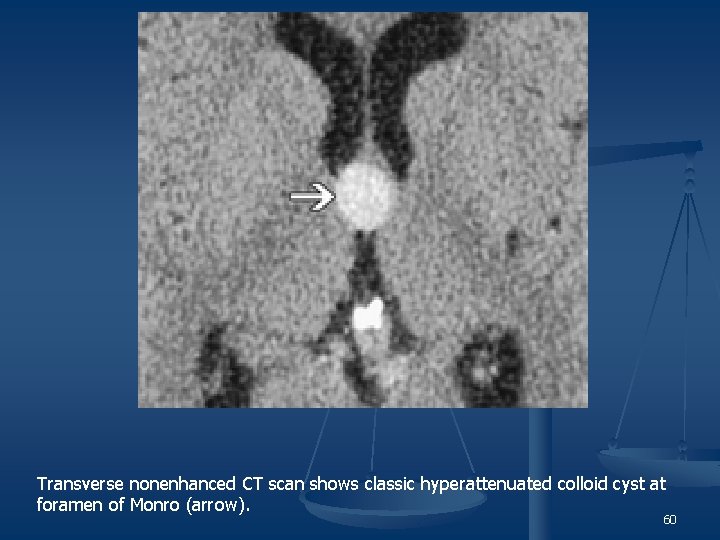
Transverse nonenhanced CT scan shows classic hyperattenuated colloid cyst at foramen of Monro (arrow). 60
Neurocysticercosis n n n Is the most common, most widely disseminated parasitic infection in the world CNS is most frequently affected organ system. Neurocysticercosis occurs in 60%– 90% of all cases of systemic cysticercosis. According to the location; cysticercosis may be of following types : 1. Meningeal 2. Parenchymal 3. Intraventricular 4. Mixed n n Meningeal & parenchymal forms are most common. Seizures are the common manifestation of neurocysticercosis 61
Intraventricular Involvement n Solitary or multiple intraventriculor cysts may be attached to the - Ventricular walls or may be - free floating n n n A large cyst or cluster of cysts within the 4 th ventricle may cause focal expansile deformities of the affected ventricle or generalised dilatation of the ventricle. Noncommunicating hydrocephalus due to obstruction of Foramen of Monro (unilateral / Bilateral) or IVth ventricle On CT intraventricular cyst may not be identified because of their thin walls , approximately CSF equavalent contents & Lack of contrast enhancement 62
n n n MR is more sensitive than CT in the evaluation of suspected intraventricular cysts. Cyst walls and also scolices can be frequently seen. Visualisation of scolex is pathognomonic of cysticercosis Occasionally the cyst are mobile Secondary obstructive hydrocephalus seen as enlargement of the ventricular system associated with thin rim of high intensity signal around the ventricle secondary to transudation of fluid through the ependyma. 63
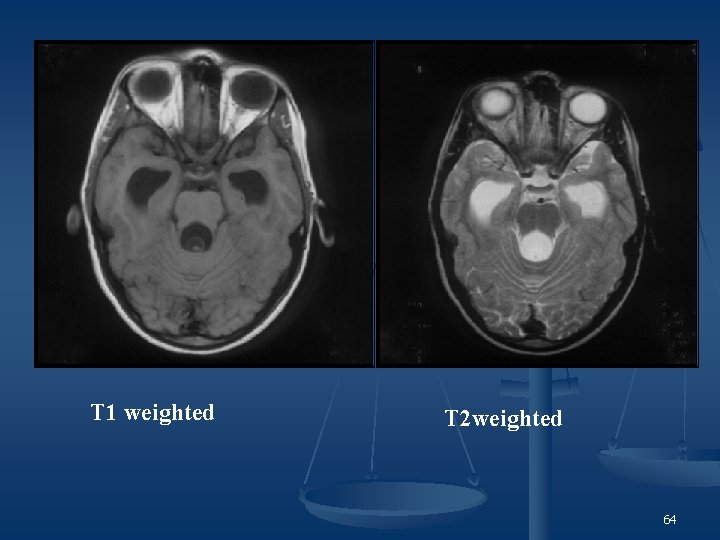
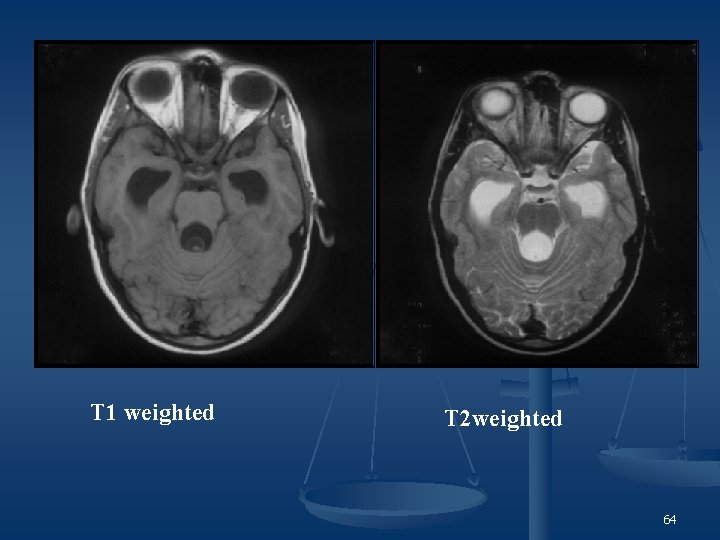
T 1 weighted T 2 weighted 64
Meningeal Involvement n n Manifested by- extra cerebral cysts - Arachnoiditis - Vasculitis CT Findings : - Since the walls of the cyst are not visible on CT & density of the fluid contents is idntical to CSF Only finding seen is focal areas of apparent enlargement of the subarachnoid spaces. 65
n MR findings : - Cyst walls are more often detected Compared to CT; Multiplanar visualisation of the basal cisterns free from bony artifact facilitates MR visualisation of these cysts. n Arachnoiditis because of breakdown of cyst walls n n n Cysts in the basal cisterns can obstruct CSF pathway with resultant communicating hydrocephalus. Vasculitis associated with memingeal cysticerosis may cause arterial narrowing & thrombosis resulting in secondary cerebral infarction. 66
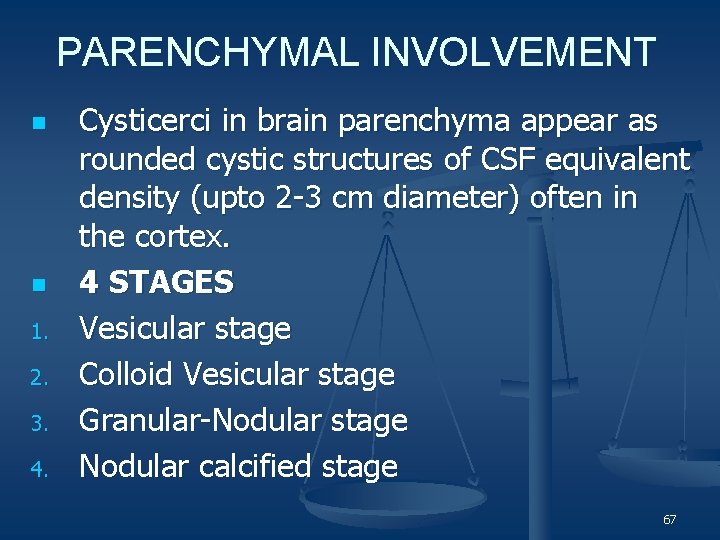
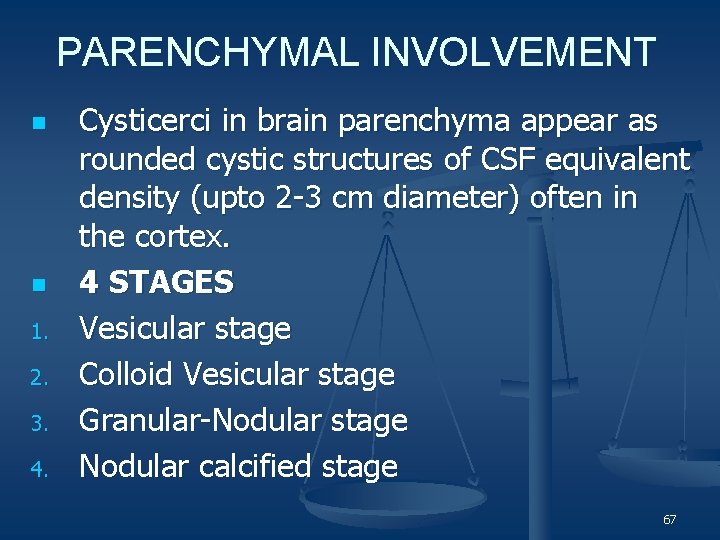
PARENCHYMAL INVOLVEMENT n n 1. 2. 3. 4. Cysticerci in brain parenchyma appear as rounded cystic structures of CSF equivalent density (upto 2 -3 cm diameter) often in the cortex. 4 STAGES Vesicular stage Colloid Vesicular stage Granular-Nodular stage Nodular calcified stage 67
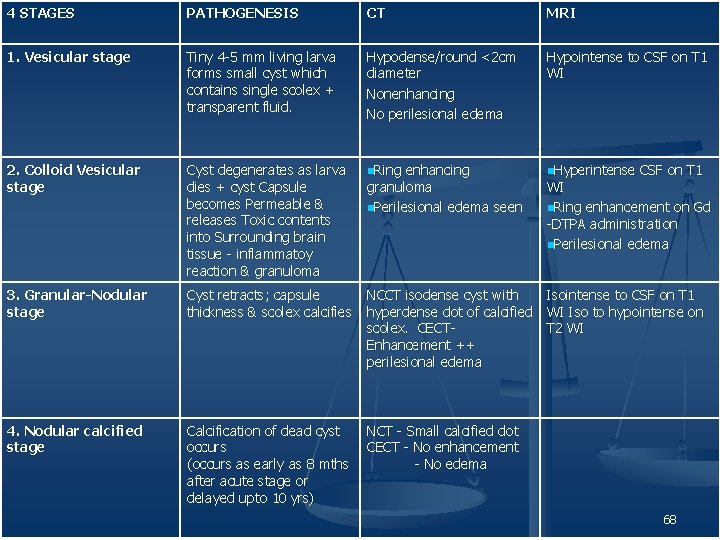
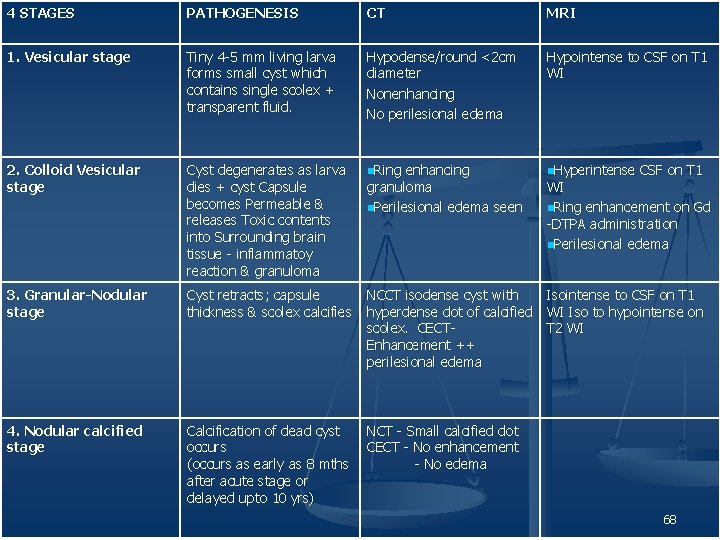
4 STAGES PATHOGENESIS CT MRI 1. Vesicular stage Tiny 4 -5 mm living larva forms small cyst which contains single scolex + transparent fluid. Hypodense/round <2 cm diameter Nonenhancing No perilesional edema Hypointense to CSF on T 1 WI 2. Colloid Vesicular stage Cyst degenerates as larva dies + cyst Capsule becomes Permeable & releases Toxic contents into Surrounding brain tissue - inflammatoy reaction & granuloma n. Ring enhancing n. Hyperintense CSF on T 1 3. Granular-Nodular stage Cyst retracts; capsule NCCT isodense cyst with thickness & scolex calcifies hyperdense dot of calcified scolex. CECTEnhancement ++ perilesional edema 4. Nodular calcified stage Calcification of dead cyst occurs (occurs as early as 8 mths after acute stage or delayed upto 10 yrs) granuloma n. Perilesional edema seen WI n. Ring enhancement on Gd -DTPA administration n. Perilesional edema Isointense to CSF on T 1 WI Iso to hypointense on T 2 WI NCT - Small calcified dot CECT - No enhancement - No edema 68
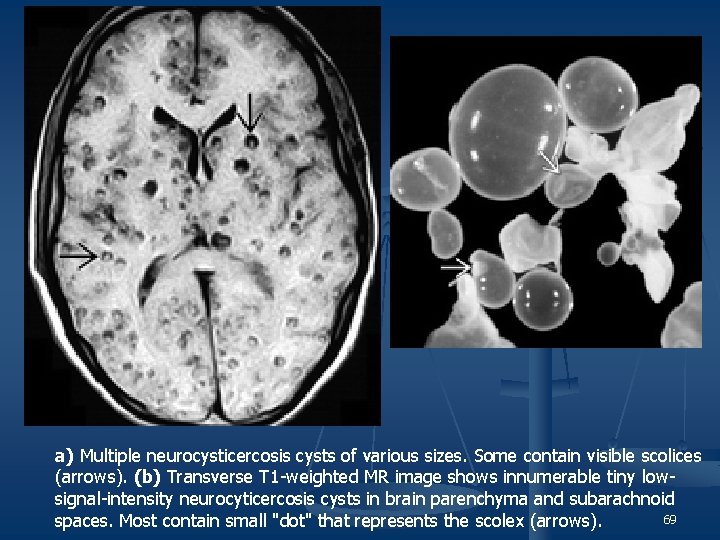
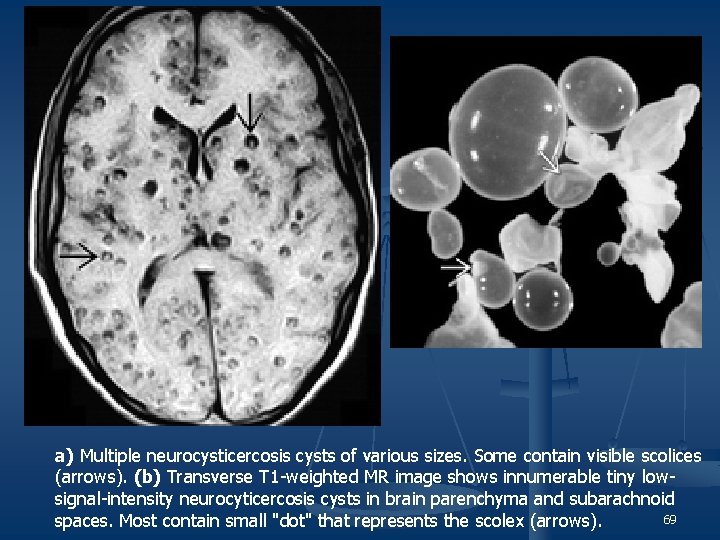
a) Multiple neurocysticercosis cysts of various sizes. Some contain visible scolices (arrows). (b) Transverse T 1 -weighted MR image shows innumerable tiny lowsignal-intensity neurocyticercosis cysts in brain parenchyma and subarachnoid 69 spaces. Most contain small "dot" that represents the scolex (arrows).
Case - 4 70
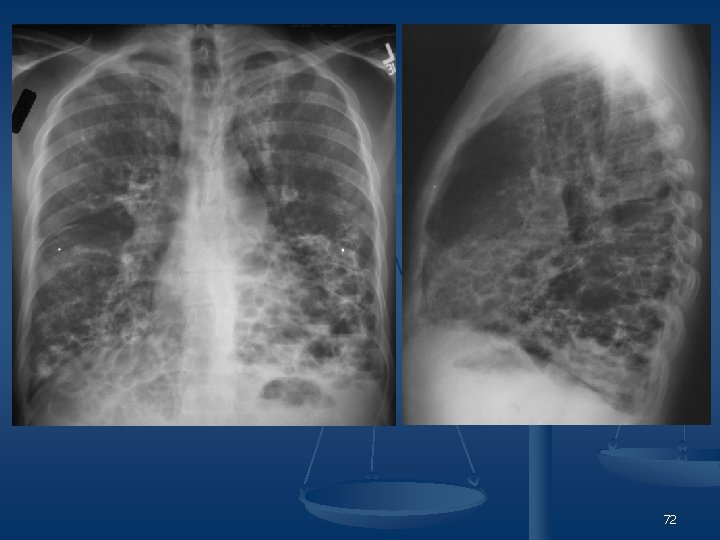
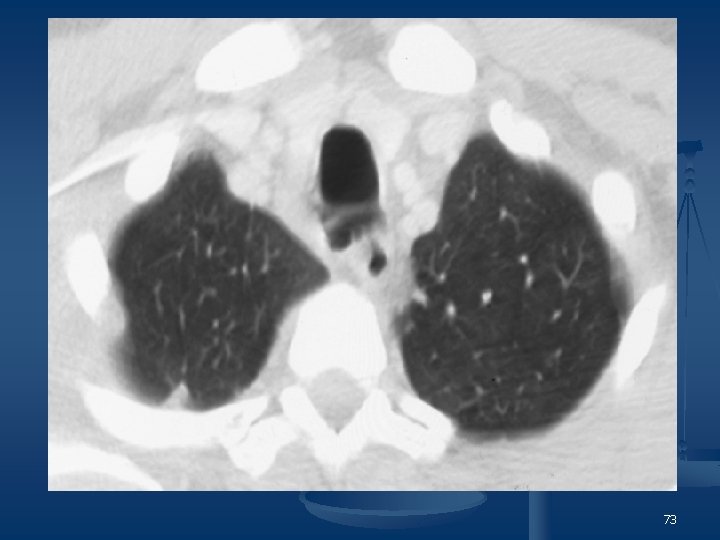
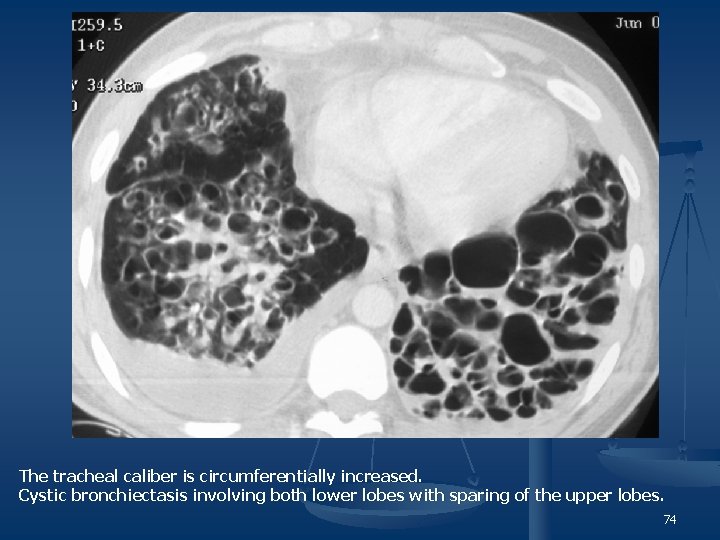
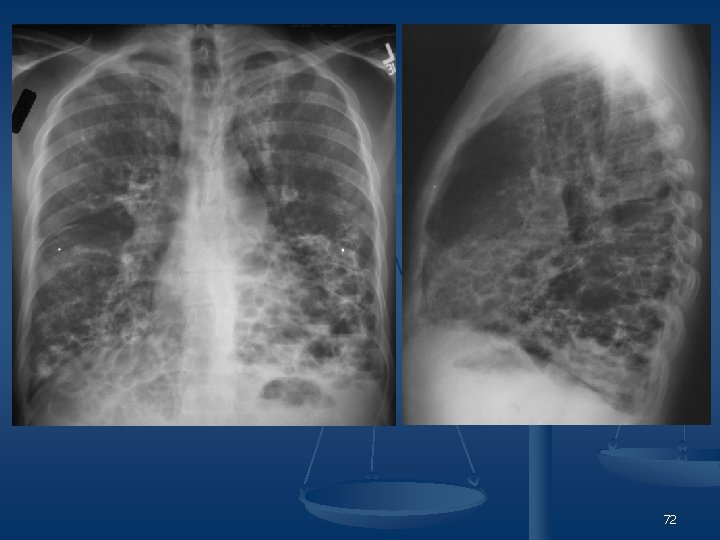
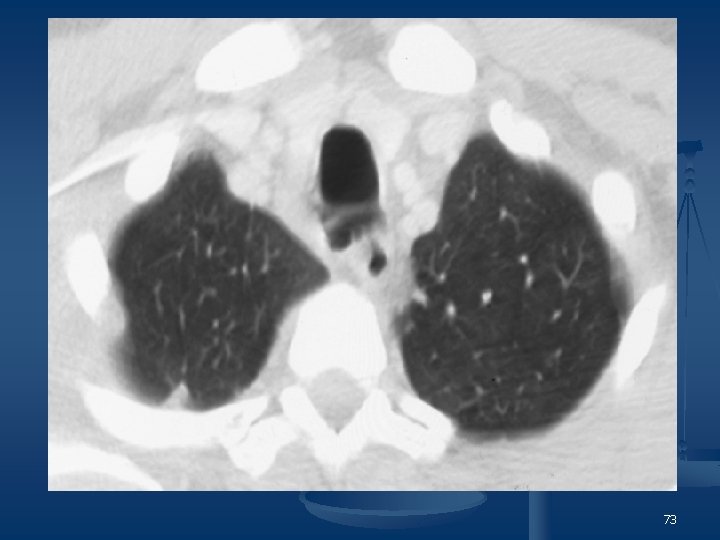
29 year old man with a history of recurrent pneumonia presenting with hemoptysis. 71
72
73
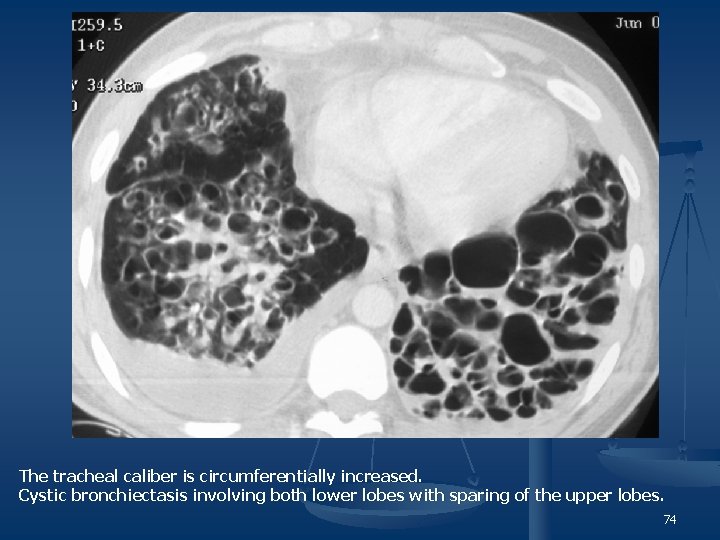
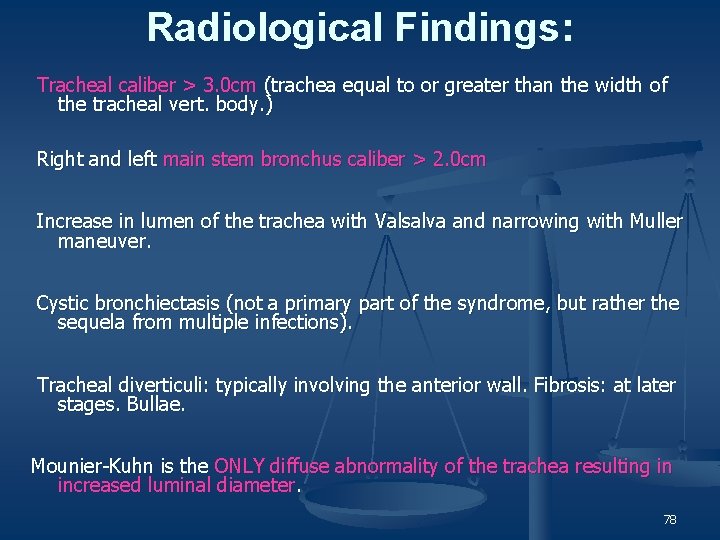
The tracheal caliber is circumferentially increased. Cystic bronchiectasis involving both lower lobes with sparing of the upper lobes. 74
Mounier Kuhn Syndrome n n Tracheobronchomegaly, is a rare congenital disorder of connective tissue that affects the trachea and major bronchi. Rapid change to normal caliber at the 4 th-5 th order of bronchi. The etiology is unknown. Most cases are sporadic, but there may be a familial trait (autosomal recessive); it has been associated with Ehlers-Danlos syndrome. Connective tissue defect > atrophy of the elastic and smooth muscle tissue of the trachea and main bronchi > protrusion of redundant mucosa through the tracheal cartilaginous rings (tracheal “diverticuli”), producing a corrugated appearance to the anterior aspect of the trachea. There is pooling of secretions in the corrugated herniations, leading to recurrent lower respiratory tract infections and bronchiectasis. 75
n Abnormal airway dynamics and pooling of secretions in broad outpouchings predispose to the development of Pulmonary fibrosis n Emphysema n Bronchiectasis n Chronic pulmonary suppuration n 76
n males >>>female n n n n n Especially African Americans Occurs most often during the third and fourth decades of life Signs and symptom range from minimal disease with preservation of pulmonary function to progressive disease leading to respiratory failure and death recurrent pneumonia loud cough with copious sputum production hoarseness dyspnea on exertion spontaneous pneumothorax The flaccid dilated trachea dilates on inspiration and collapses on exhalation and cough. 77
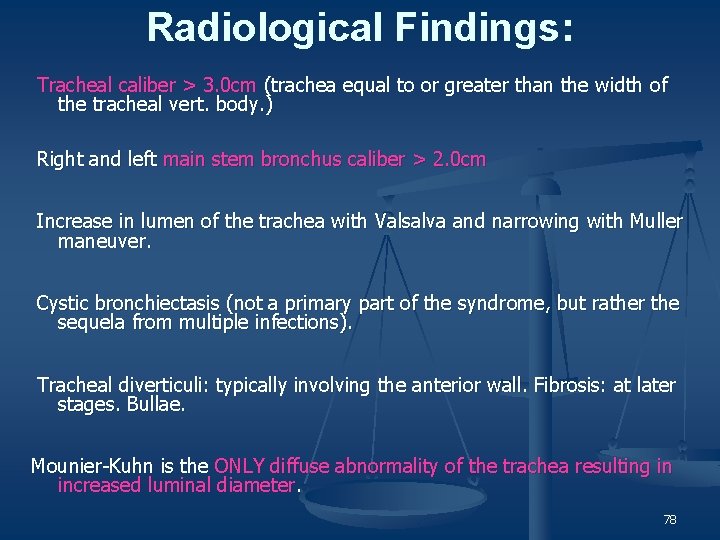
Radiological Findings: Tracheal caliber > 3. 0 cm (trachea equal to or greater than the width of the tracheal vert. body. ) Right and left main stem bronchus caliber > 2. 0 cm Increase in lumen of the trachea with Valsalva and narrowing with Muller maneuver. Cystic bronchiectasis (not a primary part of the syndrome, but rather the sequela from multiple infections). Tracheal diverticuli: typically involving the anterior wall. Fibrosis: at later stages. Bullae. Mounier-Kuhn is the ONLY diffuse abnormality of the trachea resulting in increased luminal diameter. 78
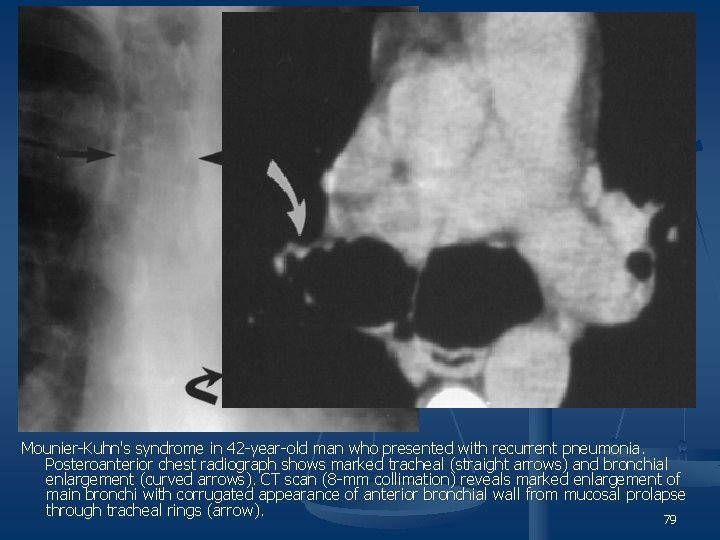
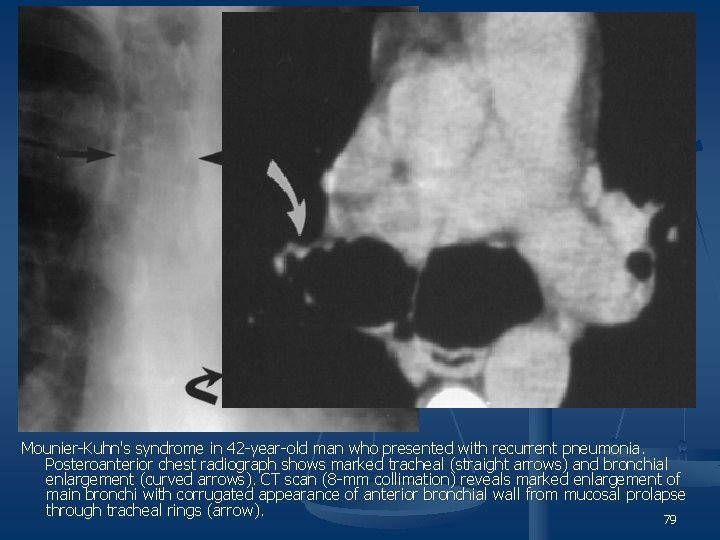
Mounier-Kuhn's syndrome in 42 -year-old man who presented with recurrent pneumonia. Posteroanterior chest radiograph shows marked tracheal (straight arrows) and bronchial enlargement (curved arrows). CT scan (8 -mm collimation) reveals marked enlargement of main bronchi with corrugated appearance of anterior bronchial wall from mucosal prolapse through tracheal rings (arrow). 79
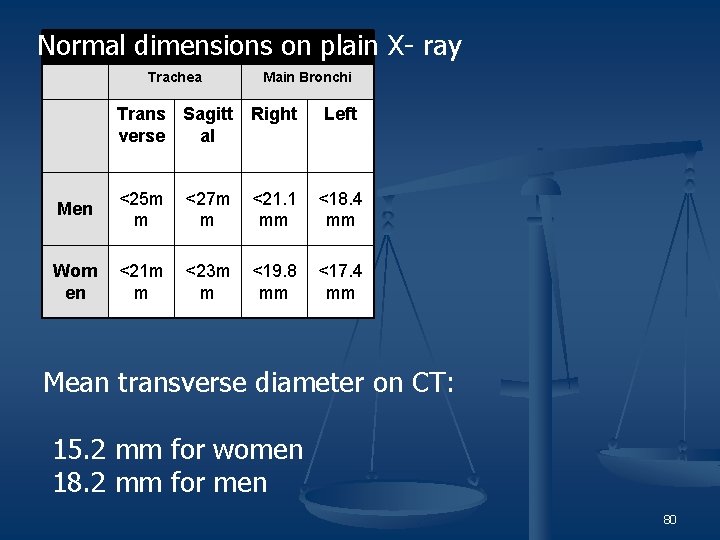
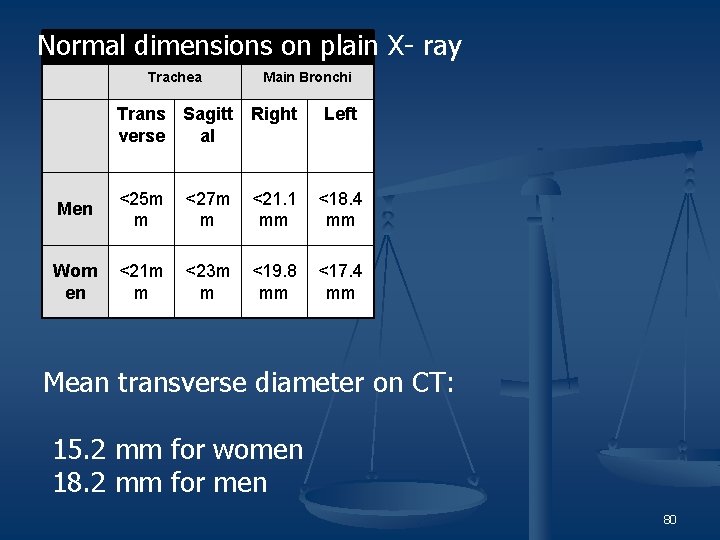
Normal Dimensions of Trachea and Bronchi Normal dimensions on plain X- ray Trachea Main Bronchi Trans Sagitt verse al Right Left Men <25 m m <27 m m <21. 1 mm <18. 4 mm Wom en <21 m m <23 m m <19. 8 mm <17. 4 mm Mean transverse diameter on CT: 15. 2 mm for women 18. 2 mm for men 80
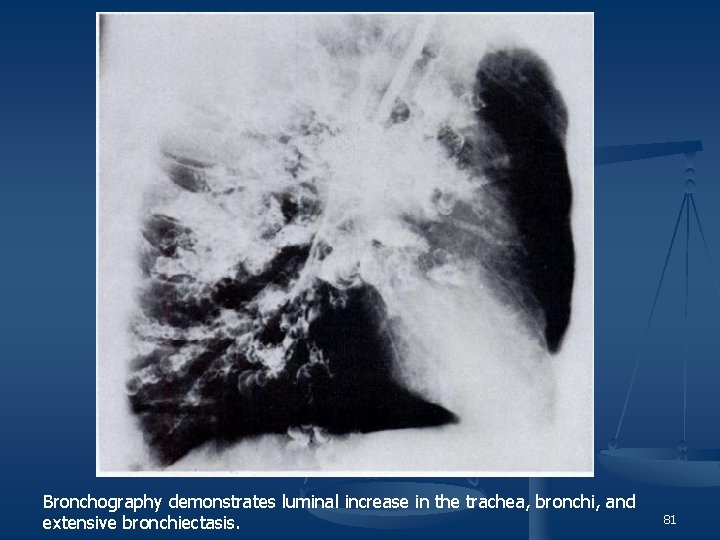
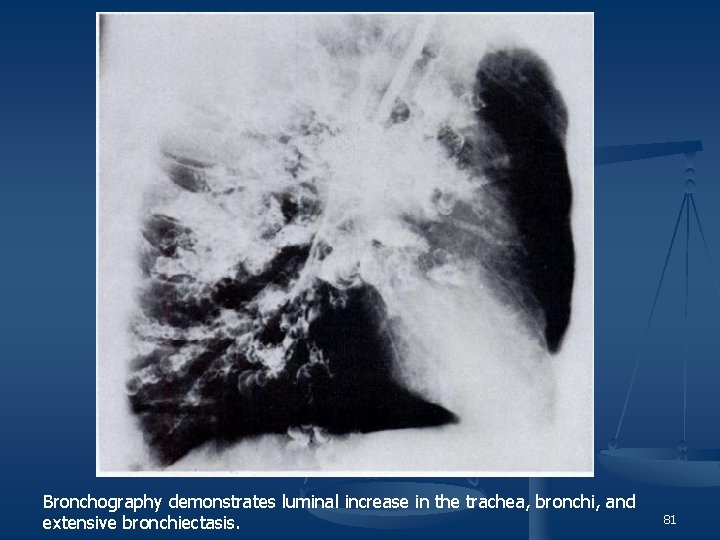
Bronchography demonstrates luminal increase in the trachea, bronchi, and extensive bronchiectasis. 81
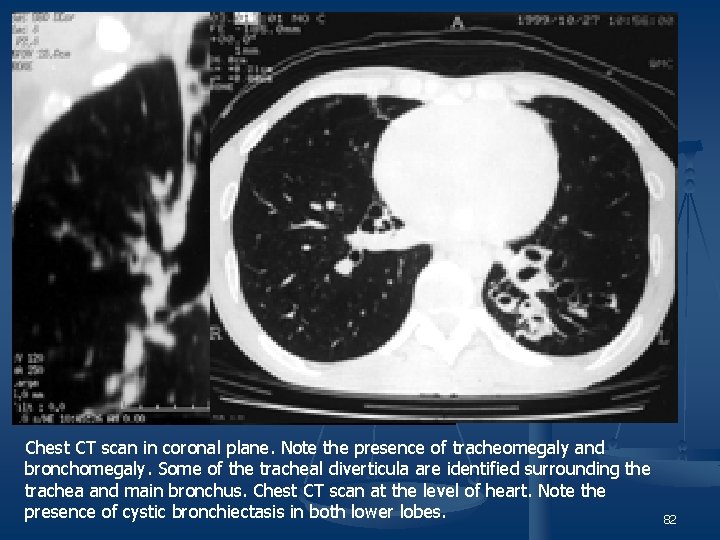
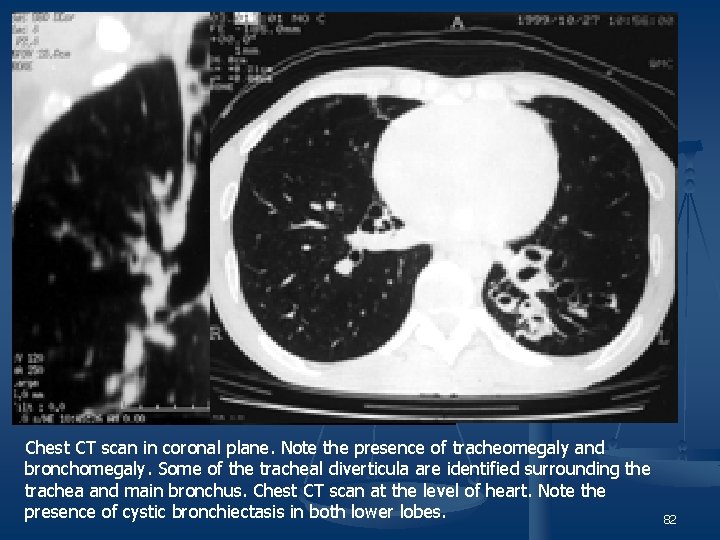
Chest CT scan in coronal plane. Note the presence of tracheomegaly and bronchomegaly. Some of the tracheal diverticula are identified surrounding the trachea and main bronchus. Chest CT scan at the level of heart. Note the presence of cystic bronchiectasis in both lower lobes. 82

83

84

85

86

87
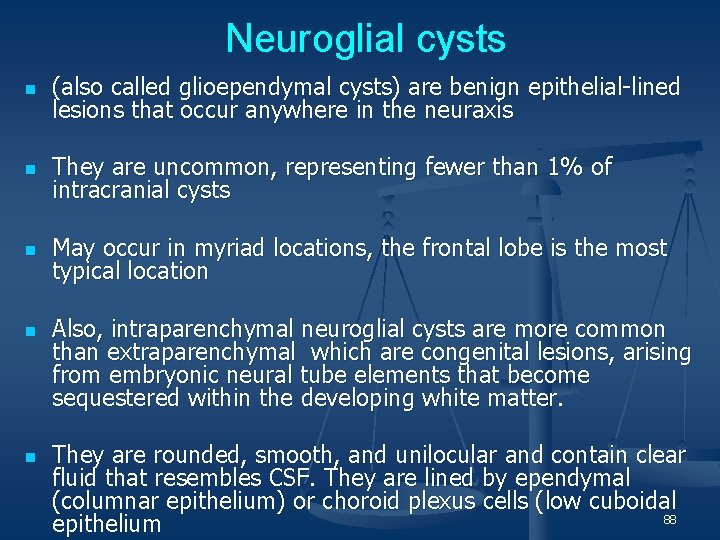
Neuroglial cysts n (also called glioependymal cysts) are benign epithelial-lined lesions that occur anywhere in the neuraxis n They are uncommon, representing fewer than 1% of intracranial cysts n May occur in myriad locations, the frontal lobe is the most typical location n n Also, intraparenchymal neuroglial cysts are more common than extraparenchymal which are congenital lesions, arising from embryonic neural tube elements that become sequestered within the developing white matter. They are rounded, smooth, and unilocular and contain clear fluid that resembles CSF. They are lined by ependymal (columnar epithelium) or choroid plexus cells (low cuboidal 88 epithelium
Imaging n n n The best diagnostic clue to a neuroglial cyst is a nonenhancing CSF-like parenchymal cyst with minimal to no surrounding signal intensity abnormality. The cysts are benign-appearing lesions with smooth, rounded borders Size is variable. 89
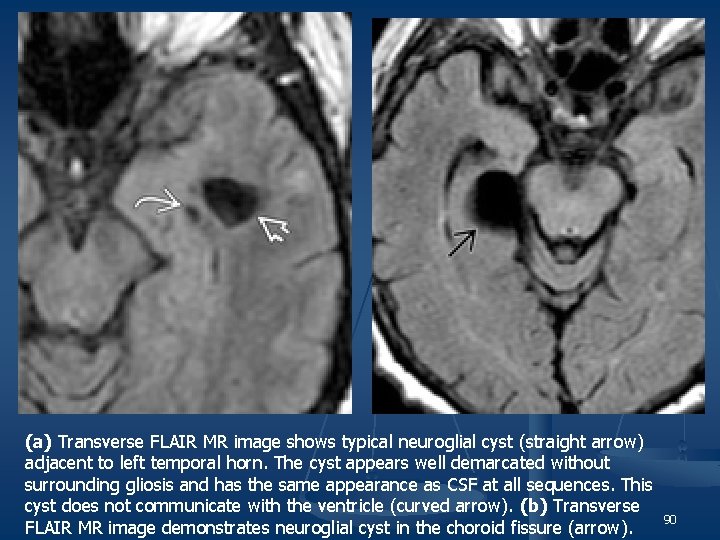
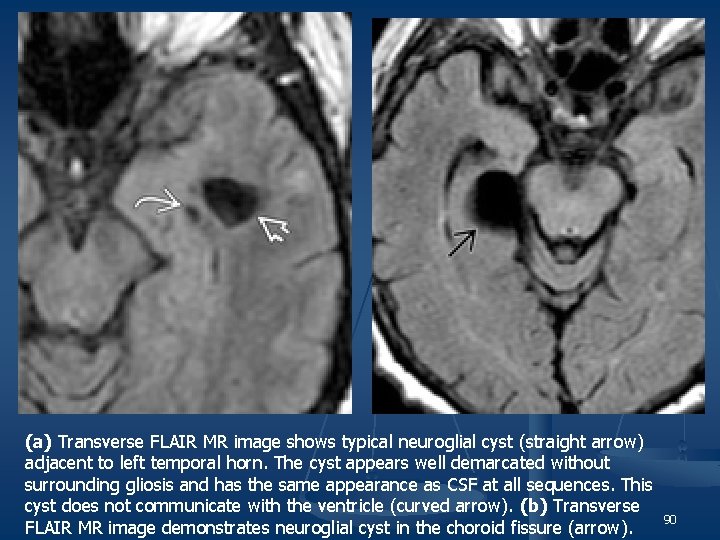
(a) Transverse FLAIR MR image shows typical neuroglial cyst (straight arrow) adjacent to left temporal horn. The cyst appears well demarcated without surrounding gliosis and has the same appearance as CSF at all sequences. This cyst does not communicate with the ventricle (curved arrow). (b) Transverse 90 FLAIR MR image demonstrates neuroglial cyst in the choroid fissure (arrow).
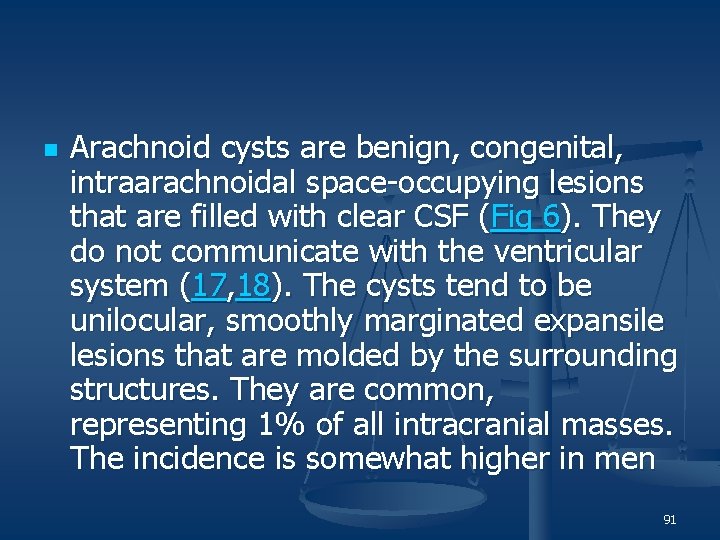
n Arachnoid cysts are benign, congenital, intraarachnoidal space-occupying lesions that are filled with clear CSF (Fig 6). They do not communicate with the ventricular system (17, 18). The cysts tend to be unilocular, smoothly marginated expansile lesions that are molded by the surrounding structures. They are common, representing 1% of all intracranial masses. The incidence is somewhat higher in men 91
n n n Most arachnoid cysts are supratentorial. Fifty to 60% are found in the middle cranial fossa, anterior to the temporal lobes. Other locations include the suprasellar cistern and posterior fossa (10%), where they occur most commonly in the cerebellopontine angle cistern. Less common locations are within the interhemispheric fissure; over the cerebral convexity; or in the choroidal fissure, cisterna magna, quadrigeminal cistern, and the vermian fissures (15– 18). The precise mechanism for the formation of arachnoid cysts is not known (15, 18). It is possible that they are secondary to "splitting" or a diverticulum of the developing arachnoid. A newer concept for the middle fossa arachnoid cyst is the failure of temporal embryonic meninges to merge as the sylvian fissure forms. These two layers remain separate, forming duplicate arachnoid. Other mechanisms might include active fluid secretion by the cyst wall, slow distention by CSF pulsations, or one-way ball-valve flow of CSF (17). The cause has also been attributed to trauma, mastoiditis, meningitis, and subarachnoid hemorrhage (19). Arachnoid cysts are generally stable over time, although cases of sudden or progressive enlargement, as well as spontaneous resolution, have been reported (20, 21). Arachnoid cysts collapse on incision. Therefore, surgical specimens are usually limited to a portion of the outer wall. The transparent cyst wall is separate from the inner dural layer and the underlying pia-arachnoid. Most are filled with clear colorless fluid. The size varies, from small and incidental to a large space-occupying lesion with extensive compression of the underlying brain (15, 17, 18). Microscopically, the cyst wall is made of a vascular collagenous membrane lined by flattened arachnoid cells (3, 18). Arachnoid cysts lack a glial-limiting membrane or an epithelial lining ( 92
n n n Imaging The best diagnostic clue is a sharply demarcated extraaxial cyst that can displace or deform adjacent brain. Scalloping of the adjacent calvarium is often seen. The classic arachnoid cyst has no identifiable internal architecture and does not enhance. The cyst typically has the same signal intensity as CSF at all sequences. Occasionally, however, hemorrhage, high protein content, or lack of flow within the cyst may complicate the MR appearance ( 15, 17, 18). Arachnoid cysts have an increased prevalence of coexisting subdural hematomas, especially when they occur in the middle cranial fossa. Differential Diagnosis The most difficult lesion to distinguish from the arachnoid cyst is an epidermoid cyst. Epidermoid cysts can appear nearly identical to CSF on CT scans. On MR images, epidermoid cysts appear isointense to CSF, although close inspection often shows they are not precisely identical in signal intensity to CSF. Arachnoid cysts typically suppress completely on FLAIR images and do not restrict on diffusion-weighted images. Occasionally an arachnoid cyst can be slightly hyperintense on images obtained with a long repetition time and a short echo time. Arachnoid cysts displace adjacent arteries and cranial nerves rather than engulf them, as epidermoid cysts often do (17– 19). Chronic subdural hematoma and porencephalic cyst can also be confused for an arachnoid cyst. Chronic subdural hematomas do not typically show CSF signal intensity on MR images and often have an enhancing membrane. Porencephalic cysts often follow a history of trauma or stroke. The cysts are normally surrounded by gliotic brain ( 93
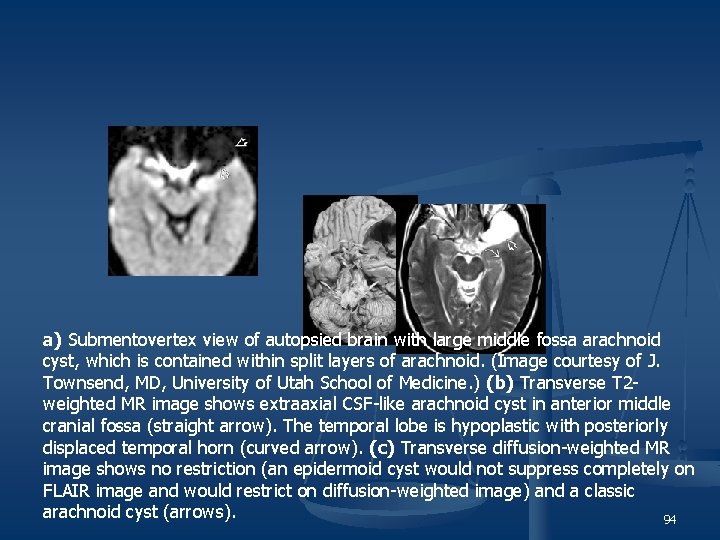
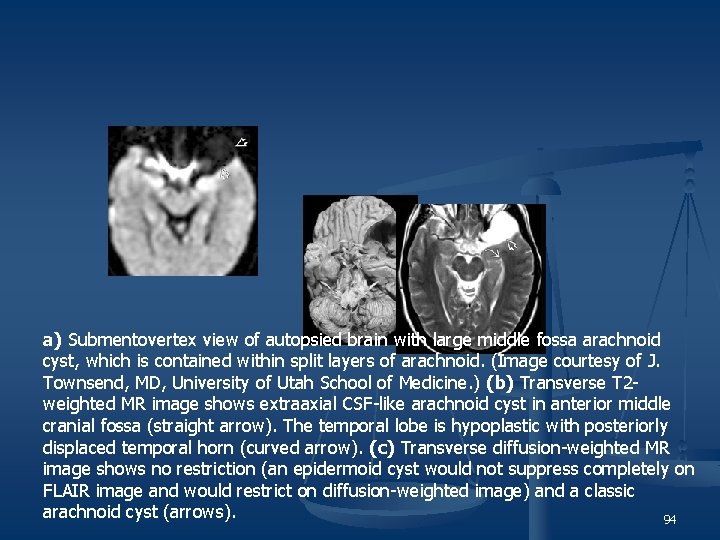
a) Submentovertex view of autopsied brain with large middle fossa arachnoid cyst, which is contained within split layers of arachnoid. (Image courtesy of J. Townsend, MD, University of Utah School of Medicine. ) (b) Transverse T 2 weighted MR image shows extraaxial CSF-like arachnoid cyst in anterior middle cranial fossa (straight arrow). The temporal lobe is hypoplastic with posteriorly displaced temporal horn (curved arrow). (c) Transverse diffusion-weighted MR image shows no restriction (an epidermoid cyst would not suppress completely on FLAIR image and would restrict on diffusion-weighted image) and a classic arachnoid cyst (arrows). 94
 Rakhi lalwani
Rakhi lalwani Rakhi lalwani
Rakhi lalwani Iron deficiency anemia
Iron deficiency anemia Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Department of agriculture consumer services
Department of agriculture consumer services Horizontal
Horizontal Albany county dept of social services
Albany county dept of social services Dept of education
Dept of education Mn dept of education
Mn dept of education Nys dept of homeland security
Nys dept of homeland security Maine department of agriculture conservation and forestry
Maine department of agriculture conservation and forestry Nebraska dept of agriculture
Nebraska dept of agriculture Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) Dept a
Dept a Finance department organizational chart
Finance department organizational chart Gome dept
Gome dept Bromocicloesano
Bromocicloesano Ms department of finance and administration
Ms department of finance and administration La dept of revenue
La dept of revenue Dept of education
Dept of education Vaginal dept
Vaginal dept Iit
Iit Worcester plumbing inspector
Worcester plumbing inspector Central islip fire dept
Central islip fire dept Hoe dept
Hoe dept Pt dept logistik
Pt dept logistik Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) La revenue dept
La revenue dept Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services Dept nmr spectroscopy
Dept nmr spectroscopy Gome dept
Gome dept Gome dept
Gome dept Dept ind onegov
Dept ind onegov Dept. name of organization
Dept. name of organization Rowan county medicaid
Rowan county medicaid Lafd interview questions
Lafd interview questions Ohio employment first
Ohio employment first Continuing education library oxford
Continuing education library oxford Torrance memorial medical center medical records
Torrance memorial medical center medical records California medical license for foreign medical graduates
California medical license for foreign medical graduates Cartersville medical center medical records
Cartersville medical center medical records Gbmc medical records
Gbmc medical records Difference between medical report and medical certificate
Difference between medical report and medical certificate Cvip medical
Cvip medical Mifepristrone
Mifepristrone Medical education reform programme
Medical education reform programme Villages medical centre
Villages medical centre Gingivia game
Gingivia game Integrative medicine santa rosa
Integrative medicine santa rosa Joint medical holdings
Joint medical holdings Regulated medical waste un3291
Regulated medical waste un3291 Medical mycology exam
Medical mycology exam Documenters of the medical record
Documenters of the medical record Ospital ng maynila address
Ospital ng maynila address Troubleshooting medical equipment
Troubleshooting medical equipment Continuing medical education
Continuing medical education Types of medical records
Types of medical records Activities of daily living index odsp
Activities of daily living index odsp Emergency medical dispatch guidecards
Emergency medical dispatch guidecards Grade medical term
Grade medical term Spie medical imaging
Spie medical imaging Fusion medical staffing llc
Fusion medical staffing llc Servier medical art
Servier medical art Lapar medical term
Lapar medical term Keputusan medical check up
Keputusan medical check up Hospital waste management ppt
Hospital waste management ppt Hawler medical university college of nursing
Hawler medical university college of nursing Kuwait medical association training center
Kuwait medical association training center Observational medical outcomes partnership
Observational medical outcomes partnership Medical meeting
Medical meeting What is a medical detective
What is a medical detective Medical terminology chapter 14 labeling exercises
Medical terminology chapter 14 labeling exercises Gastralgia medical term
Gastralgia medical term Pros and cons for animal testing
Pros and cons for animal testing What is an mr number medical
What is an mr number medical Linda stanhope
Linda stanhope Medical researchers followed 6272 swedish
Medical researchers followed 6272 swedish Queens medical center internship
Queens medical center internship Hpn medical
Hpn medical Chapter 6:2 using medical abbreviations
Chapter 6:2 using medical abbreviations Marden medical centre
Marden medical centre Pcma
Pcma Medical terminology lesson 4
Medical terminology lesson 4 Medical genetics lecture
Medical genetics lecture Servier medical art
Servier medical art Morehouse medical associates
Morehouse medical associates Outpatient medical center leesville la
Outpatient medical center leesville la Chapter 10 labeling medical terminology
Chapter 10 labeling medical terminology Rita works as a medical coder
Rita works as a medical coder Servier medical art
Servier medical art Public domain medical images
Public domain medical images Pleuralgia medical definition
Pleuralgia medical definition Etr pte
Etr pte Medical dosage calculations 10th edition
Medical dosage calculations 10th edition Medical sociology
Medical sociology