TEACHING FILE Dr Payal Damor R 2 Radiodiagnosis

![Causes of lower limb bowing • Developmental [physiological bowing] • Congenital Bowing • Tibia Causes of lower limb bowing • Developmental [physiological bowing] • Congenital Bowing • Tibia](https://slidetodoc.com/presentation_image/b9d5ca3fcb046a0a12f238c466fbf5b9/image-6.jpg)


![A six stage classification system for Blount disease [ proposed by langenskiold ] is A six stage classification system for Blount disease [ proposed by langenskiold ] is](https://slidetodoc.com/presentation_image/b9d5ca3fcb046a0a12f238c466fbf5b9/image-13.jpg)
















- Slides: 80
TEACHING FILE Dr Payal Damor R 2 Radiodiagnosis S. S. G. H BARODA
CASES 1

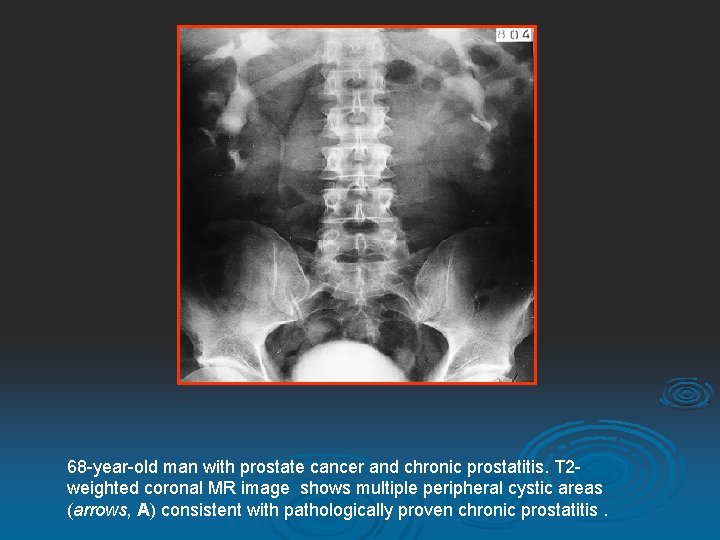
8 year male presented with a one year history of progressively worsening knee pain.
X ray both keee (AP) showing depression & irregularity of the proximal tibial metaphyses posteromedially.
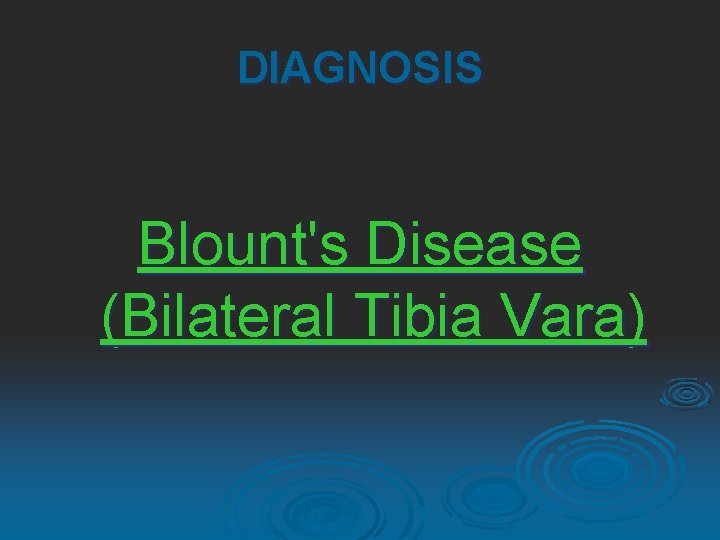
DIAGNOSIS Blount's Disease (Bilateral Tibia Vara)
![Causes of lower limb bowing Developmental physiological bowing Congenital Bowing Tibia Causes of lower limb bowing • Developmental [physiological bowing] • Congenital Bowing • Tibia](https://slidetodoc.com/presentation_image/b9d5ca3fcb046a0a12f238c466fbf5b9/image-6.jpg)
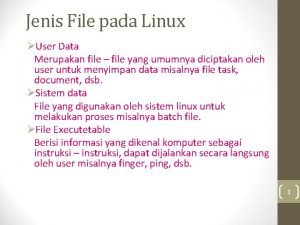
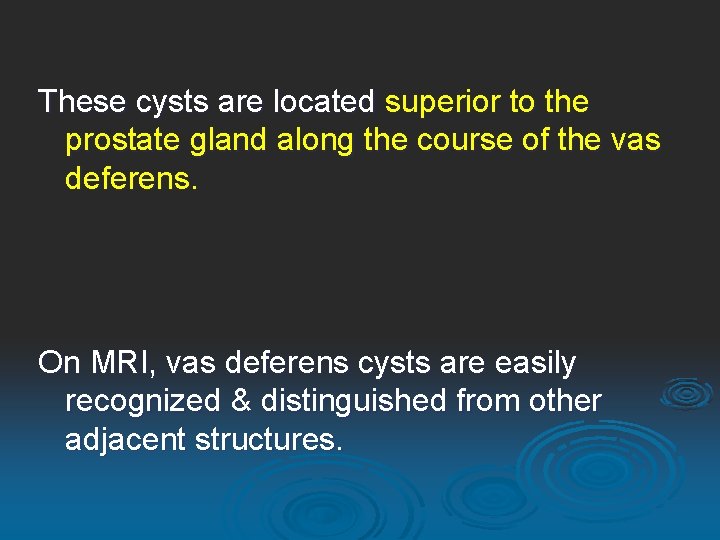
Causes of lower limb bowing • Developmental [physiological bowing] • Congenital Bowing • Tibia vara [Blount disease] • Neurofibromatosis • Osteogenesis Imperfecta • Rickets • Camptomelic Dysplasia • Achondroplasia

TIBIA VARA (Blount disease) A common condition, believed to be result from abnormal stress on the posteromedial proximal tibial physis, causing growth suppression. The growth at the epiphysis becomes asymmetric, leading to the typical varus angulation. Usually unilateral or asymmetric.
Predisposing factors Early walking and obesity - exaggerate the physiological varus angulation and African-American children – they are believed to have excessive ligamentous laxity and begin to walk earlier. Three types of the tibia vara [depending on the age at presentation] • Infantile - the most common • Juvenile • Adolescent The later onset types may represent an unrecognized and untreated variants of infantile form.
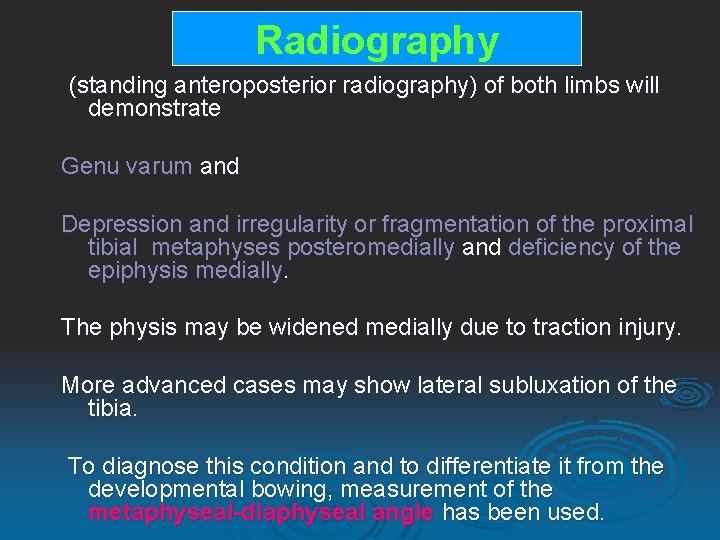
Radiography (standing anteroposterior radiography) of both limbs will demonstrate Genu varum and Depression and irregularity or fragmentation of the proximal tibial metaphyses posteromedially and deficiency of the epiphysis medially. The physis may be widened medially due to traction injury. More advanced cases may show lateral subluxation of the tibia. To diagnose this condition and to differentiate it from the developmental bowing, measurement of the metaphyseal-diaphyseal angle has been used.

The metaphyseal-diaphyseal angle is the angle between a line drawn parallel to the top of the proximal tibial metaphyses and the another line drawn perpendicular to the long axis of the tibial shaft. Physiological bowing - 50 + 2. 8 [ range 0 -11] Blount disease - 160 + 4. 3 [range 8 -22]. It has been suggested that the children with angle greater than 110 have Blount disease. Children with intermediate angles [ 80 – 110] may require the follow up radiography to clarify the diagnosis.
A line is drawn prepandicular to the longitudinal axis of the tibia & another is drawn through the two beaks of the metaphysis to determine the transverse axis of tibial metaphysis. The metaphyseal-diaphyseal angle is bisected by these two lines.
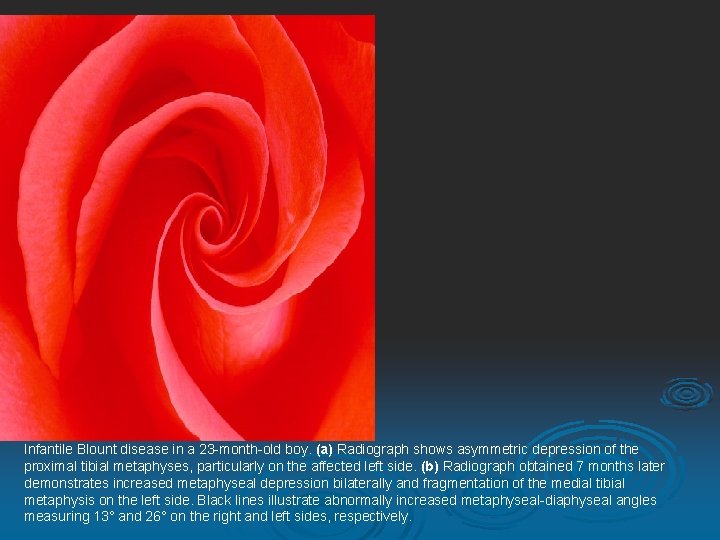
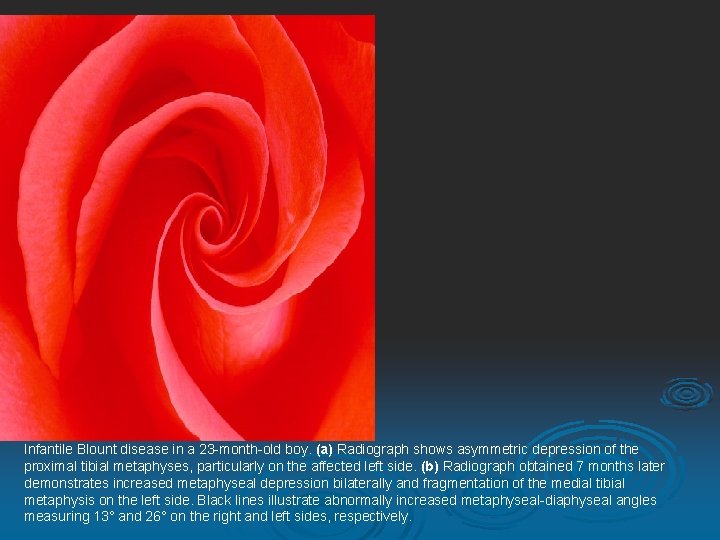
Infantile Blount disease in a 23 -month-old boy. (a) Radiograph shows asymmetric depression of the proximal tibial metaphyses, particularly on the affected left side. (b) Radiograph obtained 7 months later demonstrates increased metaphyseal depression bilaterally and fragmentation of the medial tibial metaphysis on the left side. Black lines illustrate abnormally increased metaphyseal-diaphyseal angles measuring 13° and 26° on the right and left sides, respectively.
![A six stage classification system for Blount disease proposed by langenskiold is A six stage classification system for Blount disease [ proposed by langenskiold ] is](https://slidetodoc.com/presentation_image/b9d5ca3fcb046a0a12f238c466fbf5b9/image-13.jpg)
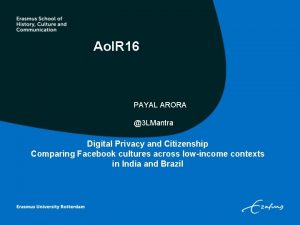
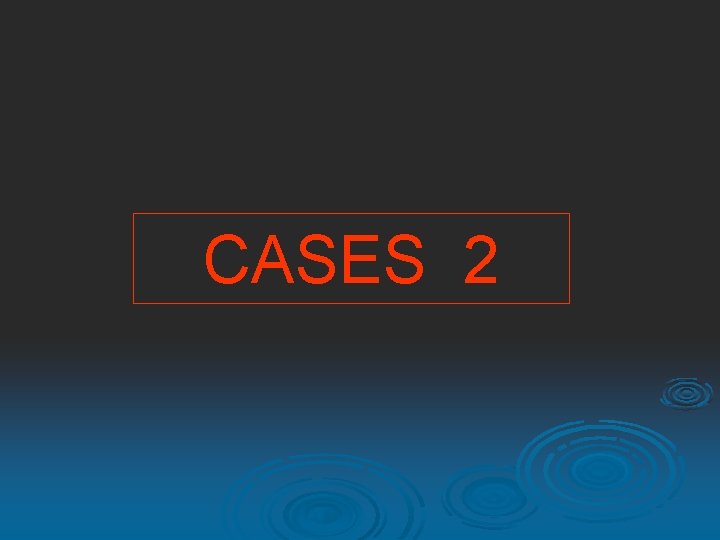
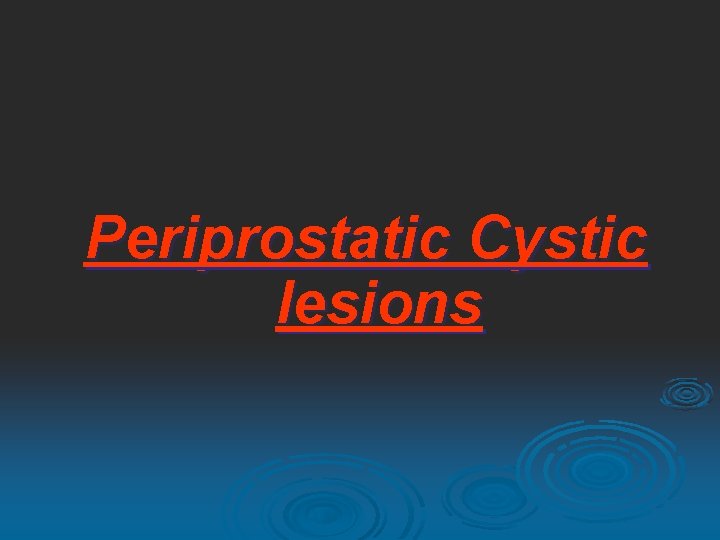
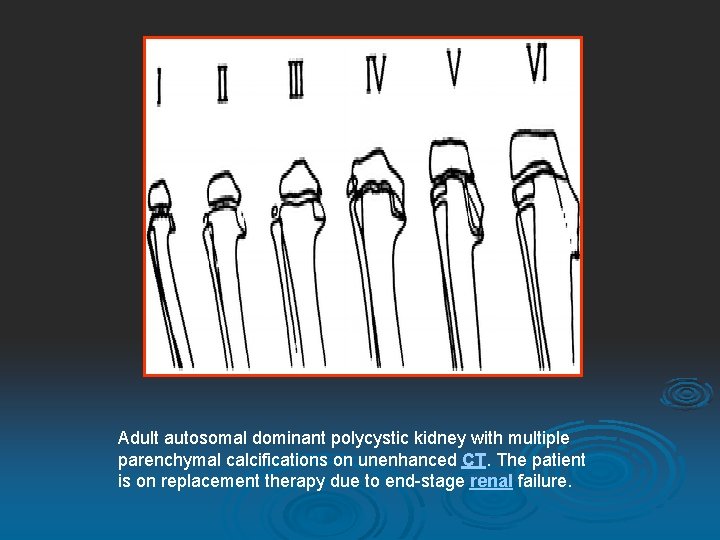
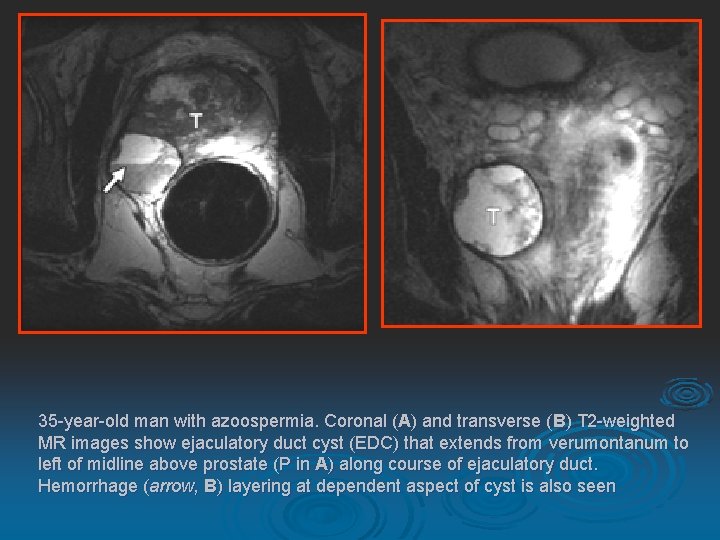
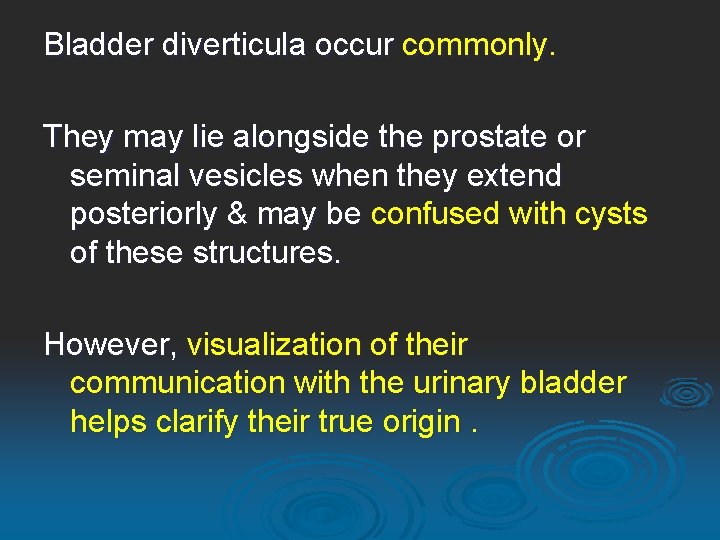
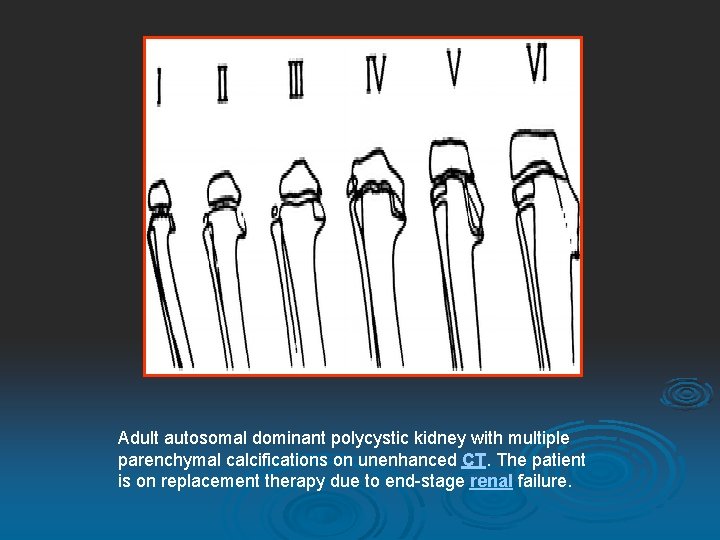
A six stage classification system for Blount disease [ proposed by langenskiold ] is commonly used. This classification is not intended to determine the prognosis or the treatment, however osteotomies of the tibia and fibula is usual treatment of choice in stage 3 disease or higher.

LANGENSKIOLD CLASSIFICATION Drawings illustrate the six stages of the Langenskiold classification system for Blount disease. Note the progressive depression, beaking, and fragmentation of the medial tibial metaphysis, also involving the epiphysis in the higher stages.
MR imaging has been performed to evaluate the growth plate in Blount disease and may be useful in the surgical planning. It may also be used to predict development of Blount disease in patient with severe physiological bowing.

Adolescent Blount disease in a 12 -year-old boy. (a) Radiograph shows metaphyseal changes in both the proximal tibia and the distal femur. Physeal widening is noted in the proximal tibia medially (arrow). (b) T 1 -weighted MR images show abnormal metaphyseal signal intensity in the distal femur and proximal tibia (arrowheads).
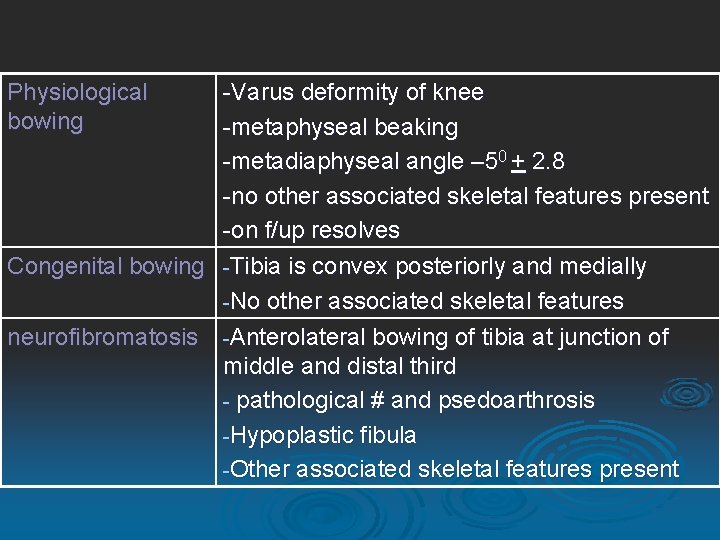
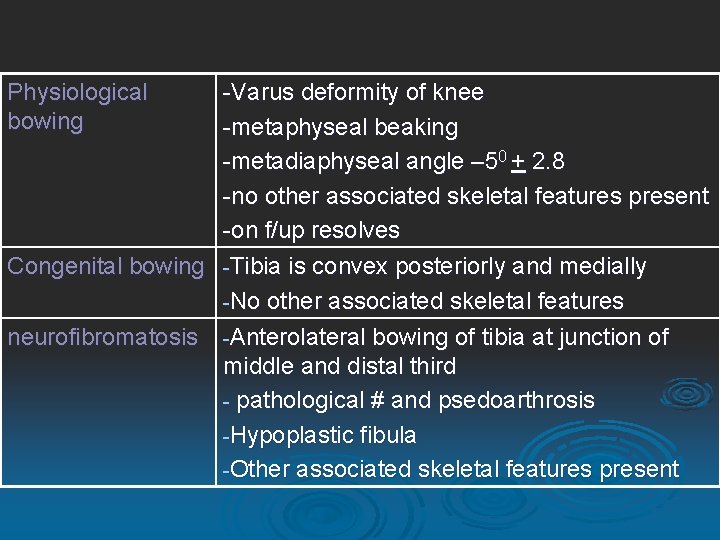
Physiological bowing -Varus deformity of knee -metaphyseal beaking -metadiaphyseal angle – 50 + 2. 8 -no other associated skeletal features present -on f/up resolves Congenital bowing -Tibia is convex posteriorly and medially -No other associated skeletal features neurofibromatosis -Anterolateral bowing of tibia at junction of middle and distal third - pathological # and psedoarthrosis -Hypoplastic fibula -Other associated skeletal features present

Osteogenesis imperfecta Rickets achodroplasia Camptomelic dysplasia -Multiple transverse # in lower limbs -Leg bones thin and fragile in tarda forms, short and thik in congenita form -Other associated skeletal features present -Metaphyseal cupping, fraying, splaying -Widening of growth plate -Pseudo# -Short and thick leg bones with metaphyseal flaring and cupping -Relative overgrowth of fibula -Other associated skeletal features present -Angular anterolateral bowing of both tibias and femurs -Other associated skeletal features present
CASES 2
7 Yrs old boy presentated with c/o dribbling.

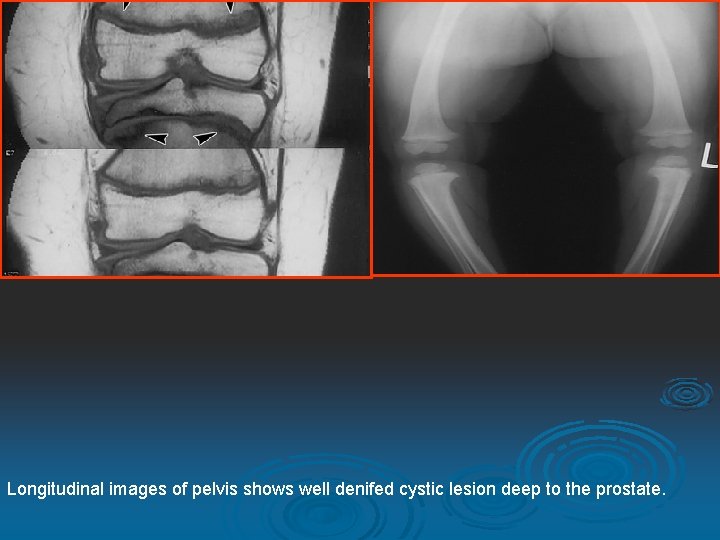
On cystgram film snows overdistended bladder with bladder wall irregularity, saculation & small diverticuli On mcug film shows acystic collection of contrast, post to prostratic urethra, communicating with prostatic urethra at verumonetum.
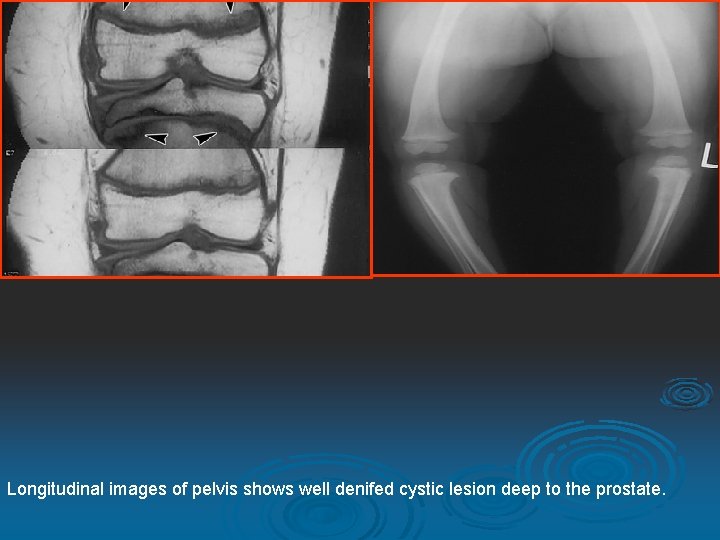
Longitudinal images of pelvis shows well denifed cystic lesion deep to the prostate.
DIAGNOSIS UTRICLE CYST
Now disscusing about cystic lesion around prostate.
Most Commonly Seen Prostatic and Periprostatic Cystic Lesions and Their Mimics

A. Intraprostatic Cystic Lesions 1. Müllerian duct cysts and prostatic utricle cysts 2. Ejaculatory duct cysts 3. Prostatic retention cysts 4. Cystic degeneration of benign prostatic hypertrophy 5. Cysts associated with tumors 6. Infectious, inflammatory, and parasitic cysts 7. Ejaculatory duct diverticulum
B. Periprostatic Cystic Lesions 1. Seminal vesicle cysts 2. Cysts of the vas deferens 3. Cowper's duct cysts
C. Entities That May Mimic Prostatic and Periprostatic Cystic Lesions 1. Defect from transurethral resection of the prostate 2. Hydroureter and ectopic insertion of the ureter 3. Bladder diverticulum 4. Prominent seminal vesicles
Intraprostatic Cystic Lesions
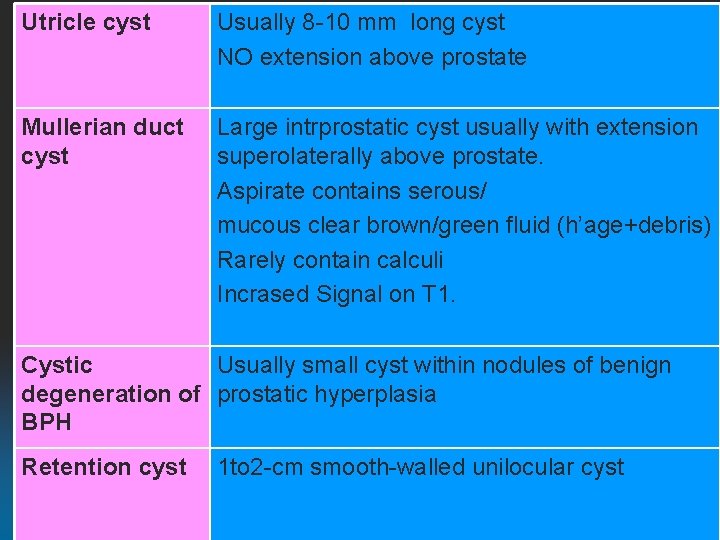
Müllerian Duct Cysts & Prostatic Utricle Cysts
Although these conditions are believed to be two different entities, it is difficult to differentiate them from one another on imaging and clinical studies. Both occur in the midline. When infected , may contain pus or hemorrhage, which can cause confusion on imaging because the appearances overlap those of abscess & cystic tumor of the prostate.
Both cause obstructive urinary symptoms, hematuria, and pelvic pain. Ejaculatory impairment by obstruction of the ejaculatory ducts. As utricle cysts communicate with urethra, it may result in postvoid dribbling. Prostatic utricle cysts are associated with some genitourinary abnormalities such as hypospadias, incomplete testicular descent, and unilateral renal agenesis
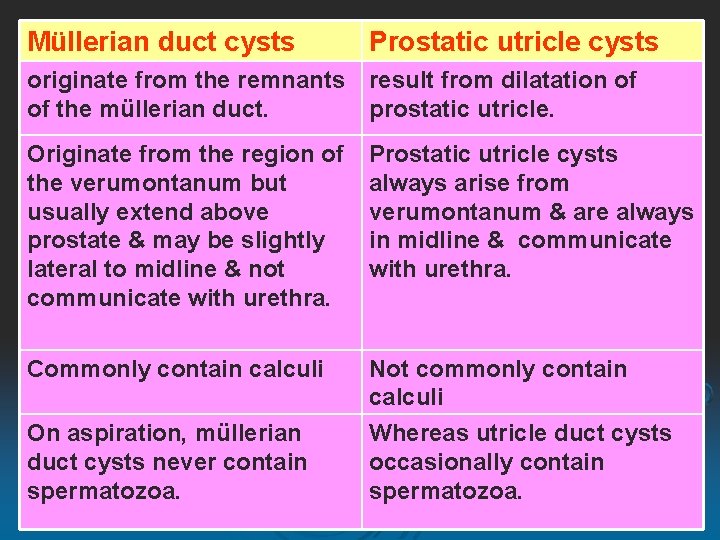
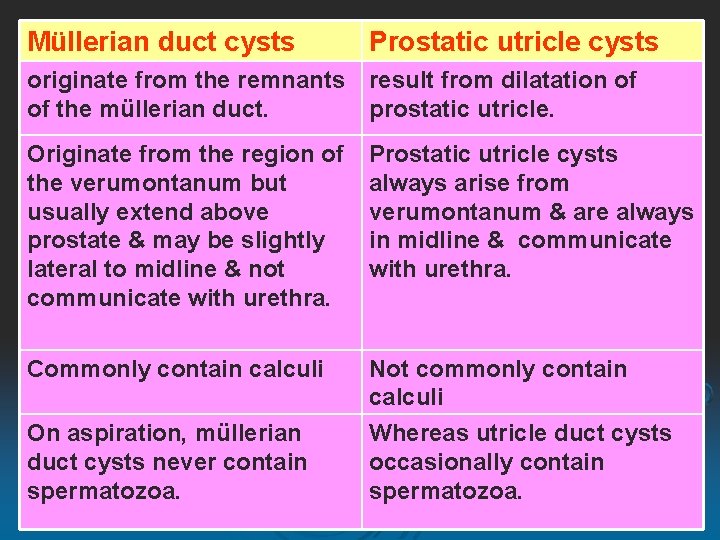
Müllerian duct cysts Prostatic utricle cysts originate from the remnants result from dilatation of of the müllerian duct. prostatic utricle. Originate from the region of the verumontanum but usually extend above prostate & may be slightly lateral to midline & not communicate with urethra. Prostatic utricle cysts always arise from verumontanum & are always in midline & communicate with urethra. Commonly contain calculi Not commonly contain calculi Whereas utricle duct cysts occasionally contain spermatozoa. On aspiration, müllerian duct cysts never contain spermatozoa.

51 -year-old man with prostate cancer. Transverse (A (A), coronal (B (B), and sagittal (C (C) T 2 -weighted MR images show prostatic utricle cyst (UC) that is located in midline, arising from verumontanum and communicating with urethra (U in C). Transverse image (A (A) shows focal lowsignal-intensity area representing tumor (T in A).
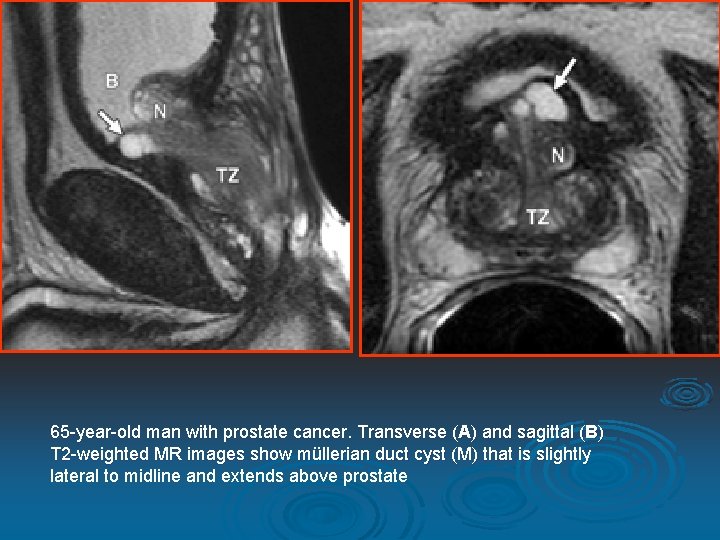
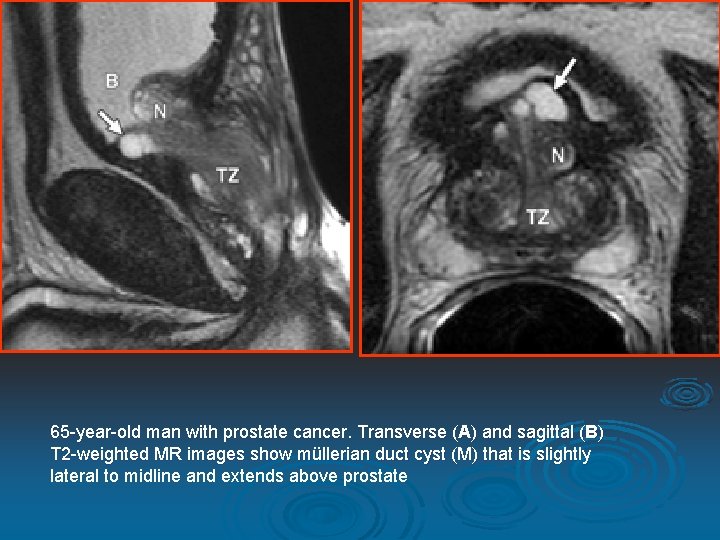
65 -year-old man with prostate cancer. Transverse (A) and sagittal (B) T 2 -weighted MR images show müllerian duct cyst (M) that is slightly lateral to midline and extends above prostate
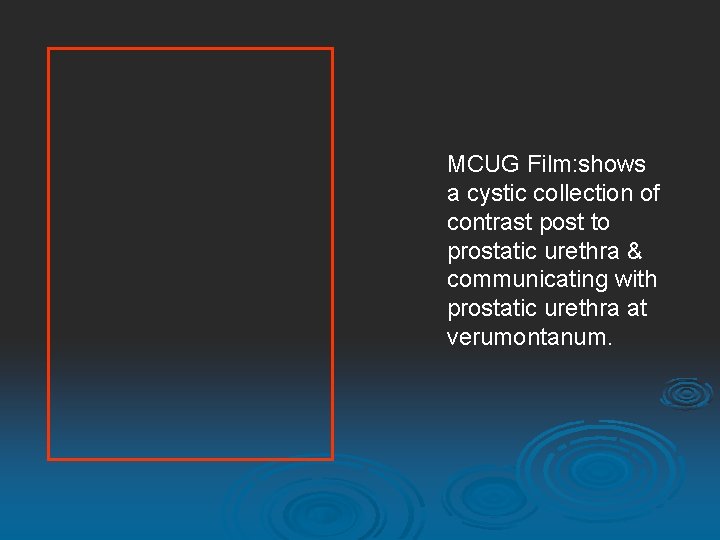
MCUG Film: shows a cystic collection of contrast post to prostatic urethra & communicating with prostatic urethra at verumontanum.

Images of the pelvis from the bladder ultrasound revealed a 3. 5 -cm midline fluid collection posterior to the bladder and superior to the prostate gland. The cystic fluid collection appears contiguous with the prostate. Echoes are noted within the cyst fluid.
Ejaculatory Duct Cysts

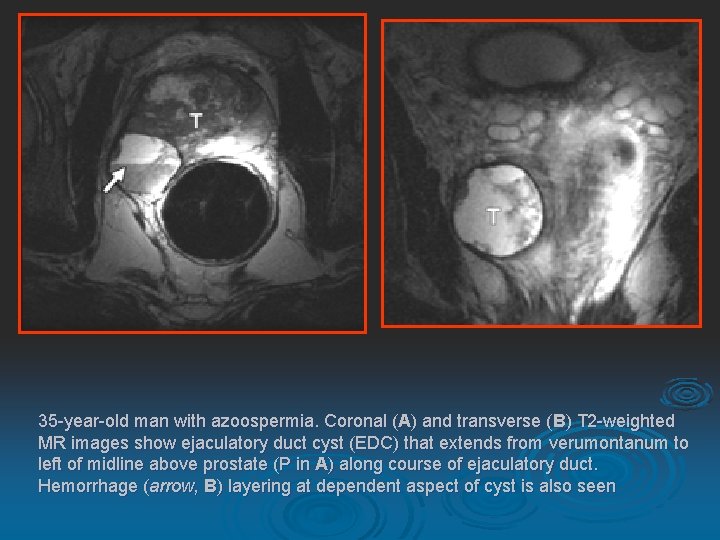
They are rare & Patients often present with hematospermia or dysuria. Occur due to obstruction of the ejaculatory duct , may be congenital or acquired. On imaging: lesions appear to be cystic structures along ejaculatory duct just lateral to midline in the central zone of the prostate. However, when large, may extend cephalad to the prostate & appear to arise centrally.
On aspiration : contain fructose or spermatozoa. Commonly contain calculi, but Sometimes may contain pus or hemorrhage. There may be associated cystic dilatation of the seminal vesicle on the same side.
35 -year-old man with azoospermia. Coronal (A) and transverse (B) T 2 -weighted MR images show ejaculatory duct cyst (EDC) that extends from verumontanum to left of midline above prostate (P in A) along course of ejaculatory duct. Hemorrhage (arrow, B) layering at dependent aspect of cyst is also seen
Prostatic Retention Cysts
They are acquired cysts. Rarely cause symptoms. Result from obstruction of the glandular ductules, causing dilatation of acini. Occur in any glandular zone of prostate. Never contain spermatozoa on aspiration. Appear as smooth-walled, unilocular simple cysts.
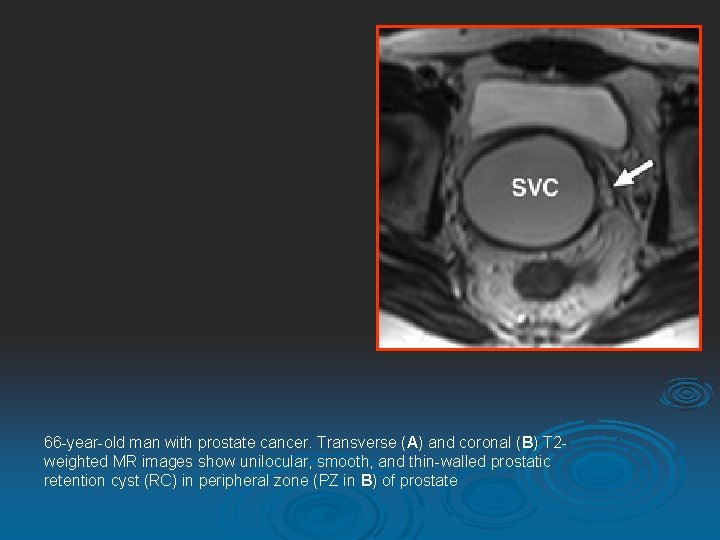
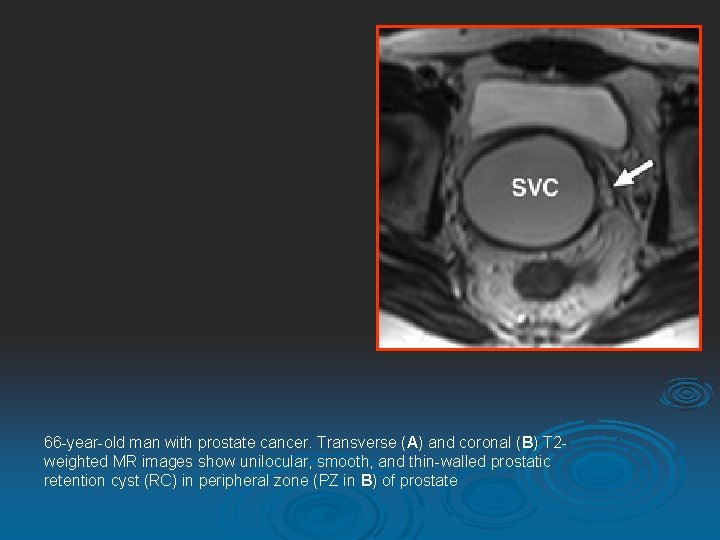
66 -year-old man with prostate cancer. Transverse (A) and coronal (B) T 2 weighted MR images show unilocular, smooth, and thin-walled prostatic retention cyst (RC) in peripheral zone (PZ in B) of prostate
Cystic Degeneration of Benign Prostatic Hypertrophy (BPH)

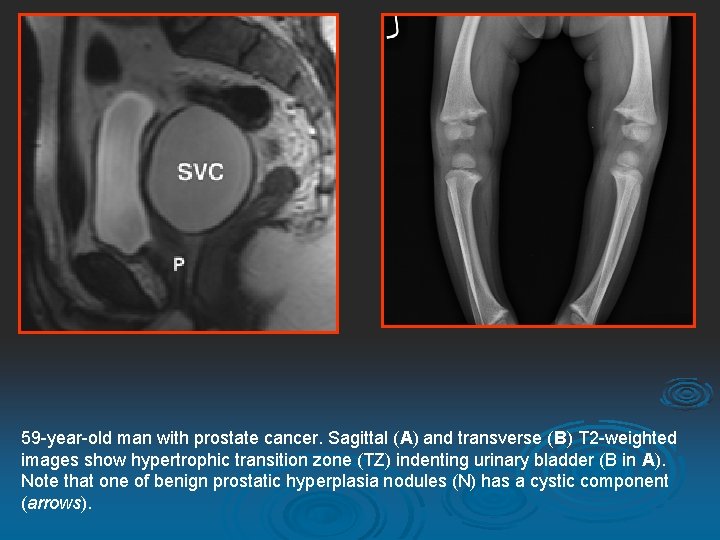
Cystic degeneration of BPH nodules is common & accounts for most prostatic cystic lesions. Patients with these cysts usually have urinary obstructive symptoms due to BPH. Cystic lesions resulting from cystic degeneration of BPH are located in the transition zone of the prostate along with BPH nodules. They seen as irregular shapes & various sizes & may contain hemorrhage or calculi.
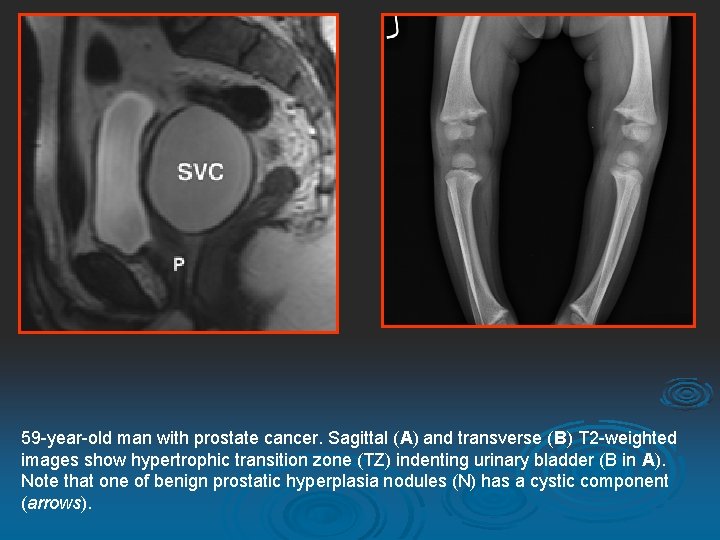
59 -year-old man with prostate cancer. Sagittal (A) and transverse (B) T 2 -weighted images show hypertrophic transition zone (TZ) indenting urinary bladder (B in A). Note that one of benign prostatic hyperplasia nodules (N) has a cystic component (arrows).
Cysts Associated with Tumors
Both benign and malignant prostate neoplasms may contain cystic components. Multilocular prostatic cystadenoma is a rare benign tumor that can grow to a large size. Prostatic adenocarcinoma may show cystic features from time to time. Other tumors of the prostate gland that exhibit cystic components include papillary cystadenocarcinoma and combined transitional cell/adenocarcinoma. Rarely, leiomyoma or liposarcoma in the prostate may have cystic elements. On MRI, the heterogeneity of signal intensity of the cystic components and the presence of soft-tissue elements in the lesion indicate a neoplastic cause.

68 -year-old man with mixed tumor of prostate containing high-grade ductal adenocarcinoma, with transitional cell and nonkeratinizing squamous cell differentiation. Transverse (A) and coronal (B) T 2 -weighted MR images show tumor (T) with cystic and solid components. Fluid-fluid level (arrow, A) is also seen at dependent portion of cystic component of tumor.
A prostatic abscess may form secondary to acute bacterial infection, most often with Escherichia coli. Older diabetic patients are at increased risk. Patients usually have typical clinical signs and symptoms including fever, chills, dysuria, urinary frequency and urgency, hematuria, and pain. Although MRI is usually not performed for this condition, suspicion of an abscess is raised when a cystic lesion with thickened walls, septations, or heterogeneous contents is seen in a patient with appropriate clinical findings.
Chronic prostatitis may lead to a condition called cavitary prostatitis, in which a combination of prolonged infections and fibrosis causes glandular ductal constriction and acinar dilatation. This results in a "Swiss cheese" appearance in the prostate, with multiple small cysts of various sizes scattered throughout the gland. Correlation with clinical history is useful in these cases.
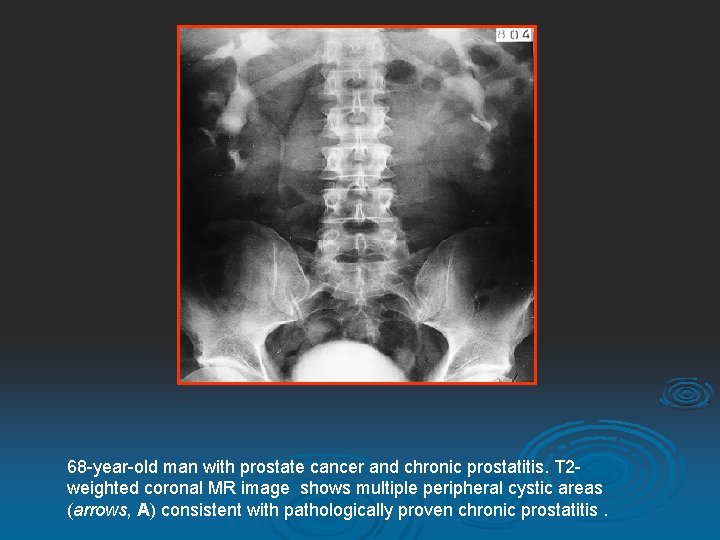
68 -year-old man with prostate cancer and chronic prostatitis. T 2 weighted coronal MR image shows multiple peripheral cystic areas (arrows, A) consistent with pathologically proven chronic prostatitis.
Periprostatic Cystic lesions
Seminal Vesicle Cysts

Cysts in the seminal vesicles are often discovered incidentally. However, if very large, they may be associated with voiding difficulties. Commonly associated with adult polycystic kidney disease. Aspiration of seminal vesicle cysts yields spermatozoa & sometimes hemorrhage.
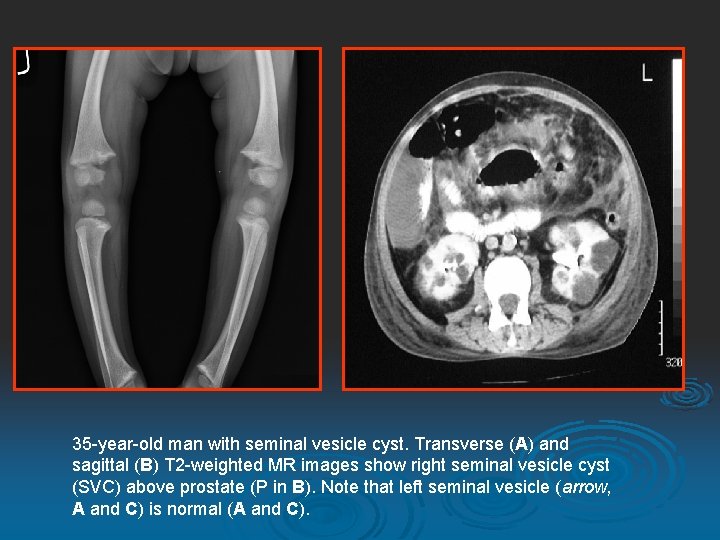
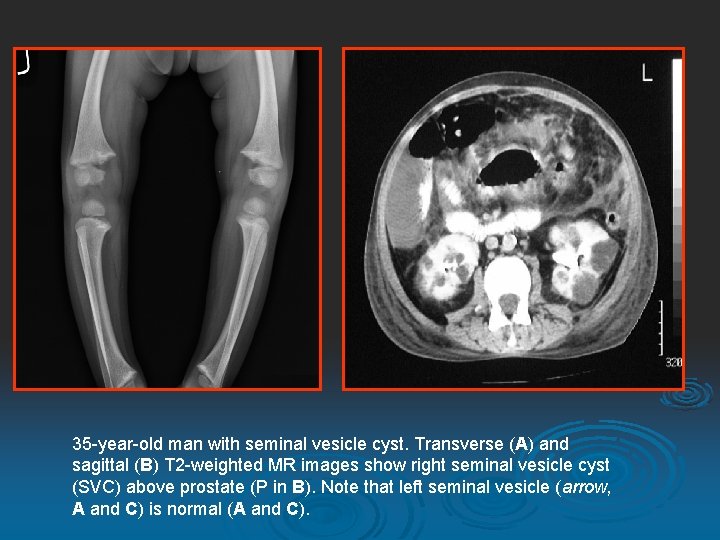
35 -year-old man with seminal vesicle cyst. Transverse (A) and sagittal (B) T 2 -weighted MR images show right seminal vesicle cyst (SVC) above prostate (P in B). Note that left seminal vesicle (arrow, A and C) is normal (A and C).
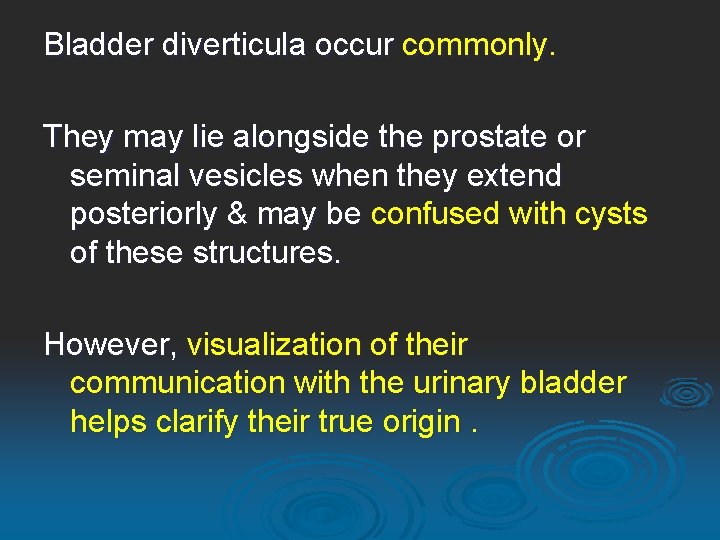
Cysts of the Vas Deferens
These cysts are located superior to the prostate gland along the course of the vas deferens. On MRI, vas deferens cysts are easily recognized & distinguished from other adjacent structures.

Bladder Diverticulum
Bladder diverticula occur commonly. They may lie alongside the prostate or seminal vesicles when they extend posteriorly & may be confused with cysts of these structures. However, visualization of their communication with the urinary bladder helps clarify their true origin.

61 -year-old man. Transverse T 2 -weighted MR image shows right posterolateral urinary bladder diverticulum (D) that extends above prostate. Note urine flow through neck of diverticulum (arrow).
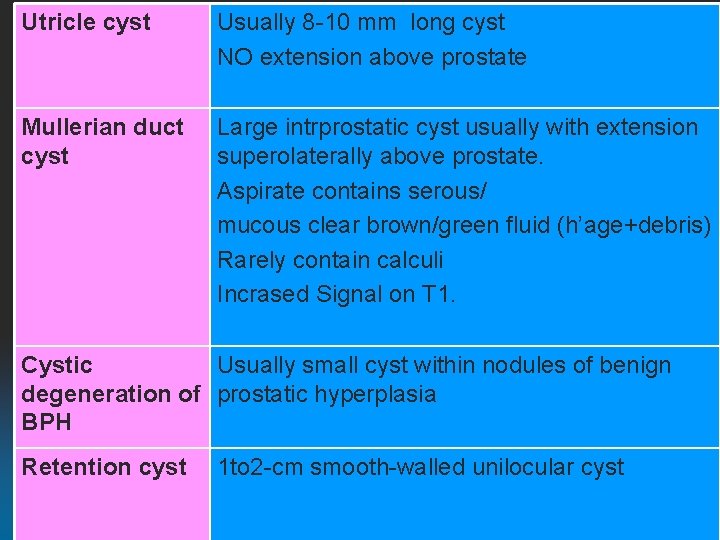
Utricle cyst Usually 8 -10 mm long cyst NO extension above prostate Mullerian duct cyst Large intrprostatic cyst usually with extension superolaterally above prostate. Aspirate contains serous/ mucous clear brown/green fluid (h’age+debris) Rarely contain calculi Incrased Signal on T 1. Cystic Usually small cyst within nodules of benign degeneration of prostatic hyperplasia BPH Retention cyst 1 to 2 -cm smooth-walled unilocular cyst
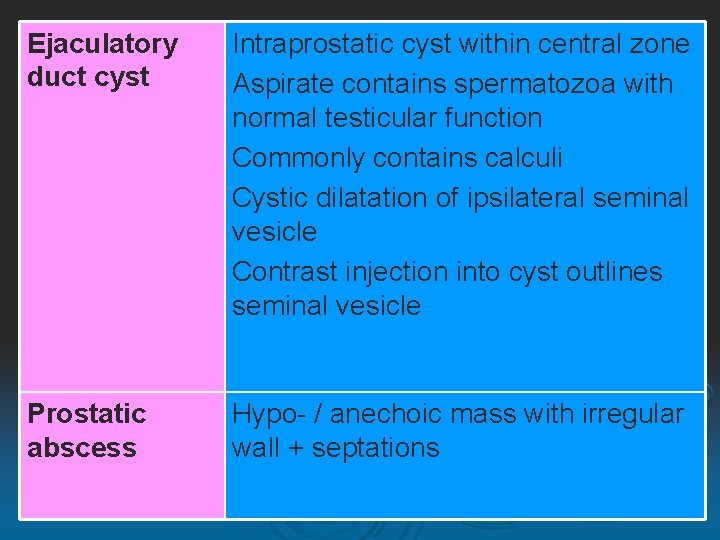
Ejaculatory duct cyst Intraprostatic cyst within central zone Aspirate contains spermatozoa with normal testicular function Commonly contains calculi Cystic dilatation of ipsilateral seminal vesicle Contrast injection into cyst outlines seminal vesicle Prostatic abscess Hypo- / anechoic mass with irregular wall + septations
CASES 3
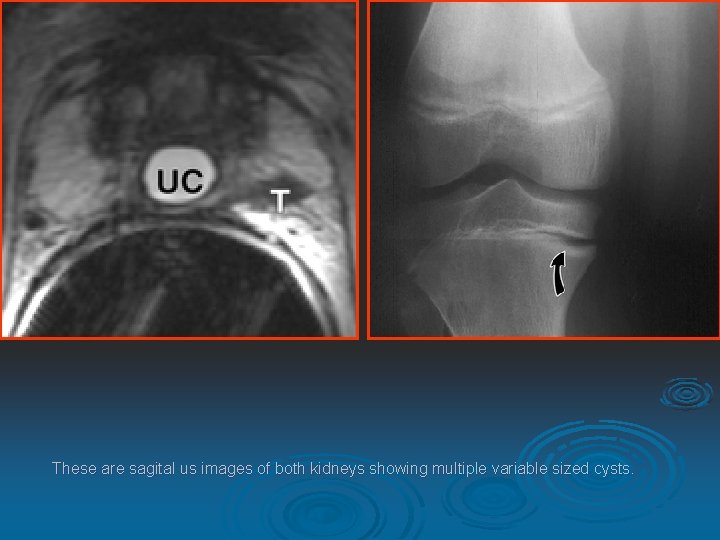
30 yr old male presentated with hematuria.
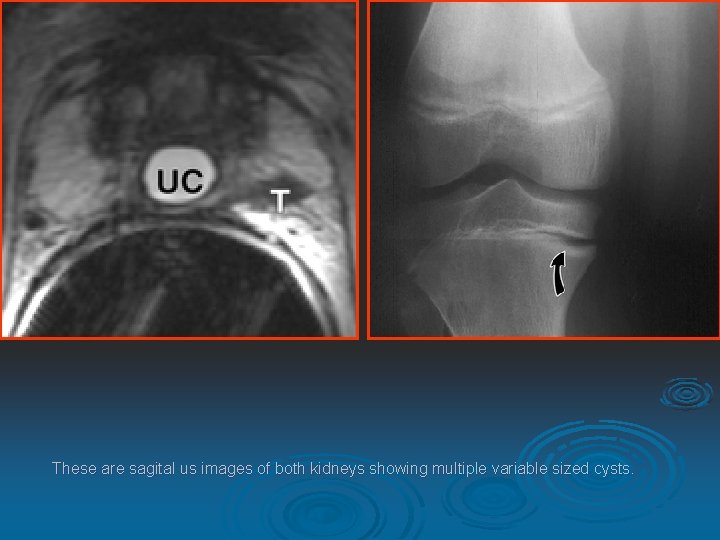
These are sagital us images of both kidneys showing multiple variable sized cysts.
DIAGNOSIS ADULT POLYCYSTIC KIDNEY DISEASE
It is an autosomal dominant condition, the cysts may occur anywhere along the nephron. 90% - positive family history. Diagnosed by imaging approx at age of 20 Y, still asymptomatic. Presenting symptoms can be pain, urinary tract infection, hematuria and hypertension at around 4 th or 5 th decade. The median age for end stage renal failure is in the late fifth decade.
Diagnostic criteria for ADPKD : At least 2 cysts in 1 kidney or 1 cyst in each kidney in an at-risk patient younger than 30 years. At least 2 cysts in each kidney in an at-risk patient aged 30 -59 years. At least 4 cysts in each kidney for an at-risk patient aged 60 years or older.
Intravenous urography demonstrates enlarged kidneys with smooth or irregular contours & multiple radiolucensies on nephrgram ("swisscheese"). The pyelocalyceal system is usually splayed and deformed by the multiple cysts. Ultrasonography demonstrating multiple cysts in a patient with positive family history is diagnostic. MRI demonstrate cysts containing hemorrhagic fluid with mixed signal intensity & fluid-level on both T 1 -W & T 2 -W sequences. CT Fine curvilinear calcifications - probably a residual of intracystic bleeding - can be diagnosed.

intravenous urography. Both kidneys are enlarged with irregular contours. The pyelocalyceal systems are splayed and deformed
Contrast-enhanced CT scan of the upper abdomen shows cysts in both kidneys. Note the free peritoneal fluid around the tip of the liver.
Adult autosomal dominant polycystic kidney with multiple parenchymal calcifications on unenhanced CT. The patient is on replacement therapy due to end-stage renal failure.
CASE 4
R X-ray both shoulder AP view shows high lined deformed both scapula with dexocardia.
DIAGNOSIS SPRENGEL SHOULDER

RADIOGRAPHIC FINDINGS Elevated Scapula Associated bony deformities Best views - AP of both shoulders with arms abducted and adducted maximally Lateral cervical and thoracic spine to look for other abnormalities Oblique and Lateral of scapula to show omovertebral bone (1/3 of cases
There is Congenital elevation of the scapula with rotation of its lower angle toward the spine. Scoliosis is frequently present, and torticollis may occasionally be associated. The abnormality may be unilateral or bilateral and occur in isolation or as a syndromic component. Abduction of shoulder beyond 90 degrees is impossible. It is due to failure of descent of the scapula during embryonic development from its position in the neck to its normal position in the posterior thorax. It happens usually in girls, and may have a genetic basis in some instances. Frequently associated with Klippel-Feil syndrome. A familial form of the Sprengel deformity is known as Corno's disease.

 Payal damor
Payal damor File-file yang dibuat oleh user pada jenis file di linux
File-file yang dibuat oleh user pada jenis file di linux Jasleen arora sex
Jasleen arora sex Women's sex
Women's sex Dr payal seth
Dr payal seth Dr payal dave
Dr payal dave Distributed file system definition
Distributed file system definition Markup tag tells the web browser
Markup tag tells the web browser Physical image vs logical image
Physical image vs logical image In a file-oriented information system, a transaction file
In a file-oriented information system, a transaction file Fungsi sistem file
Fungsi sistem file Micro teaching is a scaled down encounter
Micro teaching is a scaled down encounter Not executable: 32-bit elf file
Not executable: 32-bit elf file Ext file system
Ext file system Distributed file system
Distributed file system High performance distributed file system
High performance distributed file system Send bif files
Send bif files Arduino servo library github
Arduino servo library github Ship construction file
Ship construction file Indexed sequential organization
Indexed sequential organization Newforma app
Newforma app File system maintenance
File system maintenance How to save mesh file in ansys workbench
How to save mesh file in ansys workbench File system in operating system
File system in operating system Frangipani: a scalable distributed file system
Frangipani: a scalable distributed file system Electronic trial master file definition
Electronic trial master file definition Reframing organizations (doc or html) file
Reframing organizations (doc or html) file Sam file
Sam file Steganographic file system
Steganographic file system Hadoop distributed file system
Hadoop distributed file system Product structure file
Product structure file Geography: realms, regions, and concepts (doc or html) file
Geography: realms, regions, and concepts (doc or html) file Disk file system adalah
Disk file system adalah General alphabetic section of the numeric file
General alphabetic section of the numeric file Ntuser.dat forensics
Ntuser.dat forensics Fat file system
Fat file system Modification of alloc algorithm for allocating disk block
Modification of alloc algorithm for allocating disk block Google file system paper
Google file system paper Googledisk
Googledisk First to invent or first to file
First to invent or first to file Nur alia file upload
Nur alia file upload E file transfer
E file transfer Mechanic's lien utah
Mechanic's lien utah Download file powerpoint tentang amdal
Download file powerpoint tentang amdal Xap file
Xap file Xml file reader
Xml file reader Petr palas
Petr palas Batch file sftp
Batch file sftp File system esempi
File system esempi Enter.php?chapter=
Enter.php?chapter= What is coda file system
What is coda file system Cst file
Cst file Unix file name
Unix file name Php read file txt
Php read file txt Wwka file
Wwka file Fat file paradox
Fat file paradox Git file lifecycle
Git file lifecycle What is file concept
What is file concept Smart card file system
Smart card file system Ifstream input
Ifstream input File based processing
File based processing Xml file structure
Xml file structure File infector virus example
File infector virus example Bee 6 legs
Bee 6 legs Sam file
Sam file Balance sheet
Balance sheet Aqa a level drama
Aqa a level drama Lustre architecture
Lustre architecture Fts file transfer
Fts file transfer Google search tips pdf
Google search tips pdf Sound file size formula
Sound file size formula Ifd data
Ifd data Afs andrew file system
Afs andrew file system V-file-input
V-file-input Andrew file system
Andrew file system Employee file index
Employee file index Electronic file management
Electronic file management File formats in multimedia
File formats in multimedia File
File Thomas file md
Thomas file md Malloc_stats
Malloc_stats