IRON DEFICIENCY ANEMIA Rakhi Naik MD MHS Assistant
- Slides: 42
IRON DEFICIENCY ANEMIA Rakhi Naik, MD, MHS Assistant Professor of Medicine & Oncology, Division of Hematology
Disclosures None
Objectives • Understand the basic physiology of iron absorption, transport and storage • Understand the causes of iron deficiency and the compensatory responses seen in clinical lab tests • Understand modalities of treatment of iron deficiency and anemia
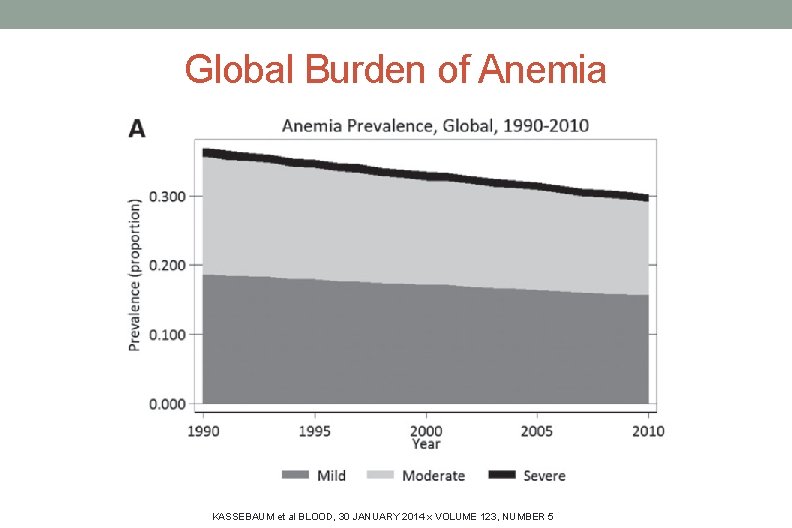
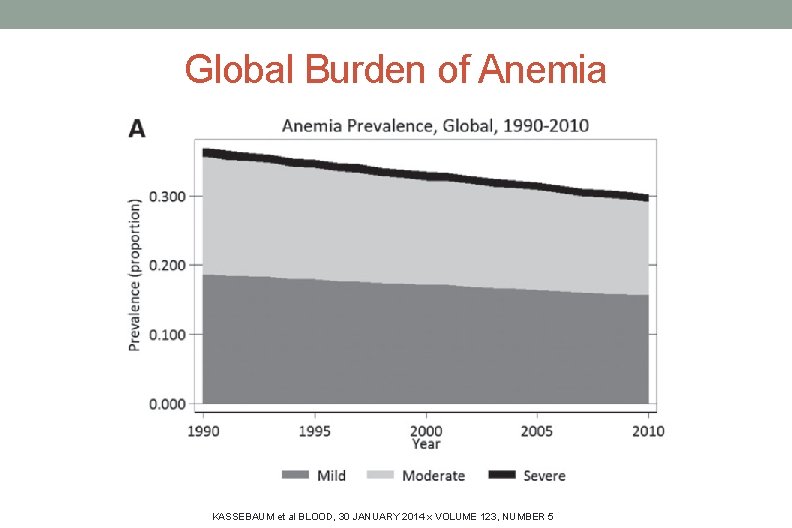
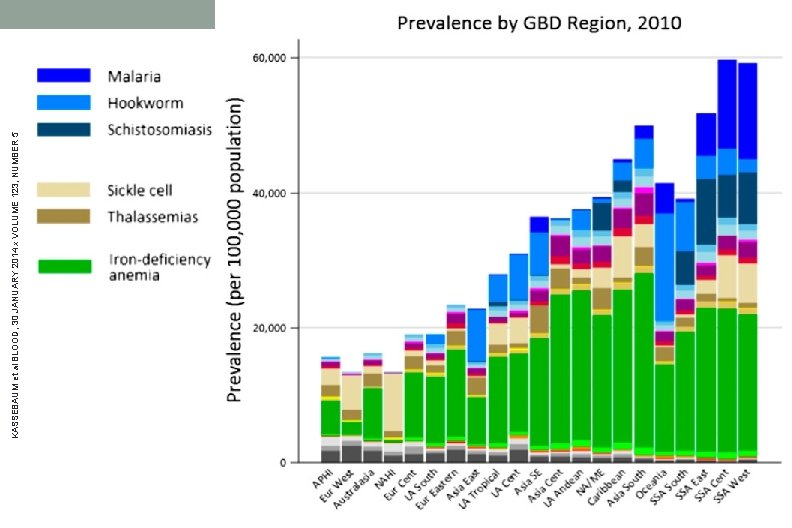
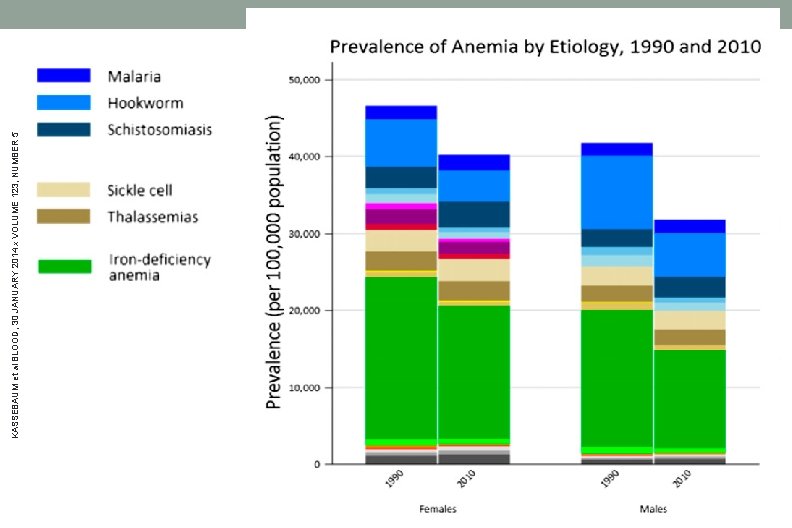
Global Burden of Anemia KASSEBAUM et al BLOOD, 30 JANUARY 2014 x VOLUME 123, NUMBER 5
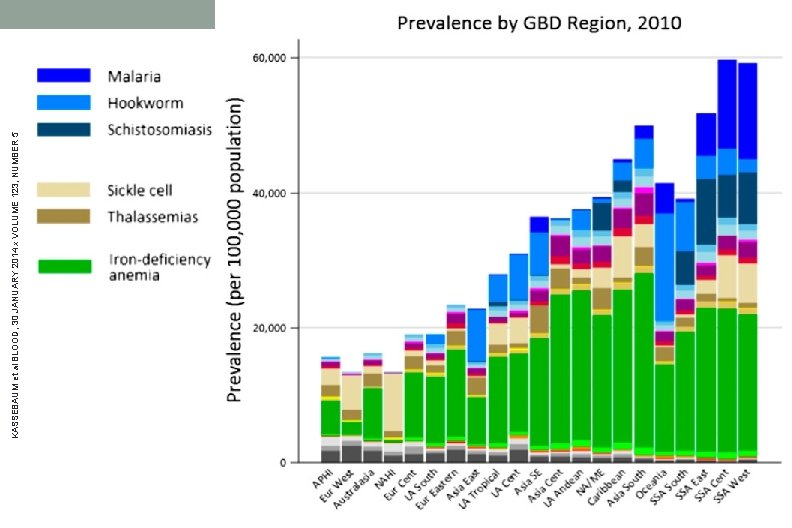
KASSEBAUM et al BLOOD, 30 JANUARY 2014 x VOLUME 123, NUMBER 5
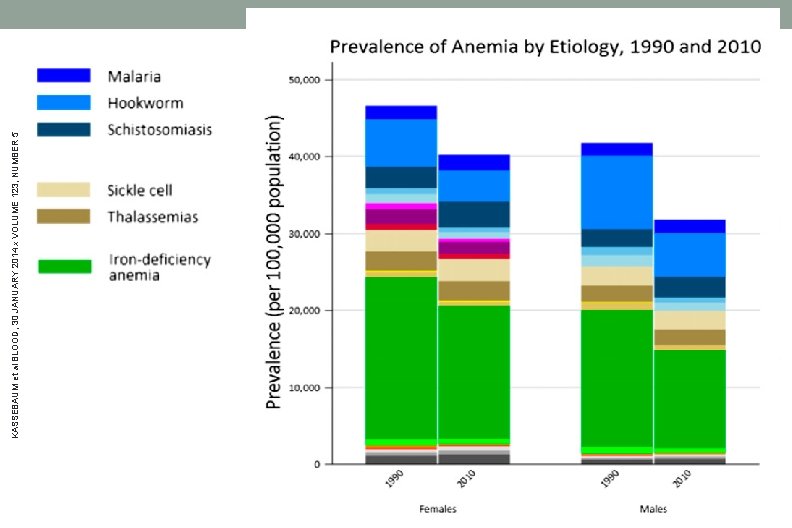
KASSEBAUM et al BLOOD, 30 JANUARY 2014 x VOLUME 123, NUMBER 5
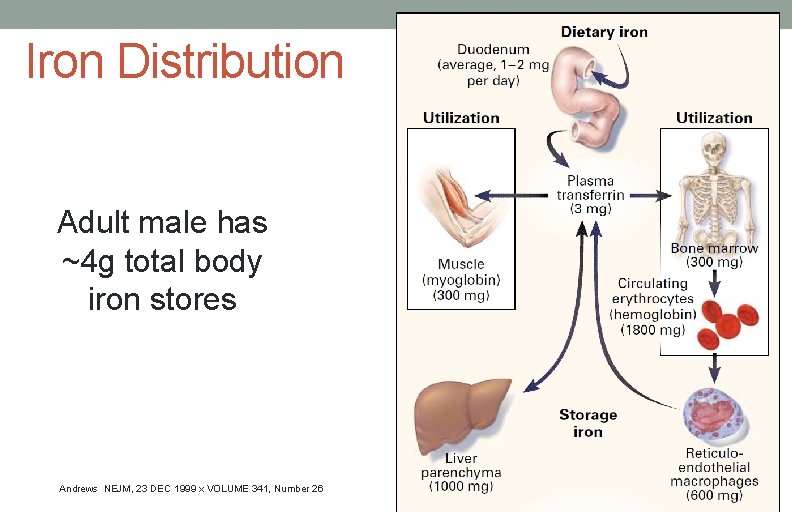
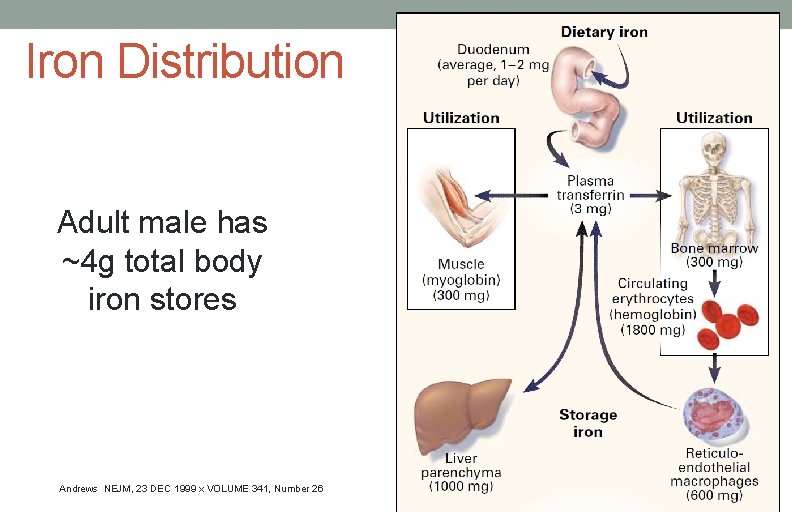
Iron Distribution Adult male has ~4 g total body iron stores Andrews NEJM, 23 DEC 1999 x VOLUME 341, Number 26
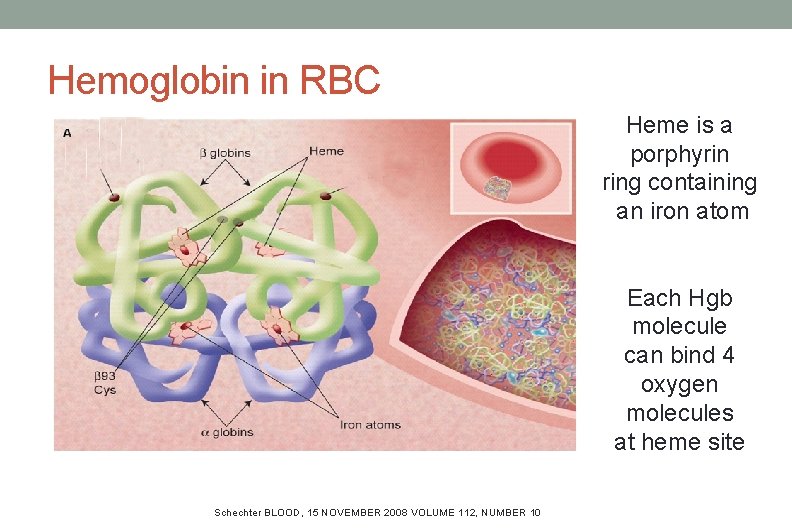
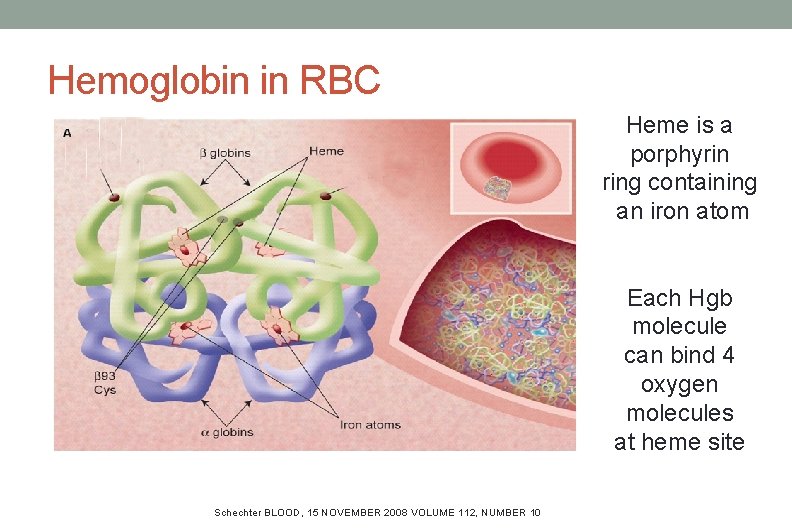
Hemoglobin in RBC Heme is a porphyrin ring containing an iron atom Each Hgb molecule can bind 4 oxygen molecules at heme site Schechter BLOOD, 15 NOVEMBER 2008 112, NUMBER Schechter BLOOD, 15 VOLUME NOVEMBER 2008 VOLUME 10 112, NUMBER 10
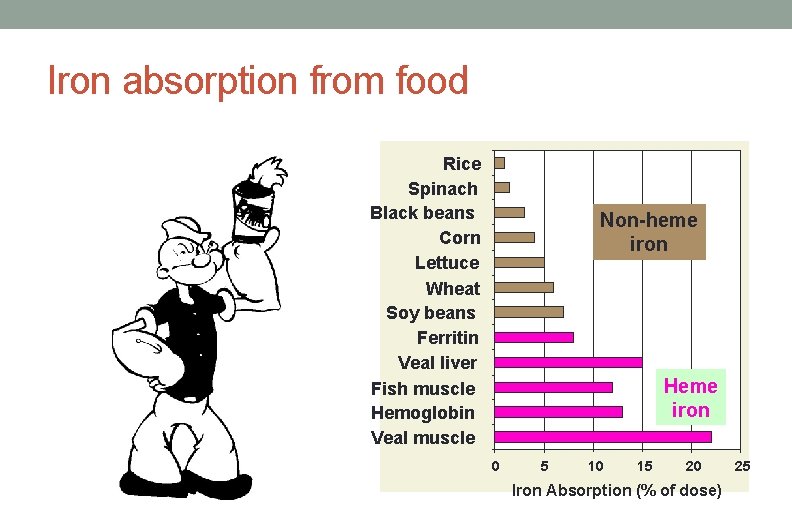
Iron Absorption • Food sources supply: 10 - 25 mg / day • Absorbed in the brush border of the upper small intestine • Enhanced by gastric acid • Inhibited by tannins, systemic inflammation • Most dietary iron is nonheme form, <5% bioavailability • < 10% dietary iron is heme form, >25% bioavailability
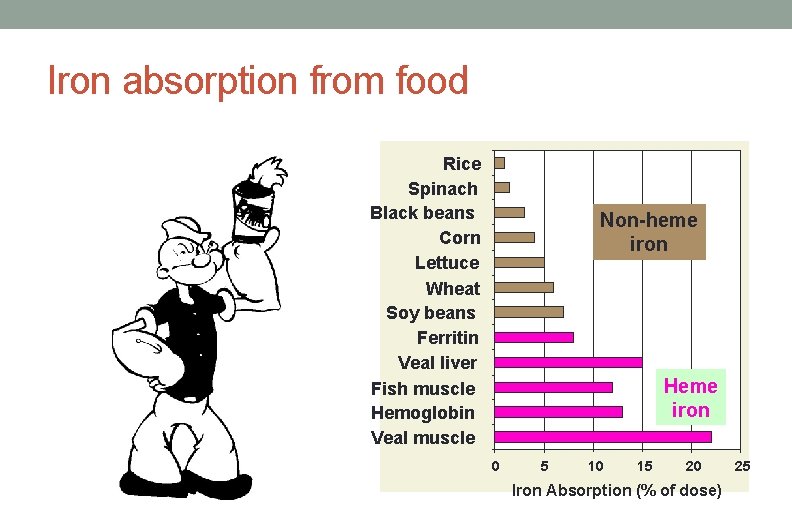
Iron absorption from food Rice Spinach Black beans Corn Lettuce Wheat Soy beans Ferritin Veal liver Fish muscle Hemoglobin Veal muscle Non-heme iron Heme iron 0 5 10 15 20 Iron Absorption (% of dose) 25
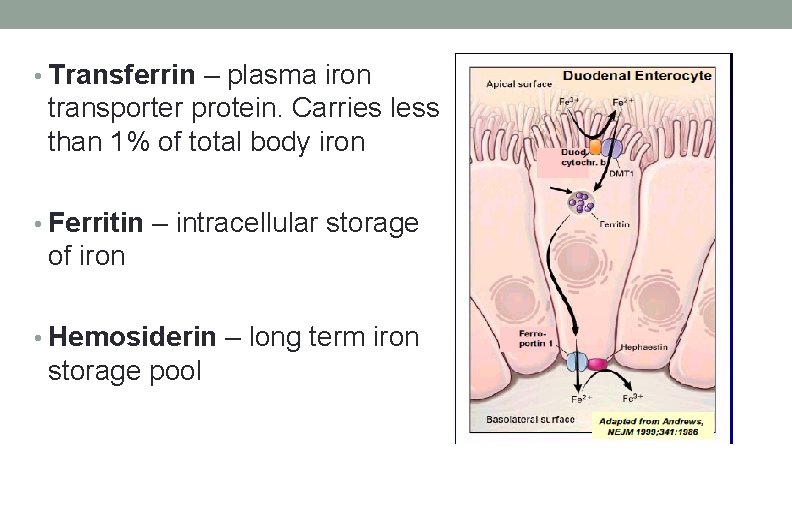
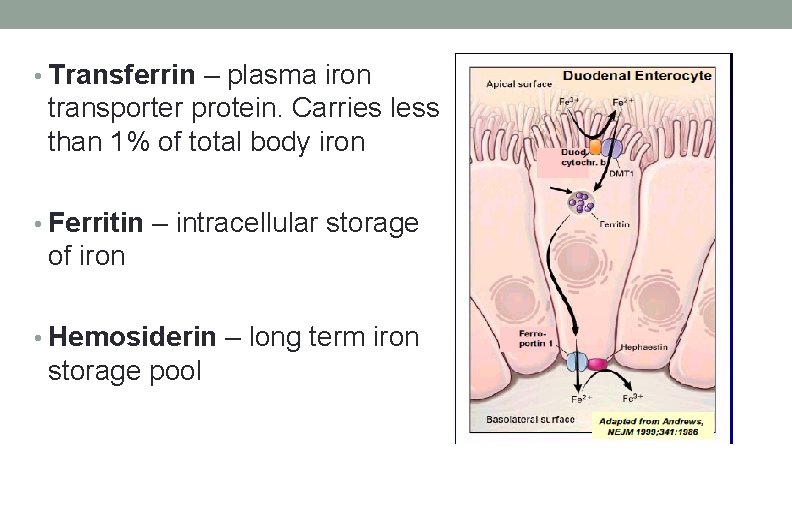
• Transferrin – plasma iron transporter protein. Carries less than 1% of total body iron • Ferritin – intracellular storage of iron • Hemosiderin – long term iron storage pool
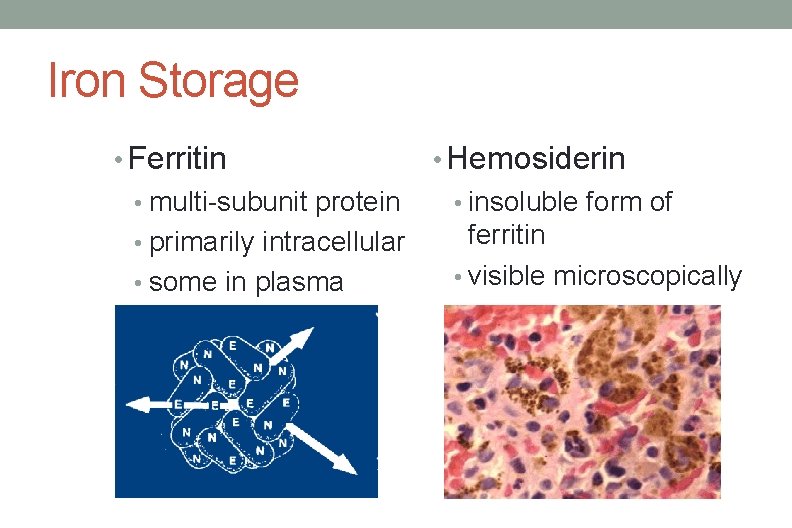
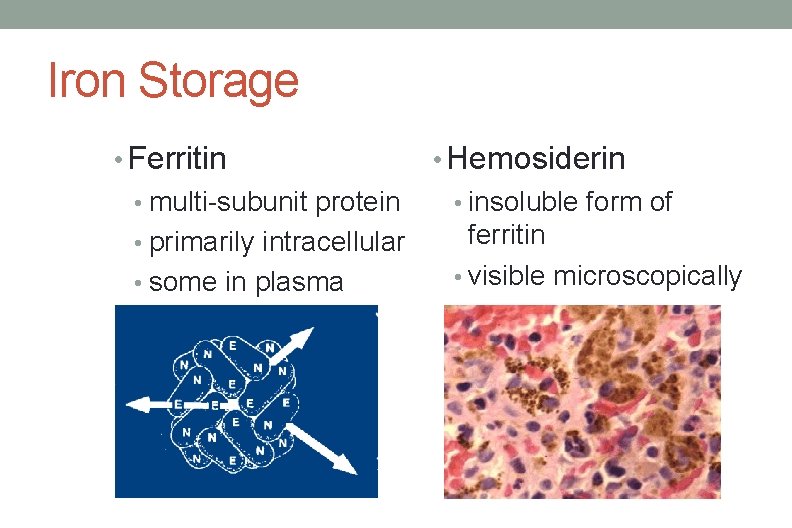
Iron Storage • Ferritin • Hemosiderin • multi-subunit protein • insoluble form of ferritin • primarily intracellular • visible microscopically • some in plasma
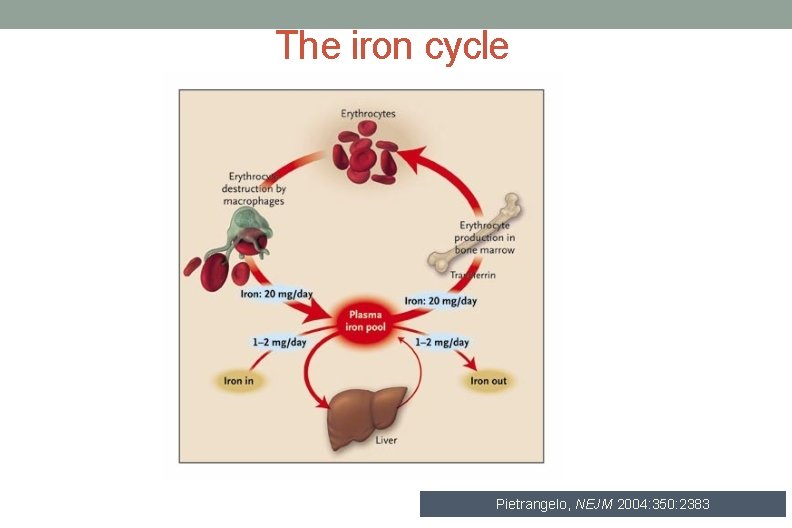
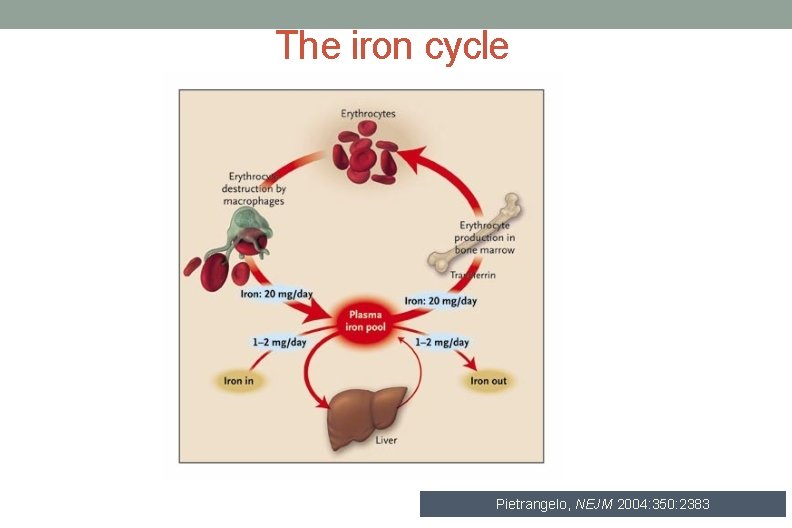
The iron cycle Pietrangelo, NEJM 2004: 350: 2383
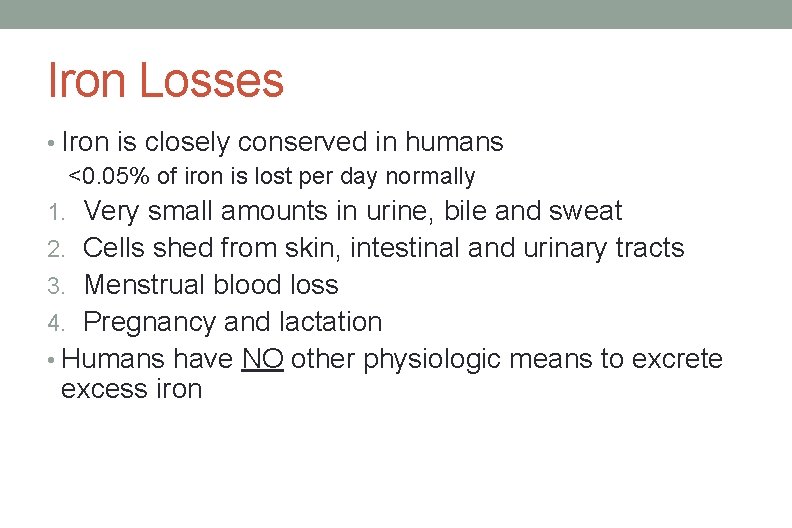
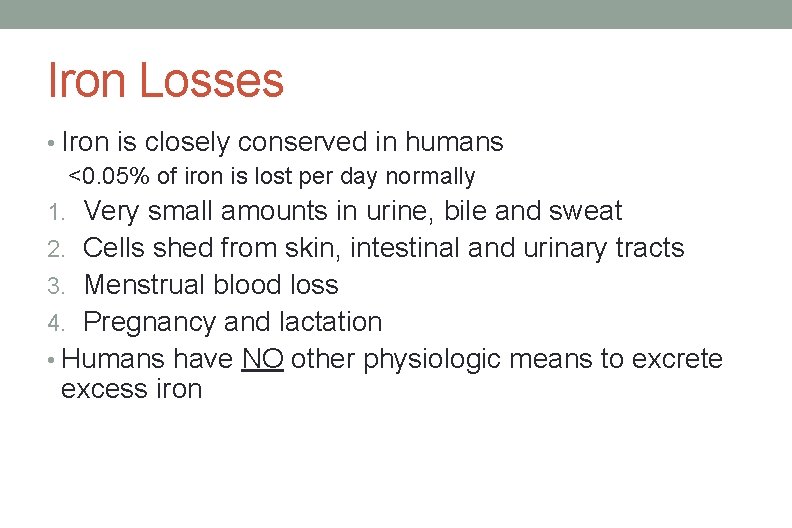
Iron Losses • Iron is closely conserved in humans <0. 05% of iron is lost per day normally 1. Very small amounts in urine, bile and sweat 2. Cells shed from skin, intestinal and urinary tracts 3. Menstrual blood loss 4. Pregnancy and lactation • Humans have NO other physiologic means to excrete excess iron
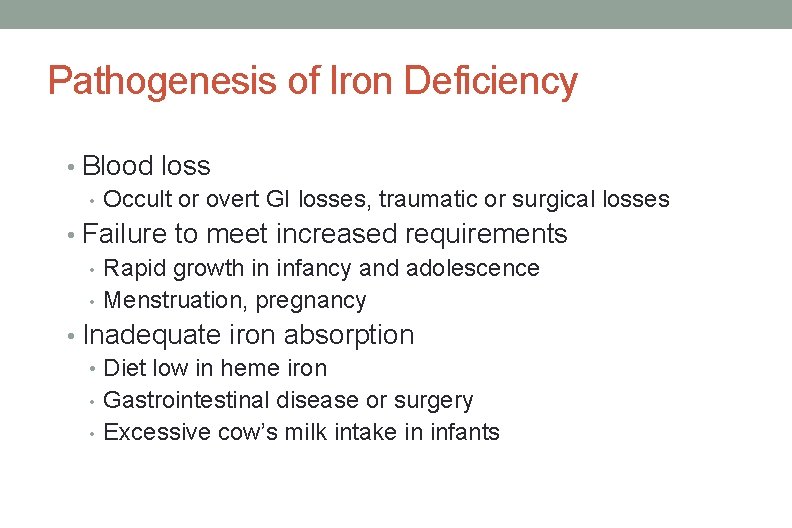
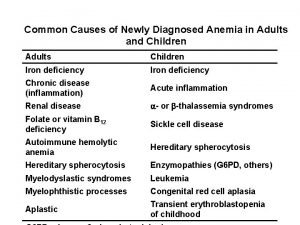
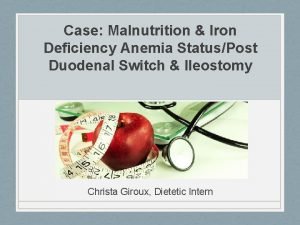
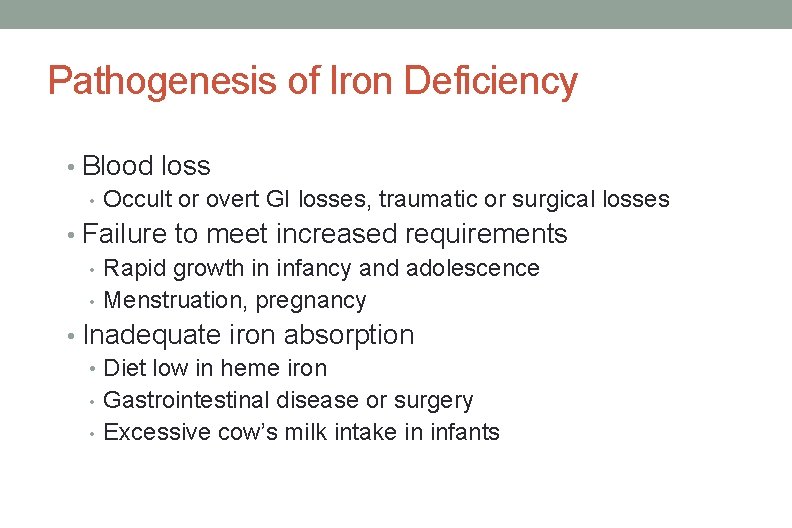
Pathogenesis of Iron Deficiency • Blood loss • Occult or overt GI losses, traumatic or surgical losses • Failure to meet increased requirements • Rapid growth in infancy and adolescence • Menstruation, pregnancy • Inadequate iron absorption • Diet low in heme iron • Gastrointestinal disease or surgery • Excessive cow’s milk intake in infants
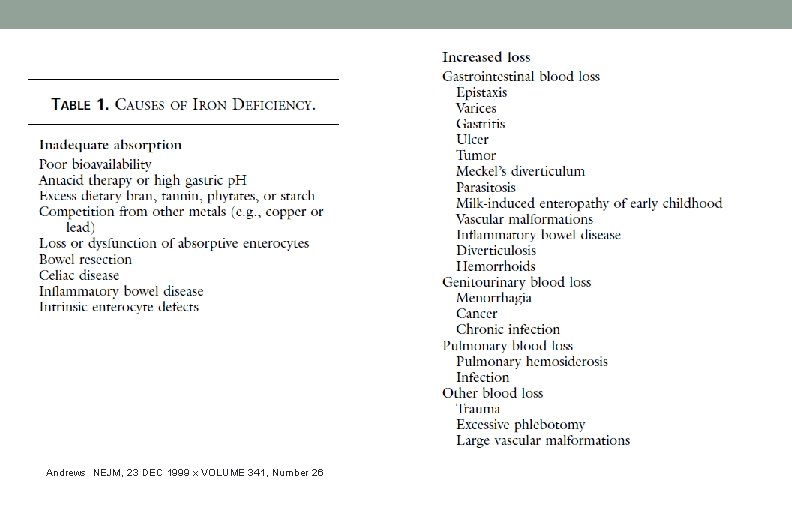
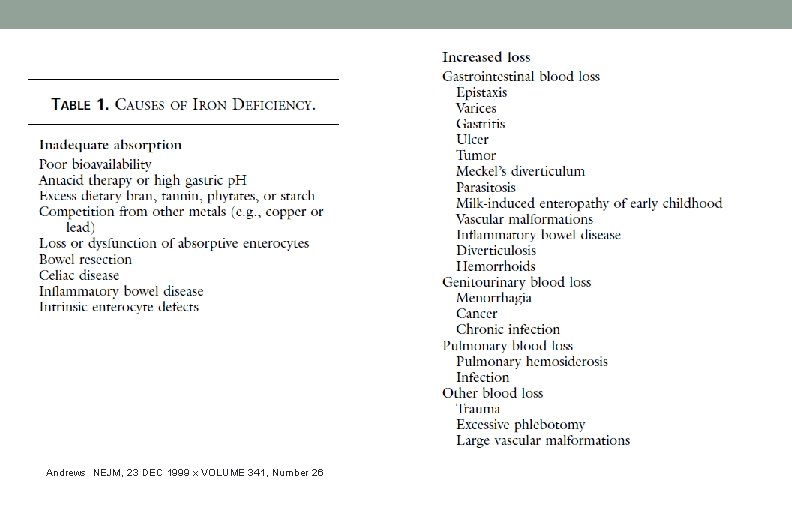
Andrews NEJM, 23 DEC 1999 x VOLUME 341, Number 26
Features of Iron Deficiency Anemia • Depends on the degree and the rate of development of anemia • Symptoms common to all anemias: • pallor, fatigability, weakness, dizziness, irritability
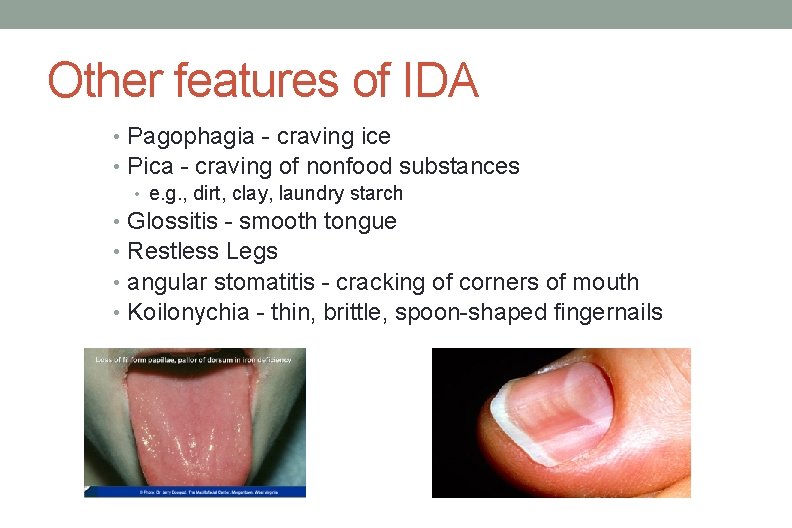
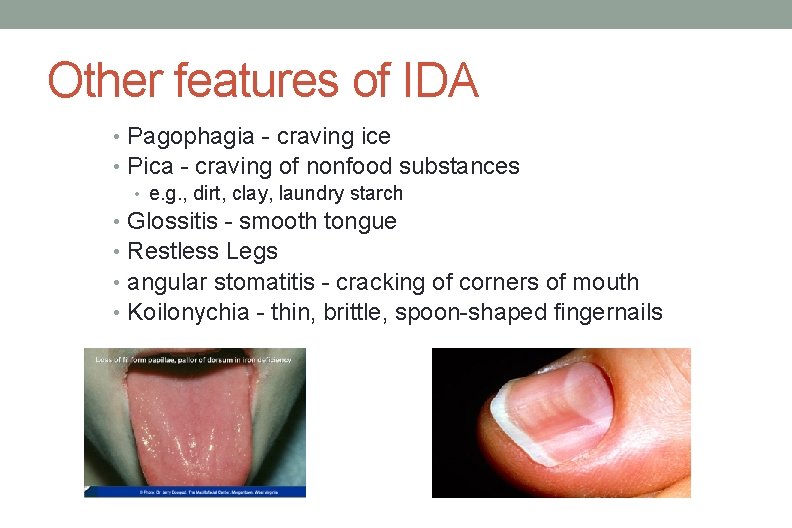
Other features of IDA • Pagophagia - craving ice • Pica - craving of nonfood substances • e. g. , dirt, clay, laundry starch • Glossitis - smooth tongue • Restless Legs • angular stomatitis - cracking of corners of mouth • Koilonychia - thin, brittle, spoon-shaped fingernails
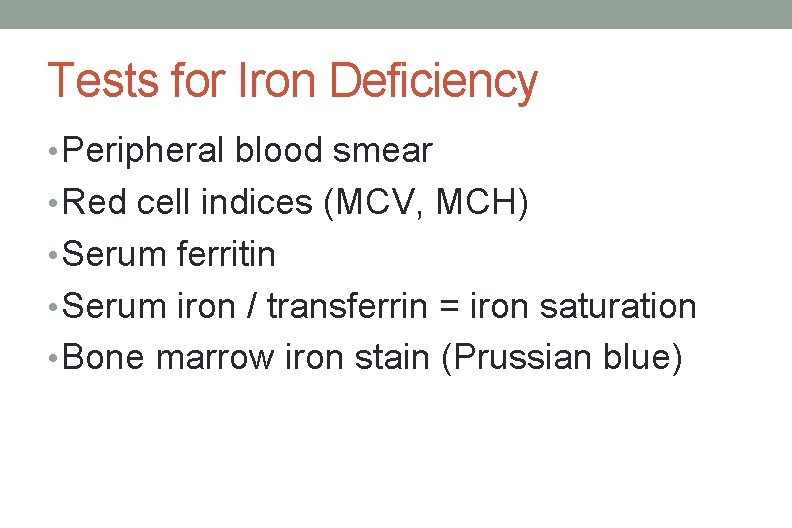
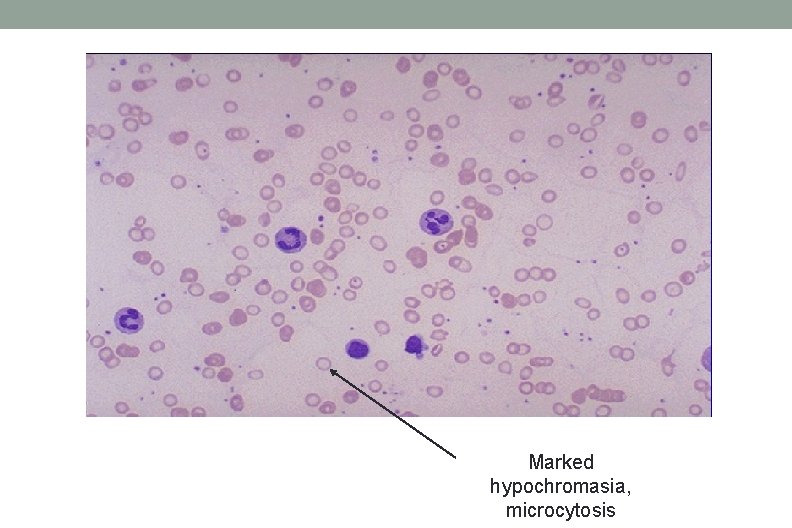
Tests for Iron Deficiency • Peripheral blood smear • Red cell indices (MCV, MCH) • Serum ferritin • Serum iron / transferrin = iron saturation • Bone marrow iron stain (Prussian blue)
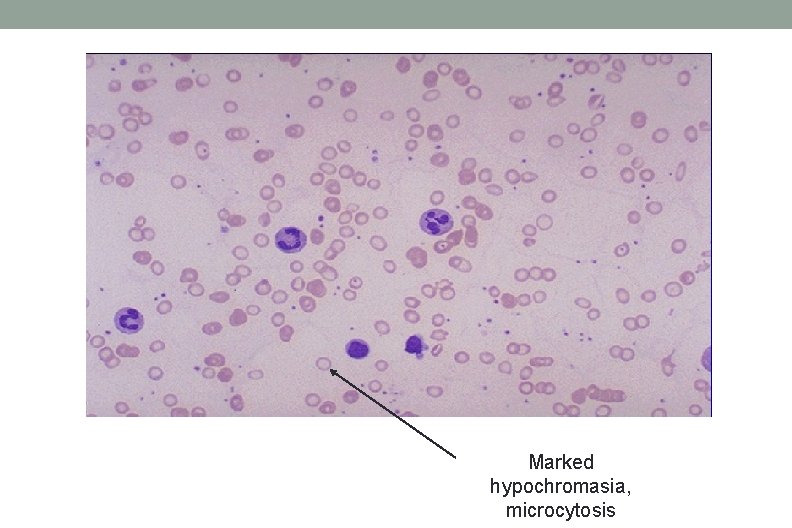
Marked hypochromasia, microcytosis
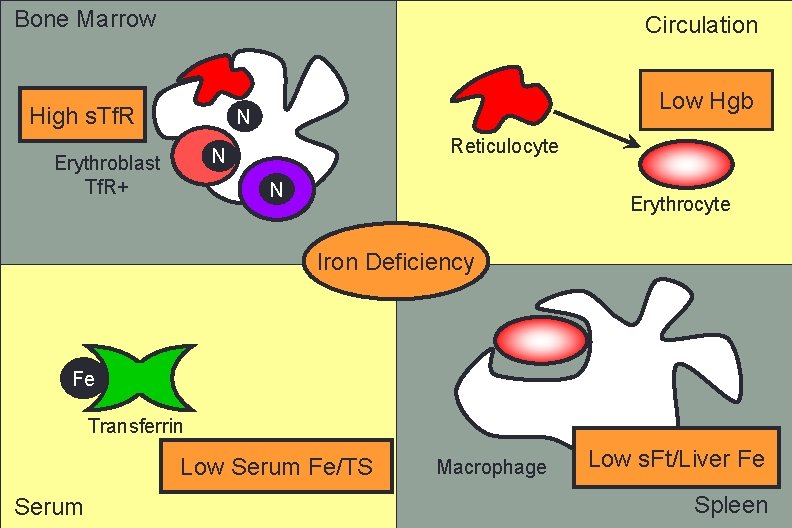
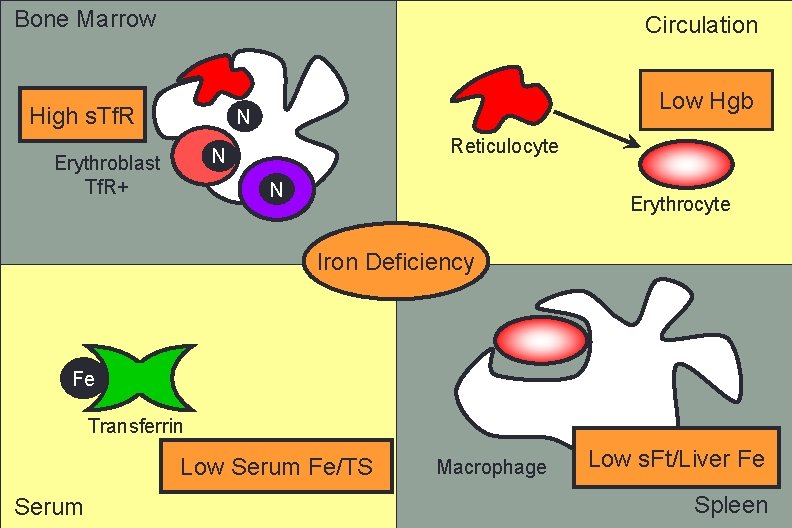
Bone Marrow Circulation High s. Tf. R Low Hgb N Reticulocyte N Erythroblast Tf. R+ N Erythrocyte Iron Deficiency Fe Transferrin Low Serum Fe/TS Serum Macrophage Low s. Ft/Liver Fe Spleen
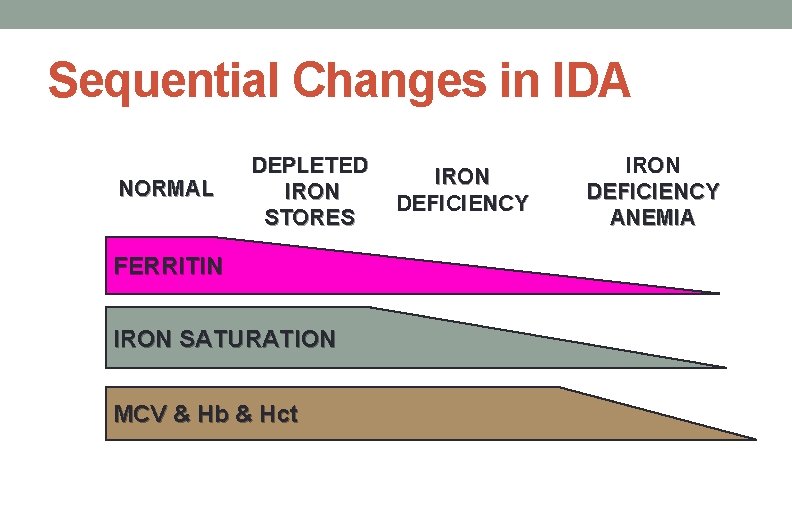
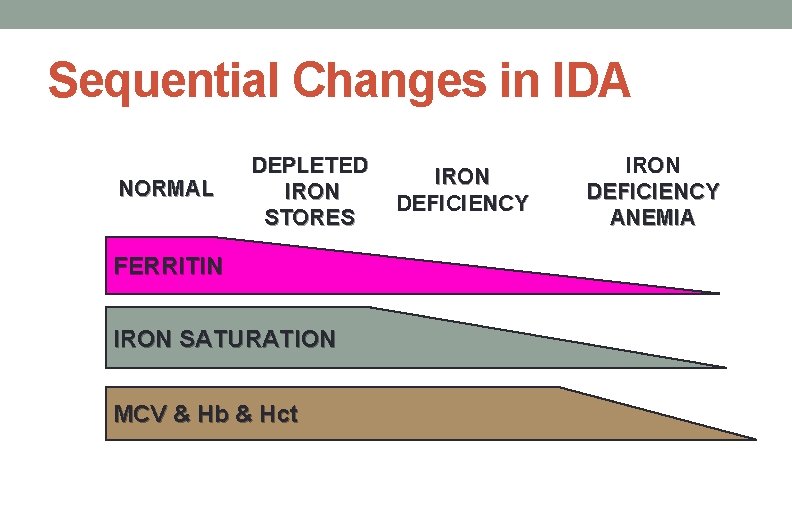
Sequential Changes in IDA NORMAL DEPLETED IRON STORES FERRITIN IRON SATURATION MCV & Hb & Hct IRON DEFICIENCY ANEMIA
Differential for low serum ferritin 1. 2. Iron Deficiency
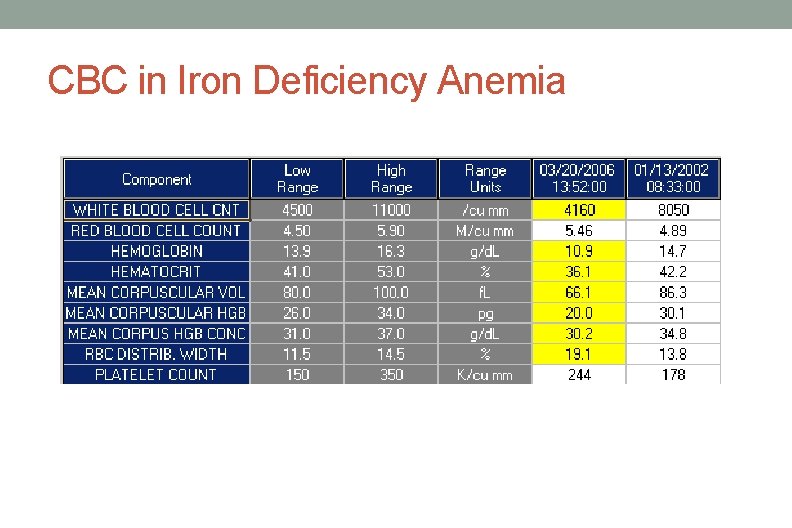
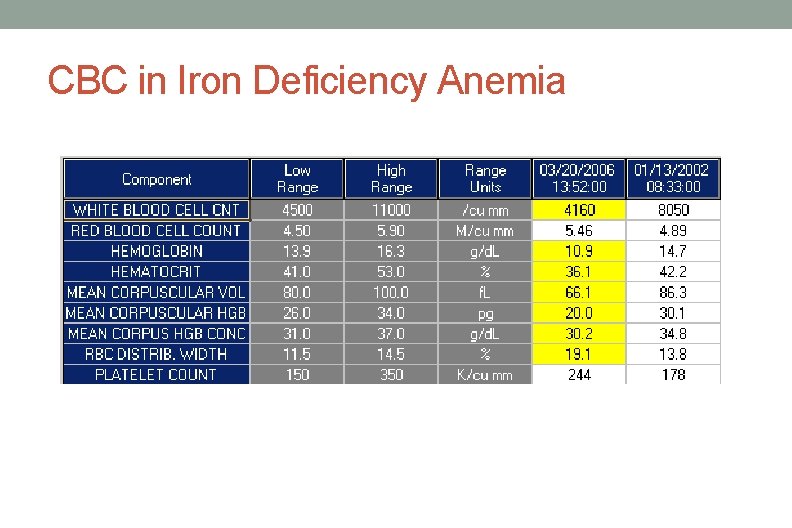
CBC in Iron Deficiency Anemia
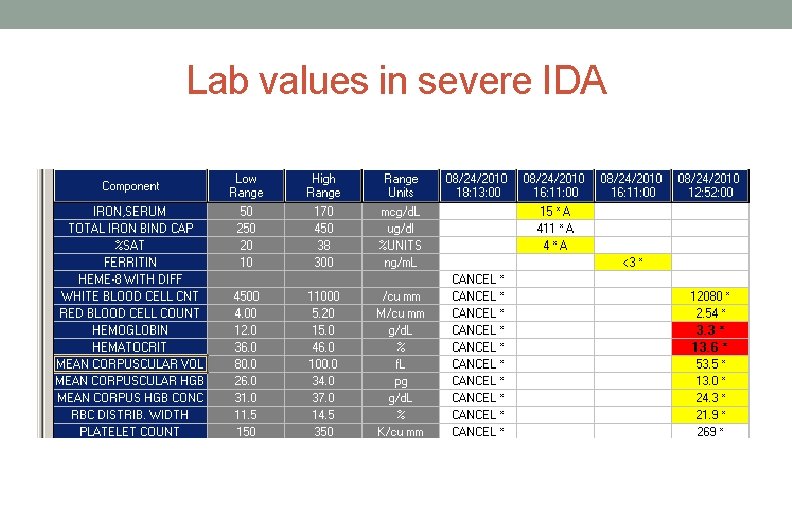
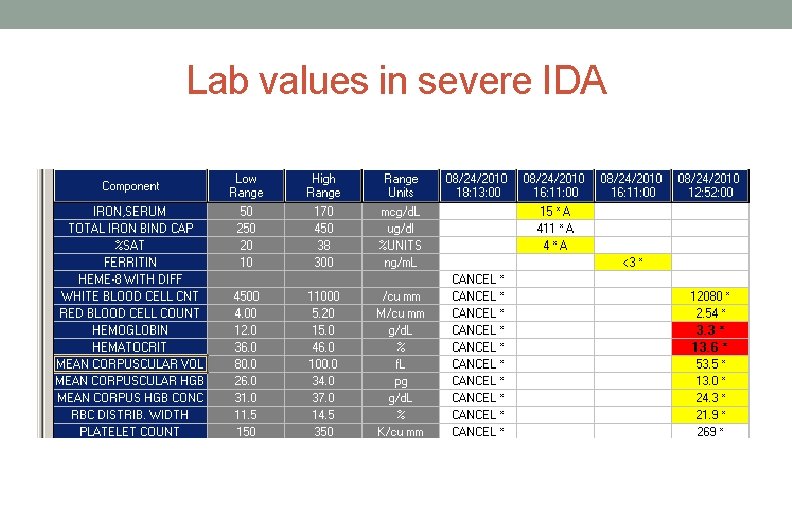
Lab values in severe IDA
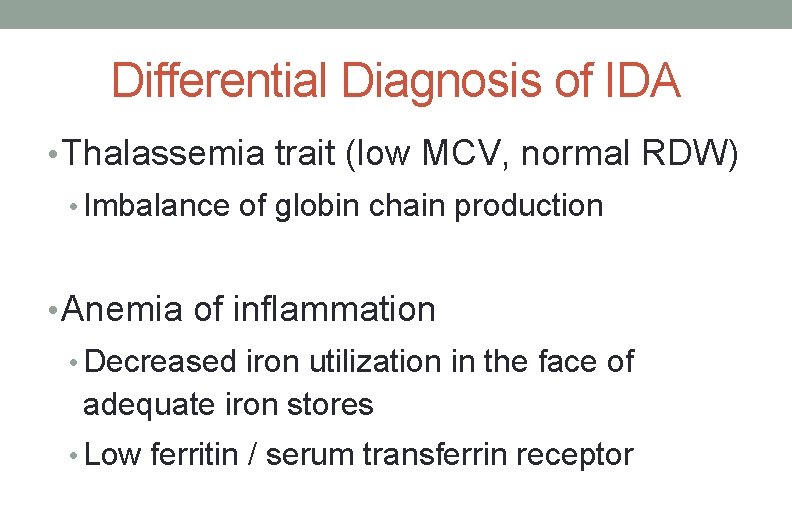
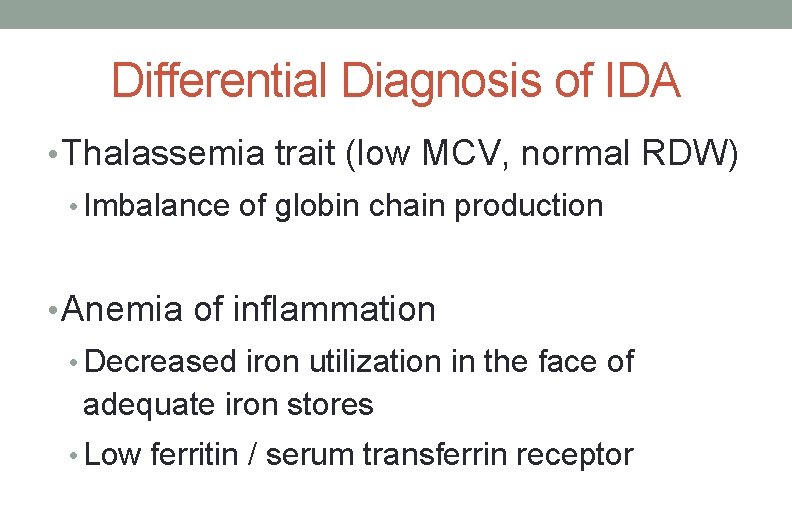
Differential Diagnosis of IDA • Thalassemia trait (low MCV, normal RDW) • Imbalance of globin chain production • Anemia of inflammation • Decreased iron utilization in the face of adequate iron stores • Low ferritin / serum transferrin receptor
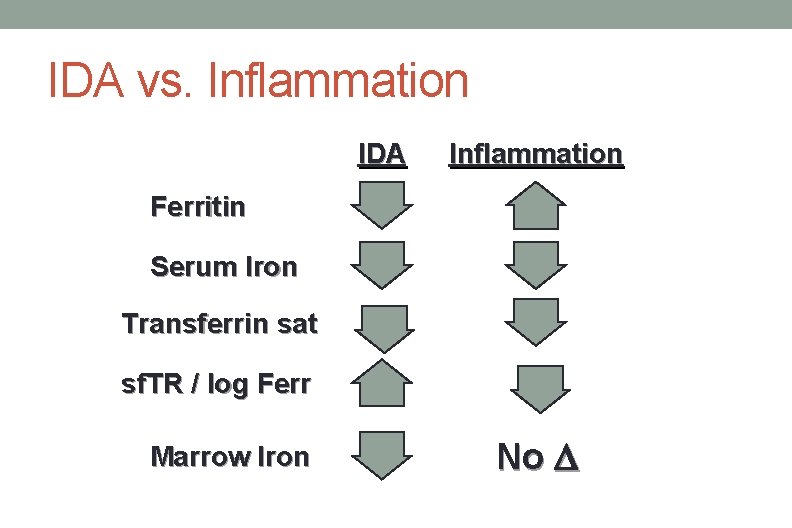
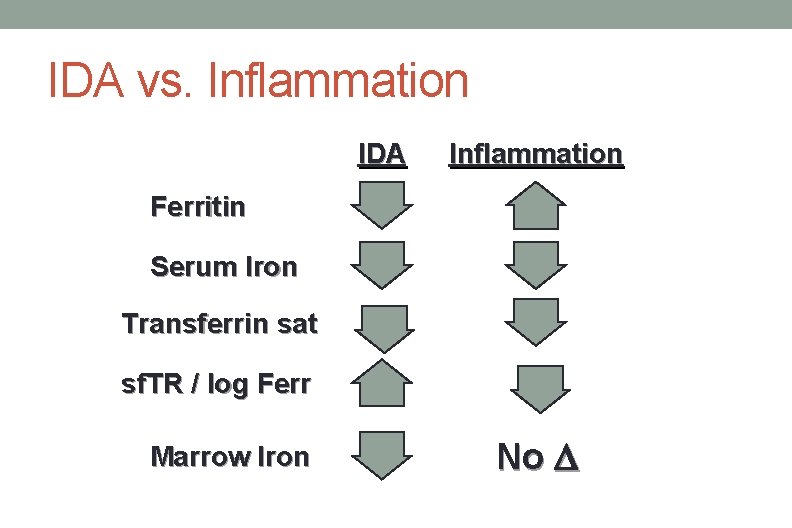
IDA vs. Inflammation IDA Inflammation Ferritin Serum Iron Transferrin sat sf. TR / log Ferr Marrow Iron No D
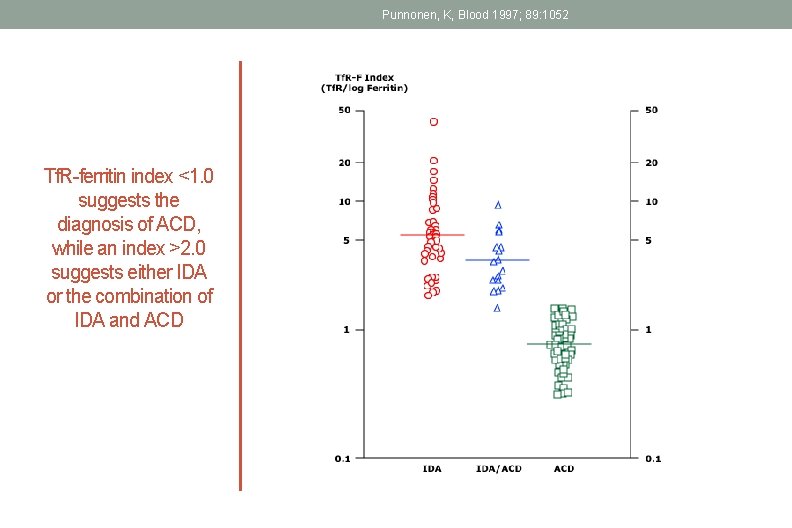
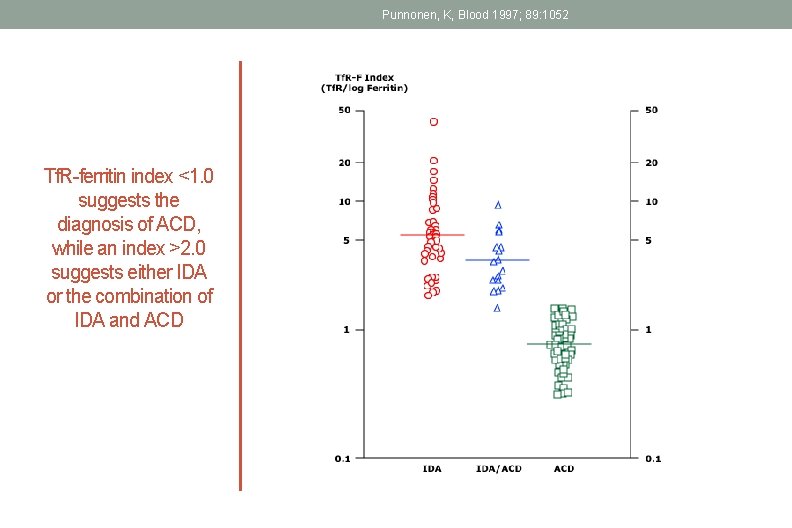
Punnonen, K, Blood 1997; 89: 1052 Tf. R-ferritin index <1. 0 suggests the diagnosis of ACD, while an index >2. 0 suggests either IDA or the combination of IDA and ACD
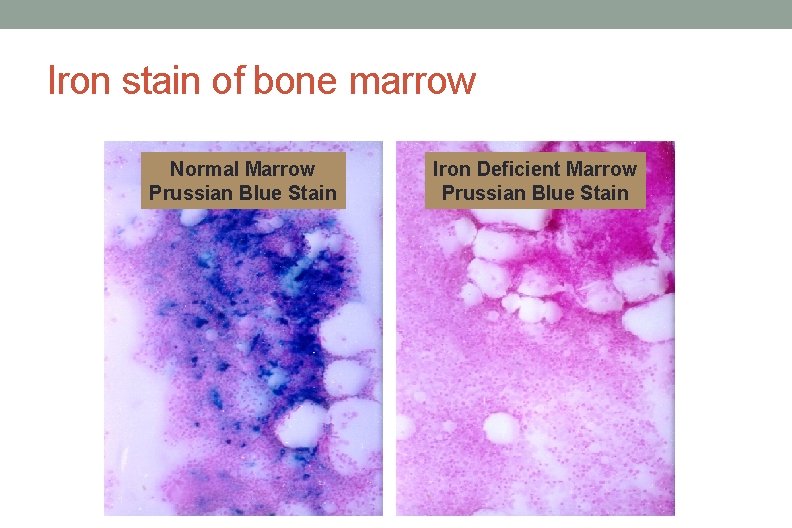
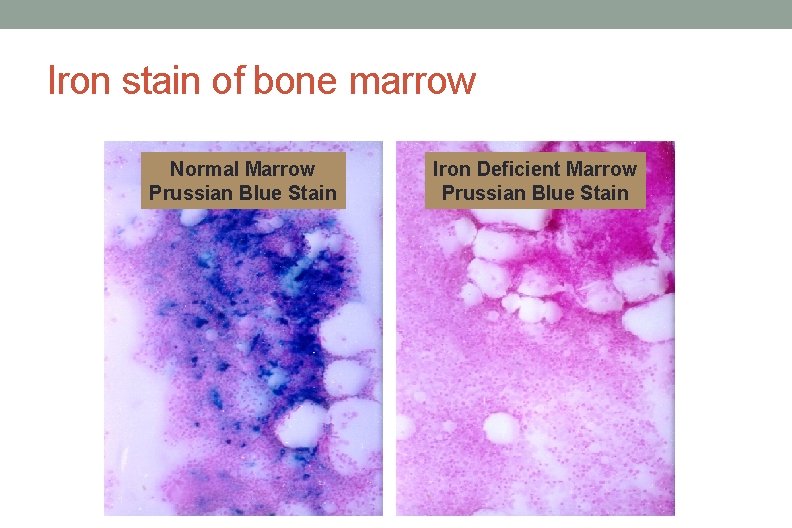
Iron stain of bone marrow Normal Marrow Prussian Blue Stain Iron Deficient Marrow Prussian Blue Stain
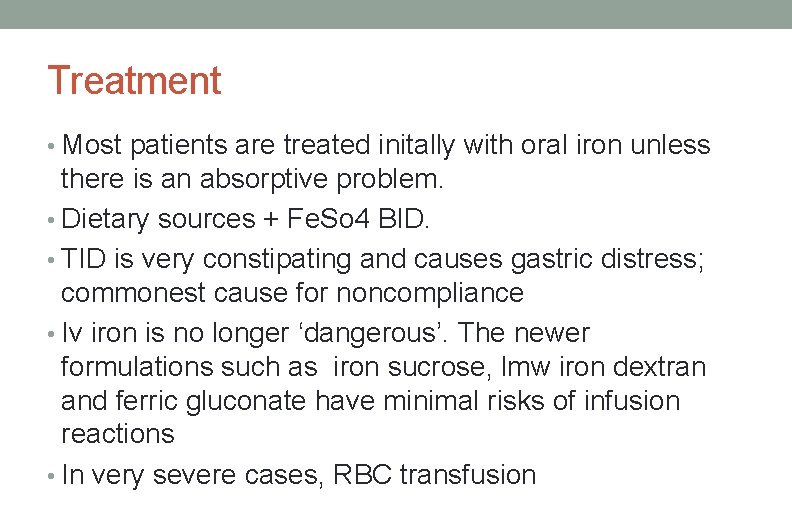
Treatment • Most patients are treated initally with oral iron unless there is an absorptive problem. • Dietary sources + Fe. So 4 BID. • TID is very constipating and causes gastric distress; commonest cause for noncompliance • Iv iron is no longer ‘dangerous’. The newer formulations such as iron sucrose, lmw iron dextran and ferric gluconate have minimal risks of infusion reactions • In very severe cases, RBC transfusion
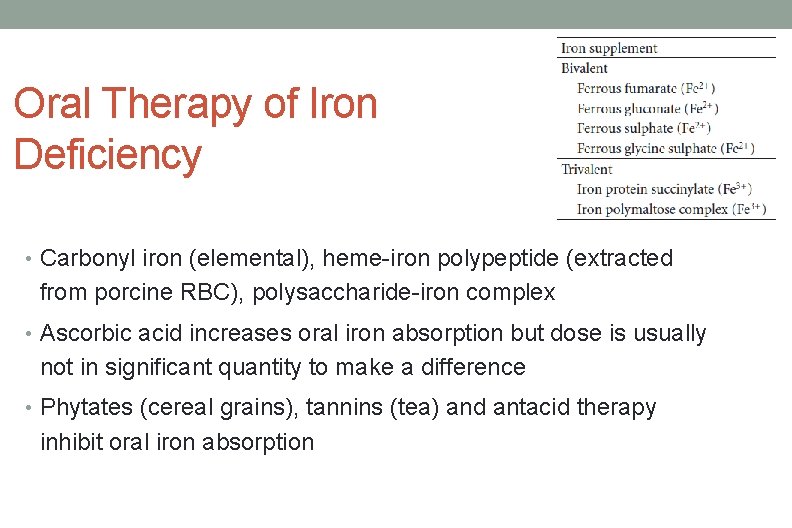
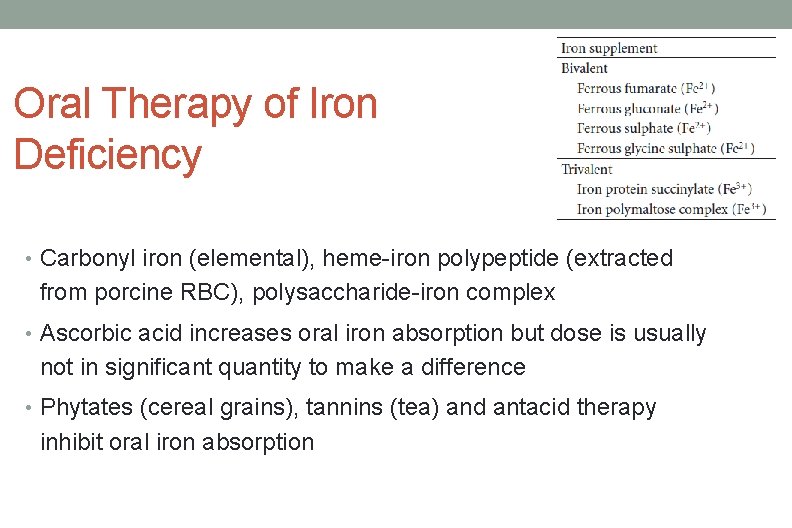
Oral Therapy of Iron Deficiency • Carbonyl iron (elemental), heme-iron polypeptide (extracted from porcine RBC), polysaccharide-iron complex • Ascorbic acid increases oral iron absorption but dose is usually not in significant quantity to make a difference • Phytates (cereal grains), tannins (tea) and antacid therapy inhibit oral iron absorption
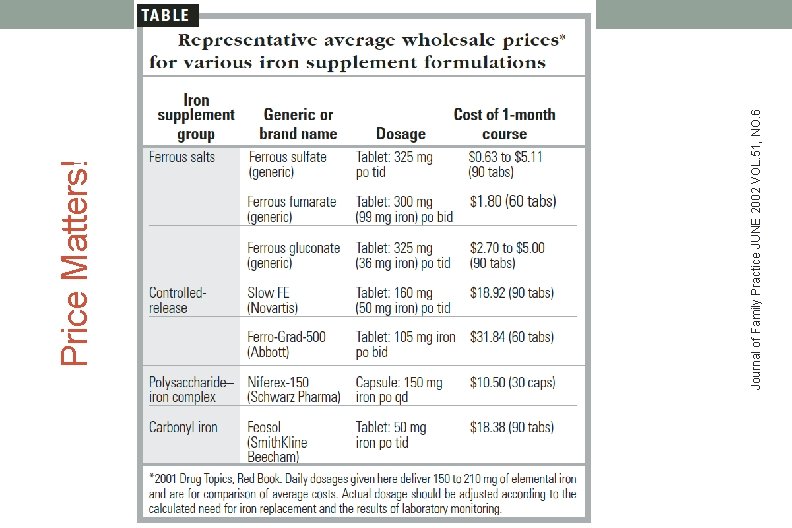
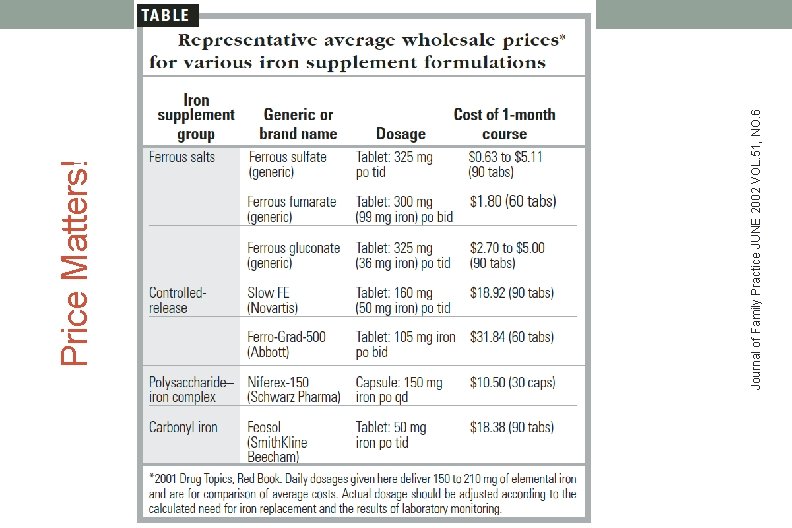
Journal of Family Practice JUNE 2002 VOL. 51, NO. 6 Price Matters!
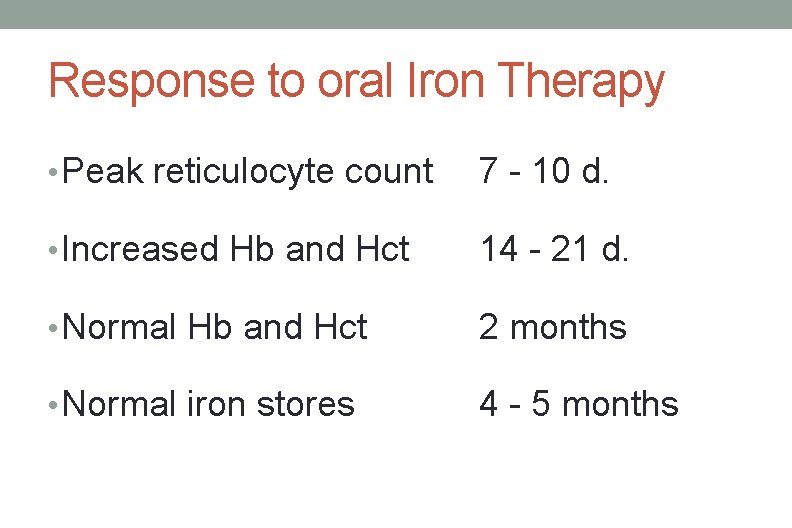
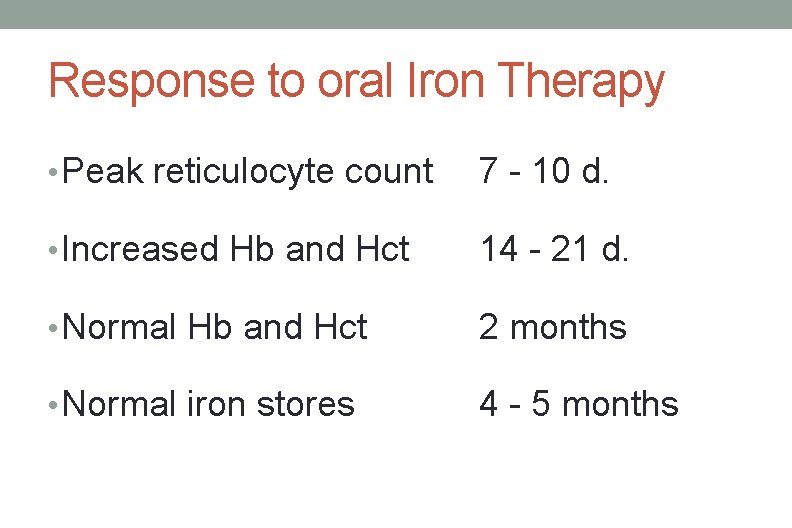
Response to oral Iron Therapy • Peak reticulocyte count 7 - 10 d. • Increased Hb and Hct 14 - 21 d. • Normal Hb and Hct 2 months • Normal iron stores 4 - 5 months
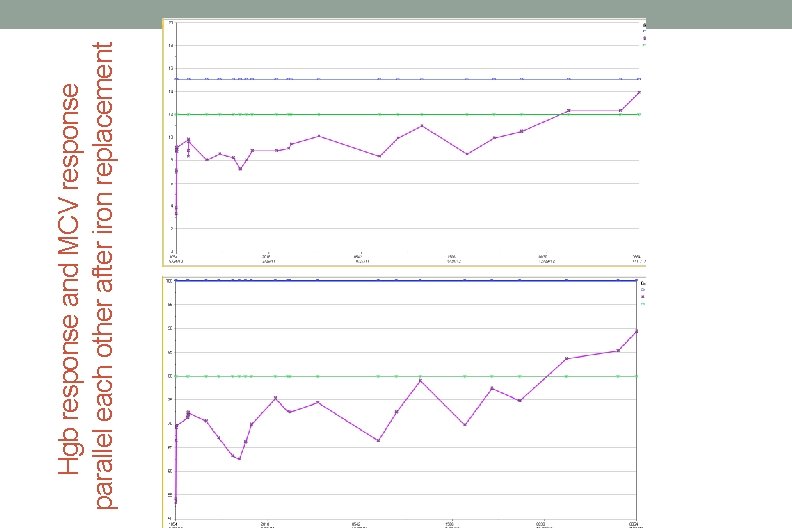
Hgb response and MCV response parallel each other after iron replacement
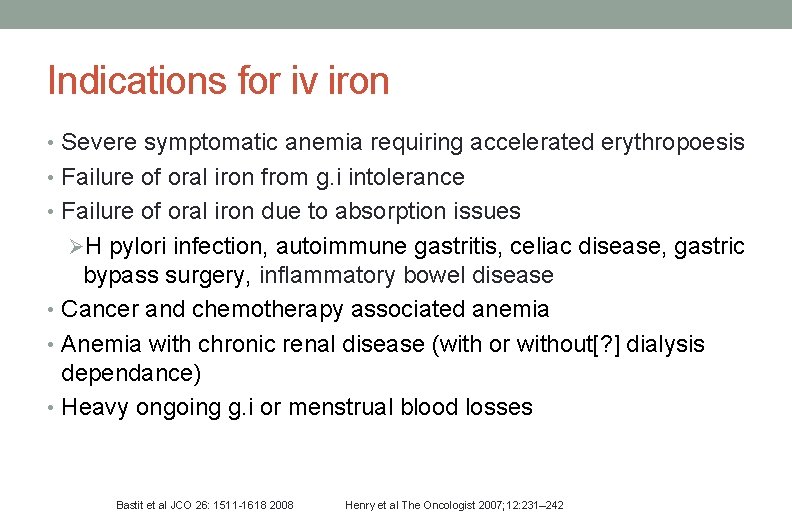
Indications for iv iron • Severe symptomatic anemia requiring accelerated erythropoesis • Failure of oral iron from g. i intolerance • Failure of oral iron due to absorption issues ØH pylori infection, autoimmune gastritis, celiac disease, gastric bypass surgery, inflammatory bowel disease • Cancer and chemotherapy associated anemia • Anemia with chronic renal disease (with or without[? ] dialysis dependance) • Heavy ongoing g. i or menstrual blood losses Bastit et al JCO 26: 1511 -1618 2008 Henry et al The Oncologist 2007; 12: 231– 242
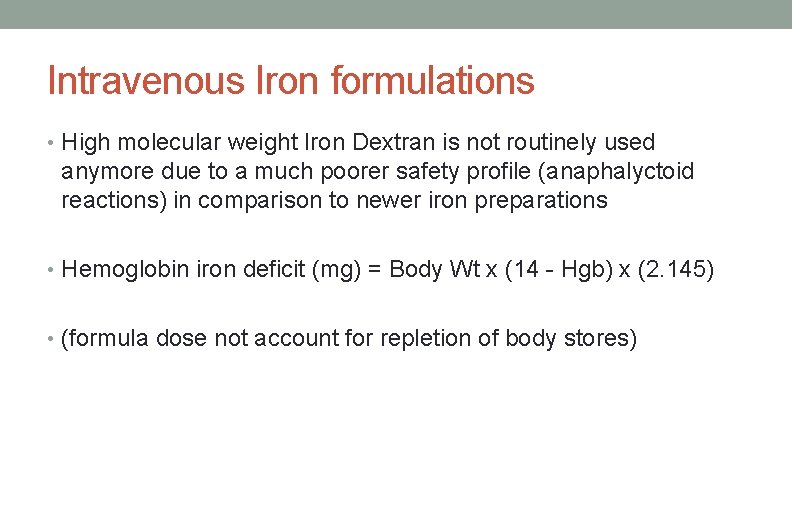
Intravenous Iron formulations • High molecular weight Iron Dextran is not routinely used anymore due to a much poorer safety profile (anaphalyctoid reactions) in comparison to newer iron preparations • Hemoglobin iron deficit (mg) = Body Wt x (14 - Hgb) x (2. 145) • (formula dose not account for repletion of body stores)
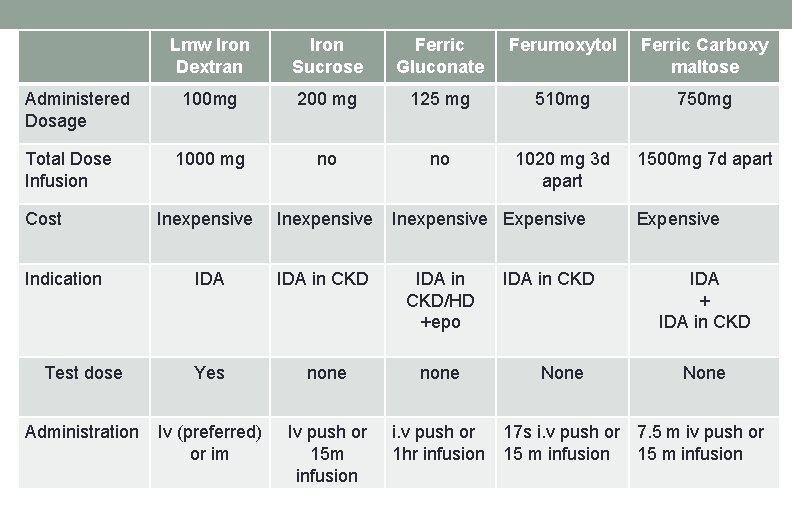
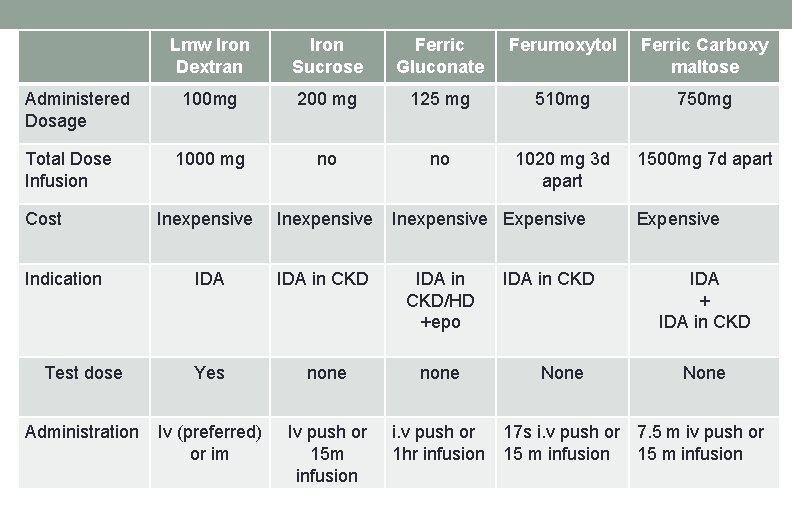
Lmw Iron Dextran Iron Sucrose Ferric Gluconate Ferumoxytol Ferric Carboxy maltose 100 mg 200 mg 125 mg 510 mg 750 mg 1000 mg no no 1020 mg 3 d apart 1500 mg 7 d apart Inexpensive IDA in CKD/HD +epo Test dose Yes none Administration Iv (preferred) or im Iv push or 15 m infusion i. v push or 1 hr infusion Administered Dosage Total Dose Infusion Cost Indication Inexpensive Expensive IDA in CKD None Expensive IDA + IDA in CKD None 17 s i. v push or 7. 5 m iv push or 15 m infusion
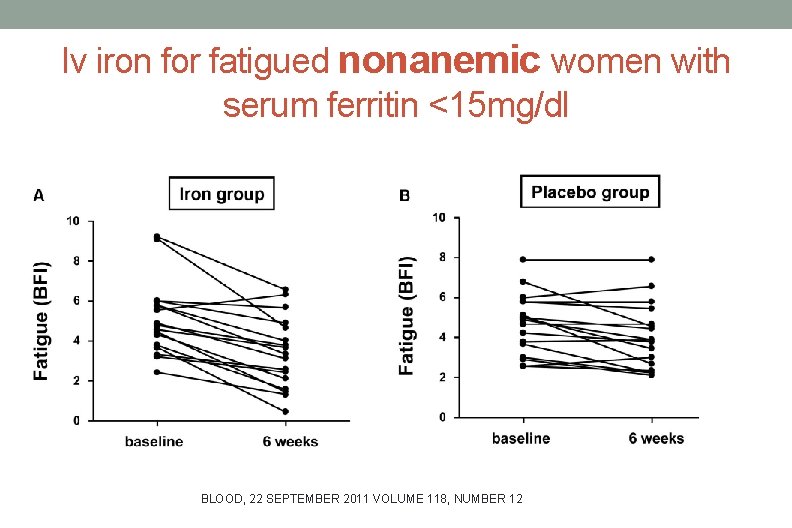
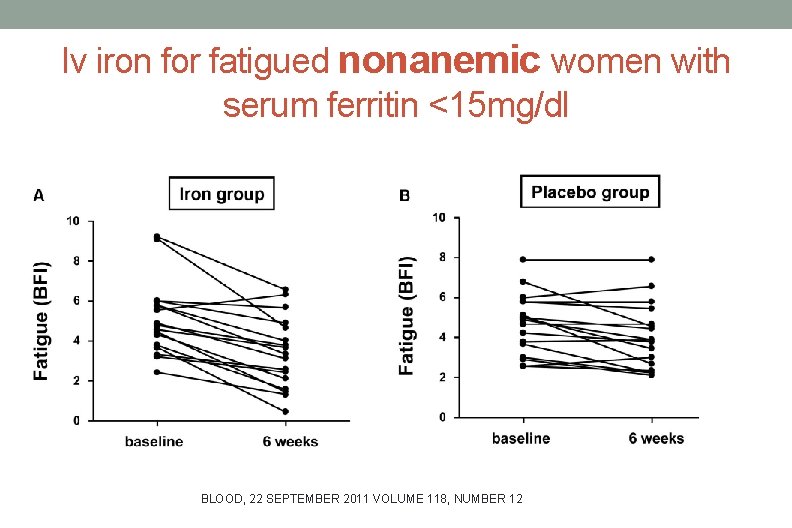
Iv iron for fatigued nonanemic women with serum ferritin <15 mg/dl BLOOD, 22 SEPTEMBER 2011 VOLUME 118, NUMBER 12
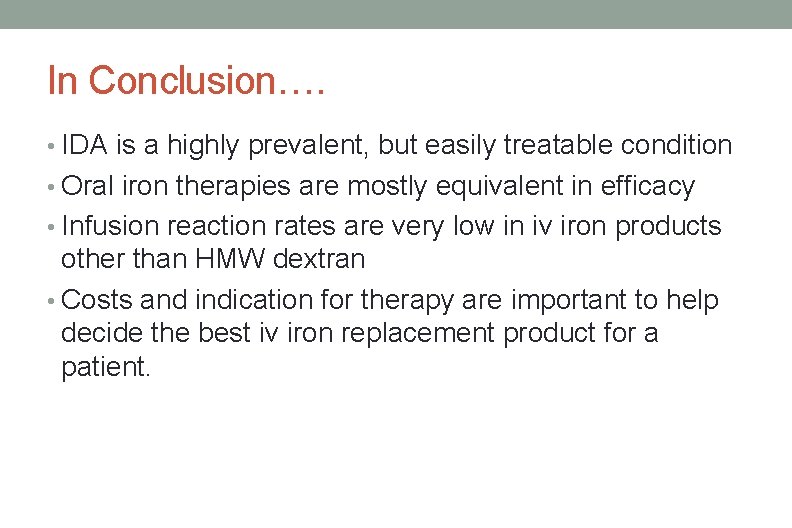
In Conclusion…. • IDA is a highly prevalent, but easily treatable condition • Oral iron therapies are mostly equivalent in efficacy • Infusion reaction rates are very low in iv iron products other than HMW dextran • Costs and indication for therapy are important to help decide the best iv iron replacement product for a patient.
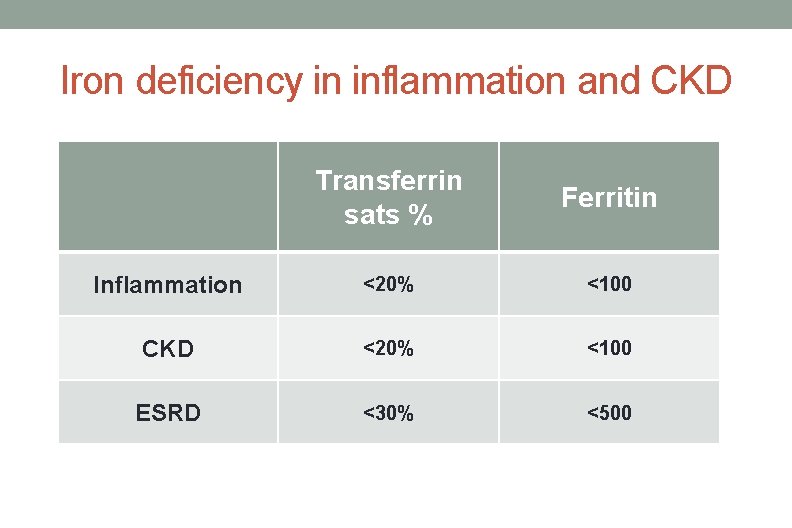
Iron studies in inflammation and CKD • There is no established goal as to what lab parameters are considered iron deficiency • Functional iron deficiency is where iron stores are present in the body but not usable due to Hepcidin • Usually normocytic but microcytic anemia in severe cases
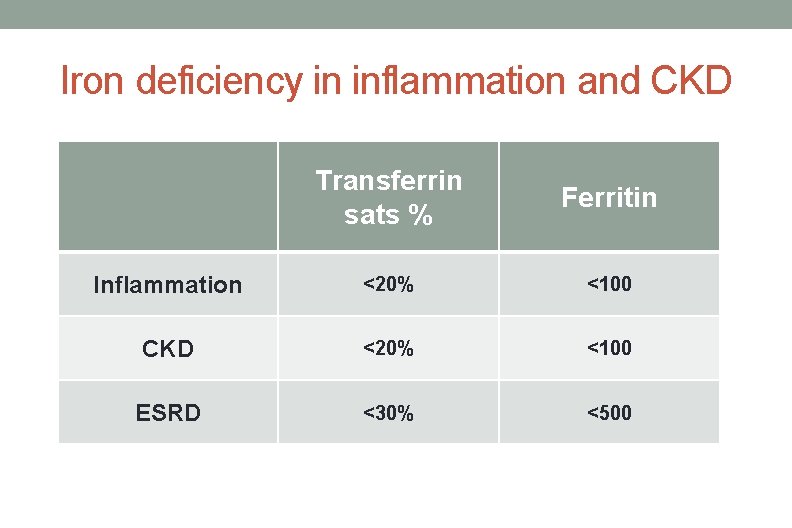
Iron deficiency in inflammation and CKD Transferrin sats % Ferritin Inflammation <20% <100 CKD <20% <100 ESRD <30% <500
Questions rakhi@jhmi. edu
 Low ferritin symptoms
Low ferritin symptoms L
L Low iron deficiency symptoms
Low iron deficiency symptoms Anemia tibc ferritin iron
Anemia tibc ferritin iron Minerals are inorganic elements that the body
Minerals are inorganic elements that the body Feroba-you sr tab
Feroba-you sr tab Dashod dog
Dashod dog Microcytic hypochromic anemia
Microcytic hypochromic anemia Retikulocyte
Retikulocyte Low ferritin symptoms
Low ferritin symptoms Iron studies interpretation
Iron studies interpretation Iron deficiency anemia differential diagnosis
Iron deficiency anemia differential diagnosis Luas layang layang
Luas layang layang Crew cut x ray
Crew cut x ray Causes of megaloblastic anaemia
Causes of megaloblastic anaemia Megaloblastic anemia vs pernicious anemia
Megaloblastic anemia vs pernicious anemia Iron deficiency in roses
Iron deficiency in roses Microcytic hypochromic anemia
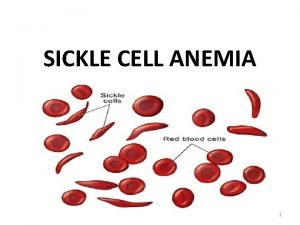
Microcytic hypochromic anemia Sickle cell anemia
Sickle cell anemia Mhs
Mhs Gmds switch
Gmds switch Equação fundamental da ondulatória
Equação fundamental da ondulatória Mhs vs mdwise vs anthem vs caresource
Mhs vs mdwise vs anthem vs caresource Rakhi lalwani
Rakhi lalwani Overfaithfulness
Overfaithfulness Tswf-mhs
Tswf-mhs Mhs hurricane battalion
Mhs hurricane battalion 2009 dress code
2009 dress code Mass of iron in an iron tablet
Mass of iron in an iron tablet Iron sharpens iron friendship
Iron sharpens iron friendship Suketu naik
Suketu naik Kadar nadi naik turun bangku
Kadar nadi naik turun bangku Suhu basal naik tanda hamil
Suhu basal naik tanda hamil Un = arn-1
Un = arn-1 Jyoti naik lijjat papad
Jyoti naik lijjat papad Ujian daya tenaga asas
Ujian daya tenaga asas Types of randomization
Types of randomization Turunan fungsi komposisi
Turunan fungsi komposisi Negasi
Negasi Epangkat kpm
Epangkat kpm Kerbau dipegang talinya manusia dipegang janjinya maksud
Kerbau dipegang talinya manusia dipegang janjinya maksud Tahap pelaksanaan penilaian
Tahap pelaksanaan penilaian Poonam naik
Poonam naik