DELIRIUM RECOGNITION AND MANAGEMENT DR AISLING OGORMAN Consultant
- Slides: 43
DELIRIUM RECOGNITION AND MANAGEMENT DR AISLING O’GORMAN Consultant in Palliative Medicine LOUTH & MEATH SPECIALIST PALLIATIVE CARE SERVICES
DELIRIUM n The entity formally known as …. – – Confusion & agitation - Organic psychosis Acute confusional state - Opioid toxicity Cognitive impairment / failure Acute brain syndrome - ITU encephalopathy 2
DELIRIUM n An aetiologically non-specific, global, cerebral dysfunction characterised by concurrent disturbance of level of consciousness, attention, thinking, perception, memory, psychomotor behaviour, emotion and the sleep-wake cycle. 3
Confused ? ? Delirium = Brain Failure
DELIRIUM n An aetiologically non-specific, global, cerebral dysfunction characterised by concurrent disturbance of level of consciousness, attention, thinking, perception, memory, psychomotor behaviour, emotion and the sleep-wake cycle. 5
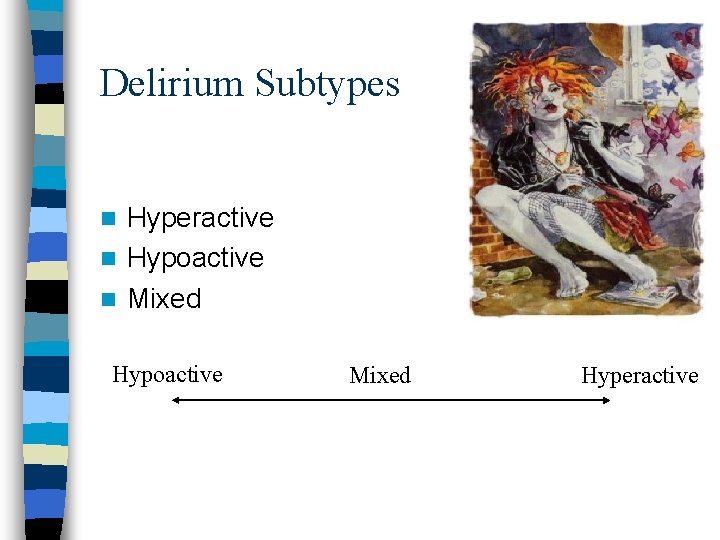
Delirium Subtypes Hyperactive n Hypoactive n Mixed n Hypoactive Mixed Hyperactive
Delirium – What’s it to YOU ? ? ? Delirious patients n n n Stop eating Stop drinking fluids Stop taking important medications May fall and injure themselves Are often placed in restraints and suffer complications such as aspiration and decubitus
n Morbidity: – Associated with prolonged hospitalisation – More hospital-acquired complications e. g. falls & pressure sores – Increased risk of long term cognitive decline – More likely to require admission to long term care – Loss of independent living
Delirium Is Deadly !!! n Mortality rates: – 10% - 65% But - With appropriate management, may be reversible in up to 50%
DELIRIUM n Prevalence: – 10% - 35% of hospitalised patients n Elderly Patients – 30% of hospitalised elderly n Cancer Patients – 25% - 40% of cancer patients – Up to 85% of cancer patients with advanced disease 10
Risk Factor. Assessment for Delirium Age 65 yrs or older n Cognitive impairment (past or present) n Current hip fracture n Severe illness n 11
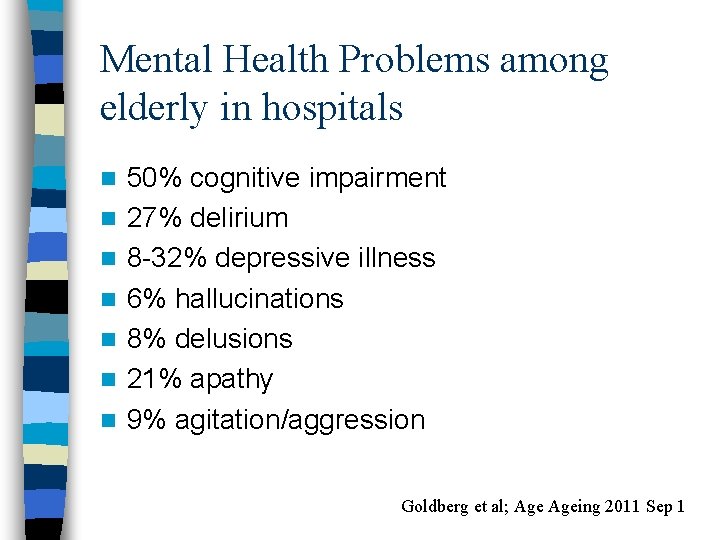
Mental Health Problems among elderly in hospitals n n n n 50% cognitive impairment 27% delirium 8 -32% depressive illness 6% hallucinations 8% delusions 21% apathy 9% agitation/aggression Goldberg et al; Ageing 2011 Sep 1
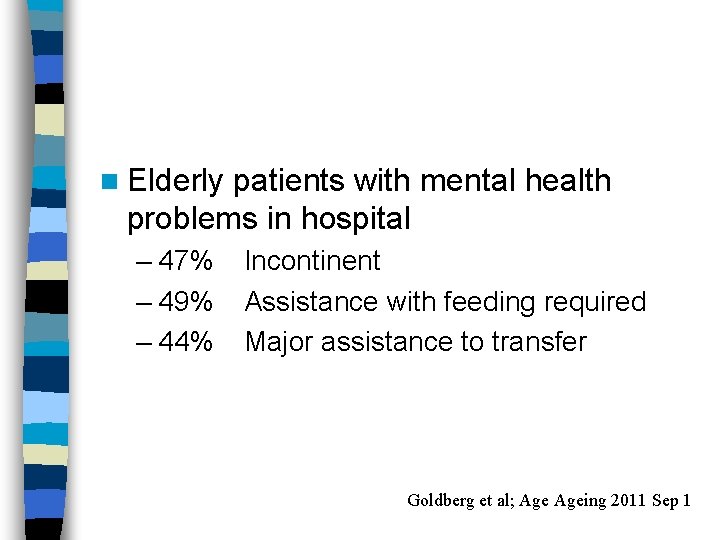
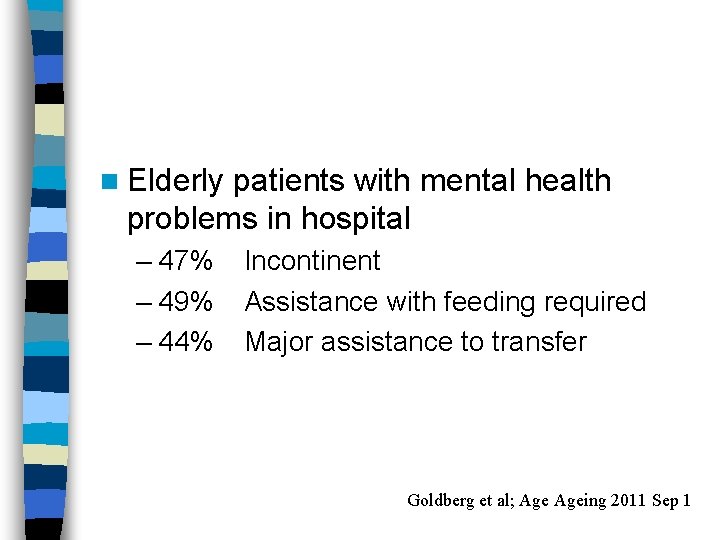
n Elderly patients with mental health problems in hospital – 47% – 49% – 44% Incontinent Assistance with feeding required Major assistance to transfer Goldberg et al; Ageing 2011 Sep 1
Delirium – Differential Diagnosis Dementia n Depression n Mania n Psychosis n
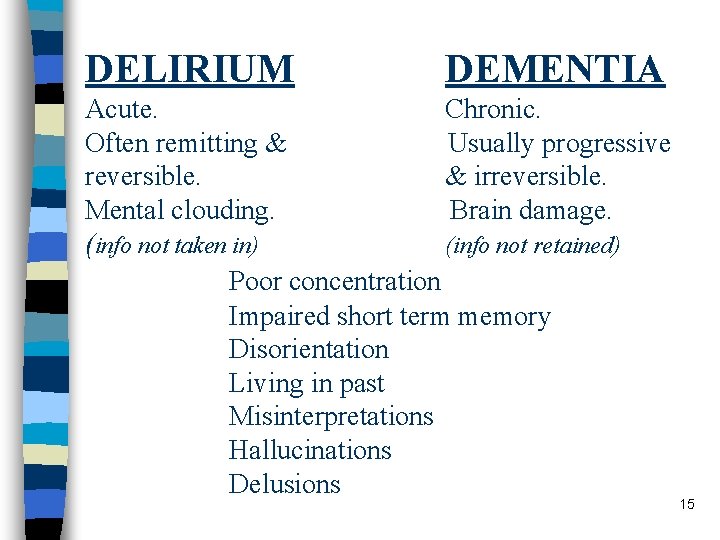
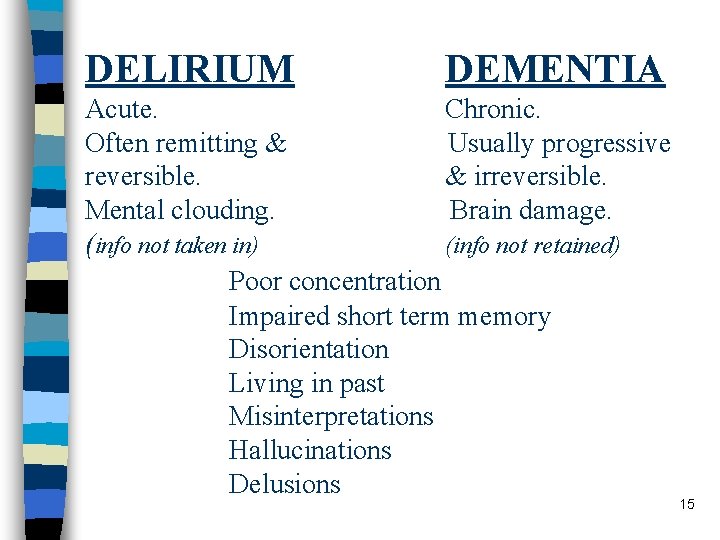
DELIRIUM DEMENTIA Acute. Chronic. Often remitting & Usually progressive reversible. & irreversible. Mental clouding. Brain damage. (info not taken in) (info not retained) Poor concentration Impaired short term memory Disorientation Living in past Misinterpretations Hallucinations Delusions 15
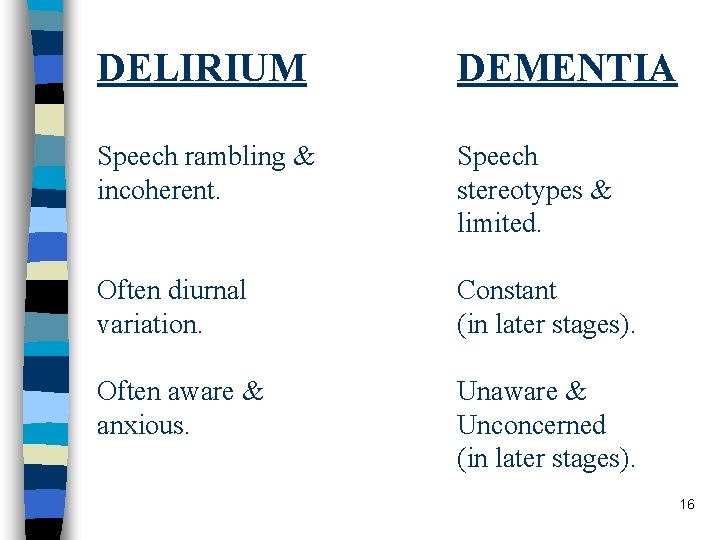
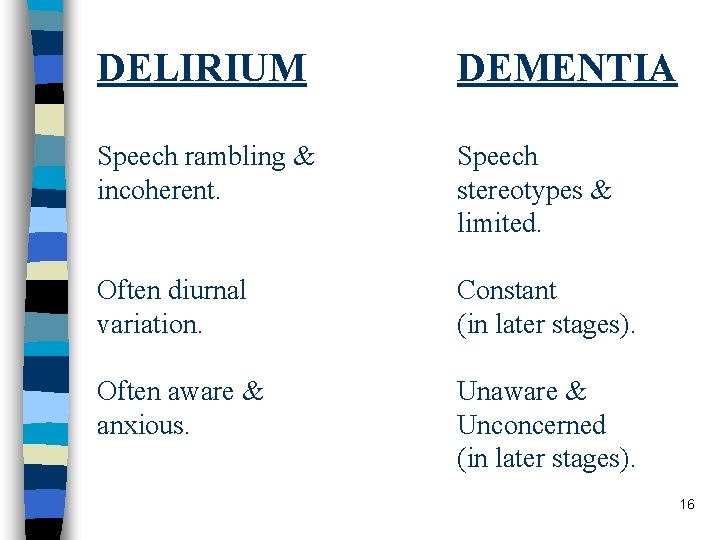
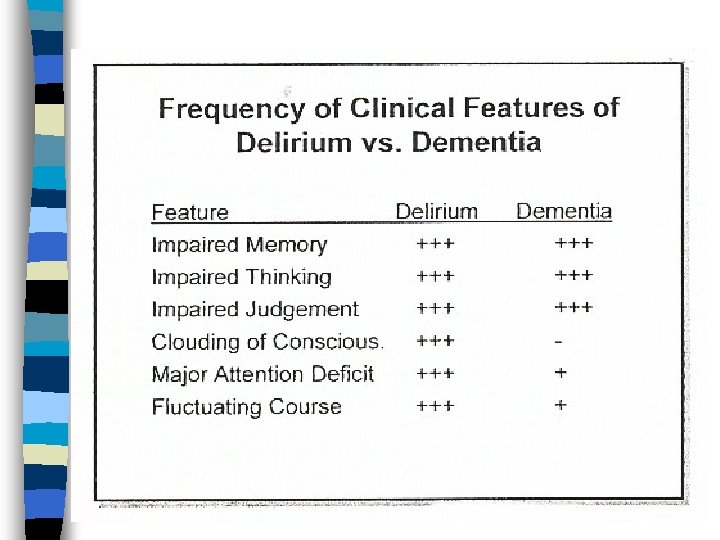
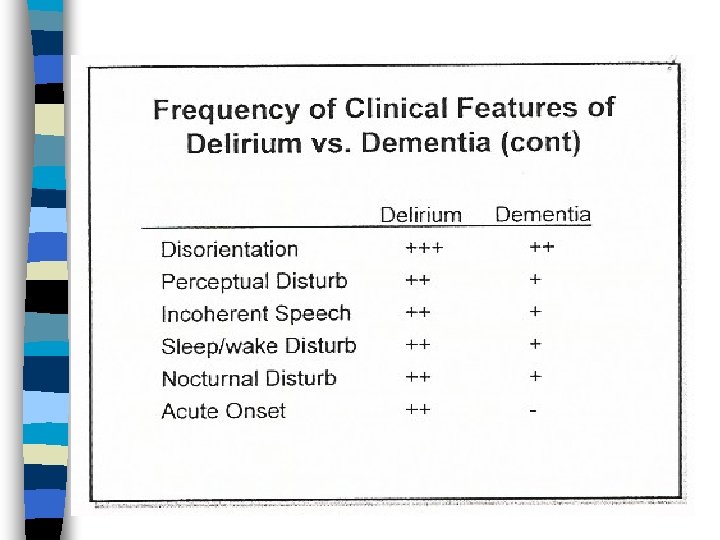
DELIRIUM DEMENTIA Speech rambling & incoherent. Speech stereotypes & limited. Often diurnal variation. Constant (in later stages). Often aware & anxious. Unaware & Unconcerned (in later stages). 16
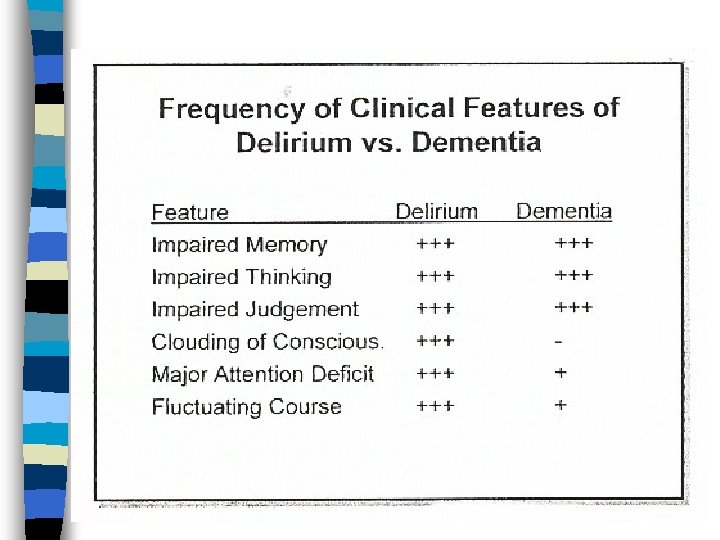
17
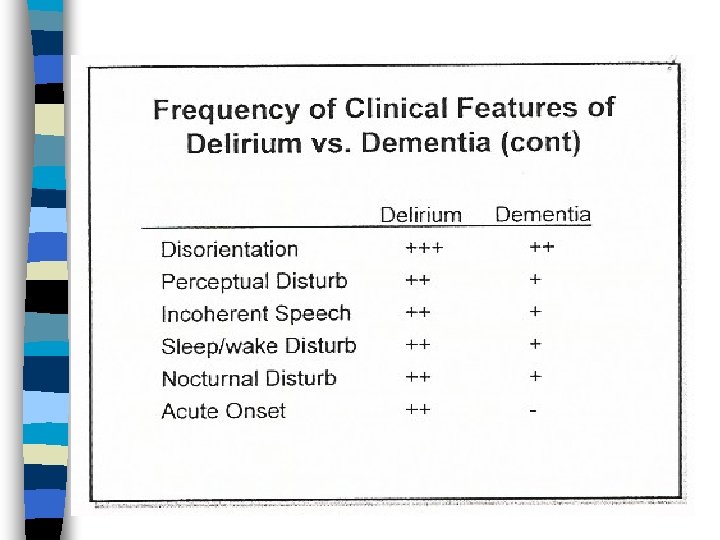
18
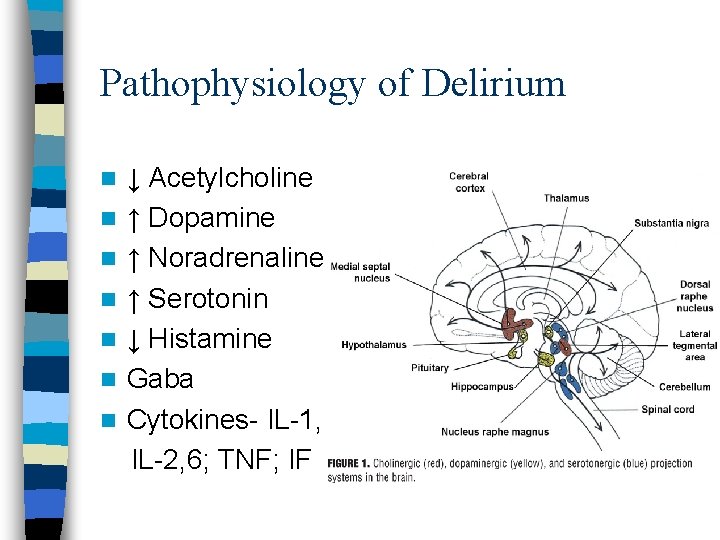
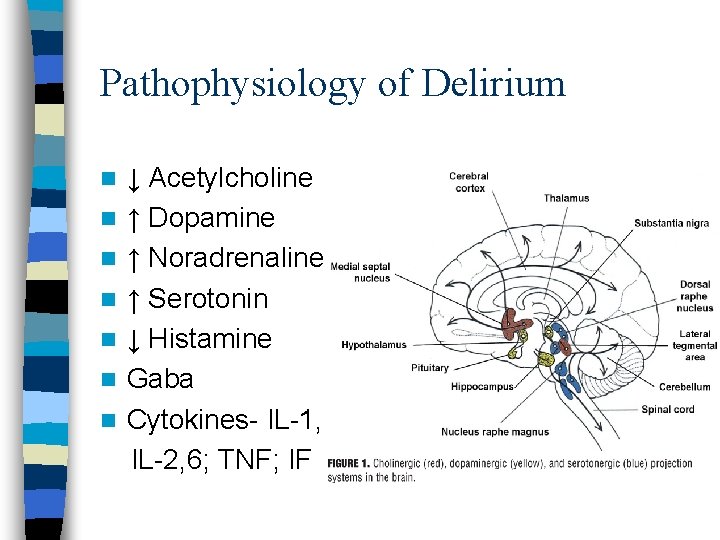
Pathophysiology of Delirium n n n n ↓ Acetylcholine ↑ Dopamine ↑ Noradrenaline ↑ Serotonin ↓ Histamine Gaba Cytokines- IL-1, IL-2, 6; TNF; IF
Recognising Delirium - Indicators n Recent changes or fluctuations in behaviour – Cognitive function – Perception – Physical function – Social behaviour
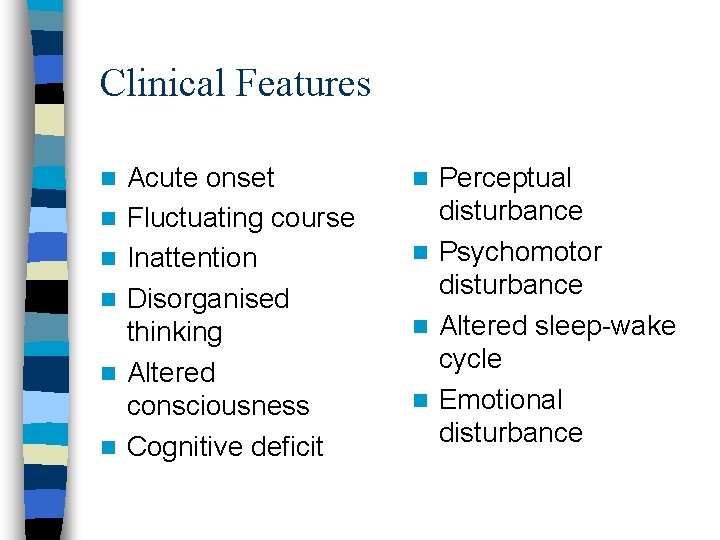
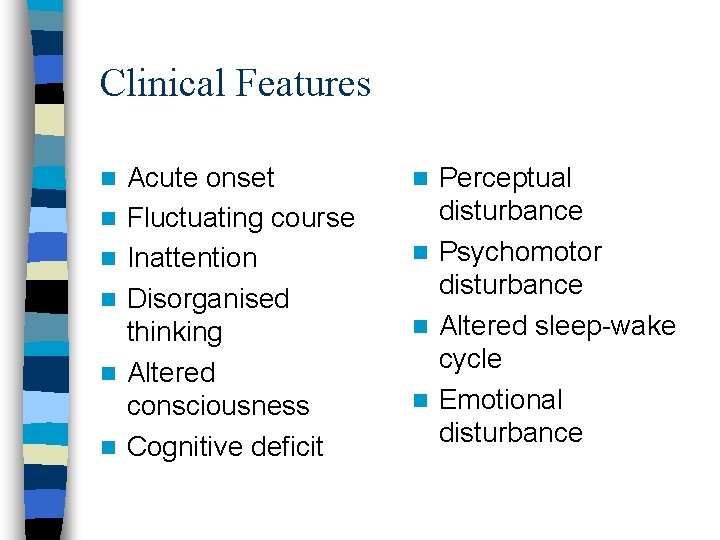
Clinical Features n n n Acute onset Fluctuating course Inattention Disorganised thinking Altered consciousness Cognitive deficit Perceptual disturbance n Psychomotor disturbance n Altered sleep-wake cycle n Emotional disturbance n
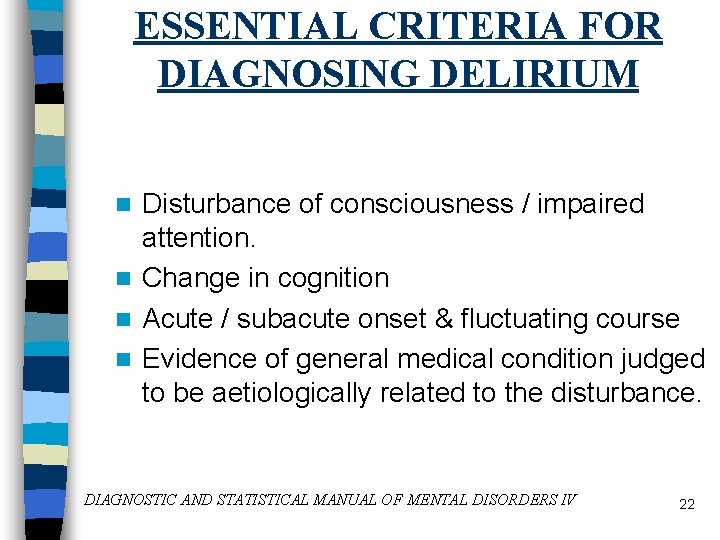
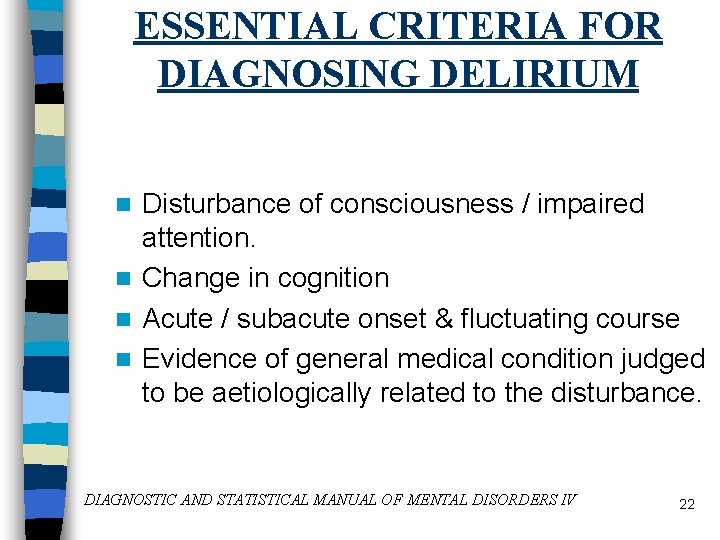
ESSENTIAL CRITERIA FOR DIAGNOSING DELIRIUM Disturbance of consciousness / impaired attention. n Change in cognition n Acute / subacute onset & fluctuating course n Evidence of general medical condition judged to be aetiologically related to the disturbance. n DIAGNOSTIC AND STATISTICAL MANUAL OF MENTAL DISORDERS IV 22
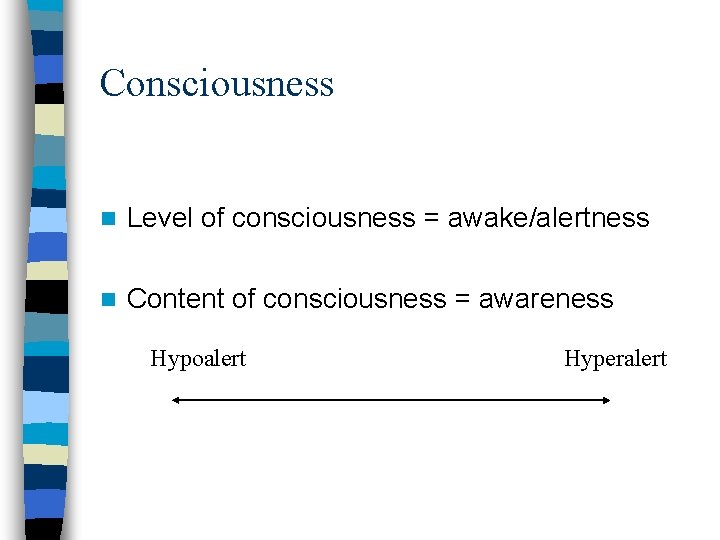
Consciousness n Level of consciousness = awake/alertness n Content of consciousness = awareness Hypoalert Hyperalert
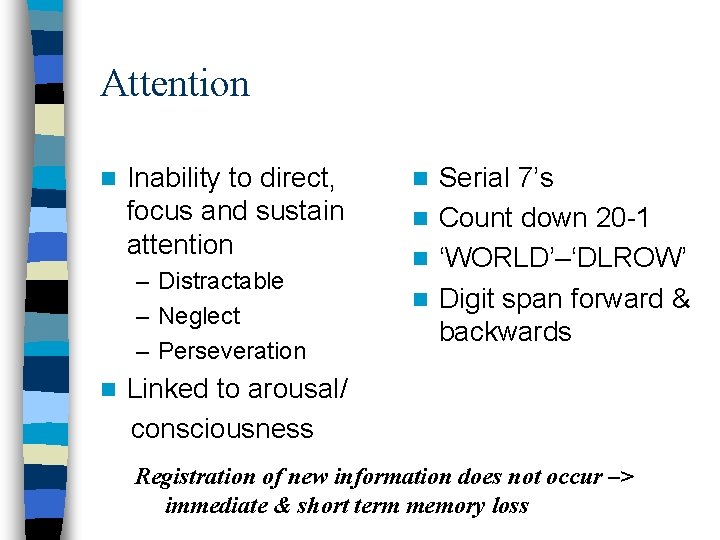
Attention n Inability to direct, focus and sustain attention – Distractable – Neglect – Perseveration n Serial 7’s n Count down 20 -1 n ‘WORLD’–‘DLROW’ n Digit span forward & backwards n Linked to arousal/ consciousness Registration of new information does not occur –> immediate & short term memory loss
Change in Cognition n Disorganised thinking – Memory deficit – Disorientation – Language disturbance – Perceptual disturbance
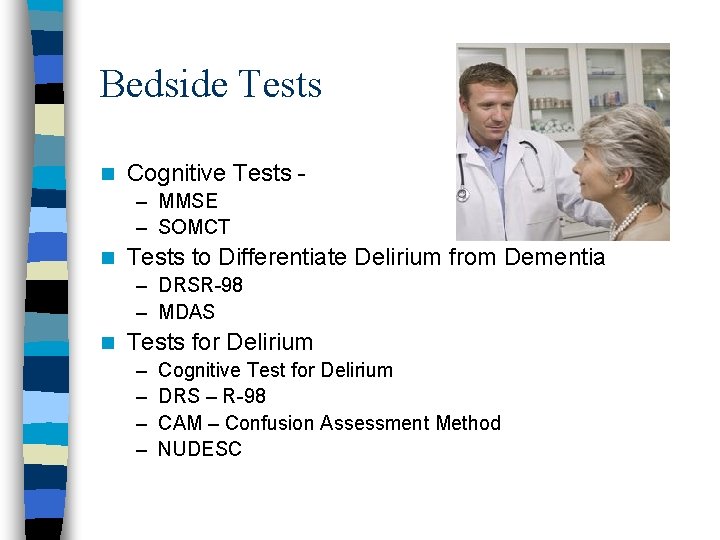
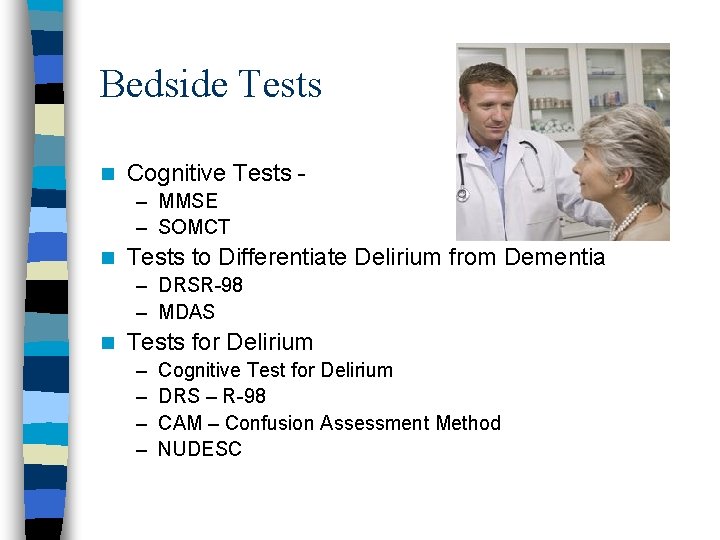
Bedside Tests n Cognitive Tests – MMSE – SOMCT n Tests to Differentiate Delirium from Dementia – DRSR-98 – MDAS n Tests for Delirium – – Cognitive Test for Delirium DRS – R-98 CAM – Confusion Assessment Method NUDESC
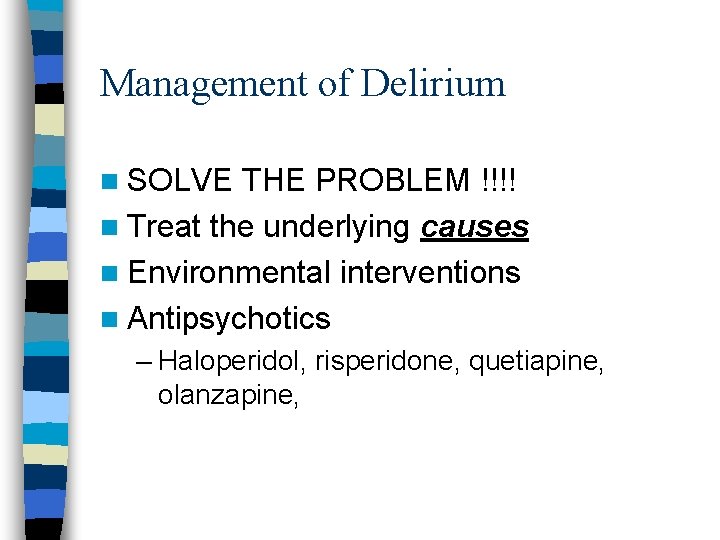
Management of Delirium n SOLVE THE PROBLEM !!!! n Treat the underlying causes n Environmental interventions n Antipsychotics – Haloperidol, risperidone, quetiapine, olanzapine,
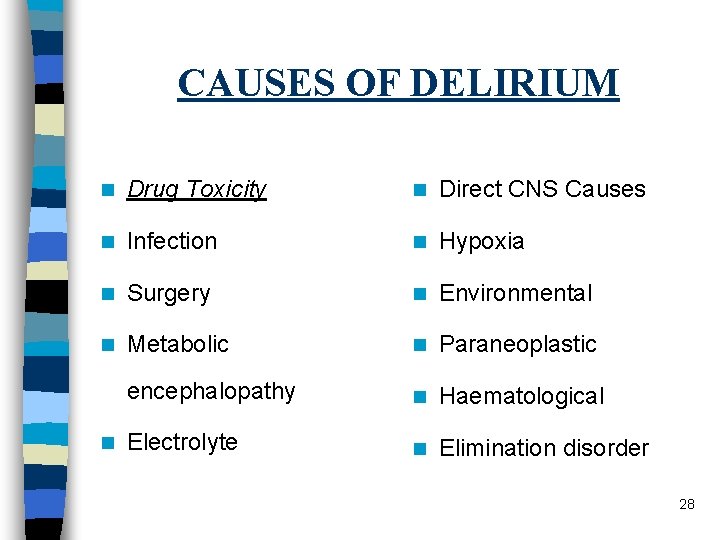
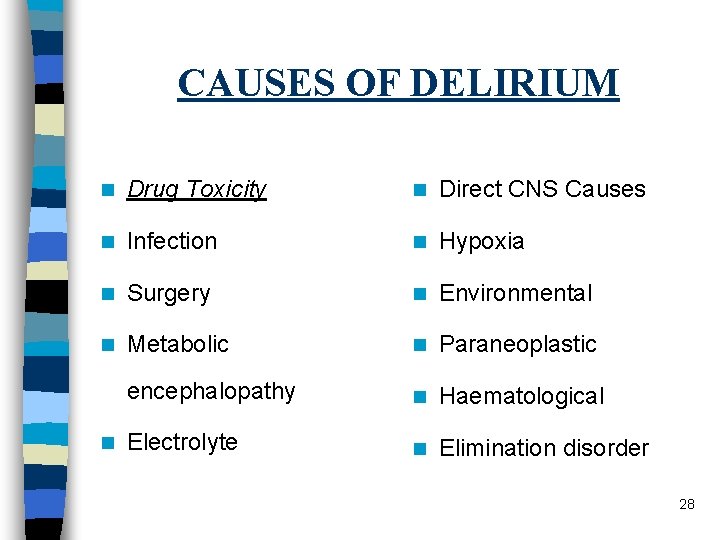
CAUSES OF DELIRIUM n Drug Toxicity n Direct CNS Causes n Infection n Hypoxia n Surgery n Environmental n Metabolic n Paraneoplastic encephalopathy n Haematological Electrolyte n Elimination disorder n 28
Delirium - Causes – Medications • • Chemotherapy Steroids Radiotherapy Opioids Benzodiazepines Anticholinergics Antiemetics Withdrawal
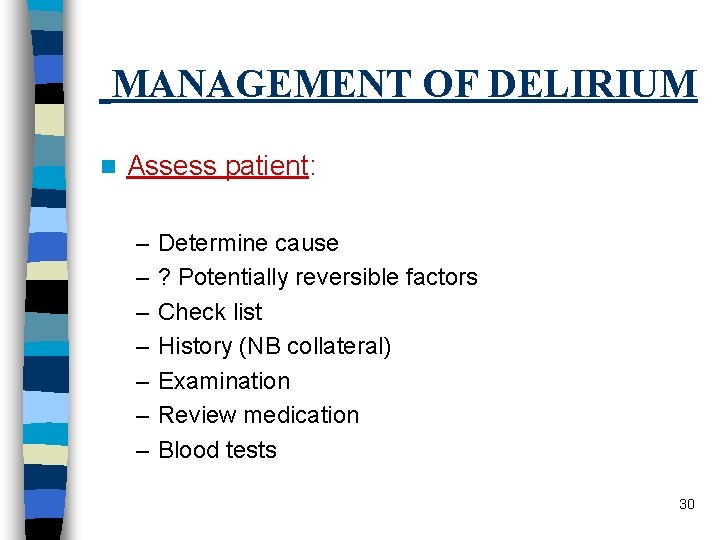
MANAGEMENT OF DELIRIUM n Assess patient: – – – – Determine cause ? Potentially reversible factors Check list History (NB collateral) Examination Review medication Blood tests 30
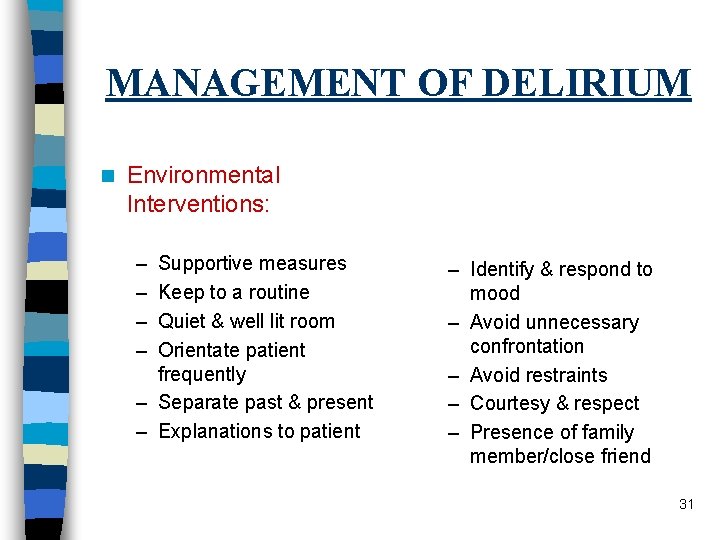
MANAGEMENT OF DELIRIUM n Environmental Interventions: – – Supportive measures Keep to a routine Quiet & well lit room Orientate patient frequently – Separate past & present – Explanations to patient – Identify & respond to mood – Avoid unnecessary confrontation – Avoid restraints – Courtesy & respect – Presence of family member/close friend 31
MANAGEMENT OF DELIRIUM n Communicate with family: – Clear explanation of goals of management & possible outcomes. 32
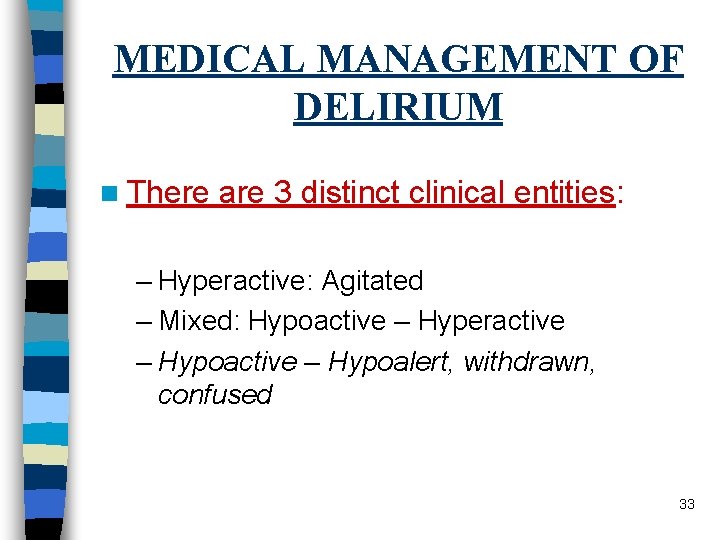
MEDICAL MANAGEMENT OF DELIRIUM n There are 3 distinct clinical entities: – Hyperactive: Agitated – Mixed: Hypoactive – Hyperactive – Hypoalert, withdrawn, confused 33
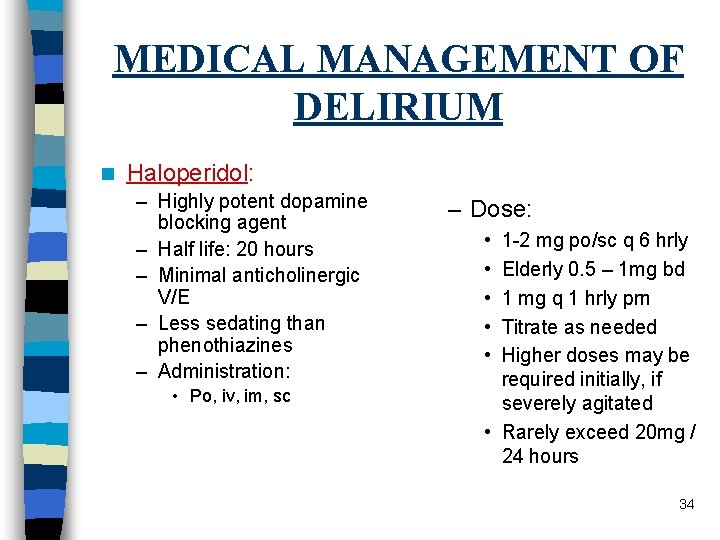
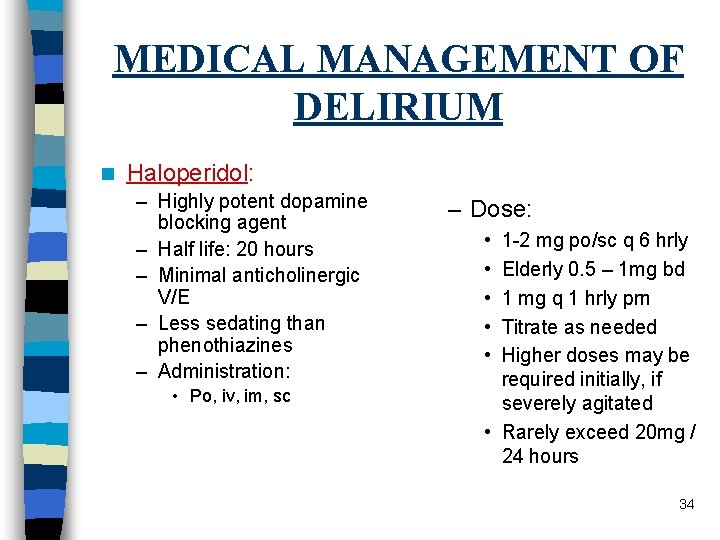
MEDICAL MANAGEMENT OF DELIRIUM n Haloperidol: – Highly potent dopamine blocking agent – Half life: 20 hours – Minimal anticholinergic V/E – Less sedating than phenothiazines – Administration: • Po, iv, im, sc – Dose: • • • 1 -2 mg po/sc q 6 hrly Elderly 0. 5 – 1 mg bd 1 mg q 1 hrly prn Titrate as needed Higher doses may be required initially, if severely agitated • Rarely exceed 20 mg / 24 hours 34
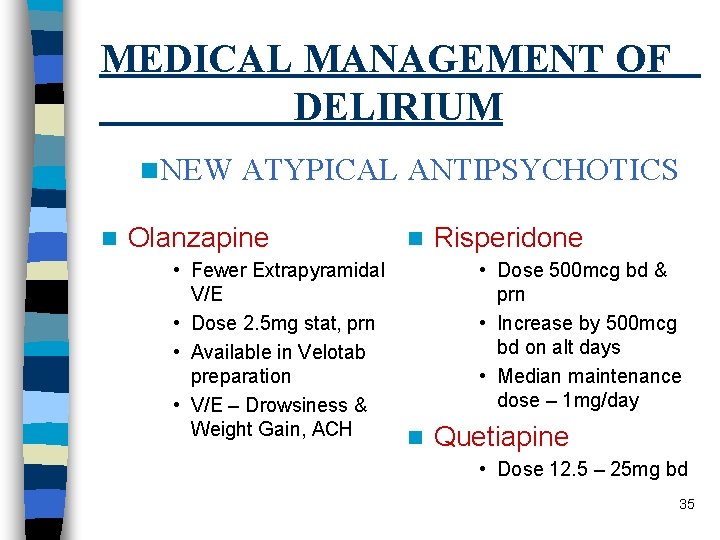
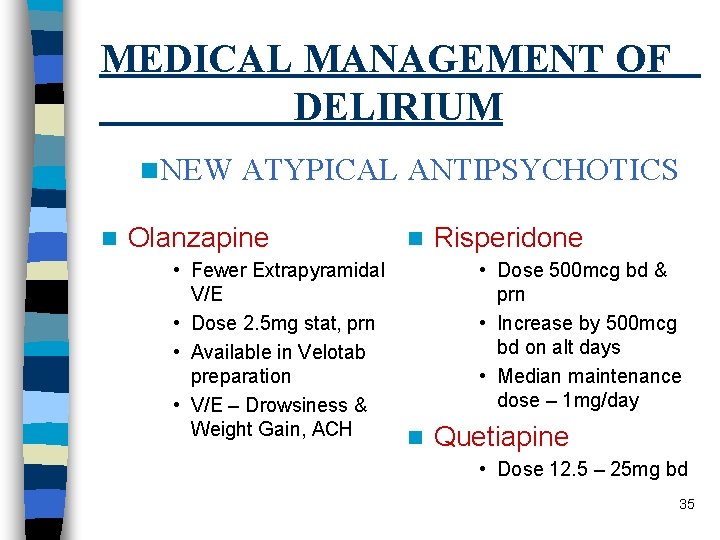
MEDICAL MANAGEMENT OF DELIRIUM n. NEW n ATYPICAL ANTIPSYCHOTICS Olanzapine • Fewer Extrapyramidal V/E • Dose 2. 5 mg stat, prn • Available in Velotab preparation • V/E – Drowsiness & Weight Gain, ACH n Risperidone • Dose 500 mcg bd & prn • Increase by 500 mcg bd on alt days • Median maintenance dose – 1 mg/day n Quetiapine • Dose 12. 5 – 25 mg bd 35
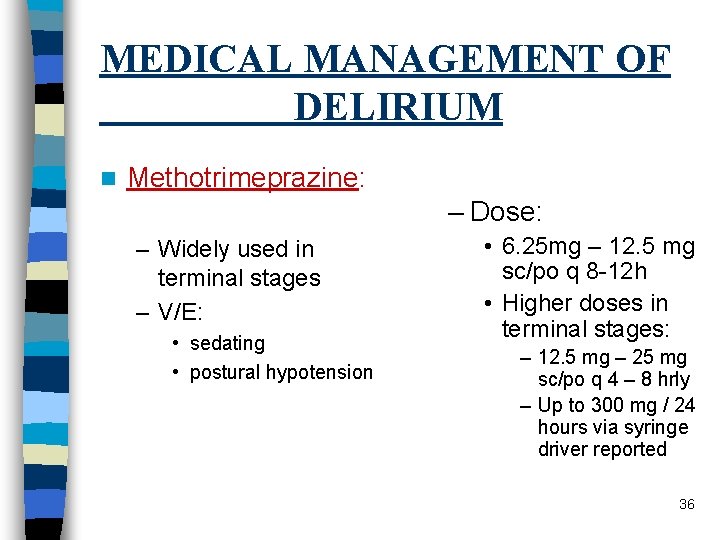
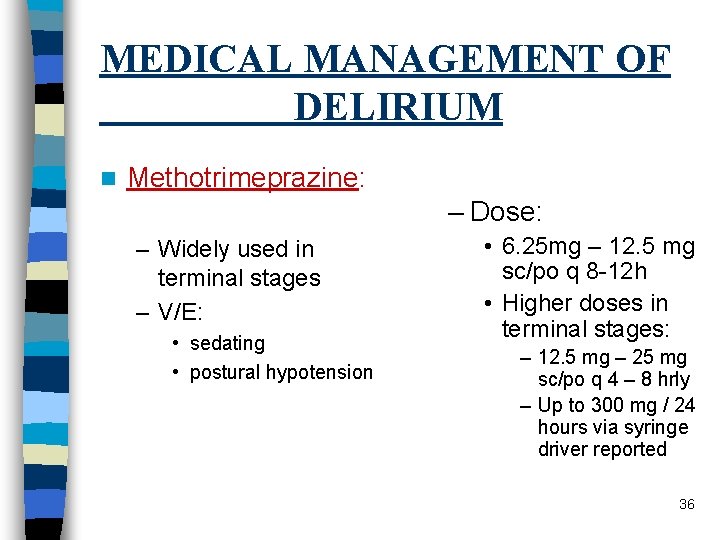
MEDICAL MANAGEMENT OF DELIRIUM n Methotrimeprazine: – Dose: – Widely used in terminal stages – V/E: • sedating • postural hypotension • 6. 25 mg – 12. 5 mg sc/po q 8 -12 h • Higher doses in terminal stages: – 12. 5 mg – 25 mg sc/po q 4 – 8 hrly – Up to 300 mg / 24 hours via syringe driver reported 36
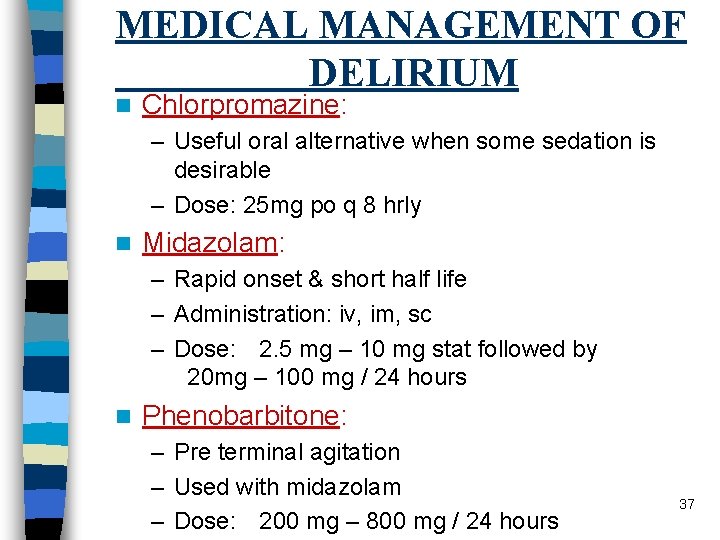
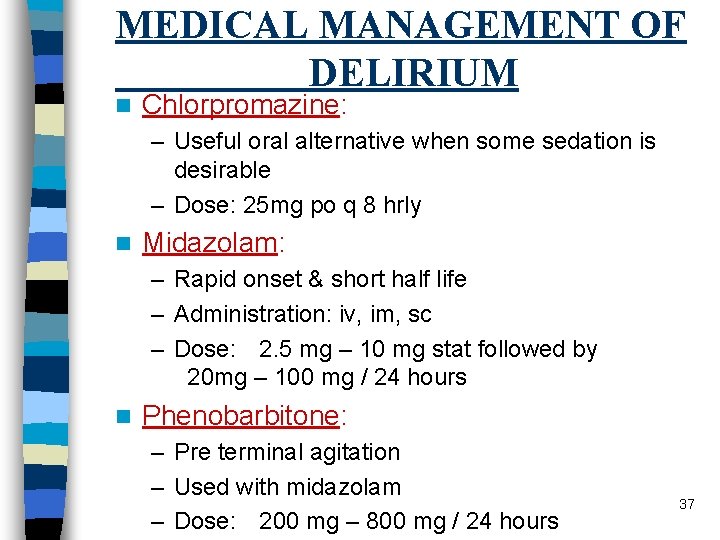
MEDICAL MANAGEMENT OF DELIRIUM n Chlorpromazine: – Useful oral alternative when some sedation is desirable – Dose: 25 mg po q 8 hrly n Midazolam: – Rapid onset & short half life – Administration: iv, im, sc – Dose: 2. 5 mg – 10 mg stat followed by 20 mg – 100 mg / 24 hours n Phenobarbitone: – Pre terminal agitation – Used with midazolam – Dose: 200 mg – 800 mg / 24 hours 37
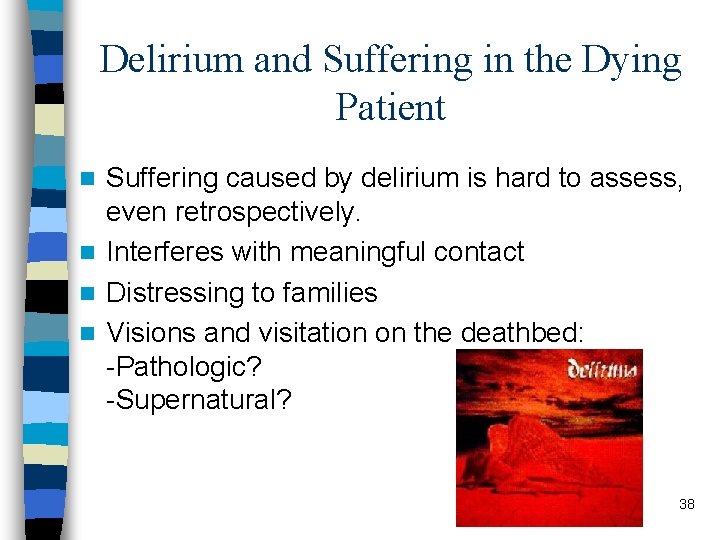
Delirium and Suffering in the Dying Patient Suffering caused by delirium is hard to assess, even retrospectively. n Interferes with meaningful contact n Distressing to families n Visions and visitation on the deathbed: -Pathologic? -Supernatural? n 38
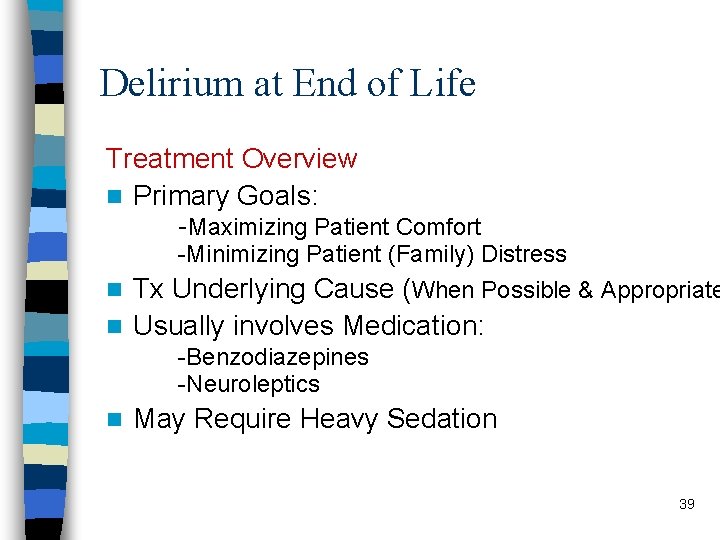
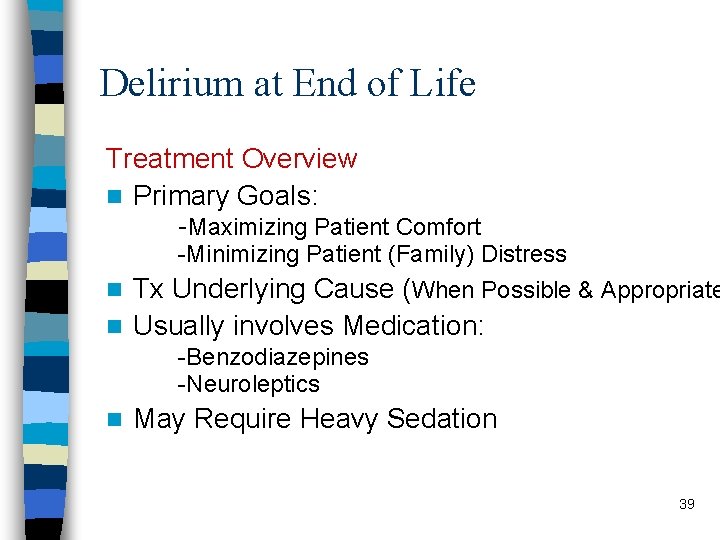
Delirium at End of Life Treatment Overview n Primary Goals: -Maximizing Patient Comfort -Minimizing Patient (Family) Distress Tx Underlying Cause (When Possible & Appropriate n Usually involves Medication: n -Benzodiazepines -Neuroleptics n May Require Heavy Sedation 39
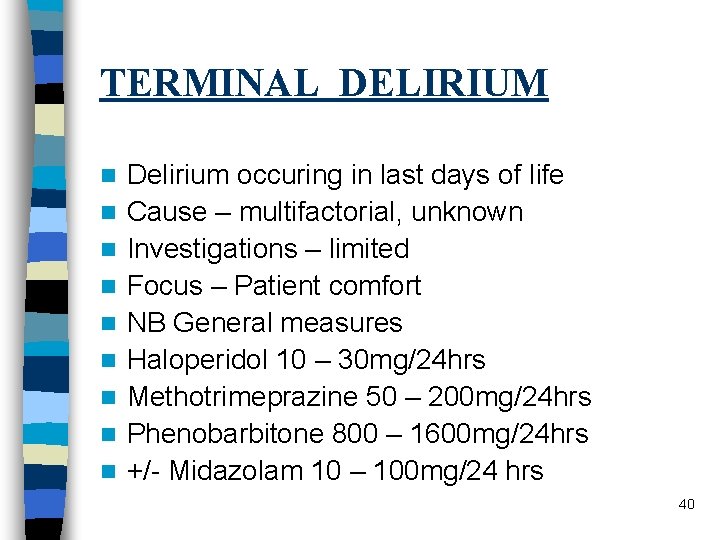
TERMINAL DELIRIUM n n n n n Delirium occuring in last days of life Cause – multifactorial, unknown Investigations – limited Focus – Patient comfort NB General measures Haloperidol 10 – 30 mg/24 hrs Methotrimeprazine 50 – 200 mg/24 hrs Phenobarbitone 800 – 1600 mg/24 hrs +/- Midazolam 10 – 100 mg/24 hrs 40
CONCLUSION n n n Prevention / Minimise Risk Early Diagnosis Early Treatment Careful Systematic Approach Correct Reversible Causes NB General Measures 41
References n Inuoye S. Delirium in Older Persons. NEJM. 2006; 354: 1157 -65 n Centeno C, Sanz A, Bruera E. Delirium in advanced cancer patients. Palliat Med. 2004; 18: 184 -94 n Lawlor P et al. Occurrence, Causes and outcome of delirium in patients with advanced cancer. Arch Intern Med; 160: 786 -94 n Caraceni A, Simonetti F. Palliating delirium in patients with cancer. The Lancet. 2009: 10; 164 -72 n Lonergan E et al. Antipsychotics for delirium. Cochrane Database Syst Rev. 2007 Apr 18; (2): CD 005594
References n Grover S, Matoo SK, Gupta N. Usefulness of atypical antipsychotics and choline esterase inhibitors in delirium: a review. Pharmacopsychiatry. 2011 Mar; 44(2): 43 -54 n Grover S, Kumar V, Chakrabarti S. Comparative efficacy study of haloperidol, olanzapine and risperidone in delirium. J Psychosom Res. 2011. Oct; 71(4): 277 -81 n Delirium: diagnosis, prevention and management. NICE clinical guideline 103.
 Aisling doherty
Aisling doherty Aisling conboy
Aisling conboy Dr aisling gough
Dr aisling gough Aisling treacy
Aisling treacy Aisling enright
Aisling enright Aisling butler
Aisling butler Difference between dementia and delirium
Difference between dementia and delirium Francisco fernandez md
Francisco fernandez md Difference between delirium and dementia table
Difference between delirium and dementia table Pinch me delirium
Pinch me delirium Sindrom delirium akut
Sindrom delirium akut Nash delirium
Nash delirium Terminalt delirium
Terminalt delirium Cam icu escala
Cam icu escala Delirium care pathways
Delirium care pathways Delirium definition
Delirium definition Delirium definition
Delirium definition Excited delirium перевод
Excited delirium перевод Escala rass
Escala rass Delirium case presentation
Delirium case presentation Flocculation delirium
Flocculation delirium Gcs normal
Gcs normal European delirium association
European delirium association Knowledge management consultant
Knowledge management consultant Dr ian smith injury management consultant
Dr ian smith injury management consultant Green world group
Green world group Ovtopodump
Ovtopodump Assertivel
Assertivel Family history consultant training
Family history consultant training Recognition and regard for oneself and one's abilities: *
Recognition and regard for oneself and one's abilities: * Jojy mathew
Jojy mathew Consultant mediu
Consultant mediu Claudia norman a marketing consultant
Claudia norman a marketing consultant Judith james educational consultant
Judith james educational consultant Behavioral genetics consultant
Behavioral genetics consultant Rcem consultant sign off
Rcem consultant sign off Open source consultant
Open source consultant Verizon business solutions consultant
Verizon business solutions consultant United states lactation consultant association
United states lactation consultant association Consultant radiographer
Consultant radiographer Recruiter cold call script
Recruiter cold call script Stuart minty camden planning consultant
Stuart minty camden planning consultant Philips talent acquisition
Philips talent acquisition Nous hospital consultant
Nous hospital consultant